Role of Oxidative Stress in Peyronie’s Disease: Biochemical Evidence and Experiences of Treatment with Antioxidants
Abstract
1. Introduction
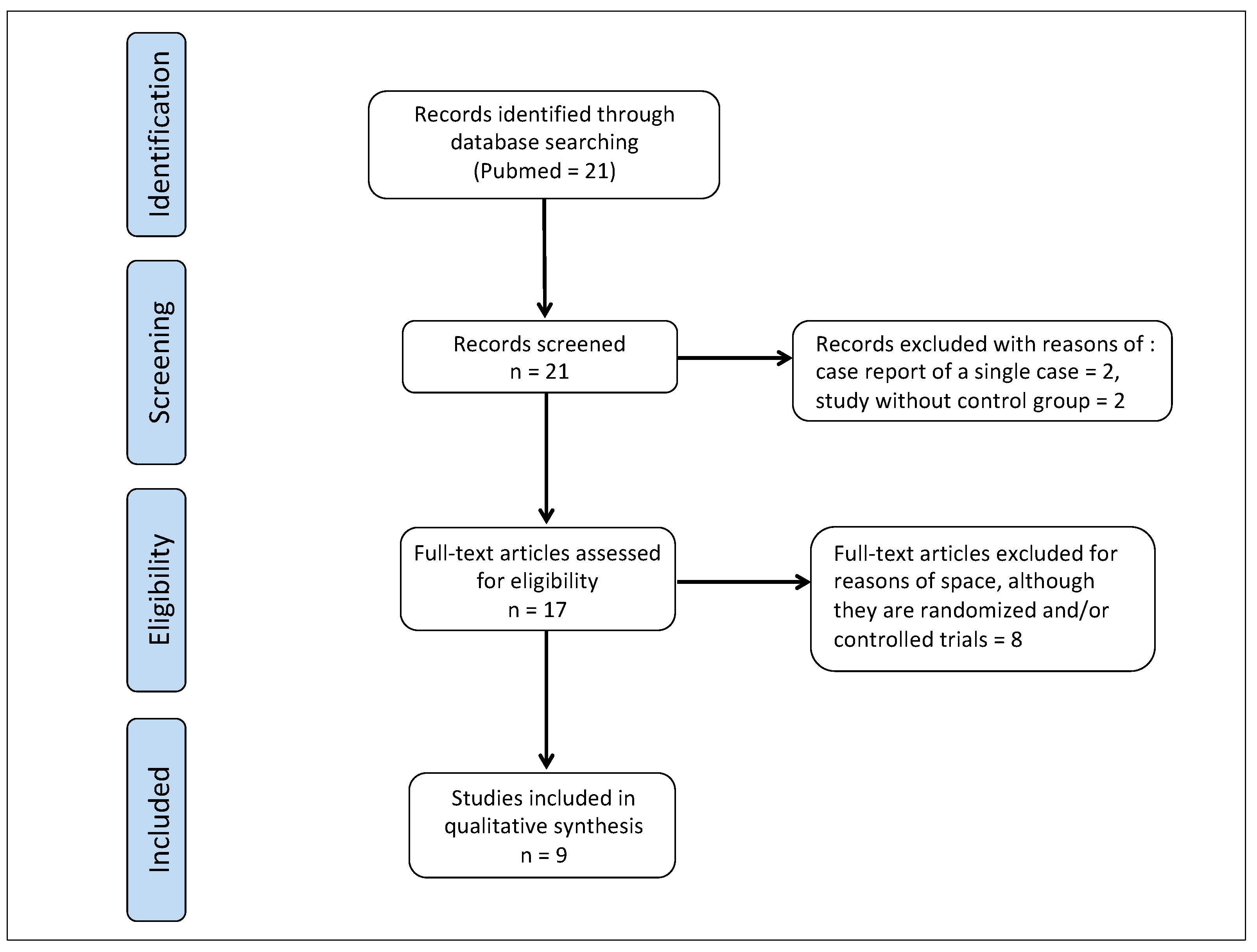
2. Role of Oxidative Stress in Peyronie’s Disease
2.1. Pathophysiological and Biochemical Mechanisms of Peyronie’s Disease
2.2. Oxidative Stress in Peyronie’s Disease
3. Experiences of Treatment with Antioxidants in PD Patients
3.1. The First Studies on the Use of Antioxidants in Patients with PD
3.2. Multimodal Treatment with Antioxidants
| (A) | |||
| Substance | Biochemical Property | Molecular Mechanism | References |
| Vitamin E | Antioxidant Anti-inflammatory Antifibrotic Antiplatelet aggregation |
| [106,107,108,109,110,111] |
| Vitamin C | Antioxidant Anti-inflammatory Antifibrotic Regenerative action on Vitamin E |
| [112,113,114,115] |
| Propolis | Antioxidant Anti-inflammatory Antifibrotic Antiplatelet aggregation |
| [105,116,117,118,119,120,121,122,123,124,125] |
| Bilberry | Antioxidant Anti-inflammatory Antifibrotic |
| [126,127,128] |
| Silymarin | Antioxidant Anti-inflammatory Antifibrotic Vasorelaxant Antiplatelet aggregation |
| [129,130,131,132] |
| Ginkgo biloba | Antioxidant Anti-inflammatory Antifibrotic Vasorelaxant Antiplatelet aggregation |
| [133,134,135,136] |
| (B) | |||
| Substance | Biochemical Property | Molecular Mechanism | References |
| Carnitine | Antioxidant Anti-inflammatory Antifibrotic Vasorelaxant Antiplatelet aggregation | It scavenges reactive oxygen species and reactive nitroxidative species. It reduces production of: i-NOS, NF-kappa-B, IL-1, IL-6, IL-8, TNF-α, TGF-β1 and PAI-1. It hinders inflammation, inhibiting: NF-kappa-B and pro-inflammatory cytokine production, and COX-2 activity. It inhibits fibrosis (deposition of collagen) by inhibiting TGF-β1. It inhibits fibroblast proliferation and the osteoblastic differentiation of fibroblasts. It inhibits myofibroblastic differentiation of fibroblasts by inhibiting TGF-β1. It determines vasodilation through an endothelial mechanism, via the nitric oxide pathway. It inhibits collagen-induced platelet aggregation. | [137,138,139,140,141,142] |
| CoenzymeQ10 | Antioxidant Anti-inflammatory Antifibrotic Vasorelaxant Antiplatelet aggregation Regenerative action on Vitamin E and Vitamin C | It scavenges reactive oxygen species and reactive nitroxidative species. It protects cell membranes from lipoperoxidation determined by reactive species. It reduces production of: i-NOS, NF-kappa-B, IL-1, IL-6, IL-10, TNF-α, TGF-β1 and PAI-1. It inhibits fibrosis (deposition of collagen) by inhibiting TGF-β1. It activates NF-E2-related factor-2 (Nrf2) which suppresses the TGF-β1 expression. It inhibits MMP-2 and MMP-9 (with elastase activity). It inhibits platelet aggregation. It determines vasodilation through an endothelial mechanism via the nitric oxide pathway. It regenerates Vitamin E in its normal and nonoxidized form. | [143,144,145,146,147,148] |
| Boswellia | Antioxidant Anti-inflammatory Antifibrotic Vasorelaxant Antiplatelet aggregation | It scavenges reactive oxygen species and reactive nitroxidative species. It protects cell membranes from lipoperoxidation determined by reactive species. It reduces production of: i-NOS, IL-1, IL-6, TNF-α, and TGF-β1. It hinders inflammation, inhibiting: NF-kappa-B and pro-inflammatory cytokine production, and COX-2 activity. It inhibits fibrosis (deposition of collagen) by inhibiting TGF-β1. It determines vasodilation through an endothelial mechanism via the nitric oxide pathway. It inhibits platelet aggregation. | [149,150,151] |
| Pentoxifylline | Antioxidant Anti-inflammatory Antifibrotic Vasorelaxant Antiplatelet aggregation | It scavenges reactive oxygen species and reactive nitroxidative species. It reduces production of: TNF-α, i-NOS, IL-1, IL-6, IL-8, IL-10, TGF-ß1, PDGF, and PAI-1. It hinders inflammation, inhibiting: NF-kappa-B and pro-inflammatory cytokine production. It inhibits fibrosis (deposition of collagen) by inhibiting TGF-β1 and PDGF. It determines vasodilation through a nonselective PDE inhibition (preventing the degradation reaction of cyclic AMP). It inhibits platelet aggregation. | [101,102,152,153,154,155,156,157] |
| Superoxide dismutase | Antioxidant Anti-inflammatory Antifibrotic | It defends the human body against tissue damage mediated by reactive oxygen species (ROS). It eliminates superoxide anion (O2•-). It inhibits neutrophil-induced inflammation. It hinders fibrosis (collagen deposition) by downregulating TGF-ß1. | [158,159] |
| Hyaluronic acid | Antioxidant Anti-inflammatory Antifibrotic Antiplatelet aggregation | It scavenges ROS, superoxide anion, and hydroxyl radicals. It inhibits lipid peroxidation. It hinders inflammation reducing production of: TNF-α, IL-6, IL-1, and PAI-1. It inhibits fibroblast proliferation. It inhibits platelet aggregation. | [160,161,162,163,164] |
| Diclofenac | Anti-inflammatory Antioxidant | Like other nonsteroidal anti-inflammatory drugs (NSAIDs), diclofenac inhibits synthesis of prostaglandins by inhibiting COX-1 and COX-2 activity. It inhibits NF-kappa-B gene expression. It inhibits TNF-induced NF-kappa-B activation. It exerts powerful dose-dependent free-radical-scavenging activity. It strongly protects against lipid peroxidation and the damage of peroxyl radicals. | [165,166,167] |
3.3. Brief Narrative Review of Peyronie’s Disease Treatment with Antioxidants
- First group: only oral therapy with pentoxifylline;
- Second group: only intralesional injections with verapamil (every other week, 12 total injections);
- Third group: oral pentoxifylline + intralesional injections with verapamil (every other week, 12 total injections) [98].
