Abstract
S100A6, also known as calcyclin, is a calcium-binding protein belonging to the S100 protein family. It was first identified and purified more than 30 years ago. Initial structural studies, focused mostly on the mode and affinity of Ca2+ binding and resolution of the resultant conformational changes, were soon complemented by research on its expression, localization and identification of binding partners. With time, the use of biophysical methods helped to resolve the structure and versatility of S100A6 complexes with some of its ligands. Meanwhile, it became clear that S100A6 expression was altered in various pathological states and correlated with the stage/progression of many diseases, including cancers, indicative of its important, and possibly causative, role in some of these diseases. This, in turn, prompted researchers to look for the mechanism of S100A6 action and to identify the intermediary signaling pathways and effectors. After all these years, our knowledge on various aspects of S100A6 biology is robust but still incomplete. The list of S100A6 ligands is growing all the time, as is our understanding of the physiological importance of these interactions. The present review summarizes available data concerning S100A6 expression/localization, interaction with intracellular and extracellular targets, involvement in Ca2+-dependent cellular processes and association with various pathologies.
1. Introduction
The S100 protein family, of which S100A6 is a member, groups more than 20 low-molecular-weight Ca2+-binding proteins [1]. Most of the genes encoding S100 proteins form a cluster on human chromosome 1 and mice chromosome 3 [2,3]. These genes and their protein products are designated with letter A and a number (S100A1–S100A16) that reflects the position of a given gene in the cluster on the human chromosome. Single S100 genes located on other chromosomes are designated by other letters (e.g., S100B, S100Z, S100G and S100P).
S100A6 was originally isolated from Ehrlich ascites tumor cells [4]. It is present in numerous cell types but is particularly abundant in epithelial cells and fibroblasts [5]. S100A6 is localized mainly in the cytoplasm but is also present in the cell nucleus and readily associates with the plasma membrane and nuclear envelope when the intracellular Ca2+ concentration increases [6,7,8].
S100A6 is composed of 89 amino acids (mouse and rat), 90 amino acids (man and rabbit) or 91–92 residues (chicken; two isoforms) [9]. Its sequence comprises two helix–loop–helix EF-hand structures, separated by a linker region. Amino acids located in the loop region coordinate Ca2+. The C-terminal EF-hand, comprising helices III and IV, has a canonical Ca2+ binding loop containing 12 amino acids and binds Ca2+ with high affinity (in a 10−6 M range), while the N-terminal loop, between helices I and II, has 14 amino acids and its Ca2+- binding affinity is slightly lower (Figure 1) [10].
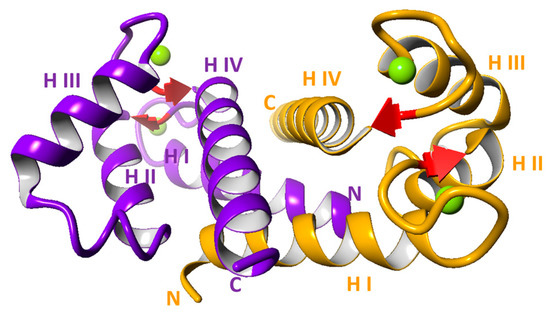
Figure 1.
Structure of S100A6 dimer with 4 Ca2+ (Protein Data Bank id:1K96) [10]. Each monomer is represented by different color (violet and yellow); green balls represent Ca2+; H indicates helix; N and C indicate N- and C-terminus, respectively.
In the cell and in solution, S100A6 exists as a non-covalent homodimer held together by hydrophobic interactions involving helices I and IV of each monomer [10,11]. Of note, it may also form a covalent dimer through a disulfide bridge between cysteine residues at position 2, and a heterodimer with another S100 family member, S100B [12,13]. Binding of two Ca2+ via the EF-hand structures induces conformational changes, mainly in helices II and III, which result in exposition of a hydrophobic surface responsible for interaction with target proteins and transduction of Ca2+ signals [10,14]. S100A6 also binds Zn2+, but the resulting conformational changes are different from those observed after binding of Ca2+ [15,16].
S100A6 Is involved in many processes inside and outside the cell, but its primary function seems to be associated with cell proliferation/tumorigenesis, cell differentiation, cytoskeletal dynamics or cellular stress response. Present extracellularly in the matrix or different body fluids, S100A6 may serve as a diagnostic marker in some diseases. This review summarizes the current state of knowledge regarding various aspects of S100A6 biology.
2. Localization and Expression of S100A6
S100A6 is a ubiquitous protein present in most human tissues and organs (https://www.proteinatlas.org/ (accessed on 5 September 2022)). The highest level of S100A6 expression is found in fibroblasts and epithelial cells [5], but it is also expressed in highly specialized cells such as certain neurons [17], glial cells [18], smooth or cardiac muscle cells [19,20] or various hematopoietic cells [21,22]. Interestingly, S100A6 has been detected in adult stem/progenitor cells of various lineages, e.g., in hematopoietic, neural and epidermal stem cells [23]. Single-cell RNA-seq experiments confirmed that S100A6 expression strongly correlated with the expression of established adult stem cell markers and was, in the majority of cases, characteristic for the most quiescent stem cell subpopulation.
S100A6 is predominantly a cytoplasmic protein, but in the presence of Ca2+ it associates with the plasma membrane and the nuclear envelope [6,7]. There are also several reports on the presence of S100A6 in cell nuclei, for example, in smooth muscle cells [19], lung carcinoma cells [24,25], skin tumor cells [26] and pancreatic ductal adenocarcinoma cells [8].
S100A6 expression can be up-regulated by multiple factors, such as epidermal growth factor (EGF) platelet-derived growth factor (PDGF), epidermal growth factor (EGF), serum [27], tumor necrosis factor (TNFα) [28], retinoic acid [29], estrogen [30], palmitate [31], glucose [32], vasopressin [33], gastrin [34] and various cytokines [35]. Transcription of the S100A6 gene is under the regulation of the following transcription factors: USF [36], NF-κB [37], SP1 and p53 [38], p63 [39], β-catenin [40], c-myc [32], ChREBP [41], ZEB1 and STAT3 [35]. Several recent studies revealed the role of microRNAs (miRNAs) in the regulation of S100A6 expression. MiR-193a and miR-493-5p were shown to inhibit S100A6 expression by binding directly to the 3′-UTR of S100A6 mRNA [42,43], while several other miRNAs were shown to affect S100A6 level indirectly [44,45]. S100A6 expression is also controlled by DNA methylation of the S100A6 gene [46,47].
3. Intracellular S100A6 Ligands
Over the years, numerous protein ligands of S100A6 have been identified. Corresponding to the distribution of S100A6 described above, the list includes cytoplasmic, membrane, nuclear and extracellular proteins. It should be emphasized that in in vitro conditions the binding occurs in the presence of Ca2+ and is abolished when Ca2+ is removed by chelators. This indicates that, in the cell, the interaction between S100A6 and the ligand can be triggered by an increase in intracellular Ca2+ concentration due to different stimuli. Thus, S100A6 and other S100 protein family members, constitute an important link in the transmission of the Ca2+ signal to effector proteins.
Data on S100A6 ligand binding have been obtained by various methods, and the strength and functional significance of these interactions have not always been investigated. Nonetheless, the apparent diversity of S100A6 ligands indicates that they might be implicated in a wide scope of cellular processes. There are several processes/phenomena in which the involvement of S100A6 seems to be particularly well documented. Worthy of note, for example, is the number of cytoskeletal proteins, both structural and regulatory ones that interact with S100A6. The list contains tropomyosin [48], caldesmon [49,50,51,52,53], calponin [54,55], non-muscle myosin IIA [56], actin [57] and cofilin-1 [58]. S100A6 also binds to components of the microtubule network such as α and β tubulin [59], kinesin light chain (KLC) [60] and centrosomal proteins FOR20, FOP and OFD1 [61]. Recent work has shown that S100A6 also interacts with tubulin polymerization-promoting protein (TPPP) [62]. This list of proteins strongly implicates S100A6 in the functioning of both the actin and the tubular cytoskeleton. In particular, through interacting directly with actin and myosin, or with actin- and myosin-binding proteins, S100A6 may affect actin–myosin interactions and myosin ATPase activity [48] or interfere with multiple activities of the actin cytoskeleton [57,58]. Likewise, via interaction with tubulin, centrosomal proteins, TPPP and KLC, it may regulate tubular network organization and/or tubular transport.
Interestingly, S100A6 also interacts with lamin B1 [63] and lamin A/C [40], the building blocks of nuclear filaments, i.e., structures that maintain the structural stability of the nucleus and play a role in chromatin organization [64]. Although the functional consequences of this interaction have not been studied, it implicates S100A6 in the structural aspects of the nucleus and, potentially, in chromatin dynamics. This assumption is reinforced by a recent report identifying high mobility group protein 20A (HMG20A), a component of the lysine-specific demethylase 1(LSD1)-REST co-repressor 1 (CoREST) complex, among S100A6 ligands [65]. Another nuclear target of S100A6, importin α, implicates it in regulation of nuclear transport. Namely, the interaction of S100A6 with the Arm domain of importin α disrupts the binding between importin and the nuclear localization signal (NLS) motif in cargo proteins and results in less efficient transport to the nucleus [66]. Last but not least, S100A6 can interact with ribosomal S6 kinase 1 (RSK1) which, when phosphorylated and activated by ERK1/2, enters the nucleus via importin-dependent transport and phosphorylates/activates numerous nuclear substrates, including transcription factors [67]. Although the consequences of the S100A6–RSK1 interaction have not been determined, it is worth stressing that RSK1, like S100A6, is linked with cell proliferation, as it promotes the G1 to S transition and DNA synthesis [67].
Other targets of S100A6 are annexins (Anx), Ca2+ and phospholipid binding proteins involved in membrane-linked processes such as membrane aggregation, fusion or permeability [68]. Among the 13 known annexins, S100A6 was found to interact with Anx1, Anx2, Anx6 and Anx11 [69,70,71,72]. The binding involves a short helical N-terminal segment, which is the most divergent part of the annexin molecule. Since annexins play a role in the anchoring of actin filaments to the cell membrane, they can be considered as cytoskeleton-linked S100A6 ligands. Taking into account the properties of annexins, it is believed that interaction with S100A6 and other S100 proteins might be important for endocytosis, secretion and other membrane-associated cellular processes.
Another interesting group of S100A6-interacting partners consists of proteins that are part of the Hsp70/Hsp90 machinery and often possess chaperone or co-chaperone properties. To this group belong Sgt1 [73,74], CacyBP/SIP [75], melusin [76], Hop (Hsp90/Hsp70-organizing protein), KLC and Tom70 [60], CHIP (C-terminus of Hsc70-interacting protein) [77], the immunophilins FKBP38 [78], FKBP52 and CyP-40 [79], and PP5 phosphatase [80]. It is worth noting that two of those proteins, Tom70 and FKBP38, are localized in the outer mitochondrial membrane. All these ligands implicate S100A6 in cellular response to stressful conditions. Although the biological effect of these interactions is not always clear, in most studied cases the binding of S100A6 results in dissociation of the pre-existing complexes of the above-mentioned co-chaperones with Hsp90 or Hsp70, allowing for complex remodeling upon the increase in intracellular Ca2+ concentration. In the case of CacyBP/SIP, it was shown that S100A6 may compete for the binding with ERK1/2 [81]. Additionally, S100A6 was found to inhibit CacyBP/SIP phosphorylation by casein kinase II [82].
Yet another set of S100A6 ligands, shared with some other S100 proteins, includes transcription factors of the p53 family, namely p53, p63 and p73 [83,84,85] and ubiquitin ligase Mdm2 (mouse double minute 2) [86]. Similarly to other S100 proteins, S100A6 binds to the tetramerization domains of p53, p63 and p73 in their monomeric, dimeric and also (in the case of p63 and p73) tetrameric form [84,87]. Interestingly, it can also interact with the N-terminal transactivation domain of these transcription factors [84]. This binding, in turn, interferes with p53 interaction with Mdm2 [86] and p300 acetyltransferase [85]. The picture is further complicated by the fact that S100A6 can also interact with Mdm2, a ubiquitin ligase degrading p53 [86]. Both positive and negative effects of S100A6 on p53 activity were reported, but the net physiological outcome of the numerous interactions is difficult to estimate also due to functional redundancy in the S100 protein family.
