Extracellular Amyloid Deposits in Alzheimer’s and Creutzfeldt–Jakob Disease: Similar Behavior of Different Proteins?
Abstract
1. Introduction
- Alpha-synuclein in Lewy bodies in Parkinson disease (PD) and dementia with cortical Lewy bodies (DLB) or in oligodendroglial inclusions in multiple systemic atrophy (MSA);
- Phosphorylated TDP-43 in frontotemporal lobar degeneration with TDP-43-positive inclusions (FTLD-TDP) [4];
- Fused in sarcoma (FUS) inclusions in FTDL-FUS [6].
2. Alzheimer’s Disease
2.1. Background of Aβ Plaque Formation
2.2. Theory—Amyloid Cascade Hypothesis
- An occurrence of familial Alzheimer’s disease (fAD) in patients carrying an autosomal dominant mutation in genes encoding APP.
- A higher fAD incidence was seen in families carrying the presenilin 1 (PSEN1) and presenilin 2 (PSEN2) mutations, which are the catalytic components of γ-secretase [35]. Most mutations in APP or PSEN1/PSEN2 alter APP proteolysis and result in increased production of the longer form of Aβ (i.e., Aβ42) [36].
- Early-onset Alzheimer disease (EOAD) is manifested in patients with Down syndrome. The trisomy of chromosome 21, on which the gene for APP is located, logically leads to a triplicate of the APP gene. Many patients suffering from Down syndrome develop AD at an early age. The presence of Aβ plaques in these patients is often described in childhood [37], and the formation of neurofibrillary tangles occurs at about the age of 40 [38]. Thence, Down syndrome is considered to be the most significant genetic risk factor for the development of AD [39].
- There are patients having numerous plaques (or even fulfilling the neuropathological criteria for AD) but have no clinical signs of cognitive impairment [44].
- Conversely, some mouse models of AD show memory deficits before the development of Aβ plaques [45].
- While senile plaques appear first in the frontal cortex and then spread beyond the cerebral cortex to the hippocampus and beyond, neurofibrillary tangles initially develop in the limbic system [36]. To this day, the mutual relationship between these two neuropathological hallmarks is not fully understood.
2.3. Morphological Classification of Senile Plaques (SP)
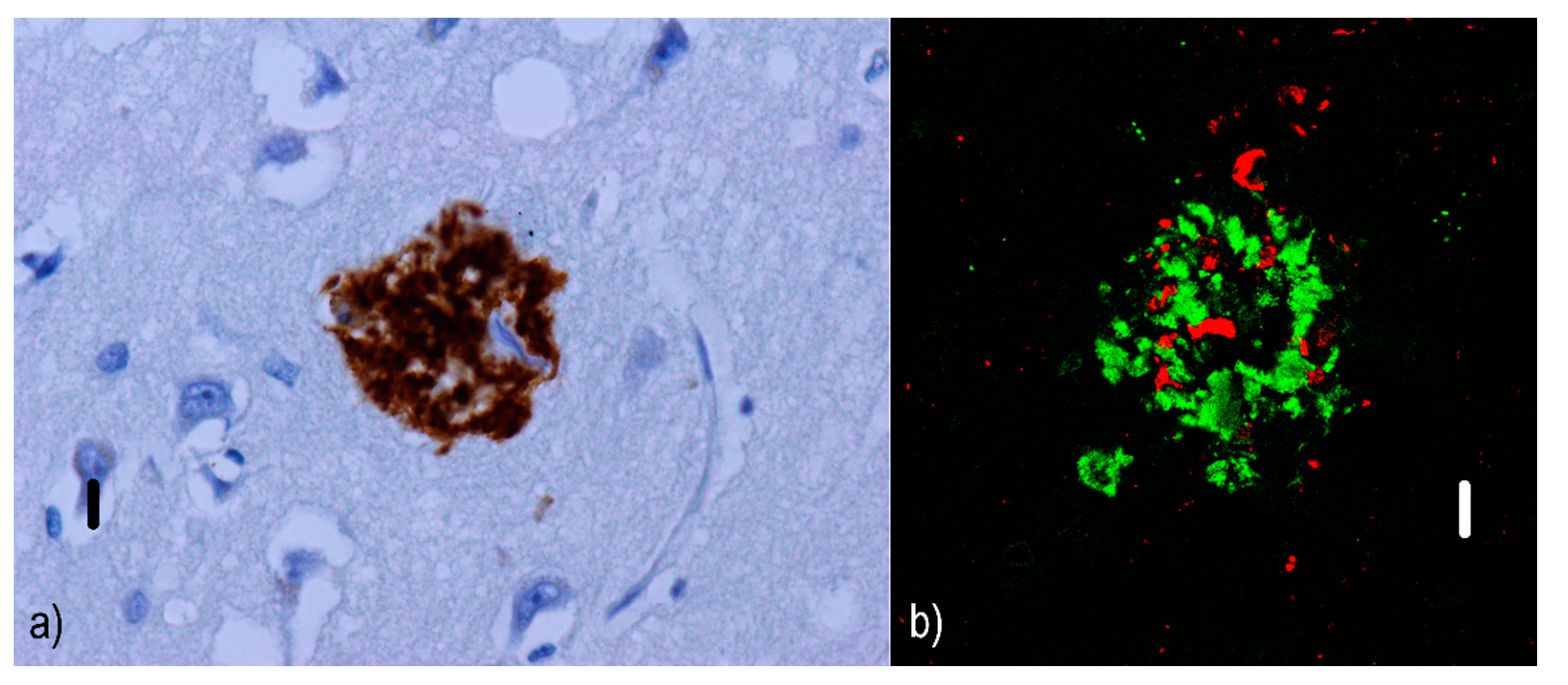
- Diffuse/pre-amyloid plaques (Figure 1) that are predominantly 10–20 µm [48] amorphous amyloid deposits with ill-defined contours [46] and lacking dystrophic neurites [49]. Diffuse plaques are not associated with a glial response [50] or synaptic loss; hence, they are not sufficient for a neuropathological diagnosis of AD. Moreover, diffuse plaques are commonly found in the elderly without signs of cognitive decline [51]. They are evident with silver staining, but invisible with Congo red [52] or thioflavin [53].
- Two subtypes of neuritic plaques can be distinguished.
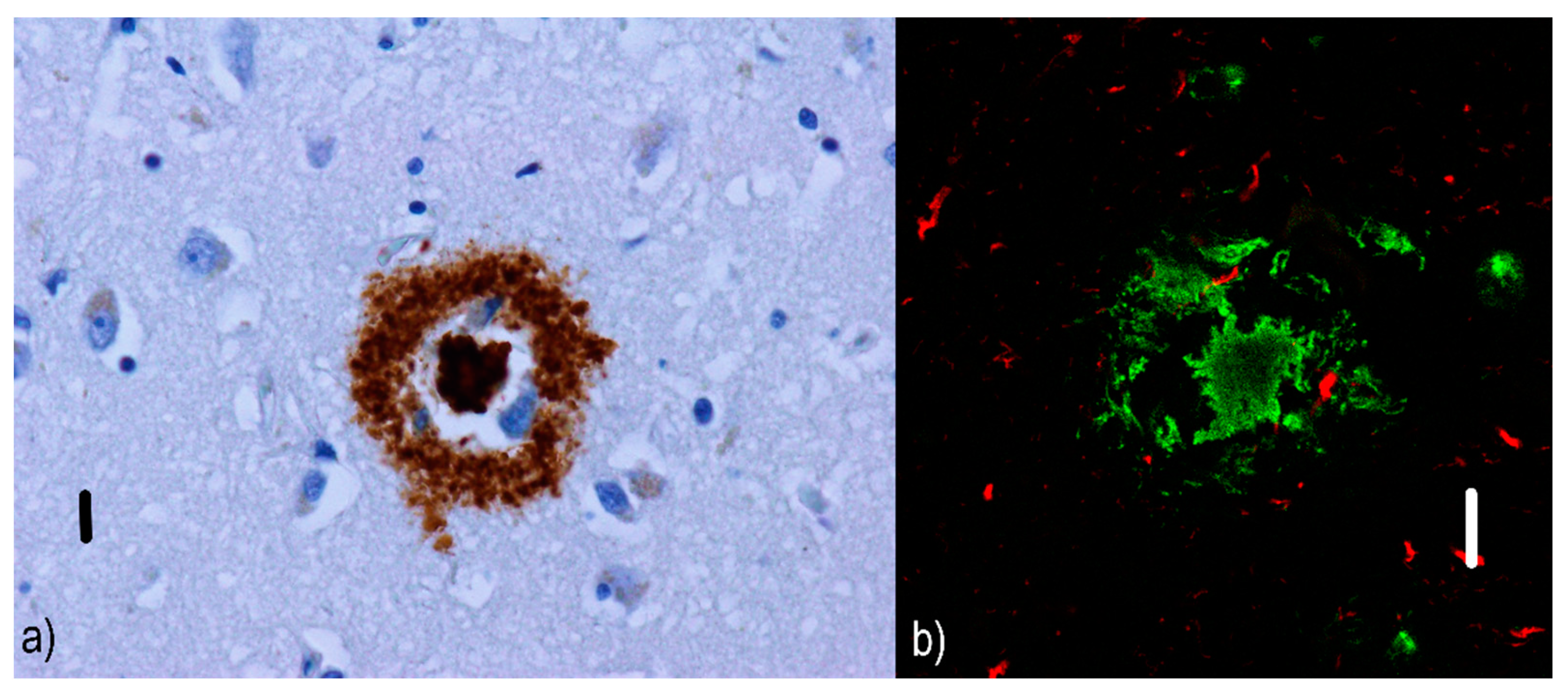
- Non-cored/primitive/immature neuritic plaques (see Figure 2) are oval or spherical structures containing Aβ and altered neurites, 20–60 µm in diameter and lacking a dense Aβ region in the central part [54]; they are also associated with astrocytic and glial responses. They are reported to occur in older AD patients [55]. Similar to diffuse plaques, they do not stain with Congo red since they do not contain Aβ in the beta-sheet conformation [56].
