Bone Marrow-Derived Mononuclear Cell Transplants Decrease Retinal Gliosis in Two Animal Models of Inherited Photoreceptor Degeneration
Abstract
1. Introduction
2. Results
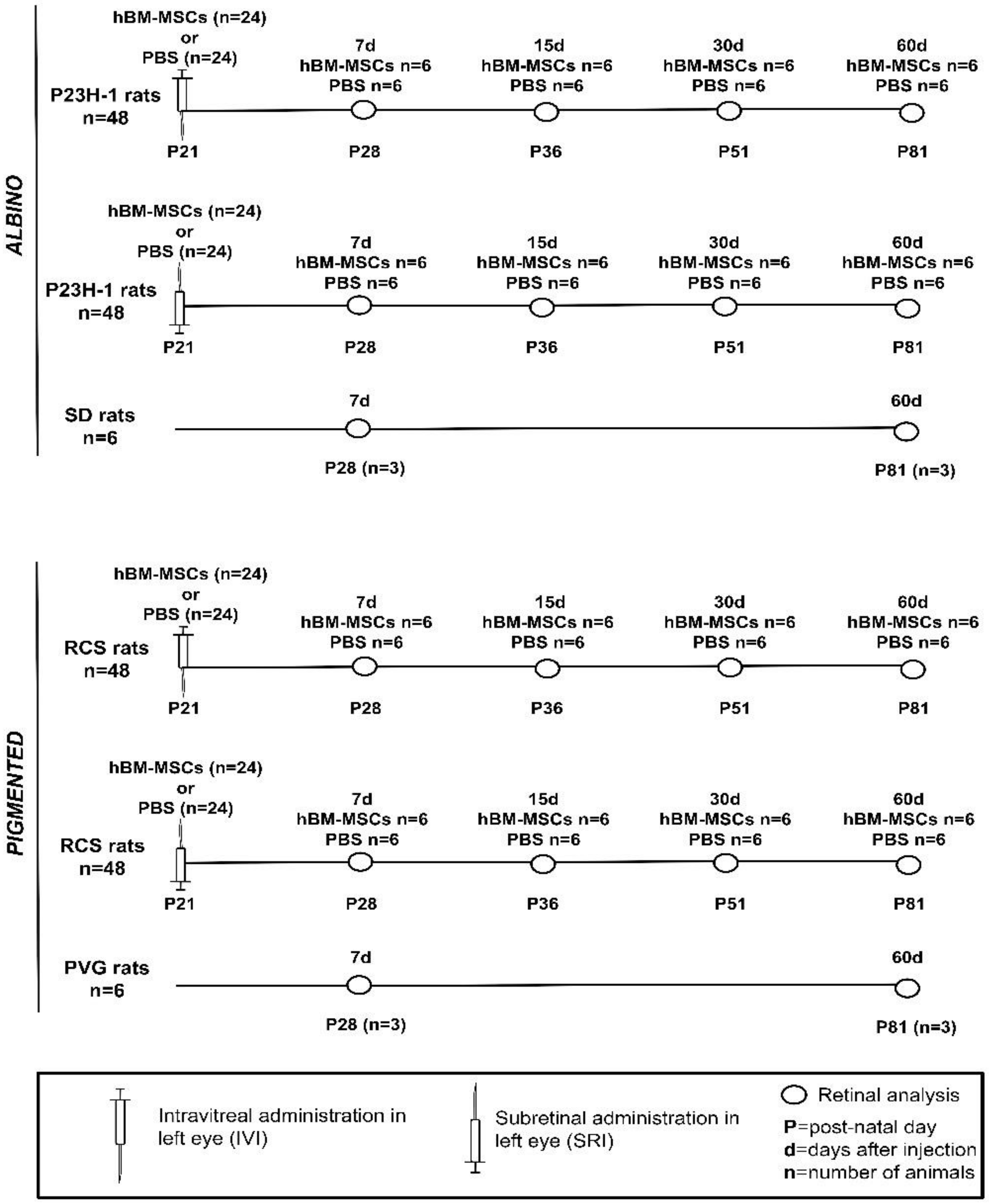
2.1. Safety and Feasibility of Intravitreal and Subretinal Injections
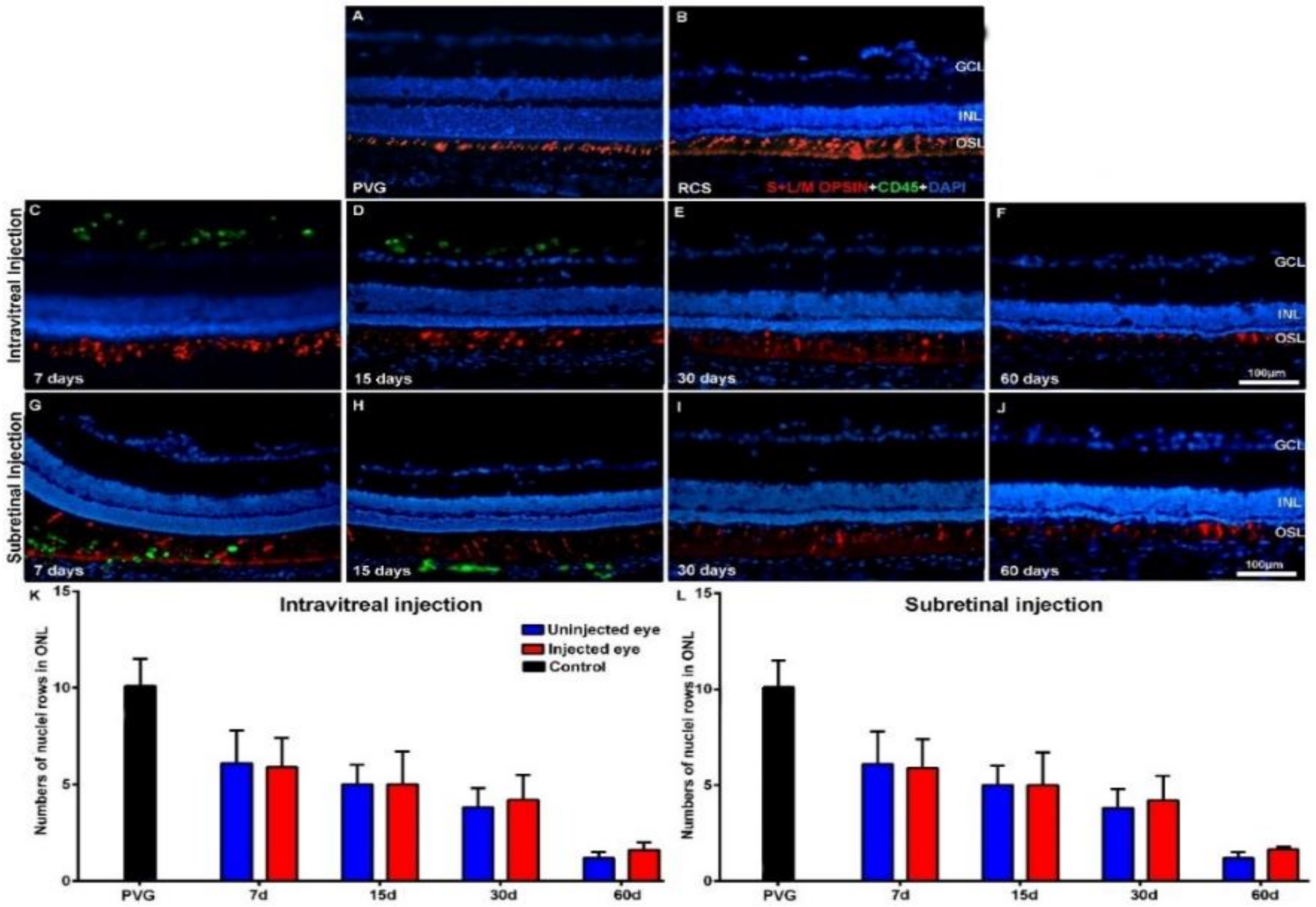
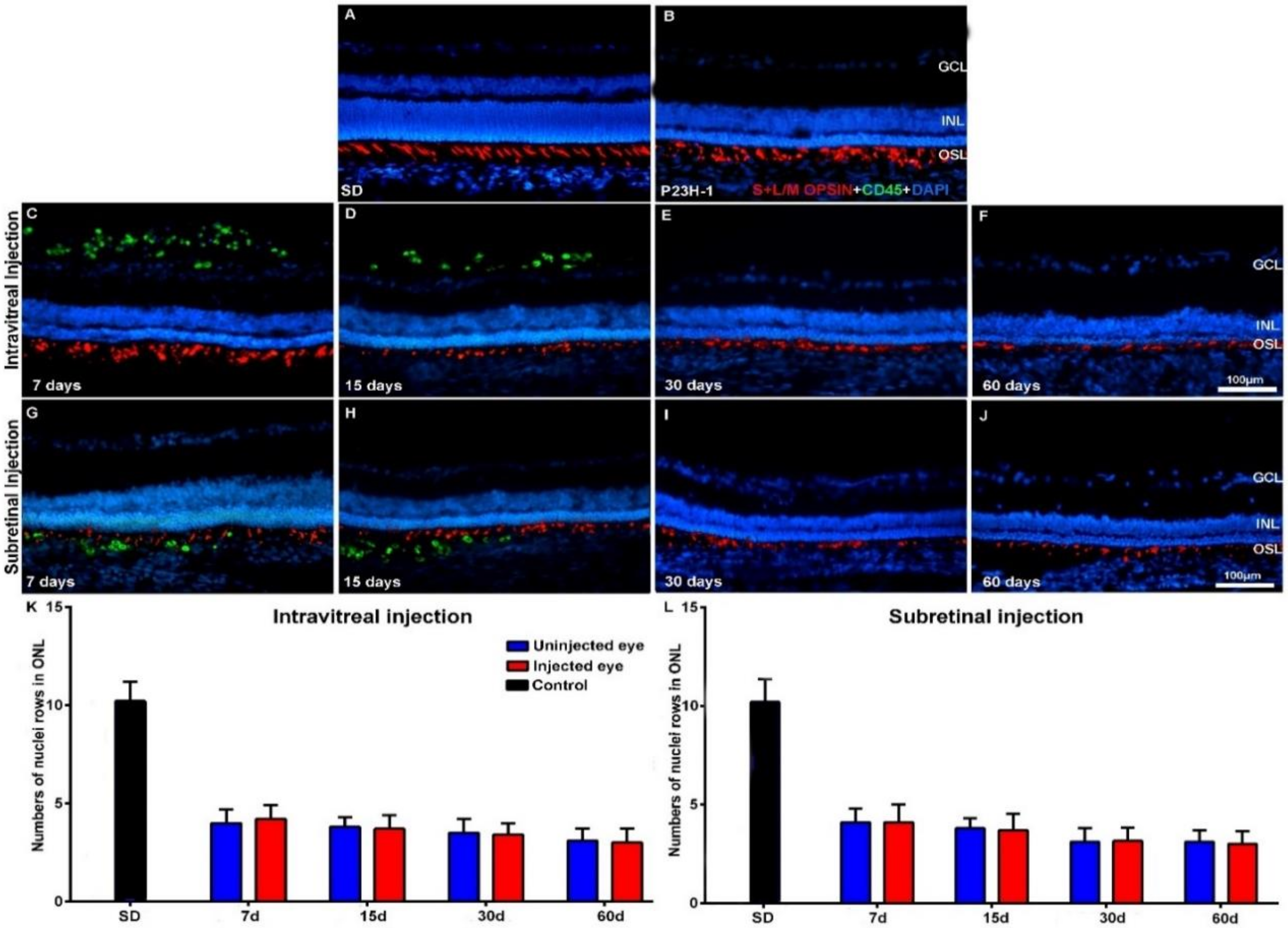
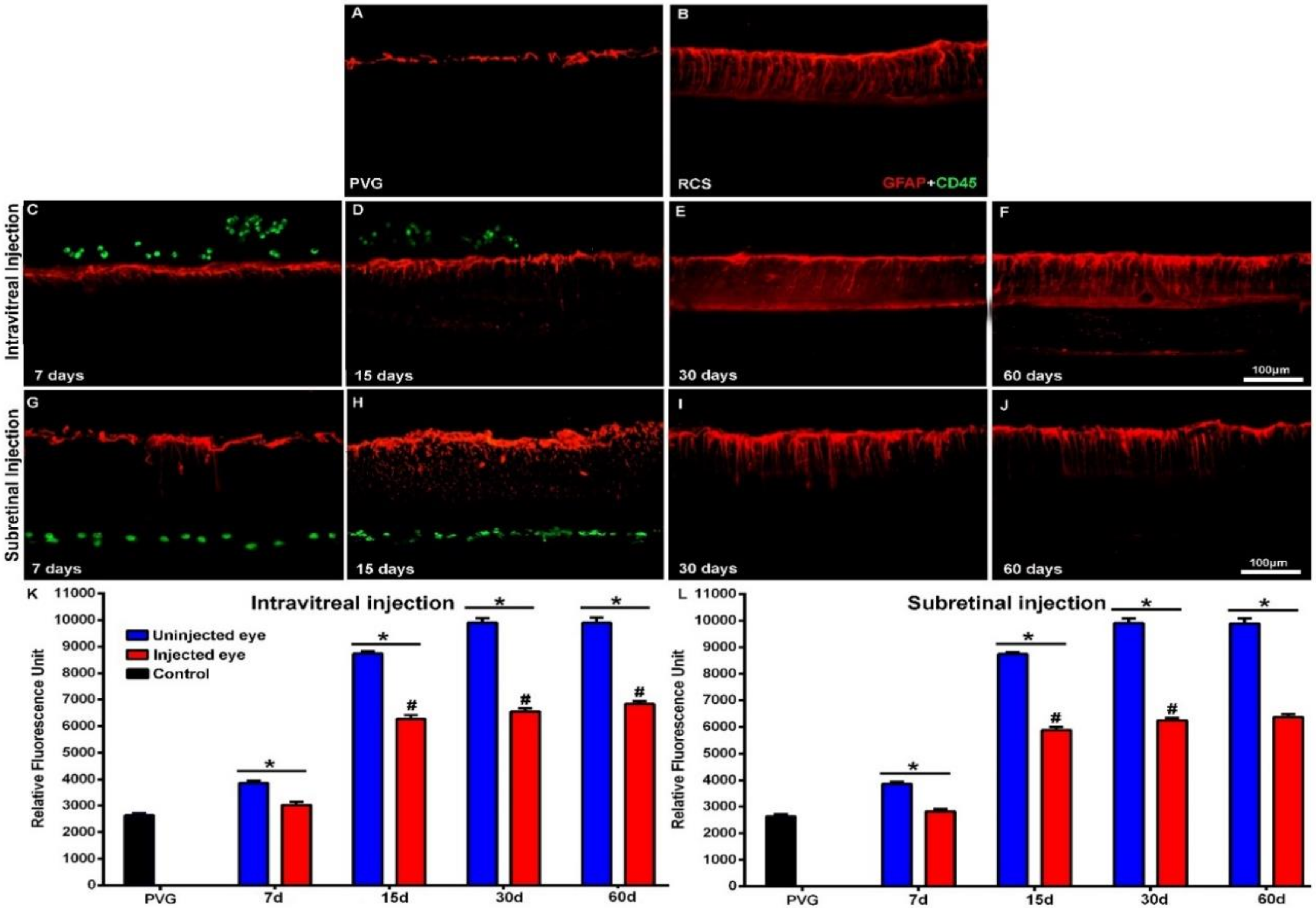
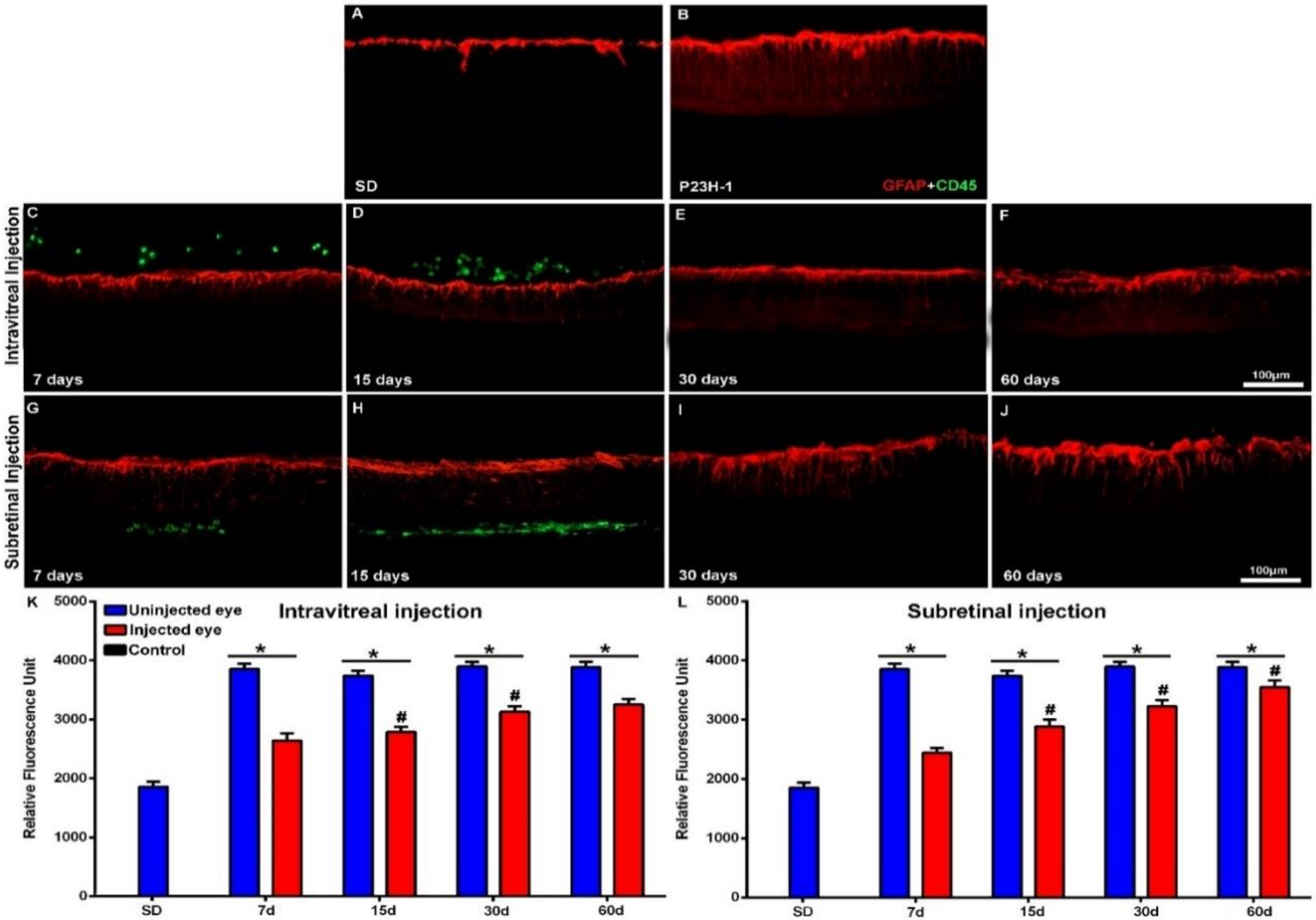
2.2. Effect of Intravitreal and Subretinal Injections in Photoreceptor Degeneration and Retinal Gliosis
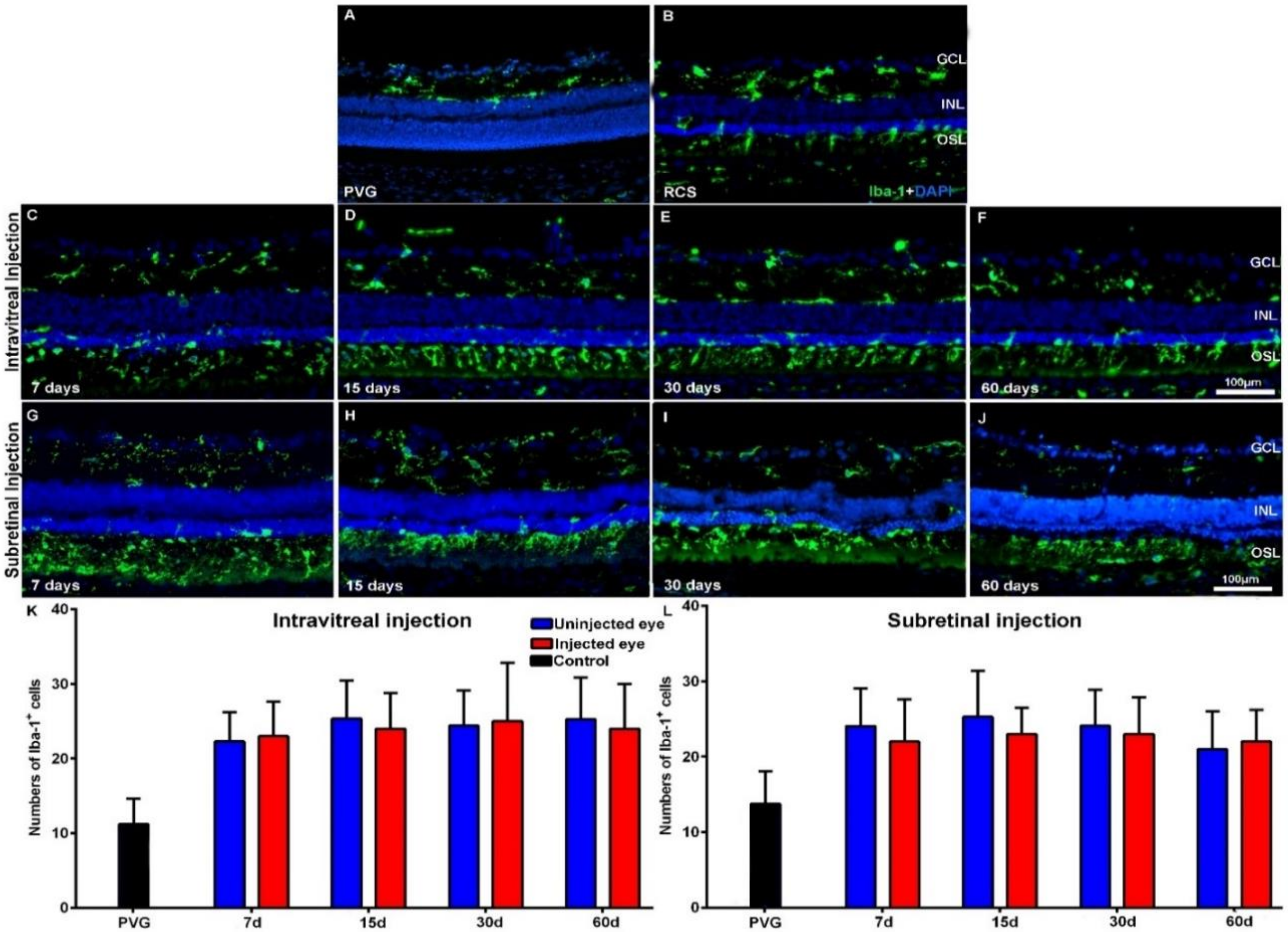
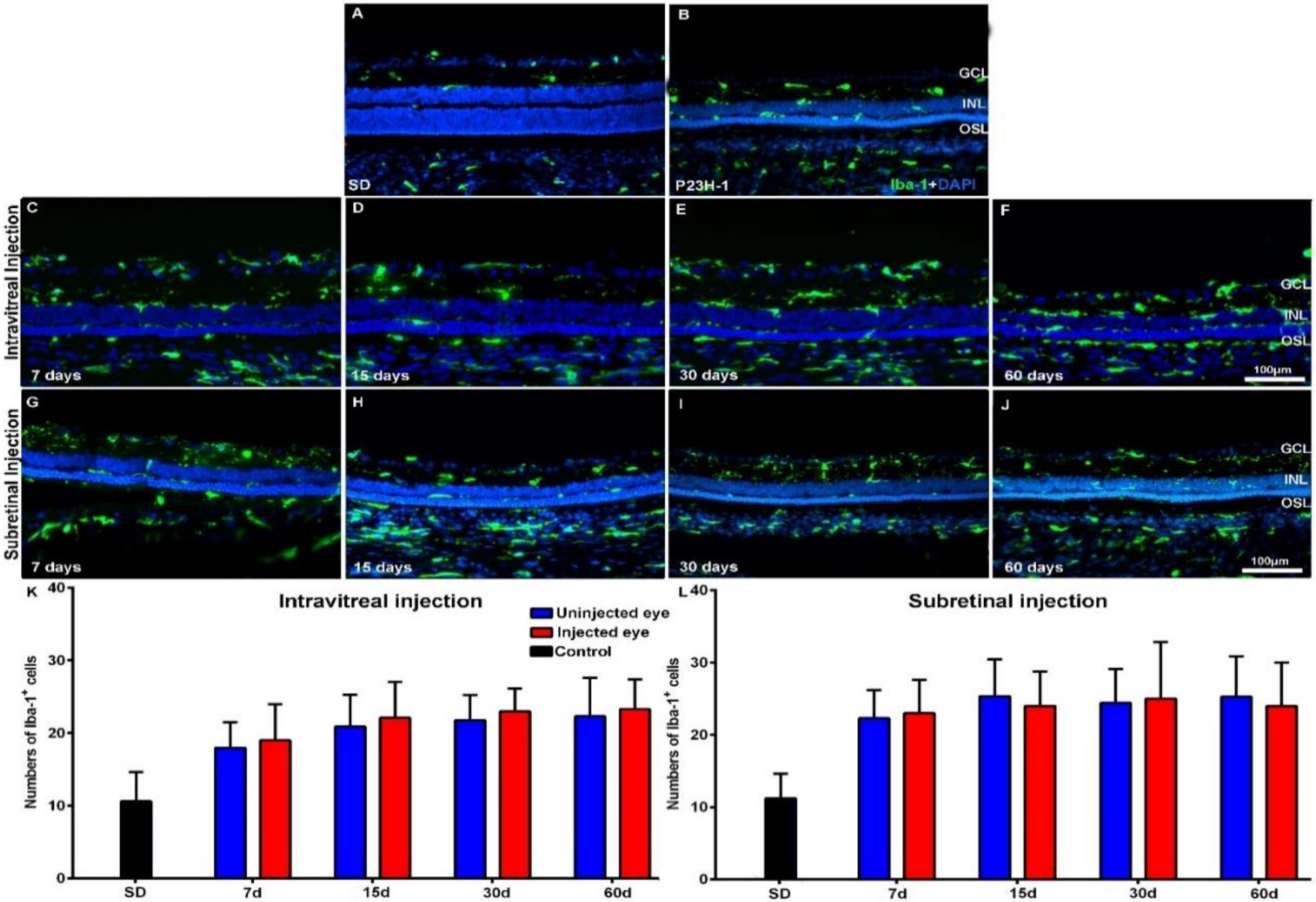
2.3. Effect of Intravitreal and Subretinal Injections in the Retinal Microglial Cells
2.4. Effect of Intravitreal and Subretinal Injections in the Retinal Macroglial Cells
3. Discussion
4. Material and Methods
4.1. Animals
4.2. Human Bone-Marrow-Derived Mononuclear Cell Isolation
4.3. Cell Transplantation
4.4. Tissue Processing
Immunohistofluorescence
4.5. Antibodies
4.6. Image Analysis
4.7. Quantification of Nuclei rows, Microglial Cells and GFAP Expression
4.8. Statistics
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Nuclei Rows in ONL | Intravitreal Injection | Subretinal Injection | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Days | Control n = 6 (FTSS) | Right Eyes n = 12 (FTSS) | PBS n = 6 (FTSS) | hBM-MSCs n = 6 (FTSS) | Right Eyes n = 12 (FTSS) | PBS n = 6 (FTSS) | hBM-MSCs n = 6 (FTSS) | |||||||
| PVG | SD | RCS | P23H-1 | RCS | P23H-1 | RCS | P23H-1 | RCS | P23H-1 | RCS | P23H-1 | RCS | P23H-1 | |
| 28 (7) | 10.4 ± 1.2 | 10.2 ± 1.1 | 6.1 ± 1.7 ◊,† | 4 ± 1 ◊,† | 6.7 ± 1.2◊,† | 4.5 ± 1.3 ◊,† | 5.9 ± 1.5 ◊,† | 4.2 ± 0.8 ◊,† | 6.3 ± 1.4 ◊,† | 4.1 ± 0.7◊,† | 6.2 ± 1.4 ◊,† | 3.9 ± 1 ◊,† | 5.7 ± 1.4 ◊,† | 4.1 ± 0.9 ◊,† |
| 36 (15) | 5 ± 1 ◊ | 3.8 ± 0.7 ◊ | 5.2 ± 1.4◊ | 3.5 ± 0.9 ◊ | 5.1 ± 1.7 ◊ | 3.7 ± 0.8 ◊ | 5.5 ± 1 ◊ | 3.8 ± 0.5 ◊ | 5 ± 1.7 ◊ | 3.1 ± 0.8 ◊ | 5 ± 2.1 ◊ | 3.7 ± 1.2 ◊ | ||
| 51 (30) | 3.8 ± 0.9 ○ | 3.5 ± 0.5 ○ | 4.6 ± 1.5○,◊ | 3.2 ± 0.4 ○,◊ | 4.2 ± 1.3 ○,◊ | 3.4 ± 0.6 ○,◊ | 3.4 ± 1.2 ○,□,◊ | 3.1 ± 0.8 ○,◊ | 3.7 ± 1.1 ○,◊ | 2.7 ± 0.5 ○,◊ | 4.6 ± 1.4 ○,◊ | 3.2 ± 0.9 ○,◊ | ||
| 81 (60) | 10.1 ± 1 | 10.4 ± 1.2 | 1.2 ± 0.3 ○,◊,† | 3.1 ± 0.8 ○,◊,† | 1.5 ± 0.5○□◊,† | 2.8 ± 0.6 ○,◊,† | 1.6 ± 0.4 ○,□,◊,† | 3 ± 0.7 ○,◊,† | 1.3 ± 0.5 ○,□,◊,† | 2.9 ± 0.6 ○,◊,† | 1.4 ± 0.3 ○,□,◊,† | 2 ± 0.7 ○,◊,† | 1.5 ± 0.2 ○,□,◊,† | 3 ± 0.8 ○,◊,† |
| Iba-1+ cells | ||||||||||||||
| 28 (7) | 11.3 ± 6.2 | 10.6 ± 4 | 22.5 ± 3.9 † | 18 ± 3.5 † | 23.5 ± 4.1 † | 17 ± 4.5 † | 23.4 ± 5.6 † | 19 ± 5 † | 24.1 ± 5 † | 22.3 ± 3.9 † | 22.8 ± 5 † | 19 ± 3.9 † | 22 ± 6.2 † | 23 ± 3.6 † |
| 36 (15) | 26.4 ± 4.3 | 20.9 ± 4.4 | 24.5 ± 5.1 | 21.2 ± 4.1 | 23.8 ± 3.5 | 22.1 ± 4.9 | 26.3 ± 6.1 | 25.3 ± 5.1 | 23.9 ± 4.9 | 22.9 ± 4.9 | 23.5 ± 3.8 | 24.3 ± 4.7 | ||
| 51 (30) | 25.1 ± 5.1 | 21.75 ± 3.5 | 26.4 ± 6.2 | 23.6 ± 4.6 | 25 ± 4.9 | 23 ± 3.1 | 24.4 ± 4.8 | 24.4 ± 4.7 | 25.9 ± 5.3 | 24.3 ± 4.2 | 23.2 ± 5.1 | 25.5 ± 7.9 | ||
| 81 (60) | 13.7 ± 4.7 | 14 ± 4.7 | 24.9 ± 6 † | 22.3 ± 5.3 † | 27.1 ± 5.8 † | 23.9 ± 5.1 † | 24.4 ± 4.2 † | 23.3 ± 4.1 † | 21 ± 5 † | 25.2 ± 5.6 † | 26.7 ± 5.7 † | 24.9 ± 4.9 † | 22 ± 4.7 † | 24 ± 6.1 † |
| RFU (GFAP expression) | ||||||||||||||
| 28 (7) | 1567 ± 8.7 | 1736 ± 96 | 3856 ± 90 † | 3987 ± 99 † | 3767 ± 102 ◊,† | 3905 ± 88 ◊,† | 3025 ± 120 ◊,*,†,€ | 2644 ± 125 ◊,*,†,€ | 3861 ± 88 † | 3799 ± 98 † | 3955 ± 95 † | 3832 ± 73 † | 2825 ± 93◊*†€ | 2444 ± 80 ◊,*,†,€ |
| 36 (15) | 8741 ± 85 ○,◊ | 3738 ± 85 ◊ | 8978 ± 112 ○,◊ | 3882 ± 102 ◊ | 6273 ± 145 ○,*,□,◊,€ | 2788 ± 87 *,□,◊,€ | 8758 ± 121 ○,◊ | 3679 ± 89 ◊ | 8797 ± 103 ○,◊ | 3922 ± 88◊ | 5880 ± 113 ○,*,□,◊,€ | 2888 ± 120 ○,*,□,◊,€ | ||
