The Role of Caspase-12 in Retinal Bystander Cell Death and Innate Immune Responses against MCMV Retinitis
Abstract
1. Introduction
2. Results
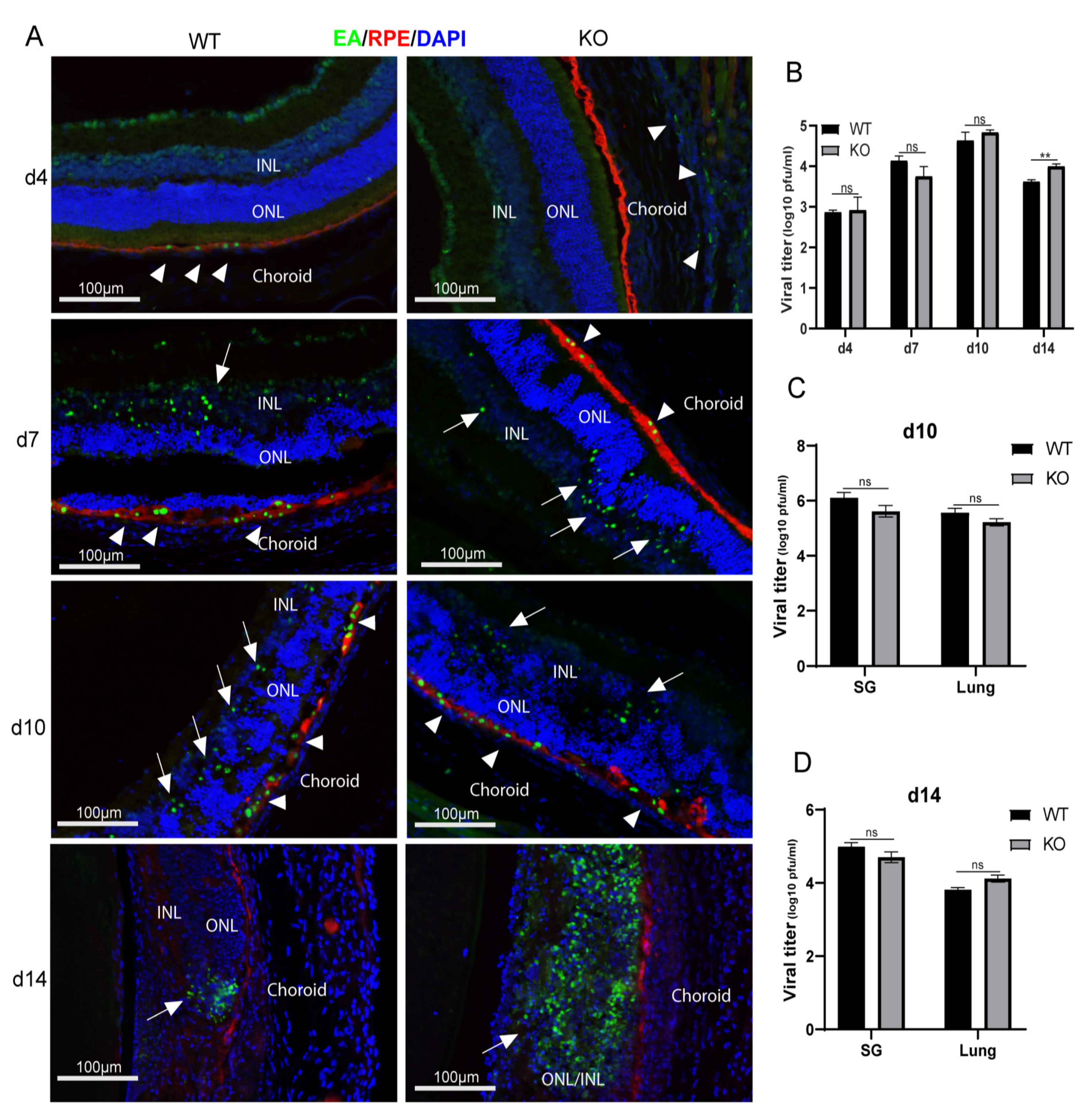
2.1. MCMV Spread and Replication
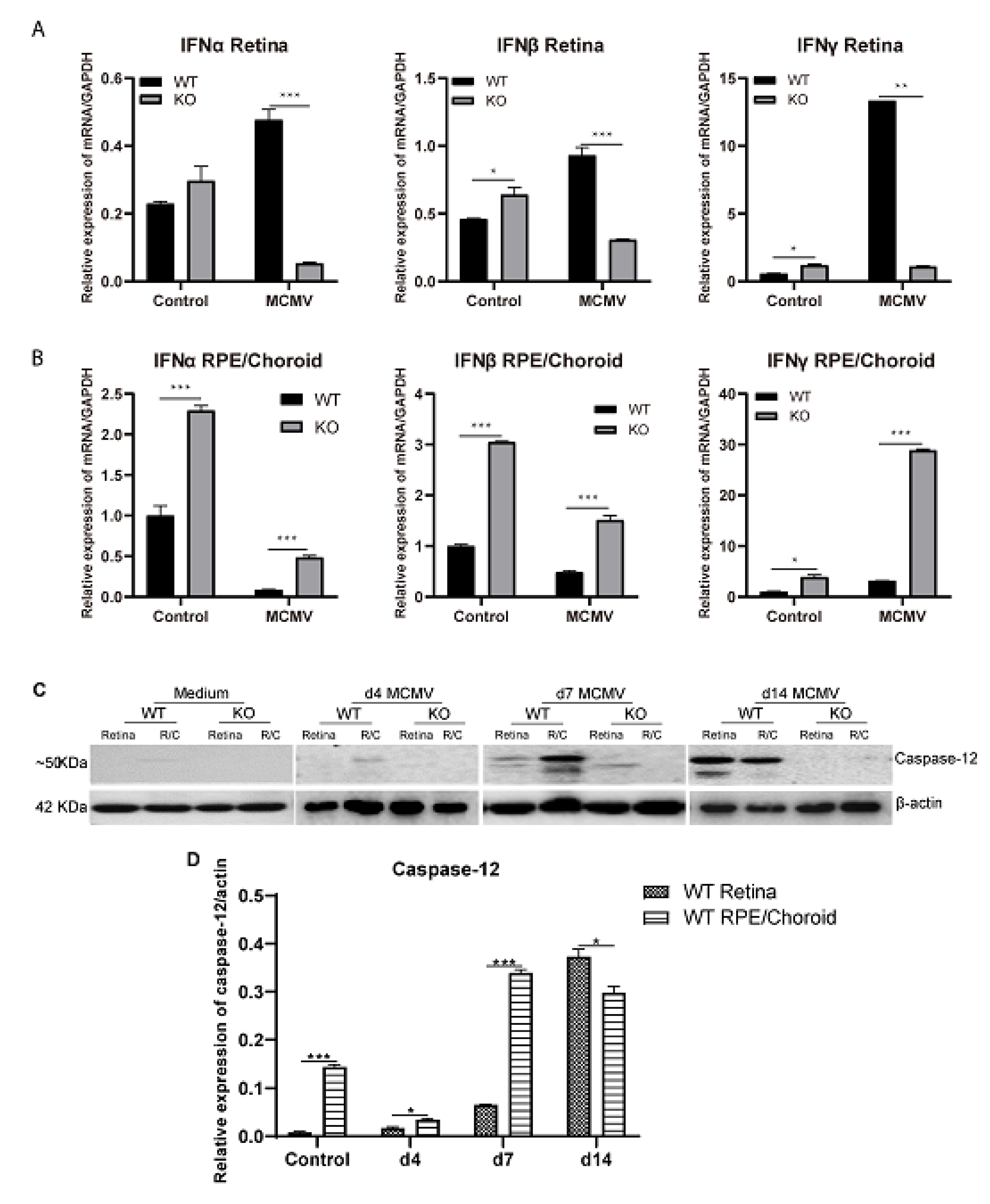
2.2. Interferon Production and Caspase-12 Expression
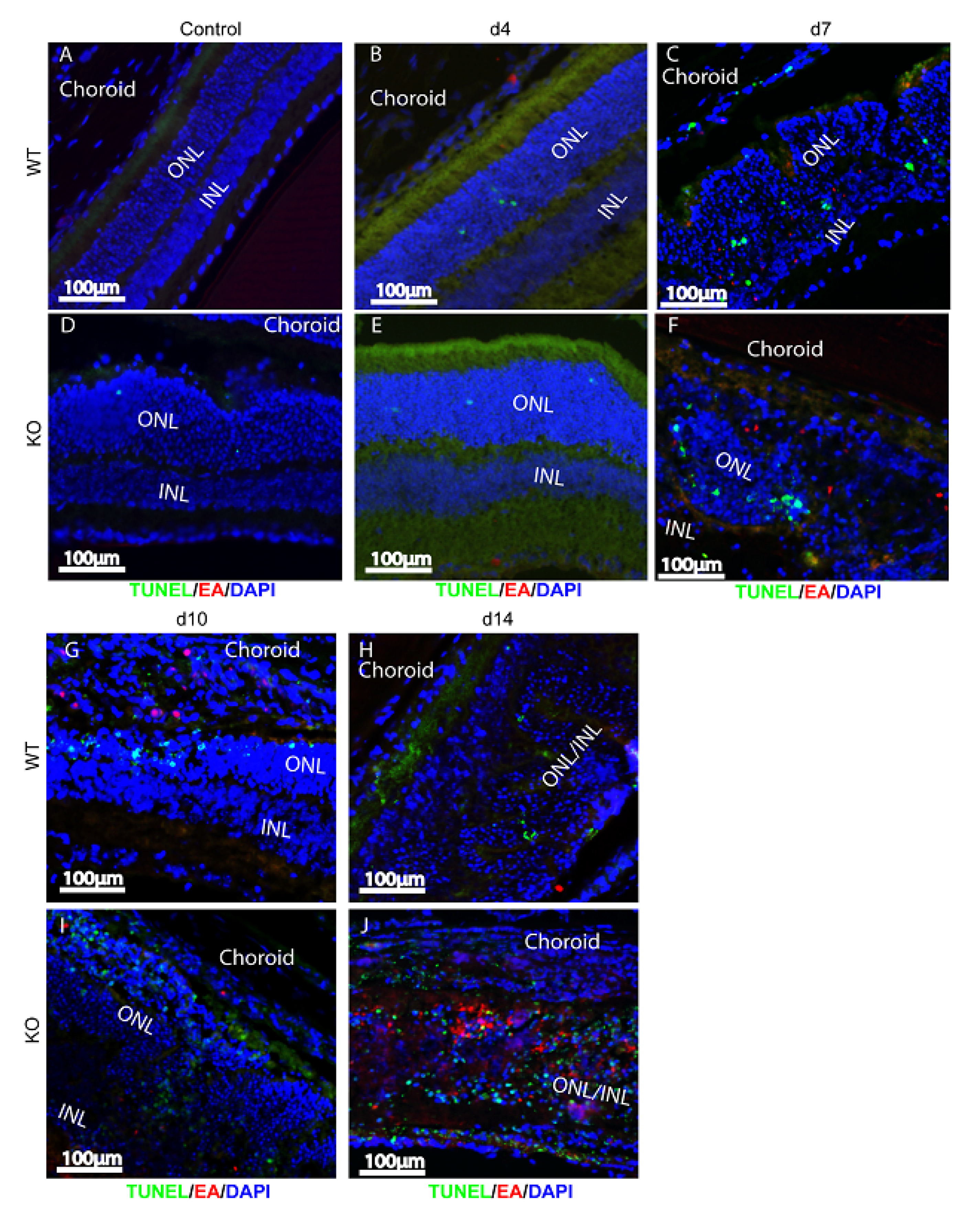
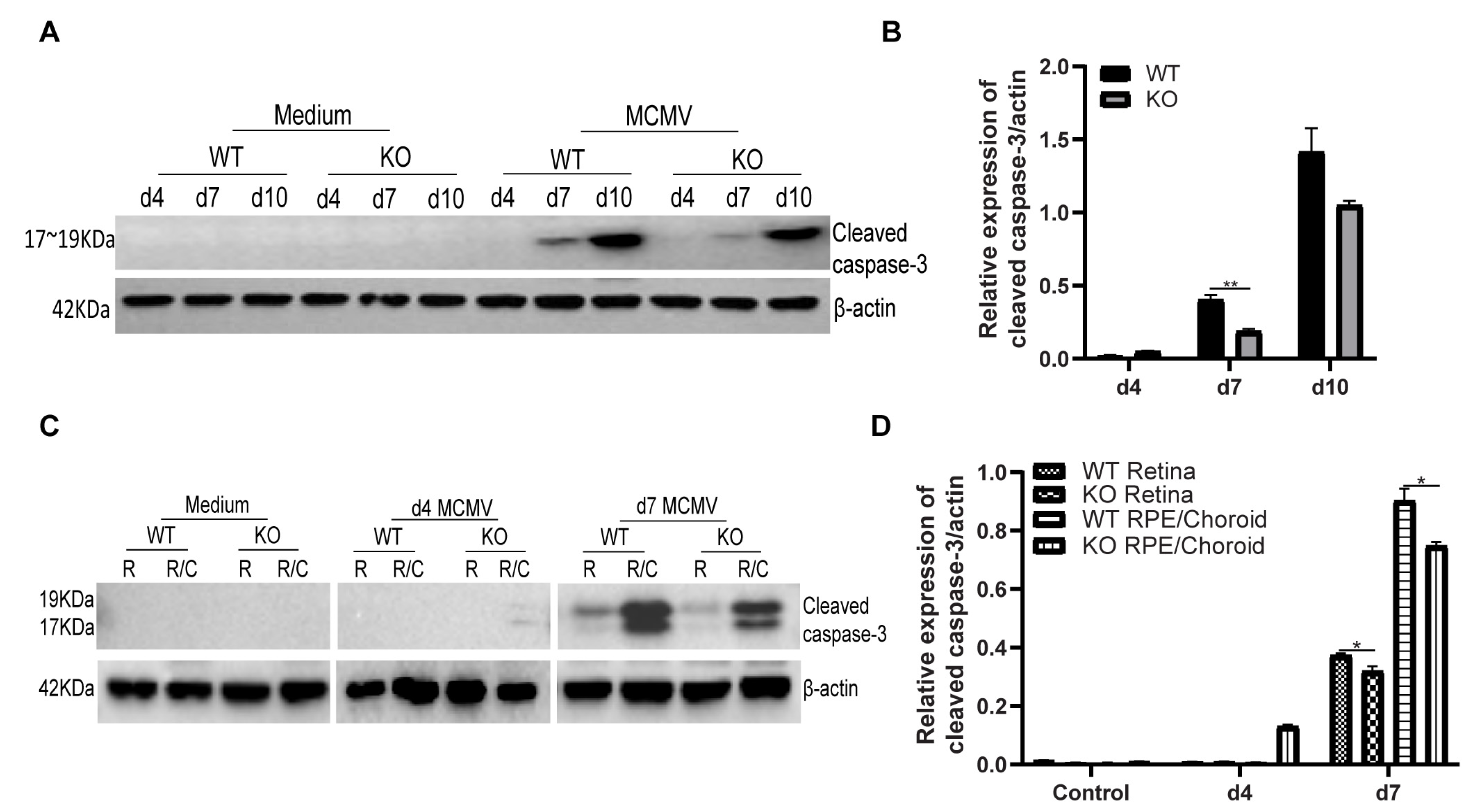
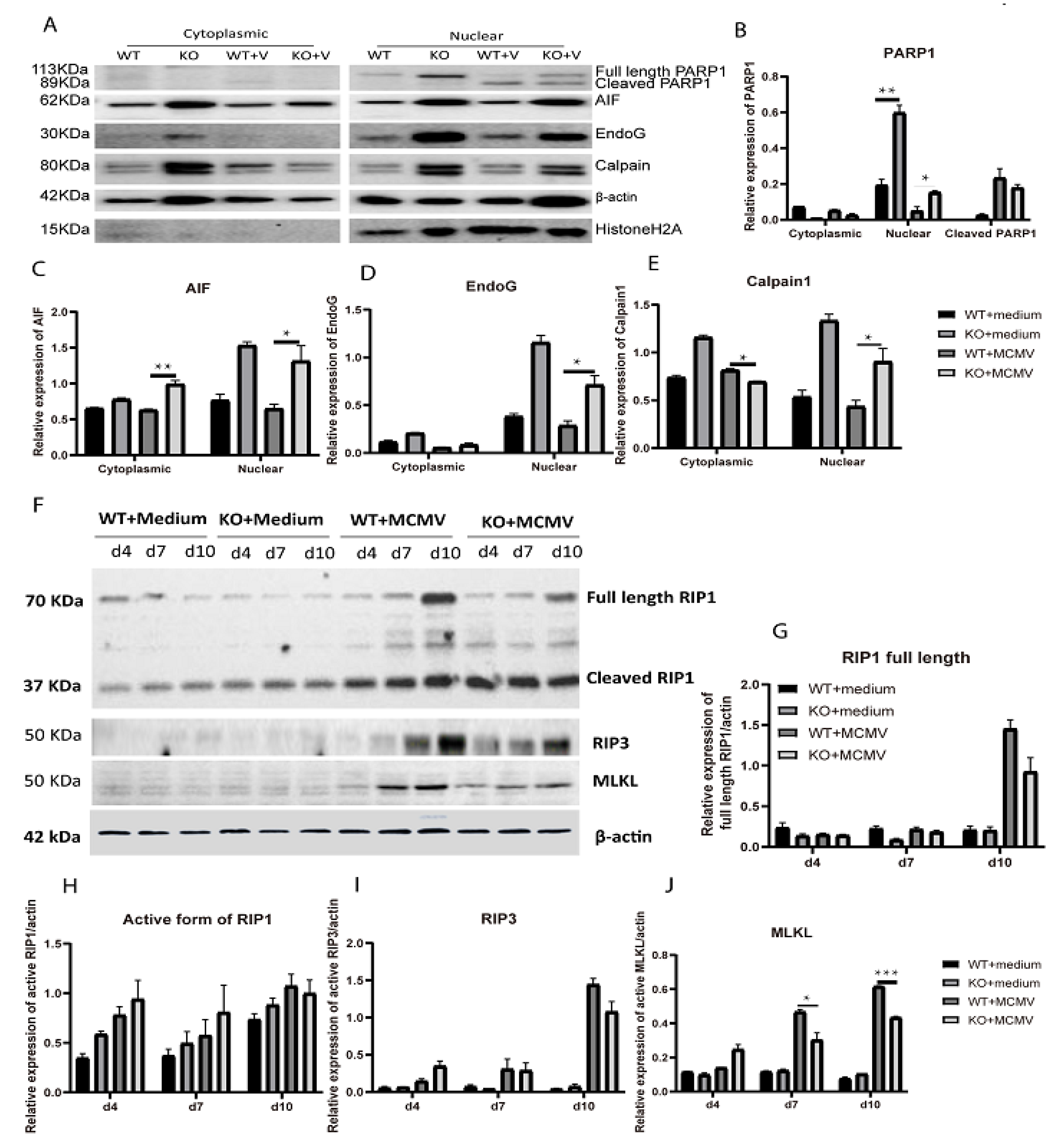
2.3. Bystander Retinal Cell Death
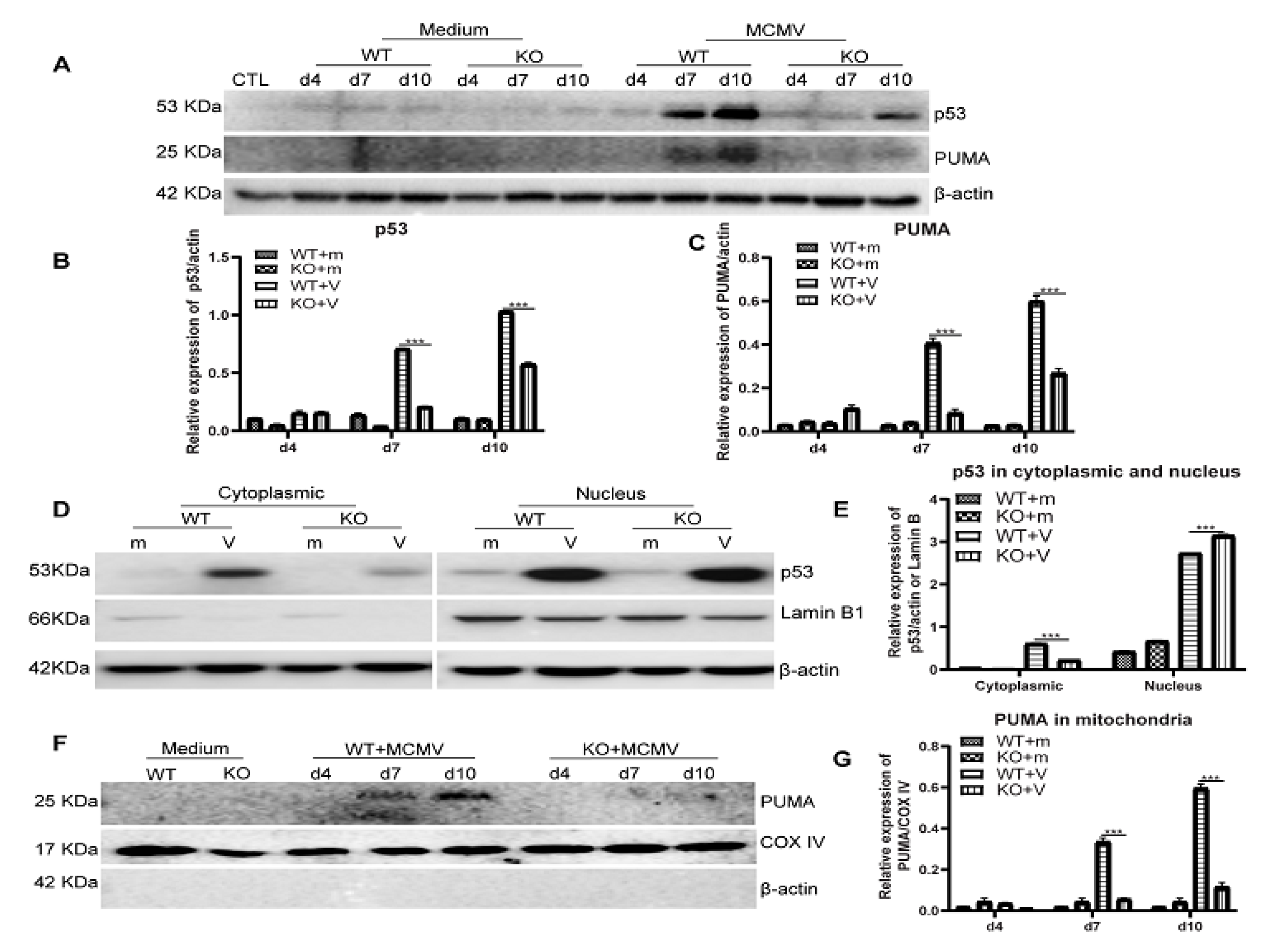
2.4. p53 Expression
3. Discussion
4. Materials and Methods
4.1. Virus
4.2. Reagents and Antibodies
4.3. Mice
4.4. Experimental Design
4.5. H&E and Immunofluorescence Staining
4.6. Western Blot
4.7. Real-Time PCR
4.8. Retinitis Scoring
4.9. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Demmler, G.J. Infectious Diseases Society of America and Centers for Disease Control. Summary of a workshop on surveillance for congenital cytomegalovirus disease. Rev. Infect. Dis. 1991, 13, 315–329. [Google Scholar] [CrossRef]
- Krishna, B.A.; Wills, M.R.; Sinclair, J.H. Advances in the treatment of cytomegalovirus. Br. Med. Bull. 2019, 131, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Chien, H.; Alston, C.I.; Dix, R.D. Suppressor of Cytokine Signaling 1 (SOCS1) and SOCS3 Are Stimulated within the Eye during Experimental Murine Cytomegalovirus Retinitis in Mice with Retrovirus-Induced Immunosuppression. J. Virol. 2018, 92, e00526-18. [Google Scholar] [CrossRef] [PubMed]
- Jabs, D.A. Cytomegalovirus retinitis and the acquired immunodeficiency syndrome--bench to bedside: LXVII Edward Jackson Memorial Lecture. Am. J. Ophthalmol. 2011, 151, 198–216 e191. [Google Scholar] [CrossRef] [PubMed]
- Thorne, J.E.; Jabs, D.A.; Kempen, J.H.; Holbrook, J.T.; Nichols, C.; Meinert, C.L. Studies of Ocular Complications of, A.R.G. Incidence of and risk factors for visual acuity loss among patients with AIDS and cytomegalovirus retinitis in the era of highly active antiretroviral therapy. Ophthalmology 2006, 113, 1432–1440. [Google Scholar] [CrossRef] [PubMed]
- Thorne, J.E.; Jabs, D.A.; Kempen, J.H.; Holbrook, J.T.; Nichols, C.; Meinert, C.L. Studies of Ocular Complications of, A.R.G. Causes of visual acuity loss among patients with AIDS and cytomegalovirus retinitis in the era of highly active antiretroviral therapy. Ophthalmology 2006, 113, 1441–1445. [Google Scholar] [CrossRef] [PubMed]
- Bidanset, D.J.; Beadle, J.R.; Wan, W.B.; Hostetler, K.Y.; Kern, E.R. Oral activity of ether lipid ester prodrugs of cidofovir against experimental human cytomegalovirus infection. J. Infect. Dis. 2004, 190, 499–503. [Google Scholar] [CrossRef]
- Bidanset, D.J.; Rybak, R.J.; Hartline, C.B.; Kern, E.R. Replication of human cytomegalovirus in severe combined immunodeficient mice implanted with human retinal tissue. J. Infect. Dis. 2001, 184, 192–195. [Google Scholar] [CrossRef]
