CTC, ctDNA, and Exosome in Thyroid Cancers: A Review
Abstract
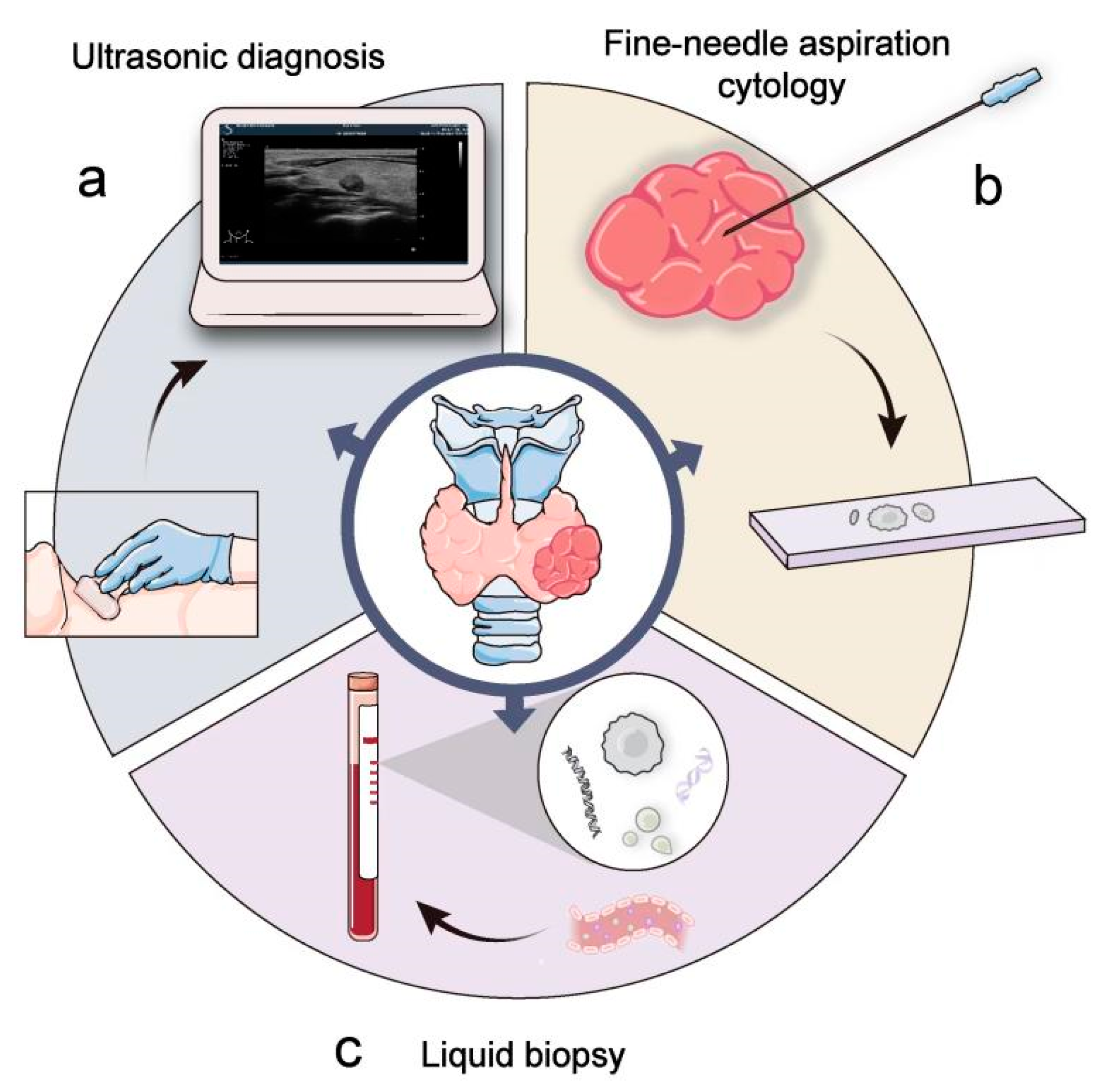
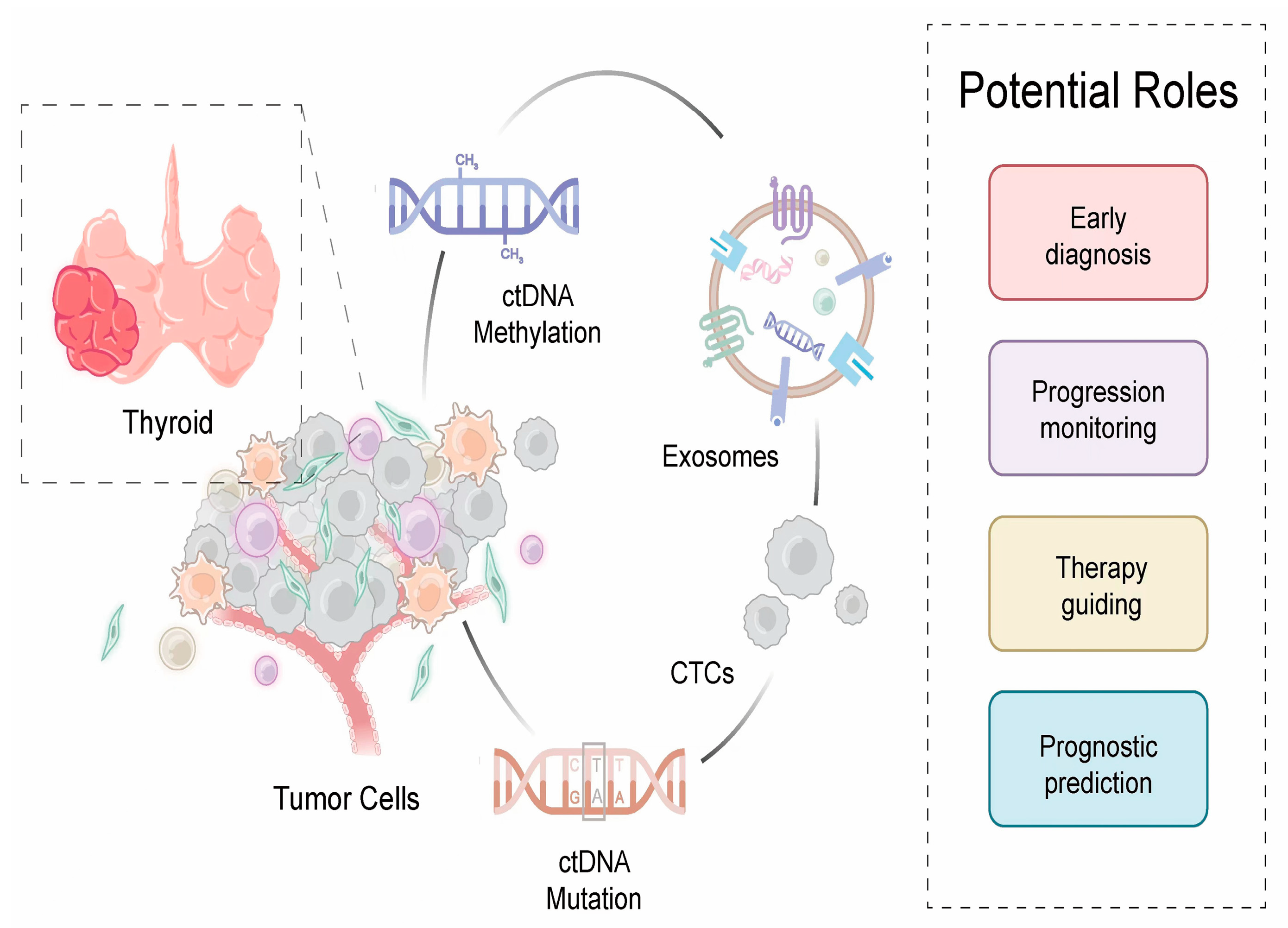
1. Introduction
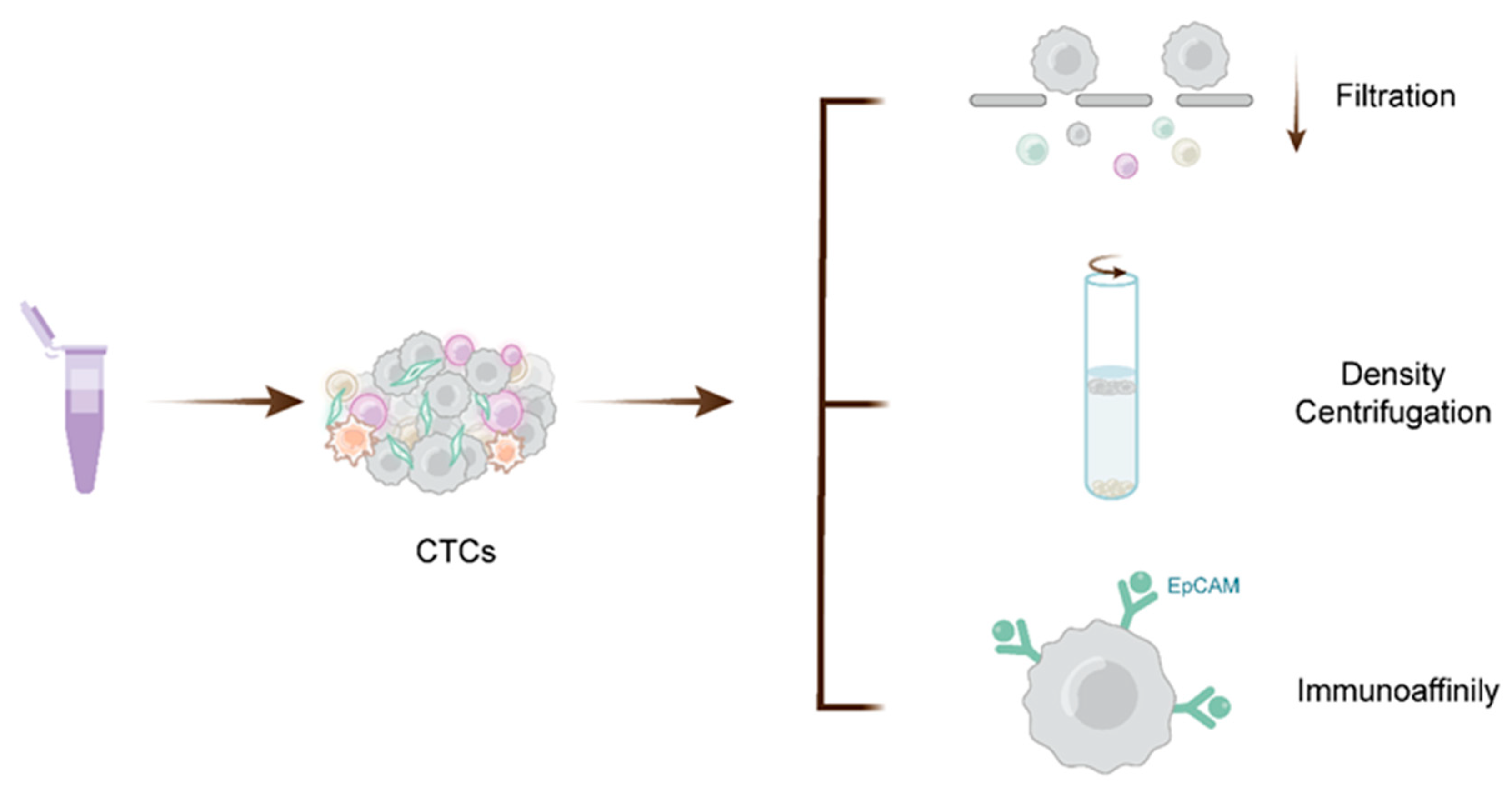
2. CTC and Its Clinical Application
2.1. CTC
2.2. CTCs in Thyroid Cancer
| Study | Year | Technique of Detection | Study Population | Main Finding | Potential Clinical Applications | Ref |
|---|---|---|---|---|---|---|
| Sato et al. | 2005 | RT-PCR test platform | 121 patients (44 patients with benign tumors, 77 patients with malignant tumors) |
|
| [55] |
| Xu et al. | 2016 | Cell Search | 42 patients (18 metMTC, 14 metDTC, 9 DTC, 1 MTC) |
|
| [62] |
| Badulescu et al. | 2018 | Immunomagnetic separation | 26 patients (22 MIFCs, 4 benign thyroid tumors) |
|
| [56] |
| Qiu. et al. | 2018 | NE-iFISH | 102 patients (72 DTC, 30 healthy controls) |
|
| [61] |
| Ehlers et al. | 2018 | Cell Search | 67 patients (33 PTC, 20 FTC, 14 MTC) |
|
| [60] |
| Zheng et al. | 2019 | CanpatrolTM | 234 DTC patients (all had undergone total thyroidectomy, 197 received one RAI therapy after total thyroidectomy) |
|
| [64] |
3. ctDNA and Its Clinical Applications
3.1. ctDNA
3.2. ctDNA in Thyroid Cancer
| Study | Year | Technique | Study Population | Main Finding | Potential Clinical Applications | Ref |
|---|---|---|---|---|---|---|
| Hu et al. | 2006 | Real-time PCR | 39 previously treated thyroid cancer patients (10 had recurrent disease, 20 had no current disease) |
|
| [101] |
| Cradic et al. | 2009 | Allele-specific real-time PCR | 193 patients (173 PTC, 8 FTC, 11 Hurthle cell carcinoma, 1 MTC) |
|
| [91] |
| Chuang et al. | 2010 | Gap-ligase chain reaction technique | 28 patients (14 benign disorders, 14 PTC) |
|
| [90] |
| Kwak et al. | 2013 | Real-time PCR | 94 patients (67 PTMC, 27 lymphocytic thyroid |
| -- | [104] |
| Zane et al. | 2013 | Real-time PCR | 181 patients (9 ATC, 58 MTC, 5 SMFC, 23 FA, 86 PTC) |
|
| [100] |
| Sandulache et al. | 2017 | Digital PCR | 23 patients with ATC |
|
| [95] |
| Lupo et al. | 2018 | PCR | 66 patients with thyroid nodules |
| -- | [105] |
| Allin et al. | 2018 | Digital droplet PCR | 51 patients (17 PTC, 15 FTC, 15 MTC, 3 poorly differentiated thyroid cancer, 1 anaplastic |
|
| [96] |
| Condello et al. | 2018 | Real-time PCR and digital PCR | 83 patients (70 thyroid nodules undergoing surgery, 13 DM-PTC |
| -- | [102] |
| Khatami et al. | 2019 | MS-HRM | 102 patients (57 PTC, 45 Goiter) |
|
| [99] |
| Li et al. | 2019 | QuantStudioTM 3D digital PCR | 59 patients with PTC |
|
| [94] |
| Lan et al. | 2020 | PCR | 36 patients (10 N0M0, 11 N1M0, 15 DM) |
|
| [93] |
| Suh et al. | 2021 | PNA-mediated real-time PCR | 73 matched neoplastic tissues and plasma samples (62 TC, 8 benign thyroid disorders, 3 parathyroid lesions); 54 plasma samples from healthy individuals |
| -- | [103] |
4. Exosomes and Their Clinical Applications
4.1. Exosomes
4.2. Exosomes in Thyroid Cancer
4.2.1. Exosomes as Biomarkers for Disease Staging and Diagnosis
| Study | Year | Components | Technique | Study Population | Main Finding | Potential Clinical Applications | Ref |
|---|---|---|---|---|---|---|---|
| miRNA | |||||||
| Boufraqech et al. | 2014 | miR-145 | qRT-PCR | -- |
|
| [123] |
| Lee et al. | 2015 | miR-146b, miR-222 | qRT-PCR | -- |
|
| [138] |
| Samsonov et al. | 2016 | miR-21, miR-31, mri-181a-5p | qRT-PCR | 50 patients (34 PTC, 8 FTC, 8 benign thyroid adenoma) |
|
| [122] |
| Wang et al. | 2019 | miR-346, miR-34a-5p, miR-10a-5p | qRT-PCR | 3 PTC pools, 1 heathy control pool |
|
| [119] |
| Jiang et al. | 2020 | miR-146b-5p, miR-222-3p | qRT-PCR | 64 patients (49 patients with LNM, 15 patients without LNM) |
|
| [125] |
| Pan et al. | 2020 | miR-5189-3p | qRT-PCR | 20 patients (13 PTC, 7 nodular goiter) |
|
| [120] |
| Dai et al. | 2020 | miR-485-3p, miR-4433a-5p | qRT-PCR | 252 patients (119 PTC, 82 benign thyroid nodules, 51 healthy controls) |
|
| [121] |
| Wen et al. | 2021 | miR-29a | qPT-PCR | 219 patients (119 PTC, 100 healthy controls) |
|
| [118] |
| Chen et al. | 2021 | miR-6774-3p, miR-6879-5p | qRT-PCR | Testing studies: 9 patients (5 PTC-N1, 4 PTC-N0); Validation studies: 59 patients (29 PTC-N1, 30 PTC-N0) |
|
| [124] |
| Capriglione et al. | 2022 | miR24-3p, miR181a-5p, miR146a-5p, miR382-5p | TaqMan Advanced miRNA Array Cards | Two different series of 56 and 58 PTC patients, 18 healthy controls |
|
| [116] |
| Liang et al. | 2020 | miR-34-5p, miR182-5p, miR-223-3p, miR-146b-5p, miR-16-2-3p, miR-223-5p | qRT-PCR | 96 patients (35 PTC patients, 30 benign thyroid nodules, 31 healthy controls) |
|
| [117] |
| IncRNA | |||||||
| Hardin et al. | 2018 | lncRNA MALAT1, lncRNA ROR | qRT-PCR | -- |
|
| [126] |
| Dai et al. | 2020 | lncRNA DOCK9-AS2 | qRT-PCR | 54 PTC patients and 44 healthy controls |
|
| [127] |
| Wen et al. | 2021 | lncSNHG9 | qRT-PCR | -- |
|
| [128] |
| circRNA | |||||||
| Yang et al. | 2019 | circ_007293, circ_031752, circ_020135 | qRT-PCR and high-throughput sequencing | 3 PTC, 3 benign thyroid goiter |
|
| [129] |
| Wu et al. | 2020 | circRASSF2 | qRT-PCR | 10 patients (5 PTC, 5 healthy controls) |
|
| [131] |
| Lin et al. | 2021 | Circ_007293 | qRT-PCR | 80 patients (40 PTC, 40 healthy controls) |
|
| [130] |
| Proteins | |||||||
| Luo et al. | 2018 | SRC, TLN1, ITGB2, CAPNS1, ACTB, Hsp27 | Western blot | 49 patients (16 PTC with LNM, 17 PTC without LNM, 16 healthy controls) |
|
| [133] |
| Caruso et al. | 2019 | Hsp27, Hsp60, and Hsp90 | Western blot | Benign goiter and PTC |
|
| [134] |
| Li et al. | 2021 | ANXA1 | Western blot | 3 PTC patients |
|
| [132] |
4.2.2. Exosomes as Biomarkers for Metastasis and Recurrence Monitoring
5. Future Perspectives
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grimm, D. Recent Advances in Thyroid Cancer Research. Int. J. Mol. Sci. 2022, 23, 4631. [Google Scholar] [CrossRef] [PubMed]
- Abe, I.; Lam, A.K. Fine-Needle Aspiration Under Guidance of Ultrasound Examination of Thyroid Lesions. Methods Mol. Biol. 2022, 2534, 29–37. [Google Scholar] [PubMed]
