Transcriptomics of Canine Inflammatory Mammary Cancer Treated with Empty Cowpea Mosaic Virus Implicates Neutrophils in Anti-Tumor Immunity
Abstract
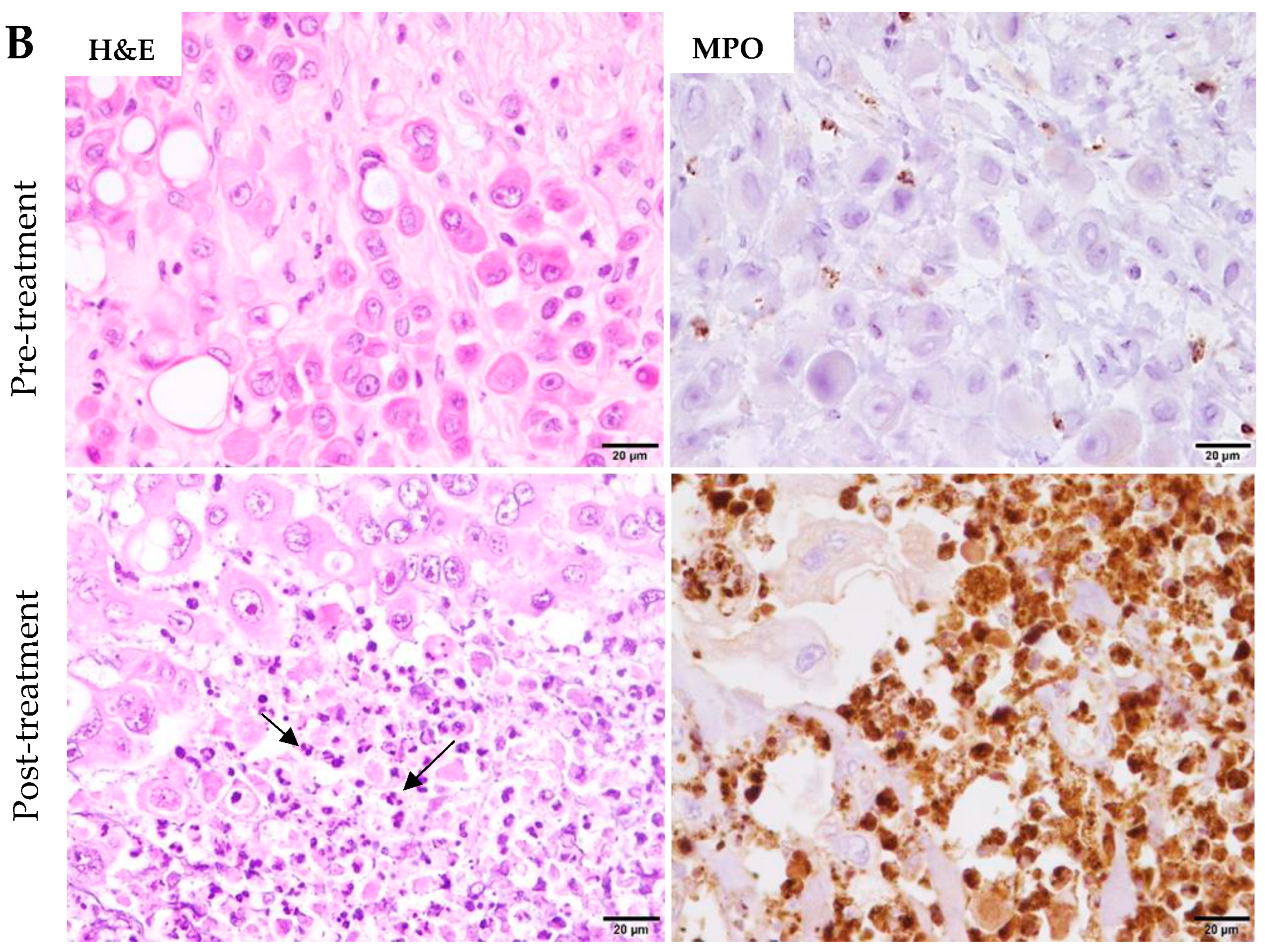
:1. Introduction
2. Results
2.1. Differentially Expressed Genes in Tumor Samples after eCPMV Treatment
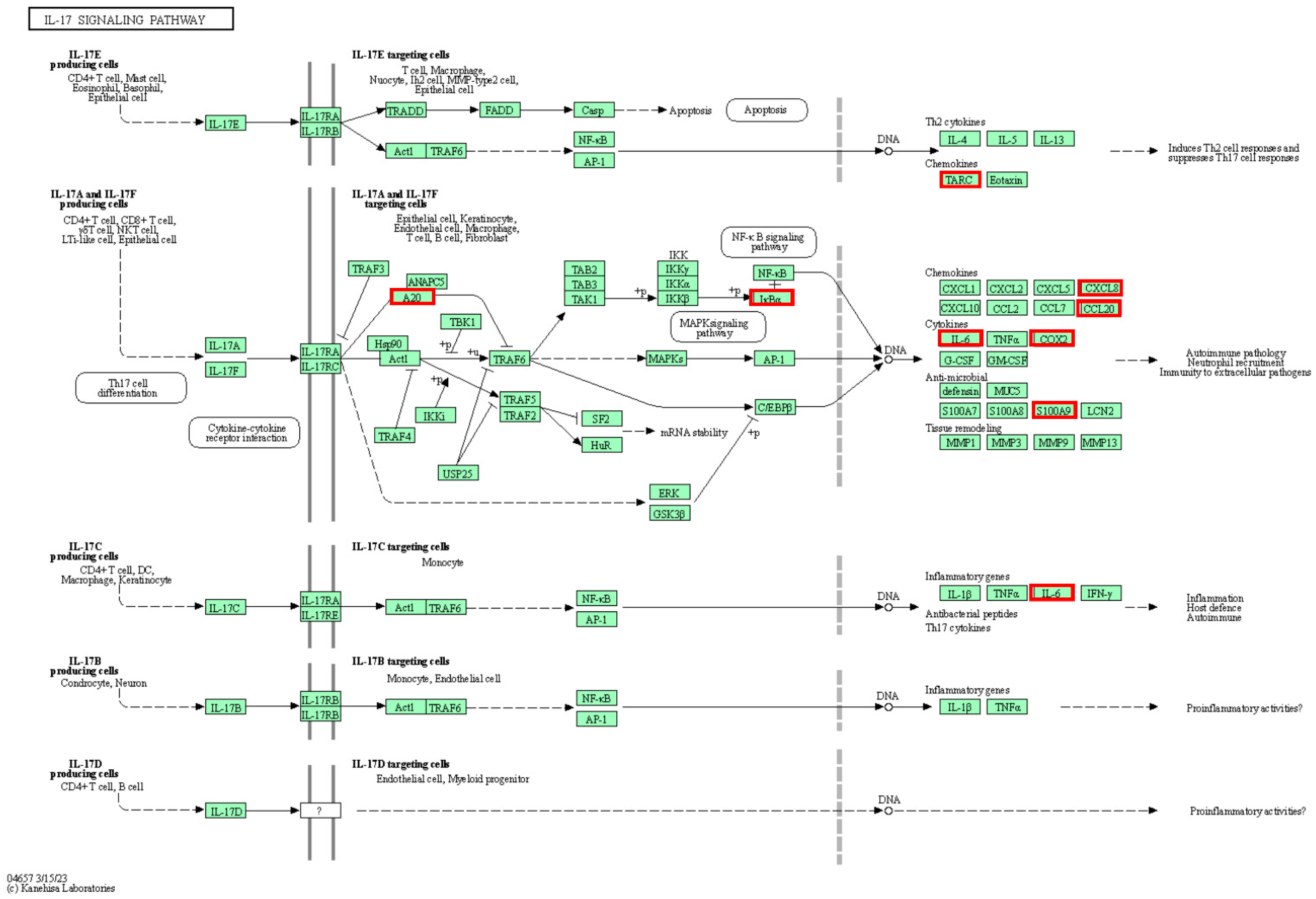
2.2. Pathway Analyses
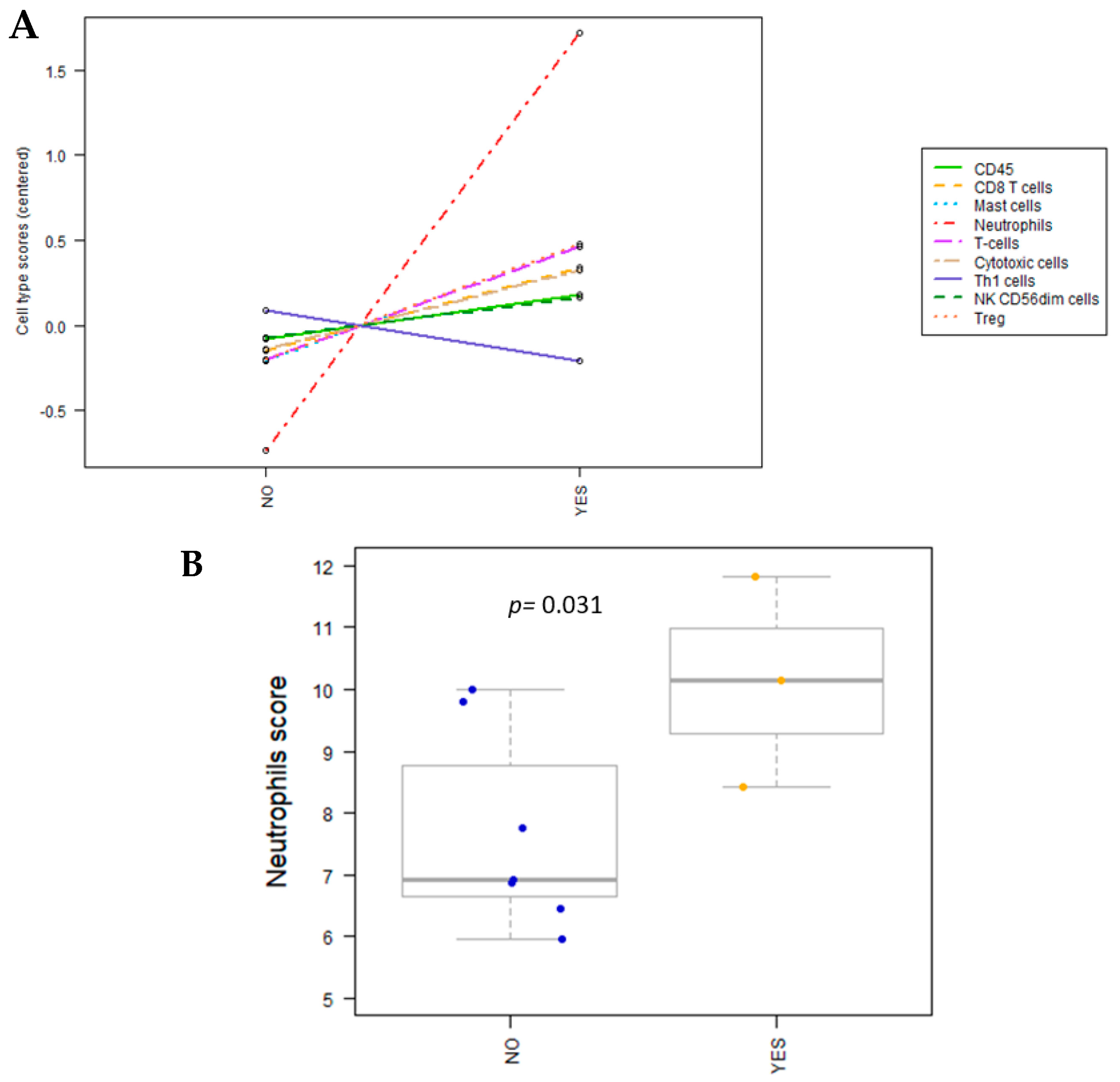
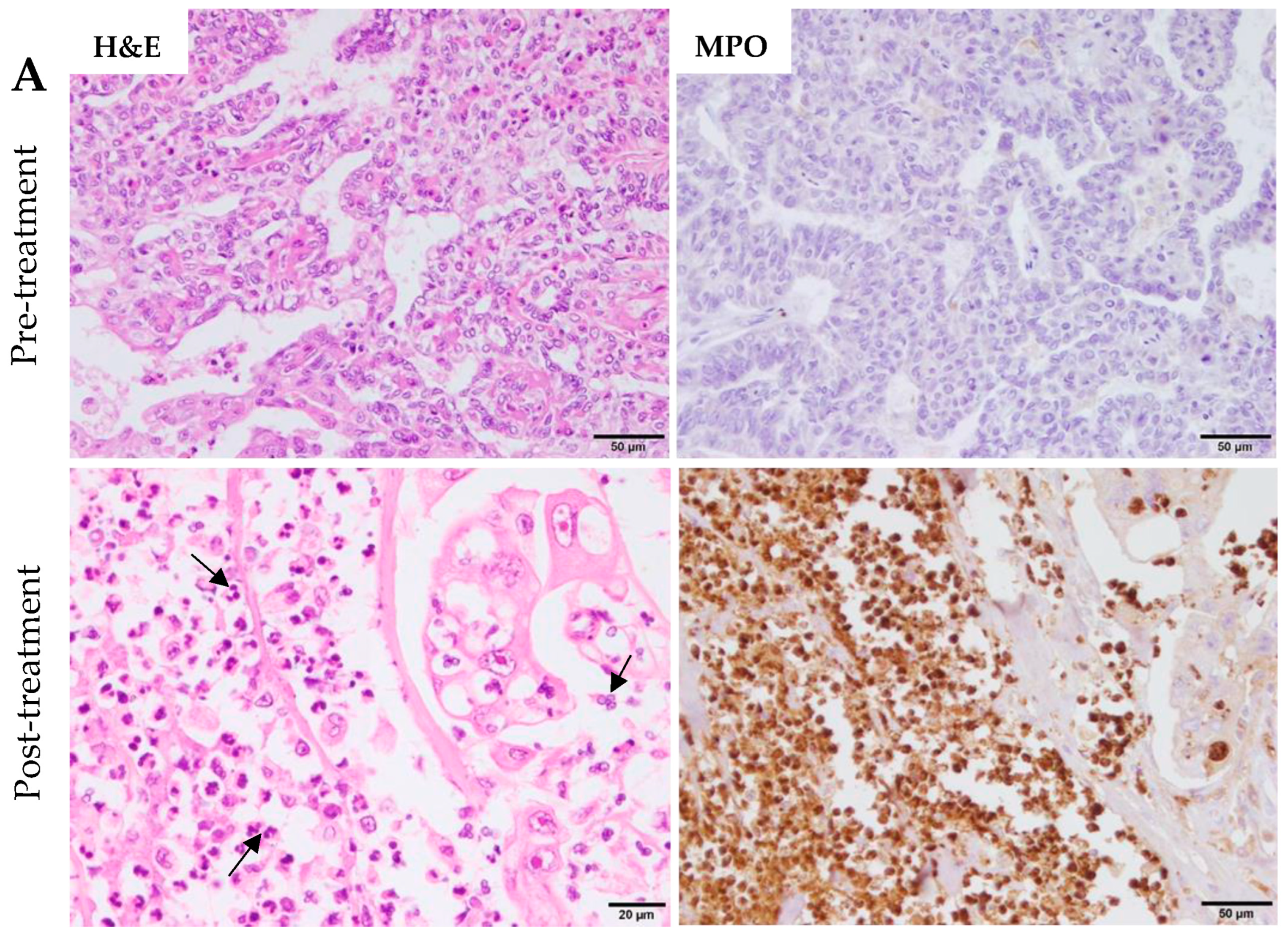
2.3. Cell Type Profiling
3. Discussion
3.1. The IL-17 Signaling Pathway’s Role in the Immune Response Triggered by eCPMV Immunotherapy
3.2. Other Upregulated Immune Pathways and Genes Triggered by eCPMV Immunotherapy
3.3. Downregulated Immune Pathways and Genes after eCPMV Immunotherapy
4. Materials and Methods
4.1. Patients and Clinical Procedures
4.2. RNA Extraction and NanoString nCounter Analyses
4.3. Transcriptomic Data and Statistical Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| APC | antigen-presenting cells |
| D0 | day of first immunotherapy dose |
| D7 | day of second immunotherapy dose |
| DAVID | Database for Annotation, Visualization, and Integrated Discovery |
| DAMPs | damage-associated molecular pattern |
| DCs | dendritic cells |
| DEGs | differentially expressed genes |
| eCPMV | empty Cowpea Mosaic Virus |
| FFPE | formalin-fixed paraffin-embedded |
| GSA | gene set analysis |
| IBC | inflammatory breast cancer |
| IHC | immunohistochemistry |
| IMC | inflammatory mammary cancer |
| IL-8 | interleukin-8 |
| IO | immuno-oncology |
| itRECIST | intratumoral Response Evaluation Criteria in Solid Tumors |
| IT-IT | Intratumoral immunotherapy |
| KEGG | Kyoto Encyclopedia of Genes and Genomes |
| MPO | mieloperoxidase |
| MT | medical therapy |
| N1/N2 | neutrophil subpopulations |
| NF-κB | nuclear factor-kappaB |
| NK cells | natural killer cells |
| Nt | nucleotide |
| PD-1 | programmed cell death 1 |
| PI | proliferation index |
| P1-12 | patients 1-12 |
| QC | quality control |
| QOL | quality of life |
| RIN | RNA integrity number |
| TANs | tumor-associated neutrophils |
| TLR2/4 | Toll-like receptors 2/4 |
| TME | tumor microenvironment |
| TNF | tumor necrosis factor |
| Treg | regulatory T cells |
| VLPs | plant-based virus-like nanoparticles |
| DEGs Abbreviations | |
| CCL17 | CC chemokine ligand 17 |
| DMBT1 | deleted in malignant brain tumor 1 |
| PTGS2 | prostaglandin-endoperoxide synthase 2 |
| S100A12 | S100 Calcium Binding Protein A12 |
| S100A9 | S100 calcium-binding protein A9 |
| IL6 | interleukin 6 |
| CR2 | complement receptor 2 |
| LIF | Leukemia Inhibitory Factor |
| CXCL8 | IL-8 or chemokine (C-X-C motif) ligand 8 |
| CD40LG | CD40 Ligand |
| CR1L | Complement Receptor 1-Like |
| CCL20 | C-C Motif Chemokine Ligand 20 |
| CLEC7A | C-type lectin domain family 7 member A |
| CD38 | Cluster of Differentiation 38 |
| CD4 | CD4 receptor, cluster of differentiation 4 |
| FCRL2 | Fc Receptor-Like 2 |
| CCRL2 | Chemokine C-C Motif Receptor-Like 2 |
| TNFAIP3 | TNF Alpha Induced Protein 3 |
| JAM3 | Junctional Adhesion Molecule 3 |
| PRDM1 | PR domain zinc finger protein 1 |
| IL18R1 | Interleukin 18 Receptor 1 |
| CD68 | Cluster of Differentiation 68 |
| NFKBIA | Nuclear Factor Kappa B Inhibitor Alpha |
| LY9 | Lymphocyte Antigen 9 |
| BAX | BCL2 Associated X Protein |
| SIGIRR | Single Immunoglobulin and Toll-Interleukin 1 Receptor Domain-Containing Protein |
| TLR5 | Toll-like receptor 5 |
| CD1E | Cluster of Differentiation 1E |
| S100B | S100 calcium-binding protein B |
| IL13RA2 | Interleukin-13 receptor subunit alpha-2 |
| CREB5 | cAMP Response Element-Binding Protein 5 |
| IFGGC1 | Interferon Gamma-Inducible GTPase Candidate 1 |
| IL12RB2 | interleukin 12 receptor, beta 2 subunit |
