Silicon Nitride as a Biomedical Material: An Overview
Abstract
1. Introduction
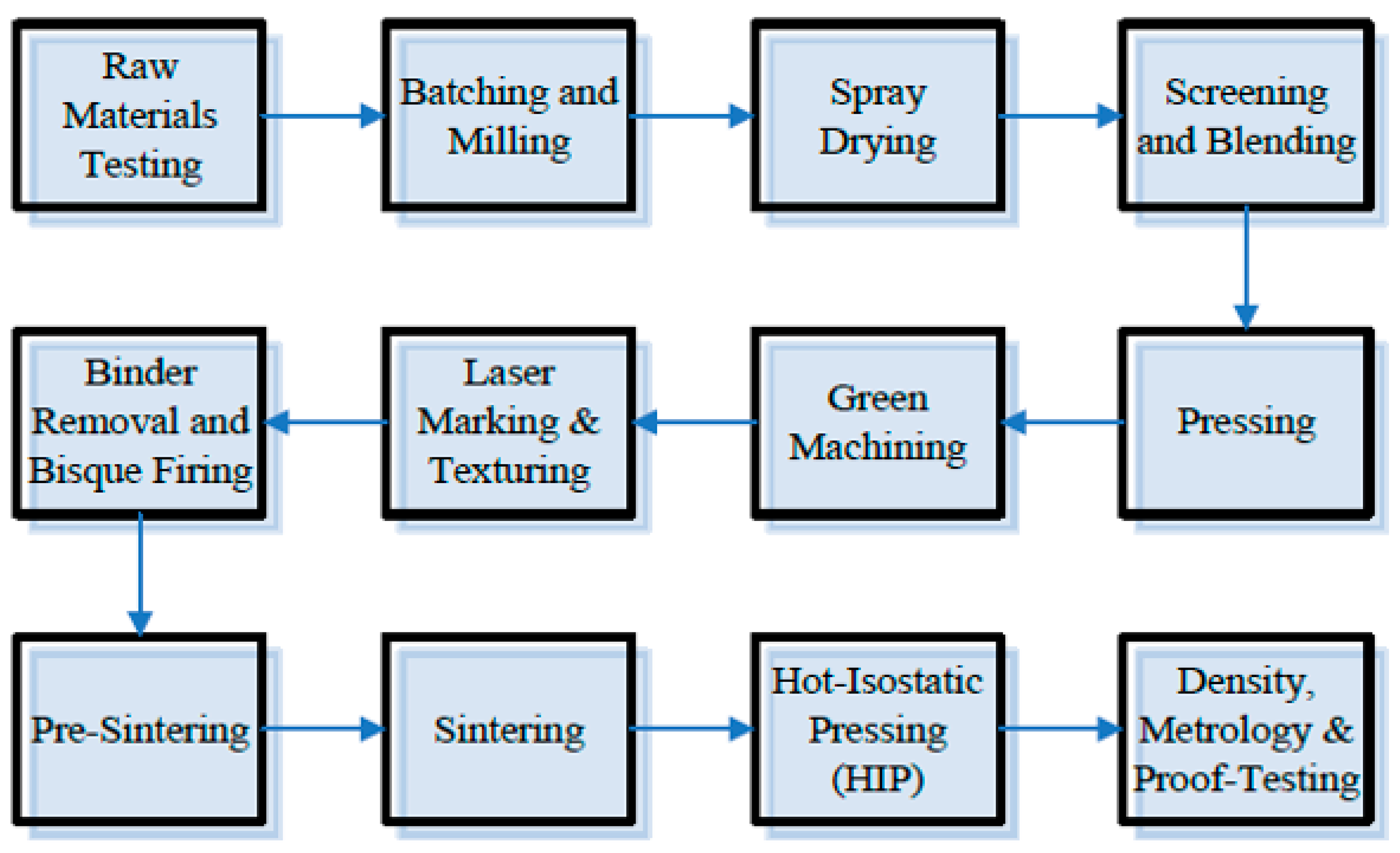
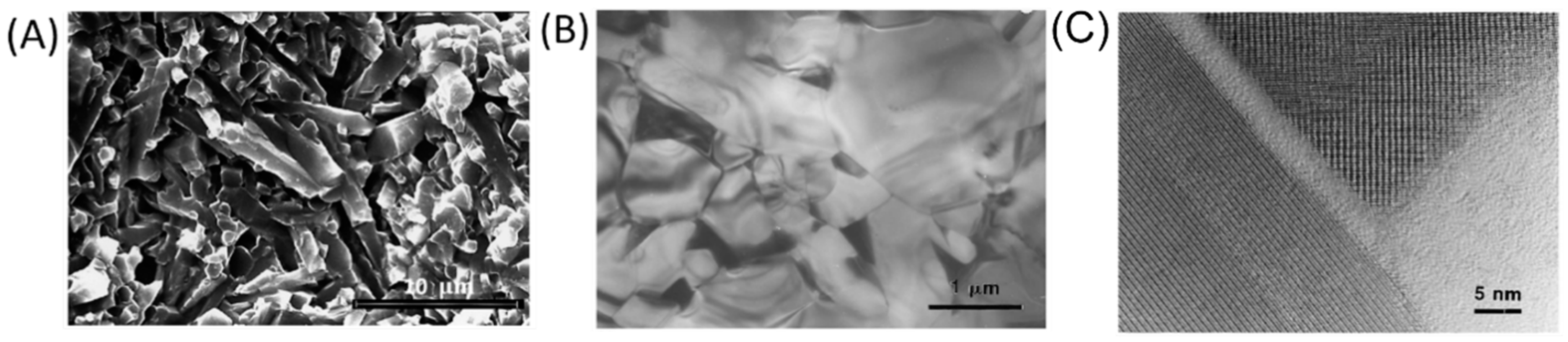
2. Synthesis and Manufacturing Process of Si3N4
3. Mechanical Properties of Si3N4
3.1. Basic Mechanical Properties
3.2. Methods to Enhance the Mechanical Properties of Si3N4
| Author | Ref. | Materials | Remarks | Bending Strength (MPa) | Flexural Strength (MPa) | Vickers Hardness (GPa) | Young’s Modulus (GPa) | Weibull Modulus | Poisson’s Ratio | Fracture Toughness (MPa/m2) | Fracture Strength (MPa) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chen et al. | [42] | Si3N4 | Disks 3 mm in diameter and typically range in thickness from 250 to 400 μm | / | / | 12–13 | 299 | / | 0.270 | / | / |
| Silva et al. | [59] | Si3N4 (SN1) | Composition with 91 wt.% Si3N4, 3 wt.% Al2O3, 3 wt.% Y2O3, and 3 wt.% Yb2O3 | / | / | 11.1 ± 0.2 | Assuming 300 | / | / | 5.0 ± 0.4 | / |
| Si3N4 (SN4) | Composition with 90 wt.% Si3N4, 6 wt.% Al2O3, and 4 wt.% Y2O3 | / | / | 13.2 ± 0.2 | Assuming 300 | / | / | 4.5 ± 0.2 | / | ||
| Bal et al. | [64] | Si3N4 | Composition with 90 wt.% Si3N4, 4 wt.% Al2O3, and 6 wt.% Y2O3. | / | 923 ± 70 | 14–16 | 300–320 | 19 | / | 10 ± 1 | / |
| Becher et al. | [38] | Si3N4 | 6.25 wt.% Y2O3 + 1 wt.% Al2O3. Average grain diameter: 0.3 mm/2 mm, distinctly bimodal | / | / | / | / | / | / | / | 1144 ± 126 |
| 6.25 wt.% Y2O3 + 1 wt.% Al2O3. Average grain diameter: ~0.4 mm, and monomodal | 660 ± 165 | ||||||||||
| 5 wt.% Y2O3 + 2 wt.% Al2O3. Average grain diameter: 10.3 mm/2 mm, distinctly bimodal | 1011 ± 78 | ||||||||||
| 5 wt.% Y2O3 + 2 wt.% Al2O3. Average grain diameter: 0.5 mm, monomodal with definite tail to larger sizes | 660 ± 20 | ||||||||||
| Liu et al. | [56] | Si3N4 | Commercially available Si3N4 powder (E-10, UBE Industries, Japan) was mixed with 3 wt.% MgO (99.9%), 1.5 wt.% Al2O3 (99.9%), and 3.5 wt.% SiO2 (99.9%) additives. | / | 1060 | 14.2 | / | / | / | 6.4 | / |
| Ling et al. | [55] | Si3N4 | Si3N4 + 5 wt.% MgO + 4 wt.% Y2O3 (sintered at 1700 °C during 60 min) | 950 | / | / | / | / | / | 7.5 | / |
| Li et al. | [35] | Si3N4/n-SiC | Si3N4 /n-SiC (85 wt.% Si3N4 + 5 wt.% n-SiC + 5 wt.% Al2O3 + 5 wt.% Y2O3) at sintering temperature of 1600 °C and holding time of 10 min | / | / | 14.44 | / | / | / | 7.77 | / |
| Benjamin et al. | [53] | Si3N4 | HPSi3N4 (density 99.6%), hot pressing | / | / | 1640 HV | / | 10.7 | / | 6.2 | 1210 |
| LPSSi3N4 (density 96.7%), pressureless sintering | 1565 HV | 10.7 | 7.1 | 990 | |||||||
| McEntire et al. | [31] | Si3N4 | 6 wt.% Y2O3, 4 wt.% Al2O3, 90 wt.% Si3N4 | / | 995 | / | / | / | / | 10.6 | / |
| Mauro et al. | [62] | Si3N4 based composite | 90 vol.% Si3N4 + 10 vol.% bioactive glass | / | 934 ± 215.5 | 15.29 ± 0.51 | 276 | / | / | / | / |
| 91.3 vol.% Si3N4 + 8.7 vol.% MgO | 969 ± 149.2 | 18.70 ± 6.63 | 316 | ||||||||
| 65 vol.% (93 wt.% Si3N4 + 2 wt.% Y2O3 + 5 wt.% Al2O3) + 35 vol.% TiN | 835 ± 116.0 | 14.70 ± 0.70 | 354 | ||||||||
| Blugan et al. | [63] | Si3N4 - Titanium Nitride Composites | Si3N4–TiN composites with 0 wt.% TiN | 790 ± 122.0 | / | / | 303 | / | / | 4.26 ± 0.09 | / |
| Si3N4–TiN composites with 10 wt.% TiN | 685 ± 51.6 | 311 | 4.47 ± 0.03 | ||||||||
| Si3N4–TiN composites with 20 wt.% TiN | 884 ± 32.6 | 317 | 4.62 ± 0.11 | ||||||||
| Si3N4–TiN composites with 30 wt.% TiN | 785 ± 51.2 | 330 | 4.71 ± 0.05 |
4. Osteogenesis Performance of Si3N4
4.1. In Vitro Cellular Response and In Vivo Study of Si3N4
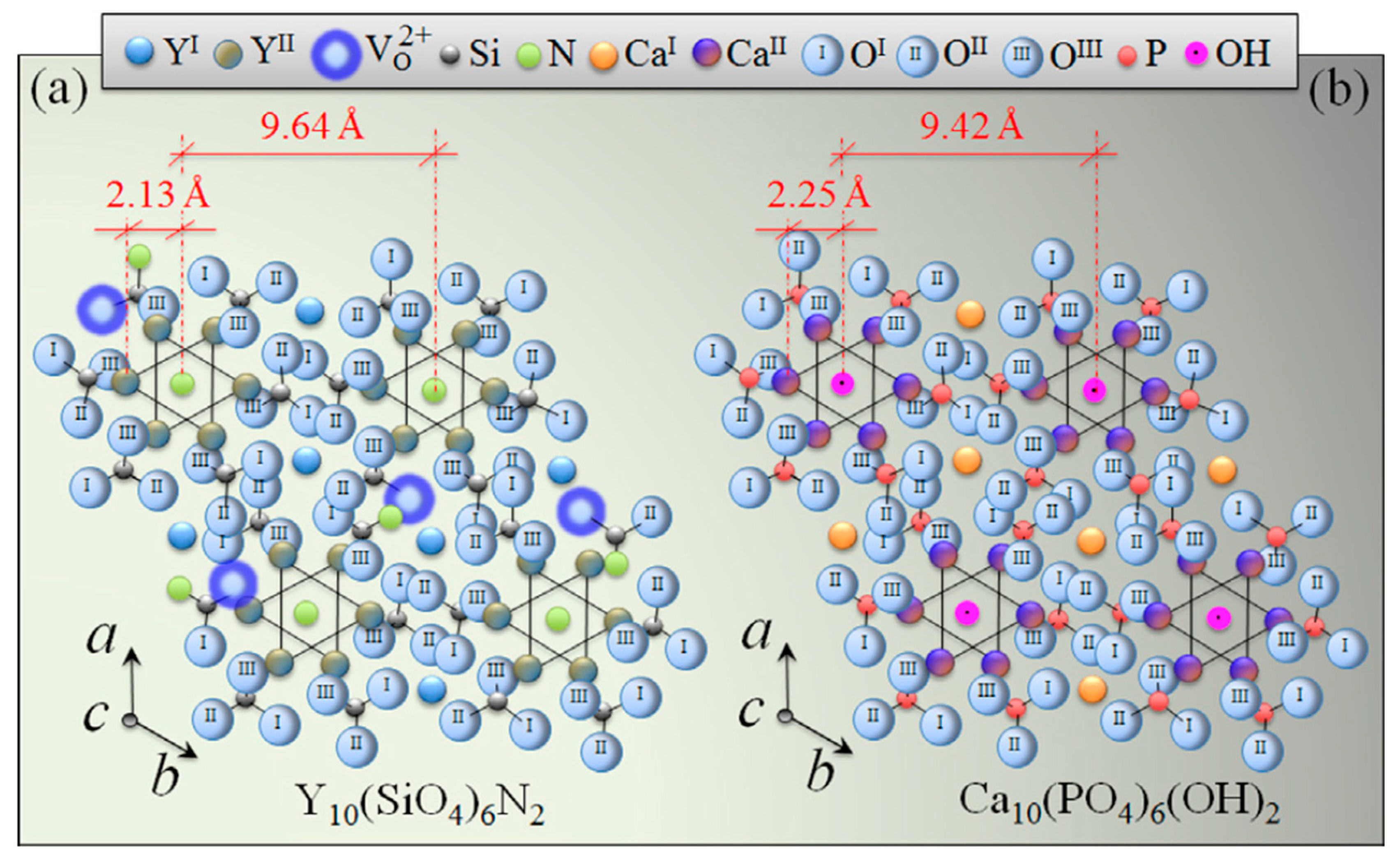
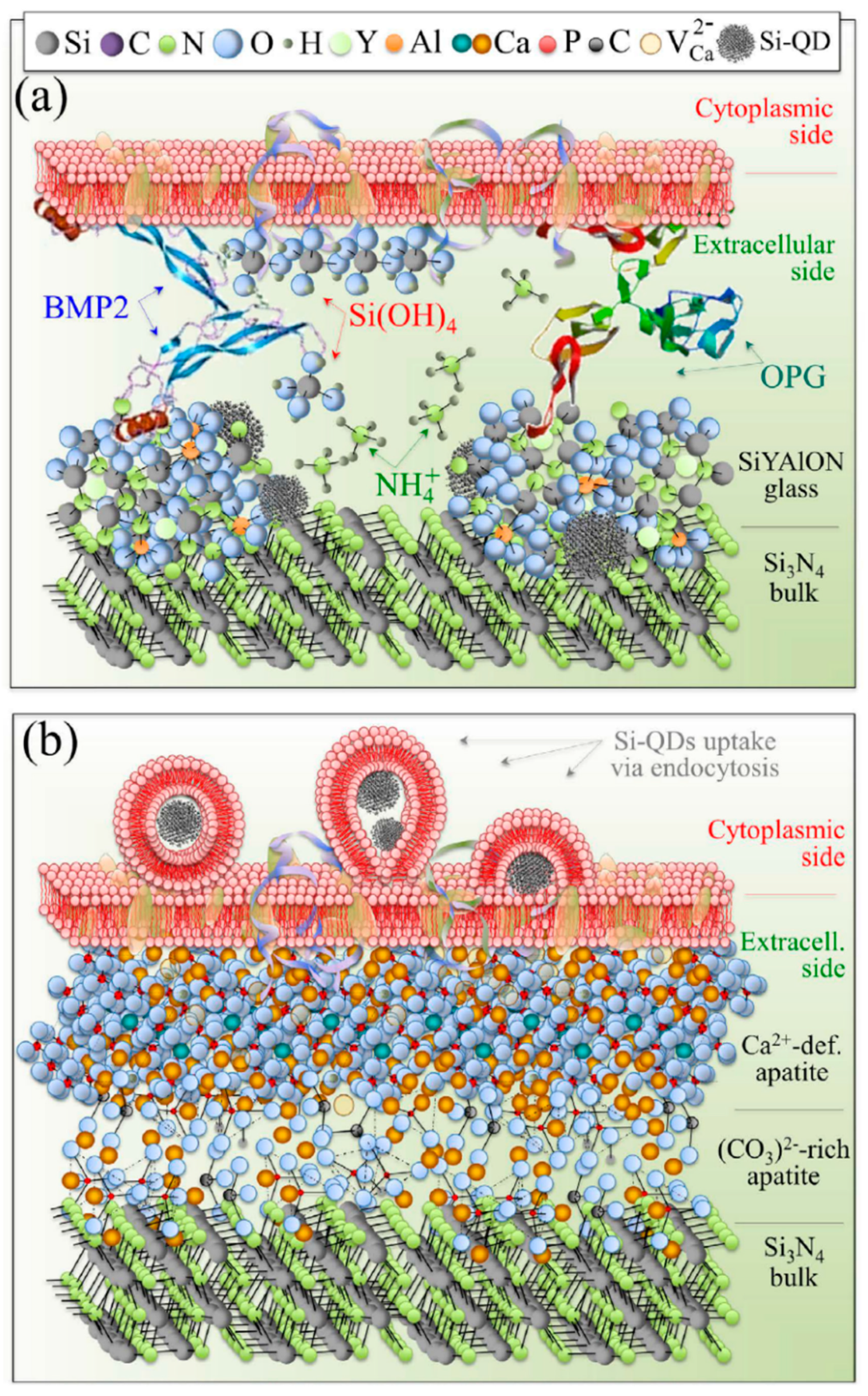
4.2. Mechanism and Influence Factors of Osteogenesis Properties
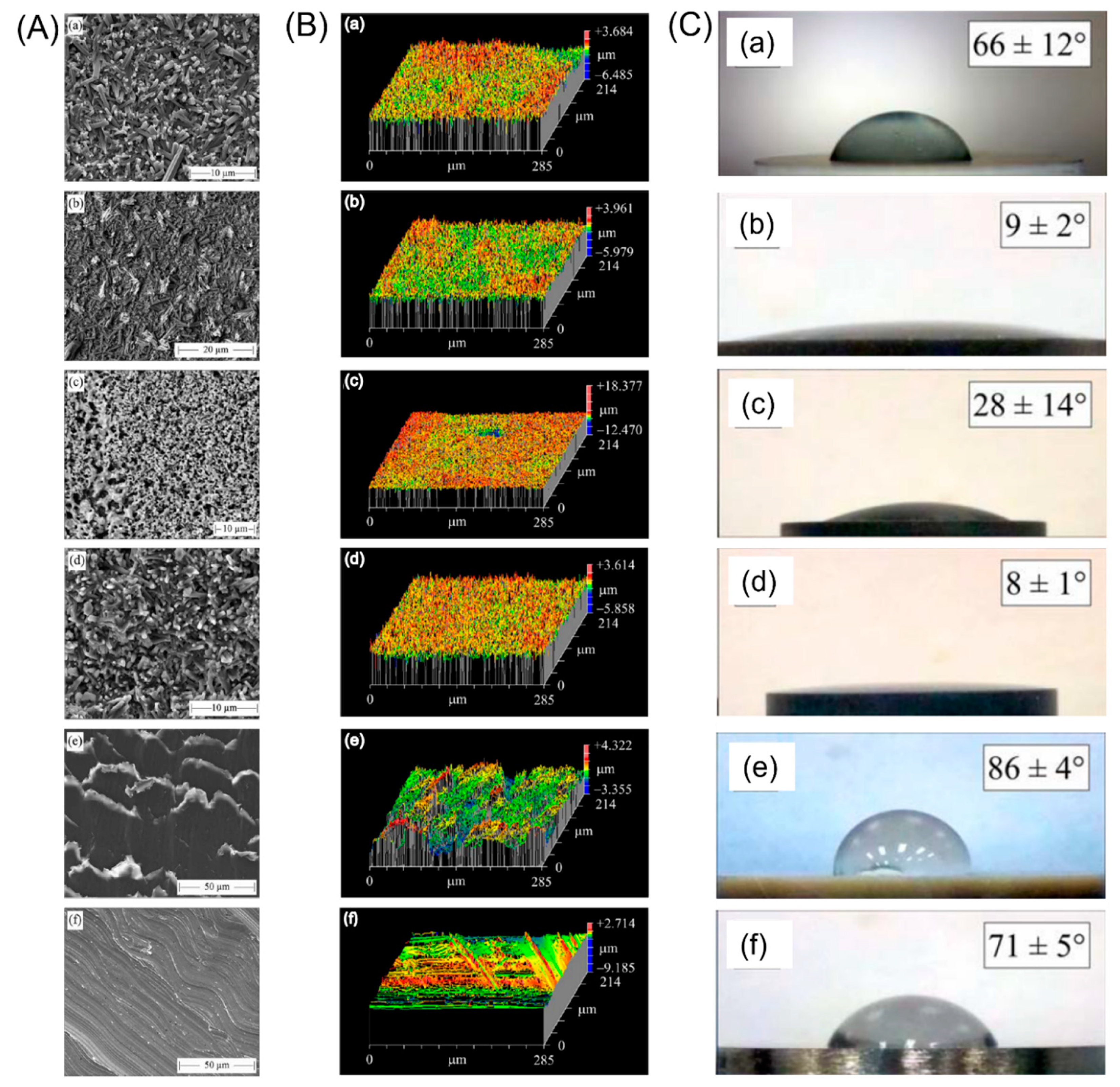
5. Antibacterial Properties of Si3N4
6. Medical Application of Si3N4
6.1. Spinal Reconstruction Field
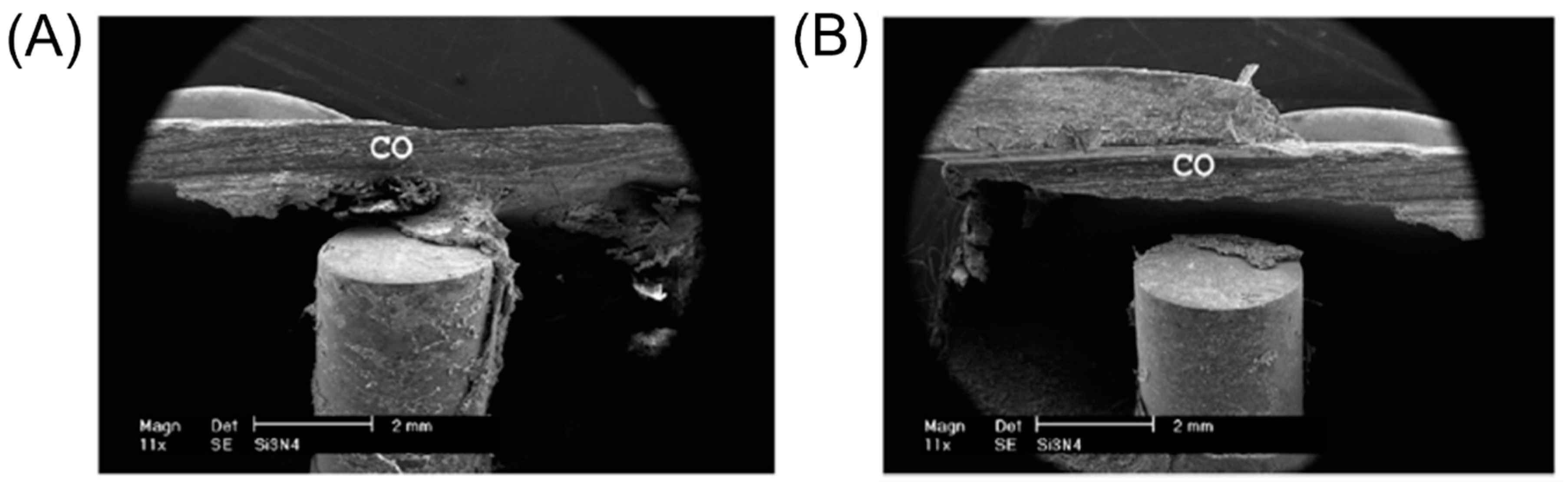
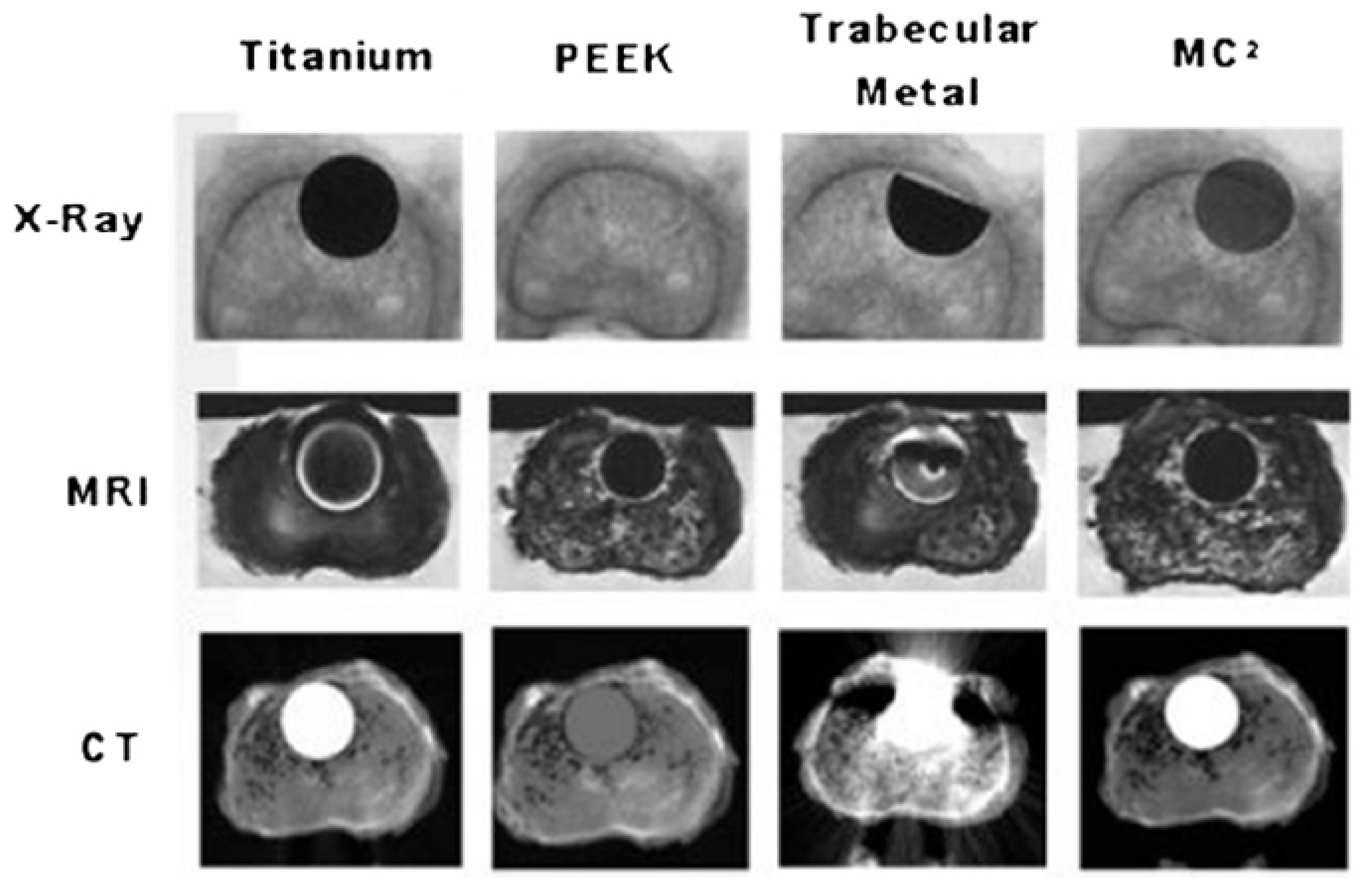
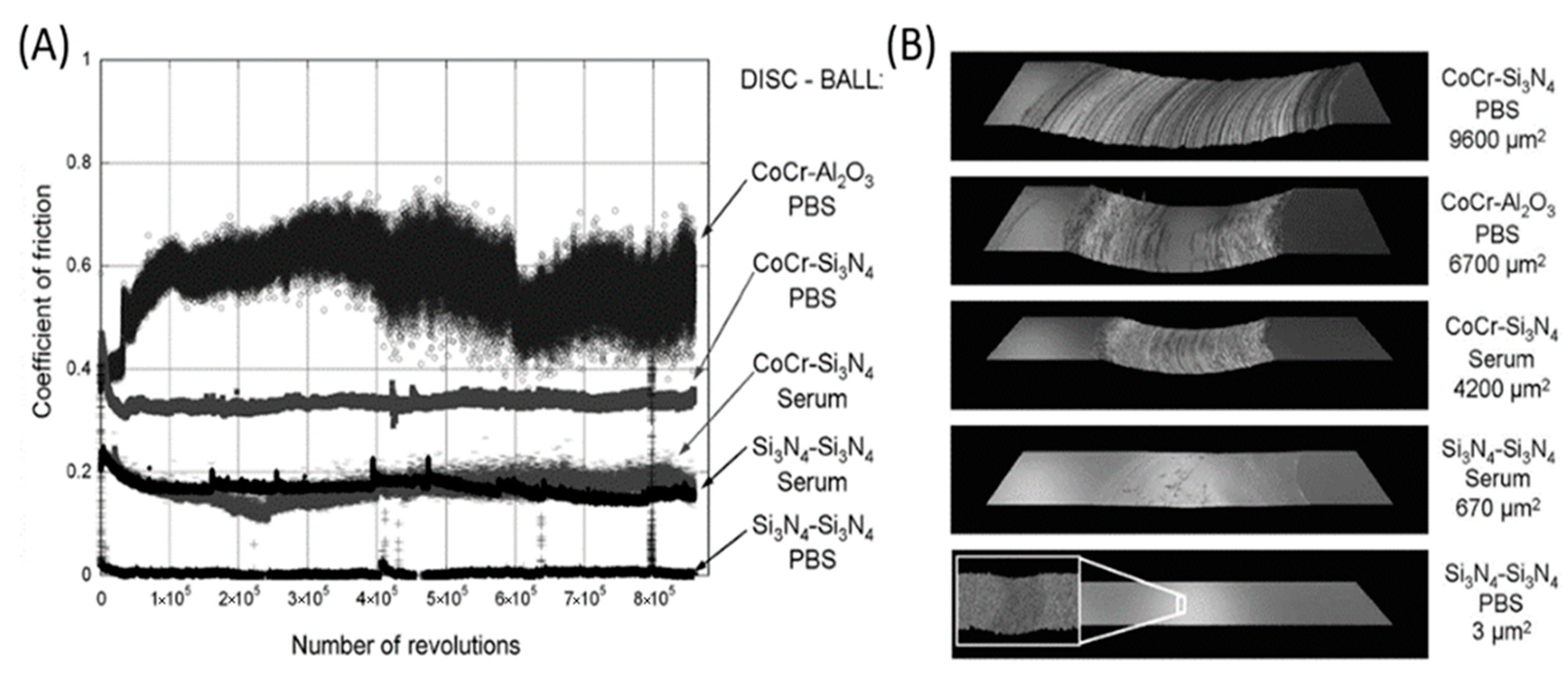
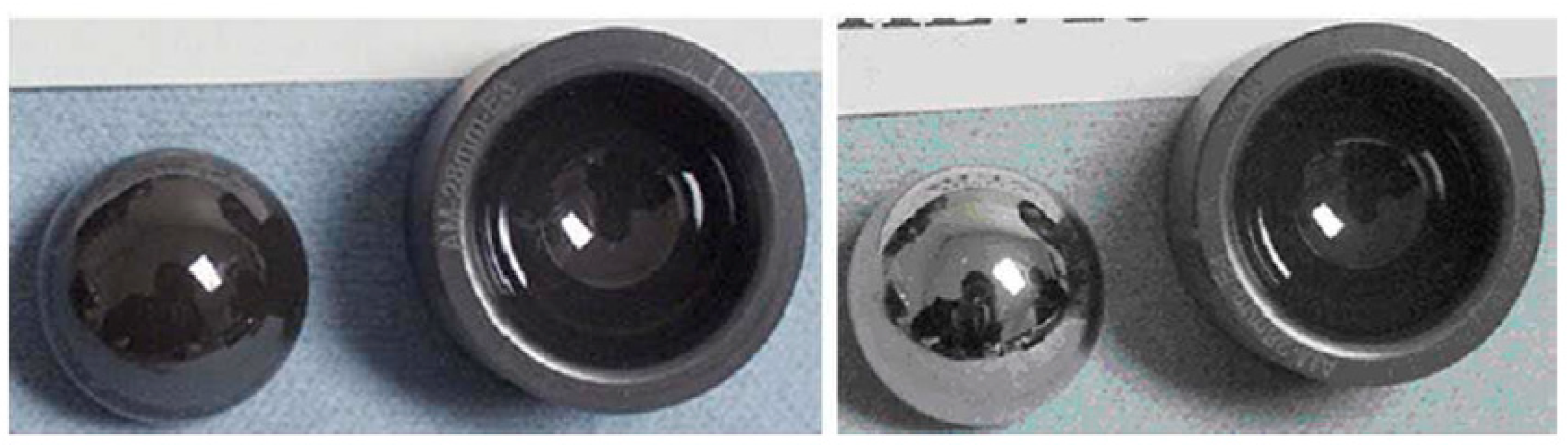
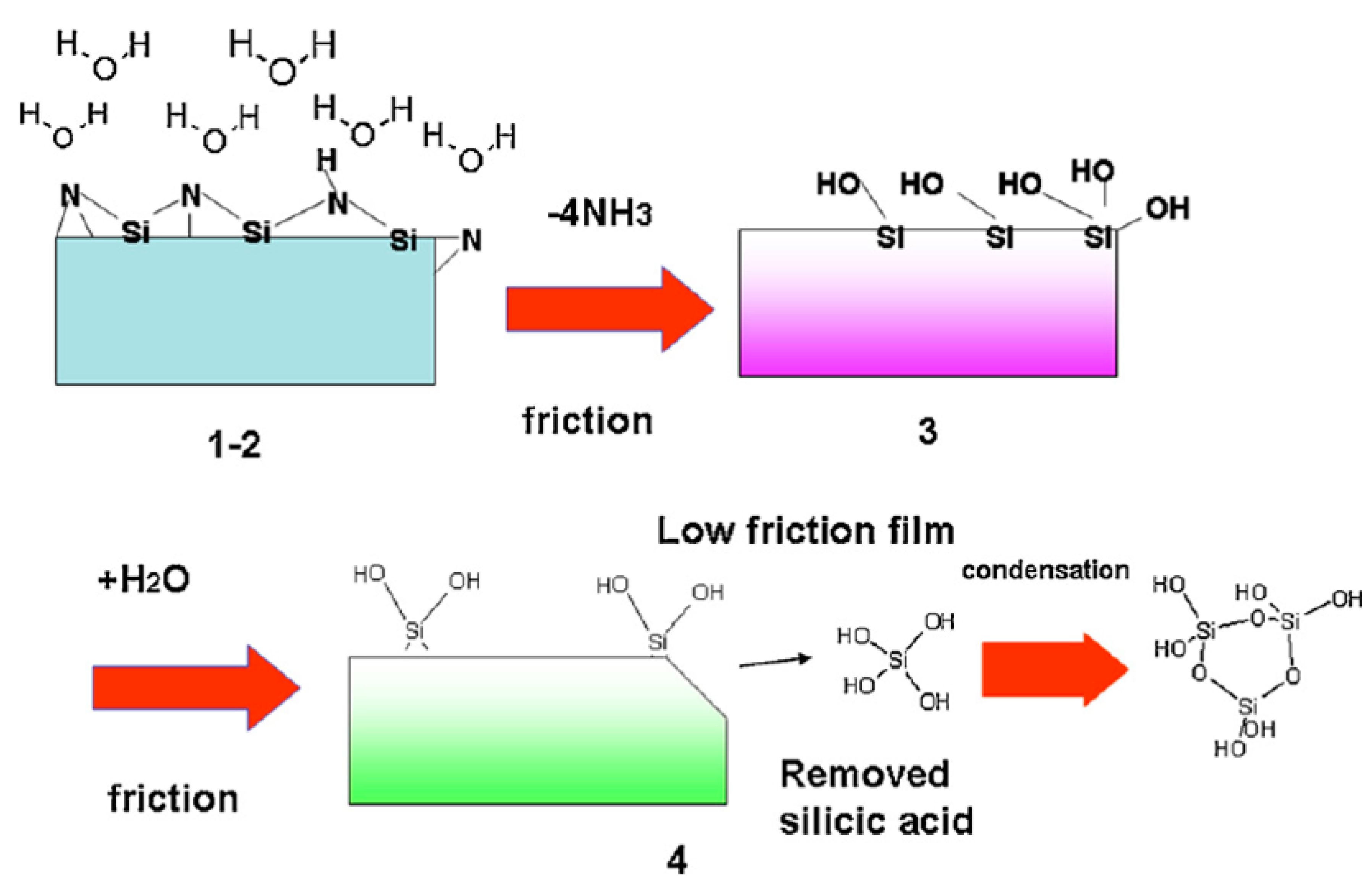
6.2. Joint Replacement Surgery
6.3. Other Clinical and Potential Use
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Riley, F.L. Silicon nitride and related materials. J. Am. Ceram. Soc. 2000, 83, 245–265. [Google Scholar] [CrossRef]
- Mantripragada, V.P.; Lecka-Czernik, B.; Ebraheim, N.A.; Jayasuriya, A.C. An overview of recent advances in designing orthopedic and craniofacial implants. J. Biomed. Mater. Res. Part A 2013, 101, 3349–3364. [Google Scholar] [CrossRef] [PubMed]
- Zerr, A.; Miehe, G.; Serghiou, G.; Schwarz, M.; Kroke, E.; Riedel, R.; Fuess, H.; Kroll, P.; Boehler, R. Synthesis of cubic silicon nitride. Nature 1999, 400, 340–342. [Google Scholar] [CrossRef]
