Brucella BtpB Manipulates Apoptosis and Autophagic Flux in RAW264.7 Cells
Abstract
1. Introduction
2. Results
2.1. Brucella BtpB Induces Apoptosis in RAW264.7
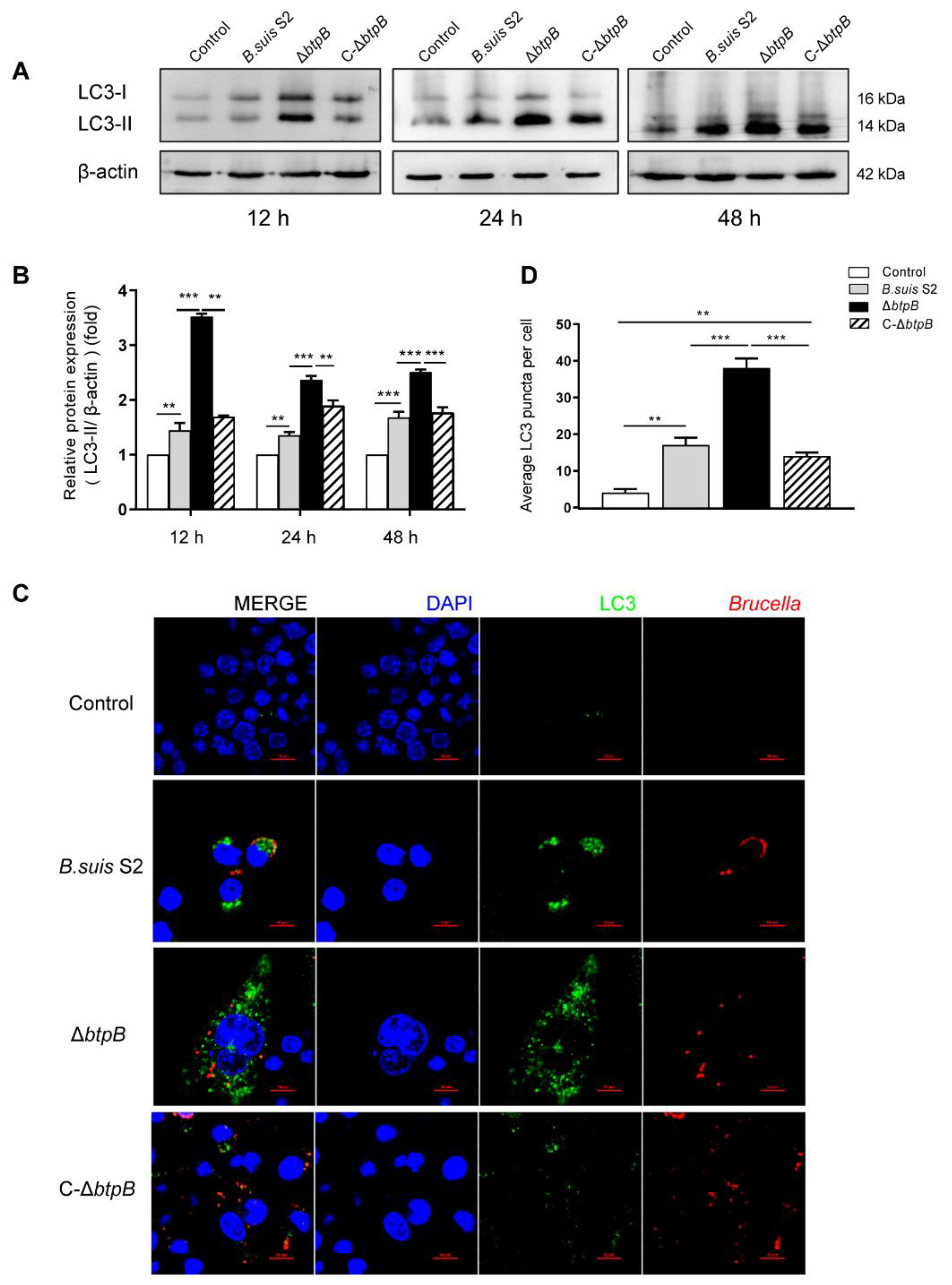
2.2. Mutant Strain ΔbtpB Infection Increases Autophagic Marker, LC3-II
2.3. Mutant Strain ΔbtpB Infection Decreases Autophagic Marker, P62
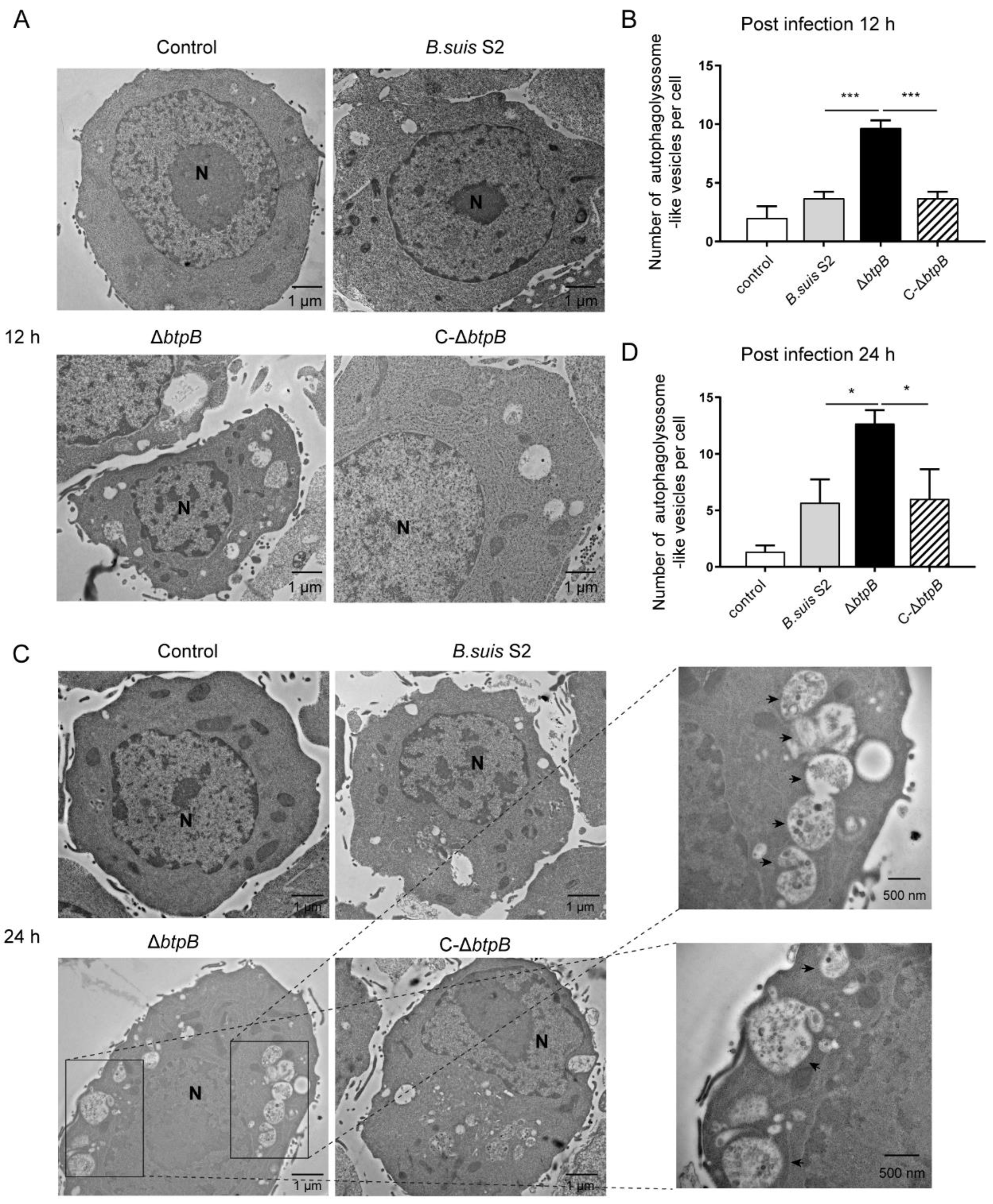
2.4. Mutant Strain ΔbtpB Induces the Accumulation of Autophagolysosomes in RAW264.7
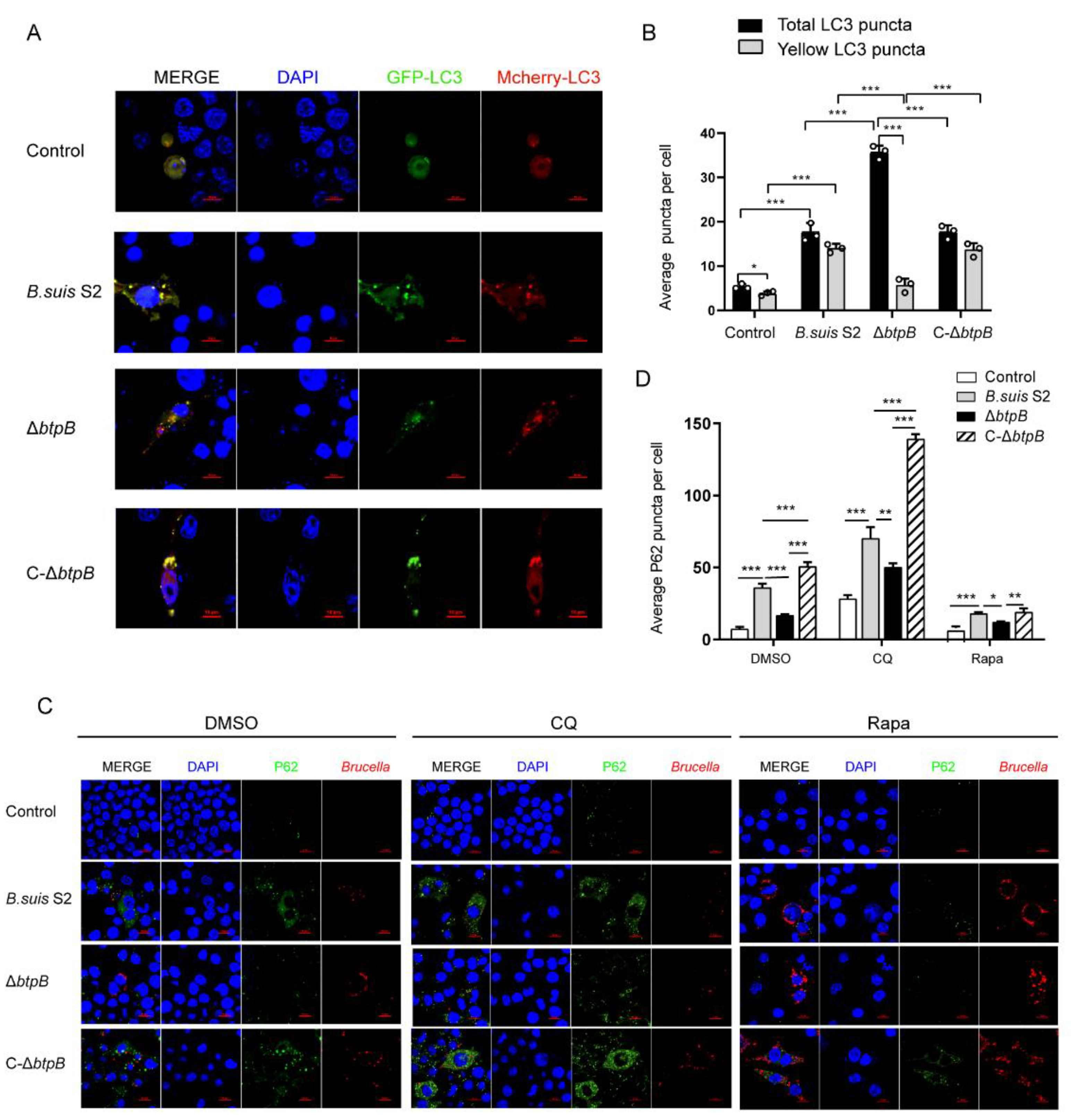
2.5. BtpB Blocks Autophagic Flux during Brucella Infection
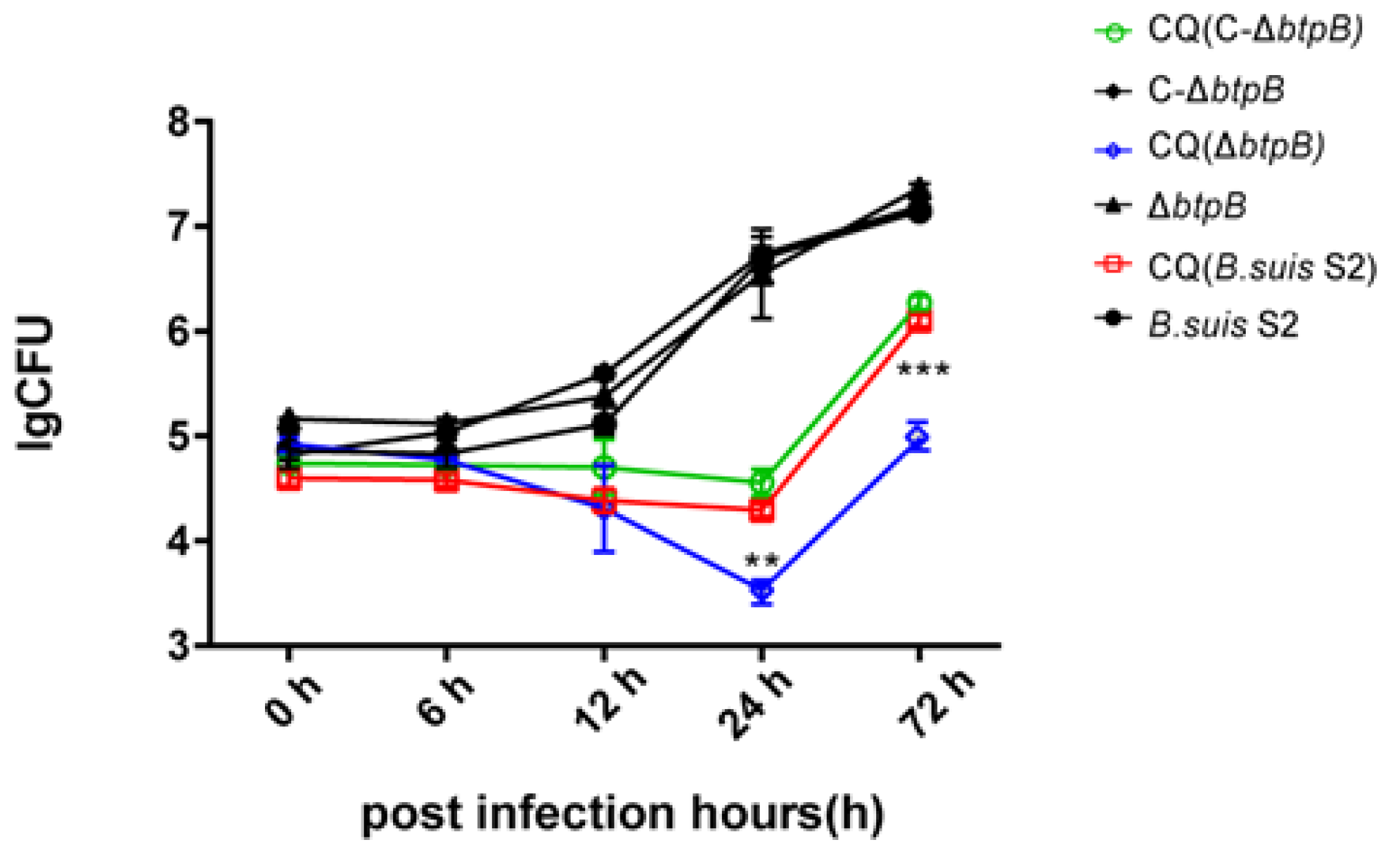
2.6. Autophagy Inhibition Decreases Brucella Replication
3. Discussion
4. Materials and Methods
4.1. Bacterial Strains and Mammalian Cells
4.2. DNA Constructs
4.3. Transfection
4.4. Macrophage Infection Assay
4.5. Transmission Electron Microscopy (TEM)
4.6. CFU Counting of Infected RAW264.7 Macrophages
4.7. TUNEL Apoptosis Assay
4.8. Flow Cytometry Analysis
4.9. Western Blotting
4.10. Immunofluorescence
4.11. GFP-mCherry-LC3 Assay
4.12. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhu, L.; Feng, Y.; Zhang, G.; Jiang, H.; Zhang, Z.; Wang, N.; Ding, J.; Suo, X. Brucella suis strain 2 vaccine is safe and protective against heterologous Brucella spp. infections. Vaccine 2016, 34, 395–400. [Google Scholar] [CrossRef]
- Atluri, V.L.; Xavier, M.N.; de Jong, M.F.; den Hartigh, A.B.; Tsolis, R.M. Interactions of the human pathogenic Brucella species with their hosts. Annu. Rev. Microbiol. 2011, 65, 523–541. [Google Scholar] [CrossRef] [PubMed]