Cell surface receptors constitute another interesting group of S100A6 ligands, especially because, as mentioned earlier, S100A6 can be released from the cell and exert its effect extracellularly. The best-studied receptor ligand is RAGE (receptor for advanced glycation end products), which belongs to the PRRs (pattern recognition receptors) and transduces signals delivered by diverse ligands, including other S100 proteins, into pro-inflammatory responses [88]. RAGE activity has been implicated in different pathologies including diabetes, neurodegenerative diseases and cancers [88]. Binding of S100A6 to the RAGE ectodomain induces its dimerization and facilitates signal transduction [89,90]. Integrin β1 is another receptor ligand of S100A6, and the binding leads to activation of GSK3β, focal adhesion kinase (FAK) and p21-activated kinase (PAK)-dependent pathways [59]. Other membrane proteins that interact with S100A6 include Na+/Ca2+ exchanger (NCX1) and the TRPM4 transient receptor potential cation channel, both involved in ion transport [56].
S100A6 was also shown to bind to soluble extracellular proteins. The list comprises cytokines such as IFN-β, IL-11, CNTF or erythropoietin [91,92,93]. Although an in vitro viability assay showed no influence of S100A6 on IFN-β-induced toxicity, this does not exclude the possibility that S100A6 and other S100 proteins can modulate cytokine signaling in vivo [93]. Other extracellular targets of S100A6 include lysozyme, lumican, prolargin (PRELP) and insulin-like growth factor binding protein 1 (IGFBP-1) [94,95]. Of note, lysozyme has been recently shown to block S100A6 binding to RAGE [95]. Lysozyme, together with FKBP38, FKBP52, Cyp-40, PP5, CHIP, RSK1 and GAPDH [96], belongs to a group of S100A6 ligands endowed with enzymatic activity. However, except for PP5 [80], there are no data on how S100A6 binding may affect their activity.
4. Structural Aspects of S100A6—Ligand Interactions
The minimal regions responsible for the interaction with S100A6 have been identified for many ligands. Generally, as for other S100 proteins [97], these are short, about 15–20 amino acid long protein segments with no apparent sequence similarity but usually enriched in hydrophobic and basic amino acids. These segments adopt a helical structure of amphipathic character upon binding to S100 proteins [98,99]. However, S100A6 was shown to interact also with protein motifs with defined secondary structures, such as tetratricopeptide repeat (TPR) domains. TPR is a 34 amino acid sequence forming a helix–loop–helix structure. TPRs are found in numerous S100A6 ligands, namely, Hop, KLC, Tom70, Cyp-40, FKBP38, FKBP52 and PP5 [60,77,78,79,80]. A structurally similar motif, called armadillo motif, is present in importin α and mediates its interaction with S100A6 [66]. A slightly different type of domain, which also has a helical structure, a so-called SGS domain, mediates the interaction of Sgt1 and CacyBP/SIP with S100A6 [73,100].
The S100 proteins usually interact with their ligands with a 1:1 stoichiometry, which means that two ligand molecules bind per S100A6 dimer, forming a heterotetramer. Nonetheless, binding of one ligand molecule to the S100A6 dimer was postulated for CacyBP/SIP, FOR20 and HMG20A [61,65,99]. Moreover, based on structural data, the possibility of simultaneous binding of more than one ligand cannot be excluded [10]. Numerous studies performed using biophysical methods established that, basically, the conformation of S100 proteins does not change upon ligand binding [101]. It is thus interesting how, having a rather rigid backbone, S100A6 and other S100 proteins can accommodate the binding of so many structurally divergent proteins. The canonical structure of S100 protein–ligand complexes assumes that the interacting domain of the ligand is positioned in a cleft formed, in a Ca2+- bound state, by the linker region between the two EF-hands and by helices III and IV of the C-terminal EF-hand [101]. In this configuration, each of the two ligand molecules would interact with a separate S100A6 monomer. However, recent methodological and analytical advances added some more complexity to this general scheme. Thus, in the case of annexin binding, it is believed, by analogy with other S100 proteins, that one end of the interacting segment of an annexin molecule contacts helix I of one S100A6 monomer while the other end interacts with residues in the linker and helix IV of the second monomer, bridging the two monomers together [101]. Yet another interaction mode was described for the complex of S100A6 with a 30 amino acid long (residues 189–219) CacyBP/SIP fragment, which is longer than most of the other binding domains studied and comprises two α helices [99]. One of those helices was shown to be positioned in a groove between helix III and IV of one S100A6 monomer, i.e., similar similarly to the canonical mode but without interaction with the linker, while the other contacted helix I of the other subunit [99]. In the complex of S100A6 mutant (C3S) with the V-domain of RAGE, the ligand interacts with amino acid residues in both Ca2+ binding loops and in helix III of S100A6 [89]. However, a different contact pattern and two types of complexes were proposed on the basis of the crystal structure of the complex formed by S100A6 and a RAGE fragment comprising the V, C1 and C2 domains [90]. A weak complex, in which each S100A6 monomer contacted one of the V domains through the N-terminal EF-hand domain, could be observed. In the second type of complex, each S100A6 monomer interacted with the C1 part of the RAGE fragment and simultaneously with the C2 domain of the other, thus bringing the two interacting molecules closer together [90]. This strong interaction could entail clustering of RAGE molecules and facilitate signal transduction [90]. Interestingly, such binding mode, which engages amino acid residues located both in the N-terminal and C-terminal part of S100A6, would require a different conformation of the S100A6 dimer which, as mentioned above, is considered to be stable; therefore, the existence of such a complex should be further confirmed.
4.1. Intracellular S100A6—Involvement in Cell Proliferation and Differentiation
S100A6 mRNA was first identified in growth-stimulated quiescent cells [102] and this finding was followed by many others, pointing to a tight correlation between high S100A6 level and cell proliferation and motility [103]. In cancer cells, this correlation extends to tumor growth and invasiveness. Data concerning S100A6 knockdown are less numerous but equally convincing. For example, it has been shown that S100A6 deficiency profoundly inhibited proliferation of fibroblasts [104,105], osteoblasts [106] and pancreatic carcinoma cells [107]. S100A6-deficient fibroblasts exhibited a prolonged G0/G1 phase of the cell cycle and demonstrated features of cellular senescence such as changes in cell shape and morphology, substantiated by altered organization of tropomyosin-containing [104] and actin filament networks [105]. S100A6 also exerts a profound impact on cell adhesion [108,109] and motile properties [63,105,110], although these may depend on cell type. Moreover, S100A6 knockdown entailed the up-regulation of several proteins recognized as negative regulators of cell division, while those involved in cell proliferation were down-regulated [107].
How the presence of S100A6 translates into cell proliferation and pro-survival cues is a matter of study (Figure 2). At least three reports show that overexpression of S100A6 results in an increase in β-catenin level or in its translocation to the nucleus [111,112,113]. β-catenin is a key mediator of the canonical Wnt signaling pathway, taking part in transcriptional regulation/stimulation of many genes, including those involved in pro-survival pathways and carcinogenesis [114]. Since β-catenin enhances S100A6 expression [40], the resulting positive feedback loop may drive cell proliferation. Another possible mechanism through which S100A6 level may influence cell proliferation involves activation of the MAP kinase signaling pathway. S100A6 overexpression was shown to result in increased phosphorylation (activation) of p38 and ERK1/2 kinases in colorectal cancer cell lines, while S100A6 knockdown corresponded to lower phosphorylation [115]. Increased p38, but not ERK1/2, phosphorylation was also detected after S100A6 overexpression in nasopharyngeal carcinoma cells, while an adverse effect was observed after S100A6 silencing [116]. S100A6 was also found to participate in the activation of yet another signaling pathway, namely the PI3K/AKT pathway [117]. Finally, as mentioned earlier, S100A6 directly interacts with RSK1 [56]. Thus, experimental data link S100A6 with several pro-survival signaling pathways, although we still do not know at which point the signal from S100A6 is integrated. In this regard, recent studies revealed that, in keratinocytes, S100A6 may act by activating the epidermal growth factor receptor (EGFR), which transmits the signal to MAPK and other kinases [118]. In addition, it was shown that S100A6, through its interaction with integrin β1, activated the following downstream kinases: GSK3β, FAK (focal adhesion kinase) and PAK (p21-activated kinase) [59]. FAK and PAK are involved in the regulation of cytoskeletal dynamics, cell motility, cell proliferation and transformation, and may act via phosphorylating MAP kinases [119]. It is also worth mentioning that extracellular S100A6, acting through RAGE, activated JNK kinase [120]. Interestingly, as revealed by microarray analysis, S100A6 not only promotes pro-survival signaling but can also attenuate anti-proliferative pathways [121].
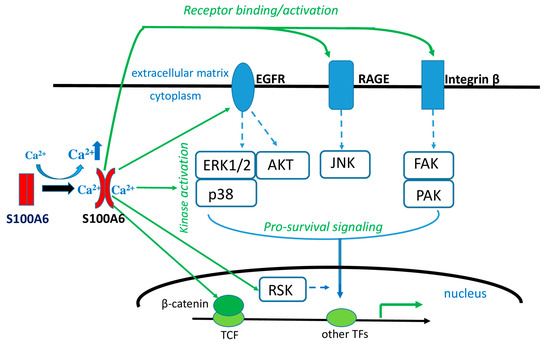
Figure 2.
Role of intracellular and extracellular S100A6 in Ca2+-cellular signaling. Increased intracellular Ca2+ level induces a conformational change of S100A6 molecule, which enables it to interact with various intracellular proteins or, following secretion, to bind to receptor proteins and activate signaling pathways and, ultimately, gene transcription that leads to cell survival/proliferation. TF—transcription factor.
There are much less experimental data concerning the impact of S100A6 on cell differentiation. It was shown, for example, that S100A6 overexpression delayed the appearance of epidermal differentiation markers both in classic and organotypic cultures of HaCaT keratinocytes [39]. On the other hand, S100A6 knockdown had no, or only a modest, effect on the pace of keratinocyte differentiation. Another study showed that S100A6 knockdown favored osteogenic differentiation of mouse embryonic fibroblasts, as could be judged by increased activity of alkaline phosphatase but was not sufficient to induce ectopic bone formation [122]. However, when differentiation was stimulated by the addition of BMP9, one of the most potent osteogenic factors, S100A6 knockdown cells, produced significantly more bone mass compared to control cells. S100A6 overexpression could not counteract BMP9-induced cell differentiation. These results suggest that S100A6 disturbs and/or delays cell differentiation by providing pro-proliferative cues rather than inhibiting those involved in differentiation.
4.2. Intracellular S100A6—Involvement in Cellular Stress Response
There are many reports showing that S100A6 level increases under stress conditions such as ischemia [123], mechanical force [124], irradiation [24], oxidative stress [125], hypertension [126] or kainic acid treatment [127]. All these conditions may lead to cell apoptosis and inflammation followed, depending on the extent of tissue damage, by regeneration [128]. Interestingly, literature data, although sometimes contradictory, indicate that S100A6 may be involved in most of the processes constituting cellular response to stress. For example, S100A6 has been shown to promote apoptosis in cells exposed to oxidative stress [83] or Ca2+ ionophore [129], while its decreased level made cells more resistant. In neuroblastoma cells, binding of extracellular S100A6 to RAGE induced apoptosis via/through reactive oxygen species (ROS)-dependent activation of JNK and caspases 3 and 7 [120]. An active role in stimulating caspase 3 transcription has also been postulated [129]. The pro-apoptotic effect of S100A6 may also stem from the fact that it inhibits the interaction between FKBP38 and Bcl-2; binding of FKBP38 to Bcl-2 exacerbates the anti-apoptotic properties of Bcl-2 [78]. However, there are also reports documenting anti-apoptotic effects of S100A6. For example, it was shown that S100A6 inhibits cardiac myocyte or renal carcinoma cell apoptosis [28,130].
