Vitamin D and Beta Cells in Type 1 Diabetes: A Systematic Review
Abstract
1. Introduction
2. Results and Discussion
2.1. Cell Culture Studies
2.2. Islet Studies
2.3. Animal Studies
2.3.1. Non-Obese Diabetic (NOD) Mice
2.3.2. Other Models
2.3.3. Negative Mouse Studies
2.3.4. Conclusions; Animal Studies
2.4. Human Studies
2.4.1. Human Polymorphism Studies (Table 1)
| Ref | Gene Polymorphism | SNP | Mutation | Location | Effect |
|---|---|---|---|---|---|
| [44] | FokI | rs2228570 | C > T | Exon 2 | Translation start site influences VDR activity |
| [45,47] | FokI | rs10735810 | C > T | Exon 2 | Translation start site influences VDR activity |
| [44] | TaqI | rs731236 | C > T | 3′ UTR | Modulation of mRNA stability |
| [44] | BsmI | rs1544410 | A > G | 3′ UTR | Modulation of mRNA stability |
| [44] | ApaI | rs7975232 | A > C | 3′ UTR | Modulation of mRNA stability |
2.4.2. Human Observational and Cross-Sectional Studies and Case Reports
2.4.3. Therapeutic Trials (Table 2)
| 1st Author | Ref | Design | N (Loss) | Age | Treatment | Notes and Effects | Strengths | Weaknesses |
|---|---|---|---|---|---|---|---|---|
| Pitocco | [64] | Open-label RCT T1D < 4 w | 70 (3) | >5 y | 1,25D 0.25 µg 2nd daily or nicotinamide | ↓ insulin dose at 3 and 6 m | Moderate size RCT. Low loss of subjects | Large age range |
| Gabbay | [65] | RCT. T1D < 6 m | 35 | 7–30 y | 25D 2000 IU daily vs. placebo | Basal D 65 nmol/L. 19% vs. 62% progression to low C-peptide | RCT (PC, DB) | ↑ basal HbA1c in D (9.2 vs. 7.7%). |
| Federico | [67] | 8 deficient people given D | 15 | 12 ± 0.9 y | 25D to achieve serum 25D > 125 nmol/L | Decreased immunoreactivity to GAD, IA2 and Pro-insulin. ↓ insulin dose with D. | Individual dosing to target 25D | Small n |
| Ataie-Jafari | [68] | Single-blind RCT. T1D < 8 w | 61 (7) | 8–15 y | Alfacalcidol 0.25 µg bd | No significant effects. Post hoc males ↓ insulin dose, ↑ C-peptide | Small age range. RCT | Assessed FCP Short duration |
| Bizzarri | [71] | RCT. T1D < 12 w FCP > 0.25 nmol/L | 34 (7) | 11–35 y | 0.25 µg 1,25D daily | 2 y follow-up. No effects. | RCT (PC, DB), long follow-up | Medium effect size due to dropout |
| Li | [70] | RCT, blinding unclear. LADA < 5 y FCP > 0.2 nmol/L | 35 | 38.5 D, 42.8 con | 1α(OH)vitamin D3 0.5 µg/d | FCP ↓ in controls (started ~50% higher), stable in D group. Similar FCP at end. | High compliance records (daily) | Small n Controls ↑ basal FCP |
| Napoli | [60] | RCT. T1D < 12 w | 27 | 22 y | 1,25D 0.25 µg/d | No significant effects | Controlled RCT | Small n |
| Sharma | [66] | RCT. Duration T1D 4.75 y and 4 y. | 52 | 9–9.5 y | 25D, 60,000 IU monthly | ↑ FCP with D, vs. ↓ in controls. No change in insulin or Hba1c. | Baseline values similar | Small n |
| Nwosu | [69] | RCT. T1D < 3 m | 36 | 10–21 y | Ergocalciferol (D2) 2 m of 50,000 IU/w | Slower rise in HbA1c. | RCT (PC, DB) Long follow-up | Single centre and small n |
| Walter | [72] | RCT | 40 | 18–39 y | 1,25D 0.25 µg/d | No differences, decline in both groups. | Low dropout rate | Small n |
| Mishra | [62] | Open label case–control | 30 | 6–12 y | 25D. 2000 IU/d | No significant differences. Trend to slower decline in D group. | Age-matched patients | Small n and relatively short term |
| Panjiyar | [73] | Open label case–control | 72 | 6–12 y | 25D. 3000 IU/d in 42 patients. 30 controls | Smaller decline in C-peptide, ↓ HbA1c | Sufficient n with long follow-up | Imbalanced control vs. treatment groups |
| Ludvig-sson | [63] | Open label | 20 | 12.4 | Calciferol 2000 IU/d + etanercept + GAD-alum | Higher C-peptide at 6 m. No obvious long-term benefits | Long follow-up | Small n |
