Impairment of SK-MEL-28 Development—A Human Melanoma Cell Line—By the Crataeva tapia Bark Lectin and Its Sequence-Derived Peptides
Abstract
1. Introduction
2. Results
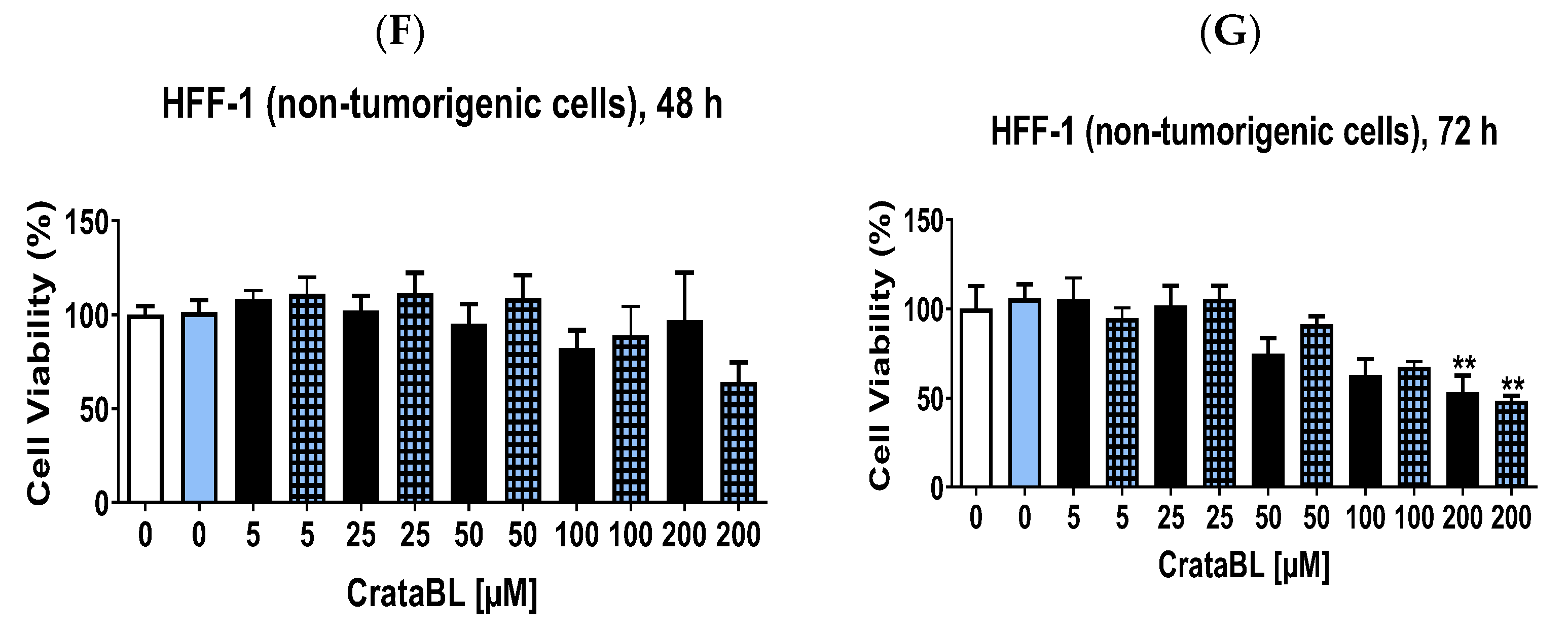
2.1. CrataBL Shows a Deleterious Effect on SK-MEL-28 Cell Viability Compared to rBbKIm and Has Low Toxicity on Healthy Fibroblast Cells
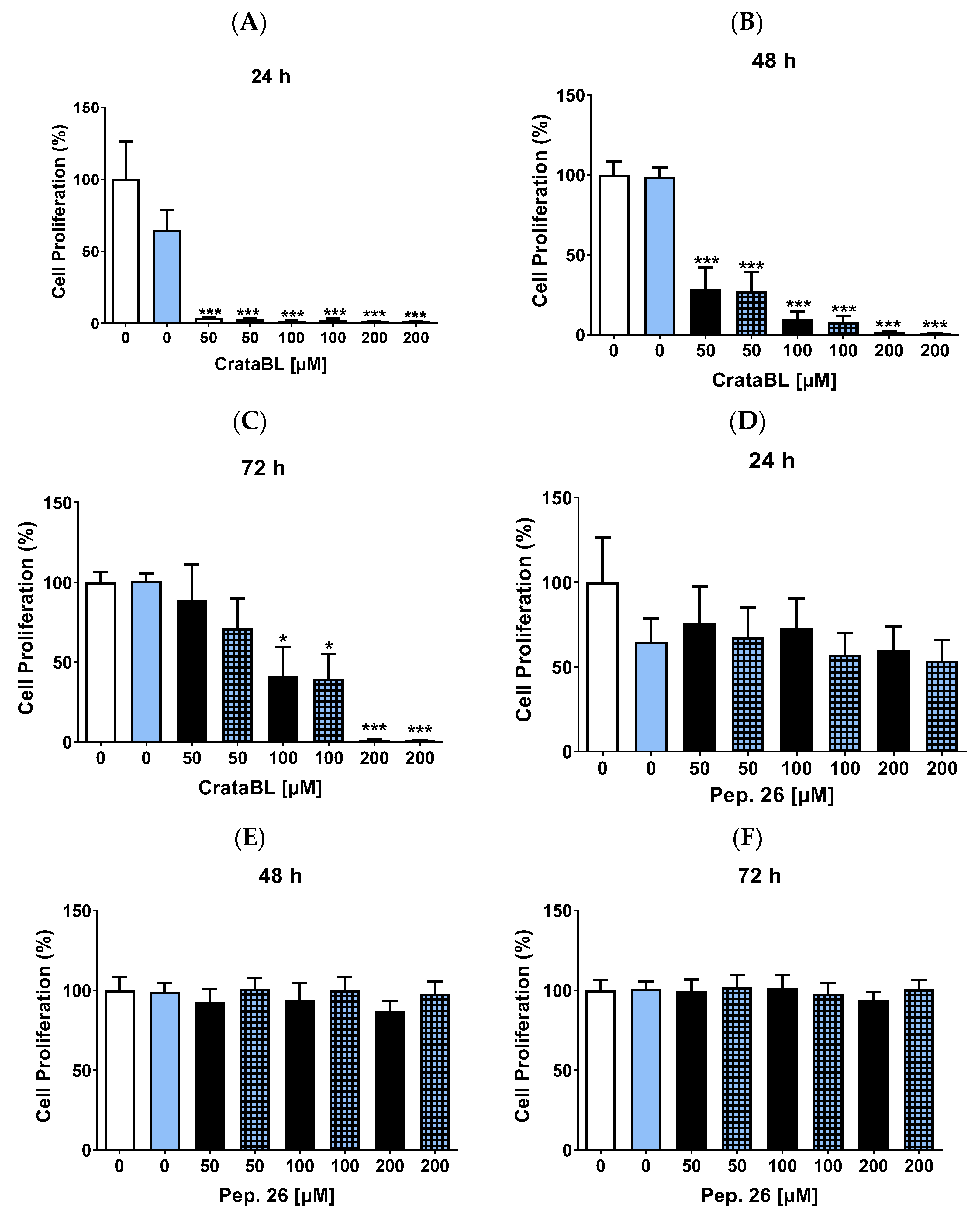
2.2. CrataBL Inhibits the Proliferation of SK-MEL-28
2.3. CrataBL Inhibits Cell Migration
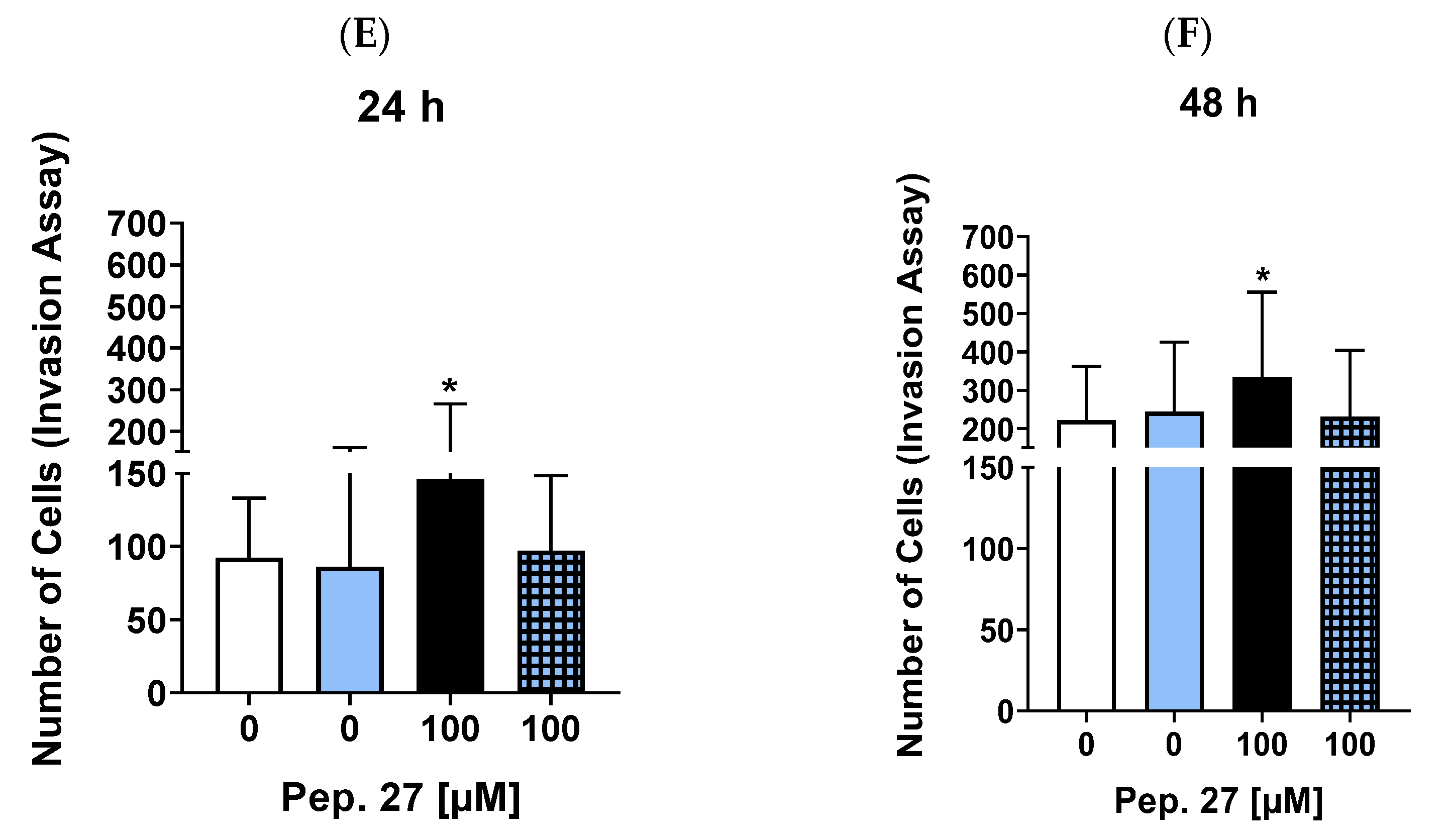
2.4. CrataBL Reduces the Invasion of Melanoma Cells by More Than 50% within 24 h of Treatment
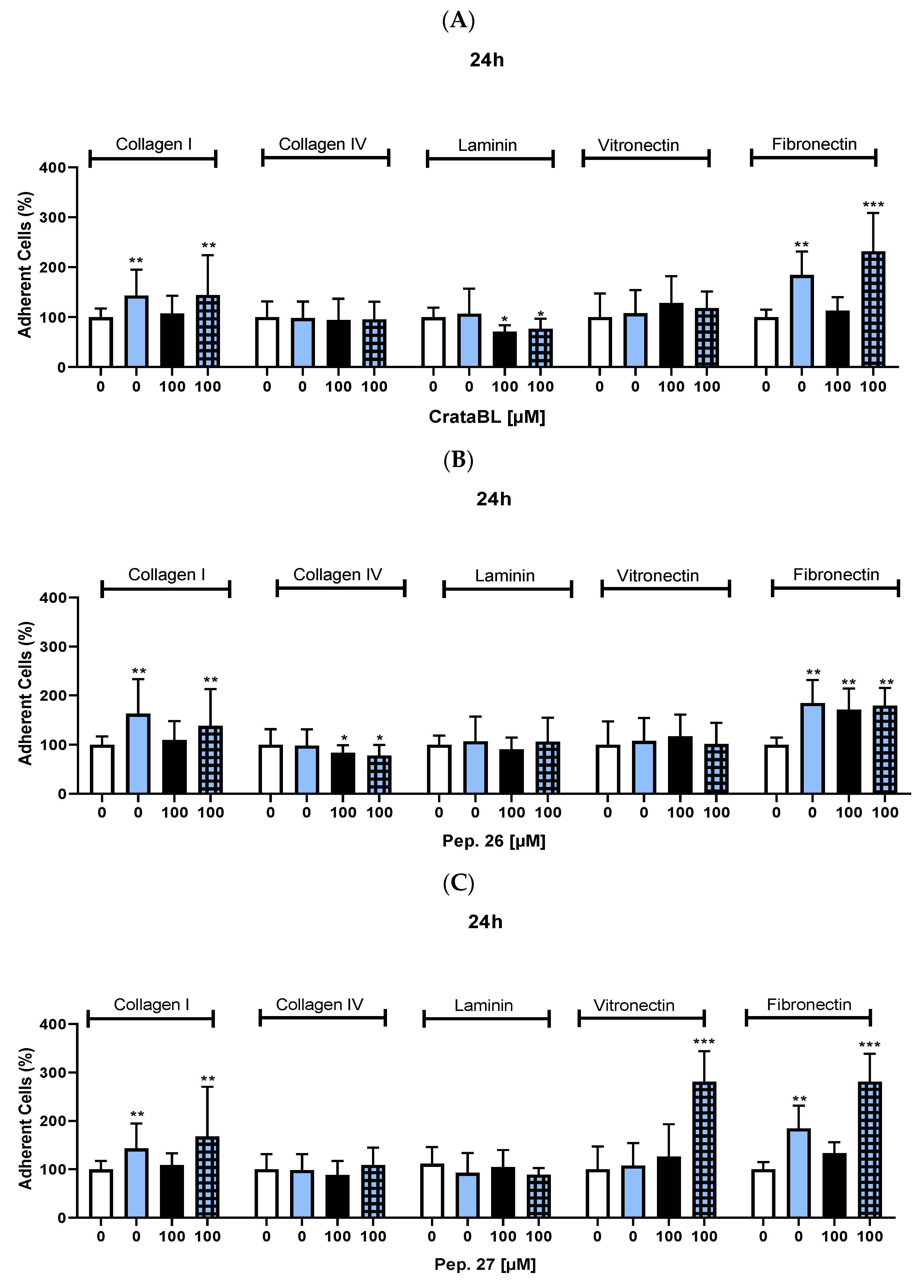
2.5. CrataBL and Pep. 26 Reduced Tumor Cell Adhesion
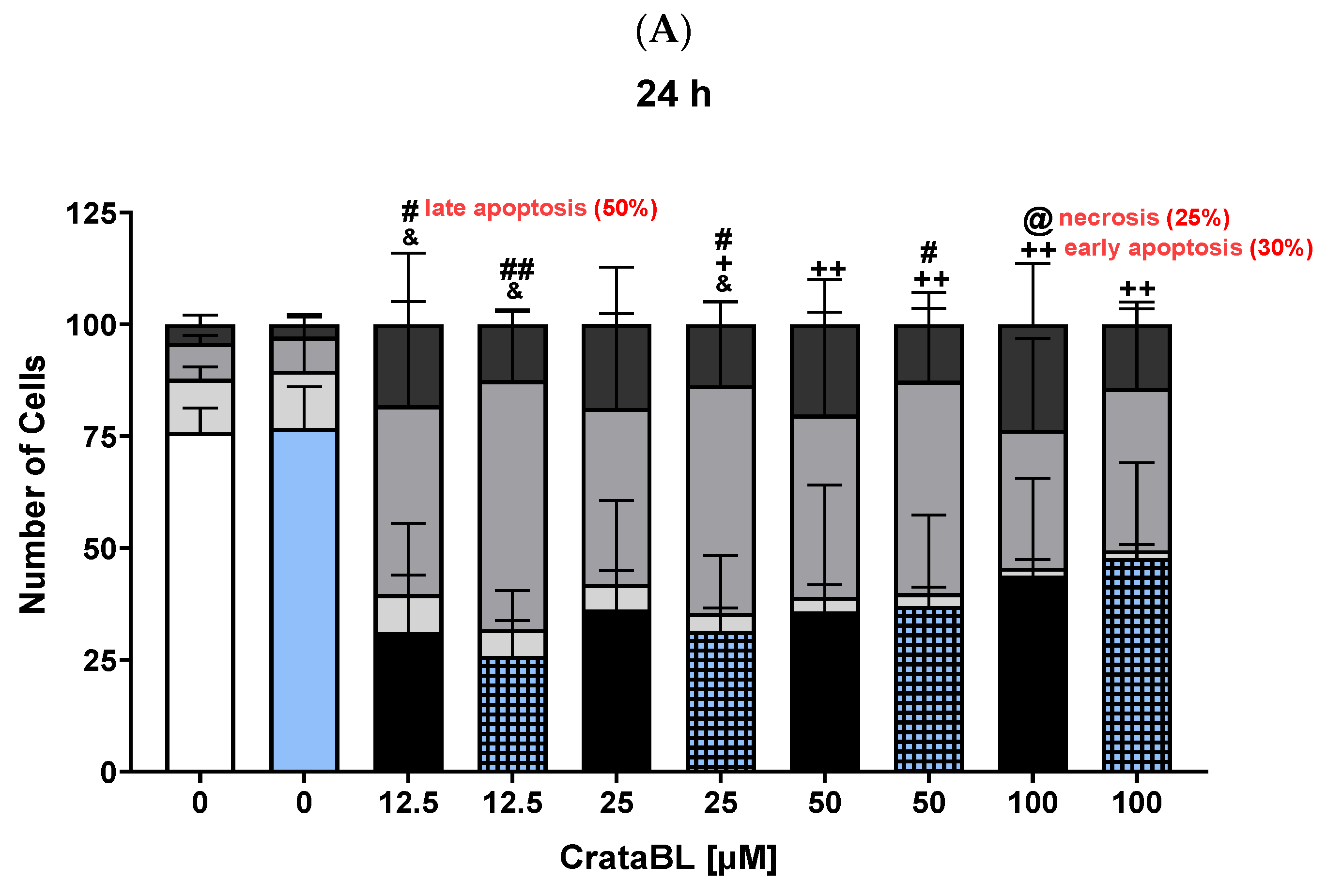
2.6. CrataBL and Its Fragment Peptides Induce Apoptosis in Melanoma Cells
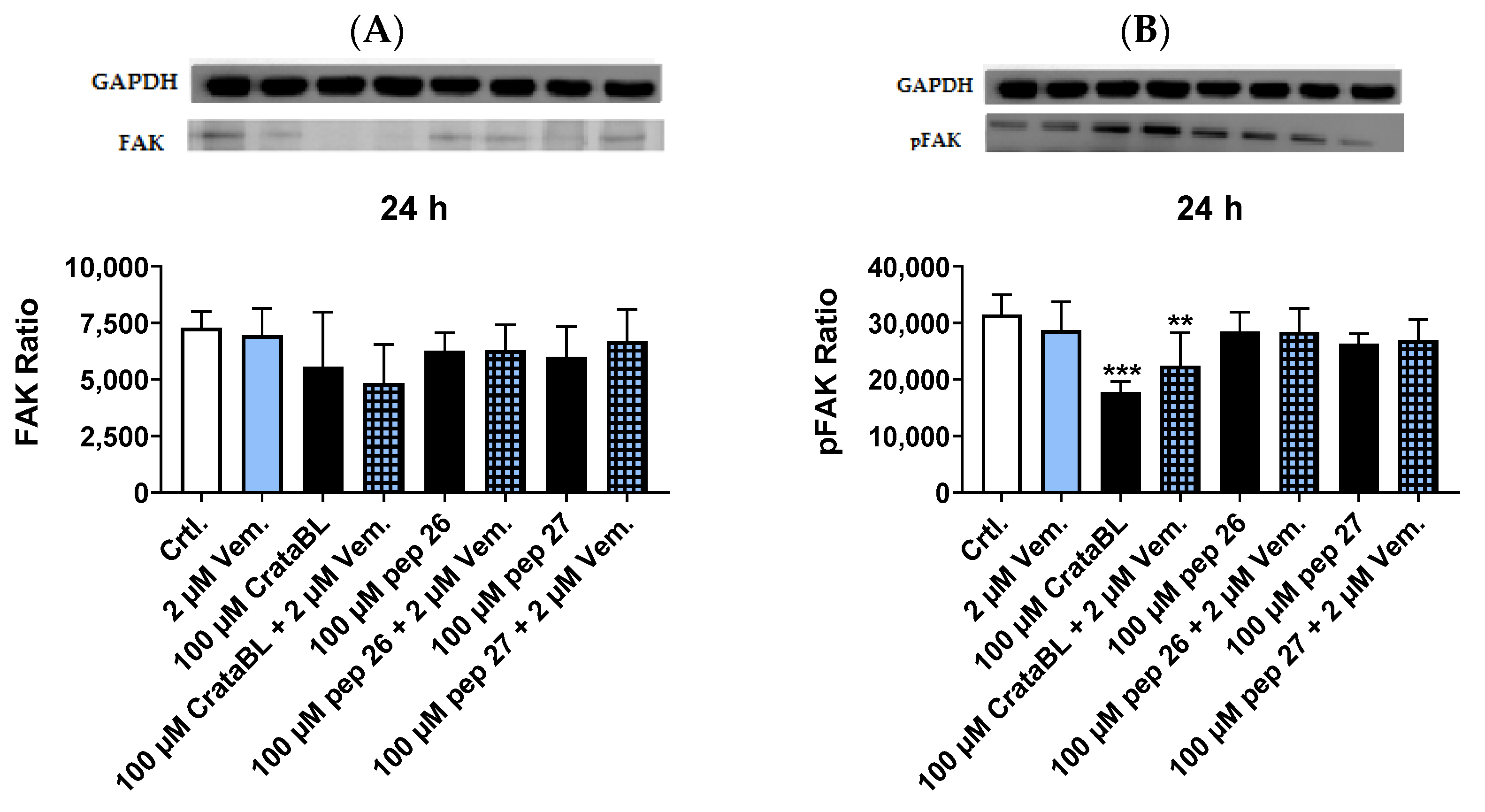
2.7. CrataBL Reduces the Expression of Phosphorylated Src Protein and NF-kB 50 kDa
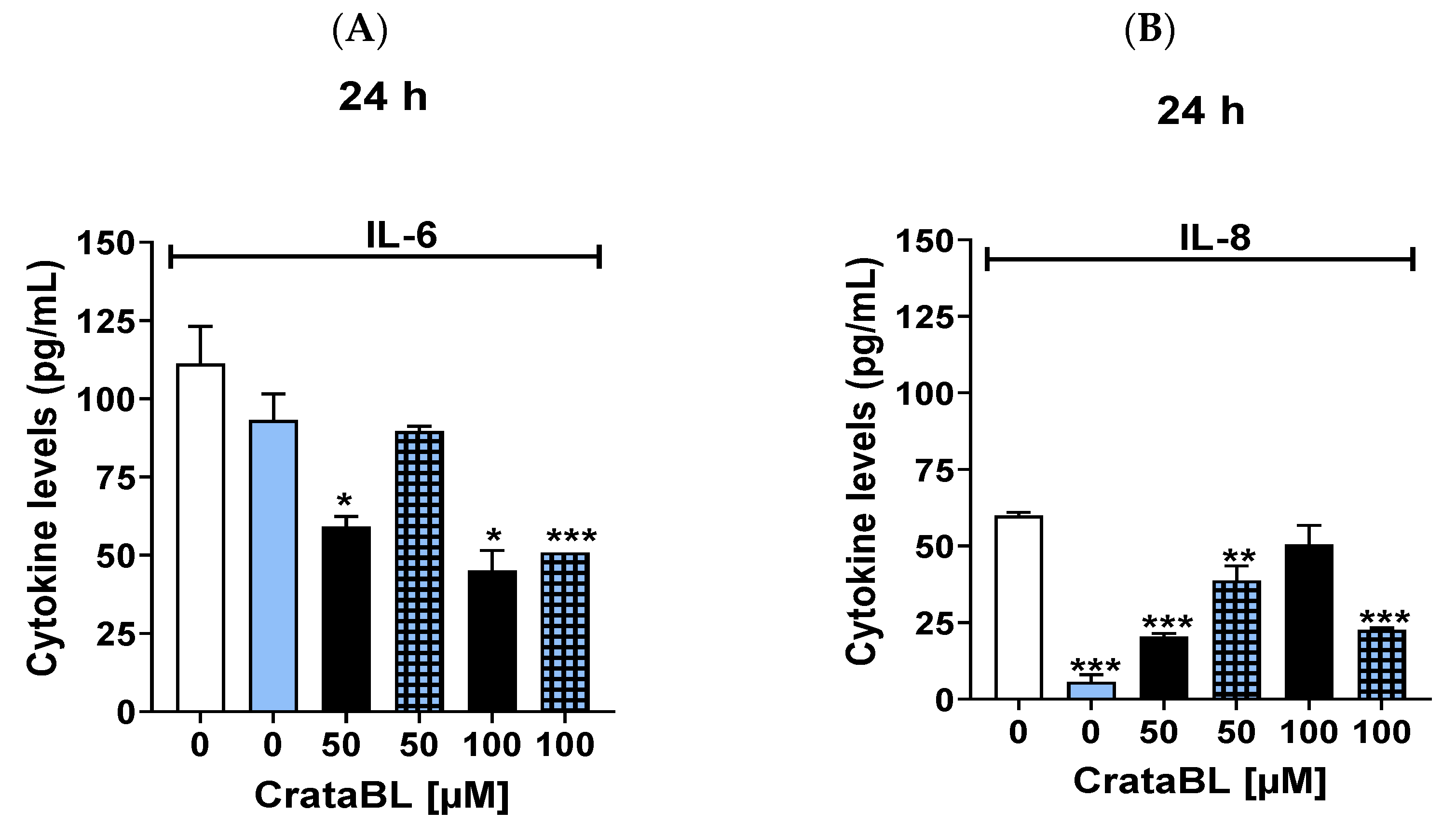
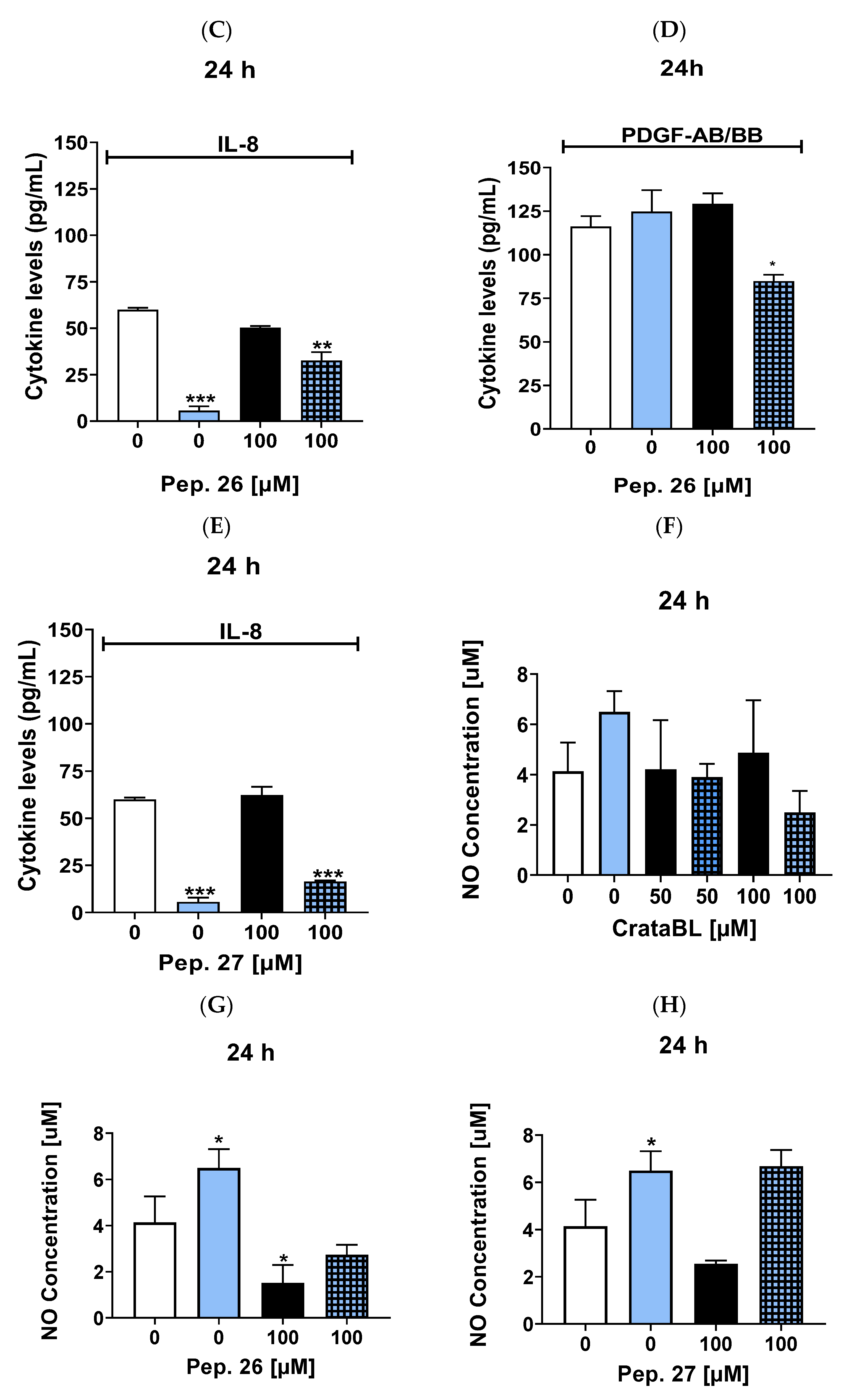
2.8. Anti-Inflammatory Properties of CrataBL and Related Peptides
3. Discussion
4. Materials and Methods
4.1. Cell Culture
4.2. CrataBL Purification
4.3. Synthetic Peptides Derived from the Protein CrataBL
4.4. Cell Viability
4.5. Cell Proliferation
4.6. Cell Migration
4.7. Cell Invasion
4.8. Cell Adhesion Assay
4.9. Cell Death Assay
4.10. Western Blotting
4.11. Cytokines Quantification
4.12. Nitric Oxide Measurements
4.13. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Silva, N.R.G.; de Araujo, F.N. Antibacterial Activity of Plant Lectins: A Review. Braz. Arch. Biol. Technol. 2021, 64, e21200631. [Google Scholar] [CrossRef]
- Mishra, A.; Behura, A.; Mawatwal, S.; Kumar, A.; Naik, L.; Mohanty, S.S.; Manna, D.; Dokania, P.; Mishra, A.; Patra, S.K.; et al. Structure-function and application of plant lectins in disease biology and immunity. Food Chem. Toxicol. 2019, 134, 110827. [Google Scholar] [CrossRef]
- Ielasi, F.S.; Alioscha-Perez, M.; Donohue, D.; Claes, S.; Sahli, H.; Schols, D.; Willaert, R.G. Lectin-Glycan Interaction Network-Based Identification of Host Receptors of Microbial Pathogenic Adhesins. mBio 2016, 7, e00584-16. [Google Scholar] [CrossRef]
