Optimization of the Preparation of Magnetic Liposomes for the Combined Use of Magnetic Hyperthermia and Photothermia in Dual Magneto-Photothermal Cancer Therapy
Abstract
1. Introduction
2. Results and Discussion
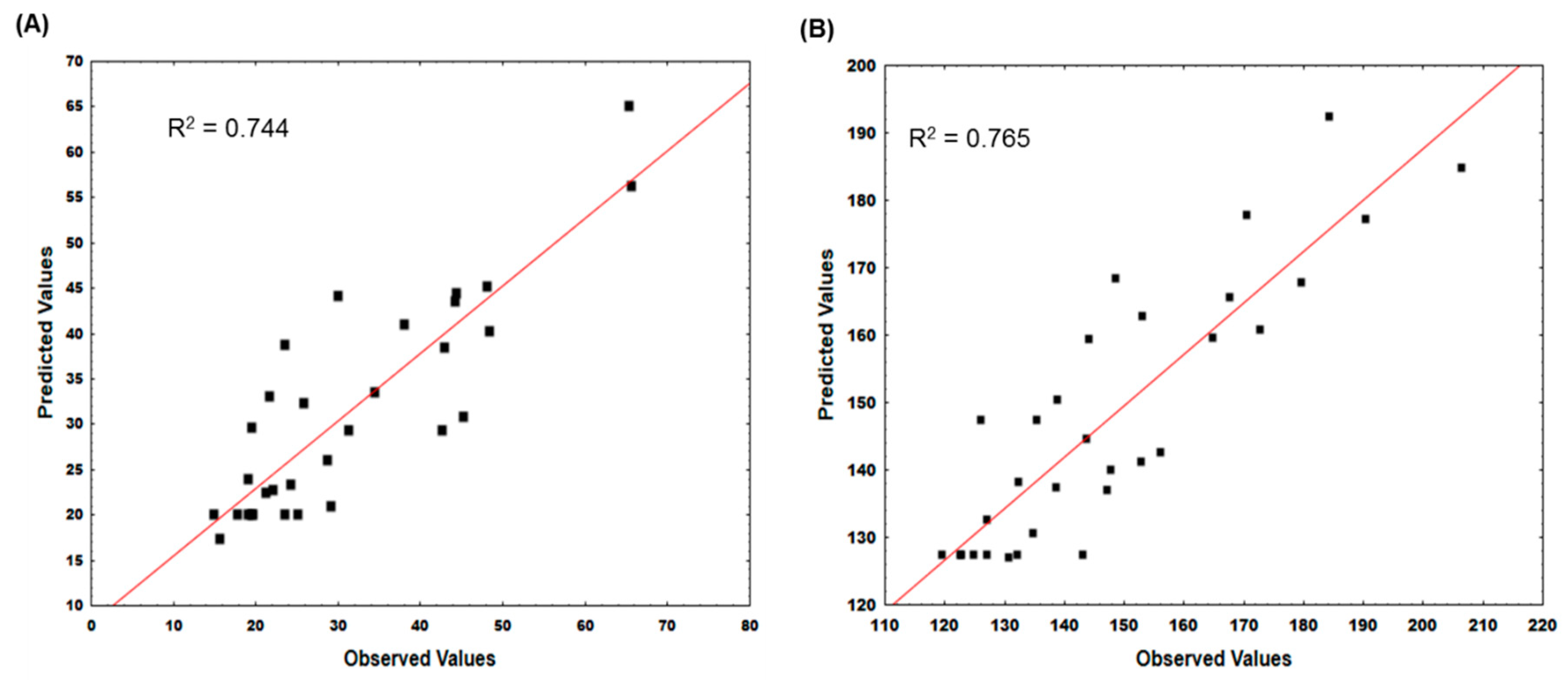
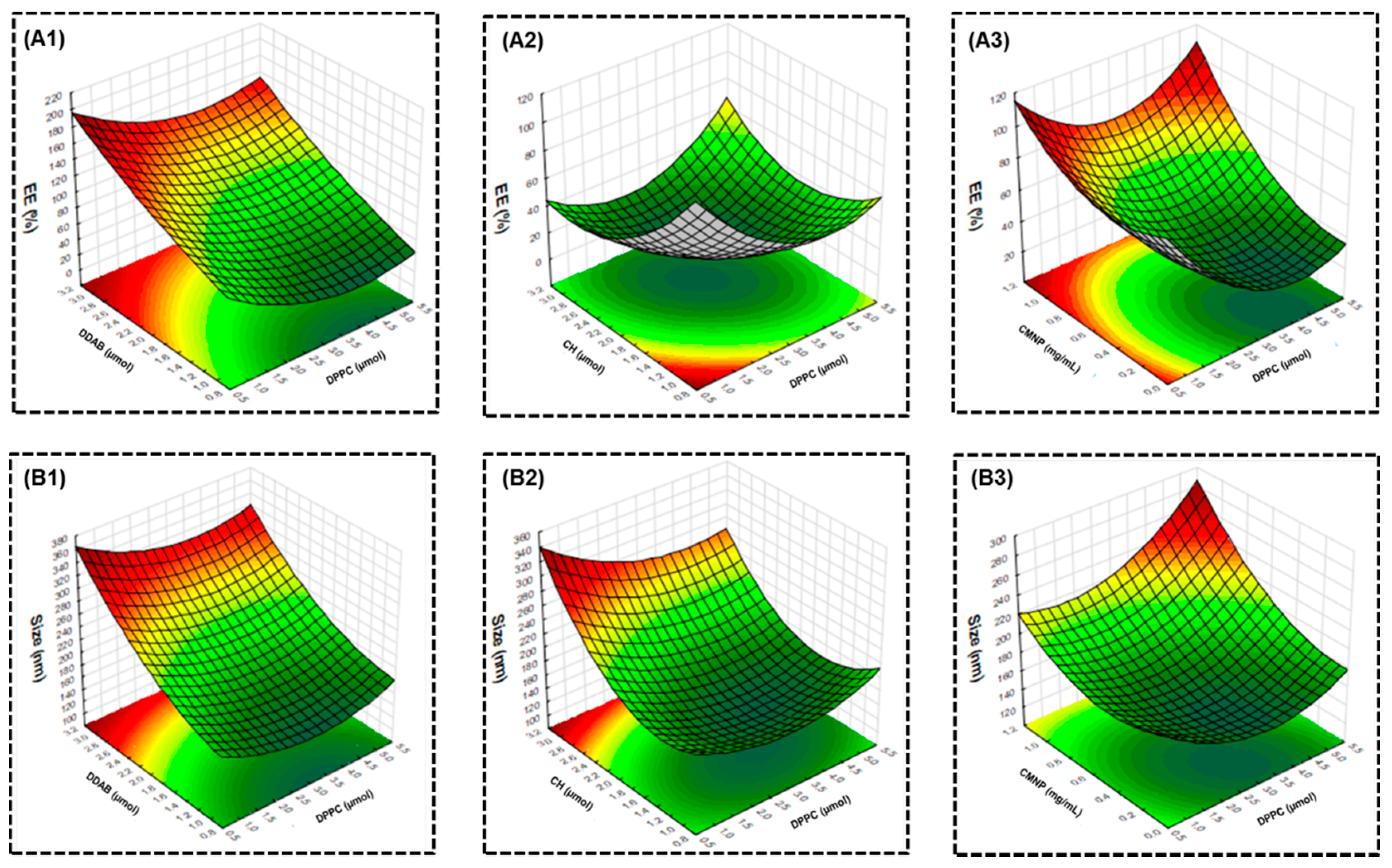
2.1. Model Development and Optimization
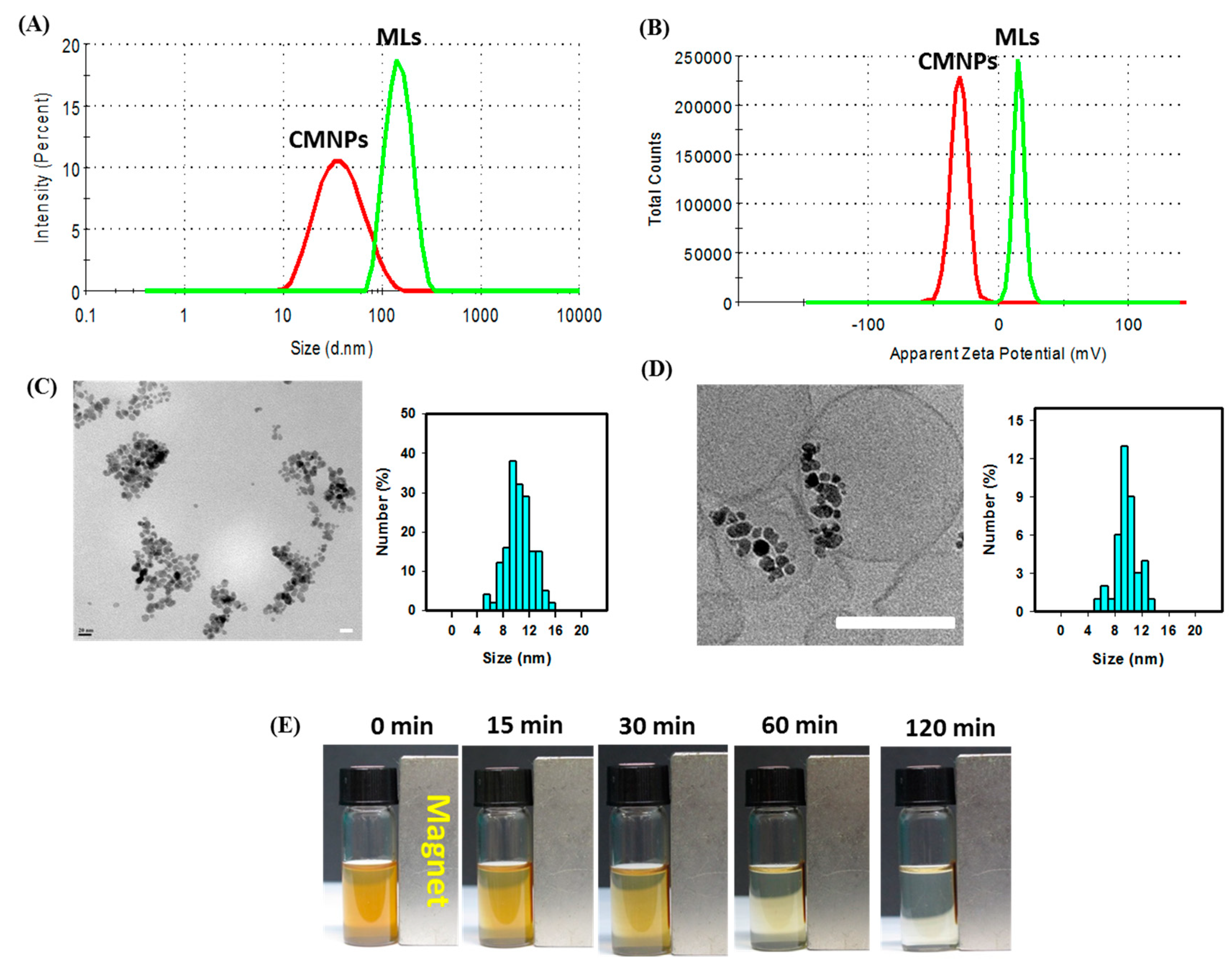
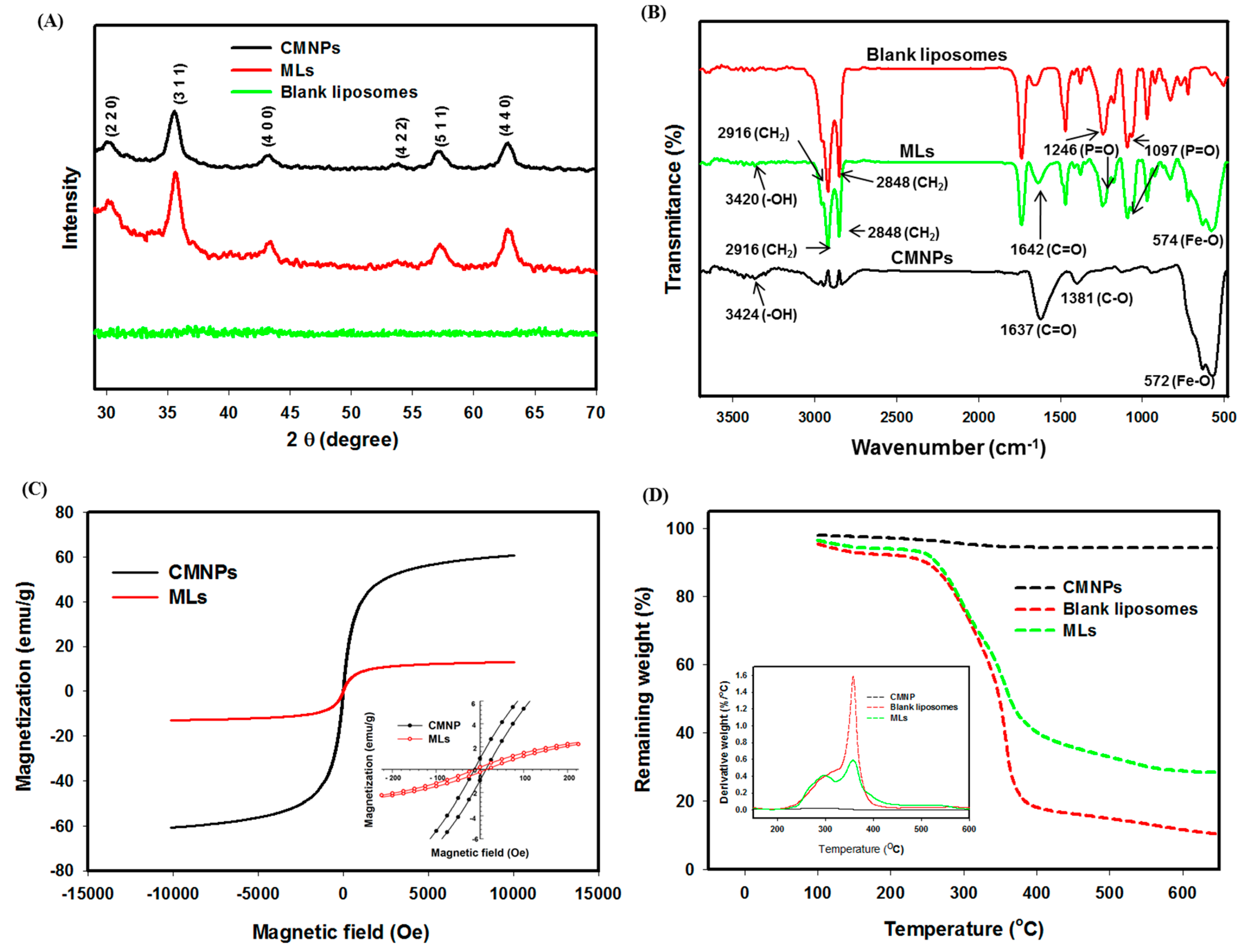
2.2. Characterization of Physico-Chemical Properties
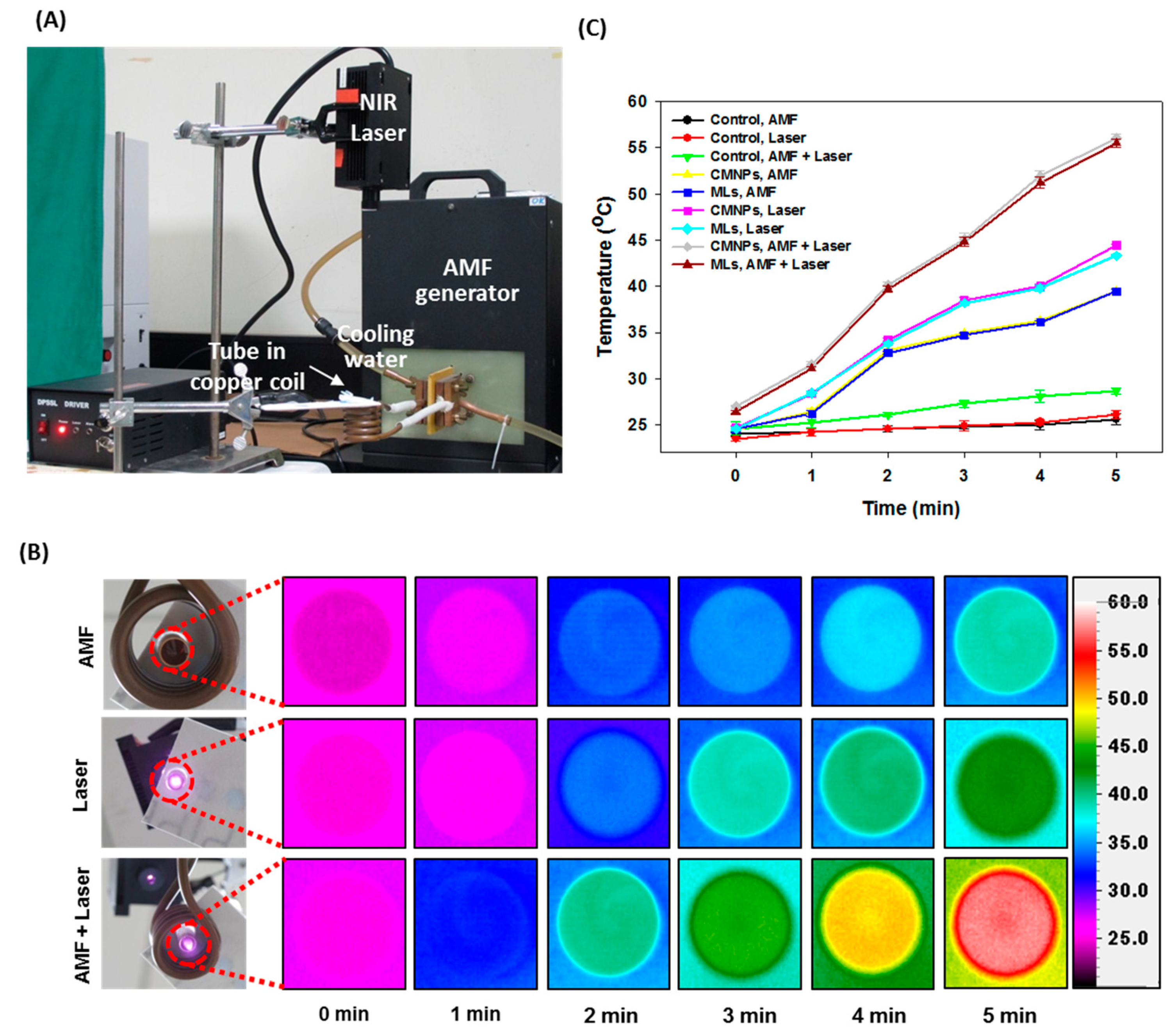
