Pre-Transplant Serum Leptin Levels and Relapse of Acute Myeloid Leukemia after Allogeneic Transplantation
Abstract
1. Introduction
2. Results
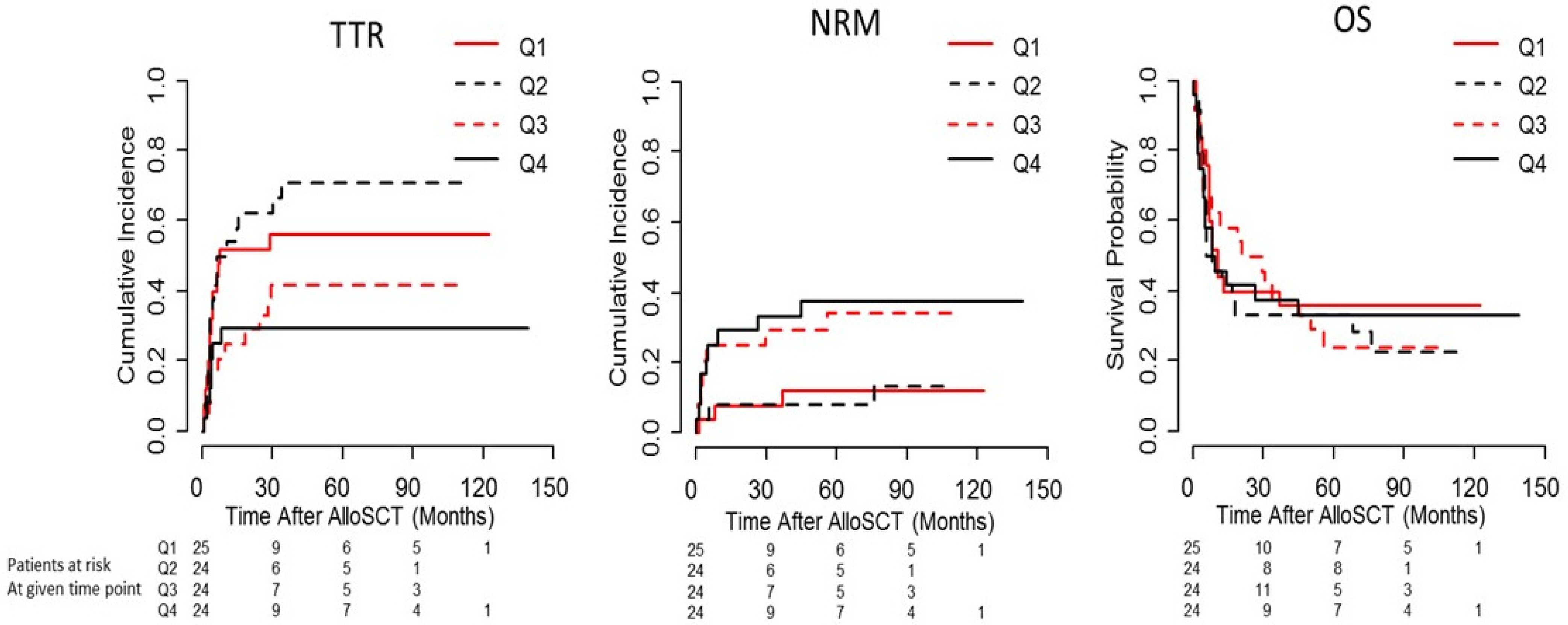
2.1. Pre-Conditioning Serum Leptin Levels Predict Time to Relapse (TTR) Depending on Disease Entity and Disease Stage
2.2. Leptin Levels and Outcome in Patients with Intermediate/Advanced Stage AL
2.3. Correlations of Leptin with BMI, Pre-Transplant Weight Change, and Adiponectin
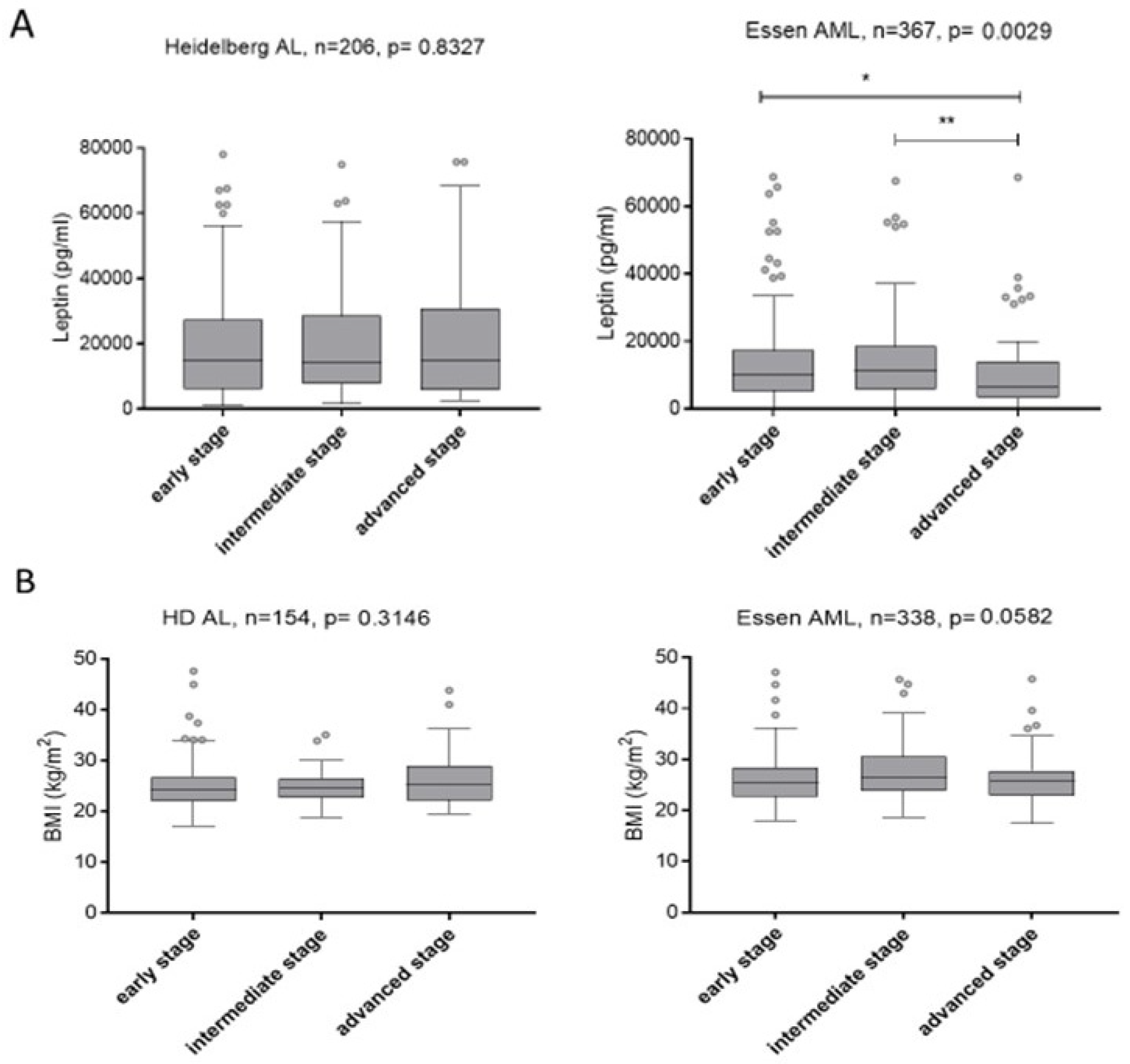
2.4. Relationship of Serum Leptin Levels and BMI with Disease Stage
2.5. Influence of Serum Leptin Levels on Incidence and Severity of Acute and Chronic GvHD
3. Discussion
4. Patients and Methods
4.1. Patient Characteristics
4.2. Determination of Serum Leptin and Adiponectin Levels
4.3. Transplantation Procedure and Supportive Care
4.4. Statistical Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Drobyski, W.R. The role of allogeneic transplantation in high-risk acute myelogenous leukemia. Leukemia 2004, 18, 1565–1568. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pui, C.H.; Evans, W.E. Treatment of acute lymphoblastic leukemia. N. Engl. J. Med. 2006, 354, 166–178. [Google Scholar] [CrossRef]
- Terwey, T.H.; Le Duc, T.M.; Hemmati, P.G.; le Coutre, P.; Nagy, M.; Martus, P.; Dorken, B.; Arnold, R. NIH-defined graft-versus-host disease and evidence for a potent graft-versus-leukemia effect in patients with acute lymphoblastic leukemia. Ann. Oncol. 2013, 24, 1363–1370. [Google Scholar] [CrossRef] [PubMed]
- Valcarcel, D.; Martino, R.; Caballero, D.; Martin, J.; Ferra, C.; Nieto, J.B.; Sampol, A.; Bernal, M.T.; Pinana, J.L.; Vazquez, L.; et al. Sustained remissions of high-risk acute myeloid leukemia and myelodysplastic syndrome after reduced-intensity conditioning allogeneic hematopoietic transplantation: Chronic graft-versus-host disease is the strongest factor improving survival. J. Clin. Oncol. 2008, 26, 577–584. [Google Scholar] [CrossRef]
- Bulley, S.; Gassas, A.; Dupuis, L.L.; Aplenc, R.; Beyene, J.; Greenberg, M.L.; Doyle, J.J.; Sung, L. Inferior outcomes for overweight children undergoing allogeneic stem cell transplantation. Br. J. Haematol. 2008, 140, 214–217. [Google Scholar] [CrossRef] [PubMed]
- White, M.; Murphy, A.J.; Hallahan, A.; Ware, R.S.; Fraser, C.; Davies, P.S. Survival in overweight and underweight children undergoing hematopoietic stem cell transplantation. Eur. J. Clin. Nutr. 2012, 66, 1120–1123. [Google Scholar] [CrossRef][Green Version]
- Le Blanc, K.; Ringden, O.; Remberger, M. A low body mass index is correlated with poor survival after allogeneic stem cell transplantation. Haematologica 2003, 88, 1044–1052. [Google Scholar]