| 51 (30) | 9900 ± 180 ○,◊ | 3934 ± 80 ◊ | 9855 ± 159 ○,◊ | 4110 ± 109 ○,◊ | 6549 ± 136 ○,*,□,◊,€ | 3130 ± 91 ○,*,□,◊ | 9906 ± 183 ○,◊ | 3958 ± 106 ◊ | 9979 ± 172 ○,◊ | 4096 ± 97 ○,◊ | 6251 ± 87 ○,*,□,◊,€ | 3230 ± 99 ○,*,□,◊ | ||
| 81 (60) | 1987 ± 85 | 1856 ± 85 | 9889 ± 195 ○,◊,† | 3893 ± 95 ◊,† | 9946 ± 185 ○,◊,† | 4001 ± 125 ○,◊,† | 6834 ± 119 *,□,◊,†,€ | 3250 ± 101 ○,*,□,◊,†,€ | 9872 ± 174 ○,◊,† | 3798 ± 90 ◊,† | 1055 ± 169 ○,◊,† | 3989 ± 115 ○,◊,† | 6365 ± 111 ○,*,◊,†,€ | 3550 ± 121 ○,*,□,◊,†,€ |
References
- Sobrin, L.; Seddon, J.M. Nature and nurture-genes and environment-predict onset and progression of macular degeneration. Prog. Retin. Eye Res. 2014, 40, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.A.; Mousavi, M. Overview of Risk Factors for Age-Related Macular Degeneration (AMD). J. Stem Cells 2015, 10, 171–191. [Google Scholar] [PubMed]
- Warwick, A.; Lotery, A. Genetics and genetic testing for age-related macular degeneration. Eye 2018, 32, 849–857. [Google Scholar] [CrossRef] [PubMed]
- Resnikoff, S.; Pascolini, D.; Etya’ale, D.; Kocur, I.; Pararajasegaram, R.; Pokharel, G.P.; Mariotti, S.P. Global data on visual impairment in the year 2002. Bull. World Health Organ. 2004, 82, 844–851. [Google Scholar]
- Flaxman, S.R.; Bourne, R.R.A.; Resnikoff, S.; Ackland, P.; Braithwaite, T.; Cicinelli, M.V.; Das, A.; Jonas, J.B.; Keeffe, J.; Kempen, J.H.; et al. Global causes of blindness and distance vision impairment 1990-2020: A systematic review and meta-analysis. Lancet Glob. Health 2017, 5, e1221–e1234. [Google Scholar] [CrossRef]
- Bourne, R.R.A.; Jonas, J.B.; Bron, A.M.; Cicinelli, M.V.; Das, A.; Flaxman, S.R.; Friedman, D.S.; Keeffe, J.E.; Kempen, J.H.; Leasher, J.; et al. Prevalence and causes of vision loss in high-income countries and in Eastern and Central Europe in 2015: Magnitude, temporal trends and projections. Br. J. Ophthalmol. 2018, 102, 575–585. [Google Scholar] [CrossRef]
- Hartong, D.T.; Berson, E.L.; Dryja, T.P. Retinitis pigmentosa. Lancet 2006, 368, 1795–1809. [Google Scholar] [CrossRef]
- Sullivan, L.S.; Bowne, S.J.; Seaman, C.R.; Blanton, S.H.; Lewis, R.A.; Heckenlively, J.R.; Birch, D.G.; Hughbanks-Wheaton, D.; Daiger, S.P. Genomic rearrangements of the PRPF31 gene account for 2.5% of autosomal dominant retinitis pigmentosa. Investig. Ophthalmol. Vis. Sci. 2006, 47, 4579–4588. [Google Scholar] [CrossRef]
- Dias, M.F.; Joo, K.; Kemp, J.A.; Fialho, S.L.; da Silva Cunha, A., Jr.; Woo, S.J.; Kwon, Y.J. Molecular genetics and emerging therapies for retinitis pigmentosa: Basic research and clinical perspectives. Prog. Retin. Eye Res. 2018, 63, 107–131. [Google Scholar] [CrossRef]
- Jones, M.K.; Lu, B.; Girman, S.; Wang, S. Cell-based therapeutic strategies for replacement and preservation in retinal degenerative diseases. Prog. Retin. Eye Res. 2017, 58, 1–27. [Google Scholar] [CrossRef]
- Silverman, S.M.; Wong, W.T. Microglia in the Retina: Roles in Development, Maturity, and Disease. Annu. Rev. Vis. Sci. 2018, 4, 45–77. [Google Scholar] [CrossRef] [PubMed]
- Chrysostomou, V.; Valter, K.; Stone, J. Cone-rod dependence in the rat retina: Variation with the rate of rod damage. Investig. Ophthalmol. Vis. Sci. 2009, 50, 3017–3023. [Google Scholar] [CrossRef] [PubMed]
- Narayan, D.S.; Wood, J.P.; Chidlow, G.; Casson, R.J. A review of the mechanisms of cone degeneration in retinitis pigmentosa. Acta Ophthalmol. 2016, 94, 748–754. [Google Scholar] [CrossRef] [PubMed]
