Intrinsically Conductive Polymers for Striated Cardiac Muscle Repair
Abstract
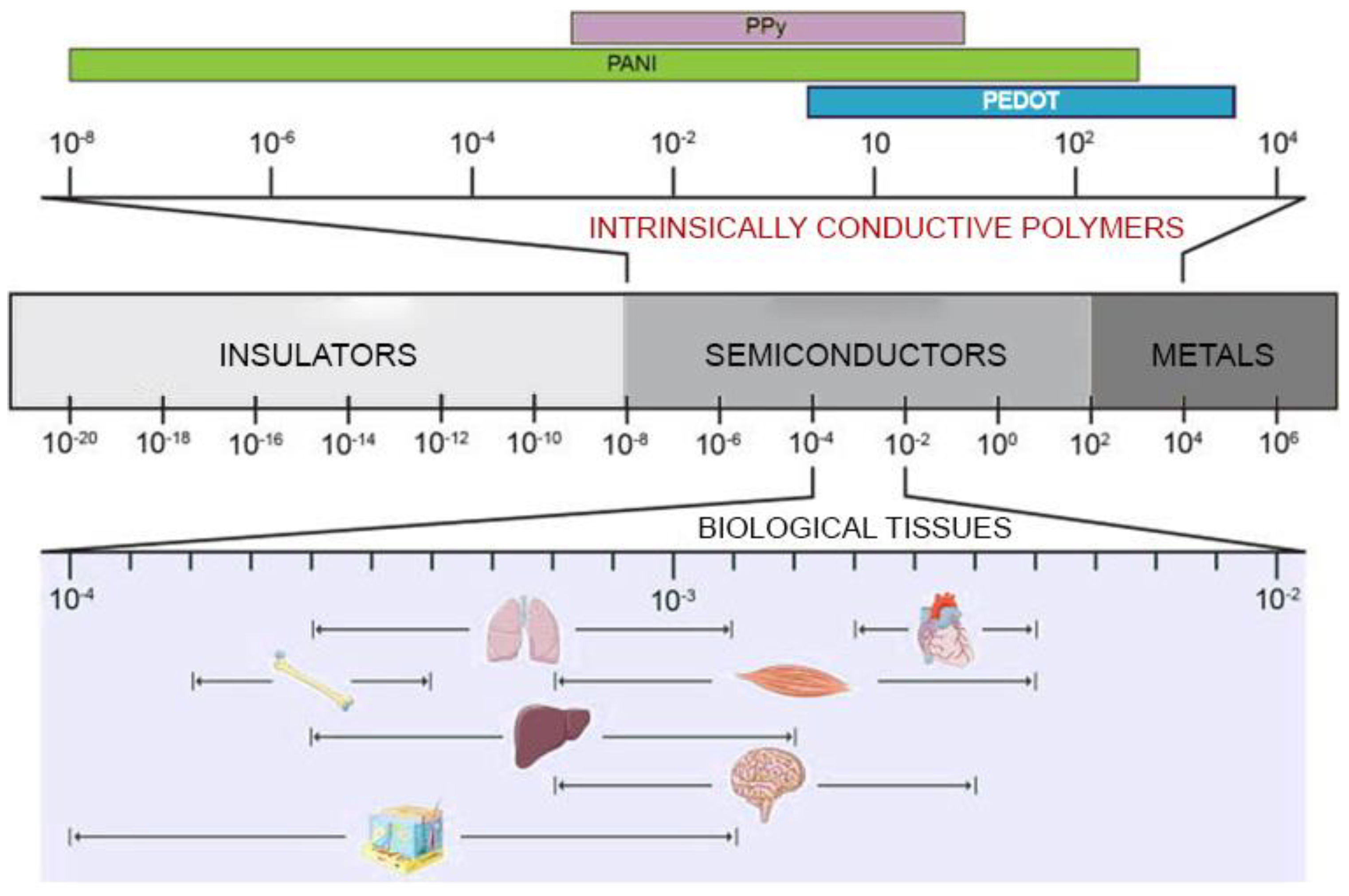
:1. Introduction
2. Conductive Polymer-Based Scaffolds in Cardiac Tissue Engineering
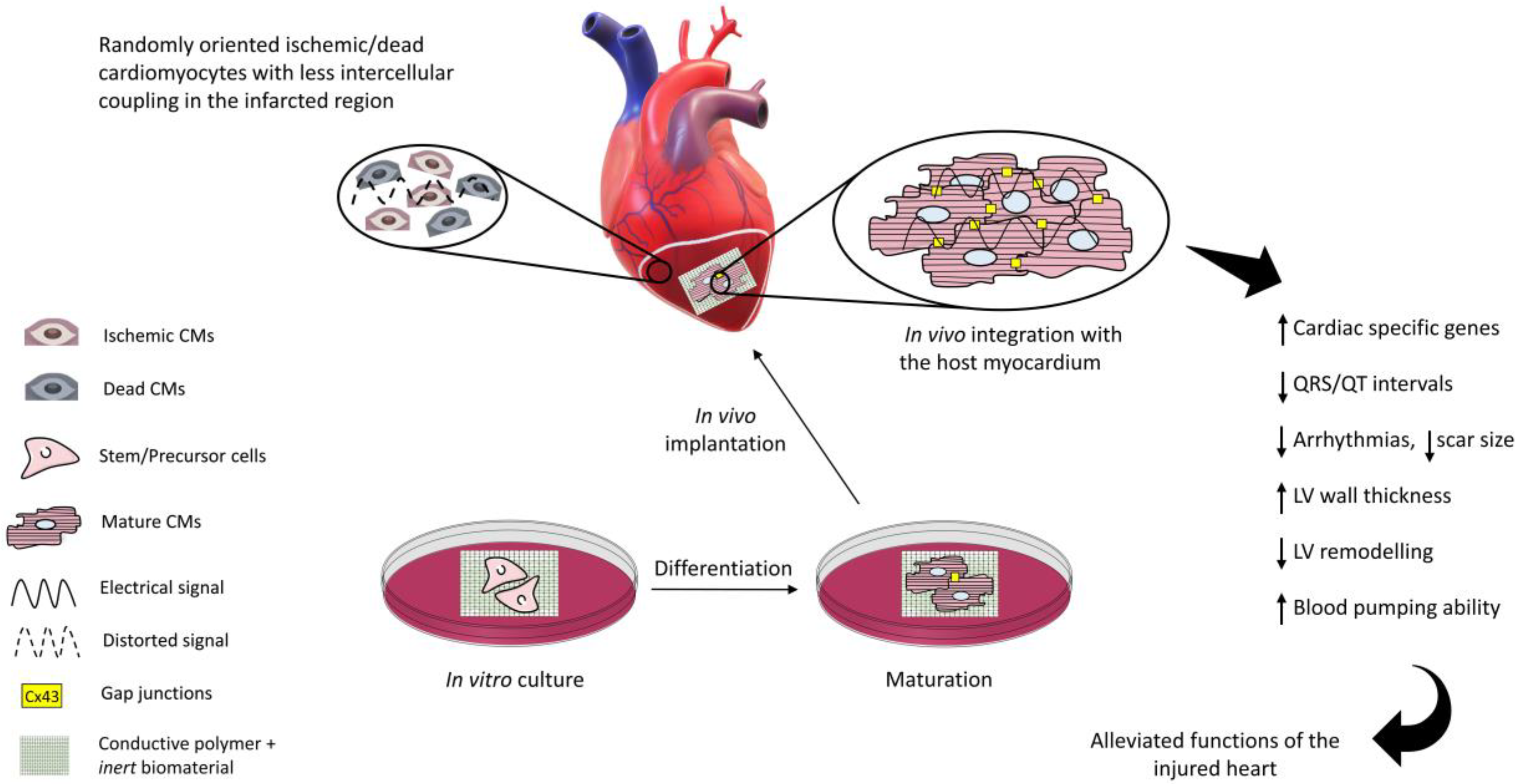
2.1. Polyaniline
2.2. Polypyrrole
2.3. Poly(3,4-Ethylenedioxythiophene)/PEDOT
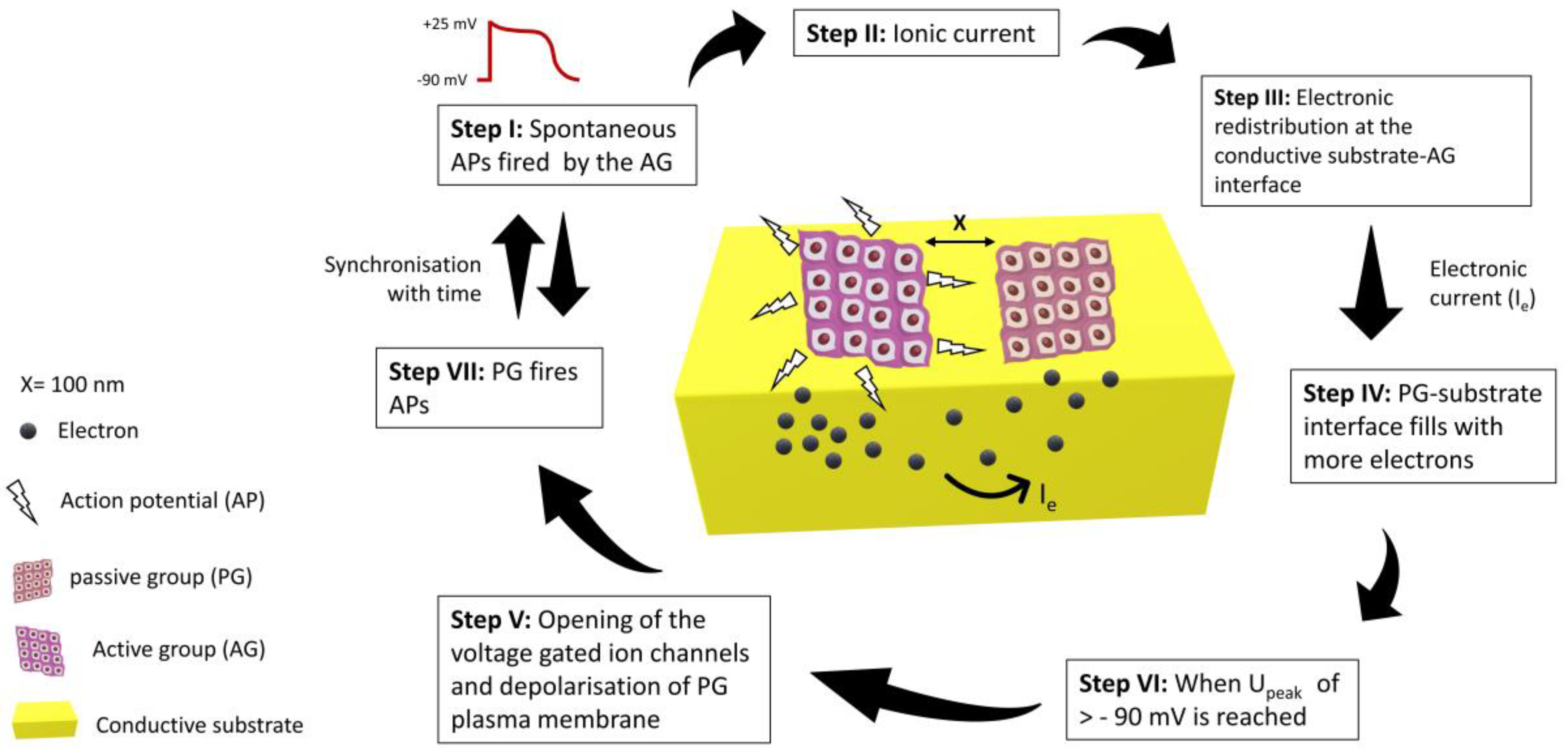
3. The Underlying Mechanisms of the Positive Role of Conductive Substrates in Cardiac Tissue Engineering
4. Conductive Substrates for In Vivo Cardiac Repair
5. Concluding Remarks
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Timmis, A.; Group, W.; Townsend, N.; Gale, C.P.; Torbica, A.; Lettino, M.; Petersen, S.E.; Mossialos, E.A.; Maggioni, A.P.; Kazakiewicz, D.; et al. European Society of Cardiology: Cardiovascular Disease Statistics 2019. Eur. Heart J. 2020, 44, 12–85. [Google Scholar] [CrossRef]
- Laslett, L.J.; Alagona, P.; Clark, B.A.; Drozda, J.P.; Saldivar, F.; Wilson, S.R.; Poe, C.; Hart, M. The worldwide environment of cardiovascular disease: Prevalence, diagnosis, therapy, and policy issues: A report from the american college of cardiology. J. Am. Coll. Cardiol. 2012, 60, S1–S49. [Google Scholar] [CrossRef] [Green Version]
- Rokicki, T.; Perkowska, A.; Ratajczak, M. Differentiation in healthcare financing in eu countries. Sustainability 2021, 13, 251. [Google Scholar] [CrossRef]
- Nabel, E.G.; Braunwald, E. A Tale of Coronary Artery Disease and Myocardial Infarction. N. Engl. J. Med. 2012, 366, 54–63. [Google Scholar] [CrossRef] [Green Version]
- Frangogiannis, N.G. Pathophysiology of myocardial infarction. Compr. Physiol. 2015, 5, 1841–1875. [Google Scholar] [PubMed]
- Bergmann, O.; Zdunek, S.; Felker, A.; Salehpour, M.; Alkass, K.; Bernard, S.; Sjostrom, S.L.; Szewczykowska, M.; Jackowska, T.; Dos Remedios, C.; et al. Dynamics of Cell Generation and Turnover in the Human Heart. Cell 2015, 161, 1566–1575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sadahiro, T. Cardiac regeneration with pluripotent stem cell-derived cardiomyocytes and direct cardiac reprogramming. Regen. Ther. 2019, 11, 95–100. [Google Scholar] [CrossRef]
- Zammaretti, P.; Jaconi, M. Cardiac tissue engineering: Regeneration of the wounded heart. Curr. Opin. Biotechnol. 2004, 15, 430–434. [Google Scholar] [CrossRef]
- Zhang, D.; Shadrin, I.Y.; Lam, J.; Xian, H.Q.; Snodgrass, H.R.; Bursac, N. Tissue-engineered cardiac patch for advanced functional maturation of human ESC-derived cardiomyocytes. Biomaterials 2013, 34, 5813–5820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hasan, A.; Khattab, A.; Islam, M.A.; Hweij, K.A.; Zeitouny, J.; Waters, R.; Sayegh, M.; Hossain, M.M.; Paul, A. Injectable Hydrogels for Cardiac Tissue Repair after Myocardial Infarction. Adv. Sci. 2015, 2, 1500122. [Google Scholar] [CrossRef] [PubMed]
- Kim, P.H.; Cho, J.Y. Myocardial tissue engineering using electrospun nanofiber composites. BMB Rep. 2016, 49, 26–36. [Google Scholar] [CrossRef] [Green Version]
- Hasan, A.; Morshed, M.; Memic, A.; Hassan, S.; Webster, T.J.; Marei, H.E.S. Nanoparticles in tissue engineering: Applications, challenges and prospects. Int. J. Nanomed. 2018, 13, 5637–5655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ciocci, M.; Mochi, F.; Carotenuto, F.; Di Giovanni, E.; Prosposito, P.; Francini, R.; De Matteis, F.; Reshetov, I.; Casalboni, M.; Melino, S.; et al. Scaffold-in-scaffold potential to induce growth and differentiation of cardiac progenitor cells. Stem Cells Dev. 2017, 26, 1438–1447. [Google Scholar] [CrossRef] [Green Version]
- Carotenuto, F.; Teodori, L.; Maccari, A.M.; Delbono, L.; Orlando, G.; Di Nardo, P. Turning regenerative technologies into treatment to repair myocardial injuries. J. Cell. Mol. Med. 2020, 24, 2704–2716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carotenuto, F.; Manzari, V.; Di Nardo, P. Cardiac Regeneration: The Heart of the Issue. Curr. Transpl. Rep. 2021, 8, 67–75. [Google Scholar] [CrossRef]
- Solazzo, M.; O’Brien, F.J.; Nicolosi, V.; Monaghan, M.G. The rationale and emergence of electroconductive biomaterial scaffolds in cardiac tissue engineering. APL Bioeng. 2019, 3, 041501. [Google Scholar] [CrossRef] [PubMed]
- Quijada, C. Special issue: Conductive polymers: Materials and applications. Materials 2020, 13, 2344. [Google Scholar] [CrossRef]
- Gelmi, A.; Cieslar-Pobuda, A.; de Muinck, E.; Los, M.; Rafat, M.; Jager, E.W.H. Direct Mechanical Stimulation of Stem Cells: A Beating Electromechanically Active Scaffold for Cardiac Tissue Engineering. Adv. Healthc. Mater. 2016, 5, 1471–1480. [Google Scholar] [CrossRef] [Green Version]
- Ahadian, S.; Yamada, S.; Estili, M.; Liang, X.; Banan Sadeghian, R.; Nakajima, K.; Shiku, H.; Matsue, T.; Khademhosseini, A. Carbon nanotubes embedded in embryoid bodies direct cardiac differentiation. Biomed. Microdevices 2017, 19, 57. [Google Scholar] [CrossRef]
