Efficacy and Renal Safety of Prophylactic Tenofovir Alafenamide for HBV-Infected Cancer Patients Undergoing Chemotherapy
Abstract
1. Introduction
2. Results
2.1. Patient Characteristics
2.2. Antiviral Efficacy and Incidence of Renal Events at One-Year Follow-Up
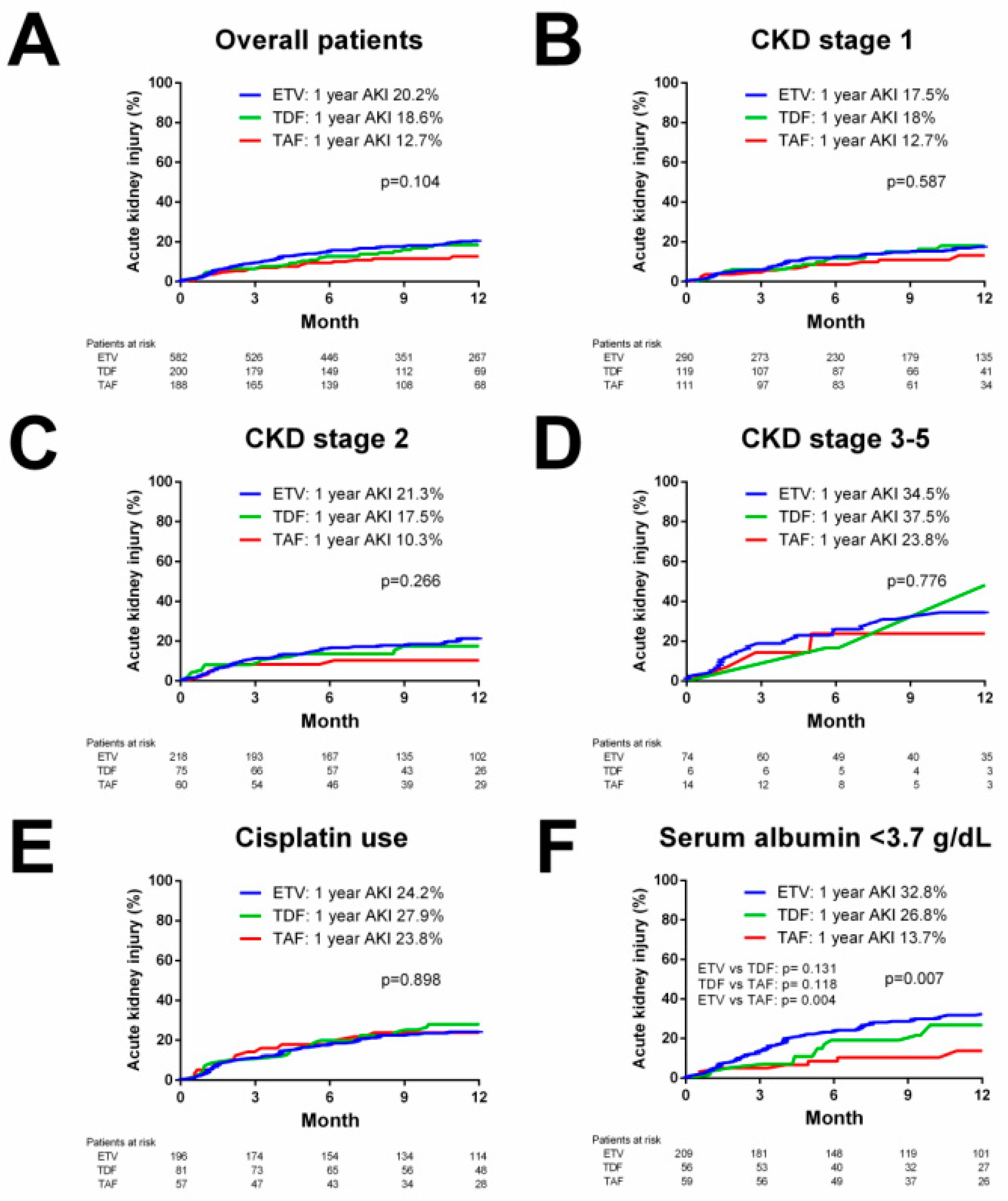
2.3. Survival Analysis for the Cumulative Incidence of Acute Kidney Injury (AKI)
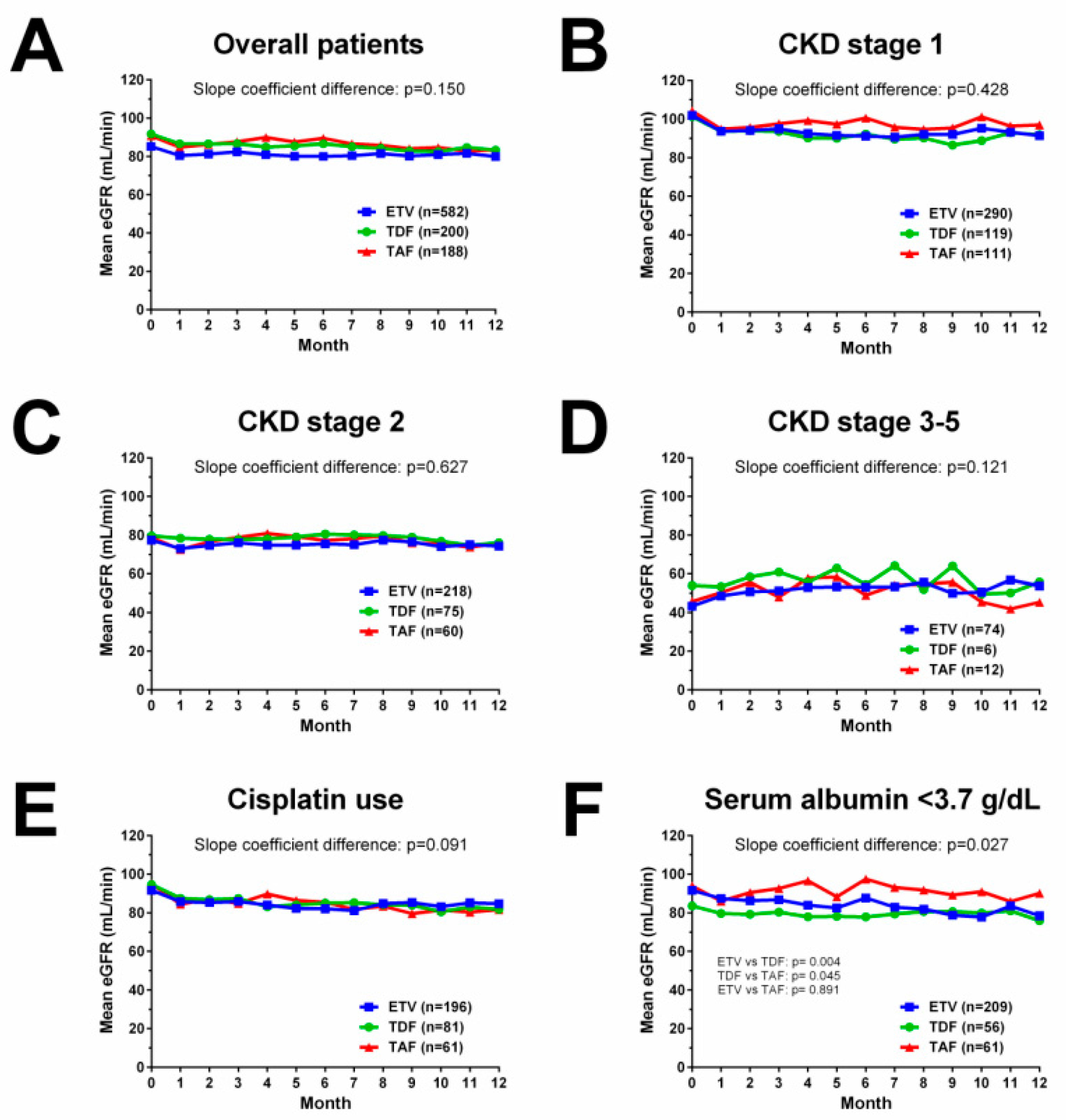
2.4. Dynamic Change in eGFR over One Year
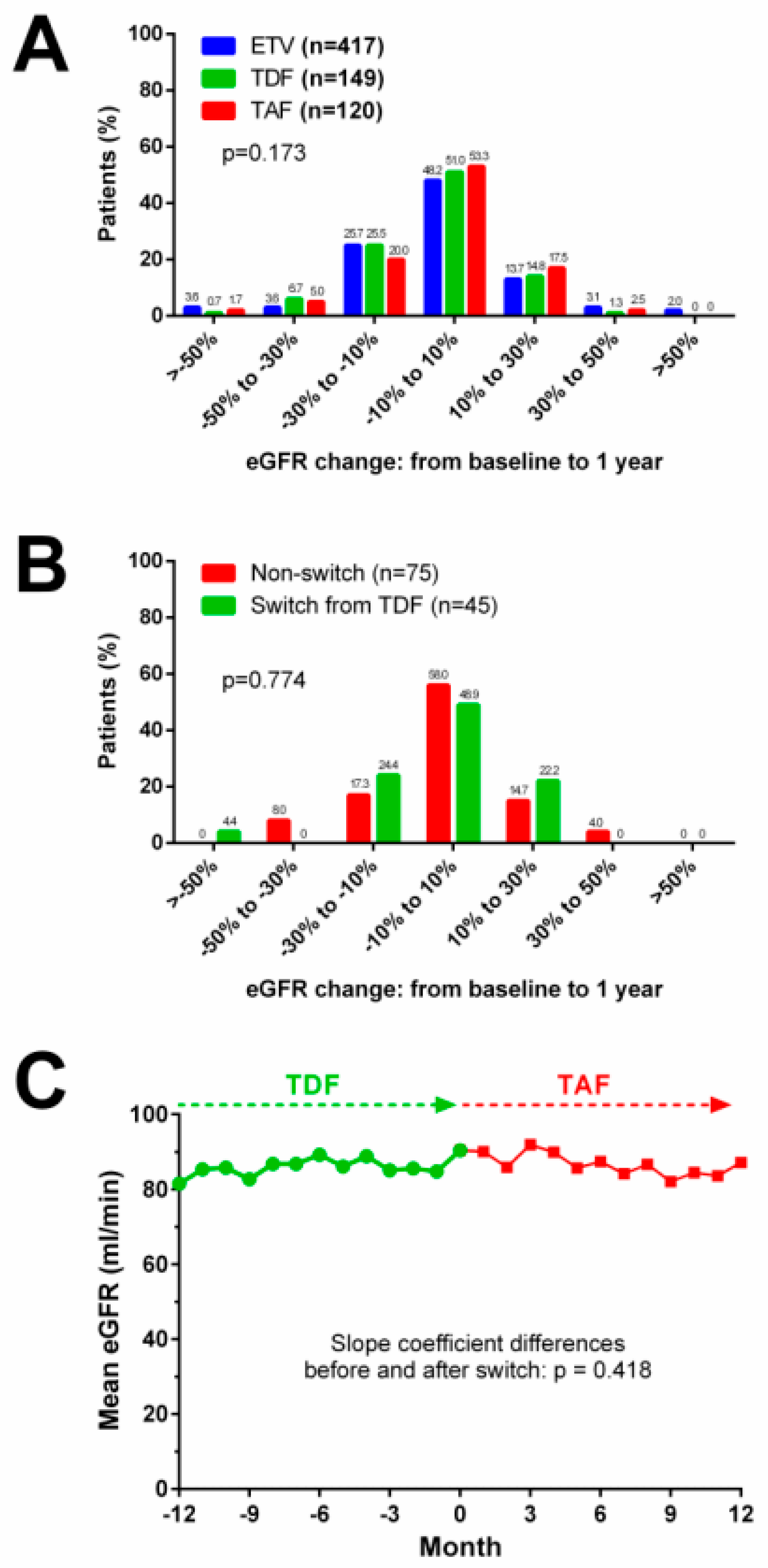
2.5. Renal Events in TAF-Treated Patients with and without Switching from TDF
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Biochemistry and Virological Tests
4.3. Outcomes
4.4. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Schweitzer, A.; Horn, J.; Mikolajczyk, R.T.; Krause, G.; Ott, J.J. Estimations of worldwide prevalence of chronic hepatitis B virus infection: A systematic review of data published between 1965 and 2013. Lancet 2015, 386, 1546–1555. [Google Scholar] [CrossRef]
- Hwang, J.; Lok, A.S.-F. Management of patients with hepatitis B who require immunosuppressive therapy. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-H.; Hsiao, L.-T.; Hong, Y.-C.; Chiou, T.-J.; Yu, Y.-B.; Gau, J.-P.; Liu, C.-Y.; Yang, M.-H.; Tzeng, C.-H.; Lee, P.-C.; et al. Randomized controlled trial of entecavir prophylaxis for rituxi-mab-associated hepatitis B virus reactivation in patients with lymphoma and resolved hepatitis B. J. Clin. Oncol. 2013, 31, 2765–2772. [Google Scholar] [CrossRef]
- Chen, M.-H.; Chen, M.-H.; Liu, C.-Y.; Tsai, C.-Y.; Huang, D.-F.; Lin, H.-Y.; Lee, M.-H.; Huang, Y.-H. Hepatitis B Virus Reactivation in Rheumatoid Arthritis Patients Undergoing Biologics Treatment. J. Infect. Dis. 2017, 215, 566–573. [Google Scholar] [CrossRef]
- Chen, M.-H.; Chou, C.-T.; Hou, M.-C.; Tsai, C.-Y.; Huang, Y.-H. Low but Long-lasting Risk of Reversal of Seroconversion in Patients with Rheumatoid Arthritis Receiving Immunosuppressive Therapy. Clin. Gastroenterol. Hepatol. 2020, 18, 2573–2581.e1. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.P.; Feld, J.J.; Hammond, S.P.; Wang, S.H.; Alston-Johnson, D.E.; Cryer, D.R.; Hershman, D.L.; Loehrer, A.P.; Sabichi, A.L.; Symington, B.E.; et al. Hepatitis B Virus Screening and Management for Patients with Cancer Prior to Therapy: ASCO Provisional Clinical Opinion Update. J. Clin. Oncol. 2020, 38, 3698–3715. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J. Hepatol. 2017, 67, 370–398. [Google Scholar] [CrossRef]
