MYD88 and Proinflammatory Chemokines in Aortic Atheromatosis: Exploring Novel Statin Effects
Abstract
1. Introduction
2. Results
2.1. Effects of Atherogenesis and Statin Therapy on Aortic Cytokine mRNA Expression
2.1.1. Thoracic Aorta
2.1.2. Abdominal Aorta
2.2. Correlations between MYD88 and Other Biomarkers during Aortic Atherogenesis and Statin Treatment
3. Discussion
4. Methods
4.1. Animal Experimental Protocol
4.2. mRNA Analysis of Rabbit Aortic Tissue
4.3. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; de Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef] [PubMed]
- Heidenreich, P.A.; Trogdon, J.G.; Khavjou, O.A.; Butler, J.; Dracup, K.; Ezekowitz, M.D.; Finkelstein, E.A.; Hong, Y.; Johnston, S.C.; Khera, A.; et al. Forecasting the future of cardiovascular disease in the United States: A policy statement from the American Heart Association. Circulation 2011, 123, 933–944. [Google Scholar] [CrossRef] [PubMed]
- Getz, G.S.; Reardon, C.A. Atherogenic lipids and macrophage subsets. Curr. Opin. Lipidol. 2015, 26, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Gomez, D.; Owens, G.K. Smooth muscle cell phenotypic switching in atherosclerosis. Cardiovasc. Res. 2012, 95, 156–164. [Google Scholar] [CrossRef]
- Hansson, G.K.; Hermansson, A. The immune system in atherosclerosis. Nat. Immunol. 2011, 12, 204–212. [Google Scholar] [CrossRef]
- Quillard, T.; Araújo, H.A.; Franck, G.; Shvartz, E.; Sukhova, G.; Libby, P. TLR2 and neutrophils potentiate endothelial stress, apoptosis and detachment: Implications for superficial erosion. Eur. Heart J. 2015, 36, 1394–1404. [Google Scholar] [CrossRef]
- Margiana, R.; Alsaikhan, F.; Al-Awsi, G.R.L.; Patra, I.; Sivaraman, R.; Fadhil, A.A.; Al-Baghdady, H.F.A.; Qasim, M.T.; Hameed, N.M.; Mustafa, Y.F.; et al. Functions and therapeutic interventions of non-coding RNAs associated with TLR signaling pathway in atherosclerosis. Cell. Signal. 2022, 100, 110471. [Google Scholar] [CrossRef]
- Mylonas, K.S.; Sarantis, P.; Kapelouzou, A.; Karamouzis, M.V.; Kapetanakis, E.I.; Kontzoglou, K.; Iliopoulos, D.C.; Nikiteas, N.; Schizas, D. Mechanosensitive Stem-Cell Genes and Klotho in Atherosclerotic Aortas: Regulating Spatially Deranged Expression Patterns Using Colchicine Regimens. J. Clin. Med. 2022, 11, 6465. [Google Scholar] [CrossRef]
