The Latest Evidence of Erythropoietin in the Treatment of Glaucoma
Abstract
1. Introduction and the Relation between Glaucoma and EPO
2. EPO/EPOR System and Its Potential Neuroprotective Function
3. Therapeutic Effect of EPO in Glaucoma/RGC Survival Studies
3.1. Mechanical Optic Nerve Injury
3.2. Episcleral Vessel Cautery-Induced Glaucoma Model
3.3. Model of Anterior Chamber Cannulation and IOP Elevation
3.4. Oligemia by Bilateral Common Carotid Artery Occlusion (BCCAO)
3.5. Mouse Strain Prone to Develop Glaucoma
3.6. Molecule-Induced Retinal Toxicity
3.7. Microbeads-Induced Glaucoma Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tham, Y.C.; Li, X.; Wong, T.Y.; Quigley, H.A.; Aung, T.; Cheng, C.Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040: A systematic review and meta-analysis. Ophthalmology 2014, 121, 2081–2090. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.W.; Chan, N.C.Y.; Sadun, A.A. Glaucoma as Neurodegeneration in the Brain. Eye Brain 2021, 13, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.K.; Kee, C. Population-based glaucoma prevalence studies in Asians. Surv. Ophthalmol. 2014, 59, 434–447. [Google Scholar] [CrossRef] [PubMed]
- Schuster, A.K.; Erb, C.; Hoffmann, E.M.; Dietlein, T.; Pfeiffer, N. The Diagnosis and Treatment of Glaucoma. Dtsch. Arztebl. Int. 2020, 117, 225–234. [Google Scholar] [CrossRef]
- Rey, F.; Balsari, A.; Giallongo, T.; Ottolenghi, S.; Di Giulio, A.M.; Samaja, M.; Carelli, S. Erythropoietin as a Neuroprotective Molecule: An Overview of Its Therapeutic Potential in Neurodegenerative Diseases. ASN Neuro 2019, 11, 1759091419871420. [Google Scholar] [CrossRef]
- García-Ramírez, M.; Hernández, C.; Simó, R. Expression of erythropoietin and its receptor in the human retina: A comparative study of diabetic and nondiabetic subjects. Diabetes Care 2008, 31, 1189–1194. [Google Scholar] [CrossRef]
- Shah, S.S.; Tsang, S.H.; Mahajan, V.B. Erythropoetin receptor expression in the human diabetic retina. BMC Res. Notes 2009, 2, 234. [Google Scholar] [CrossRef]
- Becerra, S.P.; Amaral, J. Erythropoietin--an endogenous retinal survival factor. N. Engl. J. Med. 2002, 347, 1968–1970. [Google Scholar] [CrossRef]
- Junk, A.K.; Mammis, A.; Savitz, S.I.; Singh, M.; Roth, S.; Malhotra, S.; Rosenbaum, P.S.; Cerami, A.; Brines, M.; Rosenbaum, D.M. Erythropoietin administration protects retinal neurons from acute ischemia-reperfusion injury. Proc. Natl. Acad. Sci. USA 2002, 99, 10659–10664. [Google Scholar] [CrossRef]
- Zhong, Y.; Yao, H.; Deng, L.; Cheng, Y.; Zhou, X. Promotion of neurite outgrowth and protective effect of erythropoietin on the retinal neurons of rats. Graefes Arch. Clin. Exp. Ophthalmol. 2007, 245, 1859–1867. [Google Scholar] [CrossRef]
- Tezel, G.; Yang, X.; Luo, C.; Cai, J.; Kain, A.D.; Powell, D.W.; Kuehn, M.H.; Pierce, W.M. Hemoglobin expression and regulation in glaucoma: Insights into retinal ganglion cell oxygenation. Investig. Ophthalmol. Vis. Sci. 2010, 51, 907–919. [Google Scholar] [CrossRef] [PubMed]
- Cumurcu, T.; Bulut, Y.; Demir, H.D.; Yenisehirli, G. Aqueous humor erythropoietin levels in patients with primary open-angle glaucoma. J. Glaucoma 2007, 16, 645–648. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.Y.; Zhao, K.K.; Zhao, P.Q. Erythropoietin is increased in aqueous humor of glaucomatous eyes. Curr. Eye Res. 2010, 35, 680–684. [Google Scholar] [CrossRef] [PubMed]
- Nassiri, N.; Nassiri, N.; Majdi, M.; Mehrjardi, H.Z.; Shakiba, Y.; Haghnegahdar, M.; Heidari, A.B.; Djalilian, A.R.; Mirahmadian, M. Erythropoietin levels in aqueous humor of patients with glaucoma. Mol. Vis. 2012, 18, 1991–1995. [Google Scholar] [PubMed]
