Kelulut Honey Regulates Sex Steroid Receptors in a Polycystic Ovary Syndrome Rat Model
Abstract
1. Introduction
2. Results
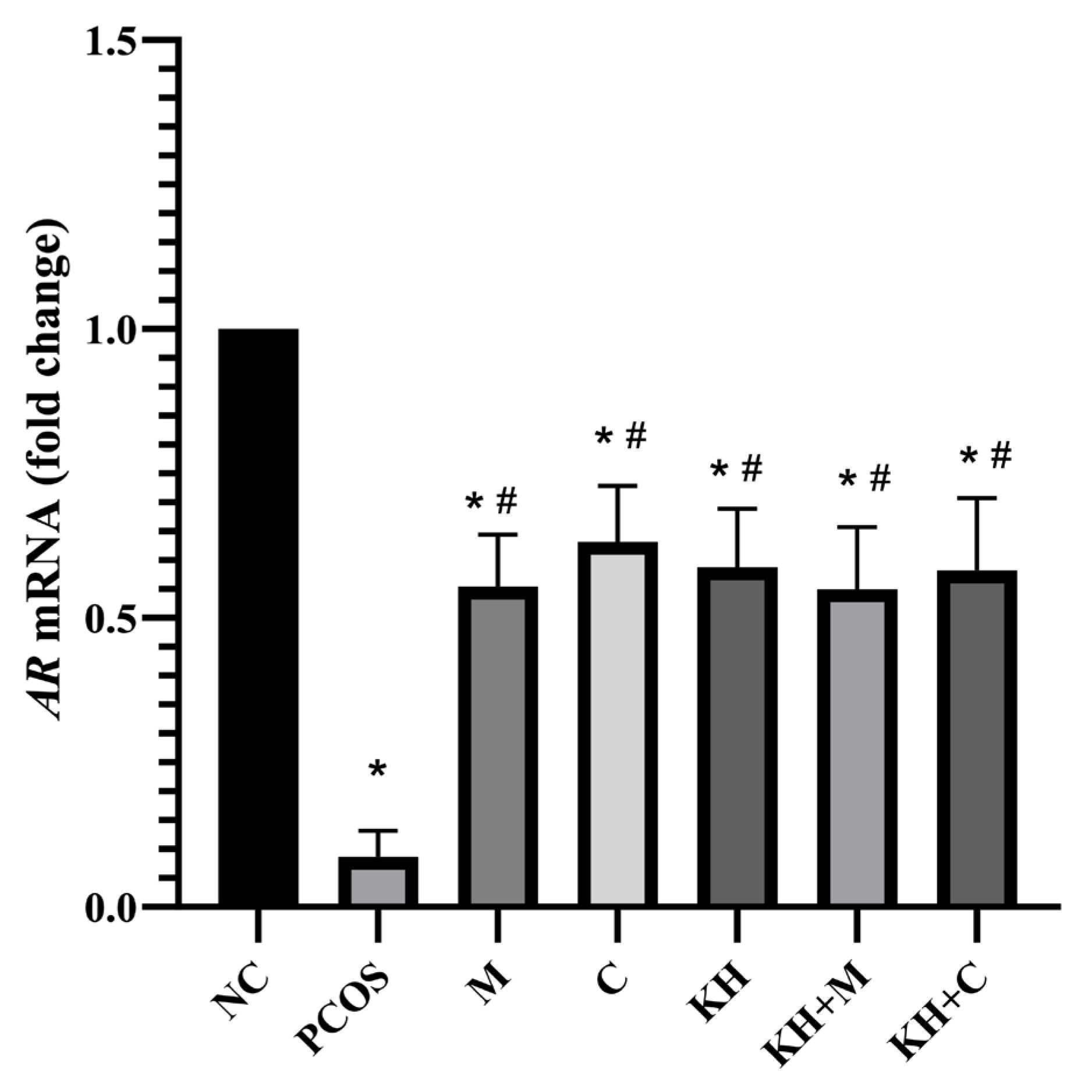
2.1. Effect of KH on AR mRNA Expression and Protein Distribution
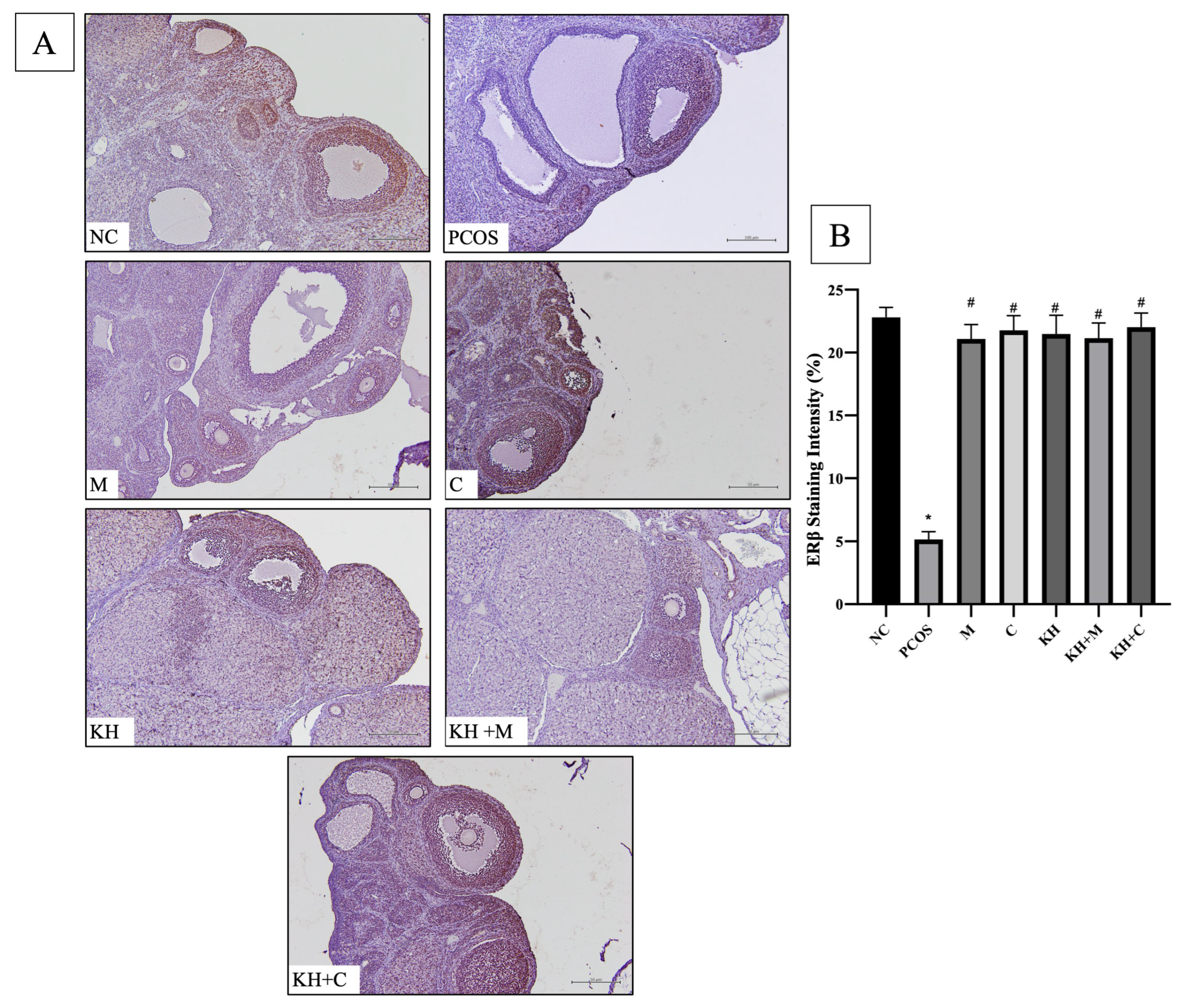
2.2. Effect of KH on ERα and ERβ mRNA Expression and Protein Distribution
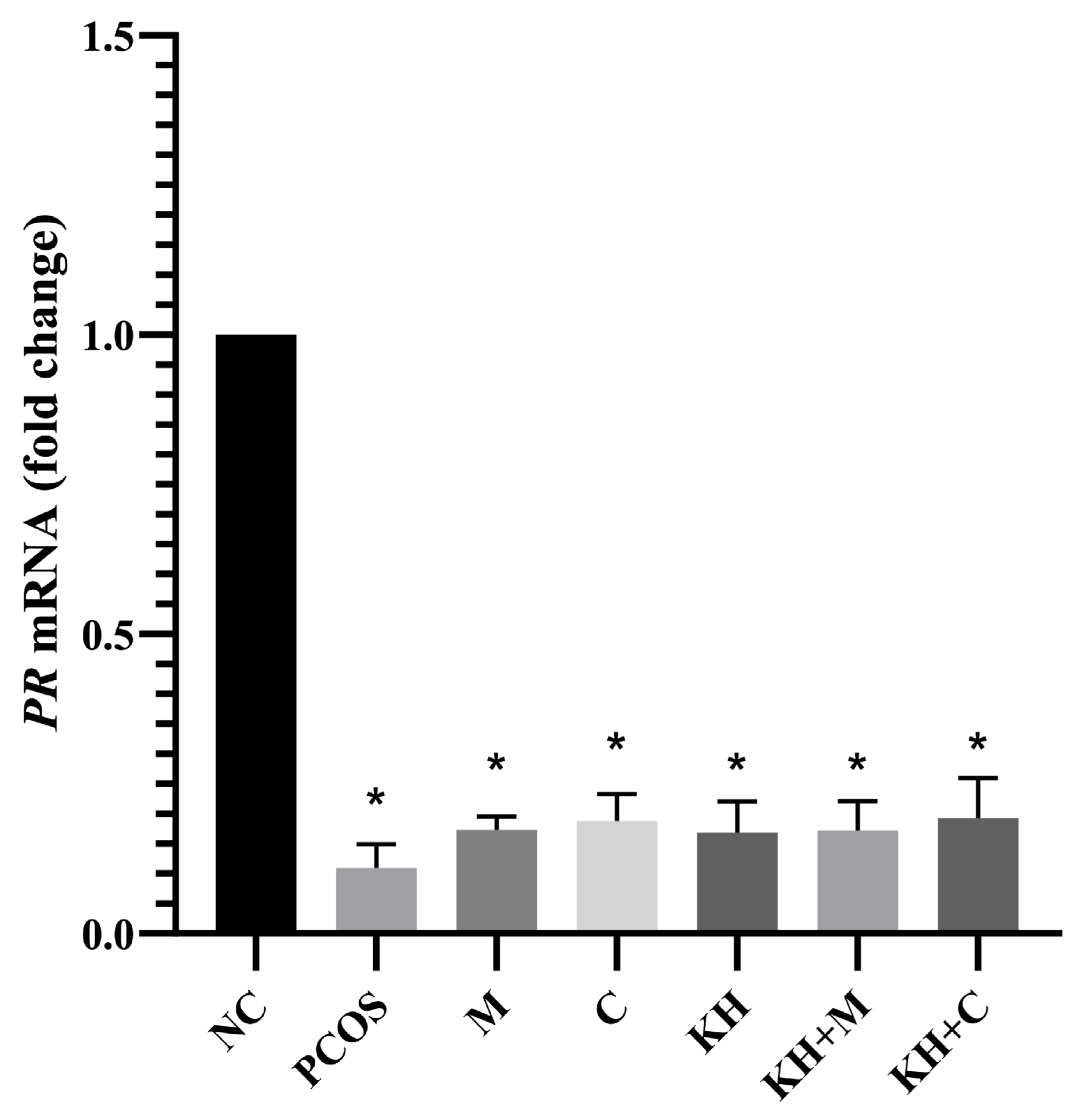
2.3. Effect of KH on PR mRNA Expression and Protein Distribution
3. Discussion
4. Materials and Methods
4.1. Honey Sample
4.2. Ethics and Animals Information
4.3. Study Design
4.4. Sex Steroid Receptor Distribution Analysis by Immunohistochemistry (IHC)
4.5. Sex Steroid Receptor Gene Expression Analysis by Real-Time PCR
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Swaroop, A.; Jaipuriar, A.S.; Gupta, S.K.; Bagchi, M.; Kumar, P.; Preuss, H.G.; Bagchi, D. Efficacy of a Novel Fenugreek Seed Extract (Trigonella foenum-graecum, Furocyst) in Polycystic Ovary Syndrome (PCOS). Int. J. Med. Sci. 2015, 12, 825–831. [Google Scholar] [CrossRef] [PubMed]
- Teede, H.; Deeks, A.; Moran, L. Polycystic ovary syndrome: A complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010, 8, 41. [Google Scholar] [CrossRef]
- Escobar-Morreale, H.F. Polycystic ovary syndrome: Definition, aetiology, diagnosis and treatment. Nat. Rev. Endocrinol. 2018, 14, 270. [Google Scholar] [CrossRef] [PubMed]
- Azziz, R.; Carmina, E.; Chen, Z.; Dunaif, A.; Laven, J.S.; Legro, R.S.; Lizneva, D.; Natterson-Horowtiz, B.; Teede, H.J.; Yildiz, B.O. Polycystic ovary syndrome. Nat. Rev. Dis. Prim. 2016, 2, 16057. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Singh, D.; Toppo, M.; Priya, A.; Sethia, S.; Gupta, P. A cross sectional study of polycystic ovarian syndrome among young women in Bhopal, Central India. Int. J. Community Med. Public Health 2018, 5, 95–100. [Google Scholar] [CrossRef]
- Sirmans, S.M.; Pate, K.A. Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clin. Epidemiol. 2014, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Dennett, C.C.; Simon, J. The role of polycystic ovary syndrome in reproductive and metabolic health: Overview and approaches for treatment. Diabetes Spectr. 2015, 28, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Kyrou, I.; Karteris, E.; Robbins, T.; Chatha, K.; Drenos, F.; Randeva, H.S. Polycystic ovary syndrome (PCOS) and COVID-19: An overlooked female patient population at potentially higher risk during the COVID-19 pandemic. BMC Med. 2020, 18, 220. [Google Scholar] [CrossRef] [PubMed]
- Rosenfield, R.L. Current concepts of polycystic ovary syndrome pathogenesis. Curr. Opin. Pediatr. 2020, 32, 698–706. [Google Scholar] [CrossRef]
- McCartney, C.R.; Marshall, J.C. Polycystic Ovary Syndrome. N. Engl. J. Med. 2016, 375, 54–64. [Google Scholar] [CrossRef]
- Franks, S.; Hardy, K. Androgen Action in the Ovary. Front. Endocrinol. 2018, 9, 452. [Google Scholar] [CrossRef]
