New Derivatives of N-Hydroxybutanamide: Preparation, MMP Inhibition, Cytotoxicity, and Antitumor Activity
Abstract
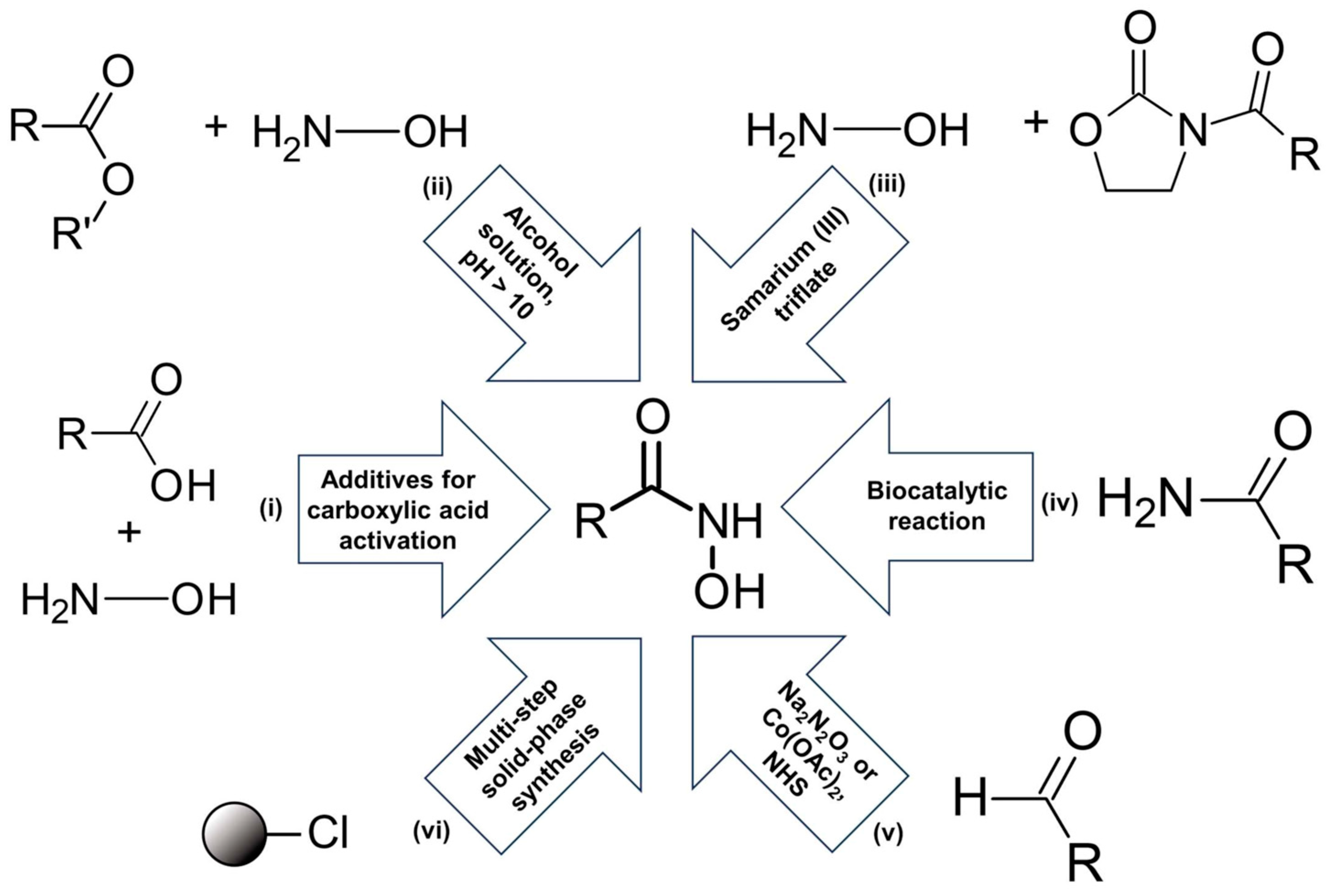
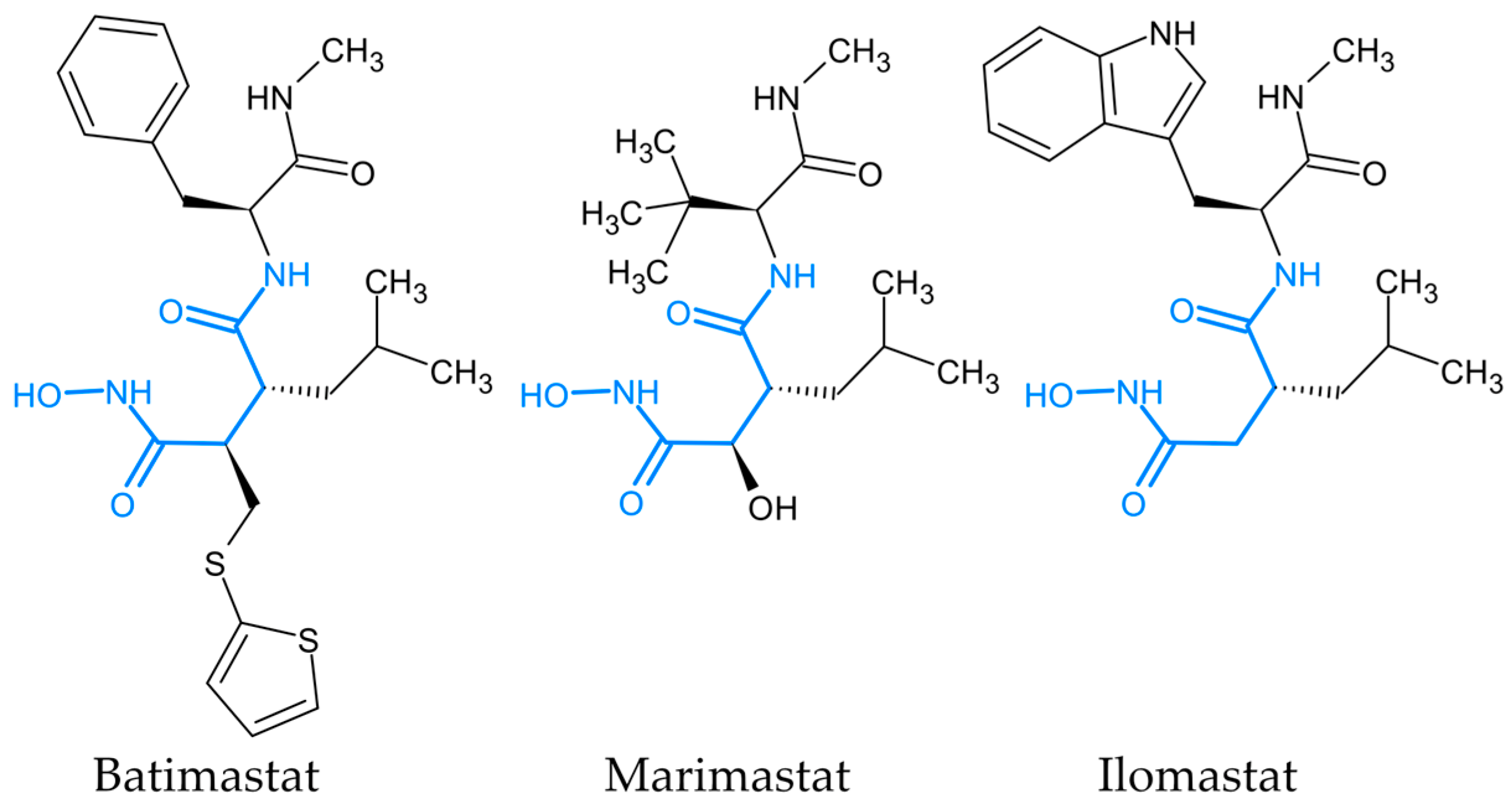
1. Introduction
2. Results
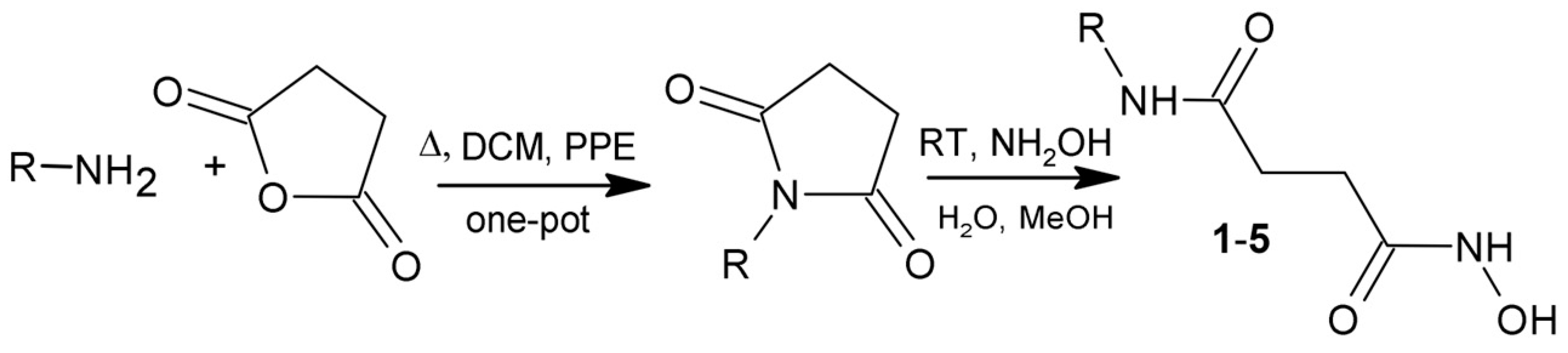
2.1. Synthesis of New N-Hydroxybutanamide Derivatives
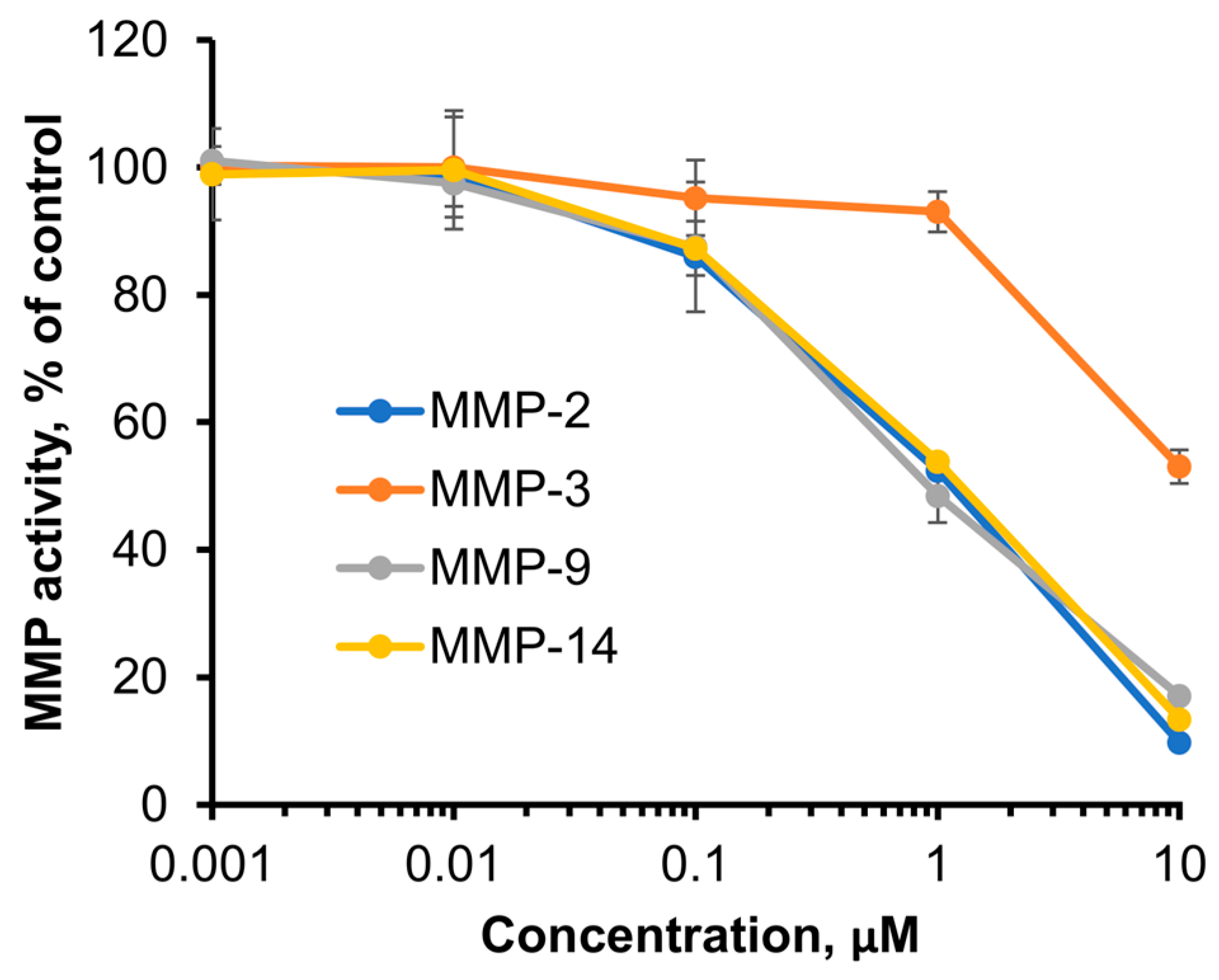
2.2. MMP Inhibitory Activity
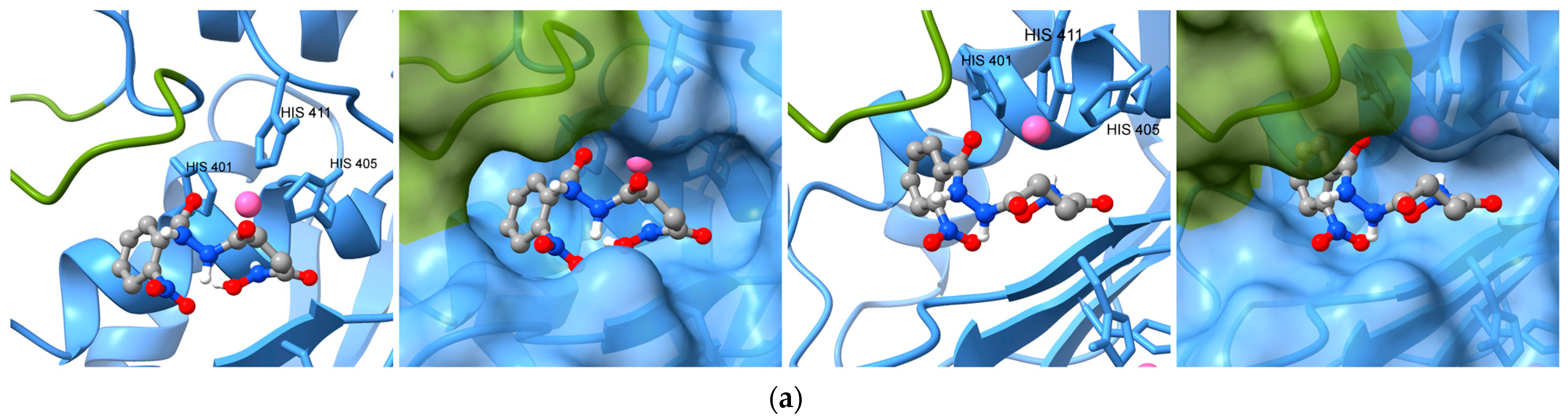
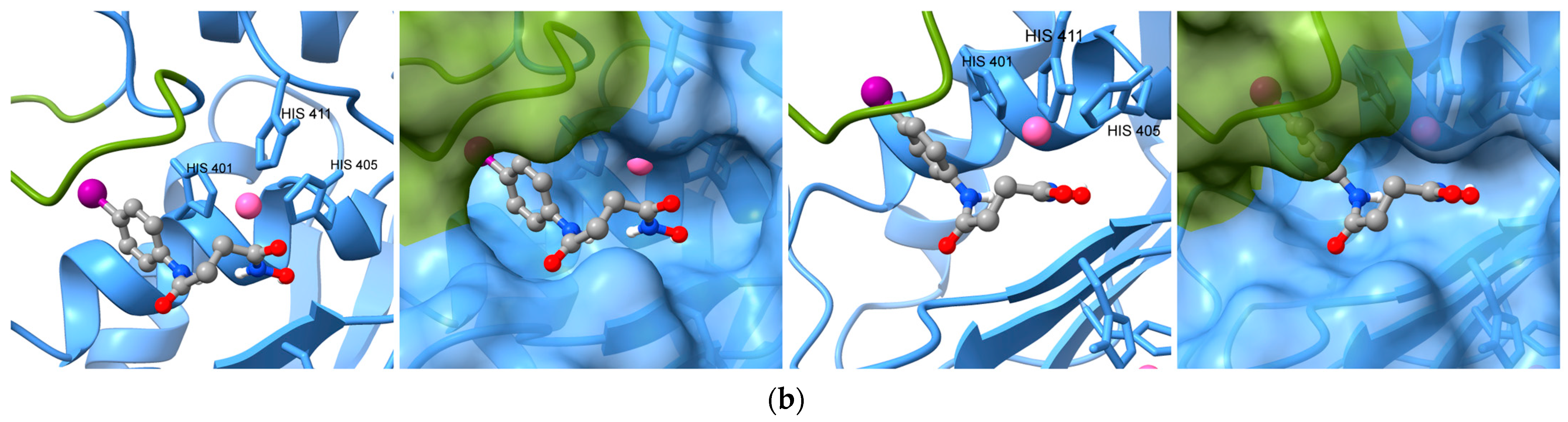
2.3. Molecular Docking
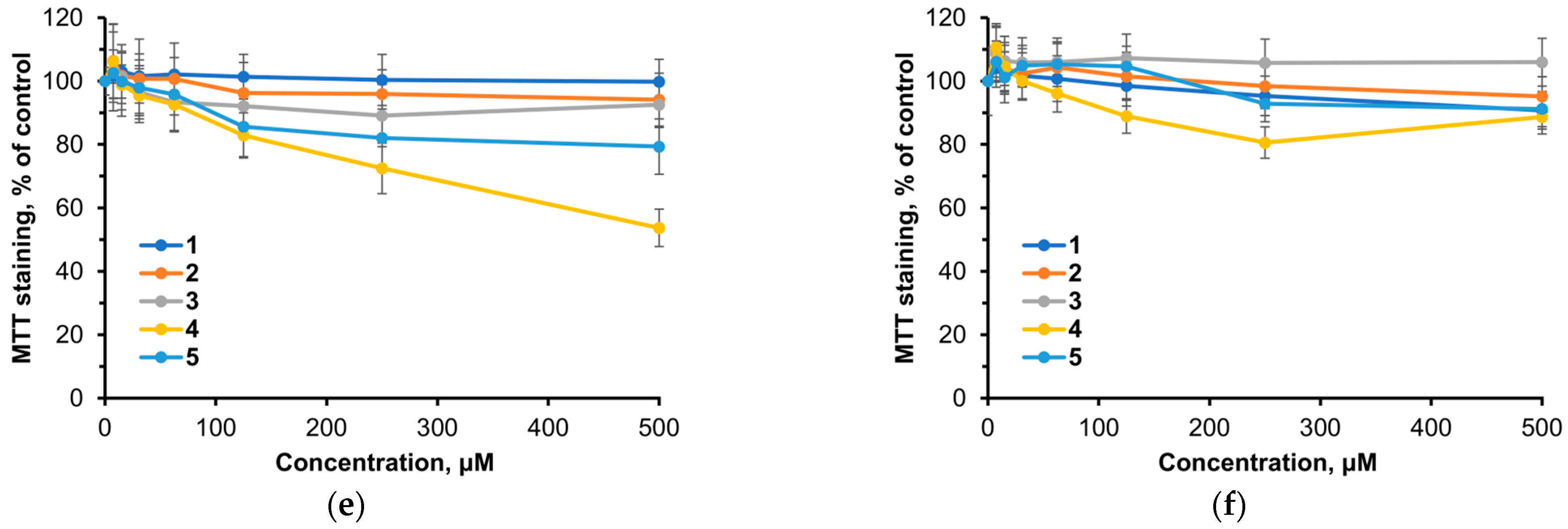
2.4. Cytotoxicity
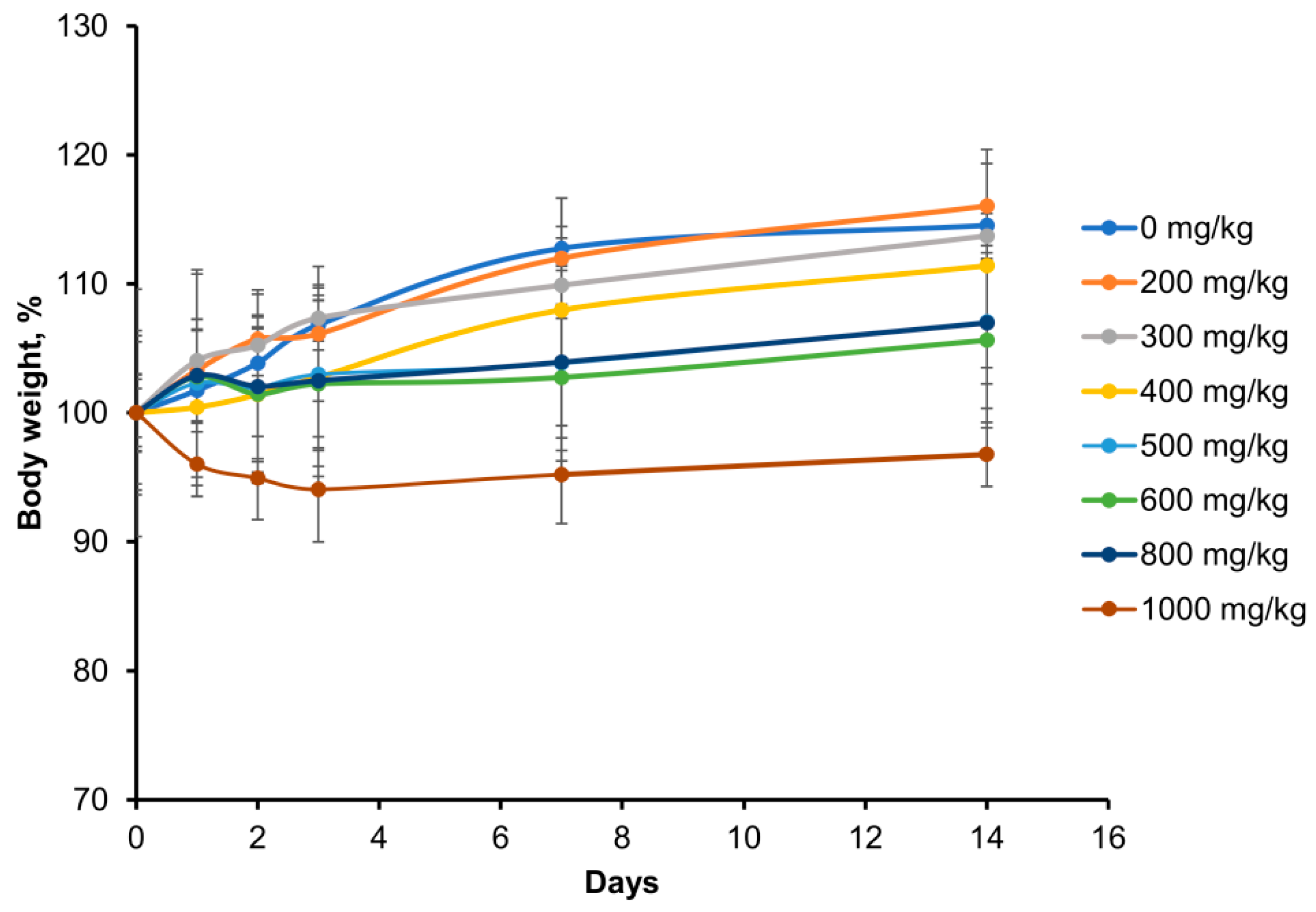
2.5. Acute Toxicity In Vivo
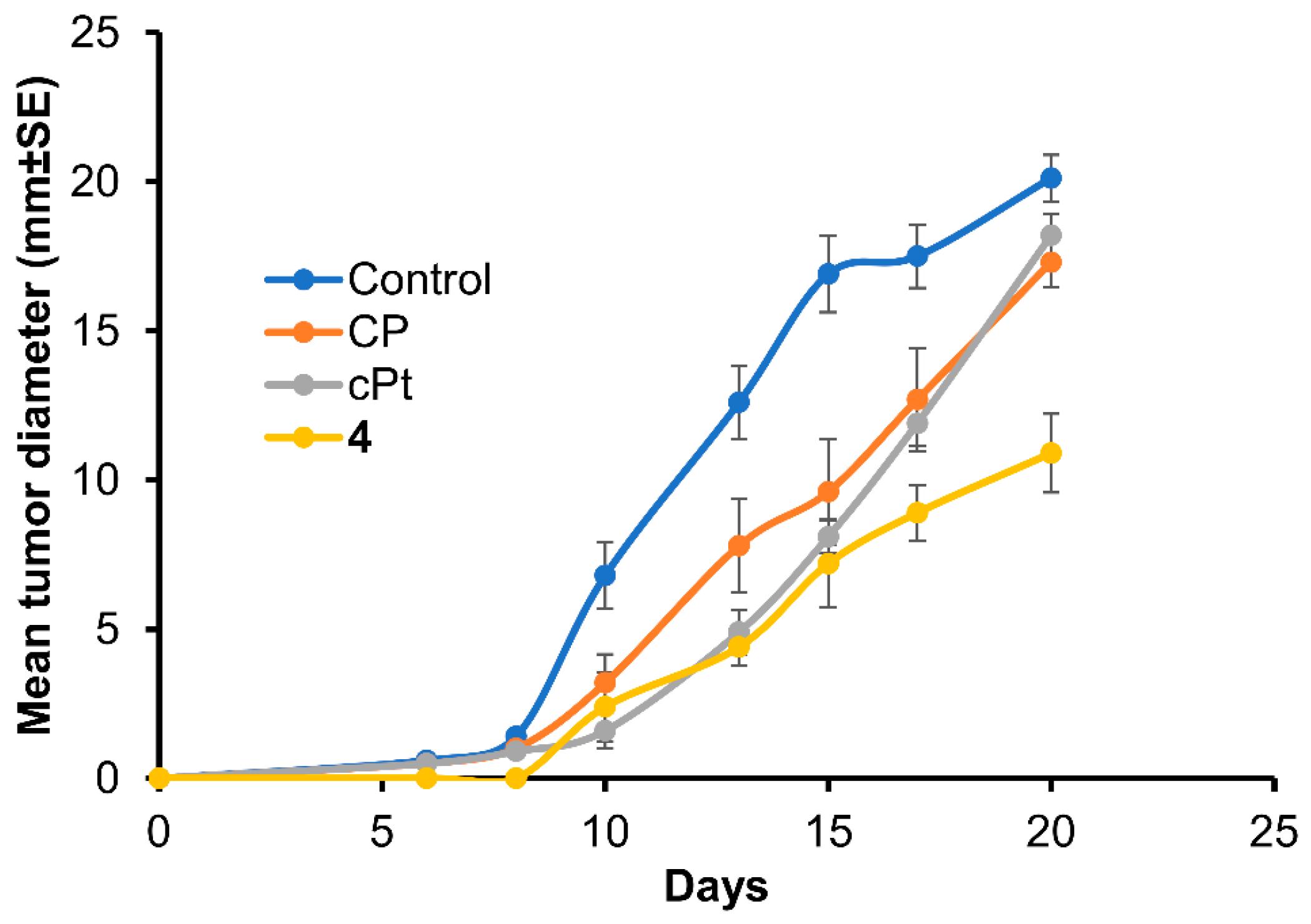
2.6. Antitumor Activity In Vivo
3. Discussion
4. Materials and Methods
4.1. Chemistry
4.2. Biological Studies
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Muri, E.M.; Nieto, M.J.; Sindelar, R.D.; Williamson, J.S. Hydroxamic acids as pharmacological agents. Curr. Med. Chem. 2002, 17, 1631–1653. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.P. Hydroxamic Acids; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Ugwu, D.I.; Ezema, B.E.; Eze, F.U.; Ayogu, J.I.; Ezema, C.G.; Ugwuja, D.I. Synthesis and Biological Applications of Hydroxamates. Am. J. Org. Chem. 2014, 4, 26–51. [Google Scholar] [CrossRef]
- Alam, M.A. Methods for Hydroxamic Acid Synthesis. Curr. Org. Chem. 2019, 23, 978–993. [Google Scholar] [CrossRef] [PubMed]
- Citarella, A.; Moi, D.; Pinzi, L.; Bonanni, D.; Rastelli, G. Hydroxamic Acid Derivatives: From Synthetic Strategies to Medicinal Chemistry Applications. ACS Omega 2021, 34, 21843–21849. [Google Scholar] [CrossRef]
- Porcheddu, A.; Giacomelli, G. Synthesis of oximes and hydroxamic acids. In The Chemistry of Hydroxylamines, Oximes and Hydroxamic Acids; Rappoport, Z., Liebman, J.F., Eds.; Wiley: Chichester, UK, 2009; Volume 1, pp. 163–231. [Google Scholar]
- Sibi, M.P.; Hasegawa, H.; Ghorpade, S.R. A Convenient Method for the Conversion of N-Acyloxazolidinones to Hydroxamic Acids. Org. Lett. 2002, 4, 3343–3346. [Google Scholar] [CrossRef]
- Tretyakov, B.A.; Gadomsky, S.Y.; Terentiev, A.A. A Reaction of N-Substituted Succinimides with Hydroxylamine as a Novel Approach to the Synthesis of Hydroxamic Acids. Organics 2023, 4, 186–195. [Google Scholar] [CrossRef]
- Tretyakov, B.A.; Filatova, N.V.; Mumyatova, V.A.; Gadomsky, S.Y.; Terent’ev, A.A. Pyridine Derivative of Succinic Acid Hydroxylamide Enhances the Cytotoxic Effect of Cisplatin and Actinomycin D. Bull. Exp. Biol. Med. 2023, 175, 23–26. [Google Scholar] [CrossRef]
- Chen, A.Y.; Adamek, R.N.; Dick, B.L.; Credille, C.V.; Morrison, C.N.; Cohen, S.M. Targeting Metalloenzymes for Therapeutic Intervention. Chem. Rev. 2019, 119, 1323–1455. [Google Scholar] [CrossRef]
- Maskos, K. Crystal structures of MMPs in complex with physiological and pharmacological inhibitors. Biochimie 2005, 87, 249–263. [Google Scholar] [CrossRef]
- Zivković, M.; Djurić, T.; Dincić, E.; Raicević, R.; Alavantić, D.; Stanković, A. Matrix metalloproteinase-9 -1562 C/T gene polymorphism in Serbian patients with multiple sclerosis. J. Neuroimmun. 2007, 189, 147–150. [Google Scholar] [CrossRef]