- Terrault, N.A.; Lok, A.S.F.; McMahon, B.J.; Chang, K.-M.; Hwang, J.P.; Jonas, M.M.; Brown, R.S., Jr.; Bzowej, N.H.; Wong, J.B. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology 2018, 67, 1560–1599. [Google Scholar] [CrossRef]
- Charlton, M.R.; Alam, A.; Shukla, A.; Dashtseren, B.; Lesmana, C.R.A.; Duger, D.; Payawal, D.A.; Cuong, D.D.; Jargalsaikhan, G.; Cua, I.H.Y.; et al. An expert review on the use of tenofovir alafenamide for the treatment of chronic hepatitis B virus infection in Asia. J. Gastroenterol. 2020, 55, 811–823. [Google Scholar] [CrossRef]
- Herlitz, L.C.; Mohan, S.; Stokes, M.B.; Radhakrishnan, J.; D’Agati, V.D.; Markowitz, G.S. Tenofovir nephrotoxicity: Acute tubular necrosis with distinctive clinical, pathological, and mitochondrial abnormalities. Kidney Int. 2010, 78, 1171–1177. [Google Scholar] [CrossRef]
- Chan, H.L.; Fung, S.; Seto, W.K.; Chuang, W.L.; Chen, C.Y.; Kim, H.J.; Hui, A.J.; Jansenn, H.L.A.; Chowdury, A.; Tsang, T.Y.O.; et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate for the treatment of HBeAg-positive chronic hepatitis B virus infection: A randomised, double-blind, phase 3, non-inferiority trial. Lancet Gastroenterol. Hepatol. 2016, 1, 185–195. [Google Scholar] [CrossRef]
- Buti, M.; Gane, E.; Seto, W.K.; Chan, H.L.; Chuang, W.L.; Stepanova, T.; Hui, A.-J.; Lim, Y.-S.; Mehta, R.; Janssen, H.L.A.; et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate for the treatment of patients with HBeAg-negative chronic hepatitis B virus infection: A randomised, double-blind, phase 3, non-inferiority trial. Lancet Gastroenterol. Hepatol. 2016, 1, 196–206. [Google Scholar] [CrossRef]
- Lampertico, P.; Buti, M.; Fung, S.; Ahn, S.H.; Chuang, W.L.; Tak, W.Y.; Ramji, A.; Chen, C.-Y.; Tam, E.; Bae, H.; et al. Switching from tenofovir disoproxil fumarate to tenofovir alafenamide in virologically suppressed patients with chronic hepatitis B: A randomised, double-blind, phase 3, multicentre non-inferiority study. Lancet Gastroenterol. Hepatol. 2020, 5, 441–453. [Google Scholar] [CrossRef]
