Pulmonary Hypertension Phenotypes in Systemic Sclerosis: The Right Diagnosis for the Right Treatment
Abstract
1. Introduction
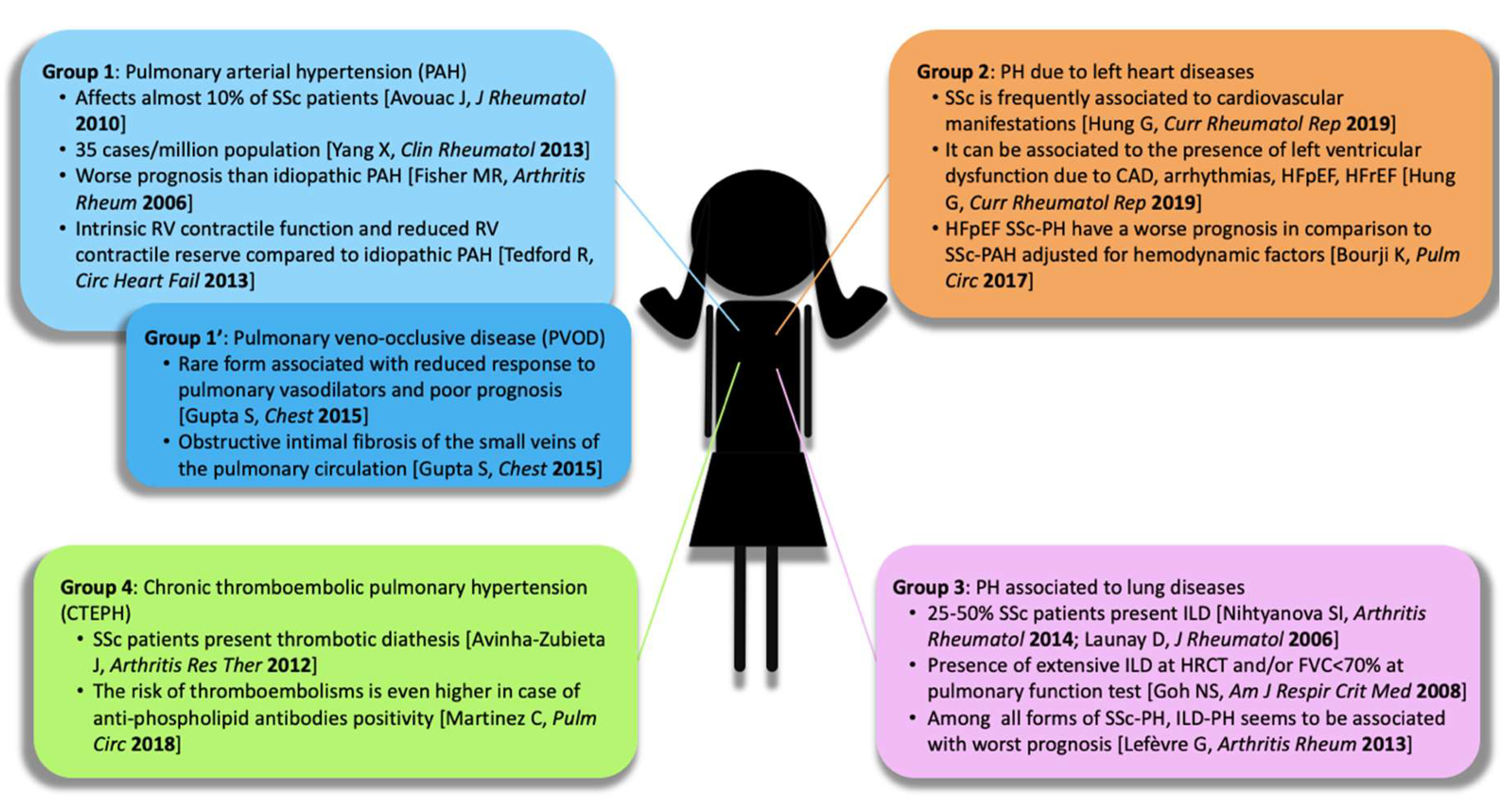
2. Systemic Sclerosis and Pulmonary Hypertension: A Dangerous Liaison
3. Pulmonary Hypertension in Systemic Sclerosis: Challenges in Screening and Diagnosis
4. Molecular and Pathophysiological Features of Idiopathic PAH versus SSc–PAH: Same Vascular Disease but Different Right Ventricular Adaptation
5. General Considerations on Treatment of Pulmonary Hypertension in SSc
6. Molecular Pathways Targeted by PAH-Specific Therapies
7. Risk Stratification, Goals of PAH-specific Therapy, and Combination Therapy
8. Further Perspectives
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| PAH | pulmonary arterial hypertension |
| SSc | systemic sclerosis |
| RV | right ventricle |
| PVOD | pulmonary veno-occlusive disease |
| PH | pulmonary hypertension |
| CAD | coronary artery disease |
| HFpEF | heart failure with preserved ejection fraction |
| HFrEF | heart failure with reduced ejection fraction |
| CTEPH | chronic thromboembolic pulmonary hypertension |
| ILD | interstitial lung disease |
| HRCT | high-resolution computed tomography |
| FVC | forced vital capacity. |
References
- Denton, C.P.; Khanna, D. Systemic sclerosis. Lancet 2017, 390, 1685–1699. [Google Scholar] [CrossRef]
- Hachulla, E.; De Groote, P.; Gressin, V.; Sibilia, J.; Diot, E.; Carpentier, P.; Mouthon, L.; Hatron, P.Y.; Jego, P.; Allanore, Y.; et al. The three-year incidence of pulmonary arterial hypertension associated with systemic sclerosis in a multicenter nationwide longitudinal study in France. Arthritis Rheum. 2009, 60, 1831–1839. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Humbert, M.; Vachiery, J.-L.; Gibbs, S.; Lang, I.; Torbicki, A.; Simonneau, G.; Peacock, A.; Vonk Noordegraaf, A.; Beghetti, M.; et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endo. Eur. Heart J. 2016, 37, 67–119. [Google Scholar] [CrossRef] [PubMed]
- Launay, D.; Sobanski, V.; Hachulla, E.; Humbert, M. Pulmonary hypertension in systemic sclerosis: Different phenotypes. Eur. Respir. Rev. 2017, 26. [Google Scholar] [CrossRef] [PubMed]
- Nihtyanova, S.I.; Schreiber, B.E.; Ong, V.H.; Rosenberg, D.; Moinzadeh, P.; Coghlan, J.G.; Wells, A.U.; Denton, C.P. Prediction of pulmonary complications and long-term survival in systemic sclerosis. Arthritis Rheumatol. 2014, 66, 1625–1635. [Google Scholar] [CrossRef]
- Fisher, M.R.; Mathai, S.C.; Champion, H.C.; Girgis, R.E.; Housten-Harris, T.; Hummers, L.; Krishnan, J.A.; Wigley, F.; Hassoun, P.M. Clinical differences between idiopathic and scleroderma-related pulmonary hypertension. Arthritis Rheum. 2006, 54, 3043–3050. [Google Scholar] [CrossRef]
- LeRoy, E.C.; Medsger, J. Criteria for the classification of early systemic sclerosis. J. Rheumatol. 2001, 28, 1573–1576. [Google Scholar]
- Hachulla, E.; Launay, D. Diagnosis and classification of systemic sclerosis. Clin. Rev. Allergy Immunol. 2011, 40, 78–83. [Google Scholar] [CrossRef]
- Hung, G.; Mercurio, V.; Hsu, S.; Mathai, S.C.; Shah, A.A.; Mukherjee, M. Progress in Understanding, Diagnosing, and Managing Cardiac Complications of Systemic Sclerosis. Curr. Rheumatol. Rep. 2019, 21, 68. [Google Scholar] [CrossRef] [PubMed]
- Simonneau, G.; Montani, D.; Celermajer, D.S.; Denton, C.P.; Gatzoulis, M.A.; Krowka, M.; Williams, P.G.; Souza, R. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur. Respir. J. 2019, 53. [Google Scholar] [CrossRef]