- You, J.O.; Rafat, M.; Ye, G.J.C.; Auguste, D.T. Nanoengineering the heart: Conductive scaffolds enhance connexin 43 expression. Nano Lett. 2011, 11, 3643–3648. [Google Scholar] [CrossRef]
- Wei, B.; Jin, J.P. TNNT1, TNNT2, and TNNT3: Isoform genes, regulation, and structure-function relationships. Gene 2016, 582, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Watt, A.J.; Battle, M.A.; Li, J.; Duncan, S.A. GATA4 is essential for formation of the proepicardium and regulates cardiogenesis. Proc. Natl. Acad. Sci. USA 2004, 101, 12573–12578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saadane, N.; Alpert, L.; Chalifour, L.E. Expression of immediate early genes, GATA-4, and Nkx-2.5 in adrenergic-induced cardiac hypertrophy and during regression in adult mice. Br. J. Pharmacol. 1999, 127, 1165–1176. [Google Scholar] [CrossRef] [Green Version]
- Kotini, M.; Barriga, E.H.; Leslie, J.; Gentzel, M.; Rauschenberger, V.; Schambon, A.; Mayor, R. Gap junction protein Connexin-43 is a direct transcriptional regulator of N-cadherin in vivo. Nat. Commun. 2018, 9, 3846. [Google Scholar] [CrossRef]
- He, S.; Wu, J.; Li, S.-H.; Wang, L.; Sun, Y.; Xie, J.; Ramnath, D.; Weisel, R.D.; Yau, T.M.; Sung, H.-W.; et al. The conductive function of biopolymer corrects myocardial scar conduction blockage and resynchronizes contraction to prevent heart failure. Biomaterials 2020, 258, 120285. [Google Scholar] [CrossRef] [PubMed]
- Lalegül-ülker, Ö.; Murat, Y. Magnetic and electrically conductive silica-coated iron oxide/polyaniline nanocomposites for biomedical applications. Mater. Sci. Eng. C 2021, 119, 111600. [Google Scholar] [CrossRef]
- Wibowo, A.; Vyas, C.; Cooper, G.; Qulub, F.; Suratman, R. 3D Printing of Polycaprolactone–Polyaniline Electroactive Sca ff olds for Bone Tissue Engineering. Materials 2020, 13, 512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, M.; Guo, B. Electroactive 3D Scaffolds Based on Silk Fibroin and Water-Borne Polyaniline for Skeletal Muscle Tissue Engineering. Macromol. Biosci. 2017, 17, 1–10. [Google Scholar] [CrossRef]
- Karimi-soflou, R.; Nejati, S.; Karkhaneh, A. Electroactive and antioxidant injectable in-situ forming hydrogels with tunable properties by polyethylenimine and polyaniline for nerve tissue engineering. Colloids Surf. B Biointerfaces 2021, 199, 111565. [Google Scholar] [CrossRef] [PubMed]
- Choi, C.H.; Park, S.H.; Woo, S.I. Binary and ternary doping of nitrogen, boron, and phosphorus into carbon for enhancing electrochemical oxygen reduction activity. ACS Nano 2012, 6, 7084–7091. [Google Scholar] [CrossRef]
- Bhadra, J.; Alkareem, A.; Al-Thani, N. A review of advances in the preparation and application of polyaniline based thermoset blends and composites. J. Polym. Res. 2020, 27, 122. [Google Scholar] [CrossRef] [Green Version]
- Fernandes, E.G.R.; Zucolotto, V.; De Queiroz, A.A.A. Electrospinning of hyperbranched poly-L-lysine/polyaniline nanofibers for application in cardiac tissue engineering. J. Macromol. Sci. Part A Pure Appl. Chem. 2010, 47, 1203–1207. [Google Scholar] [CrossRef]
- Jeong, S.I.; Jun, I.D.; Choi, M.J.; Nho, Y.C.; Lee, Y.M.; Shin, H. Development of electroactive and elastic nanofibers that contain polyaniline and poly(L-lactide-co-ε-caprolactone) for the control of cell adhesion. Macromol. Biosci. 2008, 8, 627–637. [Google Scholar] [CrossRef]
- Moura, R.M.; de Queiroz, A.A.A. Dendronized polyaniline nanotubes for cardiac tissue engineering. Artif. Organs 2011, 35, 471–477. [Google Scholar] [CrossRef]
- Baheiraei, N.; Yeganeh, H.; Ai, J.; Gharibi, R.; Ebrahimi-Barough, S.; Azami, M.; Vahdat, S.; Baharvand, H. Preparation of a porous conductive scaffold from aniline pentamer-modified polyurethane/PCL blend for cardiac tissue engineering. J. Biomed. Mater. Res. Part A 2015, 103, 3179–3187. [Google Scholar] [CrossRef]
- Borriello, A.; Guarino, V.; Schiavo, L.; Alvarez-Perez, M.A.; Ambrosio, L. Optimizing PANi doped electroactive substrates as patches for the regeneration of cardiac muscle. J. Mater. Sci. Mater. Med. 2011, 22, 1053–1062. [Google Scholar] [CrossRef] [PubMed]
- McKeon, K.D.; Lewis, A.; Freeman, J.W. Electrospun poly(D,L-lactide) and polyaniline scaffold characterization. J. Appl. Polym. Sci. 2010, 115, 1566–1572. [Google Scholar] [CrossRef]
- Li, M.; Guo, Y.; Wei, Y.; MacDiarmid, A.G.; Lelkes, P.I. Electrospinning polyaniline-contained gelatin nanofibers for tissue engineering applications. Biomaterials 2006, 27, 2705–2715. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Ge, J.; Guo, B.; Ma, P.X. In situ forming biodegradable electroactive hydrogels. Polym. Chem. 2014, 5, 2880–2890. [Google Scholar] [CrossRef]
