Thyroid Hormone Transporters in Pregnancy and Fetal Development
Abstract
:1. Introduction
2. General Overview of Thyroid Hormone Transporters
3. Thyroid Hormone Transporters during Fetal Development
3.1. MCT8
3.1.1. Substrates
3.1.2. MCT8 Deficiency
3.1.3. (Prenatal) Treatment of MCT8-Deficiency
3.2. MCT10
3.2.1. Substrates
3.2.2. Expression and Tissue Distribution
3.2.3. Physiological or Clinical Relevance
3.3. LATs
3.3.1. Substrates
3.3.2. Expression and Tissue Distribution
3.3.3. Physiological or Clinical Relevance
3.4. NTCP
3.4.1. Substrates
3.4.2. Expression and Tissue Distribution
3.4.3. Physiological or Clinical Relevance
3.5. SLC17A4
3.5.1. Substrates
3.5.2. Expression and Tissue Distribution
3.5.3. Physiological or Clinical Relevance
3.6. OATPs
3.6.1. Substrates
3.6.2. Expression and Tissue Distribution
3.6.3. Physiological or Clinical Relevance
3.7. ABCB1
4. Thyroid Hormone Transporters in the Human Placental Barrier
5. Future Perspectives
5.1. Physiological Role of Thyroid Hormone Transporters
5.2. Models for Placenta and Fetal Tissues
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Yen, P.M. Physiological and molecular basis of thyroid hormone action. Physiol. Rev. 2001, 81, 1097–1142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luongo, C.; Dentice, M.; Salvatore, D. Deiodinases and their intricate role in thyroid hormone homeostasis. Nat. Rev. Endocrinol. 2019, 15, 479–488. [Google Scholar] [CrossRef] [PubMed]
- Visser, T.J. Role of sulfation in thyroid hormone metabolism. Chem. Biol. Interact. 1994, 92, 293–303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, J.; Landers, K.; Li, H.; Mortimer, R.H.; Richard, K. Delivery of maternal thyroid hormones to the fetus. Trends Endocrinol. Metab. 2011, 22, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Haddow, J.E.; Palomaki, G.E.; Allan, W.C.; Williams, J.R.; Knight, G.J.; Gagnon, J.; O’Heir, C.E.; Mitchell, M.L.; Hermos, R.J.; Waisbren, S.E.; et al. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N. Engl. J. Med. 1999, 341, 549–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korevaar, T.I.; Muetzel, R.; Medici, M.; Chaker, L.; Jaddoe, V.W.; de Rijke, Y.B.; Steegers, E.A.; Visser, T.J.; White, T.; Tiemeier, H.; et al. Association of maternal thyroid function during early pregnancy with offspring IQ and brain morphology in childhood: A population-based prospective cohort study. Lancet Diabetes Endocrinol. 2016, 4, 35–43. [Google Scholar] [CrossRef]
- Johannes, J.; Jayarama-Naidu, R.; Meyer, F.; Wirth, E.K.; Schweizer, U.; Schomburg, L.; Kohrle, J.; Renko, K. Silychristin, a Flavonolignan Derived From the Milk Thistle, Is a Potent Inhibitor of the Thyroid Hormone Transporter MCT8. Endocrinology 2016, 157, 1694–1701. [Google Scholar] [CrossRef]
- Cao, J.; O’Day, D.R.; Pliner, H.A.; Kingsley, P.D.; Deng, M.; Daza, R.M.; Zager, M.A.; Aldinger, K.A.; Blecher-Gonen, R.; Zhang, F.; et al. A human cell atlas of fetal gene expression. Science 2020, 370, 6518. [Google Scholar] [CrossRef]
- Roost, M.S.; van Iperen, L.; Ariyurek, Y.; Buermans, H.P.; Arindrarto, W.; Devalla, H.D.; Passier, R.; Mummery, C.L.; Carlotti, F.; de Koning, E.J.; et al. KeyGenes, a Tool to Probe Tissue Differentiation Using a Human Fetal Transcriptional Atlas. Stem Cell Rep. 2015, 4, 1112–1124. [Google Scholar] [CrossRef] [Green Version]
- Hennemann, G.; Docter, R.; Friesema, E.C.; de Jong, M.; Krenning, E.P.; Visser, T.J. Plasma membrane transport of thyroid hormones and its role in thyroid hormone metabolism and bioavailability. Endocr. Rev. 2001, 22, 451–476. [Google Scholar] [CrossRef]
- Groeneweg, S.; van Geest, F.S.; Peeters, R.P.; Heuer, H.; Visser, W.E. Thyroid Hormone Transporters. Endocr. Rev. 2020, 41, bnz008. [Google Scholar] [CrossRef] [PubMed]
- Schweizer, U.; Johannes, J.; Bayer, D.; Braun, D. Structure and function of thyroid hormone plasma membrane transporters. Eur. Thyroid J. 2014, 3, 143–153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friesema, E.C.; Ganguly, S.; Abdalla, A.; Manning Fox, J.E.; Halestrap, A.P.; Visser, T.J. Identification of monocarboxylate transporter 8 as a specific thyroid hormone transporter. J. Biol. Chem. 2003, 278, 40128–40135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friesema, E.C.; Jansen, J.; Jachtenberg, J.W.; Visser, W.E.; Kester, M.H.; Visser, T.J. Effective cellular uptake and efflux of thyroid hormone by human monocarboxylate transporter 10. Mol. Endocrinol. 2008, 22, 1357–1369. [Google Scholar] [CrossRef] [Green Version]