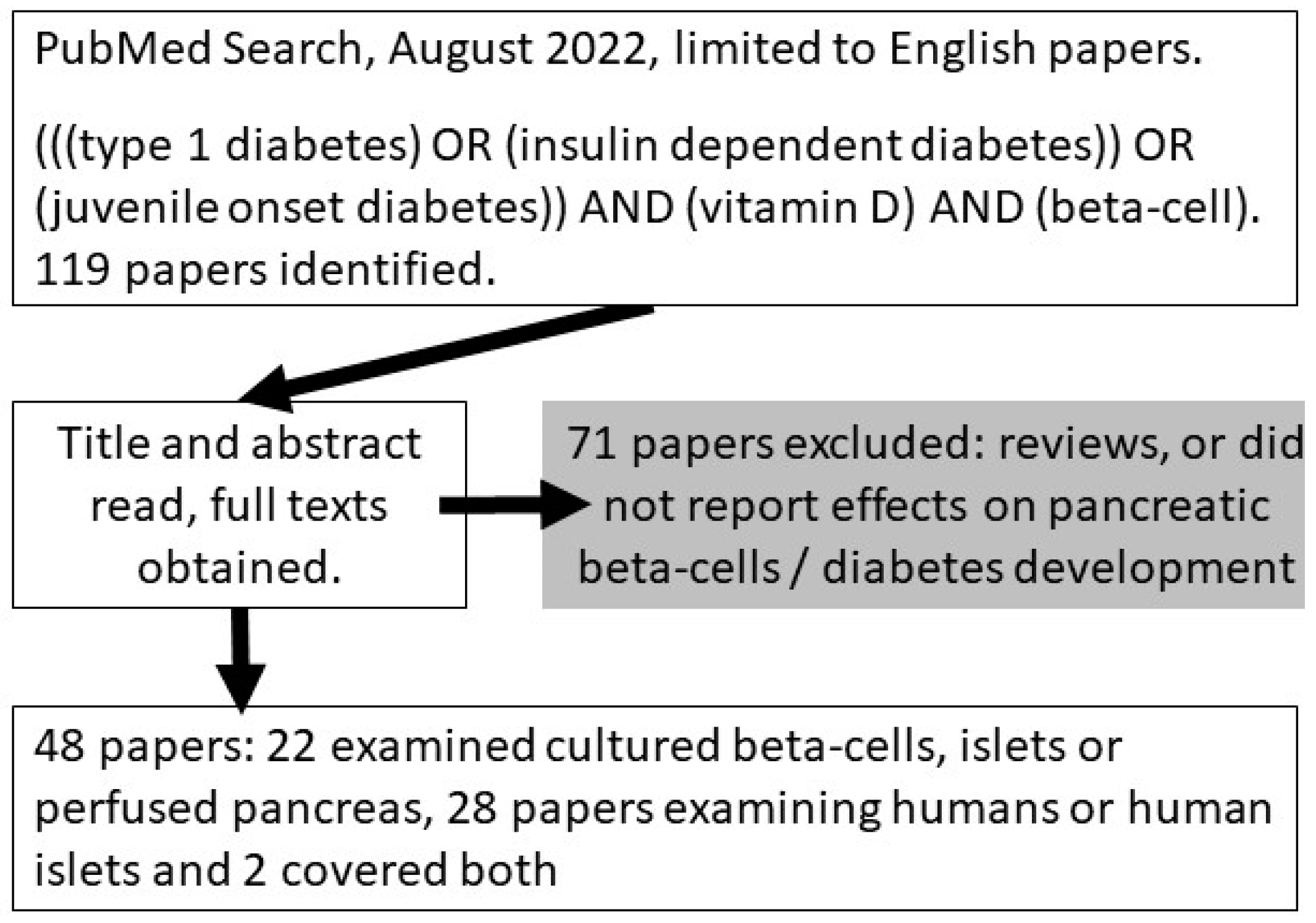
3. Methods and Materials
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 1,25D | 1,25(OH)2vitamin D |
| 25D | 25(OH)vitamin D |
| OR | Odds Ratio |
| PTH | Parathyroid hormone |
| IFNγ | Interferon gamma |
| IL-1β | Interleukin 1 beta |
| NOD | Non-obese diabetes |
| ROS | Reactive oxygen species |
| siRNA | small interfering RNA |
| T1D | Type 1 diabetes |
| TNFα | Tumor necrosis factor alpha |
| VDR | Vitamin D receptor |
References
- Soltesz, G.; Patterson, C.C.; Dahlquist, G. Worldwide childhood type 1 diabetes incidence—What can we learn from epidemiology? Pediatr. Diabetes 2007, 8 (Suppl. S6), 6–14. [Google Scholar] [CrossRef]
- Bikle, D.D.; Patzek, S.; Wang, Y. Physiologic and pathophysiologic roles of extra renal CYP27b1: Case report and review. Bone Rep. 2018, 8, 255–267. [Google Scholar] [CrossRef]
- Hewison, M. Vitamin D and the immune system: New perspectives on an old theme. Rheum. Dis. Clin. 2012, 38, 125–139. [Google Scholar] [CrossRef]
- Mathieu, C.; Badenhoop, K. Vitamin D and type 1 diabetes mellitus: State of the art. Trends Endocrinol. Metab. 2005, 16, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Takiishi, T.; Gysemans, C.; Bouillon, R.; Mathieu, C. Vitamin D and diabetes. Endocrinol. Metab. Clin. North Am. 2010, 39, 419–446. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.; Cooper, J.D.; Zeitels, L.; Smyth, D.J.; Yang, J.H.; Walker, N.M.; Hyppönen, E.; Dunger, D.B.; Ramos-Lopez, E.; Badenhoop, K. Association of the vitamin D metabolism gene CYP27B1 with type 1 diabetes. Diabetes 2007, 56, 2616–2621. [Google Scholar] [CrossRef]
- Pittas, A.G.; Dawson-Hughes, B. Vitamin D and diabetes. J. Steroid Biochem. Mol. Biol. 2010, 121, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Luong, K.; Nguyen, L.T.; Nguyen, D.N. The role of vitamin D in protecting type 1 diabetes mellitus. Diabetes Metab. Res. Rev. 2005, 21, 338–346. [Google Scholar] [CrossRef]
- Giulietti, A.; Gysemans, C.; Stoffels, K.; van Etten, E.; Decallonne, B.; Overbergh, L.; Bouillon, R.; Mathieu, C. Vitamin D deficiency in early life accelerates Type 1 diabetes in non-obese diabetic mice. Diabetologia 2004, 47, 451–462. [Google Scholar] [CrossRef]
- Storm, T.L.; Sorensen, O.H.; Lund, B.; Lund, B.; Christiansen, J.S.; Andersen, A.R.; Lumholtz, I.B.; Parving, H.H. Vitamin D metabolism in insulin-dependent diabetes mellitus. Metab. Bone Dis. Relat. Res. 1983, 5, 107–110. [Google Scholar] [CrossRef]
- Danescu, L.G.; Levy, S.; Levy, J. Vitamin D and diabetes mellitus. Endocrine 2009, 35, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-Y.; Leung, P.S.C.; Adamopoulos, I.E.; Gershwin, M.E. The Implication of Vitamin D and Autoimmunity: A Comprehensive Review. Clin. Rev. Allergy Immunol. 2013, 45, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Bener, A.; Alsaied, A.; Al-Ali, M.; Al-Kubaisi, A.; Basha, B.; Abraham, A.; Guiter, G.; Mian, M. High prevalence of vitamin D deficiency in type 1 diabetes mellitus and healthy children. Acta Diabetol. 2009, 46, 183–189. [Google Scholar] [CrossRef]
- Pozzilli, P.; Manfrini, S.; Crino, A.; Picardi, A.; Leomanni, C.; Cherubini, V.; Valente, L.; Khazrai, M.; Visalli, N. Low levels of 25-hydroxyvitamin D3 and 1,25-dihydroxyvitamin D3 in patients with newly diagnosed type 1 diabetes. Horm. Metab. Res. 2005, 37, 680–683. [Google Scholar] [CrossRef] [PubMed]
