Abstract
The calcitonin gene-related peptide (CGRP) is a neuropeptide widely distributed throughout the human body. While primarily recognized as a nociceptive mediator, CGRP antagonists are currently utilized for migraine treatment. However, its role extends far beyond this, acting as a regulator of numerous biological processes. Indeed, CGRP plays a crucial role in vasodilation, inflammation, intestinal motility, and apoptosis. In this review, we explore the non-nociceptive effects of CGRP in various body systems, revealing actions that can be contradictory at times. In the cardiovascular system, it functions as a potent vasodilator, yet its antagonists do not induce arterial hypertension, suggesting concurrent modulation by other molecules. As an immunomodulator, CGRP exhibits intriguing complexity, displaying both anti-inflammatory and pro-inflammatory effects. Furthermore, CGRP appears to be involved in obesity development while paradoxically reducing appetite. A thorough investigation of CGRP’s biological effects is crucial for anticipating potential side effects associated with its antagonists’ use and for developing novel therapies in other medical fields. In summary, CGRP represents a neuropeptide with a complex systemic impact, extending well beyond nociception, thus offering new perspectives in medical research and therapeutics
1. Introduction
Calcitonin Gene-Related Peptide (CGRP) is a neuropeptide consisting of 37 amino acids [1]. It was discovered approximately 40 years ago as a product of alternative splicing of the calcitonin gene mRNA and isolated from the thyroid of patients with thyroid carcinoma [2]. It belongs to the family of adrenomedullins, calcitonin, and amylin and is primarily located in the central nervous system, particularly in the hypothalamus, olfactory system, and gustatory system [1]. In the peripheral nervous system, it is found in type C and Aδ sensory fibers that play roles both as afferents (nociceptive) and efferents and are present near blood vessels in all organs of the body [3,4].
CGRP is primarily known for its role in pain perception processes associated with migraine [5,6,7]. It is released by the activated trigeminovascular system and is responsible for both migraine pain perception and the direct induction of migraine attacks [5,6,7]. This has generated strong pharmacological interest, and in the 1990s, it was discovered that triptans, drugs already used for decades in migraine, inhibit CGRP release [8]. Based on this evidence, drugs with a direct action on CGRP have been subsequently developed, such as monoclonal antibodies and gepants targeting CGRP and its receptor [1,9].
In addition to its role as a pain mediator, CGRP is the most potent vasodilator discovered to date [1]. Even the injection of small amounts of CGRP at the cutaneous level causes massive vasodilation of arterioles and an increase in blood flow in the inoculated area [10]. These effects indicate an important role of CGRP in the cardiovascular system. Furthermore, the ubiquitous distribution of CGRP in the body stimulates interest in the systemic effects that this molecule could have, both physiologically and pathologically. A comprehensive analysis of CGRP effects is also important, considering the increasing use of its antagonists in migraines to understand and predict the short-term and long-term effects of these drugs [11].
The purpose of this review is therefore to summarize the current understanding of the role of CGRP in the physiology and pathophysiology in different body districts. The synthesis and release of CGRP, as well as the biological effect of binding to its receptors, will be analyzed. Subsequently, the non-nociceptive and non-neurological effects of CGRP on different organs and systems will be examined.
This narrative review included a search of literature through PubMed of articles in English. We searched for studies that included “CGRP”, “Calcitonin gene related peptide”, “cardiovascular”, “heart”, “vessels”, “gastrointestinal”, “skin”, “systemic effects”, “immunology”, and “musculoskeletal”. We screened abstracts and then extracted information relevant to this review.
2. CGRP Biology
2.1. CGRP Isoforms
CGRP exists in two main forms, α and β, synthesized from two distinct genes located at different sites on chromosome 11 in humans [12,13]. The CALC I gene is part of a gene family that includes adrenomedullin (1 and 2), and amylin, and is responsible for the production of calcitonin or the alpha isoform of CGRP if alternative splicing occurs [1]. The CALC II gene determines only the formation of β-CGRP [1]. CGRP α and CGRP β share approximately 90% homology and exhibit similar biological activities [1].
2.2. Regulation of CGRP Synthesis and Release
The regulation of CGRP synthesis is still poorly understood [1]. It appears to be enhanced in situations of damage to the nerve endings of C or Aδ sensory fibers or in the presence of inflammation in tissues adjacent to the fibers [14]. Nerve growth factor (NGF) is involved in the growth and function of sensory nerves and appears to play an important role in increasing CGRP production in dorsal root ganglia [15]. Furthermore, elevated levels of NGF and CGRP are observed in patients with migraines [16]. Other factors, such as brain-derived neurotrophic factor (BDNF), may influence CGRP release and activity [17]. The Calcitonin Gene-Related Peptide (CGRP) is co-localized in pain nerve terminals along with Substance P (SP), which exhibits similar biological effects. SP acts as a cutaneous vasodilator and increases microvascular permeability, with an earlier release and less potent and enduring effects compared to CGRP [18]. SP serves as a key mediator of pain perception in pain modulation and sensation. Additionally, it is also involved in the regulation of inflammation, nausea, and vomiting, and the modulation of behavioral disorders [18].
After synthesis, CGRP is stored in dense vesicles within sensory nerve endings and is released through calcium-dependent exocytosis [19,20]. The release of CGRP occurs following the activation of TRPV1 and TRPA1 receptors [21,22]. TRPV1 can be activated by painful thermal stimuli, pH reduction, and inflammation [22].
Additionally, CGRP release also appears to occur in response to vasoconstrictors such as angiotensin II and noradrenaline, which activate α2 adrenergic receptors with NGF-induced CGRP release [23].
2.3. CGRP Receptor
The CGRP receptor consists of two subunits: the calcitonin-like receptor (CLR) and the receptor activity-modifying protein (RAMP). CLR belongs to the class B of G protein-coupled receptors (GPCR), which also includes receptors for calcitonin, vasoactive intestinal peptide (VIP), pituitary adenylate cyclase-activating polypeptide (PACAP), and parathyroid hormone (PTH) [1]. The RAMP protein family consists of three members: RAMP1, RAMP2, and RAMP3 [1].
The co-expression of CLR and RAMP1 forms a high-affinity receptor for CGRP (CGRP1 receptor), while the dimerization of CLR and RAMP2 creates a receptor highly responsive to adrenomedullin (AM1 receptor) [1]. The RAMP3 receptor confers a second receptor for adrenomedullin (AM2 receptor) with some selectivity for CGRP [24,25]. Indeed, although the true receptor for CGRP is considered to be formed by the CLR/RAMP1 complex, in vitro studies have shown that CGRP has some affinity for the CLR/RAMP3 complex (AM2 receptor) [24].
2.4. Intracellular Signaling
The binding of CGRP to the CGRP1 receptor results in increased intracellular cAMP levels, activation of protein kinase A, and the opening of ATP-sensitive K+ channels [26]. This pathway is primarily responsible for smooth muscle cell relaxation and vasodilation. Another pathway that leads to endothelium-dependent vasodilation is associated with the stimulation of nitric oxygen (NO) release [27].
Activation of protein kinase A also induces the expression of the c-fos gene, which appears to be involved in pain sensitization [28]. CGRP can activate mitogen-activated protein kinases (MAPK) that promote fibroblast proliferation [29]. Furthermore, it can stimulate antiapoptotic pathways involving MAPK, ERK1/2, and p38 [30]. Activation of ERK and p38 also appears to modulate the response to morphine [31].
3. Physiological and Pathophysiological Effect of CGRP
3.1. CGRP in the Cardiovascular System
3.1.1. CGRP as a Vasodilator
CGRP can induce vasodilation and increase blood flow in various organs. For example, the injection of femtomoles of CGRP causes an increase in microcirculation in the skin, brain, coronary, and renal regions [10,32]. As previously discussed, the vasodilation mechanism of CGRP involves both the NO-dependent pathway and the NO-independent pathway [33].