- Riedel, R.; Kleebe, H.J.; Schonfelder, H.; Aldinger, F. A Covalent Micro Nanocomposite Resistant to High-Temperature Oxidation. Nature 1995, 374, 526–528. [Google Scholar] [CrossRef]
- Pelleg, J. Creep in Silicon Nitride (Si3N4). Creep Ceram. 2017, 241, 403–441. [Google Scholar]
- Amaral, M.; Lopes, M.A.; Silva, R.F.; Santos, J.D. Densification route and mechanical properties of Si3N4-bioglass biocomposites. Biomaterials 2002, 23, 857–862. [Google Scholar] [CrossRef]
- Bal, S.B.; Rahaman, M.N. Orthopedic applications of silicon nitride ceramics. Acta Biomater. 2012, 8, 2889–2898. [Google Scholar] [CrossRef]
- Rambo, W.M. Treatment of lumbar discitis using silicon nitride spinal spacers: A case series and literature review. Int. J. Surg. Case Rep. 2018, 43, 61–68. [Google Scholar] [CrossRef]
- McEntire, B.J.; Bal, B.S.; Rahaman, M.N.; Chevalier, J.; Pezzotti, G. Ceramics and ceramic coatings in orthopaedics. J. Eur. Ceram. Soc. 2015, 35, 4327–4369. [Google Scholar] [CrossRef]
- Muthunilavan, N.; Rajaram, G. Effect on lubrication regimes with silicon nitride and bearing steel balls. Tribol. Int. 2017, 116, 403–413. [Google Scholar]
- Bocanegra-Bernal, H.M.; Matovic, B. Mechanical properties of silicon nitride-based ceramics and its use in structural applications at high temperatures. Mater. Sci. Eng. A-Struct. Mater. Prop. Microstruct. Process. 2010, 527, 1314–1338. [Google Scholar] [CrossRef]
- Willmann, G. Improving bearing surfaces of artificial joints. Adv. Eng. Mater. 2001, 3, 135–141. [Google Scholar] [CrossRef]
- Kue, R.; Sohrabi, A.; Nagle, D.; Frondoza, C.; Hungerford, D. Enhanced proliferation and osteocalcin production by human osteoblast-like MG63 cells on silicon nitride ceramic discs. Biomaterials 1999, 20, 1195–1201. [Google Scholar] [CrossRef]
- Sorrell, C.; Hardcastle, P.; Druitt, R.; Howlett, C.; McCartney, E. Results of 15-Year Clinical Study of Reaction Bonded Silicon Nitride Intervertebral Spacers. In Proceedings of the 7th World Biomaterials Congress, Sydney Convention & Exhibition Centre, Darling Harbour, Sydney, SYD, Australia, 17–21 May 2004; p. 1872. [Google Scholar]
- Pezzotti, G.; Marin, E.; Adachi, T.; Rondinella, A.; Boschetto, F.; Zhu, W.L.; Sugano, N.; Bock, R.M.; McEntire, B.; Bal, S.B. Bioactive silicon nitride: A new therapeutic material for osteoarthropathy. Sci. Rep. 2017, 7, 44848. [Google Scholar] [CrossRef]
- Rosaa, M.; Casaril, F.; Valle, M.; Poli, S. Optimization of the Industrial Synthesis of Silicon Carbide—Reaction Bonded Silicon Nitride (Sic-Rbsn). Dev. Strateg. Mater. Comput. Des. V 2015, 35, 245–257. [Google Scholar]
- Tong, J.F.; Chen, D.M.; Li, B.W.; Ling, H.H.; Wang, L. Microstructure and Performance of the Hot-Pressed Silicon Nitride Ceramics with Lu(2)O(3) Additives. High-Perform. Ceram. Vi 2010, 434–435, 37–41. [Google Scholar]
- Qiao, C.G.; Zhou, M.; Wang, M. Nanoindentation Test and Stress Fields Simulation of Hot-pressed silicon nitride ceramic. Adv. Manuf. Technol. 2012, 472–475, 2207–2210. [Google Scholar] [CrossRef]
- Radchenko, A.K.; Rachek, A.P.; Orlovskaya, N.A.; Mosina, T.V.; Lugovoi, N.I.; Subbotin, V.I.; Gi, I.; Dobido, R.; Lewis, M.; Nepomniashchii, V.V. Anisotropy of destruction viscosity of hot-pressed silicon nitride. Refract. Ind. Ceram. 2006, 47, 228–233. [Google Scholar] [CrossRef]
- Qadir, A.; Fogarassy, Z.; Horvath, Z.E.; Balazsi, K.; Balazsi, C. Effect of the oxidization of Si3N4 powder on the microstructural and mechanical properties of hot isostatic pressed silicon nitride. Ceram. Int. 2018, 44, 14601–14609. [Google Scholar] [CrossRef]
- Wills, R.R.; Brockway, M.C. Preliminary-Observations on the Hot Isostatic Pressing of Silicon-Nitride. Am. Ceram. Soc. Bull. 1980, 59, 827. [Google Scholar]
- Upadhya, K.; Hoffman, W.P.; Rodgers, S.L. Synthesis and hot isostatic pressing of nanocrystalline silicon nitride powders. J. Mater. Synth. Process. 1997, 5, 141–151. [Google Scholar]
- Hengst, R.R.; Busovne, B.J.; Kennard, F.L. Evaluation of Alternative Sintering Aids for Pressureless Sintered Silicon-Nitride. Am. Ceram. Soc. Bull. 1984, 63, 1000. [Google Scholar]
- Matovic, B.; Rixecker, G.; Aldinger, F. Pressureless sintering of silicon nitride with lithia and yttria. J. Eur. Ceram. Soc. 2004, 24, 3395–3398. [Google Scholar] [CrossRef]
- Duan, Y.S.; Zhang, J.X.; Li, X.G.; Bai, H.N.; Sajgalik, P.; Jiang, D.L. High thermal conductivity silicon nitride ceramics prepared by pressureless sintering with ternary sintering additives. Int. J. Appl. Ceram. Technol. 2019, 16, 1399–1406. [Google Scholar] [CrossRef]