- Omar, D.F.; Kamal, M.M.; El-Hefnawy, M.H.; El-Mesallamy, H.O. Serum Vitamin D and Its Upregulated Protein, Thioredoxin Interacting Protein, Are Associated With Beta-Cell Dysfunction in Adult Patients With Type 1 and Type 2 Diabetes. Can. J. Diabetes 2018, 42, 588–594. [Google Scholar] [CrossRef]
- Littorin, B.; Blom, P.; Scholin, A.; Arnqvist, H.J.; Blohme, G.; Bolinder, J.; Ekbom-Schnell, A.; Eriksson, J.W.; Gudbjornsdottir, S.; Nystrom, L.; et al. Lower levels of plasma 25-hydroxyvitamin D among young adults at diagnosis of autoimmune type 1 diabetes compared with control subjects: Results from the nationwide Diabetes Incidence Study in Sweden (DISS). Diabetologia 2006, 49, 2847–2852. [Google Scholar] [CrossRef]
- Wei, Z.; Yoshihara, E.; He, N.; Hah, N.; Fan, W.; Pinto, A.F.M.; Huddy, T.; Wang, Y.; Ross, B.; Estepa, G.; et al. Vitamin D Switches BAF Complexes to Protect β Cells. Cell 2018, 173, 1135–1149. [Google Scholar] [CrossRef]
- Chen, C.; Luo, Y.; Su, Y.; Teng, L. The vitamin D receptor (VDR) protects pancreatic beta cells against Forkhead box class O1 (FOXO1)-induced mitochondrial dysfunction and cell apoptosis. Biomed. Pharmacother. 2019, 117, 109170. [Google Scholar] [CrossRef]
- Riachy, R.; Vandewalle, B.; Kerr Conte, J.; Moerman, E.; Sacchetti, P.; Lukowiak, B.; Gmyr, V.; Bouckenooghe, T.; Dubois, M.; Pattou, F. 1,25-dihydroxyvitamin D3 protects RINm5F and human islet cells against cytokine-induced apoptosis: Implication of the antiapoptotic protein A20. Endocrinology 2002, 143, 4809–4819. [Google Scholar] [CrossRef]
- Gysemans, C.A.; Cardozo, A.K.; Callewaert, H.; Giulietti, A.; Hulshagen, L.; Bouillon, R.; Eizirik, D.L.; Mathieu, C. 1,25-Dihydroxyvitamin D3 modulates expression of chemokines and cytokines in pancreatic islets: Implications for prevention of diabetes in nonobese diabetic mice. Endocrinology 2005, 146, 1956–1964. [Google Scholar] [CrossRef]
- Pepaj, M.; Gjerlaugsen, N.; Julien, K.; Thorsby, P.M. Tmem27 is upregulated by vitamin D in INS-1 cells and its serum concentrations are low in patients with autoimmune diabetes. Scand. J. Clin. Lab. Invest. 2014, 74, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Akpinar, P.; Kuwajima, S.; Krützfeldt, J.; Stoffel, M. Tmem27: A cleaved and shed plasma membrane protein that stimulates pancreatic beta cell proliferation. Cell Metab. 2005, 2, 385–397. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Hu, C.; Liu, J.; Wu, Z.; Duan, T.; Cao, Z. 1,25-(OH)2D3 protects pancreatic beta cells against H2O2-induced apoptosis through inhibiting the PERK-ATF4-CHOP pathway. Acta Biochim. Biophys. Sin. 2021, 53, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; He, D.; Ni, C.; Zhou, H.; Wu, S.; Xue, Z.; Zhou, Z. Vitamin D induces autophagy of pancreatic β-cells and enhances insulin secretion. Mol. Med. Rep. 2016, 14, 2644–2650. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Clark, S.A.; Gill, R.K.; Christakos, S. 1,25-Dihydroxyvitamin D3 and pancreatic beta-cell function: Vitamin D receptors, gene expression, and insulin secretion. Endocrinology 1994, 134, 1602–1610. [Google Scholar] [CrossRef]
- Girgis, C.M.; Clifton-Bligh, R.J.; Mokbel, N.; Cheng, K.; Gunton, J.E. Vitamin D signaling regulates proliferation, differentiation, and myotube size in C2C12 skeletal muscle cells. Endocrinology 2014, 155, 347–357. [Google Scholar] [CrossRef]
- Riachy, R.; Vandewalle, B.; Moerman, E.; Belaich, S.; Lukowiak, B.; Gmyr, V.; Muharram, G.; Kerr Conte, J.; Pattou, F. 1,25-Dihydroxyvitamin D3 protects human pancreatic islets against cytokine-induced apoptosis via down-regulation of the Fas receptor. Apoptosis 2006, 11, 151–159. [Google Scholar] [CrossRef]