- Scherer, S.; de Souza, T.B.; de Paoli, J.; Brenol, C.V.; Xavier, R.M.; Brenol, J.C.; Chies, J.A.; Simon, D. Matrix metalloproteinase gene polymorphisms in patients with rheumatoid arthritis. Rheumat. Int. 2010, 30, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Djurić, T.; Stojković, L.; Zivković, M.; Končar, I.; Stanković, A.; Djordjević, A.; Alavantić, D. Matrix metalloproteinase-1 promoter genotypes and haplotypes are associated with carotid plaque presence. Clin. Biochem. 2012, 45, 1353–1356. [Google Scholar] [CrossRef] [PubMed]
- Djuric, T.; Zivkovic, M.; Milosevic, B.; Andjelevski, M.; Cvetkovic, M.; Kostic, M.; Stankovic, A. MMP-1 and -3 haplotype is associated with congenital anomalies of the kidney and urinary tract. Ped. Nephrol. 2014, 29, 879–884. [Google Scholar] [CrossRef] [PubMed]
- Egeblad, M.; Werb, Z. New functions for the matrix metalloproteinases in cancer progression. Nat. Rev. Cancer 2002, 2, 161–174. [Google Scholar] [CrossRef]
- Young, D.; Das, N.; Anowai, A.; Dufour, A. Matrix metalloproteases as influencers of the cells’ social media. Int. J. Mol. Sci. 2019, 20, 3847. [Google Scholar] [CrossRef]
- Piperigkou, Z.; Kyriakopoulou, K.; Koutsakis, C.; Mastronikolis, S.; Karamanos, N.K. Key matrix remodeling enzymes: Functions and targeting in cancer. Cancers 2021, 13, 1441. [Google Scholar] [CrossRef]
- Zucker, S.; Cao, J.; Chen, W.-T. Critical appraisal of the use of matrix metalloproteinase inhibitors in cancer treatment. Oncogene 2000, 19, 6642–6650. [Google Scholar] [CrossRef]
- Nelson, A.R.; Fingleton, B.; Rothenberg, M.L.; Matrisian, L.M. Matrix metalloproteinases: Biologic activity and clinical implications. J. Clin. Oncol. 2000, 18, 1135–1149. [Google Scholar] [CrossRef]
- Dufour, A.; Overall, C.M. Missing the target: Matrix metalloproteinase antitargets in inflammation and cancer. Trends Pharmacol. Sci. 2013, 34, 233–242. [Google Scholar] [CrossRef]
- Overall, C.M.; Kleifeld, O. Towards third generation matrix metalloproteinase inhibitors for cancer therapy. Br. J. Cancer 2006, 94, 941–946. [Google Scholar] [CrossRef]
- Das, N.; Benko, C.; Gill, S.E.; Dufour, A. The pharmacological TAILS of matrix metalloproteinases and their inhibitors. Pharmaceuticals 2020, 14, 31. [Google Scholar] [CrossRef] [PubMed]
- Gona, K.; Toczek, J.; Ye, Y.; Sanzida, N.; Golbazi, A.; Boodagh, P.; Salarian, M.; Jung, J.-J.; Rajendran, S.; Kukreja, G.; et al. Hydroxamate-Based Selective Macrophage Elastase (MMP-12) Inhibitors and Radiotracers for Molecular Imaging. J. Med. Chem. 2020, 63, 15037–15049. [Google Scholar] [CrossRef] [PubMed]
- Almeida, L.G.N.; Thode, H.; Eslambolchi, Y.; Chopra, S.; Young, D.; Gill, S.; Devel, L.; Dufour, A. Matrix Metalloproteinases: From Molecular Mechanisms to Physiology, Pathophysiology, and Pharmacology. Pharmacol. Rev. 2022, 74, 714–770. [Google Scholar] [CrossRef] [PubMed]
- Eissa Mohammed, Y.H.; Thirusangu, P.; Zabiulla; Vigneshwaran, V.; Prabhakar, B.T.; Khanum, S.A. The anti-invasive role of novel synthesized pyridazine hydrazide appended phenoxy acetic acid against neoplastic development targeting matrix metallo proteases. Biomed. Pharmacother. 2017, 95, 375–386. [Google Scholar] [CrossRef]