- Blalock, E.L.; Chien, H.; Dix, R.D. Systemic reduction of interleukin-4 or interleukin-10 fails to reduce the frequency or severity of experimental cytomegalovirus retinitis in mice with retrovirus-induced immunosuppression. Ophthalmol. Eye Dis. 2012, 4, 79–90. [Google Scholar] [CrossRef]
- Blalock, E.L.; Chien, H.; Dix, R.D. Murine cytomegalovirus downregulates interleukin-17 in mice with retrovirus-induced immunosuppression that are susceptible to experimental cytomegalovirus retinitis. Cytokine 2013, 61, 862–875. [Google Scholar] [CrossRef][Green Version]
- Chien, H.; Dix, R.D. Evidence for multiple cell death pathways during development of experimental cytomegalovirus retinitis in mice with retrovirus-induced immunosuppression: Apoptosis, necroptosis, and pyroptosis. J. Virol. 2012, 86, 10961–10978. [Google Scholar] [CrossRef]
- Dix, R.D.; Cousins, S.W. Interleukin-2 immunotherapy of murine cytomegalovirus retinitis during MAIDS correlates with increased intraocular CD8+ T-cell infiltration. Ophthalmic Res. 2003, 35, 154–159. [Google Scholar] [CrossRef]
- Dix, R.D.; Cousins, S.W. Interleukin-2 immunotherapy and AIDS-related cytomegalovirus retinitis. Curr. HIV Res. 2004, 2, 333–342. [Google Scholar] [CrossRef]
- Dix, R.D.; Cousins, S.W. Susceptibility to murine cytomegalovirus retinitis during progression of MAIDS: Correlation with intraocular levels of tumor necrosis factor-alpha and interferon-gamma. Curr. Eye Res. 2004, 29, 173–180. [Google Scholar] [CrossRef]
- Dix, R.D.; Cousins, S.W. Cell-mediated cytotoxicity of murine cytomegalovirus-infected target cells allows for release of residual infectious virus. Arch. Virol. 2005, 150, 797–803. [Google Scholar] [CrossRef] [PubMed]
- Dix, R.D.; Ekworomadu, C.O.; Hernandez, E.; Cousins, S.W. Perforin knockout mice, but not mice with MAIDS, show protection against experimental cytomegalovirus retinitis after adoptive transfer of immune cells with a functional perforin cytotoxic pathway. Arch. Virol. 2004, 149, 2235–2244. [Google Scholar] [CrossRef]
- Dix, R.D.; Podack, E.R.; Cousins, S.W. Loss of the perforin cytotoxic pathway predisposes mice to experimental cytomegalovirus retinitis. J. Virol. 2003, 77, 3402–3408. [Google Scholar] [CrossRef] [PubMed]
- Laycock, K.A.; Fenoglio, E.D.; Hook, K.K.; Pepose, J.S. An in vivo model of human cytomegalovirus retinal infection. Am. J. Ophthalmol. 1997, 124, 181–189. [Google Scholar] [CrossRef]
- Laycock, K.A.; Kumano, Y.; Pepose, J.S. Reproduction of antiviral effect in an in vivo model of human cytomegalovirus retinal infection. Graefes Arch. Clin. Exp. Ophthalmol. 1998, 236, 527–530. [Google Scholar] [CrossRef] [PubMed]
