Beyond PSA: The Role of Prostate Health Index (phi)
Abstract
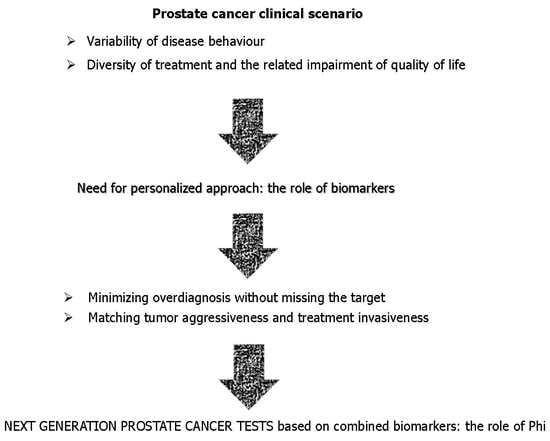
1. Background
2. The Emerging Role of Phi
3. Biopsy
4. Active Surveillance
5. PHI-Density (PHID)
6. Multi-Parametric MRI (mp-MRI)
7. Radical Prostatectomy
8. Biochemical Recurrence (BCR)
9. Comparison with Other Tests Based on Circulating Biomarkers
10. Comparison with Other Tests Based on Urinary Biomarkers
11. Limitations
12. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| DRE | digital rectal examination |
| SNP | single nucleotide polymorphism |
| HK2 | human kallikrein 2 |
| PCA3 | prostate cancer antigen 3 |
| MiPS | Mi-Prostate Score |
| TMPRRS2 | transmembrane protease, serine 2 |
| AUC | area under curve |
| DCA | decision curve analysis |
References
- Sharma, S.; Zapatero-Rodriguez, J.; O’Kennedy, R. Prostate cancer diagnostics: Clinical challenges and the ongoing need for disruptive and effective diagnostic tools. Biotechnol. Adv. 2017, 35, 135–149. [Google Scholar] [CrossRef] [PubMed]
- Carter, S.M.; Barratt, A. What is overdiagnosis and why should we take it seriously in cancer screening? Public Health Res. Pract. 2017, 27. [Google Scholar] [CrossRef] [PubMed]
- Prensner, J.R.; Rubin, M.A.; Wei, J.T.; Chinnaiyan, A.M. Beyond PSA: The next generation of prostate cancer biomarkers. Sci. Transl. Med. 2012, 4, 127rv3. [Google Scholar] [CrossRef] [PubMed]
- Kretschmer, A.; Tilki, D. Biomarkers in prostate cancer—Current clinical utility and future perspectives. Crit. Rev. Oncol. Hematol. 2017, 120, 180–193. [Google Scholar] [CrossRef] [PubMed]
- Catalona, W.J.; Bartsch, G.; Rittenhouse, H.G.; Evans, C.L.; Linton, H.J.; Horninger, W.; Klocker, H.; Mikolajczyk, S.D. Serum pro-prostate specific antigen preferentially detects aggressive prostate cancers in men with 2 to 4 ng/mL prostate specific antigen. J. Urol. 2004, 171, 2239–2244. [Google Scholar] [CrossRef] [PubMed]
- Vickers, A.J.; Cronin, A.M.; Aus, G.; Pihl, C.G.; Becker, C.; Pettersson, K.; Scardino, P.T.; Hugosson, J.; Lilja, H. A panel of kallikrein markers can reduce unnecessary biopsy for prostate cancer: Data from the European Randomized Study of Prostate Cancer Screening in Goteborg, Sweden. BMC Med. 2008, 6, 19. [Google Scholar] [CrossRef]
- Van Neste, L.; Hendriks, R.J.; Dijkstra, S.; Trooskens, G.; Cornel, E.B.; Jannink, S.A.; de Jong, H.; Hessels, D.; Smit, F.P.; Melchers, W.J.; et al. Detection of High-grade Prostate Cancer Using a Urinary Molecular Biomarker-Based Risk Score. Eur. Urol. 2016, 70, 740–748. [Google Scholar] [CrossRef]
- Tomlins, S.A.; Day, J.R.; Lonigro, R.J.; Hovelson, D.H.; Siddiqui, J.; Kunju, L.P.; Dunn, R.L.; Meyer, S.; Hodge, P.; Groskopf, J.; et al. Urine TMPRSS2:ERG Plus PCA3 for Individualized Prostate Cancer Risk Assessment. Eur. Urol. 2016, 70, 45–53. [Google Scholar] [CrossRef]
- McKiernan, J.; Donovan, M.J.; O’Neill, V.; Bentink, S.; Noerholm, M.; Belzer, S.; Skog, J.; Kattan, M.W.; Partin, A.; Andriole, G.; et al. A Novel Urine Exosome Gene Expression Assay to Predict High-grade Prostate Cancer at Initial Biopsy. JAMA Oncol. 2016, 2, 882–889. [Google Scholar] [CrossRef]