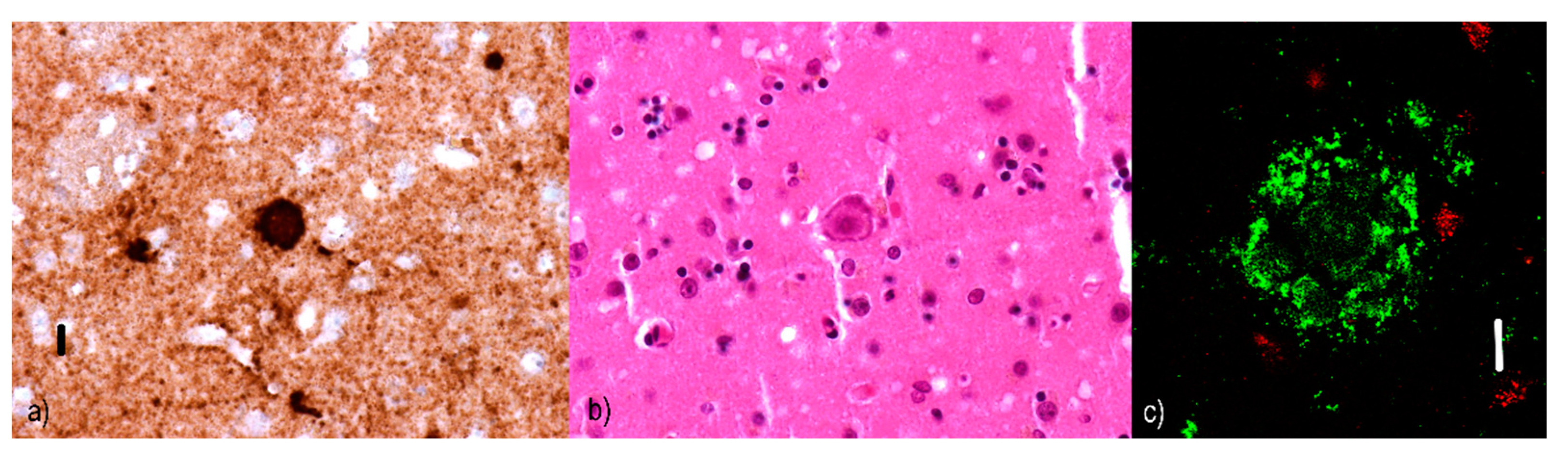
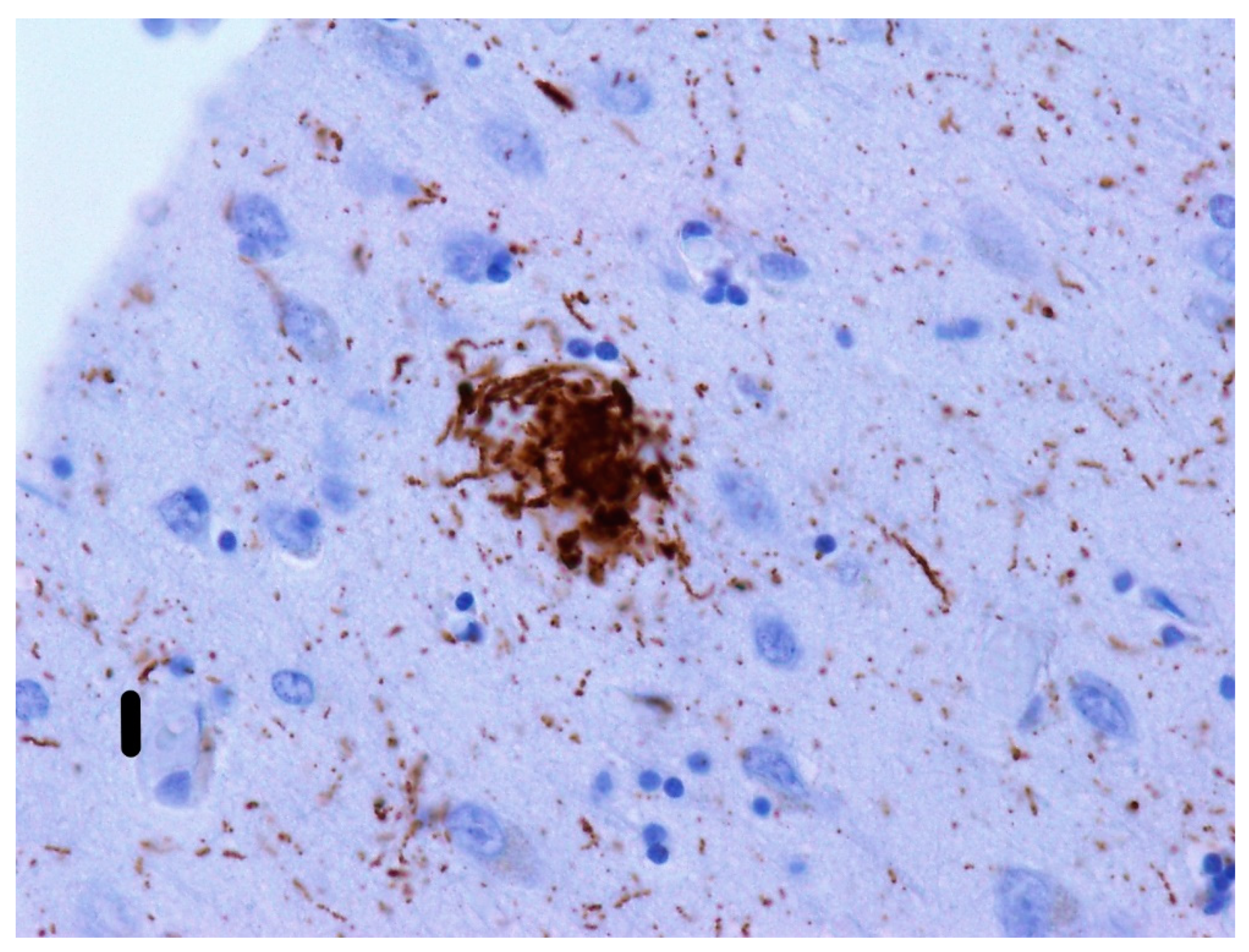
- Cored/classic/dense/mature/focal neuritic plaques (Figure 3) are 20–60 µm [53] compact cores encircled by fibrillar Aβ deposits [51]. Tau-positive dystrophic neurites [57], reactive astrocytes, and activated microglia [58,59] are found in the vicinity. Due to its relation to neuronal loss and its association with cognitive decline [60,61], these plaques are a basis for an AD diagnosis [62]. They can be visualized with silver staining [63], Congo red [64], and thioflavin [57].
2.4. Dystrophic Neurites as a Component of Aβ Plaques
2.5. The Molecular Composition of Aβ Plaques
- According to Armstrong [70], non-cored/primitive/immature neuritic plaques additionally contain both free and conjugated ubiquitin, paired helical filament antigen (PHF-antigen), phosphorylated tau protein, and numerous immunoreactive neurites.
- Cored/classic/dense/mature/focal neuritic plaques consist of an Aβ42 core and a ring of alpha-synuclein. In addition to Aβ42, they contain Aβ40, complement proteins, immunoglobulins, and apolipoproteins D [76] and E. Due to the secondary binding to Aβ, zinc, copper [77], or aluminum [78] may also be part of the core, with aluminum having the lowest affinity [79]. Chromogranin, interleukine-6 [80], or catecholamine-positive neurites are constituents of the ring.
2.6. Laminar Distribution of Aβ Plaques
3. Prion Diseases
3.1. Molecular Background and the Composition of PrP-Amyloid Plaques
3.2. Kuru
3.3. Creutzfeldt–Jakob Disease
- MM1 subtype: synaptic and perivacuolar positivity, although cases with plaques in the white matter are so rarely encountered, we will not mention them in more detail [136].
- MM2
- -
- Cortical subtype: perivacuolar positivity in all cortical layers;
- -
- Thalamic subtype: fewer plaques (which are usually described as coarse) [137]
- MV1 subtype: synaptic and perivacuolar positivity;
- MV2 subtype: distinctive “kuru-like” plaques in the cerebellum and perineuronal positivity in the cerebral cortex;
- VV1 subtype: characterized by punctate synaptic positivity in the cerebral cortex;
- VV2 subtype: perineuronal, with numerous plaque-like areas and some synaptic PrP positivity in the cerebral cortex [138].