- Prichard, M.N.; Quenelle, D.C.; Bidanset, D.J.; Komazin, G.; Chou, S.; Drach, J.C.; Kern, E.R. Human cytomegalovirus UL27 is not required for viral replication in human tissue implanted in SCID mice. Virol. J. 2006, 3, 18. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bigger, J.E.; Tanigawa, M.; Zhang, M.; Atherton, S.S. Murine cytomegalovirus infection causes apoptosis of uninfected retinal cells. Investig. Ophthalmol. Vis. Sci. 2000, 41, 2248–2254. [Google Scholar]
- Zhang, M.; Atherton, S.S. Apoptosis in the retina during MCMV retinitis in immunosuppressed BALB/c mice. J. Clin. Virol. Off. Publ. Pan Am. Soc. Clin. Virol. 2002, 25 (Suppl. 2), S137–S147. [Google Scholar] [CrossRef]
- Zhang, M.; Zhou, J.; Marshall, B.; Xin, H.; Atherton, S.S. Lack of iNOS facilitates MCMV spread in the retina. Investig. Ophthalmol. Vis. Sci. 2007, 48, 285–292. [Google Scholar] [CrossRef]
- Zhang, M.; Xin, H.; Roon, P.; Atherton, S.S. Infection of retinal neurons during murine cytomegalovirus retinitis. Investig. Ophthalmol. Vis. Sci. 2005, 46, 2047–2055. [Google Scholar] [CrossRef]
- Chiou, S.H.; Liu, J.H.; Hsu, W.M.; Chen, S.S.; Chang, S.Y.; Juan, L.J.; Lin, J.C.; Yang, Y.T.; Wong, W.W.; Liu, C.Y.; et al. Up-regulation of Fas ligand expression by human cytomegalovirus immediate-early gene product 2: A novel mechanism in cytomegalovirus-induced apoptosis in human retina. J. Immunol. 2001, 167, 4098–4103. [Google Scholar] [CrossRef]
- Buggage, R.R.; Chan, C.C.; Matteson, D.M.; Reed, G.F.; Whitcup, S.M. Apoptosis in cytomegalovirus retinitis associated with AIDS. Curr. Eye Res. 2000, 21, 721–729. [Google Scholar] [CrossRef]
- Chiou, S.H.; Liu, J.H.; Chen, S.S.; Liu, W.T.; Lin, J.C.; Wong, W.W.; Tseng, W.S.; Chou, C.K.; Liu, C.Y.; Ho, L.L.; et al. Apoptosis of human retina and retinal pigment cells induced by human cytomegalovirus infection. Ophthalmic Res. 2002, 34, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Covar, J.; Marshall, B.; Dong, Z.; Atherton, S.S. Lack of TNF-alpha promotes caspase-3-independent apoptosis during murine cytomegalovirus retinitis. Investig. Ophthalmol. Vis. Sci. 2011, 52, 1800–1808. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Zhang, M.; Atherton, S.S. Tumor necrosis factor-alpha-induced apoptosis in murine cytomegalovirus retinitis. Investig. Ophthalmol. Vis. Sci. 2007, 48, 1691–1700. [Google Scholar] [CrossRef]
- Zhang, M.; Marshall, B.; Atherton, S.S. Murine cytomegalovirus infection and apoptosis in organotypic retinal cultures. Investig. Ophthalmol. Vis. Sci. 2008, 49, 295–303. [Google Scholar] [CrossRef][Green Version]
- Oh, J.J.; Carter, J.J.; Nemeno, J.G.E.; Dix, R.D. Parthanatos-associated proteins are stimulated intraocularly during development of experimental murine cytomegalovirus retinitis in mice with retrovirus-induced immunosuppression. J. Med. Virol. 2020, 92, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Saleh, M.; Mathison, J.C.; Wolinski, M.K.; Bensinger, S.J.; Fitzgerald, P.; Droin, N.; Ulevitch, R.J.; Green, D.R.; Nicholson, D.W. Enhanced bacterial clearance and sepsis resistance in caspase-12-deficient mice. Nature 2006, 440, 1064–1068. [Google Scholar] [CrossRef] [PubMed]