- Sandler, S.; Buschard, K.; Bendtzen, K. Effects of 1,25-dihydroxyvitamin D3 and the analogues MC903 and KH1060 on interleukin-1 beta-induced inhibition of rat pancreatic islet beta-cell function in vitro. Immunol. Lett. 1994, 41, 73–77. [Google Scholar] [CrossRef]
- Mendes, A.K.B.; Sulis, P.M.; Cavalari, F.C.; Padilla, D.P.R.; Aragón, M.; Gaspar, J.M.; Silva, F. 1α,25-(OH)(2) vitamin D(3) prevents insulin resistance and regulates coordinated exocytosis and insulin secretion. J. Nutr. Biochem. 2022, 99, 108864. [Google Scholar] [CrossRef]
- Gregori, S.; Giarratana, N.; Smiroldo, S.; Uskokovic, M.; Adorini, L. A 1alpha,25-dihydroxyvitamin D(3) analog enhances regulatory T-cells and arrests autoimmune diabetes in NOD mice. Diabetes 2002, 51, 1367–1374. [Google Scholar] [CrossRef]
- van Etten, E.; Decallonne, B.; Mathieu, C. 1,25-dihydroxycholecalciferol: Endocrinology meets the immune system. Proc. Nutr. Soc. 2002, 61, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Kiekhaefer, C.M.; Weber, B.; Huggins, M.; Gorichanaz, C.; Nehring, J.A.; DeLuca, H.F. 2α-Methyl-19-nor-(20S)-1,25-dihydroxyvitamin D(3) protects the insulin 2 knockout non-obese diabetic mouse from developing type 1 diabetes without hypercalcaemia. Clin. Exp. Immunol. 2011, 166, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Baeke, F.; Van Belle, T.L.; Takiishi, T.; Ding, L.; Korf, H.; Laureys, J.; Gysemans, C.; Mathieu, C. Low doses of anti-CD3, ciclosporin A and the vitamin D analogue, TX527, synergise to delay recurrence of autoimmune diabetes in an islet-transplanted NOD mouse model of diabetes. Diabetologia 2012, 55, 2723–2732. [Google Scholar] [CrossRef] [PubMed]
- Lai, X.; Liu, X.; Cai, X.; Zou, F. Vitamin D supplementation induces CatG-mediated CD4(+) T cell inactivation and restores pancreatic β-cell function in mice with type 1 diabetes. Am. J. Physiol. Endocrinol. Metab. 2022, 322, E74–E84. [Google Scholar] [CrossRef]
- Morró, M.; Vilà, L.; Franckhauser, S.; Mallol, C.; Elias, G.; Ferré, T.; Molas, M.; Casana, E.; Rodó, J.; Pujol, A.; et al. Vitamin D Receptor Overexpression in β-Cells Ameliorates Diabetes in Mice. Diabetes 2020, 69, 927–939. [Google Scholar] [CrossRef]
- Sadek, K.M.; Shaheen, H. Biochemical efficacy of vitamin D in ameliorating endocrine and metabolic disorders in diabetic rats. Pharm. Biol. 2014, 52, 591–596. [Google Scholar] [CrossRef]
- Driver, J.P.; Lamont, D.J.; Gysemans, C.; Mathieu, C.; Serreze, D.V. Calcium insufficiency accelerates type 1 diabetes in vitamin D receptor-deficient nonobese diabetic (NOD) mice. Endocrinology 2011, 152, 4620–4629. [Google Scholar] [CrossRef]
- Girgis, C.M.; Cha, K.M.; Houweling, P.J.; Rao, R.; Mokbel, N.; Lin, M.; Clifton-Bligh, R.J.; Gunton, J.E. Vitamin D receptor ablation and vitamin D deficiency result in reduced grip strength, altered muscle fibers, and increased myostatin in mice. Calcif. Tissue Int. 2015, 97, 602–610. [Google Scholar] [CrossRef]
- Kadowaki, S.; Norman, A.W. Dietary vitamin D is essential for normal insulin secretion from the perfused rat pancreas. J. Clin. Invest. 1984, 73, 759–766. [Google Scholar] [CrossRef]
- Norman, A.W.; Frankel, B.J.; Helt, A.M.; Grodsky, G.M. Vitamin D deficiency inhibits pancreatic secretion of insulin. Science 1980, 209, 759–769. [Google Scholar] [CrossRef]
- Viloria, K.; Nasteska, D.; Briant, L.J.B.; Heising, S.; Larner, D.P.; Fine, N.H.F.; Ashford, F.B.; da Silva Xavier, G.; Ramos, M.J.; Hasib, A.; et al. Vitamin-D-Binding Protein Contributes to the Maintenance of α Cell Function and Glucagon Secretion. Cell Rep. 2020, 31, 107761. [Google Scholar] [CrossRef] [PubMed]