- Urbain, P.; Birlinger, J.; Ihorst, G.; Biesalski, H.K.; Finke, J.; Bertz, H. Body mass index and bioelectrical impedance phase angle as potentially modifiable nutritional markers are independent risk factors for outcome in allogeneic hematopoietic cell transplantation. Ann. Hematol. 2013, 92, 111–119. [Google Scholar] [CrossRef]
- Lange, B.J.; Gerbing, R.B.; Feusner, J.; Skolnik, J.; Sacks, N.; Smith, F.O.; Alonzo, T.A. Mortality in overweight and underweight children with acute myeloid leukemia. JAMA 2005, 293, 203–211. [Google Scholar] [CrossRef]
- Medeiros, B.C.; Othus, M.; Estey, E.H.; Fang, M.; Appelbaum, F.R. Impact of body-mass index on the outcome of adult patients with acute myeloid leukemia. Haematologica 2012, 97, 1401–1404. [Google Scholar] [CrossRef]
- Yang, J.; Xue, S.L.; Zhang, X.; Zhou, Y.N.; Qin, L.Q.; Shen, Y.P.; Wu, D.P. Effect of body mass index on overall survival of patients with allogeneic hematopoietic stem cell transplantation. Eur. J. Clin. Nutr. 2017, 71, 750–754. [Google Scholar] [CrossRef] [PubMed]
- Fuji, S.; Takano, K.; Mori, T.; Eto, T.; Taniguchi, S.; Ohashi, K.; Sakamaki, H.; Morishima, Y.; Kato, K.; Miyamura, K.; et al. Impact of pretransplant body mass index on the clinical outcome after allogeneic hematopoietic SCT. Bone Marrow Transplant. 2014, 49, 1505–1512. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, S.; Radujkovic, A.; Stolzel, F.; Falk, C.S.; Benner, A.; Schaich, M.; Bornhauser, M.; Ehninger, G.; Kramer, A.; Hegenbart, U.; et al. Pretransplant metabolic distress predicts relapse of acute myeloid leukemia after allogeneic stem cell transplantation. Transplantation 2015, 99, 1065–1071. [Google Scholar] [CrossRef] [PubMed]
- Radujkovic, A.; Becker, N.; Benner, A.; Penack, O.; Platzbecker, U.; Stolzel, F.; Bornhauser, M.; Hegenbart, U.; Ho, A.D.; Dreger, P.; et al. Pre-transplant weight loss predicts inferior outcome after allogeneic stem cell transplantation in patients with myelodysplastic syndrome. Oncotarget 2015, 6, 35095–35106. [Google Scholar] [CrossRef]
- Shimizu, H.; Shimomura, Y.; Hayashi, R.; Ohtani, K.; Sato, N.; Futawatari, T.; Mori, M. Serum leptin concentration is associated with total body fat mass, but not abdominal fat distribution. Int. J. Obes. Relat. Metab. Disord. 1997, 21, 536–541. [Google Scholar] [CrossRef]
- Elmquist, J.K.; Elias, C.F.; Saper, C.B. From lesions to leptin: Hypothalamic control of food intake and body weight. Neuron 1999, 22, 221–232. [Google Scholar] [CrossRef]