2.3. Heating Efficiency Induced by AMF, NIR, or Combined Laser Treament
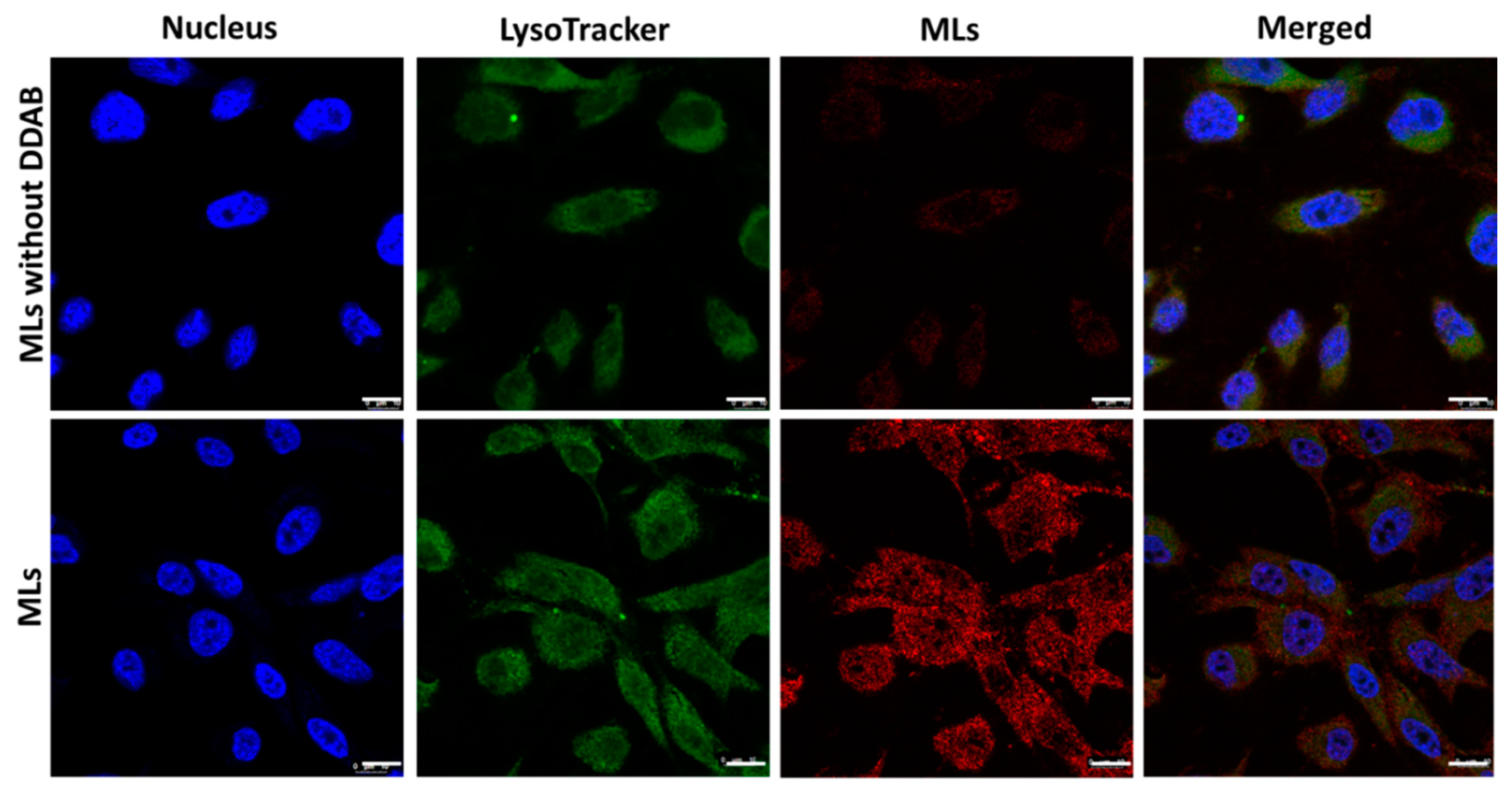
2.4. Intracellular Uptake of MLs
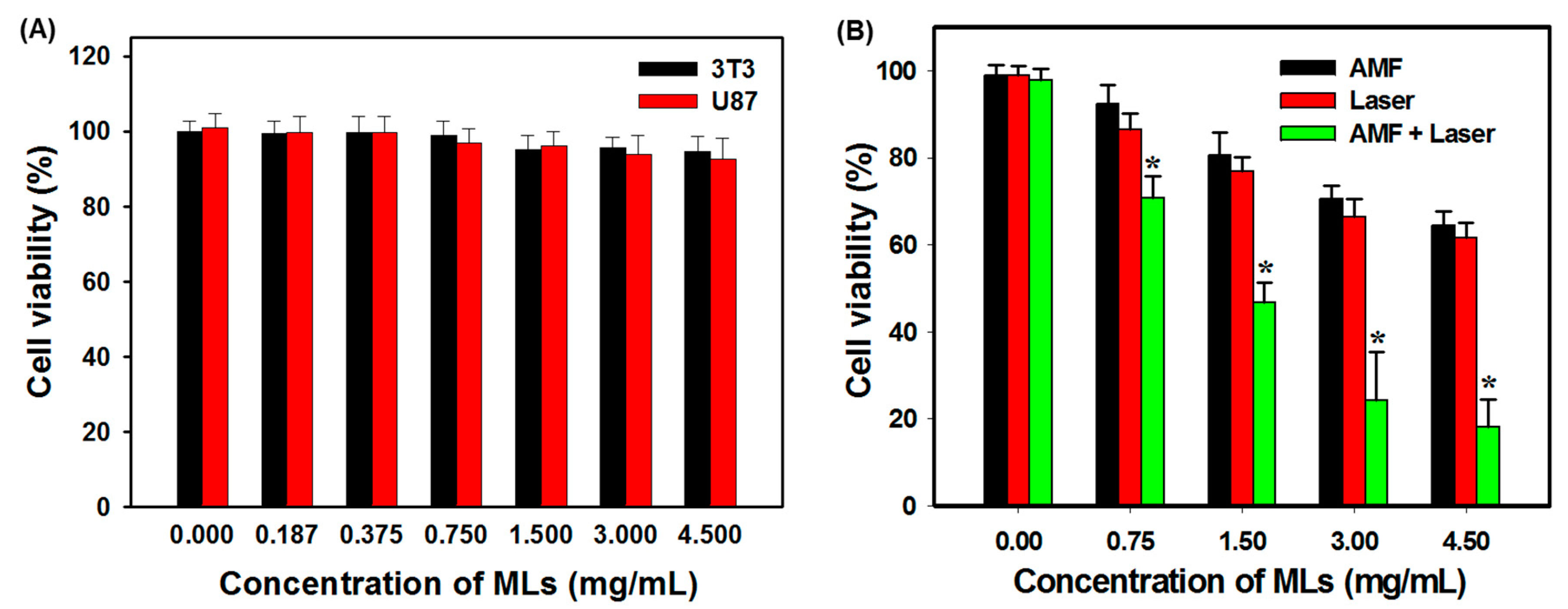
2.5. Thermally Induced Cancer Cell Killing In Vitro
3. Materials and Methods
3.1. Materials
3.2. Synthesis of Citric-Acid-Coated Iron Oxide Magnetic Nanoparticles (CMNPs)
3.3. Preparation of Magnetic Liposomes (MLs)
3.4. Experimental Design
3.5. Charactrization of Physico-Chemical Properties
3.6. Heating Efficiency Induced by AMF and NIR Lasers
3.7. Intracellular Uptake of MLs by Cancer Cells
3.8. In Vitro Biocompatibility of MLs
3.9. In Vitro Cancer Cell Killing by AMF and NIR Lasers
3.10. Flow Cytometry Analysis for Apoptosis and Necrosis
3.11. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wicki, A.; Witzigmann, D.; Balasubramanian, V.; Huwyler, J. Nanomedicine in cancer therapy: Challenges, opportunities, and clinical applications. J. Control. Release 2015, 200, 138–157. [Google Scholar] [CrossRef] [PubMed]
- Beik, J.; Abed, Z.; Ghoreishi, F.S.; Hosseini-Nami, S.; Mehrzadi, S.; Shakeri-Zadeh, A.; Kamrava, S.K. Nanotechnology in hyperthermia cancer therapy: From fundamental principles to advanced applications. J. Control. Release 2016, 235, 205–221. [Google Scholar] [CrossRef] [PubMed]
- Gas, P. Essential facts on the history of hyperthermia and their connections with electromedicine. Prz. Elektrotech. 2011, 87, 37–40. Available online: https://arxiv.org/abs/1710.00652 (accessed on 15 May 2020).