- Ledour, G.; Moroy, G.; Rouffet, M.; Bourguet, E.; Guillaume, D.; Decarme, M.; Elmourabit, H.; Augé, F.; Alix, A.J.; Laronze, J.Y.; et al. Introduction of the 4-(4-bromophenyl)benzenesulfonyl group to hydrazide analogs of Ilomastat leads to potent gelatinase B (MMP-9) inhibitors with improved selectivity. Bioorg. Med. Chem. 2008, 18, 8745–8759. [Google Scholar] [CrossRef]
- Mondal, S.; Adhikari, N.; Banerjee, S.; Amin, S.A.; Jha, T. Matrix metalloproteinase-9 (MMP-9) and its inhibitors in cancer: A minireview. Eur. J. Med. Chem. 2020, 194, 112260, Erratum in: Eur. J. Med. Chem. 2020, 205, 112642. [Google Scholar] [CrossRef]
- Bauvois, B. New facets of matrix metalloproteinases MMP-2 and MMP-9 as cell surface transducers: Outside-in signaling and relationship to tumor progression. Biochim. Biophys. Acta 2012, 1825, 29–36. [Google Scholar] [CrossRef]
- Das, S.; Amin, S.A.; Jha, T. Inhibitors of gelatinases (MMP-2 and MMP-9) for the management of hematological malignancies. Eur. J. Med. Chem. 2021, 223, 113623. [Google Scholar] [CrossRef]
- Iochmann, S.; Bléchet, C.; Chabot, V.; Saulnier, A.; Amini, A.; Gaud, G.; Gruel, Y.; Reverdiau, P. Transient RNA silencing of tissue factor pathway inhibitor-2 modulates lung cancer cell invasion. Clin. Exp. Metastasis 2009, 26, 457–467. [Google Scholar] [CrossRef]
- Safranek, J.; Pesta, M.; Holubec, L.; Kulda, V.; Dreslerova, J.; Vrzalova, J.; Topolcan, O.; Pesek, M.; Finek, J.; Treska, V. Expression of MMP-7, MMP-9, TIMP-1 and TIMP-2 mRNA in lung tissue of patients with non-small cell lung cancer (NSCLC) and benign pulmonary disease. Anticancer Res. 2009, 29, 2513–2517. [Google Scholar]
- Li, H.; Qiu, Z.; Li, F.; Wang, C. The relationship between MMP-2 and MMP-9 expression levels with breast cancer incidence and prognosis. Oncol. Lett. 2017, 14, 5865–5870. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Yu, X.; Sun, S.; Zhang, X.; Yang, W.; Zhang, J.; Zhang, X.; Jiang, Z. Increased expression of MMP-2 and MMP-9 indicates poor prognosis in glioma recurrence. Biomed. Pharmacother. 2019, 118, 109369. [Google Scholar] [CrossRef] [PubMed]
- Sternlicht, M.D.; Bissell, M.J.; Werb, Z. The matrix metalloproteinase stromelysin-1 acts as a natural mammary tumor promoter. Oncogene 2000, 19, 1102–1113. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Ni, D.; Zhang, H.; Li, X.; Jiang, Y.; Wu, J.; Gu, Y.; Gao, M.; Shi, W.; Song, J.; et al. Over-expression of USP15/MMP3 predict poor prognosis and promote growth, migration in non-small cell lung cancer cells. Cancer Genet. 2023, 272–273, 9–15. [Google Scholar] [CrossRef]
- Wan, J.; Zhang, G.; Li, X.; Qiu, X.; Ouyang, J.; Dai, J.; Min, S. Matrix Metalloproteinase 3: A Promoting and Destabilizing Factor in the Pathogenesis of Disease and Cell Differentiation. Front. Physiol. 2021, 12, 663978. [Google Scholar] [CrossRef]
- Ogata, Y.; Enghild, J.J.; Nagase, H. Matrix metalloproteinase 3 (stromelysin) activates the precursor for the human matrix metalloproteinase 9. J. Biol. Chem. 1992, 267, 3581–3584. [Google Scholar] [CrossRef]
