Prognostic and Clinicopathological Significance of Epidermal Growth Factor Receptor (EGFR) Expression in Oral Squamous Cell Carcinoma: Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Results
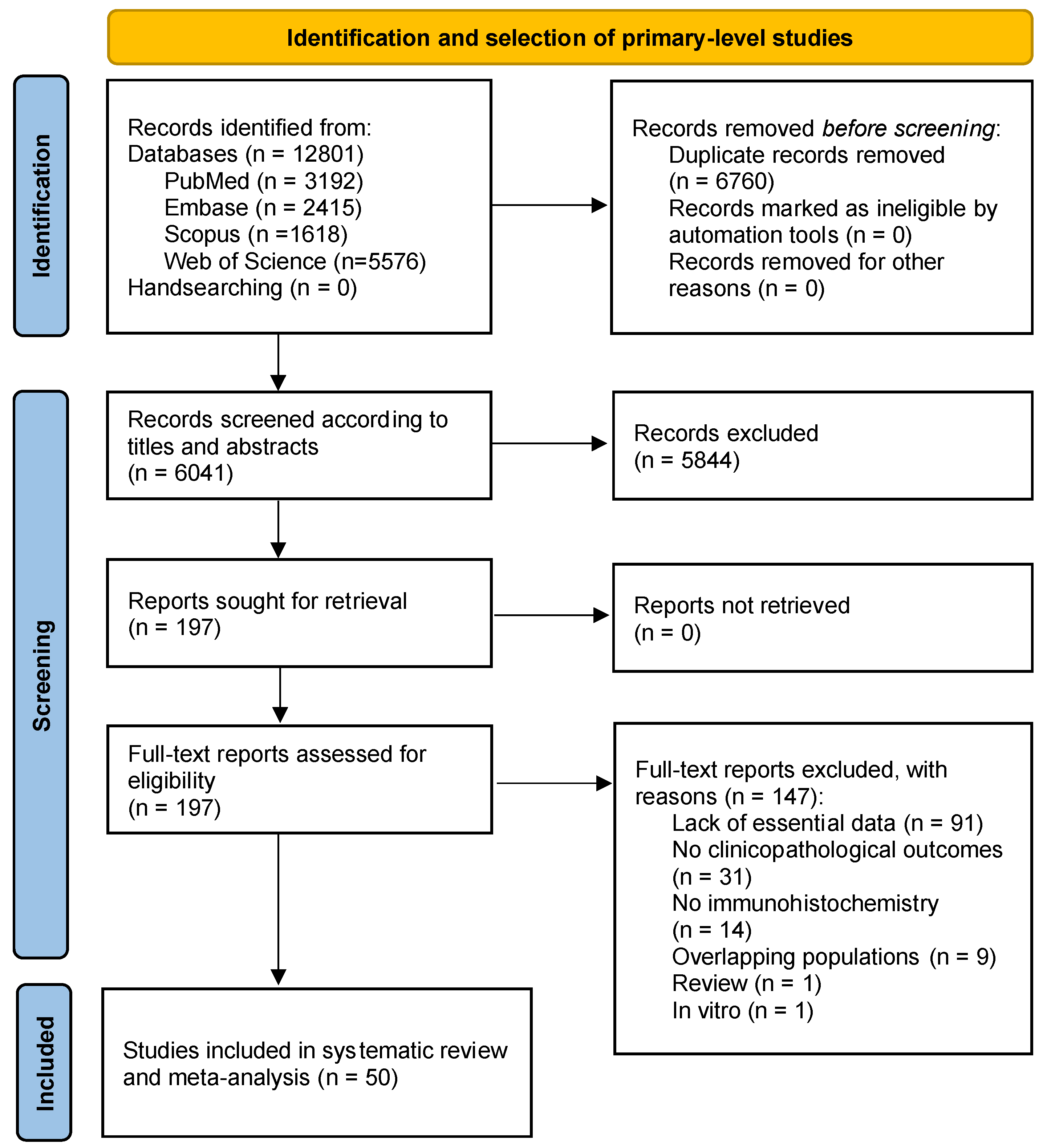
2.1. Results of the Literature Search
2.2. Study Characteristics
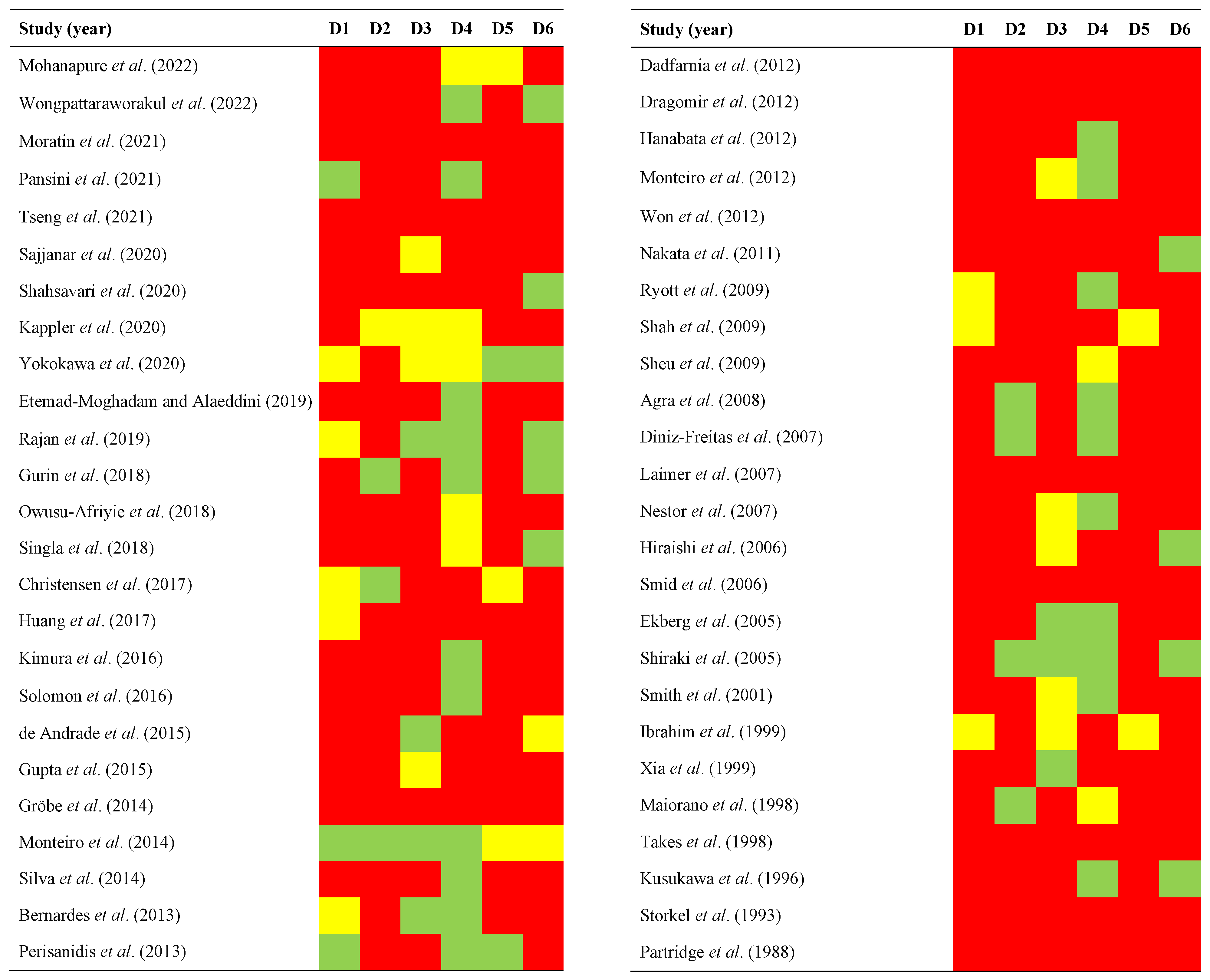
2.3. Qualitative Evaluation
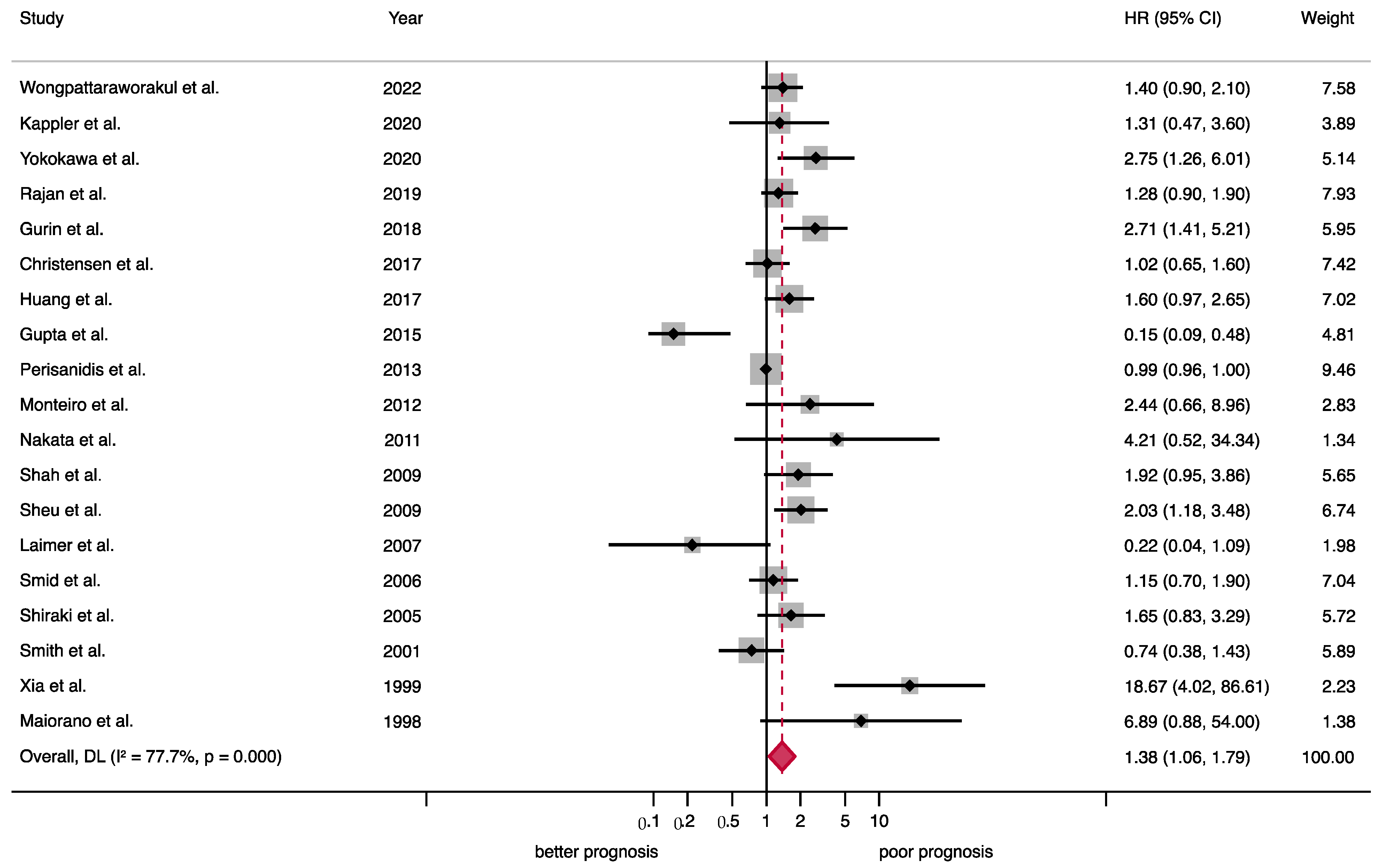
2.4. Quantitative Evaluation (Meta-Analysis)
2.4.1. Association between EGFR Overexpression and Prognostic Variables
2.4.2. Association between EGFR Overexpression and Clinicopathological Variables
2.5. Quantitative Evaluation (Secondary Analyses)
3. Discussion
4. Materials and Methods
4.1. Protocol
4.2. Search Strategy
4.3. Eligibility Criteria
4.4. Study Selection Process
4.5. Data Extraction
4.6. Evaluation of Quality and Risk of Bias
4.7. Effect Measures
4.8. Synthesis Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. The Hallmarks of Cancer. Cell 2000, 100, 57–70. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- González-Moles, M.Á.; Warnakulasuriya, S.; López-Ansio, M.; Ramos-García, P. Hallmarks of Cancer Applied to Oral and Oropharyngeal Carcinogenesis: A Scoping Review of the Evidence Gaps Found in Published Systematic Reviews. Cancers 2022, 14, 3834. [Google Scholar] [CrossRef]
- Leemans, C.R.; Braakhuis, B.J.M.; Brakenhoff, R.H. The molecular biology of head and neck cancer. Nat. Rev. Cancer 2011, 11, 9–22. [Google Scholar] [CrossRef]
- Yarden, Y.; Sliwkowski, M.X. Untangling THE ErbB signalling network. Nat. Rev. Mol Cell Biol. 2001, 2, 127–137. [Google Scholar] [CrossRef]
- Schlessinger, J. Cell signaling by receptor tyrosine kinases. Cell 2000, 103, 211–225. [Google Scholar] [CrossRef]
- Roepstorff, K.; Grandal, M.V.; Henriksen, L.; Knudsen, S.L.J.; Lerdrup, M.; Grøvdal, L.; Willumsen, B.M.; van Deurs, B. Differential effects of EGFR ligands on endocytic sorting of the receptor. Traffic 2009, 10, 1115–1127. [Google Scholar] [CrossRef]
- Wee, P.; Wang, Z. Epidermal Growth Factor Receptor Cell Proliferation Signaling Pathways. Cancers 2017, 9, 52. [Google Scholar] [CrossRef]
- Ramos-García, P.; González-Moles, M.Á.; González-Ruiz, L.; Ruiz-Ávila, I.; Ayén, Á.; Gil-Montoya, J.A. Prognostic and clinicopathological significance of cyclin D1 expression in oral squamous cell carcinoma: A systematic review and meta-analysis. Oral Oncol. 2018, 83, 96–106. [Google Scholar] [CrossRef]
- Ramos-García, P.; Gil-Montoya, A.J.; Scully, C.; Ayén, A.; González-Ruiz, L.; Navarro-Triviño, F.J.; González-Moles, A.M. An update on the implications of cyclin D1 in oral carcinogenesis. Oral Dis. 2017, 23, 897–912. [Google Scholar] [CrossRef] [PubMed]
- Humphreys, R.C.; Hennighausen, L. Transforming growth factor alpha and mouse models of human breast cancer. Oncogene 2000, 19, 1085–1091. [Google Scholar] [CrossRef]
- Kawamata, H.; Kameyama, S.; Oyasu, R. In vitro and in vivo accelertration of the neoplastic phenotype of a low-tumorigenicity rat bladder carcinoma cell line by transfected transforming growth factor-α. Mol. Carcinog. 1994, 9, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Hirai, T.; Kuwahara, M.; Yoshida, K.; Kagawa, Y.; Hihara, J.; Yamashita, Y.; Toge, T. Clinical results of transhiatal esophagectomy for carcinoma of the lower thoracic esophagus according to biological markers. Dis. Esophagus 1998, 11, 221–225. [Google Scholar] [CrossRef]
- Maurizi, M.; Almadori, G.; Ferrandina, M.G.; Distefano, M.; Romanini, M.E.; Cadoni, G.; Benedetti-Panici, P.; Paludetti, G.; Scambia, G.; Mancuso, S. Prognostic significance of epidermal growth factor receptor in laryngeal squamous cell carcinoma. Br. J. Cancer 1996, 74, 1253–1257. [Google Scholar] [CrossRef]
- Nicholson, R.; Gee, J.M.; Harper, M. EGFR and cancer prognosis. Eur. J. Cancer 2001, 37, 9–15. [Google Scholar] [CrossRef]
- Chong, C.R.; Jänne, P.A. The quest to overcome resistance to EGFR-targeted therapies in cancer. Nat. Med. 2013, 19, 1389–1400. [Google Scholar] [CrossRef] [PubMed]
