Arrhythmias after COVID-19 Vaccination: Have We Left All Stones Unturned?
Abstract
1. Introduction
2. Data from the Literature and Vigilance Databases
| Authors | Title | Year | N. of Cases | Centre/Nation | Type of Vaccine | Type of Arrhythmia |
|---|---|---|---|---|---|---|
| Aiba T et al. [5] | “Frequent Premature Ventricular Contraction and Non-Sustained Ventricular Tachycardia After the SARS-CoV-2 Vaccination in Patient with Implantable Cardioverter Defibrillator Due to Acquired Long-QT Syndrome” | June 2021 | 1 | Japan | Pfizer-BioNTech | Premature ventricular contraction and non-sustained polymorphic ventricular tachycardia |
| Abrich and Olshansky [6] | “Torsades de pointes following vaccination for COVID-19” | June 2022 | 1 | USA | Pfizer-BioNTech | Torsades de pointes-ventricular fibrillation |
| Beccarino et al. [7] | “COVID-19 vaccination associated right ventricular outflow tract ventricular tachycardia in a structurally normal heart” | March 2022 | 1 | USA | Pfizer-BioNTech | Sustained unstable ventricular tachycardia |
| Slater et al. [8] | “VT storm in long QT resulting from COVID-19 vaccine allergy treated with epinephrine” | November 2021 | 1 | Canada | Moderna | Ventricular tachycardia storm in long QT |
| M. Teresa Marco García et al. [9] | “Tachycardia as an undescribed adverse effect to the Comirnaty© vaccine (BNT162b2 Pfizer-BioNTech COVID-19 vaccine): Description of 3 cases with a history of SARS-CoV-2 disease” | May 2022 | 3 | Spain | Pfizer-BioNTech | Ventricular Tachycardia and extrasystoles in physicians |
| Hoffer Etienne et al. [10] | “Transient but recurrent complete heart block in a patient after COVID-19 vaccination—A case report” | April 2022 | 1 | Belgium | Pfizer-BioNTech | Transient but recurrent complete heart block |
| Kyung Hee Lim and Jong-Sung Park [17] | COVID-19 Vaccination-Induced Ventricular Fibrillation in an Afebrile Patient with Brugada Syndrome | April 2022 | 1 | Korea | Pfizer-BioNTech | Ventricular fibrillation |
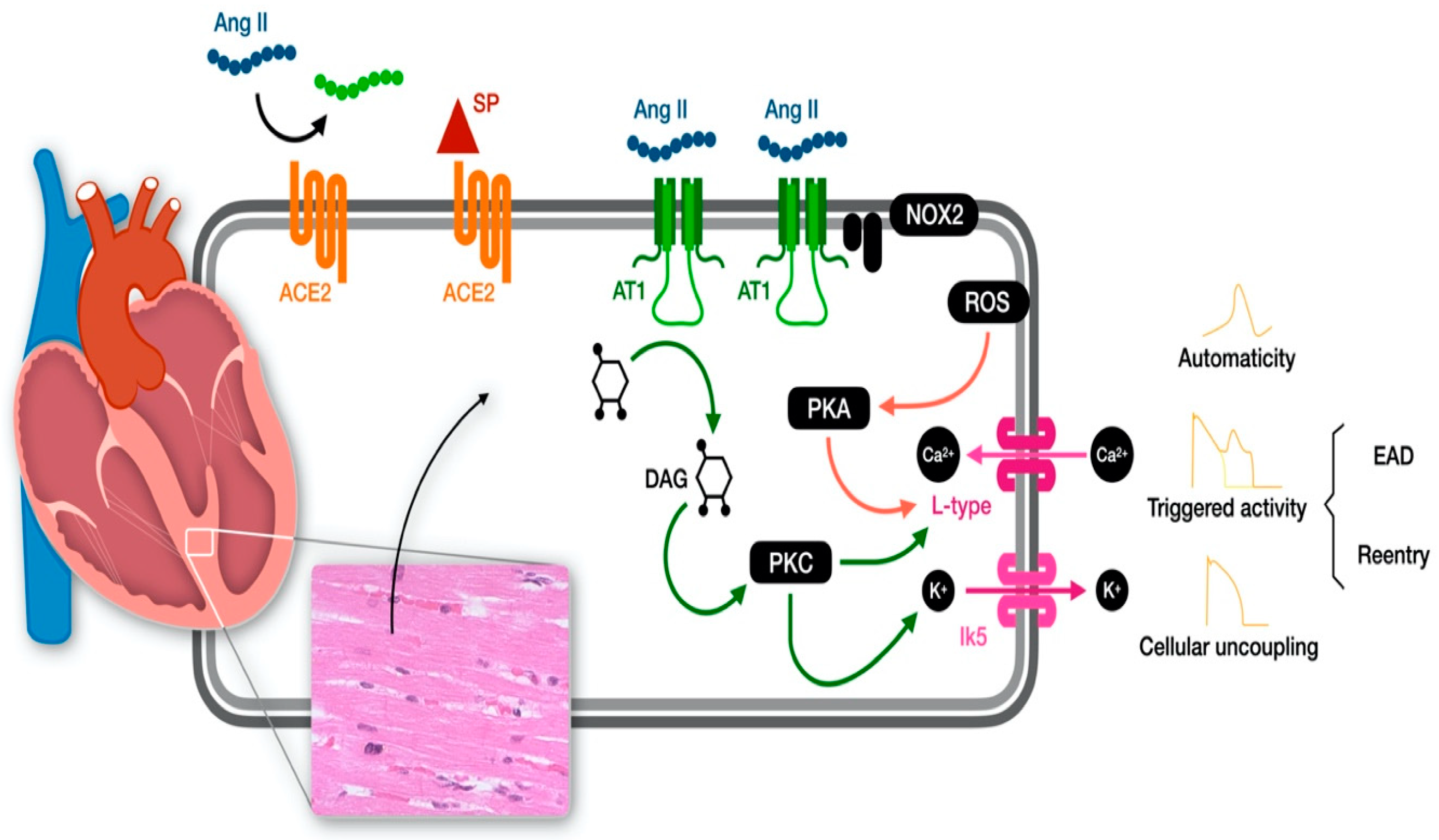
3. The Molecular Pathway behind the Heart Electrophysiology Alteration
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Steele, M.K.; Couture, A.; Reed, C.; Iuliano, D.; Whitaker, M.; Fast, H.; Hall, A.J.; MacNeil, A.; Cadwell, B.; Marks, K.J.; et al. Estimated Number of COVID-19 Infections, Hospitalizations, and Deaths Prevented Among Vaccinated Persons in the US, December 2020 to September 2021. JAMA Netw. Open 2022, 5, e2220385. [Google Scholar] [CrossRef]
- Montano, D. Frequency and Associations of Adverse Reactions of COVID-19 Vaccines Reported to Pharmacovigilance Systems in the European Union and the United States. Front. Public Health 2022, 9, 756633. [Google Scholar] [CrossRef] [PubMed]
