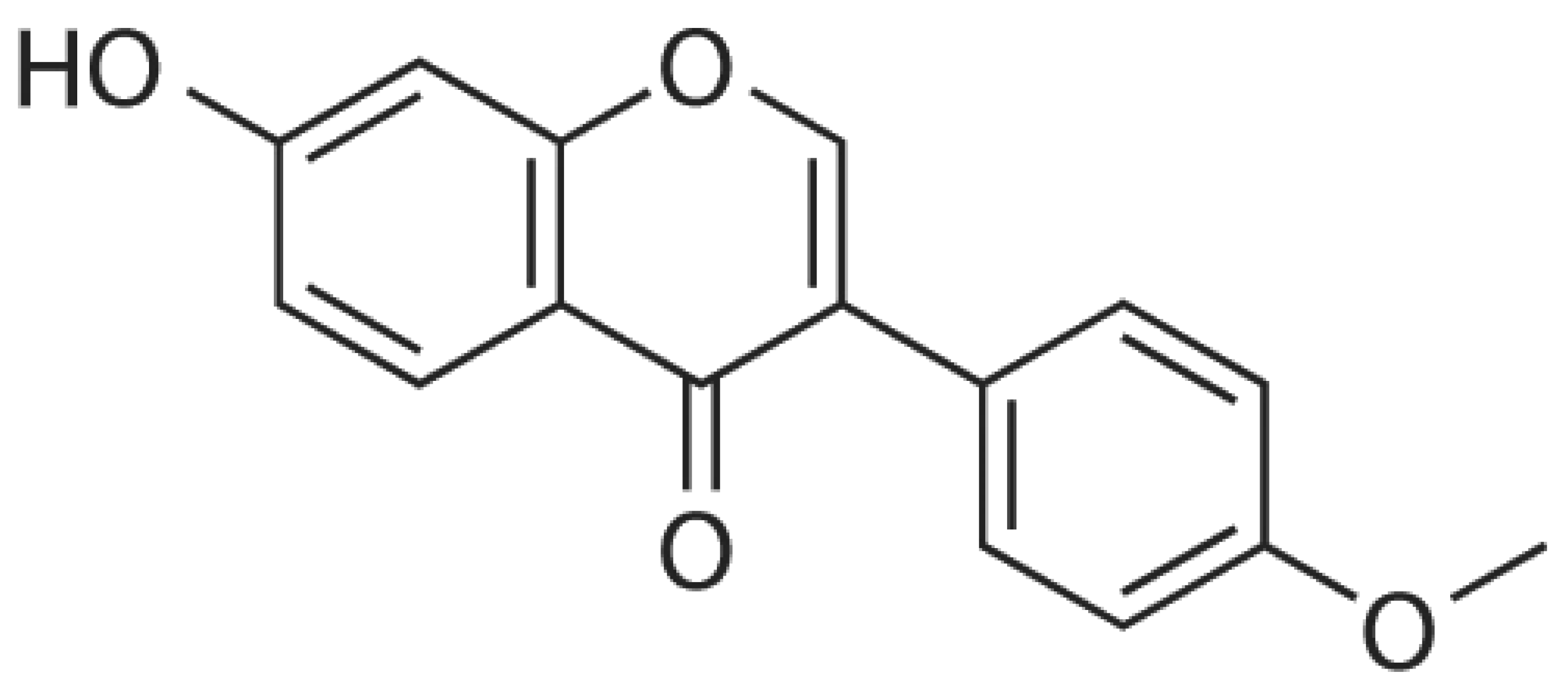
Potential Therapeutic Targets of Formononetin, a Type of Methoxylated Isoflavone, and Its Role in Cancer Therapy through the Modulation of Signal Transduction Pathways
Abstract
1. Introduction
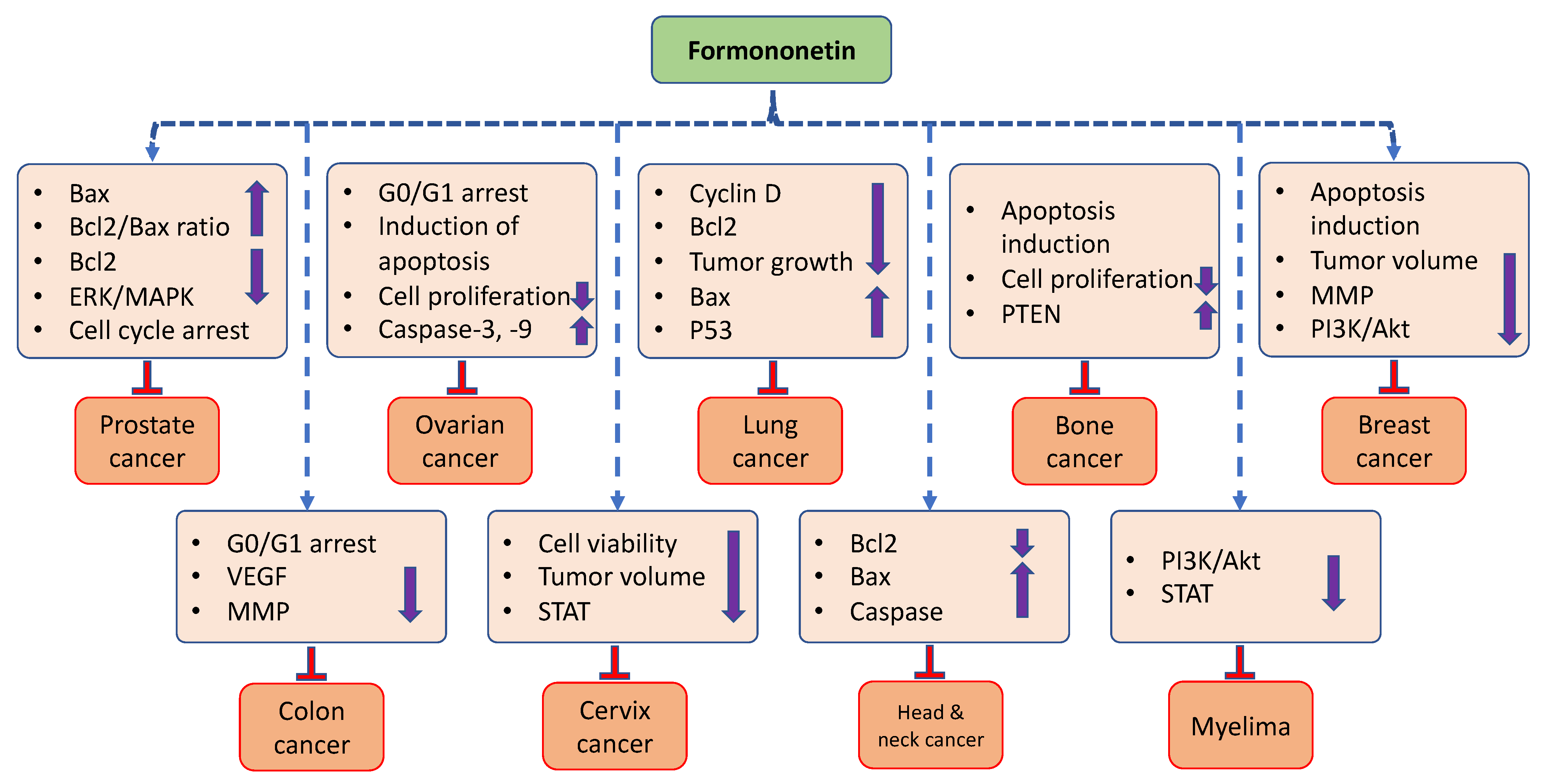
2. Mechanism of Action of Formononetin
2.1. Effect of Formononetin on Cellular Processes
2.1.1. Cell Cycle
2.1.2. Apoptosis
2.1.3. Angiogenesis
2.1.4. Inflammation
2.2. Effect of Formononetin on Cell Signaling Pathways
2.2.1. P38 MAPK Signaling Pathway
2.2.2. PI3K/Akt Signaling Pathway
2.2.3. Tumor Suppressor Gene
2.2.4. Signal Transducer and Activator of Transcription 3 (STAT3)
| Cellular Processes/ Molecular Signaling Pathways | Cancer | Cell Lines | Mechanism/Outcome of the Study | Refs. |
|---|---|---|---|---|
| Cell cycle | Prostate cancer | PC-3 and DU-145 | It prevented cancer cell proliferation by initiating cell cycle capture at the G0/G1 phase | [8] |
| Breast cancer | MCF-7 | It had a role in cell cycle arrest at the G0/G1 phase | [9] | |
| Lung cancer | A549 and NCI-H23 | This compound induced G1-phase cell cycle arrest | [10] | |
| Colon cancer | SW1116 and HCT116 | The proportion of cells in the G0–G1 stage increased with formononetin treatment (20, 50, and 100 µM concentration) | [11] | |
| Apoptosis | Prostate cancer | DU-145 | Formononetin inhibited the levels of Bcl-2 protein and caused the induction of the activation of RASD1 as well as Bax in a dose-dependent way | [13] |
| PC-3 | The treatment contributed to an elevated Bax expression and reduced Bcl-2 protein level | [14] | ||
| Bone cancer | U2SO | Higher concentrations significantly reduced Bcl-2 expression in comparison to the control group | [15] | |
| U2OS | It inhibited the growth of human osteosarcoma cells by inducing apoptosis | [16] | ||
| Prostate cancer | LNCaP and PC-3 | The ERK1/2 MAPK signaling pathway was inactivated, which elevated the expression of Bcl-2-associated X (Bax) mRNA | [17] | |
| PC-3 | This compound decreased the expression levels of the pIGF-1 R protein as well as increasing Bax mRNA | [18] | ||
| Angiogenesis | Colon cancer | HCT-116 | Colon cancer cells treated with formononetin showed a decreased expression of the VEGF gene and protein | [19] |
| Inflammation | Multiple myeloma | U266 | TNF-α, TGF-β1, IL-6, and IL-8 were upregulated in response to hypoxia, but formononetin prevented this | [28] |
| p38/Akt | Prostate cancer | PC-3 | This compound showed an anticarcinogenic effect, with potential mechanisms leading to the elevation of the Bax/Bcl-2 ratio | [14] |
| MAPK | Nasopharyngeal cancer | CNE1 | The mitochondrial apoptotic pathway may be regulated by the PI3K/Akt and MAPK cascades, which would facilitate the anticancer impacts of formononetin | [34] |
| PI3K/Akt | Breast cancer | MDA-MB-231 and 4T1 | By reducing the expression of MMP-2,9 via the PI3K/AKT signaling pathway, formononetin reduced both the migration and invasion of cancer cells | [35] |
| Colon cancer | SW1116, and HCT116 | The treatment significantly decreased p-PI3K and p-AKT protein expressions | [11] | |
| Breast cancer | MCF-7 | By deactivating the IGF1/IGF1R-PI3K/Akt pathways, formononetin demonstrated a role in cell cycle arrest | [9] | |
| PTEN | Bladder cancer | T24 | miR-21 expression was significantly reduced and this was followed by an increase in PTEN and a decrease in p-Akt | [39] |
| Bone cancer | MG-63 | Formononetin increased PTEN expression, reduced miR-214-3p levels, and decreased cell viability while promoting apoptosis | [40] | |
| p53 | Lung cancer | A549 | Expression level of p53 was upregulated when cells wereexposed to formononetin | [10] |
| Signal transducer and activator of transcription 3 (STAT3) | Multiple myeloma | U266 | Both constitutive p-STAT3 (Tyr705) and p-STAT3 (Ser727) levels were substantially reduced upon FT treatment | [45] |
| Colon cancer | W1116 and HCT116 | Suppressive potential of formononetin on colon carcinoma cell proliferation and invasion was noticed, including the inhibition of PI3K/AKT as well as STAT3 signaling pathways | [11] |
2.2.5. MMPs Role in Cancer Development
2.2.6. Epidermal Growth Factor Receptor
3. Role of Formononetin in Different Type of Cancers
3.1. Prostate Cancer
3.2. Breast Cancer
3.3. Cervix Cancer
3.4. Ovarian Cancer
3.5. Osteosarcoma
3.6. Urinary Bladder Cancer
3.7. Head and Neck Cancer
3.8. Lung Cancer
3.9. Brain Cancer
3.10. Myeloma
3.11. Colon Cancer
3.12. Gastric Cancer
| Cancer | Findings of the Study | Refs. |
|---|---|---|
| Prostate cancer | It inhibits the proliferation of LNCaP and PC-3 cells, whereas the most prominent effect was seen in LNCaP cells. | [17] |
| Formononetin treatment contributed to increased Bax and reduced Bcl-2 protein level expressions in PC-3 cells, in that way resulting in the increasing Bcl-2/Bax ratio. | [14] | |
