Design, Synthesis, and Biological Evaluation of 3-Substituted-Indolin-2-One Derivatives as Potent Anti-Inflammatory Agents
Abstract
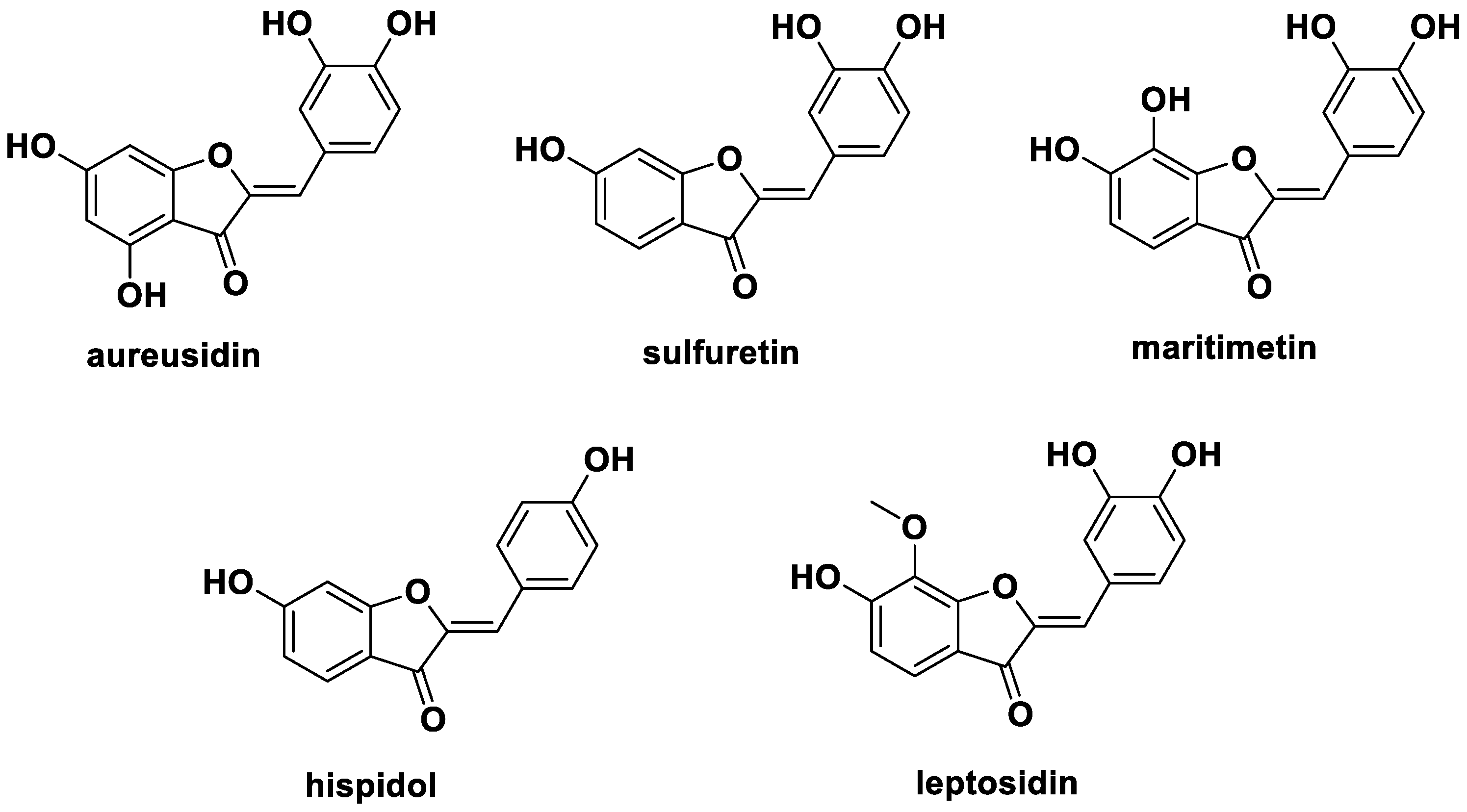
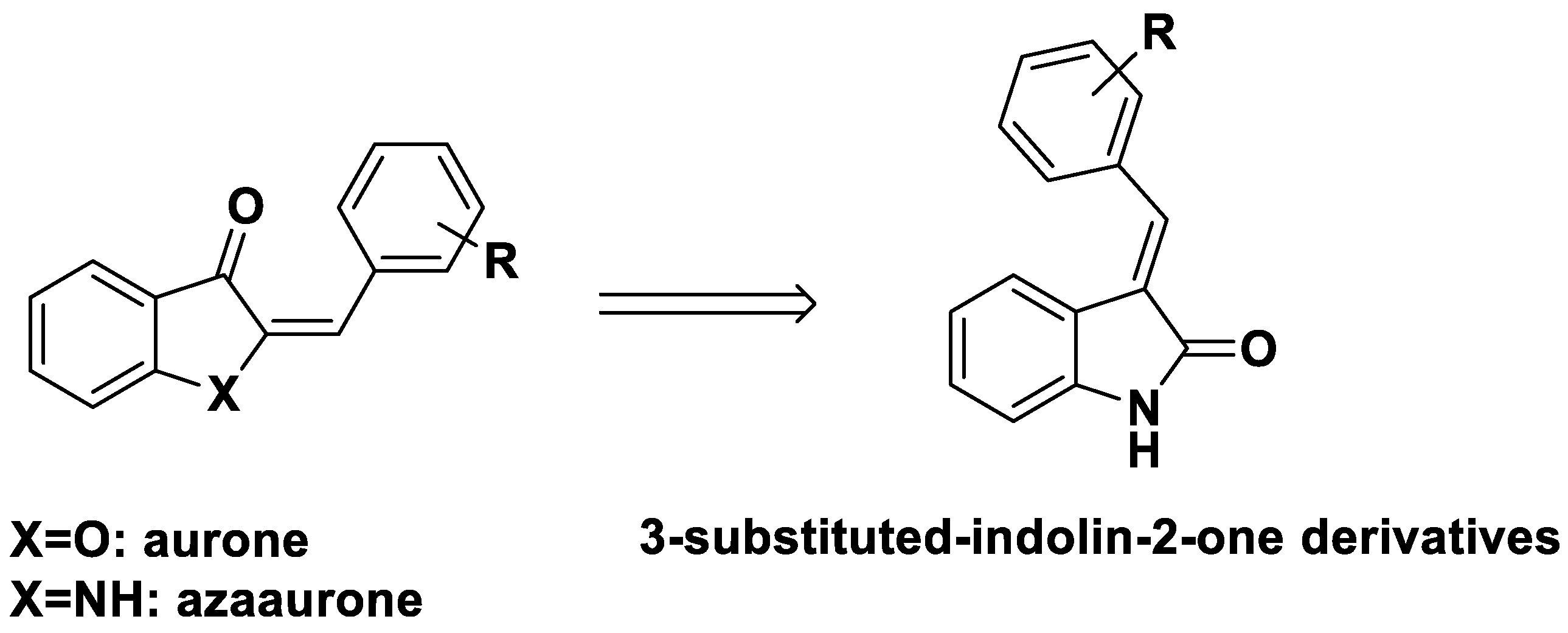
1. Introduction
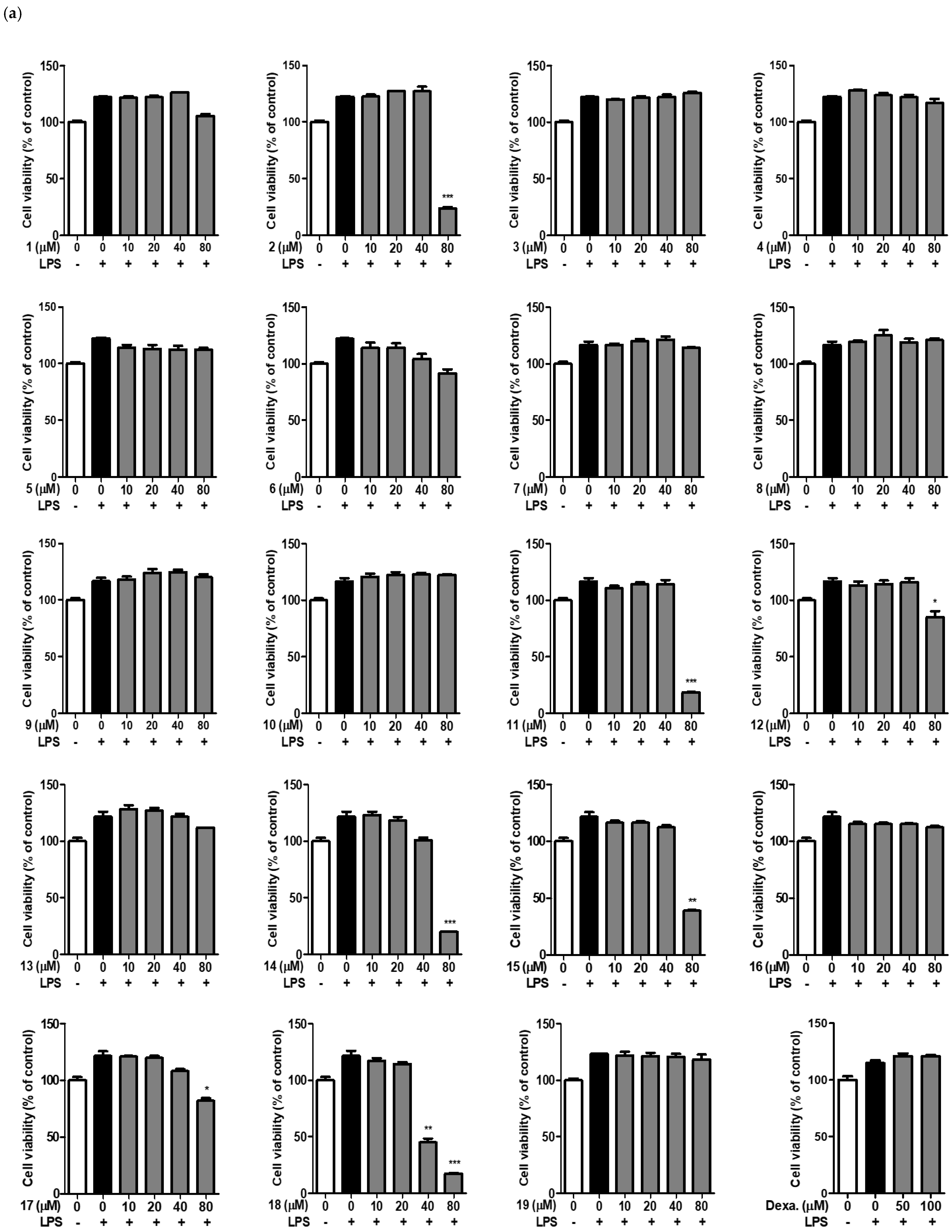
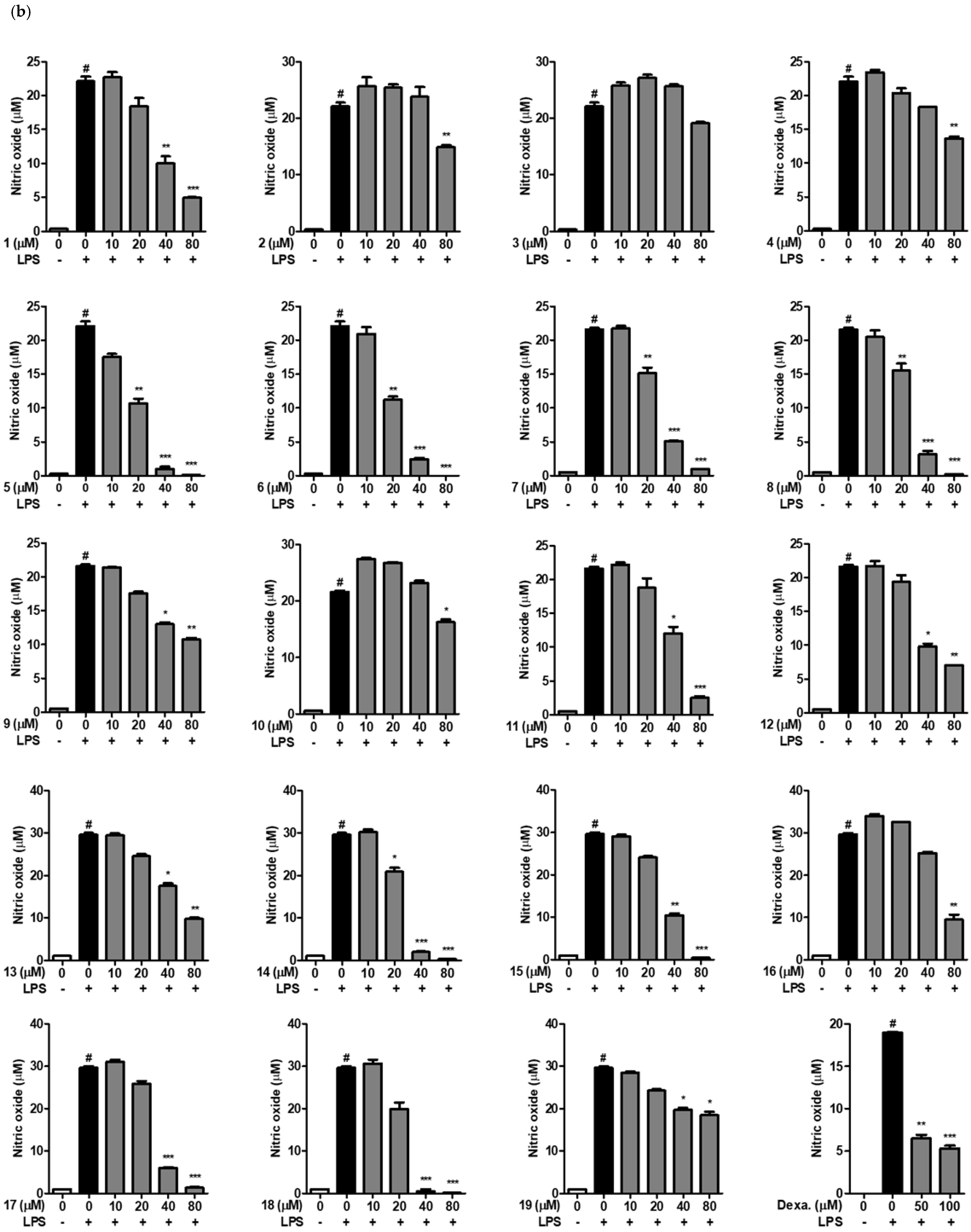
2. Results
2.1. Effects of 3-Substituted-Indolin-2-One Derivatives on Nitric Oxide Secretion in LPS-Stimulated RAW264.7 Cells
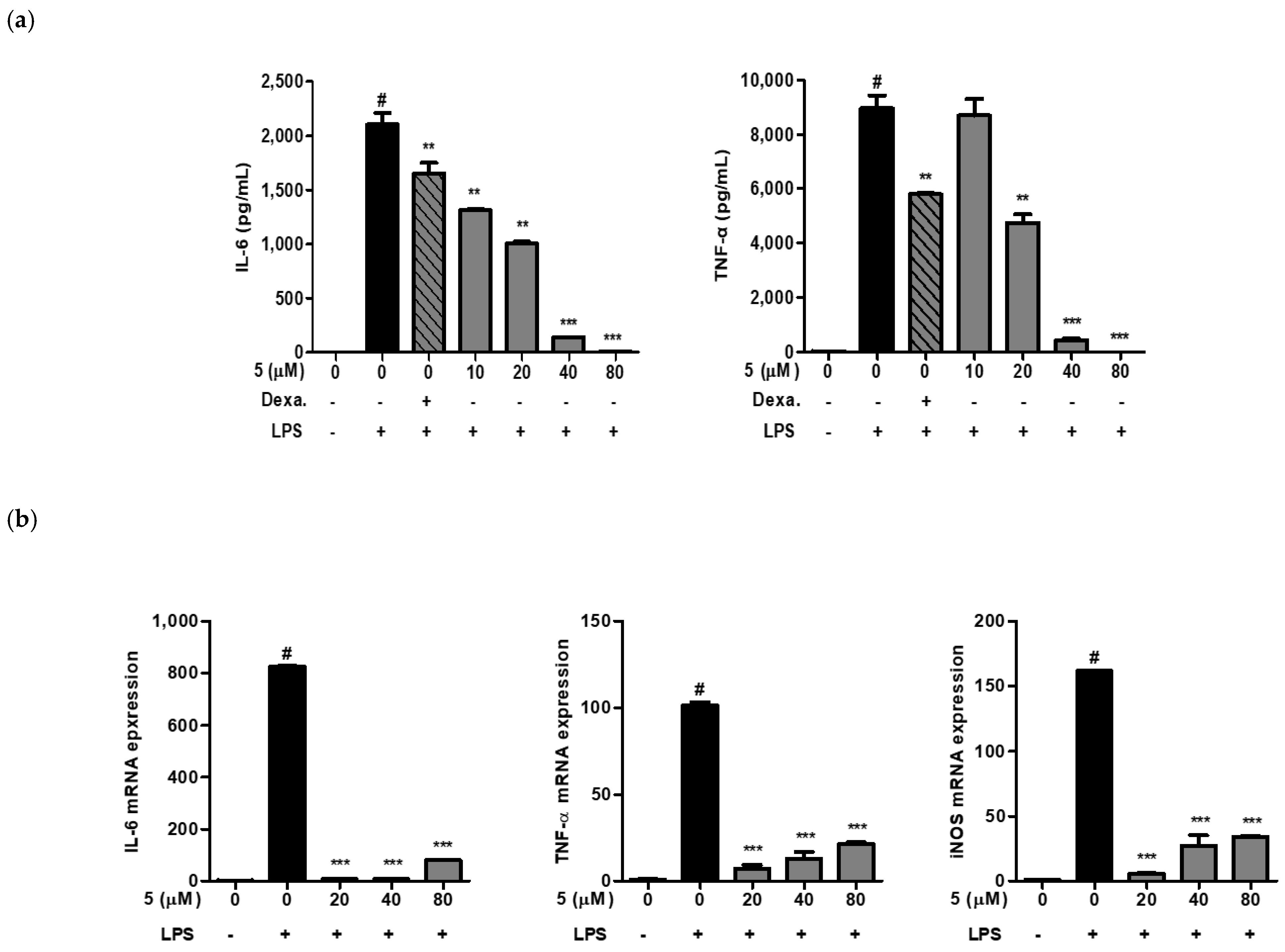
2.2. Effect of 3-(3-Hydroxyphenyl)-Indolin-2-One on IL-6 and TNF-α Production in RAW264.7 Cells
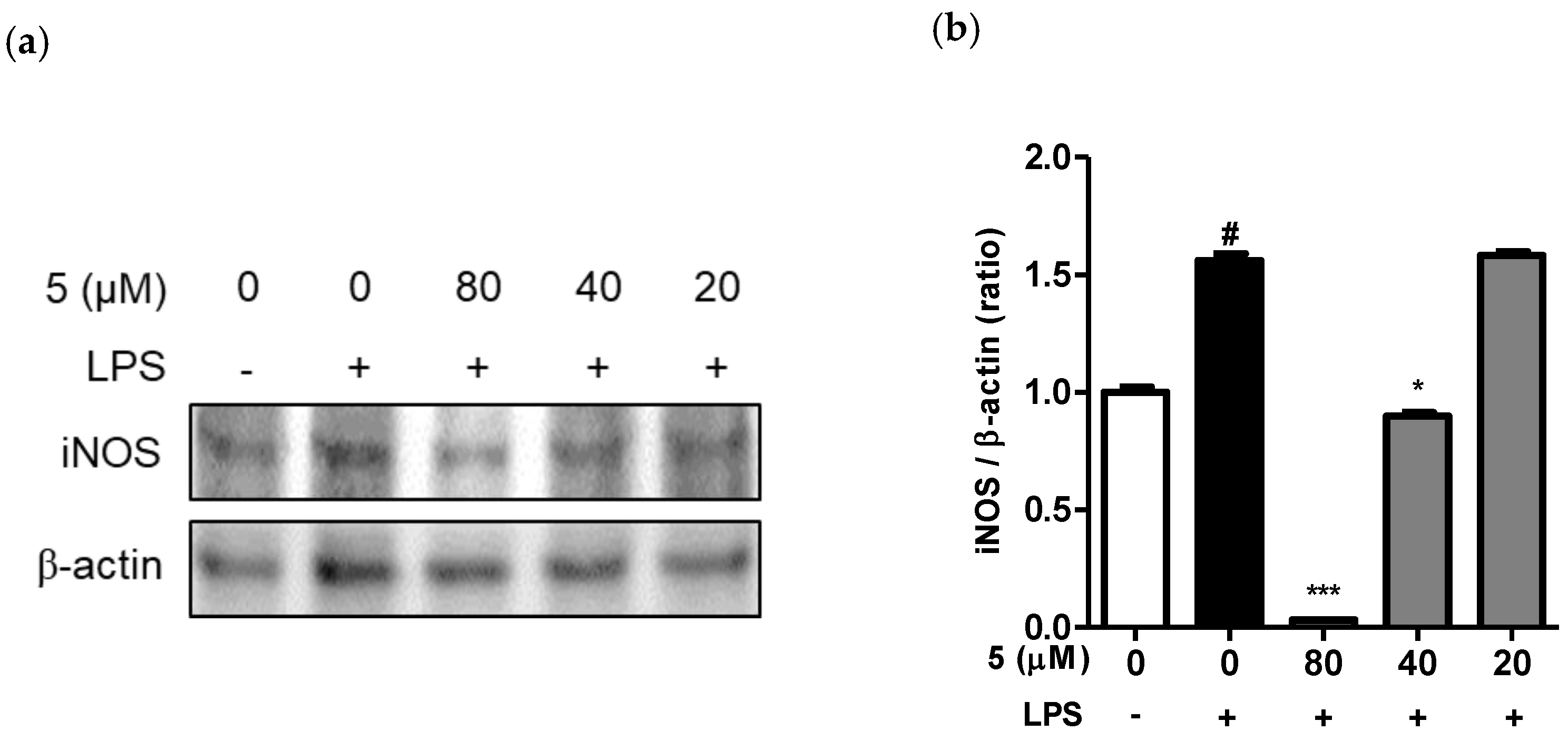
2.3. Effect of 3-(3-Hydroxyphenyl)-Indolin-2-One on iNOS Expression in LPS-Induced RAW264.7 Cells
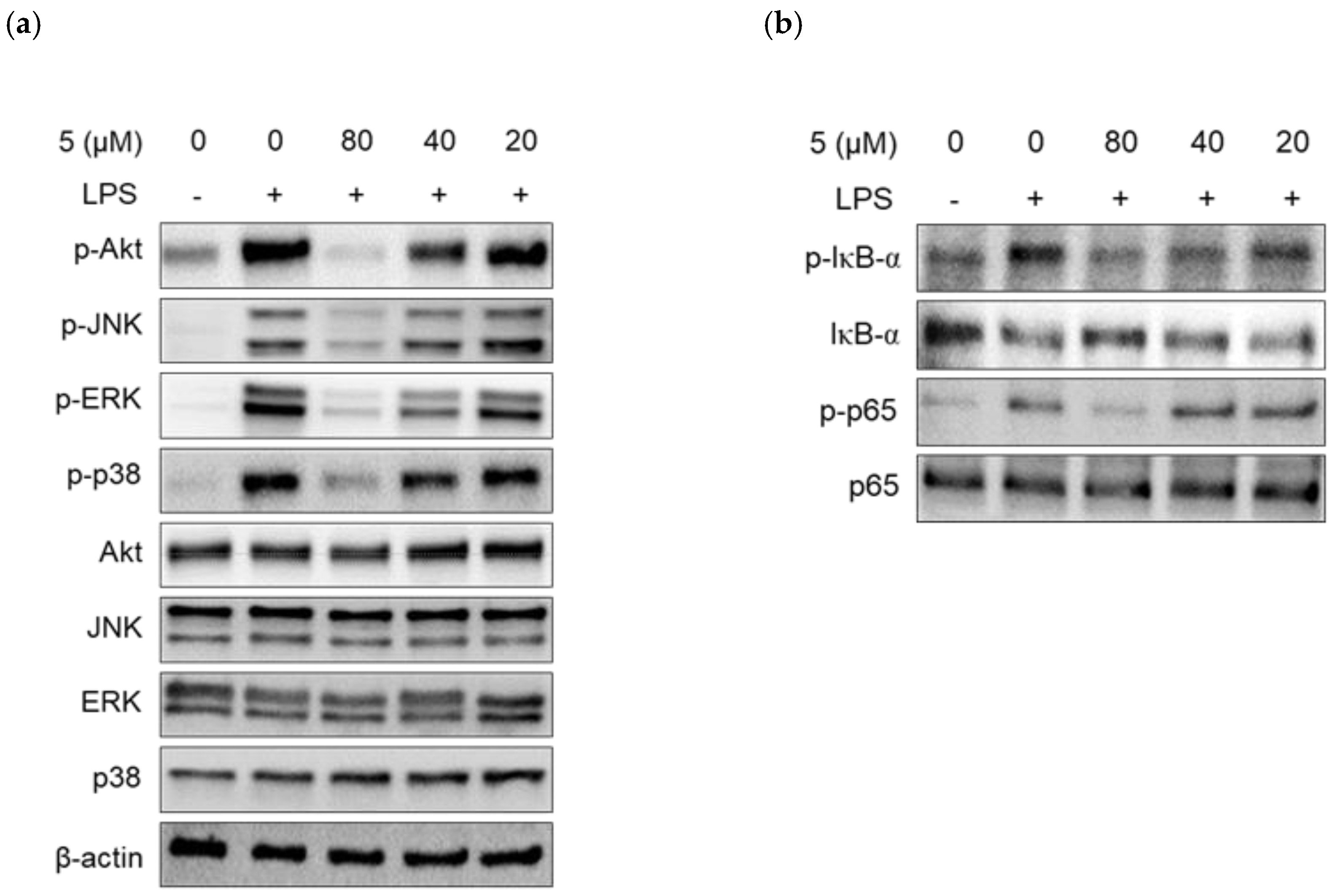
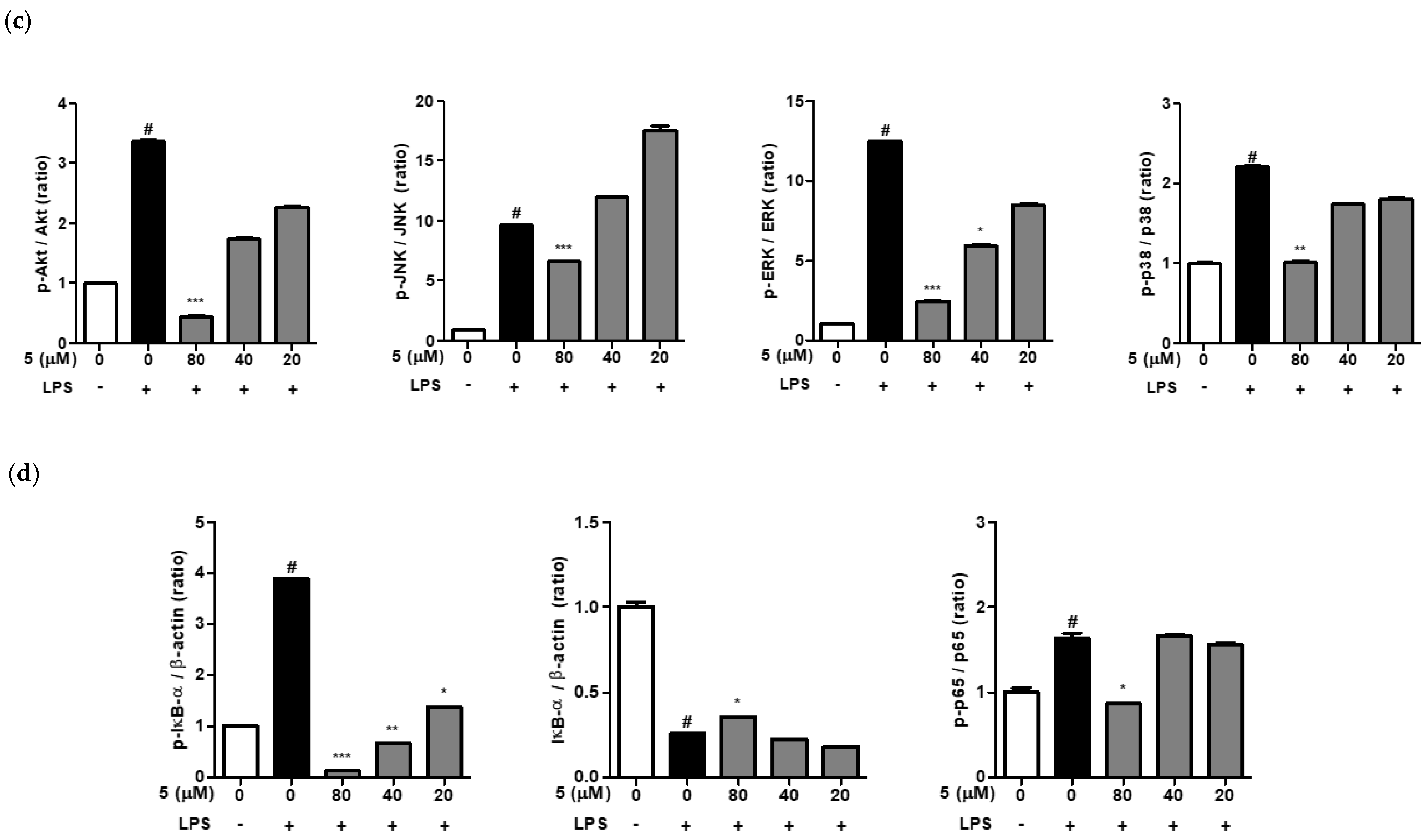
2.4. Effect of 3-(3-Hydroxyphenyl)-Indolin-2-One on Protein Kinase B (Akt), MAPKs, and NF-κB Phosphorylation in LPS-Induced RAW264.7 Cells
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Antibodies and Reagents
5.2. Cell Culture
5.3. Cell Viability
5.4. Determination of Nitric Oxide (NO)
5.5. Determination of Cytokines TNF-α and IL-6
5.6. Preparation of Cell Lysate and Immunoblotting
5.7. Quantitative Real-Time Reverse Transcription Polymerase Chain Reaction (qRT-PCR)
5.8. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Furman, D.; Campisi, J.; Verdin, E.; Carrera-Bastos, P.; Targ, S.; Franceschi, C.; Ferrucci, L.; Gilroy, D.W.; Fasano, A.; Miller, G.W. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 2019, 25, 1822–1832. [Google Scholar] [CrossRef] [PubMed]
- Netea, M.G.; Balkwill, F.; Chonchol, M.; Cominelli, F.; Donath, M.Y.; Giamarellos-Bourboulis, E.J.; Golenbock, D.; Gresnigt, M.S.; Heneka, M.T.; Hoffman, H.M. A guiding map for inflammation. Nat. Immunol. 2017, 18, 826–831. [Google Scholar] [CrossRef] [PubMed]