- Magoffin, D.A.; Agarwal, S.K.; Jakimiuk, A.J. Suppression of Aromatase Activity in Polycystic Ovary Syndrome. In Polycystic Ovary Syndrome; Chang, R.J., Ed.; Springer New York: New York, NY, USA, 1996; pp. 208–222. [Google Scholar]
- Dumesic, D.A.; Oberfield, S.E.; Stener-Victorin, E.; Marshall, J.C.; Laven, J.S.; Legro, R.S. Scientific Statement on the Diagnostic Criteria, Epidemiology, Pathophysiology, and Molecular Genetics of Polycystic Ovary Syndrome. Endocr. Rev. 2015, 36, 487–525. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.-Y.; Liu, Y.; Lv, Y.; Huang, T.; Lu, G.; Liu, H.-B.; Zhao, S.-G. Role of Androgen Receptor for Reconsidering the “true” polycystic ovarian Morphology in pcoS. Sci. Rep. 2020, 10, 8993. [Google Scholar] [CrossRef]
- Lazúrová, I.; Lazúrová, Z.; Figurová, J.; Ujházi, S.; Dravecká, I.; Mašlanková, J.; Mareková, M. Relationship between steroid hormones and metabolic profile in women with polycystic ovary syndrome. Physiol. Res. 2019, 68, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.-L.; Deng, S.-L.; Lian, Z.-X.; Yu, K. Estrogen Receptors in Polycystic Ovary Syndrome. Cells 2021, 10, 459. [Google Scholar] [CrossRef] [PubMed]
- Abdul Hamid, F.; Abu, M.A.; Abdul Karim, A.K.; Ahmad, M.F.; Abd Aziz, N.H.; Mohd Kamal, D.A.; Mokhtar, M.H. Sex Steroid Receptors in Polycystic Ovary Syndrome and Endometriosis: Insights from Laboratory Studies to Clinical Trials. Biomedicines 2022, 10, 1705. [Google Scholar] [CrossRef] [PubMed]
- Malik Aubead, N. Role of Sex Hormones in Human Body; IntechOpen: London, UK, 2021. [Google Scholar] [CrossRef]
- Walters, K.A. Polycystic ovary syndrome: Is it androgen or estrogen receptor? Curr. Opin. Endocr. Metab. Res. 2020, 12, 1–7. [Google Scholar] [CrossRef]
- Domecq, J.P.; Prutsky, G.; Mullan, R.J.; Sundaresh, V.; Wang, A.T.; Erwin, P.J.; Welt, C.; Ehrmann, D.; Montori, V.M.; Murad, M.H. Adverse effects of the common treatments for polycystic ovary syndrome: A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2013, 98, 4646–4654. [Google Scholar] [CrossRef][Green Version]
- Sharpe, A.; Morley, L.C.; Tang, T.; Norman, R.J.; Balen, A.H. Metformin for ovulation induction (excluding gonadotrophins) in women with polycystic ovary syndrome. Cochrane Database Syst. Rev. 2019, 12, Cd013505. [Google Scholar] [CrossRef]
- Brown, J.; Farquhar, C.; Beck, J.; Boothroyd, C.; Hughes, E. Clomiphene and anti-oestrogens for ovulation induction in PCOS. Cochrane Database Syst. Rev. 2009, 4, Cd002249. [Google Scholar] [CrossRef]
- Arentz, S.; Smith, C.A.; Abbott, J.A.; Bensoussan, A. A survey of the use of complementary medicine by a self-selected community group of Australian women with polycystic ovary syndrome. BMC Complement. Altern. Med. 2014, 14, 472. [Google Scholar] [CrossRef] [PubMed]
- Budin, S.; Jubaidi, F.; Azam, S.; Mohammed Yusof, N.; Taib, I.S.; Mohamed, J. Kelulut honey supplementation prevents sperm and testicular oxidative damage in streptozotocin-induced diabetic rats. J. Teknol. 2017, 79, 89–95. [Google Scholar] [CrossRef]
