Bacillus anthracis’ PA63 Delivers the Tumor Metastasis Suppressor Protein NDPK-A/NME1 into Breast Cancer Cells
Abstract
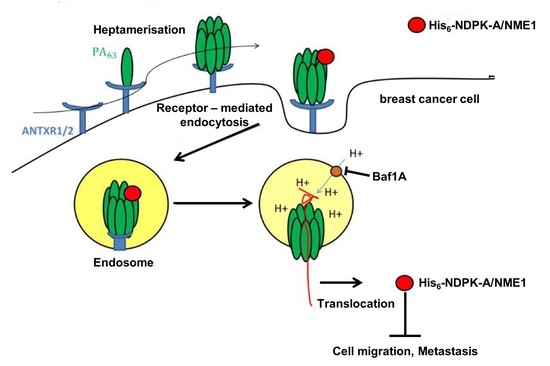
1. Introduction
2. Results
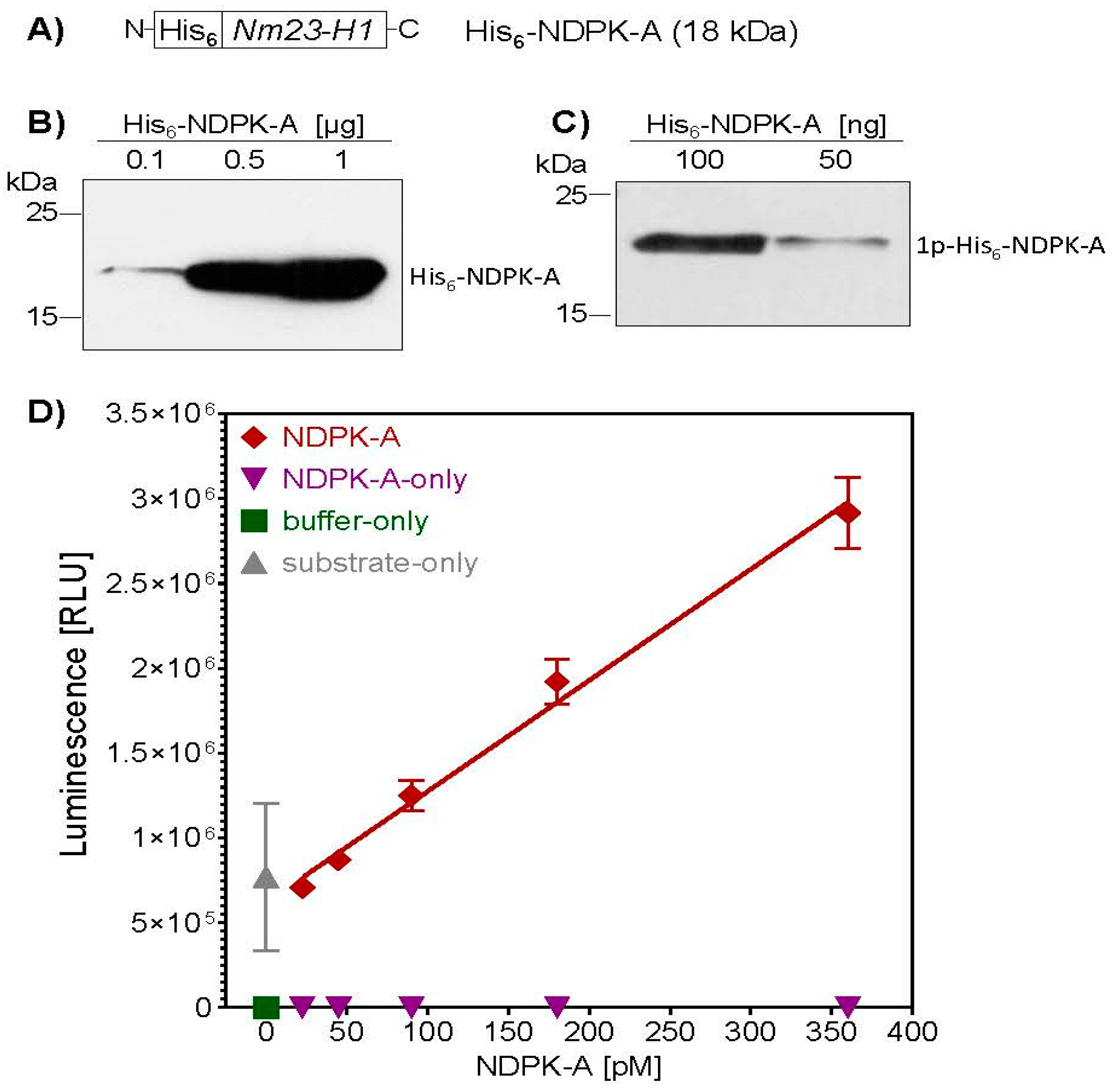
2.1. Purification and Characterization of Recombinantly Expressed His6-NDPK-A
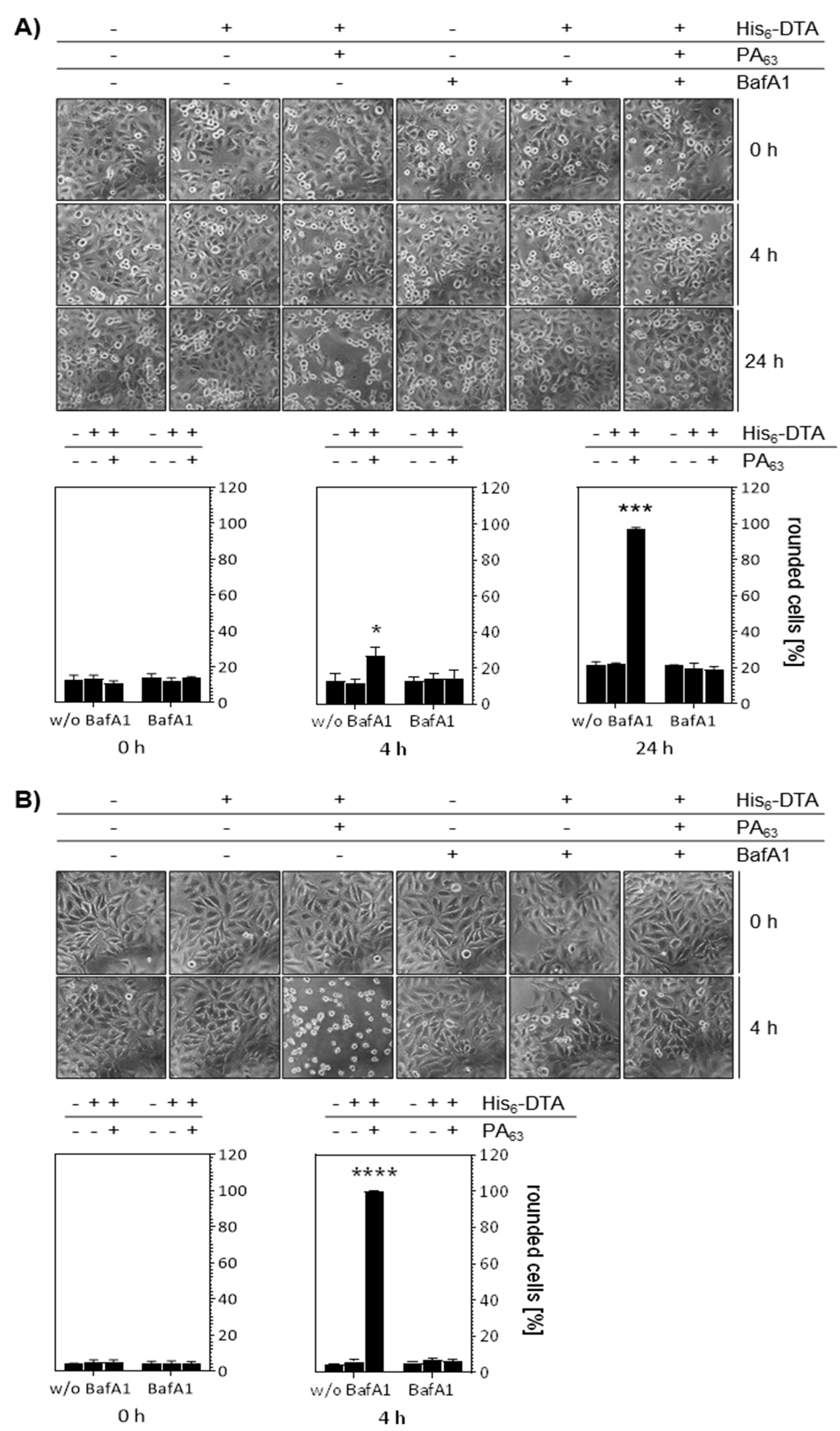
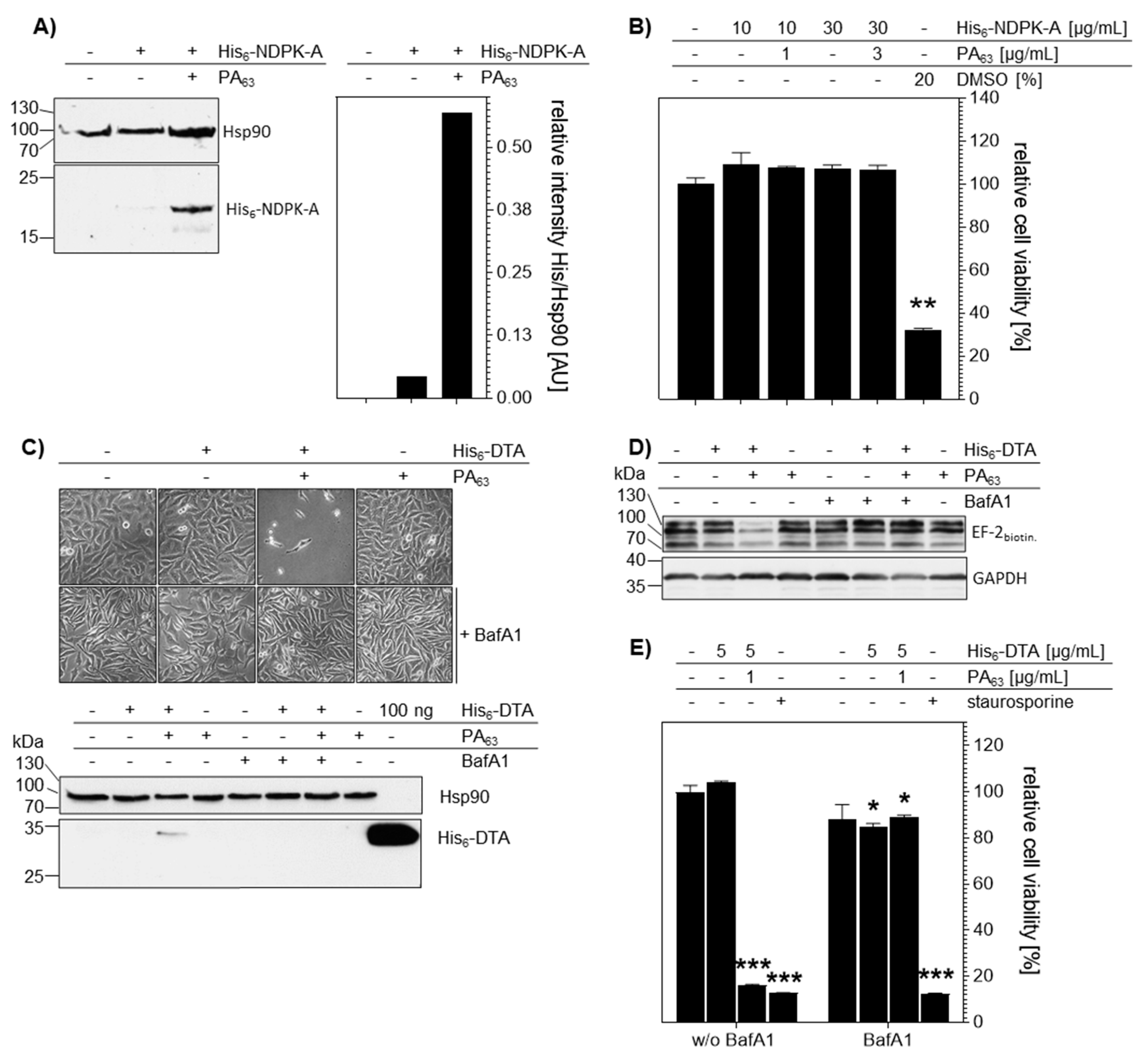
2.2. MDA-MB-231 Cells are Susceptible to PA63-Mediated Delivery of His-Tagged Protein Cargo
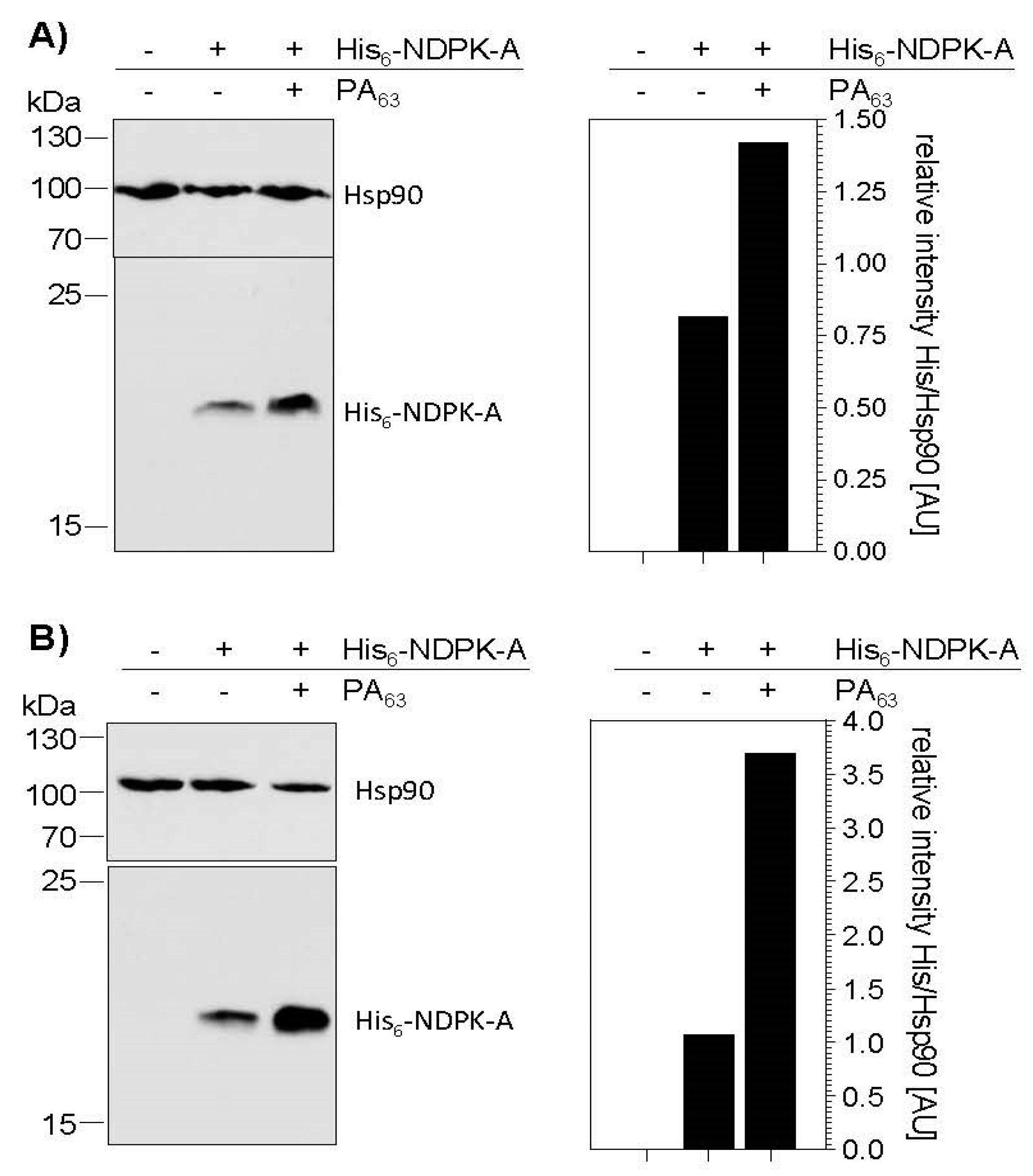
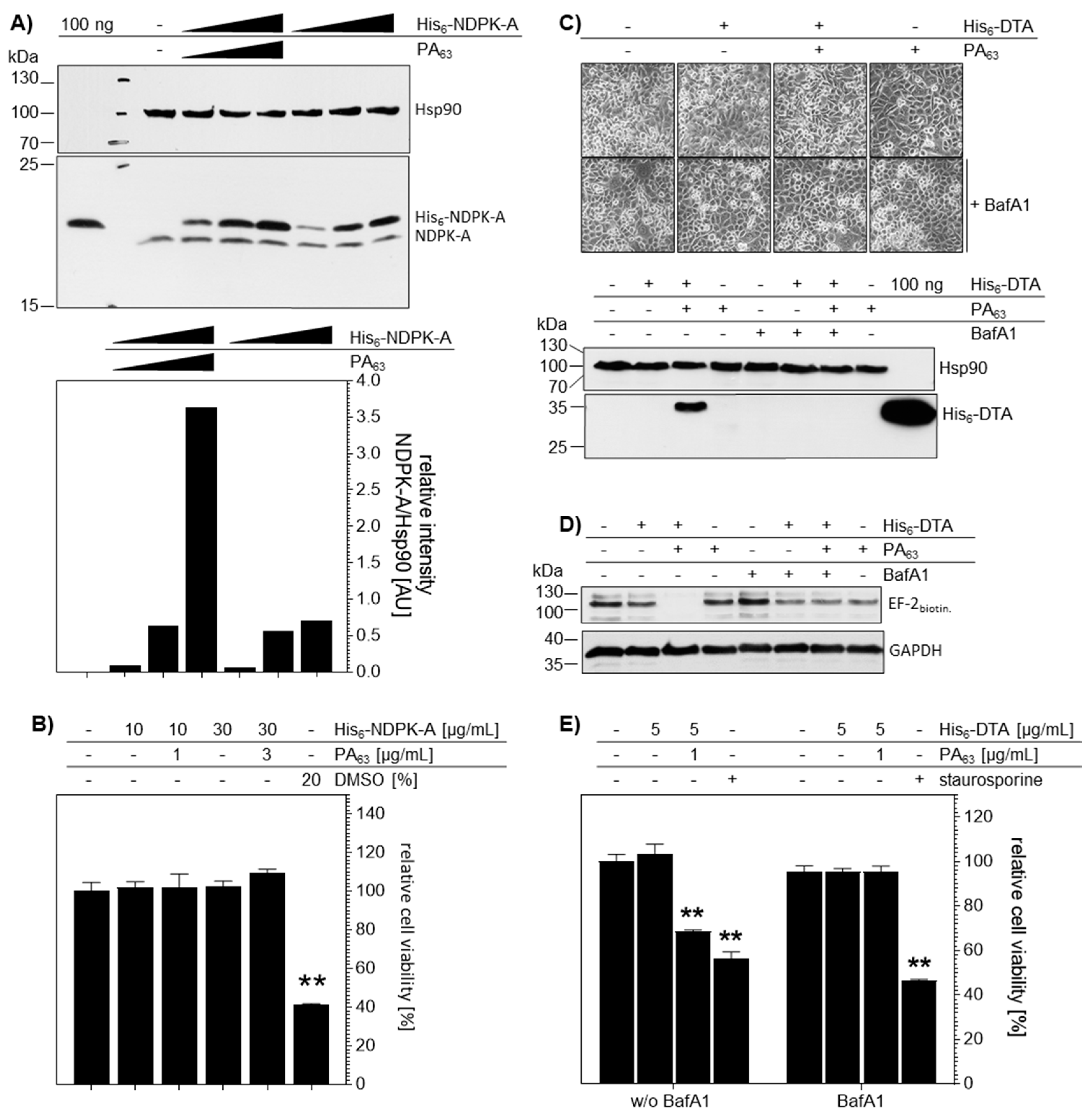
2.3. PA63 Mediates Delivery of His6-NDPK-A into Cells
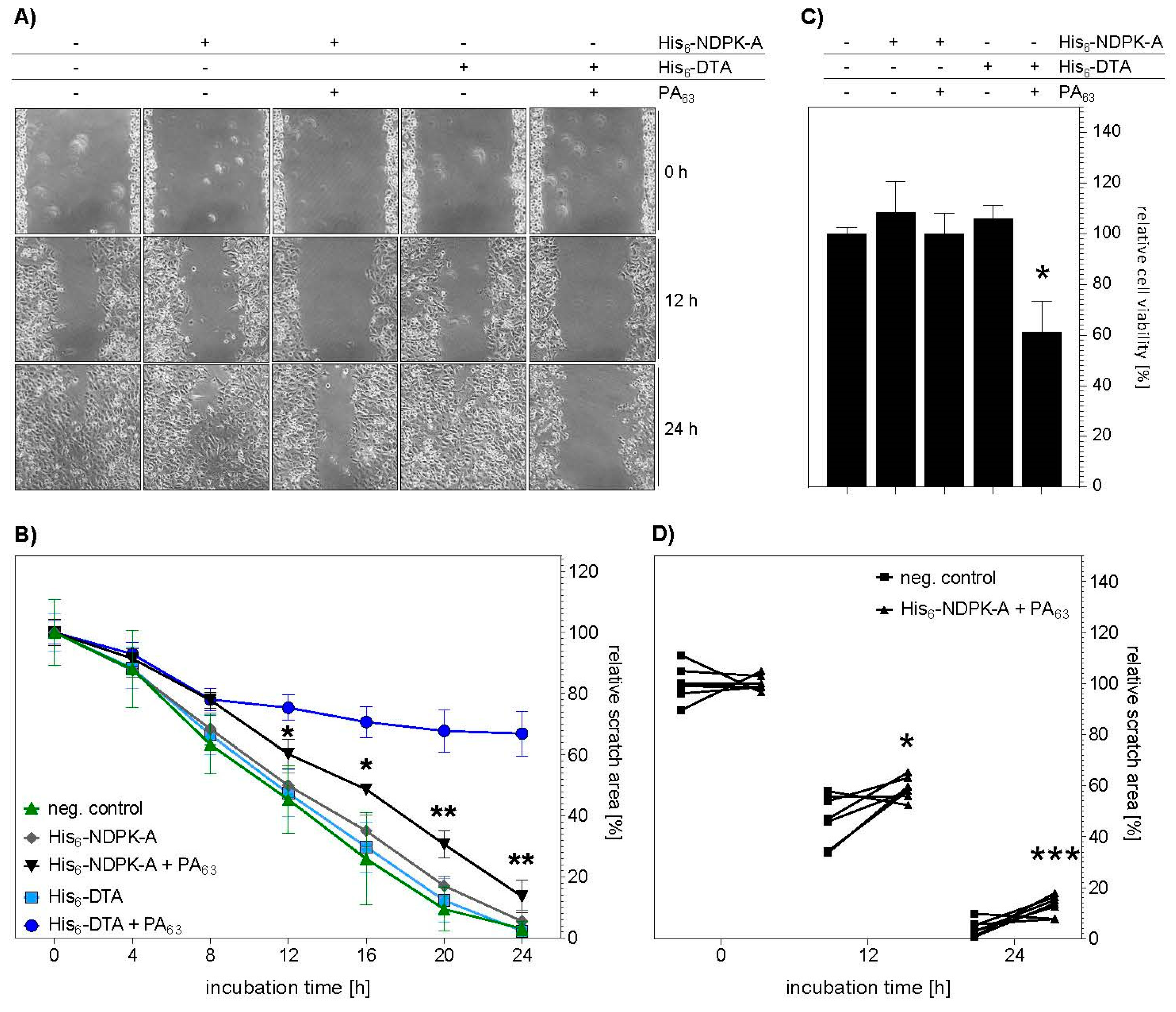
2.4. Treatment with His6-NDPK-A Plus PA63 Decreased Migration of MDA-MB-231 Cells
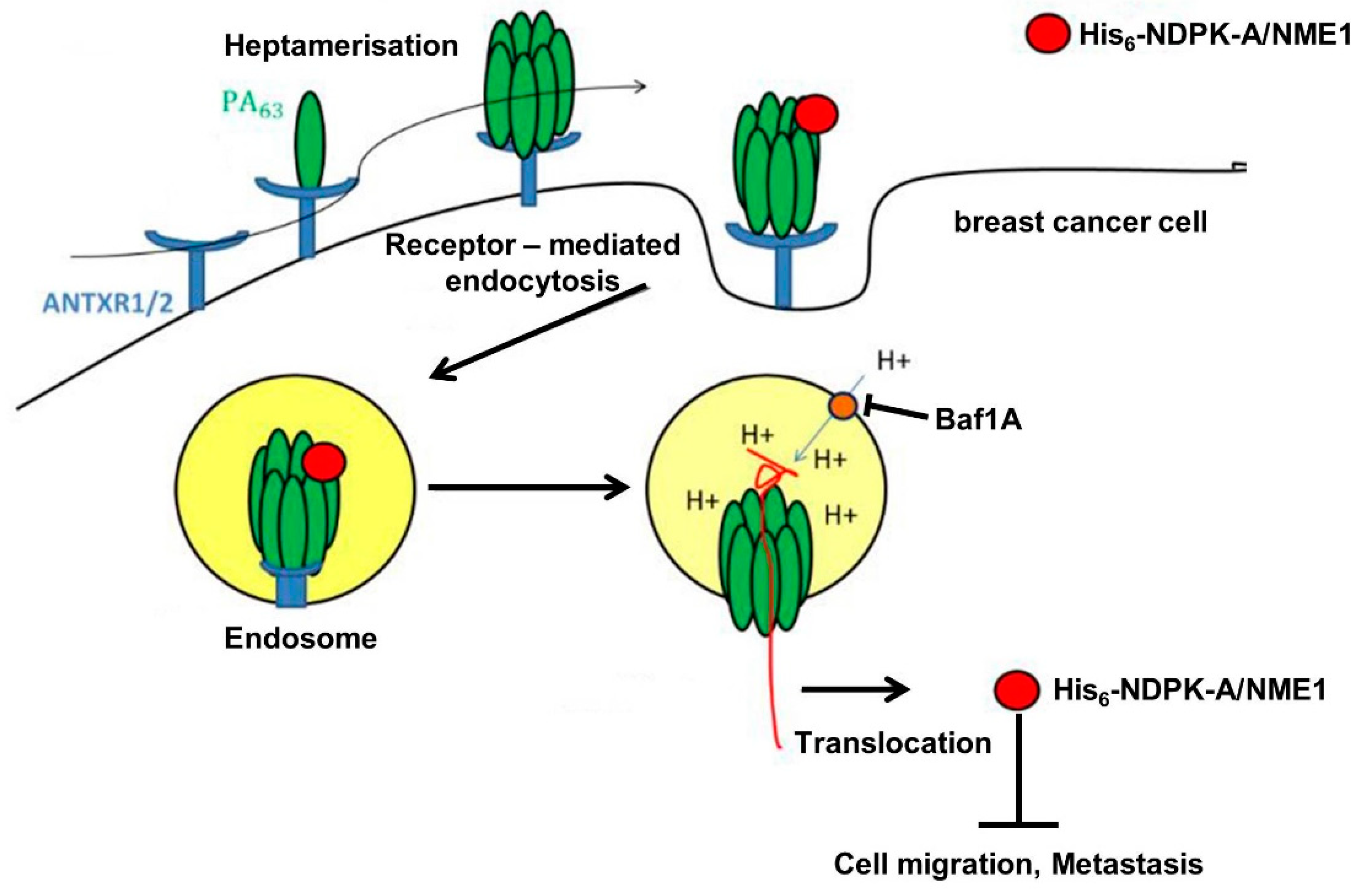
3. Discussion
4. Material and Methods
4.1. Materials
4.2. Methods
4.2.1. Cell Culture
4.2.2. Expression and Purification of Recombinant Proteins
4.2.3. Characterization of His6-NDPK-A Kinase Activity
4.2.4. SDS-PAGE and Western Blotting
4.2.5. Cell Binding Assay
4.2.6. Analysis of Protein Uptake into Cells
4.2.7. Cell Viability Assay
4.2.8. Sequential ADP-Ribosylation of EF-2 by DTA
4.2.9. Immunofluorescence Microscopy
4.2.10. Migration Assay (Wound-Healing Assay, Scratch Assay)
4.2.11. Experimental Reproducibility and Statistics
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| BafA1 | bafilomycin A1 |
| DT | diphtheria toxin of Corynebacterium diphtheriae |
| DTA | protein domain of DT harboring the ADP-ribosyltransferase activity |