| It meaningfully inhibited the viability of PC-3 cells and indorsed apoptosis, and expressions of lncRNA, H19, and Bcl-2 were downregulated. | [57] | |
| Formononetin showed inhibitory activity against cancer cells in vivo and in vitro, which is connected to G1 cell cycle arrest by the inactivation of Akt/cyclin D1/CDK4. | [8] | |
| Breast cancer | The combination therapy of formononetin and Taxol was found to be more effective in inhibiting drug resistance and autophagy. | [59] |
| This compound increased the efficacy of everolimus in suppressing breast cancer cell growth. The combination of formononetin and everolimus decreased tumor volume and cell survival. | [61] | |
| Migration and invasion of MDA-MB-231 and 4T1 cells were suppressed. Furthermore, formononetin reduced the expressions of MMP-2, MMP-9, and increased the expression of the tissue inhibitor of metalloproteinase-1 (TIMP-1) and TIMP-2. | [35] | |
| It meaningfully decreased expressions of lncRNA AFAP1-AS1, CDK4, and Raf-1, whereas it increased miR-195 and miR-545 expressions in TNBC cells. | [62] | |
| Cervix cancer | It played a role in the inhibition of the phosphorylation of AKT as well as presented apoptosis in a dose-dependent way. Additionally, formononetin decreased xenograft tumor growth in nude mice. | [65] |
| This compound increased the activity of cytotoxic T lymphocytes as well as re-established their capability to kill tumor cells in a co-culture system of T cells as well as tumor cells. | [44] | |
| Ovarian cancer | It reduced cell proliferation via sub G0/G1-phase capture and encouraged the loss of mitochondrial membrane potential as well as the generation of reactive oxygen species. | [66] |
| It suppressed cell proliferation via the induction of apoptosis and reduced expression of MMP-2/9 proteins, as well as the phosphorylation level of ERK. | [67] | |
| Bone cancer | This compound meaningfully inhibited the growth of cancer cells and caused an increase in the number of apoptotic cells. | [15] |
| It reduced cell viability and caused apoptosis via regulating miR-214-3p. FN acted as a new treatment for MG-63 cells through enhancing the PTEN level via preventing the increase in miR-214-3p level. | [40] | |
| This compound activated the apoptosis of cancer cells, and treatment with this compound led to the inactivation of ERK as well as Akt. | [16] | |
| Urinary bladder cancer | It meaningfully prevented the proliferation of bladder cancer in a time- and dose-dependent fashion. | [39] |
| Head and neck cancer | This compound initiated cancer cell death and involved death receptor-facilitated extrinsic as well as mitochondria-dependent intrinsic apoptotic pathways. | [70] |
| Lung cancer | The treatment promoted cell apoptosis and induced G1-phase cell cycle arrest. | [10] |
| It suppressed WT and mutant epidermal growth factor receptor (EGFR) kinase activity. Treatment with formononetin enhanced the interaction between Mcl-1 as well as SCFFbw7, which ultimately encouraged Mcl-1 ubiquitination and degradation. | [54] | |
| Brain cancer | Combination treatment with formononetin reversed the doxorubicin-induced epithelial–mesenchymal transition in tumor cells. | [72] |
| Myeloma | The treatment reduced the levels of diverse tumorigenic proteins participating in myeloma progression. Remarkably, it was noted that formononetin blocked persistent PI3K/AKT, NF-κB, and AP-1 activations. | [73] |
| It persuaded cell cycle arrest, decreased the expression of STAT3-regulated anti-apoptotic as well as angiogenetic gene products. | [45] | |
| Colon cancer | Proliferation and invasion of colon carcinoma cell lines was significantly inhibited. | [11] |
| It inhibited cancer cell proliferation and played a role in the induction of apoptosis. Moreover, formononetin lowered Bcl-2 protein expression and ERK1/2 phosphorylated level and upregulated Bax mRNA expression. | [74] | |
| Gastric cancer | This compound evidently inhibited the migratory capabilities of cancer cells, and this compound dose-dependently controlled the invasion of gastric cancer cells in vitro. | [75] |
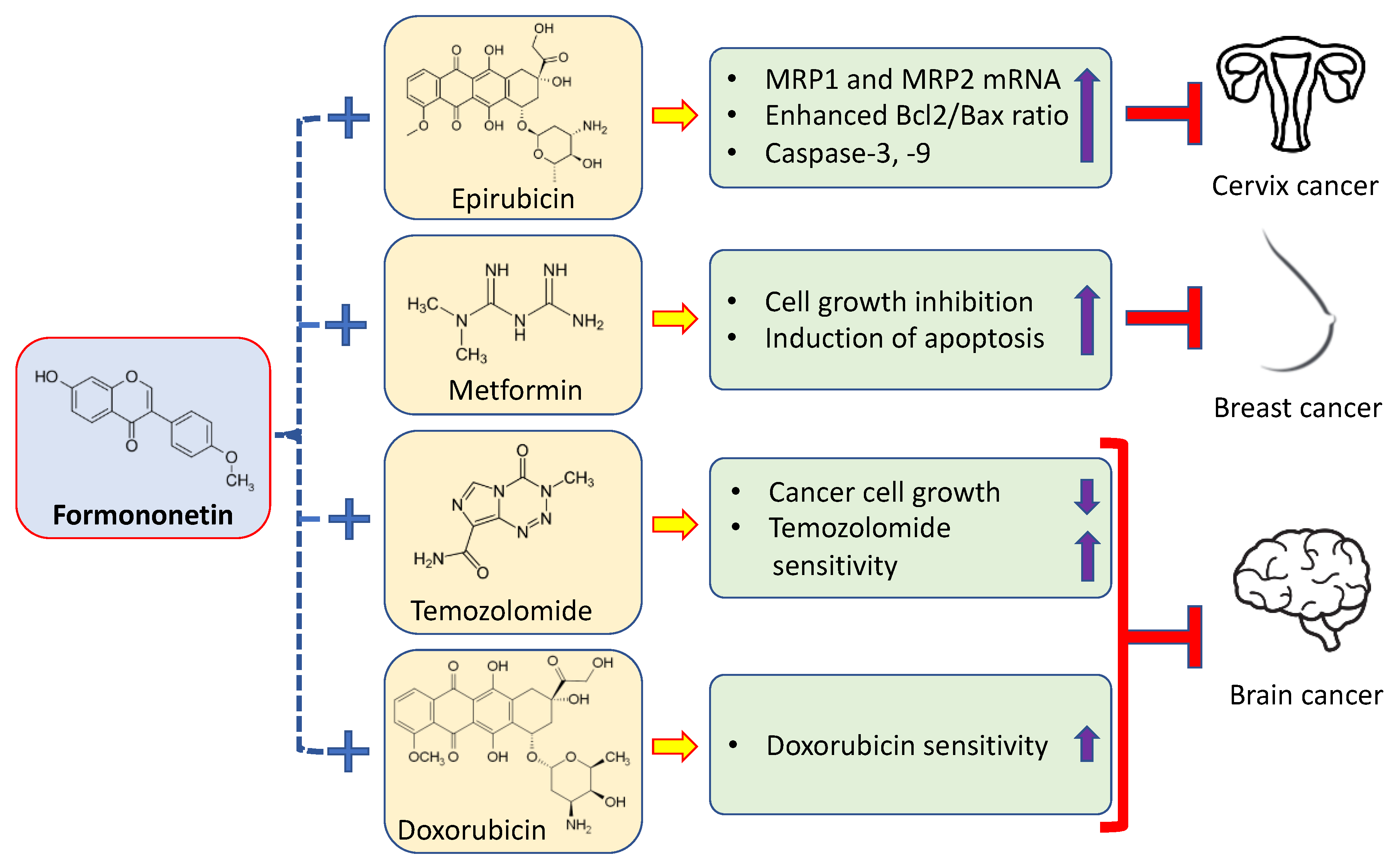
4. Synergistic Effects of Formononetin with Anticancer Drugs
| Cancer | Formononetin + Anticancer Drugs/Compounds | Findings | Refs. |
|---|---|---|---|
| Cervix cancer | Formononetin + epirubicin | Formononetin significantly enhanced the cytotoxicity of epirubicin. Moreover, the co-incubation of epirubicin with formononetin increased ROS levels, including hydrogen peroxide and superoxide free radicals. | [77] |
| Breast cancer | Formononetin + metformin | The combination use of metformin and formononetin increased cell growth inhibition and induced apoptosis in MCF-7 cells mediated via the ERK1/2 signaling pathway. | [78] |