- Baheiraei, N.; Yeganeh, H.; Ai, J.; Gharibi, R.; Azami, M.; Faghihi, F. Synthesis, characterization and antioxidant activity of a novel electroactive and biodegradable polyurethane for cardiac tissue engineering application. Mater. Sci. Eng. C 2014, 44, 24–37. [Google Scholar] [CrossRef]
- Hsiao, C.W.; Bai, M.Y.; Chang, Y.; Chung, M.F.; Lee, T.Y.; Wu, C.T.; Maiti, B.; Liao, Z.X.; Li, R.K.; Sung, H.W. Electrical coupling of isolated cardiomyocyte clusters grown on aligned conductive nanofibrous meshes for their synchronized beating. Biomaterials 2013, 34, 1063–1072. [Google Scholar] [CrossRef] [Green Version]
- Qazi, T.H.; Rai, R.; Dippold, D.; Roether, J.E.; Schubert, D.W.; Rosellini, E.; Barbani, N.; Boccaccini, A.R. Development and characterization of novel electrically conductive PANI-PGS composites for cardiac tissue engineering applications. Acta Biomater. 2014, 10, 2434–2445. [Google Scholar] [CrossRef] [PubMed]
- Deng, Z.; Guo, Y.; Zhao, X.; Li, L.; Dong, R.; Guo, B.; Ma, P.X. Stretchable degradable and electroactive shape memory copolymers with tunable recovery temperature enhance myogenic differentiation. Acta Biomater. 2016, 46, 234–244. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.C.; Sun, Y.C.; Chen, Y.H. Electrically conductive nanofibers with highly oriented structures and their potential application in skeletal muscle tissue engineering. Acta Biomater. 2013, 9, 5562–5572. [Google Scholar] [CrossRef] [PubMed]
- Bidez, P.R.; Li, S.; Macdiarmid, A.G.; Venancio, E.C.; Wei, Y.; Lelkes, P.I. Polyaniline, an electroactive polymer, supports adhesion and proliferation of cardiac myoblasts. J. Biomater. Sci. Polym. Ed. 2006, 17, 199–212. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Wu, Y.; Hu, T.; Guo, B.; Ma, P.X. Electrospun conductive nanofibrous scaffolds for engineering cardiac tissue and 3D bioactuators. Acta Biomater. 2017, 59, 68–81. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wu, Y.; Guo, B.; Ma, P.X. Nanofiber Yarn/Hydrogel Core-Shell Scaffolds Mimicking Native Skeletal Muscle Tissue for Guiding 3D Myoblast Alignment, Elongation, and Differentiation. ACS Nano 2015, 9, 9167–9179. [Google Scholar] [CrossRef]
- Dong, R.; Zhao, X.; Guo, B.; Ma, P.X. Self-Healing Conductive Injectable Hydrogels with Antibacterial Activity as Cell Delivery Carrier for Cardiac Cell Therapy. ACS Appl. Mater. Interfaces 2016, 8, 17138–17150. [Google Scholar] [CrossRef]
- Hu, T.; Wu, Y.; Zhao, X.; Wang, L.; Bi, L.; Ma, P.X.; Guo, B. Micropatterned, electroactive, and biodegradable poly(glycerol sebacate)-aniline trimer elastomer for cardiac tissue engineering. Chem. Eng. J. 2019, 366, 208–222. [Google Scholar] [CrossRef]
- Roshanbinfar, K.; Vogt, L.; Ruther, F.; Roether, J.A.; Boccaccini, A.R.; Engel, F.B. Nanofibrous Composite with Tailorable Electrical and Mechanical Properties for Cardiac Tissue Engineering. Adv. Funct. Mater. 2020, 30, 8612. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Zhang, W.; Huang, L.; Ito, Y.; Wang, Z.; Shi, X.; Wei, Y.; Jing, X.; Zhang, P. Intracellular calcium ions and morphological changes of cardiac myoblasts response to an intelligent biodegradable conducting copolymer. Mater. Sci. Eng. C 2018, 90, 168–179. [Google Scholar] [CrossRef]
- Mawad, D.; Mansfield, C.; Lauto, A.; Perbellini, F.; Nelson, G.W.; Tonkin, J.; Bello, S.O.; Carrad, D.J.; Micolich, A.P.; Mahat, M.M.; et al. A Conducting polymer with enhanced electronic stability applied in cardiac models. Sci. Adv. 2016, 2, e1601007. [Google Scholar] [CrossRef] [Green Version]
- Yin, Y.; Mo, J.; Feng, J. Conductive fabric patch with controllable porous structure and elastic properties for tissue engineering applications. J. Mater. Sci. 2020, 55, 17120–17133. [Google Scholar] [CrossRef]
- Xie, M.; Wang, L.; Guo, B.; Wang, Z.; Chen, Y.E.; Ma, P.X. Ductile electroactive biodegradable hyperbranched polylactide copolymers enhancing myoblast differentiation. Biomaterials 2015, 71, 158–167. [Google Scholar] [CrossRef] [Green Version]
- Guo, B.; Qu, J.; Zhao, X.; Zhang, M. Degradable conductive self-healing hydrogels based on dextran-graft-tetraaniline and N-carboxyethyl chitosan as injectable carriers for myoblast cell therapy and muscle regeneration. Acta Biomater. 2019, 84, 180–193. [Google Scholar] [CrossRef]
- Hoang, A.P.; Ruprai, H.; Fidanovski, K.; Eslami, M.; Lauto, A.; Daniels, J.; Mawad, D. Porous and sutureless bioelectronic patch with retained electronic properties under cyclic stretching. Appl. Mater. Today 2019, 15, 315–322. [Google Scholar] [CrossRef]
- Humpolíček, P.; Radaszkiewicz, K.A.; Kašpárková, V.; Stejskal, J.; Trchová, M.; Kuceková, Z.; Vičarová, H.; Pacherník, J.; Lehocký, M.; Minařík, A. Stem cell differentiation on conducting polyaniline. RSC Adv. 2015, 5, 68796–68805. [Google Scholar] [CrossRef] [Green Version]
