Shared Risk Factors between Dementia and Atherosclerotic Cardiovascular Disease
Abstract
:1. Introduction
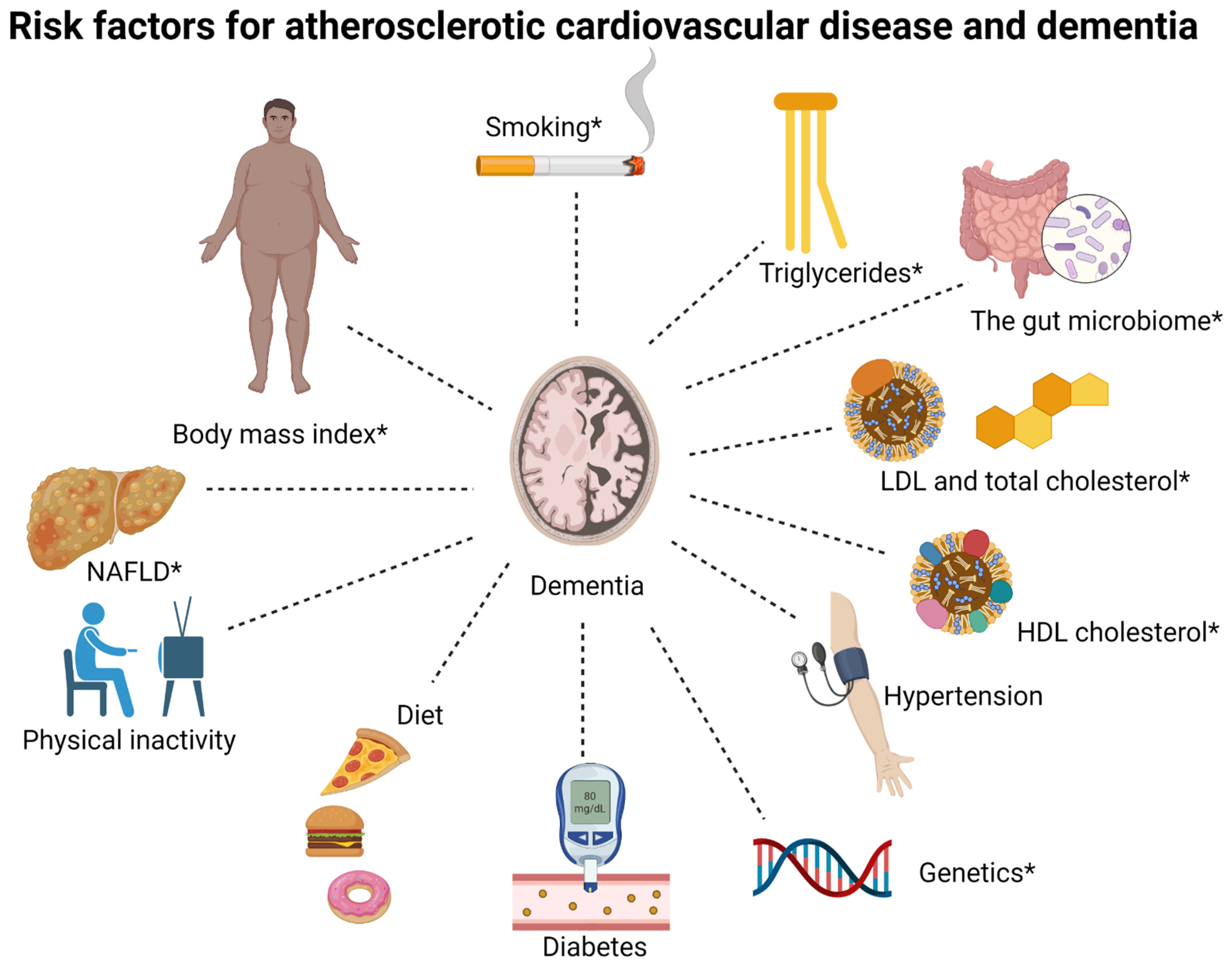
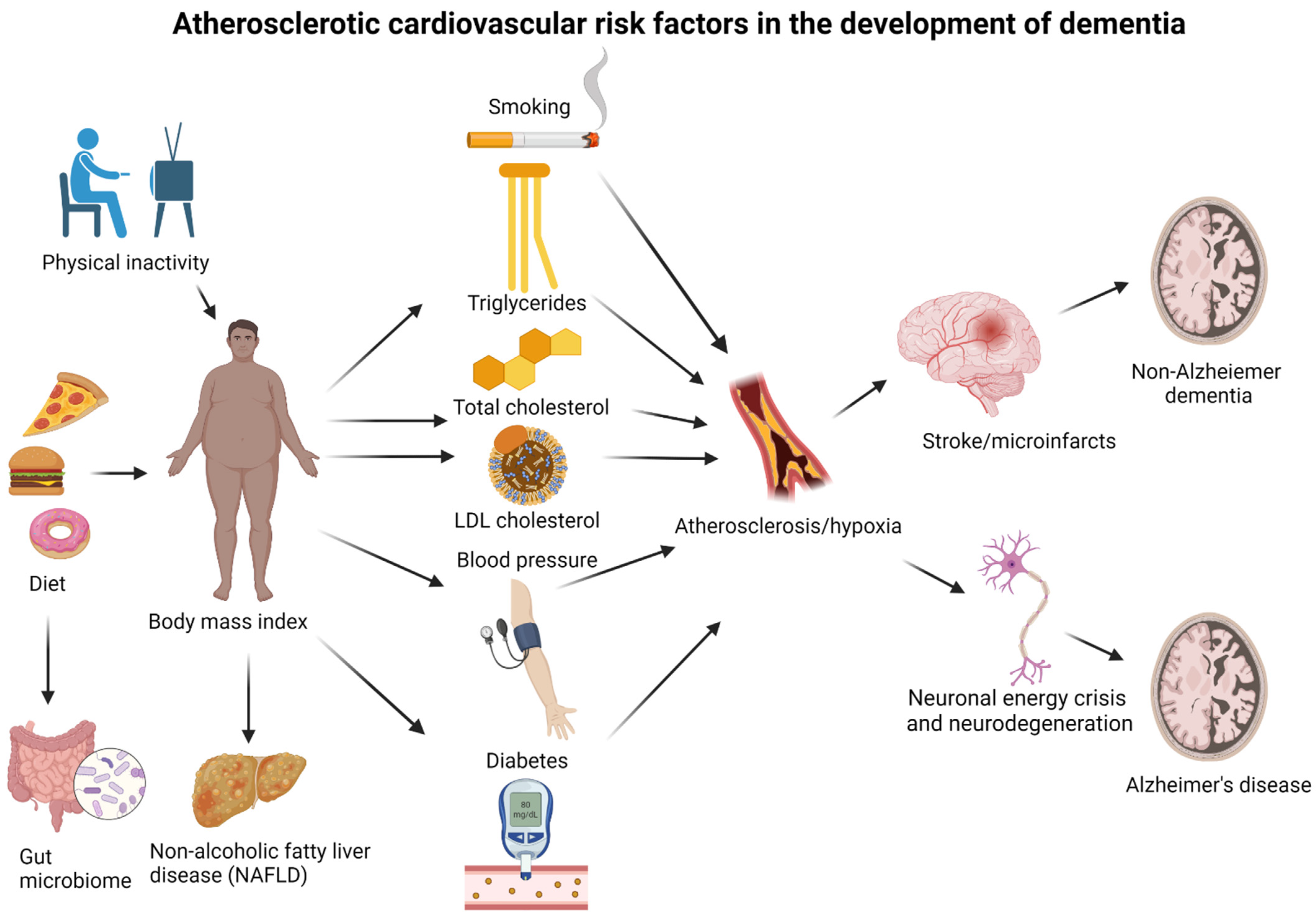
2. Alzheimer’s Disease and Vascular Dementia
3. Shared Risk Factors between Dementia and Atherosclerotic Cardiovascular Disease
4. Body Mass Index
4.1. Alzheimer’s Disease
4.2. Non-Alzheimer Dementia
4.3. All-Cause Dementia
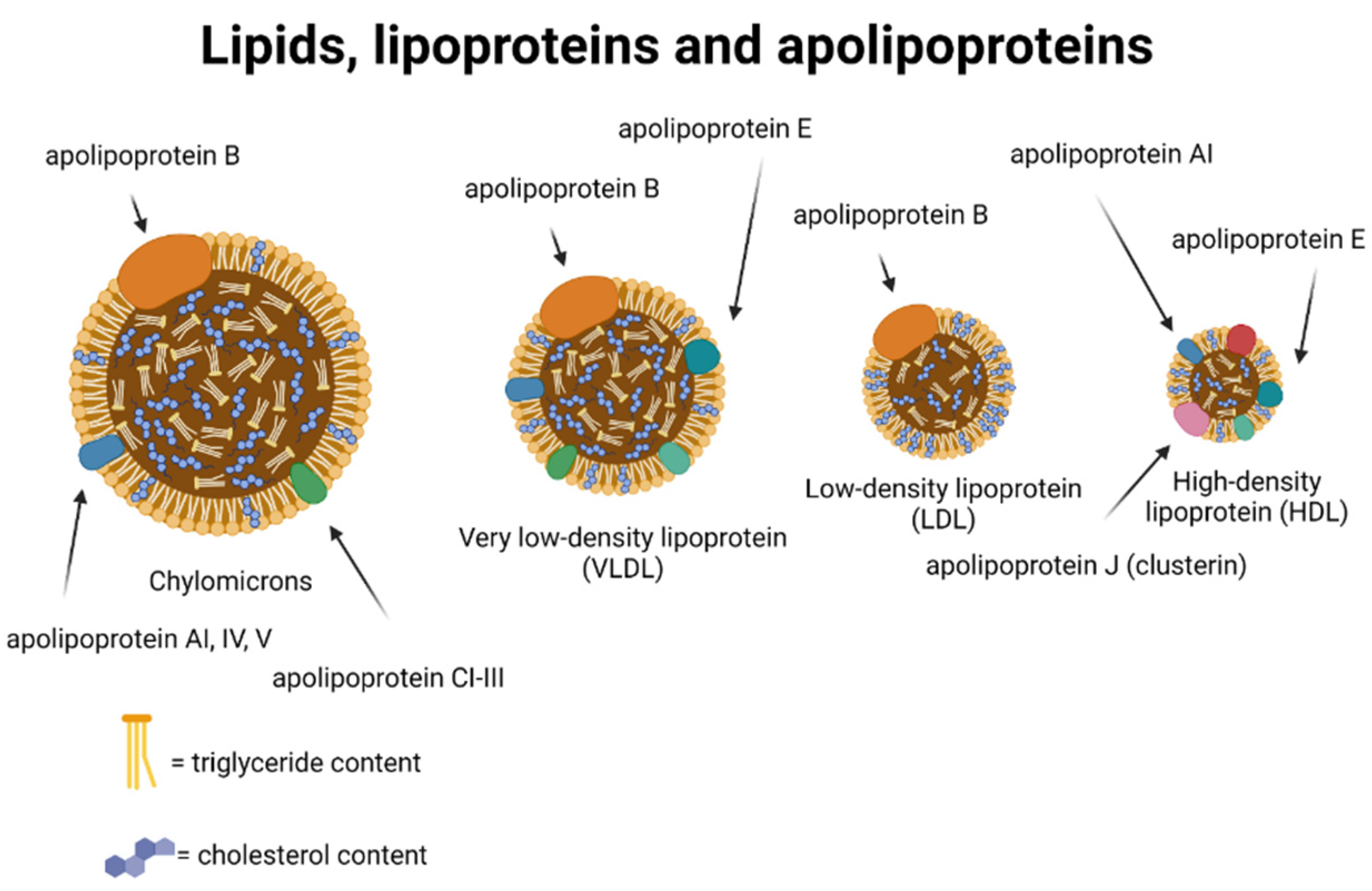
5. Lipids and Lipoproteins
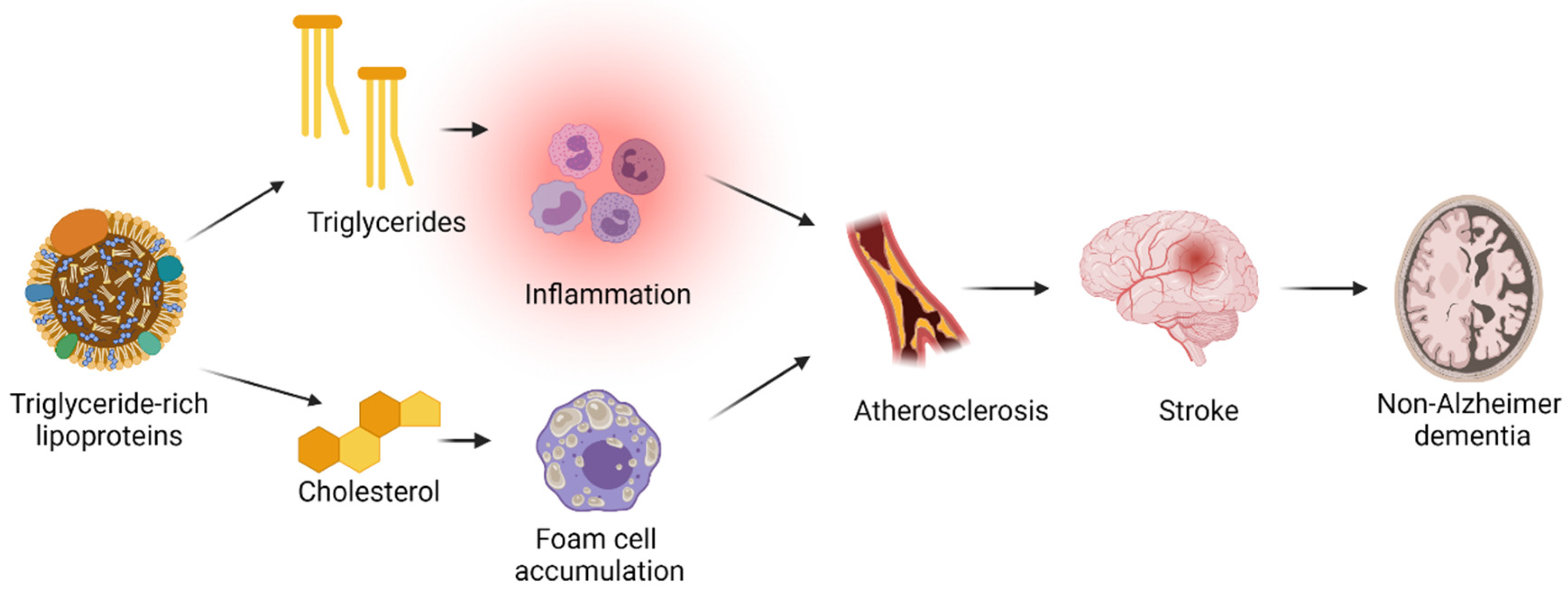
5.1. Plasma Triglyceride Concentrations
5.1.1. Alzheimer’s Disease
5.1.2. Non-Alzheimer Dementia
5.1.3. All-Cause Dementia
5.2. Plasma High-Density Lipoprotein Cholesterol Concentrations
5.2.1. Alzheimer’s Disease
5.2.2. Non-Alzheimer Dementia
5.2.3. All-Cause Dementia
5.3. Plasma Total Cholesterol Concentrations
5.3.1. Alzheimer’s Disease
5.3.2. Non-Alzheimer Dementia
5.4. Plasma Low-Density Lipoprotein Cholesterol Concentrations and Use of Lipid-Lowering Therapy
5.4.1. Alzheimer’s Disease
5.4.2. Non-Alzheimer Dementia
5.4.3. All-Cause Dementia
6. Hypertension and Antihypertensive Drugs
6.1. Alzheimer’s Disease
6.2. All-Cause Dementia
7. Diabetes
7.1. Alzheimer’s Disease
7.2. Non-Alzheimer Dementia
7.3. All-Cause Dementia
8. Non-Alcoholic Fatty Liver Disease
8.1. Non-Alzheimer Dementia
8.2. All-Cause Dementia
9. Physical Inactivity
9.1. Alzheimer’s Disease
9.2. Non-Alzheimer Dementia
9.3. All-Cause Dementia
10. Smoking
10.1. Alzheimer’s Disease
10.2. Non-Alzheimer Dementia
10.3. All-Cause Dementia
11. Diet
11.1. Alzheimer’s Disease
11.2. Non-Alzheimer Dementia
11.3. All-Cause Dementia
12. The Gut Microbiome
Alzheimer’s Disease
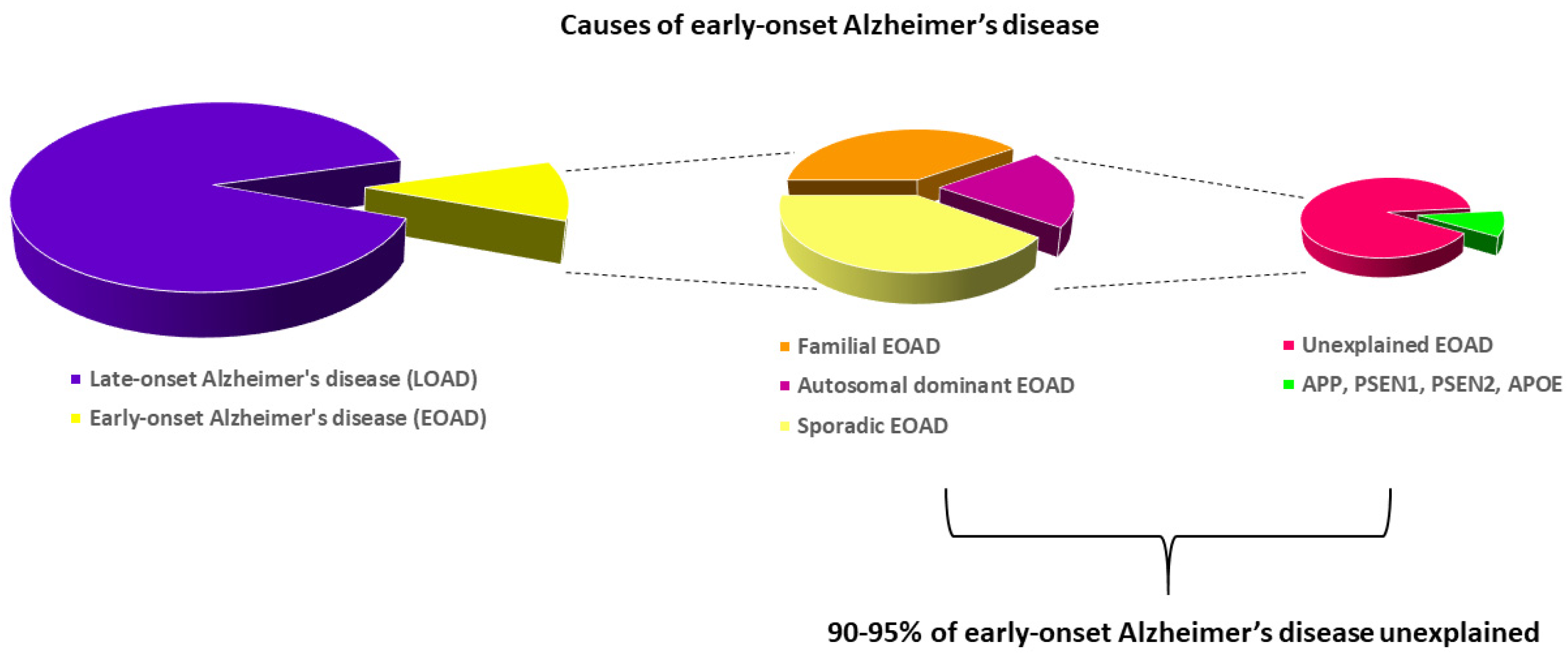
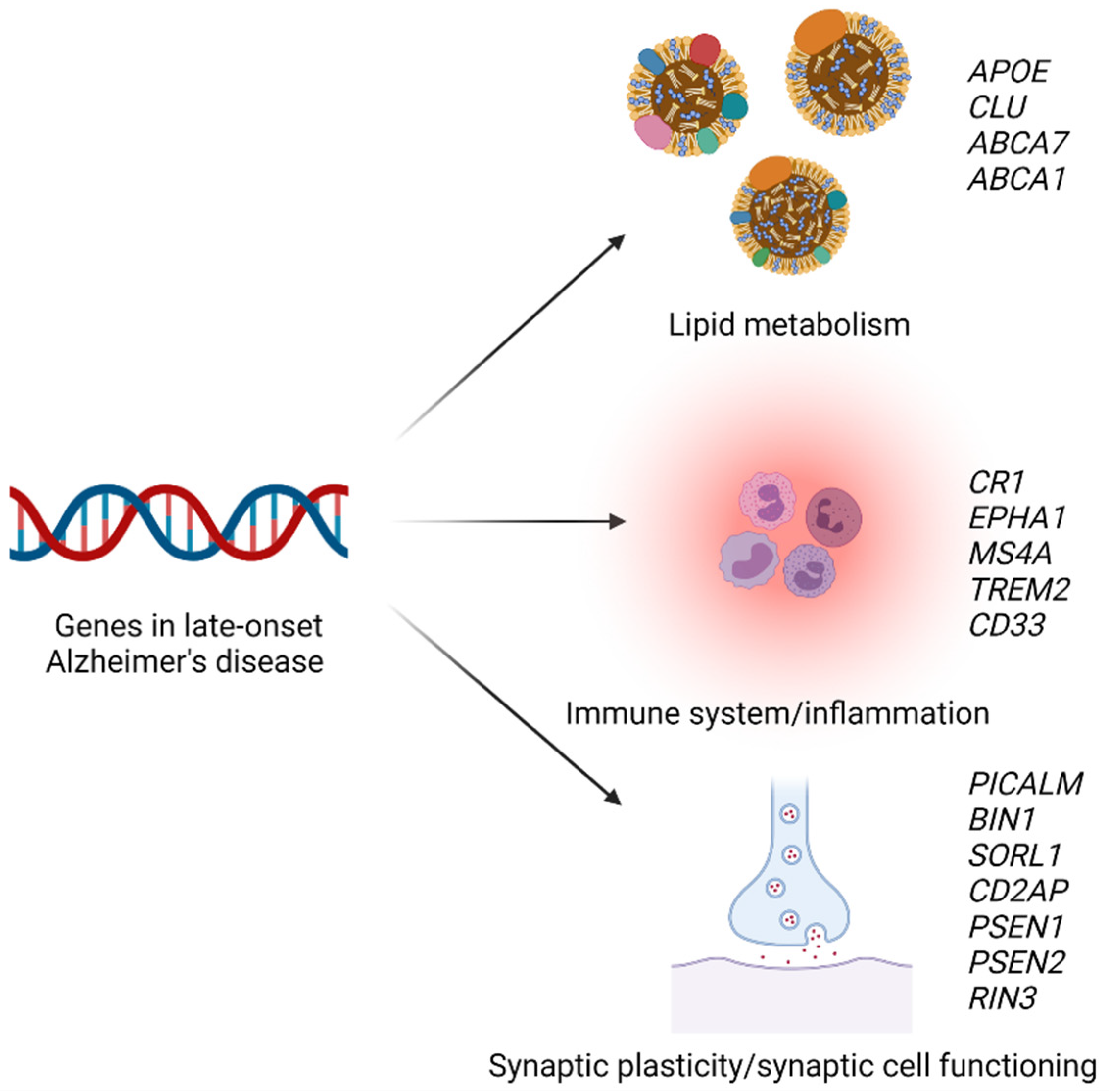
13. Genetics
13.1. Alzheimer’s Disease
13.2. Non-Alzheimer Dementia
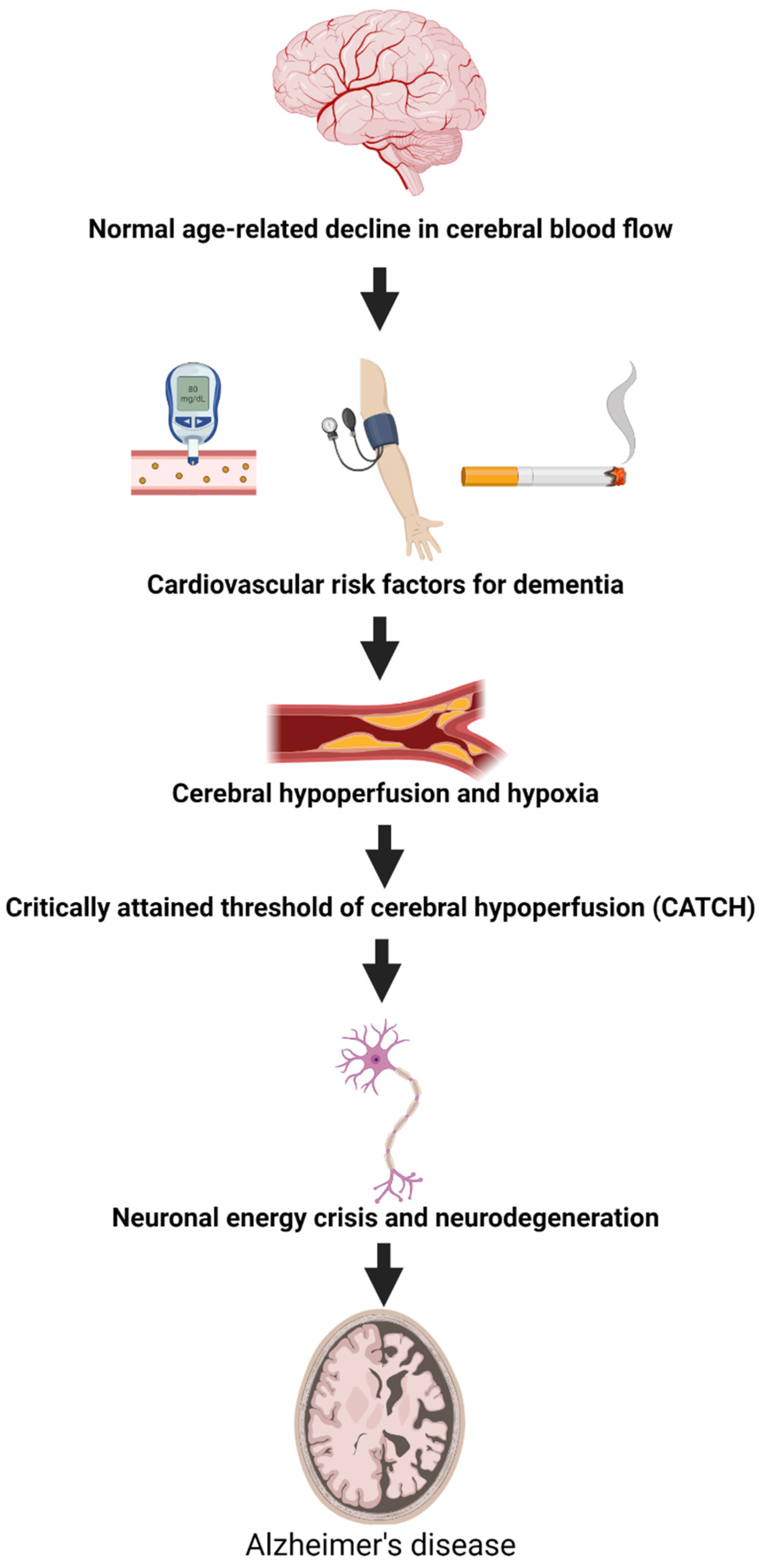
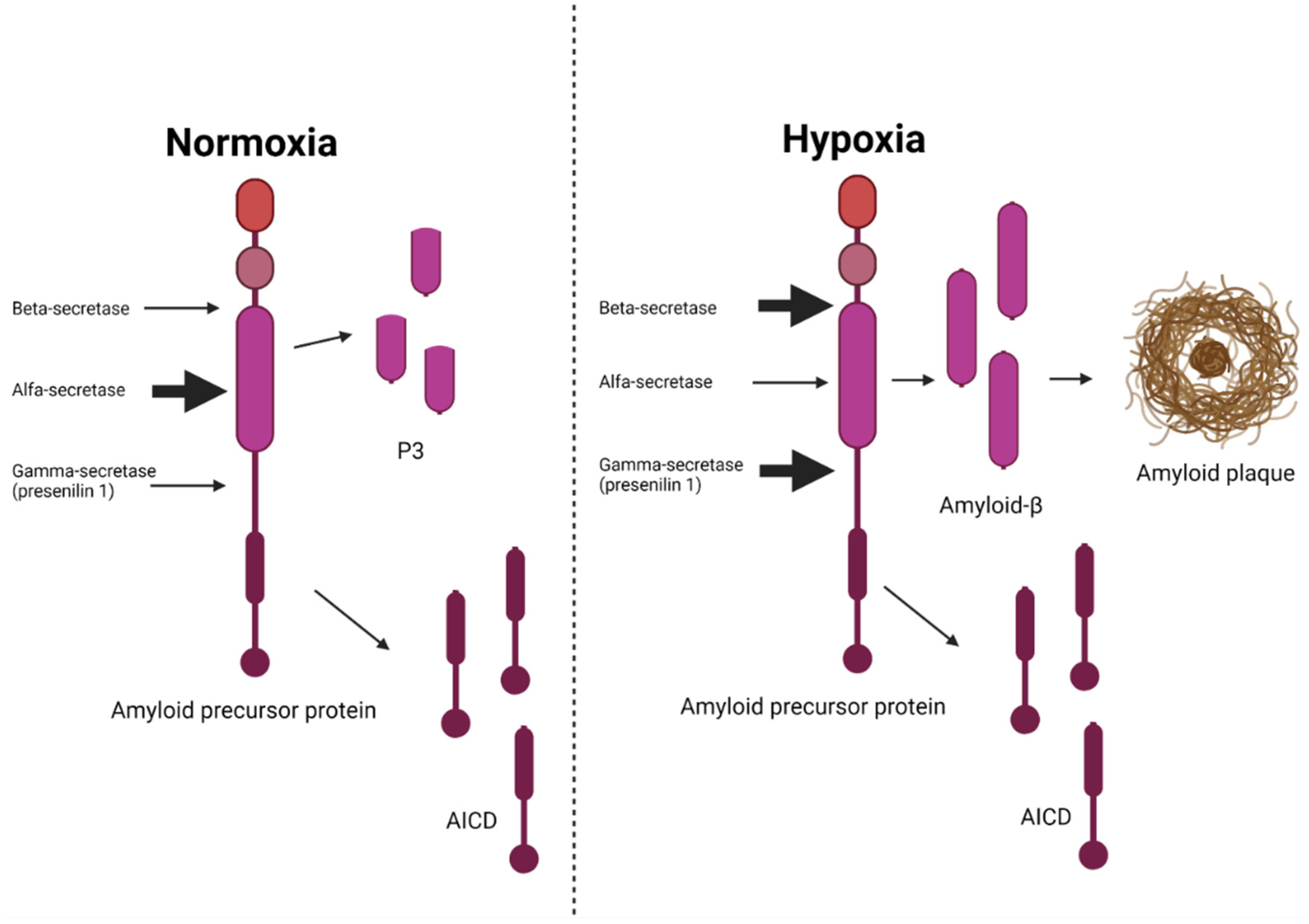
14. The Vascular Hypothesis of Alzheimer’s Disease
15. Conclusions and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McKhann, G.M.; Knopman, D.S.; Chertkow, H.; Hyman, B.T.; Jack, C.R.; Kawas, C.H.; Klunk, W.E.; Koroshetz, W.J.; Manly, J.J.; Mayeux, R.; et al. The Diagnosis of Dementia Due to Alzheimer’s Disease: Recommendations from the National Institute on Aging-Alzheimer’s Association Workgroups on Diagnostic Guidelines for Alzheimer’s Disease. Alzheimer’s Dement. 2011, 7, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia Prevention, Intervention, and Care: 2020 Report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- World Health Organization. ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research; World Health Organization: Geneva, Switzerland, 1993. [Google Scholar]
- 2021 Alzheimer’s Disease Facts and Figures. Alzheimer’s Dement. 2021, 17, 327–406. [CrossRef] [PubMed]
- Cacace, R.; Sleegers, K.; Van Broeckhoven, C. Molecular Genetics of Early-Onset Alzheimer’s Disease Revisited. Alzheimer’s Dement. 2016, 12, 733–748. [Google Scholar] [CrossRef]
- Hardy, J.A.; Higgins, G.A.; Hardy, J.A.; Higgins, G.A. Alzheimer ’ s Disease: The Amyloid Cascade Hypothesis Published by: American Association for the Advancement of Science Alzheimer ’ s Disease: The Amyloid Cascade Hypothesis. Science 1992, 256, 184–185. [Google Scholar] [CrossRef]
- Salloway, S.; Sperling, R.; Fox, N.C.; Blennow, K.; Klunk, W.; Raskind, M.; Sabbagh, M.; Honig, L.S.; Porsteinsson, A.P.; Ferris, S.; et al. Two Phase 3 Trials of Bapineuzumab in Mild-to-Moderate Alzheimer’s Disease. N. Engl. J. Med. 2014, 370, 322–333. [Google Scholar] [CrossRef]
- Honig, L.S.; Vellas, B.; Woodward, M.; Boada, M.; Bullock, R.; Borrie, M.; Hager, K.; Andreasen, N.; Scarpini, E.; Liu-Seifert, H.; et al. Trial of Solanezumab for Mild Dementia Due to Alzheimer’s Disease. N. Engl. J. Med. 2018, 378, 321–330. [Google Scholar] [CrossRef]
- Laske, C. Phase 3 Trials of Solanezumab and Bapineuzumab for Alzheimer’s Disease. N. Engl. J. Med. 2014, 370, 1459–1460. [Google Scholar] [CrossRef]
- Holmes, C.; Boche, D.; Wilkinson, D.; Yadegarfar, G.; Hopkins, V.; Bayer, A.; Jones, R.W.; Bullock, R.; Love, S.; Neal, J.W.; et al. Long-Term Effects of Aβ42 Immunisation in Alzheimer’s Disease: Follow-up of a Randomised, Placebo-Controlled Phase I Trial. Lancet 2008, 372, 216–223. [Google Scholar] [CrossRef]
- Ostrowitzki, S.; Lasser, R.A.; Dorflinger, E.; Scheltens, P.; Barkhof, F.; Nikolcheva, T.; Ashford, E.; Retout, S.; Hofmann, C.; Delmar, P.; et al. A Phase III Randomized Trial of Gantenerumab in Prodromal Alzheimer’s Disease. Alzheimer’s Res. Ther. 2017, 9, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Erten-Lyons, D.; Woltjer, R.L.; Dodge, H.; Nixon, R.; Vorobik, R.; Calvert, J.F.; Leahy, M.; Montine, T.; Kaye, J. Factors Associated with Resistance to Dementia despite High Alzheimer Disease Pathology. Neurology 2009, 72, 354–360. [Google Scholar] [CrossRef]
- Bennett, D.A.; Schneider, J.A.; Arvanitakis, Z.; Kelly, J.F.; Aggarwal, N.T.; Shah, R.C.; Wilson, R.S. Neuropathology of Older Persons without Cognitive Impairment from Two Community-Based Studies. Neurology 2006, 66, 1837–1844. [Google Scholar] [CrossRef]
- McKhann, G.M. Clinical and Pathological Diagnosis of Frontotemporal Dementia. Arch. Neurol. 2001, 58, 1803. [Google Scholar] [CrossRef]
- McKeith, I.G.; Dickson, D.W.; Lowe, J.; Emre, M.; O’Brien, J.T.; Feldman, H.; Cummings, J.; Duda, J.E.; Lippa, C.; Perry, E.K.; et al. Diagnosis and Management of Dementia with Lewy Bodies: Third Report of the DLB Consortium. Neurology 2005, 65, 1863–1872. [Google Scholar] [CrossRef]
- Rasmussen, I.J.; Thomassen, J.Q.; Frikke-Schmidt, R. Impact of Metabolic Dysfunction on Cognition in Humans. Curr. Opin. Lipidol. 2021, 32, 55–61. [Google Scholar] [CrossRef]
- Nordestgaard, L.T.; Christoffersen, M.; Afzal, S.; Nordestgaard, B.G.; Tybjærg-Hansen, A.; Frikke-Schmidt, R. Triglycerides as a Shared Risk Factor between Dementia and Atherosclerotic Cardiovascular Disease: A Study of 125 727 Individuals. Clin. Chem. 2021, 67, 245–255. [Google Scholar] [CrossRef]