| Brain cancer | Formononetin + doxorubicin | Doxorubicin sensitivity was enhanced in glioma cells after co-administration with formononetin. | [72] |
| Formononetin + Temozolomide | Formononetin or temozolomide alone inhibited the growth of C6 glioma cells in a dose-dependent way and formononetin in combination with temozolomide had a synergistic effect on C6 cells. Combination drugs decreased the expression. | [79] | |
| Formononetin and calycosin + temozolomide | Formononetin and calycosin (FMN/CAL) increased the inhibition of temozolomide on the growth as well as infiltration of C6 glioma. | [80] |
5. Pharmacokinetics, Bioavailability, and Approaches to Improve Formononetin Delivery
| Derivatives/Nano Formulation | Outcome of the Study | Refs. |
|---|---|---|
| Formononetin–dithiocarbamate derivatives | Derivatives might inhibit cell growth through MAPK signaling pathway as well as the inhibition of migration through the Wnt pathway in PC-3 cells | [92] |
| Formononetin nitrogen mustard derivatives | The results show that several of the innovative derivatives show greater cytotoxicity than alkeran | [93] |
| Multi-walled carbon nanotube–formononetin | Formononetin (FMN) and multiwalled carbon nanotube– formononetin (MWCNT-FMN) can induce apoptosis in HeLa cells; in the meantime, the cells display an effective reactive oxygen species signal | [95] |
| FN-containing vitamin-E d-α-tocopheryl polyethylene glycol 1000 succinate | Formononetin micelles improve the cellular uptake and enhance cell cytotoxicity compared to free formononetin | [96] |
| Formononetin-2-hydroxypropyl-β-cyclodextrin inclusion complex-loaded PLGA nanoparticles | The in vitro cytotoxicity shows that formononetin-2-HPβ-CD-NP displays anticancer activity in MCF-7 and Hela tumor cells compared to free formononetin | [99] |
| Hydroxypropyl-β-cyclodextrin (HP-β-CD) modified carboxylated single-walled carbon nanotubes | Antitumor activity of carboxylated single-walled carbon nanotube (CD-SWCNTs)–FMN is stronger than that of free formononetin | [100] |
6. Safety and Toxicity of Formononetin
7. Clinical Trials of Formononetin
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.M.; Wolchok, J.D.; Old, L.J. Antibody therapy of cancer. Nat. Rev. Cancer 2012, 12, 278–287. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.P.; Wahajuddin, Y.D.K.; Rawat, P.; Maurya, R.; Jain, G.K. Quantitative determination of formononetin and its metabolite in rat plasma after intravenous bolus administration by HPLC coupled with tandem mass spectrometry. J. Chromatogr. B Analyt. Technol. Biomed Life Sci. 2010, 878, 391–397. [Google Scholar] [CrossRef]
- Jiang, D.; Rasul, A.; Batool, R.; Sarfraz, I.; Hussain, G.; Mateen Tahir, M.; Qin, T.; Selamoglu, Z.; Ali, M.; Li, J.; et al. Potential anticancer properties and mechanisms of action of formononetin. Biomed Res. Int. 2019, 2019, 5854315. [Google Scholar] [CrossRef]
- Li, X.; Huang, C.; Sui, C.L.; Liang, C.M.; Qi, G.Y.; Ren, Q.Y.; Chen, J.; Huang, Z.Q. Formononetin, J1 and J2 have different effects on endothelial cells via EWSAT1 TRAF6 and its downstream pathway. J. Cell. Mol. Med. 2020, 24, 875–885. [Google Scholar] [CrossRef]
- Ong, S.K.L.; Shanmugam, M.K.; Fan, L.; Fraser, S.E.; Arfuso, F.; Ahn, K.S.; Sethi, G.; Bishayee, A. Focus on Formononetin: Anticancer Potential and Molecular Targets. Cancers 2019, 11, 611. [Google Scholar] [CrossRef] [PubMed]
- Tay, K.C.; Tan, L.T.; Chan, C.K.; Hong, S.L.; Chan, K.G.; Yap, W.H.; Pusparajah, P.; Lee, L.H.; Goh, B.H. Formononetin: A Review of Its Anticancer Potentials and Mechanisms. Front. Pharmacol. 2019, 10, 820. [Google Scholar] [CrossRef]
- Li, T.; Zhao, X.; Mo, Z.; Huang, W.; Yan, H.; Ling, Z.; Ye, Y. Formononetin promotes cell cycle arrest via downregulation of Akt/Cyclin D1/CDK4 in human prostate cancer cells. Cell. Physiol. Biochem. 2014, 34, 1351–1358. [Google Scholar] [CrossRef]
- Chen, J.; Zeng, J.; Xin, M.; Huang, W.; Chen, X. Formononetin induces cell cycle arrest of human breast cancer cells via IGF1/PI3K/Akt pathways in vitro and in vivo. Horm. Metab. Res. 2011, 43, 681–686. [Google Scholar] [CrossRef]
- Yang, Y.; Zhao, Y.; Ai, X.; Cheng, B.; Lu, S. Formononetin suppresses the proliferation of human non-small cell lung cancer through induction of cell cycle arrest and apoptosis. Int. J. Clin. Exp. Pathol. 2014, 7, 8453–8461. [Google Scholar]
- Wang, A.; Li, Y.; Zhao, Q.; Fan, L. Formononetin inhibits colon carcinoma cell growth and invasion by microRNA-149-mediated EphB3 downregulation and inhibition of PI3K/AKT and STAT3 signaling pathways. Mol. Med. Rep. 2018, 17, 7721–7729. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Wu, X.; Tang, J.; Xiao, N.; Zhao, G.; Zhang, L.; Ou, L. In vitro and in vivo studies of antiosteosarcoma activities of formononetin. J. Cell. Physiol. 2019, 234, 17305–17313. [Google Scholar] [CrossRef]