- Jug, R.; Parajuli, S.; Ahmadi, S.; Jiang, X.S. Negative Results on Thyroid Molecular Testing Decrease Rates of Surgery for Indeterminate Thyroid Nodules. Endocr. Pathol. 2019, 30, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Bongiovanni, M.; Sykiotis, G.P.; La Rosa, S.; Bisig, B.; Trimech, M.; Missiaglia, E.; Gremaud, M.; Chappuis, V.S.; De Vito, C.; Sciarra, A.; et al. Macrofollicular Variant of Follicular Thyroid Carcinoma: A Rare Underappreciated Pitfall in the Diagnosis of Thyroid Carcinoma. Thyroid 2020, 30, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.; Tennant, S.; Perros, P. Serum thyroglobulin in the monitoring of differentiated thyroid cancer. Scand. J. Clin. Lab. Investig. 2016, 76 (Suppl. 245), S119–S123. [Google Scholar] [CrossRef] [PubMed]
- Nabhan, F.; Dedhia, P.H.; Ringel, M.D. Thyroid cancer, recent advances in diagnosis and therapy. Int. J. Cancer. 2021, 149, 984–992. [Google Scholar] [CrossRef]
- Schlumberger, M.; Hitzel, A.; Toubert, M.E.; Corone, C.; Troalen, F.; Schlageter, M.H.; Claustrat, F.; Koscielny, S.; Taieb, D.; Toubeau, M.; et al. Comparison of seven serum thyroglobulin assays in the follow-up of papillary and follicular thyroid cancer patients. J. Clin. Endocrinol. Metab. 2007, 92, 2487–2495. [Google Scholar] [CrossRef]
- Stanojevic, M.; Savin, S.; Cvejic, D.; Djukic, A.; Jeremic, M.; Zivancevic Simonovic, S. Comparison of the influence of thyroglobulin antibodies on serum thyroglobulin values from two different immunoassays in post surgical differentiated thyroid carcinoma patients. J. Clin. Lab. Anal. 2009, 23, 341–346. [Google Scholar] [CrossRef]
- Wassermann, J.; Bernier, M.O.; Spano, J.P.; Lepoutre-Lussey, C.; Buffet, C.; Simon, J.M.; Ménégaux, F.; Tissier, F.; Leban, M.; Leenhardt, L. Outcomes and Prognostic Factors in Radioiodine Refractory Differentiated Thyroid Carcinomas. Oncol. 2016, 21, 50–58. [Google Scholar] [CrossRef]
- Lee, Z.J.O.; Eslick, G.D.; Edirimanne, S. Investigating Antithyroglobulin Antibody As a Prognostic Marker for Differentiated Thyroid Cancer: A Meta-Analysis and Systematic Review. Thyroid 2020, 30, 1601–1612. [Google Scholar] [CrossRef]
- Clement, S.C.; Peeters, R.P.; Ronckers, C.M.; Links, T.P.; van den Heuvel-Eibrink, M.M.; Nieveen van Dijkum, E.J.; Van Rijn, R.R.; Van Der Pal, H.J.H.; Neggers, S.J.; Kremer, L.C.M.; et al. Intermediate and long-term adverse effects of radioiodine therapy for differentiated thyroid carcinoma—A systematic review. Cancer Treat. Rev. 2015, 41, 925–934. [Google Scholar] [CrossRef] [PubMed]
- Sparano, C.; Moog, S.; Hadoux, J.; Dupuy, C.; Al Ghuzlan, A.; Breuskin, I.; Guerlain, J.; Hartl, D.; Baudin, E.; Lamartina, L. Strategies for Radioiodine Treatment: What’s New. Cancers 2022, 14, 3800. [Google Scholar] [CrossRef] [PubMed]
- Cabanillas, M.E.; McFadden, D.G.; Durante, C. Thyroid cancer. Lancet 2016, 388, 2783–2795. [Google Scholar] [CrossRef] [PubMed]
- Durante, C.; Haddy, N.; Baudin, E.; Leboulleux, S.; Hartl, D.; Travagli, J.P.; Caillou, B.; Ricard, M.; Lumbroso, J.D.; De Vathaire, F.; et al. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: Benefits and limits of radioiodine therapy. J. Clin. Endocrinol. Metab. 2006, 91, 2892–2899. [Google Scholar] [CrossRef] [PubMed]
- Alix-Panabières, C.; Pantel, K. Liquid Biopsy: From Discovery to Clinical Application. Cancer Discov. 2021, 11, 858–873. [Google Scholar] [CrossRef]
- Normanno, N.; Cervantes, A.; Ciardiello, F.; De Luca, A.; Pinto, C. The liquid biopsy in the management of colorectal cancer patients: Current applications and future scenarios. Cancer Treat. Rev. 2018, 70, 1–8. [Google Scholar] [CrossRef]
- Romano, C.; Martorana, F.; Pennisi, M.S.; Stella, S.; Massimino, M.; Tirrò, E.; Vitale, S.R.; Di Gregorio, S.; Puma, A.; Tomarchio, C.; et al. Opportunities and Challenges of Liquid Biopsy in Thyroid Cancer. Int. J. Mol. Sci. 2021, 22, 7707. [Google Scholar] [CrossRef]
- Merker, J.D.; Oxnard, G.R.; Compton, C.; Diehn, M.; Hurley, P.; Lazar, A.J.; Lindeman, N.; Lockwood, C.M.; Rai, A.J.; Schilsky, R.L.; et al. Circulating Tumor DNA Analysis in Patients With Cancer: American Society of Clinical Oncology and College of American Pathologists Joint Review. J. Clin. Oncol. 2018, 36, 1631–1641. [Google Scholar] [CrossRef]
- Russo, G.I.; Musso, N.; Romano, A.; Caruso, G.; Petralia, S.; Lanzanò, L.; Broggi, G.; Camarda, M. The Role of Dielectrophoresis for Cancer Diagnosis and Prognosis. Cancers 2021, 14, 198. [Google Scholar] [CrossRef]
- Lu, L.; Hu, W.; Liu, B.; Yang, T. Insights into Circulating Tumor Cell Clusters: A Barometer for Treatment Effects and Prognosis for Prostate Cancer Patients. Cancers 2022, 14, 3985. [Google Scholar] [CrossRef]
- Hou, J.M.; Krebs, M.G.; Lancashire, L.; Sloane, R.; Backen, A.; Swain, R.K.; Priest, L.J.C.; Greystoke, A.; Zhou, C.; Morris, K.; et al. Clinical significance and molecular characteristics of circulating tumor cells and circulating tumor microemboli in patients with small-cell lung cancer. J. Clin. Oncol. 2012, 30, 525–532. [Google Scholar] [CrossRef]
- Augustus, E.; Zwaenepoel, K.; Siozopoulou, V.; Raskin, J.; Jordaens, S.; Baggerman, G.; Sorber, L.; Roeyen, G.; Peeters, M.; Pauwels, P. Prognostic and Predictive Biomarkers in Non-Small Cell Lung Cancer Patients on Immunotherapy—The Role of Liquid Biopsy in Unraveling the Puzzle. Cancers 2021, 13, 1675. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Liu, H.; Chen, Y.; Xiao, N.; Zheng, Z.; Liu, H.; Wan, J. Liquid biopsy on the horizon in immunotherapy of non-small cell lung cancer: Current status, challenges, and perspectives. Cell Death Dis. 2023, 14, 230. [Google Scholar] [CrossRef] [PubMed]
- Heredia-Soto, V.; Rodríguez-Salas, N.; Feliu, J.J.C. Liquid Biopsy in Pancreatic Cancer: Are We Ready to Apply It in the Clinical Practice? Cancers 2021, 13, 1986. [Google Scholar] [CrossRef] [PubMed]
- Heidrich, I.; Abdalla, T.S.A.; Reeh, M.; Pantel, K. Clinical Applications of Circulating Tumor Cells and Circulating Tumor DNA as a Liquid Biopsy Marker in Colorectal Cancer. Cancers 2021, 13, 4500. [Google Scholar] [CrossRef]
