Autoantibodies to PAX5, PTCH1, and GNA11 as Serological Biomarkers in the Detection of Hepatocellular Carcinoma in Hispanic Americans
Abstract
1. Introduction
2. Results
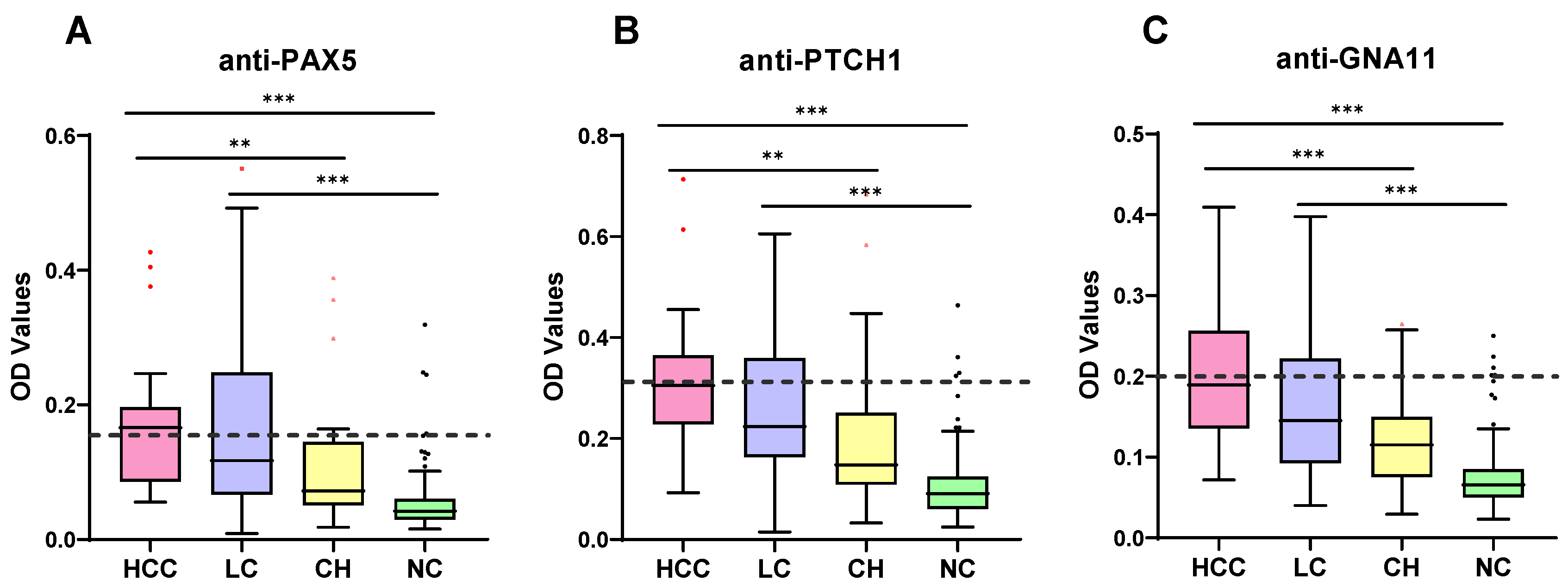
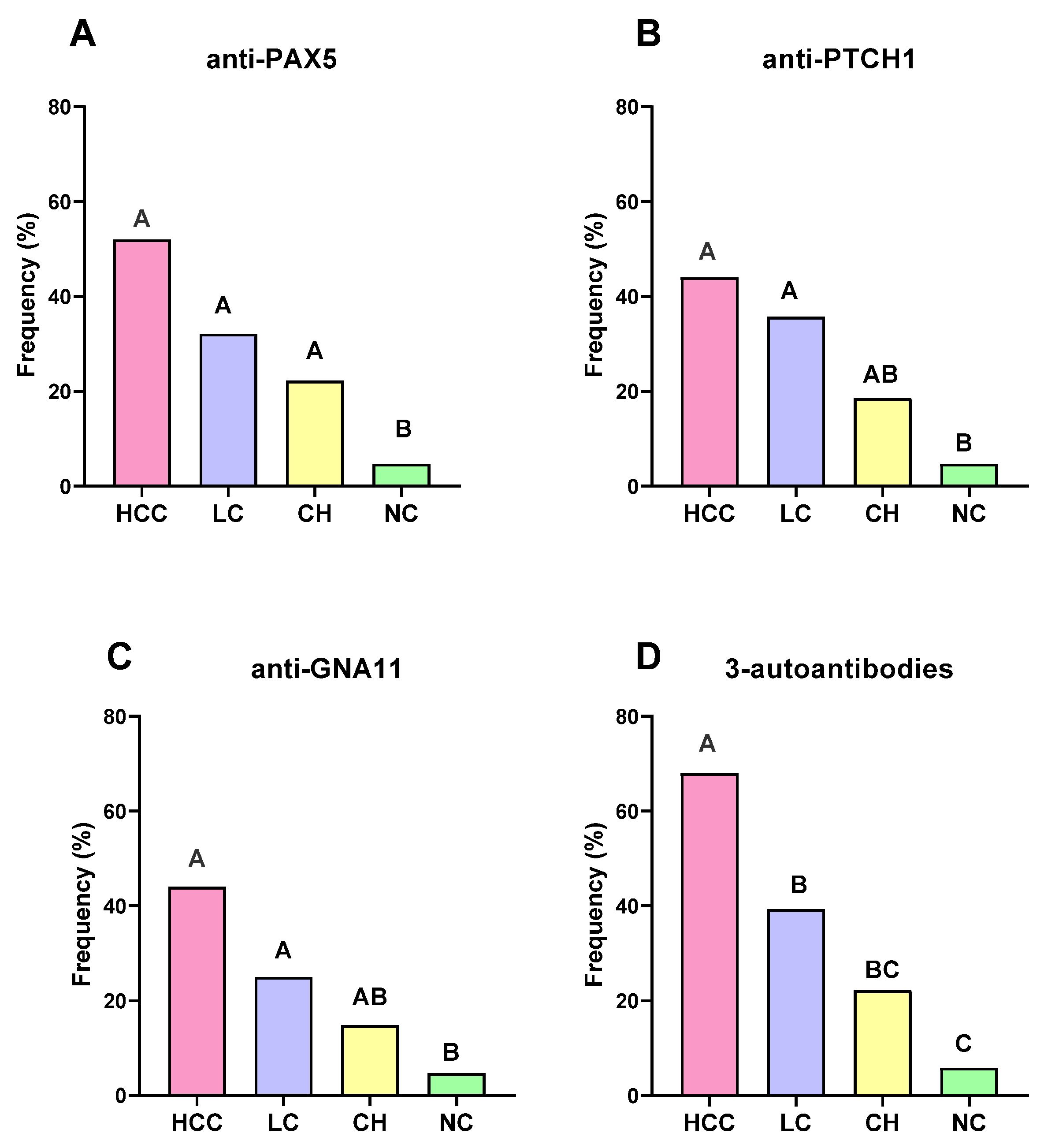
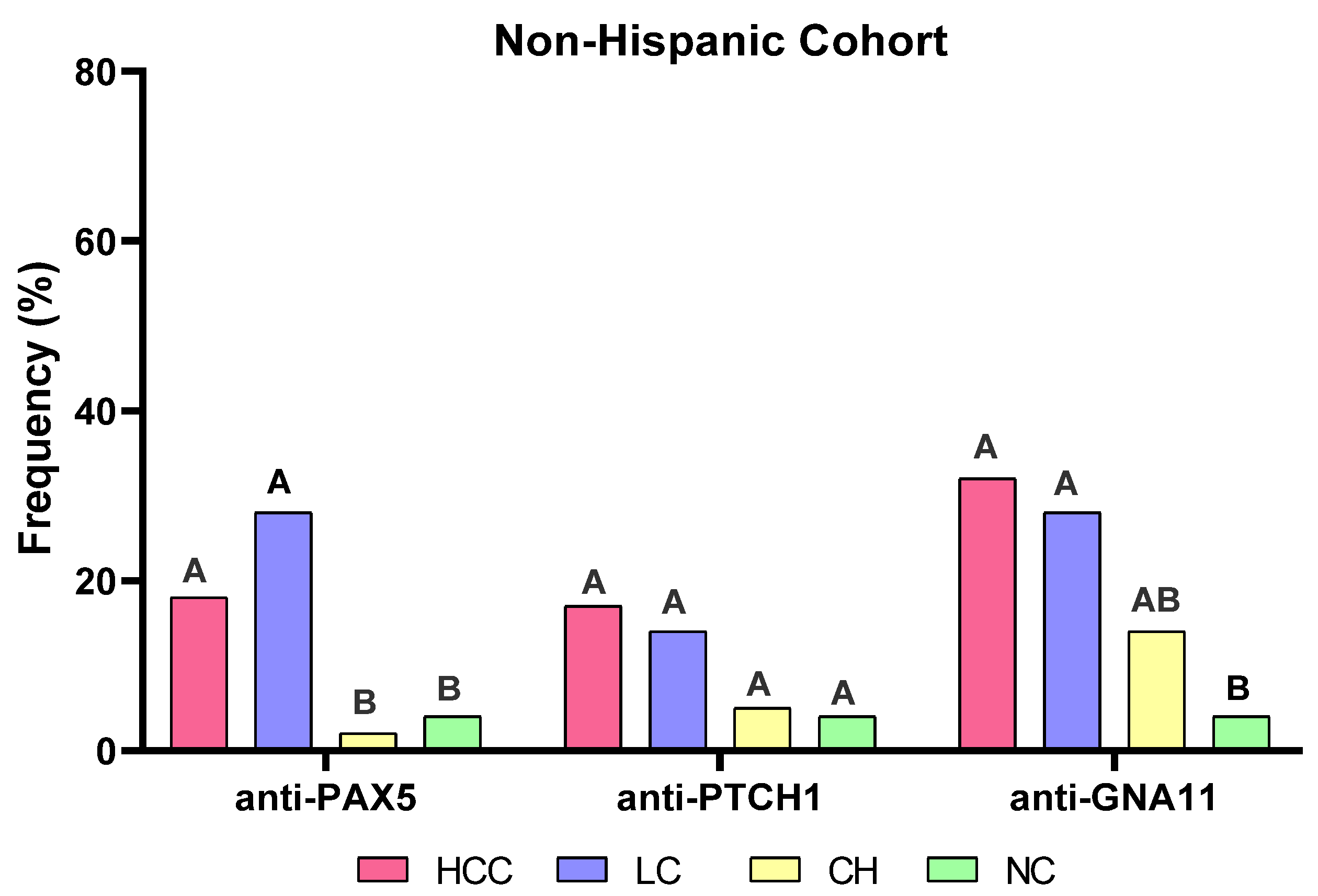
2.1. Expression of Autoantibodies to PAX5, PTCH1, and GNA11 in Different Groups of Subjects
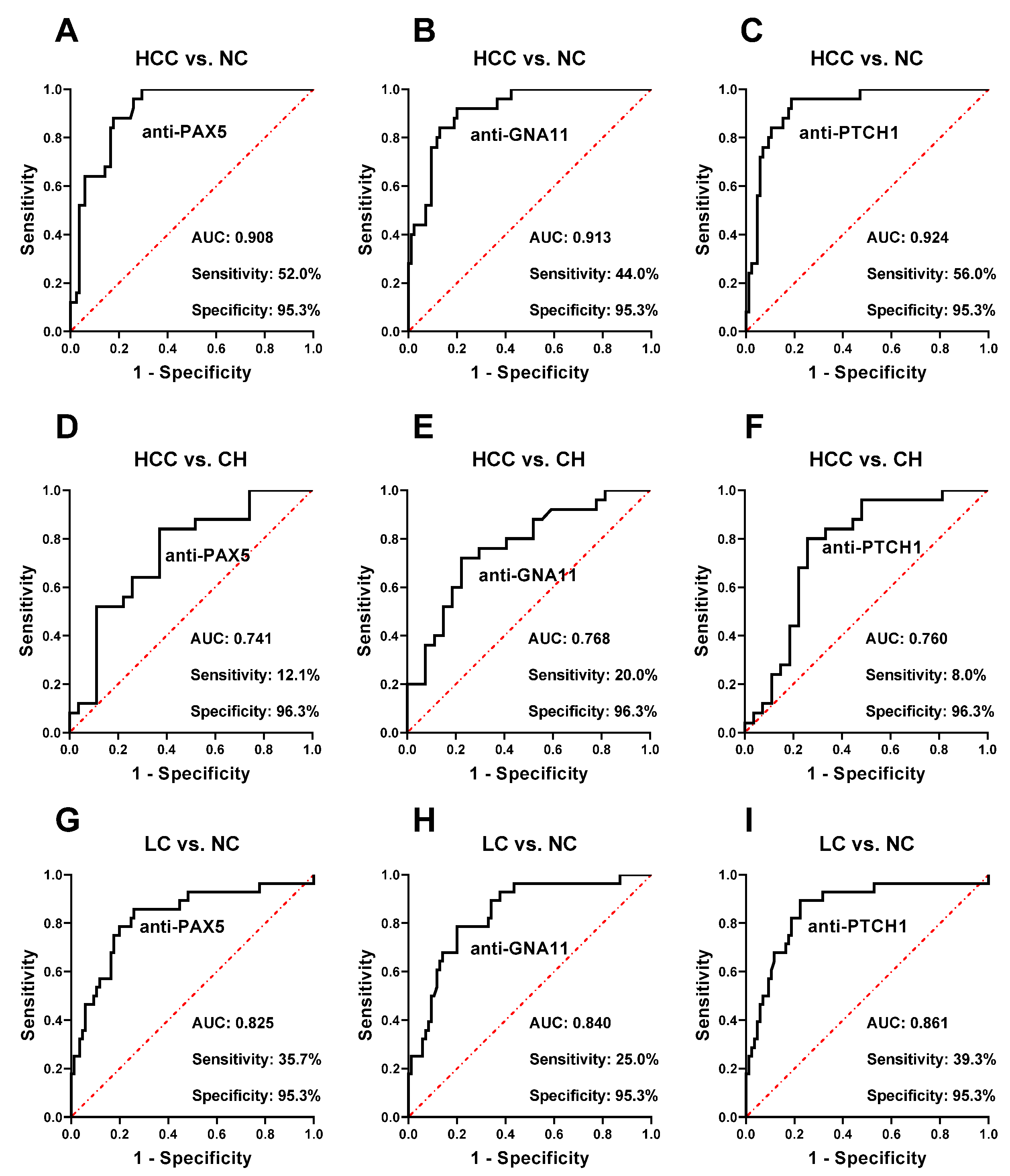
2.2. Performance of Autoantibodies to PAX5, PTCH1, and GNA11 in the Detection of HCC
2.3. Autoantibodies to PAX5, PTCH1, and GNA11 Could Identify LC from NC
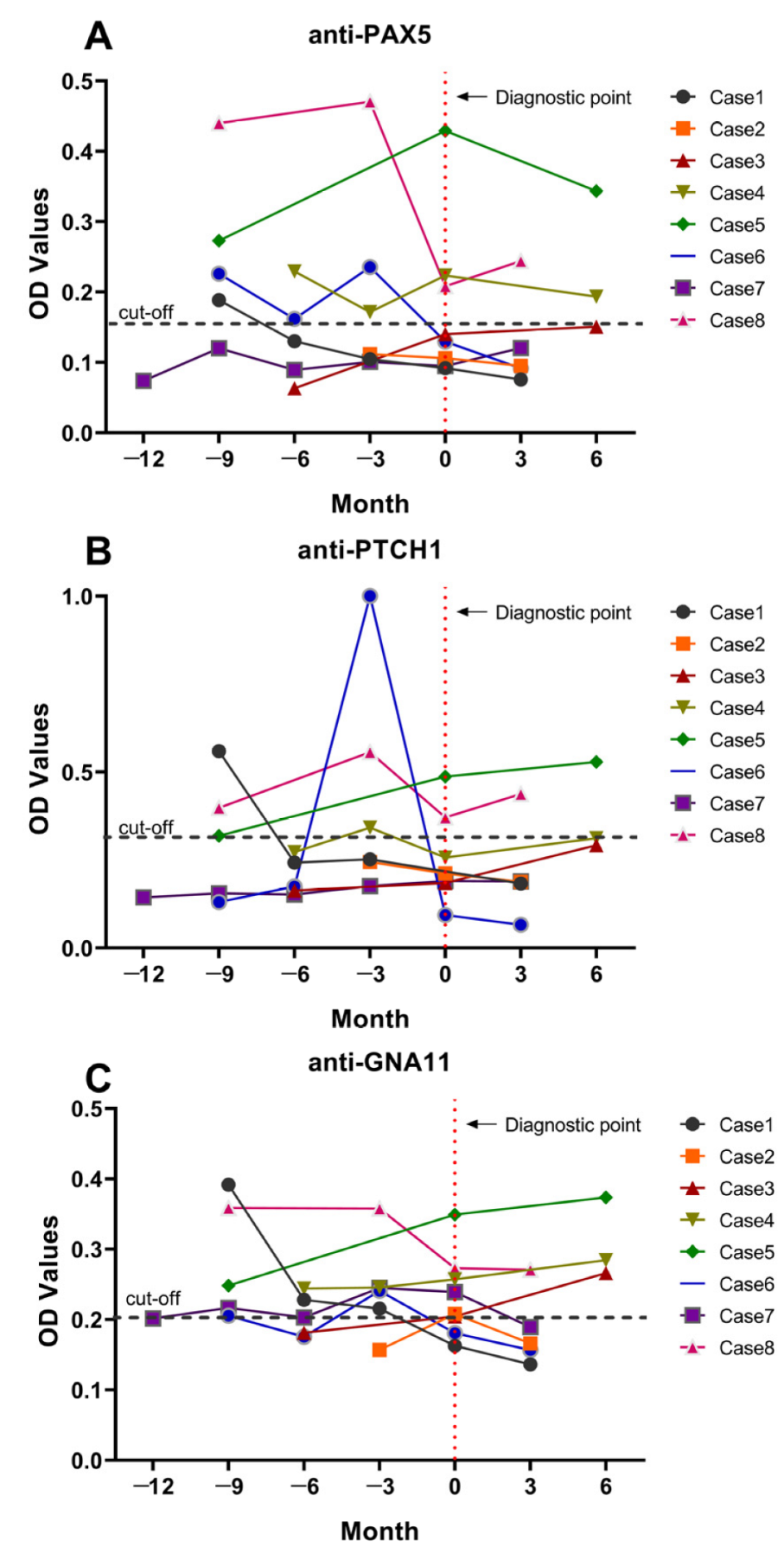
2.4. Autoantibodies to PAX5, PTCH1, and GNA11 Elevated in HCC Patients before Clinical Diagnosis
2.5. Specificity Test of Autoantibodies to PAX5, PTCH1, and GNA11
3. Discussion
4. Materials and Methods
4.1. Study Subjects
4.2. Recombinant Proteins and Enzyme-Linked Immunosorbent Assay (ELISA)
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Venepalli, N.K.; Modayil, M.V.; Berg, S.A.; Nair, T.D.; Parepally, M.; Rajaram, P.; Gaba, R.C.; Bui, J.T.; Huang, Y.; Cotler, S.J. Features of hepatocellular carcinoma in Hispanics differ from African Americans and non-Hispanic Whites. World J. Hepatol. 2017, 9, 391–400. [Google Scholar] [CrossRef]
- Miller, K.D.; Goding Sauer, A.; Ortiz, A.P.; Fedewa, S.A.; Pinheiro, P.S.; Tortolero-Luna, G.; Martinez-Tyson, D.; Jemal, A.; Siegel, R.L. Cancer Statistics for Hispanics/Latinos, 2018. CA: A Cancer J. Clin. 2018, 68, 425–445. [Google Scholar] [CrossRef]
- Bruix, J.; Sherman, M. Practice Guidelines Committee Management of hepatocellular carcinoma. Hepatology 2005, 42, 1208–1236. [Google Scholar] [CrossRef]
- Feldman, A.L.; Dogan, A. Diagnostic uses of Pax5 immunohistochemistry. Adv. Anat. Pathol. 2007, 14, 323–334. [Google Scholar] [CrossRef]