- Campochiaro, P.A.; Mir, T.A. The mechanism of cone cell death in Retinitis Pigmentosa. Prog. Retin. Eye Res. 2018, 62, 24–37. [Google Scholar] [CrossRef] [PubMed]
- Di Pierdomenico, J.; Garcia-Ayuso, D.; Agudo-Barriuso, M.; Vidal-Sanz, M.; Villegas-Perez, M.P. Role of microglial cells in photoreceptor degeneration. Neural Regen. Res. 2019, 14, 1186–1190. [Google Scholar] [PubMed]
- Wong, W.L.; Su, X.; Li, X.; Cheung, C.M.; Klein, R.; Cheng, C.Y.; Wong, T.Y. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob. Health 2014, 2, e106–e116. [Google Scholar] [CrossRef]
- Fritsche, L.G.; Igl, W.; Bailey, J.N.; Grassmann, F.; Sengupta, S.; Bragg-Gresham, J.L.; Burdon, K.P.; Hebbring, S.J.; Wen, C.; Gorski, M.; et al. A large genome-wide association study of age-related macular degeneration highlights contributions of rare and common variants. Nat. Genet. 2016, 48, 134–143. [Google Scholar] [CrossRef]
- Mitchell, P.; Liew, G.; Gopinath, B.; Wong, T.Y. Age-related macular degeneration. Lancet 2018, 392, 1147–1159. [Google Scholar] [CrossRef]
- Garcia-Ayuso, D.; Salinas-Navarro, M.; Agudo, M.; Cuenca, N.; Pinilla, I.; Vidal-Sanz, M.; Villegas-Perez, M.P. Retinal ganglion cell numbers and delayed retinal ganglion cell death in the P23H rat retina. Exp. Eye Res. 2010, 91, 800–810. [Google Scholar] [CrossRef]
- Garcia-Ayuso, D.; Salinas-Navarro, M.; Agudo-Barriuso, M.; Alarcon-Martinez, L.; Vidal-Sanz, M.; Villegas-Perez, M.P. Retinal ganglion cell axonal compression by retinal vessels in light-induced retinal degeneration. Mol. Vis. 2011, 17, 1716–1733. [Google Scholar]
- Garcia-Ayuso, D.; Salinas-Navarro, M.; Nadal-Nicolas, F.M.; Ortin-Martinez, A.; Agudo-Barriuso, M.; Vidal-Sanz, M.; Villegas-Perez, M.P. Sectorial loss of retinal ganglion cells in inherited photoreceptor degeneration is due to RGC death. Br. J. Ophthalmol. 2014, 98, 396–401. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Garcia-Ayuso, D.; Di Pierdomenico, J.; Agudo-Barriuso, M.; Vidal-Sanz, M.; Villegas-Perez, M.P. Retinal remodeling following photoreceptor degeneration causes retinal ganglion cell death. Neural Regen. Res. 2018, 13, 1885–1886. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Ayuso, D.; Di Pierdomenico, J.; Vidal-Sanz, M.; Villegas-Perez, M.P. Retinal Ganglion Cell Death as a Late Remodeling Effect of Photoreceptor Degeneration. Int. J. Mol. Sci. 2019, 20, 4696. [Google Scholar] [CrossRef] [PubMed]
- Di Pierdomenico, J.; Garcia-Ayuso, D.; Pinilla, I.; Cuenca, N.; Vidal-Sanz, M.; Agudo-Barriuso, M.; Villegas-Perez, M.P. Early Events in Retinal Degeneration Caused by Rhodopsin Mutation or Pigment Epithelium Malfunction: Differences and Similarities. Front. Neuroanat. 2017, 11, 14. [Google Scholar] [CrossRef]
- Marc, R.E.; Jones, B.W.; Watt, C.B.; Strettoi, E. Neural remodeling in retinal degeneration. Prog. Retin. Eye Res. 2003, 22, 607–655. [Google Scholar] [CrossRef]
- Jones, B.W.; Watt, C.B.; Marc, R.E. Retinal remodelling. Clin. Exp. Optom. 2005, 88, 282–291. [Google Scholar] [CrossRef]
- Pfeiffer, R.L.; Marc, R.E.; Jones, B.W. Persistent remodeling and neurodegeneration in late-stage retinal degeneration. Prog. Retin. Eye Res. 2020, 74, 100771. [Google Scholar] [CrossRef]
- Jayakody, S.A.; Gonzalez-Cordero, A.; Ali, R.R.; Pearson, R.A. Cellular strategies for retinal repair by photoreceptor replacement. Prog. Retin. Eye Res. 2015, 46, 31–66. [Google Scholar] [CrossRef] [PubMed]
- Gagliardi, G.; Ben M’Barek, K.; Goureau, O. Photoreceptor cell replacement in macular degeneration and retinitis pigmentosa: A pluripotent stem cell-based approach. Prog. Retin. Eye Res. 2019, 71, 1–25. [Google Scholar] [CrossRef]