- Mohanapure, N.; Sinai Khandeparkar, S.; Saragade, P.; Gogate, B.; Joshi, A.; Mehta, S. Immunohistochemical study of epidermal growth factor receptor, human epidermal growth factor receptor 2/neu, p53, and Ki67 in oral squamous cell carcinoma. J. Oral Maxillofac. Pathol. 2022, 26, 127. [Google Scholar] [CrossRef]
- Wongpattaraworakul, W.; Gibson-Corley, K.N.; Choi, A.; Buchakjian, M.R.; Lanzel, E.A.; Kd, A.R.; Simons, A.L. Prognostic Role of Combined EGFR and Tumor-Infiltrating Lymphocytes in Oral Squamous Cell Carcinoma. Front Oncol. 2022, 12, 885236. [Google Scholar] [CrossRef]
- Etemad-Moghadam, S.; Alaeddini, M. Upregulation of ADAM10 in oral squamous cell carcinoma and its correlation with EGFR, neoangiogenesis and clinicopathologic factors. J. Cranio-Maxillofac. Surg. 2019, 47, 1583–1588. [Google Scholar] [CrossRef]
- Singla, S.; Singla, G.; Zaheer, S.; Rawat, D.; Mandal, A. Expression of p53, epidermal growth factor receptor, c-erbB2 in oral leukoplakias and oral squamous cell carcinomas. J. Cancer Res. Ther. 2018, 14, 388. [Google Scholar] [CrossRef]
- Owusu-Afriyie, O.; Owiredu, W.K.B.A.; Owusu-Danquah, K.; Larsen-Reindorf, R.; Donkor, P.; Acheampong, E.; Quayson, S.E. Expression of immunohistochemical markers in non-oropharyngeal head and neck squamous cell carcinoma in Ghana. PLoS ONE 2018, 13, e0202790. [Google Scholar] [CrossRef]
- Gurin, D.; Slavik, M.; Hermanova, M.; Shatokhina, T.; Sana, J.; Kazda, T.; Selingerova, I.; Ahmad, P.; Smilek, P.; Horakova, Z.; et al. Prognostic impact of combined immunoprofiles in oropharyngeal squamous cell carcinoma patients with respect to AJCC 8th edition. J. Oral Pathol. Med. 2018, 47, 864–872. [Google Scholar] [CrossRef]
- Huang, S.-F.; Chien, H.-T.; Chuang, W.-Y.; Lai, C.-H.; Cheng, S.-D.; Liao, C.-T.; Wang, H.-M. Epidermal growth factor receptor intron-1 CA repeat polymorphism on protein expression and clinical outcome in Taiwanese oral squamous cell carcinoma. Sci. Rep. 2017, 7, 4963. [Google Scholar] [CrossRef]
- Christensen, A.; Kiss, K.; Lelkaitis, G.; Juhl, K.; Persson, M.; Charabi, B.W.; Mortensen, J.; Forman, J.L.; Sørensen, A.L.; Jensen, D.H.; et al. Urokinase-type plasminogen activator receptor (uPAR), tissue factor (TF) and epidermal growth factor receptor (EGFR): Tumor expression patterns and prognostic value in oral cancer. BMC Cancer 2017, 17, 572. [Google Scholar] [CrossRef]
- Kimura, I.; Kitahara, H.; Ooi, K.; Kato, K.; Noguchi, N.; Yoshizawa, K.; Nakamura, H.; Kawashiri, S. Loss of epidermal growth factor receptor expression in oral squamous cell carcinoma is associated with invasiveness and epithelial-mesenchymal transition. Oncol. Lett. 2016, 11, 201–207. [Google Scholar] [CrossRef]
- Solomon, M.C.; Vidyasagar, M.S.; Fernandes, D.; Guddattu, V.; Mathew, M.; Shergill, A.K.; Carnelio, S.; Chandrashekar, C. The prognostic implication of the expression of EGFR, p53, cyclin D1, Bcl-2 and p16 in primary locally advanced oral squamous cell carcinoma cases: A tissue microarray study. Med. Oncol. 2016, 33, 138. [Google Scholar] [CrossRef]
- Gupta, S.; Khan, H.; Kushwaha, V.S.; Husain, N.; Negi, M.; Ghatak, A.; Bhatt, M. Impact of EGFR and p53 expressions on survival and quality of life in locally advanced oral squamous cell carcinoma patients treated with chemoradiation. Cancer Biol. Ther. 2015, 16, 1269–1280. [Google Scholar] [CrossRef][Green Version]
- de Andrade, A.L.D.L.; Ferreira, S.J.; Ferreira, S.M.S.; Ribeiro, C.M.B.; Freitas, R.D.A.; Galvão, H.C. Immunoexpression of EGFR and EMMPRIN in a series of cases of head and neck squamous cell carcinoma. Pathol. Res. Pract. 2015, 211, 776–781. [Google Scholar] [CrossRef]
- Pansini, P.F.; Valle, I.B.D.; Damasceno, T.C.D.; de Abreu, P.M.; Có, A.C.G.; López, R.V.M.; Lenzi, J.; Rocha, R.M.; Souza, E.D.; Curado, M.P.; et al. Differential Expression of Potential Biomarkers of Oral Squamous Cell Carcinoma Development. Head Neck Pathol. 2021, 15, 1127–1136. [Google Scholar] [CrossRef]