| IL31RA | Interleukin 31 Receptor A |
References
- van Uden, D.J.; van Laarhoven, H.W.; Westenberg, A.H.; de Wilt, J.H.; Blanken-Peeters, C.F. Inflammatory breast cancer: An overview. Crit. Rev. Oncol. Hematol. 2015, 93, 116–126. [Google Scholar] [CrossRef]
- Dabi, Y.; Darrigues, L.; Pons, K.; Mabille, M.; Abd Alsamad, I.; Mitri, R.; Skalli, D.; Haddad, B.; Touboul, C. Incidence of inflammatory breast cancer in patients with clinical inflammatory breast symptoms. PLoS ONE 2017, 12, e0189385. [Google Scholar] [CrossRef]
- Alenza MD, P.; Tabanera, E.; Peña, L. Inflammatory mammary carcinoma in dogs: 33 cases (1995–1999). J. Am. Vet. Med. Assoc. 2001, 219, 1110–1114. [Google Scholar] [CrossRef] [PubMed]
- Clemente, M.; Perez-Alenza, M.D.; Illera, J.C.; Pena, L. Histological, immunohistological, and ultrastructural description of vasculogenic mimicry in canine mammary cancer. Vet. Pathol. 2010, 47, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Giordano, S.H. Update on Locally Advanced Breast Cancer. Oncologist 2003, 8, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Low, J.A.; Berman, A.W.; Steinberg, S.M.; Danforth, D.N.; Lippman, M.E.; Swain, S.M. Long-term follow-up for locally advanced and inflammatory breast cancer patients treated with multimodality therapy. J. Clin. Oncol. 2004, 22, 4067–4074. [Google Scholar] [CrossRef]
- Ueno, N.T.; Buzdar, A.U.; Singletary, S.E.; Ames, F.C.; McNeese, M.D.; Holmes, F.A.; Theriault, R.L.; Strom, E.A.; Wasaff, B.J.; Asmar, L.; et al. Combined-modality treatment of inflammatory breast carcinoma: Twenty years of experience at MD Anderson Cancer Center. Cancer Chemother. Pharmacol. 1997, 40, 321–329. [Google Scholar] [CrossRef]
- Lim, B.; Woodward, W.A.; Wang, X.; Reuben, J.M.; Ueno, N.T. Inflammatory breast cancer biology: The tumour microenvironment is key. Nat. Rev. Cancer 2018, 18, 485–499. [Google Scholar] [CrossRef]
- Abdelmegeed, S.M.; Mohammed, S. Canine mammary tumors as a model for human disease. Oncol. Lett. 2018, 15, 8195–8205. [Google Scholar] [CrossRef]
- Schiffman, J.D.; Breen, M. Comparative oncology: What dogs and other species can teach us about humans with cancer. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2015, 370, 20140231. [Google Scholar] [CrossRef]
- Dow, S. A Role for Dogs in Advancing Cancer Immunotherapy Research. Front. Immunol. 2019, 10, 2935. [Google Scholar] [CrossRef] [PubMed]
- Clemente, M.; Perez-Alenza, M.D.; Pena, L. Metastasis of canine inflammatory versus non-inflammatory mammary tumours. J. Comp. Pathol. 2010, 143, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Clemente, M.; Sanchez-Archidona, A.R.; Sardon, D.; Diez, L.; Martin-Ruiz, A.; Caceres, S.; Sassi, F.; Dolores Perez-Alenza, M.; Illera, J.C.; Dunner, S.; et al. Different role of COX-2 and angiogenesis in canine inflammatory and non-inflammatory mammary cancer. Vet. J. 2013, 197, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Barreno, L.; Caceres, S.; Alonso-Diez, A.; Vicente-Montana, A.; Garcia, M.L.; Clemente, M.; Illera, J.C.; Pena, L. Vasculogenic mimicry-associated ultrastructural findings in human and canine inflammatory breast cancer cell lines. BMC Cancer 2019, 19, 750. [Google Scholar] [CrossRef] [PubMed]
- Raposo, T.P.; Arias-Pulido, H.; Chaher, N.; Fiering, S.N.; Argyle, D.J.; Prada, J.; Pires, I.; Queiroga, F.L. Comparative aspects of canine and human inflammatory breast cancer. Semin. Oncol. 2017, 44, 288–300. [Google Scholar] [CrossRef]
- Hodi, F.S.; O’Day, S.J.; McDermott, D.F.; Weber, R.W.; Sosman, J.A.; Haanen, J.B.; Gonzalez, R.; Robert, C.; Schadendorf, D.; Hassel, J.C.; et al. Improved survival with ipilimumab in patients with metastatic melanoma. N. Engl. J. Med. 2010, 363, 711–723. [Google Scholar] [CrossRef] [PubMed]