- Okada, Y.; Gonoji, Y.; Naka, K.; Tomita, K.; Nakanishi, I.; Iwata, K.; Yamashita, K.; Hayakawa, T. Matrix metalloproteinase 9 (92-kDa gelatinase/type IV collagenase) from HT 1080 human fibrosarcoma cells. Purification and activation of the precursor and enzymic properties. J. Biol. Chem. 1992, 267, 21712–21719. [Google Scholar] [CrossRef]
- Gonzalez-Molina, J.; Gramolelli, S.; Liao, Z.; Carlson, J.W.; Ojala, P.M.; Lehti, K. MMP14 in Sarcoma: A Regulator of Tumor Microenvironment Communication in Connective Tissues. Cells 2019, 8, 991. [Google Scholar] [CrossRef]
- Ulasov, I.; Yi, R.; Guo, D.; Sarvaiya, P.; Cobbs, C. The emerging role of MMP14 in brain tumorigenesis and future therapeutics. Biochim. Biophys. Acta 2014, 1846, 113–120. [Google Scholar] [CrossRef]
- Yosef, G.; Arkadash, V.; Papo, N. Targeting the MMP-14/MMP-2/integrin αvβ3 axis with multispecific N-TIMP2-based antagonists for cancer therapy. J. Biol. Chem. 2018, 293, 13310–13326. [Google Scholar] [CrossRef]
- Têtu, B.; Brisson, J.; Wang, C.S.; Lapointe, H.; Beaudry, G.; Blanchette, C.; Trudel, D. The influence of MMP-14, TIMP-2 and MMP-2 expression on breast cancer prognosis. Breast Cancer Res. 2006, 8, R28. [Google Scholar] [CrossRef] [PubMed]
- Sato, H.; Takino, T. Coordinate action of membrane-type matrix metalloproteinase-1 (MT1-MMP) and MMP-2 enhances pericellular proteolysis and invasion. Cancer Sci. 2010, 101, 843–847. [Google Scholar] [CrossRef] [PubMed]
- Rowsell, S.; Hawtin, P.; Minshull, C.A.; Jepson, H.; Brockbank, S.M.; Barratt, D.G.; Slater, A.M.; McPheat, W.L.; Waterson, D.; Henney, A.M.; et al. Crystal structure of human MMP9 in complex with a reverse hydroxamate inhibitor. J. Mol. Biol. 2002, 319, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Halle, W.; Göres, E. Vorhersage von LD50-Werten mit der Zellkultur. Pharmazie 1987, 42, 245–248. [Google Scholar] [PubMed]
- Reichling, J.; Schnitzler, P.; Suschke, U.; Saller, R. Essential oils of aromatic plants with antibacterial, antifungal, antiviral, and cytotoxic properties—An overview. Forsch. Komplementmed. 2009, 16, 79–90. [Google Scholar] [CrossRef]
- Loomis, T.A.; Hayes, A.W. Loomis’s Essentials of Toxicology, 4th ed.; Loomis, T.A., Hayes, A.W., Eds.; Academic Press: San Diego, CA, USA, 1996; pp. 17–32. [Google Scholar]
- Tamura, Y.; Watanabe, F.; Nakatani, T.; Yasui, K.; Fuji, M.; Komurasaki, T.; Tsuzuki, H.; Maekawa, R.; Yoshioka, T.; Kawada, K.; et al. Highly selective and orally active inhibitors of type IV collagenase (MMP-9 and MMP-2): N-sulfonylamino acid derivatives. J. Med. Chem. 1998, 41, 640–649. [Google Scholar] [CrossRef]
- Bernardo, M.M.; Brown, S.; Li, Z.H.; Fridman, R.; Mobashery, S. Design, synthesis, and characterization of potent, slow-binding inhibitors that are selective for gelatinases. J. Biol. Chem. 2002, 277, 11201–11207. [Google Scholar] [CrossRef]
- Maekawa, R.; Maki, H.; Wada, T.; Yoshida, H.; Nishida-Nishimoto, K.; Okamoto, H.; Matsumoto, Y.; Tsuzuki, H.; Yoshioka, T. Anti-metastatic efficacy and safety of MMI-166, a selective matrix metalloproteinase inhibitor. Clin. Exp. Metastasis 2000, 18, 61–66. [Google Scholar] [CrossRef]
- Matsushita, A.; Onda, M.; Uchida, E.; Maekawa, R.; Yoshioka, T. Antitumor effect of a new selective matrix metalloproteinase inhibitor, MMI-166, on experimental pancreatic cancer. Int. J. Cancer 2001, 92, 434–440. [Google Scholar] [CrossRef]