3.4. Gerstmann–Sträussler–Scheinker Syndrome
3.5. Summary of Morphological Types of PrP Plaques in TSEs
- Unicentric/“kuru”/”kuru-like”/stellate plaques (Figure 5) are up to 30 µm [132] deposits consisting of a dense star-shaped core with thin amyloid bundles radiating into the periphery [156]. In kuru disease, the average plaque size is reported to be between 20–60 µm [117]. These plaques are surrounded by astrocytic processes that have been extensively invaded by microglia [157], although dystrophic neurites are unusual [156]. However, some studies report tau-immunoreactivity around “kuru-like” plaques [158]. “Kuru-like” plaques are present in 10–15% of sCJD patients [156], all of whom carry the MV2 polymorphism at codon 129 [138]. In CJD cases, they occur mostly in the molecular layer of the cerebellum and the Purkinje cell layer [140]. For kuru disease, typical locations include the granular cell layer of the cerebellum, the basal ganglia, thalamus, and cerebral cortex [158]. These plaques are visible with hematoxylin-eosin staining [90], which distinguishes them from plaque-like structures.
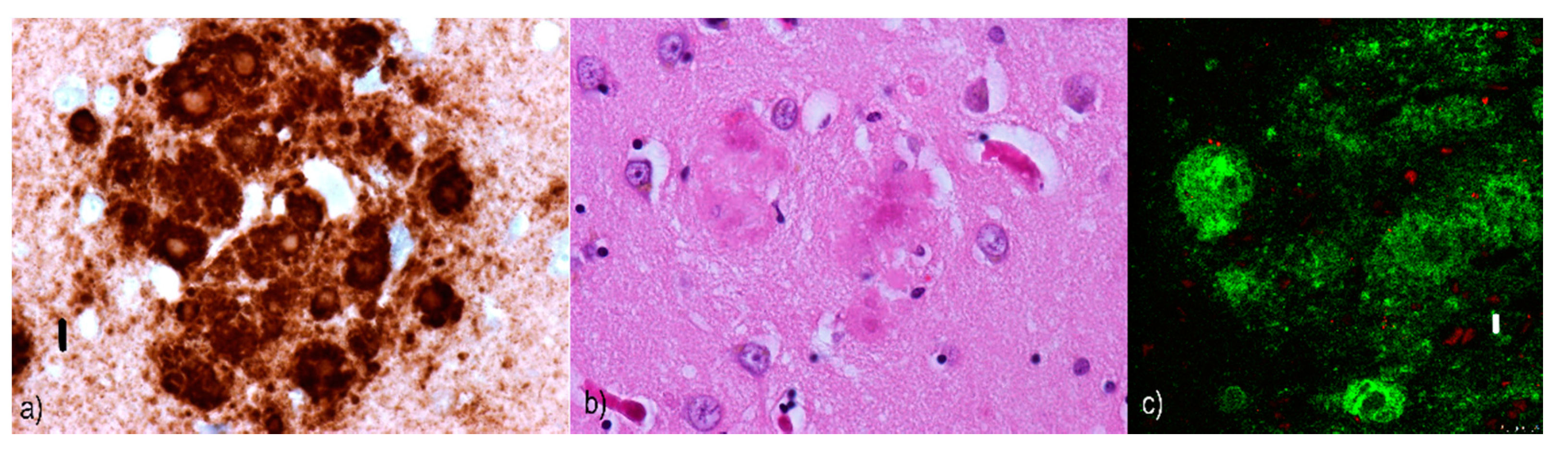
- Daisy/florid plaques measure up to 200 µm [132] and consist of a PrP-amyloid core surrounded by a “ring” of spongiform changes. Radiating fibrils are organized into thick structures, which stand in contrast to the thin structures seen in “kuru-like” plaques [158]. There are numerous tau-immunoreactive dystrophic neurites in the vicinity that distinguish them from “kuru-like” plaques. Moreover, Hirano bodies (in the processes around florid plaques) can sometimes also be found [158]. These plaques are characteristic [159], although not specific [160] for vCJD. They can occur anywhere in the cerebral cortex but are generally found occipitally and in the cerebellar molecular layer [161]. Florid plaques are visible when stained with hematoxylin-eosin [162].
- Multicentric plaques (see Figure 6) are formations up to 1500 µm [132] and are composed of many cores of different sizes that have merged. Unlike “kuru-like” plaques, they are characterized by the presence of dystrophic neurites [140]. Dystrophic neurites sometimes contain paired helical filaments (PHFs) identical to those seen in the dystrophic neurites of AD patients [163]. These larger cores tend to be surrounded by smaller amyloid deposits [156]. Like the previously mentioned plaques, they can be observed with hematoxylin-eosin staining [164].
- All of these diseases are based on a perturbance of proteins having physiological functions on the neuritic membrane to which they are anchored. Physiologically, they have a neuroprotective function and are able to interact with a number of other agents.
- They are also similar to each other in the resistance of these extracellular aggregates to degradation by endogenous proteases.
- In both AD and TSEs, extracellular aggregates may form not only compact structures such as plaques but also diffuse extracellular deposits.
- For all mentioned diseases, extracellular deposits are mainly found in the cortical areas or in the central grey matter. Their presence in white matter is possible but exceedingly rare in TSEs and absolutely unheard of in Alzheimer’s disease.
- When forming plaques, they usually contain dystrophic neurites with similar immunohistochemical characteristics in both AD and TSEs. The neuritic morphology can vary from case to case.
- The most toxic and neuronal death-inducing forms are oligomeric assemblies of both Aβ and PrP.
- While Aβ has thread-like morphology, PrP tends to be more lumpy or globular.
- In AD, plaques probably mature, i.e., the individual types probably transform from one to the next. Nothing like “plaque maturation” has been recorded in prionoses.
- Especially in GSS, plaque fusion and the formation of multicentric structures are distinctive. No similar trends are seen in AD.
- For prionoses, different appearances, locations, and frequencies of extracellular aggregates are reported depending on the form and subtype. In AD, neuropathological differences between early and late-onset or sporadic and familial variants have never been described.
- In TSEs, PrP deposits may be found intracellularly in some patients, while the occurrence of Aβ is strictly extracellular.
- In AD and prionoses, there is a different trend relative to the spread of deposits within the brain. In AD, we distinguish five phases, with phase 1 being characterized by the presence of Aβ deposits limited to neocortical areas. During phase 2, the archicortical and paleocortical (together called allocortical) regions are affected. This is followed by a spread to the striatum and subcortical nuclei in general during phase 3. Brainstem involvement defines phase 4, and the involvement of the cerebellum defines phase 5 [165]. In prionoses, no stages are distinguishable since there is no characteristic spreading pattern over time.
4. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Salardini, A. An Overview of Primary Dementias as Clinicopathological Entities. Semin. Neurol. 2019, 39, 153–166. [Google Scholar] [CrossRef]
- Braak, H.; Alafuzoff, I.; Arzberger, T.; Kretzschmar, H.; Del Tredici, K. Staging of Alzheimer disease-associated neurofibrillary pathology using paraffin sections and immunocytochemistry. Acta Neuropathol. 2006, 112, 389–404. [Google Scholar] [CrossRef] [PubMed]
- Dickson, D.W.; Kouri, N.; Murray, M.E.; Josephs, K.A. Neuropathology of frontotemporal lobar degeneration-Tau (FTLD-Tau). J. Mol. Neurosci. 2011, 45, 384–389. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, I.R.; Neumann, M. Molecular neuropathology of frontotemporal dementia: Insights into disease mechanisms from postmortem studies. J. Neurochem. 2016, 138, 54–70. [Google Scholar] [CrossRef] [PubMed]
- Jellinger, K.A. Neuropathology of Dementia Disorders. J. Alzheimers Dis. Parkinsonism. 2014, 4, 135. [Google Scholar] [CrossRef]
- Chornenka, K.; Hirsch-Reinshagen, V.; Perez-Rosendahl, M.; Feldman, H.; Segal-Gidan, F.; Vinters, H.V.; MacKenzie, I.R. Expanding the Phenotype of Frontotemporal Lobar Degeneration With FUS-Positive Pathology (FTLD-FUS). J. Neuropathol. Exp. Neurol. 2020, 79, 809–812. [Google Scholar] [CrossRef]
- Thal, D.R.; Fändrich, M. Protein aggregation in Alzheimer’s disease: Aβ and τ and their potential roles in the pathogenesis of AD. Acta Neuropathol. 2015, 129, 163–165. [Google Scholar] [CrossRef]
- Kovacs, G.G.; Budka, H. Prion diseases: From protein to cell pathology. Am. J. Pathol. 2008, 172, 555–565. [Google Scholar] [CrossRef]
- Elhaddaoui, A.; Pigorsch, E.; Delacourte, A.; Turrell, S. Competition of congo red and thioflavin S binding to amyloid sites in Alzheimer’s diseased tissue. Biospectroscopy 1995, 1, 351–356. [Google Scholar] [CrossRef]
- Schultz, C.; Del Tredici, K. Neuropathology of Alzheimer’s Disease. Alzheimers Disease Curr. Clin. Neurol. 2004, 21–31. [Google Scholar] [CrossRef]
- Hebert, L.E.; Weuve, J.; Scherr, P.A.; Evans, D.A. Alzheimer disease in the United States (2010–2050) estimated using the 2010 Census. Neurology 2013, 80, 1778–1783. [Google Scholar] [CrossRef] [PubMed]