- Garon, E.B.; Rizvi, N.A.; Hui, R.; Leighl, N.; Balmanoukian, A.S.; Eder, J.P.; Patnaik, A.; Aggarwal, C.; Gubens, M.; Horn, L.; et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N. Engl. J. Med. 2015, 372, 2018–2028. [Google Scholar] [CrossRef]
- Makkouk, A.; Weiner, G.J. Cancer immunotherapy and breaking immune tolerance: New approaches to an old challenge. Cancer Res. 2015, 75, 5–10. [Google Scholar] [CrossRef]
- Leko, V.; Rosenberg, S.A. Identifying and Targeting Human Tumor Antigens for T Cell-Based Immunotherapy of Solid Tumors. Cancer Cell 2020, 38, 454–472. [Google Scholar] [CrossRef]
- Arab, A.; Behravan, N.; Razazn, A.; Barati, N.; Mosaffa, F.; Nicastro, J.; Slavcev, R.; Behravan, J. The viral approach to breast cancer immunotherapy. J. Cell Physiol. 2019, 234, 1257–1267. [Google Scholar] [CrossRef]
- van Rooijen, J.M.; Stutvoet, T.S.; Schröder, C.P.; de Vries, E.G.E. Immunotherapeutic options on the horizon in breast cancer treatment. Pharmacol. Ther. 2015, 156, 90–101. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Bennett, Z.T.; Sumer, B.D.; Gao, J. Nano-Immune-Engineering Approaches to Advance Cancer Immunotherapy: Lessons from Ultra-pH-Sensitive Nanoparticles. Acc. Chem. Res. 2020, 53, 2546–2557. [Google Scholar] [CrossRef] [PubMed]
- Lizotte, P.H.; Wen, A.M.; Sheen, M.R.; Fields, J.; Rojanasopondist, P.; Steinmetz, N.F.; Fiering, S. In Situ vaccination with cowpea mosaic virus nanoparticles suppresses metastatic cancer. Nat. Nanotechnol. 2016, 11, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Wang, C.; Shukla, S.; Steinmetz, N.F. Cowpea Mosaic Virus Immunotherapy Combined with Cyclophosphamide Reduces Breast Cancer Tumor Burden and Inhibits Lung Metastasis. Adv. Sci. 2019, 6, 1802281. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Miguel, D.; Valdivia, G.; Guerrera, D.; Perez-Alenza, M.D.; Pantelyushin, S.; Alonso-Diez, A.; Beiss, V.; Fiering, S.; Steinmetz, N.F.; Suarez-Redondo, M.; et al. Neoadjuvant in situ vaccination with cowpea mosaic virus as a novel therapy against canine inflammatory mammary cancer. J. Immunother. Cancer 2022, 10, e004044. [Google Scholar] [CrossRef] [PubMed]
- Mao, C.; Beiss, V.; Fields, J.; Steinmetz, N.F.; Fiering, S. Cowpea mosaic virus stimulates anti-tumor immunity through recognition by multiple MYD88-dependent toll-like receptors. Biomaterials 2021, 275, 120914. [Google Scholar] [CrossRef]
- Sheen, M.R.; Fiering, S. In situ vaccination: Harvesting low hanging fruit on the cancer immunotherapy tree. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2019, 11, e1524. [Google Scholar] [CrossRef]
- Varn, F.S.; Mullins, D.W.; Arias-Pulido, H.; Fiering, S.; Cheng, C. Adaptive immunity programmes in breast cancer. Immunology 2017, 150, 25–34. [Google Scholar] [CrossRef]
- Di Bonito, M.; Cantile, M.; Botti, G. Pathological and molecular characteristics of inflammatory breast cancer. Transl. Cancer Res. 2019, 8, S449–S456. [Google Scholar] [CrossRef]
- Ross, J.S.; Ali, S.M.; Wang, K.; Khaira, D.; Palma, N.A.; Chmielecki, J.; Palmer, G.A.; Morosini, D.; Elvin, J.A.; Fernandez, S.V.; et al. Comprehensive genomic profiling of inflammatory breast cancer cases reveals a high frequency of clinically relevant genomic alterations. Breast Cancer Res. Treat. 2015, 154, 155–162. [Google Scholar] [CrossRef]
- Metzemaekers, M.; Vandendriessche, S.; Berghmans, N.; Gouwy, M.; Proost, P. Truncation of CXCL8 to CXCL8(9-77) enhances actin polymerization and in vivo migration of neutrophils. J. Leukoc. Biol. 2020, 107, 1167–1173. [Google Scholar] [CrossRef] [PubMed]
- Russo, R.C.; Garcia, C.C.; Teixeira, M.M.; Amaral, F.A. The CXCL8/IL-8 chemokine family and its receptors in inflammatory diseases. Expert. Rev. Clin. Immunol. 2014, 10, 593–619. [Google Scholar] [CrossRef] [PubMed]
