The Anion Channel TMEM16a/Ano1 Modulates CFTR Activity, but Does Not Function as an Apical Anion Channel in Colonic Epithelium from Cystic Fibrosis Patients and Healthy Individuals
Abstract
1. Introduction
2. Results
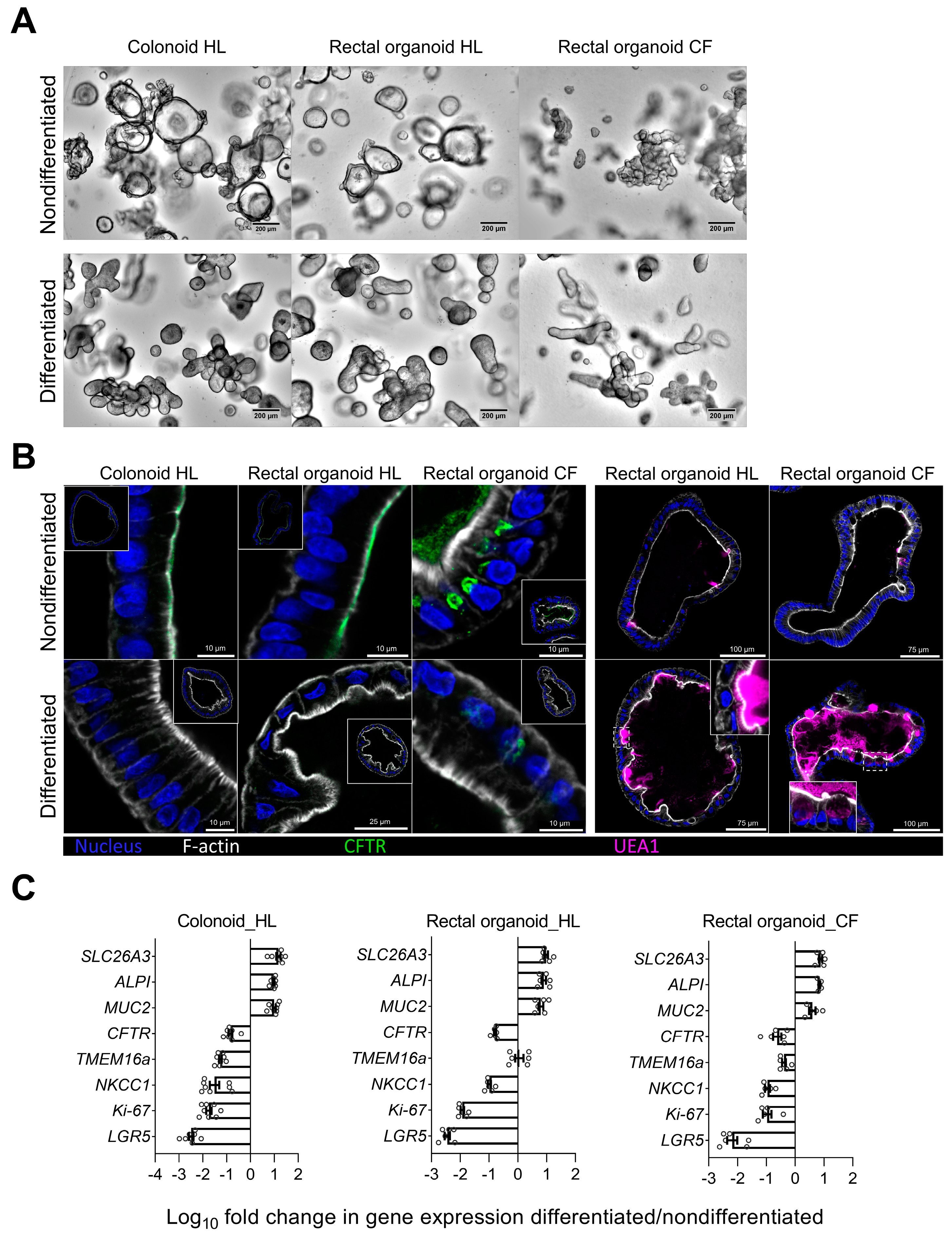
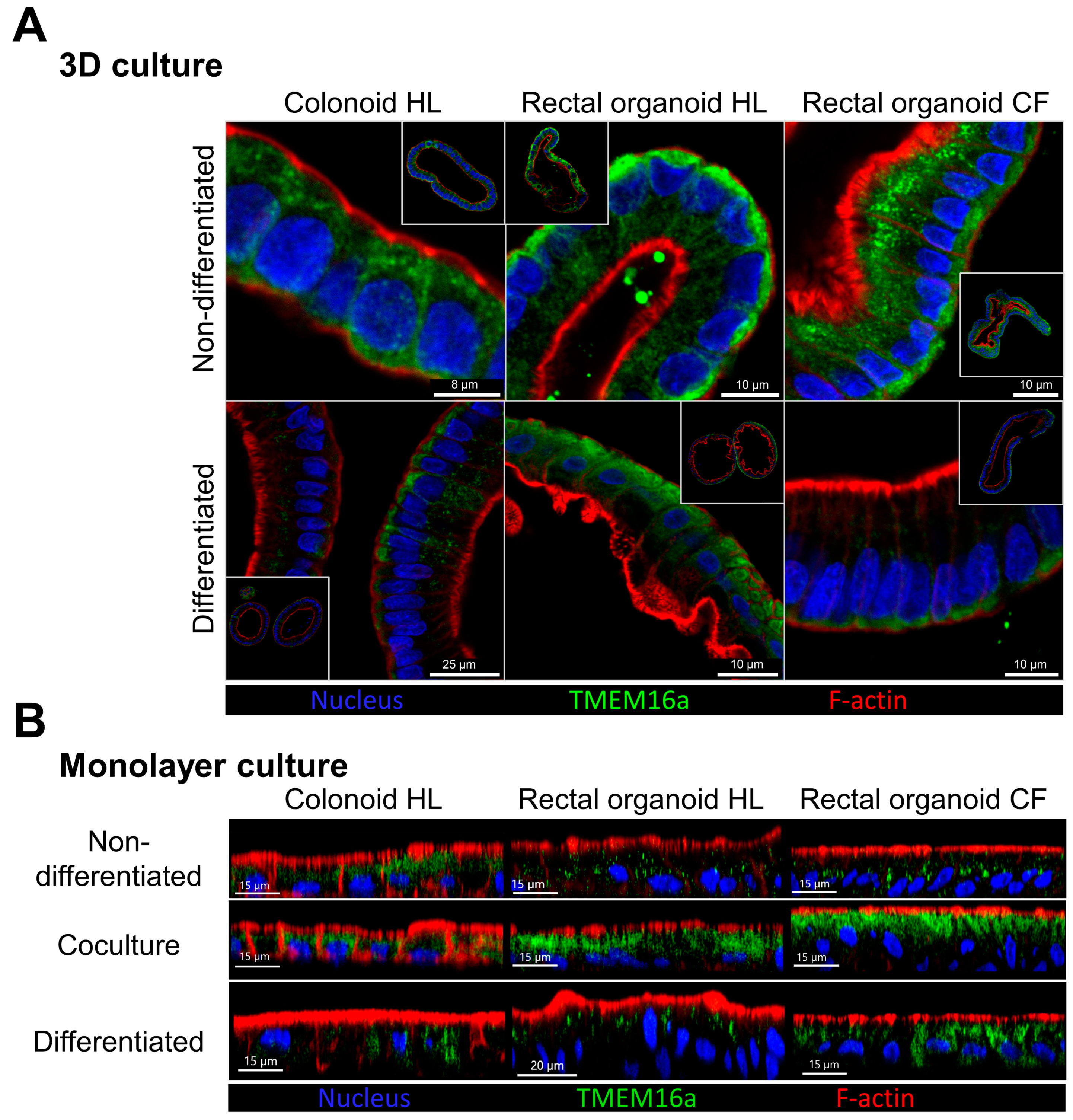
2.1. Morphological Features and Expression Profile of Differentiation Markers and Ion Transporters in Nondifferentiated and Differentiated 3D Transverse Colonic and Rectal Organoids from Healthy Volunteers and PwCF
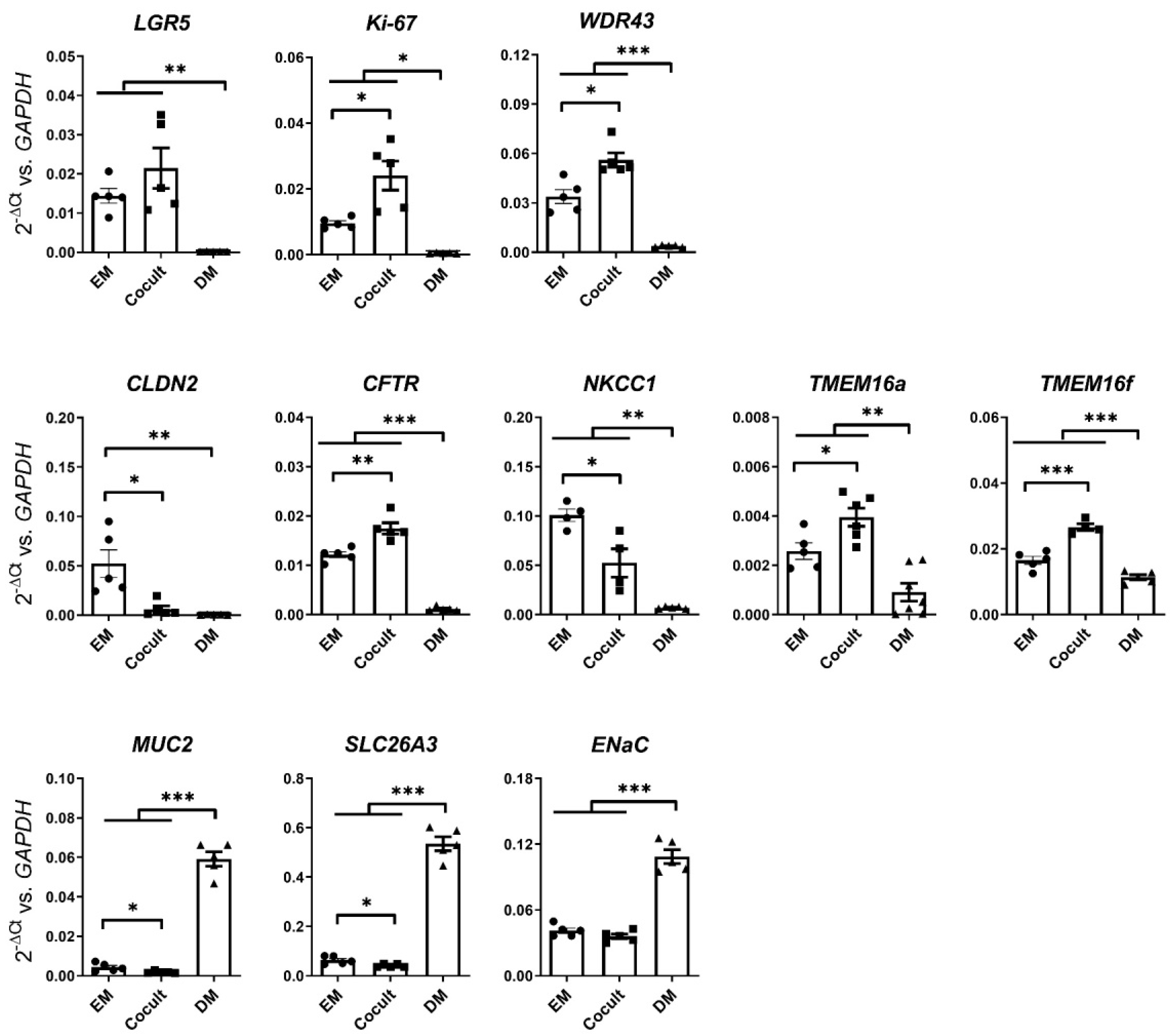
2.2. Modeling of Two-Dimensional Transverse Colon Organoid Monolayers with Myofibroblast Coculture
2.3. Electrophysiological Assessment of Anion Channel Activity in CM–-CE Monolayers
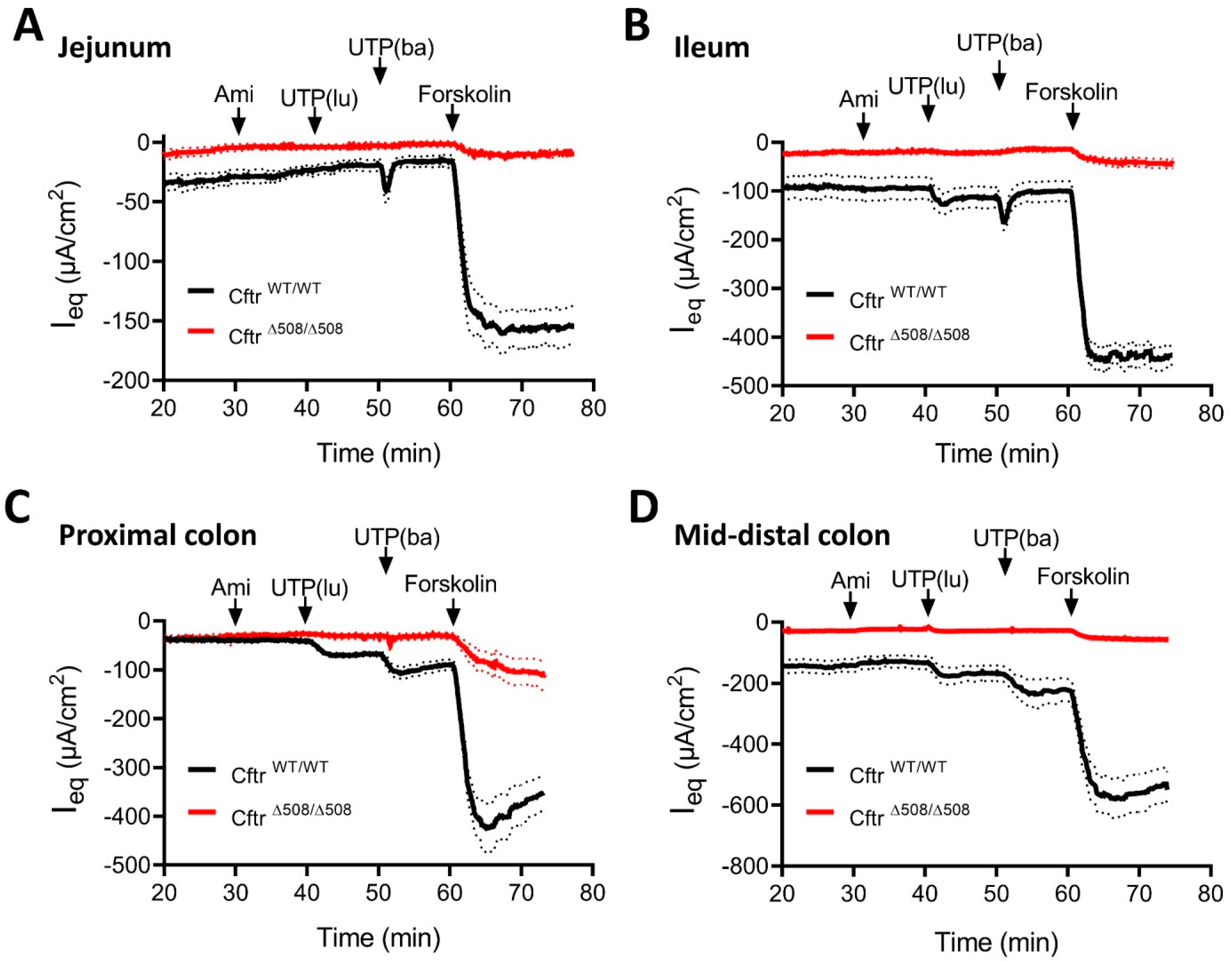
2.4. Electrophysiological Studies in Intestinal Mucosa from F508del Homozygous and WT Mice
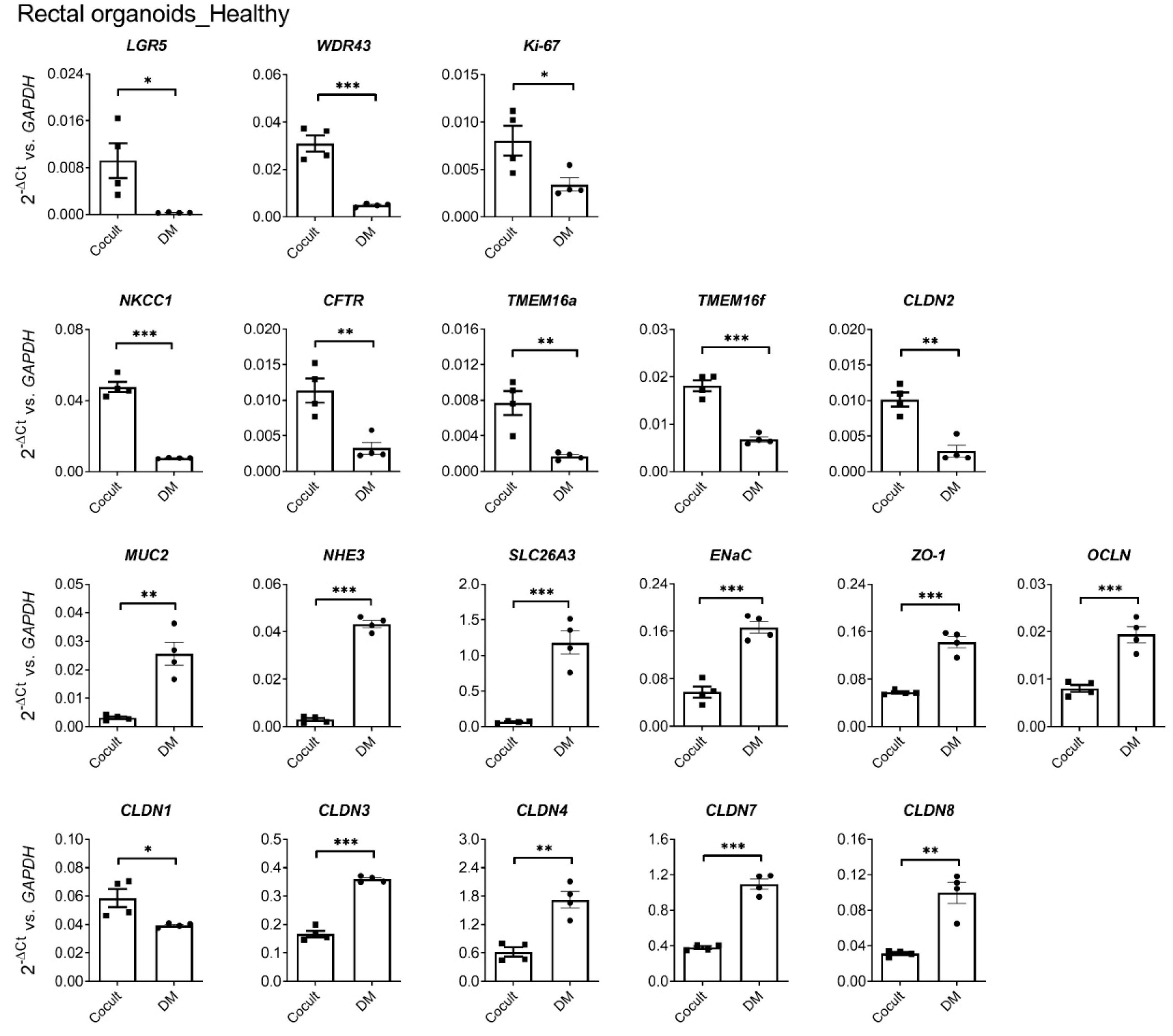
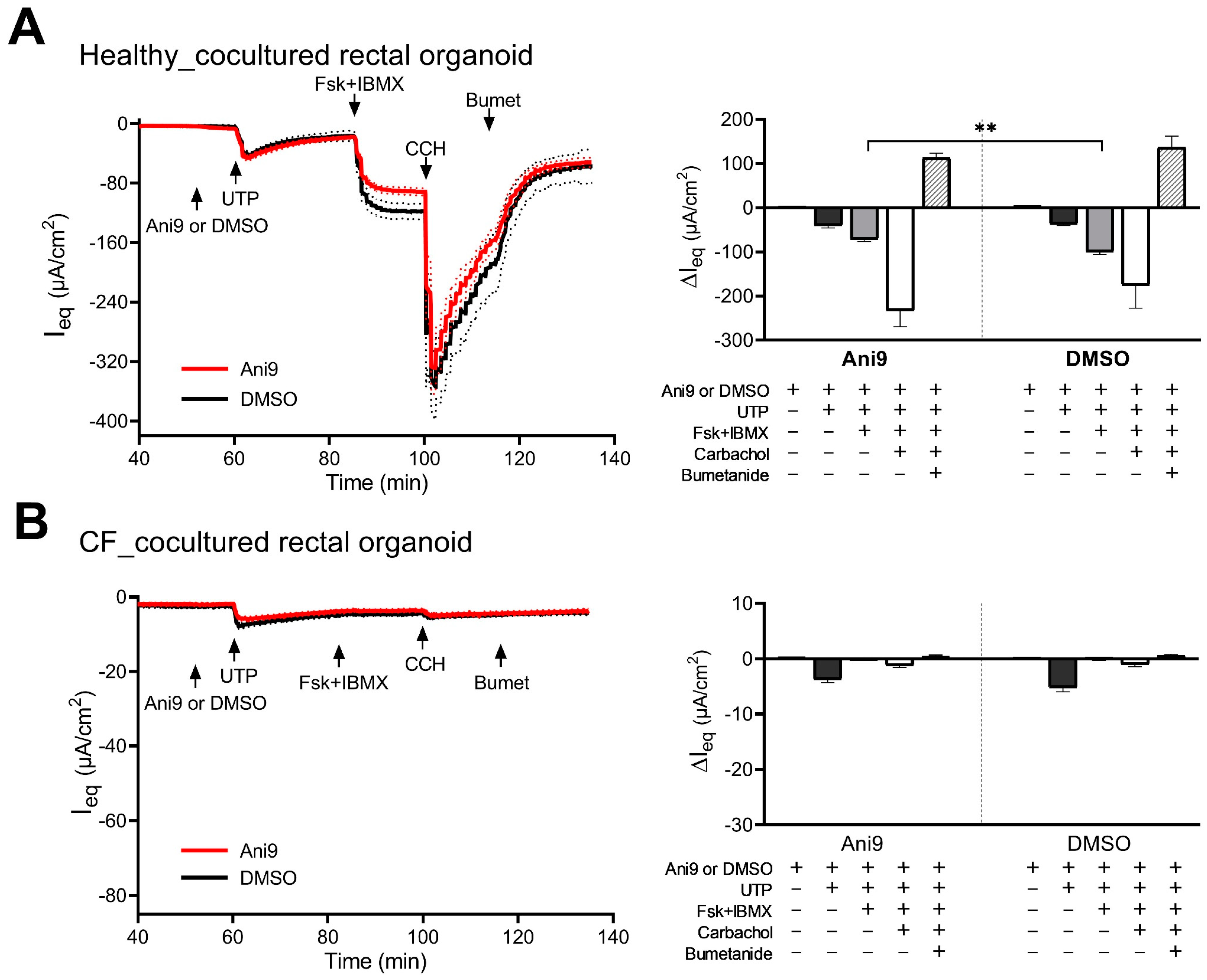
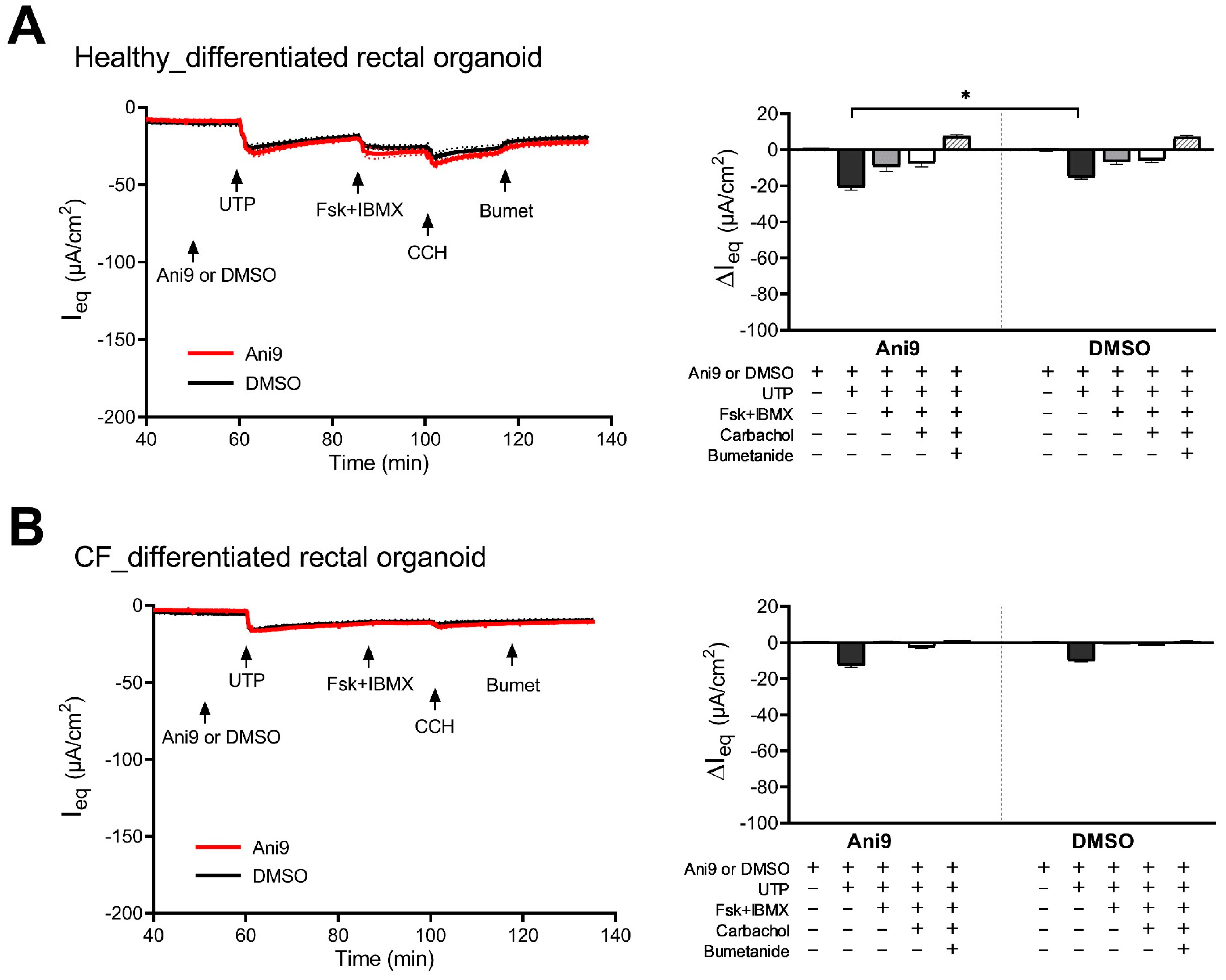
2.5. Modeling of Two-Dimensional Rectal Organoid Monolayers with Myofibroblast Coculture
2.6. Electrophysiological Experiments in RM–RE Monolayers from HL and Patients with Cystic Fibrosis
3. Discussion
4. Material and Methods
4.1. Human Subjects
4.2. Mice
4.3. Human Organoid Cultures and Cocultures with Myofibroblasts
4.4. Immunocytochemical Localization of TMEM16a and CFTR in Intestinal 2D and 3D Cultures
4.5. Electrophysiological Measurements in CM-CE and Differentiated Monolayers
4.6. Electrophysiological Measurements in Proximal and Mid-Distal Isolated Colonic Mucosa from F508del and WT Mice
4.7. RT-qPCR Analysis
4.8. Bioinformatic Analysis and Statistics
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, J.; Walker, N.M.; Ootani, A.; Strubberg, A.M.; Clarke, L.L. Defective goblet cell exocytosis contributes to murine cystic fibrosis-associated intestinal disease. J. Clin. Investig. 2015, 125, 1056–1068. [Google Scholar] [CrossRef]
- Garcia, M.A.; Yang, N.; Quinton, P.M. Normal mouse intestinal mucus release requires cystic fibrosis transmembrane regulator-dependent bicarbonate secretion. J. Clin. Investig. 2009, 119, 2613–2622. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, J.K.; Ermund, A.; Ambort, D.; Johansson, M.E.; Nilsson, H.E.; Thorell, K.; Hebert, H.; Sjövall, H.; Hansson, G.C. Bicarbonate and functional CFTR channel are required for proper mucin secretion and link cystic fibrosis with its mucus phenotype. J. Exp. Med. 2012, 209, 1263–1272. [Google Scholar] [CrossRef] [PubMed]