- Iwasaki, M.; Nishikawa, A.; Fujimoto, T.; Akutagawa, N.; Manase, K.; Endo, T.; Yoshida, K.; Maekawa, R.; Yoshioka, T.; Kudo, R. Anti-invasive effect of MMI-166, a new selective matrix metalloproteinase inhibitor, in cervical carcinoma cell lines. Gynecol. Oncol. 2002, 85, 103–107. [Google Scholar] [CrossRef]
- Laronha, H.; Carpinteiro, I.; Portugal, J.; Azul, A.; Polido, M.; Petrova, K.T.; Salema-Oom, M.; Caldeira, J. Challenges in Matrix Metalloproteinases Inhibition. Biomolecules 2020, 10, 717. [Google Scholar] [CrossRef] [PubMed]
- Wojtowicz-Praga, S.M.; Dickson, R.B.; Hawkins, M.J. Matrix metalloproteinase inhibitors. Investig. New Drugs 1997, 15, 61–75. [Google Scholar] [CrossRef] [PubMed]
- Zervos, E.E.; Norman, J.G.; Gower, W.R.; Franz, M.G.; Rosemurgy, A.S. Matrix metalloproteinase inhibition attenuates human pancreatic cancer growth in vitro and decreases mortality and tumorigenesis in vivo. J. Surg. Res. 1997, 69, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Lein, M.; Jung, K.; Le, D.K.; Hasan, T.; Ortel, B.; Borchert, D.; Winkelmann, B.; Schnorr, D.; Loenings, S.A. Synthetic inhibitor of matrix metalloproteinases (batimastat) reduces prostate cancer growth in an orthotopic rat model. Prostate 2000, 43, 77–82. [Google Scholar] [CrossRef]
- Woods, N.K.; Padmanabhan, J. Inhibition of amyloid precursor protein processing enhances gemcitabine-mediated cytotoxicity in pancreatic cancer cells. J. Biol. Chem. 2013, 288, 30114–30124. [Google Scholar] [CrossRef]
- Denis, L.J.; Verweij, J. Matrix metalloproteinase inhibitors: Present achievements and future prospects. Investig. New Drugs 1997, 15, 175–185. [Google Scholar] [CrossRef]
- Tonn, J.C.; Kerkau, S.; Hanke, A.; Bouterfa, H.; Mueller, J.G.; Wagner, S.; Vince, G.H.; Roosen, K. Effect of synthetic matrix-metalloproteinase inhibitors on invasive capacity and proliferation of human malignant gliomas in vitro. Int. J. Cancer 1999, 80, 764–772. [Google Scholar] [CrossRef]
- Jimenez, R.E.; Hartwig, W.; Antoniu, B.A.; Compton, C.C.; Warshaw, A.L.; Fernández-Del Castillo, C. Effect of matrix metalloproteinase inhibition on pancreatic cancer invasion and metastasis: An additive strategy for cancer control. Ann. Surg. 2000, 231, 644–654. [Google Scholar] [CrossRef]
- Davies, B.; Brown, P.D.; East, N.; Crimmin, M.J.; Balkwill, F.R. A synthetic matrix metalloproteinase inhibitor decreases tumor burden and prolongs survival of mice bearing human ovarian carcinoma xenografts. Cancer Res. 1993, 53, 2087–2091, Erratum in: Cancer Res. 1993, 53, 3652. [Google Scholar]
- Mesa, C.V.; Blandón, G.A.; Muñoz, D.L.; Muskus, C.E.; Flórez, A.F.; Ochoa, R.; Vélez, I.D.; Robledo, S.M. In silico screening of potential drug with antileishmanial activity and validation of their activity by in vitro and in vivo studies. J. Chem. Chem. Eng. 2015, 9, 375–402. [Google Scholar] [CrossRef][Green Version]
- Lyu, Y.; Xiao, Q.; Yin, L.; Yang, L.; He, W. Potent delivery of an MMP inhibitor to the tumor microenvironment with thermosensitive liposomes for the suppression of metastasis and angiogenesis. Signal Transduct. Target. Ther. 2019, 4, 26. [Google Scholar] [CrossRef] [PubMed]