- Liu, X.-J.; Li, Y.-Q.; Chen, Q.-Y.; Xiao, S.-J.; Zeng, S.-E. Up-regulating of RASD1 and Apoptosis of DU-145 Human Prostate Cancer Cells Induced by Formononetin in Vitro. Asian Pac. J. Cancer Prev. 2014, 15, 2835–2839. [Google Scholar] [CrossRef]
- Zhang, X.; Bi, L.; Ye, Y.; Chen, J. Formononetin induces apoptosis in PC-3 prostate cancer cells through enhancing the Bax/Bcl-2 ratios and regulating the p38/Akt pathway. Nutr. Cancer 2014, 66, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Xiao, Z. Formononetin Induces Apoptosis of Human Osteosarcoma Cell Line U2OS by Regulating the Expression of Bcl-2, Bax and MiR-375 In Vitro and In Vivo. Cell. Physiol. Biochem. 2015, 37, 933–939. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; He, J.; Chen, X.; Li, J.; Shen, M.; Yu, W.; Yang, Y.; Xiao, Z. The Proapoptotic Effect of Formononetin in Human Osteosarcoma Cells: Involvement of Inactivation of ERK and Akt Pathways. Cell. Physiol. Biochem. 2014, 34, 637–645. [Google Scholar] [CrossRef]
- Ye, Y.; Hou, R.; Chen, J.; Mo, L.; Zhang, J.; Huang, Y.; Mo, Z. Formononetin-induced apoptosis of human prostate cancer cells through ERK1/2 mitogen-activated protein kinase inactivation. Horm. Metab. Res. 2012, 44, 263–267. [Google Scholar] [CrossRef]
- Huang, W.J.; Bi, L.Y.; Li, Z.Z.; Zhang, X.; Ye, Y. Formononetin induces the mitochondrial apoptosis pathway in prostate cancer cells via downregulation of the IGF-1/IGF-1R signaling pathway. Pharm. Biol. 2013, 52, 466–470. [Google Scholar] [CrossRef]
- Auyeung, K.K.; Law, P.; Ko, J.K. Novel anti-angiogenic effects of formononetin in human colon cancer cells and tumor xenograft. Oncol. Rep. 2012, 28, 2188–2194. [Google Scholar] [CrossRef]
- Wu, X.Y.; Xu, H.; Wu, Z.F.; Chen, C.; Liu, J.Y.; Wu, G.N.; Yao, X.Q.; Liu, F.K.; Li, G.; Shen, L. Formononetin, a novel FGFR2 inhibitor, potently inhibits angiogenesis and tumor growth in preclinical models. Oncotarget 2015, 6, 44563–44578. [Google Scholar] [CrossRef]
- Balkwill, F.; Mantovani, A. Inflammation and cancer: Back to Virchow? Lancet 2002, 357, 539–545. [Google Scholar] [CrossRef] [PubMed]
- de Visser, K.E.; Eichten, A.; Coussens, L.M. Paradoxical roles of the immune system during cancer development. Nat. Rev. Cancer 2006, 6, 24–37. [Google Scholar] [CrossRef] [PubMed]
- Hardbower, D.M.; Peek, R.M., Jr.; Wilson, K.T. At the bench: Helicobacter pylori, dysregulated host responses, DNA damage, and gastric cancer. J. Leukoc. Biol. 2014, 96, 201–212. [Google Scholar] [CrossRef] [PubMed]
- Maeda, H.; Akaike, T. Nitric oxide and oxygen radicals in infection, inflammation, and cancer. Biochemistry 1998, 63, 854–865. [Google Scholar]
- Pollard, J.W. Tumour-educated macrophages promote tumour progression and metastasis. Nat. Rev. Cancer 2004, 4, 71–78. [Google Scholar] [CrossRef]
- Hussain, S.P.; Harris, C.C. Inflammation and cancer: An ancient link with novel potentials. Int. J. Cancer 2007, 121, 2373–2380. [Google Scholar] [CrossRef]
- Wang, Y.; Zhu, Y.; Gao, L.; Yin, H.; Xie, Z.; Wang, D.; Zhu, Z.; Han, X. Formononetin attenuates il-1beta-induced apoptosis and NF-κB activation in ins-1 cells. Molecules 2012, 17, 10052–10064. [Google Scholar] [CrossRef]
- Xing, Z.F.; Wang, G.H.; Liu, J.; Chen, B.H. Formononetin suppresses hypoxia inducible factor-1α/inflammatory cytokines expression via inhibiting Akt signal pathway in multiple myeloma cells. Int. J. Clin. Exp. Med. 2016, 9, 1117–1127. [Google Scholar]
- Plotnikov, A.; Flores, K.; Maik-Rachline, G.; Zehorai, E.; Kapri-Pardes, E.; Berti, D.A.; Hanoch, T.; Besser, M.J.; Seger, R. The nuclear translocation of ERK1/2 as an anticancer target. Nat. Commun. 2015, 6, 6685. [Google Scholar] [CrossRef]
- Koul, H.K.; Pal, M.; Koul, S. Role of p38 MAP kinase signal transduction in solid tumors. Genes Cancer 2013, 4, 342–359. [Google Scholar] [CrossRef]
- Burotto, M.; Chiou, V.L.; Lee, J.; Kohn, E.C. The MAPK pathway across different malignancies: A new perspective. Cancer 2014, 120, 3446–3456. [Google Scholar] [CrossRef]
- Bhowmick, N.A.; Ghiassi, M.; Bakin, A.; Aakre, M.; Lundquist, C.A.; Engel, M.E.; Arteaga, C.L.; Moses, H.L. Transforming growth factor-beta1 mediates epithelial to mesenchymal transdifferentiation through a RhoA-dependent mechanism. Mol. Biol. Cell. 2001, 12, 27–36. [Google Scholar] [CrossRef]
- Bhowmick, N.A.; Zent, R.; Ghiassi, M.; McDonnell, M.; Moses, H.L. Integrin beta 1 signaling is necessary for transforming growth factor-beta activation of p38MAPK and epithelial plasticity. J. Biol. Chem. 2001, 276, 46707–46713. [Google Scholar] [CrossRef] [PubMed]
- Qi, C.; Xie, M.; Liang, J.; Li, H.; Li, Z.; Shi, S.; Yang, X.; Wang, Z.; Tang, X. Formononetin targets the MAPK and PI3K/Akt pathways to induce apoptosis in human nasopharyngeal carcinoma cells in vitro and in vivo. Int. J. Clin. Exp. Med. 2016, 9, 1180–1189. [Google Scholar]