- Katsiolis, A.; Papadopoulos, D.K.; Giantsis, I.A.; Papageorgiou, K.; Zdragas, A.; Giadinis, N.D.; Petridou, E. Brucella spp. distribution, hosting ruminants from Greece, applying various molecular identification techniques. BMC Vet. Res. 2022, 18, 202. [Google Scholar] [CrossRef] [PubMed]
- Glowacka, P.; Zakowska, D.; Naylor, K.; Niemcewicz, M.; Bielawska-Drozd, A. Brucella—Virulence Factors, Pathogenesis and Treatment. Pol. J. Microbiol. 2018, 67, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Celli, J. The Intracellular Life Cycle of Brucella spp. Microbiol. Spectr. 2019, 7, 101–111. [Google Scholar] [CrossRef]
- De Bolle, X.; Crosson, S.; Matroule, J.Y.; Letesson, J.J. Brucella abortus Cell Cycle and Infection Are Coordinated. Trends Microbiol. 2015, 23, 812–821. [Google Scholar] [CrossRef]
- Jiao, H.; Zhou, Z.; Li, B.; Xiao, Y.; Li, M.; Zeng, H.; Guo, X.; Gu, G. The Mechanism of Facultative Intracellular Parasitism of Brucella. Int. J. Mol. Sci. 2021, 22, 3673. [Google Scholar] [CrossRef]
- Starr, T.; Child, R.; Wehrly, T.D.; Hansen, B.; Hwang, S.; Lopez-Otin, C.; Virgin, H.W.; Celli, J. Selective subversion of autophagy complexes facilitates completion of the Brucella intracellular cycle. Cell Host Microbe 2012, 11, 33–45. [Google Scholar] [CrossRef]
- Ke, Y.; Wang, Y.; Li, W.; Chen, Z. Type IV secretion system of Brucella spp. and its effectors. Front. Cell. Infect. Microbiol. 2015, 5, 72. [Google Scholar] [CrossRef]