- Montine, T.J.; Phelps, C.H.; Beach, T.G.; Bigio, E.H.; Cairns, N.J.; Dickson, D.W.; Duyckaerts, C.; Frosch, M.P.; Masliah, E.; Mirra, S.S.; et al. National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease: A practical approach. Acta Neuropathol. 2012, 123, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Hyman, B.T.; Phelps, C.H.; Beach, T.G.; Bigio, E.H.; Cairns, N.J.; Carrillo, M.C.; Dickson, D.W.; Duyckaerts, C.; Frosch, M.P.; Masliah, E.; et al. National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease. Alzheimers Dement. 2012, 8, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Mirra, S.S.; Heyman, A.; McKeel, D.; Sumi, S.M.; Crain, B.J.; Brownlee, L.M.; Vogel, F.S.; Hughes, J.P.; Van Belle, G.; Berg, L.; et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part II. Standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology 1991, 41, 479–486. [Google Scholar] [CrossRef]
- Ugalde, C.L.; Finkelstein, D.I.; Lawson, V.A.; Hill, A.F. Pathogenic mechanisms of prion protein, amyloid-β and α-synuclein misfolding: The prion concept and neurotoxicity of protein oligomers. J. Neurochem. 2016, 139, 162–180. [Google Scholar] [CrossRef]
- Lesné, S.; Koh, M.T.; Kotilinek, L.; Kayed, R.; Glabe, C.G.; Yang, A.; Gallagher, M.; Ashe, K.H. A specific amyloid-beta protein assembly in the brain impairs memory. Nature 2006, 440, 352–357. [Google Scholar] [CrossRef]
- Blessed, G.; Tomlinson, B.E.; Roth, M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br. J. Psychiatry. 1968, 114, 797–811. [Google Scholar] [CrossRef]
- Savonenko, A.V.; Melnikova, T.; Won, P.C. Alzheimer disease. In Neurobiology of Brain Disorders, 1st ed.; Zigmund, M.J., Coyle, J.T., Rowland, L.P., Eds.; Academic Press: Cambridge, MA, USA, 2014; pp. 321–338. [Google Scholar]
- O’Brien, R.J.; Wong, P.C. Amyloid precursor protein processing and Alzheimer’s disease. Annu. Rev. Neurosci. 2011, 34, 185–204. [Google Scholar] [CrossRef]
- Bush, A.I.; Multhaup, G.; Moir, R.D.; Williamson, T.G.; Small, D.H.; Rumble, B.; Pollwein, P.; Beyreuther, K.; Masters, C.L. A novel zinc(II) binding site modulates the function of the beta A4 amyloid protein precursor of Alzheimer’s disease. J. Biol. Chem. 1993, 268, 16109–16112. [Google Scholar]
- Multhaup, G.; Schlicksupp, A.; Hesse, L.; Beher, D.; Ruppert, T.; Masters, C.L.; Beyreuther, K. The amyloid precursor protein of Alzheimer’s disease in the reduction of copper(II) to copper(I). Science 1996, 271, 1406–1409. [Google Scholar] [CrossRef]
- Smith-Swintosky, V.L.; Pettigrew, L.C.; Craddock, S.D.; Culwell, A.R.; Rydel, R.E.; Mattson, M.P. Secreted forms of beta-amyloid precursor protein protect against ischemic brain injury. J. Neurochem. 1994, 63, 781–784. [Google Scholar] [CrossRef] [PubMed]
- Chow, V.W.; Mattson, M.P.; Wong, P.C.; Gleichmann, M. An overview of APP processing enzymes and products. Neuro Mol. Med. 2010, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Knowles, T.P.J.; Vendruscolo, M.; Dobson, C.M. The amyloid state and its association with protein misfolding diseases. Nat. Rev. Mol. Cell Biol. 2014, 15, 384–396. [Google Scholar] [CrossRef] [PubMed]
- Plant, L.D.; Boyle, J.P.; Smith, I.F.; Peers, C.; Pearson, H.A. The production of amyloid beta peptide is a critical requirement for the viability of central neurons. J. Neurosci. 2003, 23, 5531–5535. [Google Scholar] [CrossRef] [PubMed]
- Gravina, S.A.; Ho, L.; Eckman, C.B.; Long, K.E.; Otvos, L.; Younkin, L.H.; Suzuki, N.; Younkin, S.G. Amyloid beta protein (A beta) in Alzheimer’s disease brain. Biochemical and immunocytochemical analysis with antibodies specific for forms ending at A beta 40 or A beta 42(43). J. Biol. Chem. 1995, 270, 7013–7016. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.; Papayannopoulos, I.; Styles, J.; Bobin, S.; Lin, Y.; Biemann, K.; Iqbal, K. Peptide compositions of the cerebrovascular and senile plaque core amyloid deposits of Alzheimer’s disease. Arch. Biochem. Biophys. 1993, 301, 41–52. [Google Scholar] [CrossRef]
- Roher, A.E.; Lowenson, J.D.; Clarke, S.; Wolkow, C.; Wang, R.O.N.G.; Cotter, R.J.; Reardon, I.M.; Zürcher-Neely, H.A.; Heinrikson, R.L.; Ball, M.J. Structural alterations in the peptide backbone of β-amyloid core protein may account for its deposition and stability in Alzheimer’s disease. J. Biol. Chem. 1993, 268, 3072–3073. [Google Scholar]
- Vonsattel, J.P.G.; Myers, R.H.; Hedley-Whyte, E.T.; Ropper, A.H.; Bird, E.D.; Richardson, E.P. Cerebral amyloid angiopathy without and with cerebral hemorrhages: A comparative histological study. Ann. Neurol. 1991, 30, 637–649. [Google Scholar] [CrossRef]
- Bernstein, S.L.; Dupuis, N.F.; Lazo, N.D.; Wyttenbach, T.; Condron, M.M.; Bitan, G.; Teplow, D.B.; Shea, J.-E.; Ruotolo, B.T.; Robinson, C.V.; et al. Amyloid-β protein oligomerization and the importance of tetramers and dodecamers in the aetiology of Alzheimer’s disease. Nat. Chem. 2009, 1, 326–331. [Google Scholar] [CrossRef]
- Gunther, E.C.; Strittmatter, S.M. Beta-amyloid oligomers and cellular prion protein in Alzheimer’s disease. J. Mol. Med. 2009, 88, 331–338. [Google Scholar] [CrossRef][Green Version]
- Haass, C.; Selkoe, D.J. Soluble protein oligomers in neurodegeneration: Lessons from the Alzheimer’s amyloid beta-peptide. Nat. Rev. Mol. Cell Biol. 2007, 8, 101–112. [Google Scholar] [CrossRef] [PubMed]
- Walsh, D.M.; Klyubin, I.; Fadeeva, J.V.; Cullen, W.K.; Anwyl, R.; Wolfe, M.S.; Rowan, M.J.; Selkoe, D.J. Naturally secreted oligomers of amyloid beta protein potently inhibit hippocampal long-term potentiation in vivo. Nature 2002, 416, 535–539. [Google Scholar] [CrossRef] [PubMed]
- Hardy, J.A.; Higgins, G.A. Alzheimer’s disease: The amyloid cascade hypothesis. Science 1992, 256, 184–185. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zhang, M.; Cai, F.; Song, W. Biological function of Presenilin and its role in AD pathogenesis. Transl. Neurodegener. 2013, 2, 15. [Google Scholar] [CrossRef] [PubMed]
- Pimplikar, S.W. Reassessing the amyloid cascade hypothesis of Alzheimer’s disease. Int. J. Biochem. Cell Biol. 2009, 41, 1261–1268. [Google Scholar] [CrossRef]
- Leverenz, J.; Raskind, M.A. Early amyloid deposition in the medial temporal lobe of young Down syndrome patients: A regional quantitative analysis. Exp. Neurol. 1998, 150, 296–304. [Google Scholar] [CrossRef]
- Lemere, C.A.; Blusztajn, J.K.; Yamaguchi, H.; Wisniewski, T.; Saido, T.C.; Selkoe, D.J. Sequence of deposition of heterogeneous amyloid beta-peptides and APO E in Down syndrome: Implications for initial events in amyloid plaque formation. Neurobiol. Dis. 1996, 3, 16–32. [Google Scholar] [CrossRef]
- Wiseman, F.K.; Al-Janabi, T.; Hardy, J.; Ferguson-Smith, A.C.; Nizetic, D.; Tybulewicz, V.L.J.; Fisher, E.M.C.; Strydom, A. A genetic cause of Alzheimer disease: Mechanistic insights from Down syndrome. Nat. Rev. Neurosci. 2015, 16, 564–574. [Google Scholar] [CrossRef]
- Morris, G.P.; Clark, I.A.; Vissel, B. Inconsistencies and controversies surrounding the amyloid hypothesis of Alzheimer’s disease. Acta Neuropathol. Commun. 2014, 2, 135. [Google Scholar] [CrossRef]
- Morris, G.P.; Clark, I.; Vissel, B. Questions concerning the role of amyloid-β in the definition, aetiology and diagnosis of Alzheimer’s disease. Acta Neuropathol. 2018, 136, 663–689. [Google Scholar] [CrossRef]