- Kamal, D.A.M.; Ibrahim, S.F.; Ugusman, A.; Mokhtar, M.H. Effects of Kelulut Honey on Oestrus Cycle Regulation and Histomorphological Changes in Letrozole-Induced Polycystic Ovary Syndrome Rats: A Preliminary Study. Life 2022, 12, 890. [Google Scholar] [CrossRef]
- Mohd Kamal, D.A.; Ibrahim, S.F.; Kamal, H.; Kashim, M.I.A.M.; Mokhtar, M.H. Physicochemical and Medicinal Properties of Tualang, Gelam and Kelulut Honeys: A Comprehensive Review. Nutrients 2021, 13, 197. [Google Scholar] [CrossRef]
- Kamal, D.A.M.; Ibrahim, S.F.; Ugusman, A.; Zaid, S.S.M.; Mokhtar, M.H. Kelulut Honey Improves Folliculogenesis, Steroidogenic, and Aromatase Enzyme Profiles and Ovarian Histomorphology in Letrozole-Induced Polycystic Ovary Syndrome Rats. Nutrients 2022, 14, 4364. [Google Scholar] [CrossRef]
- Kamal, D.A.M.; Ibrahim, S.F.; Ugusman, A.; Mokhtar, M.H. Kelulut Honey Ameliorates Oestrus Cycle, Hormonal Profiles, and Oxidative Stress in Letrozole-Induced Polycystic Ovary Syndrome Rats. Antioxidants 2022, 11, 1879. [Google Scholar] [CrossRef]
- Rodriguez Paris, V.; Bertoldo, M.J. The Mechanism of Androgen Actions in PCOS Etiology. Med. Sci. 2019, 7, 89. [Google Scholar] [CrossRef]
- Ashraf, S.; Nabi, M.; Rasool, S.U.A.; Rashid, F.; Amin, S. Hyperandrogenism in polycystic ovarian syndrome and role of CYP gene variants: A review. Egypt. J. Med. Hum. Genet. 2019, 20, 25. [Google Scholar] [CrossRef]
- Yang, F.; Ruan, Y.-C.; Yang, Y.-J.; Wang, K.; Liang, S.-S.; Han, Y.-B.; Teng, X.-M.; Yang, J.-Z. Follicular hyperandrogenism downregulates aromatase in luteinized granulosa cells in polycystic ovary syndrome women. Reproduction 2015, 150, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, A.S.; Eid, S.; Kay, C.R.; Jimenez, M.; McMahon, A.C.; Desai, R.; Allan, C.M.; Smith, J.T.; Handelsman, D.J.; Walters, K.A. Haplosufficient genomic androgen receptor signaling is adequate to protect female mice from induction of polycystic ovary syndrome features by prenatal hyperandrogenization. Endocrinology 2015, 156, 1441–1452. [Google Scholar] [CrossRef] [PubMed]
- Owens, L.A.; Kristensen, S.G.; Lerner, A.; Christopoulos, G.; Lavery, S.; Hanyaloglu, A.C.; Hardy, K.; Yding Andersen, C.; Franks, S. Gene Expression in Granulosa Cells From Small Antral Follicles From Women With or Without Polycystic Ovaries. J. Clin. Endocrinol. Metab. 2019, 104, 6182–6192. [Google Scholar] [CrossRef]
- Zhang, H.; Yi, M.; Zhang, Y.; Jin, H.; Zhang, W.; Yang, J.; Yan, L.; Li, R.; Zhao, Y.; Qiao, J. High-fat diets exaggerate endocrine and metabolic phenotypes in a rat model of DHEA-induced PCOS. Reproduction 2016, 151, 431–441. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Li, J.; An, Y.; Zhang, S. Effects of androgen on immunohistochemical localization of androgen receptor and Connexin 43 in mouse ovary. Tissue Cell 2015, 47, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Lee, S.Y.; Lee, S.R.; Pyun, B.-J.; Kim, H.J.; Lee, Y.H.; Kwon, S.W.; Suh, D.H.; Lee, C.H.; Hong, E.-J.; et al. Therapeutic Effect of Ecklonia cava Extract in Letrozole-Induced Polycystic Ovary Syndrome Rats. Front. Pharmacol. 2018, 9, 1325. [Google Scholar] [CrossRef] [PubMed]