| EF-2 | elongation factor 2 |
| EF-2 biotin. | In Vitro biotinylated EF-2 |
| His6 | N-terminal protein tag consistent of 6 histidine |
| NDPK-A | nucleoside diphosphate kinase isoform A |
| PA63 | 63 kDa proteolysis product of Bacillus anthracis protective antigen (PA) |
| strep-POD | streptavidin-peroxidase conjugate. |
References
- Steeg, P.S. Targeting metastasis. Nat. Rev. Cancer 2016, 16, 201–218. [Google Scholar] [CrossRef] [PubMed]
- Wan, L.; Pantel, K.; Kang, Y. Tumor metastasis: Moving new biological insights into the clinic. Nat. Med. 2013, 19, 1450–1464. [Google Scholar] [CrossRef] [PubMed]
- Bohl, C.R.; Harihar, S.; Denning, W.L.; Sharma, R.; Welch, D.R. Metastasis suppressors in breast cancers: Mechanistic insights and clinical potential. J. Mol. Med. 2014, 92, 13–30. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.C.; Theodorescu, D. Learning therapeutic lessons from metastasis suppressor proteins. Nat. Rev. Cancer 2009, 9, 253–264. [Google Scholar] [CrossRef] [PubMed]
- Steeg, P.S.; Bevilacqua, G.; Kopper, L.; Thorgeirsson, U.P.; Talmadge, J.E.; Liotta, L.A.; Sobel, M.E. Evidence for a novel gene associated with low tumor metastatic potential. J. Natl. Cancer Inst. 1988, 80, 200–204. [Google Scholar] [CrossRef] [PubMed]
- Biggs, J.; Hersperger, E.; Steeg, P.S.; Liotta, L.A.; Shearn, A. A Drosophila gene that is homologous to a mammalian gene associated with tumor metastasis codes for a nucleoside diphosphate kinase. Cell 1990, 63, 933–940. [Google Scholar] [CrossRef]