- Anilkumar, T.S.; Shalumon, K.T.; Chen, J.P. Applications of magnetic liposomes in cancer therapies. Curr. Pharm. Des. 2019, 25, 1490–1504. [Google Scholar] [CrossRef]
- Salunkhe, A.B.; Khot, V.M.; Pawar, S.H. Magnetic hyperthermia with magnetic nanoparticles: A status review. Curr. Top. Med. Chem. 2014, 14, 572–594. [Google Scholar] [CrossRef]
- Kossatz, S.; Ludwig, R.; Dähring, H.; Ettelt, V.; Rimkus, G.; Marciello, M.; Salas, G.; Patel, V.; Teran, F.J.; Hilger, I. High therapeutic efficiency of magnetic hyperthermia in xenograft models achieved with moderate temperature dosages in the tumor area. Pharm. Res. 2014, 31, 3274–3288. [Google Scholar] [CrossRef]
- Ansari, L.; Malaekeh-Nikouei, B. Magnetic silica nanocomposites for magnetic hyperthermia applications. Int. J. Hyperth. 2017, 33, 354–363. [Google Scholar] [CrossRef] [PubMed]
- Rosensweig, R.E. Heating magnetic fluid with alternating magnetic field. J. Magn. Magn. Mater. 2002, 252, 370–374. [Google Scholar] [CrossRef]
- Lal, S.; Clare, S.E.; Halas, N.J. Nanoshell-enabled photothermal cancer therapy: Impending clinical impact. Acc. Chem. Res. 2008, 41, 1842–1851. [Google Scholar] [CrossRef] [PubMed]
- Yan, H.; Shang, W.; Sun, X.; Zhao, L.; Wang, J.; Xiong, Z.; Yuan, J.; Zhang, R.; Huang, Q.; Wang, K.; et al. “All-in-One” nanoparticles for trimodality imaging-guided intracellular photo-magnetic hyperthermia therapy under intravenous administration. Adv. Funct. Mater. 2018, 28, 1705710. [Google Scholar] [CrossRef]
- Curcio, A.; Silva, A.K.A.; Cabana, S.; Espinosa, A.; Baptiste, B.; Menguy, N.; Wilhelm, C.; Abou-Hassan, A. Iron oxide nanoflowers @ cus hybrids for cancer tri-therapy: Interplay of photothermal therapy, magnetic hyperthermia and photodynamic therapy. Theranostics 2019, 9, 1288–1302. [Google Scholar] [CrossRef] [PubMed]
- Farzin, A.; Etesami, S.A.; Quint, J.; Memic, A.; Tamayol, A. Magnetic nanoparticles in cancer therapy and diagnosis. Adv. Healthc. Mater. 2020, 9, 1901058. [Google Scholar] [CrossRef] [PubMed]
- Wankhede, M.; Bouras, A.; Kaluzova, M.; Hadjipanayis, C.G. Magnetic nanoparticles: An emerging technology for malignant brain tumor imaging and therapy. Expert Rev. Clin. Pharmacol. 2012, 5, 173–186. [Google Scholar] [CrossRef] [PubMed]
- Shen, L.; Li, B.; Qiao, Y. Fe3O4 Nanoparticles in Targeted Drug/Gene Delivery Systems. Materials 2018, 11, 324. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.J.; Lin, P.Y.; Huang, P.H.; Kuo, C.Y.; Shalumon, K.T.; Chen, M.Y.; Chen, J.P. Magnetic graphene oxide for dual targeted delivery of doxorubicin and photothermal therapy. Nanomaterials 2018, 8, 193. [Google Scholar] [CrossRef]
- Estelrich, J.; Busquets, M.A. Iron oxide nanoparticles in photothermal therapy. Molecules 2018, 23, 1567. [Google Scholar] [CrossRef]
- Espinosa, A.; Di Corato, R.; Kolosnjaj-Tabi, J.; Flaud, P.; Pellegrino, T.; Wilhelm, C. Duality of iron oxide nanoparticles in cancer therapy: Amplification of heating efficiency by magnetic hyperthermia and photothermal bimodal treatment. ACS Nano 2016, 10, 2436–2446. [Google Scholar] [CrossRef]
- Vegerhof, A.; Motei, M.; Rudinzky, A.; Malka, D.; Popovtzer, R.; Zalevsky, Z. Thermal therapy with magnetic nanoparticles for cell destruction. Biomed. Opt. Express 2016, 7, 4581–4594. [Google Scholar] [CrossRef]
- Menager, C.; Cabuil, V. Synthesis of magnetic liposomes. J. Colloid Interf. Sci. 1995, 169, 251–253. [Google Scholar] [CrossRef]
- Anilkumar, T.S.; Lu, Y.J.; Chen, H.A.; Hsu, H.L.; Jose, G.; Chen, J.P. Dual targeted magnetic photosensitive liposomes for photothermal/photodynamic tumor therapy. J. Magn. Magn. Mater. 2018, 473, 241–252. [Google Scholar] [CrossRef]
- Li, L.; Wang, Q.; Zhang, X.; Luo, L.; He, Y.; Zhu, R.; Gao, D. Dual-targeting liposomes for enhanced anticancer effect in somatostatin receptor II-positive tumor model. Nanomed. Nanotechnol. Biol. Med. 2018, 13, 2155–2169. [Google Scholar] [CrossRef]
- Bazak, R.; Houri, M.; Achy, S.E.; Hussein, W.; Refaat, T. Passive targeting of nanoparticles to cancer: A comprehensive review of the literature. Mol. Clin. Oncol. 2014, 2, 904–908. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, P.P.; Biswas, S.; Torchilin, V.P. Current trends in the use of liposomes for tumor targeting. Nanomedicine (London, England) 2013, 8, 1509–1528. [Google Scholar] [CrossRef] [PubMed]
- Vitiello, G.; Luchini, A.; D’Errico, G.; Santamaria, R.; Capuozzo, A.; Irace, C.; Montesarchio, D.; Paduano, L. Cationic liposomes as efficient nanocarriers for the drug delivery of an anticancer cholesterol-based ruthenium complex. J. Mater. Chem. B 2015, 3, 3011–3023. [Google Scholar] [CrossRef]
