Biofabrication of Sodium Alginate Hydrogel Scaffolds for Heart Valve Tissue Engineering
Abstract
1. Introduction
2. Results and Discussion
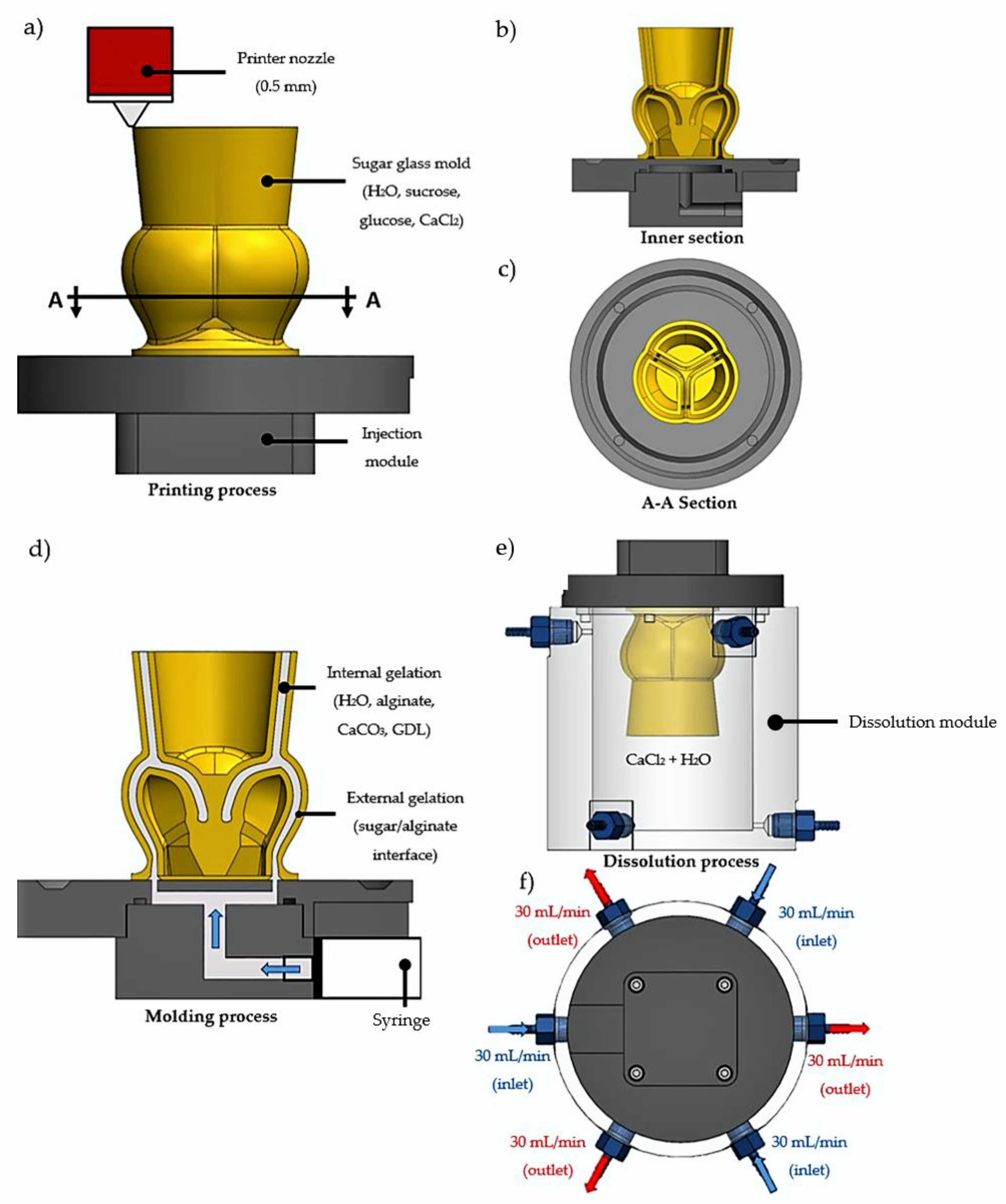
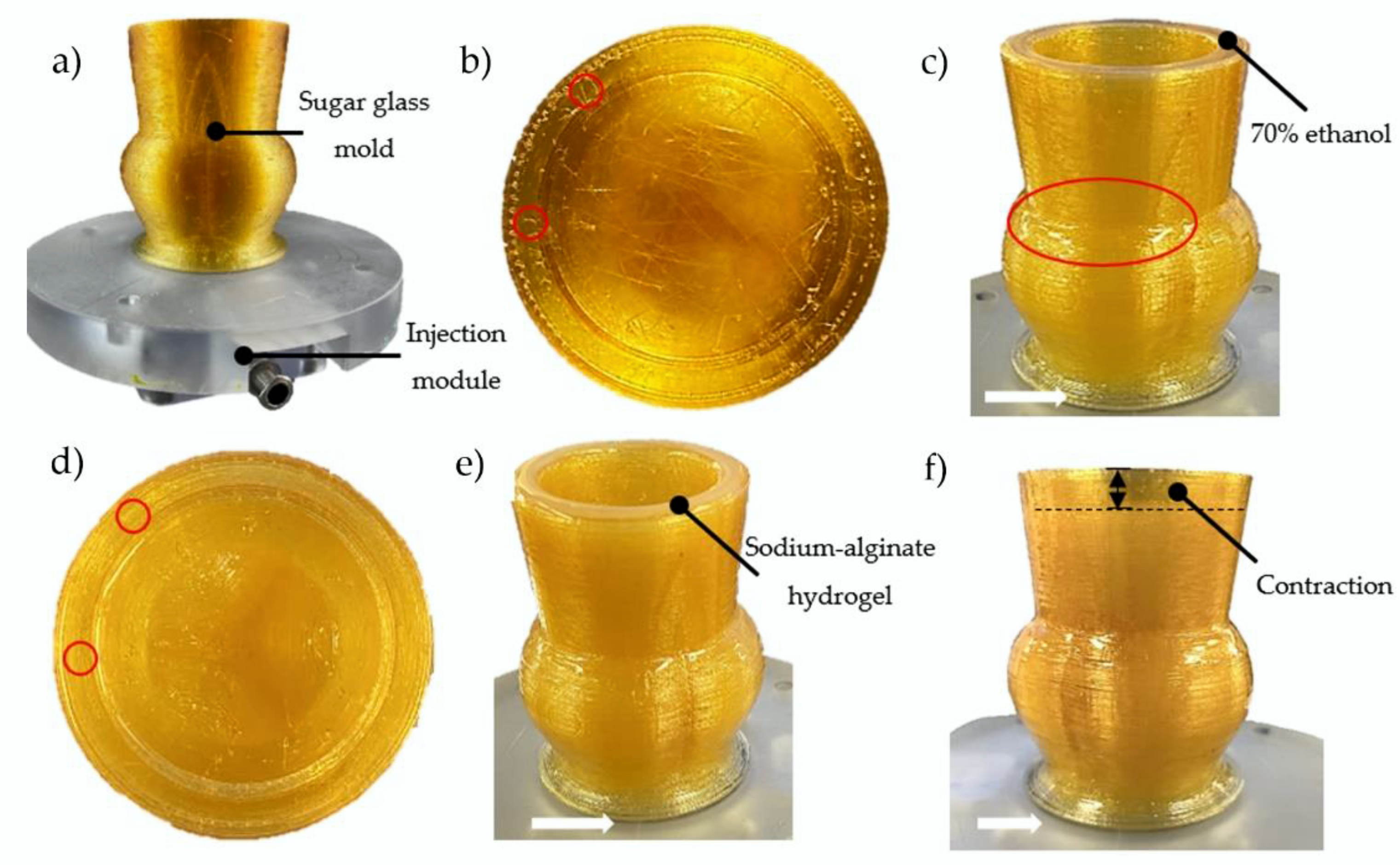
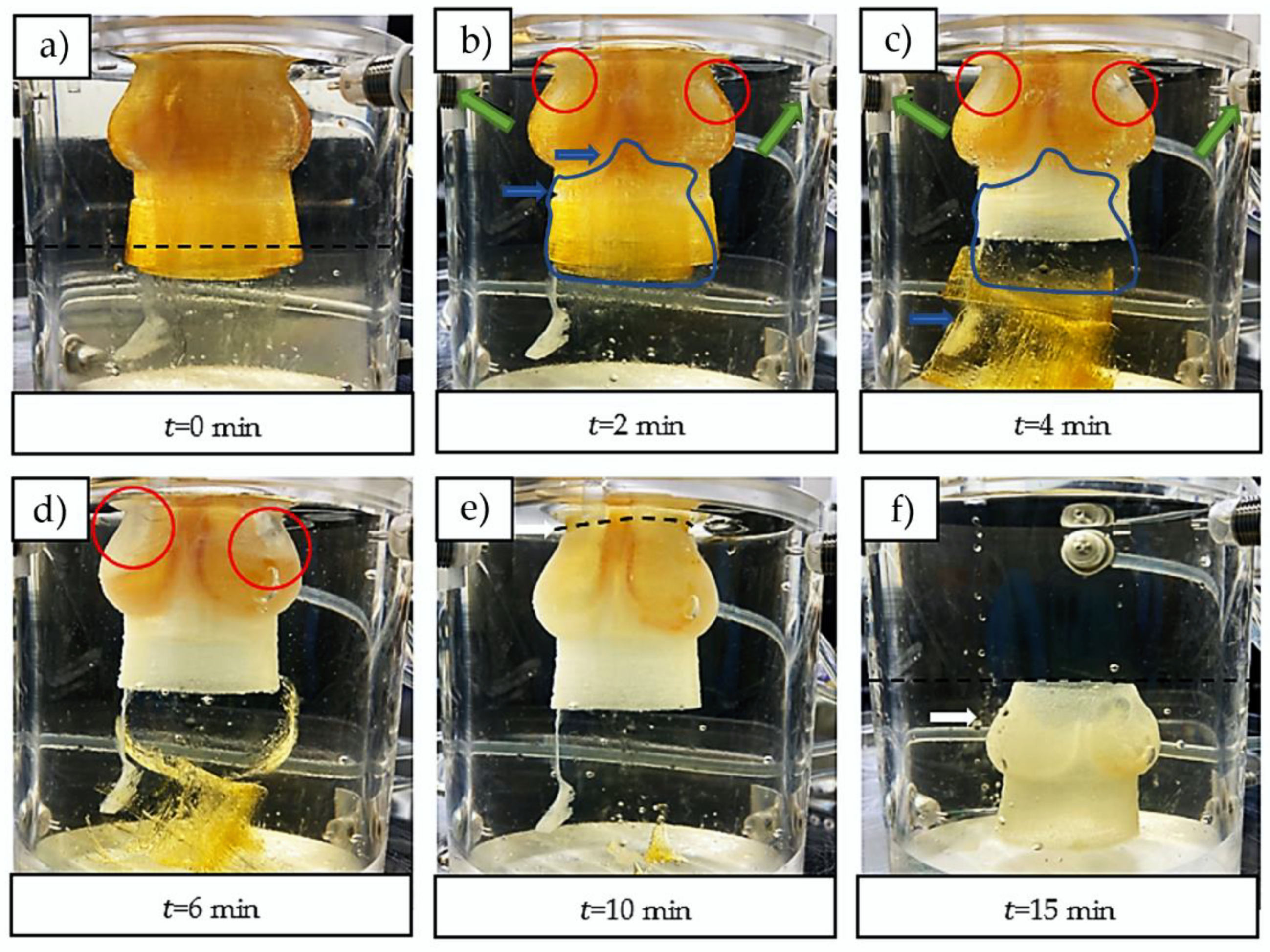
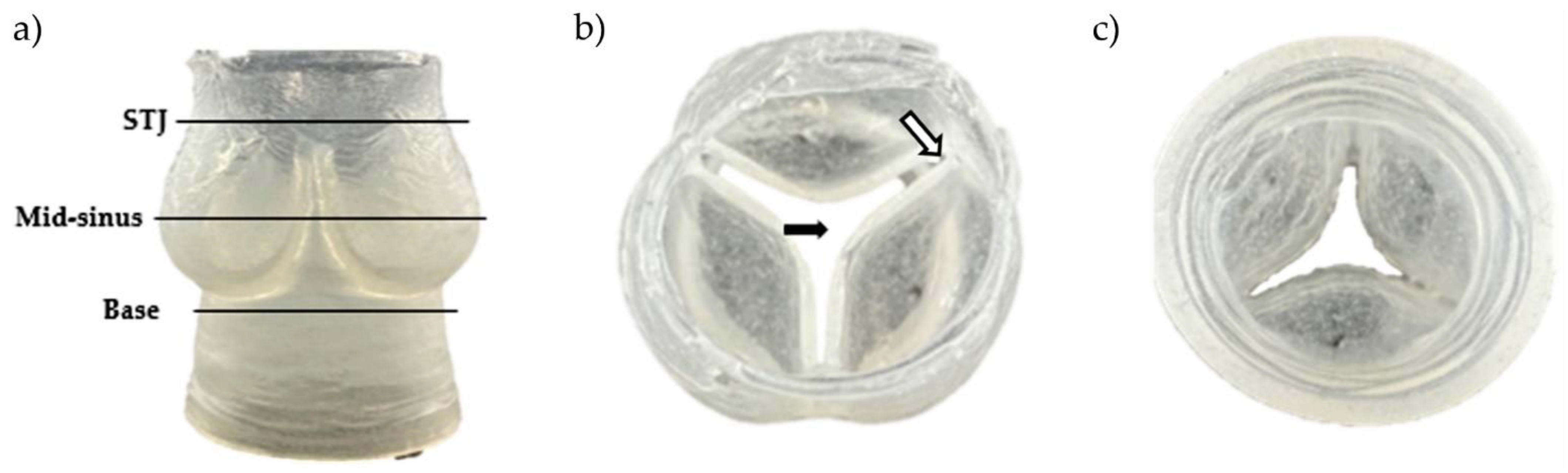
2.1. Fabrication of the Aortic Valve Scaffolds
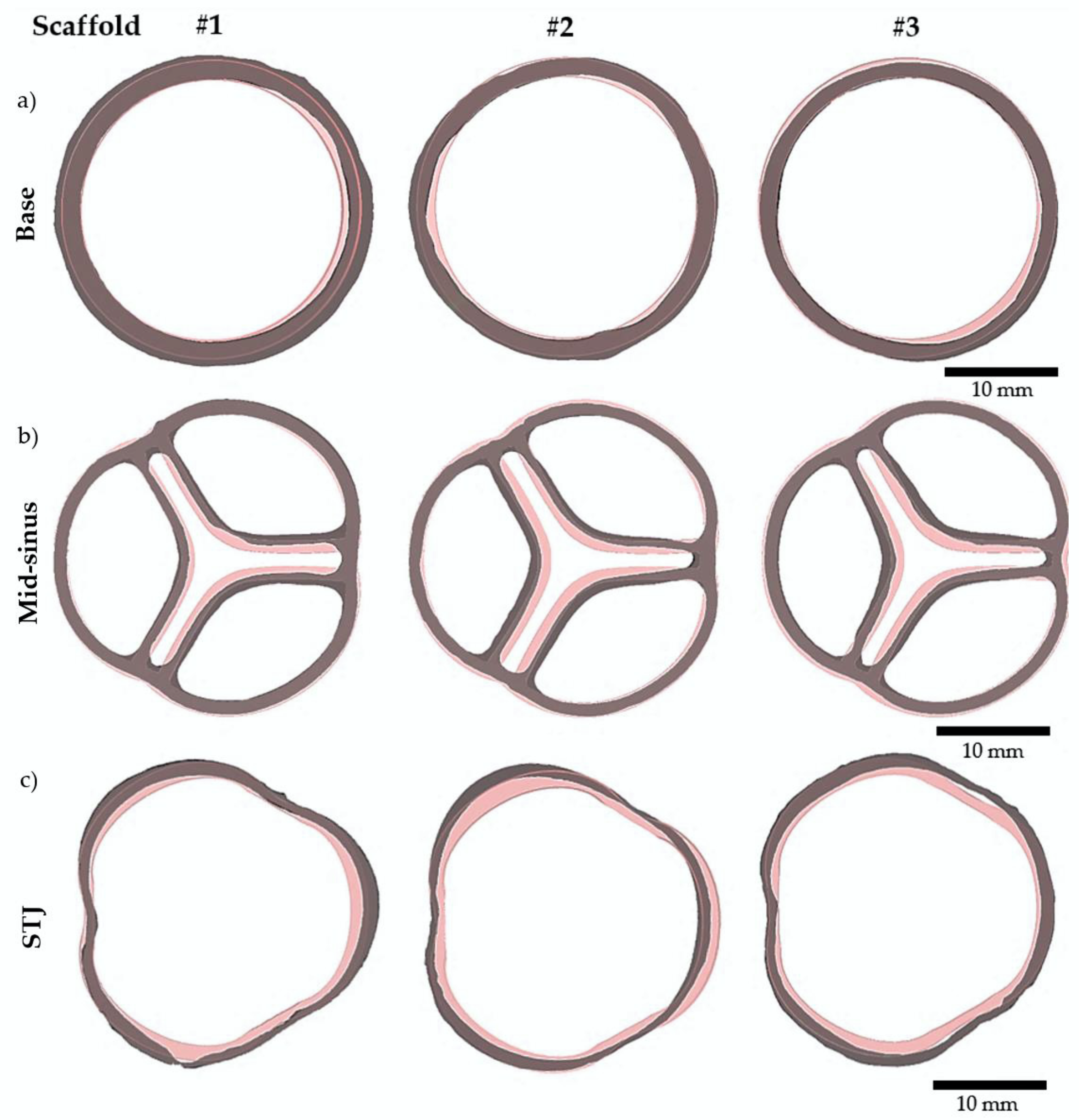
2.2. Geometric Assessment of the Aortic Valve Scaffolds Indicates Very Good Preliminary Repeatability
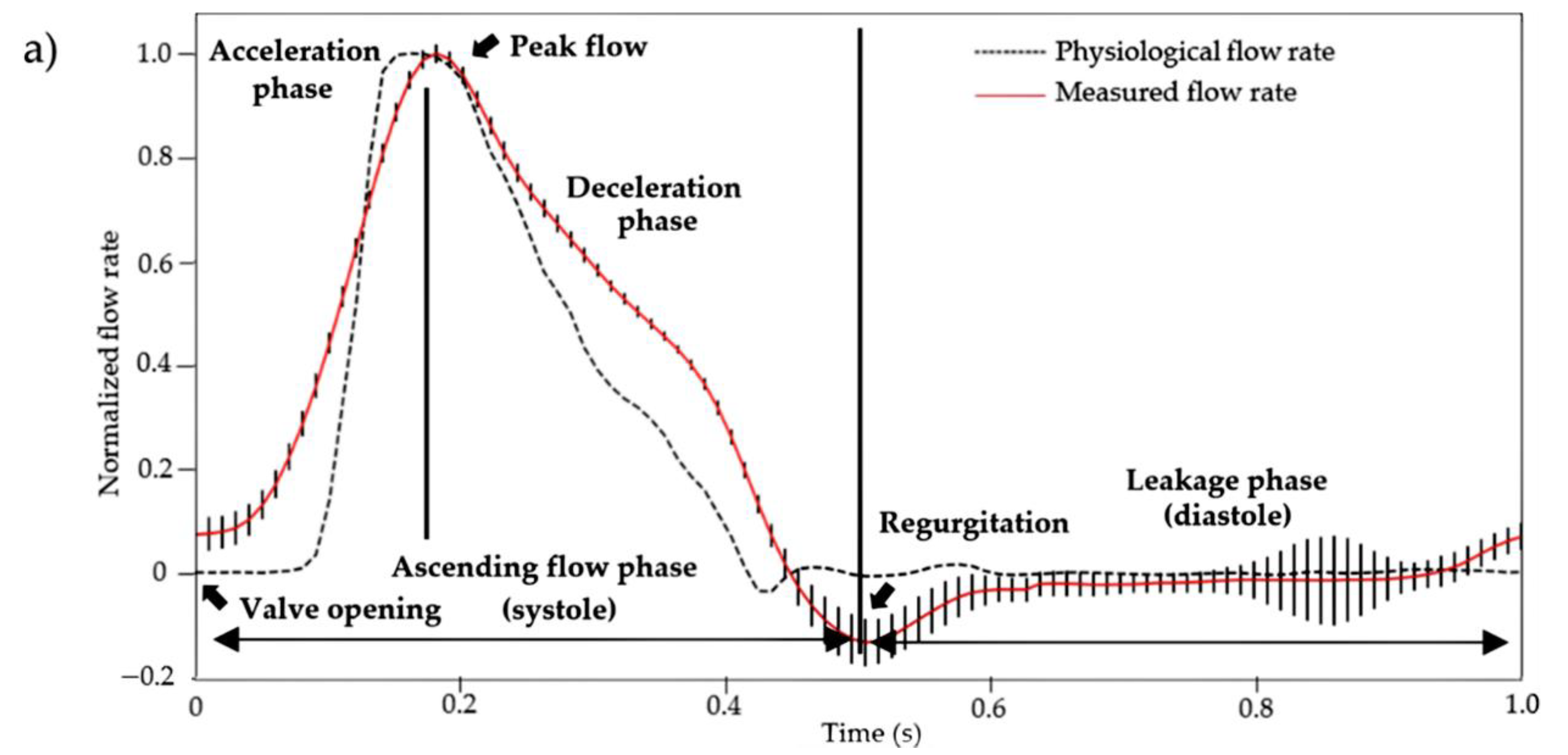
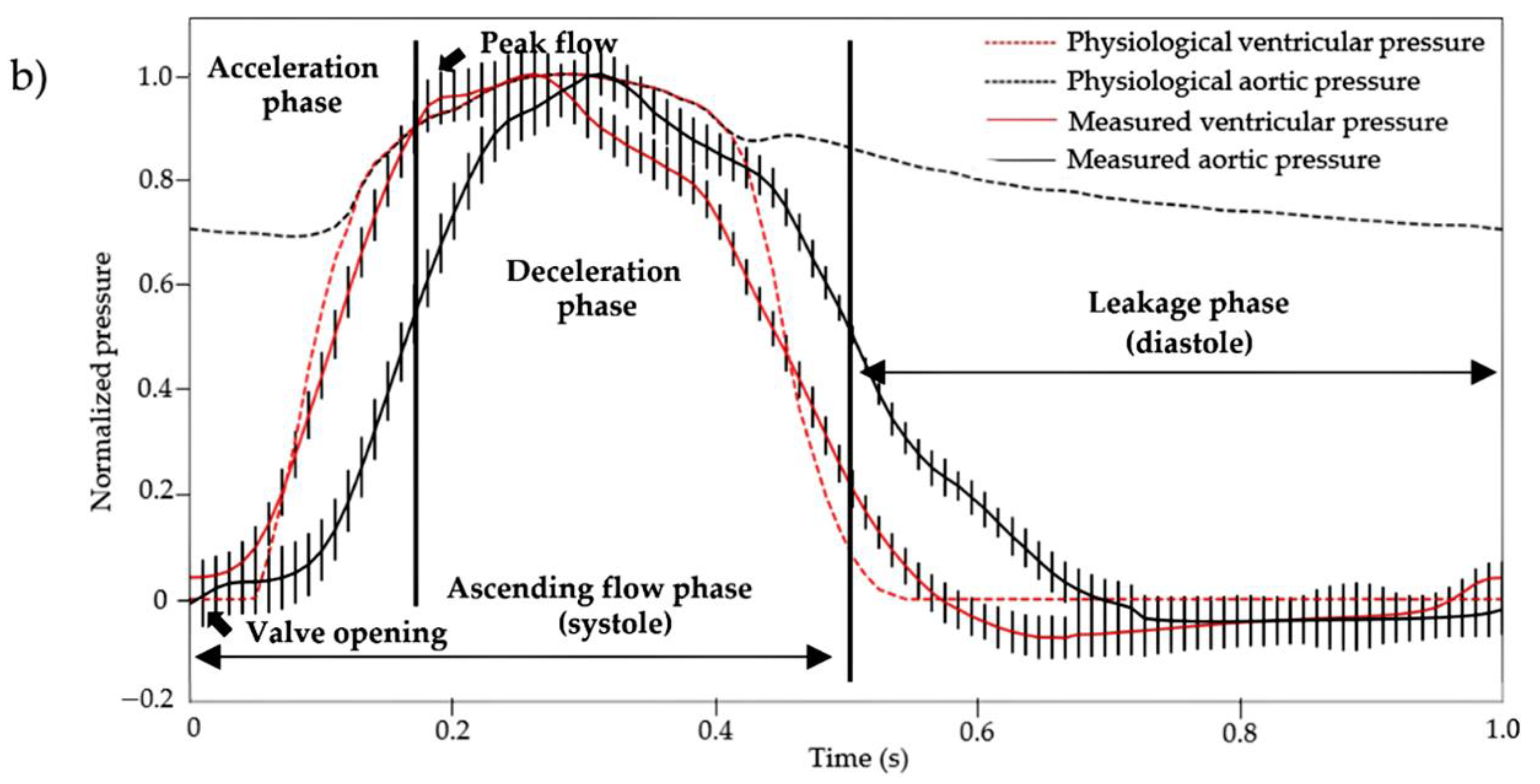
2.3. Hydrodynamic Properties of the Aortic Valve Scaffolds
3. Materials and Methods
3.1. Aortic Valve Geometries
3.2. Sugar Glass Mixture of the Molds
3.3. 3D printing of the Aortic Valve Sugar Glass Mold
3.4. Sodium Alginate Scaffold Formulation
3.5. Fabrication of the Aortic Valve Scaffolds
3.6. Geometric Evaluation of the Aortic Valve Scaffold
3.7. Mechanical Testing of the Aortic Valve Scaffolds
3.8. Physiological Assessment of the Functionality of the Aortic Valve Scaffold
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yacoub, M.H.; Takkenberg, J.J. Will heart valve tissue engineering change the world? Nat. Clin. Pract. Cardiovasc. Med. 2005, 2, 60–61. [Google Scholar] [CrossRef] [PubMed]
- Nkomo, V.T.; Gardin, J.M.; Skelton, T.N.; Gottdiener, J.S.; Scott, C.G.; Enriquez-Sarano, M. Burden of valvular heart diseases: A population-based study. Lancet 2006, 368, 1005–1011. [Google Scholar] [CrossRef]
- Carabello, B.A. Aortic Stenosis. N. Engl. J. Med. 2002, 346, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Stewart, B.; Siscovick, D.; Lind, B.K.; Gardin, J.M.; Gottdiener, J.S.; Smith, V.E.; Kitzman, D.W.; Otto, C.M. Clinical Factors Associated with Calcific Aortic Valve Disease. Cardiovascular Health Study. J. Am. Coll. Cardiol. 1997, 29, 630–634. [Google Scholar] [CrossRef]
- Schoen, F.J. Morphology, Clinicopathologic Correlations, and Mechanisms in Heart Valve Health and Disease. Cardiovasc. Eng. Technol. 2018, 9, 126–140. [Google Scholar] [CrossRef]
- Otto, C.M.; Lind, B.K.; Kitzman, D.W.; Gersh, B.J.; Siscovick, D.S. Association of Aortic-Valve Sclerosis with Cardiovascular Mortality and Morbidity in the Elderly. N. Engl. J. Med. 1999, 341, 142–147. [Google Scholar] [CrossRef]