- Kotas, M.E.; Medzhitov, R. Homeostasis, inflammation, and disease susceptibility. Cell 2015, 160, 816–827. [Google Scholar] [CrossRef] [PubMed]
- Schett, G.; Neurath, M.F. Resolution of chronic inflammatory disease: Universal and tissue-specific concepts. Nat. Commun. 2018, 9, 3261. [Google Scholar] [CrossRef]
- Schett, G.; Elewaut, D.; McInnes, I.B.; Dayer, J.-M.; Neurath, M.F. How cytokine networks fuel inflammation: Toward a cytokine-based disease taxonomy. Nat. Med. 2013, 19, 822–824. [Google Scholar] [CrossRef] [PubMed]
- McInnes, I.B.; Schett, G. Pathogenetic insights from the treatment of rheumatoid arthritis. Lancet 2017, 389, 2328–2337. [Google Scholar] [CrossRef]
- Nielsen, O.H.; Ainsworth, M.A. Tumor necrosis factor inhibitors for inflammatory bowel disease. N. Engl. J. Med. 2013, 369, 754–762. [Google Scholar] [CrossRef]
- Nathan, C.; Ding, A. Nonresolving inflammation. Cell 2010, 140, 871–882. [Google Scholar] [CrossRef]
- Lee, C.-H.; Choi, E.Y. Macrophages and inflammation. Int. J. Rheum. Dis. 2018, 25, 11–18. [Google Scholar] [CrossRef]
- Chen, C.-C.; Lin, M.-W.; Liang, C.-J.; Wang, S.-H. The anti-inflammatory effects and mechanisms of eupafolin in lipopolysaccharide-induced inflammatory responses in RAW264. 7 macrophages. PLoS ONE 2016, 11, e0158662. [Google Scholar]
- Maldonado, R.F.; Sá-Correia, I.; Valvano, M.A. Lipopolysaccharide modification in Gram-negative bacteria during chronic infection. FEMS Microbiol. Rev. 2016, 40, 480–493. [Google Scholar] [CrossRef] [PubMed]
- Boumendjel, A. [General Articles] Aurones: A subclass of flavones with promising biological potential. Curr. Med. Chem. 2003, 10, 2621–2630. [Google Scholar] [CrossRef] [PubMed]
- Mazziotti, I.; Petrarolo, G.; La Motta, C. Aurones: A Golden Resource for Active Compounds. Molecules 2021, 27, 2. [Google Scholar] [CrossRef]