- Wu, J.; Lee, A.; Lu, Y.; Lee, R.J. Vascular targeting of doxorubicin using cationic liposomes. Int. J. Pharm. 2007, 337, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Zhuang, S.; Qi, X.-R. Comparative study of the in vitro and in vivo characteristics of cationic and neutral liposomes. Int. J. Nanomed. 2011, 6, 3087–3098. [Google Scholar] [CrossRef]
- Cullis, P.R.; Chonn, A.; Semple, S.C. Interactions of liposomes and lipid-based carrier systems with blood proteins: Relation to clearance behaviour in vivo. Adv. Drug Deliv. Rev. 1998, 32, 3–17. [Google Scholar] [CrossRef]
- Dass, C.R. Improving anti-angiogenic therapy via selective delivery of cationic liposomes to tumour vasculature. Int. J. Pharm. 2003, 267, 1–12. [Google Scholar] [CrossRef]
- Kilian, G.; Milne, P. Optimization of selected liposome-encapsulated diketopiperazines. J. Drug Deliv. Sci. Technol. 2014, 24, 143–147. [Google Scholar] [CrossRef]
- Zhao, X.; Liu, J.; Hu, Y.; Fan, Y.; Wang, D.; Yuan, J.; Xu, L.; Cui, L.; Jing, Z. Optimization on condition of glycyrrhetinic acid liposome by RSM and the research of its immunological activity. Int. J. Biol. Macromol. 2012, 51, 299–304. [Google Scholar] [CrossRef]
- Bardania, H.; Shojaosadati, S.A.; Kobarfard, F.; Dorkoosh, F. Optimization of RGD-modified nano-liposomes encapsulating eptifibatide. Iran. J. Biotechnol. 2016, 14, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H.-L.; Chen, J.-P. Preparation of thermosensitive magnetic liposome encapsulated recombinant tissue plasminogen activator for targeted thrombolysis. J. Magn. Magn. Mater. 2017, 427, 188–194. [Google Scholar] [CrossRef]
- Masarudin, M.J.; Cutts, S.M.; Evison, B.J.; Phillips, D.R.; Pigram, P.J. Factors determining the stability, size distribution, and cellular accumulation of small, monodisperse chitosan nanoparticles as candidate vectors for anticancer drug delivery: Application to the passive encapsulation of [(14)C]-doxorubicin. Nanotechnol. Sci. Appl. 2015, 8, 67–80. [Google Scholar] [CrossRef] [PubMed]
- Danaei, M.; Dehghankhold, M.; Ataei, S.; Hasanzadeh Davarani, F.; Javanmard, R.; Dokhani, A.; Khorasani, S.; Mozafari, M.R. Impact of particle size and polydispersity index on the clinical applications of lipidic nanocarrier systems. Pharmaceutics 2018, 10, 57. [Google Scholar] [CrossRef] [PubMed]
- Price, P.M.; Mahmoud, W.E.; Al-Ghamdi, A.A.; Bronstein, L.M. Magnetic drug delivery: Where the field is going. Front. Chem. 2018, 6. [Google Scholar] [CrossRef] [PubMed]
- Filipe, V.; Hawe, A.; Jiskoot, W. Critical evaluation of nanoparticle tracking analysis (NTA) by nanosight for the measurement of nanoparticles and protein aggregates. Pharm. Res. 2010, 27, 796–810. [Google Scholar] [CrossRef]
- Olusanya, T.O.B.; Haj Ahmad, R.R.; Ibegbu, D.M.; Smith, J.R.; Elkordy, A.A. Liposomal drug delivery systems and anticancer drugs. Molecules 2018, 23, 907. [Google Scholar] [CrossRef]
- Ribeiro, L.N.d.M.; Couto, V.M.; Fraceto, L.F.; de Paula, E. Use of nanoparticle concentration as a tool to understand the structural properties of colloids. Sci. Rep. 2018, 8, 1–8. [Google Scholar] [CrossRef]
- Andar, A.U.; Hood, R.R.; Vreeland, W.N.; DeVoe, D.L.; Swaan, P.W. Microfluidic preparation of liposomes to determine particle size influence on cellular uptake mechanisms. Pharm. Res. 2014, 31, 401–413. [Google Scholar] [CrossRef]
- Guo, Y.; Zhang, Y.; Ma, J.; Li, Q.; Li, Y.; Zhou, X.; Zhao, D.; Song, H.; Chen, Q.; Zhu, X. Light/magnetic hyperthermia triggered drug released from multi-functional thermo-sensitive magnetoliposomes for precise cancer synergetic theranostics. J. Control. Release 2018, 272, 145–158. [Google Scholar] [CrossRef]
- Nalbandian, L.; Patrikiadou, E.; Zaspalis, V.; Patrikidou, A.; Hatzidaki, E.; Papandreou, C. Magnetic Nanoparticles in medical diagnostic applications: Synthesis, characterization and proteins conjugation. Curr. Nanosci. 2016, 12, 455–468. [Google Scholar] [CrossRef]
- Shimizu, K.; Maitani, Y.; Takayama, K.; Nagai, T. Characterization of dipalmitoylphosphatidylcholine liposomes containing a soybean-derived sterylglucoside mixture by differential scanning calorimetry, Fourier transform infrared spectroscopy, and enzymatic assay. J. Pharm. Sci. 1996, 85, 741–744. [Google Scholar] [CrossRef]
- Mahmoudi, M.; Sant, S.; Wang, B.; Laurent, S.; Sen, T. Superparamagnetic iron oxide nanoparticles (SPIONs): Development, surface modification and applications in chemotherapy. Adv. Drug Deliv. Rev. 2011, 63, 24–46. [Google Scholar] [CrossRef] [PubMed]
- Jose, G.; Lu, Y.-J.; Chen, H.-A.; Hsu, H.-L.; Hung, J.-T.; Anilkumar, T.S.; Chen, J.-P. Hyaluronic acid modified bubble-generating magnetic liposomes for targeted delivery of doxorubicin. J. Magn. Magn. Mater. 2019, 474, 355–364. [Google Scholar] [CrossRef]