- Quinton, P.M. Cystic fibrosis: Impaired bicarbonate secretion and mucoviscidosis. Lancet 2008, 372, 415–417. [Google Scholar] [CrossRef]
- Braun, J.; Mundhenk, L.; Range, F.; Gruber, A.D. Quantitative expression analyses of candidates for alternative anion conductance in cystic fibrosis mouse models. J. Cyst. Fibros. Off. J. Eur. Cyst. Fibros. Soc. 2010, 9, 351–364. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pinto, M.C.; Silva, I.A.L.; Figueira, M.F.; Amaral, M.D.; Lopes-Pacheco, M. Pharmacological Modulation of Ion Channels for the Treatment of Cystic Fibrosis. J. Exp. Pharmacol. 2021, 13, 693–723. [Google Scholar] [CrossRef]
- Li, H.; Salomon, J.J.; Sheppard, D.N.; Mall, M.A.; Galietta, L.J. Bypassing CFTR dysfunction in cystic fibrosis with alternative pathways for anion transport. Curr. Opin. Pharmacol. 2017, 34, 91–97. [Google Scholar] [CrossRef]
- Mall, M.; Wissner, A.; Seydewitz, H.H.; Kuehr, J.; Brandis, M.; Greger, R.; Kunzelmann, K. Defective cholinergic Cl− secretion and detection of K+ secretion in rectal biopsies from cystic fibrosis patients. Am. J. Physiol. Gastrointest. Liver Physiol. 2000, 278, G617–G624. [Google Scholar] [CrossRef]
- Kunzelmann, K.; Centeio, R.; Wanitchakool, P.; Cabrita, I.; Benedetto, R.; Saha, T.; Hoque, K.M.; Schreiber, R. Control of Ion Transport by Tmem16a Expressed in Murine Intestine. Front. Physiol. 2019, 10, 1262. [Google Scholar] [CrossRef]
- Veeze, H.J.; Halley, D.J.; Bijman, J.; de Jongste, J.C.; de Jonge, H.R.; Sinaasappel, M. Determinants of mild clinical symptoms in cystic fibrosis patients. Residual chloride secretion measured in rectal biopsies in relation to the genotype. J. Clin. Investig. 1994, 93, 461–466. [Google Scholar]
- Rozmahel, R.; Wilschanski, M.; Matin, A.; Plyte, S.; Oliver, M.; Auerbach, W.; Moore, A.; Forstner, J.; Durie, P.; Nadeau, J.; et al. Modulation of disease severity in cystic fibrosis transmembrane conductance regulator deficient mice by a secondary genetic factor. Nat. Genet. 1996, 12, 280–287. [Google Scholar] [CrossRef]
- Wilschanski, M.A.; Rozmahel, R.; Beharry, S.; Kent, G.; Li, C.; Tsui, L.C.; Durie, P.; Bear, C.E. In vivo measurements of ion transport in long-living CF mice. Biochem. Biophys. Res. Commun. 1996, 219, 753–759. [Google Scholar] [CrossRef]