- Friesema, E.C.; Grueters, A.; Biebermann, H.; Krude, H.; von Moers, A.; Reeser, M.; Barrett, T.G.; Mancilla, E.E.; Svensson, J.; Kester, M.H.; et al. Association between mutations in a thyroid hormone transporter and severe X-linked psychomotor retardation. Lancet 2004, 364, 1435–1437. [Google Scholar] [CrossRef]
- Chan, S.Y.; Martin-Santos, A.; Loubiere, L.S.; Gonzalez, A.M.; Stieger, B.; Logan, A.; McCabe, C.J.; Franklyn, J.A.; Kilby, M.D. The expression of thyroid hormone transporters in the human fetal cerebral cortex during early development and in N-Tera-2 neurodifferentiation. J. Physiol. 2011, 589, 2827–2845. [Google Scholar] [CrossRef] [Green Version]
- Heuer, H.; Maier, M.K.; Iden, S.; Mittag, J.; Friesema, E.C.; Visser, T.J.; Bauer, K. The monocarboxylate transporter 8 linked to human psychomotor retardation is highly expressed in thyroid hormone-sensitive neuron populations. Endocrinology 2005, 146, 1701–1706. [Google Scholar] [CrossRef] [Green Version]
- Friesema, E.C.; Visser, T.J.; Borgers, A.J.; Kalsbeek, A.; Swaab, D.F.; Fliers, E.; Alkemade, A. Thyroid hormone transporters and deiodinases in the developing human hypothalamus. Eur. J. Endocrinol. 2012, 167, 379–386. [Google Scholar] [CrossRef] [Green Version]
- Friesema, E.C.; Docter, R.; Moerings, E.P.; Verrey, F.; Krenning, E.P.; Hennemann, G.; Visser, T.J. Thyroid hormone transport by the heterodimeric human system L amino acid transporter. Endocrinology 2001, 142, 4339–4348. [Google Scholar] [CrossRef]
- Zevenbergen, C.; Meima, M.E.; Lima de Souza, E.C.; Peeters, R.P.; Kinne, A.; Krause, G.; Visser, W.E.; Visser, T.J. Transport of Iodothyronines by Human L-Type Amino Acid Transporters. Endocrinology 2015, 156, 4345–4355. [Google Scholar] [CrossRef]
- Kinne, A.; Wittner, M.; Wirth, E.K.; Hinz, K.M.; Schulein, R.; Kohrle, J.; Krause, G. Involvement of the L-Type Amino Acid Transporter Lat2 in the Transport of 3,3′-Diiodothyronine across the Plasma Membrane. Eur. Thyroid J. 2015, 4, 42–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hinz, K.M.; Neef, D.; Rutz, C.; Furkert, J.; Kohrle, J.; Schulein, R.; Krause, G. Molecular features of the L-type amino acid transporter 2 determine different import and export profiles for thyroid hormones and amino acids. Mol. Cell Endocrinol. 2017, 443, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Wirth, E.K.; Roth, S.; Blechschmidt, C.; Holter, S.M.; Becker, L.; Racz, I.; Zimmer, A.; Klopstock, T.; Gailus-Durner, V.; Fuchs, H.; et al. Neuronal 3′,3,5-triiodothyronine (T3) uptake and behavioral phenotype of mice deficient in Mct8, the neuronal T3 transporter mutated in Allan-Herndon-Dudley syndrome. J. Neurosci. 2009, 29, 9439–9449. [Google Scholar] [CrossRef] [PubMed]
- Friesema, E.C.; Docter, R.; Moerings, E.P.; Stieger, B.; Hagenbuch, B.; Meier, P.J.; Krenning, E.P.; Hennemann, G.; Visser, T.J. Identification of thyroid hormone transporters. Biochem. Biophys. Res. Commun. 1999, 254, 497–501. [Google Scholar] [CrossRef]
- Visser, W.E.; Wong, W.S.; van Mullem, A.A.; Friesema, E.C.; Geyer, J.; Visser, T.J. Study of the transport of thyroid hormone by transporters of the SLC10 family. Mol. Cell Endocrinol. 2010, 315, 138–145. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.L.; Chen, H.L.; Liu, Y.J.; Feng, C.H.; Wu, C.Y.; Shyu, M.K.; Yuan, R.H.; Chang, M.H. Developmental expression of canalicular transporter genes in human liver. J. Hepatol. 2005, 43, 472–477. [Google Scholar] [CrossRef]
- Groeneweg, S.; van Geest, F.S.; Chen, Z.; Farina, S.; van Heerebeek, R.E.A.; Meima, M.E.; Peeters, R.P.; Heuer, H.; Medici, M.; Visser, W.E. Functional Characterization of the Novel and Specific Thyroid Hormone Transporter SLC17A4. Thyroid 2022, 32, 326–335. [Google Scholar] [CrossRef]
- Teumer, A.; Chaker, L.; Groeneweg, S.; Li, Y.; Di Munno, C.; Barbieri, C.; Schultheiss, U.T.; Traglia, M.; Ahluwalia, T.S.; Akiyama, M.; et al. Genome-wide analyses identify a role for SLC17A4 and AADAT in thyroid hormone regulation. Nat. Commun. 2018, 9, 4455. [Google Scholar] [CrossRef] [Green Version]
- Fujiwara, K.; Adachi, H.; Nishio, T.; Unno, M.; Tokui, T.; Okabe, M.; Onogawa, T.; Suzuki, T.; Asano, N.; Tanemoto, M.; et al. Identification of thyroid hormone transporters in humans: Different molecules are involved in a tissue-specific manner. Endocrinology 2001, 142, 2005–2012. [Google Scholar] [CrossRef]
- Kullak-Ublick, G.A.; Hagenbuch, B.; Stieger, B.; Schteingart, C.D.; Hofmann, A.F.; Wolkoff, A.W.; Meier, P.J. Molecular and functional characterization of an organic anion transporting polypeptide cloned from human liver. Gastroenterology 1995, 109, 1274–1282. [Google Scholar] [CrossRef]