- Cambi, A.; Figdor, C.G. Dual function of C-type lectin-like receptors in the immune system. Curr. Opin. Cell Biol. 2003, 15, 539–546. [Google Scholar] [CrossRef]
- Roth, P.; Mittelbronn, M.; Wick, W.; Meyermann, R.; Tatagiba, M.; Weller, M. Malignant glioma cells counteract antitumor immune responses through expression of lectin-like transcript-1. Cancer Res. 2007, 67, 3540–3544. [Google Scholar] [CrossRef]
- Mejía, E.G.; Prisecaru, V.I. Lectins as Bioactive Plant Proteins: A Potential in Cancer Treatment. Crit. Rev. Food Sci. Nutr. 2005, 45, 425–445. [Google Scholar] [CrossRef] [PubMed]
- Hashim, O.H.; Jayapalan, J.J.; Lee, C.S. Lectins: An effective tool for screening of potential cancer biomarkers. Peer J. 2017, 5, e3784. [Google Scholar] [CrossRef] [PubMed]
- Araújo, R.M.; Ferreira, R.S.; Napoleão, T.H.; Carneiro-da-cunha, M.G.; Coelho, L.C.; Correia, M.T.; Oliva, M.L.; Paiva, P.M. Crataeva tapia bark lectin is an affinity adsorbent and insecticidal agent. Plant Sci. 2012, 183, 20–26. [Google Scholar] [CrossRef]
- Ferreira, R.d.S.; Zhou, D.; Ferreira, J.G.; Silva, M.C.C.; Silva-Lucca, R.A.; Mentele, R.; Paredes-Gamero, E.J.; Bertolin, T.C.; Correia, M.T.d.S.; Paiva, P.M.G.; et al. Crystal Structure of Crataeva tapia Bark Protein (CrataBL) and Its Effect in Human Prostate Cancer Cell Lines. PLoS ONE 2013, 8, e64426. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Walcott, B.; Zhou, D.; Gustchina, A.; Lasanajak, Y.; Smith, D.F.; Ferreira, R.S.; Correia, M.T.; Paiva, P.M.; Bovin, N.V.; et al. Structural studies of the interaction of Crataeva tapia bark protein with heparin and other glycosaminoglycans. Biochemistry 2013, 52, 2148–2156. [Google Scholar] [CrossRef] [PubMed]
- Nunes, N.N.; Ferreira, R.S.; Silva-Lucca, R.A.; de Sá, L.F.; de Oliveira, A.E.; Correia, M.T.; Paiva, P.M.; Wlodawer, A.; Oliva, M.L. Potential of the Lectin/Inhibitor Isolated from Crataeva tapia Bark (CrataBL) for Controlling Callosobruchus maculatus Larva Development. J. Agric. Food Chem. 2015, 63, 10431–10436. [Google Scholar] [CrossRef] [PubMed]
- Salu, B.R.; Ferreira, R.S.; Brito, V.; Ottaiano, T.F.; Cruz, J.W.; Silva, M.C.; Correia, M.T.; Paiva, P.M.; Maffei, F.H.; Oliva, M.L. CrataBL, a lectin and Factor Xa inhibitor, plays a role in blood coagulation and impairs thrombus formation. Biol. Chem. 2014, 395, 1027–1035. [Google Scholar] [CrossRef] [PubMed]