- Jiang, M.; Jin, S.; Han, J.; Li, T.; Shi, J.; Zhong, Q.; Li, W.; Tang, W.; Huang, Q.; Zong, H. Detection and clinical significance of circulating tumor cells in colorectal cancer. Biomark. Res. 2021, 9, 85. [Google Scholar] [CrossRef]
- Yu, M.; Stott, S.; Toner, M.; Maheswaran, S.; Haber, D.A. Circulating tumor cells: Approaches to isolation and characterization. J. Cell Biol. 2011, 192, 373–382. [Google Scholar] [CrossRef]
- Ashworth, T.R. A case of cancer in which cells similar to those in the tumors were seen in the blood after death. Aust. Med. J. 1869, 14, 146. [Google Scholar]
- Pachmann, K.; Camara, O.; Kavallaris, A.; Krauspe, S.; Malarski, N.; Gajda, M.; Kroll, T.; Jörke, C.; Hammer, U.; Altendorf-Hofmann, A.; et al. Monitoring the response of circulating epithelial tumor cells to adjuvant chemotherapy in breast cancer allows detection of patients at risk of early relapse. J. Clin. Oncol. 2008, 26, 1208–1215. [Google Scholar] [CrossRef]
- Cohen, S.J.; Punt, C.J.; Iannotti, N.; Saidman, B.H.; Sabbath, K.D.; Gabrail, N.Y.; Picus, J.; Morse, M.; Mitchell, E.; Miller, M.C.; et al. Relationship of circulating tumor cells to tumor response, progression-free survival, and overall survival in patients with metastatic colorectal cancer. J. Clin. Oncol. 2008, 26, 3213–3221. [Google Scholar] [CrossRef]
- Ehlers, M.; Allelein, S.; Haase, M.; Willenberg, H.S.; Knoefel, W.T.; Schott, M. Circulating tumor cells in patients with neuroendocrine neoplasms. Horm. Metab. Res. 2014, 46, 744–745. [Google Scholar] [CrossRef]
- Fan, J.L.; Yang, Y.F.; Yuan, C.H.; Chen, H.; Wang, F.B. Circulating Tumor Cells for Predicting the Prognostic of Patients with Hepatocellular Carcinoma: A Meta Analysis. Cell. Physiol. Biochem. 2015, 37, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Thiele, J.A.; Bethel, K.; Králíčková, M.; Kuhn, P. Circulating Tumor Cells: Fluid Surrogates of Solid Tumors. Annu. Rev. Pathol. 2017, 12, 419–447. [Google Scholar] [CrossRef] [PubMed]
- Aceto, N.; Bardia, A.; Miyamoto, D.T.; Donaldson, M.C.; Wittner, B.S.; Spencer, J.A.; Yu, M.; Pely, A.; Engstrom, A.; Zhu, H.; et al. Circulating tumor cell clusters are oligoclonal precursors of breast cancer metastasis. Cell 2014, 158, 1110–1122. [Google Scholar] [CrossRef]
- Pastushenko, I.; Brisebarre, A.; Sifrim, A.; Fioramonti, M.; Revenco, T.; Boumahdi, S.; Van Keymeulen, A.; Brown, D.; Moers, V.; Lemaire, S.; et al. Identification of the tumour transition states occurring during EMT. Nature 2018, 556, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Thiery, J.P.; Acloque, H.; Huang, R.Y.; Nieto, M.A. Epithelial-mesenchymal transitions in development and disease. Cell 2009, 139, 871–890. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Zhang, X.; Li, J.; Sun, B.; Qian, H.; Yin, Z. The biological and clinical importance of epithelial-mesenchymal transition in circulating tumor cells. J. Cancer Res. Clin. Oncol. 2015, 141, 189–201. [Google Scholar] [CrossRef]
- Li, H.; Batth, I.S.; Qu, X.; Xu, L.; Song, N.; Wang, R.; Liu, Y. IGF-IR signaling in epithelial to mesenchymal transition and targeting IGF-IR therapy: Overview and new insights. Mol. Cancer 2017, 16, 6. [Google Scholar] [CrossRef]
- Hong, B.; Zu, Y. Detecting circulating tumor cells: Current challenges and new trends. Theranostics 2013, 3, 377–394. [Google Scholar] [CrossRef]
- Bankó, P.; Lee, S.Y.; Nagygyörgy, V.; Zrínyi, M.; Chae, C.H.; Cho, D.H.; Telekes, A. Technologies for circulating tumor cell separation from whole blood. J. Hematol. Oncol. 2019, 12, 48. [Google Scholar] [CrossRef]
- Lin, Z.; Luo, G.; Du, W.; Kong, T.; Liu, C.; Liu, Z. Recent Advances in Microfluidic Platforms Applied in Cancer Metastasis: Circulating Tumor Cells’ (CTCs) Isolation and Tumor-On-A-Chip. Small 2020, 16, e1903899. [Google Scholar] [CrossRef]
- Nasiri, R.; Shamloo, A.; Ahadian, S.; Amirifar, L.; Akbari, J.; Goudie, M.J.; Lee, K.; Ashammakhi, N.; Dokmeci, M.R.; Di Carlo, D.; et al. Microfluidic-Based Approaches in Targeted Cell/Particle Separation Based on Physical Properties: Fundamentals and Applications. Small 2020, 16, e2000171. [Google Scholar] [CrossRef]
- Lee, J.S.; Park, S.S.; Lee, Y.K.; Norton, J.A.; Jeffrey, S.S. Liquid biopsy in pancreatic ductal adenocarcinoma: Current status of circulating tumor cells and circulating tumor DNA. Mol. Oncol. 2019, 13, 1623–1650. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.; Wu, J.; Lu, Y.; Chan, Y.T.; Zhang, C.; Wang, D.; Luo, D.; Huang, Y.; Feng, Y.; Wang, N. Circulating tumor cells in the early detection of human cancers. Int. J. Biol. Sci. 2022, 18, 3251–3265. [Google Scholar] [CrossRef] [PubMed]
- Petrik, J.; Verbanac, D.; Fabijanec, M.; Hulina-Tomašković, A.; Čeri, A.; Somborac-Bačura, A.; Petlevski, R.; Rajković, M.G.; Rumora, L.; Krušlin, B.; et al. Circulating Tumor Cells in Colorectal Cancer: Detection Systems and Clinical Utility. Int. J. Mol. Sci. 2022, 23, 13582. [Google Scholar] [CrossRef] [PubMed]
- Di Trapani, M.; Manaresi, N.; Medoro, G. DEPArray system: An automatic image-based sorter for isolation of pure circulating tumor cells. Cytom. Part A 2018, 93, 1260–1266. [Google Scholar] [CrossRef] [PubMed]
- Saucedo-Zeni, N.; Mewes, S.; Niestroj, R.; Gasiorowski, L.; Murawa, D.; Nowaczyk, P.; omasi, T.; Weber, E.; Dworacki, G.; Morgenthaler, G.; et al. A novel method for the in vivo isolation of circulating tumor cells from peripheral blood of cancer patients using a functionalized and structured medical wire. Int. J. Oncol. 2012, 41, 1241–1250. [Google Scholar]
- Talasaz, A.H.; Powell, A.A.; Huber, D.E.; Berbee, J.G.; Roh, K.H.; Yu, W.; Xiao, W.; Davis, M.M.; Pease, R.F.; Mindrinos, M.N.; et al. Isolating highly enriched populations of circulating epithelial cells and other rare cells from blood using a magnetic sweeper device. Proc. Natl. Acad. Sci. USA 2009, 106, 3970–3975. [Google Scholar] [CrossRef]
- Liu, Z.; Fusi, A.; Klopocki, E.; Schmittel, A.; Tinhofer, I.; Nonnenmacher, A.; Keilholz, U. Negative enrichment by immunomagnetic nanobeads for unbiased characterization of circulating tumor cells from peripheral blood of cancer patients. J. Transl. Med. 2011, 9, 70. [Google Scholar] [CrossRef]