- Almas, T.; Rehman, S.; Mansour, E.; Khedro, T.; Alansari, A.; Malik, J.; Alshareef, N.; Nagarajan, V.R.; Al-Awaid, A.H.; Alsufyani, R.; et al. Epidemiology, clinical ramifications, and cellular pathogenesis of COVID-19 mRNA-vaccination-induced adverse cardiovascular outcomes: A state-of-the-heart review. Biomed. Pharmacother. 2022, 149, 112843. [Google Scholar] [CrossRef] [PubMed]
- Witberg, G.; Barda, N.; Hoss, S.; Richter, I.; Wiessman, M.; Aviv, Y.; Grinberg, T.; Auster, O.; Dagan, N.; Balicer, R.D.; et al. Myocarditis after COVID-19 Vaccination in a Large Health Care Organization. N. Engl. J. Med. 2021, 385, 2132–2139. [Google Scholar] [CrossRef] [PubMed]
- Strickberger, S.; Ip, J.; Saksena, S.; Curry, K.; Bahnson, T.D.; Ziegler, P.D. Relationship between atrial tachyarrhythmias and symptoms. Heart Rhythm 2005, 2, 125–131. [Google Scholar] [CrossRef]
- Bikkina, M.; Larson, M.G.; Levy, D. Prognostic Implications of Asymptomatic Ventricular Arrhythmias: The Framingham Heart Study. Ann. Intern. Med. 1992, 117, 990. [Google Scholar] [CrossRef]
- Aiba, T.; Ishibashi, K.; Hattori, K.; Wada, M.; Ueda, N.; Miyazaki, Y.; Wakamiya, A.; Yamagata, K.; Inoue, Y.; Miyamoto, K.; et al. Frequent Premature Ventricular Contraction and Non-Sustained Ventricular Tachycardia After the SARS-CoV-2 Vaccination in Patient with Implantable Cardioverter Defibrillator Due to Acquired Long-QT Syndrome. Circ. J. 2021, 85, 2117. [Google Scholar] [CrossRef]
- Abrich, V.A.; Olshansky, B. Torsades de pointes following vaccination for COVID-19. Heart Rhythm Case Rep. 2022, 8, 393–397. [Google Scholar] [CrossRef]
- Beccarino, N.; Hou, L.; Sarkar, K.; Chen, L.; Mitra, R.L. COVID-19 vaccination associated right ventricular outflow tract ventricular tachycardia in a structurally normal heart. JACC 2022, 79 (Suppl. S9), 2506. [Google Scholar] [CrossRef]
- Slater, N.R.; Murphy, K.R.; Sikkel, M.B. VT storm in long QT resulting from COVID-19 vaccine allergy treated with epinephrine. Eur. Heart J. 2022, 43, 1176. [Google Scholar] [CrossRef]
- García, M.T.M.; Lana, Á.T.; Agudo, M.B.A.; de la Trinidad Rufino Delgado, M. Tachycardia as an un-described adverse effect to the Comirnaty© vaccine (BNT162b2 Pfiz-er-BioNTech COVID-19 vaccine): Description of 3 cases with a history of SARS-CoV-2 disease. Enferm. Infecc. Microbiol. Clín. 2022, 40, 275–283. [Google Scholar]
- Etienne, H.; Charles, P.; Pierre, T. Transient but recurrent complete heart block in a patient after COVID-19 vaccination—A case report. Ann. Med. Surg. 2022, 78, 103694. [Google Scholar] [CrossRef] [PubMed]
- Kaur, R.J.; Dutta, S.; Charan, J.; Bhardwaj, P.; Tandon, A.; Yadav, D.; Islam, S.; Haque, M. Cardiovascular Adverse Events Reported from COVID-19 Vaccines: A Study Based on WHO Database. Int. J. Gen. Med. 2021, 14, 3909–3927. [Google Scholar] [CrossRef] [PubMed]