- Bonturi, C.R.; Silva, M.C.C.; Motaln, H.; Salu, B.R.; Ferreira, R.D.S.; Batista, F.P.; Correia, M.T.D.S.; Paiva, P.M.G.; Turnšek, T.L.; Oliva, M.L.V. A Bifunctional Molecule with Lectin and Protease Inhibitor Activities Isolated from Crataeva tapia Bark Significantly Affects Cocultures of Mesenchymal Stem Cells and Glioblastoma Cells. Molecules 2019, 24, 2109. [Google Scholar] [CrossRef]
- Ferreira, J.G.; Diniz, P.M.; Andrade de Paula, C.A.; Lobo, Y.A.; Paredes-Gamero, E.J.; Paschoalin, T.; Nogueira-Pedro, A.; Maza, P.K.; Toledo, M.S.; Suzuki, E.; et al. The impaired viability of prostate cancer cell lines by the recombinant plant kallikrein inhibitor. J. Biol. Chem. 2013, 288, 13641–13654. [Google Scholar] [CrossRef]
- Bonturi, C.R.; Silva Teixeira, A.B.; Rocha, V.M.; Valente, P.F.; Oliveira, J.R.; Filho, C.M.B.; Fátima Correia Batista, I.; Oliva, M.L.V. Plant Kunitz Inhibitors and Their Interaction with Proteases: Current and Potential Pharmacological Targets. Int. J. Mol. Sci. 2022, 23, 4742. [Google Scholar] [CrossRef] [PubMed]
- Dzwierzynski, W.W. Melanoma risk factors and prevention. Clin. Plast. Surg. 2021, 48, 543–550. [Google Scholar] [CrossRef] [PubMed]
- Menzies, A.M.; Haydu, L.E.; Visintin, L.; Carlino, M.S.; Howle, J.R.; Thompson, J.F.; Kefford, R.F.; Scolyer, R.A.; Long, G.V. Distinguishing clinicopathologic features of patients with V600E and V600K BRAF-mutant metastatic melanoma. Clin. Cancer Res. 2012, 18, 3242–3249. [Google Scholar] [CrossRef] [PubMed]
- Solit, D.B.; Garraway, L.A.; Pratilas, C.A.; Sawai, A.; Getz, G.; Basso, A.; Ye, Q.; Lobo, J.M.; She, Y.; Osman, I.; et al. BRAF mutation predicts sensitivity to MEK inhibition. Nature 2006, 439, 358–362. [Google Scholar] [CrossRef]
- Luebker, S.A.; Koepsell, S.A. Diverse Mechanisms of BRAF Inhibitor Resistance in Melanoma Identified in Clinical and Preclinical Studies. Front. Oncol. 2019, 9, 268. [Google Scholar] [CrossRef]
- Liu, T.; Zhang, L.; Joo, D.; Sun, S.C. NF-κB signaling in inflammation. Sig. Transduct. Target Ther. 2017, 2, 17023. [Google Scholar] [CrossRef]