- Shahjahani, M.; Norozi, F.; Ahmadzadeh, A.; Shahrabi, S.; Tavakoli, F.; Asnafi, A.A.; Saki, N. The role of Pax5 in leukemia: Diagnosis and prognosis significance. Med. Oncol. 2015, 32, 360. [Google Scholar] [CrossRef] [PubMed]
- Carotta, S.; Nutt, S.L. Losing B cell identity. BioEssays News Rev. Mol. Cell. Dev. Biol. 2008, 30, 203–207. [Google Scholar] [CrossRef]
- Mullighan, C.G.; Goorha, S.; Radtke, I.; Miller, C.B.; Coustan-Smith, E.; Dalton, J.D.; Girtman, K.; Mathew, S.; Ma, J.; Pounds, S.B.; et al. Genome-wide analysis of genetic alterations in acute lymphoblastic leukaemia. Nature 2007, 446, 758–764. [Google Scholar] [CrossRef] [PubMed]
- Czapiewski, P.; Gorczynski, A.; Radecka, K.; Wiewiora, C.; Haybaeck, J.; Adam, P.; Fend, F.; Zakrzewska, M.; Zakrzewski, K.; Liberski, P.P.; et al. Expression of SOX11, PAX5, TTF-1 and ISL-1 in medulloblastoma. Pathol. Res. Pract. 2016, 212, 965–971. [Google Scholar] [CrossRef]
- Kolhe, R.; Reid, M.D.; Lee, J.R.; Cohen, C.; Ramalingam, P. Immunohistochemical expression of PAX5 and TdT by Merkel cell carcinoma and pulmonary small cell carcinoma: A potential diagnostic pitfall but useful discriminatory marker. Blood 2013, 6, 142–147. [Google Scholar] [CrossRef]
- Fu, Z.; Zuo, C.; Sheehan, C.E.; Patil, D.T.; Lin, J.; Yang, Z.; Lee, H. Novel Finding of Paired Box 5 (PAX5) Cytoplasmic Staining in Well-differentiated Rectal Neuroendocrine Tumors (Carcinoids) and Its Diagnostic and Potentially Prognostic Utility. Appl. Immunohistochem. Mol. Morphol. 2019, 27, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Ainechi, S.; Mann, S.A.; Lin, J.; Patil, D.; Sheehan, C.E.; Yang, Z.; Zuo, C.; Lee, H. Paired Box 5 (PAX5) Expression in Poorly Differentiated Neuroendocrine Carcinoma of the Gastrointestinal and Pancreatobiliary Tract: Diagnostic and Potentially Therapeutic Implications. Appl. Immunohistochem. Mol. Morphol. 2018, 26, 545–551. [Google Scholar] [CrossRef]