- Zhou, R.; Xu, L.; Ye, M.; Liao, M.; Du, H.; Chen, H. Formononetin inhibits migration and invasion of MDA-MB-231 and 4T1 breast cancer cells by suppressing MMP-2 and MMP-9 through PI3K/AKT signaling pathways. Horm. Metab. Res. 2014, 46, 753–760. [Google Scholar] [CrossRef] [PubMed]
- Masson, G.R.; Williams, R.L. Structural Mechanisms of PTEN Regulation. Cold Spring Harb. Perspect. Med. 2020, 10, a036152. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.; Jerah, A.B.; Ashraf, A.M.; Kumaresan, K.; Eisa, Z.M. Promoter methylation and loss of expression of PTEN gene in breast cancer patients from Saudi population. J. Clin. Exp. Oncol. 2017, 6, 2. [Google Scholar]
- Rizvi, M.M.; Alam, M.S.; Ali, A.; Mehdi, S.J.; Batra, S.; Mandal, A.K. Aberrant promoter methylation and inactivation of PTEN gene in cervical carcinoma from Indian population. J. Cancer Res. Clin. Oncol. 2011, 137, 1255–1262. [Google Scholar] [CrossRef]
- Wu, Y.; Zhang, X.; Li, Z.; Yan, H.; Qin, J.; Li, T. Formononetin inhibits human bladder cancer cell proliferation and invasiveness via regulation of miR-21 and PTEN. Food Funct. 2017, 8, 1061–1066. [Google Scholar] [CrossRef]
- Li, K.; Shen, H.; Lu, M.; Chen, J.; Yin, Q.; Li, P. Formononetin inhibits osteosarcoma cell proliferation and promotes apoptosis by regulating the miR-214-3p/phosphatase and tensin homolog pathway. Transl. Cancer Res. 2020, 9, 4914–4921. [Google Scholar] [CrossRef]
- Kiu, H.; Nicholson, S.E. Biology and significance of the JAK/STAT signalling pathways. Growth Factors 2012, 30, 88–106. [Google Scholar] [CrossRef]
- Vigneswara, V.; Kundi, S.; Ahmed, Z. Receptor tyrosine kinases: Molecular switches regulating CNS axon regeneration. J. Signal Transduct. 2012, 2012, 361721. [Google Scholar] [CrossRef] [PubMed]
- Lohi, O.; Lehto, V.-P. STAM/EAST/Hbp adapter proteins–integrators of signalling pathways. FEBS Lett. 2001, 508, 287–290. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.Y.; Jiang, M.W.; Li, M.Y.; Zhang, Z.H.; Xing, Y.; Ri, M.; Jin, C.H.; Xu, G.H.; Piao, L.X.; Jin, H.L.; et al. Formononetin represses cervical tumorigenesis by interfering with the activation of PD-L1 through MYC and STAT3 downregulation. J. Nutr. Biochem. 2022, 100, 108899. [Google Scholar] [CrossRef]
- Kim, C.; Lee, S.G.; Yang, W.M.; Arfuso, F.; Um, J.Y.; Kumar, A.P.; Bian, J.; Sethi, G.; Ahn, K.S. Formononetin-induced oxidative stress abrogates the activation of STAT3/5 signaling axis and suppresses the tumor growth in multiple myeloma preclinical model. Cancer Lett. 2018, 431, 123–141. [Google Scholar] [CrossRef] [PubMed]
- Curran, S.; Murray, G.I. Matrix metalloproteinases: Molecular aspects of their roles in tumour invasion and metastasis. Eur. J. Cancer 2000, 36, 1621–1630. [Google Scholar] [CrossRef]
- Kessenbrock, K.; Plaks, V.; Werb, Z. Matrix metalloproteinases: Regulators of the tumor microenvironment. Cell 2010, 141, 52–67. [Google Scholar] [CrossRef]
- Moss, L.A.S.; Jensen-Taubman, S.; Stetler-Stevenson, W.G. Matrix metalloproteinases changing roles in tumor progression and metastasis. Am. J. Pathol. 2012, 181, 1895–1899. [Google Scholar]
- Littlepage, L.E.; Sternlicht, M.D.; Rougier, N.; Phillips, J.; Gallo, E.; Yu, Y.; Williams, K.; Brenot, A.; Gordon, J.I.; Werb, Z. Matrix metalloproteinases contribute distinct roles in neuroendocrine prostate carcinogenesis, metastasis, and angiogenesis progression. Cancer Res. 2010, 70, 2224–2234. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. The hallmarks of cancer. Cell 2000, 100, 57–70. [Google Scholar] [CrossRef]
- Yu, S.; Li, A.; Liu, Q.; Yuan, X.; Xu, H.; Jiao, D.; Pestell, R.G.; Han, X.; Wu, K. Recent advances of bispecific antibodies in solid tumors. J. Hematol. Oncol. 2017, 10, 155. [Google Scholar] [CrossRef]
- Wheeler, D.L.; Huang, S.; Kruser, T.J.; Nechrebecki, M.M.; Armstrong, E.A.; Benavente, S.; Gondi, V.; Hsu, K.-T.; Harari, P.M. Mechanisms of acquired resistance to cetuximab: Role of HER (ErbB) family members. Oncogene 2008, 27, 3944–3956. [Google Scholar] [CrossRef] [PubMed]
- Roskoski, R., Jr. The ErbB/HER family of protein-tyrosine kinases and cancer. Pharmacol. Res. 2014, 79, 34–74. [Google Scholar] [CrossRef]
- Yu, X.; Gao, F.; Li, W.; Zhou, L.; Liu, W.; Li, M. Formononetin inhibits tumor growth by suppression of EGFR-Akt-Mcl-1 axis in non-small cell lung cancer. J. Exp. Clin. Cancer Res. 2020, 39, 62. [Google Scholar] [CrossRef]
- Fitzmaurice, C.; Allen, C.; Barber, R.M.; Barregard, L.; Bhutta, Z.A.; Brenner, H.; Dicker, D.J.; Chimed-Orchir, O.; Dandona, R.; Dandona, L.; et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A systematic analysis for the global burden of disease study. JAMA Oncol. 2017, 3, 524. [Google Scholar]
- Brannan, C.I.; Dees, E.C.; Ingram, R.S.; Tilghman, S.M. The Product of the H19 Gene May Function as an RNA. Mol. Cell. Biol. 1990, 10, 28–36. [Google Scholar]