- Chauhan, D.; Bartok, E.; Gaidt, M.M.; Bock, F.J.; Herrmann, J.; Seeger, J.M.; Broz, P.; Beckmann, R.; Kashkar, H.; Tait, S.W.G.; et al. BAX/BAK-Induced Apoptosis Results in Caspase-8-Dependent IL-1β Maturation in Macrophages. Cell Rep. 2018, 25, 2354–2368. [Google Scholar] [CrossRef] [PubMed]
- Hsu, P.C.; Yang, C.T.; Jablons, D.M.; You, L. The Crosstalk between Src and Hippo/YAP Signaling Pathways in Non-Small Cell Lung Cancer (NSCLC). Cancers 2020, 12, 1361. [Google Scholar] [CrossRef]
- Yang, Z.; Misner, B.; Ji, H.; Poulos, T.L.; Silverman, R.B.; Meyskens, F.L.; Yang, S. Targeting Nitric Oxide Signaling with nNOS Inhibitors As a Novel Strategy for the Therapy and Prevention of Human Melanoma. Antioxid. Redox Signal 2013, 19, 433–447. [Google Scholar] [CrossRef]
- Esquivel-velázquez, M.; Ostoa-Saloma, P.; Palacios-Arreola, M.I.; Nava-Castro, K.E.; Castro, J.I.; Morales-Montor, J. The role of cytokines in breast cancer development and progression. J. Interferon Cytokine Res. 2015, 35, 1. [Google Scholar] [CrossRef]
- Strmiska, V.; Michalek, P.; Eckschlager, T.; Stiborova, M.; Adam, V.; Krizkova, S.; Heger, Z. Prostate cancer-specific hallmarks of amino acids metabolism: Towards a paradigm of precision medicine. Biochim. Biophys. Acta Rev. Cancer 2019, 1871, 248–258. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.; Xu, B. Inspiration from the Mirror: D-Amino Acid Containing Peptides in Biomedical Approaches. Biomol. Concepts 2016, 7, 179–187. [Google Scholar] [CrossRef]
- Souza, W.F.; Fortunato-Miranda, N.; Robbs, B.K.; de Araujo, W.M.; de-Freitas-Junior, J.C.; Bastos, L.G.; Viola, J.P.; Morgado-Díaz, J.A. Claudin-3 overexpression increases the malignant potential of colorectal cancer cells: Roles of ERK1/2 and PI3K-Akt as modulators of EGFR signaling. PLoS ONE 2013, 8, e74994. [Google Scholar] [CrossRef] [PubMed]
- Mundi, P.S.; Sachdev, J.; McCourt, C.; Kalinsky, K. AKT in cancer: New molecular insights and advances in drug development. Br. J. Clin. Pharm. 2016, 82, 943–956. [Google Scholar] [CrossRef]
- Pratheeshkumar, P.; Kuttan, G. Nomilin inhibits tumor-specific angiogenesis by downregulating VEGF, NO and proinflammatory cytokine profile and also by inhibiting the activation of MMP-2 and MMP-9. Eur. J. Pharm. 2011, 668, 450–458. [Google Scholar] [CrossRef]