- Nilsson, O.; Peter, A.; Andersson, I.; Nilsson, K.; Grundstrom, B.; Karlsson, B. Antigenic determinants of prostate-specific antigen (PSA) and development of assays specific for different forms of PSA. Br. J. Cancer 1997, 75, 789–797. [Google Scholar] [CrossRef][Green Version]
- Mikolajczyk, S.D.; Marker, K.M.; Millar, L.S.; Kumar, A.; Saedi, M.S.; Payne, J.K.; Evans, C.L.; Gasior, C.L.; Linton, H.J.; Carpenter, P.; et al. A truncated precursor form of prostate-specific antigen is a more specific serum marker of prostate cancer. Cancer Res. 2001, 61, 6958–6963. [Google Scholar]
- Balk, S.P.; Ko, Y.J.; Bubley, G.J. Biology of prostate-specific antigen. J. Clin. Oncol. 2003, 21, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Sokoll, L.J.; Sanda, M.G.; Feng, Z.; Kagan, J.; Mizrahi, I.A.; Broyles, D.L.; Partin, A.W.; Srivastava, S.; Thompson, I.M.; Wei, J.T.; et al. A prospective, multicenter, National Cancer Institute Early Detection Research Network study of [-2]proPSA: Improving prostate cancer detection and correlating with cancer aggressiveness. Cancer Epidemiol. Biomarkers Prev. 2010, 19, 1193–1200. [Google Scholar] [CrossRef] [PubMed]
- Catalona, W.J.; Partin, A.W.; Sanda, M.G.; Wei, J.T.; Klee, G.G.; Bangma, C.H.; Slawin, K.M.; Marks, L.S.; Loeb, S.; Broyles, D.L.; et al. A multicenter study of [-2]pro-prostate specific antigen combined with prostate specific antigen and free prostate specific antigen for prostate cancer detection in the 2.0 to 10.0 ng/mL prostate specific antigen range. J. Urol. 2011, 185, 1650–1655. [Google Scholar] [CrossRef] [PubMed]
- Recker, F.; Kwiatkowski, M.K.; Piironen, T.; Pettersson, K.; Goepel, M.; Tscholl, R. Free-to-total prostate-specific antigen (PSA) ratio improves the specificity for detecting prostate cancer in patients with prostatism and intermediate PSA levels. Br. J. Urol. 1998, 81, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Li, Z.Z.; Huang, Y.L.; Song, H.J.; Wang, Y.J. Value of free/total prostate-specific antigen (f/t PSA) ratios for prostate cancer detection in patients with total serum prostate-specific antigen between 4 and 10 ng/mL: A meta-analysis. Medicine 2018, 97, e0249. [Google Scholar] [CrossRef]
- Loeb, S.; Sanda, M.G.; Broyles, D.L.; Shin, S.S.; Bangma, C.H.; Wei, J.T.; Partin, A.W.; Klee, G.G.; Slawin, K.M.; Marks, L.S.; et al. The prostate health index selectively identifies clinically significant prostate cancer. J. Urol. 2015, 193, 1163–1169. [Google Scholar] [CrossRef]
- Ferro, M.; Bruzzese, D.; Perdona, S.; Mazzarella, C.; Marino, A.; Sorrentino, A.; Di Carlo, A.; Autorino, R.; Di Lorenzo, G.; Buonerba, C.; et al. Predicting prostate biopsy outcome: Prostate health index (phi) and prostate cancer antigen 3 (PCA3) are useful biomarkers. Clin. Chim. Acta 2012, 413, 1274–1278. [Google Scholar] [CrossRef]
- Bruzzese, D.; Mazzarella, C.; Ferro, M.; Perdona, S.; Chiodini, P.; Perruolo, G.; Terracciano, D. Prostate health index vs percent free prostate-specific antigen for prostate cancer detection in men with “gray” prostate-specific antigen levels at first biopsy: Systematic review and meta-analysis. Transl. Res. 2014, 164, 444–451. [Google Scholar] [CrossRef]