- Salerno, M.; Ouatas, T.; Palmieri, D.; Steeg, P.S. Inhibition of signal transduction by the nm23 metastasis suppressor: Possible mechanisms. Clin. Exp. Metastasis 2003, 20, 3–10. [Google Scholar] [CrossRef]
- Horak, C.E.; Lee, J.H.; Elkahloun, A.G.; Boissan, M.; Dumont, S.; Maga, T.K.; Arnaud-Dabernat, S.; Palmieri, D.; Stetler-Stevenson, W.G.; Lacombe, M.-L.; et al. Nm23-H1 Suppresses Tumor Cell Motility by Down-regulating the Lysophosphatidic Acid Receptor EDG2. Cancer Res. 2007, 67, 7238–7246. [Google Scholar] [CrossRef]
- Kantor, J.D.; McCormick, B.; Steeg, P.S.; Zetter, B.R. Inhibition of cell motility after nm23 transfection of human and murine tumor cells. Cancer Res. 1993, 53, 1971–1973. [Google Scholar]
- Marino, N.; Marshall, J.C.; Collins, J.W.; Zhou, M.; Qian, Y.; Veenstra, T.; Steeg, P.S. Nm23-H1 binds to Gelsolin and inactivates its actin-severing capacity to promote tumor cell motility and metastasis. Cancer Res. 2013, 73, 5949–5962. [Google Scholar] [CrossRef]
- Khan, I.; Gril, B.; Steeg, P.S. Metastasis suppressors NME1 and NME2 promote dynamin 2 oligomerization and regulate tumor cell endocytosis, motility, and metastasis. Cancer Res. 2019, 79, 4689–4702. [Google Scholar] [CrossRef] [PubMed]
- Barth, H.; Blöcker, D.; Aktories, K. The uptake machinery of clostridial actin ADP-ribosylating toxins—A cell delivery system for fusion proteins and polypeptide drugs. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2002, 366, 501–512. [Google Scholar] [CrossRef] [PubMed]