- Gröbe, A.; Eichhorn, W.; Fraederich, M.; Kluwe, L.; Vashist, Y.; Wikner, J.; Smeets, R.; Simon, R.; Sauter, G.; Heiland, M.; et al. Immunohistochemical and FISH analysis of EGFR and its prognostic value in patients with oral squamous cell carcinoma. J. Oral Pathol. Med. 2014, 43, 205–210. [Google Scholar] [CrossRef]
- Silva, S.D.; Alaoui-Jamali, M.A.; Hier, M.; Soares, F.A.; Graner, E.; Kowalski, L.P. Cooverexpression of ERBB1 and ERBB4 receptors predicts poor clinical outcome in pN+ oral squamous cell carcinoma with extranodal spread. Clin. Exp. Metastasis 2014, 31, 307–316. [Google Scholar] [CrossRef]
- Monteiro, L.S.; Ricardo, S.; Delgado, M.L.; Garcez, F.; do Amaral, B.; Lopes, C. Phosphorylated EGFR at tyrosine 1173 correlates with poor prognosis in oral squamous cell carcinomas. Oral Dis. 2014, 20, 178–185. [Google Scholar] [CrossRef]
- Perisanidis, C.; Wrba, F.; Brandstetter, A.; Kornek, G.; Mitchell, D.; Seemann, R.; Selzer, E.; Ewers, R.; Filipits, M. Impact of epidermal growth factor receptor, mesenchymal–epithelial transition factor, and insulin-like growth factor receptor 1 expression on survival of patients with oral and oropharyngeal cancer. Br. J. Oral Maxillofac. Surg. 2013, 51, 234–240. [Google Scholar] [CrossRef]
- Bernardes, V.F.; Gleber-Netto, F.O.; de Sousa, S.F.; Rocha, R.M.; de Aguiar, M.C.F. EGFR status in oral squamous cell carcinoma: Comparing immunohistochemistry, FISH and CISH detection in a case series study. BMJ Open 2013, 3, e002077. [Google Scholar] [CrossRef]
- Dragomir, L.P.; Mărgăritescu, C.; Florescu, A.; Olimid, A.D.; Dragomir, M.; Popescu, M.R. The immunoexpression of EGFR and Her2/neu in oral squamous carcinoma. Rom. J. Morphol. Embryol. 2012, 53, 597–601. [Google Scholar]
- Won, H.S.; Jung, C.-K.; Chun, S.H.; Kang, J.-H.; Kim, Y.-S.; Sun, D.-I.; Kim, M.-S. Difference in expression of EGFR, pAkt, and PTEN between oropharyngeal and oral cavity squamous cell carcinoma. Oral Oncol. 2012, 48, 985–990. [Google Scholar] [CrossRef]
- Hanabata, Y.; Nakajima, Y.; Morita, K.; Kayamori, K.; Omura, K. Coexpression of SGLT1 and EGFR is associated with tumor differentiation in oral squamous cell carcinoma. Odontology 2012, 100, 156–163. [Google Scholar] [CrossRef]
- Dadfarnia, T.; Mohammed, B.S.; Eltorky, M.A. Significance of Ki-67 and p53 immunoexpression in the differential diagnosis of oral necrotizing sialometaplasia and squamous cell carcinoma. Ann. Diagn. Pathol. 2012, 16, 171–176. [Google Scholar] [CrossRef]
- Monteiro, L.S.; Diniz-Freitas, M.; Garcia-Caballero, T.; Warnakulasuriya, S.; Forteza, J.; Fraga, M. Combined cytoplasmic and membranous EGFR and p53 overexpression is a poor prognostic marker in early stage oral squamous cell carcinoma. J. Oral. Pathol. Med. 2012, 41, 559–567. [Google Scholar] [CrossRef]
- Tseng, Y.-K.; Chen, C.-F.; Shu, C.-W.; Lee, C.-H.; Chou, Y.-T.; Li, Y.-J.; Liou, H.-H.; Cheng, J.-T.; Chen, C.-L.; Ger, L.-P.; et al. Effect of EGFR on SQSTM1 Expression in Malignancy and Tumor Progression of Oral Squamous Cell Carcinoma. Int. J. Mol. Sci. 2021, 22, 12226. [Google Scholar] [CrossRef]
- Nakata, Y.; Uzawa, N.; Takahashi, K.-I.; Sumino, J.; Michikawa, C.; Sato, H.; Sonoda, I.; Ohyama, Y.; Okada, N.; Amagasa, T. EGFR gene copy number alteration is a better prognostic indicator than protein overexpression in oral tongue squamous cell carcinomas. Eur. J. Cancer 2011, 47, 2364–2372. [Google Scholar] [CrossRef]
- Shah, N.G.; Trivedi, T.I.; Tankshali, R.A.; Goswami, J.V.; Jetly, D.H.; Shukla, S.N.; Shah, P.M.; Verma, R.J. Prognostic significance of molecular markers in oral squamous cell carcinoma: A multivariate analysis. Head Neck 2009, 31, 1544–1556. [Google Scholar] [CrossRef]
- Ryott, M.; Wangsa, D.; Heselmeyer-Haddad, K.; Lindholm, J.; Elmberger, G.; Auer, G.; Lundqvist, E.; Ried, T.; Munck-Wikland, E. EGFR protein overexpression and gene copy number increases in oral tongue squamous cell carcinoma. Eur. J. Cancer 2009, 45, 1700–1708. [Google Scholar] [CrossRef]