- Banihani, S.A. Mechanisms of honey on testosterone levels. Heliyon 2019, 5, e02029. [Google Scholar] [CrossRef] [PubMed]
- Ranneh, Y.; Akim, A.M.; Hamid, H.A.; Khazaai, H.; Fadel, A.; Mahmoud, A.M. Stingless bee honey protects against lipopolysaccharide induced-chronic subclinical systemic inflammation and oxidative stress by modulating Nrf2, NF-κB and p38 MAPK. Nutr. Metab. 2019, 16, 15. [Google Scholar] [CrossRef]
- Saiful Yazan, L.; Muhamad Zali, M.F.S.; Mohd Ali, R.; Zainal, N.A.; Esa, N.; Sapuan, S.; Ong, Y.S.; Tor, Y.S.; Gopalsamy, B.; Voon, F.L.; et al. Chemopreventive Properties and Toxicity of Kelulut Honey in Sprague Dawley Rats Induced with Azoxymethane. BioMed Res. Int. 2016, 2016, 4036926. [Google Scholar] [CrossRef]
- Kuo, Y.-Y.; Huo, C.; Lin, C.-Y.; Lin, H.-P.; Liu, J.-S.; Wang, W.-C.; Chang, C.-R.; Chuu, C.-P. Caffeic acid phenethyl ester suppresses androgen receptor signaling and stability via inhibition of phosphorylation on Ser81 and Ser213. Cell Commun. Signal. 2019, 17, 100. [Google Scholar] [CrossRef]
- Karim, N. Antioxidant Properties of Stingless Bee Honey and Its Effect on the Viability of Lymphoblastoid Cell Line. Med. Health 2019, 14, 91–105. [Google Scholar] [CrossRef]
- Haron, H.; Talib, R.A.; Subramaniam, P.; Arifen, Z.N.Z.; Ibrahim, M. A Comparison Of Chemical Compositions In Kelulut Honey From Different Regions. Malays. J. Anal. Sci. 2022, 26, 447–456. [Google Scholar]
- Senevirathne, M.; Kim, S.-H.; Siriwardhana, N.; Ha, J.-H.; Lee, K.-W.; Jeon, Y.-J. Antioxidant Potential of Ecklonia cavaon Reactive Oxygen Species Scavenging, Metal Chelating, Reducing Power and Lipid Peroxidation Inhibition. Food Sci. Technol. Int. 2006, 12, 27–38. [Google Scholar] [CrossRef]
- Velazquez, E.M.; Mendoza, S.; Hamer, T.; Sosa, F.; Glueck, C.J. Metformin therapy in polycystic ovary syndrome reduces hyperinsulinemia, insulin resistance, hyperandrogenemia, and systolic blood pressure, while facilitating normal menses and pregnancy. Metabolism 1994, 43, 647–654. [Google Scholar] [CrossRef]
- Ohara, M.; Yoshida-Komiya, H.; Ono-Okutsu, M.; Yamaguchi-Ito, A.; Takahashi, T.; Fujimori, K. Metformin reduces androgen receptor and upregulates homeobox A10 expression in uterine endometrium in women with polycystic ovary syndrome. Reprod. Biol. Endocrinol. 2021, 19, 77. [Google Scholar] [CrossRef]
- Wahab, O.A.; Princely, A.C.; Oluwadamilare, A.A.; Ore-Oluwapo, D.O.; Blessing, A.O.; Alfred, E.F. Clomiphene citrate ameliorated lead acetate-induced reproductive toxicity in male Wistar rats. JBRA Assist. Reprod. 2019, 23, 336–343. [Google Scholar] [CrossRef]
- Barton, M.; Filardo, E.J.; Lolait, S.J.; Thomas, P.; Maggiolini, M.; Prossnitz, E.R. Twenty years of the G protein-coupled estrogen receptor GPER: Historical and personal perspectives. J. Steroid Biochem. Mol. Biol. 2018, 176, 4–15. [Google Scholar] [CrossRef]