- Simard, J.C.; Girard, D.; Tessier, P.A. Induction of neutrophil degranulation by S100A9 via a MAPK-dependent mechanism. J. Leukoc. Biol. 2010, 87, 905–914. [Google Scholar] [CrossRef] [PubMed]
- Ryckman, C.; Vandal, K.; Rouleau, P.; Talbot, M.; Tessier, P.A. Proinflammatory activities of S100: Proteins S100A8, S100A9, and S100A8/A9 induce neutrophil chemotaxis and adhesion. J. Immunol. 2003, 170, 3233–3242. [Google Scholar] [CrossRef]
- Shabani, F.; Farasat, A.; Mahdavi, M.; Gheibi, N. Calprotectin (S100A8/S100A9): A key protein between inflammation and cancer. Inflamm. Res. 2018, 67, 801–812. [Google Scholar] [CrossRef]
- Gunaldi, M.; Okuturlar, Y.; Gedikbasi, A.; Akarsu, C.; Karabulut, M.; Kural, A. Diagnostic importance of S100A9 and S100A12 in breast cancer. Biomed. Pharmacother. 2015, 76, 52–56. [Google Scholar] [CrossRef]
- Shaul, M.E.; Levy, L.; Sun, J.; Mishalian, I.; Singhal, S.; Kapoor, V.; Horng, W.; Fridlender, G.; Albelda, S.M.; Fridlender, Z.G. Tumor-associated neutrophils display a distinct N1 profile following TGFbeta modulation: A transcriptomics analysis of pro- vs. antitumor TANs. Oncoimmunology 2016, 5, e1232221. [Google Scholar] [CrossRef]
- Fridlender, Z.G.; Sun, J.; Kim, S.; Kapoor, V.; Cheng, G.; Ling, L.; Worthen, G.S.; Albelda, S.M. Polarization of tumor-associated neutrophil phenotype by TGF-beta: “N1” versus “N2” TAN. Cancer Cell 2009, 16, 183–194. [Google Scholar] [CrossRef]
- Jaillon, S.; Ponzetta, A.; Di Mitri, D.; Santoni, A.; Bonecchi, R.; Mantovani, A. Neutrophil diversity and plasticity in tumour progression and therapy. Nat. Rev. Cancer 2020, 20, 485–503. [Google Scholar] [CrossRef]
- Furumaya, C.; Martinez-Sanz, P.; Bouti, P.; Kuijpers, T.W.; Matlung, H.L. Plasticity in Pro- and Anti-tumor Activity of Neutrophils: Shifting the Balance. Front. Immunol. 2020, 11, 2100. [Google Scholar] [CrossRef]
- Fridlender, Z.G.; Sun, J.; Mishalian, I.; Singhal, S.; Cheng, G.; Kapoor, V.; Horng, W.; Fridlender, G.; Bayuh, R.; Worthen, G.S.; et al. Transcriptomic analysis comparing tumor-associated neutrophils with granulocytic myeloid-derived suppressor cells and normal neutrophils. PLoS ONE 2012, 7, e31524. [Google Scholar] [CrossRef] [PubMed]
- Mihaila, A.C.; Ciortan, L.; Macarie, R.D.; Vadana, M.; Cecoltan, S.; Preda, M.B.; Hudita, A.; Gan, A.M.; Jakobsson, G.; Tucureanu, M.M.; et al. Transcriptional Profiling and Functional Analysis of N1/N2 Neutrophils Reveal an Immunomodulatory Effect of S100A9-Blockade on the Pro-Inflammatory N1 Subpopulation. Front. Immunol. 2021, 12, 708770. [Google Scholar] [CrossRef] [PubMed]
- Ralph, S.J.; Reynolds, M.J. Intratumoral pro-oxidants promote cancer immunotherapy by recruiting and reprogramming neutrophils to eliminate tumors. Cancer Immunol. Immunother. 2023, 72, 527–542. [Google Scholar] [CrossRef] [PubMed]
- Semmling, V.; Lukacs-Kornek, V.; Thaiss, C.A.; Quast, T.; Hochheiser, K.; Panzer, U.; Kurts, C. Alternative cross-priming through CCL17-CCR4-mediated attraction of CTLs toward NKT cell–licensed DCs. Nat. Immunol. 2010, 11, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Cornforth, A.N.; Lee, G.J.; Fowler, A.W.; Carbonell, D.J.; Dillman, R.O. Increases in serum TARC/CCL17 levels are associated with progression-free survival in advanced melanoma patients in response to dendritic cell-based immunotherapy. J. Clin. Immunol. 2009, 29, 657–664. [Google Scholar] [CrossRef]
- Weide, B.; Allgaier, N.; Hector, A.; Forschner, A.; Leiter, U.; Eigentler, T.K.; Garbe, C.; Hartl, D. Increased CCL17 serum levels are associated with improved survival in advanced melanoma. Cancer Immunol. Immunother. 2015, 64, 1075–1082. [Google Scholar] [CrossRef]