- Miller, C.N.; Smith, E.P.; Cundiff, J.A.; Knodler, L.A.; Bailey Blackburn, J.; Lupashin, V.; Celli, J. A Brucella Type IV Effector Targets the COG Tethering Complex to Remodel Host Secretory Traffic and Promote Intracellular Replication. Cell Host Microbe 2017, 22, 317–329.e7. [Google Scholar] [CrossRef]
- Hielpos, M.S.; Ferrero, M.C.; Fernandez, A.G.; Falivene, J.; Vanzulli, S.; Comerci, D.J.; Baldi, P.C. Btp Proteins from Brucella abortus Modulate the Lung Innate Immune Response to Infection by the Respiratory Route. Front. Immunol. 2017, 8, 1011. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, G.; Zhi, F.; Zhai, Y.; Zhou, D.; Chen, H.; Lin, P.; Tang, K.; Liu, W.; Jin, Y.; et al. BtpB inhibits innate inflammatory responses in goat alveolar macrophages through the TLR/NF-kappaB pathway and NLRP3 inflammasome during Brucella infection. Microb. Pathog. 2022, 166, 105536. [Google Scholar] [CrossRef] [PubMed]
- Salcedo, S.P.; Marchesini, M.I.; Degos, C.; Terwagne, M.; Von Bargen, K.; Lepidi, H.; Herrmann, C.K.; Santos Lacerda, T.L.; Imbert, P.R.; Pierre, P.; et al. BtpB, a novel Brucella TIR-containing effector protein with immune modulatory functions. Front. Cell. Infect. Microbiol. 2013, 3, 28. [Google Scholar] [CrossRef] [PubMed]
- Deretic, V. Autophagy in inflammation, infection, and immunometabolism. Immunity 2021, 54, 437–453. [Google Scholar] [CrossRef]
- Glick, D.; Barth, S.; Macleod, K.F. Autophagy: Cellular and molecular mechanisms. J. Pathol. 2010, 221, 3–12. [Google Scholar] [CrossRef]
- Huang, J.; Brumell, J.H. Bacteria-autophagy interplay: A battle for survival. Nat. Rev. Microbiol. 2014, 12, 101–114. [Google Scholar] [CrossRef]