- –
- Reduction in curvature by at least 10 degrees: first group = 0%; second group = 17.8%; third group = 50%.
- –
- Improvement in the International Index of Erectile Function (IIEF) score (normal score > 25): first group = from 17.7 to 18.5 (increase + 0.8); second group = from 20.4 to 21.6 (increase + 1.2); third group = from 20 to 22.4 (increase + 2.2).
- –
- Change in stretched penile length: first group = from 10.5 to 10.4 cm (reduction −0.1 cm); second group = from 10.7 to 10.6 cm (reduction −0.1 cm); third group = from 10.3 to 11.0 cm (increase + 0.7 cm).
- –
- Penile pain: first group = resolution of pain in 100% of cases; second group = resolution of pain in 100% of cases; third group = resolution of pain in 100% of cases [172].
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rompel, R.; Mueller-Eckhardt, G.; Sehroeder-Printzen, I.; Weidner, W. HLA Antigens in Peyronie’s Disease. Urol. Int. 1994, 52, 34–37. [Google Scholar] [CrossRef] [PubMed]
- Herati, A.S.; Pastuszak, A.W. The Genetic Basis of Peyronie’s Disease: A Review. Sex. Med. Rev. 2016, 4, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Dolmans, G.H.; Werker, P.M.; de Jong, I.J.; Nijman, R.J.; LifeLines Cohort Study; Wijmenga, C.; Ophoff, R.A. WNT2 Locus Is Involved in Genetic Susceptibility of Peyronie’s Disease. J. Sex. Med. 2012, 9, 1430–1434. [Google Scholar] [CrossRef]
- DiBenedetti, D.B.; Nguyen, D.; Zografos, L.; Ziemiecki, R.; Zhou, X. A Population-Based Study of Peyronie’s Disease: Prevalence and Treatment Patterns in the United States. Adv. Urol. 2011, 2011, 282503. [Google Scholar] [CrossRef] [PubMed]
- Stuntz, M.; Perlaky, A.; des Vignes, F.; Kyriakides, T.; Glass, D. The Prevalence of Peyronie’s Disease in the United States: A Population-Based Study. PLoS ONE 2016, 11, e0150157. [Google Scholar] [CrossRef]
- Bella, A.J.; Lee, J.C.; Grober, E.D.; Carrier, S.; Bénard, F.; Brock, G.B. 2018 Canadian Urological Association guideline for Peyronie’s disease and congenital penile curvature. Can. Urol. Assoc. J. 2018, 12, E197–E209. [Google Scholar] [CrossRef]
- Johnson, H.M.; Weerakoon, P.; Stricker, P.D. The incidence, aetiology, and presentation of Peyronie’s disease in Sydney, Australia. J. Sex. Disabil. 2002, 20, 109–116. [Google Scholar] [CrossRef]
- La Pera, G.; Pescatori, E.S.; Calabrese, M.; Boffini, A.; Colombo, F.; Andriani, E.; Natali, A.; Vaggi, L.; Catuogno, C.; Giustini, M.; et al. SIMONA Study Group. Peyronie’s disease: Prevalence and association with cigarette smoking. A multicenter population-based study in men aged 50–69 years. Eur Urol. 2001, 40, 525–530. [Google Scholar] [CrossRef]
- Schwarzer, U.; Sommer, F.; Klotz, T.; Braun, M.; Reifenrath, B.; Engelmann, U. The prevalence of Peyronie’s disease: Results of a large survey. BJU Int. 2001, 88, 727–730. [Google Scholar] [CrossRef]
- Rhoden, E.L.; Teloken, C.; Ting, H.Y.; Lucas, M.L.; Teodósio da Ros, C.; Ary Vargas Souto, C. Prevalence of Peyronie’s disease in men over 50-y-old from Southern Brazil. Int. J. Impot. Res. 2001, 13, 291–293. [Google Scholar] [CrossRef]
- Shiraishi, K.; Shimabukuro, T.; Matsuyama, H. The prevalence of Peyronie’s disease in Japan: A study in men undergoing maintenance hemodialysis and routine health checks. J. Sex. Med. 2012, 9, 2716–2723. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.; Tsang, S.S.; O, R.Y.; Chun, S.; Tsang, C.-F.; Ho, B.S.; Ng, A.T.; Tsu, J.H.; Lam, W. Mp33-12 Prevalence of Peyronie’s disease and its psychosexual impact in the chinese population: A large cohort population-based cross-sectional study. J. Urol. 2020, 203, e499. [Google Scholar] [CrossRef]
- Kyei, M.Y.; Mensah, J.E.; Asante, E.; Bray, L.D.; Awuku-Asabre, J. Peyronie’s Disease in People of African Origin: A Mini Review. J. Ger. Ag. Res. 2017, 1, 104. Available online: https://www.researchgate.net/publication/327751134_Peyronie%27s_Disease_in_People_of_African_origin_A._Mini_Review (accessed on 11 December 2022).
- Nelson, C.J.; Diblasio, C.; Kendirci, M.; Hellstrom, W.; Guhring, P.; Mulhall, J.P. The Chronology of Depression and Distress in Men with Peyronie’s Disease. J. Sex. Med. 2008, 5, 1985–1990. [Google Scholar] [CrossRef] [PubMed]
- Kuja-Halkola, R.; Henningsohn, L.; D’Onofrio, B.M.; Mills, J.; Adolfsson, A.; Larsson, H.; Cederlöf, M. Mental Disorders in Peyronie’s Disease: A Swedish Cohort Study of 3.5 Million Men. J. Urol. 2021, 205, 864–870. [Google Scholar] [CrossRef]
- Low, P.; Wang, L.; Li, K.D.; Shibley, W.P.; Cedars, B.E.; Holler, J.T.; Enriquez, A.; Sadeghi-Nejad, H.; Amend, G.M.; Breyer, B.N. Thematic analysis of the psycho-sexual symptoms in patients with Peyronie’s disease present on online forums. Int. J. Impot. Res. 2022, 1–6. [Google Scholar] [CrossRef]
- Devine, C.J., Jr.; Somers, K.D.; Ladaga, L.E. Peyronie’s disease: Pathophysiology. Prog Clin. Biol Res. 1991, 370, 355–358. [Google Scholar]
- Devine, C.J.J.; Somers, K.D.; Jordan, G.H.; Schlossberg, S.M. Proposal: Trauma as a cause of Peyronie’s lesion. J. Urol. 1997, 157, 285–290. [Google Scholar] [CrossRef]
- Jarow, J.P.; Lowe, F.C. Penile trauma: An etiologic factor in Peyronie’s disease and erectile dysfunction. J. Urol. 1997, 158, 1388–1390. [Google Scholar] [CrossRef]
- El-Sakka, A.I.; Salabas, E.; Dinçer, M.; Kadioglu, A. The pathophysiology of Peyronie’s disease. Arab J. Urol. 2013, 11, 272–277. [Google Scholar] [CrossRef]
- Paulis, G.; Romano, G.; Paulis, L.; Barletta, D. Recent Pathophysiological Aspects of Peyronie’s Disease: Role of Free Radicals, Rationale, and Therapeutic Implications for Antioxidant Treatment—Literature Review. Adv. Urol. 2017, 2017, 4653512. [Google Scholar] [CrossRef]
- Segundo, A.; Glina, S. Prevalence, Risk Factors, and Erectile Dysfunction Associated With Peyronie’s Disease Among Men Seeking Urological Care. Sex Med. 2020, 8, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Levine, L.; Rybak, J.; Corder, C.; Farrel, M.R. Peyronie’s disease plaque calcification—Prevalence, time to identification, and development of a new grading classification. J. Sex. Med. 2013, 10, 3121–3128. [Google Scholar] [CrossRef] [PubMed]
- Garaffa, G.; Trost, L.W.; Serefoglu, E.C.; Ralph, D.; Hellstrom, W.J. Understanding the course of Peyronie’s disease. Int. J. Clin. Pract. 2013, 67, 781–788. [Google Scholar] [CrossRef]
- Levine, L.A.; Larsen, S. Diagnosis and Management of Peyronie Disease. In Campbell-Walsh Urology, 11th ed.; Wein, A.J., Kavoussi, L.R., Partin, A.W., Peters, C.A., Eds.; Elsevier Saunders: Philadelphia, PA, USA, 2015; Volume 1, pp. 722–748. [Google Scholar]
- Chung, E.; Ralph, D.; Kagioglu, A.; Garaffa, G.; Shamsodini, A.; Bivalacqua, T.; Glina, S.; Hakim, L.; Sadeghi-Nejad, H.; Broderick, G. Evidence-based management guidelines on Peyronie’s disease. J. Sex. Med. 2016, 13, 905–923. [Google Scholar] [CrossRef]
- Hauck, E.W.; Diemer, T.; Schmelz, H.U.; Weidner, W. A Critical Analysis of Nonsurgical Treatment of Peyronie’s Disease. Eur. Urol. 2006, 49, 987–997. [Google Scholar] [CrossRef] [PubMed]
- Levine, L.A.; Estrada, C.R. Intralesional verapamil for the treatment of Peyronie’s disease: A review. Int. J. Impot. Res. 2002, 14, 324–328. [Google Scholar] [CrossRef] [PubMed]