- Ferro, M.; Bruzzese, D.; Perdona, S.; Marino, A.; Mazzarella, C.; Perruolo, G.; D’Esposito, V.; Cosimato, V.; Buonerba, C.; Di Lorenzo, G.; et al. Prostate Health Index (Phi) and Prostate Cancer Antigen 3 (PCA3) significantly improve prostate cancer detection at initial biopsy in a total PSA range of 2–10 ng/mL. PLoS ONE 2013, 8, e67687. [Google Scholar] [CrossRef]
- Tosoian, J.J.; Loeb, S.; Feng, Z.; Isharwal, S.; Landis, P.; Elliot, D.J.; Veltri, R.; Epstein, J.I.; Partin, A.W.; Carter, H.B.; et al. Association of [-2]proPSA with biopsy reclassification during active surveillance for prostate cancer. J. Urol. 2012, 188, 1131–1136. [Google Scholar] [CrossRef] [PubMed]
- Hirama, H.; Sugimoto, M.; Ito, K.; Shiraishi, T.; Kakehi, Y. The impact of baseline [-2]proPSA-related indices on the prediction of pathological reclassification at 1 year during active surveillance for low-risk prostate cancer: The Japanese multicenter study cohort. J. Cancer Res. Clin. Oncol. 2014, 140, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Wang, M.; Wang, L.; Adams, T.S.; Tian, Y.; Xu, J. Diagnostic ability of %p2PSA and prostate health index for aggressive prostate cancer: A meta-analysis. Sci. Rep. 2014, 4, 5012. [Google Scholar] [CrossRef] [PubMed]
- Lazzeri, M.; Haese, A.; Abrate, A.; de la Taille, A.; Redorta, J.P.; McNicholas, T.; Lughezzani, G.; Lista, G.; Larcher, A.; Bini, V.; et al. Clinical performance of serum prostate-specific antigen isoform [-2]proPSA (p2PSA) and its derivatives, %p2PSA and the prostate health index (PHI), in men with a family history of prostate cancer: Results from a multicentre European study, the PROMEtheuS project. BJU Int. 2013, 112, 313–321. [Google Scholar]
- Chiu, P.K.; Ng, C.F.; Semjonow, A.; Zhu, Y.; Vincendeau, S.; Houlgatte, A.; Lazzeri, M.; Guazzoni, G.; Stephan, C.; Haese, A.; et al. A Multicentre Evaluation of the Role of the Prostate Health Index (PHI) in Regions with Differing Prevalence of Prostate Cancer: Adjustment of PHI Reference Ranges is Needed for European and Asian Settings. Eur. Urol. 2019, 75, 558–561. [Google Scholar] [CrossRef]
- Tosoian, J.J.; Druskin, S.C.; Andreas, D.; Mullane, P.; Chappidi, M.; Joo, S.; Ghabili, K.; Mamawala, M.; Agostino, J.; Carter, H.B.; et al. Prostate Health Index density improves detection of clinically significant prostate cancer. BJU Int. 2017, 120, 793–798. [Google Scholar] [CrossRef]
- Druskin, S.C.; Tosoian, J.J.; Young, A.; Collica, S.; Srivastava, A.; Ghabili, K.; Macura, K.J.; Carter, H.B.; Partin, A.W.; Sokoll, L.J.; et al. Combining Prostate Health Index density, magnetic resonance imaging and prior negative biopsy status to improve the detection of clinically significant prostate cancer. BJU Int. 2018, 121, 619–626. [Google Scholar] [CrossRef]
- Vos, E.K.; Kobus, T.; Litjens, G.J.; Hambrock, T.; Hulsbergen-van de Kaa, C.A.; Barentsz, J.O.; Maas, M.C.; Scheenen, T.W. Multiparametric Magnetic Resonance Imaging for Discriminating Low-Grade From High-Grade Prostate Cancer. Investig. Radiol. 2015, 50, 490–497. [Google Scholar] [CrossRef]