- Friedman, J.M.; Halaas, J.L. Leptin and the regulation of body weight in mammals. Nature 1998, 395, 763–770. [Google Scholar] [CrossRef]
- Elias, C.F.; Aschkenasi, C.; Lee, C.; Kelly, J.; Ahima, R.S.; Bjorbaek, C.; Flier, J.S.; Saper, C.B.; Elmquist, J.K. Leptin differentially regulates NPY and POMC neurons projecting to the lateral hypothalamic area. Neuron 1999, 23, 775–786. [Google Scholar] [CrossRef]
- Conde, J.; Scotece, M.; Abella, V.; Lopez, V.; Pino, J.; Gomez-Reino, J.J.; Gualillo, O. An update on leptin as immunomodulator. Expert Rev. Clin. Immunol. 2014, 10, 1165–1170. [Google Scholar] [CrossRef]
- Lord, G.M.; Matarese, G.; Howard, J.K.; Baker, R.J.; Bloom, S.R.; Lechler, R.I. Leptin modulates the T-cell immune response and reverses starvation-induced immunosuppression. Nature 1998, 394, 897–901. [Google Scholar] [CrossRef]
- Gratwohl, A.; Stern, M.; Brand, R.; Apperley, J.; Baldomero, H.; de Witte, T.; Dini, G.; Rocha, V.; Passweg, J.; Sureda, A.; et al. Risk score for outcome after allogeneic hematopoietic stem cell transplantation: A retrospective analysis. Cancer 2009, 115, 4715–4726. [Google Scholar] [CrossRef] [PubMed]
- Fathi, A.T.; Chen, Y.-B. Treatment of Relapse of Acute Myeloid Leukemia After Allogeneic Hematopoietic Stem Cell Transplantation. Curr. Hematol. Malig. Rep. 2014, 9, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Schmid, C.; Labopin, M.; Nagler, A.; Niederwieser, D.; Castagna, L.; Tabrizi, R.; Stadler, M.; Kuball, J.; Cornelissen, J.; Vorlicek, J.; et al. Treatment, risk factors, and outcome of adults with relapsed AML after reduced intensity conditioning for allogeneic stem cell transplantation. Blood 2012, 119, 1599–1606. [Google Scholar] [CrossRef] [PubMed]
- Schoch, C.; Kern, W.; Schnittger, S.; Hiddemann, W.; Haferlach, T. Karyotype is an independent prognostic parameter in therapy-related acute myeloid leukemia (t-AML): An analysis of 93 patients with t-AML in comparison to 1091 patients with de novo AML. Leukemia 2003, 18, 120. [Google Scholar] [CrossRef]
- Wingard, J.R.; Majhail, N.S.; Brazauskas, R.; Wang, Z.; Sobocinski, K.A.; Jacobsohn, D.; Sorror, M.L.; Horowitz, M.M.; Bolwell, B.; Rizzo, J.D.; et al. Long-term survival and late deaths after allogeneic hematopoietic cell transplantation. J. Clin. Oncol. 2011, 29, 2230–2239. [Google Scholar] [CrossRef]
- Jain, R.; Chung, S.M.; Jain, L.; Khurana, M.; Lau, S.W.; Lee, J.E.; Vaidyanathan, J.; Zadezensky, I.; Choe, S.; Sahajwalla, C.G. Implications of obesity for drug therapy: Limitations and challenges. Clin. Pharmacol. Ther. 2011, 90, 77–89. [Google Scholar] [CrossRef]