- Hawa, M.I.; Valorani, M.G.; Buckley, L.R.; Beales, P.E.; Afeltra, A.; Cacciapaglia, F.; Leslie, R.D.; Pozzilli, P. Lack of effect of vitamin D administration during pregnancy and early life on diabetes incidence in the non-obese diabetic mouse. Horm. Metab. Res. 2004, 36, 620–624. [Google Scholar] [CrossRef] [PubMed]
- Gysemans, C.; van Etten, E.; Overbergh, L.; Giulietti, A.; Eelen, G.; Waer, M.; Verstuyf, A.; Bouillon, R.; Mathieu, C. Unaltered diabetes presentation in NOD mice lacking the vitamin D receptor. Diabetes 2008, 57, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Li, W.; Liu, J.; Wu, W.; Ouyang, H.; Zhang, Q.; Wang, Y.; Liu, L.; Yang, R.; Liu, X.; et al. Polymorphisms in the vitamin D receptor gene and type 1 diabetes mellitus risk: An update by meta-analysis. Mol. Cell. Endocrinol. 2012, 355, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Rasoul, M.A.; Haider, M.Z.; Al-Mahdi, M.; Al-Kandari, H.; Dhaunsi, G.S. Relationship of four vitamin D receptor gene polymorphisms with type 1 diabetes mellitus susceptibility in Kuwaiti children. BMC Pediatr. 2019, 19, 71. [Google Scholar] [CrossRef] [PubMed]
- Mory, D.B.; Rocco, E.R.; Miranda, W.L.; Kasamatsu, T.; Crispim, F.; Dib, S.A. Prevalence of vitamin D receptor gene polymorphisms FokI and BsmI in Brazilian individuals with type 1 diabetes and their relation to beta-cell autoimmunity and to remaining beta-cell function. Hum. Immunol. 2009, 70, 447–451. [Google Scholar] [CrossRef]
- Bid, H.K.; Konwar, R.; Aggarwal, C.G.; Gautam, S.; Saxena, M.; Nayak, V.L.; Banerjee, M. Vitamin D receptor (FokI, BsmI and TaqI) gene polymorphisms and type 2 diabetes mellitus: A North Indian study. Indian J. Med. Sci. 2009, 63, 187–194. [Google Scholar]
- Habibian, N.; Amoli, M.M.; Abbasi, F.; Rabbani, A.; Alipour, A.; Sayarifard, F.; Rostami, P.; Dizaji, S.P.; Saadati, B.; Setoodeh, A. Role of vitamin D and vitamin D receptor gene polymorphisms on residual beta cell function in children with type 1 diabetes mellitus. Pharmacol. Rep. 2019, 71, 282–288. [Google Scholar] [CrossRef]
- Zipitis, C.S.; Akobeng, A.K. Vitamin D supplementation in early childhood and risk of type 1 diabetes: A systematic review and meta-analysis. Arch. Dis. Child. 2008, 93, 512. [Google Scholar] [CrossRef]
- Mayer-Davis, E.J.; Dabelea, D.; Crandell, J.L.; Crume, T.; D’Agostino, R.B., Jr.; Dolan, L.; King, I.B.; Lawrence, J.M.; Norris, J.M.; Pihoker, C.; et al. Nutritional factors and preservation of C-peptide in youth with recently diagnosed type 1 diabetes: SEARCH Nutrition Ancillary Study. Diabetes Care 2013, 36, 1842–1850. [Google Scholar] [CrossRef]
- Girgis, C.M.; Clifton-Bligh, R.J.; Turner, N.; Lau, S.L.; Gunton, J.E. Effects of Vitamin D in Skeletal Muscle: Falls, Strength, Athletic Performance and Insulin Sensitivity. Clin. Endocrinol. 2014, 80, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Harms, R.Z.; Ostlund, K.R.; Cabrera, M.S.; Edwards, E.; Fisher, M.; Sarvetnick, N. Confirmation and Identification of Biomarkers Implicating Environmental Triggers in the Pathogenesis of Type 1 Diabetes. Front. Immunol. 2020, 11, 1922. [Google Scholar] [CrossRef] [PubMed]
- Reinert-Hartwall, L.; Honkanen, J.; Härkönen, T.; Ilonen, J.; Simell, O.; Peet, A.; Tillmann, V.; Lamberg-Allardt, C.; Virtanen, S.M.; Knip, M.; et al. No association between vitamin D and β-cell autoimmunity in Finnish and Estonian children. Diabetes Metab. Res. Rev. 2014, 30, 749–760. [Google Scholar] [CrossRef] [PubMed]