- Barth, H.; Hofmann, F.; Olenik, C.; Just, I.; Aktories, K. The N-terminal part of the enzyme component (C2I) of the binary Clostridium botulinum C2 toxin interacts with the binding component C2II and functions as a carrier system for a Rho ADP-ribosylating C3-like fusion toxin. Infect Immun. 1998, 66, 1364–1369. [Google Scholar] [CrossRef] [PubMed]
- Barth, H.; Aktories, K.; Popoff, M.R.; Stiles, B.G. Binary Bacterial Toxins: Biochemistry, Biology, and Applications of Common Clostridium and Bacillus Proteins. Microbiol. Mol. Biol. Rev. 2004, 68, 373–402. [Google Scholar] [CrossRef] [PubMed]
- Bachran, C.; Leppla, S.H. Tumor Targeting and Drug Delivery by Anthrax Toxin. Toxins 2016, 8, 197. [Google Scholar] [CrossRef] [PubMed]
- Shorter, S.A.; Gollings, A.S.; Gorringe-Pattrick, M.A.M.; Coakley, J.E.; Dyer, P.D.R.; Richardson, S.C.W. The potential of toxin-based drug delivery systems for enhanced nucleic acid therapeutic delivery. Expert Opin. Drug Deliv. 2017, 14, 685–696. [Google Scholar] [CrossRef]
- Barth, H.; Roebling, R.; Fritz, M.; Aktories, K. The Binary Clostridium botulinum C2 Toxin as a Protein Delivery System: Identification of the minimal protein region necessary for interaction of toxin components. J. Biol. Chem. 2002, 277, 5074–5081. [Google Scholar] [CrossRef]
- Moayeri, M.; Leppla, S.H.; Vrentas, C.; Pomerantsev, A.P.; Liu, S. Anthrax Pathogenesis. Annu. Rev. Microbiol. 2015, 69, 185–208. [Google Scholar] [CrossRef]
