Mechanisms of Susceptibility and Resilience to PTSD: Role of Dopamine Metabolism and BDNF Expression in the Hippocampus
Abstract
1. Introduction
2. Results
2.1. Behavior of SM and FM in Elevated plus Maze
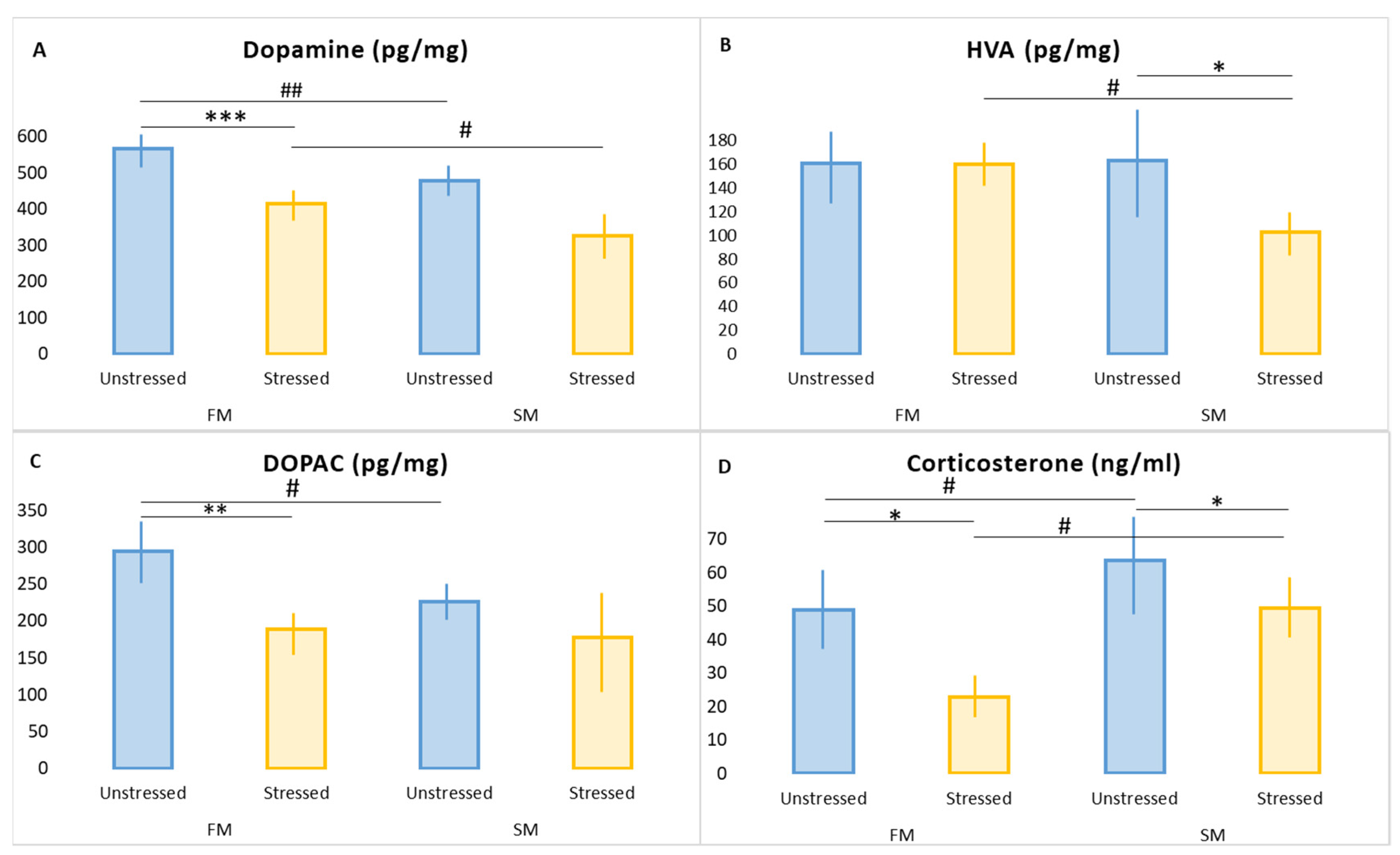
2.2. Effect of PS on Plasma CORT Concentrations in FM and SM Rats
2.3. Effect of PS on Hippocampal DA Metabolism in FM and SM Rats
2.4. The Effect of PS on Hippocampal DAT, MAO-A, MAO-B, COMT, and BDNF mRNAs in FM and SM Rats
2.5. The Effect of PS on Hippocampal and Plasma BDNF Concentrations in FM and SM Rats
3. Discussion
4. Materials and Methods
4.1. Experimental Animals
4.2. Hexobarbital Sleep Test (HST)
4.3. Predator Stress
4.4. Behavioral Testing
4.5. Measurement of Plasma Concentration of Corticosterone (CORT)
4.6. Measurement of Hippocampal Concentrations of DA and Its Metabolites
4.7. Measurement of mRNAs
4.7.1. RNA Isolation
4.7.2. cDNA Synthesis and Real-Time RT–PCR
4.8. ELISA Measurements
4.9. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sherin, J.E.; Nemeroff, C.B. Post-traumatic stress disorder: The neurobiological impact of psychological trauma. Dialogues Clin. Neurosci. 2011, 13, 263–278. [Google Scholar] [CrossRef] [PubMed]
- Lazuko, S.S.; Kuzhel, O.P.; Belyaeva, L.E.; Manukhina, E.B.; Downey, H.F.; Tseilikman, O.B.; Komelkova, M.V.; Tseilikman, V.E. Posttraumatic stress disorder disturbs coronary tone and its regulatory mechanisms. Cell Mol. Neurobiol. 2018, 38, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Tseilikman, V.; Komelkova, M.; Kondashevskaya, M.V.; Manukhina, E.; Downey, H.F.; Chereshnev, V.; Chereshneva, M.; Platkovskii, P.; Goryacheva, A.; Pashkov, A.; et al. A rat model of post-traumatic stress syndrome causes phenotype-associated morphological changes and hypofunction of the adrenal gland. Int. J. Mol. Sci. 2021, 22, 13235. [Google Scholar] [CrossRef] [PubMed]
- Manukhina, E.B.; Tseilikman, V.E.; Komelkova, M.V.; Lapshin, M.S.; Goryacheva, A.V.; Kondashevskaya, M.V.; Mkhitarov, V.A.; Lazuko, S.S.; Tseilikman, O.B.; Sarapultsev, A.P.; et al. Cardiac injury in rats with experimental posttraumatic stress disorder and mechanisms of its limitation in experimental posttraumatic stress disorder-resistant rats. J. Appl. Physiol. 2021, 130, 759–771. [Google Scholar] [CrossRef]
- Pitman, R.K.; Rasmusson, A.M.; Koenen, K.; Shin, L.M.; Orr, S.P.; Gilbertson, M.W.; Milad, M.R.; Liberzon, I. Biological studies of post-traumatic stress disorder. Nat. Rev. Neurosci. 2012, 13, 769–787. [Google Scholar] [CrossRef]