- Dewys, W.D.; Begg, C.; Lavin, P.T.; Band, P.R.; Bennett, J.M.; Bertino, J.R.; Cohen, M.H.; Douglass, H.O., Jr.; Engstrom, P.F.; Ezdinli, E.Z.; et al. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am. J. Med. 1980, 69, 491–497. [Google Scholar] [CrossRef]
- Mangili, A.; Murman, D.H.; Zampini, A.M.; Wanke, C.A. Nutrition and HIV infection: Review of weight loss and wasting in the era of highly active antiretroviral therapy from the nutrition for healthy living cohort. Clin. Infect. Dis. 2006, 42, 836–842. [Google Scholar] [CrossRef]
- Zhao, Y.; Sun, R.; You, L.; Gao, C.; Tian, Z. Expression of leptin receptors and response to leptin stimulation of human natural killer cell lines. Biochem. Biophys. Res. Commun. 2003, 300, 247–252. [Google Scholar] [CrossRef]
- De Rosa, V.; Procaccini, C.; Cali, G.; Pirozzi, G.; Fontana, S.; Zappacosta, S.; La Cava, A.; Matarese, G. A key role of leptin in the control of regulatory T cell proliferation. Immunity 2007, 26, 241–255. [Google Scholar] [CrossRef]
- Vadacca, M.; Margiotta, D.P.; Navarini, L.; Afeltra, A. Leptin in immuno-rheumatological diseases. Cell. Mol. Immunol. 2011, 8, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Mazziotti, G.; Parkes, A.B.; Lage, M.; Premawardhana, L.D.; Casanueva, F.F.; Lazarus, J.H. High leptin levels in women developing postpartum thyroiditis. Clin. Endocrinol. 2004, 60, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Bokarewa, M.; Bokarew, D.; Hultgren, O.; Tarkowski, A. Leptin consumption in the inflamed joints of patients with rheumatoid arthritis. Ann. Rheum. Dis. 2003, 62, 952–956. [Google Scholar] [CrossRef] [PubMed]
- Busso, N.; So, A.; Chobaz-Peclat, V.; Morard, C.; Martinez-Soria, E.; Talabot-Ayer, D.; Gabay, C. Leptin signaling deficiency impairs humoral and cellular immune responses and attenuates experimental arthritis. J. Immunol. 2002, 168, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Otvos, L., Jr.; Shao, W.H.; Vanniasinghe, A.S.; Amon, M.A.; Holub, M.C.; Kovalszky, I.; Wade, J.D.; Doll, M.; Cohen, P.L.; Manolios, N.; et al. Toward understanding the role of leptin and leptin receptor antagonism in preclinical models of rheumatoid arthritis. Peptides 2011, 32, 1567–1574. [Google Scholar] [CrossRef] [PubMed]
- Amarilyo, G.; Iikuni, N.; Shi, F.D.; Liu, A.; Matarese, G.; La Cava, A. Leptin promotes lupus T-cell autoimmunity. Clin. Immunol. 2013, 149, 530–533. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.D.; Zhang, M.; Zhang, Y.J.; Liu, S.S.; Pan, H.F.; Ye, D.Q. Association between leptin and systemic lupus erythematosus. Rheumatol. Int. 2014, 34, 559–563. [Google Scholar] [CrossRef]
