Different Types of Chronic Inflammation Engender Distinctive Immunosenescent Profiles in Affected Patients
Abstract
1. Introduction
2. Results
2.1. Characteristics of Patients’ Population
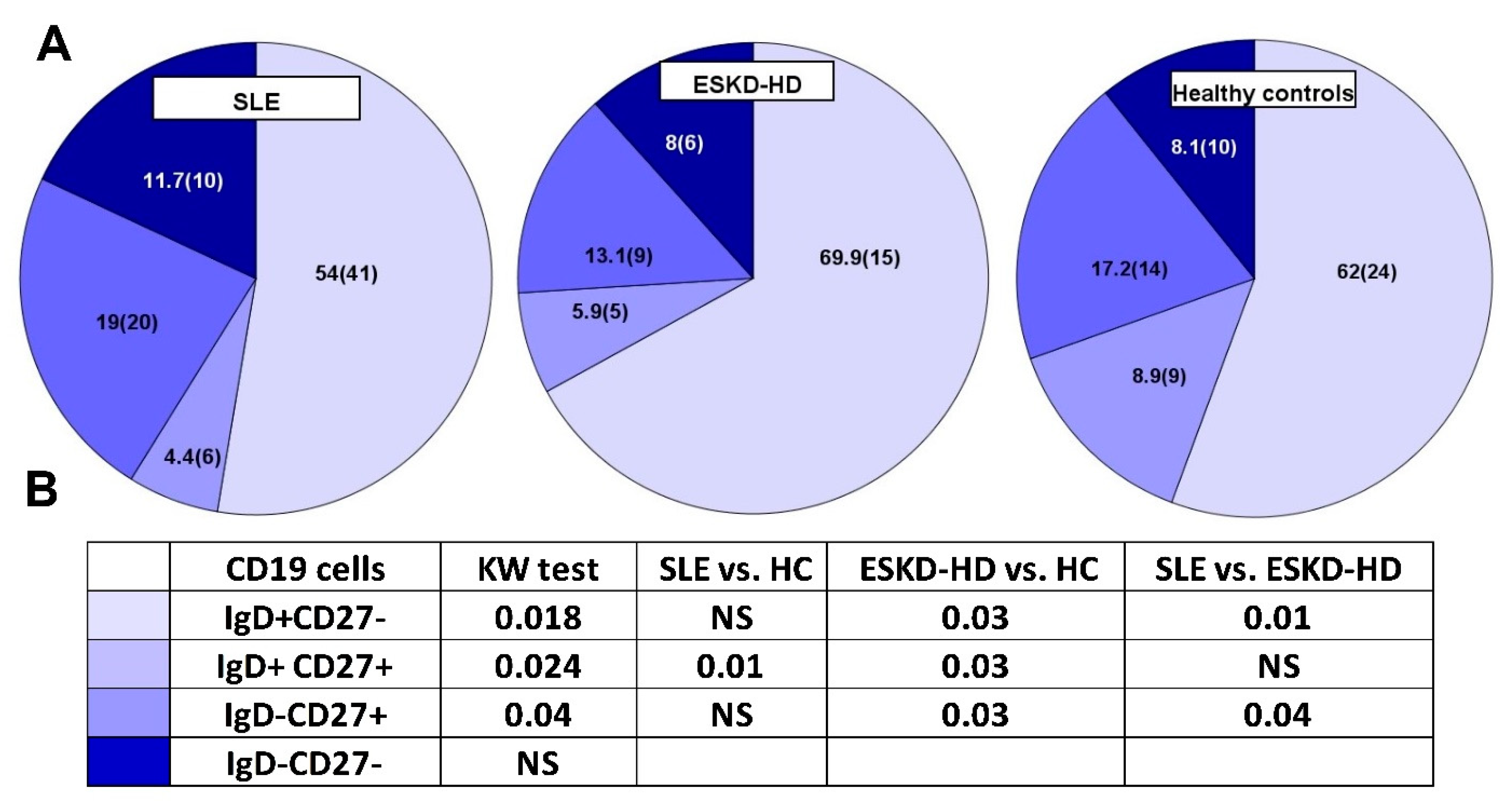
2.2. Phenotypic Analysis of B Lymphocytes in SLE, ESKD-HD Patients and HC
2.3. Phenotypic Analysis of T Lymphocytes in SLE, ESKD-HD Patients and HC
2.3.1. CD4 Lymphocytes
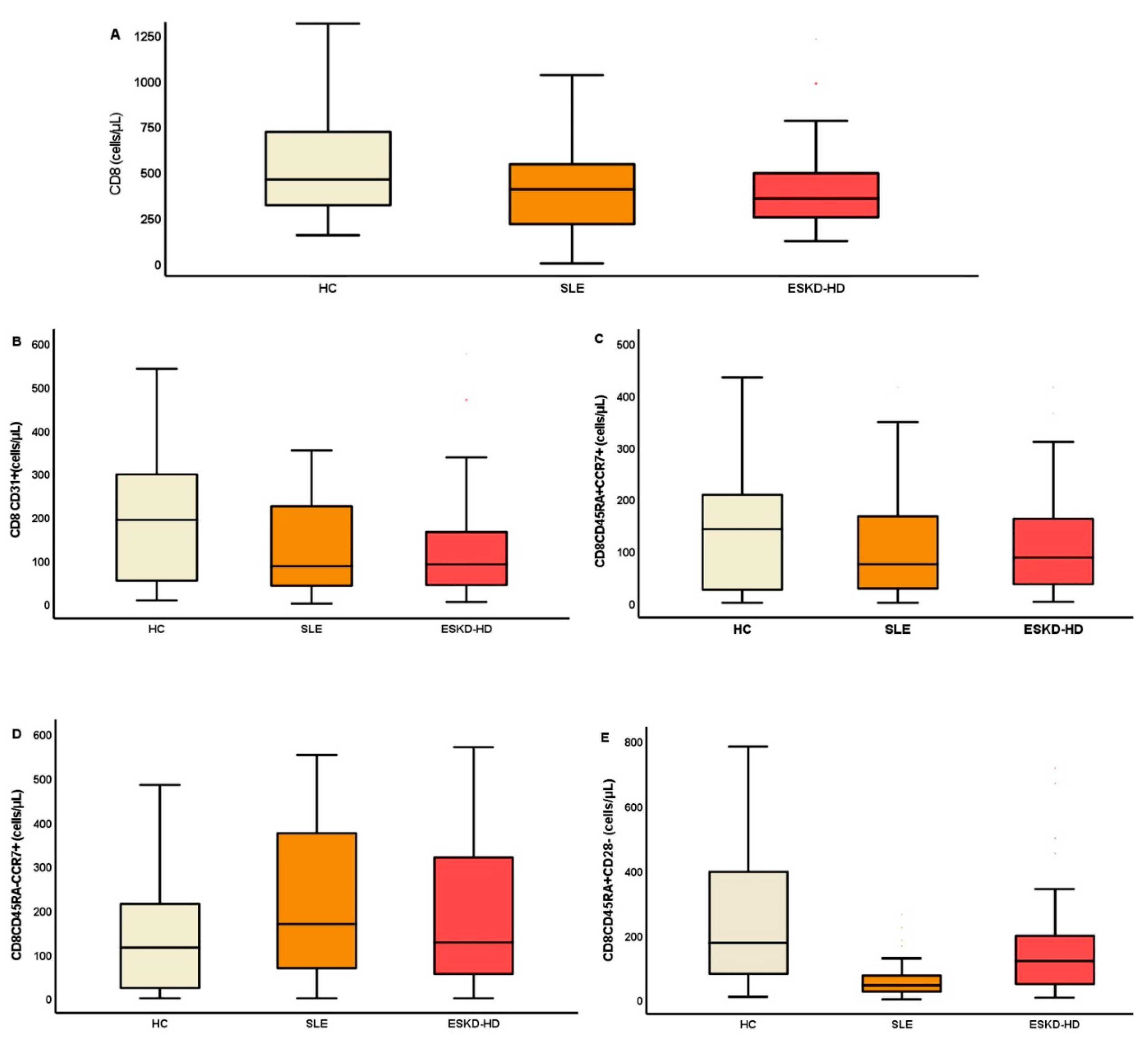
2.3.2. CD8 Lymphocytes
2.4. Adjustment of Lymphocyte Subpopulations for Age and Gender
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Schedule of the Study
4.3. Flow Cytometry
4.3.1. Flow Cytometry Reagents
4.3.2. Lymphocyte Subpopulations
4.4. Statistics
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lioulios, G.; Fylaktou, A.; Papagianni, A.; Stangou, M. T cell markers recount the course of immunosenescence in healthy individuals and chronic kidney disease. Clin. Immunol. 2021, 225, 108685. [Google Scholar] [CrossRef] [PubMed]
- Goronzy, J.J.; Weyand, C.M. Mechanisms underlying T cell ageing. Nat. Rev. Immunol. 2019, 19, 573–583. [Google Scholar] [CrossRef] [PubMed]
- Gruver, A.L.; Hudson, L.L.; Sempowski, G.D. Immunosenescence of ageing. J. Pathol. 2007, 211, 144–156. [Google Scholar] [CrossRef] [PubMed]
- Weyand, C.M.; Goronzy, J.J. Aging of the immune system: Mechanisms and therapeutic targets. Ann. Am. Thorac. Soc. 2016, 13 (Suppl. S5), S422–S428. [Google Scholar] [CrossRef]
- Xu, W.; Larbi, A. Markers of T Cell Senescence in Humans. Int. J. Mol. Sci. 2017, 18, 1742. [Google Scholar] [CrossRef]
- Pieren, D.K.J.; Smits, N.A.M.; Postel, R.J.; Kandiah, V.; de Wit, J.; van Beek, J.; van Baarle, D.; Guichelaar, T. Co-Expression of TIGIT and Helios Marks Immunosenescent CD8 + T Cells During Aging. Front. Immunol. 2022, 13, 833531. [Google Scholar] [CrossRef]
- Fulop, T.; McElhaney, J.; Pawelec, G.; Cohen, A.A.; Morais, J.A.; Dupuis, G.; Baehl, S.; Camous, X.; Witkowski, J.M.; Larbi, A. Frailty, Inflammation and Immunosenescence. Frailty Aging 2015, 41, 26–40. [Google Scholar]
- Bektas, A.; Schurman, S.H.; Sen, R.; Ferrucci, L. Human T cell immunosenescence and inflammation in aging. J. Leukoc. Biol. 2017, 102, 977–988. [Google Scholar] [CrossRef]
- Mathew, R.; Mason, D.; Kennedy, J.S. Vaccination issues in patients with chronic kidney disease. Expert Rev. Vaccines 2014, 13, 285–298. [Google Scholar] [CrossRef]