- Wang, R.; Li, K.; Xie, Z.; Wang, B.; Dai, Y.; Chen, J.; Ye, Y. Formononetin induces apoptosis of PC-3 human prostate cancer cells via regulating long noncoding RNA H19 and the mitochondrial apoptosis pathway. Pharmacogn. Mag. 2020, 16, 435–440. [Google Scholar]
- Yin, Y.; Hua, H.; Li, M.; Liu, S.; Kong, Q.; Shao, T.; Wang, J.; Luo, Y.; Wang, Q.; Luo, T.; et al. mTORC2 promotes type I insulin-like growth factor receptor and insulin receptor activation through the tyrosine kinase activity of mTOR. Cell Res. 2016, 26, 46–65. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Zhang, S.; Chen, F.; Hu, J.; Yuan, S.; Li, C.; Wang, X.; Zhang, W.; Tang, R. Formononetin ameliorates the drug resistance of Taxol resistant triple negative breast cancer by inhibiting autophagy. Am. J. Transl. Res. 2021, 13, 497–514. [Google Scholar] [PubMed]
- Marinov, M.; Ziogas, A.; Pardo, O.E.; Tan, L.T.; Dhillon, T.; Mauri, F.A.; Lane, H.A.; Lemoine, N.R.; Zangemeister-Wittke, U.; Seckl, M.J.; et al. AKT/mTOR Pathway Activation and BCL-2 Family Proteins Modulate the Sensitivity of Human Small Cell Lung Cancer Cells to RAD001. Clin. Cancer Res. 2009, 15, 1277–1287. [Google Scholar] [CrossRef]
- Zhou, Q.; Zhang, W.; Li, T.; Tang, R.; Li, C.; Yuan, S.; Fan, D. Formononetin Enhances the Tumoricidal Effect of Everolimus in Breast Cancer MDA-MB-468 Cells by Suppressing the mTOR Pathway. Evid.-Based Complement. Altern. Med. 2019, 2019, 9610629. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Xu, W.; Ma, L.; Sheng, J.; Ye, M.; Chen, H.; Zhang, Y.; Wang, B.; Liao, M.; Meng, T.; et al. Formononetin relieves the facilitating effect of lncRNA AFAP1-AS1-miR-195/miR-545 axis on progression and chemo-resistance of triple-negative breast cancer. Aging 2021, 13, 18191–18222. [Google Scholar] [CrossRef] [PubMed]
- Pal, A.; Kundu, R. Human Papillomavirus E6 and E7: The Cervical Cancer Hallmarks and Targets for Therapy. Front. Microbiol. 2019, 10, 3116. [Google Scholar] [CrossRef] [PubMed]
- Prigge, E.S.; von Knebel Doeberitz, M.; Reuschenbach, M. Clinical relevance and implications of HPV-induced neoplasia in different anatomical locations. Mutat. Res. Rev. Mutat. Res. 2017, 772, 51–66. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.-M.; Xu, T.-M.; Zhao, Y.-H.; Wang, Y.-C.; Cui, M.-H. In vitro and in vivo anti-cancer activity of formononetin on human cervical cancer cell line HeLa. Tumor Biol. 2014, 35, 2279–2284. [Google Scholar] [CrossRef]
- Park, S.; Bazer, F.W.; Lim, W.; Song, G. The O-methylated isoflavone, formononetin, inhibits human ovarian cancer cell proliferation by sub G0/G1 cell phase arrest through PI3K/AKT and ERK1/2 inactivation. J. Cell. Biochem. 2018, 119, 7377–7387. [Google Scholar] [CrossRef]
- Zhang, J.; Liu, L.; Wang, J.; Ren, B.; Zhang, L.; Li, W. Formononetin, an isoflavone from Astragalus membranaceus inhibits proliferation and metastasis of ovarian cancer cells. J. Ethnopharmacol. 2018, 221, 91–99. [Google Scholar] [CrossRef]
- Ritter, J.; Bielack, S.S. Osteosarcoma. Ann. Oncol. 2010, 21 (Suppl. S7), vii320–vii325. [Google Scholar] [CrossRef]
- Anderson, M.E. Update on Survival in Osteosarcoma. Orthop. Clin. N. Am. 2016, 47, 283–292. [Google Scholar] [CrossRef]
- Oh, J.S.; Kim, T.H.; Park, J.H.; Lim, H.; Cho, I.A.; You, J.S.; Lee, G.J.; Seo, Y.S.; Kim, D.K.; Kim, C.S.; et al. Formononetin induces apoptotic cell death through the suppression of mitogen-activated protein kinase and nuclear factor-κB phosphorylation in FaDu human head and neck squamous cell carcinoma cells. Oncol. Rep. 2020, 43, 700–710. [Google Scholar] [CrossRef]
- Guo, Y.H.; Wang, Y.; Xin, M. Low concentration of formononetin stimulates the proliferation of nasopharyngeal carcinoma cell line CNE2 by upregulating bcl-2 and p-ERK1/2 expression. Pharm. Biol. 2016, 54, 1841–1846. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Sun, Y.; Zheng, J.-M.; Yan, X.-L.; Chen, H.-M.; Chen, J.-K.; Huang, H.-Q. Formononetin sensitizes glioma cells to doxorubicin through preventing EMT via inhibition of histone deacetylase 5. Int. J. Clin. Exp. Pathol. 2015, 8, 6434–6441. [Google Scholar]
- Kim, C.; Lee, J.H.; Ko, J.-H.; Chinnathambi, A.; Alharbi, S.A.; Shair, O.H.M.; Sethi, G.; Ahn, K.S. Formononetin Regulates Multiple Oncogenic Signaling Cascades and Enhances Sensitivity to Bortezomib in a Multiple Myeloma Mouse Model. Biomolecules 2019, 9, 262. [Google Scholar] [CrossRef]
- Huang, J.; Xie, M.; Gao, P.; Ye, Y.; Liu, Y.; Zhao, Y.; Luo, W.; Ling, Z.; Cao, Y.; Zhang, S.; et al. Antiproliferative effects of formononetin on human colorectal cancer via suppressing cell growth in vitro and in vivo. Process Biochem. 2015, 50, 912–917. [Google Scholar] [CrossRef]