- Bleiziffer, S.; Simonato, M.; Webb, J.G.; Rodés-Cabau, J.; Pibarot, P.; Kornowski, R.; Windecker, S.; Erlebach, M.; Duncan, A.; Seiffert, M.; et al. Long-term outcomes after transcatheter aortic valve implantation in failed bioprosthetic valves. Eur. Heart J. 2020, 41, 2731–2742. [Google Scholar] [CrossRef]
- Roberts, W.C.; Ko, J.M. Frequency by Decades of Unicuspid, Bicuspid, and Tricuspid Aortic Valves in Adults Having Isolated Aortic Valve Replacement for Aortic Stenosis, With or Without Associated Aortic Regurgitation. Circulation 2005, 111, 920–925. [Google Scholar] [CrossRef]
- Fishbein, G.A.; Fishbein, M.C. Pathology of the Aortic Valve: Aortic Valve Stenosis/Aortic Regurgitation. Curr. Cardiol. Rep. 2019, 21, 81. [Google Scholar] [CrossRef]
- Simard, L.; Cote, N.; Dagenais, F.; Mathieu, P.; Couture, C.; Trahan, S.; Clavel, M.A. Sex-Related Discordance Between Aortic Valve Calcification and Hemodynamic Severity of Aortic Stenosis: Is Valvular Fibrosis the Explanation? Circ. Res. 2017, 120, 681–691. [Google Scholar] [CrossRef]
- Mordi, I.; Tzemos, N. Bicuspid Aortic Valve Disease: A Comprehensive Review. Cardiol. Res. Pract. 2012, 2012, 196037. [Google Scholar] [CrossRef] [PubMed]
- Ward, C. Clinical significance of the bicuspid aortic valve. Heart 2000, 83, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Head, S.J.; Çelik, M.; Kappetein, A.P. Mechanical versus bioprosthetic aortic valve replacement. Eur. Heart J. 2017, 38, 2183–2191. [Google Scholar] [CrossRef]
- Fioretta, E.S.; Motta, S.E.; Lintas, V.; Loerakker, S.; Parker, K.K.; Baaijens, F.P.T.; Falk, V.; Hoerstrup, S.P.; Emmert, M.Y. Next-generation tissue-engineered heart valves with repair, remodelling and regeneration capacity. Nat. Rev. Cardiol. 2021, 18, 92–116. [Google Scholar] [CrossRef] [PubMed]
- Manji, R.A.; Lee, W.; Cooper, D.K. Xenograft bioprosthetic heart valves: Past, present and future. Int. J. Surg. 2015, 23, 280–284. [Google Scholar] [CrossRef]
- Human, P.; Zilla, P. The Neglected Villain of Bioprosthetic Degeneration: Inflammatory and Immune Processes. J. Long-Term Eff. Med. Implant. 2017, 27, 159–180. [Google Scholar] [CrossRef] [PubMed]
- Arsalan, M.; Walther, T. Durability of prostheses for transcatheter aortic valve implantation. Nat. Rev. Cardiol. 2016, 13, 360–367. [Google Scholar] [CrossRef]
- Thiene, G.; Valente, M. Anticalcification strategies to increase bioprosthetic valve durability. J. Heart Valve Dis. 2011, 20, 37–44. [Google Scholar]