- Kato, S.; Chmielewski, M.; Honda, H.; Pecoits-Filho, R.; Matsuo, S.; Yuzawa, Y.; Tranaeus, A.; Stenvinkel, P.; Lindholm, B. Aspects of immune dysfunction in end-stage renal disease. Clin. J. Am. Soc. Nephrol. 2008, 3, 1526–1533. [Google Scholar] [CrossRef]
- Sampani, E.; Stangou, M.; Daikidou, D.V.; Nikolaidou, V.; Asouchidou, D.; Dimitriadis, C.; Lioulios, G.; Xochelli, A.; Fylaktou, A.; Papagianni, A. Influence of end stage renal disease on CD28 expression and T-cell immunity. Nephrology 2021, 26, 185–196. [Google Scholar] [CrossRef] [PubMed]
- Lioulios, G.; Fylaktou, A.; Xochelli, A.; Sampani, E.; Tsouchnikas, I.; Giamalis, P.; Daikidou, D.-V.; Nikolaidou, V.; Papagianni, A.; Theodorou, I.; et al. Clustering of End Stage Renal Disease Patients by Dimensionality Reduction Algorithms According to Lymphocyte Senescence Markers. Front. Immunol. 2022, 13, 841031. [Google Scholar] [CrossRef] [PubMed]
- Sampani, E.; Daikidou, D.V.; Lioulios, G.; Xochelli, A.; Mitsoglou, Z.; Nikolaidou, V.; Dimitriadis, C.; Fylaktou, A.; Papagianni, A.; Stangou, M. CD28null and Regulatory T Cells Are Substantially Disrupted in Patients with End-Stage Renal Disease Due to Diabetes Mellitus. Int. J. Mol. Sci. 2021, 22, 2975. [Google Scholar] [CrossRef]
- Rodríguez, Y.; Novelli, L.; Rojas, M.; De Santis, M.; Acosta-Ampudia, Y.; Monsalve, D.M.; Ramírez-Santana, C.; Costanzo, A.; Ridgway, W.M.; Ansari, A.A.; et al. Autoinflammatory and autoimmune conditions at the crossroad of COVID-19. J. Autoimmun. 2020, 114, 102506. [Google Scholar] [CrossRef] [PubMed]
- Caso, F.; Costa, L.; Nucera, V.; Barilaro, G.; Masala, I.F.; Talotta, R.; Caso, P.; Scarpa, R.; Sarzi-Puttini, P.; Atzeni, F. From autoinflammation to autoimmunity: Old and recent findings. Clin. Rheumatol. 2018, 37, 2305–2321. [Google Scholar] [CrossRef]
- Doria, A.; Zen, M.; Bettio, S.; Gatto, M.; Bassi, N.; Nalotto, L.; Ghirardello, A.; Iaccarino, L.; Punzi, L. Autoinflammation and autoimmunity: Bridging the divide. Autoimmun. Rev. 2012, 12, 22–30. [Google Scholar] [CrossRef]
- Kalim, H.; Wahono, C.S.; Permana, B.P.O.; Pratama, M.Z.; Handono, K. Association between senescence of T cells and disease activity in patients with systemic lupus erythematosus. Reumatologia 2021, 59, 292–301. [Google Scholar] [CrossRef]
- Tsai, C.Y.; Shen, C.Y.; Liao, H.T.; Li, K.J.; Lee, H.T.; Lu, C.S.; Wu, C.-H.; Kuo, Y.-M.; Hsieh, S.-C.; Yu, C.-L. Molecular and Cellular Bases of Immunosenescence, Inflammation, and Cardiovascular Complications Mimicking “Inflammaging” in Patients with Systemic Lupus Erythematosus. Int. J. Mol. Sci. 2019, 20, 3878. [Google Scholar] [CrossRef]