- Horn, S.R.; Charney, D.S.; Feder, A. Understanding resilience: New approaches for preventing and treating PTSD. Exp. Neurol. 2016, 284, 119–132. [Google Scholar] [CrossRef]
- Tseylikman, O.B.; Lapshin, M.S.; Kozochkin, D.A.; Komel’kova, M.V.; Kuzina, O.V.; Golodniy, S.V.; Lazuko, S.S.; Tseylikman, V.E. Behavioral activity and some markers of posttraumatic stress disorder among serotoninergic system indicators and glucocorticoid metabolizing enzymes in rats with different duration of hexenal sleep. Bull. Exp. Biol. Med. 2016, 161, 456–469. [Google Scholar] [CrossRef]
- Komelkova, M.; Manukhina, E.; Downey, H.F.; Sarapultsev, A.; Cherkasova, O.; Kotomtsev, V.; Platkovskiy, P.; Fedorov, S.; Sarapultsev, P.; Tseilikman, O.; et al. Hexobarbital sleep test for predicting the susceptibility or resistance to experimental posttraumatic stress disorder. Int. J. Mol. Sci. 2020, 21, 5900. [Google Scholar] [CrossRef]
- Tseilikman, V.; Lapshin, M.; Klebanov, I.; Chrousos, G.; Vasilieva, M.; Pashkov, A.; Fedotova, J.; Tseilikman, D.; Shatilov, V.; Manukhina, E.; et al. The link between activities of hepatic 11beta-Hydroxysteroid dehydrogenase-1 and monoamine oxidase-A in the brain following repeated predator stress: Focus on heightened anxiety. Int. J. Mol. Sci. 2022, 23, 4881. [Google Scholar] [CrossRef]
- Blum, K.; Giordano, J.; Oscar-Berman, M.; Bowirrat, A.; Simpatico, T.; Barh, D. Diagnosis and healing in veterans suspected of suffering from post-traumatic stress disorder (PTSD) using reward gene testing and reward circuitry natural dopaminergic activation. J. Genet. Syndr. Gene Ther. 2012, 3, 1000116. [Google Scholar] [CrossRef]
- Roy-Byrne, P.; Arguelles, L.; Vitek, M.E.; Goldberg, J.; Keane, T.M.; True, W.R.; Pitman, R.K. Persistence and change of PTSD symptomatology--a longitudinal co-twin control analysis of the Vietnam Era Twin Registry. Soc. Psychiatry Psychiatr. Epidemiol. 2004, 39, 681–685. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, T.; Blum, K.; Oscar-Berman, M.; Febo, M.; Agan, G.; Fratantonio, J.L.; Simpatico, T.; Gold, M.S. Putative dopamine agonist (KB220Z) attenuates lucid nightmares in PTSD patients: Role of enhanced brain reward functional connectivity and homeostasis redeeming joy. J. Behav. Addict. 2015, 4, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Dremencov, E.; Lapshin, M.; Komelkova, M.; Alliluev, A.; Tseilikman, O.; Karpenko, M.; Pestereva, N.; Manukhina, E.; Downey, H.F.; Tseilikman, V. Chronic predator scent stress alters serotonin and dopamine levels in the rat thalamus and hypothalamus, respectively. Gen. Physiol. Biophys. 2019, 38, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Segman, R.H.; Cooper-Kazaz, R.; Macciardi, F.; Goltser, T.; Halfon, Y.; Dobroborski, T.; Shalev, A.Y. Association between the dopamine transporter gene and posttraumatic stress disorder. Mol. Psychiatry 2002, 7, 903–907. [Google Scholar] [CrossRef][Green Version]