- Nakayama, T.; Yonekura-Sakakibara, K.; Sato, T.; Kikuchi, S.; Fukui, Y.; Fukuchi-Mizutani, M.; Ueda, T.; Nakao, M.; Tanaka, Y.; Kusumi, T. Aureusidin synthase: A polyphenol oxidase homolog responsible for flower coloration. Science 2000, 290, 1163–1166. [Google Scholar] [CrossRef] [PubMed]
- Ono, E.; Fukuchi-Mizutani, M.; Nakamura, N.; Fukui, Y.; Yonekura-Sakakibara, K.; Yamaguchi, M.; Nakayama, T.; Tanaka, T.; Kusumi, T.; Tanaka, Y. Yellow flowers generated by expression of the aurone biosynthetic pathway. Proc. Natl. Acad. Sci. USA 2006, 103, 11075–11080. [Google Scholar] [CrossRef]
- Yang, Y.; Han, C.; Sheng, Y.; Wang, J.; Zhou, X.; Li, W.; Guo, L.; Ruan, S. Corrigendum: The Mechanism of Aureusidin in Suppressing Inflammatory Response in Acute Liver Injury by Regulating MD2. Front. Pharmacol. 2021, 12, 802304. [Google Scholar] [CrossRef]
- Lee, Y.-R.; Hwang, J.-K.; Koh, H.-W.; Jang, K.Y.; Lee, J.H.; Park, J.-W.; Park, B.-H. Sulfuretin, a major flavonoid isolated from Rhus verniciflua, ameliorates experimental arthritis in mice. Life Sci. 2012, 90, 799–807. [Google Scholar] [CrossRef]
- Sun, X.; Jiang, X.; Li, X.; Qi, Z.; Lu, Y. Sulfuretin exerts anti-depressive effects in the lipopolysaccharide-induced depressive mouse models. Physiol. Behav. 2022, 250, 113800. [Google Scholar] [CrossRef]
- Johnson, B.D.; Kaulagari, S.R.; Chen, W.-C.; Hayes, K.; Geldenhuys, W.J.; Hazlehurst, L.A. Identification of Natural Product Sulfuretin Derivatives as Inhibitors for the Endoplasmic Reticulum Redox Protein ERO1α. ACS Bio Med Chem Au 2022, 2, 161–170. [Google Scholar] [CrossRef]
- Wang, W.; Chen, W.; Yang, Y.; Liu, T.; Yang, H.; Xin, Z. New phenolic compounds from Coreopsis tinctoria Nutt. and their antioxidant and angiotensin I-converting enzyme inhibitory activities. J. Agric. Food Chem. 2015, 63, 200–207. [Google Scholar] [CrossRef]