S100A6 is often detected at sites of inflammation [131], but there are contradictory reports as to its role in this process [132,133]. On the other hand, numerous data indicate that S100A6 may be involved in tissue/cell repair and regeneration after stress. First of all, as mentioned above, it interacts with many components of the heat shock machinery. Structural studies have demonstrated that the interaction of co-chaperone proteins with S100A6 engages the same domain, namely the TPR domain, through which the co-chaperones interact with Hsp90 [60,79,80]. Accordingly, it was shown using recombinant proteins and cell lysates that S100A6 competes with Hsp70/Hsp90 for binding with co-chaperone proteins, e.g., HOP, KLC and FKBP38 [60,78]. Thus, evidently, upon stressful conditions, S100A6 can induce a rearrangement of the preexisting chaperone–co-chaperone complexes but whether this contributes to more efficient protein refolding and/or disaggregation is not known. Although S100A6 was reported to inhibit β-amyloid aggregation [134] or favor β-amyloid plaque disaggregation [135], the effect was ascribed to direct interaction with β-amyloid or to Zn2+ chelation, respectively, rather than to its interaction with the components of the chaperone system. Other data link S100A6 with tissue regeneration due to its pro-proliferative properties. For example, an increase in S100A6 level after injury was interpreted as beneficial in the case of renal tubular cells or the spinal cord [136,137], since it correlated with cell proliferation or neurogenesis. Likewise, an increased S100A6 level accompanied hair and hematopoietic stem cell regeneration [138,139]. In accordance with this are the results showing that expression of S100A6 in various brain structures is different in mice subjected to mild chronic stress when compared to control mice [140]. A significant decrease in the protein level of S100A6 was observed in brainstem structures and also in the olfactory bulb, cerebellum and stress-related structures such as the hippocampus and the hypothalamus of stressed animals. An initial decrease in S100A6, followed by a gradual increase up to control levels, was detected in the hippocampus of rats subjected to traumatic brain injury [141]. These observations suggest that S100A6 expression in the brain is affected by stressful conditions to which the animals are exposed.
5. Extracellular S100A6—A Marker of Pathological States
S100A6, like some other S100 family members, can be secreted from cells most likely by a microtubule-dependent mechanism [59], and can be found in cell culture media and various physiological fluids. The presence of S100A6 has been reported for example in the culture medium of decidual cells [142] or cerebellar granule neurons treated with myelin-associated glycoprotein [143]. It has been also detected in extracellular matrix of Wharton’s jelly [144], amnion fluid [145], pancreatic juice [107,146], urine [147,148] and tears [149]. Recent results have shown that S100A6 is present in nasal lavage fluid [150], and its level is elevated in the nasal swabs of COVID-19 patients [151]. The role of extracellular S100A6 has not been extensively studied. However, it was proposed to regulate secretory processes since, when added to the medium, it stimulated the secretion of lactogen II by trophoblast cells [142] and the release of insulin from pancreatic cells [41,152] and of histamine from mast cells [153]. In the case of mesenchymal stem cells of the Wharton’s jelly extracellular S100A6 caused an increase in cell adhesion and, contrary to the intracellular protein, inhibited their proliferation [144].
There are numerous reports linking changes in S100A6 level in body fluids with various diseases. For example, serum levels of S100A6 are positively correlated with the progress of four different types of cancer: gastric cancer, non-small cell lung cancer, ovarian cancer and urinary bladder cancer [42,148,154,155,156,157,158,159]. Based on these data, it has been proposed that the serum level of S100A6 can be used as a biomarker in detecting these types of cancer and serve as an indicator of their progress. As for other diseases, an increase in the serum level of S100A6 has been observed in acute coronary syndrome [160] and primary biliary cholangitis [161]. Interestingly, the serum concentration of S100A6 was diminished in the second trimester of pregnancy in women suffering from preeclampsia [162]. In the systemic sclerosis of the lung, an increased concentration of S100A6 has been detected in the bronchoalveolar lavage fluid [163,164]. S100A6 level in tears increases in various eye pathologies [149,165,166]. A higher level of S100A6 has also been found in the amniotic fluid following intra-amniotic infection [167], and in the vaginal fluid where it likely exerts an anti-microbial function [168]. Interestingly, decreased levels of S100A6 have been observed in the sputum of people living in a high background radiation area. This might be correlated with their adaptive response to the environment, which is also reflected in their low mortality from cancer [169].
An increased/diminished level of S100A6 present in body fluids is probably a secondary phenomenon that reflects changes in cellular S100A6 expression and thus may serve as an excellent marker of various pathological states. However, extracellular S100A6 may also contribute to the severity of a disease by activating certain intracellular signaling pathways through binding to cell receptors, as shown in Figure 2.
6. S100A6 in Various Pathologies
An increased level of S100A6 has been observed in different pathologies, including cancers. Although it is not known whether enhanced S100A6 expression is the cause or effect of pathological changes, it is rather certain that S100A6 has its share in the severity and progress of many diseases, since its knockdown in cellular or animal disease models usually alleviates the symptoms.
Among non-cancer pathologies, a high S100A6 level is typical for fibrosis-related diseases, characterized by excessive deposition of extracellular matrix proteins by activated fibroblasts [170]. As mentioned above, fibroblasts are particularly rich in S100A6 [5]. A high S100A6 mRNA/protein level was found in liver cirrhosis biliaris [5,171,172], chronic renal disease [173], pulmonary fibrosis [163] and myocardial infraction [174]. Recently, S100A6 expression has been shown to be highly correlated with CCl4-induced liver fibrosis in mice. Recombinant human S100A6 introduced to these mice enhanced the symptoms. Furthermore, S100A6 induced cell cycle transition from the S to G2 stage and significantly elevated the level of ERK1/2 phosphorylation. In contrast to S100A6, the soluble receptor for advanced glycation end products (sRAGE), a natural antagonist of the S100A6/RAGE pathway, had a preventative effect on liver fibrosis in the same mouse model [175].
High/increased S100A6 level may also be an indication of astrogliosis, a pathological change observed in neurodegenerative diseases such as Alzheimer disease [134,176,177] or amyotrophic lateral sclerosis (ALS) [178,179,180,181]. Interestingly, S100A6 localizes to β-amyloid plaques [134]. An increased level of S100A6 was also found in the hippocampus and prefrontal cortex of patients with postoperative neurocognitive disorders (po-NCD) [182]. A recent study has identified differentially expressed S100A6 in the spinal cord after injury [137]. In preeclamptic patients, the level of S100A6 in the umbilical cord was found to be much higher than in healthy pregnant women. In addition, post-translational modifications of S100A6 and its protein ligands are different in diseased women than in healthy ones [183]. Significantly higher levels of mRNA and protein of S100A6 are also characteristic for endometriosis, a benign growth of endometrial tissue outside the uterus. S100A6 expression is enhanced in ectopic endometrial tissues compared to eutopic ones [184]. S100A6 knockdown in ectopic endometrial stromal cells (ESCs) suppressed p38/MAPK activity and inhibited cell viability, migration and invasion, suggesting that S100A6 may contribute to the pathogenesis of endometriosis.
Enhanced S100A6 expression has been detected in most cancer tissues with a possible exception of testis cancer [185] (https://www.proteinatlas.org/ (accessed on 5 September 2022)). Most importantly, in many studied cases, a positive correlation between S100A6 expression and the disease stage, tumor size and/or metastasis has been reported. This applies, for example, to melanoma [186], adenoma and adenocarcinoma specimens [187] and premalignant and malignant pancreatic ductal cells [8]. In stomach cancer, S100A6 overexpression was associated with larger tumor size and deeper invasion [188]. In addition, the level of S100A6 correlated with tumor metastasis in osteosarcoma [110] and prostate cancer [46]. Regarding osteosarcoma, the latest study has shown that S100A6 overexpression increased the proliferation and reduced the osteogenic differentiation of osteosarcoma cells [43]. S100A6 expression was also helpful in discriminating between various cancer types, as in the case of cholangiocarcinoma and hepatocellular carcinoma [189,190,191]. Differences in S100A6 level proved to also be useful for the discrimination between primary liver tumors such as hepatocellular carcinoma and metastases derived from colorectal carcinoma [192,193]. All these data, together with the fact that S100A6 is detected in cancer stem cells [23], point to a potential role of S100A6 in the development of malignancy. In addition, due to changes in S100A6 expression during cancer progression, the protein has been recognized as a useful diagnostic and prognostic tool for defining cancer stage and patient prognosis as, for example, in the case of pancreatic and lung adenocarcinoma [194,195].
7. Conclusions
S100 proteins, due to their ability to bind Ca2+, serve as “readers” of Ca2+-conveyed intracellular and extracellular signals, which they subsequently translate into protein–protein interactions. S100A6 shares many structural features with other members of the S100 protein family but, at the same time, possesses a specific spectrum of ligands (listed in Table 1) and, possibly, functions. Despite years that have passed since its discovery the protein is still being intensively studied, as each novel ligand identified or a newly demonstrated link to some pathology open new research perspectives. Most actual topics of research include the mechanism through which S100A6 contributes to the activation of various kinases engaged in pro-survival pathways, its role in stem cells and, invariably, its role in various human pathologies, with a special emphasis on its potential use as a disease marker in clinics. Thus, S100A6 is a protein with a long history and most likely an interesting future still ahead.

Table 1.
Intracellular and extracellular S100A6 ligands.
Author Contributions
W.L.: writing—original draft, writing—review and editing. A.F.: funding acquisition, writing—original draft, writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grant 2018/29/B/NZ4/01384 to A.F. from the National Science Centre and by statutory funds from the Nencki Institute of Experimental Biology of the Polish Academy of Sciences.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare that they have no conflict of interest with the contents of this article.