- Brant, W.O.; Dean, R.C.; Lue, T.F. Treatment of Peyronie’s disease with oral pentoxifylline. Nat. Clin. Pract Urol. 2006, 3, 111–115. [Google Scholar] [CrossRef]
- Paulis, G.; Barletta, D.; Turchi, P.; Vitarelli, A.; Dachille, G.; Fabiani, A.; Romano, G. Efficacy and safety evaluation of pentoxifylline associated with other antioxidants in medical treatment of Peyronie’s disease: A case-control study. Res. Rep. Urol. 2016, 8, 1–10. [Google Scholar] [CrossRef]
- Nguyen, H.M.T.; Anaissie, J.; DeLay, K.J.; Yafi, F.A.; Sikka, S.C.; Hellstrom, W.J. Safety and Efficacy of Collagenase Clostridium histolyticum in the Treatment of Acute-Phase Peyronie’s Disease. J. Sex. Med. 2017, 14, 1220–1225. [Google Scholar] [CrossRef]
- Krieger, J.R.; Rizk, P.J.; Kohn, T.P.; Pastuszak, A. Shockwave Therapy in the Treatment of Peyronie’s Disease. Sex. Med. Rev. 2019, 7, 499–507. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Salamanca, J.I.; Egui, A.; Moncada, I.; Minaya, J.; Ballesteros, C.M.; Del Portillo, L.; Sola, I.; Carballido, J. Acute phase Peyronie’s disease management with traction device: A nonrandomized prospective controlled trial with ultrasound correlation. J. Sex. Med. 2014, 11, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Raheem, A.A.; Garaffa, G.; Raheem, T.A.; Dixon, M.; Kayes, A.; Christopher, N.; Ralph, D. The role of vacuum pump therapy to mechanically straighten the penis in Peyronie’s disease. Br. J. Urol. 2010, 106, 1178–1180. [Google Scholar] [CrossRef] [PubMed]
- Kadioglu, A.; Akman, T.; Sanli, O.; Gurkan, L.; Cakan, M.; Celtik, M. Surgical Treatment of Peyronie’s Disease: A Critical Analysis. Eur. Urol. 2006, 50, 235–248. [Google Scholar] [CrossRef]
- Levine, L.A.; Burnett, A.L. Standard operating procedures for Peyronie’s disease. J. Sex. Med. 2013, 10, 230–244. [Google Scholar] [CrossRef]
- Cuzzocrea, S.; Thiemermann, C.; Salvemini, D. Potential Therapeutic Effect of Antioxidant Therapy in Shock and Inflammation. Curr. Med. Chem. 2004, 11, 1147–1162. [Google Scholar] [CrossRef]
- Hussain, T.; Tan, B.; Yin, Y.; Blachier, F.; Tossou, M.C.; Rahu, N. Oxidative Stress and Inflammation: What Polyphenols Can Do for Us? Oxid. Med. Cell. Longev. 2016, 2016, 7432797. [Google Scholar] [CrossRef] [PubMed]
- Kaushal, N.; Narayan, V.; Gandhi, U.H.; Nelson, S.M.; Anil Kumar, K.; Prabhu, K.S. ROS Mediated Oxidative Stress as a Source of Inflammation. In Chronic Inflammation: Molecular Pathophysiology, Nutritional and Therapeutic Interventions; Roy, S., Bagchi, D., Raychaudhuri, S.P., Eds.; CRC Press: Boca Raton, FL, USA, 2013; pp. 261–262. [Google Scholar]
- Li, T.; Zhu, Y.Z. Stress and Inflammation. In Oxidative Stress. Human Diseases and Medicine, 1st ed.; Huang, C., Zhang, Y., Eds.; Springer Nature: Singapore, 2021; pp. 277–291. [Google Scholar]
- Camps, J.; García-Heredia, A. Introduction: Oxidation and Inflammation, A Molecular Link Between Non-communicable Diseases. In Oxidative Stress and Inflammation in Non-Communicable Diseases—Molecular Mechanisms and Perspectives in Therapeutics; Camps, J., Ed.; Springer International: Cham, Switzerland, 2014; pp. 1–4. [Google Scholar]
- Sikka, S.C.; Hellstrom, W.J.G. Role of oxidative stress and antioxidants in Peyronie’s disease. Int. J. Impot. Res. 2002, 14, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Bivalacqua, T.J.; Champion, H.C.; Hellstrom, W.J. Implications of nitric oxide synthase isoforms in the pathophysiology of Peyronie’s disease. Int. J. Impot. Res. 2002, 14, 345–352. [Google Scholar] [CrossRef]
- Ferrini, M.; Vernet, D.; Magee, T.; Shahed, A.; Qian, A.; Rajfer, J.; Gonzalez-Cadavid, N. Antifibrotic Role of Inducible Nitric Oxide Synthase. Nitric Oxide 2002, 6, 283–294. [Google Scholar] [CrossRef]
- Gonzalez-Cadavid, N.F.; Magee, T.R.; Ferrini, M.; Qian, A.; Vernet, D.; Rajfer, J. Gene expression in Peyronie’s disease. Int. J. Impot. Res. 2002, 14, 361–374. [Google Scholar] [CrossRef]
- Valente, E.G.; Vernet, D.; Ferrini, M.G.; Qian, A.; Rajfer, J.; Gonzalez-Cadavid, N.F. L-Arginine and phosphodiesterase (PDE) inhibitors counteract fibrosis in the Peyronie’s fibrotic plaque and related fibroblast cultures. Nitric Oxide 2003, 9, 229–244. [Google Scholar] [CrossRef]
- Gholami, S.S.; Gonzalez-Cadavid, N.F.; Lin, C.S.; Rajfer, J.; Lue, T.F. Peyronie’s disease: A review. J. Urol. 2003, 169, 1234–1241. [Google Scholar] [CrossRef]
- Davila, H.H.; Magee, T.R.; Vernet, L.; Rajfer, J.; Gonzalez-Cadavid, N.F. Gene Transfer of Inducible Nitric Oxide Synthase Complementary DNA Regresses the Fibrotic Plaque in an Animal Model of Peyronie’s Disease1. Biol. Reprod. 2004, 71, 1568–1577. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Cadavid, N.F.; Rajfer, J. Mechanisms of Disease: New insights into the cellular and molecular pathology of Peyronie’s disease. Nat. Clin. Pract Urol. 2005, 2, 291–297. [Google Scholar] [CrossRef]
- Vernet, D.; Nolazco, G.; Cantini, L.; Magee, T.R.; Qian, A.; Rajfer, J.; Gonzalez-Cadavid, N.F. Evidence That Osteogenic Progenitor Cells in the Human Tunica Albuginea May Originate from Stem Cells: Implications for Peyronie Disease1. Biol. Reprod. 2005, 73, 1199–1210. [Google Scholar] [CrossRef]
- Paulis, G.; Brancato, T. Inflammatory mechanisms and oxidative stress in Peyronie’s disease: Therapeutic “rationale” and related emerging treatment strategies. Inflamm. Allergy Drug Targets. 2012, 11, 48–57. [Google Scholar] [CrossRef]
- Wahl, S.M.; Costa, G.L.; Mizel, D.E.; Allen, J.B.; Skaleric, U.; Mangan, D.F. Role of transforming growth factor beta in the pathophysiology of chronic inflammation. J. Periodontol. 1993, 64, 450–455. [Google Scholar] [PubMed]
- Szardening-Kirchner, C.; Konrad, L.; Hauck, E.W.; Haag, S.M.; Eickelberg, O.; Weidner, W. Upregulation of mRNA expression of MCP-1 by TGF-beta1 in fibroblast cells from Peyronie’s disease. World J. Urol. 2009, 27, 123–130. [Google Scholar] [CrossRef]
- Kumar, V.; Abbas, A.K.; Aster, J.C.; Deyrup, A.T. Inflammation and Repair. In Robbins Essential Pathology, 1st ed.; Kumar, V., Abbas, A.K., Aster, J.C., Deyrup, A.T., Eds.; Elsevier Health Sciences: Philadelphia, PA, USA, 2021; pp. 14–29. [Google Scholar]
- Di Meo, S.; Reed, T.T.; Venditti, P.; Victor, V.M. Role of ROS and RNS Sources in Physiological and Pathological Conditions. Oxid. Med. Cell. Longev. 2016, 2016, 1245049. [Google Scholar] [CrossRef] [PubMed]
- Lingappan, K. NF-κB in Oxidative Stress. Curr. Opin. Toxicol. 2018, 7, 81–86. [Google Scholar] [CrossRef]
- Xue, Q.; Yan, Y.; Zhang, R.; Xiong, H. Regulation of iNOS on Immune Cells and Its Role in Diseases. Int. J. Mol. Sci. 2018, 19, 3805. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, K.; Hattori, T.; Fujisawa, T.; Takahashi, K.; Inoue, H.; Takigawa, M. Nitric Oxide Mediates Interleukin-1-Induced Gene Expression of Matrix Metalloproteinases and Basic Fibroblast Growth Factor in Cultured Rabbit Articular Chondrocytes. J. Biochem. 1998, 123, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Nandipati, K.C.; Zippe, C.D.; Raina, R.; Sharma, R.K. Role of Oxidative Stress in the Pathophysiological Mechanism of Erectile Dysfunction. J. Androl. 2006, 27, 335–347. [Google Scholar] [CrossRef] [PubMed]
- Mittal, M.; Siddiqui, M.R.; Tran, K.; Reddy, S.P.; Malik, A.B. Reactive Oxygen Species in Inflammation and Tissue Injury. Antioxid. Redox Signal. 2014, 20, 1126–1167. [Google Scholar] [CrossRef] [PubMed]