- Kullak-Ublick, G.A.; Ismair, M.G.; Stieger, B.; Landmann, L.; Huber, R.; Pizzagalli, F.; Fattinger, K.; Meier, P.J.; Hagenbuch, B. Organic anion-transporting polypeptide B (OATP-B) and its functional comparison with three other OATPs of human liver. Gastroenterology 2001, 120, 525–533. [Google Scholar] [CrossRef]
- Pizzagalli, F.; Hagenbuch, B.; Stieger, B.; Klenk, U.; Folkers, G.; Meier, P.J. Identification of a novel human organic anion transporting polypeptide as a high affinity thyroxine transporter. Mol. Endocrinol. 2002, 16, 2283–2296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van der Deure, W.M.; Hansen, P.S.; Peeters, R.P.; Kyvik, K.O.; Friesema, E.C.; Hegedus, L.; Visser, T.J. Thyroid hormone transport and metabolism by organic anion transporter 1C1 and consequences of genetic variation. Endocrinology 2008, 149, 5307–5314. [Google Scholar] [CrossRef] [PubMed]
- Huber, R.D.; Gao, B.; Sidler Pfandler, M.A.; Zhang-Fu, W.; Leuthold, S.; Hagenbuch, B.; Folkers, G.; Meier, P.J.; Stieger, B. Characterization of two splice variants of human organic anion transporting polypeptide 3A1 isolated from human brain. Am. J. Physiol. Cell Physiol. 2007, 292, C795–C806. [Google Scholar] [CrossRef]
- Leuthold, S.; Hagenbuch, B.; Mohebbi, N.; Wagner, C.A.; Meier, P.J.; Stieger, B. Mechanisms of pH-gradient driven transport mediated by organic anion polypeptide transporters. Am. J. Physiol. Cell Physiol. 2009, 296, C570–C582. [Google Scholar] [CrossRef] [Green Version]
- Mikkaichi, T.; Suzuki, T.; Onogawa, T.; Tanemoto, M.; Mizutamari, H.; Okada, M.; Chaki, T.; Masuda, S.; Tokui, T.; Eto, N.; et al. Isolation and characterization of a digoxin transporter and its rat homologue expressed in the kidney. Proc. Natl. Acad. Sci. USA 2004, 101, 3569–3574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitchell, A.M.; Tom, M.; Mortimer, R.H. Thyroid hormone export from cells: Contribution of P-glycoprotein. J. Endocrinol. 2005, 185, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Sterenborg, R.; Galesloot, T.E.; Teumer, A.; Netea-Maier, R.T.; Speed, D.; Meima, M.E.; Visser, W.E.; Smit, J.W.A.; Peeters, R.P.; Medici, M. The Effects of Common Genetic Variation in 96 Genes Involved in Thyroid Hormone Regulation on TSH and FT4 Concentrations. J. Clin. Endocrinol. Metab. 2022, 107, e2276–e2283. [Google Scholar] [CrossRef]
- Groeneweg, S.; van Geest, F.S.; Abaci, A.; Alcantud, A.; Ambegaonkar, G.P.; Armour, C.M.; Bakhtiani, P.; Barca, D.; Bertini, E.S.; van Beynum, I.M.; et al. Disease characteristics of MCT8 deficiency: An international, retrospective, multicentre cohort study. Lancet Diabetes Endocrinol. 2020, 8, 594–605. [Google Scholar] [CrossRef]
- Groeneweg, S.; Kersseboom, S.; van den Berge, A.; Dolcetta-Capuzzo, A.; van Geest, F.S.; van Heerebeek, R.E.A.; Arjona, F.J.; Meima, M.E.; Peeters, R.P.; Visser, W.E.; et al. In Vitro Characterization of Human, Mouse, and Zebrafish MCT8 Orthologues. Thyroid 2019, 29, 1499–1510. [Google Scholar] [CrossRef]
- Dumitrescu, A.M.; Liao, X.H.; Weiss, R.E.; Millen, K.; Refetoff, S. Tissue-specific thyroid hormone deprivation and excess in monocarboxylate transporter (mct) 8-deficient mice. Endocrinology 2006, 147, 4036–4043. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liao, X.H.; Di Cosmo, C.; Dumitrescu, A.M.; Hernandez, A.; Van Sande, J.; St Germain, D.L.; Weiss, R.E.; Galton, V.A.; Refetoff, S. Distinct roles of deiodinases on the phenotype of Mct8 defect: A comparison of eight different mouse genotypes. Endocrinology 2011, 152, 1180–1191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muller, J.; Mayerl, S.; Visser, T.J.; Darras, V.M.; Boelen, A.; Frappart, L.; Mariotta, L.; Verrey, F.; Heuer, H. Tissue-specific alterations in thyroid hormone homeostasis in combined Mct10 and Mct8 deficiency. Endocrinology 2014, 155, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, A.M.; Liao, X.H.; Gil-Ibanez, P.; Marcinkowski, T.; Bernal, J.; Weiss, R.E.; Dumitrescu, A.M.; Refetoff, S. Changes in thyroid status during perinatal development of MCT8-deficient male mice. Endocrinology 2013, 154, 2533–2541. [Google Scholar] [CrossRef] [Green Version]
- Lopez-Espindola, D.; Morales-Bastos, C.; Grijota-Martinez, C.; Liao, X.H.; Lev, D.; Sugo, E.; Verge, C.F.; Refetoff, S.; Bernal, J.; Guadano-Ferraz, A. Mutations of the thyroid hormone transporter MCT8 cause prenatal brain damage and persistent hypomyelination. J. Clin. Endocrinol. Metab. 2014, 99, E2799–E2804. [Google Scholar] [CrossRef]
- Roberts, L.M.; Woodford, K.; Zhou, M.; Black, D.S.; Haggerty, J.E.; Tate, E.H.; Grindstaff, K.K.; Mengesha, W.; Raman, C.; Zerangue, N. Expression of the thyroid hormone transporters monocarboxylate transporter-8 (SLC16A2) and organic ion transporter-14 (SLCO1C1) at the blood-brain barrier. Endocrinology 2008, 149, 6251–6261. [Google Scholar] [CrossRef]