- Sheu, J.J.-C.; Hua, C.-H.; Wan, L.; Lin, Y.-J.; Lai, M.-T.; Tseng, H.-C.; Jinawath, N.; Tsai, M.-H.; Chang, N.-W.; Lin, C.-F.; et al. Functional genomic analysis identified epidermal growth factor receptor activation as the most common genetic event in oral squamous cell carcinoma. Cancer Res. 2009, 69, 2568–2576. [Google Scholar] [CrossRef]
- Agra, I.M.G.; Carvalho, A.L.; Pinto CA, L.; Martins, E.P.; Gonçalves Filho, J.; Soares, F.A.; Kowalski, L.P. Biological Markers and Prognosis in Recurrent Oral Cancer After Salvage Surgery. Arch. Otolaryngol. Neck Surg. 2008, 134, 743. [Google Scholar] [CrossRef]
- Nestor, M.; Ekberg, T.; Dring, J.; van Dongen, G.A.; Wester, K.; Tolmachev, V.; Anniko, M. Quantification of CD44v6 and EGFR Expression in Head and Neck Squamous Cell Carcinomas Using a Single-Dose Radioimmunoassay. Tumor Biol. 2007, 28, 253–263. [Google Scholar] [CrossRef]
- Laimer, K.; Spizzo, G.; Gastl, G.; Obrist, P.; Brunhuber, T.; Fong, D.; Barbieri, V.; Jank, S.; Doppler, W.; Rasse, M.; et al. High EGFR expression predicts poor prognosis in patients with squamous cell carcinoma of the oral cavity and oropharynx: A TMA-based immunohistochemical analysis. Oral Oncol. 2007, 43, 193–198. [Google Scholar] [CrossRef]
- Diniz-Freitas, M.; García-Caballero, T.; Antúnez-López, J.; Gándara-Rey, J.M.; García-García, A. Pharmacodiagnostic evaluation of EGFR expression in oral squamous cell carcinoma. Oral Dis. 2007, 13, 285–290. [Google Scholar] [CrossRef]
- Hiraishi, Y.; Wada, T.; Nakatani, K.; Negoro, K.; Fujita, S. Immunohistochemical expression of EGFR and p-EGFR in oral squamous cell carcinomas. Pathol. Oncol. Res. 2006, 12, 87–91. [Google Scholar] [CrossRef]
- Smid, E.J.; Stoter, T.R.; Bloemena, E.; Lafleur, M.V.M.; Leemans, C.R.; van der Waal, I.; Slotman, B.J.; Langendijk, J.A. The importance of immunohistochemical expression of EGFr in squamous cell carcinoma of the oral cavity treated with surgery and postoperative radiotherapy. Int. J. Radiat. Oncol. 2006, 65, 1323–1329. [Google Scholar] [CrossRef] [PubMed]
- Moratin, J.; Mock, A.; Obradovic, S.; Metzger, K.; Flechtenmacher, C.; Zaoui, K.; Fröhling, S.; Jäger, D.; Krauss, J.; Hoffmann, J.; et al. Digital Pathology Scoring of Immunohistochemical Staining Reliably Identifies Prognostic Markers and Anatomical Associations in a Large Cohort of Oral Cancers. Front Oncol. 2021, 11, 712944. [Google Scholar] [CrossRef] [PubMed]
- Shiraki, M.; Odajima, T.; Ikeda, T.; Sasaki, A.; Satoh, M.; Yamaguchi, A.; Noguchi, M.; Nagai, I.; Hiratsuka, H. Combined expression of p53, cyclin D1 and epidermal growth factor receptor improves estimation of prognosis in curatively resected oral cancer. Mod. Pathol. 2005, 18, 1482–1489. [Google Scholar] [CrossRef] [PubMed]
- Ekberg, T.; Nestor, M.; Engström, M.; Nordgren, H.; Wester, K.; Carlsson, J.; Anniko, M. Expression of EGFR, HER2, HER3, and HER4 in metastatic squamous cell carcinomas of the oral cavity and base of tongue. Int. J. Oncol. 2005, 26, 1177–1185. [Google Scholar] [CrossRef]
- Smith, B.D.; Smith, G.L.; Carter, D.; DiGiovanna, M.P.; Kasowitz, K.M.; Sasaki, C.T.; Haffty, B.G. Molecular marker expression in oral and oropharyngeal squamous cell carcinoma. Arch. Otolaryngol. Head Neck Surg. 2001, 127, 780–785. [Google Scholar]
- Xia, W.; Lau, Y.K.; Zhang, H.Z.; Xiao, F.Y.; Johnston, A.D.; Liu, A.R.; Li, L.; Katz, R.L.; Hung, M.C. Combination of EGFR, HER-2/neu, and HER-3 is a stronger predictor for the outcome of oral squamous cell carcinoma than any individual family members. Clin. Cancer Res. 1999, 5, 4164–4174. [Google Scholar] [PubMed]