- Kleebe, J.H.; Meissner, E.; Ziegler, G. Influence of Si3n4 Interface Chemistry on Both Grain Morphology and Fracture-Resistance. J. De Phys. Iv 1993, 3, 1393–1397. [Google Scholar] [CrossRef][Green Version]
- Chen, F.J.; Zhong, M. Fabrication and release of silicon nitride micro string array by convection freeze sublimation method at atmospheric pressure. J. Micromech. Microeng. 2018, 28, 105019. [Google Scholar] [CrossRef]
- Zhu, X.W.; Hayashi, H.; Zhou, Y.; Hirao, K. Influence of additive composition on thermal and mechanical properties of beta-Si3N4 ceramics. J. Mater. Res. 2004, 19, 3270–3278. [Google Scholar] [CrossRef]
- Pezzotti, G.; Bock, R.M.; Adachi, T.; Rondinella, A.; Boschetto, F.; Zhu, W.L.; Marin, E.; McEntire, B.; Bal, B.S.; Mazda, O. Silicon nitride surface chemistry: A potent regulator of mesenchymal progenitor cell activity in bone formation. Appl. Mater. Today 2017, 9, 82–95. [Google Scholar] [CrossRef]
- Liu, Q.M.; Nemat-Nasser, S. The microstructure and boundary phases of in-situ reinforced silicon nitride. Mater. Sci. Eng. a-Struct. Mater. Prop. Microstruct. Process. 1998, 254, 242–252. [Google Scholar] [CrossRef]
- McEntire, J.B.; Lakshminarayanan, R. Processing and Characterization of Silicon Nitride Bioceramics. Bioceram. Dev. Appl. 2016, 6, 1–10. [Google Scholar] [CrossRef]
- Laarz, E.; Zhmud, B.V.; Bergstrom, L. Dissolution and deagglomeration of silicon nitride in aqueous medium. J. Am. Ceram. Soc. 2000, 83, 2394–2400. [Google Scholar] [CrossRef]
- Mazzocchi, M.; Gardini, D.; Traverso, P.L.; Faga, M.G.; Bellosi, A. On the possibility of silicon nitride as a ceramic for structural orthopaedic implants. Part II: Chemical stability and wear resistance in body environment. J. Mater. Sci. -Mater. Med. 2008, 19, 2889–2901. [Google Scholar] [CrossRef] [PubMed]
- Wan, J.L.; Duan, R.G.; Gasch, M.J.; Mukherjee, A.K. Highly creep-resistant silicon nitride/silicon carbide nano-nano composites. J. Am. Ceram. Soc. 2006, 89, 274–280. [Google Scholar] [CrossRef]
- Qiao, L.; Wang, Z.; Lu, T.; Yuan, J. Effects of Microwave Sintering Temperature and Holding Time on Mechanical Properties and Microstructure of Si3N4/n-SiC ceramics. Materials 2019, 12, 3837. [Google Scholar] [CrossRef]
- Chen, W.W.; Rajendran, A.M.; Song, B.; Nie, X. Dynamic fracture of ceramics in armor applications. J. Am. Ceram. Soc. 2007, 90, 1005–1018. [Google Scholar] [CrossRef]
- Tian, X.H.; Zhao, J.; Wang, Z.B.; Liu, X.H. Design and fabrication of Si3N4/(W, Ti)C graded nano-composite ceramic tool materials. Ceram. Int. 2016, 42, 13497–13506. [Google Scholar] [CrossRef]
- Becher, P.F.; Sun, E.Y.; Plucknett, K.P.; Alexander, K.B.; Hsueh, C.H.; Lin, H.T.; Waters, S.B.; Westmoreland, C.G.; Kang, E.S.; Hirao, K.; et al. Microstructural design of silicon nitride with improved fracture toughness: I, effects of grain shape and size. J. Am. Ceram. Soc. 1998, 81, 2821–2830. [Google Scholar] [CrossRef]
- Rudnayova, E.; Dusza, J.; Kupkova, M. Comparison of Fracture-Toughness Measuring Methods Applied on Silicon-Nitride Ceramics. J. De Phys. Iv. 1993, 3, 1273–1276. [Google Scholar] [CrossRef]
- Turon-Vinas, M.; Anglada, M. Assessment in Si3N4 of a new method for determining the fracture toughness from a surface notch micro-machined by ultra-short pulsed laser ablation. J. Eur. Ceram. Soc. 2015, 35, 1737–1741. [Google Scholar] [CrossRef]
- Park, D.S.; Choi, M.J.; Roh, T.W.; Kim, H.D.; Han, B.D. Orientation-dependent properties of silicon nitride with aligned reinforcing grains. J. Mater. Res. 2000, 15, 130–135. [Google Scholar] [CrossRef]
- Chen, C.F.; Ardell, A.J. Fracture toughness of ceramics and semi-brittle alloys using a miniaturized disk-bend test. Mater. Res. Innov. 2000, 3, 250–262. [Google Scholar] [CrossRef]
- Tavangarian, F.; Hui, D.; Li, G.Q. Crack-healing in ceramics. Compos. Part B Eng. 2018, 144, 56–87. [Google Scholar] [CrossRef]
- Nakatani, M.; Ando, K.; Houjou, K. Oxidation behaviour Of Si3N4/Y2O3 system ceramics and effect of crack-healing treatment on oxidation. J. Eur. Ceram. Soc. 2008, 28, 1251–1257. [Google Scholar] [CrossRef]
- Klemm, H. Silicon Nitride for High-Temperature Applications. J. Am. Ceram. Soc. 2010, 93, 1501–1522. [Google Scholar] [CrossRef]
- Choi, R.S.; Tikare, V. Crack Healing Behavior of Hot-Pressed Silicon-Nitride Due to Oxidation. Scr. Metall. Et Mater. 1992, 26, 1263–1268. [Google Scholar] [CrossRef]
- Wiederhorn, M.S.; Tighe, N.J. Structural Reliability of Yttria-Doped Hot-Pressed Silicon-Nitride at Elevated-Temperatures. J. Am. Ceram. Soc. 1983, 66, 884–889. [Google Scholar] [CrossRef]
- Easler, E.T.; Bradt, R.C.; Tressler, R.E. Effects of Oxidation and Oxidation under Load on Strength Distributions of Si3n4. J. Am. Ceram. Soc. 1982, 65, 317–320. [Google Scholar] [CrossRef]