- Klionsky, D.J.; Abdelmohsen, K.; Abe, A.; Abedin, M.J.; Abeliovich, H.; Acevedo Arozena, A.; Adachi, H.; Adams, C.M.; Adams, P.D.; Adeli, K.; et al. Guidelines for the use and interpretation of assays for monitoring autophagy (3rd edition). Autophagy 2016, 12, 1–222. [Google Scholar] [CrossRef]
- Zheng, L.; Wei, F.; Li, G. The crosstalk between bacteria and host autophagy: Host defense or bacteria offense. J. Microbiol. 2022, 60, 451–460. [Google Scholar] [CrossRef]
- McEwan, D.G. Host-pathogen interactions and subversion of autophagy. Essays Biochem. 2017, 61, 687–697. [Google Scholar] [CrossRef]
- Jiao, Y.; Zhang, Y.G.; Lin, Z.; Lu, R.; Xia, Y.; Meng, C.; Pan, Z.; Xu, X.; Jiao, X.; Sun, J. Salmonella Enteritidis Effector AvrA Suppresses Autophagy by Reducing Beclin-1 Protein. Front. Immunol. 2020, 11, 686. [Google Scholar] [CrossRef]
- Siadous, F.A.; Cantet, F.; Van Schaik, E.; Burette, M.; Allombert, J.; Lakhani, A.; Bonaventure, B.; Goujon, C.; Samuel, J.; Bonazzi, M.; et al. Coxiella effector protein CvpF subverts RAB26-dependent autophagy to promote vacuole biogenesis and virulence. Autophagy 2021, 17, 706–722. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; He, J.; Wang, Y.; Yang, Q.; Yi, J.; Zhang, H.; Wang, Y.; Miao, Y.; Wang, Z.; Chen, C. Deletion of the type IV secretion system promoter VirB in Brucella abortus A19 strain attenuated the virulence of the bacteria and promotes autophagy. Can. J. Microbiol. 