- Begmatov, N.; Li, J.; Bobakulov, K.; Numonov, S.; Aisa, H.A. The chemical components of Coreopsis tinctoria Nutt. and their antioxidant, antidiabetic and antibacterial activities. Nat. Prod. Res. 2020, 34, 1772–1776. [Google Scholar] [CrossRef] [PubMed]
- Alsayari, A.; Muhsinah, A.B.; Hassan, M.Z.; Ahsan, M.J.; Alshehri, J.A.; Begum, N. Aurone: A biologically attractive scaffold as anticancer agent. Eur. J. Med. Chem. 2019, 166, 417–431. [Google Scholar] [CrossRef] [PubMed]
- Priyadarshani, G.; Nayak, A.; Amrutkar, S.M.; Das, S.; Guchhait, S.K.; Kundu, C.N.; Banerjee, U.C. Scaffold-Hopping of aurones: 2-arylideneimidazo [1,2-a] pyridinones as topoisomerase IIα-inhibiting anticancer agents. ACS Med. Chem. Lett. 2016, 7, 1056–1061. [Google Scholar] [CrossRef] [PubMed]
- Carrasco, M.P.; Newton, A.S.; Gonçalves, L.; Góis, A.; Machado, M.; Gut, J.; Nogueira, F.; Hänscheid, T.; Guedes, R.C.; dos Santos, D.J. Probing the aurone scaffold against Plasmodium falciparum: Design, synthesis and antimalarial activity. Eur. J. Med. Chem. 2014, 80, 523–534. [Google Scholar] [CrossRef]
- Roussaki, M.; Costa Lima, S.; Kypreou, A.-M.; Kefalas, P.; Cordeiro da Silva, A.; Detsi, A. Aurones: A promising heterocyclic scaffold for the development of potent antileishmanial agents. Int. J. Med. Chem. 2012, 2012, 196921. [Google Scholar] [CrossRef]
- Kayser, O.; Kiderlen, A.; Folkens, U.; Kolodziej, H. In vitro leishmanicidal activity of aurones. Planta Med. 1999, 65, 316–319. [Google Scholar] [CrossRef]
- Olleik, H.; Yahiaoui, S.; Roulier, B.; Courvoisier-Dezord, E.; Perrier, J.; Pérès, B.; Hijazi, A.; Baydoun, E.; Raymond, J.; Boumendjel, A. Aurone derivatives as promising antibacterial agents against resistant Gram-positive pathogens. Eur. J. Med. Chem. 2019, 165, 133–141. [Google Scholar] [CrossRef]
- Sui, G.; Li, T.; Zhang, B.; Wang, R.; Hao, H.; Zhou, W. Recent advances on synthesis and biological activities of aurones. Biorg. Med. Chem. 2021, 29, 115895. [Google Scholar] [CrossRef]