- Ibrahim, S.O.; Lillehaug, J.R.; Johannessen, A.C.; Liavaag, P.G.; Nilsen, R.; Vasstrand, E.N. Expression of biomarkers (p53, transforming growth factor alpha, epidermal growth factor receptor, c-erbB-2/neu and the proliferative cell nuclear antigen) in oropharyngeal squamous cell carcinomas. Oral Oncol. 1999, 35, 302–313. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Takes, R.P.; Baatenburg de Jong, R.J.; Schuuring, E.; Litvinov, S.V.; Hermans, J.; van Krieken, J.H. Differences in expression of oncogenes and tumor suppressor genes in different sites of head and neck squamous cell. Anticancer Res. 1998, 18, 4793–4800. [Google Scholar]
- Maiorano, E.; Favia, G.; Maisonneuve, P.; Viale, G. Prognostic implications of epidermal growth factor receptor immunoreactivity in squamous cell carcinoma of the oral mucosa. J. Pathol. 1998, 185, 167–174. [Google Scholar] [CrossRef]
- Kusukawa, J.; Harada, H.; Shima, I.; Sasaguri, Y.; Kameyama, T.; Morimatsu, M. The significance of epidermal growth factor receptor and matrix metalloproteinase-3 in squamous cell carcinoma of the oral cavity. Eur. J. Cancer B Oral Oncol. 1996, 32B, 217–221. [Google Scholar] [CrossRef]
- Störkel, S.; Reichert, T.; Reiffen, K.A.; Wagner, W. EGFR and PCNA expression in oral squamous cell carcinomas—A valuable tool in estimating the patient’s prognosis. Eur. J. Cancer B Oral Oncol. 1993, 29B, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Partridge, M.; Gullick, W.J.; Langdon, J.D.; Sherriff, M. Expression of epidermal growth factor receptor on oral squamous cell carcinoma. Br. J. Oral Maxillofac. Surg. 1988, 26, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Shahsavari, F.; Miri, R.; Ghorbanpour, M. Expression of epidermal growth factor receptor in oral and esophageal squamous-cell carcinoma. Dent. Res. J. 2020, 17, 85–91. [Google Scholar]
- Sajjanar, M.; Sajjan, P.; Puranik, R.; Vanaki, S.; Jayanth, V.; Naik, P. “Analysis of immunohistochemical expression of epidermal growth factor receptor in oral squamous cell carcinoma using tissue microarray technology and whole sections:” A comparative study. J. Oral Maxillofac. Pathol. 2020, 24, 499. [Google Scholar] [CrossRef]
- Kappler, M.; Dauter, K.; Reich, W.; Bethmann, D.; Schwabe, M.; Rot, S.; Wickenhauser, C.; Al-Nawas, B.; Eckert, A.W. Prognostic impact of cytoplasmatic EGFR upregulation in patients with oral squamous cell carcinoma: A pilot study. Mol. Clin. Oncol. 2020, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Yokokawa, M.; Morita, K.; Oikawa, Y.; Kayamori, K.; Sakamoto, K.; Ikeda, T.; Harada, H. Co-expression of EGFR and MET has a synergistic effect on the prognosis of patients with oral squamous cell carcinoma. J. Oral Pathol. Med. 2020, 49, 235–242. [Google Scholar] [CrossRef]
- Rajan, A.; Gibson-Corley, K.N.; Choi, A.B.; Ofori-Amanfo, G.K.; Eyck, P.T.; Espinosa-Cotton, M.; Sperry, S.M.; Simons, A.L. Impact of Nuclear Interleukin-1 Alpha and EGFR Expression on Recurrence and Survival Outcomes in Oral Squamous Cell Carcinomas. J. Oncol. 2019, 2019, 1–12. [Google Scholar] [CrossRef]
- Hayden, J.A.; Côté, P.; Bombardier, C. Evaluation of the quality of prognosis studies in systematic reviews. Ann. Intern. Med. 2006, 144, 427–437. [Google Scholar]
- Normanno, N.; De Luca, A.; Bianco, C.; Strizzi, L.; Mancino, M.; Maiello, M.R.; Carotenuto, A.; De Feo, G.; Caponigro, F.; Salomon, D.S. Epidermal growth factor receptor (EGFR) signaling in cancer. Gene 2006, 366, 2–16. [Google Scholar] [CrossRef]
- Ramos-García, P.; González-Moles, M.Á.; Ayén, Á.; González-Ruiz, L.; Ruiz-Ávila, I.; Lenouvel, D.; Gil-Montoya, J.A.; Bravo, M. Asymmetrical proliferative pattern loss linked to cyclin D1 overexpression in adjacent non-tumour epithelium in oral squamous cell carcinoma. Arch. Oral Biol. 2019, 97, 12–17. [Google Scholar] [CrossRef]
- Abd El-Rehim, D.M.; Pinder, S.E.; Paish, C.E.; Bell, J.A.; Rampaul, R.S.; Blamey, R.W.; Robertson, J.F.R.; Nicholson, R.I.; Ellis, I.O. Expression and co-expression of the members of the epidermal growth factor receptor (EGFR) family in invasive breast carcinoma. Br. J. Cancer 2004, 91, 1532–1542. [Google Scholar] [CrossRef]