3.1.2. CGRP in the Regulation of Systemic Circulation
CGRP can influence blood pressure regulation. It is believed that CGRP is released in response to hypertensive stimuli such as angiotensin II activation and postural changes [34] and plays an important role in modulating baroreceptor reflex sensitivity [35]. Despite CGRP administration resulting in a reduction in systemic arterial pressure [13,33,36], it is important to note that it does not act as a hypotensive mediator since it simultaneously causes a positive inotropic and chronotropic response in the heart, preventing hypotension [37,38]. The function of CGRP, therefore, appears to be that of a regulator and modulator of the pressor response. This hypothesis is supported by the fact that CGRP antagonists do not seem to cause a significant pressor effect, likely due to the consequent activation of vasodilatory mediators such as NO and prostaglandins [39,40]. Furthermore, studies on genetic polymorphisms in the CALC1 gene have shown an association between specific genetic variants, such as T-692C, and an increased susceptibility to the development of arterial hypertension [41].
3.1.3. CGRP Physiologic Effect in the Heart
CGRP plays a cardioprotective role [1]. It is found in fibers innervating coronary arteries, papillary muscle, and the sinoatrial and atrioventricular nodes [42]. As previously mentioned, CGRP has a positive effect on cardiac chronotropy and inotropy [43]. Furthermore, CGRP promotes coronary vasodilation, even if its effect is predominant in the distal portion of the coronary vessels [44], and is involved in the formation of new blood vessels in response to ischemic insults [45]. Other beneficial effects of CGRP include reducing inflammation and macrophage accumulation, decreasing apoptosis, and post-infarction fibrosis [46]. Indeed, CGRP plays an antiapoptotic role in cardiomyocytes by activating the ERK1/2 signaling pathway [47].
3.1.4. CGRP in Myocardial Infarction and Heart Failure
Following myocardial infarction or during acute heart failure, increased levels of CGRP are observed as a response to metabolic stress and reduced coronary vasodilation [48,49]. Endogenous CGRP administration improves coronary circulation in patients with cardiac pathologies [50,51,52] and performance during exercise tests [53]. CGRP also plays an important role in cardiac preconditioning, providing greater resistance of cardiomyocytes to apoptosis and reducing the inflammatory response [54]. It has also been shown that individuals with coronary artery disease have lower levels of CGRP compared to healthy subjects [55]. Importantly, CGRP inhibitors and antagonists do not seem to increase the risk of ischemia in healthy individuals [56].
3.1.5. CGRP in Atherosclerosis and Vascular Remodeling
Atherosclerosis is characterized by endothelial dysfunction, reduced NO production, intimal inflammation, and the formation of atherosclerotic plaques [57]. CGRP plays a protective role on the endothelium by reducing inflammation and promoting neointimal formation [58,59,60]. Nevertheless, monoclonal antibodies targeting the CGRP receptor (i.e., erenumab) did not modify flow-mediated (endothelial-dependent) dilation in treated patients [61]. Furthermore, CGRP reduces vascular remodeling through increased cAMP levels [62].
3.2. CGRP in the Skin
CGRP plays various roles in the skin. Physiologically, CGRP can be released not only by sensory afferents but also by keratinocytes and immune cells [63]. Primarily, it causes cutaneous vasodilation, increasing blood flow to the affected region in response to various stimuli [32]. For example, it is a modulator of the “skin axon reflex flare” phenomenon, which causes cutaneous vasodilation after stimulation of C-fiber nerve roots and, together with antidromic vasodilation, is responsible for flushing [64]. Increased plasma and urinary levels of CGRP have been observed in patients with postmenopausal flushing [65]. Another function appears to be thermoregulation through the regulation of vasodilation in dermal arterioles [1]. The vasomotor effects of CGRP lead to increased cutaneous edema formation in response to contusions and wounds, with increased vessel permeability and leukocyte accumulation in the skin [64,66]. It also plays a role in immune regulation in atopic dermatitis, reducing the inflammatory response [67].
CGRP in Cutaneous Wound Healing
CGRP enhances wound healing and modulates pain perception [68]. In CGRP gene knockout mice, a reduction in tissue repair is observed [69]. This effect may be associated with CGRP’s ability to stimulate vascular endothelial growth factor (VEGF), promoting neovascularization in the injured area. Furthermore, CGRP appears to promote the proliferation of keratinocytes [70] and fibroblasts [71].
3.3. CGRP in the Respiratory System
CGRP plays various roles in the respiratory system. It is synthesized by pulmonary neuroendocrine cells (PNECs) and is co-localized with substance P in the sensory C fibers [72]. It actively contributes to pulmonary homeostasis by causing vasodilation, and bronchoprotection, modulating the inflammatory response [73] and promoting proliferation of bronchial epithelial cells [74].
3.3.1. CGRP and Asthma
In the context of asthma, CGRP plays a complex role, having both pro-inflammatory and anti-inflammatory effects. On one hand, it activates the Th9 response and induces IL-9 and leukotriene C4 synthesis, leading to bronchial edema [1,73]. On the other hand, it suppresses eosinophilic inflammatory response, similar to anti-IL-5 monoclonal antibodies [73]. It also inhibits the activation of Th2 lymphocytes, suppressing the synthesis of type 2 cytokines, and stimulates the proliferation of regulatory T lymphocytes [75]. CGRP has bronchodilatory effects, improving lung ventilation [73]. Studies are underway to evaluate the effectiveness of a CGRP agonist in bronchial asthma [73].
3.3.2. CGRP and Pulmonary Hypertension
The significant regulatory effect of CGRP on vascular tone also affects the development of pulmonary hypertension. CGRP appears to have a protective role in the development of this condition, as evidenced by reduced plasma levels in rats with pulmonary hypertension [76]. This effect may be secondary to the suppression of endothelin-1 (ET-1) and angiotensin II (ANG2), contributing to the reduction in pulmonary resistance [77]. It has also been suggested that the degeneration of capsaicin-sensitive sensory nerve fibers due to the loss of CGRP may contribute to increased pulmonary pressure in rats [78]. The supplementation of CGRP has been proposed for the treatment of pulmonary hypertension [79].
3.3.3. CGRP and COVID-19
The FDA has approved the clinical use of CGRP antagonists to reduce lung inflammation and acute respiratory distress syndrome (ARDS) in COVID-19 patients [75]. It is believed that CGRP may stimulate IL-6 and polarize the immune response toward Th17 lymphocytes, which represent one of the main pathogenic mechanisms of COVID-19 [75]. However, there are concerns about the effectiveness and safety of these drugs due to the potential beneficial modulatory role of CGRP in pulmonary inflammation [75].
3.4. CGRP and the Gastrointestinal System
CGRP plays various functions in the gastrointestinal tract. In the gastrointestinal tract, two main autonomic nerve afferents are present: the parasympathetic component (vagus and pelvic nerves) and the sympathetic component (splanchnic and hypogastric nerves) [80]. Vagal afferents terminate in the myenteric plexus, circular muscle, and submucosal plexus, while sympathetic afferents are found in the myenteric plexus, submucosa, and mucosa surrounding blood vessels [80]. CGRP and substance P are found in the enteric plexus, interganglionic fibers, muscular layer, and mucosa of both the stomach and intestine. CGRP seems to regulate motility, inflammation, gastric acid secretion, and inflammation in the gastrointestinal system [80].
3.4.1. CGRP and the Stomach
CGRP plays a fundamental role in the protection of gastric mucosa [80]. It appears to inhibit gastric acid secretion and gastric motility [81]. Release from the dorsal roots of the ganglia and vagal ganglia of splanchnic nerves also leads to increased blood flow in the gastric mucosa [80]. It exhibits anti-inflammatory and anti-apoptotic effects on gastric mucosal cells damaged by ischemic processes [80]. CGRP antagonists seem to increase gastric lesions mediated by indomethacin and ethanol, as demonstrated in studies conducted on CGRP knockout mice [82]. The release of CGRP through the activation of TRPV-Q has been shown to improve epigastric pain in patients with dyspepsia and irritable bowel syndrome [83]. Furthermore, the TRPV1 receptors that stimulate CGRP release have been analyzed as potential targets to prevent gastric mucosal damage [84]. The effect of CGRP on gastric motility seems to be mediated both by stimulation of CGRP 1 reception and by activation of amylin receptor 1. CGRP inhibits gastrointestinal transit and gastric emptying [85]. Antagonists of CGRP such as triptans, gepant, and anti-CGRP antibodies are known to lead to gastrointestinal symptoms such as stomach pain, nausea, and vomiting [86,87]. CGRP seems to interact also with Glucagon-Like Peptide-1 (GLP-1) increasing its values by >60% with a bidirectional regulation as GLP-1 has been shown to induce secretion of CGRP [88,89]. Anti-CGRP drugs seem indeed to reduce GLP-1 secretion [88].