- Rasmussen, I.J.; Rasmussen, K.L.; Nordestgaard, B.G.; Tybjærg-Hansen, A.; Frikke-Schmidt, R. Impact of Cardiovascular Risk Factors and Genetics on 10-Year Absolute Risk of Dementia—Risk Charts for Targeted Prevention. Eur. Heart J. 2020, in press. [CrossRef]
- Iturria-Medina, Y.; Sotero, R.C.; Toussaint, P.J.; Mateos-Pérez, J.M.; Evans, A.C.; Weiner, M.W.; Aisen, P.; Petersen, R.; Jack, C.R.; Jagust, W.; et al. Early Role of Vascular Dysregulation on Late-Onset Alzheimer’s Disease Based on Multifactorial Data-Driven Analysis. Nat. Commun. 2016, 7. [Google Scholar] [CrossRef]
- Iturria-Medina, Y.; Carbonell, F.M.; Sotero, R.C.; Chouinard-Decorte, F.; Evans, A.C. Multifactorial Causal Model of Brain (Dis)Organization and Therapeutic Intervention: Application to Alzheimer’s Disease. Neuroimage 2017, 152, 60–77. [Google Scholar] [CrossRef]
- Stelzmann, R.A.; Norman Schnitzlein, H.; Reed Murtagh, F. An English Translation of Alzheimer’s 1907 Paper, “Über Eine Eigenartige Erkankung Der Hirnrinde. ” Clin. Anat. 1995, 8, 429–431. [Google Scholar] [CrossRef]
- Roman, G.C.; Tatemichi, T.K.; Erkinjuntti, T.; Cummings, J.L.; Masdeu, J.C.; Garcia, J.H. Vascular Dementia: Diagnostic Criteria for Research Studies: Report of the NINDS-AIREN International Workshop Vascular Dementia: Diagnostic Criteria for Research Studies: Report of the NINDS-AIREN International Workshop 1993. Neurology 1993, 43, 250–260. [Google Scholar] [CrossRef] [PubMed]
- Salminen, A.; Kauppinen, A.; Kaarniranta, K. Hypoxia/Ischemia Activate Processing of Amyloid Precursor Protein: Impact of Vascular Dysfunction in the Pathogenesis of Alzheimer’s Disease. J. Neurochem. 2017, 140, 536–549. [Google Scholar] [CrossRef] [PubMed]
- Braak, H.; Braak, E. Demonstration of Amyloid Deposits and Neurofibrillary Changes in Whole Brain Sections. Brain Pathol. 1991, 1, 213–216. [Google Scholar] [CrossRef]
- Lee, C.M.Y.; Woodward, M.; Batty, G.D.; Beiser, A.S.; Bell, S.; Berr, C.; Bjertness, E.; Chalmers, J.; Clarke, R.; Dartigues, J.-F.; et al. Association of Anthropometry and Weight Change with Risk of Dementia and Its Major Subtypes: A Meta-Analysis Consisting 2.8 Million Adults with 57 294 Cases of Dementia. Obes. Rev. 2020, 21, 1–14. [Google Scholar] [CrossRef]
- Østergaard, S.D.; Mukherjee, S.; Sharp, S.J.; Proitsi, P.; Lotta, L.A.; Day, F.; Perry, J.R.B.; Boehme, K.L.; Walter, S.; Kauwe, J.S.; et al. Associations between Potentially Modifiable Risk Factors and Alzheimer Disease: A Mendelian Randomization Study. PLoS Med. 2015, 12, e1001841. [Google Scholar] [CrossRef]
- Nordestgaard, L.T.; Tybjærg-Hansen, A.; Nordestgaard, B.G.; Frikke-Schmidt, R. Body Mass Index and Risk of Alzheimer’s Disease: A Mendelian Randomization Study of 399,536 Individuals. J. Clin. Endocrinol. Metab. 2017, 102, 2310–2320. [Google Scholar] [CrossRef]
- Ikeda, M.; Brown, J.; Holland, A.J.; Fukuhara, R.; Hodges, J.R. Changes in Appetite, Food Preference, and Eating Habits in Frontotemporal Dementia and Alzheimer’s Disease. J. Neurol. Neurosurg. Psychiatry 2002, 73, 371–376. [Google Scholar] [CrossRef]
- Morris, C.H.; Hope, R.A.; Fairburn, C.G. Eating Habits in Dementia. A Descriptive Study. Br. J. Psychiatry 1989, 154, 801–806. [Google Scholar] [CrossRef]
- Wysokiński, A.; Sobów, T.; Kłoszewska, I.; Kostka, T. Mechanisms of the Anorexia of Aging—A Review. Age 2015, 37, 81. [Google Scholar] [CrossRef]
- Varbo, A.; Benn, M.; Smith, G.D.; Timpson, N.J.; Tybjaerg-Hansen, A.; Nordestgaard, B.G.; Tybjærg-Hansen, A.; Nordestgaard, B.G. Remnant Cholesterol, Low-Density Lipoprotein Cholesterol, and Blood Pressure as Mediators from Obesity to Ischemic Heart Disease. Circ. Res. 2015, 116, 665–673. [Google Scholar] [CrossRef] [Green Version]
- Fitzpatrick, A.L.; Kuller, L.H.; Lopez, O.L.; Diehr, P.; O’Meara, E.S.; Longstreth, W.T.J.; Luchsinger, J.A. Midlife and Late-Life Obesity and the Risk of Dementia: Cardiovascular Health Study. Arch Neurol 2009, 66, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Qizilbash, N.; Gregson, J.; Johnson, M.E.; Pearce, N.; Douglas, I.; Wing, K.; Evans, S.J.W.; Pocock, S.J. BMI and Risk of Dementia in Two Million People over Two Decades: A Retrospective Cohort Study. Lancet Diabetes Endocrinol. 2015, 8587, 1–6. [Google Scholar] [CrossRef]
- Singh-Manoux, A.; Dugravot, A.; Shipley, M.; Brunner, E.J.; Elbaz, A.; Sabia, S.; Kivimaki, M. Obesity Trajectories and Risk of Dementia: 28 Years of Follow-up in the Whitehall II Study. Alzheimer’s Dement. 2018, 14, 178–186. [Google Scholar] [CrossRef]
- Mukherjee, S.; Walter, S.; Kauwe, J.S.K.; Saykin, A.J.; Bennett, D.A.; Larson, E.B.; Crane, P.K.; Glymour, M.M. Genetically Predicted Body Mass Index and Alzheimer’s Disease–Related Phenotypes in Three Large Samples: Mendelian Randomization Analyses. Alzheimer’s Dement. 2015, 11, 1439–1451. [Google Scholar] [CrossRef] [PubMed]
- Timpson, N.J.; Harbord, R.; Smith, G.D.; Zacho, J.; Tybjærg-Hansen, A.; Nordestgaard, B.G. Does Greater Adiposity Increase Blood Pressure and Hypertension Risk?: Mendelian Randomization Using the FTO/MC4R Genotype. Hypertension 2009, 54, 84–90. [Google Scholar] [CrossRef]
- Nordestgaard, B.G.; Varbo, A. Triglycerides and Cardiovascular Disease. Lancet 2014, 384, 626–635. [Google Scholar] [CrossRef]
- Anstey, K.J.; Ashby-Mitchell, K.; Peters, R. Updating the Evidence on the Association between Serum Cholesterol and Risk of Late-Life Dementia: Review and Meta-Analysis. J. Alzheimer’s Dis. 2017, 56, 215–228. [Google Scholar] [CrossRef]
- Raffaitin, C.; Gin, H.; Empana, J.P.; Helmer, C.; Berr, C.; Tzourio, C.; Portet, F.; Dartigues, J.F.; Alpérovitch, A.; Barberger-Gateau, P. Metabolic Syndrome and Risk for Incident Alzheimer’s Disease or Vascular Dementia. Diabetes Care 2009, 32, 169–174. [Google Scholar] [CrossRef]