- Ganapathi, A.M.; Englum, B.R.; Keenan, J.E.; Schechter, M.A.; Wang, H.; Smith, P.K.; Hughes, G.C. Long-Term Survival After Bovine Pericardial Versus Porcine Stented Bioprosthetic Aortic Valve Replacement: Does Valve Choice Matter? Ann. Thorac. Surg. 2015, 100, 550–559. [Google Scholar] [CrossRef] [PubMed]
- Hickey, G.L.; Grant, S.W.; Bridgewater, B.; Kendall, S.; Bryan, A.J.; Kuo, J.; Dunning, J. A comparison of outcomes between bovine pericardial and porcine valves in 38 040 patients in England and Wales over 10 years. Eur. J. Cardio-Thoracic Surg. 2014, 47, 1067–1074. [Google Scholar] [CrossRef] [PubMed]
- Ruel, M.; Chan, V.; Bédard, P.; Kulik, A.; Ressler, L.; Lam, B.K.; Rubens, F.D.; Goldstein, W.; Hendry, P.J.; Masters, R.G.; et al. Very Long-Term Survival Implications of Heart Valve Replacement with Tissue Versus Mechanical Prostheses in Adults <60 Years of Age. Circulation 2007, 116, I-294–I-300. [Google Scholar] [CrossRef] [PubMed]
- Mirani, B.; Nejad, S.P.; Simmons, C.A. Recent Progress Toward Clinical Translation of Tissue-Engineered Heart Valves. Can. J. Cardiol. 2021, 37, 1064–1077. [Google Scholar] [CrossRef] [PubMed]
- Goecke, T.; Theodoridis, K.; Tudorache, I.; Ciubotaru, A.; Cebotari, S.; Ramm, R.; Höffler, K.; Sarikouch, S.; Rivera, A.V.; Haverich, A.; et al. In vivo performance of freeze-dried decellularized pulmonary heart valve allo- and xenografts orthotopically implanted into juvenile sheep. Acta Biomater. 2018, 68, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Erdbrügger, W.; Konertz, W.; Dohmen, P.M.; Posner, S.; Ellerbrok, H.; Brodde, O.E.; Pauli, G. Decellularized xenogenic heart valves reveal remodeling and growth potential in vivo. Tissue Eng. 2006, 12, 2059–2068. [Google Scholar] [CrossRef] [PubMed]
- Dohmen, P.M.; Da Costa, F.; Lopes, S.V.; Yoshi, S.; Da Souza, F.P.; Vilani, R.; Da Costa, M.B.; Konertz, W. Results of a Decellularized Porcine Heart Valve Implanted into the Juvenile Sheep Model. Heart Surg. Forum 2005, 8, 100–104. [Google Scholar] [CrossRef]
- Stock, U.A.; Schenke-Layland, K. Performance of decellularized xenogeneic tissue in heart valve replacement. Biomaterials 2006, 27, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Sarikouch, S.; Horke, A.; Tudorache, I.; Beerbaum, P.; Westhoff-Bleck, M.; Boethig, D.; Repin, O.; Maniuc, L.; Ciubotaru, A.; Haverich, A.; et al. Decellularized fresh homografts for pulmonary valve replacement: A decade of clinical experience. Eur. J. Cardio-Thoracic Surg. 2016, 50, 281–290. [Google Scholar] [CrossRef] [PubMed]