- Sun, C.; Zhang, H.; Tang, Y.; Chen, Y.; Li, Y.; Nie, C.; Gu, J.; Luo, L.; Wang, Z. Aqueous Inflammation and Ischemia-Related Biomarkers in Neovascular Glaucoma with Stable Iris Neovascularization. Curr. Eye Res. 2020, 45, 1504–1513. [Google Scholar] [CrossRef]
- Tezel, G.; Wax, M.B. Hypoxia-Inducible Factor 1α in the Glaucomatous Retina and OpticNerve Head. Arch. Ophthalmol. 2004, 122, 1348–1356. [Google Scholar] [CrossRef]
- Jelkmann, W. Erythropoietin: Structure, control of production, and function. Physiol. Rev. 1992, 72, 449–489. [Google Scholar] [CrossRef]
- Bhoopalan, S.V.; Huang, L.J.; Weiss, M.J. Erythropoietin regulation of red blood cell production: From bench to bedside and back. F1000Research 2020, 9, 1153. [Google Scholar] [CrossRef]
- Zeisberg, M.; Kalluri, R. Physiology of the Renal Interstitium. Clin. J. Am. Soc. Nephrol. 2015, 10, 1831–1840. [Google Scholar] [CrossRef]
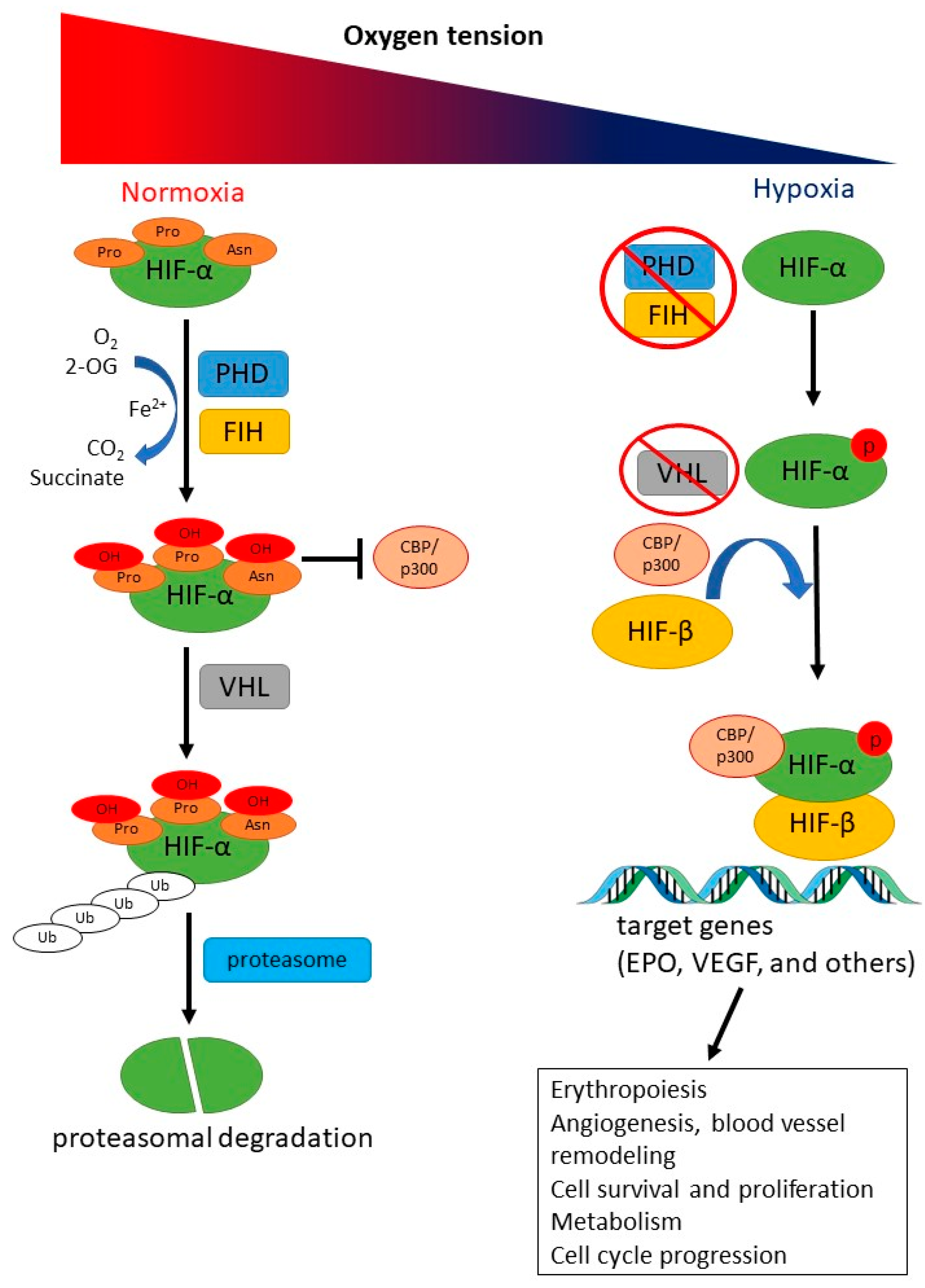
- Semenza, G.L.; Nejfelt, M.K.; Chi, S.M.; Antonarakis, S.E. Hypoxia-inducible nuclear factors bind to an enhancer element located 3’ to the human erythropoietin gene. Proc. Natl. Acad. Sci. USA 1991, 88, 5680–5684. [Google Scholar] [CrossRef]
- Maxwell, P.H.; Wiesener, M.S.; Chang, G.W.; Clifford, S.C.; Vaux, E.C.; Cockman, M.E.; Wykoff, C.C.; Pugh, C.W.; Maher, E.R.; Ratcliffe, P.J. The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature 1999, 399, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Tirpe, A.A.; Gulei, D.; Ciortea, S.M.; Crivii, C.; Berindan-Neagoe, I. Hypoxia: Overview on Hypoxia-Mediated Mechanisms with a Focus on the Role of HIF Genes. Int. J. Mol. Sci. 2019, 20, 6140. [Google Scholar] [CrossRef]
- Eales, K.L.; Hollinshead, K.E.; Tennant, D.A. Hypoxia and metabolic adaptation of cancer cells. Oncogenesis 2016, 5, e190. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.L.; Jiang, B.H.; Rue, E.A.; Semenza, G.L. Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc. Natl. Acad. Sci. USA 1995, 92, 5510–5514. [Google Scholar] [CrossRef] [PubMed]
- Jiang, B.H.; Semenza, G.L.; Bauer, C.; Marti, H.H. Hypoxia-inducible factor 1 levels vary exponentially over a physiologically relevant range of O2 tension. Am. J. Physiol. 1996, 271, C1172–C1180. [Google Scholar] [CrossRef] [PubMed]
- Haase, V.H. Regulation of erythropoiesis by hypoxia-inducible factors. Blood Rev. 2013, 27, 41–53. [Google Scholar] [CrossRef]
- Lando, D.; Peet, D.J.; Gorman, J.J.; Whelan, D.A.; Whitelaw, M.L.; Bruick, R.K. FIH-1 is an asparaginyl hydroxylase enzyme that regulates the transcriptional activity of hypoxia-inducible factor. Genes Dev. 2002, 16, 1466–1471. [Google Scholar] [CrossRef]
- Constantinescu, S.N.; Ghaffari, S.; Lodish, H.F. The Erythropoietin Receptor: Structure, Activation and Intracellular Signal Transduction. Trends Endocrinol. Metab. 1999, 10, 18–23. [Google Scholar] [CrossRef]
- McGraw, K.; List, A. Chapter Five—Erythropoietin Receptor Signaling and Lipid Rafts. In Vitamins and Hormones; Litwack, G., Ed.; Academic Press: Cambridge, MA, USA, 2017; Volume 105, pp. 79–100. [Google Scholar]
- Watowich, S.S. The erythropoietin receptor: Molecular structure and hematopoietic signaling pathways. J. Investig. Med. 2011, 59, 1067–1072. [Google Scholar] [CrossRef]
- Juul, S.E.; Pet, G.C. Erythropoietin and Neonatal Neuroprotection. Clin. Perinatol. 2015, 42, 469–481. [Google Scholar] [CrossRef]
- Koury, M.J.; Bondurant, M.C.; Atkinson, J.B. Erythropoietin control of terminal erythroid differentiation: Maintenance of cell viability, production of hemoglobin, and development of the erythrocyte membrane. Blood Cells 1987, 13, 217–226. [Google Scholar] [PubMed]
- Wojchowski, D.M.; Sathyanarayana, P.; Dev, A. Erythropoietin receptor response circuits. Curr. Opin. Hematol. 2010, 17, 169–176. [Google Scholar] [CrossRef]