- Mylonas, K.S.; Karangelis, D.; Androutsopoulou, V.; Chalikias, G.; Tziakas, D.; Mikroulis, D.; Iliopoulos, D.C.; Nikiteas, N.; Schizas, D. Stem cell genes in atheromatosis: The role of Klotho, HIF1α, OCT4, and BMP4. IUBMB Life 2022, 74, 1003–1011. [Google Scholar] [CrossRef]
- Mylonas, K.S.; Kapelouzou, A.; Spartalis, M.; Mastrogeorgiou, M.; Spartalis, E.; Bakoyiannis, C.; Liakakos, T.; Schizas, D.; Iliopoulos, D.; Nikiteas, N. KLF4 Upregulation in Atherosclerotic Thoracic Aortas: Exploring the Protective Effect of Colchicine-based Regimens in a Hyperlipidemic Rabbit Model. Ann. Vasc. Surg. 2022, 78, 328–335. [Google Scholar] [CrossRef]
- Miller, Y.I.; Viriyakosol, S.; Worrall, D.S.; Boullier, A.; Butler, S.; Witztum, J.L. Toll-like receptor 4-dependent and -independent cytokine secretion induced by minimally oxidized low-density lipoprotein in macrophages. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 1213–1219. [Google Scholar] [CrossRef]
- Lee, J.Y.; Hwang, D.H. The modulation of inflammatory gene expression by lipids: Mediation through Toll-like receptors. Mol. Cells 2006, 21, 174–185. [Google Scholar]
- O’Neill, L.A.; Dunne, A.; Edjeback, M.; Gray, P.; Jefferies, C.; Wietek, C. Mal and MyD88: Adapter proteins involved in signal transduction by Toll-like receptors. J. Endotoxin Res. 2003, 9, 55–59. [Google Scholar] [CrossRef]
- Muendlein, H.I.; Connolly, W.M.; Cameron, J.; Jetton, D.; Magri, Z.; Smirnova, I.; Vannier, E.; Li, X.; Martinot, A.J.; Batorsky, R.; et al. Neutrophils and macrophages drive TNF-induced lethality via TRIF/CD14-mediated responses. Sci. Immunol. 2022, 7, eadd0665. [Google Scholar] [CrossRef]
- Kong, P.; Cui, Z.Y.; Huang, X.F.; Zhang, D.D.; Guo, R.J.; Han, M. Inflammation and atherosclerosis: Signaling pathways and therapeutic intervention. Signal Transduct. Target. Ther. 2022, 7, 131. [Google Scholar] [CrossRef]
- Mylonas, K.S.; Iliopoulos, D.; Nikiteas, N.; Schizas, D. Looking for the Achilles heel of atheromatosis: Could it be immunotherapy? Immunotherapy 2021, 13, 557–560. [Google Scholar] [CrossRef]
- Jain, M.K.; Ridker, P.M. Anti-inflammatory effects of statins: Clinical evidence and basic mechanisms. Nat. Rev. Drug Discov. 2005, 4, 977–987. [Google Scholar] [CrossRef]
- Ii, M.; Losordo, D.W. Statins and the endothelium. Vasc. Pharmacol. 2007, 46, 1–9. [Google Scholar] [CrossRef]