- Sarikouch, S.; Theodoridis, K.; Hilfiker, A.; Boethig, D.; Laufer, G.; Andreas, M.; Cebotari, S.; Tudorache, I.; Bobylev, D.; Neubert, L.; et al. Early Insight Into In Vivo Recellularization of Cell-Free Allogenic Heart Valves. Ann. Thorac. Surg. 2019, 108, 581–589. [Google Scholar] [CrossRef]
- Lisy, M.; Kalender, G.; Schenke-Layland, K.; Brockbank, K.G.; Biermann, A.; Stock, U.A. Allograft Heart Valves: Current Aspects and Future Applications. Biopreserv. Biobank. 2017, 15, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Bobylev, D.; Sarikouch, S.; Tudorache, I.; Cvitkovic, T.; Söylen, B.; Boethig, D.; Theodoridis, K.; Bertram, H.; Beerbaum, P.; Haverich, A.; et al. Double semilunar valve replacement in complex congenital heart disease using decellularized homografts. Interact. Cardiovasc. Thorac. Surg. 2019, 28, 151–157. [Google Scholar] [CrossRef]
- Tudorache, I.; Horke, A.; Cebotari, S.; Sarikouch, S.; Boethig, D.; Breymann, T.; Beerbaum, P.; Bertram, H.; Westhoff-Bleck, M.; Theodoridis, K.; et al. Decellularized aortic homografts for aortic valve and aorta ascendens replacement. Eur. J. Cardio-Thoracic Surg. 2016, 50, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Horke, A.; Bobylev, D.; Avsar, M.; Meyns, B.; Rega, F.; Hazekamp, M.; Huebler, M.; Schmiady, M.; Tzanavaros, I.; Cesnjevar, R.; et al. Paediatric aortic valve replacement using decellularized allografts. Eur. J. Cardio-Thoracic Surg. 2020, 58, 817–824. [Google Scholar] [CrossRef] [PubMed]
- Dohmen, P.M.; Lembcke, A.; Holinski, S.; Pruss, A.; Konertz, W. Ten Years of Clinical Results with a Tissue-Engineered Pulmonary Valve. Ann. Thorac. Surg. 2011, 92, 1308–1314. [Google Scholar] [CrossRef]
- da Costa, F.D.; Costa, A.C.B.; Prestes, R.; Domanski, A.C.; Balbi, E.M.; Ferreira, A.D.; Lopes, S.V. The Early and Midterm Function of Decellularized Aortic Valve Allografts. Ann. Thorac. Surg. 2010, 90, 1854–1860. [Google Scholar] [CrossRef]
- Ebken, J.; Mester, N.; Smart, I.; Ramm, R.; Goecke, T.; Jashari, R.; Böthig, D.; Horke, A.; Cebotari, S.; Tudorache, I.; et al. Residual immune response towards decellularized homografts may be highly individual. Eur. J. Cardio-Thoracic Surg. 2021, 59, 773–782. [Google Scholar] [CrossRef]