- Anagnostou, A.; Liu, Z.; Steiner, M.; Chin, K.; Lee, E.S.; Kessimian, N.; Noguchi, C.T. Erythropoietin receptor mRNA expression in human endothelial cells. Proc. Natl. Acad. Sci. USA 1994, 91, 3974–3978. [Google Scholar] [CrossRef] [PubMed]
- Farrell, F.; Lee, A. The erythropoietin receptor and its expression in tumor cells and other tissues. Oncologist 2004, 9 (Suppl. 5), 18–30. [Google Scholar] [CrossRef] [PubMed]
- Ostrowski, D.; Heinrich, R. Alternative Erythropoietin Receptors in the Nervous System. J. Clin. Med. 2018, 7, 24. [Google Scholar] [CrossRef] [PubMed]
- Bretz, C.A.; Ramshekar, A.; Kunz, E.; Wang, H.; Hartnett, M.E. Signaling Through the Erythropoietin Receptor Affects Angiogenesis in Retinovascular Disease. Investig. Ophthalmol. Vis. Sci. 2020, 61, 23. [Google Scholar] [CrossRef]
- Katavetin, P.; Tungsanga, K.; Eiam-Ong, S.; Nangaku, M. Antioxidative effects of erythropoietin. Kidney Int. Suppl. 2007, 72, S10–S15. [Google Scholar] [CrossRef]
- Bond, W.S.; Rex, T.S. Evidence That Erythropoietin Modulates Neuroinflammation through Differential Action on Neurons, Astrocytes, and Microglia. Front. Immunol. 2014, 5, 523. [Google Scholar] [CrossRef]
- Vittori, D.C.; Chamorro, M.E.; Hernández, Y.V.; Maltaneri, R.E.; Nesse, A.B. Erythropoietin and derivatives: Potential beneficial effects on the brain. J. Neurochem. 2021, 158, 1032–1057. [Google Scholar] [CrossRef]
- Iwata, Y.; Sakai, N.; Nakajima, Y.; Oshima, M.; Nakagawa-Yoneda, S.; Ogura, H.; Sato, K.; Minami, T.; Kitajima, S.; Toyama, T.; et al. Anti-fibrotic potential of erythropoietin signaling on bone marrow derived fibrotic cell. BMC Nephrol. 2021, 22, 203. [Google Scholar] [CrossRef]
- Pradeep, S.; Huang, J.; Mora, E.M.; Nick, A.M.; Cho, M.S.; Wu, S.Y.; Noh, K.; Pecot, C.V.; Rupaimoole, R.; Stein, M.A.; et al. Erythropoietin Stimulates Tumor Growth via EphB4. Cancer Cell 2015, 28, 610–622. [Google Scholar] [CrossRef] [PubMed]
- Marcuzzi, F.; Zucchelli, S.; Bertuzzi, M.; Santoro, C.; Tell, G.; Carninci, P.; Gustincich, S. Isoforms of the Erythropoietin receptor in dopaminergic neurons of the Substantia Nigra. J. Neurochem. 2016, 139, 596–609. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Yang, B. Erythropoietin Receptor/β Common Receptor: A Shining Light on Acute Kidney Injury Induced by Ischemia-Reperfusion. Front. Immunol. 2021, 12, 697796. [Google Scholar] [CrossRef]
- Grasso, G.; Sfacteria, A.; Cerami, A.; Brines, M. Erythropoietin as a tissue-protective cytokine in brain injury: What do we know and where do we go? Neuroscientist 2004, 10, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Brines, M.; Grasso, G.; Fiordaliso, F.; Sfacteria, A.; Ghezzi, P.; Fratelli, M.; Latini, R.; Xie, Q.W.; Smart, J.; Su-Rick, C.J.; et al. Erythropoietin mediates tissue protection through an erythropoietin and common beta-subunit heteroreceptor. Proc. Natl. Acad. Sci. USA 2004, 101, 14907–14912. [Google Scholar] [CrossRef]
- Colella, P.; Iodice, C.; Di Vicino, U.; Annunziata, I.; Surace, E.M.; Auricchio, A. Non-erythropoietic erythropoietin derivatives protect from light-induced and genetic photoreceptor degeneration. Hum. Mol. Genet. 2011, 20, 2251–2262. [Google Scholar] [CrossRef]
- Vizcardo-Galindo, G.; León-Velarde, F.; Villafuerte, F.C. High-Altitude Hypoxia Decreases Plasma Erythropoietin Soluble Receptor Concentration in Lowlanders. High Alt. Med. Biol. 2020, 21, 92–98. [Google Scholar] [CrossRef]
- Brines, M.L.; Ghezzi, P.; Keenan, S.; Agnello, D.; de Lanerolle, N.C.; Cerami, C.; Itri, L.M.; Cerami, A. Erythropoietin crosses the blood-brain barrier to protect against experimental brain injury. Proc. Natl. Acad. Sci. USA 2000, 97, 10526–10531. [Google Scholar] [CrossRef]