- Sullivan, L.M.; Atkins, K.A.; LeGallo, R.D. PAX immunoreactivity identifies alveolar rhabdomyosarcoma. Am. J. Surg. Pathol. 2009, 33, 775–780. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Li, X.; Chu, E.S.; Go, M.Y.; Xu, L.; Zhao, G.; Li, L.; Dai, N.; Si, J.; Tao, Q.; et al. Paired box gene 5 is a novel tumor suppressor in hepatocellular carcinoma through interaction with p53 signaling pathway. Hepatology 2011, 53, 843–853. [Google Scholar] [CrossRef]
- Zhao, G.J.; Xu, L.X.; Chu, E.S.; Zhang, N.; Shen, J.Y.; Damirin, A.; Li, X.X. Establishment of an orthotopic transplantation tumor model of hepatocellular carcinoma in mice. World J. Gastroenterol. 2012, 18, 7087–7092. [Google Scholar] [CrossRef]
- Lo, H.W.; Choi, J.Y.; Lee, Y.S.; Shim, D.M.; Seo, S.W. PTCH1 regulates anchorage-independent growth and bone invasion of non-small cell lung cancer cells. Cells 2021, 144, 115829. [Google Scholar]
- Doheny, D.; Manore, S.G. Hedgehog Signaling and Truncated GLI1 in Cancer. Cells 2020, 9, 2114. [Google Scholar] [CrossRef]
- He, H.C.; Chen, J.H.; Chen, X.B.; Qin, G.Q.; Cai, C.; Liang, Y.X.; Han, Z.D.; Dai, Q.S.; Chen, Y.R.; Zeng, G.H.; et al. Expression of hedgehog pathway components is associated with bladder cancer progression and clinical outcome. Pathol. Oncol. Res. 2012, 18, 349–355. [Google Scholar] [CrossRef]
- You, S.; Zhou, J.; Chen, S.; Zhou, P.; Lv, J.; Han, X.; Sun, Y. PTCH1, a receptor of Hedgehog signaling pathway, is correlated with metastatic potential of colorectal cancer. Upsala J. Med. Sci. 2010, 115, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Qiu, C.; Wang, B.; Wang, P.; Wang, X.; Ma, Y.; Dai, L.; Shi, J.; Wang, K.; Sun, G.; Ye, H.; et al. Identification of novel autoantibody signatures and evaluation of a panel of autoantibodies in breast cancer. Cancer Sci. 2021, 112, 3388–3400. [Google Scholar] [CrossRef]