- Chin, K.M.; Kim, N.H.S.; Rubin, L.J. The right ventricle in pulmonary hypertension. Coron. Artery Dis. 2005, 16, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Bourji, K.I.; Kelemen, B.W.; Mathai, S.C.; Damico, R.L.; Kolb, T.M.; Mercurio, V.; Cozzi, F.; Tedford, R.J.; Hassoun, P.M. Poor survival in patients with scleroderma and pulmonary hypertension due to heart failure with preserved ejection fraction. Pulm. Circ. 2017, 7, 409–420. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Codina, A.; Simeón-Aznar, C.P.; Pinal-Fernandez, I.; Rodríguez-Palomares, J.; Pizzi, M.N.; Hidalgo, C.E.; Del Castillo, A.G.; Prado-Galbarro, F.J.; Sarria-Santamera, A.; Fonollosa-Plà, V.; et al. Cardiac involvement in systemic sclerosis: Differences between clinical subsets and influence on survival. Rheumatol. Int. 2017, 37, 75–84. [Google Scholar] [CrossRef]
- Launay, D.; Remy-Jardin, M.; Michon-Pasturel, U.; Mastora, I.; Hachulla, E.; Lambert, M.; Delannoy, V.; Queyrel, V.; Duhamel, A.; Matran, R.; et al. High resolution computed tomography in fibrosing alveolitis associated with systemic sclerosis. J. Rheumatol. 2006, 33, 1789–1801. [Google Scholar] [PubMed]
- Goh, N.S.L.; Desai, S.R.; Veeraraghavan, S.; Hansell, D.M.; Copley, S.J.; Maher, T.M.; Corte, T.J.; Sander, C.R.; Ratoff, J.; Devaraj, A.; et al. Interstitial lung disease in systemic sclerosis: A simple staging system. Am. J. Respir. Crit. Care Med. 2008, 177, 1248–1254. [Google Scholar] [CrossRef] [PubMed]
- Aviña-Zubieta, J.; Lacaille, D.; Sayre, E.; Kopec, J.; Choi, H.; Esdaile, J. Risk of pulmonary embolism and deep vein thrombosis in systemic lupus erythematosus: A population-based cohort study. Arthritis Res. Ther. 2012, 14, A53. [Google Scholar] [CrossRef]
- Martinez, C.; Wallenhorst, C.; Teal, S.; Cohen, A.T.; Peacock, A.J. Incidence and risk factors of chronic thromboembolic pulmonary hypertension following venous thromboembolism, a population-based cohort study in England. Pulm. Circ. 2018, 8. [Google Scholar] [CrossRef]
- Gupta, S.; Gupta, A.; Ocak, I.; Domsic, R.; Schneider, F.; George, P. PVOD Is Highly Prevalent in Scleroderma Patients Undergoing Lung Transplant. Chest 2015, 148, 924A. [Google Scholar] [CrossRef]
- Chaisson, N.F.; Hassoun, P.M. Systemic sclerosis-associated pulmonary arterial hypertension. Chest 2013, 144, 1346–1356. [Google Scholar] [CrossRef] [PubMed]
- Avouac, J.; Airò, P.; Meune, C.; Beretta, L.; Dieude, P.; Caramaschi, P.; Tiev, K.; Cappelli, S.; Diot, E.; Vacca, A.; et al. Prevalence of pulmonary hypertension in systemic sclerosis in European Caucasians and metaanalysis of 5 studies. J. Rheumatol. 2010, 37, 2290–2298. [Google Scholar] [CrossRef]
- Coghlan, J.G.; Denton, C.P.; Grünig, E.; Bonderman, D.; Distler, O.; Khanna, D.; Müller-Ladner, U.; Pope, J.E.; Vonk, M.C.; Doelberg, M.; et al. Evidence-based detection of pulmonary arterial hypertension in systemic sclerosis: The DETECT study. Ann. Rheum. Dis. 2014, 73, 1340–1349. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Mardekian, J.; Sanders, K.N.; Mychaskiw, M.A.; Thomas, J. Prevalence of pulmonary arterial hypertension in patients with connective tissue diseases: A systematic review of the literature. Clin. Rheumatol. 2013, 32, 1519–1531. [Google Scholar] [CrossRef] [PubMed]
- Jaafar, S.; Visovatti, S.; Young, A.; Huang, S.; Cronin, P.; Vummidi, D.; McLaughlin, V.; Khanna, D. Impact of the revised haemodynamic definition on the diagnosis of pulmonary hypertension in patients with systemic sclerosis. Eur. Respir. J. 2019, 54. [Google Scholar] [CrossRef] [PubMed]
- Hurdman, J.; Condliffe, R.; Elliot, C.A.; Davies, C.; Hill, C.; Wild, J.M.; Capener, D.; Sephton, P.; Hamilton, N.; Armstrong, I.J.; et al. ASPIRE registry: Assessing the Spectrum of Pulmonary hypertension Identified at a. Eur. Respir. J. 2012, 39, 945–955. [Google Scholar] [CrossRef] [PubMed]