- Vande Walle, L.; Jimenez Fernandez, D.; Demon, D.; Van Laethem, N.; Van Hauwermeiren, F.; Van Gorp, H.; Van Opdenbosch, N.; Kayagaki, N.; Lamkanfi, M. Does caspase-12 suppress inflammasome activation? Nature 2016, 534, E1–E4. [Google Scholar] [CrossRef] [PubMed]
- Bitko, V.; Barik, S. An endoplasmic reticulum-specific stress-activated caspase (caspase-12) is implicated in the apoptosis of A549 epithelial cells by respiratory syncytial virus. J. Cell. Biochem. 2001, 80, 441–454. [Google Scholar] [CrossRef]
- Jordan, R.; Wang, L.; Graczyk, T.M.; Block, T.M.; Romano, P.R. Replication of a cytopathic strain of bovine viral diarrhea virus activates PERK and induces endoplasmic reticulum stress-mediated apoptosis of MDBK cells. J. Virol. 2002, 76, 9588–9599. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Arjona, A.; Zhang, Y.; Sultana, H.; Dai, J.; Yang, L.; LeBlanc, P.M.; Doiron, K.; Saleh, M.; Fikrig, E. Caspase-12 controls West Nile virus infection via the viral RNA receptor RIG-I. Nat. Immunol 2010, 11, 912–919. [Google Scholar] [CrossRef] [PubMed]
- LeBlanc, P.M.; Yeretssian, G.; Rutherford, N.; Doiron, K.; Nadiri, A.; Zhu, L.; Green, D.R.; Gruenheid, S.; Saleh, M. Caspase-12 modulates NOD signaling and regulates antimicrobial peptide production and mucosal immunity. Cell Host Microbe 2008, 3, 146–157. [Google Scholar] [CrossRef]
- Nakagawa, T.; Zhu, H.; Morishima, N.; Li, E.; Xu, J.; Yankner, B.A.; Yuan, J. Caspase-12 mediates endoplasmic-reticulum-specific apoptosis and cytotoxicity by amyloid-beta. Nature 2000, 403, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Obeng, E.A.; Boise, L.H. Caspase-12 and caspase-4 are not required for caspase-dependent endoplasmic reticulum stress-induced apoptosis. J. Biol. Chem. 2005, 280, 29578–29587. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, H.; Okamoto, H.; Yoshimura, A.; Yoshida, H. ER stress-induced apoptosis and caspase-12 activation occurs downstream of mitochondrial apoptosis involving Apaf-1. J. Cell Sci. 2006, 119, 3958–3966. [Google Scholar] [CrossRef] [PubMed]
- Mo, J.; Marshall, B.; Covar, J.; Zhang, N.Y.; Smith, S.B.; Atherton, S.S.; Zhang, M. Role of Bax in death of uninfected retinal cells during murine cytomegalovirus retinitis. Investig. Ophthalmol. Vis. Sci. 2014, 55, 7137–7146. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Xu, J.; Mo, J.; Liu, X.; Marshall, B.; Atherton, S.S.; Dong, Z.; Smith, S.; Zhang, M. Depletion of the Receptor-Interacting Protein Kinase 3 (RIP3) Decreases Photoreceptor Cell Death During the Early Stages of Ocular Murine Cytomegalovirus Infection. Investig. Ophthalmol. Vis. Sci. 2018, 59, 2445–2458. [Google Scholar] [CrossRef] [PubMed]