3.4.2. CGRP and Metabolic Syndrome
CGRP is released in the pancreas, leading to a reduction in insulin release and an increase in blood glucose levels [90], as well as insulin resistance in muscle. The use of capsaicin to destroy CGRP-containing sensory nerves results in increased glucose tolerance [91]. It also appears to contribute to weight gain, as evidenced by a study on αCGRP knockout mice, which showed a reduction in diet-induced obesity incidence [92]. The activity of sensory nerves releasing CGRP appears to be increased in obesity and metabolic syndrome [1]. Conversely, CGRP has been shown to have a role in appetite reduction. One hour after a meal, an increase in CGRP release in the central nervous system and intestine is observed, with functions similar to insulin [93].
3.5. CGRP and the Musculoskeletal System
Elevated levels of CGRP have been found in the synovial fluid of patients with arthritis [12,94,95,96], suggesting that it may be considered an early mediator of the disease. CGRP can induce cytokine production by leukocytes and fibroblasts in rheumatoid arthritis and osteoarthritis [95,97]. CGRP antagonists inhibit synovial cell proliferation and the production of pro-inflammatory cytokines [98]. Furthermore, CGRP 8-37, a CGRP antagonist, appears to inhibit the hypersensitivity of joint nerve endings responsible for arthritic pain [99]. Interestingly, methotrexate, a drug used in the treatment of rheumatoid arthritis, reduces the presence of CGRP-positive fibers [100]. Although CGRP appears to play a predominant role in inflammatory arthritis, elevated CGRP expression has also been observed in neurons of joints affected by osteoarthritis [94]. Additionally, the drug LY2951742, which neutralizes CGRP, appears to have a protective role in osteoarthritis in mice [101]. Finally, CGRP also seems to play a role also on bone homeostasis and regeneration [102]. The Transient receptor potential vanilloid type 1 (TRPV1) activation in the dorsal root ganglion contributes essentially to the regulation of osteoblast physiology through the modulation of the production and secretion of CGRP [103].
3.6. CGRP and the Urinary System
CGRP is present in renal fibers, primarily in the muscle layer of the pelvis, as well as in peri-glomerular and peritubular arteries and arterioles [104]. It is also found in the ureters and bladder. At the glomerular level, it causes vasodilation and an increase in renal blood flow, leading to a reduction in mean renal pressure [105] and an increase in glomerular filtration [106]. At the tubular level, it increases the excretion of sodium, chloride, potassium, calcium, and phosphates, stimulating urine flow [107,108]. It also appears to increase renin release, although it is unclear whether it acts directly or through its pressor effects on the glomerulus [104].
3.7. CGRP and Sex Hormones
The vasodilatory properties of CGRP are exerted also during pregnancy. The circulating CGRP levels increase during gestation while declining rapidly at term and in the postpartum. In addition, in rats, the sensitivity of various vascular beds to CGRP increases with advancing pregnancy. This action may be essential in regulating uteroplacental blood flow, in addition to other vascular adaptations. Furthermore, the activation of the CGRP pathway is associated with uterine relaxation, possibly as the consequence of the upregulation of CGRP receptors. In this light, sex steroid hormones, estrogens, and progesterone regulate CGRP synthesis and its effects on both myometrial and uterine vascular tissues [109]. CGRP also possibly interacts with oxytocin, another relevant hormone with anti-nociceptive properties also relevant to uterine tone [110]. The systemic effects of CGRP are synthesized in Table 1.

Table 1.
CGRP and its antagonists’ systemic effects.
4. Discussion
The calcitonin gene-related peptide (CGRP) is a molecule that exhibits considerable complexity in its biological activities, displaying effects in various body systems that may, in some cases, appear contradictory. It serves as a molecule that regulates several processes both directly and indirectly, playing a primarily homeostatic role [1]. This characteristic may underlie the low incidence of side effects observed with drugs that interact with CGRP, such as monoclonal antibodies and gepants [87]. The main side effects of these drugs are predominantly gastrointestinal, where CGRP plays a prominent role, slowing gastric emptying, interacting with GLP-1, and reducing hydrochloric acid secretion [81,88]. Both gepants and anti-CGRP monoclonal antibodies have shown common side effects of constipation and nausea [87,111].
Although the main effect of CGRP is to modulate vascular smooth muscle tone, leading to vasodilation, the incidence of such side effects in drugs that antagonize CGRP’s effects is minimal [112], as observed in real-life studies [113,114]. As previously mentioned, the use of CGRP receptor antagonists in mice does not lead to vasoconstriction and arterial hypertension because there is a concomitant release of molecules such as NO and prostaglandins, which ultimately induce relaxation of smooth muscle [39,40]. This review highlights that CGRP’s effect on the vascular system is not exclusively that of a direct vasodilator, but rather that of a regulator that reduces susceptibility to the development of chronic arterial hypertension, as demonstrated by studies on CALC-1 gene polymorphisms [41]. Similarly, at the cardiac level, CGRP has shown protective roles toward cardiomyocytes, reducing apoptosis and inflammation and leading to improved coronary circulation [46,47]. Nonetheless, few ischemic side effects have been observed with therapies with CGRP inhibitors [112]. Studies have demonstrated improved exercise performance after CGRP infusion, but, on the other hand, a randomized trial did not show differences in terms of exercise performance during treadmill testing in patients with stable angina undergoing treatment with anti-CGRP antibodies versus placebo [115]. In the cardiovascular context, it would be beneficial to analyze the long-term effects of these drugs.
The immune role of CGRP is extremely complex and varied. It appears to have both anti-inflammatory and anti-apoptotic roles, as well as pro-inflammatory effects. In the lungs, it directs the immune response toward Th9 lymphocytes while reducing the Th2 response, resulting in increased bronchial edema and, conversely, suppressing eosinophils and causing bronchodilation. At the cutaneous level, vasodilation mediated by CGRP leads to increased edema and passage of leukocytes from the circulatory system to the dermis. On the other hand, CGRP accelerates wound healing processes. It appears to have an anti-inflammatory role in arthritic and arthrosis conditions. A case series has shown the presence of inflammatory complications in patients receiving CGRP inhibitors, such as autoimmune hepatitis, Susac syndrome, DRESS syndrome, Weber syndrome, severe polyarthralgia, exacerbation of psoriasis, and urticarial eczema, after 1–16 months of treatment [11].
5. Conclusions
CGRP represents a regulator of diverse biological processes, including nociception, vasodilation, metabolism, inflammation, and gastrointestinal emptying (Figure 1).
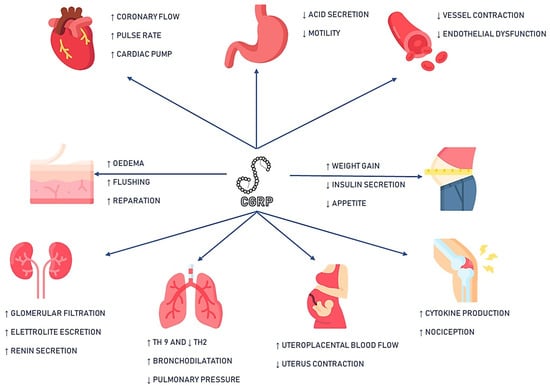
Figure 1.