- Michelsen, K.S.; Wong, M.H.; Shah, P.K.; Zhang, W.; Yano, J.; Doherty, T.M.; Akira, S.; Rajavashisth, T.B.; Arditi, M. Lack of Toll-like receptor 4 or myeloid differentiation factor 88 reduces atherosclerosis and alters plaque phenotype in mice deficient in apolipoprotein E. Proc. Natl. Acad. Sci. USA 2004, 101, 10679–10684. [Google Scholar] [CrossRef]
- Howell, K.W.; Meng, X.; Fullerton, D.A.; Jin, C.; Reece, T.B.; Cleveland, J.C., Jr. Toll-like receptor 4 mediates oxidized LDL-induced macrophage differentiation to foam cells. J. Surg. Res. 2011, 171, e27–e31. [Google Scholar] [CrossRef]
- Singh, R.K.; Haka, A.S.; Asmal, A.; Barbosa-Lorenzi, V.C.; Grosheva, I.; Chin, H.F.; Xiong, Y.; Hla, T.; Maxfield, F.R. TLR4 (Toll-Like Receptor 4)-Dependent Signaling Drives Extracellular Catabolism of LDL (Low-Density Lipoprotein) Aggregates. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 86–102. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, M.; Thorp, E.; Hansson, G.K.; Tabas, I. Treg-mediated suppression of atherosclerosis requires MYD88 signaling in DCs. J. Clin. Investig. 2013, 123, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Engelbertsen, D.; Rattik, S.; Wigren, M.; Vallejo, J.; Marinkovic, G.; Schiopu, A.; Björkbacka, H.; Nilsson, J.; Bengtsson, E. IL-1R and MyD88 signalling in CD4+ T cells promote Th17 immunity and atherosclerosis. Cardiovasc. Res. 2018, 114, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Zhou, H.; Zhao, J.; Xiao, N.; Roychowdhury, S.; Schmitt, D.; Hu, B.; Ransohoff, R.M.; Harding, C.V.; Hise, A.G.; et al. MyD88-dependent interplay between myeloid and endothelial cells in the initiation and progression of obesity-associated inflammatory diseases. J. Exp. Med. 2014, 211, 887–907. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Deng, X.; Zhang, P.; Wang, X.; Fan, Y.; Zhou, S.; Mu, S.; Mehta, J.L.; Ding, Z. Blood flow patterns regulate PCSK9 secretion via MyD88-mediated pro-inflammatory cytokines. Cardiovasc. Res. 2020, 116, 1721–1732. [Google Scholar] [CrossRef]
- Wan, W.; Murphy, P.M. Regulation of atherogenesis by chemokine receptor CCR6. Trends Cardiovasc. Med. 2011, 21, 140–144. [Google Scholar] [CrossRef]
- Calvayrac, O.; Rodríguez-Calvo, R.; Alonso, J.; Orbe, J.; Martín-Ventura, J.L.; Guadall, A.; Gentile, M.; Juan-Babot, O.; Egido, J.; Beloqui, O.; et al. CCL20 is increased in hypercholesterolemic subjects and is upregulated by LDL in vascular smooth muscle cells: Role of NF-κB. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 2733–2741. [Google Scholar] [CrossRef]