- Halaban, R.; Zhang, W.; Bacchiocchi, A.; Cheng, E.; Parisi, F.; Ariyan, S.; Krauthammer, M.; McCusker, J.P.; Kluger, Y.; Sznol, M. PLX4032, a selective BRAF(V600E) kinase inhibitor, activates the ERK pathway and enhances cell migration and proliferation of BRAF melanoma cells. Pigment. Cell Melanoma Res. 2010, 232, 190–200. [Google Scholar] [CrossRef]
- Zhang, Q.; Lenardo, M.J.; Baltimore, D. 30 Years of NF-κB: A Blossoming of Relevance to Human Pathobiology. Cell 2017, 168, 37–57. [Google Scholar] [CrossRef] [PubMed]
- Guttà, C.; Rahman, A.; Aura, C.; Dynoodt, P.; Charles, E.M.; Hirschenhahn, E.; Joseph, J.; Wouters, J.; de Chaumont, C.; Rafferty, M.; et al. Low expression of pro-apoptotic proteins Bax, Bak and Smac indicates prolonged progression-free survival in chemotherapy-treated metastatic melanoma. Cell Death Dis. 2020, 11, 124. [Google Scholar] [CrossRef] [PubMed]
- Thiery, J.P.; Sleeman, J.P. Complex networks orchestrate epithelial-mesenchymal transitions. Nat. Rev. Mol. Cell Biol. 2006, 7, 131–142. [Google Scholar] [CrossRef]
- Zamarron, B.F.; Chen, W. Dual roles of immune cells and their factors in cancer development and progression. Int. J. Biol. Sci. 2011, 7, 651–658. [Google Scholar] [CrossRef]
- Dunlop, R.J.; Campbell, C.W. Cytokines and Advanced Cancer. J. Pain Symptom. Manag. 2000, 20, 214–232. [Google Scholar] [CrossRef]
- Oliva, L.V.; Almeida-Reis, R.; Theodoro-Junior, O.; Oliveira, B.M.; Leick, E.A.; Prado, C.M.; Brito, M.V.; Correia, M.T.S.; Paiva, P.M.G.; Martins, M.A.; et al. A plant proteinase inhibitor from Crataeva tapia (CrataBL) attenuates elastase-induced pulmonary inflammation, remodeling, and mechanical alterations in mice. Process Biochem. 2015, 50, 1958–1965. [Google Scholar] [CrossRef]
- Bortolozzo, A.; Rodrigues, A.; Arantes-Costa, F.M.; Saraiva-Romanholo, B.M.; de Souza, F.; Brüggemann, T.R.; de Brito, M.V.; Ferreira, R.; Correia, M.; Paiva, P.; et al. The Plant Proteinase Inhibitor CrataBL Plays a Role in Controlling Asthma Response in Mice. Biomed. Res. Int. 2018, 2018, 9274817. [Google Scholar] [CrossRef]