- Fuentes, N.; Silveyra, P. Estrogen receptor signaling mechanisms. Adv. Protein Chem. Struct. Biol. 2019, 116, 135–170. [Google Scholar] [PubMed]
- Lee, S.; Kang, D.W.; Hudgins-Spivey, S.; Krust, A.; Lee, E.Y.; Koo, Y.; Cheon, Y.; Gye, M.C.; Chambon, P.; Ko, C. Theca-specific estrogen receptor-alpha knockout mice lose fertility prematurely. Endocrinology 2009, 150, 3855–3862. [Google Scholar] [CrossRef] [PubMed]
- Couse, J.F.; Yates, M.M.; Sanford, R.; Nyska, A.; Nilson, J.H.; Korach, K.S. Formation of Cystic Ovarian Follicles Associated with Elevated Luteinizing Hormone Requires Estrogen Receptor-β. Endocrinology 2004, 145, 4693–4702. [Google Scholar] [CrossRef] [PubMed]
- Jakimiuk, A.J.; Weitsman, S.R.; Yen, H.-W.; Bogusiewicz, M.; Magoffin, D.A. Estrogen Receptor α and β Expression in Theca and Granulosa Cells from Women with Polycystic Ovary Syndrome. J. Clin. Endocrinol. Metab. 2002, 87, 5532–5538. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Yang, H.; Lee, S.R.; Kwon, S.W.; Hong, E.J.; Lee, H.W. Welsh Onion Root (Allium fistulosum) Restores Ovarian Functions from Letrozole Induced-Polycystic Ovary Syndrome. Nutrients 2018, 10, 1430. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, K.J.; Arao, Y.; Korach, K.S. Estrogen hormone physiology: Reproductive findings from estrogen receptor mutant mice. Reprod. Biol. 2014, 14, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Schomberg, D.W.; Couse, J.F.; Mukherjee, A.; Lubahn, D.B.; Sar, M.; Mayo, K.E.; Korach, K.S. Targeted disruption of the estrogen receptor-alpha gene in female mice: Characterization of ovarian responses and phenotype in the adult. Endocrinology 1999, 140, 2733–2744. [Google Scholar] [CrossRef] [PubMed]
- Couse, J.F.; Yates, M.M.; Deroo, B.J.; Korach, K.S. Estrogen receptor-beta is critical to granulosa cell differentiation and the ovulatory response to gonadotropins. Endocrinology 2005, 146, 3247–3262. [Google Scholar] [CrossRef]
- Hewitt, S.C.; Winuthayanon, W.; Korach, K.S. What’s new in estrogen receptor action in the female reproductive tract. J. Mol. Endocrinol. 2016, 56, R55–R71. [Google Scholar] [CrossRef]
- Tang, Z.R.; Zhang, R.; Lian, Z.X.; Deng, S.L.; Yu, K. Estrogen-Receptor Expression and Function in Female Reproductive Disease. Cells 2019, 8, 1123. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Othman, N.H. Honey as a potential natural anticancer agent: A review of its mechanisms. Evid.-Based Complement. Altern. Med. 2013, 2013, 829070. [Google Scholar] [CrossRef]
- Ahmed, S.; Sulaiman, S.A.; Othman, N.H. Oral Administration of Tualang and Manuka Honeys Modulates Breast Cancer Progression in Sprague-Dawley Rats Model. Evid.-Based Complement. Altern. Med. 2017, 2017, 5904361. [Google Scholar] [CrossRef]
- Cipolletti, M.; Solar Fernandez, V.; Montalesi, E.; Marino, M.; Fiocchetti, M. Beyond the Antioxidant Activity of Dietary Polyphenols in Cancer: The Modulation of Estrogen Receptors (ERs) Signaling. Int. J. Mol. Sci. 2018, 19, 2624. [Google Scholar] [CrossRef]