2022, 68, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Li, M.; Li, Z.; Shi, J.; Zhang, Y.; Deng, X.; Liu, L.; Wang, Z.; Qi, Y.; Zhang, H. Deletion of the Type IV Secretion System Effector VceA Promotes Autophagy and Inhibits Apoptosis in Brucella-Infected Human Trophoblast Cells. Curr. Microbiol. 2019, 76, 510–519. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, G.; Wang, Y.; Liu, Q.; Li, H.; Xie, P.; Wang, Z. Omp31 of Brucella Inhibits NF-kappaB p65 Signaling Pathway by Inducing Autophagy in BV-2 Microglia. Neurochem. Res. 2021, 46, 3264–3272. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Yu, S.Y.; Ning, X.N.; Fang, H.; Li, J.; Zhi, F.J.; Li, J.M.; Zhou, D.; Wang, A.H.; Jin, Y.P. A LysR Transcriptional Regulator Manipulates Macrophage Autophagy Flux During Brucella Infection. Front. Cell. Infect. Microbiol. 2022, 12, 2958. [Google Scholar] [CrossRef] [PubMed]
- Zhi, F.; Zhou, D.; Bai, F.; Li, J.; Xiang, C.; Zhang, G.; Jin, Y.; Wang, A. VceC Mediated IRE1 Pathway and Inhibited CHOP-induced Apoptosis to Support Brucella Replication in Goat Trophoblast Cells. Int. J. Mol. Sci. 2019, 20, 1404. [Google Scholar] [CrossRef] [PubMed]
- Elbialy, A. In vivo autophagy quantification: Measuring LC3 and P62 puncta in 3D image system from zebrafish larvae. J. Cell. Biochem. 2021, 122, 1435–1444. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.J.; Chen, S.; Huang, K.X.; Le, W.D. Why should autophagic flux be assessed? Acta Pharmacol. Sin. 2013, 34, 595–599. [Google Scholar] [CrossRef]