- Findeisen, K.; Morticelli, L.; Goecke, T.; Kolbeck, L.; Ramm, R.; Höffler, H.; Brandes, G.; Korossis, S.; Haverich, A.; Hilfiker, A. Toward acellular xenogeneic heart valve prostheses: Histological and biomechanical characterization of decellularized and enzymatically deglycosylated porcine pulmonary heart valve matrices. Xenotransplantation 2020, 27, e12617. [Google Scholar] [CrossRef] [PubMed]
- Kluin, J.; Talacua, H.; Smits, A.I.; Emmert, M.Y.; Brugmans, M.C.; Fioretta, E.S.; Dijkman, P.E.; Söntjens, S.H.; Duijvelshoff, R.; Dekker, S.; et al. In situ heart valve tissue engineering using a bioresorbable elastomeric implant—From material design to 12 months follow-up in sheep. Biomaterials 2017, 125, 101–117. [Google Scholar] [CrossRef]
- Uiterwijk, M.; Smits, A.I.; van Geemen, D.; van Klarenbosch, B.; Dekker, S.; Cramer, M.J.; van Rijswijk, J.W.; Lurier, E.B.; Di Luca, A.; Brugmans, M.C.; et al. In Situ Remodeling Overrules Bioinspired Scaffold Architecture of Supramolecular Elastomeric Tissue-Engineered Heart Valves. JACC Basic Transl. Sci. 2020, 5, 1187–1206. [Google Scholar] [CrossRef]
- Capulli, A.K.; Emmert, M.Y.; Pasqualini, F.S.; Kehl, D.; Caliskan, E.; Lind, J.U.; Sheehy, S.P.; Park, S.J.; Ahn, S.; Weber, B.; et al. JetValve: Rapid manufacturing of biohybrid scaffolds for biomimetic heart valve replacement. Biomaterials 2017, 133, 229–241. [Google Scholar] [CrossRef]
- Soliman, O.I.; Miyazaki, Y.; Abdelghani, M.; Brugmans, M.; Witsenburg, M.; Onuma, Y.; Serruys, P.W. Midterm performance of a novel restorative pulmonary valved conduit: Preclinical results. EuroIntervention 2017, 13, e1418–e1427. [Google Scholar] [CrossRef]
- Duan, B.; Hockaday, L.A.; Kang, K.H.; Butcher, J.T. 3D Bioprinting of heterogeneous aortic valve conduits with alginate/gelatin hydrogels. J. Biomed. Mater. Res. Part A 2013, 101A, 1255–1264. [Google Scholar] [CrossRef] [PubMed]
- Matai, I.; Kaur, G.; Seyedsalehi, A.; McClinton, A.; Laurencin, C.T. Progress in 3D bioprinting technology for tissue/organ regenerative engineering. Biomaterials 2020, 226, 119536. [Google Scholar] [CrossRef]
- Lee, A.; Hudson, A.R.; Shiwarski, D.J.; Tashman, J.W.; Hinton, T.J.; Yerneni, S.; Bliley, J.M.; Campbell, P.G.; Feinberg, A.W. 3D bioprinting of collagen to rebuild components of the human heart. Science 2019, 365, 482–487. [Google Scholar] [CrossRef]