- Lee, B.; Hong, G.S.; Lee, S.H.; Kim, H.; Kim, A.; Hwang, E.M.; Kim, J.; Lee, M.G.; Yang, J.Y.; Kweon, M.N.; et al. Anoctamin 1/TMEM16A controls intestinal Cl− secretion induced by carbachol and cholera toxin. Exp. Mol. Med. 2019, 51, 1–14. [Google Scholar] [CrossRef]
- Saha, T.; Aoun, J.; Hayashi, M.; Ali, S.I.; Sarkar, P.; Bag, P.K.; Leblanc, N.; Ameen, N.; Woodward, O.M.; Hoque, K.M. Intestinal TMEM16A control luminal chloride secretion in a NHERF1 dependent manner. Biochem. Biophys. Rep. 2021, 25, 100912. [Google Scholar] [CrossRef]
- Xiao, F.; Li, J.; Singh, A.K.; Riederer, B.; Wang, J.; Sultan, A.; Park, H.; Lee, M.G.; Lamprecht, G.; Scholte, B.J.; et al. Rescue of epithelial HCO3- secretion in murine intestine by apical membrane expression of the cystic fibrosis transmembrane conductance regulator mutant F508del. J. Physiol. 2012, 590, 5317–5334. [Google Scholar] [CrossRef]
- Dekkers, J.F.; Wiegerinck, C.L.; de Jonge, H.R.; Bronsveld, I.; Janssens, H.M.; de Winter-de Groot, K.M.; Brandsma, A.M.; de Jong, N.W.M.; Bijvelds, M.J.C.; Scholte, B.J.; et al. A functional CFTR assay using primary cystic fibrosis intestinal organoids. Nat. Med. 2013, 19, 939–945. [Google Scholar] [CrossRef] [PubMed]
- Foulke-Abel, J.; In, J.; Yin, J.Y.; Zachos, N.C.; Kovbasnjuk, O.; Estes, M.K.; de Jonge, H.; Donowitz, M. Human Enteroids as a Model of Upper Small Intestinal Ion Transport Physiology and Pathophysiology. Gastroenterology 2016, 150, 638–649. [Google Scholar] [CrossRef]
- Salari, A.; Zhou, K.; Nikolovska, K.; Seidler, U.; Amiri, M. Human Colonoid-Myofibroblast Coculture for Study of Apical Na+/H+ Exchangers of the Lower Cryptal Neck Region. Int. J. Mol. Sci. 2023, 24, 4266. [Google Scholar] [CrossRef]
- Strong, T.V.; Boehm, K.; Collins, F.S. Localization of cystic fibrosis transmembrane conductance regulator mRNA in the human gastrointestinal tract by in situ hybridization. J. Clin. Investig. 1994, 93, 347–354. [Google Scholar] [CrossRef]
- Vega, G.; Guequén, A.; Johansson, M.E.V.; Arike, L.; Martínez-Abad, B.; Nyström, E.E.L.; Scudieri, P.; Pedemonte, N.; Millar-Büchner, P.; Philp, A.R.; et al. Normal Calcium-Activated Anion Secretion in a Mouse Selectively Lacking TMEM16A in Intestinal Epithelium. Front. Physiol. 2019, 10, 694. [Google Scholar] [CrossRef]
- Gomez-Pinilla, P.J.; Gibbons, S.J.; Bardsley, M.R.; Lorincz, A.; Pozo, M.J.; Pasricha, P.J.; Van de Rijn, M.; West, R.B.; Sarr, M.G.; Kendrick, M.L.; et al. Ano1 is a selective marker of interstitial cells of Cajal in the human and mouse gastrointestinal tract. Am. J. Physiol. Gastrointest. Liver Physiol. 2009, 296, G1370–G1381. [Google Scholar] [CrossRef] [PubMed]