- Publishing Service. Government of UK. COVID-19 mRNA Pfizer-BioNTech Vaccine Analysis Print. Updated 28 May 2021. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwjEm7-JvtH_AhUmh_0HHfYiBKgQFnoECA0QAQ&url=https%3A%2F%2Fassets.publishing.service.gov.uk%2Fgovernment%2Fuploads%2Fsystem%2Fuploads%2Fattachment_data%2Ffile%2F1072043%2FCOVID-19_mRNA_Pfizer-_BioNTech_vaccine_analysis_print.pdf&usg=AOvVaw3AWYjkyivgrcjUq0hGeP1p&opi=89978449 (accessed on 4 June 2021).
- World Health Organization. Immunization Stress-Related Responses. A Manual. Available online: https://www.who.int/publications/i/item/978-92-4-151594-8 (accessed on 4 June 2021).
- Quer, G.; Gadaleta, M.; Radin, J.M.; Andersen, K.G.; Baca-Motes, K.; Ramos, E.; Topol, E.J.; Steinhubl, S.R. The physiologic response to COVID-19 vaccination. medRxiv 2021. [Google Scholar] [CrossRef]
- Okawa, K.; Kan, T. Unmasked type 1 Brugada ECG pattern without a fever after a COVID-19 vaccination. Heart Rhythm Case Rep. 2022, 8, 267–269. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, K.J. Suspected Cardiovascular Side Effects of Two COVID-19 Vaccines. J. Biol. Today’s World 2021, 10, 1–6. [Google Scholar]
- Patone, M.; Mei, X.W.; Handunnetthi, L.; Dixon, S.; Zaccardi, F.; Shankar-Hari, M.; Watkinson, P.; Khunti, K.; Harnden, A.; Coupland, C.A.C.; et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat. Med. 2022, 28, 410–422. [Google Scholar] [CrossRef]
- Ab Rahman, N.; Lim, M.T.; Lee, F.Y.; Lee, S.C.; Ramli, A.; Saharudin, S.N.; King, T.L.; Jam, E.B.A.; Ayub, N.A.; Sevalingam, R.K.; et al. Risk of serious adverse events after the BNT162b2, CoronaVac, and ChAdOx1 vaccines in Malaysia: A self-controlled case series study. Vaccine 2022, 40, 4394–4402. [Google Scholar] [CrossRef]
- Ittiwut, C.; Mahasirimongkol, S.; Srisont, S.; Ittiwut, R.; Chockjamsai, M.; Durongkadech, P.; Sawaengdee, W.; Khunphon, A.; Larpadisorn, K.; Wattanapokayakit, S.; et al. The Genetic basis of sudden death after COVID-19 vaccination in Thailand. Heart Rhythm 2022, 19, 1874–1879. [Google Scholar] [CrossRef]
- Sun, C.L.F.; Jaffe, E.; Levi, R. Increased emergency cardiovascular events among under-40 population in Israel during vaccine rollout and third COVID-19 wave. Sci. Rep. 2022, 12, 6978. [Google Scholar] [CrossRef]
- Maffetone, P.B.; Laursen, P.B. COVID-Related Athletic Deaths: Another Perfect Storm? Front. Sports Act. Living 2022, 4, 829093. [Google Scholar] [CrossRef] [PubMed]
- Publishing Service. Government of UK. COVID-19 mRNA Moderna Vaccine Analysis Print. Updated 29 June 2022. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_da-ta/file/989996/COVID-19_mRNA_moderna_Vaccine_Analysis_Print.pdf (accessed on 15 July 2022).