- Santos, J.D.; Amaral, M.; Oliveira, S.M.; Lopes, M.A.; Silva, R.F. Silicon nitride-Bioglass (R) composite for biomedical applications. Bioceramics 2000, 192–195, 589–592. [Google Scholar]
- Pender, D.C.; Thompson, S.C.; Padture, N.P.; Giannakopoulos, A.E.; Suresh, S. Gradients in elastic modulus for improved contact-damage resistance. Part II: The silicon nitride-silicon carbide system. Acta Mater. 2001, 49, 3263–3268. [Google Scholar] [CrossRef]
- Du, X.Y.; Blugan, G.; Kunniger, T.; Lee, S.S.; Vladislavova, L.; Ferguson, S.J. Non-linear mechanical properties and dynamic response of silicon nitride bioceramic. Ceram. Int. 2021, 47, 33525–33536. [Google Scholar] [CrossRef]
- Xu, F.; Hu, X.F.; Zhao, J.H.; Yuan, Q.X. In Situ Observation of the Microstructure-evolution in Silicon Nitride Ceramics Sintering by Synchrotron Radiation X-ray Computed Tomography. Acta Chim. Sin. 2009, 67, 1205–1210. [Google Scholar]
- Cappi, B.; Neuss, S.; Salber, J.; Telle, R.; Knuchel, R.; Fischer, H. Cytocompatibility of high strength non-oxide ceramics. J. Biomed. Mater. Res. Part A 2010, 93a, 67–76. [Google Scholar] [CrossRef]
- Mizutani, T.; Matsuhiro, K.; Yamamoto, N. Advanced structural ceramics—From research to applications. J. Ceram. Soc. Jpn. 2006, 114, 905–910. [Google Scholar] [CrossRef]
- Ling, G.; Yang, H.T. Pressureless sintering of silicon nitride with Magnesia and Yttria. Mater. Chem. Phys. 2005, 90, 31–34. [Google Scholar] [CrossRef]
- Liu, X.H.; Huang, Z.Y.; Ge, Q.M.; Sun, X.W.; Huang, L.P. Microstructure and mechanical properties of silicon nitride ceramics prepared by pressureless sintering with MgO-Al2O3-SiO2 as sintering additive. J. Eur. Ceram. Soc. 2005, 25, 3353–3359. [Google Scholar] [CrossRef]
- Becher, P.F. Recent Advances in Microstructural Tailoring of Silicon Nitride Ceramics and the Effects on Thermal Conductivity and Fracture Properties. J. Korean Ceram. Soc. 2005, 42, 525–531. [Google Scholar]
- Lee, H.W.; Kim, H.E.; Cho, S.J. Microstructural evolution of gas-pressure-sintered Si3N4 with Yb2O3 as a sintering aid. J. Am. Ceram. Soc. 1997, 80, 2737–2740. [Google Scholar] [CrossRef]
- Silva, G.C.C.; Higa, O.Z.; Bressiani, J.C. Cytotoxic evaluation of silicon nitride-based ceramics. Mater. Sci. Eng. C Biomim. Supramol. Syst. 2004, 24, 643–646. [Google Scholar] [CrossRef]
- Shi, F.; Miao, H.Z.; Peng, Z.J.; Si, W.J.; Qi, L.H.; Li, W.Z. Bending strength of ceramics implanted by titanium, zirconium, and chromium ions with MEVVA source. Key Eng. Mater. 2005, 280–283, 1211–1212. [Google Scholar]
- Seiner, H.; Ramirez, C.; Koller, M.; Sedlak, P.; Landa, M.; Miranzo, P.; Belmonte, M.; Osendi, M.I. Elastic properties of silicon nitride ceramics reinforced with graphene nanofillers. Mater. Des. 2015, 87, 675–680. [Google Scholar] [CrossRef]
- Mazzocchi, M.; Bellosi, A. On the possibility of silicon nitride as a ceramic for structural orthopaedic implants. Part I: Processing, microstructure, mechanical properties, cytotoxicity. J. Mater. Sci. Mater. Med. 2008, 19, 2881–2887. [Google Scholar] [CrossRef]
- Blugan, G.; Hadad, M.; Janczak-Rusch, J.; Kuebler, J.; Graule, T. Fractography, mechanical properties, and microstructure of commercial silicon nitride-titanium nitride composites. J. Am. Ceram. Soc. 2005, 88, 926–933. [Google Scholar] [CrossRef]
- Bal, B.S.; Khandkar, A.; Lakshminarayanan, R.; Clarke, I.; Hoffman, A.A.; Rahaman, M.N. Fabrication and Testing of Silicon Nitride Bearings in Total Hip Arthroplasty Winner of the 2007 "HAP" PAUL Award. J. Arthroplast. 2009, 24, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Neumann, A.; Reske, T.; Held, M.; Jahnke, K.; Ragoss, C.; Maier, H.R. Comparative investigation of the biocompatibility of various silicon nitride ceramic qualities in vitro. J. Mater. Sci. Mater. Med. 2004, 15, 1135–1140. [Google Scholar] [CrossRef] [PubMed]
- Guedes e Silva, C.C.; Konig, B.; Carbonari, M.J.; Yoshimoto, M.; Allegrini, S.; Bressiani, J.C. Tissue response around silicon nitride implants in rabbits. J. Biomed. Mater. Res. Part A 2008, 84a, 337–343. [Google Scholar] [CrossRef]
- Lee, S.S.; Huber, S.; Ferguson, S.J. Comprehensive in vitro comparison of cellular and osteogenic response to alternative biomaterials for spinal implants. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 127, 112251. [Google Scholar] [CrossRef] [PubMed]
- Silva, C.C.G.E.; Konig, B.; Carbonari, M.J.; Yoshimoto, M.; Allegrini, S.; Bressiani, J.C. Bone growth around silicon nitride implants—An evaluation by scanning electron microscopy. Mater. Charact. 2008, 59, 1339–1341. [Google Scholar] [CrossRef]