- Centeio, R.; Cabrita, I.; Benedetto, R.; Talbi, K.; Ousingsawat, J.; Schreiber, R.; Sullivan, J.K.; Kunzelmann, K. Pharmacological Inhibition and Activation of the Ca2+ Activated Cl− Channel TMEM16A. Int. J. Mol. Sci. 2020, 21, 2557. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.; Lee, H.K.; Park, J.; Jeon, D.K.; Jo, S.; Jo, M.; Namkung, W. Ani9, A Novel Potent Small-Molecule ANO1 Inhibitor with Negligible Effect on ANO2. PLoS ONE 2016, 11, e0155771. [Google Scholar] [CrossRef] [PubMed]
- Romanenko, V.G.; Catalán, M.A.; Brown, D.A.; Putzier, I.; Hartzell, H.C.; Marmorstein, A.D.; Gonzalez-Begne, M.; Rock, J.R.; Harfe, B.D.; Melvin, J.E. Tmem16A encodes the Ca2+-activated Cl- channel in mouse submandibular salivary gland acinar cells. J. Biol. Chem. 2010, 285, 12990–13001. [Google Scholar] [CrossRef]
- Scudieri, P.; Caci, E.; Bruno, S.; Ferrera, L.; Schiavon, M.; Sondo, E.; Tomati, V.; Gianotti, A.; Zegarra-Moran, O.; Pedemonte, N.; et al. Association of TMEM16A chloride channel overexpression with airway goblet cell metaplasia. J. Physiol. 2012, 590, 6141–6155. [Google Scholar] [CrossRef]
- Ousingsawat, J.; Centeio, R.; Schreiber, R.; Kunzelmann, K. Expression of SLC26A9 in Airways and Its Potential Role in Asthma. Int. J. Mol. Sci. 2022, 23, 2998. [Google Scholar] [CrossRef]
- Matos, J.E.; Sorensen, M.V.; Geyti, C.S.; Robaye, B.; Boeynaems, J.M.; Leipziger, J. Distal colonic Na+ absorption inhibited by luminal P2Y2 receptors. Pflug. Arch. Eur. J. Physiol. 2007, 454, 977–987. [Google Scholar] [CrossRef]
- Ghanem, E.; Robaye, B.; Leal, T.; Leipziger, J.; Van Driessche, W.; Beauwens, R.; Boeynaems, J.M. The role of epithelial P2Y2 and P2Y4 receptors in the regulation of intestinal chloride secretion. Br. J. Pharmacol. 2005, 146, 364–369. [Google Scholar] [CrossRef]
- Inoue, C.N.; Woo, J.S.; Schwiebert, E.M.; Morita, T.; Hanaoka, K.; Guggino, S.E.; Guggino, W.B. Role of purinergic receptors in chloride secretion in Caco-2 cells. Am. J. Physiol. 1997, 272, C1862–C1870. [Google Scholar] [CrossRef]
- Pedemonte, N.; Galietta, L.J. Structure and function of TMEM16 proteins (anoctamins). Physiol. Rev. 2014, 94, 419–459. [Google Scholar] [CrossRef]