- Spera, J.M.; Ugalde, J.E.; Mucci, J.; Comerci, D.J.; Ugalde, R.A. A B lymphocyte mitogen is a Brucella abortus virulence factor required for persistent infection. Proc. Natl. Acad. Sci. USA 2006, 103, 16514–16519. [Google Scholar] [CrossRef]
- Gonzalez-Rivera, C.; Bhatty, M.; Christie, P.J. Mechanism and Function of Type IV Secretion During Infection of the Human Host. Microbiol. Spectr. 2016, 4, 265–303. [Google Scholar] [CrossRef]
- Weber, M.M.; Faris, R. Subversion of the Endocytic and Secretory Pathways by Bacterial Effector Proteins. Front. Cell Dev. Biol. 2018, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Lal, N.K.; Thanasuwat, B.; Chan, B.; Dinesh-Kumar, S.P. Pathogens manipulate host autophagy through injected effector proteins. Autophagy 2020, 16, 2301–2302. [Google Scholar] [CrossRef] [PubMed]
- de Figueiredo, P.; Ficht, T.A.; Rice-Ficht, A.; Rossetti, C.A.; Adams, L.G. Pathogenesis and immunobiology of brucellosis: Review of Brucella-host interactions. Am. J. Pathol. 2015, 185, 1505–1517. [Google Scholar] [CrossRef]
- Ahmed, W.; Zheng, K.; Liu, Z.F. Establishment of Chronic Infection: Brucella’s Stealth Strategy. Front. Cell. Infect. Microbiol. 2016, 6, 30. [Google Scholar] [CrossRef]
- Pei, J.; Kahl-McDonagh, M.; Ficht, T.A. Brucella dissociation is essential for macrophage egress and bacterial dissemination. Front. Cell. Infect. Microbiol. 2014, 4, 23. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Chen, Y.; Tooze, S.A. Autophagy pathway: Cellular and molecular mechanisms. Autophagy 2018, 14, 207–215. [Google Scholar] [CrossRef]