- Lefèvre, G.; Dauchet, L.; Hachulla, E.; Montani, D.; Sobanski, V.; Lambert, M.; Hatron, P.Y.; Humbert, M.; Launay, D. Survival and prognostic factors in systemic sclerosis-associated pulmonary hypertension: A systematic review and meta-analysis. Arthritis Rheum. 2013, 65, 2412–2423. [Google Scholar] [CrossRef] [PubMed]
- Khanna, D.; Gladue, H.; Channick, R.; Chung, L.; Distler, O.; Furst, D.E.; Hachulla, E.; Humbert, M.; Langleben, D.; Mathai, S.C.; et al. Recommendations for screening and detection of connective tissue disease-associated pulmonary arterial hypertension. Arthritis Rheum. 2013, 65, 3194–3201. [Google Scholar] [CrossRef]
- Frost, A.; Badesch, D.; Gibbs, J.S.R.; Gopalan, D.; Khanna, D.; Manes, A.; Oudiz, R.; Satoh, T.; Torres, F.; Torbicki, A. Diagnosis of pulmonary hypertension. Eur. Respir. J. 2019, 53. [Google Scholar] [CrossRef] [PubMed]
- Zompatori, M.; Leone, M.B.; Giannotta, M.; Galiè, N.; Palazzini, M.; Bacchi Reggiani, M.L.; Bono, L.; Pollini, G.S. Ipertensione polmonare e sclerodermia: Il ruolo della TC ad alta risoluzione. Radiol. Medica 2013, 118, 1360–1372. [Google Scholar] [CrossRef]
- Günther, S.; Jaïs, X.; Maitre, S.; Bérezné, A.; Dorfmüller, P.; Seferian, A.; Savale, L.; Mercier, O.; Fadel, E.; Sitbon, O.; et al. Computed tomography findings of pulmonary venoocclusive disease in scleroderma patients presenting with precapillary pulmonary hypertension. Arthritis Rheum. 2012, 64, 2995–3005. [Google Scholar] [CrossRef]
- Galie, N.; Hoeper, M.M.; Humbert, M.; Torbicki, A.; Vachiery, J.-L.; Barbera, J.A.; Beghetti, M.; Corris, P.; Gaine, S.; Gibbs, J.S.; et al. Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur. Respir. J. 2009, 34, 1219–1263. [Google Scholar] [CrossRef]
- Fox, B.D.; Shimony, A.; Langleben, D.; Hirsch, A.; Rudski, L.; Schlesinger, R.; Eisenberg, M.J.; Joyal, D.; Hudson, M.; Boutet, K.; et al. High prevalence of occult left heart disease in scleroderma-pulmonary hypertension. Eur. Respir. J. 2013, 42, 1083–1091. [Google Scholar] [CrossRef] [PubMed]
- Lammi, M.R.; Saketkoo, L.A.; Gordon, J.K.; Steen, V.D. Changes in hemodynamic classification over time are common in systemic sclerosis-associated pulmonary hypertension: Insights from the PHAROS cohort. Pulm. Circ. 2018, 8. [Google Scholar] [CrossRef] [PubMed]
- Mercurio, V.; Hassoun, P.M. Phenotyping pulmonary hypertension in systemic sclerosis: A moving target. Pulm. Circ. 2018, 8, 2045894018785247. [Google Scholar] [CrossRef] [PubMed]
- Allanore, Y.; Borderie, D.; Meune, C.; Cabanes, L.; Weber, S.; Ekindjian, O.G.; Kahan, A. N-Terminal Pro-Brain Natriuretic Peptide as a Diagnostic Marker of Early Pulmonary Artery Hypertension in Patients with Systemic Sclerosis and Effects of Calcium-Channel Blockers. Arthritis Rheum. 2003, 48, 3503–3508. [Google Scholar] [CrossRef]
- Oudiz, R.J. The role of exercise testing in the management of pulmonary arterial hypertension. Semin. Respir. Crit. Care Med. 2005, 26, 379–384. [Google Scholar] [CrossRef]
- de Camargo, V.M.; Martins, B.d.C.D.S.; Jardim, C.; Fernandes, C.J.C.; Hovnanian, A.; Souza, R. Validation of a treadmill six-minute walk test protocol for the evaluation of patients with pulmonary arterial hypertension. J. Bras. Pneumol. 2009, 35, 423–430. [Google Scholar] [CrossRef]
- Tedford, R.J.; Mudd, J.O.; Girgis, R.E.; Mathai, S.C.; Zaiman, A.L.; Housten-Harris, T.; Boyce, D.; Kelemen, B.W.; Bacher, A.C.; Shah, A.A.; et al. Right ventricular dysfunction in systemic sclerosis-associated pulmonary arterial hypertension. Circ. Hear. Fail. 2013, 6, 953–963. [Google Scholar] [CrossRef]