- Collier, R.J. Membrane translocation by anthrax toxin. Mol. Asp. Med. 2009, 30, 413–422. [Google Scholar] [CrossRef]
- Pentelute, B.L.; Sharma, O.; Collier, R.J. Chemical dissection of protein translocation through the anthrax toxin pore. Angew. Chem. Int. Ed. 2011, 50, 2294–2296. [Google Scholar] [CrossRef]
- Benz, R.; Barth, H. Toxin Transport by A-B Type of Toxins in Eukaryotic Target Cells and Its Inhibition by Positively Charged Heterocyclic Molecules. In Current Topics in Microbiology and Immunology; Springer: Cham, Switzerland, 2017; Volume 406, pp. 229–256. [Google Scholar]
- Young, J.A.T.; Collier, R.J. Anthrax Toxin: Receptor Binding, Internalization, Pore Formation, and Translocation. Annu. Rev. Biochem. 2007, 76, 243–265. [Google Scholar] [CrossRef] [PubMed]
- Arora, N.; Leppla, S.H. Residues 1-254 of anthrax toxin lethal factor are sufficient to cause cellular uptake of fused polypeptides. J. Biol. Chem. 1993, 268, 3334–3341. [Google Scholar] [PubMed]
- Arora, N.; Leppla, S.H. Fusions of anthrax toxin lethal factor with Shiga toxin and diphtheria toxin enzymatic domains are toxic to mammalian cells. Infect. Immun. 1994, 62, 4955–4961. [Google Scholar] [CrossRef] [PubMed]
- Leppla, S.H.; Arora, N.; Varughese, M. Anthrax toxin fusion proteins for intracellular delivery of macromolecules. J. Appl. Microbiol. 1999, 87, 284. [Google Scholar] [CrossRef] [PubMed]
- Milne, J.C.; Blanket, S.R.; Hanna, P.C.; Collier, R.J. Protective antigen-binding domain of anthrax lethal factor mediates translocation of a heterologous protein fused to its amino- or carboxy-terminus. Mol. Microbiol. 1995, 15, 661–666. [Google Scholar] [CrossRef]