- Rosner, M.H.; Perazella, M.A. Acute Kidney Injury in Patients with Cancer. N. Engl. J. Med. 2017, 377, 500–501. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.C.; Chao, Y.; Li, C.-P.; Su, C.-W.; Lan, K.-H.; Lin, H.-C.; Hou, M.-C.; Huang, Y.-H. Risk of renal events during tenofovir disoproxil fumarate and entecavir antiviral prophylaxis in HBsAg-positive cancer patients undergoing chemotherapy. J. Viral Hepat. 2018, 25, 1599–1607. [Google Scholar] [CrossRef] [PubMed]
- Toyoda, H.; Leong, J.; Landis, C.; Atsukawa, M.; Watanabe, T.; Huang, D.Q.; Liu, J.; Quek, S.X.Z.; Ishikawa, T.; Arai, T.; et al. Treatment and Renal Outcomes Up to 96 Weeks After Tenofovir Alafenamide Switch from Tenofovir Disoproxil Fumarate in Routine Practice. Hepatology 2021, 74, 656–666. [Google Scholar] [CrossRef]
- Byun, K.S.; Choi, J.; Kim, J.-H.; Lee, Y.S.; Lee, H.C.; Kim, Y.J.; Yoo, B.C.; Kwon, S.Y.; Gwak, G.-Y.; Lim, Y.-S. Tenofovir Alafenamide for Drug-Resistant Hepatitis B: A Randomized Trial for Switching from Tenofovir Disoproxil Fumarate. Clin. Gastroenterol. Hepatol. 2021, 20, 427–437.e5. [Google Scholar] [CrossRef]
- Perazella, M.A.; Moeckel, G.W. Nephrotoxicity from Chemotherapeutic Agents: Clinical Manifestations, Pathobiology, and Prevention/Therapy. Semin. Nephrol. 2010, 30, 570–581. [Google Scholar] [CrossRef]
- Angeli, P.; Garcia-Tsao, G.; Nadim, M.K.; Parikh, C.R. News in pathophysiology, definition and classification of hepatorenal syndrome: A step beyond the International Club of Ascites (ICA) consensus document. J. Hepatol. 2019, 71, 811–822. [Google Scholar] [CrossRef]
- Wiedermann, C.J.; Wiedermann, W.; Joannidis, M. Hypoalbuminemia and acute kidney injury: A meta-analysis of observational clinical studies. Intensive Care Med. 2010, 36, 1657–1665. [Google Scholar] [CrossRef]
- Custodio, J.M.; Fordyce, M.; Garner, W.; Vimal, M.; Ling, K.H.J.; Kearney, B.P.; Ramanathan, S. Pharmacokinetics and Safety of Tenofovir Alafenamide in HIV-Uninfected Subjects with Severe Renal Impairment. Antimicrob. Agents Chemother. 2016, 60, 5135–5140. [Google Scholar] [CrossRef] [PubMed]