- Ajmera, K.M. Association between COVID-19 Vaccine and New-Onset Atrial Fibrillation. Cardiol. Cardiovasc. Med. 2022, 6, 1–6. [Google Scholar] [CrossRef]
- Kattubadi, A.; Solorzano, J.; Feng, K.; Brar, V.; Dominic, P. COVID-19 vaccines and atrial fibrillation risk: A pharmacovigilance analysis. J. Am. Coll. Cardiol. 2022, 79, 1838. [Google Scholar] [CrossRef]
- Sangpornsuk, N.; Rungpradubvong, V.; Tokavanich, N.; Srisomwong, S.; Ananwattanasuk, T.; Teerawongsakul, P.; Kerr, S.J.; Suwanwalaikorn, M.; Jongnarangsin, K.; Chokesuwattanaskul, R. Arrhythmias after SARS-CoV-2 Vaccination in Patients with a Cardiac Implantable Electronic Device: A Multicenter Study. Biomedicines 2022, 10, 2838. [Google Scholar] [CrossRef] [PubMed]
- De Lusignan, S.; Correa, A.; Dos Santos, G.; Meyer, N.; Haguinet, F.; Webb, R.; McGee, C.; Byford, R.; Yonova, I.; Pathirannehelage, S.; et al. Enhanced Safety Surveillance of Influenza Vaccines in General Practice, Winter 2015-16: Feasibility Study. JMIR Public Health Surveill. 2019, 5, e12016. [Google Scholar] [CrossRef] [PubMed]
- Shi, A.; Tang, X.; Xia, P.; Hao, M.; Shu, Y.; Nakanishi, H.; Smayra, K.; Farzad, A.; Hu, K.; Liu, Q.; et al. Cardiac Arrhythmia after COVID-19 Vaccination versus Non-COVID-19 Vaccination: A Systematic Review and Meta-Analysis. medRxiv 2022, 11. [Google Scholar] [CrossRef]
- Sorgente, A.; Capulzini, L.; Brugada, P. The known into the unknown: Brugada syndrome and COVID-19. JACC Case Rep. 2020, 2, 1250–1251. [Google Scholar] [CrossRef]
- Lim, K.H.; Park, J.-S. COVID-19 Vaccination-Induced Ventricular Fibrillation in an Afebrile Patient with Brugada Syndrome. J. Korean Med. Sci. 2022, 37, e306. [Google Scholar] [CrossRef]
- Abutaleb, M.H.; Makeen, H.A.; Meraya, A.M.; Alqahtani, S.S.; Al-Mass, B.I.; Aljazaeri, R.O.; Alhazmi, B.D.; Kalakattawi, A.M.N.; Alajam, A.A. Risks of Cardiac Arrhythmia Associated with COVID-19 Vaccination: A Systematic Review and Meta-Analysis. Vaccines 2023, 11, 112. [Google Scholar] [CrossRef]
- Fazlollahi, A.; Zahmatyar, M.; Noori, M.; Nejadghaderi, S.A.; Sullman, M.J.; Shekarriz-Foumani, R.; Kolahi, A.-A.; Singh, K.; Safiri, S. Cardiac complications fol-lowing mRNA COVID-19 vaccines: A systematic review of case reports and case series. Rev. Med. Virol. 2022, 32, e2318. [Google Scholar] [CrossRef]
- Choi, S.; Lee, S.; Seo, J.-W.; Kim, M.-J.; Jeon, Y.H.; Park, J.H.; Lee, J.K.; Yeo, N.S. Myocarditis-induced Sudden Death after BNT162b2 mRNA COVID-19 Vaccination in Korea: Case Report Focusing on Histopathological Findings. J. Korean Med. Sci. 2021, 36, e286. [Google Scholar] [CrossRef] [PubMed]
- Larson, K.F.; Ammirati, E.; Adler, E.D.; Cooper, L.T., Jr.; Hong, K.N.; Saponara, G.; Couri, D.; Cereda, A.; Procopio, A.; Cavalotti, C.; et al. Myocarditis After BNT162b2 and mRNA-1273 Vaccination. Circulation 2021, 144, 506–508. [Google Scholar] [CrossRef] [PubMed]
- Mevorach, D.; Anis, E.; Cedar, N.; Bromberg, M.; Haas, E.J.; Nadir, E.; Olsha-Castell, S.; Arad, D.; Hasin, T.; Levi, N.; et al. Myocarditis after BNT162b2 mRNA Vaccine against COVID-19 in Israel. N. Engl. J. Med. 2021, 385, 2140–2149. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, J.; Ryan, M.; Engler, R.; Hoffman, D.; McClenathan, B.; Collins, L.; Loran, D.; Hrncir, D.; Herring, K.; Platzer, M.; et al. Myocarditis Following Immunization with mRNA COVID-19 Vaccines in Members of the US Military. JAMA Cardiol. 2021, 6, 1202. [Google Scholar] [CrossRef]