- Ringel, M.D.; Ladenson, P.W.; Levine, M.A. Molecular diagnosis of residual and recurrent thyroid cancer by amplification of thyroglobulin messenger ribonucleic acid in peripheral blood. J. Clin. Endocrinol. Metab. 1998, 83, 4435–4442. [Google Scholar] [CrossRef]
- Haugen, B.R. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: What is new and what has changed? Cancer 2017, 123, 372–381. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.; Shen, L.; Luo, M.; Zhang, K.; Li, J.; Yang, Q.; Zhu, F.; Zhou, D.; Zheng, S.; Chen, Y.; et al. Circulating tumor cells: Biology and clinical significance. Signal Transduct. Target. Ther. 2021, 6, 404. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Han, M.; Lee, J.H.; Song, D.E.; Kim, K.; Baek, J.H.; Shong, Y.K.; Kim, W.G. Tumour growth rate of follicular thyroid carcinoma is not different from that of follicular adenoma. Clin. Endocrinol. 2018, 88, 936–942. [Google Scholar] [CrossRef]
- Franc, B.; de la Salmonière, P.; Lange, F.; Hoang, C.; Louvel, A.; de Roquancourt, A.; Vildé, F.; Hejblum, G.; Chevret, S.; Chastang, C. Interobserver and intraobserver reproducibility in the histopathology of follicular thyroid carcinoma. Hum. Pathol. 2003, 34, 1092–1100. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Harao, M.; Nakano, S.; Jotsuka, T.; Suda, N.; Yamashita, J. Circulating tumor cells detected by reverse transcription-polymerase chain reaction for carcinoembryonic antigen mRNA: Distinguishing follicular thyroid carcinoma from adenoma. Surgery 2005, 137, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Badulescu, C.I.; Marlowe, R.J.; Piciu, A.; Buiga, R.; Barbos, O.; Bejinariu, N.I.; Chereches, G.; Barbus, E.; Bonci, E.A.; Piciu, D. Circulating tumor cells in minimally invasive follicular thyroid carcinoma and benign thyroid tumors with a follicular pattern: Pilot experience. Acta Endocrinol. 2018, 14, 1–10. [Google Scholar] [CrossRef]
- Xu, W.; Cao, L.; Chen, L.; Li, J.; Zhang, X.-F.; Qian, H.-H.; Kang, X.-Y.; Zhang, Y.; Liao, J.; Shi, L.-H.; et al. Isolation of circulating tumor cells in patients with hepatocellular carcinoma using a novel cell separation strategy. Clin. Cancer Res. 2011, 17, 3783–3793. [Google Scholar] [CrossRef]
- Wu, C.H.; Lin, S.R.; Hsieh, J.S.; Chen, F.M.; Lu, C.Y.; Yu, F.J.; Cheng, T.L.; Huang, T.J.; Huang, S.Y.; Wang, J.Y. Molecular detection of disseminated tumor cells in the peripheral blood of patients with gastric cancer: Evaluation of their prognostic significance. Dis. Markers 2006, 22, 103–109. [Google Scholar] [CrossRef]
- Pinzani, P.; Scatena, C.; Salvianti, F.; Corsini, E.; Canu, L.; Poli, G.; Paglierani, M.; Piccini, V.; Pazzagli, M.; Nesi, G.; et al. Detection of circulating tumor cells in patients with adrenocortical carcinoma: A monocentric preliminary study. J. Clin. Endocrinol. Metab. 2013, 98, 3731–3738. [Google Scholar] [CrossRef]
- Ehlers, M.; Allelein, S.; Schwarz, F.; Hautzel, H.; Kuebart, A.; Schmidt, M.; Haase, M.; Dringenberg, T.; Schott, M. Increased Numbers of Circulating Tumor Cells in Thyroid Cancer Patients. Horm. Metab. Res. 2018, 50, 602–608. [Google Scholar] [CrossRef]
- Qiu, Z.-L.; Wei, W.-J.; Sun, Z.-K.; Shen, C.-T.; Song, H.-J.; Zhang, X.-Y.; Zhang, G.-Q.; Chen, X.-Y.; Luo, Q.-Y. Circulating Tumor Cells Correlate with Clinicopathological Features and Outcomes in Differentiated Thyroid Cancer. Cell. Physiol. Biochem. 2018, 48, 718–730. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.Y.; Handy, B.; Michaelis, C.L.; Waguespack, S.G.; Hu, M.I.; Busaidy, N.; Jimenez, C.; Cabanillas, M.E.; Fritsche, H.A.; Cote, G.J.; et al. Detection and Prognostic Significance of Circulating Tumor Cells in Patients With Metastatic Thyroid Cancer. J. Clin. Endocrinol. Metab. 2016, 101, 4461–4467. [Google Scholar] [CrossRef] [PubMed]
- Winkens, T.; Pachmann, K.; Freesmeyer, M. The influence of radioiodine therapy on the number of circulating epithelial cells (CEC) in patients with differentiated thyroid carcinoma—A pilot study. Exp. Clin. Endocrinol. Diabetes 2014, 122, 246–253. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zheng, L.; Wang, G.; Guo, W.; Pan, D.; Xie, L.; He, S.; Luo, C.; Li, H.; Ran, Y.; Wu, S.; et al. NIS and epithelial-mesenchymal transition marker expression of circulating tumor cells for predicting and monitoring the radioactive iodine-131 therapy effect in differentiated thyroid cancers. Mol. Biol. Rep. 2019, 46, 4201–4212. [Google Scholar] [CrossRef]
- Shields, M.D.; Chen, K.; Dutcher, G.; Patel, I.; Pellini, B. Making the Rounds: Exploring the Role of Circulating Tumor DNA (ctDNA) in Non-Small Cell Lung Cancer. Int. J. Mol. Sci. 2022, 23, 9006. [Google Scholar] [CrossRef]
- Yoon, H.J.; Kozminsky, M.; Nagrath, S. Emerging role of nanomaterials in circulating tumor cell isolation and analysis. ACS Nano 2014, 8, 1995–2017. [Google Scholar] [CrossRef]
- Sánchez-Herrero, E.; Serna-Blasco, R.; Robado de Lope, L.; González-Rumayor, V.; Romero, A.; Provencio, M. Circulating Tumor DNA as a Cancer Biomarker: An Overview of Biological Features and Factors That may Impact on ctDNA Analysis. Front. Oncol. 2022, 12, 943253. [Google Scholar] [CrossRef]
- Siravegna, G.; Sartore-Bianchi, A.; Nagy, R.J.; Raghav, K.; Odegaard, J.I.; Lanman, R.B.; Trusolino, L.; Marsoni, S.; Siena, S.; Bardelli, A. Plasma HER2 (ERBB2) Copy Number Predicts Response to HER2-targeted Therapy in Metastatic Colorectal Cancer. Clin. Cancer Res. 2019, 25, 3046–3053. [Google Scholar] [CrossRef]
- Caputo, V.; Ciardiello, F.; Della Corte, C.M.; Martini, G.; Troiani, T.; Napolitano, S. Diagnostic value of liquid biopsy in the era of precision medicine: 10 years of clinical evidence in cancer. Explor. Target. Anti-Tumor Ther. 2023, 4, 102–138. [Google Scholar] [CrossRef]
- Corcoran, R.B.; Chabner, B.A. Application of Cell-free DNA Analysis to Cancer Treatment. N. Engl. J. Med. 2018, 379, 1754–1765. [Google Scholar] [CrossRef]
- Jiang, B.; Xie, D.; Wang, S.; Li, X.; Wu, G. Advances in early detection methods for solid tumors. Front. Genet. 2023, 14, 1091223. [Google Scholar] [CrossRef]