- Mukherjee, M.; Mercurio, V.; Tedford, R.J.; Shah, A.A.; Hsu, S.; Mullin, C.J.; Sato, T.; Damico, R.; Kolb, T.M.; Mathai, S.C.; et al. Right ventricular longitudinal strain is diminished in systemic sclerosis compared with idiopathic pulmonary arterial hypertension. Eur. Respir. J. 2017, 50, 1701436. [Google Scholar] [CrossRef]
- Mathai, S.C.; Hummers, L.K.; Champion, H.C.; Wigley, F.M.; Zaiman, A.; Hassoun, P.M.; Girgis, R.E. Survival in pulmonary hypertension associated with the scleroderma spectrum of diseases: Impact of interstitial lung disease. Arthritis Rheum. 2009, 60, 569–577. [Google Scholar] [CrossRef]
- Humbert, M.; Sitbon, O.; Chaouat, A.; Bertocchi, M.; Habib, G.; Gressin, V.; Yaïci, A.; Weitzenblum, E.; Cordier, J.F.; Chabot, F.; et al. Survival in patients with idiopathic, familial, and anorexigen-associated pulmonary arterial hypertension in the modern management era. Circulation 2010, 122, 156–163. [Google Scholar] [CrossRef]
- Benza, R.L.; Gomberg-Maitland, M.; Elliott, C.G.; Farber, H.W.; Foreman, A.J.; Frost, A.E.; McGoon, M.D.; Pasta, D.J.; Selej, M.; Burger, C.D.; et al. Predicting Survival in Patients With Pulmonary Arterial Hypertension: The REVEAL Risk Score Calculator 2.0 and Comparison With ESC/ERS-Based Risk Assessment Strategies. Chest 2019, 156, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Kelemen, B.W.; Mathai, S.C.; Tedford, R.J.; Damico, R.L.; Corona-Villalobos, C.; Kolb, T.M.; Chaisson, N.F.; Harris, T.H.; Zimmerman, S.L.; Kamel, I.R.; et al. Right ventricular remodeling in idiopathic and scleroderma-associated pulmonary arterial hypertension: Two distinct phenotypes. Pulm. Circ. 2015, 5, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Hsu, S.; Houston, B.A.; Tampakakis, E.; Bacher, A.C.; Rhodes, P.S.; Mathai, S.C.; Damico, R.L.; Kolb, T.M.; Hummers, L.K.; Shah, A.A.; et al. Right ventricular functional reserve in pulmonary arterial hypertension. Circulation 2016, 133, 2413–2422. [Google Scholar] [CrossRef] [PubMed]
- Hsu, S.; Kokkonen-Simon, K.M.; Kirk, J.A.; Kolb, T.M.; Damico, R.L.; Mathai, S.C.; Mukherjee, M.; Shah, A.A.; Wigley, F.M.; Margulies, K.B.; et al. Right ventricular myofilament functional differences in humans with systemic sclerosis-associated versus idiopathic pulmonary arterial hypertension. Circulation 2018, 137, 2360–2370. [Google Scholar] [CrossRef] [PubMed]
- Mercurio, V.; Mukherjee, M.; Tedford, R.J.; Zamanian, R.T.; Khair, R.M.; Sato, T.; Minai, O.A.; Torres, F.; Girgis, R.E.; Chin, K.; et al. Improvement in right ventricular strain with ambrisentan and tadalafil upfront therapy in scleroderma-associated pulmonary arterial hypertension. Am. J. Respir. Crit. Care Med. 2018, 197, 388–391. [Google Scholar] [CrossRef]
- Distler, O.; Highland, K.B.; Gahlemann, M.; Azuma, A.; Fischer, A.; Mayes, M.D.; Raghu, G.; Sauter, W.; Girard, M.; Alves, M.; et al. Nintedanib for systemic sclerosis-associated interstitial lung disease. N. Engl. J. Med. 2019, 380, 2518–2528. [Google Scholar] [CrossRef] [PubMed]
- Nannini, C.; West, C.P.; Erwin, P.J.; Matteson, E.L. Effects of cyclophosphamide on pulmonary function in patients with scleroderma and interstitial lung disease: A systematic review and meta-analysis of randomized controlled trials and observational prospective cohort studies. Arthritis Res. Ther. 2008, 10, 124. [Google Scholar] [CrossRef] [PubMed]
- Liossis, S.N.C.; Bounas, A.; Andonopoulos, A.P. Mycophenolate mofetil as first-line treatment improves clinically evident early scleroderma lung disease. Rheumatology 2006, 45, 1005–1008. [Google Scholar] [CrossRef] [PubMed]
- Tzouvelekis, A.; Galanopoulos, N.; Bouros, E.; Kolios, G.; Zacharis, G.; Ntolios, P.; Koulelidis, A.; Oikonomou, A.; Bouros, D. Effect and safety of mycophenolate mofetil or sodium in systemic sclerosis-associated interstitial lung disease: A meta-analysis. Pulm. Med. 2012, 2012, 143637. [Google Scholar] [CrossRef]