- Clark, R.; DeYoung, C.G.; Sponheim, S.R.; Bender, T.L.; Polusny, M.A.; Erbes, C.R.; Arbisi, P.A. Predicting post-traumatic stress disorder in veterans: Interaction of traumatic load with COMT gene variation. J. Psychiatr. Res. 2013, 47, 1849–1856. [Google Scholar] [CrossRef]
- Tseilikman, V.; Komelkova, M.; Lapshin, M.; Alliluev, A.; Tseilikman, O.; Karpenko, M.; Pestereva, N.; Manukhina, E.; Downey, H.F.; Kondashevskaya, M.; et al. High and low anxiety phenotypes in a rat model of complex post-traumatic stress disorder are associated with different alterations in regional brain monoamine neurotransmission. Psychoneuroendocrinology 2020, 117, 104691. [Google Scholar] [CrossRef]
- Surget, A.; Belzung, C. Adult hippocampal neurogenesis shapes adaptation and improves stress response: A mechanistic and integrative perspective. Mol. Psychiatry 2021, 27, 403–421. [Google Scholar] [CrossRef]
- Vlachos, I.I.; Papageorgiou, C.; Margariti, M. Neurobiological trajectories involving social isolation in PTSD: A systematic review. Brain Sci. 2020, 10, 173. [Google Scholar] [CrossRef]
- Cabib, S.; Campus, P.; Conversi, D.; Orsini, C.; Puglisi-Allegra, S. Functional and dysfunctional neuroplasticity in learning to cope with stress. Brain Sci. 2020, 10, 127. [Google Scholar] [CrossRef]
- Ghasemi, M.; Navidhamidi, M.; Rezaei, F.; Azizikia, A.; Mehranfard, N. Anxiety and hippocampal neuronal activity: Relationship and potential mechanisms. Cogn. Affect. Behav. Neurosci. 2021, 22, 431–449. [Google Scholar] [CrossRef]
- Tomar, A.; McHugh, T.J. The impact of stress on the hippocampal spatial code. Trends Neurosci. 2021, 45, 120–132. [Google Scholar] [CrossRef] [PubMed]
- Tomar, A.; Polygalov, D.; Chattarji, S.; McHugh, T.J. Stress enhances hippocampal neuronal synchrony and alters ripple-spike interaction. Neurobiol. Stress 2021, 14, 100327. [Google Scholar] [CrossRef] [PubMed]
- Ullmann, E.; Perry, S.W.; Licinio, J.; Wong, M.L.; Dremencov, E.; Zavjalov, E.L.; Shevelev, O.B.; Khotskin, N.V.; Koncevaya, G.V.; Khotshkina, A.S.; et al. From allostatic load to allostatic state-an endogenous sympathetic strategy to deal with chronic anxiety and stress? Front. Behav. Neurosci. 2019, 13, 47. [Google Scholar] [CrossRef]