References
- Gonzalez, L.L.; Garrie, K.; Turner, M.D. Role of S100 proteins in health and disease. Biochim. Biophys. Acta 2020, 1867, 118677. [Google Scholar] [CrossRef]
- Schäfer, B.W.; Wicki, R.; Engelkamp, D.; Mattei, M.G.; Heizmann, C.W. Isolation of a YAC clone covering a cluster of nine S100 genes on human chromosome 1q21: Rationale for a new nomenclature of the S100 calcium-binding protein family. Genomics 1995, 25, 638–643. [Google Scholar] [CrossRef] [PubMed]
- Ridinger, K.; Ilg, E.C.; Niggli, F.K.; Heizmann, C.W.; Schäfer, B.W. Clustered organization of S100 genes in human and mouse. Biochim. Biophys. Acta 1998, 1448, 254–263. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kuźnicki, J.; Filipek, A. Purification and properties of a novel Ca2+-binding protein (10.5 kDa) from Ehrlich-ascites-tumour cells. Biochem. J. 1987, 247, 663–667. [Google Scholar] [CrossRef] [PubMed]
- Kuźnicki, J.; Kordowska, J.; Puzianowska, M.; Woźniewicz, B.M. Calcyclin as a marker of human epithelial cells and fibroblasts. Exp. Cell Res. 1992, 200, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Lesniak, W.; Filipek, A. Ca2+-dependent interaction of calcyclin with membrane. Biochem. Biophys. Res. Commun. 1996, 220, 269–273. [Google Scholar] [CrossRef]
- Stradal, T.B.; Gimona, M. Ca(2+)-dependent association of S100A6 (Calcyclin) with the plasma membrane and the nuclear envelope. J. Biol. Chem. 1999, 274, 31593–31596. [Google Scholar] [CrossRef]
- Vimalachandran, D.; Greenhalf, W.; Thompson, C.; Lüttges, J.; Prime, W.; Campbell, F.; Dodson, A.; Watson, R.; Crnogorac-Jurcevic, T.; Lemoine, N.; et al. High nuclear S100A6 (Calcyclin) is significantly associated with poor survival in pancreatic cancer patients. Cancer Res. 2005, 65, 3218–3225. [Google Scholar] [CrossRef]
- Allen, B.G.; Andrea, J.E.; Sutherland, C.; Schönekess, B.O.; Walsh, M.P. Molecular cloning of chicken calcyclin (S100A6) and identification of putative isoforms. Biochem. Cell Biol. 1997, 75, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Otterbein, L.R.; Kordowska, J.; Witte-Hoffmann, C.; Wang, C.L.; Dominguez, R. Crystal structures of S100A6 in the Ca(2+)-free and Ca(2+)-bound states: The calcium sensor mechanism of S100 proteins revealed at atomic resolution. Structure 2002, 10, 557–567. [Google Scholar] [CrossRef]
- Wojda, U.; Kuźnicki, J. Calcyclin from mouse Ehrlich ascites tumor cells and rabbit lung form non-covalent dimers. Biochim. Biophys. Acta 1994, 1209, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; O’Hanlon, D.; Heizmann, C.W.; Marks, A. Demonstration of heterodimer formation between S100B and S100A6 in the yeast two-hybrid system and human melanoma. Exp. Cell Res. 1999, 246, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Deloulme, J.C.; Assard, N.; Mbele, G.O.; Mangin, C.; Kuwano, R.; Baudier, J. S100A6 and S100A11 are specific targets of the calcium- and zinc-binding S100B protein in vivo. J. Biol. Chem. 2000, 275, 35302–35310. [Google Scholar] [CrossRef] [PubMed]
- Sastry, M.; Ketchem, R.R.; Crescenzi, O.; Weber, C.; Lubienski, M.J.; Hidaka, H.; Chazin, W.J. The three-dimensional structure of Ca(2+)-bound calcyclin: Implications for Ca(2+)-signal transduction by S100 proteins. Structure 1998, 6, 223–231. [Google Scholar] [CrossRef]
- Filipek, A.; Heizmann, C.W. Kuźnicki J. Calcyclin is a calcium and zinc binding protein. FEBS Lett. 1990, 264, 263–266. [Google Scholar] [CrossRef]
- Moroz, O.V.; Wilson, K.S.; Bronstein, I.B. The role of zinc in the S100 proteins: Insights from the X-ray structures. Amino Acids 2011, 41, 761–772. [Google Scholar] [CrossRef]
- Filipek, A.; Puzianowska, M.; Cieślak, B.; Kuźnicki, J. Calcyclin--Ca(2+)-binding protein homologous to glial S-100 beta is present in neurones. Neuroreport 1993, 4, 383–386. [Google Scholar] [CrossRef]
- Yamashita, N.; Ilg, E.C.; Schäfer, B.W.; Heizmann, C.W.; Kosaka, T. Distribution of a specific calcium-binding protein of the S100 protein family, S100A6 (calcyclin), in subpopulations of neurons and glial cells of the adult rat nervous system. J. Comp. Neurol. 1999, 404, 235–257. [Google Scholar] [CrossRef]
- Mandinova, A.; Atar, D.; Schäfer, B.W.; Spiess, M.; Aebi, U.; Heizmann, C.W. Distinct subcellular localization of calcium binding S100 proteins in human smooth muscle cells and their relocation in response to rises in intracellular calcium. J. Cell Sci. 1998, 111 Pt 14, 2043–2054. [Google Scholar] [CrossRef]
- Engelkamp, D.; Schäfer, B.W.; Erne, P.; Heizmann, C.W. S100 alpha, CAPL, and CACY: Molecular cloning and expression analysis of three calcium-binding proteins from human heart. Biochemistry 1992, 31, 10258–10264. [Google Scholar] [CrossRef]
- Tomida, Y.; Terasawa, M.; Kobayashi, R.; Hidaka, H. Calcyclin and calvasculin exist in human platelets. Biochem. Biophys. Res. Commun. 1992, 189, 1310–1316. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, S.; Tagliafico, E.; Manfredini, R.; Grande, A.; Rossi, E.; Zucchini, P.; Torelli, G.; Torelli, U. Abundance of the primary transcript and its processed product of growth-related genes in normal and leukemic cells during proliferation and differentiation. Cancer Res. 1992, 52, 11–16. [Google Scholar] [PubMed]
- Leśniak, W.; Filipek, A. S100A6 as a Constituent and Potential Marker of Adult and Cancer Stem Cells. Stem Cell Rev. Rep. 2022, 18, 2699–2708. [Google Scholar] [CrossRef] [PubMed]
- Orre, L.M.; Pernemalm, M.; Lengqvist, J.; Lewensohn, R.; Lehtiö, J. Up-regulation, modification, and translocation of S100A6 induced by exposure to ionizing radiation revealed by proteomics profiling. Mol. Cell. Proteom. 2007, 6, 2122–2131. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Xu, X.; Khan, A.Q.; Ling, W. High Expression of S100A6 Predicts Unfavorable Prognosis of Lung Squamous Cell Cancer. Med. Sci. Monit. 2017, 23, 5011–5017. [Google Scholar] [CrossRef]
- Brinck, U.; Gabius, H.J.; Zeng, F.Y.; Gerke, V.; Lazarou, D.; Zografakis, C.; Tsambaos, D.; Berger, H. Differential expression of calcyclin and its accessible ligands in various types of cutaneous tumors. J. Dermatol. Sci. 1995, 10, 181–190. [Google Scholar] [CrossRef]
- Ghezzo, F.; Valpreda, S.; De Riel, J.K.; Baserga, R. Identification of serum-responsive elements in the promoter of human calcyclin, a growth-regulated gene. DNA 1989, 8, 171–177. [Google Scholar] [CrossRef]
- Tsoporis, J.N.; Izhar, S.; Parker, T. Expression of S100A6 in cardiac myocytes limits apoptosis induced by tumor necrosis factor-alpha. J. Biol. Chem. 2008, 283, 30174–30183. [Google Scholar] [CrossRef]
- Tonini, G.; Casalaro, A.; Cara, A.; Di Martino, D. Inducible expression of calcyclin, a gene with strong homology to S-100 protein, during neuroblastoma cell differentiation and its prevalent expression in Schwann-like cell lines. Cancer Res. 1991, 51, 1733–1737. [Google Scholar]
- Hong, E.J.; Park, S.H.; Choi, K.C.; Leung, P.C.; Jeung, E.B. Identification of estrogen-regulated genes by microarray analysis of the uterus of immature rats exposed to endocrine disrupting chemicals. Reprod. Biol. Endocrinol. 2006, 4, 49. [Google Scholar] [CrossRef]
- Busch, A.; Cordery, D.; Denyer, G.S.; Biden, T.J. Expression profiling of palmitate- and oleate-regulated genes provides novel insights into the effects of chronic lipid exposure on pancreatic beta-cell function. Diabetes 2002, 51, 977–987. [Google Scholar] [CrossRef]
- Zhang, J.; Yang, P.; Liu, D.; Gao, M.; Wang, J.; Wang, X.; Liu, Y.; Zhang, X. c-Myc Upregulated by High Glucose Inhibits HaCaT Differentiation by S100A6 Transcriptional Activation. Front. Endocrinol. 2021, 12, 676403. [Google Scholar] [CrossRef] [PubMed]
- Courtois-Coutry, N.; Le Moellic, C.; Boulkroun, S.; Fay, M.; Cluzeaud, F.; Escoubet, B.; Farman, N.; Blot-Chabaud, M. Calcyclin is an early vasopressin-induced gene in the renal collecting duct. Role in the long term regulation of ion transport. J. Biol. Chem. 2002, 277, 25728–25734. [Google Scholar] [CrossRef] [PubMed]
- Kucharczak, J.; Pannequin, J.; Camby, I.; Decaestecker, C.; Kiss, R.; Martinez, J. Gastrin induces over-expression of genes involved in human U373 glioblastoma cell migration. Oncogene 2001, 20, 7021–7028. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Al-Ismaeel, Q.; Neal, C.P.; Al-Mahmoodi, H.; Almutairi, Z.; Al-Shamarti, I.; Straatman, K.; Jaunbocus, N.; Irvine, A.; Issa, E.; Moreman, C.; et al. ZEB1 and IL-6/11-STAT3 signalling cooperate to define invasive potential of pancreatic cancer cells via differential regulation of the expression of S100 proteins. Br. J. Cancer 2019, 121, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Leśniak, W.; Jezierska, A.; Kuźnicki, J. Upstream stimulatory factor is involved in the regulation of the human calcyclin (S100A6) gene. Biochim. Biophys. Acta 2000, 1517, 73–81. [Google Scholar] [CrossRef]
- Joo, J.H.; Kim, J.W.; Lee, Y.; Yoon, S.Y.; Kim, J.H.; Paik, S.G.; Choe, I.S. Involvement of NF-kappaB in the regulation of S100A6 gene expression in human hepatoblastoma cell line HepG2. Biochem. Biophys. Res. Commun. 2003, 307, 274–280. [Google Scholar] [CrossRef]
- Króliczak, W.; Pietrzak, M.; Puzianowska-Kuznicka, M. P53-dependent suppression of the human calcyclin gene (S100A6): The role of Sp1 and of NFkappaB. Acta Biochim. Pol. 2008, 55, 559–570. [Google Scholar] [CrossRef]
- Graczyk, A.; Leśniak, W. S100A6 expression in keratinocytes and its impact on epidermal differentiation. Int. J. Biochem. Cell Biol. 2014, 57, 135–141. [Google Scholar] [CrossRef]
- Kilańczyk, E.; Graczyk, A.; Ostrowska, H.; Kasacka, I.; Leśniak, W.; Filipek, A. S100A6 is transcriptionally regulated by β-catenin and interacts with a novel target, lamin A/C, in colorectal cancer cells. Cell Calcium 2012, 51, 470–477. [Google Scholar] [CrossRef]