- Wu, Z.; Su, X.; Xu, Y.; Kong, B.; Sun, W.; Mi, S. Bioprinting three-dimensional cell-laden tissue constructs with controllable degradation. Sci. Rep. 2016, 6, 24474. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Wei, D.; Zhu, Y.; Zhong, M.; Zuo, Y.; Fan, H.; Zhang, X. A spatial patternable macroporous hydrogel with cell-affinity domains to enhance cell spreading and differentiation. Biomaterials 2014, 35, 4759–4768. [Google Scholar] [CrossRef]
- Kuo, C.K.; Ma, P.X. Ionically crosslinked alginate hydrogels as scaffolds for tissue engineering: Part 1. Structure, gelation rate and mechanical properties. Biomaterials 2001, 22, 511–521. [Google Scholar] [CrossRef]
- Sapir, Y.; Kryukov, O.; Cohen, S. Integration of multiple cell-matrix interactions into alginate scaffolds for promoting cardiac tissue regeneration. Biomaterials 2011, 32, 1838–1847. [Google Scholar] [CrossRef]
- Hockaday, A.L.; Kang, K.H.; Colangelo, N.W.; Cheung, P.Y.C.; Duan, B.; Malone, E.; Wu, J.; Girardi, L.N.; Bonassar, L.J.; Lipson, H.; et al. Rapid 3D printing of anatomically accurate and mechanically heterogeneous aortic valve hydrogel scaffolds. Biofabrication 2012, 4, 035005. [Google Scholar] [CrossRef] [PubMed]
- Liberski, A.; Latif, N.; Raynaud, C.; Bollensdorff, C.; Yacoub, M. Alginate for cardiac regeneration: From seaweed to clinical trials. Glob. Cardiol. Sci. Pract. 2016, 2016, e201604. [Google Scholar] [CrossRef]
- Cao, N.; Chen, X.B.; Schreyer, D.J. Influence of Calcium Ions on Cell Survival and Proliferation in the Context of an Alginate Hydrogel. ISRN Chem. Eng. 2012, 2012, 516461. [Google Scholar] [CrossRef]
- Lee, G.M.; Han, B.K.; Kim, J.H.; Palsson, B.O. Effect of calcium chloride treatment on hybridoma cell viability and growth. Biotechnol. Lett. 1992, 14, 891–896. [Google Scholar] [CrossRef][Green Version]
- Schiavi, A.; Cuccaro, R.; Troia, A. Functional mechanical attributes of natural and synthetic gel-based scaffolds in tissue engineering: Strain-stiffening effects on apparent elastic modulus and compressive toughness. J. Mech. Behav. Biomed. Mater. 2022, 126, 105066. [Google Scholar] [CrossRef] [PubMed]
- Bégin-Drolet, A.; Collin, S.; Gosselin, J.; Ruel, J. A new robust controller for non-linear periodic single-input/single-output systems using genetic algorithms. J. Process Control 2018, 61, 23–35. [Google Scholar] [CrossRef]