- Bauman, J.E.; Eaton, K.D.; Wallace, S.G.; Carr, L.L.; Lee, S.J.; Jones, D.V.; Arias-Pulido, H.; Cerilli, L.A.; Martins, R.G. A phase II study of pulse dose imatinib mesylate and weekly paclitaxel in patients aged 70 and over with advanced non-small cell lung cancer. BMC Cancer 2012, 12, 449. [Google Scholar] [CrossRef] [PubMed]
- Yao, X.; Huang, J.; Zhong, H.; Shen, N.; Faggioni, R.; Fung, M.; Yao, Y. Targeting interleukin-6 in inflammatory autoimmune diseases and cancers. Pharmacol. Ther. 2014, 141, 125–139. [Google Scholar] [CrossRef]
- Johnson, D.E.; O’ Keefe, R.A.; Grandis, J.R. Targeting the IL-6/JAK/STAT3 signaling axis in cancer. Nat. Rev. Clin. Oncol. 2018, 15, 234–248. [Google Scholar] [CrossRef]
- Namba, H.; Saenko, V.; Yamashita, S. Nuclear factor-kB in thyroid carcinogenesis and progression: A novel therapeutic target for advanced thyroid cancer. Arq. Bras. Endocrinol. Metab. São Paulo 2007, 51, 843–851. [Google Scholar] [CrossRef]
- Notarangelo, T.; Sisinni, L.; Trino, S.; Calice, G.; Simeon, V.; Landriscina, M. IL6/STAT3 axis mediates resistance to BRAF inhibitors in thyroid carcinoma cells. Cancer Lett. 2018, 433, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Kolář, M.; Szabo, P.; Dvořánková, B.; Lacina, L.; Gabius, H.J.; Strnad, H.; Sáchová, J.; Vlček, C.; Plzák, J.; Chovanec, M.; et al. Upregulation of IL-6, IL-8, and CXCL-1 production in dermal fibroblasts by normal and malignant epithelial cells in vitro: Immunohistochemical and transcriptomic analyses. Biol. Cell 2012, 104, 738–751. [Google Scholar] [CrossRef]
- Kazlauskas, A. PDGFs and their receptors. Gene 2017, 614, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Forsberg, K.; Valyi-Nagy, I.; Heldin, C.-H.; Herlyn, M.; Westermark, B. Platelet-derived growth factor (PDGF) in oncogenesis: Development of a vascular connective tissue stroma in xenotransplanted human melanoma producing PDGF-BB. Proc. Natl. Acad. Sci. USA 1993, 90, 393–397. [Google Scholar] [CrossRef]
- Almeida, P.C.; Nantes, I.L.; Rizzi, C.C.; Júdice, W.A.; Chagas, J.L.; Nader, H.B.; Tersariol, I.L. Cysteine proteinase activity regulation. A possible role of heparin and heparin-like glycosaminoglycans. J. Biol. Chem. 1999, 274, 30433–30438. [Google Scholar] [CrossRef] [PubMed]