- Dogra, S.; Das, D.; Maity, S.K.; Paul, A.; Rawat, P.; Daniel, P.V.; Das, K.; Mitra, S.; Chakrabarti, P.; Mondal, P. Liver-Derived S100A6 Propels β-Cell Dysfunction in NAFLD. Diabetes 2022, 71, 2284–2296. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Lv, X.; Zhang, Z.; Xie, S. S100A6/miR193a regulates the proliferation, invasion, migration and angiogenesis of lung cancer cells through the P53 acetylation. Am. J. Transl. Res. 2019, 11, 4634–4649. [Google Scholar] [PubMed]
- Liu, Q.; Luo, J.; Wang, H.; Zhang, L.; Jin, G. SNHG1 functions as an oncogenic lncRNA and promotes osteosarcoma progression by up-regulating S100A6 via miR-493-5p. Acta Biochim. Biophys. Sin. 2022, 54, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Lan, J.; Xie, K. miR-202-3p overexpression attenuates endometriosis-like lesions by modulating YAP-dependent transcription of S100A6 in murine models. Life Sci. 2020, 265, 118757. [Google Scholar] [CrossRef]
- Abdi, J.; Rashedi, I.; Keating, A. Concise Review: TLR Pathway-miRNA Interplay in Mesenchymal Stromal Cells: Regulatory Roles and Therapeutic Directions. Stem Cells 2018, 36, 1655–1662. [Google Scholar] [CrossRef]
- Rehman, I.; Cross, S.S.; Catto, J.W.; Leiblich, A.; Mukherjee, A.; Azzouzi, A.R.; Leung, H.Y.; Hamdy, F.C. Promoter hyper-methylation of calcium binding proteins S100A6 and S100A2 in human prostate cancer. Prostate 2005, 65, 322–330. [Google Scholar] [CrossRef]
- Leśniak, W.; Słomnicki, Ł.P.; Kuźnicki, J. Epigenetic control of the S100A6 (calcyclin) gene expression. J. Investig. Dermatol. 2007, 127, 2307–2314. [Google Scholar] [CrossRef]
- Golitsina, N.L.; Kordowska, J.; Wang, C.L.; Lehrer, S.S. Ca2+-dependent binding of calcyclin to muscle tropomyosin. Biochem. Biophys. Res. Commun. 1996, 220, 360–365. [Google Scholar] [CrossRef]
- Mani, R.S.; McCubbin, W.D.; Kay, C.M. Calcium-dependent regulation of caldesmon by an 11-kDa smooth muscle calcium-binding protein, caltropin. Biochemistry 1992, 31, 11896–11901. [Google Scholar] [CrossRef]
- Mani, R.S.; Kay, C.M. Calcium-dependent regulation of the caldesmon-heavy meromyosin interaction by caltropin. Biochemistry 1993, 32, 11217–11223. [Google Scholar] [CrossRef]
- Mani, R.S.; Kay, C.M. Influence of caltropin on the caldesmon induced polymerization of G-actin. Biochem. Biophys. Res. Commun. 1995, 213, 349–355. [Google Scholar] [CrossRef]
- Mani, R.S.; Kay, C.M. Effect of caltropin on caldesmon-actin interaction. J. Biol. Chem. 1995, 270, 6658–6663. [Google Scholar] [CrossRef]
- Filipek, A.; Zasada, A.; Wojda, U.; Makuch, R.; Dabrowska, R. Characterization of chicken gizzard calcyclin and examination of its interaction with caldesmon. Comp. Biochem. Physiol. B Biochem. Mol. Biol. 1996, 113, 745–752. [Google Scholar] [CrossRef] [PubMed]
- Wills, F.L.; McCubbin, W.D.; Kay, C.M. Smooth muscle calponin-caltropin interaction: Effect on biological activity and stability of calponin. Biochemistry 1994, 33, 5562–5569. [Google Scholar] [CrossRef] [PubMed]
- Filipek, A.; Wojda, U. Chicken gizzard calcyclin—Distribution and potential target proteins. Biochem. Biophys. Res. Commun. 1996, 225, 151–154. [Google Scholar] [CrossRef] [PubMed]
- Simon, M.A.; Ecsédi, P.; Kovács, G.M.; Póti, Á.L.; Reményi, A.; Kardos, J.; Gógl, G.; Nyitray, L. High-throughput competitive fluorescence polarization assay reveals functional redundancy in the S100 protein family. FEBS J. 2020, 287, 2834–2846. [Google Scholar] [CrossRef]
- Jurewicz, E.; Robaszkiewicz, K.; Moraczewska, J.; Filipek, A. Binding of S100A6 to actin and the actin-tropomyosin complex. Sci. Rep. 2020, 10, 12824. [Google Scholar] [CrossRef]
- Robaszkiewicz, K.; Jurewicz, E.; Moraczewska, J.; Filipek, A. Ca2+-dependent binding of S100A6 to cofilin-1 regulates actin filament polymerization-depolymerization dynamics. Cell Calcium 2021, 99, 102457. [Google Scholar] [CrossRef]
- Jurewicz, E.; Wyroba, E.; Filipek, A. Tubulin-dependent secretion of S100A6 and cellular signaling pathways activated by S100A6-integrin β1 interaction. Cell Signal. 2018, 42, 21–29. [Google Scholar] [CrossRef]
- Shimamoto, S.; Takata, M.; Tokuda, M.; Oohira, F.; Tokumitsu, H.; Kobayashi, R. Interactions of S100A2 and S100A6 with the tetratricopeptide repeat proteins, Hsp90/Hsp70-organizing protein and kinesin light chain. J. Biol. Chem. 2008, 283, 28246–28258. [Google Scholar] [CrossRef]
- Sakane, K.; Nishiguchi, M.; Denda, M.; Yamagchi, F.; Magari, M.; Kanayama, N.; Morishita, R.; Tokumitsu, H. Identification and characterization of a centrosomal protein, FOR20 as a novel S100A6 target. Biochem. Biophys. Res. Commun. 2017, 491, 980–985. [Google Scholar] [CrossRef] [PubMed]
- Doi, S.; Fujioka, N.; Ohtsuka, S.; Kondo, R.; Yamamoto, M.; Denda, M.; Magari, M.; Kanayama, N.; Hatano, N.; Morishita, R.; et al. Regulation of the tubulin polymerization-promoting protein by Ca2+/S100 proteins. Cell Calcium 2021, 96, 102404. [Google Scholar] [CrossRef] [PubMed]
- Nedjadi, T.; Kitteringham, N.; Campbell, F.; Jenkins, R.E.; Park, B.K.; Navarro, P.; Ashcroft, F.; Tepikin, A.; Neoptolemos, J.P.; Costello, E. S100A6 binds to annexin 2 in pancreatic cancer cells and promotes pancreatic cancer cell motility. Br. J. Cancer 2009, 101, 1145–1154. [Google Scholar] [CrossRef] [PubMed]
- Shimi, T.; Pfleghaar, K.; Kojima, S.; Pack, C.G.; Solovei, I.; Goldman, A.E.; Adam, S.A.; Shumaker, D.K.; Kinjo, M.; Cremer, T.; et al. The A- and B-type nuclear lamin networks: Microdomains involved in chromatin organization and transcription. Genes Dev. 2008, 22, 3409–3421. [Google Scholar] [CrossRef]
- Yamamoto, M.; Kondo, R.; Hozumi, H.; Doi, S.; Denda, M.; Magari, M.; Kanayama, N.; Hatano, N.; Morishita, R.; Tokumitsu, H. Identification and Biochemical Characterization of High Mobility Group Protein 20A as a Novel Ca2+/S100A6 Target. Biomolecules 2021, 11, 510. [Google Scholar] [CrossRef]
- Takata, M.; Shimamoto, S.; Yamaguchi, F.; Tokuda, M.; Tokumitsu, H.; Kobayashi, R. Regulation of nuclear localization signal-importin α interaction by Ca2+/S100A6. FEBS Lett. 2010, 584, 4517–4523. [Google Scholar] [CrossRef]
- Gao, X.; Chaturvedi, D.; Patel, T.B. Localization and retention of p90 ribosomal S6 kinase 1 in the nucleus: Implications for its function. Mol. Biol. Cell. 2012, 23, 503–515. [Google Scholar] [CrossRef]
- Schloer, S.; Pajonczyk, D.; Rescher, U. Annexins in Translational Research: Hidden Treasures to Be Found. Int. J. Mol. Sci. 2018, 19, 1781. [Google Scholar] [CrossRef]
- Filipek, A.; Gerke, V.; Weber, K.; Kuźnicki, J. Characterization of the cell-cycle-regulated protein calcyclin from Ehrlich ascites tumor cells. Identification of two binding proteins obtained by Ca2+-dependent affinity chromatography. Eur. J. Biochem. 1991, 195, 795–800. [Google Scholar] [CrossRef]
- Tokumitsu, H.; Mizutani, A.; Muramatsu, M.; Yokota, T.; Arai, K.; Hidaka, H. Molecular cloning of rabbit CAP-50, a calcyclin-associated annexin protein. Biochim. Biophys. Res. Commun. 1992, 186, 1227–1235. [Google Scholar] [CrossRef]
- Zeng, F.Y.; Gerke, V.; Gabius, H.J. Identification of annexin II, annexin VI and glyceraldehyde-3-phosphate dehydrogenase as calcyclin-binding proteins in bovine heart. Int. J. Biochem. 1993, 25, 1019–1027. [Google Scholar] [CrossRef] [PubMed]
- Streicher, W.W.; Lopez, M.M.; Makhatadze, G.I. Annexin I and annexin II N-terminal peptides binding to S100 protein family members: Specificity and thermodynamic characterization. Biochemistry 2009, 48, 2788–2798. [Google Scholar] [CrossRef]
- Nowotny, M.; Spiechowicz, M.; Jastrzebska, B.; Filipek, A.; Kitagawa, K.; Kuznick, J. Calcium-regulated interaction of Sgt1 with S100A6 (calcyclin) and other S100 proteins. J. Biol. Chem. 2003, 278, 26923–26928. [Google Scholar] [CrossRef] [PubMed]
- Spiechowicz, M.; Zylicz, A.; Bieganowski, P.; Kuznicki, J.; Filipek, A. Hsp70 is a new target of Sgt1—An interaction modulated by S100A6. Biochem. Biophys. Res. Commun. 2007, 357, 1148–1153. [Google Scholar] [CrossRef] [PubMed]
- Filipek, A.; Kuźnicki, J. Molecular cloning and expression of a mouse brain cDNA encoding a novel protein target of calcyclin. J. Neurochem. 1998, 70, 1793–1798. [Google Scholar] [CrossRef]
- Filipek, A.; Michowski, W.; Kuznicki, J. Involvement of S100A6 (calcyclin) and its binding partners in intracellular signaling pathways. Adv. Enzym. Regul. 2008, 48, 225–239. [Google Scholar] [CrossRef]
- Shimamoto, S.; Kubota, Y.; Yamaguchi, F.; Tokumitsu, H.; Kobayashi, R. Ca2+/S100 proteins act as upstream regulators of the chaperone-associated ubiquitin ligase CHIP (C terminus of Hsc70-interacting protein). J. Biol. Chem. 2013, 288, 7158–7168. [Google Scholar] [CrossRef]
- Shimamoto, S.; Tsuchiya, M.; Yamaguchi, F.; Kubota, Y.; Tokumitsu, H.; Kobayashi, R. Ca2+/S100 proteins inhibit the interaction of FKBP38 with Bcl-2 and Hsp90. Biochem. J. 2014, 458, 141–152. [Google Scholar] [CrossRef]
- Shimamoto, S.; Kubota, Y.; Tokumitsu, H.; Kobayashi, R. S100 proteins regulate the interaction of Hsp90 with Cyclophilin 40 and FKBP52 through their tetratricopeptide repeats. FEBS Lett. 2010, 584, 1119–1125. [Google Scholar] [CrossRef]
- Yamaguchi, F.; Umeda, Y.; Shimamoto, S.; Tsuchiya, M.; Tokumitsu, H.; Tokuda, M.; Kobayashi, R. S100 proteins modulate protein phosphatase 5 function: A link between CA2+ signal transduction and protein dephosphorylation. J. Biol. Chem. 2012, 287, 13787–13798. [Google Scholar] [CrossRef]