- Truong, D.T.; Dionne, A.; Muniz, J.C.; McHugh, K.E.; Portman, M.A.; Lambert, L.M.; Thacker, D.; Elias, M.D.; Li, J.S.; Toro-Salazar, O.H.; et al. Clinically Suspected Myocarditis Temporally Related to COVID-19 Vaccination in Adolescents and Young Adults: Suspected Myocarditis After COVID-19 Vaccination. Circulation 2022, 145, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Goulter, J.C.; Goddard, A.B.; Allen, M.J. ACE2 gene expression is up-regulated in the human failing heart. BMC Med. 2004, 2, 19. [Google Scholar] [CrossRef]
- Junapudi, S.S.; Junapudi, S.; Ega, K.; Chidipi, B. Major cardiac concerns in therapy and vaccinations for COVID-19. Metabol. Open 2021, 11, 100102. [Google Scholar] [CrossRef]
- Beyerstedt, S.; Casaro, E.B.; Rangel, É.B. COVID-19: Angiotensin-converting enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 905–919. [Google Scholar] [CrossRef]
- Azevedo, R.B.; Botelho, B.G.; de Hollanda, J.V.G.; Ferreira, L.V.L.; de Andrade, L.Z.J.; Oei, S.S.M.L.; Mello, T.D.S.; Muxfeldt, E.S. COVID-19 and the cardiovascular system: A comprehensive review. J. Hum. Hypertens. 2021, 35, 4–11. [Google Scholar] [CrossRef]
- Verdecchia, P.; Cavallini, C.; Spanevello, A.; Angeli, F. COVID-19: ACE2centric Infective Disease? Hypertension 2020, 76, 294–299. [Google Scholar] [CrossRef]
- Angeli, F.; Reboldi, G.; Verdecchia, P. SARS-CoV-2 infection and ACE2 inhibition. J. Hypertens. 2021, 39, 1555–1558. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, C.G.K.; Allon, S.J.; Nyquist, S.K.; Mbano, I.M.; Miao, V.N.; Tzouanas, C.N.; Cao, Y.; Yousif, A.S.; Bals, J.; Hauser, B.M.; et al. SARS-CoV-2 Receptor ACE2 Is an Interfer-on-Stimulated Gene in Human Airway Epithelial Cells and Is Detected in Specific Cell Subsets Across Tissues. Cell 2020, 181, 1016–1035.e19. [Google Scholar] [CrossRef] [PubMed]
- Glowacka, I.; Bertram, S.; Herzog, P.; Pfefferle, S.; Steffen, I.; Muench, M.O.; Simmons, G.; Hofmann, H.; Kuri, T.; Weber, F.; et al. Differential downregulation of ACE2 by the spike proteins of severe acute respiratory syndrome coronavirus and human coronavirus NL63. J. Virol. 2010, 84, 1198. [Google Scholar] [CrossRef]
- Angeli, F.; Reboldi, G.; Trapasso, M.; Zappa, M.; Spanevello, A.; Verdecchia, P. COVID-19, vaccines and deficiency of ACE2 and other angiotensinases. Closing the loop on the “Spike effect”. Eur. J. Intern. Med. 2022, 103, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Duckheim, M.; Schreieck, J. COVID-19 and Cardiac Arrhythmias. Hamostaseologie 2021, 41, 372–378. [Google Scholar] [CrossRef]
- Saha, S.A.; Russo, A.M.; Chung, M.K.; Deering, T.F.; Lakkireddy, D.; Gopinathannair, R. COVID-19 and Cardiac Arrhythmias: A Contemporary Review. Curr. Treat. Options Cardiovasc. Med. 2022, 24, 87–107. [Google Scholar] [CrossRef]
- Coromilas, E.J.; Kochav, S.; Goldenthal, I.; Biviano, A.; Garan, H.; Goldbarg, S.; Kim, J.-H.; Yeo, I.; Tracy, C.; Ayanian, S.; et al. Worldwide Survey of COVID-19–Associated Arrhythmias. Circ. Arrhythmia Electrophysiol. 2021, 14, e009458. [Google Scholar] [CrossRef]
- Jafari-Oori, M.; Moradian, S.T.; Ebadi, A.; Jafari, M.; Dehi, M. Incidence of cardiac complications following COVID-19 infection: An umbrella meta-analysis study. Heart Lung 2022, 52, 136–145. [Google Scholar] [CrossRef]