- Wang, W.S.; Zhao, C.S. Formononetin exhibits anticancer activity in gastric carcinoma cell and regulating miR-542-5p. Kaohsiung J. Med. Sci. 2021, 37, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.N.; Zhang, X.X.; Zhang, Y.Z.; Li, J.H.; Zhao, D.Y.; Gao, B.; Zhou, H.N.; Gao, S.L.; Zhang, L.F. Discovery and anticancer evaluation of a formononetin derivative against gastric cancer SGC7901 cells. Investig. New Drugs 2019, 37, 1300–1308. [Google Scholar] [CrossRef] [PubMed]
- Lo, Y.-L.; Wang, W. Formononetin potentiates epirubicin-induced apoptosis via ROS production in HeLa cells in vitro. Chem. Interact. 2013, 205, 188–197. [Google Scholar] [CrossRef]
- Xin, M.; Wang, Y.; Ren, Q.; Guo, Y. Formononetin and metformin act synergistically to inhibit growth of MCF-7 breast cancer cells in vitro. Biomed. Pharmacother. 2019, 109, 2084–2089. [Google Scholar] [CrossRef]
- Zhang, X.; Ni, Q.; Wang, Y.; Fan, H.; Li, Y. Synergistic Anticancer Effects of Formononetin and Temozolomide on Glioma C6 Cells. Biol. Pharm. Bull. 2018, 41, 1194–1202. [Google Scholar] [CrossRef]
- Li, S.; Li, J.; Fan, Y.; Huang, T.; Zhou, Y.; Fan, H.; Zhang, Q.; Qiu, R. The mechanism of formononetin/calycosin compound optimizing the effects of temozolomide on C6 malignant glioma based on metabolomics and network pharmacology. Biomed. Pharmacother. 2022, 153, 113418. [Google Scholar] [CrossRef]
- Almatroodi, S.A.; Alsahli, M.A.; Almatroudi, A.; Dev, K.; Rafat, S.; Verma, A.K.; Rahmani, A.H. Amla (Emblica officinalis): Role in health management via controlling various biological activities. Gene Rep. 2020, 21, 100820. [Google Scholar] [CrossRef]
- Almatroodi, S.A.; Alnuqaydan, A.M.; Alsahli, M.A.; Khan, A.A.; Rahmani, A.H. Thymoquinone, the Most Prominent Constituent of Nigella Sativa, Attenuates Liver Damage in Streptozotocin-Induced Diabetic Rats via Regulation of Oxidative Stress, Inflammation and Cyclooxygenase-2 Protein Expression. Appl. Sci. 2021, 11, 3223. [Google Scholar] [CrossRef]
- Anwar, S.; AAlmatroodi, S.; Almatroudi, A.; Allemailem, K.S.; Joseph, R.J.; Khan, A.A.; Alrumaihi, F.; Alsahli, M.A.; Husain Rahmani, A. Biosynthesis of silver nanoparticles using Tamarix articulata leaf extract: An effective approach for attenuation of oxidative stress mediated diseases. Int. J. Food Prop. 2021, 24, 677–701. [Google Scholar] [CrossRef]
- Rahmani, A.H.; Aldebasi, Y.H. Ficus carica and its constituents role in management of diseases. Asian J. Pharm. Clin. Res. 2017, 10, 49–53. [Google Scholar] [CrossRef]
- Almatroodi, S.A.; Almatroudi, A.; Alsahli, M.A.; Aljasir, M.A.; Syed, M.A.; Rahmani, A.H. Epigallocatechin-3-Gallate (EGCG), an active compound of green tea attenuates acute lung injury regulating macrophage polarization and Krüpple-like-factor 4 (KLF4) expression. Molecules 2020, 25, 2853. [Google Scholar] [CrossRef]
- Almatroodi, S.A.; Alsahli, M.A.; Almatroudi, A.; Rahmani, A.H. Garlic and its active compounds: A potential candidate in the prevention of cancer by modulating various cell signalling pathways. Anti-Cancer Agents Med. Chem. (Former. Curr. Med. Chem.-Anti-Cancer Agents) 2019, 19, 1314–1324. [Google Scholar] [CrossRef]
- Rahmani, A.H.; Alsahli, M.A.; Almatroodi, S.A. Potential Antitumor Effects of Pomegranates and Its Ingredients. Pharmacogn. Rev. 2017, 11, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Almatroodi, S.A.; Syed, M.A.; Rahmani, A.H. Potential Therapeutic Targets of Curcumin, Most Abundant Active Compound of Turmeric Spice: Role in the Management of Various Types of Cancer. Recent Pat. Anti-Cancer Drug Discov. 2021, 16, 3–29. [Google Scholar] [CrossRef]
- Almatroodi, S.A.; Almatroudi, A.; Alsahli, M.A.; Rahman, A.H. Grapes and their Bioactive Compounds: Role in Health Management Through Modulating Various Biological Activities. Pharmacogn. J. 2020, 12, 1455–1462. [Google Scholar] [CrossRef]
- Luo, L.Y.; Fan, M.X.; Zhao, H.Y.; Li, M.X.; Wu, X.; Gao, W.Y. Pharmacokinetics and Bioavailability of the Isoflavones Formononetin and Ononin and Their in vitro Absorption in Using Chamber and Caco-2 Cell Models. J. Agric. Food Chem. 2018, 66, 2917–2924. [Google Scholar] [CrossRef]
- Singh, S.P.; Wahajuddin Tewari, D.; Pradhan, T.; Jain, G.K. PAMPA permeability, plasma protein binding, blood partition, pharmacokinetics and metabolism of formononetin, a methoxylated isoflavone. Food Chem. Toxicol. 2011, 49, 1056–1062. [Google Scholar] [CrossRef] [PubMed]