- Humbert, M.; Lau, E.M.T.; Montani, D.; Jaïs, X.; Sitbon, O.; Simonneau, G. Advances in therapeutic interventions for patients with pulmonary arterial hypertension. Circulation 2014, 130, 2189–2208. [Google Scholar] [CrossRef]
- Kolb, M.; Raghu, G.; Wells, A.U.; Behr, J.; Richeldi, L.; Schinzel, B.; Quaresma, M.; Stowasser, S.; Martinez, F.J. Nintedanib plus sildenafil in patients with idiopathic pulmonary fibrosis. N. Engl. J. Med. 2018, 379, 1722–1731. [Google Scholar] [CrossRef] [PubMed]
- King, C.S.; Shlobin, O.A. The Trouble with Group 3 Pulmonary Hypertension in Interstitial Lung Disease: Dilemmas in Diagnosis and the Conundrum of Treatment. Chest 2020. [Google Scholar] [CrossRef] [PubMed]
- Kido, K.; Coons, J.C. Efficacy and Safety of the Use of Pulmonary Arterial Hypertension Pharmacotherapy in Patients with Pulmonary Hypertension Secondary to Left Heart Disease: A Systematic Review. Pharmacotherapy 2019, 39, 929–945. [Google Scholar] [CrossRef] [PubMed]
- Vachiéry, J.L.; Delcroix, M.; Al-Hiti, H.; Efficace, M.; Hutyra, M.; Lack, G.; Papadakis, K.; Rubin, L.J. Macitentan in pulmonary hypertension due to left ventricular dysfunction. Eur. Respir. J. 2018, 51. [Google Scholar] [CrossRef] [PubMed]
- Almaaitah, S.; Highland, K.B.; Tonelli, A.R. Management of pulmonary arterial hypertension in patients with systemic sclerosis. Integr. Blood Press. Control. 2020, 13, 15–29. [Google Scholar] [CrossRef]
- Galiè, N.; Olschewski, H.; Oudiz, R.J.; Torres, F.; Frost, A.; Ghofrani, H.A.; Badesch, D.B.; McGoon, M.D.; McLaughlin, V.V.; Roecker, E.B.; et al. Ambrisentan for the treatment of pulmonary arterial hypertension: Results of the ambrisentan in pulmonary arterial hypertension, randomized, double-Blind, placebo-controlled, multicenter, efficacy (ARIES) study 1 and 2. Circulation 2008, 117, 3010–3019. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.; Denton, C.P.; Matucci-Cerinic, M.; Gillies, H.; Blair, C.; Tislow, J.; Nathan, S.D. Ambrisentan response in connective tissue disease-associated pulmonary arterial hypertension (CTD-PAH)—A subgroup analysis of the ARIES-E clinical trial. Respir. Med. 2016, 117, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Rubin, L.J.; Badesch, D.B.; Barst, R.J.; Galiè, N.; Black, C.M.; Keogh, A.; Pulido, T.; Frost, A.; Roux, S.; Leconte, I.; et al. Bosentan therapy for pulmonary arterial hypertension. N. Engl. J. Med. 2002, 346, 896–903. [Google Scholar] [CrossRef]
- Matucci-Cerinic, M.; Denton, C.P.; Furst, D.E.; Mayes, M.D.; Hsu, V.M.; Carpentier, P.; Wigley, F.M.; Black, C.M.; Fessler, B.J.; Merke, P.A.; et al. Bosentan treatment of digital ulcers related to systemic sclerosis: Results from the RAPIDS-2 randomised, double-blind, placebo-controlled trial. Ann. Rheum. Dis. 2011, 70, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Mercurio, V.; Bianco, A.; Campi, G.; Cuomo, A.; Diab, N.; Mancini, A.; Parrella, P.; Petretta, M.; Hassoun, P.M.; Bonaduce, D. New Drugs, Therapeutic Strategies, and Future Direction for the Treatment of Pulmonary Arterial Hypertension. Curr. Med. Chem. 2018, 26, 2844–2864. [Google Scholar] [CrossRef]
- Pulido, T.; Adzerikho, I.; Channick, R.N.; Delcroix, M.; Galiè, N.; Ghofrani, H.-A.; Jansa, P.; Jing, Z.-C.; Le Brun, F.-O.; Mehta, S.; et al. Macitentan and Morbidity and Mortality in Pulmonary Arterial Hypertension. N. Engl. J. Med. 2013, 369, 809–818. [Google Scholar] [CrossRef] [PubMed]
- Rhee, R.L.; Gabler, N.B.; Sangani, S.; Praestgaard, A.; Merkel, P.A.; Kawut, S.M. Comparison of treatment response in idiopathic and connective tissue disease-associated pulmonary arterial hypertension. Am. J. Respir. Crit. Care Med. 2015, 192, 1111–1117. [Google Scholar] [CrossRef] [PubMed]