- Sutton, C.L.; Taylor, Z.E.; Farone, M.B.; Handy, S.T. Antifungal activity of substituted aurones. Bioorg. Med. Chem. Lett. 2017, 27, 901–903. [Google Scholar] [CrossRef]
- Alqahtani, F.M.; Arivett, B.A.; Taylor, Z.E.; Handy, S.T.; Farone, A.L.; Farone, M.B. Chemogenomic profiling to understand the antifungal action of a bioactive aurone compound. PLoS ONE 2019, 14, e0226068. [Google Scholar] [CrossRef]
- Bandgar, B.P.; Patil, S.A.; Korbad, B.L.; Biradar, S.C.; Nile, S.N.; Khobragade, C.N. Synthesis and biological evaluation of a novel series of 2, 2-bisaminomethylated aurone analogues as anti-inflammatory and antimicrobial agents. Eur. J. Med. Chem. 2010, 45, 3223–3227. [Google Scholar] [CrossRef] [PubMed]
- Souard, F.; Okambi, S.; Beney, C.; Chevalley, S.; Valentin, A.; Bpoumendiel, A. 1-Azaaurones derived from the naturally occurring aurones as potential antimalarial drugs. Bioorg. Med. Chem. Lett. 2010, 18, 5724–5731. [Google Scholar] [CrossRef] [PubMed]
- Toth, S.; Szepesi, A.; Tran-Nguyen, V.-K.; Sarkadi, B.; Nemet, K.; Falson, P.; Di Pietro, A.; Szakacs, G.; Boumendel, A. Synthesis and anticancer cytotoxicity of azaaurones overcoming multidrug resistance. Molecules 2020, 25, 764. [Google Scholar] [CrossRef] [PubMed]
- Roulier, B.; Rush, I.; Lazinski, L.M.; Peres, B.; Olleik, H.; Royal, G.; Fishman, A.; Maresca, M.; Haudecoeu, R. Resorcinol-based hemiindigoid derivatives as human tyrosinase inhibitors and melanogenesis suppressors in human melanoma cells. Eur. J. Med. Chem. 2023, 246, 114972. [Google Scholar] [CrossRef] [PubMed]
- Lazinski, L.M.; Royal, G.; Robin, M.; Maresca, M.; Haudecoeur, R. Bioactive Aurones, Indanones, and Other Hemiindigoid Scaffolds: Medicinal Chemistry and Photopharmacology Perspectives. J. Med. Chem. 2022, 65, 12594–125625. [Google Scholar] [CrossRef]