- Schwabe, L.; Dalm, S.; Schachinger, H.; Oitzl, M.S. Chronic stress modulates the use of spatial and stimulus-response learning strategies in mice and man. Neurobiol. Learn. Mem. 2008, 90, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Szeszko, P.R.; Bierer, L.M.; Bader, H.N.; Chu, K.W.; Tang, C.Y.; Murphy, K.M.; Hazlett, E.A.; Flory, J.D.; Yehuda, R. Cingulate and hippocampal subregion abnormalities in combat-exposed veterans with PTSD. J. Affect. Disord. 2022, 311, 432–439. [Google Scholar] [CrossRef]
- Ressler, K.J.; Berretta, S.; Bolshakov, V.Y.; Rosso, I.M.; Meloni, E.G.; Rauch, S.L.; Carlezon, W.A., Jr. Post-traumatic stress disorder: Clinical and translational neuroscience from cells to circuits. Nat. Rev. Neurol. 2022, 18, 273–288. [Google Scholar] [CrossRef]
- Hinojosa, C.A. Does hippocampal volume in patients with posttraumatic stress disorder vary by trauma type? Harv. Rev. Psychiatry 2022, 30, 118–134. [Google Scholar] [CrossRef]
- Ledreux, A.; Boger, H.A.; Hinson, V.K.; Cantwell, K.; Granholm, A.C. BDNF levels are increased by aminoindan and rasagiline in a double lesion model of Parkinson‘s disease. Brain Res. 2016, 1631, 34–45. [Google Scholar] [CrossRef]
- Fortunato, J.J.; Réus, G.Z.; Kirsch, T.R.; Stringari, R.B.; Stertz, L.; Kapczinski, F.; Pinto, J.P.; Hallak, J.E.; Zuardi, A.W.; Crippa, J.A.; et al. Acute harmine administration induces antidepressive-like effects and increases BDNF levels in the rat hippocampus. Prog. Neuropsychopharmacol. Biol. Psychiatry 2009, 33, 1425–1430. [Google Scholar] [CrossRef]
- Laham, B.J.; Gould, E. How stress influences the dynamic plasticity of the brain’s extracellular matrix. Front. Cell. Neurosci. 2022, 15, 814287. [Google Scholar] [CrossRef]
- Tseilikman, V.; Dremencov, E.; Tseilikman, O.; Pavlovicova, M.; Lacinova, L.; Jezova, D. Role of glucocorticoid- and monoamine-metabolizing enzymes in stress-related psychopathological processes. Stress 2020, 23, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kozochkin, D.A.; Manukhina, E.B.; Downey, H.F.; Tseilikman, O.B.; Komelkova, M.V.; Vasilyeva, M.V.; Lapshin, M.S.; Sahabutdinov, M.N.; Lazuko, S.S.; Tseilikman, V.E. The role of microsomal oxidation in the regulation of monoamine oxidase activity in the brain and liver of rats. Gen. Physiol. Biophys. 2017, 36, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Rao, R.M.; Sadananda, M. Influence of State and/or Trait Anxieties of Wistar Rats in an Anxiety Paradigm. Ann. Neurosci. 2016, 23, 44–50. [Google Scholar] [CrossRef]