- Manthey, H.D.; Cochain, C.; Barnsteiner, S.; Karshovska, E.; Pelisek, J.; Koch, M.; Chaudhari, S.M.; Busch, M.; Eckstein, H.H.; Weber, C.; et al. CCR6 selectively promotes monocyte mediated inflammation and atherogenesis in mice. Thromb. Haemost. 2013, 110, 1267–1277. [Google Scholar]
- Zernecke, A.; Weber, C. Chemokines in atherosclerosis: Proceedings resumed. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 742–750. [Google Scholar] [CrossRef]
- Chang, T.T.; Yang, H.Y.; Chen, C.; Chen, J.W. CCL4 Inhibition in Atherosclerosis: Effects on Plaque Stability, Endothelial Cell Adhesiveness, and Macrophages Activation. Int. J. Mol. Sci. 2020, 21, 6567. [Google Scholar] [CrossRef]
- Schechtman, L.M. Implementation of the 3Rs (refinement, reduction, and replacement): Validation and regulatory acceptance considerations for alternative toxicological test methods. ILAR J. 2002, 43 (Suppl. S1), S85–S94. [Google Scholar] [CrossRef]
- Bassiouny, H.S.; Zarins, C.K.; Kadowaki, M.H.; Glagov, S. Hemodynamic stress and experimental aortoiliac atherosclerosis. J. Vasc. Surg. 1994, 19, 426–434. [Google Scholar] [CrossRef]
- Padilla, J.; Jenkins, N.T.; Vieira-Potter, V.J.; Laughlin, M.H. Divergent phenotype of rat thoracic and abdominal perivascular adipose tissues. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2013, 304, R543–R552. [Google Scholar] [CrossRef]
- Kapelouzou, A.; Giaglis, S.; Peroulis, M.; Katsimpoulas, M.; Moustardas, P.; Aravanis, C.V.; Kostakis, A.; Karayannakos, P.E.; Cokkinos, D.V. Overexpression of Toll-Like Receptors 2, 3, 4, and 8 Is Correlated to the Vascular Atherosclerotic Process in the Hyperlipidemic Rabbit Model: The Effect of Statin Treatment. J. Vasc. Res. 2017, 54, 156–169. [Google Scholar] [CrossRef]
- Tziakas, D.; Chalikias, G.; Kapelouzou, A.; Tentes, I.; Schäfer, K.; Karayannakos, P.; Kostakis, A.; Boudoulas, H.; Konstantinides, S. Erythrocyte membrane cholesterol and lipid core growth in a rabbit model of atherosclerosis: Modulatory effects of rosuvastatin. Int. J. Cardiol. 2013, 170, 173–181. [Google Scholar] [CrossRef]
- Chomczynski, P.; Sacchi, N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal. Biochem. 1987, 162, 156–159. [Google Scholar] [CrossRef]