- Reitz, C.; Tang, M.X.; Luchsinger, J.; Mayeux, R. Relation of Plasma Lipids to Alzheimer’s Disease and Vascular Dementia. Arch. Neurol. 2005, 10, 135–141. [Google Scholar]
- Wang, P.; Zhang, H.; Wang, Y.; Zhang, M.; Zhou, Y. Plasma Cholesterol in Alzheimer’s Disease and Frontotemporal Dementia. Transl. Neurosci. 2020, 11, 116–123. [Google Scholar] [CrossRef]
- Varbo, A.; Freiberg, J.J.; Nordestgaard, B.G. Remnant Cholesterol and Myocardial Infarction in Normal Weight, Overweight, and Obese Individuals from the Copenhagen General Population Study. Clin. Chem. 2018, 64, 219–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pedersen, S.B.; Varbo, A.; Langsted, A.; Nordestgaard, B.G. Chylomicronemia Risk Factors Ranked by Importance for the Individual and Community in 108 711 Women and Men. J. Intern. Med. 2018, 283, 392–404. [Google Scholar] [CrossRef] [PubMed]
- Varbo, A.; Nordestgaard, B.G.; Tybjærg-Hansen, A.; Schnohr, P.; Jensen, G.B.; Benn, M. Nonfasting Triglycerides, Cholesterol, and Ischemic Stroke in the General Population. Ann. Neurol. 2011, 69, 628–634. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the Management of Dyslipidaemias: Lipid Modification to Reduce Cardiovascular Risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Jørgensen, A.B.; Frikke-Schmidt, R.; Nordestgaard, B.G.; Tybjærg-Hansen, A. Loss-of-Function Mutations in APOC3 and Risk of Ischemic Vascular Disease. N. Engl. J. Med. 2014, 371, 32–41. [Google Scholar] [CrossRef]
- Pedersen, S.B.; Langsted, A.; Nordestgaard, B.G. Nonfasting Mild-to-Moderate Hypertriglyceridemia and Risk of Acute Pancreatitis. JAMA Intern. Med. 2016, 176, 1834–1842. [Google Scholar] [CrossRef]
- Sarwar, N.; Sandhu, M.S.; Ricketts, S.L.; Butterworth, A.S.; Di Angelantonio, E.; Matthijs Boekholdt, S.; Ouwehand, W.; Watkins, H.; Samani, N.J.; Saleheen, D.; et al. Triglyceride-Mediated Pathways and Coronary Disease: Collaborative Analysis of 101 Studies. Lancet 2010, 375, 1634–1639. [Google Scholar] [CrossRef]
- Stitziel, N.O.; Stirrups, K.E.; Masca, N.G.D.; Erdmann, J.; Ferrario, P.G.; König, I.R.; Weeke, P.E.; Webb, T.R.; Auer, P.L.; Schick, U.M.; et al. Coding Variation in ANGPTL4, LPL, and SVEP1 and the Risk of Coronary Disease. N. Engl. J. Med. 2016, 374, 1134–1144. [Google Scholar] [CrossRef]
- Jørgensen, A.B.; Frikke-Schmidt, R.; West, A.S.; Grande, P.; Nordestgaard, B.G.; Tybjærg-Hansen, A. Genetically Elevated Non-Fasting Triglycerides and Calculated Remnant Cholesterol as Causal Risk Factors for Myocardial Infarction. Eur. Heart J. 2013, 34, 1826–1833. [Google Scholar] [CrossRef]
- Varbo, A.; Benn, M.; Tybjærg-Hansen, A.; Nordestgaard, B.G. Elevated Remnant Cholesterol Causes Both Low-Grade Inflammation and Ischemic Heart Disease, Whereas Elevated Low-Density Lipoprotein Cholesterol Causes Ischemic Heart Disease without Inflammation. Circulation 2013, 128, 1298–1309. [Google Scholar] [CrossRef]
- Dewey, F.E.; Gusarova, V.; Dunbar, R.L.; O’Dushlaine, C.; Schurmann, C.; Gottesman, O.; McCarthy, S.; Van Hout, C.V.; Bruse, S.; Dansky, H.M.; et al. Genetic and Pharmacologic Inactivation of ANGPTL3 and Cardiovascular Disease. N. Engl. J. Med. 2017, 377, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Nordestgaard, B.G. Triglyceride-Rich Lipoproteins and Atherosclerotic Cardiovascular Disease: New Insights from Epidemiology, Genetics, and Biology. Circ. Res. 2016, 118, 547–563. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, M.; Wootton, R.; Nordestgaard, B.G.; Baskerville, P.; Lumley, J.S.; La Ville, A.E.; Quiney, J.; Lewis, B. Quantitative Studies of Transfer in Vivo of Low Density, Sf 12-60, and Sf 60-400 Lipoproteins between Plasma and Arterial Intima in Humans. Arterioscler. Thromb. 1991, 11, 569–577. [Google Scholar] [CrossRef] [PubMed]
- Nordestgaard, B.G.; Wootton, R.; Lewis, B. Selective Retention of VLDL, IDL, and LDL in the Arterial Intima of Genetically Hyperlipidemic Rabbits in Vivo: Molecular Size as a Determinant of Fractional Loss from the Intima-Inner Media. Arterioscler. Thromb. Vasc. Biol. 1995, 15, 534–542. [Google Scholar] [CrossRef]
- Yaffe, K.; Lindquist, K.; Simonsick, E.M.; Harris, T.; Shorr, R.I.; Tylavsky, F.A.; Newman, A.B. The Metabolic Syndrome, Inflammation, and Risk of Cognitive Decline. JAMA 2016, 292, 2237–2242. [Google Scholar] [CrossRef]
- Launer, L.J.; White, L.R.; Petrovitch, H.; Ross, G.W.; Curb, J.D. Cholesterol and Neuropathologic Markers of AD: A Population-Based Autopsy Study (Multiple Letters). Neurology 2002, 59, 788–789. [Google Scholar] [CrossRef]
- Kjeldsen, E.W.; Thomassen, J.Q.; Juul Rasmussen, I.; Nordestgaard, B.G.; Tybjærg-Hansen, A.; Frikke-Schmidt, R. Plasma High-Density Lipoprotein Cholesterol and Risk of Dementia: Observational and Genetic Studies. Cardiovasc. Res. 2021, 118, 1330–1343. [Google Scholar] [CrossRef]
- Corder, E.; Saunders, A.; Strittmatter, W.; Schmechel, D.; Gaskell, P.; Small, G.; Roses, A.; Haines, J.; Pericak-Vance, M. Gene Dose of Apolipoprotein E Type 4 Allele and the Risk of Alzheimer’s Disease in Late Onset Families. Science 1993, 261, 921–923. [Google Scholar] [CrossRef]
- Rasmussen, K.L.; Tybjærg-Hansen, A.; Nordestgaard, B.G.; Frikke-Schmidt, R. Plasma Apolipoprotein E Levels and Risk of Dementia: A Mendelian Randomization Study of 106,562 Individuals. Alzheimer’s Dement. 2018, 14, 71–80. [Google Scholar] [CrossRef]
- Nordestgaard, L.T.; Tybjærg-Hansen, A.; Nordestgaard, B.G.; Frikke-Schmidt, R. Loss-of-Function Mutation in ABCA1 and Risk of Alzheimer’s Disease and Cerebrovascular Disease. Alzheimer’s Dement. 2015, 11, 1430–1438. [Google Scholar] [CrossRef]