- Lopez-Espindola, D.; Garcia-Aldea, A.; Gomez de la Riva, I.; Rodriguez-Garcia, A.M.; Salvatore, D.; Visser, T.J.; Bernal, J.; Guadano-Ferraz, A. Thyroid hormone availability in the human fetal brain: Novel entry pathways and role of radial glia. Brain Struct. Funct. 2019, 224, 2103–2119. [Google Scholar] [CrossRef]
- Wilpert, N.M.; Krueger, M.; Opitz, R.; Sebinger, D.; Paisdzior, S.; Mages, B.; Schulz, A.; Spranger, J.; Wirth, E.K.; Stachelscheid, H.; et al. Spatiotemporal Changes of Cerebral Monocarboxylate Transporter 8 Expression. Thyroid 2020, 30, 1366–1383. [Google Scholar] [CrossRef] [Green Version]
- Vatine, G.D.; Al-Ahmad, A.; Barriga, B.K.; Svendsen, S.; Salim, A.; Garcia, L.; Garcia, V.J.; Ho, R.; Yucer, N.; Qian, T.; et al. Modeling Psychomotor Retardation using iPSCs from MCT8-Deficient Patients Indicates a Prominent Role for the Blood-Brain Barrier. Cell Stem Cell 2017, 20, 831–843.e5. [Google Scholar] [CrossRef] [Green Version]
- Iwayama, H.; Kakita, H.; Iwasa, M.; Adachi, S.; Takano, K.; Kikuchi, M.; Fujisawa, Y.; Osaka, H.; Yamada, Y.; Okumura, A.; et al. Measurement of Reverse Triiodothyronine Level and the Triiodothyronine to Reverse Triiodothyronine Ratio in Dried Blood Spot Samples at Birth May Facilitate Early Detection of Monocarboxylate Transporter 8 Deficiency. Thyroid 2021, 31, 1316–1321. [Google Scholar] [CrossRef]
- Chan, S.Y.; Hancox, L.A.; Martin-Santos, A.; Loubiere, L.S.; Walter, M.N.; Gonzalez, A.M.; Cox, P.M.; Logan, A.; McCabe, C.J.; Franklyn, J.A.; et al. MCT8 expression in human fetal cerebral cortex is reduced in severe intrauterine growth restriction. J. Endocrinol. 2014, 220, 85–95. [Google Scholar] [CrossRef] [Green Version]
- Trajkovic, M.; Visser, T.J.; Mittag, J.; Horn, S.; Lukas, J.; Darras, V.M.; Raivich, G.; Bauer, K.; Heuer, H. Abnormal thyroid hormone metabolism in mice lacking the monocarboxylate transporter 8. J. Clin. Investig. 2007, 117, 627–635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mayerl, S.; Muller, J.; Bauer, R.; Richert, S.; Kassmann, C.M.; Darras, V.M.; Buder, K.; Boelen, A.; Visser, T.J.; Heuer, H. Transporters MCT8 and OATP1C1 maintain murine brain thyroid hormone homeostasis. J. Clin. Investig. 2014, 124, 1987–1999. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adu-Gyamfi, E.A.; Wang, Y.X.; Ding, Y.B. The interplay between thyroid hormones and the placenta: A comprehensive reviewdagger. Biol. Reprod. 2020, 102, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Grijota-Martinez, C.; Diez, D.; Morreale de Escobar, G.; Bernal, J.; Morte, B. Lack of action of exogenously administered T3 on the fetal rat brain despite expression of the monocarboxylate transporter 8. Endocrinology 2011, 152, 1713–1721. [Google Scholar] [CrossRef]
- Morte, B.; Gil-Ibanez, P.; Bernal, J. Regulation of Gene Expression by Thyroid Hormone in Primary Astrocytes: Factors Influencing the Genomic Response. Endocrinology 2018, 159, 2083–2092. [Google Scholar] [CrossRef] [Green Version]
- Verge, C.F.; Konrad, D.; Cohen, M.; Di Cosmo, C.; Dumitrescu, A.M.; Marcinkowski, T.; Hameed, S.; Hamilton, J.; Weiss, R.E.; Refetoff, S. Diiodothyropropionic acid (DITPA) in the treatment of MCT8 deficiency. J. Clin. Endocrinol. Metab. 2012, 97, 4515–4523. [Google Scholar] [CrossRef] [Green Version]
- Groeneweg, S.; Peeters, R.P.; Moran, C.; Stoupa, A.; Auriol, F.; Tonduti, D.; Dica, A.; Paone, L.; Rozenkova, K.; Malikova, J.; et al. Effectiveness and safety of the tri-iodothyronine analogue Triac in children and adults with MCT8 deficiency: An international, single-arm, open-label, phase 2 trial. Lancet Diabetes Endocrinol. 2019, 7, 695–706. [Google Scholar] [CrossRef]
- Refetoff, S.; Pappa, T.; Williams, M.K.; Matheus, M.G.; Liao, X.H.; Hansen, K.; Nicol, L.; Pierce, M.; Blasco, P.A.; Wiebers Jensen, M.; et al. Prenatal Treatment of Thyroid Hormone Cell Membrane Transport Defect Caused by MCT8 Gene Mutation. Thyroid 2021, 31, 713–720. [Google Scholar] [CrossRef]
- Liao, X.H.; Avalos, P.; Shelest, O.; Ofan, R.; Shilo, M.; Bresee, C.; Likhite, S.; Vit, J.P.; Heuer, H.; Kaspar, B.; et al. AAV9-MCT8 Delivery at Juvenile Stage Ameliorates Neurological and Behavioral Deficits in a Mouse Model of MCT8-Deficiency. Thyroid 2022, 32, 849–859. [Google Scholar] [CrossRef]
- Sundaram, S.M.; Arrulo Pereira, A.; Muller-Fielitz, H.; Kopke, H.; De Angelis, M.; Muller, T.D.; Heuer, H.; Korbelin, J.; Krohn, M.; Mittag, J.; et al. Gene therapy targeting the blood-brain barrier improves neurological symptoms in a model of genetic MCT8 deficiency. Brain 2022, awac243. [Google Scholar] [CrossRef] [PubMed]