- Howlett, R.C.; Mccartney, E.; Ching, W. The Effect of Silicon-Nitride Ceramic on Rabbit Skeletal Cells and Tissue—An In vitro and In vivo Investigation. Clin. Orthop. Relat. Res. 1989, 244, 293–304. [Google Scholar] [CrossRef]
- Webster, T.J.; Patel, A.A.; Rahaman, M.N.; Bal, B.S. Anti-infective and osteointegration properties of silicon nitride, poly(ether ether ketone), and titanium implants. Acta Biomater. 2012, 8, 4447–4454. [Google Scholar] [CrossRef]
- Neumann, A.; Kramps, M.; Ragoss, C.; Maier, H.R.; Jahnke, K. Histological and microradiographic appearances of Silicon Nitride and Aluminum Oxide in a rabbit femur implantation model. Mater. Und. Werkst. 2004, 35, 569–573. [Google Scholar] [CrossRef]
- Neumann, A.; Unkel, C.; Werry, C.; Herborn, C.U.; Maier, H.R.; Ragoss, C.; Jahnke, K. Prototype of a silicon nitride ceramic-based miniplate osteofixation system for the midface. Otolaryngol.-Head Neck Surg. 2006, 134, 923–930. [Google Scholar] [CrossRef]
- Kersten, R.F.M.R.; Wu, G.; Pouran, B.; van der Veen, A.J.; Weinans, H.H.; de Gast, A.; Oner, F.C.; van Gaalen, S.M. Comparison of polyetheretherketone versus silicon nitride intervertebral spinal spacers in a caprine model. J. Biomed. Mater. Res. Part B Appl. Biomater. 2019, 107, 688–699. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.M.; Olsen, R. Bone ingrowth into porous silicon nitride. J. Biomed. Mater. Res. Part A 2010, 92a, 1598–1605. [Google Scholar] [CrossRef] [PubMed]
- Beck, G.R.; Ha, S.W.; Camalier, C.E.; Yamaguchi, M.; Li, Y.; Lee, J.K.; Weitzmann, M.N. Bioactive silica-based nanoparticles stimulate bone-forming osteoblasts, suppress bone-resorbing osteoclasts, and enhance bone mineral density in vivo. Nanomed. Nanotechnol. Biol. Med. 2012, 8, 793–803. [Google Scholar] [CrossRef]
- Pezzotti, G.; Oba, N.; Zhu, W.L.; Marin, E.; Rondinella, A.; Boschetto, F.; McEntire, B.; Yamamoto, K.; Bal, B.S. Human osteoblasts grow transitional Si/N apatite in quickly osteointegrated Si3N4 cervical insert. Acta Biomater. 2017, 64, 411–420. [Google Scholar] [CrossRef]
- Zanocco, M.; Marin, E.; Rondinella, A.; Boschetto, F.; Horiguchi, S.; Zhu, W.; McEntire, B.J.; Bock, R.M.; Bal, B.S.; Pezzotti, G. The role of nitrogen off-stoichiometry in the osteogenic behavior of silicon nitride bioceramics. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 105, 110053. [Google Scholar] [CrossRef] [PubMed]
- Dante, C.R.; Kajdas, C.K. A review and a fundamental theory of silicon nitride tribochemistry. Wear 2012, 288, 27–38. [Google Scholar] [CrossRef]
- Finke, B.; Hempel, F.; Testrich, H.; Artemenko, A.; Rebl, H.; Kylian, O.; Meichsner, J.; Biederman, H.; Nebe, B.; Weltmann, K.D.; et al. Plasma processes for cell-adhesive titanium surfaces based on nitrogen-containing coatings. Surf. Coat. Technol. 2011, 205, S520–S524. [Google Scholar] [CrossRef]
- Kwon, S.; Lee, S.S.; Sivashanmugam, A.; Kwon, J.; Kim, S.H.L.; Noh, M.Y.; Kwon, S.K.; Jayakumar, R.; Hwang, N.S. Bioglass-Incorporated Methacrylated Gelatin Cryogel for Regeneration of Bone Defects. Polymers 2018, 10, 914. [Google Scholar] [CrossRef]
- Kaur, G.; Pickrell, G.; Kimsawatde, G.; Homa, D.; Allbee, H.A.; Sriranganathan, N. Synthesis, cytotoxicity, and hydroxyapatite formation in 27-Tris-SBF for sol-gel based CaO-P2O5-SiO2-B2O3-ZnO bioactive glasses. Sci. Rep. 2014, 4, 4392. [Google Scholar] [CrossRef]
- Costa, D.; Tougerti, A.; Tielens, F.; Gervais, C.; Stievano, L.; Lambert, J.F. DFT study of the adsorption of microsolvated glycine on a hydrophilic amorphous silica surface. Phys. Chem. Chem. Phys. 2008, 10, 6360–6368. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.W.; Loo, C.Y.; Rohanizadeh, R. A review of chemical surface modification of bioceramics: Effects on protein adsorption and cellular response. Colloids Surf. B Biointerfaces 2014, 122, 823–834. [Google Scholar] [CrossRef] [PubMed]
- Lange, F.F.; Singhal, S.C.; Kuznicki, R.C. Phase Relations and Stability Studies in Si3n4-Sio2-Y2o3 Pseudoternary System. J. Am. Ceram. Soc. 1977, 60, 249–252. [Google Scholar] [CrossRef]
- Epstein, M.; Levitzki, A.; Reuben, J. Binding of Lanthanides and of Divalent Metal-Ions to Porcine Trypsin. Biochemistry 1974, 13, 1777–1782. [Google Scholar] [CrossRef] [PubMed]
- Du, X.Y.; Yu, B.; Pei, P.; Ding, H.F.; Yu, B.Q.; Zhu, Y.F. 3D printing of pearl/CaSO4 composite scaffolds for bone regeneration. J. Mater. Chem. B 2018, 6, 499–509. [Google Scholar] [CrossRef]
- Precnerova, M.; Bodigova, K.; Frajkorova, F.; Galuskova, D.; Novakova, Z.V.; Vojtassak, J.; Lences, Z.; Sajgalik, P. In vitro bioactivity of silicon nitride-hydroxyapatite composites. Ceram. Int. 2015, 41, 8100–8108. [Google Scholar] [CrossRef]