- Fu, D.-J.; Zhang, L.; Song, J.; Mao, R.-W.; Zhao, R.-H.; Liu, Y.-C.; Hou, Y.-H.; Li, J.-H.; Yang, J.-J.; Jin, C.-Y.; et al. Design and synthesis of formononetin-dithiocarbamate hybrids that inhibit growth and migration of PC-3 cells via MAPK/Wnt signaling pathways. Eur. J. Med. Chem. 2017, 127, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Ren, J.; Xu, H.-J.; Cheng, H.; Xin, W.-Q.; Chen, X.; Hu, K. Synthesis and antitumor activity of formononetin nitrogen mustard derivatives. Eur. J. Med. Chem. 2012, 54, 175–187. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Xie, Q.; Zeng, X.; Tao, N.; Xu, Y.; Chen, Y.; Wang, J.; Zhang, L. Novel hybrids of podophyllotoxin and formononetin inhibit the growth, migration and invasion of lung cancer cells. Bioorg. Chem. 2019, 85, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Guo, B.; Liao, C.; Liu, X.; Yi, J. Preliminary study on conjugation of formononetin with multiwalled carbon nanotubes for inducing apoptosis via ROS production in HeLa cells. Drug Des. Dev. Ther. 2018, 12, 2815–2826. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.; Yan, H.; Jia, X.; Zhang, Z. Preparation and in vivo/in vitro evaluation of formononetin phospholipid/vitamin E TPGS micelles. J. Drug Target. 2016, 24, 161–168. [Google Scholar] [CrossRef]
- Dong, Z.; Wang, Y.; Guo, J.; Tian, C.; Pan, W.; Wang, H.; Yan, J. Prostate Cancer Therapy Using Docetaxel and Formononetin Combination: Hyaluronic Acid and Epidermal Growth Factor Receptor Targeted Peptide Dual Ligands Modified Binary Nanoparticles to Facilitate the in vivo Anti-Tumor Activity. Drug Des. Dev. Ther. 2022, 16, 2683–2693. [Google Scholar] [CrossRef]
- Xiong, W.; Lan, Q.; Liang, X.; Zhao, J.; Huang, H.; Zhan, Y.; Qin, Z.; Jiang, X.; Zheng, L. Cartilage-targeting poly(ethylene glycol) (PEG)-formononetin (FMN) nanodrug for the treatment of osteoarthritis. J. Nanobiotechnol. 2021, 19, 197. [Google Scholar] [CrossRef]
- Guo, B.; Xu, D.; Liu, X.; Liao, C.; Li, S.; Huang, Z.; Li, X.; Yi, J. Characterization and cytotoxicity of PLGA nanoparticles loaded with formononetin cyclodextrin complex. J. Drug Deliv. Sci. Technol. 2017, 41, 375–383. [Google Scholar] [CrossRef]
- Liu, X.; Xu, D.; Liao, C.; Fang, Y.; Guo, B. Development of a promising drug delivery for formononetin: Cyclodextrin-modified single-walled carbon nanotubes. J. Drug Deliv. Sci. Technol. 2018, 43, 461–468. [Google Scholar] [CrossRef]
- Li, C.; Li, G.; Gao, Y.; Sun, C.; Wang, X. A 90-day Subchronic Toxicity Study with Sodium Formononetin-3′-Sulphonate (Sul-F) Delivered to Dogs via Intravenous Administration. Regul. Toxicol. Pharmacol. 2016, 77, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Yang, M.; Hao, X.; Li, C.; Gao, Y.; Tao, J. Acute toxicity of sodium formononetin-3′-sulphonate (Sul-F) in Sprague-Dawley rats and Beagle dogs. Regul. Toxicol. Pharmacol. 2015, 73, 629–633. [Google Scholar] [CrossRef]
- PPark, J.; Kim, S.H.; Cho, D.; Kim, T.S. Formononetin, a phyto-oestrogen, and its metabolites up-regulate interleukin-4 production in activated T cells via increased AP-1 DNA binding activity. Immunology 2005, 116, 71–81. [Google Scholar] [CrossRef]
- Atkinson, C.; Compston, J.E.; Day, N.E.; Dowsett, M.; Bingham, S.A. The effects of phytoestrogen isoflavones on bone density in women: A double-blind, randomized, placebo-controlled trial. Am. J. Clin. Nutr. 2004, 79, 326–333. [Google Scholar] [CrossRef]
- Nestel, P.J.; Pomeroy, S.; Kay, S.; Komesaroff, P.; Behrsing, J.; Cameron, J.D.; West, L. Isoflavones from Red Clover Improve Systemic Arterial Compliance But Not Plasma Lipids in Menopausal Women 1. J. Clin. Endocrinol. Metab. 1999, 84, 895–898. [Google Scholar] [CrossRef] [PubMed]
- Jarred, R.A.; Keikha, M.; Dowling, C.; McPherson, S.J.; Clare, A.M.; Husband, A.J.; Pedersen, J.S.; Frydenberg, M.; Risbridger, G.P. Induction of apoptosis in low to moderate-grade human prostate carcinoma by red clover-derived dietary isoflavones. Cancer Epidemiol. Biomark. Prev. 2002, 11, 1689–1696. [Google Scholar]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almatroodi, S.A.; Almatroudi, A.; Khan, A.A.; Rahmani, A.H. Potential Therapeutic Targets of Formononetin, a Type of Methoxylated Isoflavone, and Its Role in Cancer Therapy through the Modulation of Signal Transduction Pathways. Int. J. Mol. Sci. 2023, 24, 9719. https://doi.org/10.3390/ijms24119719
Almatroodi SA, Almatroudi A, Khan AA, Rahmani AH. Potential Therapeutic Targets of Formononetin, a Type of Methoxylated Isoflavone, and Its Role in Cancer Therapy through the Modulation of Signal Transduction Pathways. International Journal of Molecular Sciences. 2023; 24(11):9719. https://doi.org/10.3390/ijms24119719
Chicago/Turabian StyleAlmatroodi, Saleh A., Ahmad Almatroudi, Amjad Ali Khan, and Arshad Husain Rahmani. 2023. "Potential Therapeutic Targets of Formononetin, a Type of Methoxylated Isoflavone, and Its Role in Cancer Therapy through the Modulation of Signal Transduction Pathways" International Journal of Molecular Sciences 24, no. 11: 9719. https://doi.org/10.3390/ijms24119719
APA StyleAlmatroodi, S. A., Almatroudi, A., Khan, A. A., & Rahmani, A. H. (2023). Potential Therapeutic Targets of Formononetin, a Type of Methoxylated Isoflavone, and Its Role in Cancer Therapy through the Modulation of Signal Transduction Pathways. International Journal of Molecular Sciences, 24(11), 9719. https://doi.org/10.3390/ijms24119719