- Braun, D.; Bohleber, S.; Vatine, G.D.; Svendsen, C.N.; Schweizer, U. Sodium Phenylbutyrate Rescues Thyroid Hormone Transport in Brain Endothelial-Like Cells. Thyroid 2022, 32, 860–870. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.K.; Kanai, Y.; Chairoungdua, A.; Matsuo, H.; Cha, S.H.; Endou, H. Expression cloning of a Na+-independent aromatic amino acid transporter with structural similarity to H+/monocarboxylate transporters. J. Biol. Chem. 2001, 276, 17221–17228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, D.K.; Kanai, Y.; Matsuo, H.; Kim, J.Y.; Chairoungdua, A.; Kobayashi, Y.; Enomoto, A.; Cha, S.H.; Goya, T.; Endou, H. The human T-type amino acid transporter-1: Characterization, gene organization, and chromosomal location. Genomics 2002, 79, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Mariotta, L.; Ramadan, T.; Singer, D.; Guetg, A.; Herzog, B.; Stoeger, C.; Palacin, M.; Lahoutte, T.; Camargo, S.M.; Verrey, F. T-type amino acid transporter TAT1 (Slc16a10) is essential for extracellular aromatic amino acid homeostasis control. J. Physiol. 2012, 590, 6413–6424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yanagida, O.; Kanai, Y.; Chairoungdua, A.; Kim, D.K.; Segawa, H.; Nii, T.; Cha, S.H.; Matsuo, H.; Fukushima, J.; Fukasawa, Y.; et al. Human L-type amino acid transporter 1 (LAT1): Characterization of function and expression in tumor cell lines. Biochim. Biophys. Acta 2001, 1514, 291–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fotiadis, D.; Kanai, Y.; Palacin, M. The SLC3 and SLC7 families of amino acid transporters. Mol. Aspects Med. 2013, 34, 139–158. [Google Scholar] [CrossRef]
- Roberts, L.M.; Black, D.S.; Raman, C.; Woodford, K.; Zhou, M.; Haggerty, J.E.; Yan, A.T.; Cwirla, S.E.; Grindstaff, K.K. Subcellular localization of transporters along the rat blood-brain barrier and blood-cerebral-spinal fluid barrier by in vivo biotinylation. Neuroscience 2008, 155, 423–438. [Google Scholar] [CrossRef] [PubMed]
- Muller, J.; Heuer, H. Expression pattern of thyroid hormone transporters in the postnatal mouse brain. Front. Endocrinol. 2014, 5, 92. [Google Scholar] [CrossRef] [Green Version]
- Poncet, N.; Mitchell, F.E.; Ibrahim, A.F.; McGuire, V.A.; English, G.; Arthur, J.S.; Shi, Y.B.; Taylor, P.M. The catalytic subunit of the system L1 amino acid transporter (slc7a5) facilitates nutrient signalling in mouse skeletal muscle. PLoS ONE 2014, 9, e89547. [Google Scholar] [CrossRef]
- Braun, D.; Kinne, A.; Brauer, A.U.; Sapin, R.; Klein, M.O.; Kohrle, J.; Wirth, E.K.; Schweizer, U. Developmental and cell type-specific expression of thyroid hormone transporters in the mouse brain and in primary brain cells. Glia 2011, 59, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Nunez, B.; Martinez de Mena, R.; Obregon, M.J.; Font-Llitjos, M.; Nunes, V.; Palacin, M.; Dumitrescu, A.M.; Morte, B.; Bernal, J. Cerebral cortex hyperthyroidism of newborn mct8-deficient mice transiently suppressed by lat2 inactivation. PLoS ONE 2014, 9, e96915. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hagenbuch, B.; Meier, P.J. Molecular cloning, chromosomal localization, and functional characterization of a human liver Na+/bile acid cotransporter. J. Clin. Investig. 1994, 93, 1326–1331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Craddock, A.L.; Love, M.W.; Daniel, R.W.; Kirby, L.C.; Walters, H.C.; Wong, M.H.; Dawson, P.A. Expression and transport properties of the human ileal and renal sodium-dependent bile acid transporter. Am. J. Physiol. 1998, 274, G157–G169. [Google Scholar] [CrossRef]
- Kullak-Ublick, G.A.; Glasa, J.; Boker, C.; Oswald, M.; Grutzner, U.; Hagenbuch, B.; Stieger, B.; Meier, P.J.; Beuers, U.; Kramer, W.; et al. Chlorambucil-taurocholate is transported by bile acid carriers expressed in human hepatocellular carcinomas. Gastroenterology 1997, 113, 1295–1305. [Google Scholar] [CrossRef]
- Cheng, X.; Buckley, D.; Klaassen, C.D. Regulation of hepatic bile acid transporters Ntcp and Bsep expression. Biochem. Pharmacol. 2007, 74, 1665–1676. [Google Scholar] [CrossRef] [Green Version]
- Ananthanarayanan, M.; Ng, O.C.; Boyer, J.L.; Suchy, F.J. Characterization of cloned rat liver Na(+)-bile acid cotransporter using peptide and fusion protein antibodies. Am. J. Physiol. 1994, 267, G637–G643. [Google Scholar] [CrossRef]