- Rasmussen, K.L.; Tybjærg-Hansen, A.; Nordestgaard, B.G.; Frikke-schmidt, R. Plasma Levels of Apolipoprotein E, APOE Genotype, and All-Cause and Cause-Specific Mortality in 105 949 Individuals from a White General Population Cohort. Eur. Heart J. 2019, 40, 2813–2824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nordestgaard, L.T.; Christoffersen, M.; Lauridsen, B.K.; Afzal, S.; Nordestgaard, B.G.; Frikke-schmidt, R.; Tybjærg-Hansen, A. Long-Term Benefits and Harms Associated with Genetic Cholesteryl Ester Transfer Protein Deficiency in the General Population. JAMA Cardiol. 2022, 7, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Frikke-Schmidt, R. HDL Cholesterol and Apolipoprotein A-I Concentrations and Risk of Atherosclerotic Cardiovascular Disease: Human Genetics to Unravel Causality. Atherosclerosis 2020, 299, 53–55. [Google Scholar] [CrossRef]
- Kjeldsen, E.W.; Nordestgaard, L.T.; Frikke-Schmidt, R. Hdl Cholesterol and Non-Cardiovascular Disease: A Narrative Review. Int. J. Mol. Sci. 2021, 22, 4547. [Google Scholar] [CrossRef]
- Bonarek, M.; Barberger-Gateau, P.; Letenneur, L.; Deschamps, V.; Iron, A.; Dubroca, B.; Dartigues, J.F. Relationships between Cholesterol, Apolipoprotein E Polymorphism and Dementia: A Cross-Sectional Analysis from the PAQUID Study. Neuroepidemiology 2000, 19, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Madsen, C.M.; Varbo, A.; Tybjærg-Hansen, A.; Frikke-Schmidt, R.; Nordestgaard, B.G. U-Shaped Relationship of HDL and Risk of Infectious Disease: Two Prospective Population-Based Cohort Studies. Eur. Heart J. 2018, 39, 1181–1190. [Google Scholar] [CrossRef]
- Reitz, C.; Tang, M.X.; Schupf, N.; Manly, J.J.; Mayeux, R.; Luchsinger, J.A. Association of Higher Levels of High-Density Lipoprotein Cholesterol in Elderly Individuals and Lower Risk of Late-Onset Alzheimer Disease. Arch. Neurol. 2010, 67, 1491–1497. [Google Scholar] [CrossRef]
- Benn, M.; Nordestgaard, B.G.; Frikke-Schmidt, R.; Tybjærg-Hansen, A. Low LDL Cholesterol, PCSK9 and HMGCR Genetic Variation, and Risk of Alzheimer’s Disease and Parkinson’s Disease: Mendelian Randomisation Study. BMJ 2017, 357, j1648. [Google Scholar] [CrossRef]
- Chu, C.S.; Tseng, P.T.; Stubbs, B.; Chen, T.Y.; Tang, C.H.; Li, D.J.; Yang, W.C.; Chen, Y.W.; Wu, C.K.; Veronese, N.; et al. Use of Statins and the Risk of Dementia and Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Sci. Rep. 2018, 8, 1–12. [Google Scholar] [CrossRef]
- Ference, B.A.; Ginsberg, H.N.; Graham, I.; Ray, K.K.; Packard, C.J.; Bruckert, E.; Hegele, R.A.; Krauss, R.M.; Raal, F.J.; Schunkert, H.; et al. Low-Density Lipoproteins Cause Atherosclerotic Cardiovascular Disease. 1. Evidence from Genetic, Epidemiologic, and Clinical Studies. A Consensus Statement Fromthe European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2017, 38, 2459–2472. [Google Scholar] [CrossRef]
- Borén, J.; John Chapman, M.; Krauss, R.M.; Packard, C.J.; Bentzon, J.F.; Binder, C.J.; Daemen, M.J.; Demer, L.L.; Hegele, R.A.; Nicholls, S.J.; et al. Low-Density Lipoproteins Cause Atherosclerotic Cardiovascular Disease: Pathophysiological, Genetic, and Therapeutic Insights: A Consensus Statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2020, 41, 2313–2330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mcguinness, B.; Craig, D.; Bullock, R.; Passmore, P. Statins for the Prevention of Dementia. Cochrane Database Syst. Rev. 2016, 2016. [Google Scholar] [CrossRef] [PubMed]
- Jack, C.R.; Wiste, H.J.; Therneau, T.M.; Weigand, S.D.; Knopman, D.S.; Mielke, M.M.; Lowe, V.J.; Vemuri, P.; Machulda, M.M.; Schwarz, C.G.; et al. Associations of Amyloid, Tau, and Neurodegeneration Biomarker Profiles with Rates of Memory Decline among Individuals Without Dementia. JAMA -J. Am. Med. Assoc. 2019, 321, 2316–2325. [Google Scholar] [CrossRef] [PubMed]
- Kuller, L.H. Statins, Lipids and Dementia? J. Clin. Lipidol. 2021, 15, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wen, J.; Zhang, Z. Statins Use and Risk of Dementia: A Dose–Response Meta Analysis. Medicine 2018, 97, e11304. [Google Scholar] [CrossRef] [PubMed]
- Tully, P.J.; Hanon, O.; Cosh, S.; Tzourio, C. Diuretic Antihypertensive Drugs and Incident Dementia Risk: A Systematic Review, Meta-Analysis and Meta-Regression of Prospective Studies. J. Hypertens. 2016, 34, 1027–1035. [Google Scholar] [CrossRef]
- Ding, J.; Davis-Plourde, K.L.; Sedaghat, S.; Tully, P.J.; Wang, W.; Phillips, C.; Pase, M.P.; Himali, J.J.; Gwen Windham, B.; Griswold, M.; et al. Antihypertensive Medications and Risk for Incident Dementia and Alzheimer’s Disease: A Meta-Analysis of Individual Participant Data from Prospective Cohort Studies. Lancet Neurol. 2020, 19, 61–70. [Google Scholar] [CrossRef]
- Thorin, E. Hypertension and Alzheimer Disease: Another Brick in the Wall of Awareness. Hypertension 2015, 65, 36–38. [Google Scholar] [CrossRef]
- McGrath, E.R.; Seshadri, S. Blood Pressure from Mid- to Late Life and Risk of Incident Dementia. Neurology 2018, 91, 149. [Google Scholar] [CrossRef]
- Abell, J.G.; Kivimäki, M.; Dugravot, A.; Tabak, A.G.; Fayosse, A.; Shipley, M.; Sabia, S.; Singh-Manoux, A. Association between Systolic Blood Pressure and Dementia in TheWhitehall II Cohort Study: Role of Age, Duration, and Threshold Used to Define Hypertension. Eur. Heart J. 2018, 39, 3119–3125. [Google Scholar] [CrossRef]
- Peters, R.; Warwick, J.; Anstey, K.J.; Anderson, C.S. Blood Pressure and Dementia. Neurology 2019, 92, 1017–1018. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.; Singh, A.; Rahman, S.O.; Habib, A.; Najmi, A.K. Calcium Channel Blocker Use Reduces Incident Dementia Risk in Elderly Hypertensive Patients: A Meta-Analysis of Prospective Studies. Neurosci. Lett. 2018, 671, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Delgado, J.; Bowman, K.; Ble, A.; Masoli, J.; Han, Y.; Henley, W.; Welsh, S.; Kuchel, G.A.; Ferrucci, L.; Melzer, D. Blood Pressure Trajectories in the 20 Years before Death. JAMA Intern. Med. 2018, 178, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Lane, C.A.; Barnes, J.; Nicholas, J.M.; Sudre, C.H.; Cash, D.M.; Parker, T.D.; Malone, I.B.; Lu, K.; James, S.N.; Keshavan, A.; et al. Associations between Blood Pressure across Adulthood and Late-Life Brain Structure and Pathology in the Neuroscience Substudy of the 1946 British Birth Cohort (Insight 46): An Epidemiological Study. Lancet Neurol. 2019, 18, 942–952. [Google Scholar] [CrossRef]