- Hitomi, J.; Katayama, T.; Taniguchi, M.; Honda, A.; Imaizumi, K.; Tohyama, M. Apoptosis induced by endoplasmic reticulum stress depends on activation of caspase-3 via caspase-12. Neurosci. Lett. 2004, 357, 127–130. [Google Scholar] [CrossRef]
- Galluzzi, L.; Kepp, O.; Krautwald, S.; Kroemer, G.; Linkermann, A. Molecular mechanisms of regulated necrosis. Semin. Cell Dev. Biol. 2014, 35, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Cande, C.; Vahsen, N.; Kouranti, I.; Schmitt, E.; Daugas, E.; Spahr, C.; Luban, J.; Kroemer, R.T.; Giordanetto, F.; Garrido, C.; et al. AIF and cyclophilin A cooperate in apoptosis-associated chromatinolysis. Oncogene 2004, 23, 1514–1521. [Google Scholar] [CrossRef]
- Zhu, C.; Wang, X.; Huang, Z.; Qiu, L.; Xu, F.; Vahsen, N.; Nilsson, M.; Eriksson, P.S.; Hagberg, H.; Culmsee, C.; et al. Apoptosis-inducing factor is a major contributor to neuronal loss induced by neonatal cerebral hypoxia-ischemia. Cell Death Differ. 2007, 14, 775–784. [Google Scholar] [CrossRef]
- Susin, S.A.; Lorenzo, H.K.; Zamzami, N.; Marzo, I.; Snow, B.E.; Brothers, G.M.; Mangion, J.; Jacotot, E.; Costantini, P.; Loeffler, M.; et al. Molecular characterization of mitochondrial apoptosis-inducing factor. Nature 1999, 397, 441–446. [Google Scholar] [CrossRef]
- Delavallee, L.; Cabon, L.; Galan-Malo, P.; Lorenzo, H.K.; Susin, S.A. AIF-mediated caspase-independent necroptosis: A new chance for targeted therapeutics. IUBMB Life 2011, 63, 221–232. [Google Scholar] [CrossRef]
- Yu, S.W.; Wang, H.; Poitras, M.F.; Coombs, C.; Bowers, W.J.; Federoff, H.J.; Poirier, G.G.; Dawson, T.M.; Dawson, V.L. Mediation of poly(ADP-ribose) polymerase-1-dependent cell death by apoptosis-inducing factor. Science 2002, 297, 259–263. [Google Scholar] [CrossRef]
- Baritaud, M.; Boujrad, H.; Lorenzo, H.K.; Krantic, S.; Susin, S.A. Histone H2AX: The missing link in AIF-mediated caspase-independent programmed necrosis. Cell Cycle 2010, 9, 3166–3173. [Google Scholar] [CrossRef]
- Boujrad, H.; Gubkina, O.; Robert, N.; Krantic, S.; Susin, S.A. AIF-mediated programmed necrosis: A highly regulated way to die. Cell Cycle 2007, 6, 2612–2619. [Google Scholar] [CrossRef] [PubMed]
- Sanges, D.; Comitato, A.; Tammaro, R.; Marigo, V. Apoptosis in retinal degeneration involves cross-talk between apoptosis-inducing factor (AIF) and caspase-12 and is blocked by calpain inhibitors. Proc. Natl. Acad. Sci. USA 2006, 103, 17366–17371. [Google Scholar] [CrossRef]
- Nakagawa, T.; Yuan, J. Cross-talk between two cysteine protease families. Activation of caspase-12 by calpain in apoptosis. J. Cell Biol. 2000, 150, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.; Andreeva, K.; Cooper, N.G. Ischemia-reperfusion injury of the retina is linked to necroptosis via the ERK1/2-RIP3 pathway. Mol. Vis. 2014, 20, 1374–1387. [Google Scholar] [PubMed]