- Checa, J.; Aran, J.M. Reactive Oxygen Species: Drivers of Physiological and Pathological Processes. J. Inflamm. Res. 2020, 13, 1057–1073. [Google Scholar] [CrossRef]
- Hoesel, B.; Schmid, J.A. The complexity of NF-κB signaling in inflammation and cancer. Mol. Cancer 2013, 12, 86. [Google Scholar] [CrossRef]
- Chaturvedi, M.M.; Higuchi, M.; Aggarwal, B.B. Effect of tumor necrosis factors, interferons, interleukins, and growth factors on the activation of NF-kappa B: Evidence for lack of correlation with cell proliferation. Lymphokine Cytokine Res. 1994, 13, 309–313. [Google Scholar]
- Agarwal, S.K. Integrins and cadherins as therapeutic targets in fibrosis. Front. Pharmacol. 2014, 5, 131. [Google Scholar] [CrossRef]
- Sakurai, H.; Shigemori, N.; Hasegawa, K.; Sugita, T. TGF-beta-activated kinase 1 stimulates NF-kappa B activation by an NF-kappa B-inducing kinase-independent mechanism. Biochem. Biophys Res. Commun. 1998, 243, 545–549. [Google Scholar] [CrossRef]
- Moreland, R.B.; Nehra, A. Pathophysiology of Peyronie’s disease. Int. J. Impot. Res. 2002, 14, 406–410. [Google Scholar] [CrossRef]
- Edwards, D.R.; Leco, K.J.; Beaudry, P.P.; Atadja, P.W.; Veillette, C.; Riabowol, K.T. Differential effects of transforming growth factor-beta 1 on the expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases in young and old human fibroblasts. Exp. Gerontol. 1996, 31, 207–223. [Google Scholar] [CrossRef] [PubMed]
- Mulhall, J.P. The Clinical Implications of Basic Science Research in Peyronie’s Disease. In Current Clinical Urology: Peyronie’s Disease, A Guide to Clinical Management; Levine, L.A., Ed.; Humana Press: Totowa, NJ, USA, 2007; pp. 39–57. [Google Scholar]
- Kim, E.S.; Kim, M.S.; Moon, A. Transforming growth factor (TGF)-beta in conjunction with H-ras activation promotes malignant progression of MCF10A breast epithelial cells. Cytokine 2005, 29, 84–91. [Google Scholar] [CrossRef]
- Liu, R.-M.; Desai, L.P. Reciprocal regulation of TGF-β and reactive oxygen species: A perverse cycle for fibrosis. Redox Biol. 2015, 6, 565–577. [Google Scholar] [CrossRef] [PubMed]
- Andrae, J.; Gallini, R.; Betsholtz, C. Role of platelet-derived growth factors in physiology and medicine. Genes Dev. 2008, 22, 1276–1312. [Google Scholar] [CrossRef]
- Cui, Y.; Sun, Y.-W.; Lin, H.-S.; Su, W.-M.; Fang, Y.; Zhao, Y.; Wei, X.-Q.; Qin, Y.-H.; Kohama, K.; Gao, Y. Platelet-derived growth factor-BB induces matrix metalloproteinase-2 expression and rat vascular smooth muscle cell migration via ROCK and ERK/p38 MAPK pathways. Mol. Cell. Biochem. 2014, 393, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Huleihel, M.; Douvdevani, A.; Segal, S.; Apte, R.N. Regulation of interleukin 1 generation in immune-activated fibroblasts. Eur. J. Immunol. 1990, 20, 731–738. [Google Scholar] [CrossRef]
- Pyrillou, K.; Burzynski, L.C.; Clarke, M.C.H. Alternative Pathways of IL-1 Activation, and Its Role in Health and Disease. Front. Immunol. 2020, 11, 3288. [Google Scholar] [CrossRef]
- Van’t Hof, R.J.; Armour, K.J.; Smith, L.M.; Armour, K.E.; Wei, X.Q.; Liew, F.Y.; Ralston, S.H. Requirement of the inducible nitric oxide synthase pathway for IL-1-induced osteoclastic bone resorption. Proc. Natl. Acad. Sci. USA 2000, 97, 7993–7998. [Google Scholar] [CrossRef]
- Lee, J.G.; Kay, E.P. NF-κB is the transcription factor for FGF-2 that causes endothelial mesenchymal transformation in cornea. Investig. Ophthalmol. Vis. Sci. 2012, 53, 1530–1538. [Google Scholar] [CrossRef]
- Blotnick, S.; Peoples, G.E.; Freeman, M.R.; Eberlein, T.J.; Klagsbrun, M. T lymphocytes synthesize and export heparin-binding epidermal growth factor-like growth factor and basic fibroblast growth factor, mitogens for vascular cells and fibroblasts: Differential production and release by CD4+ and CD8+ T cells. Proc. Natl. Acad. Sci. USA 1994, 91, 2890–2894. [Google Scholar] [CrossRef] [PubMed]
- Lambert, E.; Dassé, E.; Haye, B.; Petitfrère, E. TIMPs as multifacial proteins. Crit. Rev. Oncol. Hematol. 2004, 49, 187–198. [Google Scholar] [CrossRef]
- Huebner, B.R.; Moore, E.E.; Moore, H.B.; Stettler, G.R.; Nunns, G.R.; Lawson, P.; Sauaia, A.; Kelher, M.; Banerjee, A.; Silliman, C.C. Thrombin Provokes Degranulation of Platelet α-Granules Leading to the Release of Active Plasminogen Activator Inhibitor-1 (PAI-1). Shock 2018, 50, 671–676. [Google Scholar] [CrossRef] [PubMed]
- Cesari, M.; Pahor, M.; Incalzi, R.A. REVIEW: Plasminogen Activator Inhibitor-1 (PAI-1): A Key Factor Linking Fibrinolysis and Age-Related Subclinical and Clinical Conditions. Cardiovasc. Ther. 2010, 28, e72–e91. [Google Scholar] [CrossRef] [PubMed]
- Davila, H.H.; Magee, T.R.; Zuniga, F.I.; Rajfer, J.; Gonzalez-Cadavid, N.F. Peyronie’s disease associated with increase in plasminogen activator inhibitor in fibrotic plaque. Urology 2005, 65, 645–648. [Google Scholar] [CrossRef] [PubMed]
- Chu, S.-C.; Yang, S.-F.; Lue, K.-H.; Hsieh, Y.-S.; Hsiao, T.-Y.; Lu, K.-H. Urokinase-type plasminogen activator, receptor, and inhibitor correlating with gelatinase-B (MMP-9) contribute to inflammation in gouty arthritis of the knee. J. Rheumatol. 2006, 33, 311–317. [Google Scholar]
- Liu, R.M. Oxidative stress, plasminogen activator inhibitor 1, and lung fibrosis. Antioxid. Redox Signal. 2008, 10, 303–319. [Google Scholar] [CrossRef]
- Josephs, S.F.; Ichim, T.E.; Prince, S.M.; Kesari, S.; Marincola, F.M.; Escobedo, A.R.; Jafri, A. Unleashing endogenous TNF-alpha as a cancer immunotherapeutic. J. Transl. Med. 2018, 16, 242. [Google Scholar] [CrossRef]
- Chou, D.H.; Lee, W.; McCulloch, C.A. TNF-alpha inactivation of collagen receptors: Implications for fibroblast function and fibrosis. J. Immunol. 1996, 156, 4354–4362. [Google Scholar]
- Esmon, C.T. The interactions between inflammation and coagulation. Br. J. Haematol. 2005, 131, 417–430. [Google Scholar] [CrossRef]
- Zhang, Y.; McCluskey, K.; Fujii, K.; Wahl, L.M. Differential regulation of monocyte matrix metalloproteinase and TIMP-1 production by TNF-alpha, granulocyte-macrophage CSF, and IL-1 beta through prostaglandin-dependent and -independent mechanisms. J. Immunol. 1998, 161, 3071–3076. [Google Scholar] [PubMed]
- Del Carlo, M.; Cole, A.A.; Levine, L.A. Differential calcium independent regulation of matrix metalloproteinases and tissue inhibitors of matrix metalloproteinases by interleukin-1beta and transforming growth factor-beta in Peyronie’s plaque fibroblasts. J. Urol. 2008, 179, 2447–2455. [Google Scholar] [CrossRef] [PubMed]
- Scott, W.W.; Scardino, P.L. A new concept in the treatment of Peyronie’s disease. South. Med. J. 1948, 41, 173–177. [Google Scholar] [CrossRef]
- Lemourt Oliva, M.; Filgueiras López, E.; Rodríguez Barroso, A.; González Oramas, E.; Bordonado, R. Clinical evaluation of the use of propoleum in Peyronie’s disease. Arch. Esp. Urol. 1998, 51, 171–176. [Google Scholar]
- Lemourt Oliva, M.; Rodríguez Barroso, A.; Puente Guillén, M.; Vega Guerrero, C.; Navarro Cutiño, M.; Pérez Monzón, A. Propoleum and Peyronie’s disease. Arch. Esp. Urol. 2003, 56, 805–813. [Google Scholar] [PubMed]
- Lemourt Oliva, M.; Rodríguez Barroso, A.; Bordonado Ramírez, R.; González Oramas, E.; Molina Castillo, F. Study of propoleum dosage in Peyronie’s disease. Arch. Esp. Urol. 2003, 56, 814–819. [Google Scholar] [PubMed]