- Gish, R.G.; Clark, M.D.; Kane, S.D.; Shaw, R.E.; Mangahas, M.F.; Baqai, S. Similar Risk of Renal Events Among Patients Treated with Tenofovir or Entecavir for Chronic Hepatitis B. Clin. Gastroenterol. Hepatol. 2012, 10, 941–946. [Google Scholar] [CrossRef] [PubMed]
- Mallet, V.; Schwarzinger, M.; Vallet-Pichard, A.; Fontaine, H.; Corouge, M.; Sogni, P.; Pol, S. Effect of Nucleoside and Nucleotide Analogues on Renal Function in Patients with Chronic Hepatitis B Virus Monoinfection. Clin. Gastroenterol. Hepatol. 2015, 13, 1181–1188.e1. [Google Scholar] [CrossRef] [PubMed]
- Köklü, S.; Gulsen, M.T.; Tuna, Y.; Koklu, H.; Yüksel, O.; Demir, M.; Guner, R.; Dogan, Z.; Kucukazman, M.; Poyrazoglu, O.K.; et al. Differences in nephrotoxicity risk and renal effects among anti-viral therapies against hepatitis B. Aliment. Pharmacol. Ther. 2015, 41, 310–319. [Google Scholar] [CrossRef]
- Lampertico, P.; Chan, H.L.Y.; Janssen, H.L.A.; Strasser, S.I.; Schindler, R.; Berg, T. Review article: Long-term safety of nucleoside and nucleotide analogues in HBV-monoinfected patients. Aliment. Pharmacol. Ther. 2016, 44, 16–34. [Google Scholar] [CrossRef]
- Fong, T.-L.; Lee, B.T.; Tien, A.; Chang, M.; Lim, C.; Ahn, A.; Bae, H.S. Improvement of bone mineral density and markers of proximal renal tubular function in chronic hepatitis B patients switched from tenofovir disoproxil fumarate to tenofovir alafenamide. J. Viral Hepat. 2019, 26, 561–567. [Google Scholar] [CrossRef]
- Sarin, S.K.; Kumar, M.; Lau, G.K.; Abbas, Z.; Chan, H.L.Y.; Chen, C.J.; Chen, D.S.; Chen, H.L.; Chen, P.J.; Chien, R.N.; et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: A 2015 update. Hepatol. Int. 2016, 10, 1–98. [Google Scholar] [CrossRef]
- Sabanayagam, C.; Wong, T.Y.; Tai, E.S. The CKD-EPI equation and MDRD study equation find similar prevalence of chronic kidney disease in Asian populations. Ann. Intern. Med. 2009, 151, 892–893. [Google Scholar] [CrossRef]
- Khwaja, A. KDIGO Clinical Practice Guidelines for Acute Kidney Injury. Nephron Exp. Nephrol. 2012, 120, c179–c184. [Google Scholar] [CrossRef]