- Gehm, B.D.; McAndrews, J.M.; Chien, P.Y.; Jameson, J.L. Resveratrol, a polyphenolic compound found in grapes and wine, is an agonist for the estrogen receptor. Proc. Natl. Acad. Sci. USA 1997, 94, 14138–14143. [Google Scholar] [CrossRef]
- Erejuwa, O.O.; Sulaiman, S.A.; Wahab, M.S.A. Effects of Honey and Its Mechanisms of Action on the Development and Progression of Cancer. Molecules 2014, 19, 2497–2522. [Google Scholar] [CrossRef]
- Tsiapara, A.V.; Jaakkola, M.; Chinou, I.; Graikou, K.; Tolonen, T.; Virtanen, V.; Moutsatsou, P. Bioactivity of Greek honey extracts on breast cancer (MCF-7), prostate cancer (PC-3) and endometrial cancer (Ishikawa) cells: Profile analysis of extracts. Food Chem. 2009, 116, 702–708. [Google Scholar] [CrossRef]
- Ismail, N.H.; Osman, K.; Zulkefli, A.F.; Mokhtar, M.H.; Ibrahim, S.F. The Physicochemical Characteristics of Gelam Honey and Its Outcome on the Female Reproductive Tissue of Sprague-Dawley Rats: A Preliminary Study. Molecules 2021, 26, 3346. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Othman, N.H. The anti-cancer effects of Tualang honey in modulating breast carcinogenesis: An experimental animal study. BMC Complement. Altern. Med. 2017, 17, 208. [Google Scholar] [CrossRef] [PubMed]
- Kurosawa, T.; Hiroi, H.; Momoeda, M.; Inoue, S.; Taketani, Y. Clomiphene citrate elicits estrogen agonistic/antagonistic effects differentially via estrogen receptors alpha and beta. Endocr. J. 2010, 57, 517–521. [Google Scholar] [CrossRef] [PubMed]
- Haskell, S.G. Selective estrogen receptor modulators. South Med. J. 2003, 96, 469–476. [Google Scholar] [CrossRef]
- Triantafyllidou, O.; Sigalos, G.; Gkoles, L.; Kastora, S.; Vakas, P.; Batsiou, E.; Vlahos, N. The addition of clomiphene citrate to ovarian stimulation protocols for poor responders. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 251, 136–140. [Google Scholar] [CrossRef]
- Dickey, R.P.; Holtkamp, D.E. Development, pharmacology and clinical experience with clomiphene citrate. Hum. Reprod. Update 1996, 2, 483–506. [Google Scholar] [CrossRef]
- Penzias, A.; Bendikson, K.; Butts, S.; Coutifaris, C.; Falcone, T.; Fossum, G.; Gitlin, S.; Gracia, C.; Hansen, K.; La Barbera, A.; et al. Role of metformin for ovulation induction in infertile patients with polycystic ovary syndrome (PCOS): A guideline. Fertil. Steril. 2017, 108, 426–441. [Google Scholar] [CrossRef]
- Di Pietro, M.; Parborell, F.; Irusta, G.; Pascuali, N.; Bas, D.; Bianchi, M.S.; Tesone, M.; Abramovich, D. Metformin Regulates Ovarian Angiogenesis and Follicular Development in a Female Polycystic Ovary Syndrome Rat Model. Endocrinology 2015, 156, 1453–1463. [Google Scholar] [CrossRef]
- Zhang, J.; Xu, H.; Zhou, X.; Li, Y.; Liu, T.; Yin, X.; Zhang, B. Role of metformin in inhibiting estrogen-induced proliferation and regulating ERα and ERβ expression in human endometrial cancer cells. Oncol. Lett. 2017, 14, 4949–4956. [Google Scholar] [CrossRef]