- Tseilikman, V.; Dremencov, E.; Maslennikova, E.; Ishmatova, A.; Manukhina, E.; Downey, H.F.; Klebanov, I.; Tseilikman, O.; Komelkova, M.; Lapshin, M.S.; et al. Post-traumatic stress disorder chronification via monoaminooxidase and cortisol metabolism. Horm. Metab. Res. 2019, 51, 618–622. [Google Scholar] [CrossRef]
- Medvedev, A.E.; Rajgorodskaya, D.I.; Gorkin, V.Z.; Fedotova, I.B.; Semiokhina, A.F. The role of lipid peroxidation in the possible involvement of membrane-bound monoamine oxidases in gamma-aminobutyric acid and glucosamine deamination in rat brain. Mol. Chem. Neuropathol. 1992, 16, 187–201. [Google Scholar] [CrossRef] [PubMed]
- Dean, R.T.; Thomas, S.M.; Garner, A. Free-radical-mediated fragmentation of monoamine oxidase in the mitochondrial membrane Roles for lipid radicals. Biochem. J. 1986, 240, 489–494. [Google Scholar] [CrossRef] [PubMed]
- Nagatsu, T. Progress in monoamine oxidase (MAO) research in relation to genetic engineering. Neurotoxicology 2004, 25, 11–20. [Google Scholar] [CrossRef]
- Higuchi, Y.; Soga, T.; Parhar, I.S. Regulatory pathways of monoamine oxidase A during social stress. Front. Neurosci. 2017, 11, 604. [Google Scholar] [CrossRef]
- Sun, X.; Ming, Q.; Zhong, X.; Dong, D.; Li, C.; Xiong, G.; Cheng, C.; Cao, W.; He, J.; Wang, X.; et al. The MAOA gene influences the neural response to psychosocial stress in the human brain. Front. Behav. Neurosci. 2020, 14, 65. [Google Scholar] [CrossRef]
- Cvijić, G.; Radojicić, R.; Djordjević, J.; Davidović, V. The effect of glucocorticoids on the activity of monoamine oxidase, copper-zinc superoxide dismutase and catalase in the rat hypothalamus. Funct. Neurol. 1995, 10, 175–181. [Google Scholar]
- Grunewald, M.; Johnson, S.; Lu, D.; Wang, Z.; Lomberk, G.; Albert, P.R.; Stockmeier, C.A.; Meyer, J.H.; Urrutia, R.; Miczek, K.A.; et al. Mechanistic role for a novel glucocorticoid-KLF11 (TIEG2) protein pathway in stress-induced monoamine oxidase A expression. J. Biol. Chem. 2012, 87, 24195–24206. [Google Scholar] [CrossRef] [PubMed]
- Soliman, A.; Udemgba, C.; Fan, I.; Xu, X.; Miler, L.; Rusjan, P.; Houle, S.; Wilson, A.A.; Pruessner, J.; Ou, X.-M.; et al. Convergent effects of acute stress and glucocorticoid exposure upon MAO-A in humans. J. Neurosci. 2012, 32, 17120–17127. [Google Scholar] [CrossRef] [PubMed]
- Puhr, M.; Eigentler, A.; Handle, F.; Hackl, H.; Ploner, C.; Heidegger, I.; Schaefer, G.; Brandt, M.P.; Hoefer, J.; Van der Pluijm, G.; et al. Targeting the glucocorticoid receptor signature gene Mono Amine Oxidase-A enhances the efficacy of chemo- and anti-androgen therapy in advanced prostate cancer. Oncogene 2021, 40, 3087–3100. [Google Scholar] [CrossRef] [PubMed]