- Lemourt Oliva, M.; Fragas Valdés, R.; Bordonado Ramírez, R.; Santana, J.L.; González Oramas, E.; Merino, A. Peyronie’s disease. Evaluation of 3 therapeutic modalities: Propoleum, laser and simultaneous propoleum-laser. Arch. Esp. Urol. 2005, 58, 931–935. [Google Scholar]
- Biagiotti, G.; Cavallini, G. Acetyl-L-carnitine vs tamoxifen in the oral therapy of Peyronie’s disease: A preliminary report. BJU Int. 2001, 88, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Cavallini, G.; Biagiotti, G.; Koverech, A.; Vitali, G. Oral propionyl-l-carnitine and intraplaque verapamil in the therapy of advanced and resistant Peyronie’s disease. BJU Int. 2002, 89, 895–900. [Google Scholar] [CrossRef]
- Smith, J.F.; Shindel, A.W.; Huang, Y.C.; Clavijo, R.I.; Flechner, L.; Breyer, B.N.; Eisenberg, M.L.; Lue, T.F. Pentoxifylline treatment and penile calcifications in men with Peyronie’s disease. Asian J. Androl. 2011, 13, 322–325. [Google Scholar] [CrossRef]
- Dell’Atti, L.; Ughi, G. Efficacy of pentoxifylline in Peyronie’s disease: Clinical case of a young man. Arch. Ital. Urol. Androl. 2014, 86, 237. [Google Scholar] [CrossRef][Green Version]
- Alizadeh, M.; Karimi, F.; Fallah, M. Evaluation of Verapamil Efficacy in Peyronie’S Disease Comparing With Pentoxifylline. Glob. J. Health Sci. 2014, 6, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Abern, M.R.; Larsen, S.; Levine, L.A. Combination of penile traction, intralesional verapamil, and oral therapies for Peyronie’s disease. J. Sex. Med. 2012, 9, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Ciociola, F.; Colpi, G.M. Peyronie’s disease: A “triple oxygenant therapy”. Arch. Ital. Urol. Androl. 2013, 85, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Kruuse, C.; Jacobsen, T.B.; Thomsen, L.L.; Hasselbalch, S.G.; Frandsen, E.K.; Dige-Petersen, H.; Olesen, J. Effects of the non-selective phosphodiesterase inhi.ibitor pentoxifylline on regional cerebral blood flow and large arteries in healthy subjects. Eur. J. Neurol. 2000, 7, 629–638. [Google Scholar] [CrossRef]
- Sunil, V.R.; Vayas, K.N.; Cervelli, J.A.; Malaviya, R.; Hall, L.; Massa, C.B.; Gow, A.J.; Laskin, J.D.; Laskin, D.L. Pentoxifylline attenuates nitrogen mustard-induced acute lung injury, oxidative stress and inflammation. Exp. Mol. Pathol. 2014, 97, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Inar, D.; Sedanur, S.A.R.I.; Alkan, H.; Ay, K.B.; Borcaktepe, E.; Duyum, A.Y.; Filikçi, S.S.; Gençer, E.; Senem, Ç.; Soylu, S.; et al. Non-Surgical Treatment Options for Peyronie’s Disease. ACMR 2021, 2, 136–145. Available online: https://dergipark.org.tr/en/download/article-file/1981355 (accessed on 11 December 2022).
- Safarinejad, M.R. Safety and efficacy of coenzyme Q10 supplementation in early chronic Peyronie’s disease: A double-blind, placebo-controlled randomized study. Int. J. Impot. Res. 2010, 22, 298–309. [Google Scholar] [CrossRef] [PubMed]
- Khalil, M.L. Biological activity of bee propolis in health and disease. Asian Pac. J. Cancer Prev. 2006, 7, 22–31. [Google Scholar]
- Cachia, O.; Benna, J.E.; Pedruzzi, E.; Descomps, B.; Gougerot-Pocidalo, M.A.; Leger, C.L. alpha-tocopherol inhibits the respiratory burst in human monocytes. Attenuation of p47(phox) membrane translocation and phosphorylation. J. Biol. Chem. 1998, 273, 32801–32805. [Google Scholar] [CrossRef] [PubMed]
- Tasanarong, A.; Kongkham, S.; Duangchana, S.; Thitiarchakul, S.; Eiam-Ong, S. Vitamin E ameliorates renal fibrosis by inhibition of TGF-beta/Smad2/3 signaling pathway in UUO mice. J. Med. Assoc. Thai. 2011, 94 (Suppl. S7), S1–S9. [Google Scholar] [PubMed]
- Haas, A.L.; Boscoboinik, D.; Mojon, D.S.; Bohnke, M.; Azzi, A. Vitamin E Inhibits Proliferation of Human Tenon’s Capsule Fibroblasts in vitro. Ophthalmic. Res. 1996, 28, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Godbout, J.P.; Berg, B.M.; Krzyszton, C.; Johnson, R.W. Alpha-tocopherol attenuates NFkappaB activation and pro-inflammatory cytokine production in brain and improves recovery from lipopolysaccharide-induced sickness behavior. J. Neuroimmunol. 2005, 169, 97–105. [Google Scholar] [CrossRef]
- Jiang, Q.; Yin, X.; Lill, M.A.; Danielson, M.L.; Freiser, H.; Huang, J. Long-chain carboxychromanols, metabolites of vitamin, E.; are potent inhibitors of cyclooxygenases. Proc. Natl. Acad. Sci. USA 2008, 105, 20464–20469. [Google Scholar] [CrossRef]
- Kakishita, E.; Suehiro, A.; Oura, Y.; Nagai, K. Inhibitory effect of vitamin E (α -tocopherol) on spontaneous platelet aggregation in whole blood. Thromb. Res. 1990, 60, 489–499. [Google Scholar] [CrossRef]
- Bendich, A.; Machlin, L.; Scandurra, O.; Burton, G.; Wayner, D. The antioxidant role of vitamin C. Adv. Free. Radic. Biol. Med. 1986, 2, 419–444. [Google Scholar] [CrossRef]
- Niki, E.; Tsuchiya, J.; Tanimura, R.; Kamiya, Y. Regeneration of vitamin e from α-chromanoxyl radical by glutathione and vitamin C. Chem. Lett. 1982, 11, 789–792. [Google Scholar] [CrossRef]
- Ellulu, M.S.; Rahmat, A.; Ismail, P.; Khaza’Ai, H.; Abed, Y. Effect of vitamin C on inflammation and metabolic markers in hypertensive and/or diabetic obese adults: A randomized controlled trial. Drug Des. Dev. Ther. 2015, 9, 3405–3412. [Google Scholar] [CrossRef]
- Da Silva, M.R.; Schapochnik, A.; Leal, M.P.; Esteves, J.; Hebeda, C.B.; Sandri, S.; Pavani, C.; Horliana, A.C.R.T.; Farsky, S.H.P.; Lino-Dos-Santos-Franco, A. Beneficial effects of ascorbic acid to treat lung fibrosis induced by paraquat. PLoS ONE 2018, 13, e0205535. [Google Scholar] [CrossRef]
- Tan, G.; Ilk, S.; Foto, F.Z.; Foto, E.; Saglam, N. Antioxidative and antiproliferative effects of propolis-reduced silver nanoparticles. Adv. Nano Res. 2021, 10, 139–150. [Google Scholar]
- Wang, X.; Gong, G.; Yang, W.; Li, Y.; Jiang, M.; Li, L. Antifibrotic activity of galangin, a novel function evaluated in animal liver fibrosis model. Environ. Toxicol. Pharmacol. 2013, 36, 288–295. [Google Scholar] [CrossRef]
- Min, Y.D.; Choi, C.H.; Bark, H.; Son, H.Y.; Park, H.H.; Lee, S.; Park, J.W.; Park, E.K.; Shin, H.I.; Kim, S.H. Quercetin inhibits expression of inflammatory cytokines through attenuation of NF-kappaB and p38 MAPK in HMC-1 human mast cell line. Inflamm. Res. 2007, 56, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Raso, G.M.; Meli, R.; Di Carlo, G.; Pacilio, M.; Di Carlo, R. Inhibition of inducible nitric oxide synthase and cyclooxygenase-2 expression by flavonoids in macrophage J774A.1. Life Sci. 2001, 68, 921–931. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Matsushima, M.; Hayashi, Y.; Shibasaki, M.; Imaizumi, K.; Hashimoto, N.; Shimokata, K.; Hasegawa, Y.; Kawabe, T. Attenuation of transforming growth factor-β-stimulated collagen production in fibroblasts by quercetin-induced heme oxygenase-1. Am. J. Respir. Cell Mol. Biol. 2011, 44, 614–620. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.X.; Wang, L.; Yang, J.L.; Li, L.Z.; Xu, W.M.; Li, T. Caffeic acid phenethyl ester attenuates pro-inflammatory and fibrogenic phenotypes of LPS-stimulated hepatic stellate cells through the inhibition of NF-κB signaling. Int. J. Mol. Med. 2014, 33, 687–694. [Google Scholar] [CrossRef]