- Lopez, P.; Rodriguez-Carrio, J.; Martinez-Zapico, A.; Caminal-Montero, L.; Suarez, A. Senescent profile of angiogenic T cells from systemic lupus erythematosus patients. J. Leukoc. Biol. 2016, 99, 405–412. [Google Scholar] [CrossRef]
- Cheigh, J.S.; Kim, H.; Stenzel, K.H.; Tapia, L.; Sullivan, J.F.; Stubenbord, W.; Riggio, R.R.; Rubin, A.L. Systemic lupus erythematosus in patients with end-stage renal disease: Long-term follow-up on the prognosis of patients and the evolution of lupus activity. Am. J. Kidney Dis. 1990, 16, 189–195. [Google Scholar] [CrossRef]
- Sanz, I.; Wei, C.; Lee, F.E.-H.; Anolik, J. Phenotypic and functional heterogeneity of human memory B cells. Semin. Immunol. 2008, 20, 67–82. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Bayona, B.; Ramos-Amaya, A.; Pérez-Venegas, J.J.; Rodríguez, C.; Brieva, J.A. Decreased frequency and activated phenotype of blood CD27 IgD IgM B lymphocytes is a permanent abnormality in systemic lupus erythematosus patients. Arthritis Res. Ther. 2010, 12, R108. [Google Scholar] [CrossRef]
- Odendahl, M.; Jacobi, A.; Hansen, A.; Feist, E.; Hiepe, F.; Burmester, G.R.; Lipsky, P.E.; Radbruch, A.; Dörner, T. Disturbed peripheral B lymphocyte homeostasis in systemic lupus erythematosus. J. Immunol. 2000, 165, 5970–5979. [Google Scholar] [CrossRef] [PubMed]
- Dörner, T.; Jacobi, A.M.; Lee, J.; Lipsky, P.E. Abnormalities of B cell subsets in patients with systemic lupus erythematosus. J. Immunol. Methods 2011, 363, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Dörner, T.; Jacobi, A.M.; Lipsky, P.E. B cells in autoimmunity. Arthritis Res. Ther. 2009, 11, 247. [Google Scholar] [CrossRef]
- Pahl, M.v.; Gollapudi, S.; Sepassi, L.; Gollapudi, P.; Elahimehr, R.; Vaziri, N.D. Effect of end-stage renal disease on B-lymphocyte subpopulations, IL-7, BAFF and BAFF receptor expression. Nephrol. Dial. Transplant. 2010, 25, 205–212. [Google Scholar] [CrossRef]
- Kim, K.W.; Chung, B.H.; Jeon, E.J.; Kim, B.M.; Choi, B.S.; Park, C.W.; Kim, Y.-S.; Cho, S.-G.; Cho, M.-L.; Yang, C.W. B cell-associated immune profiles in patients with end-stage renal disease (ESRD). Exp. Mol. Med. 2012, 44, 465–472. [Google Scholar] [CrossRef]
- Molina, M.; Allende, L.M.; Ramos, L.E.; Gutiérrez, E.; Pleguezuelo, D.E.; Hernández, E.R.; Ríos, F.; Fernández, C.; Praga, M.; Morales, E. CD19 + B-Cells, a New Biomarker of Mortality in Hemodialysis Patients. Front. Immunol. 2018, 9, 1221. [Google Scholar] [CrossRef]