- Wang, C.-Y.; Chang, Y.-C.; Kuo, Y.-L.; Lee, K.-T.; Chen, P.-S.; Cheung, C.H.A.; Chang, C.-P.; Phan, N.N.; Shen, M.-R.; Hsu, H.-P. Mutation of the PTCH1 gene predicts recurrence of breast cancer. Sci. Rep. 2019, 9, 16359. [Google Scholar] [CrossRef]
- Alvarez-Curto, E.; Inoue, A.; Jenkins, L.; Raihan, S.Z.; Prihandoko, R.; Tobin, A.B.; Milligan, G. Targeted Elimination of G Proteins and Arrestins Defines Their Specific Contributions to Both Intensity and Duration of G Protein-coupled Receptor Signaling. J. Biol. Chem. 2016, 291, 27147–27159. [Google Scholar] [CrossRef]
- Van Raamsdonk, C.D.; Griewank, K.G.; Crosby, M.B.; Garrido, M.C.; Vemula, S.; Wiesner, T.; Obenauf, A.C.; Wackernagel, W.; Green, G.; Bouvier, N.; et al. Mutations in GNA11 in uveal melanoma. N. Engl. J. Med. 2010, 363, 2191–2199. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Azizan, E.A.B. Somatic mutations of GNA11 and GNAQ in CTNNB1-mutant aldosterone-producing adenomas presenting in puberty, pregnancy or menopause. Nat. Genet. 2021, 53, 1360–1372. [Google Scholar] [CrossRef] [PubMed]
- Tsianakas, A.; Böhm, M.R.; Getova, V.; Metze, D.; Eter, N.; Spieker, T.; Bräuninger, A.; Luger, T.; Schiller, M.; Sunderkötter, C. Skin metastases in metastatic uveal melanoma: GNAQ/GNA11 mutational analysis as a valuable tool. Br. J. Dermatol. 2013, 169, 160–163. [Google Scholar] [CrossRef]
- Joseph, N.M.; Brunt, E.M.; Marginean, C.; Nalbantoglu, I.; Snover, D.C.; Thung, S.N.; Yeh, M.M.; Umetsu, S.E.; Ferrell, L.D.; Gill, R.M. Frequent GNAQ and GNA14 Mutations in Hepatic Small Vessel Neoplasm. Am. J. Surg. Pathol. 2018, 42, 1201–1207. [Google Scholar] [CrossRef]
- Wang, H.; Yang, X.; Sun, G.; Yang, Q.; Cui, C.; Wang, X.; Ye, H.; Dai, L.; Shi, J.; Zhang, J.; et al. Identification and Evaluation of Autoantibody to a Novel Tumor-Associated Antigen GNA11 as a Biomarker in Esophageal Squamous Cell Carcinoma. Front. Oncol. 2021, 11, 661043. [Google Scholar] [CrossRef] [PubMed]