- Karahoda, R.; Horackova, H.; Kastner, P.; Matthios, A.; Cerveny, L.; Kucera, R.; Kacerovsky, M.; Duintjer Tebbens, J.; Bonnin, A.; Abad, C.; et al. Serotonin homeostasis in the materno-foetal interface at term: Role of transporters (SERT/SLC6A4 and OCT3/SLC22A3) and monoamine oxidase A (MAO-A) in uptake and degradation of serotonin by human and rat term placenta. Acta Physiol. 2020, 229, e13478. [Google Scholar] [CrossRef]
- Raitsin, S.; Tong, J.; Kish, S.; Xu, X.; Magomedova, L.; Cummins, C.; Andreazza, A.C.; Scola, G.; Baker, G.; Meyer, J.H. Subchronic glucocorticoids, glutathione depletion and a postpartum model elevate monoamine oxidase a activity in the prefrontal cortex of rats. Brain Res. 2017, 1666, 1–10. [Google Scholar] [CrossRef]
- Nasca, C.; Zelli, D.; Bigio, B.; Piccinin, S.; Scaccianoce, S.; Nisticò, R.; McEwen, B.S. Stress dynamically regulates behavior and glutamatergic gene expression in hippocampus by opening a window of epigenetic plasticity. Proc. Natl. Acad. Sci. USA 2015, 112, 14960–14965. [Google Scholar] [CrossRef]
- Colucci-D’Amato, L.; Speranza, L.; Volpicelli, F. Neurotrophic factor BDNF, physiological functions and therapeutic potential in depression, neurodegeneration and brain cancer. Int. J. Mol. Sci. 2020, 21, 7777. [Google Scholar] [CrossRef]
- Giacobbo, B.L.; Doorduin, J.; Klein, H.C.; Dierckx, R.A.J.O.; Bromberg, E.; de Vries, E.F.J. Brain-derived neurotrophic factor in brain disorders: Focus on neuroinflammation. Mol. Neurobiol. 2019, 56, 3295–3312. [Google Scholar] [CrossRef]
- McEwen, B.S. Stress-induced remodeling of hippocampal CA3 pyramidal neurons. Brain Res. 2016, 1645, 50–54. [Google Scholar] [CrossRef]
- Tseilikman, V.; Akulov, A.; Shevelev, O.; Khotskina, A.; Kontsevaya, G.; Moshkin, M.; Fedotova, J.; Pashkov, A.; Tseilikman, O.; Agletdinov, E.; et al. Paradoxical anxiety level reduction in animal chronic stress: A unique role of hippocampus neurobiology. Int. J. Mol. Sci. 2022, 23, 9151. [Google Scholar] [CrossRef]
- McEwen, B.S.; Bowles, N.P.; Gray, J.D.; Hill, M.N.; Hunter, R.G.; Karatsoreos, I.N.; Nasca, C. Mechanisms of stress in the brain. Nat. Neurosci. 2015, 18, 1353–1363. [Google Scholar] [CrossRef] [PubMed]
- Yaqun, L.; Haixia, Y.; Yuchen, S.; Mingxin, Z.; Manqi, L.; Yunlong, T.; Aizhen, W.; Xinmin, H. An Shen Ding Zhi Ling Ameliorates the Symptoms of Attention Deficit Hyperactivity Disorder via Modulating Brain-Derived Neurotrophic Factor-Related Signaling Pathways. Evid. Based Complement. Altern. Med. 2022, 21, 5471586. [Google Scholar] [CrossRef] [PubMed]