- Yuan, S.; Zeng, Y.; Li, J.; Wang, C.; Li, W.; He, Z.; Ye, J.; Li, F.; Chen, Y.; Lin, X.; et al. Phenotypical changes and clinical significance of CD4+/CD8+ T cells in SLE. Lupus Sci. Med. 2022, 9, e000660. [Google Scholar] [CrossRef]
- Piantoni, S.; Regola, F.; Zanola, A.; Andreoli, L.; Dall’Ara, F.; Tincani, A.; Airo’, P. Effector T-cells are expanded in systemic lupus erythematosus patients with high disease activity and damage indexes. Lupus 2018, 27, 143–149. [Google Scholar] [CrossRef]
- Maldonado, A.; Mueller, Y.M.; Thomas, P.; Bojczuk, P.; O’Connors, C.; Katsikis, P.D. Decreased effector memory CD45RA+ CD62L- CD8+ T cells and increased central memory CD45RA- CD62L+ CD8+ T cells in peripheral blood of rheumatoid arthritis patients. Arthritis Res. Ther. 2003, 5, R91. [Google Scholar] [CrossRef] [PubMed]
- Ugarte-Gil, M.F.; Sánchez-Zúñiga, C.; Gamboa-Cárdenas, R.v.; Aliaga-Zamudio, M.; Zevallos, F.; Tineo-Pozo, G.; Cucho-Venegas, J.M.; Mosqueira-Riveros, A.; Perich-Campos, R.A.; Alfaro-Lozano, J.L.; et al. Circulating naive and memory CD4+ T cells and metabolic syndrome in patients with systemic lupus erythematosus: Data from a primarily Mestizo population. Rheumatology 2015, 54, 1302–1307. [Google Scholar] [CrossRef] [PubMed]
- Moro-García, M.A.; Mayo, J.C.; Sainz, R.M.; Alonso-Arias, R. Influence of Inflammation in the Process of T Lymphocyte Differentiation: Proliferative, Metabolic, and Oxidative Changes. Front. Immunol. 2018, 9, 339. [Google Scholar] [CrossRef] [PubMed]
- Sallusto, F.; Geginat, J.; Lanzavecchia, A. Central Memory and Effector Memory T Cell Subsets: Function, Generation and Maintenance. Annu. Rev. Immunol. 2004, 22, 745–763. [Google Scholar] [CrossRef] [PubMed]
- Freitas, G.R.R.; da Luz Fernandes, M.; Agena, F.; Jaluul, O.; Silva, S.C.; Lemos, F.B.C.; Coelho, V.; Elias, D.-N.; Galante, N.Z. Aging and End Stage Renal Disease Cause A Decrease in Absolute Circulating Lymphocyte Counts with A Shift to A Memory Profile and Diverge in Treg Population. Aging Dis. 2019, 10, 49–61. [Google Scholar] [CrossRef]
- Litjens, N.H.R.; van Druningen, C.J.; Betjes, M.G.H. Progressive loss of renal function is associated with activation and depletion of naive T lymphocytes. Clin. Immunol. 2006, 118, 83–91. [Google Scholar] [CrossRef]
- Yoon, J.W.; Gollapudi, S.; Pahl, M.; Vaziri, N.D. Naïve and central memory T-cell lymphopenia in end-stage renal disease. Kidney Int. 2006, 70, 371–376. [Google Scholar] [CrossRef]