- Gasparini, S.J.; Llonch, S.; Borsch, O.; Ader, M. Transplantation of photoreceptors into the degenerative retina: Current state and future perspectives. Prog. Retin. Eye Res. 2019, 69, 1–37. [Google Scholar] [CrossRef]
- Singh, M.S.; Park, S.S.; Albini, T.A.; Canto-Soler, M.V.; Klassen, H.; MacLaren, R.E.; Takahashi, M.; Nagiel, A.; Schwartz, S.D.; Bharti, K. Retinal stem cell transplantation: Balancing safety and potential. Prog. Retin. Eye Res. 2020, 75, 100779. [Google Scholar] [CrossRef] [PubMed]
- Trouillet, A.; Dubus, E.; Degardin, J.; Estivalet, A.; Ivkovic, I.; Godefroy, D.; Garcia-Ayuso, D.; Simonutti, M.; Sahly, I.; Sahel, J.A.; et al. Cone degeneration is triggered by the absence of USH1 proteins but prevented by antioxidant treatments. Sci. Rep. 2018, 8, 1968. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.B.; Gao, M.L.; Deng, W.L.; Wu, K.C.; Sugita, S.; Mandai, M.; Takahashi, M. Stemming retinal regeneration with pluripotent stem cells. Prog. Retin. Eye Res. 2019, 69, 38–56. [Google Scholar] [CrossRef] [PubMed]
- Maeda, A.; Mandai, M.; Takahashi, M. Gene and Induced Pluripotent Stem Cell Therapy for Retinal Diseases. Annu. Rev. Genom. Hum. Genet. 2019, 20, 201–216. [Google Scholar] [CrossRef]
- Jiang, C.; Klassen, H.; Zhang, X.; Young, M. Laser injury promotes migration and integration of retinal progenitor cells into host retina. Mol. Vis. 2010, 16, 983–990. [Google Scholar]
- Assawachananont, J.; Mandai, M.; Okamoto, S.; Yamada, C.; Eiraku, M.; Yonemura, S.; Sasai, Y.; Takahashi, M. Transplantation of embryonic and induced pluripotent stem cell-derived 3D retinal sheets into retinal degenerative mice. Stem Cell Rep. 2014, 2, 662–674. [Google Scholar] [CrossRef]
- Petrenko, Y.; Vackova, I.; Kekulova, K.; Chudickova, M.; Koci, Z.; Turnovcova, K.; Kupcova Skalnikova, H.; Vodicka, P.; Kubinova, S. A Comparative Analysis of Multipotent Mesenchymal Stromal Cells derived from Different Sources, with a Focus on Neuroregenerative Potential. Sci. Rep. 2020, 10, 4290. [Google Scholar] [CrossRef]
- Gnecchi, M.; Melo, L.G. Bone marrow-derived mesenchymal stem cells: Isolation, expansion, characterization, viral transduction, and production of conditioned medium. Methods Mol. Biol. 2009, 482, 281–294. [Google Scholar]
- Lu, B.; Wang, S.; Girman, S.; McGill, T.; Ragaglia, V.; Lund, R. Human adult bone marrow-derived somatic cells rescue vision in a rodent model of retinal degeneration. Exp. Eye Res. 2010, 91, 449–455. [Google Scholar] [CrossRef]
- Tomita, M.; Adachi, Y.; Yamada, H.; Takahashi, K.; Kiuchi, K.; Oyaizu, H.; Ikebukuro, K.; Kaneda, H.; Matsumura, M.; Ikehara, S. Bone marrow-derived stem cells can differentiate into retinal cells in injured rat retina. Stem Cells 2002, 20, 279–283. [Google Scholar] [CrossRef]
- Li, N.; Li, X.R.; Yuan, J.Q. Effects of bone-marrow mesenchymal stem cells transplanted into vitreous cavity of rat injured by ischemia/reperfusion. Graefe’s Arch. Clin. Exp. Ophthalmol. Albrecht Von Graefes Arch. Fur Klin. Und Exp. Ophthalmol. 2009, 247, 503–514. [Google Scholar]
- Zaverucha-do-Valle, C.; Mesentier-Louro, L.; Gubert, F.; Mortari, N.; Padilha, A.B.; Paredes, B.D.; Mencalha, A.; Abdelhay, E.; Teixeira, C.; Ferreira, F.G.; et al. Sustained effect of bone marrow mononuclear cell therapy in axonal regeneration in a model of optic nerve crush. Brain Res. 2014, 1587, 54–68. [Google Scholar] [CrossRef]
- Park, S.S.; Moisseiev, E.; Bauer, G.; Anderson, J.D.; Grant, M.B.; Zam, A.; Zawadzki, R.J.; Werner, J.S.; Nolta, J.A. Advances in bone marrow stem cell therapy for retinal dysfunction. Prog. Retin. Eye Res. 2017, 56, 148–165. [Google Scholar] [CrossRef] [PubMed]