- Piazza, N.; de Jaegere, P.; Schultz, C.; Becker, A.E.; Serruys, P.W.; Anderson, R.H. Anatomy of the Aortic Valvar Complex and Its Implications for Transcatheter Implantation of the Aortic Valve. Circ. Cardiovasc. Interv. 2008, 1, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Swanson, W.M.; Clark, R.E. Dimensions and Geometric Relationships of the Human Aortic Value as a Function of Pressure. Circ. Res. 1974, 35, 871–882. [Google Scholar] [CrossRef] [PubMed]
- Silver, M.A.; Roberts, W.C. Detailed anatomy of the normally functioning aortic valve in hearts of normal and increased weight. Am. J. Cardiol. 1985, 55, 454–461. [Google Scholar] [CrossRef]
- Cataloglu, A.; Clark, R.E.; Gould, P.L. Stress analysis of aortic valve leaflets with smoothed geometrical data. J. Biomech. 1977, 10, 153–158. [Google Scholar] [CrossRef]
- Grande, K.J.; Cochran, R.P.; Reinhall, P.G.; Kunzelman, K.S. Stress variations in the human aortic root and valve: The role of anatomic asymmetry. Ann. Biomed. Eng. 1998, 26, 534–545. [Google Scholar] [CrossRef] [PubMed]
- Haj-Ali, R.; Marom, G.; Zekry, S.B.; Rosenfeld, M.; Raanani, E. A general three-dimensional parametric geometry of the native aortic valve and root for biomechanical modeling. J. Biomech. 2012, 45, 2392–2397. [Google Scholar] [CrossRef] [PubMed]
- Gauvin-Rossignol, G.; Legros, P.; Ruel, J.; Fortin, M.-A.; Bégin-Drolet, A. Sugar glass fugitive ink loaded with calcium chloride for the rapid casting of alginate scaffold designs. Heliyon 2018, 4, e00680. [Google Scholar] [CrossRef] [PubMed]
- Bégin-Drolet, A.; Dussault, M.-A.; Fernandez, S.A.; Larose-Dutil, J.; Leask, R.L.; Hoesli, C.A.; Ruel, J. Design of a 3D printer head for additive manufacturing of sugar glass for tissue engineering applications. Addit. Manuf. 2017, 15, 29–39. [Google Scholar] [CrossRef]
- Kuo, C.K.; Ma, P.X. Maintaining dimensions and mechanical properties of ionically crosslinked alginate hydrogel scaffolds in vitro. J. Biomed. Mater. Res. A 2008, 84, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Gosselin, J.; Bégin-Drolet, A.; Maciel, Y.; Ruel, J. A New Approach Based on a Multiobjective Evolutionary Algorithm for Accurate Control of Flow Rate and Blood Pressure in Cardiac Bioreactors. Cardiovasc. Eng. Technol. 2020, 11, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Ruel, J.; Lachance, G. A New Bioreactor for the Development of Tissue-Engineered Heart Valves. Ann. Biomed. Eng. 2009, 37, 674–681. [Google Scholar] [CrossRef] [PubMed]