- Williamson, J.D.; Pajewski, N.M.; Auchus, A.P.; Bryan, R.N.; Chelune, G.; Cheung, A.K.; Cleveland, M.L.; Coker, L.H.; Crowe, M.G.; Cushman, W.C.; et al. Effect of Intensive vs Standard Blood Pressure Control on Probable Dementia: A Randomized Clinical Trial. JAMA -J. Am. Med. Assoc. 2019, 321, 553–561. [Google Scholar] [CrossRef]
- Thomassen, J.Q.; Tolstrup, J.S.; Benn, M.; Frikke-Schmidt, R. Type-2 Diabetes and Risk of Dementia: Observational and Mendelian Randomisation Studies in 1 Million Individuals. Epidemiol. Psychiatr. Sci. 2020. [Google Scholar] [CrossRef]
- Chatterjee, S.; Peters, S.A.E.; Woodward, M.; Arango, S.M.; Batty, G.D.; Beckett, N.; Beiser, A.; Borenstein, A.R.; Crane, P.K.; Haan, M.; et al. Type 2diabetes as a Risk Factor for Dementia in Women Compared with Men: A Pooled Analysis of 2.3 Million People Comprising More than 100,000 Cases of Dementia. Diabetes Care 2016, 39, 300–307. [Google Scholar] [CrossRef]
- Katon, W.; Pedersen, H.S.; Ribe, A.R.; Fenger-Grøn, M.; Davydow, D.; Waldorff, F.B.; Vestergaard, M. Effect of Depression and Diabetes Mellitus on the Risk for Dementia: A National Population-Based Cohort Study. JAMA Psychiatry 2015, 72, 612–619. [Google Scholar] [CrossRef]
- Lampignano, L.; Donghia, R.; Griseta, C.; Lagravinese, G.; Sciarra, S.; Zupo, R.; Castellana, F.; Bortone, I.; Guerra, V.; Tirelli, S.; et al. Liver Health and Dementia in an Italian Older Population: Findings From the Salus in Apulia Study. Front. Aging Neurosci. 2021, 13, 1–9. [Google Scholar] [CrossRef]
- Huang, T.; Behary, J.; Zekry, A. Non-Alcoholic Fatty Liver Disease: A Review of Epidemiology, Risk Factors, Diagnosis and Management. Intern. Med. J. 2020, 50, 1038–1047. [Google Scholar] [CrossRef]
- Labenz, C.; Kostev, K.; Kaps, L.; Galle, P.R.; Schattenberg, J.M. Incident Dementia in Elderly Patients with Nonalcoholic Fatty Liver Disease in Germany. Dig. Dis. Sci. 2021, 66, 3179–3185. [Google Scholar] [CrossRef] [PubMed]
- Shang, Y.; Lidman, L.; Hagström, H. Nonalcoholic Fatty Liver Disease and Risk of Dementia: A Population-Based Cohort Study. Neurology 2022. Ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Shang, Y.; Nasr, P.; Ekstedt, M.; Widman, L.; Stål, P.; Hultcrantz, R.; Kechagias, S.; Hagström, H. Non-Alcoholic Fatty Liver Disease Does Not Increase Dementia Risk Although Histology Data Might Improve Risk Prediction. JHEP Reports 2021, 3, 100218. [Google Scholar] [CrossRef] [PubMed]
- Kabir, M.T.; Uddin, M.S.; Zaman, S.; Begum, Y.; Ashraf, G.M.; Bin-Jumah, M.N.; Bungau, S.G.; Mousa, S.A.; Abdel-Daim, M.M. Molecular Mechanisms of Metal Toxicity in the Pathogenesis of Alzheimer’s Disease. Mol. Neurobiol. 2021, 58, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Behl, T.; Kaur, I.; Sehgal, A.; Kumar, A.; Uddin, M.S.; Bungau, S. The Interplay of ABC Transporters in Aβ Translocation and Cholesterol Metabolism: Implicating Their Roles in Alzheimer’s Disease. Mol. Neurobiol. 2021, 58, 1564–1582. [Google Scholar] [CrossRef]
- Kivimäki, M.; Singh-Manoux, A.; Pentti, J.; Sabia, S.; Nyberg, S.T.; Alfredsson, L.; Goldberg, M.; Knutsson, A.; Koskenvuo, M.; Koskinen, A.; et al. Physical Inactivity, Cardiometabolic Disease, and Risk of Dementia: An Individual-Participant Meta-Analysis. BMJ 2019, 365, l1495. [Google Scholar] [CrossRef]
- Rasmussen, I.J.; Rasmussen, K.L.; Thomassen, J.Q.; Schnohr, P.; Frikke-schmidt, R.; General, C.; Study, P.; Hospital, G.; Copenhagen, T.; Heart, C.; et al. Physical Activity in Leisure Time and at Work and Risk of Dementia—A Prospective Cohort Study of 117,616 Individuals. Atherosclerosis 2022, 1–25. [Google Scholar] [CrossRef]
- Livingston, G.; Sommerlad, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Ballard, C.; Banerjee, S.; Burns, A.; Cohen-Mansfield, J.; et al. Dementia Prevention, Intervention, and Care. Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef]
- Zotcheva, E.; Selbæk, G.; Bjertness, E.; Ernstsen, L.; Strand, B.H. Leisure-Time Physical Activity Is Associated with Reduced Risk of Dementia-Related Mortality in Adults with and without Psychological Distress: The Cohort of Norway. Front. Aging Neurosci. 2018, 10, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Sabia, S.; Fayosse, A.; Dumurgier, J.; Schnitzler, A.; Empana, J.P.; Ebmeier, K.P.; Dugravot, A.; Kivimäki, M.; Singh-Manoux, A. Association of Ideal Cardiovascular Health at Age 50 with Incidence of Dementia: 25 Year Follow-up of Whitehall II Cohort Study. BMJ 2019, 366, 1–10. [Google Scholar] [CrossRef]
- Hörder, H.; Johansson, L.; Guo, X.; Grimby, G.; Kern, S.; Östling, S.; Skoog, I. Midlife Cardiovascular Fitness and Dementia. Neurology 2018, 90, e1298–e1305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Northey, J.M.; Cherbuin, N.; Pumpa, K.L.; Smee, D.J.; Rattray, B. Exercise Interventions for Cognitive Function in Adults Older than 50: A Systematic Review with Meta-Analysis. Br. J. Sports Med. 2018, 52, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Song, D.; Yu, D.S.F.; Li, P.W.C.; Lei, Y. The Effectiveness of Physical Exercise on Cognitive and Psychological Outcomes in Individuals with Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Int. J. Nurs. Stud. 2018, 79, 155–164. [Google Scholar] [CrossRef] [PubMed]
- De Souto Barreto, P.; Demougeot, L.; Vellas, B.; Rolland, Y. Exercise Training for Preventing Dementia, Mild Cognitive Impairment, and Clinically Meaningful Cognitive Decline: A Systematic Review and Meta-Analysis. J. Gerontol. -Ser. A Biol. Sci. Med. Sci. 2018, 73, 1504–1511. [Google Scholar] [CrossRef] [PubMed]
- WHO. Risk Reduction Of Cognitive Decline And Dementia; WHO: Geneva, Switzerland, 2019; ISBN 9789241550543. [Google Scholar]