- Bozic, T.; Sersa, G.; Kranjc Brezar, S.; Cemazar, M.; Markelc, B. Gene electrotransfer of proinflammatory chemokines CCL5 and CCL17 as a novel approach of modifying cytokine expression profile in the tumor microenvironment. Bioelectrochemistry 2021, 140, 107795. [Google Scholar] [CrossRef]
- Martin-Orozco, N.; Muranski, P.; Chung, Y.; Yang, X.O.; Yamazaki, T.; Lu, S.; Hwu, P.; Restifo, N.P.; Overwijk, W.W.; Dong, C. T helper 17 cells promote cytotoxic T cell activation in tumor immunity. Immunity 2009, 31, 787–798. [Google Scholar] [CrossRef]
- Abi Abdallah, D.S.; Egan, C.E.; Butcher, B.A.; Denkers, E.Y. Mouse neutrophils are professional antigen-presenting cells programmed to instruct Th1 and Th17 T-cell differentiation. Int. Immunol. 2011, 23, 317–326. [Google Scholar] [CrossRef]
- Kwantwi, L.B.; Wang, S.; Zhang, W.; Peng, W.; Cai, Z.; Sheng, Y.; Xiao, H.; Wang, X.; Wu, Q. Tumor-associated neutrophils activated by tumor-derived CCL20 (C-C motif chemokine ligand 20) promote T cell immunosuppression via programmed death-ligand 1 (PD-L1) in breast cancer. Bioengineered 2021, 12, 6996–7006. [Google Scholar] [CrossRef]
- Kadomoto, S.; Izumi, K.; Mizokami, A. The CCL20-CCR6 Axis in Cancer Progression. Int. J. Mol. Sci. 2020, 21, 5186. [Google Scholar] [CrossRef] [PubMed]
- Scapini, P.; Crepaldi, L.; Pinardi, C.; Calzetti, F.; Cassatella, M.A. CCL20/macrophage inflammatory protein-3alpha production in LPS-stimulated neutrophils is enhanced by the chemoattractant formyl-methionyl-leucyl-phenylalanine and IFN-gamma through independent mechanisms. Eur. J. Immunol. 2002, 32, 3515–3524. [Google Scholar] [CrossRef] [PubMed]
- Maddur, M.S.; Miossec, P.; Kaveri, S.V.; Bayry, J. Th17 cells: Biology, pathogenesis of autoimmune and inflammatory diseases, and therapeutic strategies. Am. J. Pathol. 2012, 181, 8–18. [Google Scholar] [CrossRef]
- Hashemi Goradel, N.; Najafi, M.; Salehi, E.; Farhood, B.; Mortezaee, K. Cyclooxygenase-2 in cancer: A review. J. Cell Physiol. 2019, 234, 5683–5699. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Zhang, Y.; Li, M. Identification of genes and miRNAs in paclitaxel treatment for breast cancer. Gynecol. Endocrinol. 2021, 37, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Ma, N.; Zhao, Y. DMBT1 suppresses cell proliferation, migration and invasion in ovarian cancer and enhances sensitivity to cisplatin through galectin-3/PI3k/Akt pathway. Cell Biochem. Funct. 2020, 38, 801–809. [Google Scholar] [CrossRef]
- Braidotti, P.; Nuciforo, P.G.; Mollenhauer, J.; Poustka, A.; Pellegrini, C.; Moro, A.; Bulfamante, G.; Coggi, G.; Bosari, S.; Pietra, G.G. DMBT1 expression is down-regulated in breast cancer. BMC Cancer 2004, 4, 46. [Google Scholar] [CrossRef]
- Kalia, N.; Singh, J.; Kaur, M. The role of dectin-1 in health and disease. Immunobiology 2021, 226, 152071. [Google Scholar] [CrossRef]
- Zhu, Z.; Wang, H.; Wei, Y.; Meng, F.; Liu, Z.; Zhang, Z. Downregulation of PRDM1 promotes cellular invasion and lung cancer metastasis. Tumour Biol. 2017, 39, 1010428317695929. [Google Scholar] [CrossRef]
- Shen, L.; Chen, Q.; Yang, C.; Wu, Y.; Yuan, H.; Chen, S.; Ou, S.; Jiang, Y.; Huang, T.; Ke, L.; et al. Role of PRDM1 in Tumor Immunity and Drug Response: A Pan-Cancer Analysis. Front. Pharmacol. 2020, 11, 593195. [Google Scholar] [CrossRef]
- Kuhn, N.F.; Purdon, T.J.; van Leeuwen, D.G.; Lopez, A.V.; Curran, K.J.; Daniyan, A.F.; Brentjens, R.J. CD40 Ligand-Modified Chimeric Antigen Receptor (CAR) T Cells Enhance Antitumor Function by Eliciting an Endogenous Antitumor Response. Cancer Cell. 2019, 35, 473–488. [Google Scholar] [CrossRef] [PubMed]