- Clark, I.A.; Vissel, B. Amyloid beta: One of three danger-associated molecules that are secondary inducers of the proinflammatory cytokines that mediate Alzheimer’s disease. Br. J. Pharmacol. 2015, 172, 3714–3727. [Google Scholar] [CrossRef] [PubMed]
- Clark, I.A.; Vissel, B. Therapeutic implications of how TNF links apolipoprotein E, phosphorylated tau, α-synuclein, amyloid-β and insulin resistance in neurodegenerative diseases. Br. J. Pharmacol. 2018, 175, 3859–3875. [Google Scholar] [CrossRef] [PubMed]
- Nelson, P.T.; Braak, H.; Markesbery, W.R. Neuropathology and cognitive impairment in Alzheimer disease: A complex but coherent relationship. J. Neuropathol. Exp. Neurol. 2009, 68, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Lesné, S.; Kotilinek, L.; Ashe, K.H. Plaque-bearing mice with reduced levels of oligomeric amyloid-beta assemblies have intact memory function. Neuroscience 2008, 151, 745–749. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Pozo, A.; Frosch, M.P.; Masliah, E.; Hyman, B.T. Neuropathological alterations in Alzheimer disease. Cold Spring Harb. Perspect. Med. 2011, 1, a006189. [Google Scholar] [CrossRef]
- Querol-Vilaseca, M.; Colom-Cadena, M.; Pegueroles, J.; Nuñez-Llaves, R.; Luque-Cabecerans, J.; Muñoz-Llahuna, L.; Andilla, J.; Belbin, O.; Spires-Jones, T.; Gelpi, E.; et al. Nanoscale structure of amyloid-β plaques in Alzheimer’s disease. Sci. Rep. 2019, 9, 5181. [Google Scholar] [CrossRef]
- Chuen-Chung, C.R. Advanced Understanding of Neurodegenerative Diseases Hardcover; IntechOpen: London, UK, 2011; p. 54. ISBN 978-9533075297. [Google Scholar] [CrossRef]
- Ringman, J.M.; Network, D.I.A.; Goate, A.; Masters, C.L.; Cairns, N.J.; Danek, A.; Graff-Radford, N.; Ghetti, B.; Morris, J.C. Dominantly Inherited Alzheimer Network. Genetic heterogeneity in Alzheimer disease and implications for treatment strategies. Curr. Neurol. Neurosci. Rep. 2014, 14, 499. [Google Scholar] [CrossRef]
- Cabranes, J.A.; Anein, I.; Barros-Loscertales, A.; Campos, S.; Canonico, V.; Fernandez, C.; Munoz, M.C.; Antonello, R.M.; Belloch-Ugarte, V.; Avila, C.; et al. Alzheimer’s Disease Research Trends, 1st ed.; Chan, A.P., Ed.; Nova Science Publishers Inc.: New York, NY, USA, 2008; p. 324. ISBN 9781600217128. [Google Scholar]
- Masliah, E.; Terry, R.D.; Mallory, M.; Alford, M.; Hansen, L.A. Diffuse plaques do not accentuate synapse loss in Alzheimer’s disease. Am. J. Pathol. 1990, 137, 1293–1297. [Google Scholar]
- Allen, S.J. Neurobiology of Alzheimer’s Disease, 3rd ed.; Dawbarn, D., Ed.; Oxford University Press: Oxford, UK, 2007; ISBN 9780198566618. [Google Scholar]
- Bussière, T.; Bard, F.; Barbour, R.; Grajeda, H.; Guido, T.; Khan, K.; Schenk, D.; Games, D.; Seubert, P.; Buttini, M. Morphological Characterization of Thioflavin-S-Positive Amyloid Plaques in Transgenic Alzheimer Mice and Effect of Passive Aβ Immunotherapy on Their Clearance. Am. J. Pathol. 2004, 165, 987–995. [Google Scholar] [CrossRef]
- Probst, A.; Brunnschweiler, H.; Lautenschlager, C.; Ulrich, J. A special type of senile plaque, possibly an initial stage. Acta Neuropathol. 1987, 74, 133–141. [Google Scholar] [CrossRef]
- Tseng, B.P.; Esler, W.P.; Clish, C.B.; Stimson, E.R.; Ghilardi, J.R.; Vinters, H.V.; Mantyh, P.W.; Lee, J.P.; Maggio, J.E. Deposition of monomeric, not oligomeric, Abeta mediates growth of Alzheimer’s disease amyloid plaques in human brain preparations. Biochemistry 1999, 38, 10424–10431. [Google Scholar] [CrossRef] [PubMed]
- Duckett, S.; De La Torre, J.C. Pathology of the Aging Human Nervous System, 2nd ed.; Oxford University Press: Oxford, UK, 2001; p. 161. ISBN 0195130693. [Google Scholar]
- DeTure, M.A.; Dickson, D.W. The neuropathological diagnosis of Alzheimer’s disease. Mol, Neurodegener. 2019, 14, 32. [Google Scholar] [CrossRef]
- Dickson, T.C.; Vickers, J.C. The morphological phenotype of amyloid-beta deposits and associated neuritic change in Alzheimer’s disease. Neuroscience 2001, 105, 99–107. [Google Scholar] [CrossRef]
- Itagaki, S.; McGeer, P.; Akiyama, H.; Zhu, S.; Selkoe, D. Relationship of microglia and astrocytes to amyloid deposits of Alzheimer disease. J. Neuroimmunol. 1989, 24, 173–182. [Google Scholar] [CrossRef]
- Malek-Ahmadi, M.; Perez, S.E.; Chen, K.; Mufson, E.J. Neuritic and diffuse plaque associations with memory in non-cognitively impaired elderly. J. Alzheimers Dis. 2016, 53, 1641–1652. [Google Scholar] [CrossRef] [PubMed]
- Knowles, R.B.; Wyart, C.; Buldyrev, S.V.; Cruz, L.; Urbanc, B.; Hasselmo, M.E.; Stanley, H.E.; Hyman, B.T. Plaque-induced neurite abnormalities: Implications for disruption of neural networks in Alzheimer’s disease. Proc. Natl. Acad. Sci. USA 1999, 96, 5274–5279. [Google Scholar] [CrossRef]
- Seth, L.S.; Louis, D.N.; Ellison, D.W. Greenfield’s Neuropathology, 8th ed.; Hodder Education Publishers: London, UK, 2008; p. 2400. ISBN 978-0340906811. [Google Scholar]
- Perry, A.; Brat, D. Practical Surgical Neuropathology: A Diagnostic Approach, 2nd ed.; Elsevier Health Sciences: Philadelphia, PA, USA, 2017; p. 752. [Google Scholar]
- Baumann, B.; Woehrer, A.; Ricken, G.; Augustin, M.; Mitter, C.; Pircher, M.; Kovacs, G.G.; Hitzenberger, C.K. Visualization of neuritic plaques in Alzheimer’s disease by polarization-sensitive optical coherence microscopy. Sci. Rep. 2017, 7, 43477. [Google Scholar] [CrossRef]
- Perl, D.P. Neuropathology of Alzheimer’s disease. Mt. Sinai J. Med. 2010, 77, 32–42. [Google Scholar] [CrossRef]
- Thal, D.R.; Capetillo-Zarate, E.; Del Tredici, K.; Braak, H. The development of amyloid beta protein deposits in the aged brain. Sci. Aging Knowl. Environ. 2006, 2006, re1. [Google Scholar] [CrossRef]
- Yasuhara, O.; Kawamata, T.; Aimi, Y.; McGeer, E.G.; McGeer, P.L. Two types of dystrophic neurites in senile plaques of Alzheimer disease and elderly non-demented cases. Neurosci. Lett. 1994, 171, 73–76. [Google Scholar] [CrossRef]
- Valyi-Nagy, T. Dementias in Neuropathology: A Reference Text of CNS Pathology, 3rd ed.; Ellison, D., Love, S., Chimelli, L.M.C., Harding, B., Lowe, J., Vinters, H.V., Eds.; Elsevier Publishing: Philadephia, PA, USA, 2012; pp. 614–617. [Google Scholar]
- Jankovska, N.; Olejar, T.; Kukal, J.; Matej, R. Different Morphology of Neuritic Plaques in the Archicortex of Alzheimer Disease with Comorbid Synucleinopathy: A Pilot Study. Curr. Alzheimer Res. 2020. Epub ahead of print. [Google Scholar] [CrossRef]
- Armstrong, R. The molecular biology of senile plaques and neurofibrillary tangles in Alzheimer’s disease. Stage of PublicationFolia Neuro Pathol. 2009, 47, 289–299. [Google Scholar]
- Yamaguchi, H.; Ishiguro, K.; Sugihara, S.; Nakazato, Y.; Kawarabayashi, T.; Sun, X.Y. Presence of apolipoprotein E on extracellular neurofibrillary tangles and on meningeal blood vessels precedes the Alzheimer β-amyloid deposition. Acta Neuropathol. 1994, 88, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Eikelenboom, P.; Zhan, S.-S.; Van Gool, W.A.; Allsop, D. Inflammatory mechanisms in Alzheimer’s disease. Trends Pharmacol. Sci. 1994, 15, 447–450. [Google Scholar] [CrossRef]