- Tseilikman, V.E.; Kozochkin, D.A.; Manukhina, E.B.; Downey, H.F.; Tseilikman, O.B.; Misharina, M.E.; Nikitina, A.A.; Komelkova, M.V.; Lapshin, M.S.; Kondashevskaya, M.V.; et al. Duration of hexobarbital-induced sleep and monoamine oxidase activities in rat brain: Focus on the behavioral activity and on the free-radical oxidation. Gen. Physiol. Biophys. 2016, 35, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Manukhina, E.B.; Tseilikman, V.E.; Karpenko, M.N.; Pestereva, N.S.; Tseilikman, O.B.; Komelkova, M.V.; Kondashevskaya, M.V.; Goryacheva, A.V.; Lapshin, M.S.; Platkovskii, P.O.; et al. Intermittent hypoxic conditioning alleviates post-traumatic stress disorder-induced samage and dysfunction of rat visceral organs and brain. Int. J. Mol. Sci. 2020, 21, 345. [Google Scholar] [CrossRef]
- Cohen, H.; Matar, M.A.; Joseph, Z. Animal models of post-traumatic stress disorder. Curr. Protoc. Neurosci. 2013, 64, 9–45. [Google Scholar] [CrossRef]
- Ullmann, E.; Chrousos, G.; Perry, S.W.; Wong, M.L.; Licinio, J.; Bornstein, S.R.; Tseilikman, O.; Komelkova, M.; Lapshin, M.S.; Vasilyeva, M.; et al. Offensive behavior, striatal glutamate metabolites, and limbic-hypothalamic-pituitary-adrenal responses to stress in chronic anxiety. Int. J. Mol. Sci. 2020, 21, 7440. [Google Scholar] [CrossRef]
- Manukhina, E.B.; Tseilikman, V.E.; Tseilikman, O.B.; Komelkova, M.V.; Kondashevskaya, M.V.; Goryacheva, A.V.; Lapshin, M.S.; Platkovskii, P.O.; Alliluev, A.V.; Downey, H.F. Intermittent hypoxia improves behavioral and adrenal gland dysfunction induced by posttraumatic stress disorder in rats. J. Appl. Physiol. 2018, 125, 931–937. [Google Scholar] [CrossRef]
- Wilson, C.B.; Ebenezer, P.J.; McLaughlin, L.D.; Francis, J. Predator exposure/psychosocial stress animal model of post-traumatic stress disorder modulates neurotransmitters in the rat hippocampus and prefrontal cortex. PLoS ONE 2014, 9, e89104. [Google Scholar] [CrossRef]

| Variable | FM | SM | ||
|---|---|---|---|---|
| Unstressed (n = 10) | Stressed (n = 12) | Unstressed (n = 10) | Stressed (n = 10) | |
| Time spent in open arms (sec) | 117 ± 18 | 284 ± 78 ** | 58 ± 17 ## | 46 ± 10 ## |
| Time spent in closed arms (sec) | 483 ± 18 | 317 ± 78 ** | 542 ± 27 ## | 554 ± 27 ## |
| Entries into open arms | 8.2 ± 1.0 | 8.1 ± 3.9 | 5.3 ± 1.2 ## | 2.0 ± 0.5 *## |
| Entries into closed arms | 5.7 ± 1.9 | 4.1 ± 2.7 | 5.0 ± 3.0 | 3.3 ± 1.2 |
| AI | 0.60 ± 0.04 | 0.45 ± 0.02 * | 0.67 ± 0.08 # | 0.80 ± 0.13 *## |
| FM | SM | |||
|---|---|---|---|---|