- Ye, Q.; Ling, S.; Zheng, S.; Xu, X. Liquid biopsy in hepatocellular carcinoma: Circulating tumor cells and circulating tumor DNA. Mol. Cancer 2019, 18, 114. [Google Scholar] [CrossRef]
- Tan, L.; Sandhu, S.; Lee, R.J.; Li, J.; Callahan, J.; Ftouni, S.; Dhomen, N.; Middlehurst, P.; Wallace, A.; Raleigh, J.; et al. Prediction and monitoring of relapse in stage III melanoma using circulating tumor DNA. Ann. Oncol. 2019, 30, 804–814. [Google Scholar] [CrossRef]
- Nikanjam, M.; Kato, S.; Kurzrock, R. Liquid biopsy: Current technology and clinical applications. J. Hematol. Oncol. 2022, 15, 131. [Google Scholar] [CrossRef]
- De Abreu, A.R.; Op de Beeck, K.; Laurent-Puig, P.; Taly, V.; Benhaim, L. The Position of Circulating Tumor DNA in the Clinical Management of Colorectal Cancer. Cancers 2023, 15, 1284. [Google Scholar] [CrossRef]
- Yu, S.C.; Lee, S.W.; Jiang, P.; Leung, T.Y.; Chan, K.C.A.; Chiu, R.W.; Lo, Y.D. High-resolution profiling of fetal DNA clearance from maternal plasma by massively parallel sequencing. Clin. Chem. 2013, 59, 1228–1237. [Google Scholar] [CrossRef] [PubMed]
- Scherer, F. Capturing Tumor Heterogeneity and Clonal Evolution by Circulating Tumor DNA Profiling. Recent. Results Cancer Res. 2020, 215, 213–230. [Google Scholar]
- Hannigan, B.; Ye, W.; Mehrotra, M.; Lam, V.; Bolivar, A.; Zalles, S.; Barkoh, B.; Duose, D.; Hu, P.; Broaddus, R.; et al. Liquid biopsy assay for lung carcinoma using centrifuged supernatants from fine-needle aspiration specimens. Ann. Oncol. 2019, 30, 963–969. [Google Scholar] [CrossRef]
- Huang, T.Y.; Piunti, A.; Lulla, R.R.; Qi, J.; Horbinski, C.M.; Tomita, T.; James, C.D.; Shilatifard, A.; Saratsis, A.M. Detection of Histone H3 mutations in cerebrospinal fluid-derived tumor DNA from children with diffuse midline glioma. Acta Neuropathol. Commun. 2017, 5, 28. [Google Scholar] [CrossRef] [PubMed]
- Olmedillas-López, S.; Olivera-Salazar, R.; García-Arranz, M.; García-Olmo, D. Current and Emerging Applications of Droplet Digital PCR in Oncology: An Updated Review. Mol. Diagn. Ther. 2022, 26, 61–87. [Google Scholar] [CrossRef] [PubMed]
- Palacín-Aliana, I.; García-Romero, N.; Asensi-Puig, A.; Carrión-Navarro, J.; González-Rumayor, V.; Ayuso-Sacido, Á. Clinical Utility of Liquid Biopsy-Based Actionable Mutations Detected via ddPCR. Biomedicines 2021, 9, 906. [Google Scholar] [CrossRef]
- Hindson, B.J.; Ness, K.D.; Masquelier, D.A.; Belgrader, P.; Heredia, N.J.; Makarewicz, A.J.; Bright, I.J.; Lucero, M.Y.; Hiddessen, A.L.; Legler, T.C.; et al. High-throughput droplet digital PCR system for absolute quantitation of DNA copy number. Anal. Chem. 2011, 83, 8604–8610. [Google Scholar] [CrossRef] [PubMed]
- Sacher, A.G.; Paweletz, C.; Dahlberg, S.E.; Alden, R.S.; O’Connell, A.; Feeney, N.; Mach, S.L.; Jänne, P.A.; Oxnard, G.R. Prospective Validation of Rapid Plasma Genotyping for the Detection of EGFR and KRAS Mutations in Advanced Lung Cancer. JAMA Oncol. 2016, 2, 1014–1022. [Google Scholar] [CrossRef] [PubMed]
- Stahlberg, A.; Krzyzanowski, P.M.; Egyud, M.; Filges, S.; Stein, L.; Godfrey, T.E. Simple multiplexed PCR-based barcoding of DNA for ultrasensitive mutation detection by next-generation sequencing. Nat. Protoc. 2017, 12, 664–682. [Google Scholar] [CrossRef] [PubMed]
- Sanger, F.; Nicklen, S.; Coulson, A.R. DNA sequencing with chain-terminating inhibitors. Proc. Natl. Acad. Sci. USA 1977, 74, 5463–5467. [Google Scholar] [CrossRef] [PubMed]
- Beaver, J.A.; Jelovac, D.; Balukrishna, S.; Cochran, R.; Croessmann, S.; Zabransky, D.J.; Wong, H.Y.; Toro, P.V.; Cidado, J.; Blair, B.G.; et al. Detection of cancer DNA in plasma of patients with early-stage breast cancer. Clin. Cancer Res. 2014, 20, 2643–2650. [Google Scholar] [CrossRef]
- Postel, M.; Roosen, A.; Laurent-Puig, P.; Taly, V.; Wang-Renault, S.F. Droplet-based digital PCR and next generation sequencing for monitoring circulating tumor DNA: A cancer diagnostic perspective. Expert. Rev. Mol. Diagn. 2018, 18, 7–17. [Google Scholar] [CrossRef]
- Chae, Y.K.; Davis, A.A.; Jain, S.; Santa-Maria, C.; Flaum, L.; Beaubier, N.; Platanias, L.C.; Gradishar, W.; Giles, F.J.; Cristofanilli, M. Concordance of Genomic Alterations by Next-Generation Sequencing in Tumor Tissue versus Circulating Tumor DNA in Breast Cancer. Mol. Cancer Ther. 2017, 16, 1412–1420. [Google Scholar] [CrossRef]
- Giroux Leprieur, E.; Herbretau, G.; Dumenil, C.; Julie, C.; Giraud, V.; Labrune, S.; Dumoulin, J.; Tisserand, J.; Emile, J.-F.; Blons, H.; et al. Circulating tumor DNA evaluated by Next-Generation Sequencing is predictive of tumor response and prolonged clinical benefit with nivolumab in advanced non-small cell lung cancer. Oncoimmunology 2018, 7, e1424675. [Google Scholar] [CrossRef]
- Chuang, T.C.; Chuang, A.Y.; Poeta, L.; Koch, W.M.; Califano, J.A.; Tufano, R.P. Detectable BRAF mutation in serum DNA samples from patients with papillary thyroid carcinomas. Head. Neck 2010, 32, 229–234. [Google Scholar]
- Cradic, K.W.; Milosevic, D.; Rosenberg, A.M.; Erickson, L.A.; McIver, B.; Grebe, S.K. Mutant BRAFT1799A can be detected in the blood of papillary thyroid carcinoma patients and correlates with disease status. J. Clin. Endocrinol. Metab. 2009, 94, 5001–5009. [Google Scholar] [CrossRef] [PubMed]
- Vdovichenko, K.K.; Markova, S.I.; Belokhvostov, A.S. Mutant form of BRAF gene in blood plasma of cancer patients. Ann. N. Y Acad. Sci. 2004, 1022, 228–231. [Google Scholar] [CrossRef] [PubMed]
- Lan, X.; Bao, H.; Ge, X.; Cao, J.; Fan, X.; Zhang, Q.; Liu, K.; Zhang, X.; Tan, Z.; Zheng, C.; et al. Genomic landscape of metastatic papillary thyroid carcinoma and novel biomarkers for predicting distant metastasis. Cancer Sci. 2020, 111, 2163–2173. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zhao, J.; Zhang, J.; Wang, C.; Li, M.; Wu, S.; Su, Z.; Pan, Q. Detection of ctDNA in the plasma of patients with papillary thyroid carcinoma. Exp. Ther. Med. 2019, 18, 3389–3396. [Google Scholar] [CrossRef]