- Yin, W.; Li, Y.; Song, Y.; Zhang, J.; Wu, C.; Chen, Y.; Miao, Y.; Lin, C.; Lin, Y.; Yan, D.; et al. CCRL2 promotes antitumor T-cell immunity via amplifying TLR4-mediated immunostimulatory macrophage activation. Proc. Natl. Acad. Sci. USA 2021, 118, e2024171118. [Google Scholar] [CrossRef] [PubMed]
- Marchetti, P.; Antonov, A.; Anemona, L.; Vangapandou, C.; Montanaro, M.; Botticelli, A.; Mauriello, A.; Melino, G.; Catani, M.V. New immunological potential markers for triple negative breast cancer: IL18R1, CD53, TRIM, Jaw1, LTB, PTPRCAP. Discov. Oncol. 2021, 12, 6. [Google Scholar] [CrossRef]
- Segaert, P.; Lopes, M.B.; Casimiro, S.; Vinga, S.; Rousseeuw, P.J. Robust identification of target genes and outliers in triple-negative breast cancer data. Stat. Methods Med. Res. 2019, 28, 3042–3056. [Google Scholar] [CrossRef]
- Li, X.; Yang, Q.; Yu, H.; Wu, L.; Zhao, Y.; Zhang, C.; Hu, W. LIF promotes tumorigenesis and metastasis of breast cancer through the AKT-mTOR pathway. Oncotarget 2014, 5, 788. [Google Scholar] [CrossRef]
- Chen, L.; Diao, L.; Yang, Y.; Yi, X.; Rodriguez, B.L.; Li, Y.; Villalobos, P.A.; Cascone, T.; Liu, X.; Tan, L.; et al. CD38-Mediated Immunosuppression as a Mechanism of Tumor Cell Escape from PD-1/PD-L1 Blockade. Cancer Discov. 2018, 8, 1156–1175. [Google Scholar] [CrossRef] [PubMed]
- Campesato, L.F. High IL-1R8 expression in breast tumors promotes tumor growth and contributes to impaired antitumor immunity. Oncotarget 2017, 8, 49470–49483. [Google Scholar] [CrossRef]
- Stevens, L.E.; Peluffo, G.; Qiu, X.; Temko, D.; Fassl, A.; Li, Z.; Trinh, A.; Seehawer, M.; Jovanovic, B.; Aleckovic, M.; et al. JAK-STAT Signaling in Inflammatory Breast Cancer Enables Chemotherapy-Resistant Cell States. Cancer Res. 2023, 83, 264–284. [Google Scholar] [CrossRef]
- Marquez-Ortiz, R.A.; Contreras-Zarate, M.J.; Tesic, V.; Alvarez-Eraso, K.L.F.; Kwak, G.; Littrell, Z.; Costello, J.C.; Sreekanth, V.; Ormond, D.R.; Karam, S.D.; et al. IL13Ralpha2 Promotes Proliferation and Outgrowth of Breast Cancer Brain Metastases. Clin. Cancer Res. 2021, 27, 6209–6221. [Google Scholar] [CrossRef]
- Chong, S.T.; Tan, K.M.; Kok, C.Y.L.; Guan, S.P.; Lai, S.H.; Lim, C.; Hu, J.; Sturgis, C.; Eng, C.; Lam, P.Y.P.; et al. IL13RA2 Is Differentially Regulated in Papillary Thyroid Carcinoma vs Follicular Thyroid Carcinoma. J. Clin. Endocrinol. Metab. 2019, 104, 5573–5584. [Google Scholar] [CrossRef]
- Liu, Z.G.; Lei, Y.Y.; Li, W.W.; Chen, Z.G. The co-expression of ERbeta2 and IL-12Rbeta2 is better prognostic factor in non-small-cell lung cancer progression. Med. Oncol. 2013, 30, 592. [Google Scholar] [CrossRef] [PubMed]
- Fessas, P.; Spina, P.; Boldorini, R.L.; Pirisi, M.; Minisini, R.; Mauri, F.A.; Simpson, F.; Olivieri, P.; Gennari, A.; Wong, C.N.; et al. Phenotypic Characteristics of the Tumour Microenvironment in Primary and Secondary Hepatocellular Carcinoma. Cancers 2021, 13, 2137. [Google Scholar] [CrossRef] [PubMed]
- Harpio, R.; Einarsson, R. S100 proteins as cancer biomarkers with focus on S100B in malignant melanoma. Clin. Biochem. 2004, 37, 512–518. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Zhang, X.; Pan, W.; Tai, F.; Liang, L.; Shi, J. Interleukin-31 Receptor alpha Is Required for Basal-Like Breast Cancer Progression. Front. Oncol. 2020, 10, 816. [Google Scholar] [CrossRef]
- Ahmed, M.B.; Alghamdi, A.A.A.; Islam, S.U.; Lee, J.S.; Lee, Y.S. cAMP Signaling in Cancer: A PKA-CREB and EPAC-Centric Approach. Cells 2022, 11, 2020. [Google Scholar] [CrossRef]
- Marconato, L.; Romanelli, G.; Stefanello, D.; Giacoboni, C.; Bonfanti, U.; Bettini, G.; Finotello, R.; Verganti, S.; Valenti, P.; Ciaramella, L.; et al. Prognostic factors for dogs with mammary inflammatory carcinoma: 43 cases (2003–2008). J. Am. Vet. Med. Assoc. 2009, 235, 967–972. [Google Scholar] [CrossRef]