- Kataoka, K.; Matsumoto, H.; Kaneko, H.; Notomi, S.; Takeuchi, K.; Sweigard, J.H.; Atik, A.; Murakami, Y.; Connor, K.M.; Terasaki, H.; et al. Macrophage- and RIP3-dependent inflammasome activation exacerbates retinal detachment-induced photoreceptor cell death. Cell Death Dis. 2015, 6, e1731. [Google Scholar] [CrossRef]
- Sato, K.; Li, S.; Gordon, W.C.; He, J.; Liou, G.I.; Hill, J.M.; Travis, G.H.; Bazan, N.G.; Jin, M. Receptor interacting protein kinase-mediated necrosis contributes to cone and rod photoreceptor degeneration in the retina lacking interphotoreceptor retinoid-binding protein. J. Neurosci. Off. J. Soc. Neurosci. 2013, 33, 17458–17468. [Google Scholar] [CrossRef]
- Viringipurampeer, I.A.; Shan, X.; Gregory-Evans, K.; Zhang, J.P.; Mohammadi, Z.; Gregory-Evans, C.Y. Rip3 knockdown rescues photoreceptor cell death in blind pde6c zebrafish. Cell Death Differ. 2014, 21, 665–675. [Google Scholar] [CrossRef]
- Castillo, J.P.; Frame, F.M.; Rogoff, H.A.; Pickering, M.T.; Yurochko, A.D.; Kowalik, T.F. Human cytomegalovirus IE1-72 activates ataxia telangiectasia mutated kinase and a p53/p21-mediated growth arrest response. J. Virol. 2005, 79, 11467–11475. [Google Scholar] [CrossRef]
- Lazo, P.A.; Santos, C.R. Interference with p53 functions in human viral infections, a target for novel antiviral strategies? Rev. Med. Virol. 2011, 21, 285–300. [Google Scholar] [CrossRef]
- Sato, Y.; Tsurumi, T. Genome guardian p53 and viral infections. Rev. Med. Virol 2013, 23, 213–220. [Google Scholar] [CrossRef]
- Kalai, M.; Lamkanfi, M.; Denecker, G.; Boogmans, M.; Lippens, S.; Meeus, A.; Declercq, W.; Vandenabeele, P. Regulation of the expression and processing of caspase-12. J. Cell Biol. 2003, 162, 457–467. [Google Scholar] [CrossRef]
- Lee, W.; Kim, D.H.; Boo, J.H.; Kim, Y.H.; Park, I.S.; Mook-Jung, I. ER stress-induced caspase-12 activation is inhibited by PKC in neuronal cells. Apoptosis Int. J. Program. Cell Death 2005, 10, 407–415. [Google Scholar] [CrossRef]
- Song, S.; Lee, H.; Kam, T.I.; Tai, M.L.; Lee, J.Y.; Noh, J.Y.; Shim, S.M.; Seo, S.J.; Kong, Y.Y.; Nakagawa, T.; et al. E2-25K/Hip-2 regulates caspase-12 in ER stress-mediated Abeta neurotoxicity. J. Cell Biol. 2008, 182, 675–684. [Google Scholar] [CrossRef]
- Hetz, C.; Russelakis-Carneiro, M.; Maundrell, K.; Castilla, J.; Soto, C. Caspase-12 and endoplasmic reticulum stress mediate neurotoxicity of pathological prion protein. EMBO J. 2003, 22, 5435–5445. [Google Scholar] [CrossRef]
- Kim, H.T.; Waters, K.; Stoica, G.; Qiang, W.; Liu, N.; Scofield, V.L.; Wong, P.K. Activation of endoplasmic reticulum stress signaling pathway is associated with neuronal degeneration in MoMuLV-ts1-induced spongiform encephalomyelopathy. Lab. Investig. J. Tech. Methods Pathol. 2004, 84, 816–827. [Google Scholar] [CrossRef]