- Sandulache, V.C.; Williams, M.D.; Lai, S.Y.; Lu, C.; William, W.N.; Busaidy, N.L.; Cote, G.J.; Singh, R.R.; Luthra, R.; Cabanillas, M.E.; et al. Real-Time Genomic Characterization Utilizing Circulating Cell-Free DNA in Patients with Anaplastic Thyroid Carcinoma. Thyroid 2017, 27, 81–87. [Google Scholar] [CrossRef]
- Allin, D.; Shaikh, R.; Carter, P.; Thway, K.; Sharabiani, M.; Gonzales-de-Castro, D.; O’Leary, B.; Garcia-Murillas, I.; Bhide, S.; Hubank, M.; et al. Circulating tumour DNA is a potential biomarker for disease progression and response to targeted therapy in advanced thyroid cancer. Eur. J. Cancer 2018, 103, 165–175. [Google Scholar] [CrossRef]
- Khatami, F.; Larijani, B.; Heshmat, R.; Keshtkar, A.; Mohammadamoli, M.; Teimoori-Toolabi, L.; Nasiri, S.; Tavangar, S.M. Meta-analysis of promoter methylation in eight tumor-suppressor genes and its association with the risk of thyroid cancer. PLoS ONE 2017, 12, e0184892. [Google Scholar] [CrossRef]
- Gu, P.; Zeng, Y.; Ma, W.; Zhang, W.; Liu, Y.; Guo, F.; Ruan, X.; Chi, J.; Zheng, X.; Gao, M. Characterization of the CpG island methylator phenotype subclass in papillary thyroid carcinoma. Front. Endocrinol. 2022, 13, 1008301. [Google Scholar] [CrossRef]
- Khatami, F.; Teimoori-Toolabi, L.; Heshmat, R.; Nasiri, S.; Saffar, H.; Mohammadamoli, M.; Aghdam, M.H.; Larijani, B. Circulating ctDNA methylation quantification of two DNA methyl transferases in papillary thyroid carcinoma. J. Cell. Biochem. 2019, 120, 17422–17437. [Google Scholar] [CrossRef]
- Zane, M.; Agostini, M.; Enzo, M.V.; Casal Ide, E.; Del Bianco, P.; Torresan, F.; Boschin, I.M.; Pennelli, G.; Saccani, A.; Rubello, D.; et al. Circulating cell-free DNA, SLC5A8 and SLC26A4 hypermethylation, BRAFV600E: A non-invasive tool panel for early detection of thyroid cancer. Biomed. Pharmacother. 2013, 67, 723–730. [Google Scholar] [CrossRef]
- Hu, S.; Ewertz, M.; Tufano, R.P.; Brait, M.; Carvalho, A.L.; Liu, D.; Tufaro, A.P.; Basaria, S.; Cooper, D.S.; Sidransky, D.; et al. Detection of serum deoxyribonucleic acid methylation markers: A novel diagnostic tool for thyroid cancer. J. Clin. Endocrinol. Metab. 2006, 91, 98–104. [Google Scholar] [CrossRef]
- Condello, V.; Macerola, E.; Ugolini, C.; De Napoli, L.; Romei, C.; Materazzi, G.; Elisei, R.; Basolo, F. Analysis of circulating tumor DNA does not improve the clinical management of patients with locally advanced and metastatic papillary thyroid carcinoma. Head Neck 2018, 40, 1752–1758. [Google Scholar] [CrossRef]
- Suh, Y.; Kwon, M.; Noh, H.; Lee, H.; Ra, Y.; Kim, N.J.H. Limited Clinical and Diagnostic Utility of Circulating Tumor DNA Detection in Patients with Early-Stage Well-Differentiated Thyroid Cancer: Comparison with Benign Thyroid Nodules and Healthy Indi-viduals. Healthcare 2021, 9, 386. [Google Scholar] [CrossRef]
- Kwak, J.Y.; Jeong, J.J.; Kang, S.W.; Park, S.; Choi, J.R.; Park, S.J.; Kim, E.K.; Chung, W.Y. Study of peripheral BRAFV600E mutation as a possible novel marker for papillary thyroid carcinomas. Head Neck 2013, 35, 1630–1633. [Google Scholar] [CrossRef]
- Lupo, M.; Guttler, R.; Geck, Z.; Tonozzi, T.R.; Kammesheidt, A.; Braunstein, G.D. Is measurement of circulating tumor dna of diagnostic use in patients with thyroid nodules? Endocr. Pract. 2018, 24, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Kalluri, R.; LeBleu, V.S. The biology, function, and biomedical applications of exosomes. Science 2020, 367, eaau6977. [Google Scholar] [CrossRef] [PubMed]
- Alzhrani, G.N.; Alanazi, S.T.; Alsharif, S.Y.; Albalawi, A.M.; Alsharif, A.A.; Abdel-Maksoud, M.S.; Elsherbiny, N. Exosomes: Isolation, characterization, and biomedical applications. Cell Biol. Int. 2021, 45, 1807–1831. [Google Scholar] [CrossRef] [PubMed]
- Mashouri, L.; Yousefi, H.; Aref, A.R.; Ahadi, A.M.; Molaei, F.; Alahari, S.K. Exosomes: Composition, biogenesis, and mechanisms in cancer metastasis and drug resistance. Mol. Cancer 2019, 18, 75. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.; Li, D.; Hou, S.; Zhu, X. The cancer exosomes: Clinical implications, applications and challenges. Int. J. Cancer 2020, 146, 2946–2959. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhang, Y.; Gong, H.; Luo, S.; Cui, Y. The Role of Exosomes and Their Applications in Cancer. Int. J. Mol. Sci. 2021, 22, 12204. [Google Scholar] [CrossRef]
- Thery, C.; Zitvogel, L.; Amigorena, S. Exosomes: Composition, biogenesis and function. Nat. Rev. Immunol. 2002, 2, 569–579. [Google Scholar] [CrossRef] [PubMed]
- Asaadi, A.; Dolatabad, N.A.; Atashi, H.; Raes, A.; Van Damme, P.; Hoelker, M.; Hendrix, A.; Pascottini, O.B.; Van Soom, A.; Kafi, M.; et al. Extracellular Vesicles from Follicular and Ampullary Fluid Isolated by Density Gradient Ultracentrifugation Improve Bovine Embryo Development and Quality. Int. J. Mol. Sci. 2021, 22, 578. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.-L.; Zhu, J.; Liu, J.-X.; Jiang, F.; Ni, W.-K.; Qu, L.S.; Ni, R.-Z.; Lu, C.-H.; Xiao, M.-B. A Comparison of Traditional and Novel Methods for the Separation of Exosomes from Human Samples. Biomed. Res. Int. 2018, 2018, 3634563. [Google Scholar] [CrossRef]
- Sundaram, P.M.; Casadei, L.; Lopez, G.; Braggio, D.; Balakirsky, G.; Pollock, R.; Prakash, S. Multi-Layer Micro-Nanofluidic Device for Isolation and Capture of Extracellular Vesicles Derived from Liposarcoma Cell Conditioned Media. J. Microelectromech. Syst. 2020, 29, 776–782. [Google Scholar] [CrossRef]
- Zhang, K.; Yue, Y.; Wu, S.; Liu, W.; Shi, J.; Zhang, Z. Rapid Capture and Nondestructive Release of Extracellular Vesicles Using Aptamer-Based Magnetic Isolation. ACS Sens. 2019, 4, 1245–1251. [Google Scholar] [CrossRef]
- Capriglione, F.; Verrienti, A.; Celano, M.; Maggisano, V.; Sponziello, M.; Pecce, V.; Gagliardi, A.; Giacomelli, L.; Aceti, V.; Durante, C.; et al. Analysis of serum microRNA in exosomal vehicles of papillary thyroid cancer. Endocrine 2022, 75, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Liang, M.; Yu, S.; Tang, S.; Bai, L.; Cheng, J.; Gu, Y.; Li, S.; Zheng, X.; Duan, L.; Wang, L.; et al. A Panel of Plasma Exosomal miRNAs as Potential Biomarkers for Differential Diagnosis of Thyroid Nodules. Front. Genet. 2020, 11, 449. [Google Scholar] [CrossRef]