- Sanna, V.; Di Giacomo, A.; La Cava, A.; Lechler, R.I.; Fontana, S.; Zappacosta, S.; Matarese, G. Leptin surge precedes onset of autoimmune encephalomyelitis and correlates with development of pathogenic T cell responses. J. Clin. Investig. 2003, 111, 241–250. [Google Scholar] [CrossRef]
- Singh, U.P.; Singh, N.P.; Guan, H.; Busbee, B.; Price, R.L.; Taub, D.D.; Mishra, M.K.; Fayad, R.; Nagarkatti, M.; Nagarkatti, P.S. The emerging role of leptin antagonist as potential therapeutic option for inflammatory bowel disease. Int. Rev. Immunol. 2014, 33, 23–33. [Google Scholar] [CrossRef]
- DiCarlo, J.; Agarwal-Hashmi, R.; Shah, A.; Kim, P.; Craveiro, L.; Killen, R.; Rosenberg-Hasson, Y.; Maecker, H. Cytokine and chemokine patterns across 100 days after hematopoietic stem cell transplantation in children. J. Am. Soc. Blood Marrow Transplant. 2014, 20, 361–369. [Google Scholar] [CrossRef]
- Tauchmanova, L.; Matarese, G.; Carella, C.; De Rosa, G.; Serio, B.; Ricci, P.; Lombardi, G.; Rotoli, B.; Colao, A.; Selleri, C. High serum leptin in patients with chronic graft-versus-host disease after hematopoietic stem cell transplantation. Transplantation 2004, 78, 1376–1383. [Google Scholar] [CrossRef] [PubMed]
- Fantuzzi, G.; Faggioni, R. Leptin in the regulation of immunity, inflammation, and hematopoiesis. J. Leukoc. Biol. 2000, 68, 437–446. [Google Scholar] [PubMed]
- Stern, M.; de Wreede, L.C.; Brand, R.; van Biezen, A.; Dreger, P.; Mohty, M.; de Witte, T.M.; Kroger, N.; Ruutu, T. Sensitivity of hematological malignancies to graft-versus-host effects: An EBMT megafile analysis. Leukemia 2014, 28, 2235–2240. [Google Scholar] [CrossRef] [PubMed]
- Hahn, M.; Bottcher, S.; Dietrich, S.; Hegenbart, U.; Rieger, M.; Stadtherr, P.; Bondong, A.; Schulz, R.; Ritgen, M.; Schmitt, T.; et al. Allogeneic hematopoietic stem cell transplantation for poor-risk CLL: Dissecting immune-modulating strategies for disease eradication and treatment of relapse. Bone Marrow Transplant. 2015, 50, 1279–1285. [Google Scholar] [CrossRef]
- Horowitz, M.M.; Gale, R.P.; Sondel, P.M.; Goldman, J.M.; Kersey, J.; Kolb, H.J.; Rimm, A.A.; Ringden, O.; Rozman, C.; Speck, B.; et al. Graft-versus-leukemia reactions after bone marrow transplantation. Blood 1990, 75, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Ringdén, O.; Labopin, M.; Gorin, N.C.; Schmitz, N.; Schaefer, U.W.; Prentice, H.G.; Bergmann, L.; Jouet, J.P.; Mandelli, F.; Blaise, D.; et al. Is there a graft-versus-leukaemia effect in the absence of graft-versus-host disease in patients undergoing bone marrow transplantation for acute leukaemia? Br. J. Haematol. 2000, 111, 1130–1137. [Google Scholar] [CrossRef]