- Gnanapragasam, V.J.; Burling, K.; George, A.; Stearn, S.; Warren, A.; Barrett, T.; Koo, B.; Gallagher, F.A.; Doble, A.; Kastner, C.; et al. The Prostate Health Index adds predictive value to multi-parametric MRI in detecting significant prostate cancers in a repeat biopsy population. Sci. Rep. 2016, 6, 35364. [Google Scholar] [CrossRef]
- Hsieh, P.F.; Li, W.J.; Lin, W.C.; Chang, H.; Chang, C.H.; Huang, C.P.; Yang, C.R.; Chen, W.C.; Chang, Y.H.; Wu, H.C. Combining prostate health index and multiparametric magnetic resonance imaging in the diagnosis of clinically significant prostate cancer in an Asian population. World J. Urol. 2019. [Google Scholar] [CrossRef]
- Futterer, J.J.; Briganti, A.; De Visschere, P.; Emberton, M.; Giannarini, G.; Kirkham, A.; Taneja, S.S.; Thoeny, H.; Villeirs, G.; Villers, A. Can Clinically Significant Prostate Cancer Be Detected with Multiparametric Magnetic Resonance Imaging? A Systematic Review of the Literature. Eur. Urol. 2015, 68, 1045–1053. [Google Scholar] [CrossRef]
- Guazzoni, G.; Lazzeri, M.; Nava, L.; Lughezzani, G.; Larcher, A.; Scattoni, V.; Gadda, G.M.; Bini, V.; Cestari, A.; Buffi, N.M.; et al. Preoperative prostate-specific antigen isoform p2PSA and its derivatives, %p2PSA and prostate health index, predict pathologic outcomes in patients undergoing radical prostatectomy for prostate cancer. Eur. Urol. 2012, 61, 455–466. [Google Scholar] [CrossRef]
- Ferro, M.; Lucarelli, G.; Bruzzese, D.; Perdona, S.; Mazzarella, C.; Perruolo, G.; Marino, A.; Cosimato, V.; Giorgio, E.; Tagliamonte, V.; et al. Improving the prediction of pathologic outcomes in patients undergoing radical prostatectomy: The value of prostate cancer antigen 3 (PCA3), prostate health index (phi) and sarcosine. Anticancer Res. 2015, 35, 1017–1023. [Google Scholar]
- Tosoian, J.J.; Druskin, S.C.; Andreas, D.; Mullane, P.; Chappidi, M.; Joo, S.; Ghabili, K.; Agostino, J.; Macura, K.J.; Carter, H.B.; et al. Use of the Prostate Health Index for detection of prostate cancer: Results from a large academic practice. Prostate Cancer Prostatic Dis. 2017, 20, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Cantiello, F.; Russo, G.I.; Cicione, A.; Ferro, M.; Cimino, S.; Favilla, V.; Perdona, S.; De Cobelli, O.; Magno, C.; Morgia, G.; et al. PHI and PCA3 improve the prognostic performance of PRIAS and Epstein criteria in predicting insignificant prostate cancer in men eligible for active surveillance. World J. Urol. 2016, 34, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Heidegger, I.; Klocker, H.; Pichler, R.; Pircher, A.; Prokop, W.; Steiner, E.; Ladurner, C.; Comploj, E.; Lunacek, A.; Djordjevic, D.; et al. ProPSA and the Prostate Health Index as predictive markers for aggressiveness in low-risk prostate cancer-results from an international multicenter study. Prostate Cancer Prostatic Dis. 2017, 20, 271–275. [Google Scholar] [CrossRef]