- Crépin, T.; Legendre, M.; Carron, C.; Vachey, C.; Courivaud, C.; Rebibou, J.M.; Ferrand, C.; Laheurte, C.; Vauchy, C.; Gaiffe, E.; et al. Uraemia-induced immune senescence and clinical outcomes in chronic kidney disease patients. Nephrol. Dial. Transplant. 2020, 35, 624–632. [Google Scholar] [CrossRef]
- Betjes, M.G.H.; Langerak, A.W.; van der Spek, A.; de Wit, E.A.; Litjens, N.H.R. Premature aging of circulating T cells in patients with end-stage renal disease. Kidney Int. 2011, 80, 208–217. [Google Scholar] [CrossRef]
- Chung, B.H.; Kim, K.W.; Sun, I.O.; Choi, S.R.; Park, H.S.; Jeon, E.J.; Kim, B.-M.; Choi, B.S.; Park, C.W.; Kim, Y.-S.; et al. Increased interleukin-17 producing effector memory T cells in the end-stage renal disease patients. Immunol. Lett. 2012, 141, 181–189. [Google Scholar] [CrossRef]
- Sen, Y.; Chunsong, H.; Baojun, H.; Linjie, Z.; Qun, L.; San, J.; Qiuping, Z.; Junyan, L.; Zhang, X.; Jinquan, T. Aberration of CCR7 CD8 memory T cells from patients with systemic lupus erythematosus: An inducer of T helper type 2 bias of CD4 T cells. Immunology 2004, 112, 274–289. [Google Scholar] [CrossRef] [PubMed]
- Fritsch, R.D.; Shen, X.; Illei, G.G.; Yarboro, C.H.; Prussin, C.; Hathcock, K.S.; Hodes, R.J.; Lipsky, P.E. Abnormal differentiation of memory T cells in systemic lupus erythematosus. Arthritis Rheumatol. 2006, 54, 2184–2197. [Google Scholar] [CrossRef] [PubMed]
- Kaech, S.M.; Wherry, E.J. Heterogeneity and cell-fate decisions in effector and memory CD8+ T cell differentiation during viral infection. Immunity 2007, 27, 393–405. [Google Scholar] [CrossRef]
- Hartzell, S.; Bin, S.; Cantarelli, C.; Haverly, M.; Manrique, J.; Angeletti, A.; La Manna, G.; Murphy, B.; Zhang, W.; Levitsky, J.; et al. Kidney Failure Associates With T Cell Exhaustion and Imbalanced Follicular Helper T Cells. Front. Immunol. 2020, 11, 583702. [Google Scholar] [CrossRef] [PubMed]
- Kosmaczewska, A.; Ciszak, L.; Stosio, M.; Szteblich, A.; Madej, M.; Frydecka, I.; Wiland, P.; Szmyrka, M. CD4 + CD28 null T cells are expanded in moderately active systemic lupus erythematosus and secrete pro-inflammatory interferon gamma, depending on the Disease Activity Index. Lupus 2020, 29, 705–714. [Google Scholar] [CrossRef] [PubMed]
- Tulunay, A.; Yavuz, S.; Direskeneli, H.; Eksioglu-Demiralp, E. CD8+CD28−, suppressive T cells in systemic lupus erythematosus. Lupus 2008, 17, 630–637. [Google Scholar] [CrossRef]