- Ku, S.H.; Lee, S.H.; Park, C.B. Synergic effects of nanofiber alignment and electroactivity on myoblast differentiation. Biomaterials 2012, 33, 6098–6104. [Google Scholar] [CrossRef] [PubMed]
- Jun, I.; Jeong, S.; Shin, H. The stimulation of myoblast differentiation by electrically conductive sub-micron fibers. Biomaterials 2009, 30, 2038–2047. [Google Scholar] [CrossRef]
- Aznar-Cervantes, S.; Roca, M.I.; Martinez, J.G.; Meseguer-Olmo, L.; Cenis, J.L.; Moraleda, J.M.; Otero, T.F. Fabrication of conductive electrospun silk fibroin scaffolds by coating with polypyrrole for biomedical applications. Bioelectrochemistry 2012, 85, 36–43. [Google Scholar] [CrossRef]
- Zanjanizadeh Ezazi, N.; Shahbazi, M.A.; Shatalin, Y.V.; Nadal, E.; Mäkilä, E.; Salonen, J.; Kemell, M.; Correia, A.; Hirvonen, J.; Santos, H.A. Conductive vancomycin-loaded mesoporous silica polypyrrole-based scaffolds for bone regeneration. Int. J. Pharm. 2018, 536, 241–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Broda, C.R.; Lee, J.Y.; Sirivisoot, S.; Schmidt, C.E.; Harrison, B.S. A chemically polymerized electrically conducting composite of polypyrrole nanoparticles and polyurethane for tissue engineering. J. Biomed. Mater. Res. Part A 2011, 98, 509–516. [Google Scholar] [CrossRef]
- Pan, X.; Sun, B.; Mo, X. Electrospun polypyrrole-coated polycaprolactone nanoyarn nerve guidance conduits for nerve tissue engineering. Front. Mater. Sci. 2018, 12, 438–446. [Google Scholar] [CrossRef]
- Zhou, J.F.; Wang, Y.G.; Cheng, L.; Wu, Z.; Sun, X.D.; Peng, J. Preparation of polypyrrole-embedded electrospun poly(lactic acid) nanofibrous scaffolds for nerve tissue engineering. Neural Regen. Res. 2016, 11, 1644–1652. [Google Scholar] [PubMed]
- Björninen, M.; Gilmore, K.; Pelto, J.; Seppänen-Kaijansinkko, R.; Kellomäki, M.; Miettinen, S.; Wallace, G.; Grijpma, D.; Haimi, S. Electrically Stimulated Adipose Stem Cells on Polypyrrole-Coated Scaffolds for Smooth Muscle Tissue Engineering. Ann. Biomed. Eng. 2017, 45, 1015–1026. [Google Scholar] [CrossRef]
- Humpolíček, P.; Kašpárková, V.; Pacherník, J.; Stejskal, J.; Bober, P.; Capáková, Z.; Radaszkiewicz, K.A.; Junkar, I.; Lehocký, M. The biocompatibility of polyaniline and polypyrrole: A comparative study of their cytotoxicity, embryotoxicity and impurity profile. Mater. Sci. Eng. C 2018, 91, 303–310. [Google Scholar] [CrossRef]
- Gelmi, A.; Zhang, J.; Cieslar-Pobuda, A.; Ljunngren, M.K.; Los, M.J.; Rafat, M.; Jager, E.W.H. Electroactive 3D materials for cardiac tissue engineering. In Electroactive Polymer Actuators and Devices (EAPAD) 2015; SPIE-International Society for Optics and Photonics: Bellingham, WA, USA, 2015; Volume 9430. [Google Scholar]
- Mihic, A.; Cui, Z.; Wu, J.; Vlacic, G.; Miyagi, Y.; Li, S.H.; Lu, S.; Sung, H.W.; Weisel, R.D.; Li, R.K. A conductive polymer hydrogel supports cell electrical signaling and improves cardiac function after implantation into myocardial infarct. Circulation 2015, 132, 772–784. [Google Scholar] [CrossRef] [Green Version]
- Tsui, J.H.; Ostrovsky-Snider, N.A.; Yama, D.M.P.; Donohue, J.D.; Choi, J.S.; Chavanachat, R.; Larson, J.D.; Murphy, A.R.; Kim, D.H. Conductive silk-polypyrrole composite scaffolds with bioinspired nanotopographic cues for cardiac tissue engineering. J. Mater. Chem. B 2018, 6, 7185–7196. [Google Scholar] [CrossRef] [PubMed]
- Bird, S.D.; Doevendans, P.A.; Van Rooijen, M.A.; Brutel De La Riviere, A.; Hassink, R.J.; Passier, R.; Mummery, C.L. The human adult cardiomyocyte phenotype. Cardiovasc. Res. 2003, 58, 423–434. [Google Scholar] [CrossRef]
- Spearman, B.S.; Hodge, A.J.; Porter, J.L.; Hardy, J.G.; Davis, Z.D.; Xu, T.; Zhang, X.; Schmidt, C.E.; Hamilton, M.C.; Lipke, E.A. Conductive interpenetrating networks of polypyrrole and polycaprolactone encourage electrophysiological development of cardiac cells. Acta Biomater. 2015, 28, 109–120. [Google Scholar] [CrossRef] [Green Version]
- Song, X.; Mei, J.; Ye, G.; Wang, L.; Ananth, A.; Yu, L.; Qiu, X. In situ pPy-modification of chitosan porous membrane from mussel shell as a cardiac patch to repair myocardial infarction. Appl. Mater. Today 2019, 15, 87–99. [Google Scholar] [CrossRef]
- Kai, D.; Prabhakaran, M.P.; Jin, G.; Ramakrishna, S. Polypyrrole-contained electrospun conductive nanofibrous membranes for cardiac tissue engineering. J. Biomed. Mater. Res. Part A 2011, 99, 376–385. [Google Scholar] [CrossRef]
- Liang, S.; Zhang, Y.; Wang, H.; Xu, Z.; Chen, J.; Bao, R.; Tan, B.; Cui, Y.; Fan, G.; Wang, W.; et al. Paintable and Rapidly Bondable Conductive Hydrogels as Therapeutic Cardiac Patches. Adv. Mater. 2018, 30, e1704235. [Google Scholar] [CrossRef] [PubMed]
- Fearnley, C.J.; Llewelyn Roderick, H.; Bootman, M.D. Calcium signaling in cardiac myocytes. Cold Spring Harb. Perspect. Biol. 2011, 3, a004242. [Google Scholar] [CrossRef] [Green Version]