Synthesis of CGRP systemic effects. Icon’s copyright is to Flaticon (Freepik, Futuer, Vitaly Gorbachev, Smashicon, MindWorlds, England, UK) https://www.flaticon.com/ (accessed on 30 June 2023) Legend: ↑: increase ↓: decrease.
Many of the effects it exerts also appear to have long-term implications. These aspects become even more relevant, considering that migraine, the present indication for CGRP pathway targeted therapies, is often comorbid with disorders involving the same systems [115,116]. Therefore, it is crucial to continue investigating CGRP activities and to be mindful of potential effects resulting from chronic use of its inhibitors especially if comorbid conditions coexist. In this light, to gain a holistic and cutting-edge perspective on CGRP’s functions and its potential applications in diverse somatic domains, future approaches may also include quantitative systems pharmacology modeling, multi-omics analyses, advanced neuronal manipulation techniques, 3D organoid models, machine learning predictive modeling, and synthetic biology [117].
Author Contributions
Conceptualization, C.A. and F.V.; methodology, A.B.; software, A.B.; writing—original draft preparation, A.B.; writing—review and editing C.A., N.B., M.M., G.I. and L.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
C.A. is an associate editor at Frontiers of Human Neuroscience, and has received travel grants and/or personal fees for advisory boards and speaker panels, from Novartis, Eli-Lilly, Lundbeck, Teva, Lusofarmaco, Laborest, Abbvie/Allergan, Almirall. Luisa Fofi has received travel grants, honoraria for advisory boards, and speaker panels, from Novartis, Eli Lilly, and Teva. F.V. has received travel grants, and honoraria for advisory boards, speaker panels, or clinical investigation studies from Allergan/Abbvie, Amgen, Angelini, Eli Lilly, Lundbeck, Novartis, and Teva. N.B., M.M., and A.B. have nothing to disclose.
References
- Russell, F.A.; King, R.; Smillie, S.-J.; Kodji, X.; Brain, S.D.; Pressly, J.D.; Soni, H.; Jiang, S.; Wei, J.; Liu, R.; et al. Calcitonin Gene-Related Peptide: Physiology and Pathophysiology. Physiol. Rev. 2014, 94, 1099–1142. [Google Scholar] [CrossRef]
- Morris, H.R.; Panico, M.; Etienne, T.; Tippins, J.; Girgis, S.I.; MacIntyre, I. Isolation and characterization of human calcitonin gene-related peptide. Nature 1984, 308, 746–748. [Google Scholar] [CrossRef]
- Amara, S.G.; Arriza, J.L.; Leff, S.E.; Swanson, L.W.; Evans, R.M.; Rosenfeld, M.G. Expression in Brain of a Messenger RNA Encoding a Novel Neuropeptide Homologous to Calcitonin Gene-Related Peptide. Science 1985, 229, 1094–1097. [Google Scholar] [CrossRef]
- Maggi, C.A. Tachykinins and calcitonin gene-related peptide (CGRP) as co-transmitters released from peripheral endings of sensory nerves. Prog. Neurobiol. 1995, 45, 1–98. [Google Scholar] [CrossRef]
- Goadsby, P.J.; Edvinsson, L.; Ekman, R. Release of vasoactive peptides in the extracerebral circulation of humans and the cat during activation of the trigeminovascular system. Ann. Neurol. 1988, 23, 193–196. [Google Scholar] [CrossRef]
- Goadsby, P.J.; Edvinsson, L.; Ekman, R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann. Neurol. 1990, 28, 183–187. [Google Scholar] [CrossRef]
- Lassen, L.H.; Haderslev, P.A.; Jacobsen, V.B.; Iversen, H.K.; Sperling, B.; Olesen, J. Cgrp May Play A Causative Role in Migraine. Cephalalgia Int. J. Headache 2002, 22, 54–61. [Google Scholar] [CrossRef]
- Goadsby, P.J.; Edvinsson, L. Peripheral and Central Trigeminovascular Activation in Cat is Blocked by the Serotonin (5HT)-I D Receptor Agonist 311C90. Headache J. Head Face Pain 1994, 34, 394–399. [Google Scholar] [CrossRef]
- Altamura, C.; Brunelli, N.; Marcosano, M.; Fofi, L.; Vernieri, F. Gepants—A long way to cure: A narrative review. Neurol. Sci. 2022, 43, 5697–5708. [Google Scholar] [CrossRef] [PubMed]
- Brain, S.D.; Williams, T.J.; Tippins, J.R.; Morris, H.R.; MacIntyre, I. Calcitonin gene-related peptide is a potent vasodilator. Nature 1985, 313, 54–56. [Google Scholar] [CrossRef]
- Ray, J.C.; Allen, P.; Bacsi, A.; Bosco, J.J.; Chen, L.; Eller, M.; Kua, H.; Lim, L.L.; Matharu, M.S.; Monif, M.; et al. Inflammatory complications of CGRP monoclonal antibodies: A case series. J. Headache Pain 2021, 22, 121. [Google Scholar] [CrossRef]
- Alstergren, P.; Appelgren, A.; Appelgren, B.; Kopp, S.; Lundeberg, T.; Theodorsson, E. Co-variation of neuropeptide Y, calcitonin gene-related peptide, substance P and neurokinin A in joint fluid from patients with temporomandibular joint arthritis. Arch. Oral Biol. 1995, 40, 127–135. [Google Scholar] [CrossRef]
- Wimalawansa, S.J.; Morris, H.R.; Etienne, A.; Blench, I.; Panico, M.; MacIntyre, I. Isolation, purification and characterization of β-hCGRP from human spinal cord. Biochem. Biophys. Res. Commun. 1990, 167, 993–1000. [Google Scholar] [CrossRef]
- Donnerer, J.; Stein, C. Evidence for an Increase in the Release of CGRP from Sensory Nerves during Inflammation. Ann. N. Y. Acad. Sci. 1992, 657, 505–506. [Google Scholar] [CrossRef]
- Supowit, S.C.; Zhao, H.; DiPette, D.J. Nerve growth factor enhances calcitonin gene-related peptide expression in the spontaneously hypertensive rat. Hypertension 2001, 37 Pt 2, 728–732. [Google Scholar] [CrossRef]
- Jang, M.-U.; Park, J.-W.; Kho, H.-S.; Chung, S.-C.; Chung, J.-W. Plasma and saliva levels of nerve growth factor and neuropeptides in chronic migraine patients. Oral Dis. 2010, 17, 187–193. [Google Scholar] [CrossRef]
- Salio, C.; Averill, S.; Priestley, J.; Merighi, A. Costorage of BDNF and neuropeptides within individual dense-core vesicles in central and peripheral neurons. Dev. Neurobiol. 2007, 67, 326–338. [Google Scholar] [CrossRef]
- Schlereth, T.; Schukraft, J.; Krämer-Best, H.H.; Geber, C.; Ackermann, T.; Birklein, F. Interaction of calcitonin gene related peptide (CGRP) and substance P (SP) in human skin. Neuropeptides 2016, 59, 57–62. [Google Scholar] [CrossRef]
- Matteoli, M.; Haimann, C.; Torri-Tarelli, F.; Polak, J.M.; Ceccarelli, B.; De Camilli, P. Differential effect of alpha-latrotoxin on exocytosis from small synaptic vesicles and from large dense-core vesicles containing calcitonin gene-related peptide at the frog neuromuscular junction. Proc. Natl. Acad. Sci. USA 1988, 85, 7366–7370. [Google Scholar] [CrossRef]