- Garcia de la Cadena, S.; Massieu, L. Caspases and their role in inflammation and ischemic neuronal death. Focus on caspase-12. Apoptosis Int. J. Program. Cell Death 2016, 21, 763–777. [Google Scholar] [CrossRef] [PubMed]
- Shibata, M.; Hattori, H.; Sasaki, T.; Gotoh, J.; Hamada, J.; Fukuuchi, Y. Activation of caspase-12 by endoplasmic reticulum stress induced by transient middle cerebral artery occlusion in mice. Neuroscience 2003, 118, 491–499. [Google Scholar] [CrossRef]
- Zulliger, R.; Lecaude, S.; Eigeldinger-Berthou, S.; Wolf-Schnurrbusch, U.E.; Enzmann, V. Caspase-3-independent photoreceptor degeneration by N-methyl-N-nitrosourea (MNU) induces morphological and functional changes in the mouse retina. Graefes Arch. Clin. Exp. Ophthalmol. 2011, 249, 859–869. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sanges, D.; Marigo, V. Cross-talk between two apoptotic pathways activated by endoplasmic reticulum stress: Differential contribution of caspase-12 and AIF. Apoptosis 2006, 11, 1629–1641. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.W.; Andrabi, S.A.; Wang, H.; Kim, N.S.; Poirier, G.G.; Dawson, T.M.; Dawson, V.L. Apoptosis-inducing factor mediates poly(ADP-ribose) (PAR) polymer-induced cell death. Proc. Natl. Acad. Sci. USA 2006, 103, 18314–18319. [Google Scholar] [CrossRef]
- Munoz-Fontela, C.; Macip, S.; Martinez-Sobrido, L.; Brown, L.; Ashour, J.; Garcia-Sastre, A.; Lee, S.W.; Aaronson, S.A. Transcriptional role of p53 in interferon-mediated antiviral immunity. J. Exp. Med. 2008, 205, 1929–1938. [Google Scholar] [CrossRef] [PubMed]
- Hummer, B.T.; Li, X.L.; Hassel, B.A. Role for p53 in gene induction by double-stranded RNA. J. Virol. 2001, 75, 7774–7777. [Google Scholar] [CrossRef] [PubMed]
- Perng, Y.C.; Lenschow, D.J. ISG15 in antiviral immunity and beyond. Nat. Rev. Microbiol. 2018, 16, 423–439. [Google Scholar] [CrossRef] [PubMed]
- Tabeta, K.; Georgel, P.; Janssen, E.; Du, X.; Hoebe, K.; Crozat, K.; Mudd, S.; Shamel, L.; Sovath, S.; Goode, J.; et al. Toll-like receptors 9 and 3 as essential components of innate immune defense against mouse cytomegalovirus infection. Proc. Natl. Acad. Sci. USA 2004, 101, 3516–3521. [Google Scholar] [CrossRef] [PubMed]
- Taura, M.; Eguma, A.; Suico, M.A.; Shuto, T.; Koga, T.; Komatsu, K.; Komune, T.; Sato, T.; Saya, H.; Li, J.D.; et al. p53 regulates Toll-like receptor 3 expression and function in human epithelial cell lines. Mol. Cell. Biol. 2008, 28, 6557–6567. [Google Scholar] [CrossRef]
- Takaoka, A.; Hayakawa, S.; Yanai, H.; Stoiber, D.; Negishi, H.; Kikuchi, H.; Sasaki, S.; Imai, K.; Shibue, T.; Honda, K.; et al. Integration of interferon-alpha/beta signalling to p53 responses in tumour suppression and antiviral defence. Nature 2003, 424, 516–523. [Google Scholar] [CrossRef]
- Hsu, C.H.; Chang, M.D.; Tai, K.Y.; Yang, Y.T.; Wang, P.S.; Chen, C.J.; Wang, Y.H.; Lee, S.C.; Wu, C.W.; Juan, L.J. HCMV IE2-mediated inhibition of HAT activity downregulates p53 function. EMBO J. 2004, 23, 2269–2280. [Google Scholar] [CrossRef]