- Carrasco, M.P.; Machado, M.; Goncalves, L.; Sharma, M.; Gut, J.; Lukens, A.K.; Wirth, D.F.; Andre, V.; Duarte, M.T.; Guedes, R.C.; et al. Probing the Azaaurone Scaffold against the Hepatic and Erythrocytic Stages of Malaria Parasites. ChemMedChem 2016, 11, 2194–2204. [Google Scholar] [CrossRef]
- Lai, Y.; Ma, L.; Huang, W.; Yu, X.; Zhang, Y.; Ji, H.; Tian, J. Synthesis and biological evaluation of 3-[4-(amino/methylsulfonyl)phenyl]methylene-indolin-2-one derivatives as novel COX-1/2 and 5-LOX inhibitors. Bioorg. Med. Chem. Lett. 2010, 20, 7349–7353. [Google Scholar] [CrossRef]
- Sun, L.; Tran, N.; Tang, F.; App, H.; Hirth, P.; McMahon, G.; Tang, C. Synthesis and Biological Evaluations of 3-Substituted Indolin-2-ones: A Novel Class of Tyrosine Kinase Inhibitors That Exhibit Selectivity toward Particular Receptor Tyrosine Kinases. J. Med. Chem. 1998, 41, 2588–2603. [Google Scholar] [CrossRef]
- Lee, S.-T. Induction of Nitric Oxide and TNF-alpha by Herbal Plant Extracts in Mouse Macrophages. J. Korean Soc. Food Sci. Nutr. 2000, 29, 342–348. [Google Scholar]
- Kim, J.W. NSAID-induced gastroenteropathy. Korean J. Gastroenterol. 2008, 52, 134–141. [Google Scholar]
- Cho, J.; Lee, E.; Shin, W.G. Evaluation of NSAID usage and appropriateness for prevention of NSAID-related ulcer complications. Korean J. Clin. Pharm. 2012, 22, 211–219. [Google Scholar]
- Cho, Y.; Moon, S.; Park, K.; Cho, N.; Song, Y. Comparison of Side Effect of Non-Steroidal Antiinflammatory Drugs (NSAIDs) in Rhumatoid Arthritis Patients. J. Korean Soc. Health-Syst. Pharm. 1998, 15, 186–192. [Google Scholar]
- Shin, M.-S.; Kim, S.-B.; Lee, J.; Choi, H.-S.; Park, J.; Park, J.Y.; Lee, S.; Hwang, G.S.; Koo, B.A.; Kang, K.S. Beneficial effect of herbal formulation KM1608 on inflammatory bowl diseases: A preliminary experimental study. Molecules 2018, 23, 2068. [Google Scholar] [CrossRef] [PubMed]