- Grimm, C.; Wenzel, A.; Groszer, M.; Mayser, H.; Seeliger, M.; Samardzija, M.; Bauer, C.; Gassmann, M.; Remé, C.E. HIF-1-induced erythropoietin in the hypoxic retina protects against light-induced retinal degeneration. Nat. Med. 2002, 8, 718–724. [Google Scholar] [CrossRef]
- Weishaupt, J.H.; Rohde, G.; Pölking, E.; Siren, A.L.; Ehrenreich, H.; Bähr, M. Effect of erythropoietin axotomy-induced apoptosis in rat retinal ganglion cells. Investig. Ophthalmol. Vis. Sci. 2004, 45, 1514–1522. [Google Scholar] [CrossRef]
- Kilic, U.; Kilic, E.; Soliz, J.; Bassetti, C.I.; Gassmann, M.; Hermann, D.M. Erythropoietin protects from axotomy-induced degeneration of retinal ganglion cells by activating ERK-1/-2. Faseb J. 2005, 19, 249–251. [Google Scholar] [CrossRef]
- King, C.E.; Rodger, J.; Bartlett, C.; Esmaili, T.; Dunlop, S.A.; Beazley, L.D. Erythropoietin is both neuroprotective and neuroregenerative following optic nerve transection. Exp. Neurol. 2007, 205, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Rong, X.; Mo, X.; Ren, T.; Yang, S.; Yuan, W.; Dong, J.; Wang, Y.; Wang, X. Neuroprotective effect of erythropoietin-loaded composite microspheres on retinal ganglion cells in rats. Eur. J. Pharm. Sci. 2011, 43, 334–342. [Google Scholar] [CrossRef]
- Tan, H.; Kang, X.; Zhong, Y.; Shen, X.; Cheng, Y.; Jiao, Q.; Deng, L. Erythropoietin upregulates growth associated protein-43 expression and promotes retinal ganglion cell axonal regeneration in vivo after optic nerve crush. Neural Regen. Res. 2012, 7, 295–301. [Google Scholar] [CrossRef]
- Tsai, J.C.; Wu, L.; Worgul, B.; Forbes, M.; Cao, J. Intravitreal administration of erythropoietin and preservation of retinal ganglion cells in an experimental rat model of glaucoma. Curr. Eye Res. 2005, 30, 1025–1031. [Google Scholar] [CrossRef]
- Fu, Q.L.; Wu, W.; Wang, H.; Li, X.; Lee, V.W.; So, K.F. Up-regulated endogenous erythropoietin/erythropoietin receptor system and exogenous erythropoietin rescue retinal ganglion cells after chronic ocular hypertension. Cell. Mol. Neurobiol. 2008, 28, 317–329. [Google Scholar] [CrossRef]
- Resende, A.P.; Rosolen, S.G.; Nunes, T.; São Braz, B.; Delgado, E. Functional and Structural Effects of Erythropoietin Subconjunctival Administration in Glaucomatous Animals. Biomed. Hub 2018, 3, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Y.S.; Liu, X.H.; Cheng, Y.; Min, Y.J. Erythropoietin with retrobulbar administration protects retinal ganglion cells from acute elevated intraocular pressure in rats. J. Ocul. Pharmacol. Ther. 2008, 24, 453–459. [Google Scholar] [CrossRef]
- Jehle, T.; Meschede, W.; Dersch, R.; Feltgen, N.; Bach, M.; Lagrèze, W.A. Erythropoietin protects retinal ganglion cells and visual function after ocular ischemia and optic nerve compression. Ophthalmologe 2010, 107, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, L.A.; Fleming, R.; Sant’Anna, M.; Guimarães, R.; Dantas, A.M.; Morizot-Leite, E.; Cavalcante, L.A.; Allodi, S. Neuroprotective effects of erythropoietin on rat retinas subjected to oligemia. Clinics 2018, 73, e161. [Google Scholar] [CrossRef]
- Zhou, Y.; Sun, B.; Guo, J.; Zhou, G. Intranasal injection of recombinant human erythropoietin improves cognitive and visual impairments in chronic cerebral ischemia rats. Biomed. Rep. 2020, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- Zhong, L.; Bradley, J.; Schubert, W.; Ahmed, E.; Adamis, A.P.; Shima, D.T.; Robinson, G.S.; Ng, Y.S. Erythropoietin promotes survival of retinal ganglion cells in DBA/2J glaucoma mice. Investig. Ophthalmol. Vis. Sci. 2007, 48, 1212–1218. [Google Scholar] [CrossRef] [PubMed]