- Zabińska, M.; Krajewska, M.; Kościelska-Kasprzak, K.; Klinger, M. CD3+CD8+CD28− T Lymphocytes in Patients with Lupus Nephritis. J. Immunol. Res. 2016, 2016, 1058165. [Google Scholar] [CrossRef]
- Handono, K.; Zaka Pratama, M.; Partan, R.U.; Susianti, H.; Firdaningrum, N.E.; Roziah, S.; Fachry, A.W.R.; Sumarta, N.H.; Kalim, H. Performance of the T cell senescence markers in predicting the active disease of systemic lupus erythematosus. F1000Research 2022, 11, 285. [Google Scholar] [CrossRef]
- Li, H.; Adamopoulos, I.E.; Moulton, V.R.; Stillman, I.E.; Herbert, Z.; Moon, J.J.; Sharabi, A.; Krishfield, S.; Tsokos, M.G.; Tsokos, G.C. Systemic lupus erythematosus favors the generation of IL-17 producing double negative T cells. Nat. Commun. 2020, 11, 2859. [Google Scholar] [CrossRef]
- Alexander, J.J.; Jacob, A.; Chang, A.; Quigg, R.J.; Jarvis, J.N. Double negative T cells, a potential biomarker for systemic lupus erythematosus. Precis. Clin. Med. 2020, 3, 34–43. [Google Scholar] [CrossRef]
- Ricker, E.; Manni, M.; Flores-Castro, D.; Jenkins, D.; Gupta, S.; Rivera-Correa, J.; Meng, W.; Rosenfeld, A.M.; Pannellini, T.; Bachu, M.; et al. Altered function and differentiation of age-associated B cells contribute to the female bias in lupus mice. Nat. Commun. 2021, 12, 4813. [Google Scholar] [CrossRef] [PubMed]



| SLE | ESKD-HD | HC | p * | p * | p * | p * | |
|---|---|---|---|---|---|---|---|
| n | 30 | 53 | 31 | KW Test | SLE vs. HC | HD vs. HC | SLE vs. HD |
| Female (%) | 29 (96.7) | 19 (35.8) | 17 (54.8) | <0.0001 | - | - | - |
| Age (yrs) | 43 ± 14 | 47 ± 14 | 49 ± 13 | NS | NS | NS | NS |
| Time since diagnosis (mo) | 84 (45–125) | 67 (28–84) | - | - | - | - | NS |
| Laboratory results | |||||||
| WCC | 7200 (3350) | 7100 (1950) | 6400 (1800) | NS | - | - | - |
| Neutrophils (%) | 69.6 (20.7) | 63.3 (9.6) | 58.1 (10.35) | <0.0001 | <0.0001 | 0.004 | NS |
| Neutrophils | 4600 (3500) | 4550 (1675) | 3500 (1200) | 0.007 | 0.03 | 0.009 | NS |
| Lymphocytes (%) | 23.1 (16.1) | 19.8 (8.9) | 25.6 (9) | 0.001 | 0.03 | <0.0001 | NS |
| Lymphocytes | 1400 (900) | 1500 (500) | 2100 (900) | 0.001 | 0.005 | 0.001 | NS |
| NLR | 3 (4) | 2.8 (1.37) | 1.8 (0.85) | <0.0001 | <0.0001 | <0.0001 | NS |
| SLE | ESKD-HD | HC | p * | p * | p * | p * | |
|---|---|---|---|---|---|---|---|
| n | 30 | 53 | 31 | KW Test | SLE vs. HC | ESKD-HD vs. HC | SLE vs. ESKD-HD |
| CD19 ** | 75.4 (14.4–520.8) | 97 (32–341) | 214 (84–576) | <0.001 | <0.001 | <0.001 | NS |