- Feng, Y.; He, D.; Yao, Z.; Klionsky, D.J. The machinery of macroautophagy. Cell Res. 2014, 24, 24–41. [Google Scholar] [CrossRef]
- Leong, J.X.; Raffeiner, M.; Spinti, D.; Langin, G.; Franz-Wachtel, M.; Guzman, A.R.; Kim, J.G.; Pandey, P.; Minina, A.E.; Macek, B.; et al. A bacterial effector counteracts host autophagy by promoting degradation of an autophagy component. EMBO J. 2022, 41, e110352. [Google Scholar] [CrossRef]
- Shahnazari, S.; Brumell, J.H. Mechanisms and consequences of bacterial targeting by the autophagy pathway. Curr. Opin. Microbiol. 2011, 14, 68–75. [Google Scholar] [CrossRef]
- Feng, Z.Z.; Jiang, A.J.; Mao, A.W.; Feng, Y.; Wang, W.; Li, J.; Zhang, X.; Xing, K.; Peng, X. The Salmonella effectors SseF and SseG inhibit Rab1A-mediated autophagy to facilitate intracellular bacterial survival and replication. J. Biol. Chem. 2018, 293, 9662–9673. [Google Scholar] [CrossRef]
- Ge, P.P.; Lei, Z.H.; Yu, Y.; Lu, Z.; Qiang, L.H.; Chai, Q.Y.; Zhang, Y.; Zhao, D.D.; Li, B.X.; Pang, Y.; et al. M. tuberculosis PknG manipulates host autophagy flux to promote pathogen intracellular survival. Autophagy 2022, 18, 576–594. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.; Celli, J. Avoidance and Subversion of Eukaryotic Homeostatic Autophagy Mechanisms by Bacterial Pathogens. J. Mol. Biol. 2016, 428, 3387–3398. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.G.; Codogno, P.; Zhang, H. Machinery, regulation and pathophysiological implications of autophagosome maturation. Nat. Rev. Mol. Cell Biol. 2021, 22, 733–750. [Google Scholar] [CrossRef] [PubMed]