- Yamasaki, M.; Mishima, H.K.; Yamashita, H.; Kashiwagi, K.; Murata, K.; Minamoto, A.; Inaba, T. Neuroprotective effects of erythropoietin on glutamate and nitric oxide toxicity in primary cultured retinal ganglion cells. Brain Res. 2005, 1050, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Chang, Z.Y.; Yeh, M.K.; Chiang, C.H.; Chen, Y.H.; Lu, D.W. Erythropoietin protects adult retinal ganglion cells against NMDA-, trophic factor withdrawal-, and TNF-α-induced damage. PLoS ONE 2013, 8, e55291. [Google Scholar] [CrossRef]
- Cheng, W.-S.; Lin, I.H.; Feng, K.M.; Chang, Z.-Y.; Huang, Y.C.; Lu, D.-W. Neuroprotective effects of exogenous erythropoietin in Wistar rats by downregulating apoptotic factors to attenuate N-methyl-D-aspartate-mediated retinal ganglion cells death. PLoS ONE 2020, 15, e0223208. [Google Scholar] [CrossRef]
- Rex, T.S.; Naguib, S.; Backstrom, J.; DeJulius, C.; Artis, E.; Duvall, C. Intraocular sustained release of EPO-R76E mitigates glaucoma pathogenesis by activating the NRF2/ARE pathway in a mouse model of glaucoma. Investig. Ophthalmol. Vis. Sci. 2022, 63, 1138. [Google Scholar]
- Resende, A.P.; São Braz, B.; Delgado, E. Ocular Erythropoietin Penetration after Subconjunctival Administration in Glaucomatous Rats. Ophthalmic Res. 2016, 56, 104–110. [Google Scholar] [CrossRef]
- Bernaudin, M.; Marti, H.H.; Roussel, S.; Divoux, D.; Nouvelot, A.; MacKenzie, E.T.; Petit, E. A potential role for erythropoietin in focal permanent cerebral ischemia in mice. J. Cereb. Blood Flow Metab. 1999, 19, 643–651. [Google Scholar] [CrossRef]
- Sirén, A.L.; Fratelli, M.; Brines, M.; Goemans, C.; Casagrande, S.; Lewczuk, P.; Keenan, S.; Gleiter, C.; Pasquali, C.; Capobianco, A.; et al. Erythropoietin prevents neuronal apoptosis after cerebral ischemia and metabolic stress. Proc. Natl. Acad. Sci. USA 2001, 98, 4044–4049. [Google Scholar] [CrossRef]
- Aktas, Z.; Unlu, M.; Uludag, K.; Erten, Y.; Hasanreisoglu, B. The effect of systemic erythropoietin treatment on retinal nerve fiber layer parameters in patients with chronic renal failure undergoing peritoneal dialysis. J. Glaucoma 2015, 24, 214–218. [Google Scholar] [CrossRef]
- Hemani, S.; Lane, O.; Agarwal, S.; Yu, S.P.; Woodbury, A. Systematic Review of Erythropoietin (EPO) for Neuroprotection in Human Studies. Neurochem. Res. 2021, 46, 732–739. [Google Scholar] [CrossRef] [PubMed]
- Singbartl, G. Adverse events of erythropoietin in long-term and in acute/short-term treatment. Clin. Investig. 1994, 72, S36–S43. [Google Scholar] [PubMed]
- Torup, L.; Leist, M. Development of non-erythropoietic erythropoietin variants for neuroprotection. In Erythropoietin and the Nervous System; Springer: Berlin/Heidelberg, Germany, 2006; pp. 211–219. [Google Scholar]
- Ribatti, D.; Presta, M.; Vacca, A.; Ria, R.; Giuliani, R.; Dell’Era, P.; Nico, B.; Roncali, L.; Dammacco, F. Human erythropoietin induces a pro-angiogenic phenotype in cultured endothelial cells and stimulates neovascularization in vivo. Blood 1999, 93, 2627–2636. [Google Scholar] [CrossRef] [PubMed]
- Annese, T.; Tamma, R.; Ruggieri, S.; Ribatti, D. Erythropoietin in tumor angiogenesis. Exp. Cell Res. 2019, 374, 266–273. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, D.; Suzuma, K.; Matsui, S.; Kurimoto, M.; Kiryu, J.; Kita, M.; Suzuma, I.; Ohashi, H.; Ojima, T.; Murakami, T.; et al. Erythropoietin as a retinal angiogenic factor in proliferative diabetic retinopathy. N. Engl. J. Med. 2005, 353, 782–792. [Google Scholar] [CrossRef]
- Wen, C.T.; He, T.; Xing, Y.Q. Erythropoietin promotes retinal angiogenesis in a mouse model. Mol. Med. Rep. 2014, 10, 2979–2984. [Google Scholar] [CrossRef][Green Version]