- Zhang, Q.; He, Z.; Liu, Z.; Gong, L. Integrated plasma and liver gas chromatography mass spectrometry and liquid chromatography mass spectrometry metabolomics to reveal physiological functions of sodium taurocholate cotransporting polypeptide (NTCP) with an Ntcp knockout mouse model. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2021, 1165, 122531. [Google Scholar] [CrossRef]
- Mao, F.; Wang, M.X.; Hou, X.; Zhou, Z.; Yan, Y.Y.; Fang, L.J.; Tan, Z.; Fang, W.Y.; Liu, T.; He, W.; et al. NTCP Deficiency Causes Gallbladder Abnormalities in Mice and Human Beings. Cell Mol. Gastroenterol. Hepatol. 2021, 11, 831–839. [Google Scholar] [CrossRef]
- Mao, F.; Liu, T.; Hou, X.; Zhao, H.; He, W.; Li, C.; Jing, Z.; Sui, J.; Wang, F.; Liu, X.; et al. Increased sulfation of bile acids in mice and human subjects with sodium taurocholate cotransporting polypeptide deficiency. J. Biol. Chem. 2019, 294, 11853–11862. [Google Scholar] [CrossRef]
- Slijepcevic, D.; Kaufman, C.; Wichers, C.G.; Gilglioni, E.H.; Lempp, F.A.; Duijst, S.; de Waart, D.R.; Elferink, R.P.; Mier, W.; Stieger, B.; et al. Impaired uptake of conjugated bile acids and hepatitis b virus pres1-binding in Na(+)-taurocholate cotransporting polypeptide knockout mice. Hepatology 2015, 62, 207–219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deng, M.; Mao, M.; Guo, L.; Chen, F.P.; Wen, W.R.; Song, Y.Z. Clinical and molecular study of a pediatric patient with sodium taurocholate cotransporting polypeptide deficiency. Exp. Ther. Med. 2016, 12, 3294–3300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaz, F.M.; Paulusma, C.C.; Huidekoper, H.; de Ru, M.; Lim, C.; Koster, J.; Ho-Mok, K.; Bootsma, A.H.; Groen, A.K.; Schaap, F.G.; et al. Sodium taurocholate cotransporting polypeptide (SLC10A1) deficiency: Conjugated hypercholanemia without a clear clinical phenotype. Hepatology 2015, 61, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Togawa, N.; Miyaji, T.; Izawa, S.; Omote, H.; Moriyama, Y. A Na+-phosphate cotransporter homologue (SLC17A4 protein) is an intestinal organic anion exporter. Am. J. Physiol. Cell Physiol. 2012, 302, C1652–C1660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roth, M.; Obaidat, A.; Hagenbuch, B. OATPs, OATs and OCTs: The organic anion and cation transporters of the SLCO and SLC22A gene superfamilies. Br. J. Pharmacol. 2012, 165, 1260–1287. [Google Scholar] [CrossRef] [Green Version]
- Hagenbuch, B. Cellular entry of thyroid hormones by organic anion transporting polypeptides. Best Pract Res. Clin. Endocrinol. Metab. 2007, 21, 209–221. [Google Scholar] [CrossRef]
- Chen, Z.; van der Sman, A.S.E.; Groeneweg, S.; de Rooij, L.J.; Visser, W.E.; Peeters, R.P.; Meima, M.E. Thyroid hormone transporters in a human placental cell model. Thyroid 2022, 32, 1129–1137. [Google Scholar] [CrossRef]
- Loubiere, L.S.; Vasilopoulou, E.; Bulmer, J.N.; Taylor, P.M.; Stieger, B.; Verrey, F.; McCabe, C.J.; Franklyn, J.A.; Kilby, M.D.; Chan, S.Y. Expression of thyroid hormone transporters in the human placenta and changes associated with intrauterine growth restriction. Placenta 2010, 31, 295–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mayerl, S.; Visser, T.J.; Darras, V.M.; Horn, S.; Heuer, H. Impact of Oatp1c1 deficiency on thyroid hormone metabolism and action in the mouse brain. Endocrinology 2012, 153, 1528–1537. [Google Scholar] [CrossRef] [Green Version]
- Sugiyama, D.; Kusuhara, H.; Taniguchi, H.; Ishikawa, S.; Nozaki, Y.; Aburatani, H.; Sugiyama, Y. Functional characterization of rat brain-specific organic anion transporter (Oatp14) at the blood-brain barrier: High affinity transporter for thyroxine. J. Biol. Chem. 2003, 278, 43489–43495. [Google Scholar] [CrossRef]
- Tohyama, K.; Kusuhara, H.; Sugiyama, Y. Involvement of multispecific organic anion transporter, Oatp14 (Slc21a14), in the transport of thyroxine across the blood-brain barrier. Endocrinology 2004, 145, 4384–4391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van der Deure, W.M.; Peeters, R.P.; Visser, T.J. Molecular aspects of thyroid hormone transporters, including MCT8, MCT10, and OATPs, and the effects of genetic variation in these transporters. J. Mol. Endocrinol. 2010, 44, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van der Deure, W.M.; Friesema, E.C.; de Jong, F.J.; de Rijke, Y.B.; de Jong, F.H.; Uitterlinden, A.G.; Breteler, M.M.; Peeters, R.P.; Visser, T.J. Organic anion transporter 1B1: An important factor in hepatic thyroid hormone and estrogen transport and metabolism. Endocrinology 2008, 149, 4695–4701. [Google Scholar] [CrossRef] [PubMed]