- Knip, M.; Virtanen, S.M.; Akerblom, H.K. Infant feeding and the risk of type 1 diabetes. Am. J. Clin. Nutr. 2010, 91, 1506s–1513s. [Google Scholar] [CrossRef] [PubMed]
- Hyppönen, E.; Läärä, E.; Reunanen, A.; Järvelin, M.-R.; Virtanen, S.M. Intake of vitamin D and risk of type 1 diabetes: A birth-cohort study. Lancet 2001, 358, 1500–1503. [Google Scholar] [CrossRef]
- Fronczak, C.M.; Baron, A.E.; Chase, H.P.; Ross, C.; Brady, H.L.; Hoffman, M.; Eisenbarth, G.S.; Rewers, M.; Norris, J.M. In utero dietary exposures and risk of islet autoimmunity in children. Diabetes Care 2003, 26, 3237–3242. [Google Scholar] [CrossRef]
- Marjamäki, L.; Niinistö, S.; Kenward, M.G.; Uusitalo, L.; Uusitalo, U.; Ovaskainen, M.L.; Kronberg-Kippilä, C.; Simell, O.; Veijola, R.; Ilonen, J.; et al. Maternal intake of vitamin D during pregnancy and risk of advanced beta cell autoimmunity and type 1 diabetes in offspring. Diabetologia 2010, 53, 1599–1607. [Google Scholar] [CrossRef]
- Group, E.S.S. Vitamin D supplement in early childhood and risk for Type I (insulin-dependent) diabetes mellitus. Diabetologia 1999, 42, 51–54. [Google Scholar]
- Stene, L.C.; Joner, G.; Group, N.C.D.S. Use of cod liver oil during the first year of life is associated with lower risk of childhood-onset type 1 diabetes: A large, population-based, case-control study. Am. J. Clin. Nutr. 2003, 78, 1128–1134. [Google Scholar] [CrossRef]
- Napoli, N.; Strollo, R.; Pitocco, D.; Bizzarri, C.; Maddaloni, E.; Maggi, D.; Manfrini, S.; Schwartz, A.; Pozzilli, P. Effect of calcitriol on bone turnover and osteocalcin in recent-onset type 1 diabetes. PLoS ONE 2013, 8, e56488. [Google Scholar] [CrossRef]
- Baidal, D.A.; Ricordi, C.; Garcia-Contreras, M.; Sonnino, A.; Fabbri, A. Combination high-dose omega-3 fatty acids and high-dose cholecalciferol in new onset type 1 diabetes: A potential role in preservation of beta-cell mass. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 3313–3318. [Google Scholar] [PubMed]
- Mishra, A.; Dayal, D.; Sachdeva, N.; Attri, S.V. Effect of 6-months’ vitamin D supplementation on residual beta cell function in children with type 1 diabetes: A case control interventional study. J. Pediatr. Endocrinol. Metab. 2016, 29, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.; Routray, I.; Vigård, T.; Hanås, R.; Rathsman, B.; Carlsson, A.; Särnblad, S.; Albin, A.K.; Arvidsson, C.G.; Samuelsson, U.; et al. Combined Etanercept, GAD-alum and vitamin D treatment: An open pilot trial to preserve beta cell function in recent onset type 1 diabetes. Diabetes Metab. Res. Rev. 2021, 37, e3440. [Google Scholar] [CrossRef] [PubMed]
- Pitocco, D.; Crino, A.; Di Stasio, E.; Manfrini, S.; Guglielmi, C.; Spera, S.; Anguissola, G.B.; Visalli, N.; Suraci, C.; Matteoli, M.C.; et al. The effects of calcitriol and nicotinamide on residual pancreatic beta-cell function in patients with recent-onset Type 1 diabetes (IMDIAB XI). Diabet. Med. 2006, 23, 920–923. [Google Scholar] [CrossRef] [PubMed]
- Gabbay, M.A.; Sato, M.N.; Finazzo, C.; Duarte, A.J.; Dib, S.A. Effect of cholecalciferol as adjunctive therapy with insulin on protective immunologic profile and decline of residual β-cell function in new-onset type 1 diabetes mellitus. Arch. Pediatr. Adolesc. Med. 2012, 166, 601–607. [Google Scholar] [CrossRef]
- Sharma, S.; Biswal, N.; Bethou, A.; Rajappa, M.; Kumar, S.; Vinayagam, V. Does Vitamin D Supplementation Improve Glycaemic Control In Children With Type 1 Diabetes Mellitus?—A Randomized Controlled Trial. J. Clin. Diagn. Res. 2017, 11, SC15–SC17. [Google Scholar] [CrossRef] [PubMed]