| Unstressed (n = 10) | Stressed (n = 12) | Unstressed (n = 10) | Stressed (n = 10) | |
| DAT eDAT/GAPDH | 0.76 ± 0.09 | 1.5 ± 0.4 * | 2.42 ± 3.24 # | 2.54 ± 1.11 |
| MAO-A eMAO-A/GAPDH | 0.76 ± 0.3 | 0.98 ± 0.4 | 2.39 ± 1.35 | 6.54 ± 0.97 ***# |
| MAO-B (eMAO-B/GAPDH) | 0.61 ± 0.15 | 2.7 ± 1.36 | 0.47 ± 0.28 | 3.28 ± 0.96 * |
| COMT (eCOMT/GAPDH) | 0.96 ± 0.09 | 1.97 ± 0.35 * | 1.04 ± 3.89 | 2.35 ± 0.83 |
| BDNF eBDNF/GAPDH | 1.37 ± 0.49 | 3.01 ± 0.24 ** | 0.8 ± 0.2 | 0.4 ± 0.1 *### |
| Name of the Gene | Primer Sequence 5′ → 3′ | Annealing Temperature, °C |
|---|---|---|
| MAO-A | F GCCAGGAACGGAAATTTGTA R TCTCAGGTGGAAGCTCTGGT | 64 |
| MAO-B | F TGGGCCAAGAGATTCCCAGTGATG R AGAGTGTGGCAATCTGCTTTGTAG | 60 |
| Comt | F CTGGAGGCCATCGACACCTA R AGTAAGCTCCCAGCTCCAGCA | 60 |
| BDNF | F GAAAGTCCCGGTATCAAAAG R CGCCAGCCAATTCTCTTTTTG | 60 |
| DAT | F TTGGGTTTGGAGTGCTGATTGC R AGAAGACGACGAAGCCAGAGG | 55 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tseilikman, V.E.; Tseilikman, O.B.; Pashkov, A.A.; Ivleva, I.S.; Karpenko, M.N.; Shatilov, V.A.; Zhukov, M.S.; Fedotova, J.O.; Kondashevskaya, M.V.; Downey, H.F.; et al. Mechanisms of Susceptibility and Resilience to PTSD: Role of Dopamine Metabolism and BDNF Expression in the Hippocampus. Int. J. Mol. Sci. 2022, 23, 14575. https://doi.org/10.3390/ijms232314575
Tseilikman VE, Tseilikman OB, Pashkov AA, Ivleva IS, Karpenko MN, Shatilov VA, Zhukov MS, Fedotova JO, Kondashevskaya MV, Downey HF, et al. Mechanisms of Susceptibility and Resilience to PTSD: Role of Dopamine Metabolism and BDNF Expression in the Hippocampus. International Journal of Molecular Sciences. 2022; 23(23):14575. https://doi.org/10.3390/ijms232314575
Chicago/Turabian StyleTseilikman, Vadim E., Olga B. Tseilikman, Anton A. Pashkov, Irina S. Ivleva, Marina N. Karpenko, Vladislav A. Shatilov, Maxim S. Zhukov, Julia O. Fedotova, Marina V. Kondashevskaya, H. Fred Downey, and et al. 2022. "Mechanisms of Susceptibility and Resilience to PTSD: Role of Dopamine Metabolism and BDNF Expression in the Hippocampus" International Journal of Molecular Sciences 23, no. 23: 14575. https://doi.org/10.3390/ijms232314575
APA StyleTseilikman, V. E., Tseilikman, O. B., Pashkov, A. A., Ivleva, I. S., Karpenko, M. N., Shatilov, V. A., Zhukov, M. S., Fedotova, J. O., Kondashevskaya, M. V., Downey, H. F., & Manukhina, E. B. (2022). Mechanisms of Susceptibility and Resilience to PTSD: Role of Dopamine Metabolism and BDNF Expression in the Hippocampus. International Journal of Molecular Sciences, 23(23), 14575. https://doi.org/10.3390/ijms232314575