- Rosenke, K.; Samuel, M.A.; McDowell, E.T.; Toerne, M.A.; Fortunato, E.A. An intact sequence-specific DNA-binding domain is required for human cytomegalovirus-mediated sequestration of p53 and may promote in vivo binding to the viral genome during infection. Virology 2006, 348, 19–34. [Google Scholar] [CrossRef]
- Casavant, N.C.; Luo, M.H.; Rosenke, K.; Winegardner, T.; Zurawska, A.; Fortunato, E.A. Potential role for p53 in the permissive life cycle of human cytomegalovirus. J. Virol. 2006, 80, 8390–8401. [Google Scholar] [CrossRef]
- Atherton, S.S.; Newell, C.K.; Kanter, M.Y.; Cousins, S.W. T-Cell Depletion Increases Susceptibility to Murine Cytomegalovirus Retinitis. Investig. Ophthalmol. Vis. Sci. 1992, 33, 3353–3360. [Google Scholar]
- Duan, Y.; Ji, Z.; Atherton, S.S. Dissemination and replication of MCMV after supraciliary inoculation in immunosuppressed BALB/c mice. Investig. Ophthalmol. Vis. Sci. 1994, 35, 1124–1131. [Google Scholar]
- Xu, J.; Liu, X.; Mo, J.; Marshall, B.; Perry, L.; Dong, Z.; Zhang, M. Inflammation and outer blood-retina barrier (BRB) compromise following choroidal murine cytomegalovirus (MCMV) infections. Mol. Vis. 2018, 24, 379–394. [Google Scholar] [PubMed]

| Genes | Primers | |
|---|---|---|
| Ifnα | Forward | AACTCCACCAGCAGACAGTG |
| Reverse | CATCCAGGCGTAGCTGTTGT | |
| Ifnβ | Forward | AGCGCCAAGCATTCAATGAG |
| Reverse | AATCTCTTCCCCACCCCGAA | |
| Ifnγ | Forward | TGCCCAGCAGATCAAGAAGG |
| Reverse | TCAGGGGAAATTCCTGCACC | |
| Caspase12 genotyping | GS(E) | GCCAGGAGGACACATGAAAGAGATC |
| GS(E,T) | CAGCTGTTCCTGGGAATTGGCAATG | |
| Neo | GGGTGGATTAGATAAATGCCTGCTCT |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, X.; Xu, J.; Marshall, B.; Dong, Z.; Smith, S.B.; Zhang, M. The Role of Caspase-12 in Retinal Bystander Cell Death and Innate Immune Responses against MCMV Retinitis. Int. J. Mol. Sci. 2021, 22, 8135. https://doi.org/10.3390/ijms22158135
Zhang X, Xu J, Marshall B, Dong Z, Smith SB, Zhang M. The Role of Caspase-12 in Retinal Bystander Cell Death and Innate Immune Responses against MCMV Retinitis. International Journal of Molecular Sciences. 2021; 22(15):8135. https://doi.org/10.3390/ijms22158135
Chicago/Turabian StyleZhang, Xinyan, Jinxian Xu, Brendan Marshall, Zheng Dong, Sylvia B. Smith, and Ming Zhang. 2021. "The Role of Caspase-12 in Retinal Bystander Cell Death and Innate Immune Responses against MCMV Retinitis" International Journal of Molecular Sciences 22, no. 15: 8135. https://doi.org/10.3390/ijms22158135
APA StyleZhang, X., Xu, J., Marshall, B., Dong, Z., Smith, S. B., & Zhang, M. (2021). The Role of Caspase-12 in Retinal Bystander Cell Death and Innate Immune Responses against MCMV Retinitis. International Journal of Molecular Sciences, 22(15), 8135. https://doi.org/10.3390/ijms22158135