- Mia, M.M.; Bank, R.A. The pro-fibrotic properties of transforming growth factor on human fibroblasts are counteracted by caffeic acid by inhibiting myofibroblast formation and collagen synthesis. Cell Tissue Res. 2015, 363, 775–789. [Google Scholar] [CrossRef]
- Cho, H.; Yun, C.W.; Park, W.K.; Kong, J.Y.; Kim, K.S.; Park, Y.; Lee, S.; Kim, B.K. Modulation of the activity of pro-inflammatory enzymes, COX-2 and iNOS, by chrysin derivatives. Pharmacol. Res. 2004, 49, 37–43. [Google Scholar] [CrossRef]
- Lo, H.-M.; Wu, M.-W.; Pan, S.-L.; Peng, C.-Y.; Wu, P.-H.; Wu, W.-B. Chrysin restores PDGF-induced inhibition on protein tyrosine phosphatase and reduces PDGF signaling in cultured VSMCs. J. Nutr. Biochem. 2012, 23, 667–678. [Google Scholar] [CrossRef] [PubMed]
- Landolfi, R.; Mower, R.L.; Steiner, M. Modification of platelet function and arachidonic acid metabolism by bioflavonoids: Structure-activity relations. Biochem. Pharmacol. 1984, 33, 1525–1530. [Google Scholar] [CrossRef]
- Boots, A.W.; Haenen, G.R.; Bast, A. Health effects of quercetin: From antioxidant to nutraceutical. Eur. J. Pharmacol. 2008, 585, 325–337. [Google Scholar] [CrossRef]
- Rahman, M.M.; Ichiyanagi, T.; Komiyama, T.; Hatano, Y.; Konishi, T. Superoxide radical- and peroxynitrite-scavenging activity of anthocyanins; structure-activity relationship and their synergism. Free Radic. Res. 2006, 40, 993–1002. [Google Scholar] [CrossRef] [PubMed]
- Hou, D.-X.; Yanagita, T.; Uto, T.; Masuzaki, S.; Fujii, M. Anthocyanidins inhibit cyclooxygenase-2 expression in LPS-evoked macrophages: Structure–activity relationship and molecular mechanisms involved. Biochem. Pharmacol. 2005, 70, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Chtourou, Y.; Garoui, E.; Boudawara, T.; Zeghal, N. Therapeutic efficacy of silymarin from milk thistle in reducing manganese-induced hepatic damage and apoptosis in rats. Hum. Exp. Toxicol. 2012, 32, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.R.; Seo, H.S.; Ku, J.M.; Kim, G.J.; Jeon, C.Y.; Park, J.H.; Jang, B.H.; Park, S.J.; Shin, Y.C.; Ko, S.G. Silibinin inhibits the production of pro-inflammatory cytokines through inhibition of NF-κB signaling pathway in HMC-1 human mast cells. Inflamm. Res. 2013, 62, 941–950. [Google Scholar] [CrossRef]
- Wadhwa, K.; Pahwa, R.; Kumar, M.; Kumar, S.; Sharma, P.C.; Singh, G.; Verma, R.; Mittal, V.; Singh, I.; Kaushik, D.; et al. Mechanistic Insights into the Pharmacological Significance of Silymarin. Molecules 2022, 27, 5327. [Google Scholar] [CrossRef]
- Pourová, J.; Applová, L.; Macáková, K.; Vopršalová, M.; Migkos, T.; Bentanachs, R.; Biedermann, D.; Petrásková, L.; Tvrdý, V.; Hrubša, M.; et al. The Effect of Silymarin Flavonolignans and Their Sulfated Conjugates on Platelet Aggregation and Blood Vessels Ex Vivo. Nutrients 2019, 11, 2286. [Google Scholar] [CrossRef]
- Noor-E-Tabassum, U.; Das, R.; Lami, M.S.; Chakraborty, A.J.; Mitra, S.; Tallei, T.E.; Idroes, R.; Mohamed, A.A.-R.; Hossain, J.; Dhama, K.; et al. Ginkgo biloba: A Treasure of Functional Phytochemicals with Multimedicinal Applications. Evid.-Based Complement. Altern. Med. 2022, 2022, 8288818. [Google Scholar] [CrossRef]
- Sochocka, M.; Ochnik, M.; Sobczyński, M.; Gębura, K.; Zambrowicz, A.; Naporowski, P.; Leszek, J. Ginkgo Biloba Leaf Extract Improves an Innate Immune Response of Peripheral Blood Leukocytes of Alzheimer’s Disease Patients. Nutrients 2022, 14, 2022. [Google Scholar] [CrossRef]
- Dogan, R.; Sjostrand, A.P.; Yenıgun, A.; Karatas, E.; Kocyigit, A.; Ozturan, O. Influence of Ginkgo Biloba extract (EGb 761) on expression of IL-1 Beta, IL-6, TNF-alfa, HSP-70, HSF-1 and COX-2 after noise exposure in the rat cochlea. Auris Nasus Larynx 2018, 45, 680–685. [Google Scholar] [CrossRef]
- Kubota, Y.; Tanaka, N.; Kagota, S.; Nakamura, K.; Kunitomo, M.; Shinozuka, K.; Umegaki, K. Effects of Ginkgo biloba extract on blood pressure and vascular endothelial response by acetylcholine in spontaneously hypertensive rats. J. Pharm. Pharmacol. 2006, 58, 243–249. [Google Scholar] [CrossRef]
- Gülçin, I. Antioxidant and antiradical activities of l-carnitine. Life Sci. 2006, 78, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Ge, P.; Cui, Y.; Liu, F.; Luan, J.; Zhou, X.; Han, J. L-carnitine affects osteoblast differentiation in NIH3T3 fibroblasts by the IGF-1/PI3K/Akt signalling pathway. Biosci. Trends 2015, 9, 42–48. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhao, H.Y.; Li, H.Y.; Jin, J.; Jin, J.Z.; Zhang, L.Y.; Xuan, M.Y.; Jin, X.M.; Jiang, Y.J.; Zheng, H.L.; Jin, Y.S.; et al. L-carnitine treatment attenuates renal tubulointerstitial fibrosis induced by unilateral ureteral obstruction. Korean J. Intern. Med. 2021, 36, S180–S195. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Meng, F.; Li, H.; Hua, X.; Wu, L.; Yuan, X. L-carnitine alleviates oxidative stress-related damage via MAPK signaling in human lens epithelial cells exposed to H2O2. Int. J. Mol. Med. 2019, 44, 1515–1522. [Google Scholar] [CrossRef] [PubMed]
- Güçlü, O.; Yüksel, V.; Hüseyin, S.; Ege, T.; Canbaz, S.; Süngün, M. In vitro effects of L-carnitine on coronary artery bypass grafts. Exp. Clin. Cardiol. 2013, 18, 118–120. [Google Scholar]
- Pignatelli, P.; Lenti, L.; Sanguigni, V.; Frati, G.; Simeoni, I.; Gazzaniga, P.P.; Pulcinelli, F.M.; Violi, F. Carnitine inhibits arachidonic acid turnover, platelet function, and oxidative stress. Am. J. Physiol. Circ. Physiol. 2003, 284, H41–H48. [Google Scholar] [CrossRef]
- Frei, B.; Kim, M.C.; Ames, B.N. Ubiquinol-10 is an effective lipid-soluble antioxidant at physiological concentrations. Proc. Natl. Acad. Sci. USA 1990, 87, 4879–4883. [Google Scholar] [CrossRef]
- Sifuentes-Franco, S.; Sánchez-Macías, D.C.; Carrillo-Ibarra, S.; Rivera-Valdés, J.J.; Zuñiga, L.Y.; Sánchez-López, V.A. Antioxidant and Anti-Inflammatory Effects of Coenzyme Q10 Supplementation on Infectious Diseases. Healthcare 2022, 10, 487. [Google Scholar] [CrossRef]
- Mohamed, H.A.; Said, R.S. Coenzyme Q10 attenuates inflammation and fibrosis implicated in radiation enteropathy through suppression of NF-kB/TGF-β/MMP-9 pathways. Int. Immunopharmacol. 2021, 92, 107347. [Google Scholar] [CrossRef]
- Zozina, V.I.; Covantev, S.; Goroshko, O.A.; Krasnykh, L.M.; Kukes, V.G. Coenzyme Q10 in Cardiovascular and Metabolic Diseases: Current State of the Problem. Curr. Cardiol. Rev. 2018, 14, 164–174. [Google Scholar] [CrossRef]
- Ya, F.; Xu, X.R.; Shi, Y.; Gallant, R.C.; Song, F.; Zuo, X.; Zhao, Y.; Tian, Z.; Zhang, C.; Xu, X.; et al. Coenzyme Q10 Upregulates Platelet cAMP/PKA Pathway and Attenuates Integrin αIIbβ3 Signaling and Thrombus Growth. Mol. Nutr. Food Res. 2019, 63, 1900662. [Google Scholar] [CrossRef] [PubMed]
- Testai, L.; Martelli, A.; Flori, L.; Cicero, A.; Colletti, A. Coenzyme Q10: Clinical Applications beyond Cardiovascular Diseases. Nutrients 2021, 13, 1697. [Google Scholar] [CrossRef] [PubMed]