- Loeffler, D.A.; Camp, D.M.; Bennett, D.A. Plaque complement activation and cognitive loss in Alzheimer’s disease. J. Neuro Inflamm. 2008, 5, 9. [Google Scholar] [CrossRef] [PubMed]
- Verga, L.; Frangione, B.; Tagliavini, F.; Giaccone, G.; Migheli, A.; Bugiani, O. Alzheimer’s and Down’s patients: Cerebral preamyloid deposits differ ultrastructurally and histochemically from the amyloid of senile plaques. Neurosci. Lett. 1989, 105, 294–299. [Google Scholar] [CrossRef]
- Snow, A.D.; Sekiguchi, R.T.; Nochlin, D.; Kalaria, R.N.; Kimata, K. Heparan sulfate proteoglycan in diffuse plaques of hippocampus but not of cerebellum in Alzheimer’s disease brain. Am. J. Pathol. 1994, 144, 337–347. [Google Scholar] [PubMed]
- Desai, P.P.; Ikonomovic, M.D.; Abrahamson, E.E.; Hamilton, R.L.; Isanski, B.A.; Hope, C.E.; Klunk, W.E.; DeKosky, S.T.; Kamboh, M.I. Apolipoprotein D is a component of compact but not diffuse amyloid-beta plaques in Alzheimer’s disease temporal cortex. Neurobiol. Dis. 2005, 20, 574–582. [Google Scholar] [CrossRef]
- Atwood, C.S.; Obrenovitch, M.E.; Liu, T.; Chan, H.; Perry, G.; Smith, M.A.; Martins, R.N. Amyloid-beta: A chameleon walking in two worlds: A review of the trophic and toxic properties of amyloid-β. Brain Res. Rev. 2004, 43, 1–6. [Google Scholar] [CrossRef]
- Mann, D.M.A.; Younis, N.; Jones, D.; Stoddart, R.W. The time course of pathological events in Down’s syndrome with particular reference to the involvement of microglial cells and deposits of b/A4. Neurodegeneration 1992, 1, 201–215. [Google Scholar]
- Bush, A.I.; Pettingell, W.H.; Multhaup, G.; Paradis, M.D.; Vonsattel, J.P.; Gusella, J.F.; Beyreuther, K.; Masters, C.L.; Tanzi, R.E. Rapid induction of Alzheimer A beta amyloid formation by zinc. Science 1994, 265, 1464–1467. [Google Scholar] [CrossRef]
- Shalit, F.; Sredni, B.; Stern, L.; Kott, E.; Huberman, M. Elevated interleukin-6 secretion levels by mononuclear cells of Alzheimer’s patients. Neurosci. Lett. 1994, 174, 130–132. [Google Scholar] [CrossRef]
- Vogt, B. Cingulate Neurobiology and Disease, 3rd ed.; Oxford University Press: Oxford, UK, 2009; ISBN 978-0198566960. [Google Scholar]
- Bahmanyar, S.; Higgins, G.A.; Goldgaber, D. Localization of amyloid β protein messenger RNA in brains from patients with Alzheimer’s disease. Science 1987, 237, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.A. Diffuse β-amyloid (Aβ) deposits and neurons: In situ secretion or diffusion of Aβ? Alzheimer Rep. 2001, 3, 289–294. [Google Scholar]
- Armstrong, R.A. Laminar distribution of β-amyloid (Aβ) peptide deposits in the frontal lobe in familial and sporadic Alzheimer’s disease. Folia Neuropathol. 2015, 53, 15–23. [Google Scholar] [CrossRef]
- Imran, M.; Mahmood, S. An overview of human prion diseases. Virol. J. 2011, 8, 559. [Google Scholar] [CrossRef]
- Asher, D.M.; Gregori, L. Human transmissible spongiform encephalopathies: Historic view. Handb. Clin. Neurol. 2018, 153, 1–17. [Google Scholar] [CrossRef]
- Voigtländer, T.; Klöppel, S.; Birner, P.; Jarius, C.; Flicker, H.; Verghese-Nikolakaki, S.; Sklaviadis, T.; Guentchev, M.; Budka, H. Marked increase of neuronal prion protein immunoreactivity in Alzheimer’s disease and human prion diseases. Acta Neuropathol. 2011, 101, 417–423. [Google Scholar] [CrossRef]
- Kazlauskaite, J.; Young, A.; Gardner, C.E.; MacPherson, J.V.; Vénien-Bryan, C.; Pinheiro, T.J.T. An unusual soluble β-turn-rich conformation of prion is involved in fibril formation and toxic to neuronal cells. Biochem. Biophys. Res. Commun. 2005, 328, 292–305. [Google Scholar] [CrossRef]
- Chiesa, R. The elusive role of the prion protein and the mechanism of toxicity in prion disease. PLoS Pathog. 2015, 11, e1004745. [Google Scholar] [CrossRef]
- Hörnlimann, B.; Riesner, D.; Kretzschmar, H.A. Prions in Humans and Animals, 1st ed.; De Gruyter Publishing: Boston, MA, USA, 2006; p. 292. ISBN 978-3-11-018275-0. [Google Scholar]
- Klatzo, I.; Gajusek, D.C.; Zigas, V. Evaluation of pathological findings in twelve cases of kuru. In Encephalities; Van Boagert, L., Radermecker, J., Hozay, J., Lowenthal, A., Eds.; Elsevier: Amsterdam, The Netherlands, 1959; pp. 172–190. [Google Scholar]
- Beck, E.; Daniel, P.M.; Asher, D.M.; Gajdusek, D.C.; Gibbs, C.J. Experimental kuru in the chimpanzee. A neuropathological study. Jr. Brain. 1973, 96, 441–462. [Google Scholar] [CrossRef]
- Kitamoto, T.; Tateishi, J.; Tashima, T.; Takeshita, I.; Barry, R.A.; DeArmond, S.J.; Prusiner, S.B. Amyloid plaques in Creutzfeldt–Jakob disease stain with prion protein antibodies. Ann. Neurol. 1986, 20, 204–208. [Google Scholar] [CrossRef]
- Kuwahara, C.; Takeuchi, A.M.; Nishimura, T.; Haraguchi, K.; Kubosaki, A.; Matsumoto, Y.; Saeki, K.; Matsumoto, Y.; Yokoyama, T.; Itohara, S.; et al. Prions prevent neuronal cell-line death. Nature 1999, 400, 225–226. [Google Scholar] [CrossRef]
- Wulf, M.-A.; Senatore, A.; Aguzzi, A. The biological function of the cellular prion protein: An update. BMC Biol. 2017, 15, 34. [Google Scholar] [CrossRef]
- Chiesa, R.; Harris, D.A. Fishing for prion protein function. PLoS Biol. 2009, 7, e75. [Google Scholar] [CrossRef][Green Version]
- Steele, A.D.; Lindquist, S.; Aguzzi, A. The prion protein knockout mouse: A phenotype under challenge. Prion 2007, 1, 83–93. [Google Scholar] [CrossRef]
- Linden, R.; Martins, V.R.; Prado, M.A.M.; Cammarota, M.; Izquierdo, I.; Brentani, R.R. Physiology of the prion protein. Physiol. Rev. 2008, 88, 673–728. [Google Scholar] [CrossRef]
- McLennan, N.F.; Brennan, P.M.; McNeill, A.; Davies, I.; Fotheringham, A.; Rennison, K.A.; Ritchie, D.; Brannan, F.; Head, M.W.; Ironside, J.W.; et al. Prion protein accumulation and neuro-protection in hypoxic brain damage. Am. J Pathol. 2004, 165, 227–235. [Google Scholar] [CrossRef]
- Spudich, A.; Frigg, R.; Kilic, E.; Kilic, Ü.; Oesch, B.; Raeber, A.; Bassetti, C.L.; Hermann, D.M. Aggravation of ischemic brain injury by prion protein deficiency: Role of ERK-1/-2 and STAT-1. Neurobiol. Dis. 2005, 20, 442–449. [Google Scholar] [CrossRef]
- Freixes, M.; Puig, B.; Blanco, R.; Ferrer, I. Clusterin solubility and aggregation in Creutzfeldt–Jakob disease. Acta Neuropathol. 2004, 108, 295–301. [Google Scholar] [CrossRef]
- Lammie, A. Cerebral amyloid angiopathy in Alzheimer’s disease and related disorders. In Brain; Verbeel, M.M., De Waal, R.M.W., Vinters, H.W., Eds.; Kluwer Academic Publishers: Amsterdam, The Netherlands, 2001; p. 384. [Google Scholar] [CrossRef][Green Version]
- Laurén, J.; Gimbel, D.A.; Nygaard, H.B.; Gilbert, J.W.; Strittmatter, S.M. Cellular prion protein mediates impairment of synaptic plasticity by amyloid-beta oligomers. Nature 2009, 457, 1128–1132. [Google Scholar] [CrossRef]
- Resenberger, U.K.; Harmeier, A.; Woerner, A.C.; Goodman, J.L.; Müller, V.; Krishnan, R.; Vabulas, R.M.; A Kretzschmar, H.; Lindquist, S.; Hartl, F.U.; et al. The cellular prion protein mediates neurotoxic signalling of β-sheet-rich conformers independent of prion replication. EMBO J. 2011, 30, 2057–2070. [Google Scholar] [CrossRef]
- Vincent, B.; Sunyach, C.; Orzechowski, H.-D.; George-Hyslop, P.S.; Checler, F. p53-Dependent transcriptional control of cellular prion by presenilins. J. Neurosci. 2009, 29, 6752–6760. [Google Scholar] [CrossRef]