- Yazdanyar, A.; Zhang, P.; Dolf, C.; Smit-McBride, Z.; Cary, W.; Nolta, J.A.; Zawadzki, R.J.; Marsh-Armstrong, N.; Park, S.S. Effects of intravitreal injection of human CD34(+) bone marrow stem cells in a murine model of diabetic retinopathy. Exp. Eye Res. 2020, 190, 107865. [Google Scholar] [CrossRef]
- Otani, A.; Dorrell, M.I.; Kinder, K.; Moreno, S.K.; Nusinowitz, S.; Banin, E.; Heckenlively, J.; Friedlander, M. Rescue of retinal degeneration by intravitreally injected adult bone marrow-derived lineage-negative hematopoietic stem cells. J. Clin. Investig. 2004, 114, 765–774. [Google Scholar] [CrossRef] [PubMed]
- Tzameret, A.; Sher, I.; Belkin, M.; Treves, A.J.; Meir, A.; Nagler, A.; Levkovitch-Verbin, H.; Barshack, I.; Rosner, M.; Rotenstreich, Y. Transplantation of human bone marrow mesenchymal stem cells as a thin subretinal layer ameliorates retinal degeneration in a rat model of retinal dystrophy. Exp. Eye Res. 2014, 118, 135–144. [Google Scholar] [CrossRef]
- Tzameret, A.; Sher, I.; Belkin, M.; Treves, A.J.; Meir, A.; Nagler, A.; Levkovitch-Verbin, H.; Rotenstreich, Y.; Solomon, A.S. Epiretinal transplantation of human bone marrow mesenchymal stem cells rescues retinal and vision function in a rat model of retinal degeneration. Stem Cell Res. 2015, 15, 387–394. [Google Scholar] [CrossRef]
- Moisseiev, E.; Smit-McBride, Z.; Oltjen, S.; Zhang, P.; Zawadzki, R.J.; Motta, M.; Murphy, C.J.; Cary, W.; Annett, G.; Nolta, J.A.; et al. Intravitreal Administration of Human Bone Marrow CD34+ Stem Cells in a Murine Model of Retinal Degeneration. Investig. Ophthalmol. Vis. Sci. 2016, 57, 4125–4135. [Google Scholar] [CrossRef]
- Mackie, A.R.; Losordo, D.W. CD34-positive stem cells: In the treatment of heart and vascular disease in human beings. Tex. Heart Inst. J. 2011, 38, 474–485. [Google Scholar]
- Michler, R.E. The current status of stem cell therapy in ischemic heart disease. J. Card. Surg. 2018, 33, 520–531. [Google Scholar] [CrossRef]
- Caballero, S.; Sengupta, N.; Afzal, A.; Chang, K.H.; Li Calzi, S.; Guberski, D.L.; Kern, T.S.; Grant, M.B. Ischemic vascular damage can be repaired by healthy, but not diabetic, endothelial progenitor cells. Diabetes 2007, 56, 960–967. [Google Scholar] [CrossRef] [PubMed]
- Park, S.S.; Caballero, S.; Bauer, G.; Shibata, B.; Roth, A.; Fitzgerald, P.G.; Forward, K.I.; Zhou, P.; McGee, J.; Telander, D.G.; et al. Long-term effects of intravitreal injection of GMP-grade bone-marrow-derived CD34+ cells in NOD-SCID mice with acute ischemia-reperfusion injury. Investig. Ophthalmol. Vis. Sci. 2012, 53, 986–994. [Google Scholar] [CrossRef] [PubMed]
- Arnhold, S.; Absenger, Y.; Klein, H.; Addicks, K.; Schraermeyer, U. Transplantation of bone marrow-derived mesenchymal stem cells rescue photoreceptor cells in the dystrophic retina of the rhodopsin knockout mouse. Graefe’s Arch. Clin. Exp. Ophthalmol. Albrecht Von Graefes Arch. Fur Klin. Und Exp. Ophthalmol. 2007, 245, 414–422. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Lu, B.; Girman, S.; Duan, J.; McFarland, T.; Zhang, Q.S.; Grompe, M.; Adamus, G.; Appukuttan, B.; Lund, R. Non-invasive stem cell therapy in a rat model for retinal degeneration and vascular pathology. Plos ONE 2010, 5, e9200. [Google Scholar] [CrossRef] [PubMed]
- Jonas, J.B.; Witzens-Harig, M.; Arseniev, L.; Ho, A.D. Intravitreal autologous bone marrow-derived mononuclear cell transplantation: A feasibility report. Acta Ophthalmol. 2008, 86, 225–226. [Google Scholar] [CrossRef]