- Stromme, P.; Groeneweg, S.; Lima de Souza, E.C.; Zevenbergen, C.; Torgersbraten, A.; Holmgren, A.; Gurcan, E.; Meima, M.E.; Peeters, R.P.; Visser, W.E.; et al. Mutated Thyroid Hormone Transporter OATP1C1 Associates with Severe Brain Hypometabolism and Juvenile Neurodegeneration. Thyroid 2018, 28, 1406–1415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diez, D.; Morte, B.; Bernal, J. Single-Cell Transcriptome Profiling of Thyroid Hormone Effectors in the Human Fetal Neocortex: Expression of SLCO1C1, DIO2, and THRB in Specific Cell Types. Thyroid 2021, 31, 1577–1588. [Google Scholar] [CrossRef] [PubMed]
- Zibara, K.; Zein, N.E.; Sabra, M.; Hneino, M.; Harati, H.; Mohamed, W.; Kobeissy, F.H.; Kassem, N. Thyroxine (T4) Transfer from Blood to Cerebrospinal Fluid in Sheep Isolated Perfused Choroid Plexus: Role of Multidrug Resistance-Associated Proteins and Organic Anion Transporting Polypeptides. Front. Neurol. 2017, 8, 214. [Google Scholar] [CrossRef] [Green Version]
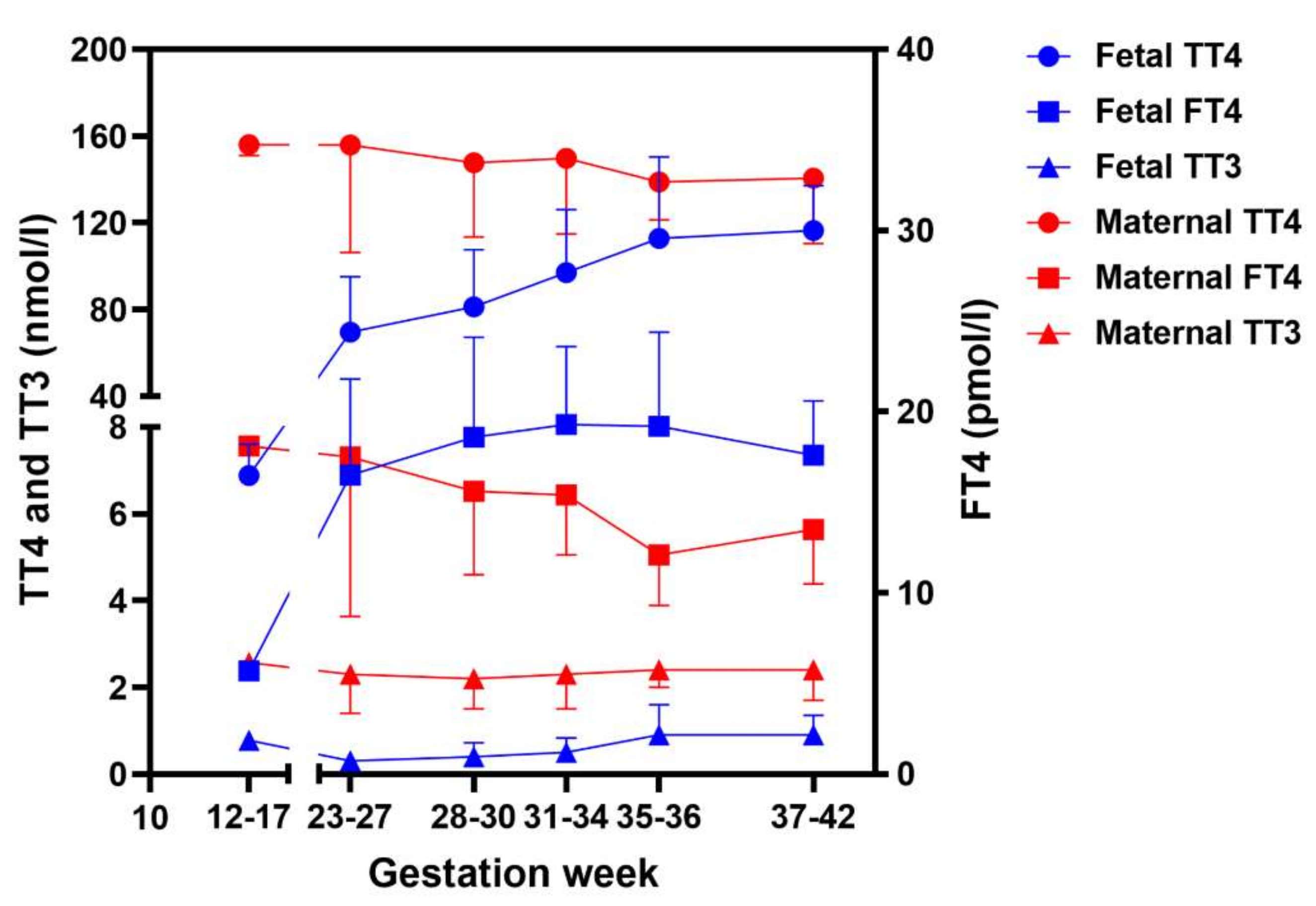
- Calvo, R.M.; Jauniaux, E.; Gulbis, B.; Asuncion, M.; Gervy, C.; Contempre, B.; Morreale de Escobar, G. Fetal tissues are exposed to biologically relevant free thyroxine concentrations during early phases of development. J. Clin. Endocrinol. Metab. 2002, 87, 1768–1777. [Google Scholar] [CrossRef]
- Landers, K.; Richard, K. Traversing barriers—How thyroid hormones pass placental, blood-brain and blood-cerebrospinal fluid barriers. Mol. Cell Endocrinol. 2017, 458, 22–28. [Google Scholar] [CrossRef] [Green Version]
- Grumbach, M.M.; Werner, S.C. Transfer of thyroid hormone across the human placenta at term. J. Clin. Endocrinol. Metab. 1956, 16, 1392–1395. [Google Scholar] [CrossRef]
- Hume, R.; Simpson, J.; Delahunty, C.; van Toor, H.; Wu, S.Y.; Williams, F.L.; Visser, T.J.; Scottish Preterm Thyroid, G. Human fetal and cord serum thyroid hormones: Developmental trends and interrelationships. J. Clin. Endocrinol. Metab. 2004, 89, 4097–4103. [Google Scholar] [CrossRef]
- Loubiere, L.S.; Vasilopoulou, E.; Glazier, J.D.; Taylor, P.M.; Franklyn, J.A.; Kilby, M.D.; Chan, S.Y. Expression and function of thyroid hormone transporters in the microvillous plasma membrane of human term placental syncytiotrophoblast. Endocrinology 2012, 153, 6126–6135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, M.; Kingdom, J.; Baczyk, D.; Lye, S.J.; Matthews, S.G.; Gibb, W. Expression of the multidrug resistance P-glycoprotein, (ABCB1 glycoprotein) in the human placenta decreases with advancing gestation. Placenta 2006, 27, 602–609. [Google Scholar] [CrossRef] [PubMed]
- Saben, J.; Zhong, Y.; McKelvey, S.; Dajani, N.K.; Andres, A.; Badger, T.M.; Gomez-Acevedo, H.; Shankar, K. A comprehensive analysis of the human placenta transcriptome. Placenta 2014, 35, 125–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, S.Y.; Franklyn, J.A.; Pemberton, H.N.; Bulmer, J.N.; Visser, T.J.; McCabe, C.J.; Kilby, M.D. Monocarboxylate transporter 8 expression in the human placenta: The effects of severe intrauterine growth restriction. J. Endocrinol. 2006, 189, 465–471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ritchie, J.W.; Taylor, P.M. Role of the System L permease LAT1 in amino acid and iodothyronine transport in placenta. Biochem. J. 2001, 356, 719–725. [Google Scholar] [CrossRef]
- St-Pierre, M.V.; Hagenbuch, B.; Ugele, B.; Meier, P.J.; Stallmach, T. Characterization of an organic anion-transporting polypeptide (OATP-B) in human placenta. J. Clin. Endocrinol. Metab. 2002, 87, 1856–1863. [Google Scholar] [CrossRef]
- Mortimer, R.H.; Galligan, J.P.; Cannell, G.R.; Addison, R.S.; Roberts, M.S. Maternal to fetal thyroxine transmission in the human term placenta is limited by inner ring deiodination. J. Clin. Endocrinol. Metab. 1996, 81, 2247–2249. [Google Scholar] [CrossRef]
- Koopdonk-Kool, J.M.; de Vijlder, J.J.; Veenboer, G.J.; Ris-Stalpers, C.; Kok, J.H.; Vulsma, T.; Boer, K.; Visser, T.J. Type II and type III deiodinase activity in human placenta as a function of gestational age. J. Clin. Endocrinol. Metab. 1996, 81, 2154–2158. [Google Scholar] [CrossRef]
- Stulp, M.R.; de Vijlder, J.J.; Ris-Stalpers, C. Placental iodothyronine deiodinase III and II ratios, mRNA expression compared to enzyme activity. Mol. Cell Endocrinol. 1998, 142, 67–73. [Google Scholar] [CrossRef]
- Ballabh, P.; Hu, F.; Kumarasiri, M.; Braun, A.; Nedergaard, M. Development of tight junction molecules in blood vessels of germinal matrix, cerebral cortex, and white matter. Pediatr. Res. 2005, 58, 791–798. [Google Scholar] [CrossRef]
