Preimplantation Genetic Testing: Where We Are Today
Abstract
1. Introduction
2. PGT Techniques
2.1. Polar Body Biopsy
2.2. Blastomere Biopsy
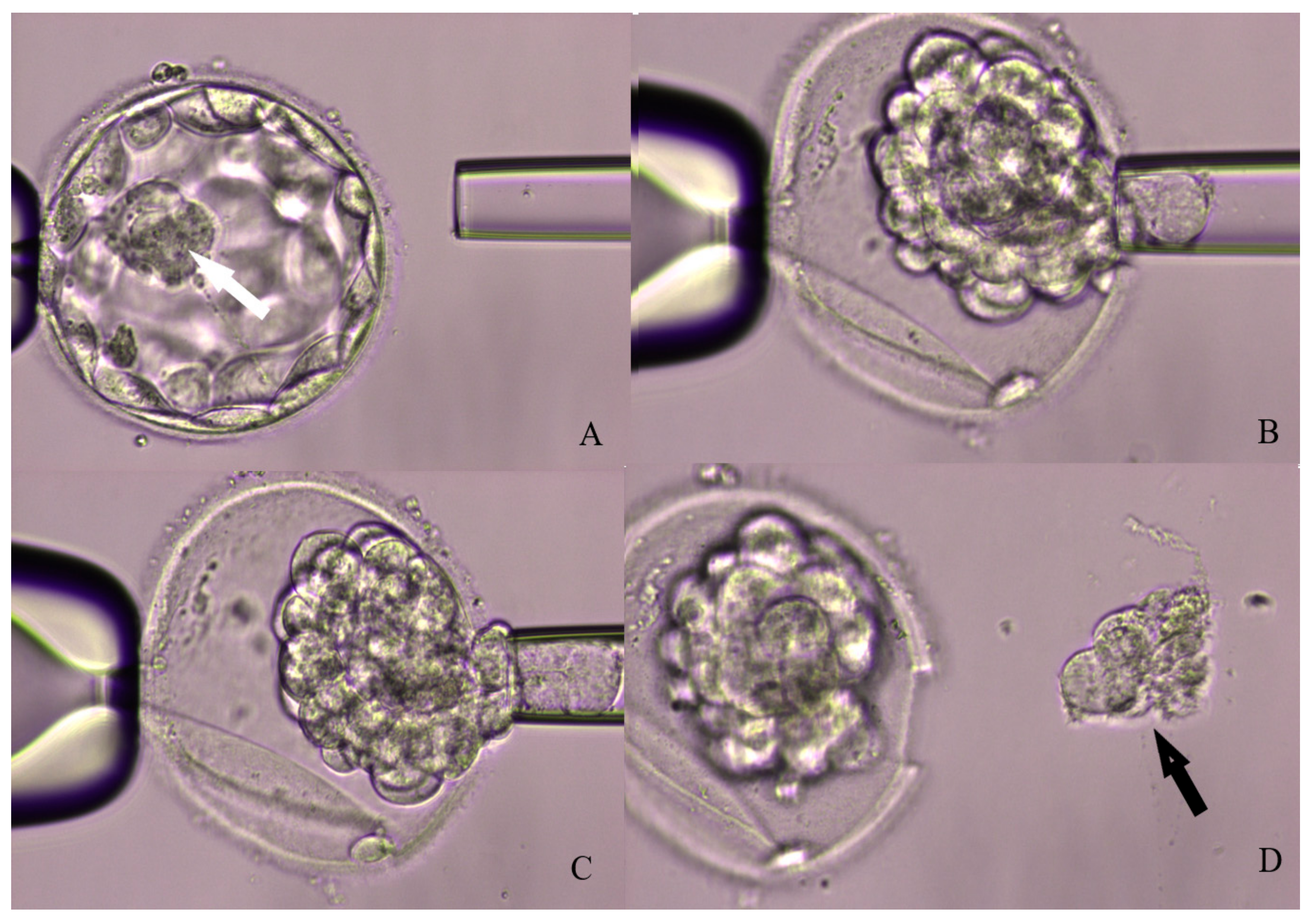
2.3. Trophoectoderm Biopsy
2.4. Non-Invasive PGT
3. PGT Molecular Techniques
4. Current Insications for PGT
4.1. Advanced Maternal Age
4.2. Recurrent Pregnancy Loss
4.3. Repeated Implantation Failure
4.4. Male Factor Infertility
4.5. PGT in a Good-Prognosis Patients Undergoing SET
4.6. PGT-A in Donor Egg Cycles
4.7. PGT for Monogenic Diseases
5. Mosaicism
6. Strategies for Euploid/Mosaic Blastocysts Transfer
7. Maternal and Neonatal Outcomes
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| PGT | Preimplantation genetic testing |
| IVF | in-vitro fertilization |
| SET | Single embryo transfer |
| PGT-A | Preimplantation gentic testing for aneuploidies |
| LB | Live birth |
| FISH | Fluorescence in Situ Hybridization |
| aCGH | Array-Comparative Genomic Hybridization |
| NGS | Next Generation Sequencing |
| rtq-PCR | Real Time Quantitative Polymerase Chain Reaction |
| PB | Polar body |
| ICSI | Intracitoplasmatic sperm injection |
| TE | Trophoectoderm |
| BF | Blastocyst fluid |
| WGA | Whole Genome Amplification |
| AMH | Anti-Müllerian hormone |
| AMA | Advanced maternal age |
| FTET | Frozen.thawed embryo transfer |
| RPL | Recurrent pregnancy loss |
| PGT-M | Preimplantation gentic testing for monogenic disease |
| DOR | Diminished ovarian reserve |
| RIF | Repeated implantation failure |
| SMF | Severe male factor |
| KS | Klinefelter syndrome |
| WHO | World Health Organization |
| NOA | Nonobstructive azoospermia |
| DFI | DNA fragmentation index |
| SCOS | Sertoli cell-only syndrome |
| DE | Donor egg |
References
- Kupka, M.S.; Ferraretti, A.P.; de Mouzon, J.; Erb, K.; D’Hooghe, T.; Castilla, J.A.; Calhaz-Jorge, C.; De Geyter, C. Assisted reproductive technology in Europe, 2010: Results generated from European registers by ESHRE. Hum. Reprod. 2014, 29, 2099–2113. [Google Scholar] [CrossRef]
- Paternot, G.; Devroe, J.; Debrock, S.; D’Hooghe, T.M.; Spiessens, C. Intra- and inter-observer analysis in the morphological assessment of early-stage embryos. Reprod. Biol. Endocrinol. 2009, 7, 105. [Google Scholar] [CrossRef]
- Abeyta, M.; Behr, B. Morphological assessment of embryo viability. Semin. Reprod. Med. 2014, 32, 114–126. [Google Scholar] [CrossRef]
- Minasi, M.G.; Colasante, A.; Riccio, T.; Ruberti, A.; Casciani, V.; Scarselli, F.; Spinella, F.; Fiorentino, F.; Varricchio, M.T.; Greco, E. Correlation between aneuploidy, standard morphology evaluation and morphokinetic development in 1730 biopsied blastocysts: A consecutive case series study. Hum. Reprod. 2016, 31, 2245–2254. [Google Scholar] [CrossRef]