- Kilanczyk, E.; Filipek, S.; Jastrzebska, B.; Filipek, A. CacyBP/SIP binds ERK1/2 and affects transcriptional activity of Elk-1. Biochem. Biophys. Res. Commun. 2009, 380, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Wasik, U.; Kadziolka, B.; Kilanczyk, E.; Filipek, A. Influence of S100A6 on CacyBP/SIP Phosphorylation and Elk-1 Transcriptional Activity in Neuroblastoma NB2a Cells. J. Cell. Biochem. 2016, 117, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Słomnicki, Ł.P.; Nawrot, B.; Leśniak, W. S100A6 binds p53 and affects its activity. Int. J. Biochem. Cell Biol. 2009, 41, 784–790. [Google Scholar] [CrossRef] [PubMed]
- van Dieck, J.; Brandt, T.; Teufel, D.P.; Veprintsev, D.B.; Joerger, A.C.; Fersht, A.R. Molecular basis of S100 proteins interacting with the p53 homologs p63 and p73. Oncogene 2010, 29, 2024–2035. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Graczyk, A.; Słomnicki, L.P.; Leśniak, W. S100A6 competes with the TAZ2 domain of p300 for binding to p53 and attenuates p53 acetylation. J. Mol. Biol. 2013, 425, 3488–3494. [Google Scholar] [CrossRef]
- van Dieck, J.; Lum, J.K.; Teufel, D.P.; Fersht, A.R. S100 proteins interact with the N-terminal domain of MDM2. FEBS Lett. 2010, 584, 3269–3274. [Google Scholar] [CrossRef]
- Fernandez-Fernandez, M.R.; Rutherford, T.J.; Fersht, A.R. Members of the S100 family bind p53 in two distinct ways. Protein Sci. 2008, 17, 1663–1670. [Google Scholar] [CrossRef]
- Xie, J.; Méndez, J.D.; Méndez-Valenzuela, V.; Aguilar-Hernández, M.M. Cellular signalling of the receptor for advanced glycation end products (RAGE). Cell Signal. 2013, 25, 2185–2197. [Google Scholar] [CrossRef]
- Mohan, S.K.; Gupta, A.A.; Yu, C. Interaction of the S100A6 mutant (C3S) with the V domain of the receptor for advanced glycation end products (RAGE). Biochem. Biophys. Res. Commun. 2013, 434, 328–333. [Google Scholar] [CrossRef]
- Yatime, L.; Betzer, C.; Jensen, R.K.; Mortensen, S.; Jensen, P.H.; Andersen, G.R. The Structure of the RAGE: S100A6 Complex Reveals a Unique Mode of Homodimerization for S100 Proteins. Structure 2016, 24, 2043–2052. [Google Scholar] [CrossRef]
- Kazakov, A.S.; Sofin, A.D.; Avkhacheva, N.V.; Denesyuk, A.I.; Deryusheva, E.I.; Rastrygina, V.A.; Sokolov, A.S.; Permyakova, M.E.; Litus, E.A.; Uversky, V.N.; et al. Interferon Beta Activity Is Modulated via Binding of Specific S100 Proteins. Int. J. Mol. Sci. 2020, 21, 9473. [Google Scholar] [CrossRef] [PubMed]
- Kazakov, A.S.; Deryusheva, E.I.; Sokolov, A.S.; Permyakova, M.E.; Litus, E.A.; Rastrygin, V.A.; Uversky, V.N.; Permyakov, E.A.; Permyakov, S.E. Erythropoietin Interacts with Specific S100 Proteins. Biomolecules 2022, 12, 120. [Google Scholar] [CrossRef]
- Kazakov, A.; Sokolov, A.S.; Permyakova, M.E.; Litus, E.A.; Uversky, V.N.; Permyakov, E.A.; Permyakov, S.E. Specific cytokines of interleukin-6 family interact with S100 proteins. Cell Calcium 2022, 101, 102520. [Google Scholar] [CrossRef]
- Jurewicz, E.; Kasacka, I.; Bankowski, E.; Filipek, A. S100A6 and its extracellular targets in Wharton’s jelly of healthy and preeclamptic patients. Placenta 2014, 35, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.I.; Dowarha, D.; Katte, R.; Chou, R.H.; Filipek, A.; Yu, C. Lysozyme as the anti-proliferative agent to block the interaction between S100A6 and the RAGE V domain. PLoS ONE 2019, 14, e0216427. [Google Scholar] [CrossRef] [PubMed]
- Filipek, A.; Wojda, U.; Leśniak, W. Interaction of calcyclin and its cyanogen bromide fragments with annexin II and glyceraldehyde 3-phosphate dehydrogenase. Int. J. Biochem. Cell Biol. 1995, 27, 1123–1131. [Google Scholar] [CrossRef]
- Bhattacharya, S.; Bunick, C.G.; Chazin, W.J. Target selectivity in EF-hand calcium binding proteins. Biochim. Biophys. Acta. 2004, 1742, 69–79. [Google Scholar] [CrossRef]
- Sudo, T.; Hidaka, H. Characterization of the calcyclin (S100A6) binding site of annexin XI-A by site-directed mutagenesis. FEBS Lett. 1999, 444, 11–14. [Google Scholar] [CrossRef]
- Lee, Y.T.; Dimitrova, Y.N.; Schneider, G.; Ridenour, W.B.; Bhattacharya, S.; Soss, S.E.; Caprioli, R.M.; Filipek, A.; Chazin, W.J. Structure of the S100A6 complex with a fragment from the C-terminal domain of Siah-1 interacting protein: A novel mode for S100 protein target recognition. Biochemistry 2008, 47, 10921–10932. [Google Scholar] [CrossRef][Green Version]
- Nowotny, M.; Bhattacharya, S.; Filipek, A.; Krezel, A.M.; Chazin, W.; Kuznicki, J. Characterization of the interaction of calcyclin (S100A6) and calcyclin-binding protein. J. Biol. Chem. 2000, 275, 31178–31182. [Google Scholar] [CrossRef]
- Rezvanpour, A.; Shaw, G.S. Unique S100 target protein interactions. Gen. Physiol. Biophys. 2009, 28, F39–F46. [Google Scholar] [PubMed]
- Calabretta, B.; Battini, R.; Kaczmarek, L.; de Riel, J.K.; Baserga, R. Molecular cloning of the cDNA for a growth factor-inducible gene with strong homology to S-100, a calcium-binding protein. J. Biol. Chem. 1986, 261, 12628–12632. [Google Scholar] [CrossRef] [PubMed]
- Leśniak, W.; Słomnicki, Ł.P.; Filipek, A. S100A6—New facts and features. Biochem. Biophys. Res. Commun. 2009, 390, 1087–1092. [Google Scholar] [CrossRef]
- Breen, E.C.; Tang, K. Calcyclin (S100A6) regulates pulmonary fibroblast proliferation, morphology, and cytoskeletal organization in vitro. J. Cell Biochem. 2003, 88, 848–854. [Google Scholar] [CrossRef] [PubMed]
- Słomnicki, L.P.; Leśnia, W. S100A6 (calcyclin) deficiency induces senescence-like changes in cell cycle, morphology and functional characteristics of mouse NIH 3T3 fibroblasts. J. Cell Biochem. 2010, 109, 576–584. [Google Scholar] [PubMed]
- Hwang, R.; Lee, E.J.; Kim, M.H.; Li, S.Z.; Jin, Y.J.; Rhee, Y.; Kim, Y.M.; Lim, S.K. Calcyclin, a Ca2+ ion-binding protein, contributes to the anabolic effects of simvastatin on bone. J. Biol. Chem. 2004, 279, 21239–21247. [Google Scholar] [CrossRef]
- Ohuchida, K.; Mizumoto, K.; Ishikawa, N.; Fujii, K.; Konomi, H.; Nagai, E.; Yamaguch, K.; Tsuneyoshi, M.; Tanaka, M. The role of S100A6 in pancreatic cancer development and its clinical implication as a diagnostic marker and therapeutic target. Clin. Cancer Res. 2005, 11, 7785–7793. [Google Scholar] [CrossRef]
- Luo, X.; Sharff, K.A.; Chen, J.; He, T.C.; Luu, H.H. S100A6 expression and function in human osteosarcoma. Clin. Orthop. Relat. Res. 2008, 466, 2060–2070. [Google Scholar] [CrossRef][Green Version]
- Cervera, A.M.; Apostolova, N.; Crespo, F.L.; Mata, M.; McCreath, K.J. Cells silenced for SDHB expression display characteristic features of the tumor phenotype. Cancer Res. 2008, 68, 4058–4067. [Google Scholar] [CrossRef]
- Luu, H.H.; Zhou, L.; Haydon, R.C.; Deyrup, A.T.; Monta, A.G.; Huo, D.; Heck, R.; Heizmann, C.W.; Peabody, T.D.; Simon, M.A.; et al. Increased expression of S100A6 is associated with decreased metastasis and inhibition of cell migration and anchorage independent growth in human osteosarcoma. Cancer Lett. 2005, 229, 135–148. [Google Scholar] [CrossRef]
- Li, Z.; Tang, M.; Ling, B.; Liu, S.; Zheng, Y.; Nie, C.; Yuan, Z.; Zhou, L.; Guo, G.; Tong, A.; et al. Increased expression of S100A6 promotes cell proliferation and migration in human hepatocellular carcinoma. J. Mol. Med. 2014, 92, 291–303. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Liu, X.; Lang, H.; Zhang, S.; Luo, Y.; Zhang, J. S100 calcium-binding protein A6 promotes epithelial-mesenchymal transition through β-catenin in pancreatic cancer cell line. PLoS ONE 2015, 10, e0121319. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhang, X.; Chen, M.; Cao, Q.; Huang, D. Effect of S100A6 over-expression on β-catenin in endometriosis. J. Obstet. Gynaecol. Res. 2015, 41, 1457–1462. [Google Scholar] [CrossRef] [PubMed]
- Rijsewijk, F.; van Deemter, L.; Wagenaar, E.; Sonnenberg, A.; Nusse, R. Transfection of the int-1 mammary oncogene in cuboidal RAC mammary cell line results in morphological transformation and tumorigenicity. EMBO J. 1987, 6, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Duan, L.; Wu, R.; Zou, Z.; Wang, H.; Ye, L.; Li, H.; Yuan, S.; Li, X.; Zha, H.; Sun, H.; et al. S100A6 stimulates proliferation and migration of colorectal carcinoma cells through activation of the MAPK pathways. Int. J. Oncol. 2014, 44, 781–790. [Google Scholar] [CrossRef]
- Li, A.; Shi, D.; Xu, B.; Wang, J.; Tang, Y.L.; Xiao, W.; Shen, G.; Deng, W.; Zhao, C. S100A6 promotes cell proliferation in human nasopharyngeal carcinoma via the p38/MAPK signaling pathway. Mol. Carcinog. 2017, 56, 972–984. [Google Scholar] [CrossRef]
- Li, A.; Gu, Y.; Li, X.; Sun, H.; Zha, H.; Xie, J.; Zhao, J.; Huang, M.; Chen, L.; Peng, Q.; et al. S100A6 promotes the proliferation and migration of cervical cancer cells via the PI3K/Akt signaling pathway. Oncol. Lett. 2018, 15, 5685–5693. [Google Scholar] [CrossRef]
- Graczyk-Jarzynka, A.; Sobiak, B.; Mlącki, M.; Wilanowski, T.; Leśniak, W. S100A6 activates EGFR and its downstream signaling in HaCaT keratinocytes. J. Cell Physiol. 2019, 234, 17561–17569. [Google Scholar] [CrossRef]
- Parsons, J.T. Focal adhesion kinase: The first ten years. J. Cell Sci. 2003, 116, 1409–1416. [Google Scholar] [CrossRef]
- Leclerc, E.; Fritz, G.; Weibel, M.; Heizmann, C.W.; Galichet, A. S100B and S100A6 differentially modulate cell survival by interacting with distinct RAGE (receptor for advanced glycation end products) immunoglobulin domains. J. Biol. Chem. 2007, 282, 31317–31331. [Google Scholar] [CrossRef]
- Lerchenmüller, C.; Heißenberg, J.; Damilano, F.; Bezzeridis, V.J.; Krämer, I.; Bochaton-Piallat, M.L.; Hirschberg, K.; Busch, M.; Katus, H.A.; Peppel, K.; et al. S100A6 Regulates Endothelial Cell Cycle Progression by Attenuating Antiproliferative Signal Transducers and Activators of Transcription 1 Signaling. Arterioscler. Thromb. Vasc. Biol. 2016, 36, 1854–1867. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wagner, E.R.; Yan, Z.; Wang, Z.; Luther, G.; Jiang, W.; Ye, J.; Wei, Q.; Wang, J.; Zhao, L.; et al. The Calcium-Binding Protein S100A6 Accelerates Human Osteosarcoma Growth by Promoting Cell Proliferation and Inhibiting Osteogenic Differentiation. Cell Physiol. Biochem. 2015, 37, 2375–2392. [Google Scholar] [CrossRef] [PubMed]