- Price, A.; Shi, Q.; Morris, D.; Wilcox, M.E.; Brasher, P.M.; Rewcastle, N.B.; Shalinsky, D.; Zou, H.; Appelt, K.; Johnston, R.N.; et al. Marked inhibition of tumor growth in a malignant glioma tumor model by a novel synthetic matrix metalloproteinase inhibitor AG3340. Clin. Cancer Res. 1999, 5, 845–854. [Google Scholar] [PubMed]
- Romero-Perez, D.; Agrawal, A.; Jacobsen, J.; Yan, Y.; Thomas, R.; Cohen, S.; Villarreal, F. Effects of novel semiselective matrix metalloproteinase inhibitors on ex vivo cardiac structure-function. J. Cardiovasc. Pharmacol. 2009, 53, 452–461. [Google Scholar] [CrossRef]
- Qu, X.J.; Yuan, Y.X.; Tian, Z.G.; Xu, W.F.; Chen, M.H.; Cui, S.X.; Guo, Q.; Gai, R.; Makuuchi, M.; Nakata, M.; et al. Using caffeoyl pyrrolidine derivative LY52, a potential inhibitor of matrix metalloproteinase-2, to suppress tumor invasion and metastasis. Int. J. Mol. Med. 2006, 18, 609–614. [Google Scholar] [CrossRef][Green Version]
- Zhang, H.; Wang, X.; Mao, J.; Huang, Y.; Xu, W.; Duan, Y.; Zhang, J. Synthesis and biological evaluation of novel benzofuroxan-based pyrrolidine hydroxamates as matrix metalloproteinase inhibitors with nitric oxide releasing activity. Bioorg. Med. Chem. 2018, 26, 4363–4374. [Google Scholar] [CrossRef] [PubMed]
- Noha, M.; Yoshida, D.; Watanabe, K.; Teramoto, A. Suppression of cell invasion on human malignant glioma cell lines by a novel matrix-metalloproteinase inhibitor SI-27: In vitro study. J. Neurooncol. 2000, 48, 217–223. [Google Scholar] [CrossRef]
- Yoshida, D.; Watanabe, K.; Noha, M.; Takahashi, H.; Teramoto, A. Suppression of matrix metalloproteinase activity by SI-27: Detection by a new activity assay with S-2444, a specific chromogenic peptide. J. Neurooncol. 2002, 58, 1–11. [Google Scholar] [CrossRef]
- Nakamura, Y.; Sato, K.; Wakimoto, N.; Kimura, F.; Okuyama, A.; Motoyoshi, K. A new matrix metalloproteinase inhibitor SI-27 induces apoptosis in several human myeloid leukemia cell lines and enhances sensitivity to TNF alpha-induced apoptosis. Leukemia 2001, 15, 1217–1224. [Google Scholar] [CrossRef][Green Version]
- Kho, Y.H.; Chun, H.K.; Kim, H.M.; Lee, H.J.; Chung, M.C.; Lee, C.H. Pyridoxatin, an Inhibitor of Gelatinase A with Cytotoxic Activity. J. Microbiol. Biotechnol. 1996, 6, 445–450. [Google Scholar]
- Haiba, N.S.; Khalil, H.H.; Bergas, A.; Abu-Serie, M.M.; Khattab, S.N.; Teleb, M. First-in-Class Star-Shaped Triazine Dendrimers Endowed with MMP-9 Inhibition and VEGF Suppression Capacity: Design, Synthesis, and Anticancer Evaluation. ACS Omega 2022, 7, 21131–21144. [Google Scholar] [CrossRef]
- Brown, P.D.; Giavazzi, R. Matrix metalloproteinase inhibition: A review of anti-tumour activity. Ann. Oncol. 1995, 6, 967–974. [Google Scholar] [CrossRef] [PubMed]
- Fedorov, B.S.; Fadeev, M.A.; Eremeev, A.B.; Konovalova, N.P.; Bogdanov, G.N.; Tatyanenko, L.V.; Sashenkova, T.E.; Mishchenko, D.V. Hydroxamic acids: Synthesis and adjuvant activity in combinatorial anticancer therapy. Rus. Chem. Bull. 2016, 65, 801–805. [Google Scholar] [CrossRef]