- Liu, J.; Colditz, G.A. Optimal design of longitudinal data analysis using generalized estimating equation models. Biom. J. 2016, 59, 315–330. [Google Scholar] [CrossRef]

| ETV (n = 582, 60%) | TDF (n = 200, 20.6%) | TAF (n = 188, 19.4%) | p | |
|---|---|---|---|---|
| Age (years) | 59.4 ± 12.2 | 56.9 ± 11.7 | 58.6 ± 11.1 | 0.024 |
| Sex (male), n (%) | 267 (45.9) | 99 (49.5) | 79 (42.0) | 0.385 |
| Body mass index (kg/m2) | 23.6 ± 3.8 | 23.8 ± 4.5 | 23.5 ± 4.1 | 0.623 |
| Diabetes, n (%) | 79 (13.6) | 27 (13.5) | 20 (10.6) | 0.565 |
| Hypertension, n (%) | 154 (26.5) | 57 (28.5) | 45 (23.9) | 0.594 |
| Cancer types, n (%) | <0.001 | |||
| Gastrointestinal cancers | 114 (19.6) | 65 (32.5) | 59 (31.4) | |
| Hematological cancers | 106 (18.2) | 17 (8.5) | 26 (13.6) | |
| Lung cancer | 93 (16) | 30 (15) | 25 (13.3) | |
| Head and neck cancers | 66 (11.3) | 29 (14.5) | 13 (6.9) | |
| Breast cancer | 64 (11) | 33 (16.5) | 24 (12.8) | |
| Hepatobiliary cancer | 39 (6.7) | 7 (3.5) | 4 (2.1) | |
| Gynecological cancer | 43 (7.4) | 9 (4.5) | 15 (8) | |
| Others | 57 (9.8) | 10 (5) | 22 (11.7) | |
| Chemotherapy duration (months) | 7.7 (4.2–18.4) | 6.0 (4.0–11.6) | 6.4 (3.7–11.7) | 0.001 |
| Chemotherapy regimen, n (%) | ||||
| Rituximab-containing | 66 (11.3) | 9 (4.5) | 21 (11.2) | 0.016 |
| Platinum-containing | 298 (51.2) | 108 (54) | 102 (54.3) | 0.671 |
| Cisplatin-containing | 196 (33.7) | 81 (40.5) | 61 (32.4) | 0.162 |
| Concurrent radiotherapy | 157 (27) | 60 (30) | 45 (23.9) | 0.405 |
| NUC therapy duration (months) | 12.4 (8–21.6) | 10.6 (8.2–17) | 10.2 (7.7–13.2) | <0.001 |
| Ongoing NUC therapy, n (%) | 162 (27.8) | 7 (3.5) | 122 (64.9) | <0.001 |
| Follow-up period (months) | 18.4 (10.2–35.1) | 20 (10.7–40.5) | 11.9 ± 3.5 | <0.001 |
| Death during follow-up period | 169 (29) | 116 (42) | 15 (8) | <0.001 |
| HBV DNA (Log IU/mL) * | 2.99 ± 1.68 | 2.78 ± 1.57 | 2.93 ± 1.85 | 0.071 |
| Undetectable HBV DNA, n (%) * | 134 (23.9) | 49 (25.7) | 53 (30.5) | 0.220 |
| HBV DNA < 2000 IU/mL, n (%) * | 350 (62.4) | 128 (67) | 112 (64.4) | 0.507 |
| HBsAg (Log IU/mL) * | 1.95 ± 1.43 | 1.71 ± 1.52 | 2.06 ± 1.38 | 0.173 |
| HBV status, n (%) | 0.080 | |||
| HBeAg-positive carrier | 22 (3.8) | 5 (2.5) | 10 (5.3) | |