- Meng, J.; Wang, J.; Lawrence, G.; Dolly, J.O.; Etournay, R.; Zwaenepoel, I.; Perfettini, I.; Legrain, P.; Petit, C.; El-Amraoui, A. Synaptobrevin I mediates exocytosis of CGRP from sensory neurons and inhibition by botulinum toxins reflects their anti-nociceptive potential. J. Cell Sci. 2007, 120 Pt 16, 2864–2874. [Google Scholar] [CrossRef]
- Caterina, M.J.; Schumacher, M.A.; Tominaga, M.; Rosen, T.A.; Levine, J.D.; Julius, D. The capsaicin receptor: A heat-activated ion channel in the pain pathway. Nature 1997, 389, 816–824. [Google Scholar] [CrossRef]
- Vriens, J.; Appendino, G.; Nilius, B. Pharmacology of Vanilloid Transient Receptor Potential Cation Channels. Mol. Pharmacol. 2009, 75, 1262–1279. [Google Scholar] [CrossRef]
- Deng, P.-Y.; Li, Y.-J. Calcitonin gene-related peptide and hypertension. Peptides 2005, 26, 1676–1685. [Google Scholar] [CrossRef] [PubMed]
- Choksi, T.; Hay, D.L.; Legon, S.; Poyner, D.R.; Hagner, S.; Bloom, S.R.; Smith, D.M. Comparison of the expression of calcitonin receptor-like receptor (CRLR) and receptor activity modifying proteins (RAMPs) with CGRP and adrenomedullin binding in cell lines. Br. J. Pharmacol. 2002, 136, 784–792. [Google Scholar] [CrossRef] [PubMed]
- Muff, R.; Leuthäuser, K.; Bühlmann, N.; Foord, S.M.; Fischer, J.A.; Born, W. Receptor activity modifying proteins regulate the activity of a calcitonin gene-related peptide receptor in rabbit aortic endothelial cells. FEBS Lett. 1998, 441, 366–368. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.T.; Huang, Y.; Brayden, J.E.; Hescheler, J.; Standen, N.B. Arterial dilations in response to calcitonin gene-related peptide involve activation of K+ channels. Nature 1990, 344, 770–773. [Google Scholar] [CrossRef]
- Smillie, S.-J.; King, R.; Kodji, X.; Outzen, E.; Pozsgai, G.; Fernandes, E.; Marshall, N.; de Winter, P.; Heads, R.J.; Dessapt-Baradez, C.; et al. An Ongoing Role of α-Calcitonin Gene–Related Peptide as Part of a Protective Network Against Hypertension, Vascular Hypertrophy, and Oxidative Stress. Hypertension 2014, 63, 1056–1062. [Google Scholar] [CrossRef]
- McGillis, J.P.; Miller, C.N.; Schneider, D.B.; Fernandez, S.; Knopf, M. Calcitonin gene-related peptide induces AP-1 activity by a PKA and c-fos-dependent mechanism in pre-B cells. J. Neuroimmunol. 2002, 123, 83–90. [Google Scholar] [CrossRef]
- Kawase, T.; Okuda, K.; Burns, D.M.; Russell, F.A.; King, R.; Smillie, S.-J.; Kodji, X.; Brain, S.D. Immature osteoblastic MG63 cells possess two calcitonin gene-related peptide receptor subtypes that respond differently to [Cys(Acm)2,7] calcitonin gene-related peptide and CGRP8–37. Am. J. Physiol. Physiol. 2005, 289, C811–C818. [Google Scholar] [CrossRef]
- Schaeffer, C.; Vandroux, D.; Thomassin, L.; Athias, P.; Rochette, L.; Connat, J.-L. Calcitonin gene-related peptide partly protects cultured smooth muscle cells from apoptosis induced by an oxidative stress via activation of ERK1/2 MAPK. Biochim. et Biophys. Acta (BBA)-Mol. Cell Res. 2003, 1643, 65–73. [Google Scholar] [CrossRef]
- Wang, Z.; Ma, W.; Chabot, J.-G.; Quirion, R. Calcitonin gene-related peptide as a regulator of neuronal CaMKII–CREB, microglial p38–NFκB and astroglial ERK–Stat1/3 cascades mediating the development of tolerance to morphine-induced analgesia. Pain 2010, 151, 194–205. [Google Scholar] [CrossRef] [PubMed]
- Brain, S.D.; Tippins, J.R.; Morris, H.R.; Maclntyre, I.; Williams, T.J. Potent Vasodilator Activity of Calcitonin Gene-Related Peptide in Human Skin. J. Investig. Dermatol. 1986, 87, 533–536. [Google Scholar] [CrossRef] [PubMed]
- Itabashi, A.; Kashiwabara, H.; Shibuya, M.; Tanaka, K.; Masaoka, H.; Katayama, S.; Ishii, J. The interaction of calcitonin gene-related peptide with angiotensin II on blood pressure and renin release. J. Hypertens. 1988, 6, S418–S420. [Google Scholar] [CrossRef] [PubMed]
- Portaluppi, F.; Vergnani, L.; Margutti, A.; Ambrosio, M.R.; Bondanelli, M.; Trasforini, G.; Rossi, R.; Degli Uberti, E.C. Modulatory effect of the renin-angiotensin system on the plasma levels of calcitonin gene-related peptide in normal man. J. Clin. Endocrinol. Metab. 1993, 77, 816–820. [Google Scholar] [CrossRef] [PubMed]
- Tatasciore, A.; Renda, G.; Zimarino, M.; Soccio, M.; Bilo, G.; Parati, G.; Schillaci, G.; De Caterina, R. Awake Systolic Blood Pressure Variability Correlates with Target-Organ Damage in Hypertensive Subjects. Hypertension 2007, 50, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Gangula, P.R.R.; Zhao, H.; Supowit, S.; Wimalawansa, S.; DiPette, D.; Yallampalli, C.; Russell, F.A.; King, R.; Smillie, S.-J.; Kodji, X.; et al. Pregnancy and steroid hormones enhance the vasodilation responses to CGRP in rats. Am. J. Physiol. Circ. Physiol. 1999, 276, H284–H288. [Google Scholar] [CrossRef]
- Ando, K.; Pegram, B.L.; Frohlich, E.D.; Russell, F.A.; King, R.; Smillie, S.-J.; Kodji, X.; Brain, S.D.; Grant, A.D. Hemodynamic effects of calcitonin gene-related peptide in spontaneously hypertensive rats. Am. J. Physiol. Integr. Comp. Physiol. 1990, 258 Pt 2, R425–R429. [Google Scholar] [CrossRef]
- Gardiner, S.M.; Compton, A.M.; Kemp, P.A.; Bennett, T.; Bose, C.; Foulkes, R.; Hughes, B. Antagonistic Effect of Human α-Calcitonin Gene–Related Peptide (8–37) on Regional Hemodynamic Actions of Rat Islet Amyloid Polypeptide in Conscious Long-Evans Rats. Diabetes 1991, 40, 948–951. [Google Scholar] [CrossRef]
- Olesen, J.; Diener, H.-C.; Husstedt, I.W.; Goadsby, P.J.; Hall, D.; Meier, U.; Pollentier, S.; Lesko, L.M. Calcitonin Gene–Related Peptide Receptor Antagonist BIBN 4096 BS for the Acute Treatment of Migraine. N. Engl. J. Med. 2004, 350, 1104–1110. [Google Scholar] [CrossRef]
- Petersen, K.; Birk, S.; Lassen, L.; Kruuse, C.; Jonassen, O.; Lesko, L.; Olesen, J. The CGRP-Antagonist, BIBN4096BS Does not Affect Cerebral or Systemic Haemodynamics in Healthy Volunteers. Cephalalgia 2005, 25, 139–147. [Google Scholar] [CrossRef]
- Luo, X.-L.; Yang, T.-L.; Chen, X.-P.; Li, Y.-J. Association of CALCA genetic polymorphism with essential hypertension. Chin. Med. J. 2008, 121, 1407–1410. [Google Scholar] [CrossRef] [PubMed]