- Cheng, Y.T.; Huang, C.Y.; Chen, C.H.; Chiu, S.T.; Hong, J.H.; Pu, Y.S.; Liu, S.P.; Lu, Y.C.; Chang, Y.K.; Chang, H.C.; et al. Preoperative %p2PSA and Prostate Health Index Predict Pathological Outcomes in Patients with Prostate Cancer Undergoing Radical Prostatectomy. Sci. Rep. 2020, 10, 776. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Lee, S.W.; Song, G.; Kang, T.W.; Jung, J.H.; Chung, H.C.; Kim, S.J.; Park, J.Y.; Shin, T.Y.; Kim, J.H. Preoperative prostate health index and %p2PSA as the significant biomarkers of postoperative pathological outcomes of prostate cancer in Korean males: A prospective multi-institutional study. Investig. Clin. Urol. 2020, 61, 42–50. [Google Scholar] [CrossRef]
- Dolejsova, O.; Kucera, R.; Fuchsova, R.; Topolcan, O.; Svobodova, H.; Hes, O.; Eret, V.; Pecen, L.; Hora, M. The Ability of Prostate Health Index (PHI) to Predict Gleason Score in Patients With Prostate Cancer and Discriminate Patients Between Gleason Score 6 and Gleason Score Higher Than 6-A Study on 320 Patients After Radical Prostatectomy. Technol. Cancer Res. Treat 2018, 17, 1533033818787377. [Google Scholar] [CrossRef]
- Lughezzani, G.; Lazzeri, M.; Buffi, N.M.; Abrate, A.; Mistretta, F.A.; Hurle, R.; Pasini, L.; Castaldo, L.; Zandegiacomo De Zorzi, S.; Peschechera, R.; et al. Preoperative prostate health index is an independent predictor of early biochemical recurrence after radical prostatectomy: Results from a prospective single-center study. Urol. Oncol. 2015, 33, 337.e7–337.e14. [Google Scholar] [CrossRef]
- Maxeiner, A.; Kilic, E.; Matalon, J.; Friedersdorff, F.; Miller, K.; Jung, K.; Stephan, C.; Busch, J. The prostate health index PHI predicts oncological outcome and biochemical recurrence after radical prostatectomy—Analysis in 437 patients. Oncotarget 2017, 8, 79279–79288. [Google Scholar] [CrossRef] [PubMed]
- Punnen, S.; Pavan, N.; Parekh, D.J. Finding the Wolf in Sheep’s Clothing: The 4Kscore Is a Novel Blood Test That Can Accurately Identify the Risk of Aggressive Prostate Cancer. Rev. Urol. 2015, 17, 3–13. [Google Scholar]
- Nordstrom, T.; Vickers, A.; Assel, M.; Lilja, H.; Gronberg, H.; Eklund, M. Comparison Between the Four-kallikrein Panel and Prostate Health Index for Predicting Prostate Cancer. Eur. Urol. 2015, 68, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Russo, G.I.; Regis, F.; Castelli, T.; Favilla, V.; Privitera, S.; Giardina, R.; Cimino, S.; Morgia, G. A Systematic Review and Meta-analysis of the Diagnostic Accuracy of Prostate Health Index and 4-Kallikrein Panel Score in Predicting Overall and High-grade Prostate Cancer. Clin. Genitourin Cancer 2017, 15, 429–439.e1. [Google Scholar] [CrossRef] [PubMed]
- Gronberg, H.; Adolfsson, J.; Aly, M.; Nordstrom, T.; Wiklund, P.; Brandberg, Y.; Thompson, J.; Wiklund, F.; Lindberg, J.; Clements, M.; et al. Prostate cancer screening in men aged 50–69 years (STHLM3): A prospective population-based diagnostic study. Lancet Oncol. 2015, 16, 1667–1676. [Google Scholar] [CrossRef]
- Strom, P.; Nordstrom, T.; Aly, M.; Egevad, L.; Gronberg, H.; Eklund, M. The Stockholm-3 Model for Prostate Cancer Detection: Algorithm Update, Biomarker Contribution, and Reflex Test Potential. Eur. Urol. 2018, 74, 204–210. [Google Scholar] [CrossRef]
- Gronberg, H.; Eklund, M.; Picker, W.; Aly, M.; Jaderling, F.; Adolfsson, J.; Landquist, M.; Haug, E.S.; Strom, P.; Carlsson, S.; et al. Prostate Cancer Diagnostics Using a Combination of the Stockholm3 Blood Test and Multiparametric Magnetic Resonance Imaging. Eur. Urol. 2018, 74, 722–728. [Google Scholar] [CrossRef]