- Sar, M.; Welsch, F. Differential expression of estrogen receptor-beta and estrogen receptor-alpha in the rat ovary. Endocrinology 1999, 140, 963–971. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Kriatchko, A.; Roy, S.K. Expression of ER-α and ER-β in the Hamster Ovary: Differential Regulation by Gonadotropins and Ovarian Steroid Hormones. Endocrinology 2002, 143, 2385–2398. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cope, D.I.; Monsivais, D. Progesterone Receptor Signaling in the Uterus Is Essential for Pregnancy Success. Cells 2022, 11, 1474. [Google Scholar] [CrossRef] [PubMed]
- Lydon, J.P.; DeMayo, F.J.; Funk, C.R.; Mani, S.K.; Hughes, A.R.; Montgomery, C.A., Jr.; Shyamala, G.; Conneely, O.M.; O’Malley, B.W. Mice lacking progesterone receptor exhibit pleiotropic reproductive abnormalities. Genes Dev. 1995, 9, 2266–2278. [Google Scholar] [CrossRef] [PubMed]
- Artimani, T.; Saidijam, M.; Aflatoonian, R.; Amiri, I.; Ashrafi, M.; Shabab, N.; Mohammadpour, N.; Mehdizadeh, M. Estrogen and progesterone receptor subtype expression in granulosa cells from women with polycystic ovary syndrome. Gynecol. Endocrinol. 2015, 31, 379–383. [Google Scholar] [CrossRef]
- Meenakumari, K.J.; Agarwal, S.; Krishna, A.; Pandey, L.K. Effects of metformin treatment on luteal phase progesterone concentration in polycystic ovary syndrome. Braz. J. Med. Biol. Res. 2004, 37, 1637–1644. [Google Scholar] [CrossRef]
- Ndeingang, E.C.; Defo Deeh, P.B.; Watcho, P.; Kamanyi, A. Phyllanthus muellerianus (Euphorbiaceae) Restores Ovarian Functions in Letrozole-Induced Polycystic Ovarian Syndrome in Rats. Evid.-Based Complement. Altern. Med. 2019, 2019, 2965821. [Google Scholar] [CrossRef]
- Atashpour, S.; Kargar Jahromi, H.; Kargar Jahromi, Z.; Maleknasab, M. Comparison of the effects of Ginger extract with clomiphene citrate on sex hormones in rats with polycystic ovarian syndrome. Int. J. Reprod. Biomed. 2017, 15, 561–568. [Google Scholar] [CrossRef]
- Ismail, N.H.; Ibrahim, S.F.; Jaffar, F.H.F.; Mokhtar, M.H.; Chin, K.Y.; Osman, K. Augmentation of the Female Reproductive System Using Honey: A Mini Systematic Review. Molecules 2021, 26, 649. [Google Scholar] [CrossRef]
- Zaid, S.S.; Sulaiman, S.A.; Sirajudeen, K.N.; Othman, N.H. The effects of Tualang honey on female reproductive organs, tibia bone and hormonal profile in ovariectomised rats—Animal model for menopause. BMC Complement. Altern. Med. 2010, 10, 82. [Google Scholar] [CrossRef]
- Gava, N.; Clarke, C.L.; Byth, K.; Arnett-Mansfield, R.L.; deFazio, A. Expression of Progesterone Receptors A and B in the Mouse Ovary during the Estrous Cycle. Endocrinology 2004, 145, 3487–3494. [Google Scholar] [CrossRef] [PubMed]
- Telleria, C.M.; Stocco, C.O.; Stati, A.O.; Deis, R.P. Progesterone receptor is not required for progesterone action in the rat corpus luteum of pregnancy. Steroids 1999, 64, 760–766. [Google Scholar] [CrossRef]