- Desai, N.; Ploskonk, S.; Goodman, L.R.; Austin, C.; Goldberg, J.; Falcone, T. Analysis of embryo morphokinetics, multinucleation and cleavage anomalies using continuous time-lapse monitoring in blastocyst transfer cycles. Reprod. Biol. Endocrinol. 2014, 20, 12–54. [Google Scholar] [CrossRef]
- Katz-Jaffe, M.G.; McReynolds, S. Embryology in the era of proteomics. Fertil. Steril. 2013, 15, 1073–1077. [Google Scholar] [CrossRef]
- Uyar, A.; Seli, E. Metabolomic assessment of embryo viability. Semin. Reprod. Med. 2014, 32, 141–152. [Google Scholar] [CrossRef]
- Papanikolaou, E.G.; Camus, M.; Kolibianakis, E.M.; Van Landuyt, L.; Van Steirteghem, A.; Devroey, P. In vitro fertilization with single blastocyst-stage versus single cleavage-stage embryos. N. Engl. J. Med. 2006, 354, 1139–1146. [Google Scholar] [CrossRef]
- Munne, S.; Chen, S. Cromosome abnormalities in over 6000 cleavage-stage embryos. Reprod. Biomed. Online 2007, 14, 628–634. [Google Scholar] [CrossRef]
- Forman, E.J.; Hong, K.H.; Franasiak, J.M.; Scott, R.J. Obstetrical and neonatal out-comes from the BEST Trial: Single embryo transfer with aneuploidy screening improves outcomes after in vitro fertilization without compromising delivery rates. Am. J. Obstet. Gynecol. 2014, 210, 157.e1–157.e6. [Google Scholar] [CrossRef]
- Fragouli, E.; Alfarawati, S.; Spath, K.; Jaroudi, S.; Sarasa, J.; Enciso, M. The origin and impact of embryonic aneuploidy. Hum. Genet. 2013, 132, 1001–1013. [Google Scholar] [CrossRef]
- Minasi, M.G.; Fiorentino, F.; Ruberti, A.; Biricik, A.; Cursio, E.; Cotroneo, E.; Varricchio, M.T.; Surdo, M.; Spinella, F.; Greco, E. Genetic diseases and aneuploidies can be detected with a single blastocyst biopsy: A successful clinical approach. Hum. Reprod. 2017, 32, 1770–1777. [Google Scholar] [CrossRef]
- Pandian, Z.; Bhattacharya, S.; Ozturk, O.; Serour, G.; Templeton, A. Number of embryos for transfer following in-vitro fertilisation or intra-cytoplasmic sperm injection. Cochrane Database Syst. Rev. 2009, 2, CD003416. [Google Scholar]
- Gelbaya, T.A.; Tsoumpou, I.; Nardo, L.G. The likelihood of live birth and multiple birth after single versus double embryo transfer at the cleavage stage: Asystematic review and meta-analysis. Fertil. Steril. 2010, 94, 936–994. [Google Scholar] [CrossRef]
- Fragouli, E.; Lenzi, M.; Ross, R.; Katz-Jaffe, M.; Schoolcraft, W.B.; Wells, D. Comprehensive molecular cytogenetic analysis of the human blastocyst stage. Hum. Reprod. 2008, 23, 2596–2608. [Google Scholar] [CrossRef]