- Lu, Y.-J.; Chuang, E.-Y.; Cheng, Y.-H.; Anilkumar, T.S.; Chen, H.-A.; Chen, J.-P. Thermosensitive magnetic liposomes for alternating magnetic field-inducible drug delivery in dual targeted brain tumor chemotherapy. Chem. Eng. J. 2019, 373, 720–733. [Google Scholar] [CrossRef]
- Gupta, A.K.; Curtis, A.S. Surface modified superparamagnetic nanoparticles for drug delivery: Interaction studies with human fibroblasts in culture. J. Mater. Sci. Mater. Med. 2004, 15, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.A.; Ma, Y.H.; Hsu, T.Y.; Chen, J.P. Preparation of peptide and recombinant tissue plasminogen activator conjugated poly(lactic-co-glycolic acid) (PLGA) magnetic nanoparticles for dual targeted thrombolytic therapy. Int. J. Mol. Sci. 2020, 21, 2690. [Google Scholar] [CrossRef]
- Kręcisz, M.; Rybka, J.D.; Strugała, A.J.; Skalski, B.; Figlerowicz, M.; Kozak, M.; Giersig, M. Interactions between magnetic nanoparticles and model lipid bilayers—Fourier transformed infrared spectroscopy (FTIR) studies of the molecular basis of nanotoxicity. J. Appl. Phys. 2016, 120, 124701. [Google Scholar] [CrossRef]
- Chu, M.; Shao, Y.; Peng, J.; Dai, X.; Li, H.; Wu, Q.; Shi, D. Near-infrared laser light mediated cancer therapy by photothermal effect of Fe3O4 magnetic nanoparticles. Biomaterials 2013, 34, 4078–4088. [Google Scholar] [CrossRef]
- Shen, S.; Wang, S.; Zheng, R.; Zhu, X.; Jiang, X.; Fu, D.; Yang, W. Magnetic nanoparticle clusters for photothermal therapy with near-infrared irradiation. Biomaterials 2015, 39, 67–74. [Google Scholar] [CrossRef]
- Hedayati, M.; Attaluri, A.; Bordelon, D.; Goh, R.; Armour, M.; Zhou, H.; Cornejo, C.; Wabler, M.; Zhang, Y.; DeWeese, T.; et al. New iron-oxide particles for magnetic nanoparticle hyperthermia: An in-vitro and in-vivo pilot study. In Proceedings of the SPIE, Progress in Biomedical Optics and Imaging, San Francisco, CA, USA, 3–4 February 2013; Volume 8584. [Google Scholar] [CrossRef]
- Shubitidze, F.; Kekalo, K.; Stigliano, R.; Baker, I. Magnetic nanoparticles with high specific absorption rate of electromagnetic energy at low field strength for hyperthermia therapy. J. Appl. Phys. 2015, 117, 094302. [Google Scholar] [CrossRef] [PubMed]
- Soetaert, F.; Kandala, S.K.; Bakuzis, A.; Ivkov, R. Experimental estimation and analysis of variance of the measured loss power of magnetic nanoparticles. Sci. Rep. 2017, 7, 1–15. [Google Scholar] [CrossRef]
- Campbell, R.B.; Fukumura, D.; Brown, E.B.; Mazzola, L.M.; Izumi, Y.; Jain, R.K.; Torchilin, V.P.; Munn, L.L. Cationic charge determines the distribution of liposomes between the vascular and extravascular compartments of tumors. Cancer Res. 2002, 62, 6831–6836. [Google Scholar] [PubMed]
- Lin, Q.; Mao, K.L.; Tian, F.R.; Yang, J.J.; Chen, P.P.; Xu, J.; Fan, Z.L.; Zhao, Y.P.; Li, W.F.; Zheng, L.; et al. Brain tumor-targeted delivery and therapy by focused ultrasound introduced doxorubicin-loaded cationic liposomes. Cancer Chemother. Pharm. 2016, 77, 269–280. [Google Scholar] [CrossRef]
- Dicheva, B.M.; ten Hagen, T.L.; Schipper, D.; Seynhaeve, A.L.; van Rhoon, G.C.; Eggermont, A.M.; Koning, G.A. Targeted and heat-triggered doxorubicin delivery to tumors by dual targeted cationic thermosensitive liposomes. J. Control. Release 2014, 195, 37–48. [Google Scholar] [CrossRef]
- Rayamajhi, S.; Marchitto, J.; Nguyen, T.D.T.; Marasini, R.; Celia, C.; Aryal, S. pH-responsive cationic liposome for endosomal escape mediated drug delivery. Colloids Surf. B Biointerfaces 2020, 188, 110804. [Google Scholar] [CrossRef]
- Chen, B.; Le, W.; Wang, Y.; Li, Z.; Wang, D.; Ren, L.; Lin, L.; Cui, S.; Hu, J.J.; Hu, Y.; et al. Targeting Negative Surface Charges of Cancer Cells by Multifunctional Nanoprobes. Theranostics 2016, 6, 1887–1898. [Google Scholar] [CrossRef]
- Yin, P.T.; Shah, B.P.; Lee, K.-B. Combined magnetic nanoparticle-based microRNA and hyperthermia therapy to enhance apoptosis in brain cancer cells. Small 2014, 10, 4106–4112. [Google Scholar] [CrossRef]
- Perez-Hernandez, M.; Del Pino, P.; Mitchell, S.G.; Moros, M.; Stepien, G.; Pelaz, B.; Parak, W.J.; Galvez, E.M.; Pardo, J.; de la Fuente, J.M. Dissecting the molecular mechanism of apoptosis during photothermal therapy using gold nanoprisms. ACS Nano 2015, 9, 52–61. [Google Scholar] [CrossRef]
- Zhang, H. Thin-film hydration followed by extrusion method for liposome preparation. In Liposomes. Methods in Molecular Biology; D’Souza, G., Ed.; Humana Press: New York, NY, USA, 2017; Volume 1522. [Google Scholar]
- Petralito, S.; Spera, R.; Memoli, A.; D’Inzeo, G.; Liberti, M.; Apollonio, F. Preparation and characterization of lipid vesicles entrapping iron oxide nanoparticles. Asia-Pac. J. Chem. Eng. 2012, 7, S335–S341. [Google Scholar] [CrossRef]