- Mishchenko, D.V.; Neganova, M.E.; Klimanova, E.N.; Sashenkova, T.E.; Klochkov, S.G.; Shevtsova, E.F.; Vystorop, I.V.; Tarasov, V.V.; Chubarev, V.N.; Samsonov, A.N.; et al. Chemosensitizing Activity of Histone Deacetylases Inhibitory Cyclic Hydroxamic Acids for Combination Chemotherapy of Lymphatic Leukemia. Curr. Cancer Drug Targets 2018, 18, 365–371. [Google Scholar] [CrossRef]
- Vystorop, I.V.; Shilov, G.V.; Chernyak, A.V.; Klimanova, E.N.; Sashenkova, T.E.; Allayarova, U.Y.; Mishchenko, D.V.; Klochkov, S.G.; Neganova, M.E.; Aleksandrova, Y.R. Regioselective synthesis, structure, and chemosensitizing antitumor activity of cyclic hydroxamic acid based on DL-valine. Rus. J. Bioorg. Chem. 2021, 47, 757–764. [Google Scholar] [CrossRef]
- Fingleton, B. MMPs as therapeutic targets—Still a viable option? Semin. Cell Dev. Biol. 2008, 19, 61–68. [Google Scholar] [CrossRef]
- Chirivi, R.G.; Garofalo, A.; Crimmin, M.J.; Bawden, L.J.; Stoppacciaro, A.; Brown, P.D.; Giavazzi, R. Inhibition of the metastatic spread and growth of B16-BL6 murine melanoma by a synthetic matrix metalloproteinase inhibitor. Int. J. Cancer 1994, 58, 460–464. [Google Scholar] [CrossRef] [PubMed]
- Shalinsky, D.R.; Brekken, J.; Zou, H.; Bloom, L.A.; McDermott, C.D.; Zook, S.; Varki, N.M.; Appelt, K. Marked antiangiogenic and antitumor efficacy of AG3340 in chemoresistant human non-small cell lung cancer tumors: Single agent and combination chemotherapy studies. Clin. Cancer Res. 1999, 5, 1905–1917. [Google Scholar]
- Santos, O.; McDermott, C.D.; Daniels, R.G.; Appelt, K. Rodent pharmacokinetic and anti-tumor efficacy studies with a series of synthetic inhibitors of matrix metalloproteinases. Clin. Exp. Metastasis 1997, 15, 499–508. [Google Scholar] [CrossRef]
- Marusak, C.; Bayles, I.; Ma, J.; Gooyit, M.; Gao, M.; Chang, M.; Bedogni, B. The thiirane-based selective MT1-MMP/MMP2 inhibitor ND-322 reduces melanoma tumor growth and delays metastatic dissemination. Pharmacol. Res. 2016, 113, 515–520. [Google Scholar] [CrossRef]
- Abramjuk, C.; Jung, K.; Krell, H.W.; Juchem, R.; Peters, R.; Taymoorian, K.; Staack, A.; Stephan, C.; Schnorr, J.; Loening, S.A.; et al. Matrix metalloproteinase inhibitor Ro 28-2653 in combination with estramustine: Tumor-reducing effects on hormone-sensitive prostate cancer in rats. Anticancer Drugs 2005, 16, 855–861. [Google Scholar] [CrossRef]
- Pettersen, E.F.; Goddard, T.D.; Huang, C.C.; Couch, G.S.; Greenblatt, D.M.; Meng, E.C.; Ferrin, T.E. UCSF Chimera—A visualization system for exploratory research and analysis. J. Comput. Chem. 2004, 25, 1605–1612. [Google Scholar] [CrossRef] [PubMed]
- Hanwell, M.D.; Curtis, D.E.; Lonie, D.C.; Vandermeersch, T.; Zurek, E.; Hutchison, G.R. Avogadro: An advanced semantic chemical editor, visualization, and analysis platform. J. Cheminform. 2012, 4, 17. [Google Scholar] [CrossRef] [PubMed]
- Morris, G.M.; Huey, R.; Lindstrom, W.; Sanner, M.F.; Belew, R.K.; Goodsell, D.S.; Olson, A.J. Auto-Dock4 and AutoDockTools4: Automated docking with selective receptor flexibility. J. Comput. Chem. 2009, 30, 2785–2791. [Google Scholar] [CrossRef] [PubMed]
- Chou, T.C.; Talalay, P. Quantitative analysis of dose-effect relationships: The combined effects of multiple drugs or enzyme inhibitors. Adv. Enzyme Regul. 1984, 22, 27–55. [Google Scholar] [CrossRef]