- Jakovac, H.; Ferenčić, A.; Stemberger, C.; Vitezić, B.M.; Cuculić, D. Detection of SARS-CoV-2 Antigens in the AV-Node of a Cardiac Conduction System—A Case Report. Trop. Med. Infect. Dis. 2022, 7, 43. [Google Scholar] [CrossRef]
- Dagher, L.; Wanna, B.; Mikdadi, G.; Young, M.; Sohns, C.; Marrouche, N.F. High-degree atrioventricular block in COVID-19 hospitalized patients. Europace 2021, 23, 451–455. [Google Scholar] [CrossRef]
- Varney, J.A.; Dong, V.S.; Tsao, T.; Sabir, M.S.; Rivera, A.T.; Ghula, S.; Moriles, K.E.; Cherukuri, M.L.; Fazal, R.; Azevedo, C.B.; et al. COVID-19 and arrhythmia: An overview. J. Cardiol. 2022, 79, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Daleau, P.; Turgeon, J. Angiotensin II modulates the delayed rectifier potassium current of guinea pig ventricular myocytes. Pflug. Arch. 1994, 427, 553–555. [Google Scholar] [CrossRef] [PubMed]
- Kass, R.; Blair, M. Effects of angiotensin II on membrane current in cardiac Purkinje fibers. J. Mol. Cell Cardiol. 1981, 13, 797–809. [Google Scholar] [CrossRef] [PubMed]
- Saito, K.; Gutkind, J.S.; Saavedra, J.M. Angiotensin II binding sites in the conduction system of rat hearts. Am. J. Physiol. Circ. Physiol. 1987, 253, H1618–H1622. [Google Scholar] [CrossRef] [PubMed]
- De Mello, W.C.; Crespo, M.J. Cardiac refractoriness in rats is reduced by angiotensin II. J. Cardiovasc. Pharmacol. 1995, 25, 51–56. [Google Scholar] [CrossRef]
- De Mello, W.C.; Altieri, P. The role of the renin-angiotensin system in the control of cell communication in the heart: Effects of en-alapril and angiotensin II. J. Cardiovasc. Pharmacol. 1992, 20, 643–651. [Google Scholar] [CrossRef]
- De Mello, W.C. Renin-Angiotensin System and Cell Communication in the Failing Heart. Hypertension 1996, 27, 1267–1272. [Google Scholar] [CrossRef]
- De Mello, W.C. Cardiac arrhythmias: The possible role of the renin-angiotensin system. J. Mol. Med. 2001, 79, 103–108. [Google Scholar] [CrossRef]
- Wit, A.L. Reentrant excitation in the ventricle. In Cardiac Electrophysiology; Rosen, M.R., Janse, M.J., Wtt, A.L., Eds.; Futura: New York, NY, USA, 1990; pp. 603–622. [Google Scholar]
- De Langen, C.D.J.; de Graeff, P.A.; van Gilst, W.H.; Bel, K.J.; Kingma, J.H.; Wesseling, H. Effects of angiotensin II and captopril on in-ducible sustained ventricular tachycardia two weeks after myocardial infarction in the pig. J. Cardiovasc. Pharmacol. 1989, 13, 186–191. [Google Scholar] [CrossRef]
- Zankov, D.P.; Omatsu-Kanbe, M.; Isono, T.; Toyoda, F.; Ding, W.-G.; Matsuura, H.; Horie, M. Angiotensin II Potentiates the Slow Component of Delayed Rectifier K+ Current via the AT1 Receptor in Guinea Pig Atrial Myocytes. Circulation 2006, 113, 1278–1286. [Google Scholar] [CrossRef]
- Gunasegaram, S.; Haworth, R.S.; Hearse, D.J.; Avkiran, M. Regulation of Sarcolemmal Na+/H+ Exchanger Activity by Angiotensin II in Adult Rat Ventricular Myocytes: Opposing actions via AT(1) versus AT(2) receptors. Circ. Res. 1999, 85, 919–930. [Google Scholar] [CrossRef]
- Wagner, S.; Dantz, C.; Flebbe, H.; Azizian, A.; Sag, C.M.; Engels, S.; Möllencamp, J.; Dybkova, N.; Islam, T.; Shah, A.M.; et al. NADPH oxidase 2 mediates angiotensin II-dependent cellular arrhythmias via PKA and CaMKII. J. Mol. Cell. Cardiol. 2014, 75, 206–215. [Google Scholar] [CrossRef]