- Yang, Z.; Wang, H.; Jiang, Y.; Hartnett, M.E. VEGFA activates erythropoietin receptor and enhances VEGFR2-mediated pathological angiogenesis. Am. J. Pathol. 2014, 184, 1230–1239. [Google Scholar] [CrossRef]
- Chen, J.; Connor, K.M.; Aderman, C.M.; Smith, L.E. Erythropoietin deficiency decreases vascular stability in mice. J. Clin. Investig. 2008, 118, 526–533. [Google Scholar] [CrossRef]
- Silva, M.; Benito, A.; Sanz, C.; Prosper, F.; Ekhterae, D.; Nuñez, G.; Fernandez-Luna, J.L. Erythropoietin can induce the expression of bcl-x(L) through Stat5 in erythropoietin-dependent progenitor cell lines. J. Biol. Chem. 1999, 274, 22165–22169. [Google Scholar] [CrossRef]
- Wen, T.C.; Sadamoto, Y.; Tanaka, J.; Zhu, P.X.; Nakata, K.; Ma, Y.J.; Hata, R.; Sakanaka, M. Erythropoietin protects neurons against chemical hypoxia and cerebral ischemic injury by up-regulating Bcl-xL expression. J. Neurosci. Res. 2002, 67, 795–803. [Google Scholar] [CrossRef]
- Digicaylioglu, M.; Lipton, S.A. Erythropoietin-mediated neuroprotection involves cross-talk between Jak2 and NF-κB signalling cascades. Nature 2001, 412, 641–647. [Google Scholar] [CrossRef]
- Gui, D.M.; Yang, Y.; Li, X.; Gao, D.W. Effect of erythropoietin on the expression of HIF-1 and iNOS in retina in chronic ocular hypertension rats. Int. J. Ophthalmol. 2011, 4, 40–43. [Google Scholar] [CrossRef]
- Kang, J.Q.; Chong, Z.Z.; Maiese, K. Akt1 protects against inflammatory microglial activation through maintenance of membrane asymmetry and modulation of cysteine protease activity. J. Neurosci. Res. 2003, 74, 37–51. [Google Scholar] [CrossRef]
- Kang, J.Q.; Chong, Z.Z.; Maiese, K. Critical role for Akt1 in the modulation of apoptotic phosphatidylserine exposure and microglial activation. Mol. Pharmacol. 2003, 64, 557–569. [Google Scholar] [CrossRef]
- Rex, T.S.; Wong, Y.; Kodali, K.; Merry, S. Neuroprotection of photoreceptors by direct delivery of erythropoietin to the retina of the retinal degeneration slow mouse. Exp. Eye Res. 2009, 89, 735–740. [Google Scholar] [CrossRef]
- Sullivan, T.A.; Geisert, E.E.; Hines-Beard, J.; Rex, T.S. Systemic adeno-associated virus-mediated gene therapy preserves retinal ganglion cells and visual function in DBA/2J glaucomatous mice. Hum. Gene Ther. 2011, 22, 1191–1200. [Google Scholar] [CrossRef]
- Guan, Y.; Cui, L.; Qu, Z.; Lu, L.; Wang, F.; Wu, Y.; Zhang, J.; Gao, F.; Tian, H.; Xu, L.; et al. Subretinal transplantation of rat MSCs and erythropoietin gene modified rat MSCs for protecting and rescuing degenerative retina in rats. Curr. Mol. Med. 2013, 13, 1419–1431. [Google Scholar] [CrossRef]
- Rhee, J.; Shih, K.C. Use of Gene Therapy in Retinal Ganglion Cell Neuroprotection: Current Concepts and Future Directions. Biomolecules 2021, 11, 581. [Google Scholar] [CrossRef]
- Bond, W.S.; Hines-Beard, J.; GoldenMerry, Y.L.; Davis, M.; Farooque, A.; Sappington, R.M.; Calkins, D.J.; Rex, T.S. Virus-mediated EpoR76E Therapy Slows Optic Nerve Axonopathy in Experimental Glaucoma. Mol. Ther. 2016, 24, 230–239. [Google Scholar] [CrossRef]
- Hines-Beard, J.; Bond, W.S.; Backstrom, J.R.; Rex, T.S. Virus-mediated EpoR76E gene therapy preserves vision in a glaucoma model by modulating neuroinflammation and decreasing oxidative stress. J. Neuroinflamm. 2016, 13, 39. [Google Scholar] [CrossRef]
| Injury Model | Study Design | Methods | Sample Size | Authors | Year | Main Results and Remarks |
|---|---|---|---|---|---|---|
| Mechanical optic nerve injury | ||||||
| Optic nerve transection | Intervention study | Groups: (1) Axotomy + vehicle (2) Axotomy + 0.5 U rhEPO (3) Axotomy + 1 U rhEPO (4) Axotomy + 2 U rhEPO (5) Axotomy + 4 U rhEPO (6) Axotomy + 8 U rhEPO (7) Axotomy +2 U rhEPO + 0.1 mM Wortmannin Intravitreal injections (IVI) on days 0, 4, 7, and 10 after optic nerve transection | 25 adult Sprague–Dawley rats | Weishaupt et al. [51] | 2004 |