- Jiang, D.; Zhang, X.; Liu, M.; Wang, Y.; Wang, T.; Pei, L.; Wang, P.; Ye, H.; Shi, J.; Song, C.; et al. Discovering Panel of Autoantibodies for Early Detection of Lung Cancer Based on Focused Protein Array. Front. Immunol. 2021, 12, 658922. [Google Scholar] [CrossRef]
- Zinkin, N.T.; Grall, F.; Bhaskar, K.; Otu, H.H.; Spentzos, D.; Kalmowitz, B.; Wells, M.; Guerrero, M.; Asara, J.M.; Libermann, T.A.; et al. Serum proteomics and biomarkers in hepatocellular carcinoma and chronic liver disease. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2008, 14, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Paradis, V.; Degos, F.; Dargère, D.; Pham, N.; Belghiti, J.; Degott, C.; Janeau, J.L.; Bezeaud, A.; Delforge, D.; Cubizolles, M.; et al. Identification of a new marker of hepatocellular carcinoma by serum protein profiling of patients with chronic liver diseases. Hepatology 2005, 41, 40–47. [Google Scholar] [CrossRef]
- Zhang, J.; Chan, E.K. Autoantibodies to IGF-II mRNA binding protein p62 and overexpression of p62 in human hepatocellular carcinoma. Autoimmun. Rev. 2002, 1, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Han, K.J.; Pang, X.W.; Vaughan, H.A.; Qu, W.; Dong, X.Y.; Peng, J.R.; Zhao, H.T.; Rui, J.A.; Leng, X.S.; et al. Large scale identification of human hepatocellular carcinoma-associated antigens by autoantibodies. J. Immunol. 2002, 169, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Kim, G.A.; Han, S.; Lee, W.; Chun, S.; Lim, Y.S. Longitudinal Assessment of Three Serum Biomarkers to Detect Very Early-Stage Hepatocellular Carcinoma. Hepatology 2019, 69, 1983–1994. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Liu, Y.; Chen, J.; Shu, H.; Shen, S.; Li, Y.; Lu, X.; Cao, X.; Dong, L.; Shi, J.; et al. Autoantibody signature in hepatocellular carcinoma using seromics. J. Hematol. Oncol. 2020, 13, 85. [Google Scholar] [CrossRef]