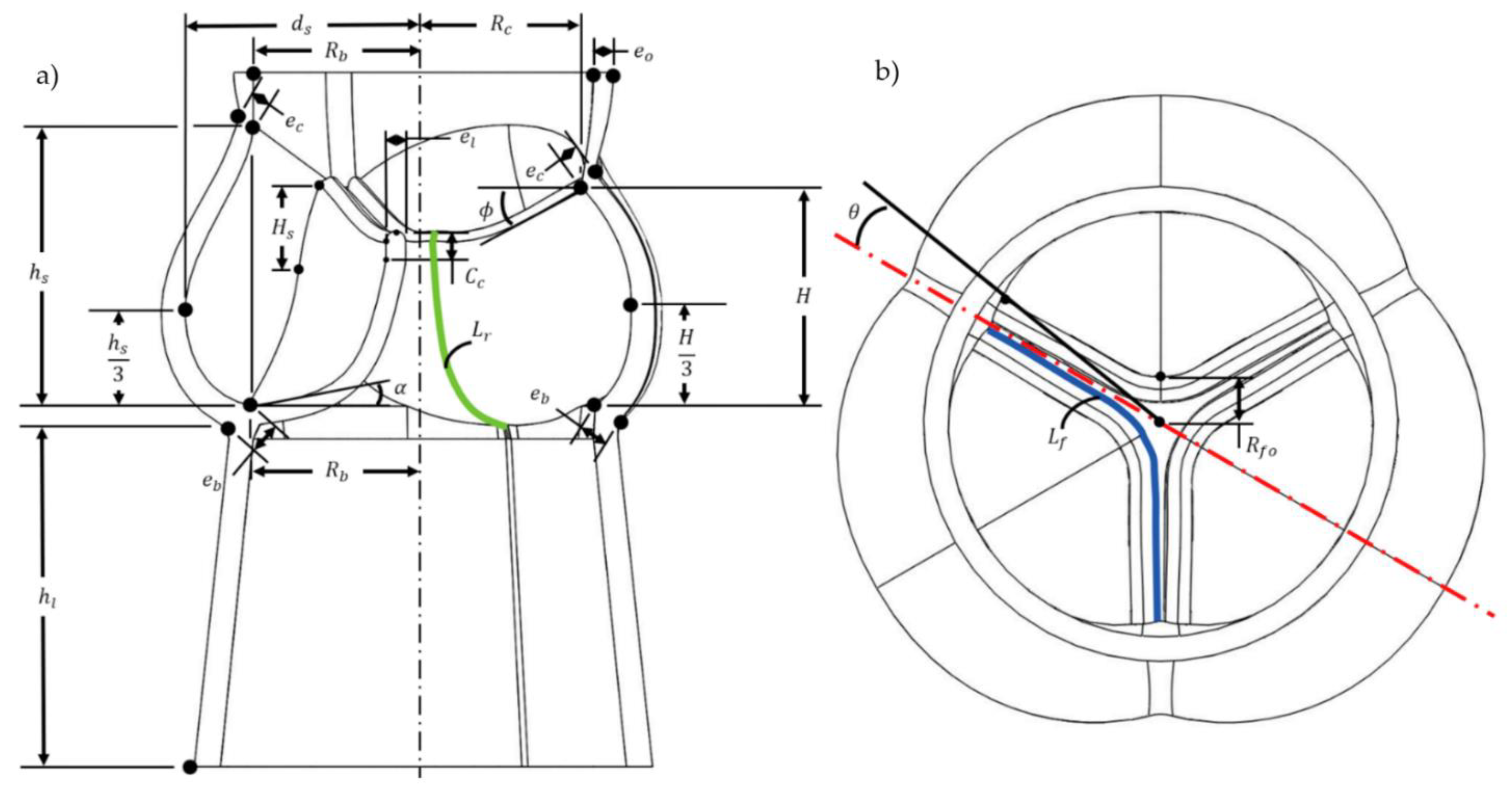
| Parameters | Value | Literature Range | Description |
|---|---|---|---|
| 13 mm | 11.3–14 mm | Radius of the base | |
| 0.9 | 0.78–1.0 | Radius of the commissures | |
| 1.24 | 1.34–1.5 | Valve height | |
| 0.5 | 0.71 | Commissures height | |
| 0.26 | 0.20–0.26 | Coaptation height | |
| 1.61 | 1.32–1.4 | Radius of the outermost wall of the sinus | |
| 1.4 | 1.52–1.96 | Sinus height | |
| 20 mm | Extension of the aortic valve wall | ||
| 25 | 29–51 | Angle of the free edge to the plane through the three commissures | |
| 22 | 15–25 [55] * | Angle of the bottom surface of the leaflet to the plane through the three commissures | |
| 1.92 | 2.42–2.48 | Length of the leaflet free edge | |
| 1.41 | 1.2–1.4 [55,56] * | Length of the leaflet in the radial direction | |
| 1.5 mm | 0.25–1.33 mm [57] ** | Leaflets thickness | |
| 2.0 mm | 0.6–1.977 mm | Thickness at the base | |
| 1.5 mm | 1.824–2.138 mm | Thickness at commissures and sinus ends | |
| 1.5 mm | 2.128–2.137 mm [58] | Thickness at the base of the ascending aorta | |
| 2.9 mm | Length between the center of the aortic valve and the leaflet | ||
| 8.3 | [59] | Angle between the commissure and the center of the aortic valve |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rioux, Y.; Fradette, J.; Maciel, Y.; Bégin-Drolet, A.; Ruel, J. Biofabrication of Sodium Alginate Hydrogel Scaffolds for Heart Valve Tissue Engineering. Int. J. Mol. Sci. 2022, 23, 8567. https://doi.org/10.3390/ijms23158567
Rioux Y, Fradette J, Maciel Y, Bégin-Drolet A, Ruel J. Biofabrication of Sodium Alginate Hydrogel Scaffolds for Heart Valve Tissue Engineering. International Journal of Molecular Sciences. 2022; 23(15):8567. https://doi.org/10.3390/ijms23158567
Chicago/Turabian StyleRioux, Yannick, Julie Fradette, Yvan Maciel, André Bégin-Drolet, and Jean Ruel. 2022. "Biofabrication of Sodium Alginate Hydrogel Scaffolds for Heart Valve Tissue Engineering" International Journal of Molecular Sciences 23, no. 15: 8567. https://doi.org/10.3390/ijms23158567
APA StyleRioux, Y., Fradette, J., Maciel, Y., Bégin-Drolet, A., & Ruel, J. (2022). Biofabrication of Sodium Alginate Hydrogel Scaffolds for Heart Valve Tissue Engineering. International Journal of Molecular Sciences, 23(15), 8567. https://doi.org/10.3390/ijms23158567