- Ngandu, T.; Lehtisalo, J.; Solomon, A.; Levälahti, E.; Ahtiluoto, S.; Antikainen, R.; Bäckman, L.; Hänninen, T.; Jula, A.; Laatikainen, T.; et al. A 2 Year Multidomain Intervention of Diet, Exercise, Cognitive Training, and Vascular Risk Monitoring versus Control to Prevent Cognitive Decline in at-Risk Elderly People (FINGER): A Randomised Controlled Trial. Lancet 2015, 385, 2255–2263. [Google Scholar] [CrossRef]
- Rosenberg, A.; Ngandu, T.; Rusanen, M.; Antikainen, R.; Bäckman, L.; Havulinna, S.; Hänninen, T.; Laatikainen, T.; Lehtisalo, J.; Levälahti, E.; et al. Multidomain Lifestyle Intervention Benefits a Large Elderly Population at Risk for Cognitive Decline and Dementia Regardless of Baseline Characteristics: The FINGER Trial. Alzheimer’s Dement. 2018, 14, 263–270. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, D.; Liu, Y.; Sun, X.; Han, C.; Wang, B.; Ren, Y.; Zhou, J.; Zhao, Y.; Shi, Y.; et al. Dose-Response Association between Physical Activity and Incident Hypertension: A Systematic Review and Meta-Analysis of Cohort Studies. Hypertension 2017, 69, 813–820. [Google Scholar] [CrossRef]
- Owen, C.G.; Nightingale, C.M.; Rudnicka, A.R.; Sattar, N.; Cook, D.G.; Ekelund, U.; Whincup, P.H. Physical Activity, Obesity and Cardiometabolic Risk Factors in 9- to 10-Year-Old UK Children of White European, South Asian and Black African-Caribbean Origin: The Child Heart and Health Study in England (CHASE). Diabetologia 2010, 53, 1620–1630. [Google Scholar] [CrossRef]
- Norton, S.; Matthews, F.E.; Barnes, D.E.; Yaffe, K.; Brayne, C. Potential for Primary Prevention of Alzheimer’s Disease: An Analysis of Population-Based Data. Lancet Neurol. 2014, 13, 788–794. [Google Scholar] [CrossRef]
- Choi, D.; Choi, S.; Park, S.M. Effect of Smoking Cessation on the Risk of Dementia: A Longitudinal Study. Ann. Clin. Transl. Neurol. 2018, 5, 1192–1199. [Google Scholar] [CrossRef]
- Nordestgaard, A.T.; Nordestgaard, B.G.; Frikke-Schmidt, R.; Juul Rasmussen, I.; Bojesen, S.E. Self-Reported and Genetically Predicted Coffee Consumption and Smoking in Dementia: A Mendelian Randomization Study. Atherosclerosis 2022, 348, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.; Luo, Y.; Roberts, A.R. Secondhand Smoke and Women’s Cognitive Function in China. Am. J. Epidemiol. 2018, 187, 911–918. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-C.H.; Zhao, Y.; Lee, C.-W.; Ganguli, M. Smoking, Death, and Alzheimer’s Disease: A Case of Competing Risks. Alzheimer Dis Assoc Disord. 2012, 26, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Coca, A. Hypertension and Brain Damage; Springer: Berlin/Heidelberg, Germany, 2016; ISBN 0370-629X. [Google Scholar]
- Ahrens, J.; Anthony, M.; Asahara, T.; Aviram, M.; Bellosta, S.; Bernini, F.; Bode, C. Atherosclerosis: Diet and Drugs; Springer: Berlin/Heidelberg, Germany, 2005; Volume 170, ISBN 9783540225690. [Google Scholar]
- Kjeldsen, E.W.; Thomassen, J.Q.; Rasmussen, K.L.; Tybjærg-Hansen, A.; Nordestgaard, B.G.; Frikke-Schmidt, R. Adherence to Dietary Guidelines and Risk of Dementia: A Prospective Cohort Study of 94,184 Individuals. Epidemiol. Psychiatr. Sci. 2022. submitted. [Google Scholar] [CrossRef]
- Van Den Brink, A.C.; Brouwer-Brolsma, E.M.; Berendsen, A.A.M.; Van De Rest, O. The Mediterranean, Dietary Approaches to Stop Hypertension (DASH), and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) Diets Are Associated with Less Cognitive Decline and a Lower Risk of Alzheimer’s Disease-A Review. Adv. Nutr. 2019, 10, 1040–1065. [Google Scholar] [CrossRef]
- Féart, C.; Samieri, C.; Rondeau, V.; Amieva, H.; Portet, F.; Dartigues, J.F.; Scarmeas, N.; Barberger-Gateau, P. Adherence to a Mediterranean Diet, Cognitive Decline, and Risk of Dementia. JAMA -J. Am. Med. Assoc. 2009, 302, 638–648. [Google Scholar] [CrossRef]
- Morris, M.C.; Tangney, C.C.; Wang, Y.; Sacks, F.M.; Barnes, L.L.; Bennett, D.A.; Aggarwal, N.T. MIND Diet Slows Cognitive Decline with Ageing. Alzheimer’s Dement. 2015, 11, 1015–1022. [Google Scholar] [CrossRef] [PubMed]
- Harring, B.; Wu, C.; Mossavar-Rahmani, Y.; Snetselaar, L.; Brunner, R.; Wallace, R.B.; Neuhouser, M.L.; Wassertheil-Smoller, S. No Association between Dietary Patterns and Risk for Cognitive Decline in Older Women with Nine-Year Follow-up: Data from the Women’s Health Initiative Memory Study. Physiol. Behav. 2016, 116, 921–930. [Google Scholar] [CrossRef]
- Tektonidis, T.G.; Åkesson, A.; Gigante, B.; Wolk, A.; Larsson, S.C. A Mediterranean Diet and Risk of Myocardial Infarction, Heart Failure and Stroke: A Population-Based Cohort Study. Atherosclerosis 2015, 243, 93–98. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Cryan, J.F.; O’Riordan, K.J.; Sandhu, K.; Peterson, V.; Dinan, T.G. The Gut Microbiome in Neurological Disorders. Lancet Neurol. 2020, 19, 179–194. [Google Scholar] [CrossRef]
- Cattaneo, A.; Cattane, N.; Galluzzi, S.; Provasi, S.; Lopizzo, N.; Festari, C.; Ferrari, C.; Guerra, U.P.; Paghera, B.; Muscio, C.; et al. Association of Brain Amyloidosis with Pro-Inflammatory Gut Bacterial Taxa and Peripheral Inflammation Markers in Cognitively Impaired Elderly. Neurobiol. Aging 2017, 49, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Roubaud-Baudron, C.; Krolak-Salmon, P.; Quadrio, I.; Mégraud, F.; Salles, N. Impact of Chronic Helicobacter Pylori Infection on Alzheimer’s Disease: Preliminary Results. Neurobiol. Aging 2012, 33, 1009.e11–1009.e19. [Google Scholar] [CrossRef] [PubMed]
- Sochocka, M.; Donskow-Łysoniewska, K.; Diniz, B.S.; Kurpas, D.; Brzozowska, E.; Leszek, J. The Gut Microbiome Alterations and Inflammation-Driven Pathogenesis of Alzheimer’s Disease—A Critical Review. Mol. Neurobiol. 2019, 56, 1841–1851. [Google Scholar] [CrossRef]
- Cani, P.D.; Bibiloni, R.; Knauf, C.; Neyrinck, A.M.; Delzenne, N.M. Changes in Gut Microbiota Control Metabolic Diet–Induced Obesity and Diabetes in Mice. Diabetes 2008, 57, 1470–1481. [Google Scholar] [CrossRef] [PubMed]