- Mulderry, P.K.; Ghatei, M.A.; Bishop, A.E.; Allen, Y.S.; Polak, J.; Bloom, S.R. Distribution and chromatographic characterisation of CGRP-like immunoreactivity in the brain and gut of the rat. Regul. Pept. 1985, 12, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, J.M.; Hua, Y.; Fredholm, B.B. Capsaicin-induced stimulation of the guinea-pig atrium. Involvement of a novel sensory transmitter or a direct action on myocytes? Naunyn-Schmiedeberg’s Arch. Pharmacol. 1984, 325, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.Y.; Edvinsson, L.; Eftekhari, S.; Kimblad, P.O.; Kane, S.A.; Lynch, J.; Hargreaves, R.J.; de Vries, R.; Garrelds, I.M.; Bogaerdt, A.J.v.D.; et al. Characterization of the Calcitonin Gene-Related Peptide Receptor Antagonist Telcagepant (MK-0974) in Human Isolated Coronary Arteries. Experiment 2010, 334, 746–752. [Google Scholar] [CrossRef]
- Tuo, Y.; Guo, X.; Zhang, X.; Wang, Z.; Zhou, J.; Xia, L.; Zhang, Y.; Wen, J.; Jin, D. The biological effects and mechanisms of calcitonin gene-related peptide on human endothelial cell. J. Recept. Signal Transduct. 2013, 33, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Carnevale, K.A.; DiPette, D.J.; Supowit, S.C. Renal protective effects of α-calcitonin gene-related peptide in deoxycorticosterone-salt hypertension. Am. J. Physiol. Physiol. 2013, 304, F1000–F1008. [Google Scholar] [CrossRef][Green Version]
- Zhao, F.-P.; Guo, Z.; Wang, P.-F. Calcitonin gene related peptide (CGRP) inhibits norepinephrine induced apoptosis in cultured rat cardiomyocytes not via PKA or PKC pathways. Neurosci. Lett. 2010, 482, 163–166. [Google Scholar] [CrossRef]
- Mair, J.; Lechleitner, P.; Längle, T.; Wiedermann, C.; Dienstl, F.; Saria, A. Plasma CGRP in acute myocardial infarction. Lancet 1990, 335, 168. [Google Scholar] [CrossRef]
- Preibisz, J.J. Calcitonin Gene-Related Peptide and Regulation of Human Cardiovascular Homeostasis. Am. J. Hypertens. 1993, 6 Pt 1, 434–450. [Google Scholar] [CrossRef]
- Dubois-Randé, J.L.; Merlet, P.; Benvenuti, C.; Sediame, S.; Macquin-Mavier, I.; Chabrier, E.; Braquet, P.; Castaigne, A.; Adnot, S. Effects of calcitonin gene-related peptide on cardiac contractility, coronary hemodynamics and myocardial energetics in idiopathic dilated cardiomyopathy. Am. J. Cardiol. 1992, 70, 906–912. [Google Scholar] [CrossRef]
- Gennari, C.; Nami, R.; Agnusdei, D.; Fischer, J.A. Improved cardiac performance with human calcitonin gene related peptide in patients with congestive heart failure. Cardiovasc. Res. 1990, 24, 239–241. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, R.N.; Roberts, R.H.; Timmis, A.D. Calcitonin gene-related peptide: A haemodynamic study of a novel vasodilator in patients with severe chronic heart failure. Int. J. Cardiol. 1992, 37, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Uren, N.G.; Seydoux, C.; Davies, G.J. Effect of intravenous calcitonin gene related peptide on ischaemia threshold and coronary stenosis severity in humans. Cardiovasc. Res. 1993, 27, 1477–1481. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.J.; Song, Q.J.; Xiao, J. Calcitonin gene-related peptide: An endogenous mediator of preconditioning. Acta Pharmacol. Sin. 2000, 21, 865–869. [Google Scholar] [PubMed]
- Wang, L.H.; Zhou, S.X.; Li, R.C.; Zheng, L.R.; Zhu, J.H.; Hu, S.J.; Sun, Y.L. Serum Levels of Calcitonin Gene-Related Peptide and Substance P are Decreased in Patients with Diabetes Mellitus and Coronary Artery Disease. J. Int. Med. Res. 2012, 40, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Chaitman, B.R.; Ho, A.P.; Behm, M.O.; Rowe, J.F.; Palcza, J.S.; Laethem, T.; Heirman, I.; Panebianco, D.L.; Kobalava, Z.; Martsevich, S.Y.; et al. A Randomized, Placebo-Controlled Study of the Effects of Telcagepant on Exercise Time in Patients with Stable Angina. Clin. Pharmacol. Ther. 2012, 91, 459–466. [Google Scholar] [CrossRef]
- Schiffrin, E.L. Beyond blood pressure: The endothelium and atherosclerosis progression*. Am. J. Hypertens. 2002, 15 Pt 2, 115S–122S. [Google Scholar] [CrossRef]
- DeFeudis, F. Coronary atherosclerosis: Current therapeutic approaches and future trends. Life Sci. 1991, 49, 689–705. [Google Scholar] [CrossRef]
- Huang, J.; Stohl, L.L.; Zhou, X.; Ding, W.; Granstein, R.D. Calcitonin gene-related peptide inhibits chemokine production by human dermal microvascular endothelial cells. Brain Behav. Immun. 2011, 25, 787–799. [Google Scholar] [CrossRef]
- Yang, L.; Sakurai, T.; Kamiyoshi, A.; Ichikawa-Shindo, Y.; Kawate, H.; Yoshizawa, T.; Koyama, T.; Iesato, Y.; Uetake, R.; Yamauchi, A.; et al. Endogenous CGRP protects against neointimal hyperplasia following wire-induced vascular injury. J. Mol. Cell. Cardiol. 2013, 59, 55–66. [Google Scholar] [CrossRef]
- Altamura, C.; Viticchi, G.; Fallacara, A.; Costa, C.M.; Brunelli, N.; Fiori, C.; Silvestrini, M.; Vernieri, F. Erenumab does not alter cerebral hemodynamics and endothelial function in migraine without aura. Cephalalgia 2020, 41, 90–98. [Google Scholar] [CrossRef]
- Li, Y.; Fiscus, R.; Wu, J.; Yang, L.; Wang, X. The antiproliferative effects of calcitonin gene-related peptide in different passages of cultured vascular smooth muscle cells. Neuropeptides 1997, 31, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Roosterman, D.; Goerge, T.; Schneider, S.W.; Bunnett, N.W.; Steinhoff, M. Neuronal Control of Skin Function: The Skin as a Neuroimmunoendocrine Organ. Physiol. Rev. 2006, 86, 1309–1379. [Google Scholar] [CrossRef] [PubMed]
- Brain, S.; Williams, T. Inflammatory oedema induced by synergism between calcitonin gene-related peptide (CGRP) and mediators of increased vascular permeability. Br. J. Pharmacol. 1985, 86, 855–860. [Google Scholar] [CrossRef]
- Hay, D.L.; Poyner, D.R. Calcitonin gene-related peptide, adrenomedullin and flushing. Maturitas 2009, 64, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Buckley, T.L.; Brain, S.D.; Collins, P.D.; Williams, T.J. Inflammatory edema induced by interactions between IL-1 and the neuropeptide calcitonin gene-related peptide. J. Immunol. 1991, 146, 3424–3430. [Google Scholar] [CrossRef]
- Antúnez, C.; Torres, M.; López, S.; Rodriguez-Pena, R.; Blanca, M.; Mayorga, C.; Santamaría-Babi, L. Calcitonin gene-related peptide modulates interleukin-13 in circulating cutaneous lymphocyte-associated antigen-positive T cells in patients with atopic dermatitis. Br. J. Dermatol. 2009, 161, 547–553. [Google Scholar] [CrossRef]
- Khalil, Z.; Helme, R. Sensory Peptides as Neuromodulators of Wound Healing in Aged Rats. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1996, 51, B354–B361. [Google Scholar] [CrossRef]