| HBeAg-positive chronic hepatitis | 10 (1.7) | 0 (0) | 1 (0.5) | |
| HBeAg-negative carrier | 510 (87.6) | 189 (94.5) | 165 (87.8) | |
| HBeAg-negative chronic hepatitis | 40 (6.9) | 6 (3) | 12 (6.4) | |
| BUN (mg/dL) | 15.9 ± 9.2 | 13.6 ± 4.4 | 14.2 ± 5.8 | 0.015 |
| Creatinine (mg/dL) | 0.93 ± 0.54 | 0.81 ± 0.16 | 0.81 ± 0.25 | <0.001 |
| eGFR (mL/min) | 80.5 ± 23.4 | 86.6 ± 18.9 | 84.9 ± 23.1 | 0.001 |
| Chronic kidney disease (CKD) stage 1/2/3/4/5, n (%) | 290/218/63/7/4 (49.8/37.5/10.8/1.2/0.7) | 119/75/6/0/0 (59.5/37.5/3/0/0) | 111/60/15/2/0 (59/31.9/8/1.1/0) | 0.008 |
| Albumin (g/dL) | 3.78 ± 0.54 | 3.86 ± 0.46 | 3.80 ± 0.57 | 0.166 |
| Total bilirubin (mg/dL) | 0.59 ± 0.35 | 0.61 ± 0.34 | 0.57 ± 0.36 | 0.308 |
| ALT (U/L) | 40.5 ± 86.0 | 29.1 ± 32.8 | 32.9 ± 41.1 | 0.575 |
| AST (U/L) | 36.1 ± 52.1 | 29.6 ± 27.1 | 30.1 ± 26.1 | 0.093 |
| Events, n (%) | ETV (n = 417, 60.8%) | TDF (n = 149, 21.7%) | TAF (n = 120, 17.5%) | p |
|---|---|---|---|---|
| Antiviral efficacy | ||||
| Virological response * | 250 (94.7) | 89 (94.7) | 74 (96.1) | 0.877 |
| HBV reactivation | 2 (0.5) | 1 (0.7) | 0 (0) | 0.694 |
| Renal events—all CKD stages | ||||
| Acute kidney injury | 61 (14.6) | 17 (11.4) | 13 (10.8) | 0.420 |
| eGFR decrease > 30% | 121 (29) | 40 (26.8) | 24 (20) | 0.146 |
| eGFR < 50 mL/min | 101 (24.2) | 13 (8.7) | 16 (13.3) | <0.001 |
| Dose reduction | 14 (13.9) | 5 (38.5) | - | 0.041 |
| ≥1 stage worsening in CKD stage at 1 year | 56 (13.4) | 21 (14.1) | 12 (10) | 0.554 |
| ≥1 stage improvement in CKD stage at 1 year | 52 (12.5) | 15 (10.1) | 14 (11.7) | 0.737 |
| Serum phosphorus < 2 mg/dL | 64 (15.3) | 17 (11.4) | 14 (11.7) | 0.367 |
| Renal events—CKD stage 1 | ||||
| Case number | 213 | 85 | 62 | |
| Acute kidney injury | 25 (11.7) | 9 (10.6) | 4 (6.5) | 0.491 |
| eGFR decrease > 30% | 58 (27.2) | 25 (29.4) | 8 (12.9) | 0.044 |
| eGFR < 50 mL/min | 18 (8.5) | 2 (2.4) | 2 (3.2) | 0.081 |
| Dose reduction | 1 (5.6) | 1 (50) | - | 0.195 |
| ≥1 stage worsening in CKD stage at 1 year | 54 (25.4) | 21 (24.7) | 9 (14.5) | 0.195 |
| Serum phosphorus < 2 mg/dL | 34 (16) | 7 (8.2) | 7 (11.3) | 0.182 |
| Renal events—CKD stage 2 | ||||
| Case number | 157 | 60 | 49 | |