- Silva, C.C.G.E.; Rigo, E.C.D.; Marchi, J.; Bressiani, A.H.D.; Bressiani, J.C. Hydroxyapatite Coating on Silicon Nitride Surfaces Using the Biomimetic Method. Mater. Res. -Ibero-Am. J. Mater. 2008, 11, 47–50. [Google Scholar] [CrossRef]
- Frajkorova, F.; Bodisova, K.; Bohac, M.; Bartonickova, E.; Sedlacek, J. Preparation and characterisation of porous composite biomaterials based on silicon nitride and bioglass. Ceram. Int. 2015, 41, 9770–9778. [Google Scholar] [CrossRef]
- Amaral, M.; Costa, M.A.; Lopes, M.A.; Silva, R.F.; Santos, J.D.; Fernandes, M.H. Si3N4-bioglass composites stimulate the proliferation of MG63 osteoblast-like cells and support the osteogenic differentiation of human bone marrow cells. Biomaterials 2002, 23, 4897–4906. [Google Scholar] [CrossRef]
- Gorth, D.J.; Puckett, S.; Ercan, B.; Webster, T.J.; Rahaman, M.; Bal, B.S. Decreased bacteria activity on Si3N4 surfaces compared with PEEK or titanium. Int. J. Nanomed. 2012, 7, 4829–4840. [Google Scholar]
- Hoffman, L.R.; D’Argenio, D.A.; MacCoss, M.J.; Zhang, Z.Y.; Jones, R.A.; Miller, S.I. Aminoglycoside antibiotics induce bacterial biofilm formation. Nature 2005, 436, 1171–1175. [Google Scholar] [CrossRef]
- Howell, C.; Grinthal, A.; Sunny, S.; Aizenberg, M.; Aizenberg, J. Designing Liquid-Infused Surfaces for Medical Applications: A Review. Adv. Mater. 2018, 30, 1802724. [Google Scholar] [CrossRef] [PubMed]
- Gbejuade, O.H.; Lovering, A.M.; Webb, J.C. The role of microbial biofilms in prosthetic joint infections. Acta Orthop. 2015, 86, 147–158. [Google Scholar] [CrossRef]
- Matar, W.Y.; Jafari, S.M.; Restrepo, C.; Austin, M.; Purtill, J.J.; Parvizi, J. Preventing Infection in Total Joint Arthroplasty. J. Bone Jt. Surg. Am. Vol. 2010, 92a, 36–46. [Google Scholar] [CrossRef]
- Sewick, A.; Makani, A.; Wu, C.; O’Donnell, J.; Baldwin, K.D.; Lee, G.C. Does Dual Antibiotic Prophylaxis Better Prevent Surgical Site Infections in Total Joint Arthroplasty? Clin. Orthop. Relat. Res. 2012, 470, 2702–2707. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, M.; Bentley, K.L.D.; McEntire, B.J.; Bal, B.S.; Schwarz, E.M.; Xie, C. Surface topography of silicon nitride affects antimicrobial and osseointegrative properties of tibial implants in a murine model. J. Biomed. Mater. Res. Part A 2017, 105, 3413–3421. [Google Scholar] [CrossRef] [PubMed]
- Anagnostou, F.; Debet, A.; Pavon-Djavid, G.; Goudaby, Z.; Helary, G.; Migonney, V. Osteoblast functions on functionalized PMMA-based polymers exhibiting Staphylococcus aureus adhesion inhibition. Biomaterials 2006, 27, 3912–3919. [Google Scholar] [CrossRef]
- Kinnari, T.J.; Peltonen, L.I.; Kuusela, T.; Kivilahti, J.; Kononen, M.; Jero, J. Bacterial adherence to titanium surface coated with human serum albumin. Otol. Neurotol. 2005, 26, 380–384. [Google Scholar] [CrossRef]
- Puckett, S.D.; Taylor, E.; Raimondo, T.; Webster, T.J. The relationship between the nanostructure of titanium surfaces and bacterial attachment. Biomaterials 2010, 31, 706–713. [Google Scholar] [CrossRef]
- Gittens, R.A.; Scheideler, L.; Rupp, F.; Hyzy, S.L.; Geis-Gerstorfer, J.; Schwartz, Z.; Boyan, B.D. A review on the wettability of dental implant surfaces II: Biological and clinical aspects. Acta Biomater. 2014, 10, 2907–2918. [Google Scholar] [CrossRef]
- Ribeiro, M.; Monteiro, F.J.; Ferraz, M.P. Infection of orthopedic implants with emphasis on bacterial adhesion process and techniques used in studying bacterial-material interactions. Biomatter 2012, 2, 176–194. [Google Scholar] [CrossRef] [PubMed]
- Bock, R.M.; Jones, E.N.; Ray, D.A.; Bal, B.S.; Pezzotti, G.; McEntire, B.J. Bacteriostatic behavior of surface modulated silicon nitride in comparison to polyetheretherketone and titanium. J. Biomed. Mater. Res. Part A 2017, 105, 1521–1534. [Google Scholar] [CrossRef] [PubMed]
- Kelleher, S.M.; Habimana, O.; Lawler, J.; O’Rilly, B.; Daniels, S.; Casey, E.; Cowley, A. Cicada Wing Surface Topography: An Investigation into the Bactericidal Properties of Nanostructural Features. Acs Appl. Mater. Interfaces 2016, 8, 14966–14974. [Google Scholar] [CrossRef]
- Ivanova, E.P.; Hasan, J.; Webb, H.K.; Truong, V.K.; Watson, G.S.; Watson, J.A.; Baulin, V.A.; Pogodin, S.; Wang, J.Y.; Tobin, M.J.; et al. Natural Bactericidal Surfaces: Mechanical Rupture of Pseudomonas aeruginosa Cells by Cicada Wings. Small 2012, 8, 2489–2494. [Google Scholar] [CrossRef]
- Desrousseaux, C.; Sautou, V.; Descamps, S.; Traore, O. Modification of the surfaces of medical devices to prevent microbial adhesion and biofilm formation. J. Hosp. Infect. 2013, 85, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.L.; Siedlecki, C.A. Submicron-textured biomaterial surface reduces staphylococcal bacterial adhesion and biofilm formation. Acta Biomater. 2012, 8, 72–81. [Google Scholar] [CrossRef]