- Toda, M.; Suzuki, T.; Hosono, K.; Kurihara, Y.; Kurihara, H.; Hayashi, I.; Kitasato, H.; Hoka, S.; Majima, M. Roles of calcitonin gene-related peptide in facilitation of wound healing and angiogenesis. BioMedicine 2008, 62, 352–359. [Google Scholar] [CrossRef]
- Roggenkamp, D.; Köpnick, S.; Stäb, F.; Wenck, H.; Schmelz, M.; Neufang, G. Epidermal Nerve Fibers Modulate Keratinocyte Growth via Neuropeptide Signaling in an Innervated Skin Model. J. Investig. Dermatol. 2013, 133, 1620–1628. [Google Scholar] [CrossRef]
- Scholzen, T.; Armstrong, C.A.; Bunnett, N.W.; Luger, T.A.; Olerud, J.E.; Ansel, J.C. Neuropeptides in the skin: Interactions between the neuroendocrine and the skin immune systems. Exp. Dermatol. 1998, 7, 81–96. [Google Scholar] [CrossRef] [PubMed]
- Pavón-Romero, G.F.; Serrano-Pérez, N.H.; García-Sánchez, L.; Ramírez-Jiménez, F.; Terán, L.M. Neuroimmune Pathophysiology in Asthma. Front. Cell Dev. Biol. 2021, 9, 663535. [Google Scholar] [CrossRef] [PubMed]
- Dakhama, A.; Larsen, G.L.; Gelfand, E.W. Calcitonin gene-related peptide: Role in airway homeostasis. Curr. Opin. Pharmacol. 2004, 4, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhang, M.; Sun, G.-Y.; Liu, Y.-P.; Ran, W.-Z.; Peng, L.; Guan, C.-X. Calcitonin gene-related peptide promotes the wound healing of human bronchial epithelial cells via PKC and MAPK pathways. Regul. Pept. 2013, 184, 22–29. [Google Scholar] [CrossRef]
- Skaria, T.; Wälchli, T.; Vogel, J. CGRP Receptor Antagonism in COVID-19: Potential Cardiopulmonary Adverse Effects. Trends Mol. Med. 2020, 27, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Keith, I.M.; Ekman, R. Dynamic Aspects of Regulatory Lung Peptides in Chronic Hypoxic Pulmonary Hypertension. Exp. Lung Res. 1992, 18, 205–224. [Google Scholar] [CrossRef] [PubMed]
- Champion, H.C.; Bivalacqua, T.J.; Lambert, D.; McNamara, D.B.; Kadowitz, P.J. The influence of candesartan and PD123319 on responses to angiotensin II in the hindquarters vascular bed of the rat. J. Am. Soc. Nephrol. 1999, 10 (Suppl. S11), S95–S97. [Google Scholar]
- Vaishnava, P.; Wang, D.H. Capsaicin Sensitive-Sensory Nerves and Blood Pressure Regulation. Curr. Med. Chem. Hematol. Agents 2003, 1, 177–188. [Google Scholar] [CrossRef]
- Deng, W.; Hilaire, R.-C.S.; Chattergoon, N.N.; Jeter, J.R.; Kadowitz, P.J. Inhibition of vascular smooth muscle cell proliferation in vitro by genetically engineered marrow stromal cells secreting calcitonin gene-related peptide. Life Sci. 2006, 78, 1830–1838. [Google Scholar] [CrossRef]
- Sharkey, K.A. Substance P and Calcitonin Gene-Related Peptide (CGRP) in Gastrointestinal Inflammation. Ann. N. Y. Acad. Sci. 1992, 664, 425–442. [Google Scholar] [CrossRef]
- Taché, Y.; Raybould, H.; Wei, J.Y. Central and Peripheral Actions of Calcitonin Gene-Related Peptide on Gastric Secretory and Motor Function. Adv. Exp. Med. Biol. 1991, 298, 183–198. [Google Scholar] [CrossRef] [PubMed]
- Magierowska, K.; Wojcik, D.; Chmura, A.; Bakalarz, D.; Wierdak, M.; Kwiecien, S.; Sliwowski, Z.; Brzozowski, T.; Magierowski, M. Alterations in Gastric Mucosal Expression of Calcitonin Gene-Related Peptides, Vanilloid Receptors, and Heme Oxygenase-1 Mediate Gastroprotective Action of Carbon Monoxide against Ethanol-Induced Gastric Mucosal Lesions. Int. J. Mol. Sci. 2018, 19, 2960. [Google Scholar] [CrossRef] [PubMed]
- Evangelista, S. Capsaicin Receptor as Target of Calcitonin Gene-Related Peptide in the Gut. Prog. Drug Res. 2014, 68, 259–276. [Google Scholar] [CrossRef] [PubMed]
- Mózsik, G.; Szolcsányi, J.; Dömötör, A. Capsaicin research as a new tool to approach of the human gastrointestinal physiology, pathology and pharmacology. Inflammopharmacology 2007, 15, 232–245. [Google Scholar] [CrossRef]
- Lenz, H.J.; De Schepper, H.U.; De Man, J.G.; Ruyssers, N.E.; Deiteren, A.; Van Nassauw, L.; Timmermans, J.-P.; Martinet, W.; Herman, A.G.; Pelckmans, P.A.; et al. Calcitonin and CGRP inhibit gastrointestinal transit via distinct neuronal pathways. Am. J. Physiol. Liver Physiol. 1988, 254 Pt 1, G920–G924. [Google Scholar] [CrossRef]
- Ailani, J.; Kaiser, E.A.; Mathew, P.G.; McAllister, P.; Russo, A.F.; Vélez, C.; Ramajo, A.P.; Abdrabboh, A.; Xu, C.; Rasmussen, S.; et al. Role of Calcitonin Gene-Related Peptide on the Gastrointestinal Symptoms of Migraine—Clinical Considerations: A Narrative Review. Neurology 2022, 99, 841–853. [Google Scholar] [CrossRef]
- Haanes, K.A.; Edvinsson, L.; Sams, A. Understanding side-effects of anti-CGRP and anti-CGRP receptor antibodies. J. Headache Pain 2020, 21, 26. [Google Scholar] [CrossRef]
- Nilsson, C.; Hansen, T.K.; Rosenquist, C.; Hartmann, B.; Kodra, J.T.; Lau, J.F.; Clausen, T.R.; Raun, K.; Sams, A. Long acting analogue of the calcitonin gene-related peptide induces positive metabolic effects and secretion of the glucagon-like peptide-1. Eur. J. Pharmacol. 2016, 773, 24–31. [Google Scholar] [CrossRef]
- Handelsman, Y.; Wyne, K.; Cannon, A.; Shannon, M.; Schneider, D. Glycemic Efficacy, Weight Effects, and Safety of Once-Weekly Glucagon-Like Peptide-1 Receptor Agonists. J. Manag. Care Spec. Pharm. 2018, 24, S14–S29. [Google Scholar] [CrossRef]
- Bretherton-Watt, D.; Ghatei, M.A.; Jamal, H.; Gilbey, S.G.; Jones, P.M.; Bloom, S.R. The Physiology of Calcitonin Gene?Related Peptide in the Islet Compared with That of Islet Amyloid Polypeptide (Amylin). Ann. N. Y. Acad. Sci. 1992, 657, 299–312. [Google Scholar] [CrossRef]
- Gram, D.X.; Hansen, A.J.; Wilken, M.; Elm, T.; Svendsen, O.; Carr, R.D.; Ahrén, B.; Brand, C.L. Plasma calcitonin gene-related peptide is increased prior to obesity, and sensory nerve desensitization by capsaicin improves oral glucose tolerance in obese Zucker rats. Eur. J. Endocrinol. 2005, 153, 963–969. [Google Scholar] [CrossRef] [PubMed]
- Walker, C.S.; Li, X.; Whiting, L.; Glyn-Jones, S.; Zhang, S.; Hickey, A.J.; Sewell, M.A.; Ruggiero, K.; Phillips, A.R.J.; Kraegen, E.W.; et al. Mice Lacking the Neuropeptide alpha-Calcitonin Gene-Related Peptide Are Protected against Diet-Induced Obesity. Endocrinology 2010, 151, 4257–4269. [Google Scholar] [CrossRef]
- Geary, N. Effects of glucagon, insulin, amylin and CGRP on feeding. Neuropeptides 1999, 33, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Arnalich, F.; de Miguel, E.; Perez-Ayala, C.; Martinez, M.; Vazquez, J.; Gijon-Banos, J.; Hernanz, A. Neuropeptides and interleukin-6 in human joint inflammation. Relationship between intraarticular substance P and interleukin-6 concentrations. Neurosci. Lett. 1994, 170, 251–254. [Google Scholar] [CrossRef] [PubMed]