- Hino, M.; Nakao, T.; Yamane, T.; Ohta, K.; Takubo, T.; Tatsumi, N. Leptin Receptor and Leukemia. Leuk. Lymphoma 2000, 36, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Konopleva, M.; Mikhail, A.; Estrov, Z.; Zhao, S.; Harris, D.; Sanchez-Williams, G.; Kornblau, S.M.; Dong, J.; Kliche, K.-O.; Jiang, S.; et al. Expression and Function of Leptin Receptor Isoforms in Myeloid Leukemia and Myelodysplastic Syndromes: Proliferative and Anti-Apoptotic Activities. Blood 1999, 93, 1668–1676. [Google Scholar] [CrossRef]
- McLeod, C.J.; Wang, L.; Wong, C.; Jones, D.L. Stem cell dynamics in response to nutrient availability. Curr. Biol. 2010, 20, 2100–2105. [Google Scholar] [CrossRef]
- Gan, B.; Hu, J.; Jiang, S.; Liu, Y.; Sahin, E.; Zhuang, L.; Fletcher-Sananikone, E.; Colla, S.; Wang, Y.A.; Chin, L.; et al. Lkb1 regulates quiescence and metabolic homeostasis of haematopoietic stem cells. Nature 2010, 468, 701. [Google Scholar] [CrossRef]
- Nakada, D.; Saunders, T.L.; Morrison, S.J. Lkb1 regulates cell cycle and energy metabolism in haematopoietic stem cells. Nature 2010, 468, 653. [Google Scholar] [CrossRef] [PubMed]
- Weisdorf, D.; Zhang, M.J.; Arora, M.; Horowitz, M.M.; Rizzo, J.D.; Eapen, M. Graft-versus-host disease induced graft-versus-leukemia effect: Greater impact on relapse and disease-free survival after reduced intensity conditioning. J. Am. Soc. Blood Marrow Transplant. 2012, 18, 1727–1733. [Google Scholar] [CrossRef] [PubMed]
- Craddock, C.; Versluis, J.; Labopin, M.; Socie, G.; Huynh, A.; Deconinck, E.; Volin, L.; Milpied, N.; Bourhis, J.H.; Rambaldi, A.; et al. Distinct factors determine the kinetics of disease relapse in adults transplanted for acute myeloid leukaemia. J. Intern. Med. 2018, 283, 371–379. [Google Scholar] [CrossRef] [PubMed]
- Mo, X.D.; Xu, L.P.; Zhang, X.H.; Liu, D.H.; Wang, Y.; Chen, H.; Yan, C.H.; Chen, Y.H.; Han, W.; Wang, F.R.; et al. Chronic GVHD induced GVL effect after unmanipulated haploidentical hematopoietic SCT for AML and myelodysplastic syndrome. Bone Marrow Transplant. 2015, 50, 127–133. [Google Scholar] [CrossRef]
- Glucksberg, H.; Storb, R.; Fefer, A.; Buckner, C.D.; Neiman, P.E.; Clift, R.A.; Lerner, K.G.; Thomas, E.D. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation 1974, 18, 295–304. [Google Scholar] [CrossRef]
- Jagasia, M.H.; Greinix, H.T.; Arora, M.; Williams, K.M.; Wolff, D.; Cowen, E.W.; Palmer, J.; Weisdorf, D.; Treister, N.S.; Cheng, G.S.; et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: I. The 2014 Diagnosis and Staging Working Group report. J. Am. Soc. Blood Marrow Transplant. 2015, 21, 389–401.E1. [Google Scholar] [CrossRef]