- Katsikogianni, M.; Missirlis, Y.F. Concise review of mechanisms of bacterial adhesion to biomaterials and of techniques used in estimating bacteria-material interactions. Eur. Cell Mater. 2004, 8, 37–57. [Google Scholar] [CrossRef]
- Gallo, J.; Holinka, M.; Moucha, C.S. Antibacterial Surface Treatment for Orthopaedic Implants. Int. J. Mol. Sci. 2014, 15, 13849–13880. [Google Scholar] [CrossRef]
- Pezzotti, G.; Bock, R.M.; McEntire, B.J.; Jones, E.; Boffelli, M.; Zhu, W.L.; Baggio, G.; Boschetto, F.; Puppulin, L.; Adachi, T.; et al. Silicon Nitride Bioceramics Induce Chemically Driven Lysis in Porphyromonas gingivalis. Langmuir 2016, 32, 3024–3035. [Google Scholar] [CrossRef]
- Stimmelmayr, M.; Edelhoff, D.; Guth, J.F.; Erdelt, K.; Happe, A.; Beuer, F. Wear at the titanium-titanium and the titanium-zirconia implant-abutment interface: A comparative in vitro study. Dent. Mater. 2012, 28, 1215–1220. [Google Scholar] [CrossRef]
- Klotz, W.M.; Taylor, T.D.; Goldberg, A.J. Wear at the Titanium-Zirconia Implant-Abutment Interface: A Pilot Study. Int. J. Oral Maxillofac. Implant. 2011, 26, 970–975. [Google Scholar]
- Olofsson, J.; Grehk, T.M.; Berlind, T.; Persson, C.; Jacobson, S.; Engqvist, H. Evaluation of silicon nitride as a wear resistant and resorbable alternative for total hip joint replacement. Biomatter 2012, 2, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Pezzotti, G. Silicon Nitride: A Bioceramic with a Gift. Acs Appl. Mater. Interfaces 2019, 11, 26619–26636. [Google Scholar] [CrossRef] [PubMed]
- Le, T.V.; Baaj, A.A.; Dakwar, E.; Burkett, C.J.; Murray, G.; Smith, D.A.; Uribe, J.S. Subsidence of Polyetheretherketone Intervertebral Cages in Minimally Invasive Lateral Retroperitoneal Transpsoas Lumbar Interbody Fusion. Spine 2012, 37, 1268–1273. [Google Scholar] [CrossRef]
- Arts, P.M.; Wolfs, J.F.C.; Corbin, T.P. The CASCADE trial: Effectiveness of ceramic versus PEEK cages for anterior cervical discectomy with interbody fusion; protocol of a blinded randomized controlled trial. BMC Musculoskelet. Disord. 2013, 14, 244. [Google Scholar] [CrossRef]
- Mobbs, R.J.; Rao, P.J.; Phan, K.; Hardcastle, P.; Choy, W.J.; McCartney, E.R.; Druitt, R.K.; Mouatt, C.A.L.; Sorrell, C.C. Anterior Lumbar Interbody Fusion Using Reaction Bonded Silicon Nitride Implants: Long-Term Case Series of the First Synthetic Anterior Lumbar Interbody Fusion Spacer Implanted in Humans. World Neurosurg. 2018, 120, 256–264. [Google Scholar] [CrossRef]
- Arts, P.M.; Wolfs, J.F.C.; Corbin, T.P. Porous silicon nitride spacers versus PEEK cages for anterior cervical discectomy and fusion: Clinical and radiological results of a single-blinded randomized controlled trial. Eur. Spine J. 2017, 26, 2372–2379. [Google Scholar] [CrossRef]
- Kersten, R.F.M.R.; van Gaalen, S.M.; Arts, M.P.; Roes, K.C.B.; de Gast, A.; Corbin, T.P.; Oner, F.C. The SNAP trial: A double blind multi-center randomized controlled trial of a silicon nitride versus a PEEK cage in transforaminal lumbar interbody fusion in patients with symptomatic degenerative lumbar disc disorders: Study protocol. Bmc Musculoskelet. Disord. 2014, 15, 57. [Google Scholar] [CrossRef]
- Jim, Y.A.; Sue, L.; Myhre; Bal, B.S. Radiographic Follow-up of Transforaminal Lumbar Fusion with Silicon Nitride Spacers A case Report of Two Patients. J. Musculoskelet. Disord. Treat. 2016, 2, 8. [Google Scholar]
- Aoki, Y.; Yamagata, M.; Nakajima, F.; Ikeda, Y.; Takahashi, K. Posterior Migration of Fusion Cages in Degenerative Lumbar Disease Treated with Transforaminal Lumbar Interbody Fusion A Report of Three Patients. Spine 2009, 34, E54–E58. [Google Scholar] [CrossRef]
- Nguyen, H.V.; Akbarnia, B.A.; van Dam, B.E.; Raiszadeh, K.; Bagheri, R.; Canale, S.; Sylvain, G.M.; Barone, R.; Bench, G. Anterior exposure of the spine for removal of lumbar interbody devices and implants. Spine 2006, 31, 2449–2453. [Google Scholar] [CrossRef] [PubMed]
- Sonntag, R.; Reinders, J.; Kretzer, J.P. What’s next? Alternative materials for articulation in total joint replacement. Acta Biomater. 2012, 8, 2434–2441. [Google Scholar] [CrossRef]
- Sugita, T.; Ueda, K.; Kanemura, Y. Material Removal Mechanism of Silicon-Nitride during Rubbing in Water. Wear 1984, 97, 1–8. [Google Scholar] [CrossRef]
- Tomizawa, H.; Fischer, T.E. Friction and Wear of Silicon-Nitride at 150-Degrees-C to 800-Degrees-C. Asle Trans. 1986, 29, 481–488. [Google Scholar] [CrossRef]