- Meng, Y.; Yang, P.; Ma, L.; Tarantino, G. Prognostic and clinical implications of c-erbB-2 expression in patients with oral cancer: A meta-analysis. Medicine 2020, 99, e20575. [Google Scholar] [CrossRef]
- Ramos-García, P.; Bravo, M.; González-Ruiz, L.; González-Moles, M.Á. Significance of cytoplasmic cyclin D1 expression in oral oncogenesis. Oral Dis. 2018, 24, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Riley, R.D.; Ridley, G.; Williams, K.; Altman, D.G.; Hayden, J.; de Vet, H.C.W. Prognosis research: Toward evidence-based results and a Cochrane methods group. J. Clin. Epidemiol. 2007, 60, 863–865, author reply 865–866. [Google Scholar] [CrossRef]
- Kyzas, P.A.; Denaxa-Kyza, D.; Ioannidis, J.P.A. Almost all articles on cancer prognostic markers report statistically significant results. Eur. J. Cancer 2007, 43, 2559–2579. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. J. Am. Med. Assoc. 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series; Wiley and Sons: Hoboken, NJ, USA, 2008; pp. 1–649. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef]
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat. Methods Med. Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef]
- González-Moles, M.Á.; Ayén, Á.; González-Ruiz, I.; De Porras-Carrique, T.; González-Ruiz, L.; Ruiz-Ávila, I.; Ramos-García, P. Prognostic and Clinicopathological Significance of FADD Upregulation in Head and Neck Squamous Cell Carcinoma: A Systematic Review and Meta-Analysis. Cancers 2020, 12, 2393. [Google Scholar] [CrossRef]
- Ramos-García, P.; González-Moles, M.Á. Prognostic and Clinicopathological Significance of the Aberrant Expression of β-Catenin in Oral Squamous Cell Carcinoma: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 479. [Google Scholar] [CrossRef]
- Ramos-García, P.; González-Moles, M.Á.; Warnakulasuriya, S. Significance of p53 overexpression in the prediction of the malignant transformation risk of oral potentially malignant disorders: A systematic review and meta-analysis. Oral Oncol. 2022, 126, 105734. [Google Scholar] [CrossRef]
- González-Moles, M.Á.; Moya-González, E.; García-Ferrera, A.; Nieto-Casado, P.; Ramos-García, P. Prognostic and Clinicopathological Significance of Telomerase Reverse Transcriptase Upregulation in Oral Cancer: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 3673. [Google Scholar] [CrossRef]
- Tierney, J.F.; Stewart, L.A.; Ghersi, D.; Burdett, S.; Sydes, M.R. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007, 8, 16. [Google Scholar] [CrossRef]
- Parmar, M.K.; Torri, V.; Stewart, L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat. Med. 1998, 17, 2815–2834. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Thompson, S.G.; Higgins, J.P.T. How should meta-regression analyses be undertaken and interpreted? Stat. Med. 2002, 21, 1559–1573. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Controlling the risk of spurious findings from meta-regression. Stat. Med. 2004, 23, 1663–1682. [Google Scholar] [CrossRef]
- Kemp, A.W.; Manly, B.F.J. Randomization, Bootstrap and Monte Carlo Methods in Biology; CRC Press: Boca Raton, FL, USA, 2006; Volume 53. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
| Summarized Characteristics of the Study Sample | |
|---|---|
| Total | 50 studies |
| Year of publication | 1988–2022 |
| Total patients (range) | 4631 (9—429) |
| Study design | |
| Retrospective cohort | 50 studies |
| Experimental methods for EGFR expression determination | |
| Immunohistochemistry | 50 studies |
| Anti-EGFR antibody | |
| Clone 31G7 | 6 studies |
| Clone 2-18C9 | 5 studies |
| Clone H11 | 4 studies |
| D38B1 | 4 studies |
| Clone 25 | 2 studies |
| Clone EP-22 | 2 studies |
| sc-03 | 2 studies |
| Ab-1 | 1 study |
| Ab-4 | 1 study |
| Clone 111.6 | 1 study |
| Clone 29.1 | 1 study |
| Clone 5B7 | 1 study |
| Clone SP9 | 1 study |
| E30 | 1 study |
| HPA018530 | 1 study |
| RPN 513 | 1 study |
| sc-003 | 1 study |
| Not reported | 15 studies |