- Lewington, A.; Padanilam, B.J.; Hammerman, M.R. Induction of calcyclin after ischemic injury to rat kidney. Am. J. Physiol. 1997, 273, F380–F385. [Google Scholar] [CrossRef] [PubMed]
- Breen, E.C.; Fu, Z.; Normand, H. Calcyclin gene expression is increased by mechanical strain in fibroblasts and lung. Am. J. Respir. Cell Mol. Biol. 1999, 21, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Leśniak, W.; Szczepańska, A.; Kuźnicki, J. Calcyclin (S100A6) expression is stimulated by agents evoking oxidative stress via the antioxidant response element. Biochim. Biophys. Acta 2005, 1744, 29–37. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kasacka, I.; Piotrowska, Ż.; Filipek, A.; Majewski, M. Influence of doxazosin on biosynthesis of S100A6 and atrial natriuretic factor peptides in the heart of spontaneously hypertensive rats. Exp. Biol. Med. 2016, 241, 375–381. [Google Scholar] [CrossRef]
- Yamada, J.; Jinno, S. Upregulation of calcium binding protein, S100A6, in activated astrocytes is linked to glutamate toxicity. Neuroscience 2012, 226, 119–129. [Google Scholar] [CrossRef]
- Fulda, S.; Gorman, A.M.; Hori, O.; Samali, A. Cellular stress responses: Cell survival and cell death. Int. J. Cell Biol. 2010, 2010, 214074. [Google Scholar] [CrossRef]
- Joo, J.; Yoon, S.Y.; Kim, J.H.; Paik, S.G.; Min, S.R.; Lim, J.S.; Choe, I.S.; Choi, I.; Kim, J.W. S100A6 (calcyclin) enhances the sensitivity to apoptosis via the upregulation of caspase-3 activity in Hep3B cells. J. Cell. Biochem. 2008, 103, 1183–1197. [Google Scholar] [CrossRef]
- Lyu, X.; Li, H.Z.; Ma, X.; Li, X.T.; Gao, Y.; Ni, D.; Shen, D.L.; Gu, L.Y.; Wang, B.J.; Zhang, Y.; et al. Elevated S100A6 (Calcyclin) enhances tumorigenesis and suppresses CXCL14-induced apoptosis in clear cell renal cell carcinoma. Oncotarget 2015, 6, 6656–6669. [Google Scholar] [CrossRef]
- Wirths, O.; Breyhan, H.; Marcello, A.; Cotel, M.C.; Bruck, W.; Bayer, T.A. Inflammatory changes are tightly associated with neurodegeneration in the brain and spinal cord of the APP/PS1KI mouse model of Alzheimer’s disease. Neurobiol. Aging 2010, 31, 747–757. [Google Scholar] [CrossRef] [PubMed]
- Tong, H.; Wang, L.; Zhang, K.; Shi, J.; Wu, Y.; Bao, Y.; Wang, C. S100A6 promotes inflammation and infiltration of mononuclear/macrophages via the p-P38 and p-JNK pathways in acute liver injury. Res. Sq. 2021. [CrossRef]
- Zhang, X.F.; Ma, J.X.; Wang, Y.L.; Ma, X.L. Calcyclin (S100A6) Attenuates Inflammatory Response and Mediates Apoptosis of Chondrocytes in Osteoarthritis via the PI3K/AKT Pathway. Orthop. Surg. 2021, 13, 1094–1101. [Google Scholar] [CrossRef] [PubMed]
- Tian, Z.Y.; Wang, C.Y.; Wang, T.; Li, Y.C.; Wang, Z.Y. Glial S100A6 Degrades β-amyloid Aggregation through Targeting Competition with Zinc Ions. Aging Dis. 2019, 10, 756–769. [Google Scholar] [CrossRef] [PubMed]
- Hagmeyer, S.; Romão, M.A.; Cristóvão, J.S.; Vilella, A.; Zoli, M.; Gomes, C.M.; Grabrucker, A.M. Distribution and Relative Abundance of S100 Proteins in the Brain of the APP23 Alzheimer’s Disease Model Mice. Front. Neurosci. 2019, 13, 640. [Google Scholar] [CrossRef]
- Cheng, C.W.; Rifai, A.; Ka, S.M.; Shui, H.A.; Lin, Y.F.; Lee, W.H.; Chen, A. Calcium-binding proteins annexin A2 and S100A6 are sensors of tubular injury and recovery in acute renal failure. Kidney Int. 2005, 68, 2694–2703. [Google Scholar] [CrossRef]
- Ding, H.; Yu, J.; Chang, W.; Liu, F.; He, Z. Searching for differentially expressed proteins in spinal cord injury based on the proteomics analysis. Life Sci. 2020, 242, 117235. [Google Scholar] [CrossRef]
- Ito, M.; Kizawa, K. Expression of calcium-binding S100 proteins A4 and A6 in regions of the epithelial sac associated with the onset of hair follicle regeneration. J. Investig. Dermatol. 2001, 116, 956–963. [Google Scholar] [CrossRef][Green Version]
- Grahn, T.H.M.; Niroula, A.; Végvári, Á.; Oburoglu, L.; Pertesi, M.; Warsi, S.; Safi, F.; Miharada, N.; Garcia, S.C.; Siva, K.; et al. S100A6 is a critical regulator of hematopoietic stem cells. Leukemia 2020, 34, 3323–3337. [Google Scholar] [CrossRef]
- Bartkowska, K.; Swiatek, I.; Aniszewska, A.; Jurewicz, E.; Turlejski, K.; Filipek, A.; Djavadian, R.L. Stress-Dependent Changes in the CacyBP/SIP Interacting Protein S100A6 in the Mouse Brain. PLoS ONE 2017, 12, e0169760. [Google Scholar] [CrossRef]
- Fang, B.; Liang, M.; Yang, G.; Ye, Y.; Xu, H.; He, X.; Huang, J.H. Expression of S100A6 in Rat Hippocampus after Traumatic Brain Injury Due to Lateral Head Acceleration. Int. J. Mol. Sci. 2014, 15, 6378–6390. [Google Scholar] [CrossRef] [PubMed]
- Thordarson, G.; Southard, J.N.; Talamantes, F. Purification and characterization of mouse decidual calcyclin: A novel stimulator of mouse placental lactogen-II secretion. Endocrinology 1991, 129, 1257–1265. [Google Scholar] [CrossRef] [PubMed]
- Jurewicz, E.; Góral, A.; Filipek, A. S100A6 is secreted from Wharton’s jelly mesenchymal stem cells and interacts with integrin β1. Int. J. Biochem. Cell Biol. 2014, 55, 298–303. [Google Scholar] [CrossRef]
- Stewart, V.D.; Cadieux, J.; Thulasiram, M.R.; Douglas, T.C.; Drewnik, D.A.; Selamat, S.; Lao, Y.; Spicer, V.; Hannila, S.S. Myelin-associated glycoprotein alters the neuronal secretome and stimulates the release of TGFβ and proteins that affect neural plasticity. FEBS Lett. 2022, 596, 2952–2973. [Google Scholar] [CrossRef]
- Celis, J.E.; Gesser, B.; Rasmussen, H.H.; Madsen, P.; Leffers, H.; Dejgaard, K.; Honore, B.; Olsen, E.; Ratz, G.; Lauridsen, J.B.; et al. Comprehensive two-dimensional gel protein databases offer a global approach to the analysis of human cells: The transformed amnion cells (AMA) master database and its link to genome DNA sequence data. Electrophoresis 1990, 11, 989–1071. [Google Scholar] [CrossRef] [PubMed]
- Ohuchida, K.; Mizumoto, K.; Yu, J.; Yamaguchi, H.; Konomi, H.; Nagai, E.; Yamaguchi, K.; Tsuneyoshi, M.; Tanaka, M. S100A6 is increased in a stepwise manner during pancreatic carcinogenesis: Clinical value of expression analysis in 98 pancreatic juice samples. Cancer Epidemiol. Biomark. Prev. 2007, 16, 649–654. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Turnier, J.L.; Fall, N.; Thornton, S.; Witte, D.; Bennett, M.R.; Appenzeller, S.; Klein-Gitelman, M.S.; Grom, A.A.; Brunner, H.I. Urine S100 proteins as potential biomarkers of lupus nephritis activity. Arthritis Res. Ther. 2017, 19, 242. [Google Scholar] [CrossRef]
- Dubois, J.; Rueger, J.; Haubold, B.; Far, R.K.; Sczakiel, G. Transcriptome analyses of urine RNA reveal tumor markers for human bladder cancer: Validated amplicons for RT-qPCR-based detection. Oncotarget 2021, 12, 1011–1023. [Google Scholar] [CrossRef]
- Recalde, J.I.; Duran, J.A.; Rodriguez-Agirretxe, I.; Soria, J.; Sanchez-Tena, M.A.; Pereiro, X.; Suarez, T.; Acera, A. Changes in tear biomarker levels in keratoconus after corneal collagen crosslinking. Mol. Vis. 2019, 25, 12–21. [Google Scholar]
- Assenhöj, M.; Ward, L.J.; Ghafouri, B.; Graff, P.; Ljunggren, S.A. Metal exposure from additive manufacturing and its effect on the nasal lavage fluid proteome—A pilot study. PLoS ONE 2021, 16, e0256746. [Google Scholar] [CrossRef]
- Biji, A.; Khatun, O.; Swaraj, S.; Narayan, R.; Rajmani, R.S.; Sardar, R.; Satish, D.; Mehta, S.; Bindhu, H.; Jeevan, M.; et al. Identification of COVID-19 prognostic markers and therapeutic targets through meta-analysis and validation of Omics data from nasopharyngeal samples. EBioMedicine 2021, 70, 103525. [Google Scholar] [CrossRef] [PubMed]
- Okazaki, K.; Niki, I.; Iino, S.; Kobayashi, S.; Hidaka, H. A role of calcyclin, a Ca(2+)-binding protein, on the Ca(2+)-dependent insulin release from the pancreatic beta cell. J. Biol. Chem. 1994, 269, 6149–6152. [Google Scholar] [CrossRef] [PubMed]
- Fujii, T.; Kuzumaki, N.; Ogoma, Y.; Kondo, Y. Effects of calcium-binding proteins on histamine release from permeabilized rat peritoneal mast cells. Biol. Pharm. Bull. 1994, 17, 581–585. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wei, B.R.; Hoover, S.B.; Ross, M.M.; Zhou, W.; Meani, F.; Edwards, J.B.; Spehalski, E.I.; Risinger, J.I.; Alvord, W.G.; Quiñones, O.A.; et al. Serum S100A6 concentration predicts peritoneal tumor burden in mice with epithelial ovarian cancer and is associated with advanced stage in patients. PLoS ONE 2009, 4, e7670. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, K.; Jiang, X.; Zhang, J. S100A6 as a potential serum prognostic biomarker and therapeutic target in gastric cancer. Dig. Dis. Sci. 2014, 59, 2136–2144. [Google Scholar] [CrossRef]
- Nishi, M.; Matsumoto, K.; Kobayashi, M.; Yanagita, K.; Matsumoto, T.; Nagashio, R.; Ishii, D.; Fujita, T.; Sato, Y.; Iwamura, M. Serum expression of S100A6 is a potential detection marker in patients with urothelial carcinoma in the urinary bladder. Biomed. Res. 2014, 35, 351–356. [Google Scholar] [CrossRef]
- Ismail, M.F.; El Boghdady, N.A.; Shabayek, M.I.; Awida, H.A.; Abozeed, H. Evaluation and screening of mRNA S100A genes as serological biomarkers in different stages of bladder cancer in Egypt. Tumour Biol. 2016, 37, 4621–4631. [Google Scholar] [CrossRef]
- Wang, T.; Liang, Y.; Thakur, A.; Zhang, S.; Yang, T.; Chen, T.; Gao, L.; Chen, M.; Ren, H. Diagnostic significance of S100A2 and S100A6 levels in sera of patients with non-small cell lung cancer. Tumour Biol. 2016, 37, 2299–2304. [Google Scholar] [CrossRef]
- Bai, Y.; Li, L.D.; Li, J.; Lu, X. Prognostic values of S100 family members in ovarian cancer patients. BMC Cancer 2018, 18, 1256. [Google Scholar] [CrossRef]