- Aron, R.A.C.; Abid, A.; Vesa, C.M.; Nechifor, A.C.; Behl, T.; Ghitea, T.C.; Munteanu, M.A.; Fratila, O.; Andronie-Cioara, F.L.; Toma, M.M.; et al. Recognizing the Benefits of Pre-/Probiotics in Metabolic Syndrome and Type 2 Diabetes Mellitus Considering the Influence of Akkermansia Muciniphila as a Key Gut Bacterium. Microorganisms 2021, 9, 618. [Google Scholar] [CrossRef]
- Claesson, M.J.; Jeffery, I.B.; Conde, S.; Power, S.E.; O’connor, E.M.; Cusack, S.; Harris, H.M.B.; Coakley, M.; Lakshminarayanan, B.; O’sullivan, O.; et al. Gut Microbiota Composition Correlates with Diet and Health in the Elderly. Nature 2012, 488, 178–184. [Google Scholar] [CrossRef]
- Prince, M.; Jackson, J. World Alzheimer Report 2009; Alzheimer’s Disease International: London, UK, 2009; pp. 1–96. [Google Scholar]
- Van Duijn, C.M.; de Knijff, P.; Cruts, M.; Wehnert, A.; Havekes, L.M.; Hofman, A.; Van Broeckhoven, C. Apolipoprotein E4 Allele in a Population–Based Study of Early–Onset Alzheimer’s Disease. Nat. Genet. 1994, 7, 74–78. [Google Scholar] [CrossRef]
- Mastana, S.S.; Calderon, R.; Pena, J.; Reddy, P.H.; Papiha, S.S. Anthropology of the Apolipoprotein e (Apo E) Gene: Low Frequency of Apo E4 Allele in Basques and in Tribal (Baiga) Populations of India. Ann. Hum. Biol. 1998, 25, 137–143. [Google Scholar] [CrossRef]
- Lalli, M.A.; Bettcher, B.M.; Arcila, M.L.; Garcia, G.; Guzman, C.; Madrigal, L.; Ramirez, L.; Acosta-Uribe, J.; Baena, A.; Wojta, K.J.; et al. Whole-Genome Sequencing Suggests a Chemokine Gene Cluster That Modifies Age at Onset in Familial Alzheimer’s Disease. Mol. Psychiatry 2015, 20, 1294–1300. [Google Scholar] [CrossRef]
- Chabriat, H.; Joutel, A.; Dichgans, M.; Tournier-Lasserve, E.; Bousser, M.G. Cadasil. Lancet Neurol. 2009, 8, 643–653. [Google Scholar] [CrossRef]
- Guerreiro, R.J.; Lohman, E.; Kinsella, E.; Bras, J.M.; Luu, N.; Gurulian, N. Exome Sequencing Reveals an Unexpected Genetic Cause of Disease: NOTCH3 Mutation in a Turkish Family with Alzheimer’s Disease. Neurobiol Aging. 2012, 33, 1008.e17–1008.e23. [Google Scholar] [CrossRef]
- Pottier, C.; Hannequin, D.; Coutant, S.; Rovelet-Lecrux, A.; Wallon, D.; Rousseau, S.; Legallic, S.; Paquet, C.; Bombois, S.; Pariente, J.; et al. High Frequency of Potentially Pathogenic SORL1 Mutations in Autosomal Dominant Early-Onset Alzheimer Disease. Mol. Psychiatry 2012, 17, 875–879. [Google Scholar] [CrossRef]
- Lardenoije, R.; Iatroua, A.; Kenis, G.; Kompotisb, K.; Steinbuscha, H.W.M.; Mastroenia, D.; Colemanc, P.; Lemered, C.A.; Hof, P.R.; van den Hove, D.L.A.; et al. The Epigenetics of Aging and Neurodegeneration. Prog Neurobiol. 2015, 131, 21–64. [Google Scholar] [CrossRef] [PubMed]
- Seshadri, S.; Fitzpatrick, A.L.; Ikram, A.; DeStafano, A.L.; Gudnason, V.; Boada, M.; Bis, J.C.; Smith, A.V.; Carrasquillo, M.M.; Lambert, J.C.; et al. Genome-Wide Analysis of Genetic Loci Associated With Alzheimer Disease. J. Am. Med. Assoc. 2010, 303, 1832–1840. [Google Scholar] [CrossRef] [PubMed]
- Lambert, J.C.; Ibrahim-Verbaas, C.A.; Harold, D.; Naj, A.C.; Sims, R.; Bellenguez, C.; Jun, G.; DeStefano, A.L.; Bis, J.C.; Beecham, G.W.; et al. Meta-Analysis of 74,046 Individuals Identifies 11 New Susceptibility Loci for Alzheimer’s Disease. Supplementary Information. Nat. Genet. 2013, 45, 1452–1458. [Google Scholar] [CrossRef]
- Kunkle, B.W.; Grenier-Boley, B.; Sims, R.; Bis, J.C.; Damotte, V.; Naj, A.C.; Boland, A.; Vronskaya, M.; van der Lee, S.J.; Amlie-Wolf, A.; et al. Genetic Meta-Analysis of Diagnosed Alzheimer’s Disease Identifies New Risk Loci and Implicates Aβ, Tau, Immunity and Lipid Processing. Nat. Genet. 2019, 51, 414–430. [Google Scholar] [CrossRef]
- Bellenguez, C.; Küçükali, F.; Jansen, I.E.; Kleineidam, L.; Moreno-Grau, S.; Amin, N.; Naj, A.C.; Campos-Martin, R.; Grenier-Boley, B.; Andrade, V.; et al. New Insights into the Genetic Etiology of Alzheimer’s Disease and Related Dementias. Nat. Genet. 2022, 54, 412–436. [Google Scholar] [CrossRef]
- Karch, C.M.; Jeng, A.T.; Nowotny, P.; Cady, J.; Cruchaga, C.; Goate, A.M. Expression of Novel Alzheimer’s Disease Risk Genes in Control and Alzheimer’s Disease Brains. PLoS ONE 2012, 7, e50976. [Google Scholar] [CrossRef]
- Bettens, K.; Sleegers, K.; Van Broeckhoven, C. Genetic Insights in Alzheimer’s Disease. Lancet Neurol. 2013, 12, 92–104. [Google Scholar] [CrossRef]
- Song, Y.; Stampfer, M.J.; Liu, S. Meta-Analysis: Apolipoprotein E Genotypes and Risk for Coronary Heart Disease. Ann. Intern. Med. 2004, 141, 137–147. [Google Scholar] [CrossRef]
- Hollingworth, P.; Harold, D.; Sims, R.; Gerrish, A.; Lambert, C.; Carrasquillo, M.M.; Abraham, R.; Marian, L.; Pahwa, J.S.; Moskvina, V.; et al. Common Variants in ABCA7, MS4A6A/MS4A4E, EPHA1, CD33 and CD2AP Are Associated with Alzheimer’s Disease. Nat. Genet. 2011, 43, 429–435. [Google Scholar] [CrossRef]
- Jonsson, T.; Stefansson, H.; Steinberg, S.; Jonsdottir, I.; Jonsson, P.V.; Snaedal, J.; Bjornsson, S.; Huttenlocher, J.; Levey, A.I.; Lah, J.J.; et al. Variant of TREM2 Associated with the Risk of Alzheimer’s Disease. N. Engl. J. Med. 2013, 368, 107–116. [Google Scholar] [CrossRef]
- Guerreiro, R.; Wojtas, A.; Bras, J.; Carrasquillo, M.; Rogaeva, E.; Majounie, E.; Cruchaga, C.; Sassi, C.; Kauwe, J.S.K.; Younkin, S.; et al. TREM2 Variants in Alzheimer’s Disease. N. Engl. J. Med. 2013, 368, 117–127. [Google Scholar] [CrossRef]
- Nordestgaard, L.T.; Tybjærg-Hansen, A.; Rasmussen, K.L.; Nordestgaard, B.G.; Frikke-Schmidt, R. Genetic Variation in Clusterin and Risk of Dementia and Ischemic Vascular Disease in the General Population—Cohort Studies and Meta-Analyses of 362,338 Individuals. BMC Med. 2018, 16, 1–11. [Google Scholar] [CrossRef]
- Juul Rasmussen, I.; Tybjærg-Hansen, A.; Rasmussen, K.L.; Nordestgaard, B.G.; Frikke-Schmidt, R. Blood–Brain Barrier Transcytosis Genes, Risk of Dementia and Stroke: A Prospective Cohort Study of 74,754 Individuals. Eur. J. Epidemiol. 2019, 34, 579–590. [Google Scholar] [CrossRef]