|
| Optic nerve transection | Comparative study | Comparison between tg21 mice versus wild-type mice 14 days after axotomy | 5–6 animals per strain for tissue processing | Kilic et al. [52] | 2005 |
|
| Optic nerve transection | Intervention study | Optic nerve transection: (1) IVI of 5 units of EPO (2) IVI of 10 units of EPO (3) IVI of 25 units of EPO (4) IVI of 50 units of EPO (5) IVI of PBS Optic nerve transection + peripheral nerve grafting: (1) IVI of 25 units of EPO (2) IVI of PBS | 58 PVG hooded rats | King et al. [53] | 2007 |
|
| Optic nerve crush | Intervention study | Groups: (1) no treatment (2) single intraperitoneal (i.p.) injection of 20 mg EPO-loaded PLGA/PLA microspheres (corresponding to 24,000 IU/kg EPO) (3) single i.p. injection of 20 mg blank PLGA/PLA microspheres (4) i.p. injection of EPO (3000 IU/kg BW) every week (5) i.p. injection of 0.01 M PBS every week | 7 adult Sprague– Dawley rats/each group | Rong et al. [54] | 2011 |
|
| Optic nerve crush | Randomized, controlled, animal experiment | Groups: (1) sham-surgery group (2) IVI of 3.5 µL (6 U) EPO (3) IVI of 3.5 µL PBS IVI for 4 times: immediate (day 0), days 3, 6, and 9 | 72 adult Sprague–Dawley rats | Tan et al. [55] | 2012 |
|
| Episcleral vessel cautery-induced glaucoma model | ||||||
| Episcleral venous cautery | Intervention study | Groups: (1) unoperated controls (2) episcleral vessel cautery only (EVC) (3) EVC + IVI of normal saline (EVC-NS) (4) EVC + IVI of recombinant rat EPO (EVC-EPO) | 29 adult Sprague–Dawley rats (11 controls, 4 EVC, 5 EVC-NS, 9 EVC-EPO) | Tsai et al. [56] | 2005 |
|
| 1. Argon laser photocoagulation of episcleral and limbal veins 2. Optic nerve transection | Intervention study | Groups: (1) IVI of PBS (2) IVI of 2 μl sEPOR (20 ng) (3) IVI of 2U Epoetin alpha at 0, 4, 7, and 11 days after the injury (4) i.p. injection of 5000 units (42 μg, 1 mL) Epoetin alpha/kg (5) i.p. injection of normal saline 24 h before and 30 min before the injury * Chronic glaucoma model:(1)–(5); Optic nerve transection model:(4), (5) | adult Sprague–Dawley rats (n = 8/experiment group) | Fu et al. [57] | 2007 |
|
| Coagulation of episcleral veins | Intervention study | Groups: (1) subconjunctival injection of 1000 IU of rhEPO (2) subconjunctival injection of equal volume of saline | 26 Wistar Hannover albino rats | Resende et al. [58] | 2018 |
|
| Model of anterior chamber cannulation and IOP elevation | ||||||
| Cannulated anterior chamber (AC) and raised IOP to 120 mmHg for up to 60 min | Intervention study | Groups: (1) IVI of 2 ng sEPOR (2) IVI of 20 ng sEPOR (3) IVI of saline just before the induction of ischemia. (4) i.p. injection of 5000 units/kg rhEPO (5) i.p. injection of normal saline 24 h before and just before the onset of ischemia (6) i.p. injection of 5000 units/kg rhEPO immediately after the onset of ischemia | 61 Sprague–Dawley rats | Junk et al. [9] | 2002 |
|
| Cannulated AC and raised IOP to 70 or 15 (sham-operated group) mmHg for up to 60 min | Intervention study | Groups: (1) untouched control (2) sham-operated (3) acute elevated IOP (4) acute elevated IOP + immediate retrobulbar injection of 100 μL rhEPO (1000 units) (5) acute elevated IOP + immediate retrobulbar injection of 100 μL vehicle solution | 75 Sprague–Dawley rats | Zhong et al. [59] | 2008 |
|
| 1. The IOP was raised to 120 mmHg for 55 min 2. Optic nerve compression for 10 s | Intervention study | Groups: (1) IVI of PBS (2) IVI of 2U EPO (3) IVI of 20 U EPO For EPO safety evaluation: (1) IVI of 5 μL BSS (2) IVI of 5 U EPO (3) IVI of 50 U EPO (4) IVI of 200 U EPO | Brown Norway rats (n = 9–21 in elevate IOP, and n = 6–8 in optic nerve compression; n = 6–7 for safety evaluation) | Jehle et al. [60] | 2010 |