- Siqueira, R.C.; Voltarelli, J.C.; Messias, A.M.; Jorge, R. Possible mechanisms of retinal function recovery with the use of cell therapy with bone marrow-derived stem cells. Arq. Bras. De Oftalmol. 2010, 73, 474–479. [Google Scholar] [CrossRef]
- Siqueira, R.C.; Messias, A.; Voltarelli, J.C.; Scott, I.U.; Jorge, R. Intravitreal injection of autologous bone marrow-derived mononuclear cells for hereditary retinal dystrophy: A phase I trial. Retina 2011, 31, 1207–1214. [Google Scholar] [CrossRef]
- Park, S.S.; Bauer, G.; Abedi, M.; Pontow, S.; Panorgias, A.; Jonnal, R.; Zawadzki, R.J.; Werner, J.S.; Nolta, J. Intravitreal autologous bone marrow CD34+ cell therapy for ischemic and degenerative retinal disorders: Preliminary phase 1 clinical trial findings. Investig. Ophthalmol. Vis. Sci. 2014, 56, 81–89. [Google Scholar] [CrossRef]
- Schwartz, S.D.; Regillo, C.D.; Lam, B.L.; Eliott, D.; Rosenfeld, P.J.; Gregori, N.Z.; Hubschman, J.P.; Davis, J.L.; Heilwell, G.; Spirn, M.; et al. Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt’s macular dystrophy: Follow-up of two open-label phase 1/2 studies. Lancet 2015, 385, 509–516. [Google Scholar] [CrossRef]
- Sobrado-Calvo, P.; Vidal-Sanz, M.; Villegas-Perez, M.P. Rat retinal microglial cells under normal conditions, after optic nerve section, and after optic nerve section and intravitreal injection of trophic factors or macrophage inhibitory factor. J. Comp. Neurol. 2007, 501, 866–878. [Google Scholar] [CrossRef]
- Kondo, Y.; Ogawa, N.; Asanuma, M.; Nishibayashi, S.; Iwata, E.; Mori, A. Cyclosporin A prevents ischemia-induced reduction of muscarinic acetylcholine receptors with suppression of microglial activation in gerbil hippocampus. Neurosci. Res. 1995, 22, 22–123. [Google Scholar] [CrossRef]
- Sliwa, M.; Markovic, D.; Gabrusiewicz, K.; Synowitz, M.; Glass, R.; Zawadzka, M.; Wesolowska, A.; Kettenmann, H.; Kaminska, B. The invasion promoting effect of microglia on glioblastoma cells is inhibited by cyclosporin A. Brain J. Neurol. 2007, 130 Pt 2, 476–489. [Google Scholar] [CrossRef]
- Wowro, S.J.; Tong, G.; Krech, J.; Rolfs, N.; Berger, F.; Schmitt, K.R.L. Combined Cyclosporin A and Hypothermia Treatment Inhibits Activation of BV-2 Microglia but Induces an Inflammatory Response in an Ischemia/Reperfusion Hippocampal Slice Culture Model. Front. Cell. Neurosci. 2019, 13, 273. [Google Scholar] [CrossRef]
- LaVail, M.M.; Nishikawa, S.; Steinberg, R.H.; Naash, M.I.; Duncan, J.L.; Trautmann, N.; Matthes, M.T.; Yasumura, D.; Lau-Villacorta, C.; Chen, J.; et al. Phenotypic characterization of P23H and S334ter rhodopsin transgenic rat models of inherited retinal degeneration. Exp. Eye Res. 2018, 167, 56–90. [Google Scholar] [CrossRef] [PubMed]
- Qu, L.; Gao, L.; Xu, H.; Duan, P.; Zeng, Y.; Liu, Y.; Yin, Z.Q. Combined transplantation of human mesenchymal stem cells and human retinal progenitor cells into the subretinal space of RCS rats. Sci. Rep. 2017, 7, 199. [Google Scholar] [CrossRef] [PubMed]
- Noailles, A.; Fernandez-Sanchez, L.; Lax, P.; Cuenca, N. Microglia activation in a model of retinal degeneration and TUDCA neuroprotective effects. J. Neuroinflammation 2014, 11, 186. [Google Scholar] [CrossRef]
- De Hoz, R.; Rojas, B.; Ramirez, A.I.; Salazar, J.J.; Gallego, B.I.; Trivino, A.; Ramirez, J.M. Retinal Macroglial Responses in Health and Disease. Biomed Res. Int. 2016, 2016, 2954721. [Google Scholar] [CrossRef] [PubMed]
- Tomita, M.; Mori, T.; Maruyama, K.; Zahir, T.; Ward, M.; Umezawa, A.; Young, M.J. A comparison of neural differentiation and retinal transplantation with bone marrow-derived cells and retinal progenitor cells. Stem Cells 2006, 24, 2270–2278. [Google Scholar] [CrossRef]