- Danahay, H.; Gosling, M. TMEM16A: An Alternative Approach to Restoring Airway Anion Secretion in Cystic Fibrosis? Int. J. Mol. Sci. 2020, 21, 2386. [Google Scholar] [CrossRef] [PubMed]
- Yule, A.; Sills, D.; Smith, S.; Spiller, R.; Smyth, A.R. Thinking outside the box: A review of gastrointestinal symptoms and complications in cystic fibrosis. Expert Rev. Respir. Med. 2023, 17, 547–561. [Google Scholar] [CrossRef] [PubMed]
- Ward, A.; Mauleon, R.; Arellano, J.; Ooi, C.Y.; Rosic, N. Critical disease burdens of Australian adults with cystic fibrosis: Results from an online survey. Pediatr. Pulmonol. 2023, 58, 1931–1941. [Google Scholar] [CrossRef] [PubMed]
- Moshiree, B.; Freeman, A.J.; Vu, P.T.; Khan, U.; Ufret-Vincenty, C.; Heltshe, S.L.; Goss, C.H.; Schwarzenberg, S.J.; Freedman, S.D.; Borowitz, D.; et al. Multicenter prospective study showing a high gastrointestinal symptom burden in cystic fibrosis. J. Cyst. Fibros. Off. J. Eur. Cyst. Fibros. Soc. 2023, 22, 266–274. [Google Scholar] [CrossRef]
- Ley, D.; Turck, D. Digestive outcomes in Cystic fibrosis. Best. Pract. Res. Clin. Gastroenterol. 2022, 56–57, 101788. [Google Scholar] [CrossRef]
- Rodenburg, L.W.; Delpiano, L.; Railean, V.; Centeio, R.; Pinto, M.C.; Smits, S.M.A.; van der Windt, I.S.; van Hugten, C.F.J.; van Beuningen, S.F.B.; Rodenburg, R.N.P.; et al. Drug Repurposing for Cystic Fibrosis: Identification of Drugs That Induce CFTR-Independent Fluid Secretion in Nasal Organoids. Int. J. Mol. Sci. 2022, 23, 12657. [Google Scholar] [CrossRef]
- Tan, Q.H.; Stefano, G.; Tan, X.J.; Renjie, X.; Romermann, D.; Talbot, S.R.; Seidler, U.E. Inhibition of Na+/H+ exchanger isoform 3 improves gut fluidity and alkalinity in cystic fibrosis transmembrane conductance regulator-deficient and F508del mutant mice. Br. J. Pharmacol. 2021, 178, 1018–1036. [Google Scholar] [CrossRef] [PubMed]
- Tan, X.J.; Kini, A.; Romermann, D.; Seidler, U. The NHE3 Inhibitor Tenapanor Prevents Intestinal Obstructions in CFTR-Deleted Mice. Int. J. Mol. Sci. 2022, 23, 9993. [Google Scholar] [CrossRef]
- Sørensen, M.V.; Sausbier, M.; Ruth, P.; Seidler, U.; Riederer, B.; Praetorius, H.A.; Leipziger, J. Adrenaline-induced colonic K+ secretion is mediated by KCa1.1 (BK) channels. J. Physiol. 2010, 588, 1763–1777. [Google Scholar] [CrossRef] [PubMed]
- Seidler, U.; Blumenstein, I.; Kretz, A.; Viellard-Baron, D.; Rossmann, H.; Colledge, W.H.; Evans, M.; Ratcliff, R.; Gregor, M. A functional CFTR protein is required for mouse intestinal cAMP-, cGMP- and Ca2+-dependent HCO3− secretion. J. Physiol. 1997, 505, 411–423. [Google Scholar] [CrossRef]