- Weisser-Thomas, J.; Piacentino, V.; Gaughan, J.P.; Margulies, K.; Houser, S.R. Calcium entry via Na/Ca exchange during the action potential directly contributes to contraction of failing human ventricular myocytes. Cardiovasc. Res. 2003, 57, 974–985. [Google Scholar] [CrossRef] [Green Version]
- García-Castro, M.; Reguero, J.R.; Batalla, A.; Díaz-Molina, B.; González, P.; Alvarez, V.; Cortina, A.; Cubero, G.I.; Coto, E. Hypertrophic cardiomyopathy: Low frequency of mutations in the β-myosin heavy chain (MYH7) and cardiac troponin T (TNNT2) genes among Spanish patients. Clin. Chem. 2003, 49, 1279–1285. [Google Scholar] [CrossRef]
- Park, D.S.; Fishman, G.I. The cardiac conduction system. Circulation 2011, 123, 904–915. [Google Scholar] [CrossRef] [Green Version]
- Lu, B.; Yuk, H.; Lin, S.; Jian, N.; Qu, K.; Xu, J.; Zhao, X. Pure PEDOT:PSS hydrogels. Nat. Commun. 2019, 10, 1043. [Google Scholar] [CrossRef] [Green Version]
- Guex, A.G.; Puetzer, J.L.; Armgarth, A.; Littmann, E.; Stavrinidou, E.; Giannelis, E.P.; Malliaras, G.G.; Stevens, M.M. Highly porous scaffolds of PEDOT:PSS for bone tissue engineering. Acta Biomater. 2017, 62, 91–101. [Google Scholar] [CrossRef]
- Heo, D.N.; Lee, S.J.; Timsina, R.; Qiu, X.; Castro, N.J.; Zhang, L.G. Development of 3D printable conductive hydrogel with crystallized PEDOT:PSS for neural tissue engineering. Mater. Sci. Eng. C 2019, 99, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Cho, K.; Lee, H.J.; Chang, S.; Lee, H.; Kim, J.H.; Koh, W.G. Highly conductive and hydrated PEG-based hydrogels for the potential application of a tissue engineering scaffold. React. Funct. Polym. 2016, 109, 15–22. [Google Scholar] [CrossRef]
- Fallahi, A.; Mandla, S.; Kerr-Phillip, T.; Seo, J.; Rodrigues, R.O.; Jodat, Y.A.; Samanipour, R.; Hussain, M.A.; Lee, C.K.; Bae, H.; et al. Flexible and Stretchable PEDOT-Embedded Hybrid Substrates for Bioengineering and Sensory Applications. ChemNanoMat 2019, 5, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Yao, F.; Ye, L.; Hao, T.; Zhang, Y.; Zhang, L.; Dong, D.; Fang, W.; Wang, Y.; Zhang, X.; et al. A conductive PEDOT/alginate porous scaffold as a platform to modulate the biological behaviors of brown adipose-derived stem cells. Biomater. Sci. 2020, 8, 3173–3185. [Google Scholar] [CrossRef]
- Roshanbinfar, K.; Vogt, L.; Greber, B.; Diecke, S.; Boccaccini, A.R.; Scheibel, T.; Engel, F.B. Electroconductive Biohybrid Hydrogel for Enhanced Maturation and Beating Properties of Engineered Cardiac Tissues. Adv. Funct. Mater. 2018, 28, 1803951. [Google Scholar] [CrossRef] [Green Version]
- Lei, Q.; He, J.; Li, D. Electrohydrodynamic 3D printing of layer-specifically oriented, multiscale conductive scaffolds for cardiac tissue engineering. Nanoscale 2019, 11, 15195–15205. [Google Scholar] [CrossRef]
- Spencer, A.R.; Primbetova, A.; Koppes, A.N.; Koppes, R.A.; Fenniri, H.; Annabi, N. Electroconductive Gelatin Methacryloyl-PEDOT:PSS Composite Hydrogels: Design, Synthesis, and Properties. ACS Biomater. Sci. Eng. 2018, 4, 1558–1567. [Google Scholar] [CrossRef]
- Sikorski, P. Electroconductive scaffolds for tissue engineering applications. Biomater. Sci. 2020, 8, 5583–5588. [Google Scholar] [CrossRef]
- Wu, Y.; Guo, L. Enhancement of intercellular electrical synchronization by conductive materials in cardiac tissue engineering. IEEE Trans. Biomed. Eng. 2018, 65, 264–272. [Google Scholar] [CrossRef]
- Fendyur, A.; Mazurski, N.; Shappir, J.; Spira, M.E. Formation of essential ultrastructural interface between cultured hippocampal cells and gold mushroom-shaped MEA- towards “IN-CELL” recordings from vertebrate neurons. Front. Neuroeng. 2011, 4, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nerbonne, J.M.; Kass, R.S. Molecular physiology of cardiac repolarization. Physiol. Rev. 2005, 85, 1205–1253. [Google Scholar] [CrossRef] [Green Version]
- Santana, L.F.; Cheng, E.P.; Lederer, W.J. How does the shape of the cardiac action potential control calcium signaling and contraction in the heart? J. Mol. Cell. Cardiol. 2010, 49, 901–903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cui, Z.; Ni, N.C.; Wu, J.; Du, G.Q.; He, S.; Yau, T.M.; Weisel, R.D.; Sung, H.W.; Li, R.K. Polypyrrole-chitosan conductive biomaterial synchronizes cardiomyocyte contraction and improves myocardial electrical impulse propagation. Theranostics 2018, 8, 2752–2764. [Google Scholar] [CrossRef]