- Tomizawa, H.; Fischer, T.E. Friction and Wear of Silicon-Nitride and Silicon-Carbide in Water—Hydrodynamic Lubrication at Low Sliding Speed Obtained by Tribochemical Wear. Asle Trans. 1987, 30, 41–46. [Google Scholar] [CrossRef]
- Pezzotti, G. Bioceramics for Hip Joints: The Physical Chemistry Viewpoint. Materials 2014, 7, 4367–4410. [Google Scholar] [CrossRef]
- Learmonth, D.I.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Bayliss, L.E.; Culliford, D.; Monk, A.P.; Glyn-Jones, S.; Prieto-Alhambra, D.; Judge, A.; Cooper, C.; Carr, A.J.; Arden, N.K.; Beard, D.J.; et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: A population-based cohort study. Lancet 2017, 389, 1424–1430. [Google Scholar] [CrossRef]
- Evans, J.T.; Walker, R.W.; Evans, J.P.; Blom, A.W.; Sayers, A.; Whitehouse, M.R. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019, 393, 876. [Google Scholar] [CrossRef]
- Rondinella, A.; Marin, E.; Zanocco, M.; Boschetto, F.; Pezzotti, G. Surface pre-oxidation improves the wear performance of Si3N4 against UHMWPE. Appl. Surf. Sci. 2019, 463, 1037–1045. [Google Scholar] [CrossRef]
- Back, D.L.; Dalziel, R.; Young, D.; Shimmin, A. Early results of primary Birmingham hip resurfacings—An independent prospective study of the first 230 hips. J. Bone Jt. Surg. Br. Vol. 2005, 87b, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Titze, M.; Cappi, B.; Wirtz, D.C.; Telle, R.; Fischer, H. Improved mechanical long-term reliability of hip resurfacing prostheses by using silicon nitride. J. Mater. Sci. Mater. Med. 2010, 21, 3049–3057. [Google Scholar] [CrossRef] [PubMed]
- Jahanmir, S.; Ozmen, Y.; Ives, L.K. Water lubrication of silicon nitride in sliding. Tribol. Lett. 2004, 17, 409–417. [Google Scholar] [CrossRef]
- Fillion, M.; Aubazac, D.; Bessadet, M.; Allegre, M.; Nicolas, E. The impact of implant treatment on oral health related quality of life in a private dental practice: A prospective cohort study. Health Qual. Life Outcomes 2013, 11, 197. [Google Scholar] [CrossRef] [PubMed]
- Wasanapiarnpong, T.; Cherdtham, N.; Padipatvuthikul, P.; Mongkolkachit, C.; Wananuruksawong, R.; Jinawath, S. Fabrication of Dental Ceramics from Silicon Nitride Core with Borosilicate Glass Veneer. Biomater. Appl. 2012, 506, 493. [Google Scholar] [CrossRef]




| Author | Materials Used | Type of Implants | Animal Model | Control Group | Results | Ref. |
|---|---|---|---|---|---|---|
| Guedes e Silva et al. | Si3N4 | / | Rabbits’ tibias | / | Bone growth occurred mainly in the cortical areas, and the bone bridge can be formed when the implants are installed into distal regions. | [68] |
| Kersten et al. | Si3N4 | Lumbar interbody fusion implant | Caprine model | PEEK | Bone formation: the Si3N4 group (52.6%) was greater than PEEK (27.9%). BIC ratios and biodynamic stability: comparable. | [73] |
| Howlett et al. | Si3N4 | / | Femoral marrow cavities in rabbit | / | In vivo test results showed that Si3N4 implants were permeated by new mature bone after being inserted into femoral massow cavities for three months. | [69] |
| Neumann et al. | Si3N4 | / | lateral condyli of the femurs of New Zealand male rabbits | Aluminum oxide | Si3N4 shows good biocompatibility and presumably better osseointegration than Al2O3. | [71] |
| Neumann et al. | Si3N4 | Miniplates and screws | Frontal bone defects in minipigs | / | These osteofixation system showed satisfactory results in terms of the aspects of biocompatibility and mechanical stability. | [72] |
| Anderson et al. | Cancellous-structured Si3N4 | / | Femoral condyle of sheep | / | The results showed that in some implants, the depth of newly formed bone was greater than 3 mm after 3 months in situ, which meant that a porous structure is beneficial for achieving skeletal attachment. | [74] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Du, X.; Lee, S.S.; Blugan, G.; Ferguson, S.J. Silicon Nitride as a Biomedical Material: An Overview. Int. J. Mol. Sci. 2022, 23, 6551. https://doi.org/10.3390/ijms23126551
Du X, Lee SS, Blugan G, Ferguson SJ. Silicon Nitride as a Biomedical Material: An Overview. International Journal of Molecular Sciences. 2022; 23(12):6551. https://doi.org/10.3390/ijms23126551
Chicago/Turabian StyleDu, Xiaoyu, Seunghun S. Lee, Gurdial Blugan, and Stephen J. Ferguson. 2022. "Silicon Nitride as a Biomedical Material: An Overview" International Journal of Molecular Sciences 23, no. 12: 6551. https://doi.org/10.3390/ijms23126551
APA StyleDu, X., Lee, S. S., Blugan, G., & Ferguson, S. J. (2022). Silicon Nitride as a Biomedical Material: An Overview. International Journal of Molecular Sciences, 23(12), 6551. https://doi.org/10.3390/ijms23126551