| IgD+CD27− | 37.71 (0.26–434.84) | 73 (2–303) | 117 (5–364) | <0.001 | <0.001 | <0.001 | NS |
| IgD+CD27+ | 5.12 (0.13–17.55) | 5 (0–31) | 23 (2–700) | <0.001 | <0.001 | <0.001 | NS |
| IgD-CD27+ | 18.58 (0.47–89.58) | 13 (1–75) | 38 (11–258) | <0.001 | 0.001 | <0.001 | NS |
| IgD-CD27− | 10.84 (0.93–122.91) | 8 (1–132) | 21 (3–202) | <0.001 | 0.007 | <0.001 | NS |
| SLE | ESKD-HD | HC | p * | p * | p * | p * | |
|---|---|---|---|---|---|---|---|
| n | 30 | 53 | 31 | KW Test | SLE vs. HC | ESKD−HD vs. HC | SLE vs. ESKD−HD |
| CD4 ** | 651.2 (71.1–1478.2) | 713 (234–1509) | 986 (344–1591) | <0.001 | 0.004 | 0.001 | NS |
| Early differentiated cells ** | |||||||
| CD4+CD31+ | 216.38 (16.3–904.7) | 131 (27–560) | 250 (69–967) | 0.014 | NS | 0.01 | NS |
| CD45RA+CCR7+ | 298.2 (21.3–1049.5) | 242 (47–854) | 359 (28–1357) | NS | NS | 0.022 | NS |
| CD4CD45RA+CD28+ | 267.97 (20.62–1030.31) | 200 (7–768) | 388 (139–1402) | 0.001 | NS | <0.001 | NS |
| CD4CD28+CD57− | 610.7 (54.68–1461.94) | 631 (201–1346) | 958 (332–1569) | <0.001 | 0.004 | <0.001 | NS |
| CD4CD45RA+CD57− | 254.03 (21.05–1077.61) | 258 (27–916) | 401 (160–1373) | 0.005 | 0.035 | 0.005 | NS |
| CD4CD45RA-CD57− | 290.67 (38.96–884.43) | 375 (133–972) | 539 (173–991) | <0.001 | <0.001 | 0.01 | NS |
| Memmory cells ** | NS | ||||||
| CD45RA-CCR7+ | 402.35 (38.7–972.4) | 384 (80–1015) | 563 (40–1001) | NS | 0.046 | NS | NS |
| CD45RA-CCR7− | 1.62 (0–73.49) | 5 (0–109) | 11 (0–590) | 0.002 | 0.002 | NS | 0.01 |
| Senescent/Advanced differentiated cells ** | |||||||
| CD45RA+CCR7− | 7.29 (0–180.62) | 14 (0–150) | 23 (0–487) | 0.031 | 0.027 | NS | NS |
| CD4CD28− | 20.12 (1.27–139.06) | 42 (3–851) | 38 (3–299) | 0.02 | NS | NS | 0.01 |
| CD4CD28-CD57− | 11.82 (0–65.26) | 20 (2–175) | 13 (2–119) | NS | NS | NS | 0.016 |
| CD4CD28-CD57+ | 9.90 (0.46–73.8) | 17 (0–783) | 23 (0–274) | NS | NS | NS | 0.041 |
| SLE | ESKD-HD | HC | p * | p * | p * | p * | |
|---|---|---|---|---|---|---|---|
| n | 30 | 53 | 31 | KW Test | SLE vs. HC | ESKD-HD vs. HC | SLE vs. ESKD-HD |
| CD8 ** | 414.8 (60.6–2017.8) | 354 (121–1225) | 454.5 (154–1310) | NS | NS | 0.04 | NS |
| Early differentiated cells ** | |||||||
| CD8+CD31+ | 88.19 (8.2–1047) | 91 (4–576) | 187.5 (8–541) | NS | NS | 0.03 ** | NS |
| CD8CD45RA+CD28+ | 113.56 (1.81–753.7) | 86 (0–748) | 212.5 (7–1257) | NS | NS | 0.025 ** | NS |
| CD8CD28+CD57− | 249.45 (5.49–1362) | 169 (46–569) | 298 (95–646) | 0.003 | NS | <0.001 | NS |