- Sotoodehnia, N.; Li, G.; Johnson, C.O.; Lemaitre, R.N.; Rice, K.M.; Rea, T.D.; Siscovick, D.S. Genetic variation in angiotensin-converting enzyme–related pathways associated with sudden cardiac arrest risk. Heart Rhythm 2009, 6, 1306–1314. [Google Scholar] [CrossRef] [PubMed]
- Bracke, A.; De Hert, E.; De Bruyn, M.; Claesen, K.; Vliegen, G.; Vujkovic, A.; van Petersen, L.; De Winter, F.H.R.; Hotterbeekx, A.; Brosius, I.; et al. Proline-specific peptidase activities (DPP4, PRCP, FAP and PREP) in plasma of hospitalized COVID-19 pa-tients. Clin. Chim. Acta 2022, 531, 4–11. [Google Scholar] [CrossRef]
- Osman, I.O.; Melenotte, C.; Brouqui, P.; Million, M.; Lagier, J.-C.; Parola, P.; Stein, A.; La Scola, B.; Meddeb, L.; Mege, J.-L.; et al. Expression of ACE2, Soluble ACE2, Angiotensin I, Angiotensin II and Angiotensin-(1-7) Is Modulated in COVID-19 Patients. Front. Immunol. 2021, 12, 625732. [Google Scholar] [CrossRef]
- Teijaro, J.R.; Farber, D.L. COVID-19 vaccines: Modes of immune activation and future challenges. Nat. Rev. Immunol. 2021, 21, 195–197. [Google Scholar] [CrossRef]
- Heinz, F.X.; Stiasny, K. Distinguishing features of current COVID-19 vaccines: Knowns and unknowns of antigen presentation and modes of action. NPJ Vaccines 2021, 6, 104. [Google Scholar] [CrossRef] [PubMed]
- Murphy, W.J.; Longo, D.L. A Possible Role for Anti-idiotype Antibodies in SARS-CoV-2 Infection and Vaccination. N. Engl. J. Med. 2022, 386, 394–396. [Google Scholar] [CrossRef] [PubMed]
- Xue, W.; Orten, D.; Abdelmagid, O.; Rider, M.; Blecha, F.; Minocha, H. Anti-idiotypic antibodies mimic bovine viral diarrhea virus antigen. Vet. Microbiol. 1991, 29, 201–212. [Google Scholar] [CrossRef]
- Paque, R.E.; Miller, R. Autoanti-idiotypes exhibit mimicry of myocyte antigens in virus-induced myocarditis. J. Virol. 1991, 65, 16–22. [Google Scholar] [CrossRef]
- Rodriguez-Perez, A.I.; Labandeira, C.M.; Pedrosa, M.A.; Valenzuela, R.; Suarez-Quintanilla, J.A.; Cortes-Ayaso, M.; Mayán-Conesa, P.; Labandeira-Garcia, J.L. Autoantibodies against ACE2 and angiotensin type-1 receptors increase severity of COVID-19. J. Autoimmun. 2021, 122, 102683. [Google Scholar] [CrossRef] [PubMed]
- Arthur, J.M.; Forrest, J.C.; Boehme, K.W.; Kennedy, J.L.; Owens, S.; Herzog, C.; Liu, J.; Harville, T.O. Development of ACE2 autoantibodies after SARS-CoV-2 infection. PLoS ONE 2021, 16, e0257016. [Google Scholar] [CrossRef] [PubMed]
- Stefanou, M.I.; Karachaliou, E.; Chondrogianni, M.; Moschovos, C.; Bakola, E.; Foska, A.; Melanis, K.; Andreadou, E.; Voumvourakis, K.; Papathanasiou, M.; et al. Guillain-Barré syndrome and fulminant encephalomyelitis following Ad26.COV2.S vaccination: Double jeopardy. Neurol. Res. Pract. 2022, 4, 6. [Google Scholar] [CrossRef] [PubMed]
- Donoghue, M.; Wakimoto, H.; Maguire, C.T.; Acton, S.; Hales, P.; Stagliano, N.; Fairchild-Huntress, V.; Xu, J.; Lorenz, J.N.; Kadambi, V.; et al. Heart block, ventricular tachycardia, and sudden death in ACE2 transgenic mice with downregulated connexins. J. Mol. Cell Cardiol. 2003, 35, 1043–1053. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.K.; Juno, J.A.; Lee, W.S.; Wragg, K.M.; Hogarth, P.M.; Kent, S.J.; Burrell, L.M. Plasma ACE2 activity is persistently elevated following SARS-CoV-2 infection: Implications for COVID-19 pathogenesis and consequences. Eur. Respir. J. 2021, 57, 2003730. [Google Scholar] [CrossRef]