- Kapelouzou, A.; Katsimpoulas, M.; Kontogiannis, C.; Lidoriki, I.; Georgiopoulos, G.; Kourek, C.; Papageorgiou, C.; Mylonas, K.S.; Dritsas, S.; Charalabopoulos, A.; et al. A High-Cholesterol Diet Increases Toll-like Receptors and Other Harmful Factors in the Rabbit Myocardium: The Beneficial Effect of Statins. Curr. Issues Mol. Biol. 2021, 43, 818–830. [Google Scholar] [CrossRef]
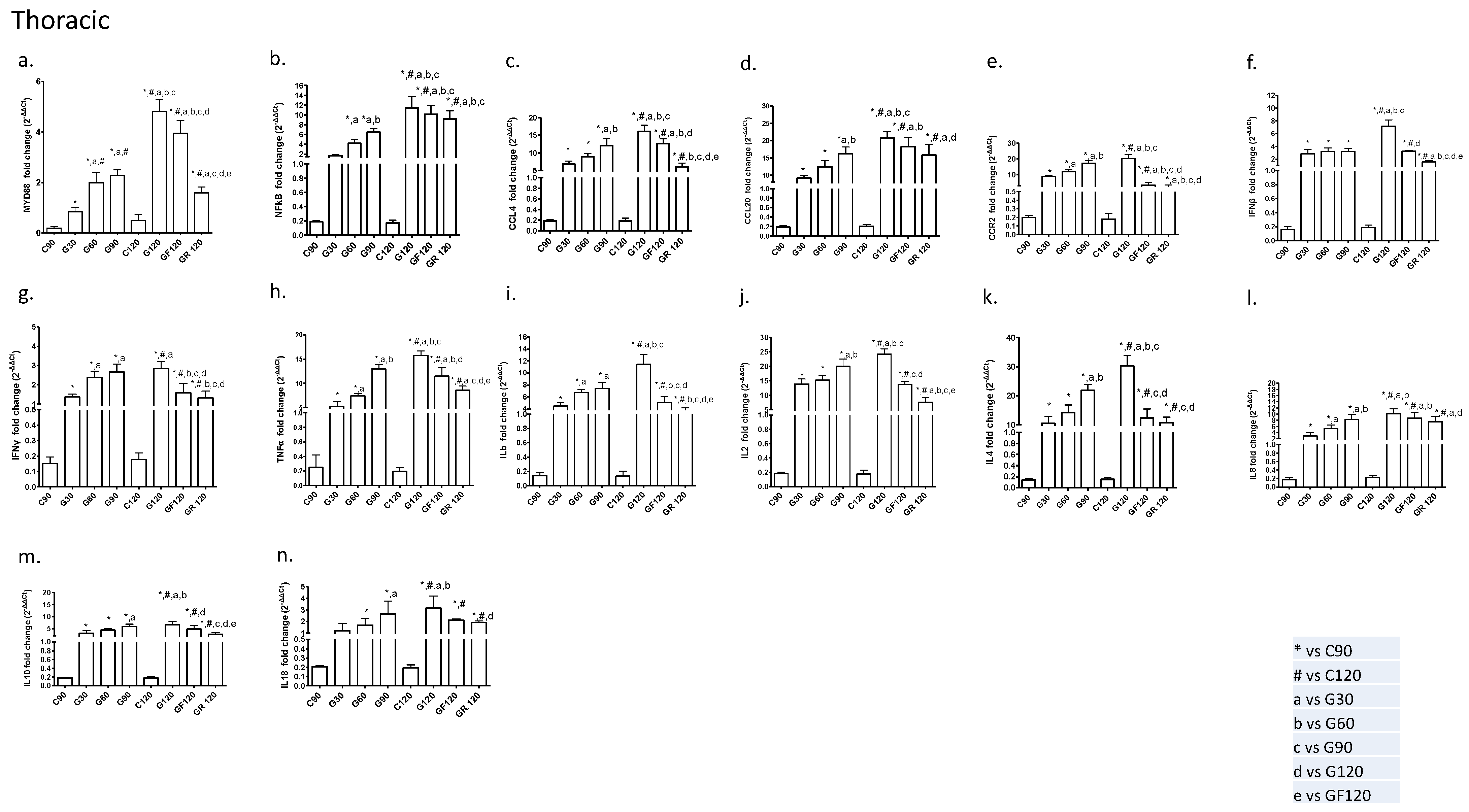

| Thoracic | ||||||||
| Groups | C90 | G30 | G60 | G90 | C120 | G120 | GF120 | GR 120 |
| N | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 |
| MYD88 | ||||||||
| Mean | 0.19 | 0.84 | 1.99 | 2.28 | 0.49 | 4.81 | 3.94 | 1.59 |
| SD | 0.05 | 0.17 | 0.40 | 0.21 | 0.25 | 0.46 | 0.49 | 0.23 |
| NF-kB | ||||||||
| Mean | 0.18 | 1.70 | 4.21 | 6.49 | 0.17 | 11.44 | 10.15 | 9.18 |
| SD | 0.02 | 0.21 | 0.81 | 0.74 | 0.04 | 2.25 | 1.80 | 1.63 |
| CCL4 | ||||||||
| Mean | 0.18 | 6.78 | 8.92 | 12.06 | 0.18 | 16.03 | 12.58 | 6.11 |
| SD | 0.03 | 0.92 | 0.93 | 2.05 | 0.05 | 1.80 | 1.42 | 0.99 |
| CCL20 | ||||||||
| Mean | 0.18 | 9.20 | 12.45 | 16.23 | 0.20 | 20.75 | 18.26 | 15.84 |
| SD | 0.03 | 0.65 | 1.80 | 1.87 | 0.03 | 1.81 | 2.68 | 3.06 |
| CCR2 | ||||||||
| Mean | 0.19 | 9.02 | 11.85 | 17.14 | 0.18 | 20.29 | 3.51 | 2.36 |
| SD | 0.02 | 0.74 | 1.17 | 1.76 | 0.06 | 2.60 | 1.55 | 1.09 |
| IFNβ | ||||||||
| Mean | 0.16 | 2.87 | 3.19 | 3.21 | 0.18 | 7.16 | 3.25 | 1.55 |
| SD | 0.04 | 0.70 | 0.56 | 0.43 | 0.03 | 0.99 | 0.11 | 0.24 |
| IFNγ | ||||||||
| Mean | 0.15 | 1.37 | 2.38 | 2.66 | 0.17 | 2.84 | 1.58 | 1.33 |
| SD | 0.04 | 0.15 | 0.31 | 0.41 | 0.04 | 0.35 | 0.47 | 0.34 |
| TNFα | ||||||||
| Mean | 0.25 | 5.25 | 7.39 | 12.98 | 0.19 | 15.76 | 11.49 | 8.55 |
| SD | 0.17 | 1.02 | 0.45 | 0.88 | 0.04 | 0.90 | 1.75 | 0.87 |
| Ilb | ||||||||
| Mean | 0.14 | 4.48 | 6.73 | 7.43 | 0.13 | 11.46 | 5.05 | 3.43 |
| SD | 0.04 | 0.50 | 0.51 | 0.99 | 0.06 | 1.69 | 1.00 | 0.74 |
| IL-2 | ||||||||
| Mean | 0.18 | 13.91 | 15.27 | 20.04 | 0.17 | 24.25 | 13.82 | 7.62 |
| SD | 0.01 | 1.69 | 1.72 | 2.47 | 0.05 | 1.83 | 0.99 | 1.61 |
| IL-4 | ||||||||
| Mean | 0.13 | 10.50 | 14.27 | 21.83 | 0.15 | 30.30 | 12.39 | 10.78 |
| SD | 0.02 | 2.42 | 2.59 | 2.04 | 0.03 | 3.53 | 3.09 | 1.92 |
| IL-8 | ||||||||
| Mean | 0.17 | 2.86 | 5.38 | 8.25 | 0.22 | 10.10 | 8.76 | 7.55 |
| SD | 0.05 | 1.14 | 1.12 | 1.74 | 0.05 | 1.62 | 1.90 | 1.74 |
| IL-10 | ||||||||