- Huang, D.W.; Sherman, B.T.; Lempicki, R.A. Systematic and integrative analysis of large gene lists using DAVID Bioinformatics Resources. Nat. Protoc. 2009, 4, 44–57. [Google Scholar] [CrossRef]
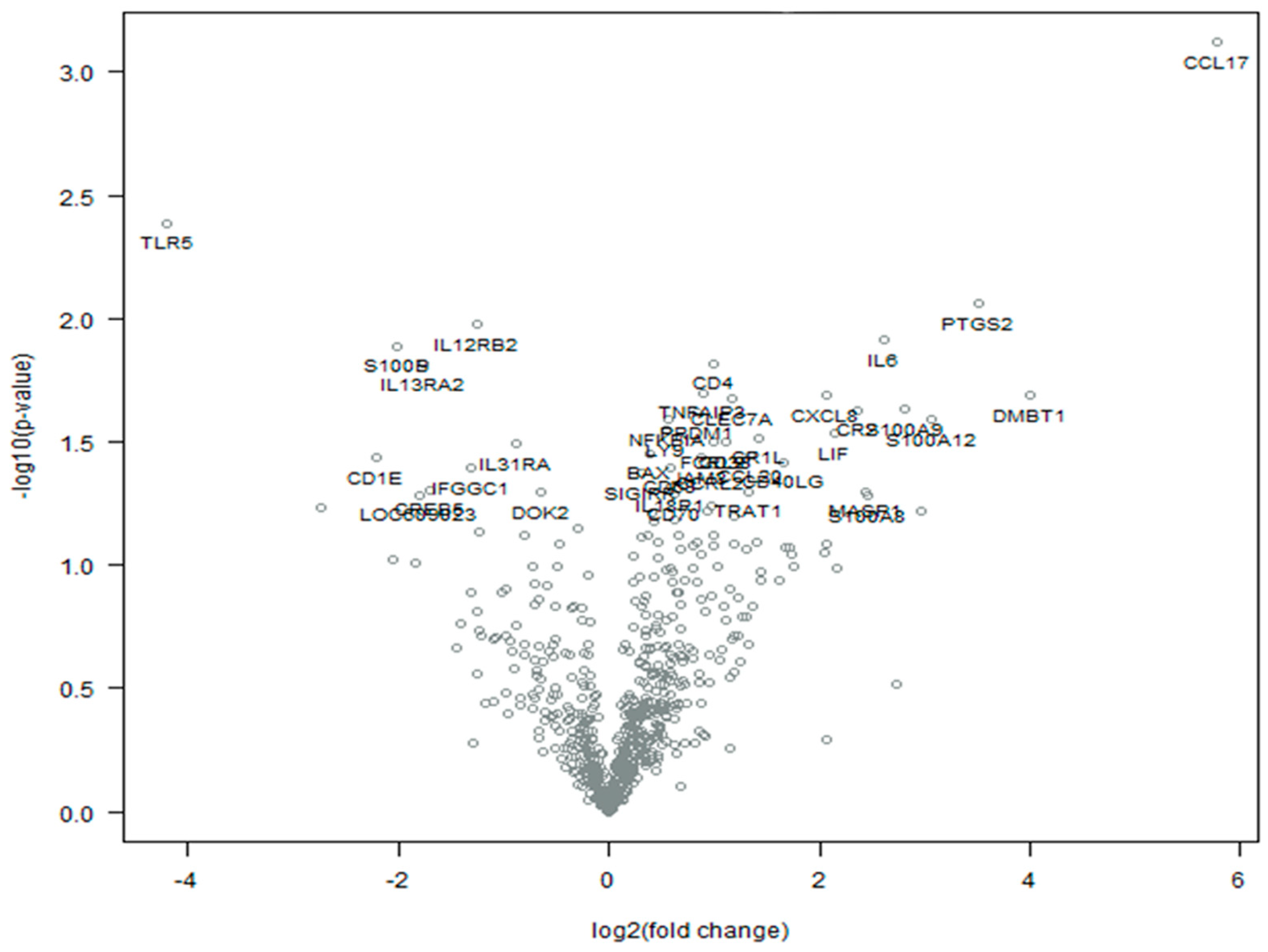
| Gene Symbol | Log2 Fold Change | Std Error (log2) | p-Value | NanoString nCounter Immuno-Oncology Gene Sets |
|---|---|---|---|---|
| Upregulated | ||||
| CCL17 | 5.77 | 1.1 | 0.00076 | Chemokines, Cytokine and Chemokine Signaling |
| DMBT1 | 4 | 1.39 | 0.0204 | |
| PTGS2 | 3.51 | 1.02 | 0.0087 | Angiogenesis, Costimulatory Signaling, Cytokine and Chemokine Signaling, Cytokines, Hypoxia, Myeloid Compartment, NF-kB Signaling |
| S100A12 | 3.06 | 1.12 | 0.0257 | Cytokine and Chemokine Signaling, Myeloid Compartment |
| S100A9 | 2.8 | 1 | 0.0233 | Angiogenesis, Hypoxia |
| IL6 | 2.62 | 0.814 | 0.0122 | Angiogenesis, Cytokine and Chemokine Signaling, Hypoxia, Interleukins, JAK-STAT Signaling, Metabolic Stress, PI3K-Akt |
| CR2 | 2.36 | 0.847 | 0.0235 | B-Cell Functions, Complement System |
| LIF | 2.14 | 0.805 | 0.0291 | Angiogenesis, Cell Functions, Cytokine and Chemokine Signaling, Cytotoxicity, JAK-STAT Signaling, Myeloid Compartment |
| CXCL8 | 2.07 | 0.72 | 0.0206 | Chemokines, Cytokine and Chemokine Signaling, Cytokines, Interleukins, Pathogen Defense, Regulation |
| CD40LG | 1.66 | 0.669 | 0.0382 | Costimulatory Signaling, Cytokine and Chemokine Signaling, Immune Cell Adhesion and Migration, Lymphoid Compartment, NF-kB Signaling, Regulation |
| CR1L | 1.43 | 0.545 | 0.0304 | Complement System |
| CCL20 | 1.35 | 0.538 | 0.036 | Chemokines, Cytokine and Chemokine Signaling, Myeloid Compartment |
| CLEC7A | 1.17 | 0.411 | 0.0212 | Immune Cell Adhesion and Migration, Myeloid Compartment |
| CD38 | 1.11 | 0.426 | 0.0316 | B-Cell Functions, Hypoxia, Lymphoid Compartment, Regulation, T Cell Functions |
| CD4 | 0.993 | 0.323 | 0.0152 | Antigen Presentation, Costimulatory Signaling, Cytokine and Chemokine Signaling, Immune Cell Adhesion and Migration |
| FCRL2 | 0.989 | 0.38 | 0.0316 | |
| CCRL2 | 0.972 | 0.394 | 0.0389 | Chemokines |
| TNFAIP3 | 0.891 | 0.308 | 0.02 | Angiogenesis, Hypoxia, NF-kB Signaling, TNF Superfamily |
| JAM3 | 0.883 | 0.352 | 0.0365 | Angiogenesis, Immune Cell Adhesion and Migration |
| PRDM1 | 0.829 | 0.299 | 0.0242 | Cell Functions, Epigenetic Regulation |
| IL18R1 | 0.585 | 0.25 | 0.0478 | Costimulatory Signaling, Cytokine and Chemokine Signaling, Lymphoid Compartment, NK Cell Functions, T Cell Functions |
| CD68 | 0.578 | 0.236 | 0.0401 | Cell Functions |
| NFKBIA | 0.573 | 0.21 | 0.0257 | Apoptosis, Costimulatory Signaling, Cytokine and Chemokine Signaling, NF-kB Signaling |
| LY9 | 0.534 | 0.2 | 0.0284 | Costimulatory Signaling, Lymphoid Compartment |
| BAX | 0.384 | 0.152 | 0.0353 | Apoptosis, Cell Cycle, Regulation |
| SIGIRR | 0.314 | 0.13 | 0.0423 | Cytokine and Chemokine Signaling |
| Downregulated | ||||
| TLR5 | −4.21 | 1.06 | 0.0041 | TLR |
| CD1E | −2.21 | 0.882 | 0.0365 | Antigen Processing |
| S100B | −2.02 | 0.635 | 0.0129 | Cytokine and Chemokine Signaling |
| IL13RA2 | −1.77 | 0.577 | 0.0153 | Chemokines, Cytokine and Chemokine Signaling, JAK-STAT Signaling, T Cell Functions |
| CREB5 | −1.7 | 0.736 | 0.0494 | |
| IFGGC1 | −1.32 | 0.54 | 0.0406 | Macrophage Functions, Myeloid Compartment |
| IL12RB2 | −1.25 | 0.378 | 0.0106 | Cytokine and Chemokine Signaling, Cytokines, Cytotoxicity, JAK-STAT Signaling, Lymphoid Compartment, NK Cell Functions, T Cell Functions |
| IL31RA | −0.884 | 0.342 | 0.0323 | Cytokine and Chemokine Signaling, Cytokines, Regulation |
| Cell Type | Untreated IMC Dogs | Treated IMC Dogs | p-Value * |
|---|---|---|---|
| CD45 | 10.8 ± 0.4 | 11.0 ± 0.2 | 0.192 |