- Alfarawati, S.; Fragouli, E.; Colls, P.; Stevens, J.; Gutiérrez-Mateo, C.; Schoolcraft, W.B.; Katz-Jaffe, M.G.; Wells, D. The relationship between blastocyst morphology, chromosomal abnormality, and embryo gender. Fertil. Steril. 2011, 95, 520–524. [Google Scholar] [CrossRef]
- Litwicka, K.; Mencacci, C.; Arrivi, C.; Varricchio, M.T.; Caragia, A.; Minasi, M.G.; Greco, E. HCG administration after endogenous LH rise negatively influences pregnancy rate in modified natural cycle for frozen-thawed-euploid-blastocyst-transfer: A pilot study. J. Assist. Reprod. Genet. 2018, 35, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Dahdouh, E.M.; Balayla, J.; García-Velasco, J.A. Impact of blastocyst biopsy and comprehensive chromosome screening technology on preimplantation genetic screening: A systematic review of randomized controlled trials. Reprod. Biomed. Online 2015, 30, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Sahin, L.; Bozkurt, M.; Sahin, H.; Gürel, A.; Yumru, A.E. Is preimplantation genetic diagnosis the ideal embryo selection method in aneuploidy screening? Kaohsiung J. Med. Sci. 2014, 30, 491–498. [Google Scholar] [CrossRef]
- Franasiak, J.M.; Forman, E.J.; Hong, K.H.; Werner, M.D.; Upham, K.M.; Treff, N.R. The nature of aneuploidy with increasing age of the female partner: A review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil. Steril. 2014, 101, 656–663. [Google Scholar] [CrossRef]
- Colaco, S.; Sakkas, D. Paternal factors contributing toembryoquality. J. Assist. Reprod. Genet. 2018, 35, 1953–1968. [Google Scholar] [CrossRef] [PubMed]
- Munné, S.; Lee, A.; Rosenwaks, Z.; Grifo, J.; Cohen, J. Diagnosis of major chromosome aneuploidies in human preimplantation embryos. Hum. Reprod. 1993, 8, 2185–2191. [Google Scholar] [CrossRef] [PubMed]
- Mastenbroek, S.; Twisk, M.; van der Veen, F.; Repping, S. Preimplantation genetic screening: A systematic review and meta-analysis of RCTs. Hum. Reprod. Update 2011, 17, 454–466. [Google Scholar] [CrossRef]
- Geraedts, J.; Collins, J.; Gianaroli, L.; Goossens, V.; Handyside, A.; Harper, J.; Montag, M.; Repping, S.; Schmutzler, A.G. What next for preimplantation genetic screening? A polar body approach! Hum. Reprod. 2010, 25, 575–577. [Google Scholar] [CrossRef] [PubMed]
- Schmutzler, A.G. Theory and practice of preimplantation genetic screening (PGS). Eur. J. Med. Genet. 2019, 62, 103670. [Google Scholar] [CrossRef] [PubMed]
- Delhanty, J.D. Is the polar body approach best for pre-implantation genetic screening? Placenta 2011, 32 (Suppl. 3), 68–70. [Google Scholar] [CrossRef]