- Eltahir, H.M.; Fawzy, M.A.; Mohamed, E.M.; Alrehany, M.A.; Shehata, A.M.; Abouzied, M.M. Antioxidant, anti-inflammatory and anti-fibrotic effects of Boswellia serrate gum resin in CCl4-induced hepatotoxicity. Exp. Ther. Med. 2020, 19, 1313–1321. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, R.M.; Fillmann, H.S.; Martins, M.I.M.; Meurer, L.; Marroni, N.P. Boswellia serrata has Beneficial Anti-Inflammatory and Antioxidant Properties in a Model of Experimental Colitis. Phytother. Res. 2014, 28, 1392–1398. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Chen, M.; Ding, Y.; Zhu, Z.; Zhang, Y.; Wei, P.; Wang, J.; Qiao, Y.; Li, L.; Li, Y.; et al. Pretreatment with β-Boswellic Acid Improves Blood Stasis Induced Endothelial Dysfunction: Role of eNOS Activation. Sci. Rep. 2015, 5, 15357. [Google Scholar] [CrossRef]
- Costantini, T.W.; Deree, J.; Peterson, C.Y.; Putnam, J.G.; Woon, T.; Loomis, W.H.; Bansal, V.; Coimbra, R. Pentoxifylline modulates p47phox activation and downregulates neutrophil oxidative burst through PKA-dependent and -independent mechanisms. Immunopharmacol. Immunotoxicol. 2009, 32, 82–91. [Google Scholar] [CrossRef]
- Freitas, J.P.; Filipe, P.M. Pentoxifylline. A hydroxyl radical scavenger. Biol. Trace Elem. Res. 1995, 47, 307–311. [Google Scholar] [CrossRef]
- Ji, Q.; Zhang, L.; Jia, H.; Xu, J. Pentoxifylline inhibits endotoxin-induced NF-kappa B activation and associated production of proinflammatory cytokines. Ann. Clin. Lab. Sci. 2004, 34, 427–436. [Google Scholar]
- Shindel, A.W.; Lin, G.; Ning, H.; Banie, L.; Huang, Y.-C.; Liu, G.; Lin, C.-S.; Lue, T.F. Pentoxifylline Attenuates Transforming Growth Factor-β1-Stimulated Collagen Deposition and Elastogenesis in Human Tunica Albuginea-Derived Fibroblasts Part 1: Impact on Extracellular Matrix. J. Sex. Med. 2010, 7, 2077–2085. [Google Scholar] [CrossRef]
- Lin, S.-L.; Chen, R.-H.; Chen, Y.-M.; Chiang, W.-C.; Tsai, T.-J.; Hsieh, B.-S. Pentoxifylline Inhibits Platelet-Derived Growth Factor-Stimulated Cyclin D1 Expression in Mesangial Cells by Blocking Akt Membrane Translocation. Mol. Pharmacol. 2003, 64, 811–822. [Google Scholar] [CrossRef]
- De la Cruz, J.P.; Romero, M.M.; Sanchez, P.; Sanchez de la Cuesta, F. Antiplatelet effect of pentoxifylline in human whole blood. Gen. Pharmacol. 1993, 24, 605–609. [Google Scholar] [CrossRef] [PubMed]
- Younus, H. Therapeutic potentials of superoxide dismutase. Int. J. Health Sci. 2018, 12, 88–93. [Google Scholar]
- Vozenin-Brotons, M.C.; Sivan, V.; Gault, N.; Renard, C.; Geffrotin, C.; Delanian, S.; Lefaix, J.L.; Martin, M. Antifibrotic action of Cu/Zn SOD is mediated by TGF-beta1 repression and phenotypic reversion of myofibroblasts. Free Radic Biol. Med. 2001, 30, 30–42. [Google Scholar] [CrossRef] [PubMed]
- Zucchi, A.; Scroppo, F.I.; Capogrosso, P.; Salonia, A.; Duante, J.; Bini, V.; Liguori, G.; Bartoletti, R. Clinical use of hyaluronic acid in andrology: A review. Andrology 2021, 10, 42–50. [Google Scholar] [CrossRef]
- Sudha, P.N.; Rose, M.H. Beneficial Effects of Hyaluronic Acid. Adv. Food Nutr. Res. 2014, 72, 137–176. [Google Scholar]
- Lee, B.M.; Park, S.J.; Noh, I.; Kim, C.-H. The effects of the molecular weights of hyaluronic acid on the immune responses. Biomater. Res. 2021, 25, 27. [Google Scholar] [CrossRef]
- Mast, B.A.; Diegelmann, R.F.; Krummel, T.M.; Cohen, I.K. Hyaluronic Acid Modulates Proliferation, Collagen and Protein Synthesis of Cultured Fetal Fibroblasts. Matrix Stuttg. Ger. 1993, 13, 441–446. [Google Scholar] [CrossRef]
- Verheye, S.; Markou, C.P.; Salame, M.Y.; Wan, B.; King, S.B., 3rd; Robinson, K.A.; Chronos, N.A.; Hanson, S.R. Reduced thrombus formation by hyaluronic acid coating of endovascular devices. Arterioscler. Thromb. Vasc. Biol. 2000, 20, 1168–1172. [Google Scholar] [CrossRef]
- Tang, Y.-Z.; Liu, Z.-Q. Evaluation of the free-radical-scavenging activity of diclofenac acid on the free-radical-induced haemolysis of human erythrocytes. J. Pharm. Pharmacol. 2006, 58, 625–631. [Google Scholar] [CrossRef]
- Rojo, C.; Álvarez-Figueroa, M.J.; Pessoa-Mahana, D.; Soto, M.; Cañete, A.; López-Alarcón, C. Scavenging activity of diclofenac: Interaction with abts radical cation and peroxyl radicals. J. Chil. Chem. Soc. 2009, 54, 58–62. [Google Scholar] [CrossRef][Green Version]
- Takada, Y.; Bhardwaj, A.; Potdar, P.; Aggarwal, B.B. Nonsteroidal anti-inflammatory agents differ in their ability to suppress NF-kappaB activation, inhibition of expression of cyclooxygenase-2 and cyclin D1, and abrogation of tumor cell proliferation. Oncogene 2004, 23, 9247–9258. [Google Scholar] [CrossRef] [PubMed]
- Hatzimouratidis, K.; Eardley, I.; Giuliano, F.; Hatzichristou, D.; Moncada, I.; Salonia, A.; Vardi, Y.; Wespes, E.; European Association of Urology. EAU guidelines on penile curvature. Eur Urol. 2012, 62, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Nehra, A.; Alterowitz, R.; Culkin, D.J.; Faraday, M.M.; Hakim, L.S.; Heidelbaugh, J.J.; Khera, M.; Kirkby, E.; McVary, K.T.; Miner, M.M.; et al. Peyronie’s disease: AUA guideline. J. Urol. 2015, 194, 745–753. [Google Scholar] [CrossRef] [PubMed]
- Riedl, C.R.; Sternig, P.; Gallé, G.; Langmann, F.; Vcelar, B.; Vorauer, K.; Wagner, A.; Katinger, H.; Pflüger, H. Liposomal recombinant human superoxide dismutase for the treatment of Peyronie’s disease: A randomized placebo-controlled double-blind prospective clinical study. Eur Urol. 2005, 48, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Favilla, V.; Russo, G.I.; Privitera, S.; Castelli, T.; Madonia, M.; La Vignera, S.; Condorelli, R.; Calogero, A.E.; Farina, F.P.; Cimino, S.; et al. Combination of intralesional verapamil and oral antioxidants for Peyronie’s disease: A prospective, randomised controlled study. Andrologia 2014, 46, 936–942. [Google Scholar] [CrossRef]
- Gallo, L.; Sarnacchiaro, P. Ten-year experience with multimodal treatment for acute phase Peyronie’s disease: A real life clinical report. Actas Urol. Esp. 2019, 43, 182–189. [Google Scholar] [CrossRef]
- Paulis, G.; Brancato, T.; D’Ascenzo, R.; De Giorgio, G.; Nupieri, P.; Orsolini, G.; Alvaro, R. Efficacy of vitamin E in the conservative treatment of Peyronie’s disease: Legend or reality? A controlled study of 70 cases. Andrology 2013, 1, 120–128. [Google Scholar] [CrossRef]
- Paulis, G.; De Giorgio, G. Complete Plaque Regression in Patients with Peyronie’s Disease After Multimodal Treatment with Antioxidants: A Report of 2 Cases. Am. J. Case Rep. 2022, 23, e936146-1–e936146-8. [Google Scholar] [CrossRef]
- Paulis, G.; De Giorgio, G. Full Regression of Peyronie’s Disease Plaque Following Combined Antioxidant Treatment: A Three-Case Report. Antioxidants 2022, 11, 1661. [Google Scholar] [CrossRef]
- Paulis, G.; De Giorgio, G. Patients with Peyronie’s disease achieve complete plaque regression after multimodal treatment with antioxidants: A case series. J. Med. Case Rep. 2022, 16, 359. [Google Scholar] [CrossRef]
- Paulis, G.; D’Ascenzo, R.; Nupieri, P.; De Giorgio, G.; Orsolini, G.; Brancato, T.; Alvaro, R. Effectiveness of antioxidants (propolis, blueberry, vitamin E) associated with verapamil in the medical management of Peyronie’s disease: A study of 151 cases. Int. J. Androl. 2012, 35, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Cavallini, G.; De Giorgio, G.; Quattrocchi, S.; Brancato, T.; Alvaro, R. Long-term multimodal therapy (verapamil associated with propolis, blueberry, vitamin E and local diclofenac) on patients with Peyronie’s disease (chronic inflammation of the tunica albuginea). Results of a controlled study. Inflamm. Allergy Drug Targets 2013, 12, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Cavallini, G.; Brancato, T.; Alvaro, R. Peironimev-Plus® in the treatment of chronic inflammation of tunica albuginea (Peyronie’s disease). results of a controlled study. Inflamm. Allergy Drug Targets 2013, 12, 61–67. [Google Scholar] [CrossRef]