| Acute kidney injury | 25 (15.9) | 7 (11.7) | 6 (12.2) | 0.655 |
| eGFR decrease > 30% | 54 (34.4) | 13 (21.7) | 13 (26.5) | 0.157 |
| eGFR < 50 mL/min | 45 (28.7) | 8 (13.3) | 8 (16.3) | 0.027 |
| Dose reduction | 2 (4.4) | 2 (25) | - | 0.104 |
| ≥1 stage worsening in CKD stage at 1 year | 1 (0.6) | 0 (0) | 2 (4.1) | 0.088 |
| ≥1 stage improvement in CKD stage at 1 year | 34 (21.7) | 14 (23.3) | 11 (22.4) | 0.964 |
| Serum phosphorus < 2 mg/dL | 23 (14.6) | 9 (15) | 6 (12.2) | 0.901 |
| Renal events—CKD stage 3–5 | ||||
| Case number | 47 | 4 | 9 | |
| Acute kidney injury | 11 (23.4) | 1 (25) | 3 (33.3) | 0.820 |
| eGFR decrease > 30% | 9 (19.1) | 2 (50) | 3 (33.3) | 0.279 |
| eGFR < 50 mL/min | 38 (80.9) | 3 (75) | 6 (66.6) | 0.630 |
| Dose reduction | 11 (28.9) | 2 (66.7) | - | 0.232 |
| ≥1 stage worsening in CKD stage at 1 year | 1 (2.1) | 0 (0) | 1 (11.1) | 0.361 |
| ≥1 stage improvement in CKD stage at 1 year | 18 (38.3) | 1 (25) | 3 (33.3) | 0.847 |
| Serum phosphorus < 2 mg/dL | 7 (14.9) | 1 (25) | 9 (100) | 0.810 |
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | |
| Age (years) | 1.014 | 1.003–1.025 | 0.015 | NS | ||
| Sex (male) | 0.688 | 0.520–0.909 | 0.009 | NS | ||
| Diabetes (yes vs. no) | 1.428 | 0.993–2.053 | 0.055 | NS | ||
| Hypertension (yes vs. no) | 1.366 | 1.019–1.832 | 0.037 | NS | ||
| Hematologic cancer (yes vs. no) | 1.245 | 0.875–1.769 | 0.223 | |||
| Platinum-based chemotherapy (yes vs. no) | 1.095 | 0.83–1.438 | 0.516 | |||
| Cisplatin-based chemotherapy (yes vs. no) | 1.477 | 1.122–1.944 | 0.005 | 1.437 | 1.072–1.925 | 0.015 |
| Radiotherapy (yes vs. no) | 1.128 | 0.836–1.523 | 0.430 | |||
| HBeAg-positive (yes vs. no) | 0.973 | 0.515–1.837 | 0.933 | |||
| HBV DNA (Log IU/mL) | 1.014 | 0.933–1.101 | 0.751 | |||
| HBsAg (Log IU/mL) | 0.974 | 0.881–1.077 | 0.613 | |||
| Body mass index (kg/m2) | 1.013 | 0.980–1.048 | 0.438 | |||
| BUN (mg/dL) | 1.026 | 1.011–1.040 | <0.001 | NS | ||
| Creatinine (mg/dL) | 1.501 | 1.300–1.733 | <0.001 | 1.384 | 1.164–1.646 | <0.001 |
| eGFR | 0.990 | 0.983–0.996 | 0.001 | NS | ||
| ALT (U/L) | 0.999 | 0.997–1.002 | 0.531 | |||
| AST (U/L) | 1.000 | 0.998–1.003 | 0.726 | |||
| Albumin (g/dL) | 0.520 | 0.407–0.664 | <0.001 | 0.544 | 0.426–0.696 | <0.001 |