- Graeber, S.Y.; Renz, D.M.; Stahl, M.; Pallenberg, S.T.; Sommerburg, O.; Naehrlich, L.; Berges, J.; Dohna, M.; Ringshausen, F.C.; Doellinger, F.; et al. Effects of Elexacaftor/Tezacaftor/Ivacaftor Therapy on Lung Clearance Index and Magnetic Resonance Imaging in Patients with Cystic Fibrosis and One or Two F508del Alleles. Am. J. Respir. Crit. Care Med. 2022, 206, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Benedetto, R.; Cabrita, I.; Schreiber, R.; Kunzelmann, K. TMEM16A is indispensable for basal mucus secretion in airways and intestine. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2019, 33, 4502–4512. [Google Scholar] [CrossRef] [PubMed]
- Strubberg, A.M.; Liu, J.H.; Walker, N.M.; Stefanski, C.D.; MacLeod, R.J.; Magness, S.T.; Clarke, L.L. Cftr Modulates Wnt/beta-Catenin Signaling and Stem Cell Proliferation in Murine Intestine. Cell. Mol. Gastroenterol. Hepatol. 2018, 5, 253–271. [Google Scholar] [CrossRef] [PubMed]
- Nikolovska, K.; Cao, L.; Hensel, I.; Di Stefano, G.; Seidler, A.E.; Zhou, K.Y.; Qian, J.J.; Singh, A.K.; Riederer, B.; Seidler, U. Sodium/hydrogen-exchanger-2 modulates colonocyte lineage differentiation. Acta Physiol. 2022, 234, e13774. [Google Scholar] [CrossRef]
- Dulin, N.O. Calcium-Activated Chloride Channel ANO1/TMEM16A: Regulation of Expression and Signaling. Front. Physiol. 2020, 11, 590262. [Google Scholar] [CrossRef]
- van Barneveld, A.; Stanke, F.; Ballmann, M.; Naim, H.Y.; Tümmler, B. Ex vivo biochemical analysis of CFTR in human rectal biopsies. Biochim. Biophys. Acta 2006, 1762, 393–397. [Google Scholar] [CrossRef][Green Version]
- Saint-Criq, V.; Haq, I.J.; Gardner, A.I.; Garnett, J.P.; Ward, C.; Brodlie, M.; Gray, M.A. Real-Time, Semi-Automated Fluorescent Measurement of the Airway Surface Liquid pH of Primary Human Airway Epithelial Cells. J. Vis. Exp. 2019, 9, e59815. [Google Scholar]
- Chambers, L.A.; Rollins, B.M.; Tarran, R. Liquid movement across the surface epithelium of large airways. Respir. Physiol. Neurobiol. 2007, 159, 256–270. [Google Scholar] [CrossRef]
- Stanke, F.; Ballmann, M.; Bronsveld, I.; Dörk, T.; Gallati, S.; Laabs, U.; Derichs, N.; Ritzka, M.; Posselt, H.G.; Harms, H.K.; et al. Diversity of the basic defect of homozygous CFTR mutation genotypes in humans. J. Med. Genet. 2008, 45, 47–54. [Google Scholar] [CrossRef]