- Shin, M.-S.; Park, J.Y.; Lee, J.; Yoo, H.H.; Hahm, D.-H.; Lee, S.C.; Lee, S.; Hwang, G.S.; Jung, K.; Kang, K.S. Anti-inflammatory effects and corresponding mechanisms of cirsimaritin extracted from Cirsium japonicum var. maackii Maxim. Bioorg. Med. Chem. Lett. 2017, 27, 3076–3080. [Google Scholar] [CrossRef] [PubMed]
- Byun, S.-H.; Yang, C.-H.; Kim, S.-C. Inhibitory effect of Scrophulariae Radix extract on TNF-α, IL-1β, IL-6 and nitric oxide production in lipopolysaccharide-activated Raw 264.7 cells. Korean J. Herbol. 2005, 20, 7–16. [Google Scholar]
- Kindt, T.; Goldsby, R.; Osborne, B. Hypersensitivity Reactions. Kuby–Immunology; Kindt, T.J., Goldsby, R.A., Osborne, B.A., Eds.; WH Freeman & Co., Ltd.: New York, NY, USA, 2007; pp. 371–400. [Google Scholar]
- Carter, A.B.; Knudtson, K.L.; Monick, M.M.; Hunninghake, G.W. The p38 mitogen-activated protein kinase is required for NF-κB-dependent gene expression: The role of TATA-binding protein (TBP). J. Biol. Chem. 1999, 274, 30858–30863. [Google Scholar] [CrossRef]
- Yun, H.-Y.; Dawson, V.L.; Dawson, T.M. Neurobiology of nitric oxide. J. Crit. Rev. 1996, 10, 291–316. [Google Scholar] [CrossRef]
- Stuehr, D.J.; Cho, H.J.; Kwon, N.S.; Weise, M.F.; Nathan, C.F. Purification and characterization of the cytokine-induced macrophage nitric oxide synthase: An FAD-and FMN-containing flavoprotein. Proc. Natl. Acad. Sci. USA 1991, 88, 7773–7777. [Google Scholar] [CrossRef]
- Hyun, M.-S.; Woo, W.-H.; Hur, J.-M.; Kim, D.-H.; Mun, Y.-J. The role of ROS and p38 MAP kinase in berberine-induced apoptosis on human hepatoma HepG2 cells. J. Appl. Biol. Chem. 2008, 51, 129–135. [Google Scholar]
- Ahn, J.Y.; Lee, E.-R.; Kim, J.-Y.; Cho, S.-G. Protein phosphorylation as a regulatory mechanism of various cellular function. Cancer Prev. Res. 2006, 11, 1–8. [Google Scholar]