| Mean | 0.17 | 3.14 | 4.41 | 5.91 | 0.18 | 6.63 | 4.88 | 2.71 |
| SD | 0.01 | 1.16 | 0.70 | 0.99 | 0.02 | 1.20 | 1.53 | 0.73 |
| IL-18 | ||||||||
| Mean | 0.20 | 1.20 | 1.66 | 2.65 | 0.19 | 3.15 | 2.10 | 1.91 |
| SD | 0.01 | 0.63 | 0.57 | 1.11 | 0.03 | 1.05 | 0.12 | 0.12 |
| Abdominal | ||||||||
| Groups | C90 | G30 | G60 | G90 | C120 | G120 | GF120 | GR 120 |
| N | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 |
| MYD88 | ||||||||
| Mean | 0.16 | 0.55 | 0.44 | 1.27 | 0.18 | 2.61 | 2.01 | 1.76 |
| SD | 0.03 | 0.25 | 0.22 | 0.35 | 0.06 | 0.44 | 0.40 | 0.28 |
| NF-kB | ||||||||
| Mean | 0.18 | 1.25 | 2.57 | 3.88 | 0.16 | 9.82 | 8.32 | 8.26 |
| SD | 0.02 | 0.21 | 0.32 | 0.25 | 0.05 | 1.89 | 2.05 | 1.35 |
| CCL4 | ||||||||
| Mean | 0.17 | 5.37 | 7.21 | 8.55 | 0.17 | 9.66 | 8.39 | 7.52 |
| SD | 0.02 | 1.09 | 0.77 | 0.86 | 0.05 | 1.63 | 1.60 | 1.42 |
| CCL20 | ||||||||
| Mean | 0.18 | 7.06 | 10.4 | 13.83 | 0.22 | 17.33 | 12.70 | 6.21 |
| SD | 0.03 | 2.48 | 1.00 | 2.24 | 0.07 | 2.32 | 5.72 | 1.15 |
| CCR2 | ||||||||
| Mean | 0.19 | 5.88 | 7.45 | 12.16 | 0.18 | 16.84 | 4.31 | 1.98 |
| SD | 0.02 | 1.56 | 0.91 | 1.57 | 0.04 | 1.36 | 1.53 | 0.6 |
| IFNβ | ||||||||
| Mean | 0.16 | 1.96 | 2.36 | 2.40 | 0.18 | 5.37 | 2.61 | 1.35 |
| SD | 0.02 | 0.44 | 0.33 | 0.50 | 0.03 | 0.48 | 0.45 | 0.20 |
| IFNγ | ||||||||
| Mean | 0.16 | 0.88 | 1.50 | 1.60 | 0.17 | 5.91 | 1.72 | 1.57 |
| SD | 0.03 | 0.13 | 0.32 | 0.33 | 0.03 | 0.34 | 0.23 | 0.23 |
| TNFα | ||||||||
| Mean | 0.30 | 347 | 514 | 9.88 | 0.27 | 12.98 | 11.58 | 10.58 |
| SD | 0.19 | 0.47 | 0.76 | 1.06 | 0.16 | 1.40 | 1.34 | 1.22 |
| Ilb | ||||||||
| Mean | 0.12 | 2.11 | 2.60 | 4.36 | 0.17 | 5.69 | 2.85 | 2.22 |
| SD | 0.04 | 0.54 | 0.44 | 0.69 | 0.05 | 0.46 | 0.82 | 0.44 |
| IL-2 | ||||||||
| Mean | 0.15 | 10.35 | 12.50 | 14.50 | 0.22 | 15.67 | 13.22 | 6.31 |
| SD | 0.03 | 1.30 | 1.37 | 1.51 | 0.07 | 2.25 | 2.16 | 1.66 |
| IL-4 | ||||||||
| Mean | 0.12 | 9.59 | 12.27 | 14.42 | 0.15 | 15.92 | 13.65 | 8.96 |
| SD | 0.03 | 0.67 | 1.36 | 2.48 | 0.04 | 1.87 | 2.48 | 1.45 |
| IL-8 | ||||||||
| Mean | 0.173 | 2.08 | 3.38 | 5.13 | 0.19 | 7.01 | 7.06 | 5.08 |
| SD | 0.02 | 0.89 | 0.72 | 0.67 | 0.04 | 1.72 | 0.70 | 0.83 |
| IL-10 | ||||||||
| Mean | 0.19 | 2.33 | 3.10 | 4.1 | 0.18 | 4.71 | 3.18 | 1.53 |
| SD | 0.01 | 1.15 | 1.16 | 0.83 | 0.02 | 0.71 | 0.89 | 0.79 |
| IL-18 | ||||||||