- Qiu, C.; Wang, P.; Wang, B.; Shi, J.; Wang, X.; Li, T.; Qin, J.; Dai, L.; Ye, H.; Zhang, J. Establishment and validation of an immunodiagnostic model for prediction of breast cancer. Oncoimmunology 2020, 9, 1682382. [Google Scholar] [CrossRef]
- Wang, K.; Li, M.; Qin, J.; Sun, G.; Dai, L.; Wang, P.; Ye, H.; Shi, J.; Cheng, L.; Yang, Q. Serological biomarkers for early detection of hepatocellular carcinoma: A focus on autoantibodies against tumor-associated antigens encoded by cancer driver genes. Cancers 2020, 12, 1271. [Google Scholar] [CrossRef] [PubMed]
- Konyn, P.; Ahmed, A.; Kim, D. Current epidemiology in hepatocellular carcinoma. Expert Rev. Gastroenterol. Hepatol. 2021, 15, 1295–1307. [Google Scholar] [CrossRef]
- Mokdad, A.H.; Dwyer-Lindgren, L.; Fitzmaurice, C.; Stubbs, R.W.; Bertozzi-Villa, A.; Morozoff, C.; Charara, R.; Allen, C.; Naghavi, M.; Murray, C.J. Trends and patterns of disparities in cancer mortality among US counties, 1980–2014. Jama 2017, 317, 388–406. [Google Scholar] [CrossRef] [PubMed]
- Petrick, J.L.; Kelly, S.P.; Altekruse, S.F.; McGlynn, K.A.; Rosenberg, P.S. Future of hepatocellular carcinoma incidence in the United States forecast through 2030. J. Clin. Oncol. 2016, 34, 1787. [Google Scholar] [CrossRef]
- Raja, A.; Haq, F. Molecular classification of hepatocellular carcinoma: Prognostic importance and clinical applications. J. Cancer Res. Clin. Oncol. 2021, 148, 15–29. [Google Scholar] [CrossRef] [PubMed]
- Goossens, N.; Sun, X.; Hoshida, Y. Molecular classification of hepatocellular carcinoma: Potential therapeutic implications. Hepatic Oncol. 2015, 2, 371–379. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, N.; Friedman, S.L.; Goossens, N.; Hoshida, Y. Risk factors and prevention of hepatocellular carcinoma in the era of precision medicine. J. Hepatol. 2018, 68, 526–549. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.Y.; Tan, E.M. Autoantibodies to tumor-associated antigens as diagnostic biomarkers in hepatocellular carcinoma and other solid tumors. Expert Rev. Mol. Diagn. 2010, 10, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.-Y.; Casiano, C.A.; Peng, X.-X.; Koziol, J.A.; Chan, E.K.; Tan, E.M. Enhancement of antibody detection in cancer using panel of recombinant tumor-associated antigens. Cancer Epidemiol. Biomark. Prev. 2003, 12, 136–143. [Google Scholar]
- Wu, J.; Wang, P.; Han, Z.; Li, T.; Yi, C.; Qiu, C.; Yang, Q.; Sun, G.; Dai, L.; Shi, J. A novel immunodiagnosis panel for hepatocellular carcinoma based on bioinformatics and the autoantibody-antigen system. Cancer Sci. 2022, 113, 411. [Google Scholar] [CrossRef]
- Wang, X.; Wang, K.; Qiu, C.; Wang, B.; Zhang, X.; Ma, Y.; Dai, L.; Zhang, J.-Y. Autoantibody to GNAS in Early Detection of Hepatocellular Carcinoma: A Large-Scale Sample Study Combined with Verification in Serial Sera from HCC Patients. Biomedicines 2022, 10, 97. [Google Scholar] [CrossRef] [PubMed]
- Meistere, I.; Werner, S.; Zayakin, P.; Siliņa, K.; Rulle, U.; Pismennaja, A.; Šantare, D.; Kikuste, I.; Isajevs, S.; Leja, M. The Prevalence of Cancer-Associated Autoantibodies in Patients with Gastric Cancer and Progressive Grades of Premalignant LesionsAutoantibodies in Gastric Cancer and Premalignant Lesions. Cancer Epidemiol. Biomark. Prev. 2017, 26, 1564–1574. [Google Scholar] [CrossRef] [PubMed]
| TAAs | UniProt ID | Full Protein Name | Gene Classification | Core Pathway | Process | Function * |
|---|---|---|---|---|---|---|
| PAX5 | Q02548 | Paired box protein Pax-5 | TSG | Chromatin Modification | Cell Fate | DNA-binding transcription activator activity; DNA-binding transcription factor activity |
| PTCH1 | Q13635 | Protein patched homolog 1 | TSG | HH | Cell Fate | Cholesterol binding, cell differentiation, liver regeneration |