- Halliwell, B. The antioxidant paradox. Lancet 2000, 355, 1179–1180. [Google Scholar] [CrossRef] [PubMed]
- Dutta, S.; Sengupta, P.; Roychoudhury, S.; Chakravarthi, S.; Wang, C.W.; Slama, P. Antioxidant Paradox in Male Infertility: ‘A Blind Eye’ on Inflammation. Antioxidants 2022, 11, 167. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimpour-Koujan, S.; Gargari, B.P.; Mobasseri, M.; Valizadeh, H.; Asghari-Jafarabadi, M. Lower glycemic indices and lipid profile among type 2 diabetes mellitus patients who received novel dose of Silybum marianum (L.) Gaertn. (silymarin) extract supplement: A Triple-blinded randomized controlled clinical trial. Phytomedicine 2018, 44, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Rizk, S.M.; Sabri, N.A. Evaluation of clinical activity and safety of Daflon 500 mg in type 2 diabetic female patients. Saudi Pharm. J. 2009, 17, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Paulis, A.; Romano, G.; Barletta, D.; Fabiani, A. Rationale of combination therapy with antioxidants in medical management of Peyronie’s disease: Results of clinical application. Res. Rep. Urol. 2017, 9, 129–139. [Google Scholar] [CrossRef][Green Version]
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 2021, 183, 109119. [Google Scholar] [CrossRef]
- Langston, J.P.; Carson, C.C., III. Peyronie’s disease: Review and recent advances. Maturitas 2014, 78, 341–343. [Google Scholar] [CrossRef]
- Barrett-Harlow, B.; Wang, R. Oral therapy for Peyronie’s disease, does it work? Transl. Androl. Urol. 2016, 5, 296–302. [Google Scholar] [CrossRef] [PubMed]

| Name | Acronym | Activity | Cellular Source | Positive Regulators |
|---|---|---|---|---|
| Nuclear factor-B | NF-kB | It controls the transcription of DNA. It induces gene overexpression of TGF-ß1, iNOS, bFGF, fibrin, collagen, etc. | All cell types | ROS, TGF-beta-1, IL-1, TNF-alpha |
| Inducible nitric oxide synthase | i-NOS | It induces local overproduction of nitric oxide radical (NO •). It enhances collagen synthesis. | Macrophages, monocytes, T-lymphocytes, smooth muscle cells, fibroblasts, myofibroblasts | NF-kB, IL-1, TNF-alpha |
| Transforming growth factor beta-1 | TGF-beta-1 | Chemotactic action on neutrophils, monocytes, lymphocytes, and fibroblasts. It induces the production of collagen by fibroblasts. It stimulates the proliferation of fibroblasts and the transformation of fibroblasts into myofibroblasts. It induces collagen synthesis and deposition. It induces the production of ROS. It increases the synthesis of tissue inhibitors of matrix metalloproteinase (TIMP-1). It inhibits the production of matrix metalloproteinases (MMPs) with collagenase action (MMP-1, MMP-8, and MMP-13). It induces the production of MMP-2 and MMP-9 (with elastase activity). It induces the activation of NF-kB. It induces osteogenesis in PD plaque. It inhibits production of plasminogen activator inhibitor-1 (PAI-1). | Platelets, macrophages, neutrophils, T-lymphocytes | NF-kB, Reactive oxygen species (ROS), PAI-1 |
| Platelet-derived growth factor | PDGF | Chemotactic action on fibroblasts. It induces the production of TIMP-1 and MMP-2 (with elastase activity). It induces collagen synthesis and deposition. It stimulates the proliferation of fibroblasts and the transformation of fibroblasts into myofibroblasts. It contributes to plaque calcification and ossification. Furthermore, it acts as an osteoblast recruiter. | Platelets and macrophages | Local accumulation of fibrin |
| Interleukin-1 | IL-1 | Chemotactic action on fibroblasts. It induces collagen synthesis and deposition. It stimulates bFGF and iNOS production. It induces the activation of NF-kB. It increases the production of MMPs. | Macrophages and fibroblasts | Thrombin in the damaged site |
| Basic fibroblast growth factor | bFGF | Chemotactic action fibroblasts. It stimulates the proliferation of fibroblasts. It induces collagen synthesis and deposition. It increases the synthesis of tissue inhibitors of matrix metalloproteinase (TIMP-1). It induces the production of MMP-2, MMP-9 (with elastase activity). It determines the further deposition of fibrin on site. | Fibroblasts, myofibroblasts, T-lymphocytes | Nuclear factor kappa-B (NF-kB), IL-1 PAI-1 |
| Plasminogen activator inhibitor-1 | PAI-1 | It inhibits fibrinolysis by determining the persistence of fibrin in loco and triggering the recruitment of inflammatory cells. It stimulates the release of profibrogenic factors (cytokines, etc.) and then it induces collagen synthesis and deposition. It hinders collagenolysis by inhibiting MMPs with collagenase action. It increases the synthesis of MMP-9 (with elastase activity). | Platelets, endothelial cells, smooth muscle cells, fibroblasts, monocytes, macrophages | Thrombin in the damaged site TNF-alpha |
| Tumor necrosis factor-alpha | TNF-alpha | It induces the synthesis of PAI-1. It stimulates the proliferation of fibroblasts. At high concentrations it stimulates collagenase synthesis in fibroblasts. It stimulates iNOS production. It induces the activation of NF-kB. It increases the synthesis of MMP-9 (with elastase activity). It induces cellular apoptosis. | Monocytes, macrophages, T-lymphocytes | Fibrinogen and fibrin |
| Tissue inhibitors of metalloproteinases | TIMPs | They inhibit matrix metalloproteinases (MMPs). They regulate the connective tissue metabolism. | Many cell types (monocytes, macrophages, vascular smooth muscle cells, fibroblasts) | TGF-beta-1, PDGF, bFGF |
| Matrix metalloproteinases (MMPs) | MMP-1, MMP-2, MMP-8, MMP-9, MMP-10, MMP-12, MMP-13, MMP-18 | MMP-2, MMP-9, MMP-10, MMP-12 (with elastase activity). MMP-1, MM- 8, MMP-13, MMP-18 (with collagenase action). MMPs can regulate cytokine activity. | Fibroblasts, myofibroblasts, neutrophils, macrophages, endothelial cells, vascular smooth muscle cells | IL-1, bFGF, TNF-alpha, PAI-1, PDGF, TGF-beta-1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paulis, G.; De Giorgio, G.; Paulis, L. Role of Oxidative Stress in Peyronie’s Disease: Biochemical Evidence and Experiences of Treatment with Antioxidants. Int. J. Mol. Sci. 2022, 23, 15969. https://doi.org/10.3390/ijms232415969
Paulis G, De Giorgio G, Paulis L. Role of Oxidative Stress in Peyronie’s Disease: Biochemical Evidence and Experiences of Treatment with Antioxidants. International Journal of Molecular Sciences. 2022; 23(24):15969. https://doi.org/10.3390/ijms232415969
Chicago/Turabian StylePaulis, Gianni, Giovanni De Giorgio, and Luca Paulis. 2022. "Role of Oxidative Stress in Peyronie’s Disease: Biochemical Evidence and Experiences of Treatment with Antioxidants" International Journal of Molecular Sciences 23, no. 24: 15969. https://doi.org/10.3390/ijms232415969
APA StylePaulis, G., De Giorgio, G., & Paulis, L. (2022). Role of Oxidative Stress in Peyronie’s Disease: Biochemical Evidence and Experiences of Treatment with Antioxidants. International Journal of Molecular Sciences, 23(24), 15969. https://doi.org/10.3390/ijms232415969