- Inoue, Y.; Iriyama, A.; Ueno, S.; Takahashi, H.; Kondo, M.; Tamaki, Y.; Araie, M.; Yanagi, Y. Subretinal transplantation of bone marrow mesenchymal stem cells delays retinal degeneration in the RCS rat model of retinal degeneration. Exp. Eye Res. 2007, 85, 234–241. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, W. Effects of bone marrow mesenchymal stem cell transplantation on light-damaged retina. Investig. Ophthalmol. Vis. Sci. 2010, 51, 3742–3748. [Google Scholar] [CrossRef]
- Park, D.H.; Sun, H.J.; Lee, S.J. A comparison of responses to intravitreal bevacizumab, ranibizumab, or aflibercept injections for neovascular age-related macular degeneration. Int. Ophthalmol. 2017, 37, 1205–1214. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Zhuang, J.; Hu, P.; Ye, W.; Chen, S.; Pang, Y.; Li, N.; Deng, C.; Zhang, X. Resveratrol Delays Retinal Ganglion Cell Loss and Attenuates Gliosis-Related Inflammation from Ischemia-Reperfusion Injury. Investig. Ophthalmol. Vis. Sci. 2018, 59, 3879–3888. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Shu, Q.; Ni, Y.; Xu, G. CRISPR-mediated SOX9 knockout inhibits GFAP expression in retinal glial (Muller) cells. Neuroreport 2018, 29, 1504–1508. [Google Scholar] [CrossRef]
- Di Pierdomenico, J.; Scholz, R.; Valiente-Soriano, F.J.; Sanchez-Migallon, M.C.; Vidal-Sanz, M.; Langmann, T.; Agudo-Barriuso, M.; Garcia-Ayuso, D.; Villegas-Perez, M.P. Neuroprotective Effects of FGF2 and Minocycline in Two Animal Models of Inherited Retinal Degeneration. Investig. Ophthalmol. Vis. Sci. 2018, 59, 4392–4403. [Google Scholar] [CrossRef]
- Lucas-Ruiz, F.; Galindo-Romero, C.; Rodriguez-Ramirez, K.T.; Vidal-Sanz, M.; Agudo-Barriuso, M. Neuronal Death in the Contralateral Un-Injured Retina after Unilateral Axotomy: Role of Microglial Cells. Int. J. Mol. Sci. 2019, 20, 5733. [Google Scholar] [CrossRef] [PubMed]
- Galindo-Romero, C.; Valiente-Soriano, F.J.; Jimenez-Lopez, M.; Garcia-Ayuso, D.; Villegas-Perez, M.P.; Vidal-Sanz, M.; Agudo-Barriuso, M. Effect of brain-derived neurotrophic factor on mouse axotomized retinal ganglion cells and phagocytic microglia. Investig. Ophthalmol. Vis. Sci. 2013, 54, 974–985. [Google Scholar] [CrossRef]
- Zhu, X.J.; Wolff, D.; Zhang, K.K.; He, W.W.; Sun, X.H.; Lu, Y.; Zhou, P. Molecular Inflammation in the Contralateral Eye After Cataract Surgery in the First Eye. Investig. Ophthalmol. Vis. Sci. 2015, 56, 5566–5573. [Google Scholar] [CrossRef]
- Vidal-Villegas, B.; Di Pierdomenico, J.; Miralles de Imperial-Ollero, J.A.; Ortin-Martinez, A.; Nadal-Nicolas, F.M.; Bernal-Garro, J.M.; Cuenca Navarro, N.; Villegas-Perez, M.P.; Vidal-Sanz, M. Melanopsin(+)RGCs Are fully Resistant to NMDA-Induced Excitotoxicity. Int. J. Mol. Sci. 2019, 20, 3012. [Google Scholar] [CrossRef]
- Nadal-Nicolas, F.M.; Jimenez-Lopez, M.; Salinas-Navarro, M.; Sobrado-Calvo, P.; Vidal-Sanz, M.; Agudo-Barriuso, M. Microglial dynamics after axotomy-induced retinal ganglion cell death. J. Neuroinflammation 2017, 14, 218. [Google Scholar] [CrossRef]
- Di Pierdomenico, J.; Martinez-Vacas, A.; Hernandez-Munoz, D.; Gomez-Ramirez, A.M.; Valiente-Soriano, F.J.; Agudo-Barriuso, M.; Vidal-Sanz, M.; Villegas-Perez, M.P.; Garcia-Ayuso, D. Coordinated Intervention of Microglial and Muller Cells in Light-Induced Retinal Degeneration. Investig. Ophthalmol. Vis. Sci. 2020, 61, 47. [Google Scholar] [CrossRef]
- Tassoni, A.; Gutteridge, A.; Barber, A.C.; Osborne, A.; Martin, K.R. Molecular Mechanisms Mediating Retinal Reactive Gliosis Following Bone Marrow Mesenchymal Stem Cell Transplantation. Stem Cells 2015, 33, 3006–3016. [Google Scholar] [CrossRef] [PubMed]