| CD8CD45RA+CD57− | 63.65 (3.83–889.8) | 69 (8–450) | 133 (8–552) | NS | NS | 0.039 | NS |
| CD8CD45RA-CD57− | 194.52 (1.8–945.1) | 154 (6–936) | 179 (28–555) | NS | NS | NS | NS |
| Memory cells ** | |||||||
| CD8CD45RA-CCR7+ | 171.52 (2.5–1417) | 127 (0–1104) | 123 (1–941) | NS | NS | NS | NS |
| CD8CD45RA-CCR7− | 13.94 (0.59–92.37) | 13 (0–136) | 25 (0–355) | NS | NS | NS | NS |
| Senescent/Advanced differentiated cells ** | |||||||
| CD8CD45RA+CCR7- | 11.13 (0–279.6) | 20 (0–242) | 49.5 (0–534) | 0.043 | 0.04 | NS | NS |
| CD8CD28− | 87.83 (4.56–1361.2) | 139 (18–839) | 135 (36–633) | NS | NS | NS | NS |
| CD8CD28-CD57− | 46.49 (0.33–796.1) | 62 (9–364) | 46 (7–332) | NS | NS | NS | NS |
| CD8CD28-CD57+ | 53.17 (0.83–571.04) | 79 (1–746) | 71 (0–470) | NS | NS | NS | NS |
| CD8CD45RA+CD28− | 52.27 (2.13–263.6) | 120 (6–716) | 197.5 (9–783) | <0.001 | <0.001 | NS | 0.005 |
| CD8CD45+CD57+ | 10.05 (0.45–141) | 26 (0–388) | 20 (0–333) | 0.021 | 0.03 | NS | 0.047 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moysidou, E.; Lioulios, G.; Xochelli, A.; Nikolaidou, V.; Christodoulou, M.; Mitsoglou, Z.; Stai, S.; Fylaktou, A.; Papagianni, A.; Stangou, M. Different Types of Chronic Inflammation Engender Distinctive Immunosenescent Profiles in Affected Patients. Int. J. Mol. Sci. 2022, 23, 14688. https://doi.org/10.3390/ijms232314688
Moysidou E, Lioulios G, Xochelli A, Nikolaidou V, Christodoulou M, Mitsoglou Z, Stai S, Fylaktou A, Papagianni A, Stangou M. Different Types of Chronic Inflammation Engender Distinctive Immunosenescent Profiles in Affected Patients. International Journal of Molecular Sciences. 2022; 23(23):14688. https://doi.org/10.3390/ijms232314688
Chicago/Turabian StyleMoysidou, Eleni, Georgios Lioulios, Aliki Xochelli, Vasiliki Nikolaidou, Michalis Christodoulou, Zoi Mitsoglou, Stamatia Stai, Asimina Fylaktou, Aikaterini Papagianni, and Maria Stangou. 2022. "Different Types of Chronic Inflammation Engender Distinctive Immunosenescent Profiles in Affected Patients" International Journal of Molecular Sciences 23, no. 23: 14688. https://doi.org/10.3390/ijms232314688
APA StyleMoysidou, E., Lioulios, G., Xochelli, A., Nikolaidou, V., Christodoulou, M., Mitsoglou, Z., Stai, S., Fylaktou, A., Papagianni, A., & Stangou, M. (2022). Different Types of Chronic Inflammation Engender Distinctive Immunosenescent Profiles in Affected Patients. International Journal of Molecular Sciences, 23(23), 14688. https://doi.org/10.3390/ijms232314688