- Han, B.H.; DeMattos, R.B.; Dugan, L.L.; Kim-Han, J.S.; Brendza, R.P.; Fryer, J.D.; Kierson, M.; Cirrito, J.; Quick, K.; Harmony, J.A.K.; et al. Clusterin contributes to caspase-3-independent brain injury following neonatal hypoxia-ischemia. Nat Med. 2001, 7, 338–343. [Google Scholar] [CrossRef]
- Jones, S.E.; Jomary, C. Clusterin. Int. J. Biochem. Cell Biol. 2002, 34, 427–431. [Google Scholar] [CrossRef]
- McLaughlin, L.; Zhu, G.; Mistry, M.; Ley-Ebert, C.; Stuart, W.D.; Florio, C.J.; Groen, P.A.; Witt, S.A.; Kimball, T.R.; Witte, D.P.; et al. Apolipoprotein J/clusterin limits the severity of murine autoimmune myocarditis. J. Clin. Investig. 2000, 106, 1105–1113. [Google Scholar] [CrossRef]
- Michel, D.; Chatelain, G.; North, S.; Brun, G. Stress-induced transcription of the clusterin/apoJ gene. Biochem. J. 1997, 328, 45–50. [Google Scholar] [CrossRef]
- Yang, C.R.; Leskov, K.; Elberlein, H.; Criswell, T.; Pink, J.J.; Kinsella, T.J.; Boothman, D.A. Nuclear clusterin/XIP8, and x-ray-induced Ku70-binding protein that signals cell death. Proc. Natl. Acad. Sci. USA 2001, 97, 5907–5912. [Google Scholar] [CrossRef]
- Schwochau, G.B.; Nath, K.A.; Rosenberg, M.E. Clusterin protects against oxidative stress in vitro through aggregative and nonaggregative properties. Kidney Int. 1998, 53, 1647–1653. [Google Scholar] [CrossRef]
- Rosenberg, M.E.; Silkensen, J. Clusterin: Physiologic and pathophysiologic considerations. Int. J. Biochem. Cell Biol. 1995, 27, 633–645. [Google Scholar] [CrossRef]
- Ishii, T.; Haga, S.; Yagishita, S.; Tateishi, J. The presence of complements in amyloid plaques of Creutzfeldt–Jakob disease and Gerstmann–Straussler–Scheinker disease. Appl. Pathol. 1984, 2, 370–379. [Google Scholar] [PubMed]
- Graner, E.; Mercadante, A.F.; Zanata, S.M.; Forlenza, O.V.; Cabral, A.L.; Veiga, S.S.; A Juliano, M.; Roesler, R.; Walz, R.; Minetti, A.; et al. Cellular prion protein binds laminin and mediates neuritogenesis. Mol. Brain Res. 2000, 76, 85–92. [Google Scholar] [CrossRef]
- Gajdusek, D.; Zigas, V. Kuru; clinical, pathological and epidemiological study of an acute progressive degenerative disease of the central nervous system among natives of the Eastern Highlands of New Guinea. Am. J. Med. 1959, 26, 442–469. [Google Scholar] [CrossRef]
- Gajdusek, D.; Zigas, V. Studies on kuru. 1. The ethnologic setting of kuru. Am. J. Trop. Med. Hyg. 1961, 10, 80–91. [Google Scholar] [CrossRef]
- Liberski, P.P.; Gajos, A.; Sikorska, B.; Lindenbaum, S. Kuru, the First Human Prion Disease. Viruses 2019, 11, 232. [Google Scholar] [CrossRef]
- Beck, E.; Daniel, P.M. Prion diseases from a neuropathologist’s perspective. In Prion Diseases of Humans and Animals; Prusiner, S.B., Collinge, J., Powell, J., Anderton, B., Eds.; Ellis Horwood: New York, NY, USA, 1993; pp. 63–65. [Google Scholar]
- Hainfellner, J.A.; Liberski, P.P.; Guiroy, D.C.; Cervenáková, L.; Brown, P.; Gajdusek, D.C.; Budka, H. Pathology and immunocytochemistry of a kuru brain. Brain Pathol. 1997, 7, 547–553. [Google Scholar] [CrossRef]
- Piccardo, P.; Šafář, J.; Ceroni, M.; Gajdusek, D.C.; Gibbs, C.J., Jr. Immunohistochemical localization of prion protein in spongiform encephalopathies and normal brain tissue. Neurology 1990, 40, 518–522. [Google Scholar] [CrossRef]
- Vacca, V.M., Jr. CJD: Understanding Creutzfeldt–Jakob disease. Nursing 2016, 46, 36–42. [Google Scholar] [CrossRef]
- Gençer, A.G.; Pelin, Z.; Kucukali, C.I.; Topçuoğlu, Ö.B.; Yilmaz, N. Creutzfeldt–Jakob disease. Psychogeriatrics 2011, 11, 119–124. [Google Scholar] [CrossRef]
- Sikorska, B.; Knight, R.; Ironside, J.W.; Liberski, P.P. Creutzfeldt–Jakob disease. Adv. Exp. Med. Biol. 2012, 724, 76–90. [Google Scholar] [CrossRef]
- Budka, H.; Aguzzi, A.; Brown, P.; Brucher, J.-M.; Bugiani, O.; Gullotta, F.; Haltia, M.; Hauw, J.-J.; Ironside, J.W.; Jellinger, K.; et al. Neuropathological diagnostic criteria for Creutzfeldt–Jakob disease (CJD) and other human spongiform encephalopathies (prion diseases). Brain Pathol. 1995, 5, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.E.; Ironside, J.W. Neuropathology of spongiform encephalopathies in humans. Br. Med. Bull. 1993, 49, 738–777. [Google Scholar] [CrossRef] [PubMed]
- Collinge, J. Variant Creutzfeldt–Jakob disease. Lancet 1999, 354, 317–323. [Google Scholar] [CrossRef]
- Hill, A.F.; Joiner, S.; Wadsworth, J.D.F.; Sidle, K.C.L.; Bell, J.E.; Budka, H.; Ironside, J.W.; Collinge, J. Molecular classification of sporadic Creutzfeldt–Jakob disease. Brain 2003, 126, 1333–1346. [Google Scholar] [CrossRef]
- Brown, P.; Cathala, F.; Raubertas, R.F.; Gajdusek, D.C.; Castaigne, P. The epidemiology of Creutzfeldt–Jakob disease: Conclusion of a 15-year investigation in France and review of the world literature. Neurology 1987, 37, 895–904. [Google Scholar] [CrossRef]
- Gao, L.-P.; Shi, Q.; Xiao, K.; Wang, J.; Zhou, W.; Chen, C.; Dong, X. The genetic Creutzfeldt–Jakob disease with E200K mutation: Analysis of clinical, genetic and laboratory features of 30 Chinese patients. Sci. Rep. 2019, 9, 1836. [Google Scholar] [CrossRef]
- Will, R.G. Acquired prion disease: Iatrogenic CJD, variant CJD, kuru. Br. Med Bull. 2003, 66, 255–265. [Google Scholar] [CrossRef]
- Lantos, P. From slow virus to prion: A review of transmissible spongiform encephalopathies. Histopathology. 1992, 20, 1–11. [Google Scholar] [CrossRef]
- Duyckaerts, C.; Dickson, D.W. Neurodegeneration: The Molecular Pathology of Dementia and Movement Disorders, 2nd ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2011; pp. 68–71. ISBN 978140519632. [Google Scholar]
- Vickers, J.C.; Mitew, S.; Woodhouse, A.; Fernandez-Martos, C.M.; Kirkcaldie, M.T.; Canty, A.J.; McCormack, G.H.; King, A.E. Defining the Earliest Pathological Changes of Alzheimer’s Disease. Curr. Alzheimer Res. 2016, 13, 281–287. [Google Scholar] [CrossRef]
- D’Amore, J.D.; Kajdasz, S.T.; McLellan, M.E.; Bacskai, B.J.; Stern, E.A.; Hyman, B.T. In vivo multiphoton imaging of a transgenic mouse model of Alzheimer disease reveals marked thioflavine-S-associated alterations in neurite trajectories. J. Neuropathol. Exp. Neurol. 2003, 62, 137–145. [Google Scholar] [CrossRef][Green Version]
- Parchi, P.; Giese, A.; Capellari, S.; Brown, P.; Schulz-Schaeffer, W.; Windl, O.; Zerr, I.; Budka, H.; Kopp, N.; Piccardo, P.; et al. Classification of sporadic Creutzfeldt–Jakob disease based on molecular and phenotypic analysis of 300 subjects. Ann. Neurol. 1999, 46, 224–233. [Google Scholar] [CrossRef]
- Rossi, M.; Saverioni, D.; Di Bari, M.A.; Baiardi, S.; Lemstra, A.W.; Pirisinu, L.; Capellari, S.; Rozemuller, A.; Nonno, R.; Parchi, P. Atypical Creutzfeldt–Jakob disease with PrP-amyloid plaques in white matter: Molecular characterization and transmission to bank voles show the M1 strain signature. Acta Neuropathol. Commun. 2017, 5, 87. [Google Scholar] [CrossRef]
- Tatzelt, J. Prion Proteins; Springer: Berlin\Heidelberg, Germany, 2011; p. 29. ISBN 978-3-642-24067-6. [Google Scholar]
- The Neuropathology of CJD. Available online: https://www.cjd.ed.ac.uk/sites/default/files/neuropath.pdf (accessed on 13 November 2020).