- Chung, J.H.; Kang, S.; Varani, J.; Lin, J.; Fisher, G.J.; Voorhees, J.J. Decreased extracellular-signal-regulated kinase and increased stress-activated MAP kinase activities in aged human skin in vivo. J. Investig. Dermatol. 2000, 115, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Liden, J.; Rafter, I.; Truss, M.; Gustafsson, J.-Å.; Okret, S. Glucocorticoid effects on NF-κB binding in the transcription of the ICAM-1 gene. Biochem. Biophys. Res. Commun. 2000, 273, 1008–1014. [Google Scholar] [CrossRef] [PubMed]
- Pruett, S.B.; Fan, R.; Zheng, Q. Characterization of glucocorticoid receptor translocation, cytoplasmic IκB, nuclear NFκB, and activation of NFκB in T lymphocytes exposed to stress-inducible concentrations of corticosterone in vivo. Int. Immunopharmacol. 2003, 3, 1–16. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.J.; Lee, S.H.; Lee, H.; Shin, M.-S.; Lee, J.W. Design, Synthesis, and Biological Evaluation of 3-Substituted-Indolin-2-One Derivatives as Potent Anti-Inflammatory Agents. Int. J. Mol. Sci. 2023, 24, 2066. https://doi.org/10.3390/ijms24032066
Kim SJ, Lee SH, Lee H, Shin M-S, Lee JW. Design, Synthesis, and Biological Evaluation of 3-Substituted-Indolin-2-One Derivatives as Potent Anti-Inflammatory Agents. International Journal of Molecular Sciences. 2023; 24(3):2066. https://doi.org/10.3390/ijms24032066
Chicago/Turabian StyleKim, Sung Jin, Sang Hyuk Lee, Heesu Lee, Myoung-Sook Shin, and Jae Wook Lee. 2023. "Design, Synthesis, and Biological Evaluation of 3-Substituted-Indolin-2-One Derivatives as Potent Anti-Inflammatory Agents" International Journal of Molecular Sciences 24, no. 3: 2066. https://doi.org/10.3390/ijms24032066
APA StyleKim, S. J., Lee, S. H., Lee, H., Shin, M.-S., & Lee, J. W. (2023). Design, Synthesis, and Biological Evaluation of 3-Substituted-Indolin-2-One Derivatives as Potent Anti-Inflammatory Agents. International Journal of Molecular Sciences, 24(3), 2066. https://doi.org/10.3390/ijms24032066