- Blanke, S.R.; Milne, J.C.; Benson, E.L.; Collier, R.J. Fused polycationic peptide mediates delivery of diphtheria toxin A chain to the cytosol in the presence of anthrax protective antigen. Proc. Natl. Acad. Sci. USA 1996, 93, 8437–8442. [Google Scholar] [CrossRef]
- Sharma, O.; Collier, R.J. Polylysine-mediated translocation of the diphtheria toxin catalytic domain through the anthrax protective antigen pore. Biochemistry 2014, 53, 6934–6940. [Google Scholar] [CrossRef]
- Rabideau, A.E.; Pentelute, B.L. Delivery of Non-Native Cargo into Mammalian Cells Using Anthrax Lethal Toxin. ACS Chem. Biol. 2016, 11, 1490–1501. [Google Scholar] [CrossRef]
- Beitzinger, C.; Stefani, C.; Kronhardt, A.; Rolando, M.; Flatau, G.; Lemichez, E.; Benz, R. Role of N-terminal His6-Tags in binding and efficient translocation of polypeptides into cells using anthrax protective antigen (PA). PLoS ONE 2012, 7, e46964. [Google Scholar] [CrossRef]
- Schnell, L.; Felix, I.; Müller, B.; Sadi, M.; von Bank, F.; Papatheodorou, P.; Popoff, M.R.; Aktories, K.; Waltenberger, E.; Benz, R.; et al. Revisiting an old antibiotic: Bacitracin neutralizes binary bacterial toxins and protects cells from intoxication. FASEB J. 2019, 33, 5755–5771. [Google Scholar] [CrossRef]