- Griese, M.; Costa, S.; Linnemann, R.W.; Mall, M.A.; McKone, E.F.; Polineni, D.; Quon, B.S.; Ringshausen, F.C.; Taylor-Cousar, J.L.; Withers, N.J.; et al. Safety and Efficacy of Elexacaftor/Tezacaftor/Ivacaftor for 24 Weeks or Longer in People with Cystic Fibrosis and One or More F508del Alleles: Interim Results of an Open-Label Phase 3 Clinical Trial. Am. J. Respir. Crit. Care Med. 2021, 203, 381–385. [Google Scholar] [CrossRef]
- French, P.J.; vanDoorninck, J.H.; Peters, R.; Verbeek, E.; Ameen, N.A.; Marino, C.R.; deJonge, H.R.; Bijman, J.; Scholte, B.J. A Delta F508 mutation in mouse cystic fibrosis transmembrane conductance regulator results in a temperature-sensitive processing defect in vivo. J. Clin. Investig. 1996, 98, 1304–1312. [Google Scholar] [CrossRef] [PubMed]
- Xiao, F.; Juric, M.; Li, J.H.; Riederer, B.; Yeruva, S.; Singh, A.K.; Zheng, L.F.; Glage, S.; Kollias, G.; Dudeja, P.; et al. Loss of downregulated in adenoma (DRA) impairs mucosal HCO3-secretion in murine ileocolonic inflammation. Inflamm. Bowel Dis. 2012, 18, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Stange, D.E.; Ferrante, M.; Vries, R.G.J.; van Es, J.H.; van den Brink, S.; van Houdt, W.J.; Pronk, A.; van Gorp, J.; Siersema, P.D.; et al. Long-term Expansion of Epithelial Organoids From Human Colon, Adenoma, Adenocarcinoma, and Barrett's Epithelium. Gastroenterology 2011, 141, 1762–1772. [Google Scholar] [CrossRef]
- Khalil, H.; Nie, W.X.; Edwards, R.A.; Yoo, J. Isolation of Primary Myofibroblasts from Mouse and Human Colon Tissue. J. Vis. Exp. 2013, e50611. [Google Scholar] [CrossRef]
- Dekkers, J.F.; Alieva, M.; Wellens, L.M.; Ariese, H.C.R.; Jamieson, P.R.; Vonk, A.M.; Amatngalim, G.D.; Hu, H.L.; Oost, K.C.; Snippert, H.J.G.; et al. High-resolution 3D imaging of fixed and cleared organoids. Nat. Protoc. 2019, 14, 1756–1771. [Google Scholar] [CrossRef] [PubMed]
- Cui, L.; Aleksandrov, L.; Chang, X.B.; Hou, Y.X.; He, L.; Hegedus, T.; Gentzsch, M.; Aleksandrov, A.; Balch, W.E.; Riordan, J.R. Domain interdependence in the biosynthetic assembly of CFTR. J. Mol. Biol. 2007, 365, 981–994. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, J.K.; Davis, J.E.; Rappai, T.; McDonald, K.G.; Kulkarni, D.H.; Knoop, K.A.; Hogan, S.P.; Fitzpatrick, J.A.; Lencer, W.I.; Newberry, R.D. Intestinal goblet cells sample and deliver lumenal antigens by regulated endocytic uptake and transcytosis. eLife 2021, 10, e67292. [Google Scholar] [CrossRef]