- Chin, K.; Kim, N.; Channick, R.; Muros-Le Rouzic, E.; Selej, M.; McLaughlin, V. OPUS Registry: Treatment Patterns and Safety of Macitentan in Patients With Pulmonary Arterial Hypertension Associated With Systemic Sclerosis (PAH-SSc). Chest 2017, 152, A999–A1000. [Google Scholar] [CrossRef]
- McLaughlin, V.; Channick, R.; Kim, N.; Lammi, M.; Sulica, R.; Brand, M.; Flynn, M.; Leroy, S.; Morganti, A.; Chin, K. Macitentan in Pulmonary Arterial Hypertension Associated With Connective Tissue Disease: Real-World Evidence From the Combined Opus/Orpheus Data Sets. Chest 2019, 156, A874–A876. [Google Scholar] [CrossRef]
- Galiè, N.; Müller, K.; Scalise, A.V.; Grünig, E. Patent Plus: A blinded, randomised and extension study of riociguat plus sildenafil in pulmonary arterial hypertension. Eur. Respir. J. 2015, 45, 1314–1322. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Ghofrani, H.A.; Torbicki, A.; Barst, R.J.; Rubin, L.J.; Badesch, D.; Fleming, T.; Parpia, T.; Burgess, G.; Branzi, A.; et al. Sildenafil citrate therapy for pulmonary arterial hypertension. N. Engl. J. Med. 2005, 353, 2148–2157. [Google Scholar] [CrossRef] [PubMed]
- Badesch, D.B.; Hill, N.S.; Burgess, G.; Rubin, L.J.; Barst, R.J.; Galiè, N.; Simonneau, G. Sildenafil for pulmonary arterial hypertension associated with connective tissue disease. J. Rheumatol. 2007, 34, 2417–2422. [Google Scholar] [PubMed]
- Galiè, N.; Brundage, B.H.; Ghofrani, H.A.; Oudiz, R.J.; Simonneau, G.; Safdar, Z.; Shapiro, S.; White, R.J.; Chan, M.; Beardsworth, A.; et al. Tadalafil therapy for pulmonary arterial hypertension. Circulation 2009, 119, 2894–2903. [Google Scholar] [CrossRef] [PubMed]
- Goudie, A.R.; Lipworth, B.J.; Hopkinson, P.J.; Wei, L.; Struthers, A.D. Tadalafil in patients with chronic obstructive pulmonary disease: A randomised, double-blind, parallel-group, placebo-controlled trial. Lancet Respir. Med. 2014, 2, 293–300. [Google Scholar] [CrossRef]
- Kowal-Bielecka, O.; Fransen, J.; Avouac, J.; Becker, M.; Kulak, A.; Allanore, Y.; Distler, O.; Clements, P.; Cutolo, M.; Czirjak, L.; et al. Update of EULAR recommendations for the treatment of systemic sclerosis. Ann. Rheum. Dis. 2017, 76, 1327–1339. [Google Scholar] [CrossRef]
- Ghofrani, H.A.; Galiè, N.; Grimminger, F.; Grünig, E.; Humbert, M.; Jing, Z.C.; Keogh, A.M.; Langleben, D.; Kilama, M.O.; Fritsch, A.; et al. Riociguat for the treatment of pulmonary arterial hypertension. N. Engl. J. Med. 2013, 369, 330–340. [Google Scholar] [CrossRef] [PubMed]
- Rubin, L.J.; Galié, N.; Grimminger, F.; Grünig, E.; Humbert, M.; Jing, Z.C.; Keogh, A.; Langleben, D.; Fritsch, A.; Menezes, F.; et al. Riociguat for the treatment of pulmonary arterial hypertension: A long-term extension study (patent-2). Eur. Respir. J. 2015, 45, 1303–1313. [Google Scholar] [CrossRef] [PubMed]
- Humbert, M.; Coghlan, J.G.; Ghofrani, H.A.; Grimminger, F.; He, J.G.; Riemekasten, G.; Vizza, C.D.; Boeckenhoff, A.; Meier, C.; De Oliveira Pena, J.; et al. Riociguat for the treatment of pulmonary arterial hypertension associated with connective tissue disease: Results from PATENT-1 and PATENT-2. Ann. Rheum. Dis. 2017, 76, 422–426. [Google Scholar] [CrossRef] [PubMed]
- Sitbon, O.; Channick, R.; Chin, K.M.; Frey, A.; Gaine, S.; Galiè, N.; Ghofrani, H.A.; Hoeper, M.M.; Lang, I.M.; Preiss, R.; et al. Selexipag for the treatment of pulmonary arterial hypertension. N. Engl. J. Med. 2015, 373, 2522–2533. [Google Scholar] [CrossRef] [PubMed]
- Gaine, S.; Chin, K.; Coghlan, G.; Channick, R.; Di Scala, L.; Galiè, N.; Ghofrani, H.A.; Lang, I.M.; McLaughlin, V.; Preiss, R.; et al. Selexipag for the treatment of connective tissue disease-associated pulmonary arterial hypertension. Eur. Respir. J. 2017, 50. [Google Scholar] [CrossRef] [PubMed]