- Aoki, A.; Nakashima, A.; Kusabiraki, T.; Ono, Y.; Yoshino, O.; Muto, M.; Kumasawa, K.; Yoshimori, T.; Ikawa, M.; Saito, S. Trophoblast-Specific Conditional Atg7 Knockout Mice Develop Gestational Hypertension. Am. J. Pathol. 2018, 188, 2474–2486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richard, S.; Flamant, F. Regulation of T3 Availability in the Developing Brain: The Mouse Genetics Contribution. Front. Endocrinol. 2018, 9, 265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clevers, H. Modeling Development and Disease with Organoids. Cell 2016, 165, 1586–1597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rossi, G.; Manfrin, A.; Lutolf, M.P. Progress and potential in organoid research. Nat. Rev. Genet. 2018, 19, 671–687. [Google Scholar] [CrossRef] [PubMed]
- Camp, J.G.; Badsha, F.; Florio, M.; Kanton, S.; Gerber, T.; Wilsch-Brauninger, M.; Lewitus, E.; Sykes, A.; Hevers, W.; Lancaster, M.; et al. Human cerebral organoids recapitulate gene expression programs of fetal neocortex development. Proc. Natl. Acad. Sci. USA 2015, 112, 15672–15677. [Google Scholar] [CrossRef] [Green Version]
- Quadrato, G.; Nguyen, T.; Macosko, E.Z.; Sherwood, J.L.; Min Yang, S.; Berger, D.R.; Maria, N.; Scholvin, J.; Goldman, M.; Kinney, J.P.; et al. Cell diversity and network dynamics in photosensitive human brain organoids. Nature 2017, 545, 48–53. [Google Scholar] [CrossRef] [Green Version]
- Camp, J.G.; Sekine, K.; Gerber, T.; Loeffler-Wirth, H.; Binder, H.; Gac, M.; Kanton, S.; Kageyama, J.; Damm, G.; Seehofer, D.; et al. Multilineage communication regulates human liver bud development from pluripotency. Nature 2017, 546, 533–538. [Google Scholar] [CrossRef]
- Czerniecki, S.M.; Cruz, N.M.; Harder, J.L.; Menon, R.; Annis, J.; Otto, E.A.; Gulieva, R.E.; Islas, L.V.; Kim, Y.K.; Tran, L.M.; et al. High-Throughput Screening Enhances Kidney Organoid Differentiation from Human Pluripotent Stem Cells and Enables Automated Multidimensional Phenotyping. Cell Stem Cell 2018, 22, 929–940.e4. [Google Scholar] [CrossRef]

| Transporter | Gene Name | Substrates Uptake | Substrates Efflux | Expression and Tissue Distribution | Relevance for Thyroid Hormone Physiology | Reference |
|---|---|---|---|---|---|---|
| MCT8 | SLC16A2 | T3, T4 > rT3 > 3, 3′-T2 | T3, T4 | Ubiquitously (including brain, eye, liver, kidney, muscle) | MCT8 deficiency (Allan-Herndon-Dudley syndrome) | [9,13,14,15] |
| MCT10 | SLC16A10 | T3 >> T4 | T3 | Ubiquitously (including liver, kidney, pancreas, placenta, heart, lung, stomach, brain) | Unknown | [9,14,16,17,18] |
| LAT1 | SLC7A5 | 3, 3′-T2 > rT3 > T3 > T4 | 3, 3′-T2 | Brain, liver, placenta, spleen | Unknown | [9,16,19] |
| LAT2 | SLC7A8 | 3, 3′-T2 > T3 | No | Ubiquitously (including eye, kidney, lung, pancreas, placenta, skin, spleen, stomach) | Unknown | [9,20,21,22,23] |
| NTCP | SLC10A1 | T3S, T4S > T3, T4 | No | Liver | Unknown | [9,24,25,26] |
| SLC17A4 | SLC17A4 | T3, T4 > rT3 | T3, T4 | Intestine, liver | SNP associated with serum FT4 concentrations | [9,27,28] |
| OATP1A2 | SLCO1A2 | T3 > rT3, T4, T3S, rT3S, T4S | Unknown | Brain, gonad | SNPs associated with higher T3 or T4S concentration | [9,29,30] |
| OATP1B1 | SLCO1B1 | T3, T4 | Unknown | Liver | SNP associated with serum FT4 concentrations | [9,31] |
| OATP1B3 | SLCO1B3 | T3, T4 | Unknown | Liver | SNP associated with serum FT4 concentrations | [9,31] |
| OATP1C1 | SLCO1C1 | T4, T4S, rT3 | Unknown | Brain | OATP1C1 deficiency | [9,32,33] |
| OATP2B1 | SLCO2B1 | T4 | Unknown | Liver, brain, intestine, lung, placenta, spleen | Unknown | [9,29,30] |
| OATP3A1 | SLCO3A1 | T4 | Unknown | Brain, heart, skin, spleen | Unknown | [9,34,35] |
| OATP4A1 | SLCO4A1 | T3 > T4, rT3 | Unknown | Amnion, placenta | Unknown | [9,29] |
| OATP4C1 | SLCO4C1 | T3, T4 | Unknown | Kidney, liver | Unknown | [9,35,36] |
| ABCB1 | ABCB1 | Unknown | T3 | Heart, liver, placenta | SNP associated with serum FT4 concentrations | [9,37,38] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Z.; Meima, M.E.; Peeters, R.P.; Visser, W.E. Thyroid Hormone Transporters in Pregnancy and Fetal Development. Int. J. Mol. Sci. 2022, 23, 15113. https://doi.org/10.3390/ijms232315113
Chen Z, Meima ME, Peeters RP, Visser WE. Thyroid Hormone Transporters in Pregnancy and Fetal Development. International Journal of Molecular Sciences. 2022; 23(23):15113. https://doi.org/10.3390/ijms232315113
Chicago/Turabian StyleChen, Zhongli, Marcel E. Meima, Robin P. Peeters, and W. Edward Visser. 2022. "Thyroid Hormone Transporters in Pregnancy and Fetal Development" International Journal of Molecular Sciences 23, no. 23: 15113. https://doi.org/10.3390/ijms232315113
APA StyleChen, Z., Meima, M. E., Peeters, R. P., & Visser, W. E. (2022). Thyroid Hormone Transporters in Pregnancy and Fetal Development. International Journal of Molecular Sciences, 23(23), 15113. https://doi.org/10.3390/ijms232315113