- Wen, Q.; Wang, Y.; Li, X.; Jin, X.; Wang, G. Decreased serum exosomal miR-29a expression and its clinical significance in papillary thyroid carcinoma. J. Clin. Lab. Anal. 2021, 35, e23560. [Google Scholar] [CrossRef]
- Wang, Z.; Lv, J.; Zou, X.; Huang, Z.; Zhang, H.; Liu, Q.; Jiang, L.; Zhou, X.; Zhu, W. A three plasma microRNA signature for papillary thyroid carcinoma diagnosis in Chinese patients. Gene 2019, 693, 37–45. [Google Scholar] [CrossRef]
- Pan, Q.; Zhao, J.; Li, M.; Liu, X.; Xu, Y.; Li, W.; Wu, S.; Su, Z. Exosomal miRNAs are potential diagnostic biomarkers between malignant and benign thyroid nodules based on next-generation sequencing. Carcinogenesis 2020, 41, 18–24. [Google Scholar] [CrossRef]
- Dai, D.; Tan, Y.; Guo, L.; Tang, A.; Zhao, Y. Identification of exosomal miRNA biomarkers for diagnosis of papillary thyroid cancer by small RNA sequencing. Eur. J. Endocrinol. 2020, 182, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Samsonov, R.; Burdakov, V.; Shtam, T.; Radzhabova, Z.; Vasilyev, D.; Tsyrlina, E.; Titov, S.; Ivanov, M.; Berstein, L.; Filatov, M.; et al. Plasma exosomal miR-21 and miR-181a differentiates follicular from papillary thyroid cancer. Tumour Biol. 2016, 37, 12011–12021. [Google Scholar] [CrossRef] [PubMed]
- Boufraqech, M.; Zhang, L.; Jain, M.; Patel, D.; Ellis, R.; Xiong, Y.; He, M.; Nilubol, N.; Merino, M.J.; Kebebew, E. miR-145 suppresses thyroid cancer growth and metastasis and targets AKT3. Endocr. Relat. Cancer 2014, 21, 517–531. [Google Scholar] [CrossRef]
- Chen, W.; Li, G.; Li, Z.; Zhu, J.; Wei, T.; Lei, J. Evaluation of plasma exosomal miRNAs as potential diagnostic biomarkers of lymph node metastasis in papillary thyroid carcinoma. Endocrine 2022, 75, 846–855. [Google Scholar] [CrossRef]
- Jiang, K.; Li, G.; Chen, W.; Song, L.; Wei, T.; Li, Z.; Gong, R.; Lei, J.; Shi, H.; Zhu, J. Plasma Exosomal miR-146b-5p and miR-222-3p are Potential Biomarkers for Lymph Node Metastasis in Papillary Thyroid Carcinomas. Onco Targets Ther. 2020, 13, 1311–1319. [Google Scholar] [CrossRef] [PubMed]
- Hardin, H.; Helein, H.; Meyer, K.; Robertson, S.; Zhang, R.; Zhong, W.; Lloyd, R.V. Thyroid cancer stem-like cell exosomes: Regulation of EMT via transfer of lncRNAs. Lab. Investig. 2018, 98, 1133–1142. [Google Scholar] [CrossRef]
- Dai, W.; Jin, X.; Han, L.; Huang, H.; Ji, Z.; Xu, X.; Tang, M.; Jiang, B.; Chen, W. Exosomal lncRNA DOCK9-AS2 derived from cancer stem cell-like cells activated Wnt/β-catenin pathway to aggravate stemness, proliferation, migration, and invasion in papillary thyroid carcinoma. Cell Death Dis. 2020, 11, 743. [Google Scholar] [CrossRef]
- Wen, D.; Liu, W.L.; Lu, Z.W.; Cao, Y.M.; Ji, Q.H.; Wei, W.J. SNHG9, a Papillary Thyroid Cancer Cell Exosome-Enriched lncRNA, Inhibits Cell Autophagy and Promotes Cell Apoptosis of Normal Thyroid Epithelial Cell Nthy-ori-3 through YBOX3/P21 Pathway. Front. Oncol. 2021, 11, 647034. [Google Scholar] [CrossRef]
- Yang, C.J.; Wei, Y.C.; Yu, L.T.; Xiao, Y. Identification of Altered Circular RNA Expression in Serum Exosomes from Patients with Papillary Thyroid Carcinoma by High-Throughput Sequencing. Med. Sci. Monitor. 2019, 25, 2785–2791. [Google Scholar] [CrossRef]
- Lin, Q.; Qi, Q.; Hou, S.; Chen, Z.; Jiang, N.; Zhang, L.; Lin, C. Exosomal circular RNA hsa_circ_007293 promotes proliferation, migration, invasion, and epithelial-mesenchymal transition of papillary thyroid carcinoma cells through regulation of the microRNA-653-5p/paired box 6 axis. Bioengineered 2021, 12, 10136–10149. [Google Scholar] [CrossRef]
- Wu, G.; Zhou, W.; Lin, X.; Sun, Y.; Li, J.; Xu, H.; Shi, P.; Gao, L.; Tian, X. circRASSF2 Acts as ceRNA and Promotes Papillary Thyroid Carcinoma Progression through miR-1178/TLR4 Signaling Pathway. Mol. Ther.-Nucleic Acids 2020, 19, 1153–1163. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Liu, W.; Wang, Z.; Wang, C.; Ai, Z. Exosomal ANXA1 derived from thyroid cancer cells is associated with malignant transformation of human thyroid follicular epithelial cells by promoting cell proliferation. Int. J. Oncol. 2021, 59, 104. [Google Scholar] [CrossRef]
- Luo, D.; Zhan, S.H.; Xia, W.C.; Huang, L.; Ge, W.; Wang, T.X. Proteomics study of serum exosomes from papillary thyroid cancer patients. Endocr-Relat. Cancer 2018, 25, 879–891. [Google Scholar] [CrossRef]
- Caruso Bavisotto, C.; Cipolla, C.; Graceffa, G.; Barone, R.; Bucchieri, F.; Bulone, D.; Cabibi, D.; Campanella, C.; Marino Gammazza, A.; Pitruzzella, A.; et al. Immunomorphological Pattern of Molecular Chaperones in Normal and Pathological Thyroid Tissues and Circulating Exosomes: Potential Use in Clinics. Int. J. Mol. Sci. 2019, 20, 4496. [Google Scholar] [CrossRef] [PubMed]
- Rabinovich, G.A. Galectin-1 as a potential cancer target. Br. J. Cancer 2005, 92, 1188–1192. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.-W.; Chang, H.-T.; Chen, C.-H.; Chen, C.-H.; Lin, S.-W.; Hsu, T.-L.; Wong, C.-H. Galectin-3 Binding Protein and Galectin-1 Interaction in Breast Cancer Cell Aggregation and Metastasis. J. Am. Chem. Soc. 2015, 137, 9685–9693. [Google Scholar] [CrossRef]
- Tang, W.; Huang, C.; Tang, C.; Xu, J.; Wang, H. Galectin-3 may serve as a potential marker for diagnosis and prognosis in papillary thyroid carcinoma: A meta-analysis. OncoTargets Ther. 2016, 9, 455–460. [Google Scholar] [CrossRef]
- Lee, J.C.; Zhao, J.T.; Gundara, J.; Serpell, J.; Bach, L.A.; Sidhu, S. Papillary thyroid cancer-derived exosomes contain miRNA-146b and miRNA-222. J. Surg. Res. 2015, 196, 39–48. [Google Scholar] [CrossRef]
- Huang, T.Y.; Wang, C.Y.; Chen, K.Y.; Huang, L.T. Urinary Exosomal Thyroglobulin in Thyroid Cancer Patients With Post-ablative Therapy: A New Biomarker in Thyroid Cancer. Front. Endocrinol. 2020, 11, 382. [Google Scholar] [CrossRef]
- Li, G.; He, L.; Huang, J.; Liu, J.; Chen, W.; Zhong, J.; Wei, T.; Li, Z.; Zhu, J.; Lei, J. miR-142-3p encapsulated in T lymphocyte-derived tissue small extracellular vesicles induces Treg function defect and thyrocyte destruction in Hashimoto’s thyroiditis. BMC Med. 2023, 21, 206. [Google Scholar] [CrossRef]