- Zhang, C.; Hsieh, M.H.; Wu, S.Y.; Li, S.H.; Wu, J.; Liu, S.M.; Wei, H.J.; Weisel, R.D.; Sung, H.W.; Li, R.K. A self-doping conductive polymer hydrogel that can restore electrical impulse propagation at myocardial infarct to prevent cardiac arrhythmia and preserve ventricular function. Biomaterials 2020, 231, 119672. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Hsieh, M.H.; Li, S.H.; Wu, J.; Weisel, R.D.; Chang, Y.; Sung, H.W.; Li, R.K. A conductive cell-delivery construct as a bioengineered patch that can improve electrical propagation and synchronize cardiomyocyte contraction for heart repair. J. Control. Release 2020, 320, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Fukuta, H.; Little, W.C. Contribution of Systolic and Diastolic Abnormalities to Heart Failure With a Normal and a Reduced Ejection Fraction. Prog. Cardiovasc. Dis. 2007, 49, 229–240. [Google Scholar] [CrossRef]
- King, D.L.; El-Khoury Coffin, L.; Maurer, M.S. Myocardial contraction fraction: A volumetric index of myocardial shortening by freehand three-dimensional echocardiography. J. Am. Coll. Cardiol. 2002, 40, 325–329. [Google Scholar] [CrossRef] [Green Version]
- Mihardja, S.S.; Sievers, R.E.; Lee, R.J. The effect of polypyrrole on arteriogenesis in an acute rat infarct model. Biomaterials 2008, 29, 4205–4210. [Google Scholar] [CrossRef] [Green Version]
- Jugdutt, B.I. Current Perspective Ventricular Remodeling After Infarction and the Extracellular Collagen Matrix When Is Enough Enough? Circulation 2003, 108, 1395–1403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willems, I.E.; Havenith, M.G.; De Mey, J.G.; Daemen, M.J. The alpha-Smooth Muscle actin-Positive Cells in Healing Human Myocardial Scars. Am. J. Pathol. 1994, 145, 868–875. [Google Scholar]
- Sun, Y.; Weber, K.T. Infarct scar: A dynamic tissue. Cardiovasc. Res. 2000, 46, 250–256. [Google Scholar] [CrossRef] [Green Version]
- Darby, I.; Skalli, O.; Gabbiani, G. α-Smooth muscle actin is transiently expressed by myofibroblasts during experimental wound healing. Lab. Investig. 1990, 63, 21–29. [Google Scholar]
- Jugdutt, B.I. Remodeling of the myocardium and potential targets in the collagen degradation and synthesis pathways. Curr. Drug Targets Cardiovasc. Haematol. Disord. 2003, 3, 1–30. [Google Scholar] [CrossRef]
- Kapnisi, M.; Mansfield, C.; Marijon, C.; Guex, A.G.; Perbellini, F.; Bardi, I.; Humphrey, E.J.; Puetzer, J.L.; Mawad, D.; Koutsogeorgis, D.C.; et al. Auxetic Cardiac Patches with Tunable Mechanical and Conductive Properties toward Treating Myocardial Infarction. Adv. Funct. Mater. 2018, 28, 1800618. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, J.; Li, X.; Hu, J.; Chen, F.; Qiao, S.; Sun, X.; Gao, L.; Xie, J.; Xu, B. Mesenchymal stromal cell-derived exosomes attenuate myocardial ischaemia-reperfusion injury through miR-182-regulated macrophage polarization. Cardiovasc. Res. 2019, 115, 1205–1216. [Google Scholar] [CrossRef] [Green Version]
- Teng, X.; Chen, L.; Chen, W.; Yang, J.; Yang, Z.; Shen, Z. Mesenchymal stem cell-derived exosomes improve the microenvironment of infarcted myocardium contributing to angiogenesis and anti-inflammation. Cell. Physiol. Biochem. 2015, 37, 2415–2424. [Google Scholar] [CrossRef] [PubMed]
- Shi, G.; Rouabhia, M.; Wang, Z.; Dao, L.H.; Zhang, Z. A novel electrically conductive and biodegradable composite made of polypyrrole nanoparticles and polylactide. Biomaterials 2004, 25, 2477–2488. [Google Scholar] [CrossRef]
- Shi, G.; Rouabhia, M.; Meng, S.; Zhang, Z. Electrical stimulation enhances viability of human cutaneous fibroblasts on conductive biodegradable substrates. J. Biomed. Mater. Res. Part A 2008, 84, 1026–1037. [Google Scholar] [CrossRef]
- Bettinger, C.J.; Bruggeman, J.P.; Misra, A.; Borenstein, J.T.; Langer, R. Biocompatibility of biodegradable semiconducting melanin films for nerve tissue engineering. Biomaterials 2009, 30, 3050–3057. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miriani, R.M.; Abidian, M.R.; Kipke, D.R. Cytotoxic analysis of the conducting polymer PEDOT using myocytes. In Proceedings of the 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Vancouver, BC, Canada, 20–25 August 2008; pp. 1841–1844. [Google Scholar]
| Conductive Substrate | Mechanical Properties | Electrical Properties | Cell Line or Tissue | Biological Response |
|---|---|---|---|---|
| Poly-l-Lysine-PANI nanotubes membranes [32] | Rat CMs | Better CMs proliferation | ||
| PLCL, PANI electrospun membranes [33] | E = 50 MPa, εr = 207.85%, UTS = 0.69 MPa | Four-probe technique, σ = 13.8 mS/cm | Human fibroblasts, NIH-3T3, C2C12 | Improved cell adhesion and metabolic activity |
| PGLD, PANI nanotubes membranes [34] | Cho cells, neonatal rat CMs | Good biocompatibility | ||
| PU-AP/PCL porous scaffold [35] | Ec = 4.1 MPa, C.S = 1.3 MPa | Four-probe technique, σ = 10−5 S/cm | Neonatal rat CMs | Enhanced Actn4, Cx43, and cTnT2 expressions. |
| PANI/PCL patch [36] | Two-probe technique, σ = 80 µS/cm | hMSCs | Differentiation of hMSCs to CM-like cells | |
| PDLA/PANI electrospun membranes [37] | σ = 44 mS/cm | primary rat muscle cells | Improved cell adhesion and proliferation | |