| GNA11 | P29992 | Guanine nucleotide-binding protein subunit alpha-11 | Oncogene | PI3K; RAS; MAPK | Cell Survival | G-protein beta/gamma-subunit complex binding; G-protein-coupled receptor binding; GTP binding |
| Autoantibodies | Se (%) | Sp (%) | FPR (%) | FNR (%) | PPV (%) | NPV (%) | +LR | −LR | YI | Accuracy (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Anti-PAX5 | 52.0 | 95.3 | 4.7 | 48.0 | 76.5 | 87.1 | 11.06 | 0.50 | 0.47 | 85.5 |
| Anti-PAX5 or anti-PTCH1 | 64.0 | 94.1 | 5.9 | 36.0 | 76.2 | 89.9 | 10.85 | 0.38 | 0.58 | 87.3 |
| Anti-PAX5 or anti-PTCH1 or anti-GNA11 | 68.0 | 94.1 | 5.9 | 32.0 | 77.3 | 91.7 | 11.53 | 0.34 | 0.62 | 88.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qiu, C.; Ma, Y.; Wang, B.; Zhang, X.; Wang, X.; Zhang, J.-Y. Autoantibodies to PAX5, PTCH1, and GNA11 as Serological Biomarkers in the Detection of Hepatocellular Carcinoma in Hispanic Americans. Int. J. Mol. Sci. 2023, 24, 3721. https://doi.org/10.3390/ijms24043721
Qiu C, Ma Y, Wang B, Zhang X, Wang X, Zhang J-Y. Autoantibodies to PAX5, PTCH1, and GNA11 as Serological Biomarkers in the Detection of Hepatocellular Carcinoma in Hispanic Americans. International Journal of Molecular Sciences. 2023; 24(4):3721. https://doi.org/10.3390/ijms24043721
Chicago/Turabian StyleQiu, Cuipeng, Yangcheng Ma, Bofei Wang, Xiaojun Zhang, Xiao Wang, and Jian-Ying Zhang. 2023. "Autoantibodies to PAX5, PTCH1, and GNA11 as Serological Biomarkers in the Detection of Hepatocellular Carcinoma in Hispanic Americans" International Journal of Molecular Sciences 24, no. 4: 3721. https://doi.org/10.3390/ijms24043721
APA StyleQiu, C., Ma, Y., Wang, B., Zhang, X., Wang, X., & Zhang, J.-Y. (2023). Autoantibodies to PAX5, PTCH1, and GNA11 as Serological Biomarkers in the Detection of Hepatocellular Carcinoma in Hispanic Americans. International Journal of Molecular Sciences, 24(4), 3721. https://doi.org/10.3390/ijms24043721