- Klings, E.S.; Hill, N.S.; Ieong, M.H.; Simms, R.W.; Korn, J.H.; Farber, H.W. Systemic sclerosis-associated pulmonary hypertension: Short- and long- term effects of epoprostenol (prostacyclin). Arthritis Rheum. 1999, 42, 2638–2645. [Google Scholar] [CrossRef]
- Oudiz, R.J.; Schilz, R.J.; Barst, R.J.; Galié, N.; Rich, S.; Rubin, L.J.; Simonneau, G. Treprostinil, a prostacyclin analogue, in pulmonary arterial hypertension associated with connective tissue disease. Chest 2004, 126, 420–427. [Google Scholar] [CrossRef]
- Caravita, S.; Wu, S.C.; Secchi, M.B.; Dadone, V.; Bencini, C.; Pierini, S. Long-term effects of intermittent Iloprost infusion on pulmonary arterial pressure in connective tissue disease. Eur. J. Intern. Med. 2011, 22, 518–521. [Google Scholar] [CrossRef]
- Galiè, N.; Channick, R.N.; Frantz, R.P.; Grünig, E.; Jing, Z.C.; Moiseeva, O.; Preston, I.R.; Pulido, T.; Safdar, Z.; Tamura, Y.; et al. Risk stratification and medical therapy of pulmonary arterial hypertension. Eur. Respir. J. 2019, 53. [Google Scholar] [CrossRef]
- Benza, R.L.; Miller, D.P.; Gomberg-Maitland, M.; Frantz, R.P.; Foreman, A.J.; Coffey, C.S.; Frost, A.; Barst, R.J.; Badesch, D.B.; Elliott, C.G.; et al. Predicting survival in pulmonary arterial hypertension: Insights from the registry to evaluate early and long-term pulmonary arterial hypertension disease management (REVEAL). Circulation 2010, 122, 164–172. [Google Scholar] [CrossRef]
- Boucly, A.; Weatherald, J.; Savale, L.; Jaïs, X.; Cottin, V.; Prevot, G.; Picard, F.; De Groote, P.; Jevnikar, M.; Bergot, E.; et al. Risk assessment, prognosis and guideline implementation in pulmonary arterial hypertension. Eur. Respir. J. 2017, 50. [Google Scholar] [CrossRef] [PubMed]
- Kylhammar, D.; Kjellström, B.; Hjalmarsson, C.; Jansson, K.; Nisell, M.; Söderberg, S.; Wikström, G.; Rådegran, G. A comprehensive risk stratification at early follow-up determines prognosis in pulmonary arterial hypertension. Eur. Heart J. 2018, 39, 4175–4181. [Google Scholar] [CrossRef] [PubMed]
- Hoeper, M.M.; Kramer, T.; Pan, Z.; Eichstaedt, C.A.; Spiesshoefer, J.; Benjamin, N.; Olsson, K.M.; Meyer, K.; Vizza, C.D.; Vonk-Noordegraaf, A.; et al. Mortality in pulmonary arterial hypertension: Prediction by the 2015 European pulmonary hypertension guidelines risk stratification model. Eur. Respir. J. 2017, 50. [Google Scholar] [CrossRef] [PubMed]
- Mercurio, V.; Diab, N.; Peloquin, G.; Housten-Harris, T.; Damico, R.; Kolb, T.M.; Mathai, S.C.; Hassoun, P.M. Risk assessment in scleroderma patients with newly diagnosed pulmonary arterial hypertension: Application of the ESC/ERS risk prediction model. Eur. Respir. J. 2018, 52, 1800497. [Google Scholar] [CrossRef]
- Gali, N.; Palazzini, M.; Manes, A. Pulmonary arterial hypertension: From the kingdom of the near-dead to multiple clinical trial meta-analyses. Eur. Heart J. 2010, 31, 2080–2086. [Google Scholar] [CrossRef]
- Jansa, P.; Pulido, T. Macitentan in Pulmonary Arterial Hypertension: A Focus on Combination Therapy in the seraphin trial. Am. J. Cardiovasc. Drugs 2018, 18, 1–11. [Google Scholar] [CrossRef]
- Coghlan, J.G.; Channick, R.; Chin, K.; Di Scala, L.; Galiè, N.; Ghofrani, H.A.; Hoeper, M.M.; Lang, I.M.; McLaughlin, V.; Preiss, R.; et al. Targeting the Prostacyclin Pathway with Selexipag in Patients with Pulmonary Arterial Hypertension Receiving Double Combination Therapy: Insights from the Randomized Controlled GRIPHON Study. Am. J. Cardiovasc. Drugs 2018, 18, 37–47. [Google Scholar] [CrossRef]