- Federico, G.; Focosi, D.; Marchi, B.; Randazzo, E.; De Donno, M.; Vierucci, F.; Bugliani, M.; Campi, F.; Scatena, F.; Saggese, G.; et al. Administering 25-hydroxyvitamin D3 in vitamin D-deficient young type 1A diabetic patients reduces reactivity against islet autoantigens. Clin. Nutr. 2014, 33, 1153–1156. [Google Scholar] [CrossRef]
- Ataie-Jafari, A.; Loke, S.C.; Rahmat, A.B.; Larijani, B.; Abbasi, F.; Leow, M.K.; Yassin, Z. A randomized placebo-controlled trial of alphacalcidol on the preservation of beta cell function in children with recent onset type 1 diabetes. Clin. Nutr. 2013, 32, 911–917. [Google Scholar] [CrossRef]
- Nwosu, B.U.; Parajuli, S.; Jasmin, G.; Fleshman, J.; Sharma, R.B.; Alonso, L.C.; Lee, A.F.; Barton, B.A. Ergocalciferol in New-onset Type 1 Diabetes: A Randomized Controlled Trial. J. Endocr. Soc. 2022, 6, bvab179. [Google Scholar] [CrossRef]
- Li, X.; Liao, L.; Yan, X.; Huang, G.; Lin, J.; Lei, M.; Wang, X.; Zhou, Z. Protective effects of 1-alpha-hydroxyvitamin D3 on residual beta-cell function in patients with adult-onset latent autoimmune diabetes (LADA). Diabetes Metab. Res. Rev. 2009, 25, 411–416. [Google Scholar] [CrossRef]
- Bizzarri, C.; Pitocco, D.; Napoli, N.; Di Stasio, E.; Maggi, D.; Manfrini, S.; Suraci, C.; Cavallo, M.G.; Cappa, M.; Ghirlanda, G.; et al. No protective effect of calcitriol on beta-cell function in recent-onset type 1 diabetes: The IMDIAB XIII trial. Diabetes Care 2010, 33, 1962–1963. [Google Scholar] [CrossRef]
- Walter, M.; Kaupper, T.; Adler, K.; Foersch, J.; Bonifacio, E.; Ziegler, A.G. No effect of the 1alpha,25-dihydroxyvitamin D3 on beta-cell residual function and insulin requirement in adults with new-onset type 1 diabetes. Diabetes Care 2010, 33, 1443–1448. [Google Scholar] [CrossRef] [PubMed]
- Panjiyar, R.P.; Dayal, D.; Attri, S.V.; Sachdeva, N.; Sharma, R.; Bhalla, A.K. Sustained serum 25-hydroxyvitamin D concentrations for one year with cholecalciferol supplementation improves glycaemic control and slows the decline of residual β cell function in children with type 1 diabetes. Pediatr. Endocrinol. Diabetes Metab. 2018, 2018, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Dantas, J.R.; Araújo, D.B.; Silva, K.R.; Souto, D.L.; de Fátima Carvalho Pereira, M.; Luiz, R.R.; Dos Santos Mantuano, M.; Claudio-da-Silva, C.; Gabbay, M.A.L.; Dib, S.A.; et al. Adipose tissue-derived stromal/stem cells + cholecalciferol: A pilot study in recent-onset type 1 diabetes patients. Arch. Endocrinol. Metab. 2021, 65, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Thorsen, S.U.; Pipper, C.B.; Johannesen, J.; Mortensen, H.B.; Pociot, F.; Svensson, J. ‘25-Hydroxyvitamin D, Autoantigenic and Total Antibody Concentrations: Results from a Danish Case-control Study of Newly Diagnosed Patients with Childhood Type 1 Diabetes and their Healthy Siblings’. Scand. J. Immunol. 2018, 87, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Kodama, K.; Zhao, Z.; Toda, K.; Yip, L.; Fuhlbrigge, R.; Miao, D.; Fathman, C.G.; Yamada, S.; Butte, A.J.; Yu, L. Expression-Based Genome-Wide Association Study Links Vitamin D-Binding Protein With Autoantigenicity in Type 1 Diabetes. Diabetes 2016, 65, 1341–1349. [Google Scholar] [CrossRef]
- Hou, Y.; Song, A.; Jin, Y.; Xia, Q.; Song, G.; Xing, X. A dose-response meta-analysis between serum concentration of 25-hydroxy vitamin D and risk of type 1 diabetes mellitus. Eur. J. Clin. Nutr. 2021, 75, 1010–1023. [Google Scholar] [CrossRef]
- Dong, J.Y.; Zhang, W.G.; Chen, J.J.; Zhang, Z.L.; Han, S.F.; Qin, L.Q. Vitamin D intake and risk of type 1 diabetes: A meta-analysis of observational studies. Nutrients 2013, 5, 3551–3562. [Google Scholar] [CrossRef]