- Schuster, M.; Schnell, L.; Feigl, P.; Birkhofer, C.; Mohr, K.; Roeder, M.; Carle, S.; Langer, S.; Tippel, F.; Buchner, J.; et al. The Hsp90 machinery facilitates the transport of diphtheria toxin into human cells. Sci. Rep. 2017, 7, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Lang, A.E.; Ernst, K.; Lee, H.; Papatheodorou, P.; Schwan, C.; Barth, H.; Aktories, K. The chaperone Hsp90 and PPIases of the cyclophilin and FKBP families facilitate membrane translocation of Photorhabdus luminescens ADP-ribosyltransferases. Cell. Microbiol. 2014, 16, 490–503. [Google Scholar] [CrossRef] [PubMed]
- McCluskey, A.J.; Collier, R.J. Receptor-directed chimeric toxins created by sortase-mediated protein fusion. Mol. Cancer Ther. 2013, 12, 2273–2281. [Google Scholar] [CrossRef] [PubMed]
- McCluskey, A.J.; Olive, A.J.; Starnbach, M.N.; Collier, R.J. Targeting HER2-positive cancer cells with receptor-redirected anthrax protective antigen. Mol. Oncol. 2013, 7, 440–451. [Google Scholar] [CrossRef]
- Mechaly, A.; McCluskey, A.J.; Collier, R.J. Changing the receptor specificity of anthrax toxin. MBio 2012, 3, e00088-12. [Google Scholar] [CrossRef]
- Zahaf, N.-I.; Lang, A.E.; Kaiser, L.; Fichter, C.D.; Lassmann, S.; McCluskey, A.; Augspach, A.; Aktories, K.; Schmidt, G. Targeted delivery of an ADP-ribosylating bacterial toxin into cancer cells. Sci. Rep. 2017, 27, 41252. [Google Scholar] [CrossRef]
- Jack, S.; Madhivanan, K.; Ramadesikan, S.; Subramanian, S.; Edwards, D.F.; Elzey, B.D.; Dhawan, D.; McCluskey, A.; Kischuk, E.M.; Loftis, A.R.; et al. A novel, safe, fast and efficient treatment for Her2-positive and negative bladder cancer utilizing an EGF-anthrax toxin chimera. Int. J. Cancer 2020, 146, 449–460. [Google Scholar] [CrossRef]