| Mean | 0.18 | 0.54 | 1.44 | 1.90 | 0.17 | 2.33 | 1.83 | 1.45 |
| SD | 0.03 | 0.46 | 0.45 | 0.76 | 0.03 | 0.76 | 0.65 | 0.89 |
| MYD88 | MYD88 | MYD88 | MYD88 | MYD88 | MYD88 | |
|---|---|---|---|---|---|---|
| Group | G30 | G60 | G90 | G120 | GF120 | GR120 |
| Biomarker | ||||||
| NFKB | −0.04 | +0.001 | +0.04 | −0.09 | ||
| (−0.82) | (0.45) | (0.81) | (−0.64) | |||
| CCL4 | −0.02 | |||||
| (−0.881) | ||||||
| CCL20 | +0.02 | 0.01 | ||||
| (0.86) | (0.89) | |||||
| CCR2 | +0.03 | +0.04 | ||||
| (−0.85) | (0.82) | |||||
| IFNβ | +0.01 | |||||
| (0.89) | ||||||
| IFNγ | ||||||
| TNFa | ||||||
| ILb | +0.02 | −0.01 | ||||
| (0.86) | (−0.91) | |||||
| IL2 | ||||||
| IL4 | −0.02 | |||||
| (−0.86) | ||||||
| IL8 | ||||||
| IL10 | ||||||
| IL18 | +0.02 | +0.03 | ||||
| (0.86) | (0.83) |
| MYD88 | MYD88 | MYD88 | MYD88 | MYD88 | MYD88 | |
|---|---|---|---|---|---|---|
| Group | G30 | G60 | G90 | G120 | GF120 | GR120 |
| Biomarker | ||||||
| NFKB | ||||||
| CCL4 | ||||||
| CCL20 | 0.001 | |||||
| (0.97) | ||||||
| CCR2 | ||||||
| IFNβ | ||||||
| IFNγ | ||||||
| TNFa | ||||||
| ILb | +0.02 | |||||
| (0.50) | ||||||
| IL2 | ||||||
| IL4 | −0.008 | +0.04 | 0.04 | |||
| (−0.92) | (0.81) | (−0.82) | ||||
| IL8 | ||||||
| IL10 | ||||||
| IL18 | +0.01 | |||||
| (0.89) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mylonas, K.S.; Peroulis, M.; Schizas, D.; Kapelouzou, A. MYD88 and Proinflammatory Chemokines in Aortic Atheromatosis: Exploring Novel Statin Effects. Int. J. Mol. Sci. 2023, 24, 9248. https://doi.org/10.3390/ijms24119248
Mylonas KS, Peroulis M, Schizas D, Kapelouzou A. MYD88 and Proinflammatory Chemokines in Aortic Atheromatosis: Exploring Novel Statin Effects. International Journal of Molecular Sciences. 2023; 24(11):9248. https://doi.org/10.3390/ijms24119248
Chicago/Turabian StyleMylonas, Konstantinos S., Michail Peroulis, Dimitrios Schizas, and Alkistis Kapelouzou. 2023. "MYD88 and Proinflammatory Chemokines in Aortic Atheromatosis: Exploring Novel Statin Effects" International Journal of Molecular Sciences 24, no. 11: 9248. https://doi.org/10.3390/ijms24119248
APA StyleMylonas, K. S., Peroulis, M., Schizas, D., & Kapelouzou, A. (2023). MYD88 and Proinflammatory Chemokines in Aortic Atheromatosis: Exploring Novel Statin Effects. International Journal of Molecular Sciences, 24(11), 9248. https://doi.org/10.3390/ijms24119248