- Galie, N.; Barbera, J.A.; Frost, A.E.; Ghofrani, H.A.; Hoeper, M.M.; McLaughlin, V.V.; Peacock, A.J.; Simonneau, G.; Vachiery, J.L.; Grunig, E.; et al. Initial use of ambrisentan plus tadalafil in pulmonary arterial hypertension. N. Engl. J. Med. 2015, 373, 834–844. [Google Scholar] [CrossRef]
- Coghlan, J.G.; Galiè, N.; Barberà, J.A.; Frost, A.E.; Ghofrani, H.A.; Hoeper, M.M.; Kuwana, M.; McLaughlin, V.V.; Peacock, A.J.; Simonneau, G.; et al. Initial combination therapy with ambrisentan and tadalafil in connective tissue disease-associated pulmonary arterial hypertension (CTD-PAH): Subgroup analysis from the AMBITION trial. Ann. Rheum. Dis. 2017, 76, 1219–1227. [Google Scholar] [CrossRef] [PubMed]
- Hassoun, P.M.; Zamanian, R.T.; Damico, R.; Lechtzin, N.; Khair, R.; Kolb, T.M.; Tedford, R.J.; Hulme, O.L.; Housten, T.; Pisanello, C.; et al. Ambrisentan and tadalafil up-front combination therapy in scleroderma-associated pulmonary arterial hypertension. Am. J. Respir. Crit. Care Med. 2015, 192, 1102–1110. [Google Scholar] [CrossRef]
- NCT02682511 Oral Ifetroban to Treat Diffuse Cutaneous Systemic Sclerosis (SSc) or SSc-associated Pulmonary Arterial Hypertension. 2016. Available online: Https://clinicaltrials.gov/show/nct02682511 (accessed on 15 March 2020).
- NCT02981082 Dimethyl Fumarate (DMF) in Systemic Sclerosis-Associated Pulmonary Arterial Hypertension. 2016. Available online: https://clinicaltrials.gov/show/nct02981082 (accessed on 2 December 2016).
- EUCTR2016-004793-17-DE Bardoxolone Methyl Evaluation in Patients with Pulmonary Hypertension (PH). Available online: http://www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2016-004793-17-DE (accessed on 6 March 2017).
- NCT01086540 Rituximab for Treatment of Systemic Sclerosis-Associated Pulmonary Arterial Hypertension (SSc-PAH). 2010. Available online: https://clinicaltrials.gov/show/nct01086540 (accessed on 15 March 2010).
- Zamanian, R.; Badesch, D.; Chung, L.; Domsic, R.; Medsger, T.; Pinckney, A.; Keyes-Elstein, L.; D’Aveta, C.; Spychala, M.; White, J.; et al. Late Breaking Abstract—Safety and efficacy of B-cell depletion with rituximab for the treatment of systemic sclerosis-associated pulmonary arterial hypertension. Eur. Respir. J. 2019, 54. [Google Scholar] [CrossRef]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Attanasio, U.; Cuomo, A.; Pirozzi, F.; Loffredo, S.; Abete, P.; Petretta, M.; Marone, G.; Bonaduce, D.; De Paulis, A.; Rossi, F.W.; et al. Pulmonary Hypertension Phenotypes in Systemic Sclerosis: The Right Diagnosis for the Right Treatment. Int. J. Mol. Sci. 2020, 21, 4430. https://doi.org/10.3390/ijms21124430
Attanasio U, Cuomo A, Pirozzi F, Loffredo S, Abete P, Petretta M, Marone G, Bonaduce D, De Paulis A, Rossi FW, et al. Pulmonary Hypertension Phenotypes in Systemic Sclerosis: The Right Diagnosis for the Right Treatment. International Journal of Molecular Sciences. 2020; 21(12):4430. https://doi.org/10.3390/ijms21124430
Chicago/Turabian StyleAttanasio, Umberto, Alessandra Cuomo, Flora Pirozzi, Stefania Loffredo, Pasquale Abete, Mario Petretta, Gianni Marone, Domenico Bonaduce, Amato De Paulis, Francesca Wanda Rossi, and et al. 2020. "Pulmonary Hypertension Phenotypes in Systemic Sclerosis: The Right Diagnosis for the Right Treatment" International Journal of Molecular Sciences 21, no. 12: 4430. https://doi.org/10.3390/ijms21124430
APA StyleAttanasio, U., Cuomo, A., Pirozzi, F., Loffredo, S., Abete, P., Petretta, M., Marone, G., Bonaduce, D., De Paulis, A., Rossi, F. W., Tocchetti, C. G., & Mercurio, V. (2020). Pulmonary Hypertension Phenotypes in Systemic Sclerosis: The Right Diagnosis for the Right Treatment. International Journal of Molecular Sciences, 21(12), 4430. https://doi.org/10.3390/ijms21124430