- Cai, X.Y.; Lu, L.; Wang, Y.N.; Jin, C.; Zhang, R.Y.; Zhang, Q.; Chen, Q.J.; Shen, W.F. Association of increased S100B, S100A6 and S100P in serum levels with acute coronary syndrome and also with the severity of myocardial infarction in cardiac tissue of rat models with ischemia-reperfusion injury. Atherosclerosis 2011, 217, 536–542. [Google Scholar] [CrossRef]
- Dong, X.H.; Dai, D.; Yang, Z.D.; Yu, X.O.; Li, H.; Kang, H. S100 calcium binding protein A6 and associated long noncoding ribonucleic acids as biomarkers in the diagnosis and staging of primary biliary cholangitis. World J. Gastroenterol. 2021, 27, 1973–1992. [Google Scholar] [CrossRef]
- Güzel, C.; van den Berg, C.B.; Duvekot, J.J.; Stingl, C.; van den Bosch, T.P.P.; van der Weiden, M.; Steegers, E.A.P.; Steegers-Theunisse, R.P.M.; Luider, T.M. Quantification of Calcyclin and Heat Shock Protein 90 in Sera from Women with and without Preeclampsia by Mass Spectrometry. Proteom. Clin. Appl. 2019, 13, e1800181. [Google Scholar] [CrossRef] [PubMed]
- Landi, C.; Bargagli, E.; Bianchi, L.; Gagliardi, A.; Carleo, A.; Bennett, D.; Perari, M.G.; Armini, A.; Prasse, A.; Rottoli, P.; et al. Towards a functional proteomics approach to the comprehension of idiopathic pulmonary fibrosis, sarcoidosis, systemic sclerosis and pulmonary Langerhans cell histiocytosis. J. Proteom. 2013, 83, 60–75. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Chen, P.W.; Tsai, P.J.; Su, S.H.; Liao, P.C. Proteomics analysis revealed changes in rat bronchoalveolar lavage fluid proteins associated with oil mist exposure. Proteomics 2006, 6, 2236–2250. [Google Scholar] [CrossRef] [PubMed]
- Benitez-Del-Castillo, J.M.; Soria, J.; Acera, A.; Muñoz, A.M.; Rodríguez, S.; Suárez, T. Quantification of a panel for dry-eye protein biomarkers in tears: A comparative pilot study using standard ELISA and customized microarrays. Mol. Vis. 2021, 27, 243–261. [Google Scholar] [PubMed]
- Valencia, E.; García, M.; Fernández-Vega, B.; Pereiro, R.; Lobo, L.; González-Iglesias, H. Targeted Analysis of Tears Revealed Specific Altered Metal Homeostasis in Age-Related Macular Degeneration. Investig. Ophthalmol. Vis. Sci. 2022, 63, 10. [Google Scholar] [CrossRef]
- Klein, L.L.; Freitag, B.C.; Gibbs, R.S.; Reddy, A.P.; Nagalla, S.R.; Gravett, M.G. Detection of intra-amniotic infection in a rabbit model by proteomics-based amniotic fluid analysis. Am. J. Obstet. Gynecol. 2005, 193, 1302–1306. [Google Scholar] [CrossRef]
- Patgaonkar, M.; Aranha, C.; Bhonde, G.; Reddy, K.V. Identification and characterization of anti-microbial peptides from rabbit vaginal fluid. Vet. Immunol. Immunopathol. 2011, 139, 176–186. [Google Scholar] [CrossRef]
- Zhang, S.P.; Wu, Z.Z.; Wu, Y.W.; Su, S.B.; Tong, J. Mechanism study of adaptive response in high background radiation area of Yangjiang in China. Zhonghua Yu Fang Yi Xue Za Zhi 2010, 44, 815–819. (In Chinese) [Google Scholar]
- Henderson, N.C.; Rieder, F.; Wynn, T.A. Fibrosis: From mechanisms to medicines. Nature 2020, 587, 555–566. [Google Scholar] [CrossRef]
- Krenkel, O.; Hundertmark, J.; Ritz, T.P.; Weiskirchen, R.; Tacke, F. Single Cell RNA Sequencing Identifies Subsets of Hepatic Stellate Cells and Myofibroblasts in Liver Fibrosis. Cells 2019, 8, 503. [Google Scholar] [CrossRef] [PubMed]
- Landi, C.; Bargagli, E.; Carleo, A.; Refini, R.M.; Bennett, D.; Bianchi, L.; Cillis, G.; Prasse, A.; Bini, L.; Rottoli, P. Bronchoalveolar lavage proteomic analysis in pulmonary fibrosis associated with systemic sclerosis: S100A6 and 14-3-3ε as potential biomarkers. Rheumatology 2019, 58, 165–178. [Google Scholar] [PubMed]
- Ju, W.; Eichinger, F.; Bitzer, M.; Oh, J.; McWeeney, S.; Berthier, C.C.; Shedden, K.; Cohen, C.D.; Henger, A.; Krick, S.; et al. Renal gene and protein expression signatures for prediction of kidney disease progression. Am. J. Pathol. 2009, 174, 2073–2085. [Google Scholar] [CrossRef]
- Stanton, L.W.; Garrard, L.J.; Damm, D.; Garrick, B.L.; Lam, A.; Kapoun, A.M.; Zheng, Q.; Protter, A.A.; Schreiner, G.F.; White, R.T. Altered patterns of gene expression in response to myocardial infarction. Circ. Res. 2000, 86, 939–945. [Google Scholar] [CrossRef] [PubMed]
- Xia, P.; He, H.; Kristine, M.S.; Guan, W.; Gao, J.; Wang, Z.; Hu, J.; Han, L.; Li, J.; Han, W.; et al. Therapeutic effects of recombinant human S100A6 and soluble receptor for advanced glycation end products(sRAGE) on CCl4-induced liver fibrosis in mice. Eur. J. Pharmacol. 2018, 833, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Boom, A.; Pochet, R.; Authelet, M.; Pradier, L.; Borghgraef, P.; Van Leuven, F.; Heizmann, C.W.; Brion, J.P. Astrocytic calcium/zinc binding protein S100A6 over expression in Alzheimer’s disease and in PS1/APP transgenic mice models. Biochim. Biophys. Acta 2004, 1742, 161–168. [Google Scholar] [CrossRef]
- Astillero-Lopez, V.; Gonzalez-Rodriguez, M.; Villar-Conde, S.; Flores-Cuadrado, A.; Martinez-Marcos, A.; Ubeda-Banon, I.; Saiz-Sanchez, D. Neurodegeneration and astrogliosis in the entorhinal cortex in Alzheimer’s disease: Stereological layer-specific assessment and proteomic analysis. Alzheimers Dement. 2022, 18, 2468–2480. [Google Scholar] [CrossRef]
- Hoyaux, D.; Alao, J.; Fuchs, J.; Kiss, R.; Keller, B.; Heizmann, C.W.; Pochet, R.; Frermann, D. S100A6, a calcium- and zinc-binding protein, is overexpressed in SOD1 mutant mice, a model for amyotrophic lateral sclerosis. Biochim. Biophys. Acta 2000, 1498, 264–272. [Google Scholar] [CrossRef]
- Hoyaux, D.; Boom, A.; Van Den Bosch, L.; Belot, N.; Martin, J.-J.; Heizmann, C.W.; Kiss, R.; Pochet, R. S100A6 Overexpression within Astrocytes Associated with Impaired Axons from Both ALS Mouse Model and Human Patients. J. Neuropath. Exp. Neurol. 2002, 61, 736–744. [Google Scholar] [CrossRef]
- Iridoy, M.O.; Zubiri, I.; Zelaya, M.V.; Martinez, L.; Ausín, K.; Lachen-Montes, M.; Santamaría, E.; Fernandez-Irigoyen, J.; Jericó, I. Neuroanatomical Quantitative Proteomics Reveals Common Pathogenic Biological Routes between Amyotrophic Lateral Sclerosis (ALS) and Frontotemporal Dementia (FTD). Int. J. Mol. Sci. 2019, 20, 4. [Google Scholar] [CrossRef]
- Filipek, A.; Leśniak, W. S100A6 and Its Brain Ligands in Neurodegenerative Disorders. Int. J. Mol. Sci. 2020, 21, 3979. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Chen, L.; Li, Z.; Song, Y.; Yuan, Y.; Liu, T.; Hong, J.; Wang, Q.; Chang, H.; Kuang, Z.; et al. Potential Serum Biomarkers for Postoperative Neurocognitive Disorders Based on Proteomic Analysis of Cognitive-Related Brain Regions. Front. Aging Neurosci. 2021, 13, 741263. [Google Scholar] [CrossRef] [PubMed]
- Jurewicz, E.; Filipek, A. Ca2+- binding proteins of the S100 family in preeclampsia. Placenta 2022, 127, 43–51. [Google Scholar] [CrossRef]
- Peng, Y.; Lin, J.; Ma, J.; Lin, K.; Xu, K.; Lin, J. Upregulation of S100A6 in patients with endometriosis and its role in ectopic endometrial stromal cells. Gynecol. Endocrinol. 2018, 34, 815–820. [Google Scholar] [CrossRef] [PubMed]
- Allgöwer, C.; Kretz, A.L.; von Karstedt, S.; Wittau, M.; Henne-Bruns, D.; Lemke, J. Friend or Foe: S100 Proteins in Cancer. Cancers 2020, 12, 2037. [Google Scholar] [CrossRef]
- Weterman, M.A.; Stoopen, G.M.; van Muijen, G.N.; Kuznicki, J.; Ruiter, D.J.; Bloemers, H.P. Expression of calcyclin in human melanoma cell lines correlates with metastatic behavior in nude mice. Cancer Res. 1992, 52, 1291–1296. [Google Scholar]
- Komatsu, K.; Andoh, A.; Ishiguro, S.; Suzuki, N.; Hunai, H.; Kobune-Fujiwara, Y.; Kameyama, M.; Miyoshi, J.; Akedo, H.; Nakamura, H. Increased expression of S100A6 (Calcyclin), a calcium-binding protein of the S100 family, in human colorectal adenocarcinomas. Clin. Cancer Res. 2000, 6, 172–177. [Google Scholar]
- Yang, Y.Q.; Zhang, L.J.; Dong, H.; Jiang, C.L.; Zhu, Z.G.; Wu, J.X.; Wu, Y.L.; Han, J.S.; Xiao, H.S.; Gao, H.J.; et al. Upregulated expression of S100A6 in human gastric cancer. J. Dig. Dis. 2007, 8, 186–193. [Google Scholar] [CrossRef]
- Kim, J.; Kim, J.; Yoon, S.; Joo, J.; Lee, Y.; Lee, K.; Chung, J.; Choe, I. S100A6 protein as a marker for differential diagnosis of cholangiocarcinoma from hepatocellular carcinoma. Hepatol. Res. 2002, 23, 274. [Google Scholar] [CrossRef]
- Onsurathum, S.; Haonon, O.; Pinlaor, P.; Pairojkul, C.; Khuntikeo, N.; Thanan, R.; Roytrakul, S.; Pinlaor, S. Proteomics detection of S100A6 in tumor tissue interstitial fluid and evaluation of its potential as a biomarker of cholangiocarcinoma. Tumour Biol. 2018, 40, 1010428318767195. [Google Scholar] [CrossRef]
- Zhang, C.; Yao, R.; Chen, J.; Zou, Q.; Zeng, L. S100 family members: Potential therapeutic target in patients with hepatocellular carcinoma: A STROBE study. Medicine 2021, 100, e24135. [Google Scholar] [CrossRef] [PubMed]
- Melle, C.; Ernst, G.; Schimmel, B.; Bleul, A.; von Eggeling, F. Colon-derived liver metastasis, colorectal carcinoma, and hepatocellular carcinoma can be discriminated by the Ca(2+)-binding proteins S100A6 and S100A11. PLoS ONE 2008, 3, e3767. [Google Scholar] [CrossRef] [PubMed]
- Peterova, E.; Bures, J.; Moravkova, P.; Kohoutova, D. Tissue mRNA for S100A4, S100A6, S100A8, S100A9, S100A11 and S100P Proteins in Colorectal Neoplasia: A Pilot Study. Molecules 2021, 26, 402. [Google Scholar] [CrossRef] [PubMed]
- Jia, R.; Sui, Z.; Zhang, H.; Yu, Z. Identification and Validation of Immune-Related Gene Signature for Predicting Lymph Node Metastasis and Prognosis in Lung Adenocarcinoma. Front. Mol. Biosci. 2021, 8, 679031. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Li, X.; Xie, J.; Zhu, Q.; Yuan, Y. A Novel Immune-Related Prognostic Signature Predicting Survival in Patients with Pancreatic Adenocarcinoma. J. Oncol. 2022, 2022, 8909631. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).