| Gelatin/PANI electrospun membranes [38] | E = 1384 MPa, UTS = 10.49 MPa, εr = 9% | Four-probe technique, σ = 17 mS/cm | H9c2 | Smooth muscle-like morphology rich in microfilaments |
| Gelatin/PANI hydrogels [39] | G’ = 5 Pa, G” = 26 Pa | Pocket conductivity meter, σ = 0.45 mS/cm | C2C12, BM-MSCs | Improved cell-cell signalling and proliferation |
| PU-AP/PCL films [40] | E’ = 10 MPa at 37 °C | Four-probe technique, σ = 10−5 S/cm | L929, HUVECs | Improved cytocompatibility, good antioxidant properties |
| PLGA, PANI electrospun meshes [41] | E = 91.7 MPa | Four-point probe, σ = 3.1 mS/cm | Neonatal rat CMs | Enhanced Cx43 and cTnI expressions |
| PGS/PANI composites [42] | E = 6 MPa, UTS = 9.2 MPa, εr = 40% | Four-probe technique, σ = 18 mS/cm | C2C12 | Good cell retention, growth, and proliferation |
| PCL, amino capped AT films [43] | E = 31.2 MPa, UTS = 48.3 MPa, εr = 646% | - | C2C12 | Spindle like morphology, myotube formation |
| PCL, PANI electrospun membranes [44] | E = 55.2 MPa, UTS = 10.5 MPa, εr = 38.0% | Four-point probe, σ = 63.6 mS/cm | C2C12 | Myotube formation |
| PANI, E-PANI films [45] | Z > 10 MΩ/sqr for PANI Z = 6 MΩ/sqr for E-PANI | H9c2 | Improved proliferation and cell attachment on E-PANI | |
| PLA/PANI electrospun membranes [46] | Four-probe technique, σ = 21 µS/m | H9c2, rat CMs | Myotube formation from H9c2 cells, enhanced Cx43 and α-actinin expression, improved Ca2+ transients for CMs | |
| PCL/SF/PANI hydrogels [47] | εr = 107% | C2C12 | Excellent cell alignment, myotube formation | |
| Chitosan-AT/PEG-DA hydrogels [48] | G’ = 7 kPa | Pocket conductivity meter, σ = 2.42 mS/cm | C2C12, H9c2 | Improved cell viability |
| PGS-AT elastomers [49] | E = 2.2 MPa, UTS = 2.0 MPa, εr = 141% | - | H9c2, rat CMs | Synchronous CM beating with improved Ca2+ transients, H9c2 showed good orientation, enhanced Cx43 and α-actinin expression |
| PANI, Collagen, HA electrospun mats [50] | E = 0.02 MPa, UTS= 4 MPa, εr = 78% | Four-probe technique, σ = 2 mS/cm | Neonatal rat CMs, hiPSCs | Synchronous beating of CMs derived from hiPSCs. Enhanced Cx43 and cTnI expression |
| AP, PLA films [51] | Four-point probe, σ = 10−6 to 10−5 S/cm | H9c2 | Pseudopodia like morphology, improved Ca2+ transients | |
| Chitosan, PANI patch [52] | E = 6.73 MPa, UTS = 5.26 MPa, εr = 79% | Four-probe technique, σ = 0.162 S/cm | Rat MI heart | Improved CV in the infarcted region with healing effects |
| PA, PANI patch [53] | Elongation = 84% | Digital Avometer, σ = 2.79 S/m | Pork heart | Cardiac ECM mimicking |
| HPLA/AT films [54] | εr = 42.7%, E = 758 MPa | C2C12 | Myotube formation | |
| Dextran-AT/chitosan [55] | G’ = 620 Pa at t = 50 min | Four-probe technique, σ = 0.03 mS/cm | L929, C2C12 | high proliferation rate, good in vivo degradation, generation of new myofibers |
| Conductive Substrate | Mechanical Properties | Electrical Properties | Cell Line or Tissue | Biological Response |
|---|---|---|---|---|
| PCL, PPy films [71] | Nanoindentation test, E = 0.93 GPa | Keithley Parameter Analyzer, ρ = 1.0 kΩ-cm | HL-1 murine CMs | Enhanced Cx43 expression, improved Ca2+ transients |
| Chitosan, PPy porous membranes [72] | E = 486.7 kPa | Three-probe detector, σ = 63 mS/m | NRVMs, rat MI model | Improved cytoskeletal organisation with high beating amplitude, tissue morphogenesis at the MI site |
| SF, PPy composites [69] | E = 200 MPa, UTS = 7 MPa | Four-probe technique, σ = 1 S/cm | hPSC-CMs | Enhanced expression of Cx43, Myh7, cTnT2, SCN5A genes, elongated Z-band width and sarcomeric length |
| Chitosan, PPy hydrogels [68] | E = 3 kPa | Four-point probe, σ = 0.23 mS/cm | Neonatal rat CMs, rat SMCs | Good proliferation with elevated calcium transients and shorter QRS intervals |
| PLGA, PPy membranes [67] | Mice CPCs, hiPSCs | Good biocompatibility and proliferation rate | ||
| PLGA, PPy membranes [18] | hiPSCs | Differentiation of hiPSCs to CMs, enhanced expression of actinin, Nkx2.5, GATA4, and Oct4 | ||
| PCL, gelatin, PPy electrospun membranes [73] | E = 50.3 MPa, εr = 3.7% | Four-probe technique, σ = 0.37 mS/cm | Rabbit primary CMs | High proliferation rate, enhanced expression of Cx43, cTnT, and α-actinin |
| PPy, HPAE hydrogels [74] | G’ = 35 kPa, | Four-probe technique, σ = 0.65 mS/cm | L929, BMSCs | Enhanced Cx43, α-SMA expressions, excellent cell viability and biocompatibility |
| Conductive Substrate | Mechanical Properties | Electrical Properties | Cell Line | Biological Response |
|---|---|---|---|---|
| PEG/PEDOT:PSS hydrogels [82] | Ec = 21 kPa | Four-probe technique, σ = 16.9 mS/cm | H9c2 | Good cell viability and proliferation |
| GelMA/PEDOT:PSS hydrogels [87] | E = 10.3 kPa | ElS, Z = 261 kΩ at 1 Hz | C2C12 | Good cell viability and proliferation but high polymer concentration was detrimental to cells |