| Total bilirubin (mg/dL) | 1.442 | 1.014–2.052 | 0.042 | 1.449 | 1.002–2.096 | 0.049 |
| WBC count | 1.000 | 1.000–1.000 | 0.924 | |||
| Hemoglobin | 0.885 | 0.827–0.946 | <0.001 | NS | ||
| Platelet count | 1.000 | 1.000–1.000 | 0.692 | |||
| NUCs therapy | ||||||
| ETV | 1 | 0.026 | NS | |||
| TDF | 0.848 | 0.603–1.193 | 0.345 | |||
| TAF | 0.549 | 0.353–0.855 | 0.008 | |||
| Renal Events, n (%) | No Switching (n = 75) | Switching from TDF (n = 45) | p |
|---|---|---|---|
| Acute kidney injury | 8 (10.7) | 5 (11.1) | 1.000 |
| eGFR decrease > 30% | 18 (24) | 6 (13.3) | 0.239 |
| eGFR < 50 mL/min | 11 (14.7) | 5 (11.1) | 0.782 |
| ≥1 stage worsening in CKD stage at 1 year | 7 (9.3) | 5 (11.1) | 0.762 |
| ≥1 stage improvement in CKD stage at 1 year | 10 (13.3) | 4 (8.9) | 0.660 |
| Serum phosphorus < 2 mg/dL | 7 (9.3) | 7 (15.6) | 0.463 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, I.-C.; Lan, K.-H.; Su, C.-W.; Li, C.-P.; Chao, Y.; Lin, H.-C.; Hou, M.-C.; Huang, Y.-H. Efficacy and Renal Safety of Prophylactic Tenofovir Alafenamide for HBV-Infected Cancer Patients Undergoing Chemotherapy. Int. J. Mol. Sci. 2022, 23, 11335. https://doi.org/10.3390/ijms231911335
Lee I-C, Lan K-H, Su C-W, Li C-P, Chao Y, Lin H-C, Hou M-C, Huang Y-H. Efficacy and Renal Safety of Prophylactic Tenofovir Alafenamide for HBV-Infected Cancer Patients Undergoing Chemotherapy. International Journal of Molecular Sciences. 2022; 23(19):11335. https://doi.org/10.3390/ijms231911335
Chicago/Turabian StyleLee, I-Cheng, Keng-Hsin Lan, Chien-Wei Su, Chung-Pin Li, Yee Chao, Han-Chieh Lin, Ming-Chih Hou, and Yi-Hsiang Huang. 2022. "Efficacy and Renal Safety of Prophylactic Tenofovir Alafenamide for HBV-Infected Cancer Patients Undergoing Chemotherapy" International Journal of Molecular Sciences 23, no. 19: 11335. https://doi.org/10.3390/ijms231911335
APA StyleLee, I.-C., Lan, K.-H., Su, C.-W., Li, C.-P., Chao, Y., Lin, H.-C., Hou, M.-C., & Huang, Y.-H. (2022). Efficacy and Renal Safety of Prophylactic Tenofovir Alafenamide for HBV-Infected Cancer Patients Undergoing Chemotherapy. International Journal of Molecular Sciences, 23(19), 11335. https://doi.org/10.3390/ijms231911335