- Fuhs, S.R.; Meisenhelder, J.; Aslanian, A.; Lemke, G.; Yates Iii, J.R.; Correspondence, T.H.; Ma, L.; Zagorska, A.; Stankova, M.; Binnie, A.; et al. Monoclonal 1- and 3-Phosphohistidine Antibodies: New Tools to Study Histidine Phosphorylation. Cell 2015, 162, 198–210. [Google Scholar] [CrossRef]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Felix, I.; Lomada, S.K.; Barth, H.; Wieland, T. Bacillus anthracis’ PA63 Delivers the Tumor Metastasis Suppressor Protein NDPK-A/NME1 into Breast Cancer Cells. Int. J. Mol. Sci. 2020, 21, 3295. https://doi.org/10.3390/ijms21093295
Felix I, Lomada SK, Barth H, Wieland T. Bacillus anthracis’ PA63 Delivers the Tumor Metastasis Suppressor Protein NDPK-A/NME1 into Breast Cancer Cells. International Journal of Molecular Sciences. 2020; 21(9):3295. https://doi.org/10.3390/ijms21093295
Chicago/Turabian StyleFelix, Ina, Santosh K. Lomada, Holger Barth, and Thomas Wieland. 2020. "Bacillus anthracis’ PA63 Delivers the Tumor Metastasis Suppressor Protein NDPK-A/NME1 into Breast Cancer Cells" International Journal of Molecular Sciences 21, no. 9: 3295. https://doi.org/10.3390/ijms21093295
APA StyleFelix, I., Lomada, S. K., Barth, H., & Wieland, T. (2020). Bacillus anthracis’ PA63 Delivers the Tumor Metastasis Suppressor Protein NDPK-A/NME1 into Breast Cancer Cells. International Journal of Molecular Sciences, 21(9), 3295. https://doi.org/10.3390/ijms21093295