| Collagen/alginate/ PEDOT:PSS hydrogels [85] | G = 220 Pa, τmax = 41 Pa | Four-probe technique, σ = 3.5 mS/cm | CMs, hiPSCs-CMs | Good cell viability, proliferation, and adhesion, synchronous beating patterns |
| Alginate/PEDOT hydrogels [84] | Ec = 175 kPa, G’ = 100 kPa, G” = 10 kPa | Electrochemical workstation, σ = 61 mS/cm | BADSCs | Differentiation of BADSCs to CMs with enhanced expression of cTnT, α-actinin, Cx43 |
| NBR/PEGDM/PEDOT electrospun membranes [83] | E = 3.8 MPa, εr = 75.1% | Four-probe technique, σ = 5.8 S/cm | Cardiac fibroblasts | Well organised sarcomeres, enhanced expression of α-actinin, Cx43 |
| PCL/PEDOT:PSS microfibrous scaffold [86] | E = 13 MPa | H9c2, primary CMs | Enhanced expression of Cx43 and α-actinin, synchronous beating patterns of CMs |
| Conductive Substrate | Outcomes |
|---|---|
| Chitosan, PANI patch [52] | CV increased from 24.3 cm/s in the apex of the MI zone to 30.1 cm/s after applying the conductive patch. |
| Chitosan, PANI auxetic patch [104] | Minimal in vivo fibrotic response, good adhesion with the heart wall, no significant improvements in the cardiac functions though. |
| Alginate, PPy hydrogel [98] | Conductive hydrogel injected hearts: Increased angiogenesis with arteriole density of 33 arteriole/µm2, five weeks post-injection. PBS injected hearts: low arteriole density of 21 arteriole/µm2. |
| Chitosan, PPy hydrogel [25] | Conductive hydrogel injected hearts: EF/FS improved to 67%/34%, QRS/QT intervals reduced to 13/42 ms, and high CV of 62 cm/s, three months post-injection. Saline injected hearts: EF/FS was around 53%/25%, prolonged QRS/QT intervals of 17/70 ms, CV dropped to 43 cm/s. |
| Chitosan, PPy hydrogel [68] | Improved electrical signal conduction in the infarcted zone with reduced QRS intervals. |
| Chitosan, PPy patch [72] | Patch implanted hearts: Enhanced angiogenesis with 180 blood vessels/mm2, tissue regeneration area of 0.3 µm2, four weeks post-implantation. Chitosan injected hearts: Reduced angiogenesis with 68 blood vessels/mm2 and tissue regeneration area of 0.2 µm2. |
| PPy, HPAE, gelatin hydrogel [74] | Conductive hydrogel injected hearts: EF/FS improved to 56%/31%, EDV/ESV to 325/150 µL, QRS interval reduced to 16 ms, after four weeks of injection. MI hearts: EF/FS dropped to 29%/15%, EDV/ESV to 525/420 µL, prolonged QRS of 40 ms. |
| PPy, chitosan hydrogel [93] | Conductive hydrogel injected hearts: Improved longitudinal CV of 74.3 cm/s through the scar tissue after seven days of injection, shorter QRS interval of 18.6 ms, four weeks post-injection. Saline injected hearts: longitudinal CV dropped to 57.7 cm/s, prolonged QRS interval of 23.7 ms. |
| PAMB-G hydrogel [94] | Conductive hydrogel injected hearts: Regional field potential increased to 1.5 mV and CV to 40 cm/s in the scar tissue, EF/EF improved to 67%/31%, LVIDs and LVIDd reduced to 6.2 mm and 8.7 mm, respectively, four weeks post-injection. Gelatin injected hearts: Regional field potential was around 0.7 mV with a slow CV of 27 cm/s, EF/FS dropped to 56%/23%, LVIDs and LVIDd were around 7 mm and 9.3 mm, respectively. |
| PAMB-G patch [95] | Patch implanted hearts: Regional field potential increased to 1.9 mV with a CV of 39 cm/s in the scar tissue, reduced QRS intervals of 13 ms, EF/FS improved to 60%/28%, LVIDs and LVIDd reduced to 5.3 mm and 7.8 mm, respectively, four weeks post-implantation. Gelatin injected hearts: Reduced regional field potential of 0.7 mV with a slow CV of 19 cm/s, prolonged QRS intervals of 22 ms, EF/FS dropped to 57%/26%, LVIDs and LVIDs were around 5.6 mm and 8.2 mm. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ul Haq, A.; Carotenuto, F.; De Matteis, F.; Prosposito, P.; Francini, R.; Teodori, L.; Pasquo, A.; Di Nardo, P. Intrinsically Conductive Polymers for Striated Cardiac Muscle Repair. Int. J. Mol. Sci. 2021, 22, 8550. https://doi.org/10.3390/ijms22168550
Ul Haq A, Carotenuto F, De Matteis F, Prosposito P, Francini R, Teodori L, Pasquo A, Di Nardo P. Intrinsically Conductive Polymers for Striated Cardiac Muscle Repair. International Journal of Molecular Sciences. 2021; 22(16):8550. https://doi.org/10.3390/ijms22168550
Chicago/Turabian StyleUl Haq, Arsalan, Felicia Carotenuto, Fabio De Matteis, Paolo Prosposito, Roberto Francini, Laura Teodori, Alessandra Pasquo, and Paolo Di Nardo. 2021. "Intrinsically Conductive Polymers for Striated Cardiac Muscle Repair" International Journal of Molecular Sciences 22, no. 16: 8550. https://doi.org/10.3390/ijms22168550
APA StyleUl Haq, A., Carotenuto, F., De Matteis, F., Prosposito, P., Francini, R., Teodori, L., Pasquo, A., & Di Nardo, P. (2021). Intrinsically Conductive Polymers for Striated Cardiac Muscle Repair. International Journal of Molecular Sciences, 22(16), 8550. https://doi.org/10.3390/ijms22168550