- Nair, A.K.; Sabbagh, M.N. Geriatric Neurology, 1st ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2014; p. 277. ISBN 978-1-118-73068-3. [Google Scholar]
- Brown, D. Neurodegeneration and Prion Disease; Springer: New York, NY, USA, 2005; p. 33. ISBN 978-0387239224. [Google Scholar]
- Sobel, R.A. Greenfield’s Neuropathology, Ninth Edition; 2-Volume Set. J. Neuropathol. Exp. Neurol. 2015, 74, 1185. [Google Scholar] [CrossRef][Green Version]
- Kobayashi, A.; Arima, K.; Ogawa, M.; Murata, M.; Fukuda, T.; Kitamoto, T. Plaque-type deposition of prion protein in the damaged white matter of sporadic Creutzfeldt–Jakob disease MM1 patients. Acta Neuropathol. 2008, 116, 561–566. [Google Scholar] [CrossRef]
- Liberski, P.P. Gerstmann–Sträussler–Scheinker Disease. In Neurodegenerative Diseases. Advances in Experimental Medicine and Biology; Ahmad, S.I., Ed.; Springer: New York, NY, USA, 2012; Available online: https://doi.org/10.1007/978-1-4614-0653-2_10 (accessed on 20 October 2020).
- Gambetti, P.; Kong, Q.; Zou, W.; Parchi, P.; Chen, S.G. Sporadic and familial CJD: Classification and characterisation. Br. Med. Bull. 2003, 66, 213–239. [Google Scholar] [CrossRef]
- Ghetti, B.; Tagliavini, F.; Takao, M.; Bugiani, O.; Piccardo, P. Hereditary prion protein amyloidoses. Clin. Lab. Med. 2003, 23, 65–85. [Google Scholar] [CrossRef]
- Galatioto, S.; Ruggeri, D.; Gullotta, F. Gerstmann–Sträussler–Scheinker syndrome in a Sicilian patient. Neuropathological aspects. Pathologica 1995, 87, 659–665. [Google Scholar] [PubMed]
- Campbell, T.A.; Palmer, M.S.; Will, R.G.; Gibb, W.; Luthert, P.J.; Collinge, J. A prion disease with a novel 96-base pair insertional mutation in the prion protein gene. Neurology 1996, 46, 761–766. [Google Scholar] [CrossRef]
- Cochran, E.J.; Bennett, D.A.; Cervenakova, L.; Kenney, K.; Bernard, B.; Foster, N.L.; Benson, D.F.; Goldfarb, L.G.; Brown, P. Familial Creutzfeldt–Jakob disease with a five-repeat octapeptide insert mutation. Neurology 1996, 47, 727–733. [Google Scholar] [CrossRef]
- Capellari, S.; Vital, C.; Parchi, P.; Petersen, R.B.; Ferrer, X.; Jarnier, D.; Pegoraro, E.; Gambetti, P.; Julien, J. Familial prion disease with a novel 144-bp insertion in the prion protein gene in a Basque family. Neurology 1997, 49, 133–141. [Google Scholar] [CrossRef]
- Collinge, J.; Brown, J.; Hardy, J.; Mullan, M.; Rossor, M.N.; Baker, H.; Crow, T.J.; Lofthouse, R.; Poulter, M.; Ridley, R.; et al. Inherited prion disease with 144 base pair gene insertion. 2. Clinical and pathological features. Brain 1992, 115, 687–710. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.; Goldfarb, L.G.; McCombie, W.R.; Nieto, A.; Squillacote, D.; Sheremata, W.; Little, B.W.; Godec, M.S.; Gibbs, C.J.; Gajdusek, D.C. Atypical Creutzfeldt-Jakob disease in an American family with an insert mutation in the PRNP amyloid precursor gene. Neurology 1992, 42, 422. [Google Scholar] [CrossRef] [PubMed]
- Goldfarb, L.G.; Brown, P.; McCombie, W.R.; Goldgaber, D.; Swergold, G.D.; Wills, P.R.; Cervenakova, L.; Baron, H.; Gibbs, C.J.; Gajdusek, D.C. Transmissible familial Creutzfeldt–Jakob disease associated with five, seven, and eight extra octapeptide coding repeats in the PRNP gene. Proc. Natl. Acad. Sci. USA 1991, 88, 10926–10930. [Google Scholar] [CrossRef] [PubMed]
- Krasemann, S.; Zerr, I.; Weber, T.; Poser, S.; Kretzschmar, H.; Hunsmann, G.; Bodemer, W. Prion disease associated with a novel nine octapeptide repeat insertion in the PRNP gene. Brain Res. 1995, 34, 173–176. [Google Scholar] [CrossRef]
- Vital, C.; Gray, F.; Vital, A.; Parchi, P.; Capellari, S.; Petersen, R.B.; Ferrer, X.; Jarnier, D.; Julien, J.; Gambetti, P. Prion encephalopathy with insertion of octapeptide repeats: The number of repeats determines the type of cerebellar deposits. Neuropathol. Appl. Neurobiol. 1998, 24, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Webb, T.E.F.; Poulter, M.; Beck, J.; Uphill, J.; Adamson, G.; Campbell, T.; Linehan, J.; Powell, C.; Brandner, S.; Pal, S.; et al. Phenotypic heterogeneity and genetic modification of P102L inherited prion disease in an international series. Brain 2008, 131, 2632–2646. [Google Scholar] [CrossRef]
- Liberski, P.P. Amyloid plaques in transmissible spongiform encephalopathies (prion diseases). Folia Neuropathol. 2004, 42 (Suppl. B), 109–119. [Google Scholar]
- Liberski, P.P.; Bratosiewicz, J.; Waliś, A.; Kordek, R.; Jeffrey, M.; Brown, P. A special report I. Prion protein (PrP)--amyloid plaques in the transmissible spongiform encephalopathies, or prion diseases revisited. Folia Neuropathol. 2001, 39, 217–235. [Google Scholar]
- Liberski, P.P.; Sikorska, B.; Lindenbaum, S.; Goldfarb, L.G.; McLean, C.; Hainfellner, J.A.; Brown, P. Kuru: Genes, cannibals and neuropathology. J. Neuropathol. Exp. Neurol. 2012, 71, 92–103. [Google Scholar] [CrossRef]
- Will, R.; Ironside, J.; Zeidler, M.; Estibeiro, K.; Cousens, S.; Smith, P.; Alperovitch, A.; Poser, S.; Pocchiari, M.; Hofman, A. A new variant of Creutzfeldt–Jakob disease in the UK. Lancet 1996, 347, 921–925. [Google Scholar] [CrossRef]
- Ironside, J.W.; E Bell, J. Florid plaques and new variant Creutzfeldt–Jakob disease. Lancet 1997, 350, 1475. [Google Scholar] [CrossRef]
- Ironside, J.W.; Head, M.W.; McCardle, L.; Knight, R. Neuropathology of variant Creutzfeldt–Jakob disease. Acta Neurobiol. Exp. 2002, 62, 175–182. [Google Scholar] [CrossRef]
- World Federation of Scientists. Visualization of a Battlefield: The Pathology of Human Transmissible Spongiform Encephalopathies by Budka H. Available online: http://www.federationofscientists.org/PMPanels/TSE/Visuals.php (accessed on 14 November 2020).
- Ghetti, B.; Dlouhy, S.R.; Giaccone, G.; Bugiani, O.; Frangione, B.; Farlow, M.R.; Tagliavini, F. Gerstmann–Sträussler–Scheinker disease and the Indiana kindred. Brain Pathol. 1995, 5, 61–75. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, I.; Carmona, M.; Blanco, R.; Recio, M.; Segundo, R. Gerstmann–Straüssler–Scheinker PRNP P102L-129V mutation. Transl. Neurosci. 2011, 2, 23–32. [Google Scholar] [CrossRef]
- Thal, D.R.; Rüb, U.; Orantes, M.; Braak, H. Phases of A beta-deposition in the human brain and its relevance for the development of AD. Neurology 2002, 58, 1791–1800. [Google Scholar] [CrossRef] [PubMed]


| Amyloid/Senile Plaques | |||
|---|---|---|---|
| Diffuse/pre-amyloid | Neuritic | Compact/burnt-out | |
| Non-cored/ primitive/immature | Cored/classic/dense/ mature/focal |
| |
| PrP Plaques | |||
|---|---|---|---|
| - Extracellular Deposits of PrP Visible with Hematoxylin-eosin Staining | |||
| Unicentric/“Kuru”/”Kuru-like”/Stellate | Daisy/Florid | Multicentric | Neuritic |
| |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jankovska, N.; Olejar, T.; Matej, R. Extracellular Amyloid Deposits in Alzheimer’s and Creutzfeldt–Jakob Disease: Similar Behavior of Different Proteins? Int. J. Mol. Sci. 2021, 22, 7. https://doi.org/10.3390/ijms22010007
Jankovska N, Olejar T, Matej R. Extracellular Amyloid Deposits in Alzheimer’s and Creutzfeldt–Jakob Disease: Similar Behavior of Different Proteins? International Journal of Molecular Sciences. 2021; 22(1):7. https://doi.org/10.3390/ijms22010007
Chicago/Turabian StyleJankovska, Nikol, Tomas Olejar, and Radoslav Matej. 2021. "Extracellular Amyloid Deposits in Alzheimer’s and Creutzfeldt–Jakob Disease: Similar Behavior of Different Proteins?" International Journal of Molecular Sciences 22, no. 1: 7. https://doi.org/10.3390/ijms22010007
APA StyleJankovska, N., Olejar, T., & Matej, R. (2021). Extracellular Amyloid Deposits in Alzheimer’s and Creutzfeldt–Jakob Disease: Similar Behavior of Different Proteins? International Journal of Molecular Sciences, 22(1), 7. https://doi.org/10.3390/ijms22010007