- Valiente-Soriano, F.J.; Salinas-Navarro, M.; Di Pierdomenico, J.; Garcia-Ayuso, D.; Lucas-Ruiz, F.; Pinilla, I.; Cuenca, N.; Vidal-Sanz, M.; Villegas-Perez, M.P.; Agudo-Barriuso, M. Tracing the retina to analyze the integrity and phagocytic capacity of the retinal pigment epithelium. Sci. Rep. 2020, 10, 7273. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Lu, B.; Girman, S.; Holmes, T.; Bischoff, N.; Lund, R.D. Morphological and functional rescue in RCS rats after RPE cell line transplantation at a later stage of degeneration. Investig. Ophthalmol. Vis. Sci. 2008, 49, 416–421. [Google Scholar] [CrossRef] [PubMed]
- Di Pierdomenico, J.; Garcia-Ayuso, D.; Jimenez-Lopez, M.; Agudo-Barriuso, M.; Vidal-Sanz, M.; Villegas-Perez, M.P. Different Ipsi- and Contralateral Glial Responses to Anti-VEGF and Triamcinolone Intravitreal Injections in Rats. Investig. Ophthalmol. Vis. Sci. 2016, 57, 3533–3544. [Google Scholar] [CrossRef]
- Bennett, J.; Tanabe, T.; Sun, D.; Zeng, Y.; Kjeldbye, H.; Gouras, P.; Maguire, A.M. Photoreceptor cell rescue in retinal degeneration (rd) mice by in vivo gene therapy. Nat. Med. 1996, 2, 649–654. [Google Scholar] [CrossRef]
- Westenskow, P.D.; Kurihara, T.; Bravo, S.; Feitelberg, D.; Sedillo, Z.A.; Aguilar, E.; Friedlander, M. Performing subretinal injections in rodents to deliver retinal pigment epithelium cells in suspension. J. Vis. Exp. JoVE 2015, 95, 52247. [Google Scholar] [CrossRef]
- Garcia-Ayuso, D.; Di Pierdomenico, J.; Hadj-Said, W.; Marie, M.; Agudo-Barriuso, M.; Vidal-Sanz, M.; Picaud, S.; Villegas-Perez, M.P. Taurine Depletion Causes ipRGC Loss and Increases Light-Induced Photoreceptor Degeneration. Investig. Ophthalmol. Vis. Sci. 2018, 59, 1396–1409. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Pierdomenico, J.; García-Ayuso, D.; González-Herrero, M.E.R.; García-Bernal, D.; Blanquer, M.; Bernal-Garro, J.M.; García-Hernández, A.M.; Vidal-Sanz, M.; Villegas-Pérez, M.P. Bone Marrow-Derived Mononuclear Cell Transplants Decrease Retinal Gliosis in Two Animal Models of Inherited Photoreceptor Degeneration. Int. J. Mol. Sci. 2020, 21, 7252. https://doi.org/10.3390/ijms21197252
Di Pierdomenico J, García-Ayuso D, González-Herrero MER, García-Bernal D, Blanquer M, Bernal-Garro JM, García-Hernández AM, Vidal-Sanz M, Villegas-Pérez MP. Bone Marrow-Derived Mononuclear Cell Transplants Decrease Retinal Gliosis in Two Animal Models of Inherited Photoreceptor Degeneration. International Journal of Molecular Sciences. 2020; 21(19):7252. https://doi.org/10.3390/ijms21197252
Chicago/Turabian StyleDi Pierdomenico, Johnny, Diego García-Ayuso, María Elena Rodríguez González-Herrero, David García-Bernal, Miguel Blanquer, José Manuel Bernal-Garro, Ana M. García-Hernández, Manuel Vidal-Sanz, and María P. Villegas-Pérez. 2020. "Bone Marrow-Derived Mononuclear Cell Transplants Decrease Retinal Gliosis in Two Animal Models of Inherited Photoreceptor Degeneration" International Journal of Molecular Sciences 21, no. 19: 7252. https://doi.org/10.3390/ijms21197252
APA StyleDi Pierdomenico, J., García-Ayuso, D., González-Herrero, M. E. R., García-Bernal, D., Blanquer, M., Bernal-Garro, J. M., García-Hernández, A. M., Vidal-Sanz, M., & Villegas-Pérez, M. P. (2020). Bone Marrow-Derived Mononuclear Cell Transplants Decrease Retinal Gliosis in Two Animal Models of Inherited Photoreceptor Degeneration. International Journal of Molecular Sciences, 21(19), 7252. https://doi.org/10.3390/ijms21197252