| Anti-EGFR antibody dilution | |
| >1:100 | 16 studies |
| <1:100 | 16 studies |
| Not reported | 18 studies |
| Anti-EGFR antibody incubation time | |
| Overnight | 12 studies |
| 1 h | 9 studies |
| Other | 6 studies |
| Not reported | 23 studies |
| Anti-EGFR antibody incubation temperature | |
| 4 °C | 11 studies |
| Room temperature | 9 studies |
| Not reported | 30 studies |
| Cut-off point | |
| >10 | 5 studies |
| 10 | 14 studies |
| 0 | 4 studies |
| Intensity-based | 25 studies |
| Not reported | 2 studies |
| Immunostaining pattern | |
| Membrane | 29 studies |
| Membrane-cytoplasm | 12 studies |
| Membrane-cytoplasm-nucleus | 1 study |
| Not reported | 8 studies |
| Geographical region | |
| Asian countries | 20 studies |
| Non-Asian countries | 30 studies |
| Meta-Analyses | No. of Studies | No. of Patients | Stat. Model | Wt | Pooled Data | Heterogeneity | ||
|---|---|---|---|---|---|---|---|---|
| ES (95% CI) | p-Value | Phet | I2 (%) | |||||
| SURVIVAL PARAMETERS | ||||||||
| Overall survival | ||||||||
| EGFR overexpression (all) a | 19 | 2256 | REM | D-L | HR = 1.38 (1.06–1.79) | 0.02 | <0.001 | 77.7 |
| Subgroup analysis by geographical area b | ||||||||
| Asian | 8 | 1053 | REM | D-L | HR = 1.79 (0.89–3.58) | 0.10 | <0.001 | 84.2 |
| Non-Asian | 11 | 1203 | REM | D-L | HR = 1.20 (0.95–1.52) | 0.12 | 0.01 | 57.0 |
| Subgroup analysis by anti-EGFR antibody dilution b | ||||||||
| >100 | 6 | 743 | REM | D-L | HR = 1.56 (1.04–2.33) | 0.03 | <0.001 | 80.2 |
| <100 | 6 | 689 | REM | D-L | HR = 1.59 (1.21–2.11) | 0.001 | 0.60 | 0.0 |
| Not reported | 7 | 824 | REM | D-L | HR = 0.95 (0.44–2.03) | 0.89 | <0.001 | 85.3 |
| Subgroup analysis by anti-EGFR antibody incubation time b | ||||||||
| 1 h | 1 | 208 | — | — | HR = 2.75 (1.26–6.01) | 0.01 | — | 0.0 |
| Overnight | 5 | 616 | REM | D-L | HR = 0.86 (0.40–1.83) | 0.70 | <0.001 | 84.7 |
| Other | 4 | 506 | REM | D-L | HR = 1.96 (0.93–4.10) | 0.08 | 0.004 | 77.9 |
| Not reported | 9 | 926 | REM | D-L | HR = 1.52 (1.04–2.22) | 0.03 | <0.001 | 73.8 |
| Subgroup analysis by anti-EGFR antibody incubation temperatureb | ||||||||
| 4 °C | 4 | 451 | REM | D-L | HR = 0.79 (0.28–2.23) | 0.65 | <0.001 | 88.2 |
| Room temperature | 4 | 523 | REM | D-L | HR = 2.93 (1.16–7.38) | 0.02 | 0.004 | 77.5 |
| Not reported | 11 | 1282 | REM | D-L | HR = 1.38 (1.04–1.82) | 0.02 | 0.001 | 67.6 |
| Subgroup analysis by anti-EGFR antibody b | ||||||||
| Clone 111.6 | 1 | 135 | — | — | HR = 1.92 (0.95–3.86) | 0.07 | — | 0.0 |
| Clone 2-18C9 | 1 | 63 | — | — | HR = 2.44 (0.66–8.96) | 0.18 | — | 0.0 |
| Clone 25 | 1 | 135 | — | — | HR = 1.60 (0.97–2.64) | 0.07 | — | 0.0 |
| Clone 29.1 | 1 | 100 | — | — | HR = 6.89 (0.88–53.97) | 0.07 | — | 0.0 |
| Clone 31G7 | 2 | 204 | REM | D-L | HR = 2.12 (1.26–3.59) | 0.005 | 0.51 | 0.0 |
| Clone 5B7 | 1 | 77 | — | — | HR = 2.71 (1.41–5.21) | 0.003 | — | 0.0 |
| Clone EP-22 | 1 | 120 | — | — | HR = 0.15 (0.06–0.35) | <0.001 | — | 0.0 |
| Clone H11 | 2 | 284 | REM | D-L | HR = 1.33 (1.01–1.76) | 0.05 | 0.76 | 0.0 |
| D38B1 | 2 | 253 | REM | D-L | HR = 2.05 (1.00–4.17) | 0.05 | 0.26 | 22.0 |
| E30 | 1 | 56 | — | — | HR = 0.74 (0.38–1.44) | 0.37 | — | 0.0 |
| sc-003 | 1 | 111 | — | — | HR = 18.67 (4.02–86.66) | <0.001 | — | 0.0 |
| sc-03 | 1 | 140 | — | — | HR = 1.65 (0.83–3.29) | 0.15 | — | 0.0 |
| Not reported | 4 | 578 | REM | D-L | HR = 0.99 (0–85–1.16) | 0.93 | 0.31 | 15.5 |
| Subgroup analysis by cut-off point b | ||||||||
| 10 | 7 | 704 | REM | D-L | HR = 1.62 (1.24–2.11) | <0.001 | 0.32 | 13.8 |
| >10 | 3 | 320 | REM | D-L | HR = 2.15 (0.07–61.90) | 0.66 | <0.001 | 94.0 |
| Intensity-based | 9 | 1232 | REM | D-L | HR = 1.24 (0.95–1.63) | 0.12 | 0.03 | 65.5 |
| Subgroup analysis by immunostaining pattern b | ||||||||
| Membrane | 10 | 1138 | REM | D-L | HR = 1.31 (0.98–1.74) | 0.07 | 0.001 | 67.0 |
| Mixed membrane-cytoplasm | 6 | 669 | REM | D-L | HR = 2.02 (0.61–6.70) | 0.25 | <0.001 | 88.2 |