| CD8+ T cells | 7.0 ± 0.9 | 7.5 ± 0.4 | 0.208 |
| Mast cells | 6.8 ± 1.4 | 7.5 ± 1.2 | 0.248 |
| Neutrophils | 7.7 ± 1.6 | 10.1 ± 1.7 | 0.031 * |
| T cells | 7.6 ± 0.7 | 8.3 ± 0.6 | 0.09 |
| Cytotoxic cells | 6.1 ± 0.9 | 6.6 ± 0.7 | 0.227 |
| Th1 cells | 6.8 ± 0.6 | 6.5 ± 0.3 | 0.226 |
| NK CD56dim cells | 8.0 ± 0.5 | 8.2 ± 0.7 | 0.276 |
| Treg | 4.9 ± 0.6 | 5.6 ± 0.6 | 0.069 |
| PATIENT | Age y | Weight kg | Breed | Type | Histo Grade | Histo Type | sdLVI | LNI | Treatments Target Tumor | Therapy | OS Days |
|---|---|---|---|---|---|---|---|---|---|---|---|
| eCPMV-treated IMC patients | |||||||||||
| P1 | 11 | 10.3 | Mixed | Primary | III | Special type | Yes | Yes | 8 | FCT+ | 174 |
| P2 | 13.5 | 25.6 | Mixed | Secondary | III | Simple | Yes | Yes | 7 | FCT+ | 156 |
| P3 | 10.7 | 8.2 | Poodle | Secondary | III | Simple | Yes | Yes | 2 | FCT+ | 109 |
| P4 | 10.7 | 17 | Kerry Blue Terrier | Secondary | III | Simple | Yes | Yes | 3 | FCT+ | 165 |
| P5 | 11.9 | 2.7 | Bichon Frise | Secondary | III | Simple | Yes | Yes | 2 | FCT+ | 67 |
| P6 | 13 | 22.3 | German Sheperd | Secondary | III | Simple | Yes | Yes | 2 | FCT+ | 104 |
| Untreated IMC patients | |||||||||||
| P7 | 13 | 26.2 | Mixed | Secondary | III | DA | Yes | Yes | FCT | 27 | |
| P8 | 14.2 | 7.6 | Maltese | Secondary | III | Simple | Yes | Yes | FCT | 40 | |
| P9 | 9.7 | 10.3 | Mixed | Secondary | III | Simple | Yes | Yes | FCT | 132 | |
| P10 | 13 | 9.3 | Miniature Schnauzer | Secondary | III | Simple | Yes | Yes | FCT | 63 | |
| P11 | 8.9 | 7.7 | Poodle | Secondary | III | Simple | Yes | Yes | FCT | 73 | |
| P12 | 8.3 | 26 | German Sheperd | Secondary | III | Simple | Yes | Yes | FCT | 14 | |
| Patient | Group | D0 | Post—TT |
|---|---|---|---|
| P1 | IMC—eCPMV | RNA-T1a * | RNA-T1b |
| P2 | IMC—eCPMV | RNA-T2a | RNA-T2b * |
| P5 | IMC—eCPMV | RNA-T3a | RNA-T3b |
| P6 | IMC—eCPMV | RNA-T4a | RNA-T4b |
| P7 | IMC—control | RNA-C1 | |
| P8 | IMC—control | RNA-C2 | |
| P9 | IMC—control | RNA-C3 | |
| P12 | IMC—control | RNA-C4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barreno, L.; Sevane, N.; Valdivia, G.; Alonso-Miguel, D.; Suarez-Redondo, M.; Alonso-Diez, A.; Fiering, S.; Beiss, V.; Steinmetz, N.F.; Perez-Alenza, M.D.; et al. Transcriptomics of Canine Inflammatory Mammary Cancer Treated with Empty Cowpea Mosaic Virus Implicates Neutrophils in Anti-Tumor Immunity. Int. J. Mol. Sci. 2023, 24, 14034. https://doi.org/10.3390/ijms241814034
Barreno L, Sevane N, Valdivia G, Alonso-Miguel D, Suarez-Redondo M, Alonso-Diez A, Fiering S, Beiss V, Steinmetz NF, Perez-Alenza MD, et al. Transcriptomics of Canine Inflammatory Mammary Cancer Treated with Empty Cowpea Mosaic Virus Implicates Neutrophils in Anti-Tumor Immunity. International Journal of Molecular Sciences. 2023; 24(18):14034. https://doi.org/10.3390/ijms241814034
Chicago/Turabian StyleBarreno, Lucia, Natalia Sevane, Guillermo Valdivia, Daniel Alonso-Miguel, María Suarez-Redondo, Angela Alonso-Diez, Steven Fiering, Veronique Beiss, Nicole F. Steinmetz, Maria Dolores Perez-Alenza, and et al. 2023. "Transcriptomics of Canine Inflammatory Mammary Cancer Treated with Empty Cowpea Mosaic Virus Implicates Neutrophils in Anti-Tumor Immunity" International Journal of Molecular Sciences 24, no. 18: 14034. https://doi.org/10.3390/ijms241814034
APA StyleBarreno, L., Sevane, N., Valdivia, G., Alonso-Miguel, D., Suarez-Redondo, M., Alonso-Diez, A., Fiering, S., Beiss, V., Steinmetz, N. F., Perez-Alenza, M. D., & Peña, L. (2023). Transcriptomics of Canine Inflammatory Mammary Cancer Treated with Empty Cowpea Mosaic Virus Implicates Neutrophils in Anti-Tumor Immunity. International Journal of Molecular Sciences, 24(18), 14034. https://doi.org/10.3390/ijms241814034