- Kaur, G.; Yogeswaran, S.; Muthumalage, T.; Rahman, I. Persistently Increased Systemic ACE2 Activity Is Associated with an Increased Inflammatory Response in Smokers with COVID-19. Front. Physiol. 2021, 12, 653045. [Google Scholar] [CrossRef]
- Ramchand, J.; Burrell, L.M. Circulating ACE2: A novel biomarker of cardiovascular risk. Lancet 2020, 396, 937–939. [Google Scholar] [CrossRef]
- Al Banna, R.; Husain, A.; Al-Ghamdi, B. Ventricular arrhythmia and tachycardia-induced cardiomyopathy in Gitelman syndrome, hypokalaemia is not the only culpable. BMJ Case Rep. 2019, 12, e232086. [Google Scholar] [CrossRef]
- Pachulski, R.T.; Lopez, F.; Sharaf, R. Gitelman’s Not-So-Benign Syndrome. N. Engl. J. Med. 2005, 353, 850–851. [Google Scholar] [CrossRef]
- Calò, L.A.; Rigato, M.; Sgarabotto, L.; Gianesello, L.; Bertoldi, G.; Ravarotto, V.; Davis, P.A. ACE2 and SARS-CoV-2 Infection Risk: Insights From Patients with Two Rare Genetic Tubulopathies, Gitelman’s and Bartter’s Syndromes. Front. Med. 2021, 8, 647319. [Google Scholar] [CrossRef]
- Jansson, K.; Dahlstrom, U.; Karlberg, B.E.; Karlsson, E.; Nylander, E.; Nyquist, O. The circulating renin-angiotensin system during treatment with metoprolol or captopril in patients with heart failure due to non-ischaemic dilated cardiomyopathy. J. Intern. Med. 1999, 245, 435–443. [Google Scholar] [CrossRef]
- Fung, J.W.; Yu, C.M.; Yip, G.; Chan, S.; Yandle, T.G.; Richards, A.; Nicholls, M.; Sanderson, J.E. Effect of beta blockade (carvedilol or metoprolol) on activation of the renin-angiotensin-aldosterone system and natriuretic peptides in chronic heart failure. Am. J. Cardiol. 2003, 92, 406–410. [Google Scholar] [CrossRef] [PubMed]
- Theoharides, T.C.; Conti, P. Be aware of SARS-CoV-2 spike protein: There is more than meets the eye. J. Biol. Regul. Homeost. Agents 2021, 35, 833–838. [Google Scholar] [CrossRef] [PubMed]
- Trougakos, I.P.; Terpos, E.; Alexopoulos, H.; Politou, M.; Paraskevis, D.; Scorilas, A.; Kastritis, E.; Andreakos, E.; Dimopoulos, M.A. Adverse effects of COVID-19 mRNA vaccines: The spike hypothesis. Trends Mol. Med. 2022, 28, 542–554. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cocco, N.; Leibundgut, G.; Pelliccia, F.; Cammalleri, V.; Nusca, A.; Mangiacapra, F.; Cocco, G.; Fanale, V.; Ussia, G.P.; Grigioni, F. Arrhythmias after COVID-19 Vaccination: Have We Left All Stones Unturned? Int. J. Mol. Sci. 2023, 24, 10405. https://doi.org/10.3390/ijms241210405
Cocco N, Leibundgut G, Pelliccia F, Cammalleri V, Nusca A, Mangiacapra F, Cocco G, Fanale V, Ussia GP, Grigioni F. Arrhythmias after COVID-19 Vaccination: Have We Left All Stones Unturned? International Journal of Molecular Sciences. 2023; 24(12):10405. https://doi.org/10.3390/ijms241210405
Chicago/Turabian StyleCocco, Nino, Gregor Leibundgut, Francesco Pelliccia, Valeria Cammalleri, Annunziata Nusca, Fabio Mangiacapra, Giulio Cocco, Valerio Fanale, Gian Paolo Ussia, and Francesco Grigioni. 2023. "Arrhythmias after COVID-19 Vaccination: Have We Left All Stones Unturned?" International Journal of Molecular Sciences 24, no. 12: 10405. https://doi.org/10.3390/ijms241210405
APA StyleCocco, N., Leibundgut, G., Pelliccia, F., Cammalleri, V., Nusca, A., Mangiacapra, F., Cocco, G., Fanale, V., Ussia, G. P., & Grigioni, F. (2023). Arrhythmias after COVID-19 Vaccination: Have We Left All Stones Unturned? International Journal of Molecular Sciences, 24(12), 10405. https://doi.org/10.3390/ijms241210405