- Luft, T.; Dietrich, S.; Falk, C.; Conzelmann, M.; Hess, M.; Benner, A.; Neumann, F.; Isermann, B.; Hegenbart, U.; Ho, A.D.; et al. Steroid-refractory GVHD: T-cell attack within a vulnerable endothelial system. Blood 2011, 118, 1685–1692. [Google Scholar] [CrossRef]
- Dietrich, S.; Okun, J.G.; Schmidt, K.; Falk, C.S.; Wagner, A.H.; Karamustafa, S.; Radujkovic, A.; Hegenbart, U.; Ho, A.D.; Dreger, P.; et al. High pre-transplant serum nitrate levels predict risk of acute steroid-refractory graft-versus-host disease in the absence of statin therapy. Haematologica 2014, 99, 541–547. [Google Scholar] [CrossRef]
- Dietrich, S.; Falk, C.S.; Benner, A.; Karamustafa, S.; Hahn, E.; Andrulis, M.; Hegenbart, U.; Ho, A.D.; Dreger, P.; Luft, T. Endothelial vulnerability and endothelial damage are associated with risk of graft-versus-host disease and response to steroid treatment. J. Am. Soc. Blood Marrow Transplant. 2013, 19, 22–27. [Google Scholar] [CrossRef]


| Heidelberg (Training Cohort) | Essen (Validation Cohort) | p | |
|---|---|---|---|
| n | 97 | 184 | NA |
| Year alloSCT performed | 2002–2013 | 2009–2013 | NA |
| Median Age at alloSCT (range) | 56 (19–70) | 58 (17–73) | 0.149 |
| Recipient Sex Female Male | 38 (39%) 59 (61%) | 90 (49%) 94 (51%) | 0.132 |
| Donor Sex Female Male | 22 (23%) 75 (77%) | 69 (38%) 115 (62%) | 0.016 |
| Disease entity AML ALL | 86 (89%) 11 (11%) | 184 (100%) | NA |
| HLA match Match (10/10) Mismatch | 66 (68%) 31 (32%) | 124 (67%) 60 (33%) | >0.999 |
| Conditioning MAC RIC | 16 (16%) 81 (84%) | 25 (14%) 159 (86%) | 0.594 |
| Pre-transplant ATG Given Not given | 75 (77%) 22 (23%) | 92 (50%) 92 (50%) | <0.001 |
| Disease score before alloSCT * 1 2 | 31 (32%) 66 (68%) | 97 (53%) 87 (47%) | 0.005 |
| Serum Leptin Median in pg/mL (range) | 14,924 (1518–90,212) | 8581 (91.62–92,219) | 0.001 |
| Serum Adiponectin Median in ng/mL (range) | 4971.2 (1080–20,000) | NA |
| TTR | NRM | OS | ||||
|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | |
| Pre-conditioning Leptin (per log2 increase) | 0.75 (0.59–0.96) | 0.020 | 1.63 (1.15–2.31) | 0.006 | 1.05 (0.87–1.28) | 0.589 |
| Age at transplant (per 10 years) | 1.11 (0.87–1.40) | 0.411 | 1.20 (0.83–1.74) | 0.329 | 1.14 (0.93–1.38) | 0.201 |
| HLA match match (10/10) mismatch | Ref 1.39 (0.79–2.63) | Ref 0.187 | Ref 1.27 (0.48–3.23) | Ref 0.635 | Ref 1.37 (0.79–2.44) | Ref 0.264 |
| Conditioning MAC RIC | Ref 0.72 (0.38–1.26) | Ref 0.310 | Ref 1.04 (0.43–2.51) | Ref 0.936 | Ref 0.93 (0.56–1.55) | Ref 0.774 |
| ATG Not given Given | Ref 0.46 (0.22–1.04) | Ref 0.060 | Ref 0.55(0.17–1.78) | Ref 0.320 | Ref 0.48 (0.25–0.94) | Ref 0.034 |