| Primers | Sequences (5′-3′) |
|---|---|
| BtpB F | GGTACCGCGGGCCCGGGATCCATGTACAATTTATTTGTTTCG (BamH I) |
| BtpB R | TTATCTAGATCCGGTGGATCCCTAGGTGATGAGGGCGACGCGCTC (BamH I) |
| mCherry F | GTACCGCGGGCCCGGGATCCATGGTGAGCAAGGGC (BamH I) |
| mCherry R | cttctcggacggcatCTTGTACAGCTCGTC |
| LC3B F | GACGAGCTGTACAAGatgccgtccgagaag |
| LC3B R | TATCTAGATCCGGTGGATCCttacacagccattgct (BamH I) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, J.; Qi, L.; Diao, Z.; Zhang, M.; Li, B.; Zhai, Y.; Hao, M.; Zhou, D.; Liu, W.; Jin, Y.; et al. Brucella BtpB Manipulates Apoptosis and Autophagic Flux in RAW264.7 Cells. Int. J. Mol. Sci. 2022, 23, 14439. https://doi.org/10.3390/ijms232214439
Li J, Qi L, Diao Z, Zhang M, Li B, Zhai Y, Hao M, Zhou D, Liu W, Jin Y, et al. Brucella BtpB Manipulates Apoptosis and Autophagic Flux in RAW264.7 Cells. International Journal of Molecular Sciences. 2022; 23(22):14439. https://doi.org/10.3390/ijms232214439
Chicago/Turabian StyleLi, Junmei, Lin Qi, Ziyang Diao, Mengyu Zhang, Bin Li, Yunyi Zhai, Mingyue Hao, Dong Zhou, Wei Liu, Yaping Jin, and et al. 2022. "Brucella BtpB Manipulates Apoptosis and Autophagic Flux in RAW264.7 Cells" International Journal of Molecular Sciences 23, no. 22: 14439. https://doi.org/10.3390/ijms232214439
APA StyleLi, J., Qi, L., Diao, Z., Zhang, M., Li, B., Zhai, Y., Hao, M., Zhou, D., Liu, W., Jin, Y., & Wang, A. (2022). Brucella BtpB Manipulates Apoptosis and Autophagic Flux in RAW264.7 Cells. International Journal of Molecular Sciences, 23(22), 14439. https://doi.org/10.3390/ijms232214439