- Hernanz, A.; DE Miguel, E.; Romera, N.; Perez-Ayala, C.; Gijon, J.; Arnalich, F. Calcitonin gene-related peptide II, substance P and vasoactive intestinal peptide in plasma and synovial fluid from patients with inflammatory joint disease. Rheumatology 1993, 32, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Holmlund, A.; Ekblom, A.; Hansson, P.; Lind, J.; Lundeberg, T.; Theodorsson, E. Concentrations of neuropeptides substance P, neurokinin A, calcitonin gene-related peptide, neuropeptide Y and vasoactive intestinal polypeptide in synovial fluid of the human temporomandibular joint: A correlation with symptoms, signs and arthroscopicfindings. Int. J. Oral Maxillofac. Surg. 1991, 20, 228–231. [Google Scholar] [CrossRef]
- Raap, T.; Jüsten, H.P.; Miller, L.E.; Cutolo, M.; Schölmerich, J.; Straub, R.H. Neurotransmitter modulation of interleukin 6 (IL-6) and IL-8 secretion of synovial fibroblasts in patients with rheumatoid arthritis compared to osteoarthritis. J. Rheumatol. 2000, 27, 2558–2565. [Google Scholar]
- Takeba, Y.; Suzuki, N.; Kaneko, A.; Asai, T.; Sakane, T. Evidence for neural regulation of inflammatory synovial cell func-tions by secreting calcitonin gene-related peptide and vasoactive intestinal peptide in patients with rheumatoid arthritis. Arthritis Rheum. Off. J. Am. Coll. Rheumatol. 1999, 42, 2418–2429. [Google Scholar] [CrossRef]
- McDougall, J.J.; Ferrell, W.R.; Bray, R.C.; Russell, F.A.; King, R.; Smillie, S.-J.; Kodji, X.; Brain, S.D.; Miller, D.; Forrester, K.; et al. Neurogenic origin of articular hyperemia in early degenerative joint disease. Am. J. Physiol. Integr. Comp. Physiol. 1999, 276, R745–R752. [Google Scholar] [CrossRef]
- Baig, J.A.; Iqbal, M.P.; Rehman, R.; Qureshi, A.A.; Ahmed, M. Anti-inflammatory role of methotrexate in adjuvant arthri-tis: Effect on substance p and calcitonin gene-related Peptide in thymus and spleen. J. Coll. Physicians Surg. Pak. 2007, 17, 490–494. [Google Scholar]
- Benschop, R.; Collins, E.; Darling, R.; Allan, B.; Leung, D.; Conner, E.; Nelson, J.; Gaynor, B.; Xu, J.; Wang, X.-F.; et al. Development of a novel antibody to calcitonin gene-related peptide for the treatment of osteoarthritis-related pain. Osteoarthr. Cartil. 2014, 22, 578–585. [Google Scholar] [CrossRef]
- Xu, J.; Wang, J.; Chen, X.; Li, Y.; Mi, J.; Qin, L. The Effects of Calcitonin Gene-Related Peptide on Bone Homeostasis and Regeneration. Curr. Osteoporos. Rep. 2020, 18, 621–632. [Google Scholar] [CrossRef]
- Jiang, Y.; Zhu, Z.; Wang, B.; Yuan, Y.; Zhang, Q.; Li, Y.; Du, Y.; Gong, P. Neuronal TRPV1-CGRP axis regulates bone defect repair through Hippo signaling pathway. Cell. Signal. 2023, 109, 110779. [Google Scholar] [CrossRef]
- Kurtz, A.; Muff, R.; Fischer, J.A. Calcitonin gene products and the kidney. J. Mol. Med. 1989, 67, 870–875. [Google Scholar] [CrossRef]
- Villarreal, D.; Freeman, R.H.; Verburg, K.M.; Brands, M.W. Effects of Calcitonin Gene-Related Peptide on Renal Blood Flow in the Rat. Exp. Biol. Med. 1988, 188, 316–322. [Google Scholar] [CrossRef]
- Kurtz, A.; Schurek, H.-J.; Jelkmann, W.; Muff, R.; Lipp, H.-P.; Heckmann, U.; Eckardt, K.-U.; Scholz, H.; Fischer, J.A.; Bauer, C. Renal mesangium is a target for calcitonin gene-related peptide. Kidney Int. 1989, 36, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Haas, H.G.; Dambacher, M.A.; Aga, J.G.; Lauffenburger, T. Renal effects of calcitonin and parathyroid extract in man. Studies in hypoparathyroidism. J. Clin. Investig. 1971, 50, 2689–2702. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Morel, F. Regulation of Kidney Functions by Hormones: A New Approach. Recent Prog. Horm. Res. 1983, 39, 271–304. [Google Scholar] [CrossRef] [PubMed]
- Yallampalli, C.; Chauhan, M.; Thota, C.S.; Kondapaka, S.; Wimalawansa, S.J. Calcitonin gene-related peptide in pregnancy and its emerging receptor heterogeneity. Trends Endocrinol. Metab. 2002, 13, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Krause, D.N.; Warfvinge, K.; Haanes, K.A.; Edvinsson, L. Hormonal influences in migraine—Interactions of oestrogen, oxytocin and CGRP. Nat. Rev. Neurol. 2021, 17, 621–633. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Ajona, D.; Villar-Martínez, M.D.; Goadsby, P.J. New Generation Gepants: Migraine Acute and Preventive Medications. J. Clin. Med. 2022, 11, 1656. [Google Scholar] [CrossRef] [PubMed]
- Favoni, V.; European Headache Federation School of Advanced Studies (EHF-SAS); Giani, L.; Al-Hassany, L.; Asioli, G.M.; Butera, C.; de Boer, I.; Guglielmetti, M.; Koniari, C.; Mavridis, T.; et al. CGRP and migraine from a cardiovascular point of view: What do we expect from blocking CGRP? J. Headache Pain 2019, 20, 27. [Google Scholar] [CrossRef] [PubMed]
- Vernieri, F.; Brunelli, N.; Marcosano, M.; Aurilia, C.; Egeo, G.; Lovati, C.; Favoni, V.; Perrotta, A.; Maestrini, I.; Rao, R.; et al. Maintenance of response and predictive factors of 1-year GalcanezumAb treatment in real-life migraine patients in Italy: The multicenter prospective cohort GARLIT study. Eur. J. Neurol. 2022, 30, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Vernieri, F.; Brunelli, N.; Guerzoni, S.; Iannone, L.F.; Baraldi, C.; Rao, R.; di Cola, F.S.; Ornello, R.; Cevoli, S.; Lovati, C.; et al. Retreating migraine patients in the second year with monoclonal antibodies anti-CGRP pathway: The multicenter prospective cohort RE-DO study. J. Neurol. 2023. [Google Scholar] [CrossRef]
- Depre, C.; Antalik, L.; Starling, A.; Koren, M.; Eisele, O.; Lenz, R.A.; Mikol, D.D. A Randomized, Double-Blind, Placebo-Controlled Study to Evaluate the Effect of Erenumab on Exercise Time During a Treadmill Test in Patients with Stable Angina. Headache J. Head Face Pain 2018, 58, 715–723. [Google Scholar] [CrossRef]
- Altamura, C.; Corbelli, I.; de Tommaso, M.; Di Lorenzo, C.; Di Lorenzo, G.; Di Renzo, A.; Filippi, M.; Jannini, T.B.; Messina, R.; Parisi, P.; et al. Pathophysiological Bases of Comorbidity in Migraine. Front. Hum. Neurosci. 2021, 15, 640574. [Google Scholar] [CrossRef]
- McComb, M.; Blair, R.H.; Lysy, M.; Ramanathan, M. Machine learning-guided, big data-enabled, biomarker-based systems pharmacology: Modeling the stochasticity of natural history and disease progression. J. Pharmacokinet. Pharmacodyn. 2021, 49, 65–79. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).