- Gallotta, A.; Giannarini, G.; Laurini, L.; Zani, D.; Garbeglio, A.; Guazzieri, S.; Plebani, M.; Fassina, G.; Zattoni, F. Clinical validation of the iXip index in avoiding unnecessary prostate biopsy: Results from a prospective multicenter study involving 426 patients. Cancer Treat. Res. Commun. 2017, 10, 40–45. [Google Scholar] [CrossRef]
- Galosi, A.B.; Dell’Atti, L.; Bertaccini, A.; Gion, M.; Francavilla, S.; Ferretti, S.; Maestroni, U.; Gallotta, A.; Parrozzani, C.; Paneghetti, L.; et al. Clinical evaluation of the iXip index to reduce prostate re-biopsies. Cancer Treat. Res. Commun. 2018, 16, 59–63. [Google Scholar] [CrossRef]
- Fujita, K.; Nonomura, N. Urinary biomarkers of prostate cancer. Int. J. Urol. 2018, 25, 770–779. [Google Scholar] [CrossRef]
- Martignano, F.; Rossi, L.; Maugeri, A.; Galla, V.; Conteduca, V.; De Giorgi, U.; Casadio, V.; Schepisi, G. Urinary RNA-based biomarkers for prostate cancer detection. Clin. Chim. Acta 2017, 473, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Cao, W.; Li, Q.; Shen, H.; Liu, C.; Deng, J.; Xu, J.; Shao, Q. Evaluation of prostate cancer antigen 3 for detecting prostate cancer: A systematic review and meta-analysis. Sci. Rep. 2016, 6, 25776. [Google Scholar] [CrossRef] [PubMed]
- Scattoni, V.; Lazzeri, M.; Lughezzani, G.; De Luca, S.; Passera, R.; Bollito, E.; Randone, D.; Abdollah, F.; Capitanio, U.; Larcher, A.; et al. Head-to-head comparison of prostate health index and urinary PCA3 for predicting cancer at initial or repeat biopsy. J. Urol. 2013, 190, 496–501. [Google Scholar] [CrossRef]
- Cantiello, F.; Russo, G.I.; Ferro, M.; Cicione, A.; Cimino, S.; Favilla, V.; Perdona, S.; Bottero, D.; Terracciano, D.; De Cobelli, O.; et al. Prognostic accuracy of Prostate Health Index and urinary Prostate Cancer Antigen 3 in predicting pathologic features after radical prostatectomy. Urol. Oncol. 2015, 33, 163.e15–163.e23. [Google Scholar] [CrossRef] [PubMed]
- Auprich, M.; Chun, F.K.; Ward, J.F.; Pummer, K.; Babaian, R.; Augustin, H.; Luger, F.; Gutschi, S.; Budaus, L.; Fisch, M.; et al. Critical assessment of preoperative urinary prostate cancer antigen 3 on the accuracy of prostate cancer staging. Eur. Urol. 2011, 59, 96–105. [Google Scholar] [CrossRef]
- Hessels, D.; van Gils, M.P.; van Hooij, O.; Jannink, S.A.; Witjes, J.A.; Verhaegh, G.W.; Schalken, J.A. Predictive value of PCA3 in urinary sediments in determining clinico-pathological characteristics of prostate cancer. Prostate 2010, 70, 10–16. [Google Scholar] [CrossRef]
- Sanda, M.G.; Feng, Z.; Howard, D.H.; Tomlins, S.A.; Sokoll, L.J.; Chan, D.W.; Regan, M.M.; Groskopf, J.; Chipman, J.; Patil, D.H.; et al. Association Between Combined TMPRSS2:ERG and PCA3 RNA Urinary Testing and Detection of Aggressive Prostate Cancer. JAMA Oncol. 2017, 3, 1085–1093. [Google Scholar] [CrossRef]
- Feibus, A.H.; Sartor, O.; Moparty, K.; Chagin, K.; Kattan, M.W.; Ledet, E.; Levy, J.; Lee, B.; Thomas, R.; Silberstein, J.L. Clinical Use of PCA3 and TMPRSS2:ERG Urinary Biomarkers in African-American Men Undergoing Prostate Biopsy. J. Urol. 2016, 196, 1053–1060. [Google Scholar] [CrossRef]