| Not reported | 3 | 449 | REM | D-L | HR = 1.39 (0.97–2.01) | 0.08 | 0.16 | 45.7 |
| Subgroup analysis by overall risk of bias in primary-level studies b | ||||||||
| Low RoB | 6 | 776 | REM | D-L | HR = 1.83 (1.12–2.98) | 0.02 | <0.001 | 81.0 |
| Moderate RoB | 5 | 547 | REM | D-L | HR = 0.79 (0.37–1.67) | 0.53 | <0.001 | 82.8 |
| High RoB | 8 | 933 | REM | D-L | HR = 1.63 (1.14–2.31) | 0.007 | 0.06 | 48.5 |
| Univariable meta-regressions by study design and patients characteristics c | ||||||||
| Follow up (months, average) | 6 | 1419 | random-effects meta-regression | Coef = 0.000 (−0.032 to 0.032) | 0.96 ±0.002 d | hetexplained = −64.29% e | ||
| Sex (proportion of males, %) | 18 | 2141 | random-effects meta-regression | Coef = −0.010 (−0.056 to 0.036) | 0.66 ±0.005 d | hetexplained = −13.93% e | ||
| Age (years, mean) | 16 | 1968 | random-effects meta-regression | Coef = −0.003 (−0.108 to 0.102) | 0.98 ±0.001 d | hetexplained = −14.39% e | ||
| Clinical stage (proportion of stage-III/IV patients,%) | 7 | 1032 | random-effects meta-regression | Coef = −0.005 (−0.036 to 0.024) | 0.56 ±0.005 d | hetexplained = −225.16% e | ||
| Tobacco consumption (proportion of smokers, %) | 9 | 12707 | random-effects meta-regression | Coef = −0.008 (−0.032 to 0.016) | 0.48 ±0.005 d | hetexplained = −13.06% e | ||
| Areca nut/Betel quid consumption (proportion right chewers, %) | 2 | 250 | — | — | — | — | ||
| Alcohol consumption (% of patients with positive habit) | 5 | 660 | random-effects meta-regression | Coef = −0.047 (−0.111 to 0.018) | 0.25 ±0.004 d | hetexplained = 77.90% e | ||
| Disease-free survival | ||||||||
| EGFR overexpression (all) a | 19 | 2320 | REM | D-L | HR = 1.22 (0.28–1.53) | 0.08 | <0.001 | 65.0 |
| CLINICOPATHOLOGICAL CHARACTERISTICS | ||||||||
| T status | ||||||||
| EGFR overexpression (all) a | 20 | 1565 | REM | D-L | OR = 1.17 (0.72–1.90) | 0.53 | <0.001 | 65.0 |
| N status | ||||||||
| EGFR overexpression (all) a | 24 | 2040 | REM | D-L | OR = 1.37 (1.01–1.86) | 0.04 | 0.06 | 33.6 |
| Clinical Stage | ||||||||
| EGFR overexpression (all) a | 18 | 1456 | REM | D-L | OR = 1.12 (0.68–1.84) | 0.65 | <0.001 | 65.2 |
| Histological grade | ||||||||
| EGFR overexpression (all) a | 25 | 1860 | REM | D-L | OR = 1.43 (1.05–1.94) | 0.02 | 0.14 | 23.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cívico-Ortega, J.L.; González-Ruiz, I.; Ramos-García, P.; Cruz-Granados, D.; Samayoa-Descamps, V.; González-Moles, M.Á. Prognostic and Clinicopathological Significance of Epidermal Growth Factor Receptor (EGFR) Expression in Oral Squamous Cell Carcinoma: Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2023, 24, 11888. https://doi.org/10.3390/ijms241511888
Cívico-Ortega JL, González-Ruiz I, Ramos-García P, Cruz-Granados D, Samayoa-Descamps V, González-Moles MÁ. Prognostic and Clinicopathological Significance of Epidermal Growth Factor Receptor (EGFR) Expression in Oral Squamous Cell Carcinoma: Systematic Review and Meta-Analysis. International Journal of Molecular Sciences. 2023; 24(15):11888. https://doi.org/10.3390/ijms241511888
Chicago/Turabian StyleCívico-Ortega, José Luis, Isabel González-Ruiz, Pablo Ramos-García, David Cruz-Granados, Valerie Samayoa-Descamps, and Miguel Ángel González-Moles. 2023. "Prognostic and Clinicopathological Significance of Epidermal Growth Factor Receptor (EGFR) Expression in Oral Squamous Cell Carcinoma: Systematic Review and Meta-Analysis" International Journal of Molecular Sciences 24, no. 15: 11888. https://doi.org/10.3390/ijms241511888
APA StyleCívico-Ortega, J. L., González-Ruiz, I., Ramos-García, P., Cruz-Granados, D., Samayoa-Descamps, V., & González-Moles, M. Á. (2023). Prognostic and Clinicopathological Significance of Epidermal Growth Factor Receptor (EGFR) Expression in Oral Squamous Cell Carcinoma: Systematic Review and Meta-Analysis. International Journal of Molecular Sciences, 24(15), 11888. https://doi.org/10.3390/ijms241511888