- Miwa, Y.; Takiuchi, S.; Kamide, K.; Yoshii, M.; Horio, T.; Tanaka, C.; Banno, M.; Miyata, T.; Sasaguri, T.; Kawano, Y. Insertion/Deletion Polymorphism in Clusterin Gene Influences Serum Lipid Levels and Carotid Intima-Media Thickness in Hypertensive Japanese Females. Biochem. Biophys. Res. Commun. 2005, 331, 1587–1593. [Google Scholar] [CrossRef]
- Kjeldsen, E.W.; Tybjærg-Hansen, A.; Nordestgaard, B.G.; Frikke-Schmidt, R. ABCA7 and Risk of Dementia and Vascular Disease in the Danish Population. Ann. Clin. Transl. Neurol. 2018, 5, 41–51. [Google Scholar] [CrossRef]
- Steinberg, S.; Stefansson, H.; Jonsson, T.; Johannsdottir, H.; Ingason, A.; Helgason, H.; Sulem, P.; Magnusson, O.T.; Gudjonsson, S.A.; Unnsteinsdottir, U.; et al. Loss-of-Function Variants in ABCA7 Confer Risk of Alzheimer’s Disease. Nat. Genet. 2015, 47, 445–447. [Google Scholar] [CrossRef]
- Li, H.; Zhou, J.; Yue, Z.; Feng, L.; Luo, Z.; Chen, S.; Yang, X.; Xiao, B. A Complex Association between ABCA7 Genotypes and Blood Lipid Levels in Southern Chinese Han Patients of Sporadic Alzheimer’s Disease. J. Neurol. Sci. 2017, 382, 13–17. [Google Scholar] [CrossRef]
- Cohen, J.C.; Boerwinkle, E.; Mosley, T.H.; Hobbs, H.H. Sequence Variations in in PCSK9, Low LDL, and Protection against Coronary Heart Disease. Hear. Dis. 2011, 23, 1264–1272. [Google Scholar]
- Ference, B.A.; Robinson, J.G.; Brook, R.D.; Catapano, A.L.; Chapman, M.J.; Neff, D.R.; Voros, S.; Giugliano, R.P.; Davey Smith, G.; Fazio, S.; et al. Variation in PCSK9 and HMGCR and Risk of Cardiovascular Disease and Diabetes. N. Engl. J. Med. 2016, 375, 2144–2153. [Google Scholar] [CrossRef] [Green Version]
- De la Torre, J. The Vascular Hypothesis of Alzheimer’s Disease: A Key to Preclinical Prediction of Dementia Using Neuroimaging. J. Alzheimers. Dis. 2018, 63, 35–52. [Google Scholar] [CrossRef]
- Skoog, I.; Lernfelt, B.; Landahl, S.; Palmertz, B.; Andreasson, L.A.; Nilsson, L.; Persson, G.; Odén, A.; Svanborg, A. 15-Year Longitudinal Study of Blood Pressure and Dementia. Lancet 1996, 347, 1141–1145. [Google Scholar] [CrossRef]
- Hofman, A.; Ott, A.; Breteler, M.M.B.; Bots, M.L.; Slooter, A.J.C.; Van Harskamp, F.; Van Duijn, C.N.; Van Broeckhoven, C.; Grobbee, D.E. Atherosclerosis, Apolipoprotein E, and Prevalence of Dementia and Alzheimer’s Disease in the Rotterdam Study. Lancet 1997, 349, 151–154. [Google Scholar] [CrossRef]
- Lakatta, E.G. Myocardial Adaptations in Advanced Age. Basic Res. Cardiol. 1993, 88 (Suppl. 2), 125–133. [Google Scholar]
- De la Torre, J.C. Vascular Risk Factor Detection and Control May Prevent Alzheimer’s Disease. Ageing Res. Rev. 2010, 9, 218–225. [Google Scholar] [CrossRef]
- De la Torre, J.C. Critically Attained Threshold of Cerebral Hypoperfusion: The CATCH Hypothesis of Alzheimer’s Pathogenesis. Neurobiol. Aging 2000, 21, 331–342. [Google Scholar] [CrossRef]
- De la Torre, J.C. Alzheimer’s Turning Point A Vascular Approach to Clinical Prevention; Springer: Berlin/Heidelberg, Germany, 2016; ISBN 9783319340562. [Google Scholar]
- Xie, Y.; Mies, G.; Hossmann, K.A. Ischemic Threshold of Brain Protein Synthesis after Unilateral Carotid Artery Occlusion in Gerbils. Stroke 1989, 20, 620–626. [Google Scholar] [CrossRef]
- Prince, M.J.; Wimo, A.; Guerchet, M.M.; Ali, G.C.; Wu, Y.T.; Prina, M. World Alzheimer Report 2015: The Global Impact of Dementia|Alzheimer’s Disease International; World Alzheimer’s Report; Alzheimer’s Disease International: London, UK, 2015; pp. 1–87. [Google Scholar]
- Sweeney, M.D.; Montagne, A.; Sagare, A.P.; Nation, D.A.; Schneider, L.S.; Chui, H.C.; Harrington, M.G.; Wardlaw, J.M.; Zlokovic, B.V. Vascular Dysfunction—The Disregarded Partner of Alzheimer’ s Disease. Alzheimer’ s and Dementia. Alzheimer’s Dement. 2019, 15, 158–167. [Google Scholar] [CrossRef]
- Hachinski, V. Dementia: Paradigm Shifting into High Gear. Alzheimer’s Dement. 2019, 15, 985–994. [Google Scholar] [CrossRef]
- Esiri, M.M.; Nagy, Z.; Smith, M.Z.; Barnetson, L.; Smith, A.D.; Joachim, C. Cerebrovascular Disease and Threshold for Dementia in the Early Stages of Alzheimer’s Disease. Lancet 1999, 354, 919–920. [Google Scholar] [CrossRef]
- Emrani, S.; Lamar, M.; Price, C.C.; Wasserman, V.; Matusz, E.; Au, R.; Swenson, R.; Nagele, R.; Heilman, K.M.; Libon, D.J. Alzheimer’s/Vascular Spectrum Dementia: Classification in Addition to Diagnosis. J. Alzheimer’s Dis. 2020, 73, 63–71. [Google Scholar] [CrossRef]
- Agüero-Torres, H.; Kivipelto, M.; Von Strauss, E. Rethinking the Dementia Diagnoses in a Population-Based Study: What Is Alzheimer’s Disease and What Is Vascular Dementia? A Study from the Kungsholmen Project. Dement. Geriatr. Cogn. Disord. 2006, 22, 244–249. [Google Scholar] [CrossRef]
- De la Torre, J.C. Vascular Risk Factors: A Ticking Time Bomb to Alzheimer’s Disease. Am. J. Alzheimers. Dis. Other Demen. 2013, 28, 551–559. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nordestgaard, L.T.; Christoffersen, M.; Frikke-Schmidt, R. Shared Risk Factors between Dementia and Atherosclerotic Cardiovascular Disease. Int. J. Mol. Sci. 2022, 23, 9777. https://doi.org/10.3390/ijms23179777
Nordestgaard LT, Christoffersen M, Frikke-Schmidt R. Shared Risk Factors between Dementia and Atherosclerotic Cardiovascular Disease. International Journal of Molecular Sciences. 2022; 23(17):9777. https://doi.org/10.3390/ijms23179777
Chicago/Turabian StyleNordestgaard, Liv Tybjærg, Mette Christoffersen, and Ruth Frikke-Schmidt. 2022. "Shared Risk Factors between Dementia and Atherosclerotic Cardiovascular Disease" International Journal of Molecular Sciences 23, no. 17: 9777. https://doi.org/10.3390/ijms23179777
APA StyleNordestgaard, L. T., Christoffersen, M., & Frikke-Schmidt, R. (2022). Shared Risk Factors between Dementia and Atherosclerotic Cardiovascular Disease. International Journal of Molecular Sciences, 23(17), 9777. https://doi.org/10.3390/ijms23179777