- Sadeghi, S.; Tehrani, F.R.; Tahmasebi, S.; Shafiee, A.; Hashemi, S.M. Exosome engineering in cell therapy and drug delivery. Inflammopharmacology 2023, 31, 145–169. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.S.; Haney, M.J.; Zhao, Y.; Mahajan, V.; Deygen, I.; Klyachko, N.L.; Inskoe, E.; Piroyan, A.; Sokolsky, M.; Okolie, O.; et al. Development of exosome-encapsulated paclitaxel to overcome MDR in cancer cells. Nanomedicine 2016, 12, 655–664. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Wang, S.; Sun, M.; Cui, Y.; Xing, J.; Teng, L.; Xi, Z.; Yang, Z. Exosomes as smart drug delivery vehicles for cancer immunotherapy. Front. Immunol. 2022, 13, 1093607. [Google Scholar] [CrossRef] [PubMed]
- Gangadaran, P.; Li, X.J.; Kalimuthu, S.K.; Min, O.J.; Hong, C.M.; Rajendran, R.L.; Lee, H.W.; Zhu, L.; Baek, S.H.; Jeong, S.Y.; et al. New Optical Imaging Reporter-labeled Anaplastic Thyroid Cancer-Derived Extracellular Vesicles as a Platform for In Vivo Tumor Targeting in a Mouse Model. Sci. Rep. 2018, 8, 13509. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.H.; Ye, Y.; Zhang, M.; Zhou, B.R.; Wang, J.N.; Song, Y.N.; Xia, W. Exosome-mediated delivery of SCD-1 siRNA promoted the death of anaplastic thyroid carcinoma cells via regulating ROS level. Clin. Transl. Oncol. 2021, 24, 288–296. [Google Scholar] [CrossRef]
- Tang, F.; Barbacioru, C.; Wang, Y.; Nordman, E.; Lee, C.; Xu, N.; Wang, X.; Bodeau, J.; Tuch, B.B.; Siddiqui, A.; et al. mRNA-Seq whole-transcriptome analysis of a single cell. Nat. Methods 2009, 6, 377–382. [Google Scholar] [CrossRef]
- Albert, T.K.; Interlandi, M.; Sill, M.; Graf, M.; Moreno, N.; Menck, K.; Rohlmann, A.; Melcher, V.; Korbanka, S.; zu Hörste, G.M.; et al. An extracellular vesicle-related gene expression signature identifies high-risk patients in medulloblastoma. Neuro Oncol. 2021, 23, 586–598. [Google Scholar] [CrossRef]
- Zhang, M.; Yang, H.; Wan, L.; Wang, Z.; Wang, H.; Ge, C.; Liu, Y.; Hao, Y.; Zhang, D.; Shi, G.; et al. Single-cell transcriptomic architecture and intercellular crosstalk of human intrahepatic cholangiocarcinoma. J. Hepatol. 2020, 73, 1118–1130. [Google Scholar] [CrossRef]
- Gao, Y.; Li, X.; Zeng, C.; Liu, C.; Hao, Q.; Li, W.; Zhang, K.; Zhang, W.; Wang, S.; Zhao, H.; et al. CD63+ Cancer-Associated Fibroblasts Confer Tamoxifen Resistance to Breast Cancer Cells through Exosomal miR-22. Adv. Sci. 2020, 7, 2002518. [Google Scholar] [CrossRef]
- Geeurickx, E.; Hendrix, A. Targets, pitfalls and reference materials for liquid biopsy tests in cancer diagnostics. Mol. Asp. Med. 2020, 72, 100828. [Google Scholar] [CrossRef]
- Li, S.; Ren, C.; Gong, Y.; Ye, F.; Tang, Y.; Xu, J.; Guo, C.; Huang, J. The Role of Thyroglobulin in Preoperative and Postoperative Evaluation of Patients With Differentiated Thyroid Cancer. Front. Endocrinol. 2022, 13, 872527. [Google Scholar] [CrossRef] [PubMed]
- Wijewardene, A.A.; Chehade, M.; Gild, M.L.; Clifton-Bligh, R.J.; Bullock, M. Translational Utility of Liquid Biopsies in Thyroid Cancer Management. Cancers 2021, 13, 3443. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.; Li, Y.; Wang, M.; Gu, J.; Xu, W.; Cai, H.; Fang, X.; Zhang, X. Exosomes as a new frontier of cancer liquid biopsy. Mol. Cancer 2022, 21, 56. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.; Li, X.; Xie, K.P. Coupled liquid biopsy and bioinformatics for pancreatic cancer early detection and precision prognostication. Mol. Cancer 2021, 20, 34. [Google Scholar] [CrossRef]
- Costante, G.; Meringolo, D. Calcitonin as a biomarker of C cell disease: Recent achievements and current challenges. Endocrine 2020, 67, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Peng, R.; Zhang, R.; Horan, M.P.; Zhou, L.; Chai, S.Y.; Pillay, N.; Tay, K.H.; Badrick, T.; Li, J. From Somatic Variants Toward Precision Oncology: An Investigation of Reporting Practice for Next-Generation Sequencing-Based Circulating Tumor DNA Analysis. Oncol. 2020, 25, 218–228. [Google Scholar] [CrossRef]
- Li, W.; Liu, J.B.; Hou, L.K.; Yu, F.; Zhang, J.; Wu, W.; Tang, X.-M.; Sun, F.; Lu, H.-M.; Deng, J.; et al. Liquid biopsy in lung cancer: Significance in diagnostics, prediction, and treatment monitoring. Mol. Cancer 2022, 21, 25. [Google Scholar] [CrossRef]
- Freitas, A.J.A.; Causin, R.L.; Varuzza, M.B.; Calfa, S.; Hidalgo Filho, C.M.T.; Komoto, T.T.; Souza, C.d.P.; Marques, M.M.C. Liquid Biopsy as a Tool for the Diagnosis, Treatment, and Monitoring of Breast Cancer. Int. J. Mol. Sci. 2022, 23, 9952. [Google Scholar] [CrossRef]
- Min, L.; Zhu, S.; Chen, L.; Liu, X.; Wei, R.; Zhao, L.; Yang, Y.; Zhang, Z.; Kong, G.; Li, P.; et al. Evaluation of circulating small extracellular vesicles derived miRNAs as biomarkers of early colon cancer: A comparison with plasma total miRNAs. J. Extracell. Vesicles 2019, 8, 1643670. [Google Scholar] [CrossRef]
| LB Component | Technique | Advantages | Disadvantages |
|---|---|---|---|
| CTCs | Physical-based enrichment |
|
|
| Immunomagnetic-based enrichment |
|
| |
| ctDNA | qPCR |
|
|
| ddPCR |
|
| |
| Sanger sequencing |
|
| |
| NGS |
|
| |
| exosomes | Differential ultracentrifugation |
|
|
| Size-based isolation |
|
| |
| Immunomagnetic separation |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, W.; Zheng, Z.; Lei, J. CTC, ctDNA, and Exosome in Thyroid Cancers: A Review. Int. J. Mol. Sci. 2023, 24, 13767. https://doi.org/10.3390/ijms241813767
Wang W, Zheng Z, Lei J. CTC, ctDNA, and Exosome in Thyroid Cancers: A Review. International Journal of Molecular Sciences. 2023; 24(18):13767. https://doi.org/10.3390/ijms241813767
Chicago/Turabian StyleWang, Wenwen, Zhiyao Zheng, and Jianyong Lei. 2023. "CTC, ctDNA, and Exosome in Thyroid Cancers: A Review" International Journal of Molecular Sciences 24, no. 18: 13767. https://doi.org/10.3390/ijms241813767
APA StyleWang, W., Zheng, Z., & Lei, J. (2023). CTC, ctDNA, and Exosome in Thyroid Cancers: A Review. International Journal of Molecular Sciences, 24(18), 13767. https://doi.org/10.3390/ijms241813767