| Compound | Structure |
|---|---|
| 1 | 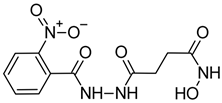 |
| 2 | 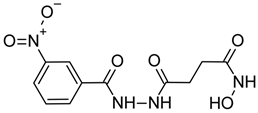 |
| 3 | 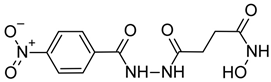 |
| 4 | 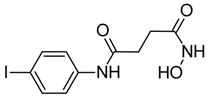 |
| 5 | 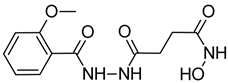 |
| Compound | MMP-2 | MMP-3 | MMP-9 | MMP-14 |
|---|---|---|---|---|
| 1 | >10 | >10 | >10 | >10 |
| 2 | >10 | >10 | >10 | >10 |
| 3 | >10 | >10 | >10 | >10 |
| 4 | 1.26 ± 0.01 | >10 | 1.06 ± 0.01 | 1.49 ± 0.01 |
| 5 | >10 | >10 | >10 | >10 |
| Compound | A-172 | U-251 MG | HeLa | HepG2 | FetMSC | Vero |
|---|---|---|---|---|---|---|
| 1 | >500 | >500 | 376.7 ± 25.2 | 392.7 ± 26.2 | >500 | >500 |
| 2 | >500 | >500 | 184.9 ± 15.3 | 213.0 ± 15.3 | >500 | >500 |
| 3 | >500 | >500 | 237.0 ± 14.2 | 251.8 ± 15.8 | >500 | >500 |
| 4 | 418.3 ± 17.4 | 400.6 ± 21.1 | 296.8 ± 15.7 | 487.5 ± 23.9 | >500 | >500 |
| 5 | >500 | >500 | 194.5 ± 13.4 | 220.9 ± 12.6 | >500 | >500 |
| Cisplatin | 8.46 ± 0.92 | - * | 11.74 ± 2.41 | 13.21 ± 1.62 | - * | 10.74 ± 1.45 |
| Compound | Dose, mg/kg | Administration Regimen, Day | Tumor Growth Inhibition, % | ||||
|---|---|---|---|---|---|---|---|
| Day 10 | Day 13 | Day 15 | Day 17 | Day 20 | |||
| CP | 100 | 2; 7 | 52.94 | 38.10 | 43.20 | 27.43 | 14.02 |
| cPt | 4 | 2–9 | 76.47 | 61.11 | 52.07 | 32.00 | 9.54 |
| 4 | 300 | 2–9 | 34.5 | 61.5 | 50.4 | 44.6 | 42.3 |
| Compound | Dose, mg/kg | Administration Regimen, Day | Number of Animals in the Group | Number of Animals without Metastases | Metastasis Rate, % | Mean Number of Metastases per Mouse | % Inhibition of Metastases |
|---|---|---|---|---|---|---|---|
| Control | - | 2–9 | 6 | 0 | 100 | 11.7 ± 3.4 | - |
| CP | 100 | 2; 7 | 6 | 0 | 100 | 7.1 ± 2.2 | 39.3 |
| cPt | 4 | 2–9 | 6 | 1 | 83.3 | 3.3 ± 2.4 * | 71.9 |
| 4 | 300 | 2–9 | 6 | 3 | 50 | 1.3 ± 0.9 ** | 88.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balakina, A.; Gadomsky, S.; Kokovina, T.; Sashenkova, T.; Mishchenko, D.; Terentiev, A. New Derivatives of N-Hydroxybutanamide: Preparation, MMP Inhibition, Cytotoxicity, and Antitumor Activity. Int. J. Mol. Sci. 2023, 24, 16360. https://doi.org/10.3390/ijms242216360
Balakina A, Gadomsky S, Kokovina T, Sashenkova T, Mishchenko D, Terentiev A. New Derivatives of N-Hydroxybutanamide: Preparation, MMP Inhibition, Cytotoxicity, and Antitumor Activity. International Journal of Molecular Sciences. 2023; 24(22):16360. https://doi.org/10.3390/ijms242216360
Chicago/Turabian StyleBalakina, Anastasia, Svyatoslav Gadomsky, Tatyana Kokovina, Tatyana Sashenkova, Denis Mishchenko, and Alexei Terentiev. 2023. "New Derivatives of N-Hydroxybutanamide: Preparation, MMP Inhibition, Cytotoxicity, and Antitumor Activity" International Journal of Molecular Sciences 24, no. 22: 16360. https://doi.org/10.3390/ijms242216360
APA StyleBalakina, A., Gadomsky, S., Kokovina, T., Sashenkova, T., Mishchenko, D., & Terentiev, A. (2023). New Derivatives of N-Hydroxybutanamide: Preparation, MMP Inhibition, Cytotoxicity, and Antitumor Activity. International Journal of Molecular Sciences, 24(22), 16360. https://doi.org/10.3390/ijms242216360