|
| Oligemia by bilateral common carotid artery occlusion (BCCAO) | ||||||
| BCCAO | Intervention study | Groups: (1) sham-operated group (2) BCCAO only (3) BCCAO + IVI of 1 μL PBS 2 days later (4) BCCAO + IVI of 1 μL EPO (400 μg) 2 days later | 30 adult Wistar rats (n = 5 in sham and BCCAO only group) | Carvalho et al. [61] | 2018 |
|
| BCCAO | Intervention study | Groups: (1) sham-operated+ intranasal saline (2) BCCAO + intranasal saline (3) BCCAO + intranasal rhEPO (50 U/100 g/week for 8 weeks) | 90 Sprague–Dawley rats (n = 30/group)) | Zhou et al. [62] | 2020 |
|
| Mouse strain prone to develop glaucoma | ||||||
| The DBA/2J mice spontaneously develop glaucomatous loss of RGCs with aging. | Intervention study | Groups: (1) i.p. injection of BSA (2) i.p. injection of memantine (70 mg/kg/wk) (3) i.p. injection of rhEPO-α (3000 U/kg/wk) (4) i.p. injection of rhEPO-α(6000 U/kg/wk) (5) i.p. injection of rhEPO-α(12,000 U/kg/wk) | 294 DBA/2J mice and 91 C57BL/6J mice | Zhong et al. [63] | 2007 |
|
| Molecule-induced retinal toxicity | ||||||
| 1. Glutamate and nitric oxide toxicity 2. Cannulated AC and raised IOP to 120 mmHg for 60 min | Intervention study | *. Glutamate: (1) EPO (0.15, 0.5, and 1.5 U/mL) for 12 h + low concentration glutamate (50 and 100 μM) for 48 h (2) EPO (0.15, 0.5, and 1.5 U/mL) for 12 h + high concentration glutamate (1 and 10 mM) for 24 h *. Nitric oxide: EPO (1.5 U/mL) for 12 h + SNP(10, 100, and 500 μM) for 6 h *. Immunohistochemical analysis: right eye (operated eye), left eye (sham operated eye) | 1. RGCs isolated from neonatal Wistar rats 2. Wistar rats for immunohistochemical analysis | Yamasaki et al. [64] | 2005 |
|
| NMDA, TFW, and inflammatory toxicity | Intervention study | (1) NMDA (20–500 μM) + 1, 10, or 100 ng/mL of EPO (2) TFW+ 1, 10, or 100 ng/mL of EPO (3) Inflammatory (TNF-α at 12.5–50 ng/mL) + 1, 10, or 100 ng/mL of EPO Time-course effects of EPO exposure: (1) EPO at 8 h before (2) EPO at 4 h before (3) EPO at 0 h (3) EPO at 4 h after (3) EPO at 8 h after | RGCs isolated from adult Wistar rats | Chang et al. [65] | 2013 |
|
| NMDA toxicity | Randomized intervention study | Groups: (1) negative control (2) IVI of 80 nmoles NMDA80 (3) IVI of 80 nmoles NMDA80 + 10 ng EPO (4) IVI of 80 nmoles NMDA80 + 50 ng EPO (5) IVI of 80 nmoles NMDA80 + 250 ng EPO | 125 Wistar rats | Cheng et al. [66] | 2020 |
|
| Microbeads-induced glaucoma model | ||||||
| Elevated IOP induced by intracameral injection of microbeads | Intervention study | Groups: (1) IVI of EPO-R76E loaded PLGA particles (2) IVI of EPO-R76E loaded PPS microspheres one day after elevation of IOP | Mice | Rex et al. [67] | 2022 |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, T.-Y.; Lai, Y.-F.; Chen, Y.-H.; Lu, D.-W. The Latest Evidence of Erythropoietin in the Treatment of Glaucoma. Int. J. Mol. Sci. 2022, 23, 16038. https://doi.org/10.3390/ijms232416038
Lin T-Y, Lai Y-F, Chen Y-H, Lu D-W. The Latest Evidence of Erythropoietin in the Treatment of Glaucoma. International Journal of Molecular Sciences. 2022; 23(24):16038. https://doi.org/10.3390/ijms232416038
Chicago/Turabian StyleLin, Ting-Yi, Yi-Fen Lai, Yi-Hao Chen, and Da-Wen Lu. 2022. "The Latest Evidence of Erythropoietin in the Treatment of Glaucoma" International Journal of Molecular Sciences 23, no. 24: 16038. https://doi.org/10.3390/ijms232416038
APA StyleLin, T.-Y., Lai, Y.-F., Chen, Y.-H., & Lu, D.-W. (2022). The Latest Evidence of Erythropoietin in the Treatment of Glaucoma. International Journal of Molecular Sciences, 23(24), 16038. https://doi.org/10.3390/ijms232416038