- Colella, R.; Goodwyn, E.; Gopal, P. Increased cell density decreases cysteine proteinase inhibitor activity and increases invasive ability of two prostate tumor cell lines. Cancer Lett. 2002, 185, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Gozzo, A.J.; Nunes, V.A.; Cruz-Silva, I.; Carmona, A.K.; Nader, B.; Faljoni-Alario, A.; Sampaio, M.U.; Araújo, M.S. Heparin modulation of human plasma kallikrein on different substrates and inhibitors. Biol. Chem. 2006, 387, 1129–1138. [Google Scholar] [CrossRef]
- Thierauf, J.; Veit, J.A.; Lennerz, J.K.; Weissinger, S.E.; Affolter, A.; Döscher, J.; Bergmann, C.; Knopf, A.; Grünow, J.; Grünmüller, L.; et al. Expression of kallikrein-related peptidase 6 in primary mucosal malignant melanoma of the head and neck. Head Neck Pathol. 2017, 11, 314–320. [Google Scholar] [CrossRef]
- Costa, P.L.; Sirois, P.; Tannock, I.F.; Chammas, R. The role of kinin receptors in cancer and therapeutic opportunities. Cancer Lett. 2014, 345, 27–38. [Google Scholar] [CrossRef]
- Lowry, O.H.; Rosebrough, N.J.; Farr, A.L.; Randall, R.J. Protein measurement with the Folin phenol reagent. J. Biol. Chem. 1951, 193, e265. [Google Scholar] [CrossRef]
- Boncler, M.; Różalski, M.; Krajewska, U.; Podsędek, A.; Watala, C. Comparison of PrestoBlue and MTT assays of cellular viability in the assessment of anti-proliferative effects of plant extracts on human endothelial cells. J. Pharm. Toxicol. Methods 2014, 69, 9–16. [Google Scholar] [CrossRef]
- Dolbeare, F.; Beisker, W.; Pallavicini, M.G.; Vanderlaan, M.; Gray, J.W. Cytochemistry for bromodeoxyuridine/DNA analysis: Stoichiometry and sensitivity. Cytometry 1985, 6, 521–530. [Google Scholar] [CrossRef]
- Rodriguez, L.G.; Wu, X.; Guan, J.L. Wound-healing assay. Methods Mol. Biol. 2005, 294, 23–29. [Google Scholar] [PubMed]
- Falasca, M.; Raimondi, C.; Maffucci, T. Boyden chamber. Methods Mol. Biol. 2011, 769, 87–95. [Google Scholar] [PubMed]
- Moore, A.; Donahue, C.J.; Bauer, K.D.; Mather, J.P. Simultaneous measurement of cell cycle and apoptotic cell death. Methods Cell Biol. 1998, 57, 265–278. [Google Scholar]
- Towbin, H.; Staehelin, T.; Gordon, J. Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets: Procedure and some applications. Proc. Natl. Acad. Sci. USA 1979, 76, 4350–4354. [Google Scholar] [CrossRef]