- Loeb, S. Time to replace prostate-specific antigen (PSA) with the Prostate Health Index (PHI)? Yet more evidence that the PHI consistently outperforms PSA across diverse populations. BJU Int. 2015, 115, 500. [Google Scholar] [CrossRef]
- Semjonow, A.; Kopke, T.; Eltze, E.; Pepping-Schefers, B.; Burgel, H.; Darte, C. Pre-analytical in-vitro stability of [-2]proPSA in blood and serum. Clin. Biochem. 2010, 43, 926–928. [Google Scholar] [CrossRef]
- Igawa, T.; Takehara, K.; Onita, T.; Ito, K.; Sakai, H. Stability of [-2]Pro-PSA in whole blood and serum: Analysis for optimal measurement conditions. J. Clin. Lab. Anal. 2014, 28, 315–319. [Google Scholar] [CrossRef] [PubMed]
- Dittadi, R.; Fabricio, A.S.C.; Rainato, G.; Peroni, E.; Di Tonno, F.; Vezzu, B.; Mazzariol, C.; Squarcina, E.; Tammone, L.; Gion, M. Preanalytical stability of [-2]proPSA in whole blood stored at room temperature before separation of serum and plasma: Implications to Phi determination. Clin. Chem. Lab. Med. 2019, 57, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Bouttell, J.; Teoh, J.; Chiu, P.K.; Chan, K.S.; Ng, C.F.; Heggie, R.; Hawkins, N. Economic evaluation of the introduction of the Prostate Health Index as a rule-out test to avoid unnecessary biopsies in men with prostate specific antigen levels of 4-10 in Hong Kong. PLoS ONE 2019, 14, e0215279. [Google Scholar] [CrossRef] [PubMed]
- Heijnsdijk, E.A.; Denham, D.; de Koning, H.J. The Cost-Effectiveness of Prostate Cancer Detection with the Use of Prostate Health Index. Value Health 2016, 19, 153–157. [Google Scholar] [CrossRef]
- Mathieu, R.; Castelli, C.; Fardoun, T.; Peyronnet, B.; Shariat, S.F.; Bensalah, K.; Vincendeau, S. Cost analysis of prostate cancer detection including the prostate health index (phi). World J. Urol. 2019, 37, 481–487. [Google Scholar] [CrossRef]
- Nichol, M.B.; Wu, J.; An, J.J.; Huang, J.; Denham, D.; Frencher, S.; Jacobsen, S.J. Budget impact analysis of a new prostate cancer risk index for prostate cancer detection. Prostate Cancer Prostatic Dis. 2011, 14, 253–261. [Google Scholar] [CrossRef]
- Nichol, M.B.; Wu, J.; Huang, J.; Denham, D.; Frencher, S.K.; Jacobsen, S.J. Cost-effectiveness of Prostate Health Index for prostate cancer detection. BJU Int. 2012, 110, 353–362. [Google Scholar] [CrossRef]
- Ablin, A.J. Prostate cancer screening. Lancet 2001, 357, 1201–1202, author reply 1201-2. [Google Scholar] [CrossRef]
- Loeb, S.; Shin, S.S.; Broyles, D.L.; Wei, J.T.; Sanda, M.; Klee, G.; Partin, A.W.; Sokoll, L.; Chan, D.W.; Bangma, C.H.; et al. Prostate Health Index improves multivariable risk prediction of aggressive prostate cancer. BJU Int. 2017, 120, 61–68. [Google Scholar] [CrossRef]
- Roobol, M.J.; Vedder, M.M.; Nieboer, D.; Houlgatte, A.; Vincendeau, S.; Lazzeri, M.; Guazzoni, G.; Stephan, C.; Semjonow, A.; Haese, A.; et al. Comparison of Two Prostate Cancer Risk Calculators that Include the Prostate Health Index. Eur. Urol Focus. 2015, 1, 185–190. [Google Scholar] [CrossRef]
| Test | Variables | Reference |