- Hardiansyah, A.; Huang, L.Y.; Yang, M.C.; Liu, T.Y.; Tsai, S.C.; Yang, C.Y.; Kuo, C.Y.; Chan, T.Y.; Zou, H.M.; Lian, W.N.; et al. Magnetic liposomes for colorectal cancer cells therapy by high-frequency magnetic field treatment. Nanoscale Res. Lett. 2014, 9, 497. [Google Scholar] [CrossRef] [PubMed]
- Frascione, D.; Diwoky, C.; Almer, G.; Opriessnig, P.; Vonach, C.; Gradauer, K.; Leitinger, G.; Mangge, H.; Stollberger, R.; Prassl, R. Ultrasmall superparamagnetic iron oxide (USPIO)-based liposomes as magnetic resonance imaging probes. Int. J. Nanomed. 2012, 7, 2349–2359. [Google Scholar] [CrossRef]
- Xiong, Y.; Guo, D.; Wang, L.; Zheng, X.; Zhang, Y.; Chen, J. Development of nobiliside A loaded liposomal formulation using response surface methodology. Int. J. Pharm. 2009, 371, 197–203. [Google Scholar] [CrossRef] [PubMed]



| Design Points | Coded Independent Variables | Response Values | ||||
|---|---|---|---|---|---|---|
| X1 | X2 | X3 | X4 | EE (%) | Size (nm) | |
| 1 | −1 | −1 | −1 | −1 | 23.6 | 135.2 |
| 2 | 1 | −1 | −1 | −1 | 31.3 | 153.0 |
| 3 | −1 | 1 | −1 | −1 | 65.3 | 183.5 |
| 4 | 1 | 1 | −1 | −1 | 65.6 | 170.1 |
| 5 | −1 | −1 | 1 | −1 | 22.1 | 132.4 |
| 6 | 1 | −1 | 1 | −1 | 28.8 | 152.8 |
| 7 | −1 | 1 | 1 | −1 | 48.4 | 180.8 |
| 8 | 1 | 1 | 1 | −1 | 30.0 | 138.9 |
| 9 | −1 | −1 | −1 | 1 | 45.9 | 155.5 |
| 10 | 1 | −1 | −1 | 1 | 19.5 | 126.1 |
| 11 | −1 | 1 | −1 | 1 | 24.7 | 148.7 |
| 12 | 1 | 1 | −1 | 1 | 21.9 | 179.6 |
| 13 | −1 | −1 | 1 | 1 | 44.3 | 143.6 |
| 14 | 1 | −1 | 1 | 1 | 18.3 | 147.1 |
| 15 | −1 | 1 | 1 | 1 | 43.6 | 147.8 |
| 16 | 1 | 1 | 1 | 1 | 43.0 | 130.8 |
| 17 | −2 | 0 | 0 | 0 | 38.0 | 164.8 |
| 18 | 2 | 0 | 0 | 0 | 29.1 | 138.6 |
| 19 | 0 | −2 | 0 | 0 | 19.2 | 134.8 |
| 20 | 0 | 2 | 0 | 0 | 44.3 | 157.5 |
| 21 | 0 | 0 | −2 | 0 | 34.5 | 206.3 |
| 22 | 0 | 0 | 2 | 0 | 48.1 | 144.2 |
| 23 | 0 | 0 | 0 | −2 | 21.2 | 172.7 |
| 24 | 0 | 0 | 0 | 2 | 25.9 | 127.0 |
| 25 | 0 | 0 | 0 | 0 | 19.5 | 142.9 |
| 26 | 0 | 0 | 0 | 0 | 23.6 | 119.6 |
| 27 | 0 | 0 | 0 | 0 | 14.9 | 122.5 |
| 28 | 0 | 0 | 0 | 0 | 19.6 | 124.8 |
| 29 | 0 | 0 | 0 | 0 | 24.8 | 127.0 |
| 30 | 0 | 0 | 0 | 0 | 26.7 | 133.1 |
| 31 | 0 | 0 | 0 | 0 | 28.1 | 129.7 |
| Predicted Values | Experimental Values | |||||
|---|---|---|---|---|---|---|
| Factors 1 | Codes | Variables | EE (%) 2 | Size (nm) 3 | EE (%) 2 | Size (nm) 3 |
| DPPC | X1 | 2 μmol | 86.9 | 121.1 | 84.2 ± 4.7 | 124.3 ± 6.5 |
| DDAB | X2 | 0.5 μmol | ||||
| CH | X3 | 1 μmol | ||||
| CMNP | X4 | 0.25 mg/mL | ||||
| Samples 1 | Size from DLS (nm) 2 | PDI 3 | Zeta Potential (mV) |
|---|---|---|---|
| CMNPs | 36.5 ± 5.4 | 0.21 ± 0.06 | −19.4 ± 4.3 |
| MLs | 124.3 ± 6.5 | 0.28 ± 0.09 | 16.3 ± 3.7 |
| Sample 2 | AMF 3 | Laser | AMF + Laser |
|---|---|---|---|
| CMNPs | 21.20 ± 0.14 | 28.06 ± 0.21 * | 42.13 ± 0.58 *,# |
| MLs | 21.08 ± 0.16 | 28.12 ± 0.17 * | 42.04 ± 0.48 *,# |
| Control | AMF 1 | Laser | AMF + Laser | |
|---|---|---|---|---|
| Live cell (Q3) | 95.1% | 77.9% | 71.9% | 38.0% |
| Early apoptosis (Q4) | 4.1% | 18.8% | 22.2% | 25.8% |
| Late apoptosis (Q2) | 0.7% | 3.0% | 5.6% | 33.7% |
| Necrotic cell (Q1) | 0.4% | 0.3% | 0.2% | 2.5% |
| Factors | Codes | Variable Levels | ||||
|---|---|---|---|---|---|---|
| 2 | −1 | 0 | −1 | −2 | ||
| DPPC (µmol) | X1 | 1 | 2 | 3 | 4 | 5 |
| DDAB (µmol) | X2 | 1 | 1.5 | 2 | 2.5 | 3 |
| CH (µmol) | X3 | 1 | 1.5 | 2 | 2.5 | 3 |
| CMNPs (mg/mL) | X4 | 0.1 | 0.35 | 0.6 | 0.85 | 1.1 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
T. S., A.; Lu, Y.-J.; Chen, J.-P. Optimization of the Preparation of Magnetic Liposomes for the Combined Use of Magnetic Hyperthermia and Photothermia in Dual Magneto-Photothermal Cancer Therapy. Int. J. Mol. Sci. 2020, 21, 5187. https://doi.org/10.3390/ijms21155187
T. S. A, Lu Y-J, Chen J-P. Optimization of the Preparation of Magnetic Liposomes for the Combined Use of Magnetic Hyperthermia and Photothermia in Dual Magneto-Photothermal Cancer Therapy. International Journal of Molecular Sciences. 2020; 21(15):5187. https://doi.org/10.3390/ijms21155187
Chicago/Turabian StyleT. S., Anilkumar, Yu-Jen Lu, and Jyh-Ping Chen. 2020. "Optimization of the Preparation of Magnetic Liposomes for the Combined Use of Magnetic Hyperthermia and Photothermia in Dual Magneto-Photothermal Cancer Therapy" International Journal of Molecular Sciences 21, no. 15: 5187. https://doi.org/10.3390/ijms21155187
APA StyleT. S., A., Lu, Y.-J., & Chen, J.-P. (2020). Optimization of the Preparation of Magnetic Liposomes for the Combined Use of Magnetic Hyperthermia and Photothermia in Dual Magneto-Photothermal Cancer Therapy. International Journal of Molecular Sciences, 21(15), 5187. https://doi.org/10.3390/ijms21155187