| Model | Treatments | Primary Outcomes |
|---|---|---|
| Cell/Cell Culture Studies | ||
| β-cell lines | 1,25D | Improved maintenance of normal cell function with cytokines [19] Increased β-cell proliferation [22] Reduced ER stress and apoptosis in the presence of H2O2 [23] Effects on cell survival unclear: pro-survival [19,24], no effect [20] |
| Isolated rat β-cells | 1,25D | Reduced cytokine overexpression, no change cellular apoptosis when treated with cytokines [20] Improved islet insulin release [28] |
| Human islets | 1,25D | Reduced apoptosis [19,27] |
| Human IPS β-like cells | Calcipotriol | Reduced apoptosis in presence of IL-1β [17] |
| Animal Studies | ||
| NOD mice | Analogues | Improved β-cell survival and decreased insulitis [30] Reduced incidence of T1D and improved pancreatic insulin [20,31,32] Decreased progression to T1D (mice lacking Ins2 gene) [32] Improved efficacy of islet transplants and delayed recurrence of autoimmune diabetes [33] |
| 1,25D | Reduced incidence of T1D and improved pancreatic insulin [31] | |
| VDR mice | Transgenic | Preservation of β-cell mass following STZ [35] |
| Null | Develop hypocalcaemia and β-cell dysfunction [37] which is ameliorated by rescue diet (high calcium, lactulose, phosphate) [38] | |
| C57Bl/6 mice | 1,25D | Improved blood glucose and serum insulin when treated with low-dose STZ [24] |
| Diabetic Wistar rats | Vitamin D | Improved β-cell function and HbA1c [36] |
| Human Studies | ||
| Early life | Supplementation with vitamin D | Reduced risk of T1D development intake of vitamin D and risk of type 1 diabetes: a birth-cohort study [55,59] Conflicting evidence regarding increased maternal vitamin D intake (pro No effect of the 1alpha,25-dihydroxyvitamin D3 on beta-cell residual function and insulin requirement in adults vs. no effect [58] |
| Recent onset T1D | 25D | Beneficial effects on C-peptide levels over time (trend to slower decrease in C-peptide [62], if not elevated C-peptide levels [66] |
| Analogues | Lower insulin dose and enhanced C-peptide (boys only) [68] | |
| Recent onset T1D | 1,25D | Lower insulin requirements at 3 and 6 months [64] |
| 25D | Enhanced/higher C-peptide levels [65,73,74] Lower insulin requirements [67] Improved HbA1c [73] | |
| Analogues | Slower decline in HbA1c levels over time [69] | |
| Human Studies (Negative/Null Findings) | ||
| Recent onset T1D | Combined Rx + D | Study in children. No beneficial effects [63] |
| Recent onset T1D | 1,25D | No effects on β-cell function [60,71,72] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, J.; Sharma, P.; Girgis, C.M.; Gunton, J.E. Vitamin D and Beta Cells in Type 1 Diabetes: A Systematic Review. Int. J. Mol. Sci. 2022, 23, 14434. https://doi.org/10.3390/ijms232214434
Yu J, Sharma P, Girgis CM, Gunton JE. Vitamin D and Beta Cells in Type 1 Diabetes: A Systematic Review. International Journal of Molecular Sciences. 2022; 23(22):14434. https://doi.org/10.3390/ijms232214434
Chicago/Turabian StyleYu, Josephine, Preeti Sharma, Christian M. Girgis, and Jenny E. Gunton. 2022. "Vitamin D and Beta Cells in Type 1 Diabetes: A Systematic Review" International Journal of Molecular Sciences 23, no. 22: 14434. https://doi.org/10.3390/ijms232214434
APA StyleYu, J., Sharma, P., Girgis, C. M., & Gunton, J. E. (2022). Vitamin D and Beta Cells in Type 1 Diabetes: A Systematic Review. International Journal of Molecular Sciences, 23(22), 14434. https://doi.org/10.3390/ijms232214434