- Natraj, U.; Richards, J.S. Hormonal regulation, localization, and functional activity of the progesterone receptor in granulosa cells of rat preovulatory follicles. Endocrinology 1993, 133, 761–769. [Google Scholar] [CrossRef] [PubMed]
- Park-Sarge, O.K.; Parmer, T.G.; Gu, Y.; Gibori, G. Does the rat corpus luteum express the progesterone receptor gene? Endocrinology 1995, 136, 1537–1543. [Google Scholar] [CrossRef] [PubMed]
- Shao, R.; Markström, E.; Friberg, P.A.; Johansson, M.; Billig, H. Expression of progesterone receptor (PR) A and B isoforms in mouse granulosa cells: Stage-dependent PR-mediated regulation of apoptosis and cell proliferation. Biol. Reprod. 2003, 68, 914–921. [Google Scholar] [CrossRef]
- Kafali, H.; Iriadam, M.; Ozardali, I.; Demir, N. Letrozole-induced polycystic ovaries in the rat: A new model for cystic ovarian disease. Arch. Med. Res. 2004, 35, 103–108. [Google Scholar] [CrossRef]
- Morgante, G.; Massaro, M.G.; Di Sabatino, A.; Cappelli, V.; De Leo, V. Therapeutic approach for metabolic disorders and infertility in women with PCOS. Gynecol. Endocrinol. 2018, 34, 4–9. [Google Scholar] [CrossRef]
- Kamal, D.A.M.; Ibrahim, S.F.; Mokhtar, M.H. Effects of Testosterone on the Expression of Connexin 26 and Connexin 43 in the Uterus of Rats During Early Pregnancy. In Vivo 2020, 34, 1863–1870. [Google Scholar] [CrossRef] [PubMed]
- Crowe, A.R.; Yue, W. Semi-quantitative Determination of Protein Expression using Immunohistochemistry Staining and Analysis: An Integrated Protocol. Bio-Protocol 2019, 9, e3465. [Google Scholar] [CrossRef]





| Target Genes | Forward (F) and Reverse (R) Primer Sequence |
|---|---|
| AR | F CCTTGTTCCCTTTTCAGATG R GTAAAAGAGGCAGAGAAGAAG |
| ESR1 | F ATATGATCAACTGGGCAAAG R CATTTACCTTGATTCCTGTCC |
| ESR2 | F GGAAATCTTTGACATGCTCC R GGTACATACTGGAGTTGAGG |
| PGR | F TCTAATCCTGAATGAGCAGAG R GACTTTCATACAGAGGAACTC |
| GAPDH | F CTCAATGGGAACTTAACAGG R CTCTGTATAAGCAAGGATGC |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamal, D.A.M.; Ibrahim, S.F.; Ugusman, A.; Mokhtar, M.H. Kelulut Honey Regulates Sex Steroid Receptors in a Polycystic Ovary Syndrome Rat Model. Int. J. Mol. Sci. 2022, 23, 14757. https://doi.org/10.3390/ijms232314757
Kamal DAM, Ibrahim SF, Ugusman A, Mokhtar MH. Kelulut Honey Regulates Sex Steroid Receptors in a Polycystic Ovary Syndrome Rat Model. International Journal of Molecular Sciences. 2022; 23(23):14757. https://doi.org/10.3390/ijms232314757
Chicago/Turabian StyleKamal, Datu Agasi Mohd, Siti Fatimah Ibrahim, Azizah Ugusman, and Mohd Helmy Mokhtar. 2022. "Kelulut Honey Regulates Sex Steroid Receptors in a Polycystic Ovary Syndrome Rat Model" International Journal of Molecular Sciences 23, no. 23: 14757. https://doi.org/10.3390/ijms232314757
APA StyleKamal, D. A. M., Ibrahim, S. F., Ugusman, A., & Mokhtar, M. H. (2022). Kelulut Honey Regulates Sex Steroid Receptors in a Polycystic Ovary Syndrome Rat Model. International Journal of Molecular Sciences, 23(23), 14757. https://doi.org/10.3390/ijms232314757