- Mahmood, T.; Yang, P.C. Western blot: Technique, theory, and trouble shooting. N. Am. J. Med. Sci. 2012, 4, 429–434. [Google Scholar]
- Kupcova Skalnikova, H.; Cizkova, J.; Cervenka, J.; Vodicka, P. Advances in Proteomic Techniques for Cytokine Analysis: Focus on Melanoma Research. Int. J. Mol. Sci. 2017, 18, 2697. [Google Scholar] [CrossRef]
- Dweik, R.A.; Laskowski, D.; Abu-Soud, H.M.; Kaneko, F.T.; Hutte, R.; Stuehr, D.J.; Erzurum, S.C. Nitric oxide synthesis in the lung. Regulation by oxygen through a kinetic mechanism. J. Clin. Investig. 1998, 101, 660–666. [Google Scholar]









Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lie, K.C.M.; Bonturi, C.R.; Salu, B.R.; de Oliveira, J.R.; Bonini Galo, M.; Paiva, P.M.G.; Correia, M.T.d.S.; Oliva, M.L.V. Impairment of SK-MEL-28 Development—A Human Melanoma Cell Line—By the Crataeva tapia Bark Lectin and Its Sequence-Derived Peptides. Int. J. Mol. Sci. 2023, 24, 10617. https://doi.org/10.3390/ijms241310617
Lie KCM, Bonturi CR, Salu BR, de Oliveira JR, Bonini Galo M, Paiva PMG, Correia MTdS, Oliva MLV. Impairment of SK-MEL-28 Development—A Human Melanoma Cell Line—By the Crataeva tapia Bark Lectin and Its Sequence-Derived Peptides. International Journal of Molecular Sciences. 2023; 24(13):10617. https://doi.org/10.3390/ijms241310617
Chicago/Turabian StyleLie, Kathleen Chwen Ming, Camila Ramalho Bonturi, Bruno Ramos Salu, Juliana Rodrigues de Oliveira, Márcia Bonini Galo, Patrícia Maria Guedes Paiva, Maria Tereza dos Santos Correia, and Maria Luiza Vilela Oliva. 2023. "Impairment of SK-MEL-28 Development—A Human Melanoma Cell Line—By the Crataeva tapia Bark Lectin and Its Sequence-Derived Peptides" International Journal of Molecular Sciences 24, no. 13: 10617. https://doi.org/10.3390/ijms241310617
APA StyleLie, K. C. M., Bonturi, C. R., Salu, B. R., de Oliveira, J. R., Bonini Galo, M., Paiva, P. M. G., Correia, M. T. d. S., & Oliva, M. L. V. (2023). Impairment of SK-MEL-28 Development—A Human Melanoma Cell Line—By the Crataeva tapia Bark Lectin and Its Sequence-Derived Peptides. International Journal of Molecular Sciences, 24(13), 10617. https://doi.org/10.3390/ijms241310617