|---|---|---|
| BLOOD-BASED | ||
| Phi | [-2]proPSA, freePSA, PSA | [5] |
| 4Kscore | Age, DRE, prior negative biopsy status, PSA, freePSA, intactPSA, hK2 | [6] |
| Stockholm 3 (S3M) | Age, Family history, Previous biopsy, Prostate volume, DRE, PSA, fPSA, iPSA, HK2, beta-microseminoprotein, macrophage inhibitory cytokine, 232 SNP | [7] |
| URINE-BASED | ||
| MI-Prostate score | Serum PSA, PCA3, TMPRSS2-ERG | [8] |
| Exo-Dx | Urine PCA3, TMPRSS2-ERG exosome expression | [9] |
| Select-MDX | Age, PSA, Prostate volume, Family history, DRE, DLX1, HOXC6, KLK3, | [7] |
| Phi | 4K Score | S3M | |
|---|---|---|---|
| AUC * ranges reported for csPCa | 0.66–0.76 | 0.67–0.77 | 0.73–0.77 |
| Cost | 120 € | 300 € | Estimated > 200 € |
| Calculated as | Mathematical Model | Algorithm | Algorithm |
| Availability | FDA-approved and CE-mark | CLIA-approved | For clinical use only in Sweden |
| Outcome | Authors, Year | Sample Size | Study Design | Reference |
|---|---|---|---|---|
| Detecting PCa at biopsy | Catalona et al., 2011 | 892 | Prospective, multicenter | [68] |
| Ferro et al., 2012 | 251 | prospective | [18] | |
| Loeb et al., 2015 | 658 | Prospective, multicenter | [17] | |
| Chiu et al., 2019 | 1652 | Prospective, multicenter | [25] | |
| Predicting aggressiveness at RP | Guazzoni, 2012 | 350 | prospective | [32] |
| Ferro, 2015 | 78 | prospective | [33] | |
| Cantiello, 2016 | 188 | retrospective | [35] | |
| Tosoian, 2017 | 1663 | prospective | [26] | |
| Dolejsova, 2018 | 320 | prospective | [39] | |
| Selecting and reclassifying patients for AS | Tosoian, 2012 | 167 | Follow-up AS | [21] |
| Ferro, 2013 | 300 | prospective | [20] | |
| Hirama, 2015 | 118 | Follow-up AS | [22] | |
| Predicting BCR | Lughezzani, 2015 | 313 | Follow-up after RARP | [40] |
| Maxeiner, 2017 | 437 | Follow-up after RP | [41] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferro, M.; De Cobelli, O.; Lucarelli, G.; Porreca, A.; Busetto, G.M.; Cantiello, F.; Damiano, R.; Autorino, R.; Musi, G.; Vartolomei, M.D.; et al. Beyond PSA: The Role of Prostate Health Index (phi). Int. J. Mol. Sci. 2020, 21, 1184. https://doi.org/10.3390/ijms21041184
Ferro M, De Cobelli O, Lucarelli G, Porreca A, Busetto GM, Cantiello F, Damiano R, Autorino R, Musi G, Vartolomei MD, et al. Beyond PSA: The Role of Prostate Health Index (phi). International Journal of Molecular Sciences. 2020; 21(4):1184. https://doi.org/10.3390/ijms21041184
Chicago/Turabian StyleFerro, Matteo, Ottavio De Cobelli, Giuseppe Lucarelli, Angelo Porreca, Gian Maria Busetto, Francesco Cantiello, Rocco Damiano, Riccardo Autorino, Gennaro Musi, Mihai Dorin Vartolomei, and et al. 2020. "Beyond PSA: The Role of Prostate Health Index (phi)" International Journal of Molecular Sciences 21, no. 4: 1184. https://doi.org/10.3390/ijms21041184
APA StyleFerro, M., De Cobelli, O., Lucarelli, G., Porreca, A., Busetto, G. M., Cantiello, F., Damiano, R., Autorino, R., Musi, G., Vartolomei, M. D., Muto, M., & Terracciano, D. (2020). Beyond PSA: The Role of Prostate Health Index (phi). International Journal of Molecular Sciences, 21(4), 1184. https://doi.org/10.3390/ijms21041184