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An open-source platform for biological-image analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef]
- Liu, Y.J.; Tan, Q.H.; Riederer, B.; di Stefano, G.; Romermann, D.; Qian, J.J.; Reiner, J.; Seidler, U. Deciphering ion transporters, kinases and PDZ-adaptor molecules that mediate guanylate cyclase C agonist-dependent intestinal fluid loss in vivo. Biochem. Pharmacol. 2020, 178, 11. [Google Scholar] [CrossRef]
- Simossis, V.A.; Heringa, J. PRALINE: A multiple sequence alignment toolbox that integrates homology-extended and secondary structure information. Nucleic Acids Res. 2005, 33, W289–W294. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salari, A.; Xiu, R.; Amiri, M.; Pallenberg, S.T.; Schreiber, R.; Dittrich, A.-M.; Tümmler, B.; Kunzelmann, K.; Seidler, U. The Anion Channel TMEM16a/Ano1 Modulates CFTR Activity, but Does Not Function as an Apical Anion Channel in Colonic Epithelium from Cystic Fibrosis Patients and Healthy Individuals. Int. J. Mol. Sci. 2023, 24, 14214. https://doi.org/10.3390/ijms241814214
Salari A, Xiu R, Amiri M, Pallenberg ST, Schreiber R, Dittrich A-M, Tümmler B, Kunzelmann K, Seidler U. The Anion Channel TMEM16a/Ano1 Modulates CFTR Activity, but Does Not Function as an Apical Anion Channel in Colonic Epithelium from Cystic Fibrosis Patients and Healthy Individuals. International Journal of Molecular Sciences. 2023; 24(18):14214. https://doi.org/10.3390/ijms241814214
Chicago/Turabian StyleSalari, Azam, Renjie Xiu, Mahdi Amiri, Sophia Theres Pallenberg, Rainer Schreiber, Anna-Maria Dittrich, Burkhard Tümmler, Karl Kunzelmann, and Ursula Seidler. 2023. "The Anion Channel TMEM16a/Ano1 Modulates CFTR Activity, but Does Not Function as an Apical Anion Channel in Colonic Epithelium from Cystic Fibrosis Patients and Healthy Individuals" International Journal of Molecular Sciences 24, no. 18: 14214. https://doi.org/10.3390/ijms241814214
APA StyleSalari, A., Xiu, R., Amiri, M., Pallenberg, S. T., Schreiber, R., Dittrich, A.-M., Tümmler, B., Kunzelmann, K., & Seidler, U. (2023). The Anion Channel TMEM16a/Ano1 Modulates CFTR Activity, but Does Not Function as an Apical Anion Channel in Colonic Epithelium from Cystic Fibrosis Patients and Healthy Individuals. International Journal of Molecular Sciences, 24(18), 14214. https://doi.org/10.3390/ijms241814214