| Recipient sex Female Male | Ref 0.66 (0.34–1.29) | Ref 0.225 | Ref 1.88 (0.73–4.84) | Ref 0.188 | Ref 1.18 (0.69–2.01) | Ref 0.555 |
| Donor sex Female Male | Ref 0.38 (0.19–0.77) | Ref 0.007 | Ref 0.52 (0.17–1.57) | Ref 0.248 | Ref 0.42 (0.23–0.77) | Ref 0.005 |
| TTR | NRM | OS | ||||
|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | |
| Pre-conditioning Leptin (per log2 increase) | 0.84 (0.72–0.97) | 0.020 | 1.09 (0.91–1.31) | 0.359 | 0.94 (0.83–1.06) | 0.292 |
| Age at transplant (per 10 years) | 0.95 (0.76–1.17) | 0.607 | 1.21 (0.96–1.51) | 0.100 | 1.08 (0.93–1.27) | 0.315 |
| HLA match match (10/10) mismatch | Ref 1.69 (0.95–3.03) | Ref 0.075 | Ref 2.13 (1.26–3.62) | Ref 0.005 | Ref 2.14 (1.43–3.21) | Ref <0.001 |
| Conditioning MAC RIC | Ref 1.48 (0.64–3.43) | Ref 0.361 | Ref 1.84 (0.66–5.15) | Ref 0.243 | Ref 1.77 (0.89–3.55) | Ref 0.106 |
| ATG Not given given | Ref 0.98 (0.56–1.71) | Ref 0.946 | Ref 0.57 (0.34–0.96) | Ref 0.033 | Ref 0.69 (0.47–1.02) | Ref 0.061 |
| Recipient sex Female Male | Ref 0.71 (0.41–1.23) | Ref 0.218 | Ref 0.92 (0.54–1.57) | Ref 0.771 | Ref 0.70 (0.47–1.05) | Ref 0.086 |
| Donor sex Female Male | Ref 1.12 (0.62–2.01) | Ref 0.711 | Ref 0.52 (0.17–1.57) | Ref 0.248 | Ref 0.42 (0.23–0.77) | Ref 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schwarzbich, M.-A.; Dai, H.; Kordelas, L.; Beelen, D.W.; Radujkovic, A.; Müller-Tidow, C.; Dreger, P.; Luft, T. Pre-Transplant Serum Leptin Levels and Relapse of Acute Myeloid Leukemia after Allogeneic Transplantation. Int. J. Mol. Sci. 2022, 23, 2337. https://doi.org/10.3390/ijms23042337
Schwarzbich M-A, Dai H, Kordelas L, Beelen DW, Radujkovic A, Müller-Tidow C, Dreger P, Luft T. Pre-Transplant Serum Leptin Levels and Relapse of Acute Myeloid Leukemia after Allogeneic Transplantation. International Journal of Molecular Sciences. 2022; 23(4):2337. https://doi.org/10.3390/ijms23042337
Chicago/Turabian StyleSchwarzbich, Mark-Alexander, Hao Dai, Lambros Kordelas, Dietrich W. Beelen, Aleksandar Radujkovic, Carsten Müller-Tidow, Peter Dreger, and Thomas Luft. 2022. "Pre-Transplant Serum Leptin Levels and Relapse of Acute Myeloid Leukemia after Allogeneic Transplantation" International Journal of Molecular Sciences 23, no. 4: 2337. https://doi.org/10.3390/ijms23042337
APA StyleSchwarzbich, M.-A., Dai, H., Kordelas, L., Beelen, D. W., Radujkovic, A., Müller-Tidow, C., Dreger, P., & Luft, T. (2022). Pre-Transplant Serum Leptin Levels and Relapse of Acute Myeloid Leukemia after Allogeneic Transplantation. International Journal of Molecular Sciences, 23(4), 2337. https://doi.org/10.3390/ijms23042337