- Verpoest, W.; Staessen, C.; Bossuyt, P.M.; Goossens, V.; Altarescu, G.; Bonduelle, M.; Devesa, M.; Eldar-Geva, T.; Gianaroli, L.; Griesinger, G.; et al. Preimplantation genetic testing for aneuploidy by microarray analysis of polar bodies in advanced maternal age: A randomized clinical trial. Hum. Reprod. 2018, 33, 1767–1776. [Google Scholar] [CrossRef]
- Neumann, K.; Sermon, K.; Bossuyt, P.; Goossens, V.; Geraedts, J.; Traeger-Synodinos, J.; Parriego, M.; Schmutzler, A.G.; van der Ven, K.; Rudolph-Rothfeld, W.; et al. An economic analysis of preimplantation genetic testing for aneuploidy by polar body biopsy in advanced maternal age. BJOG 2020, 127, 710–718. [Google Scholar] [CrossRef]
- Harton, G.L.; Magli, M.C.; Lundin, K.; Montag, M.; Lemmen, J.; Harper, J.C.; European Society for Human Reproduction and Embryology (ESHRE); PGD Consortium/Embryology Special Interest Group. ESHRE PGD Consortium/Embryology Special Interest Group-best practice guidelines for polar body and embryo biopsy for preimplantation genetic diagnosis/screening (PGD/PGS). Hum. Reprod. 2011, 26, 41–46. [Google Scholar]
- Capalbo, A.; Bono, S.; Spizzichino, L.; Biricik, A.; Baldi, M.; Colamaria, S.; Ubaldi, F.M.; Rienzi, L.; Fiorentino, F. Sequential comprehensive chromosome analysis onpolarbodies, blastomeres and trophoblast: Insights into female meiotic errors and chromosomal segregation in the preimplantation window of embryo development. Hum. Reprod. 2013, 28, 509–518. [Google Scholar] [CrossRef]
- Scott, K.L.; Hong, K.H.; Scott, R.T., Jr. Selecting the optimal time to perform biopsy for preimplantation genetic testing. Fertil. Steril. 2013, 100, 608–661. [Google Scholar] [CrossRef] [PubMed]
- Scott, R.T., Jr.; Upham, K.M.; Forman, E.J.; Hong, K.H.; Scott, K.L.; Taylor, D.; Tao, X.; Tref, N.R. Blastocyst biopsy with comprehensive chromosome screening and fresh embryo transfer significantly increases in vitro fertilization implantation and delivery rates: A randomized controlled trial. Fertil. Steril. 2013, 100, 697–703. [Google Scholar] [CrossRef] [PubMed]
- De Vos, A.; Staessen, C.; De Rycke, M.; Verpoest, W.; Haentjens, P.; Devroey, P.; Liebaers, I.; Van de Velde, H. Impact of cleavage-stage embryo biopsy in view of PGD on human blastocyst implantation: A prospective cohort of single embryo transfers. Hum. Reprod. 2009, 24, 2988–2996. [Google Scholar] [CrossRef]
- Zeng, M.; Su, S.; Li, L. Comparison of pregnancy outcomes after vitrification at the cleavage and blastocyst stage: A meta-analysis. J. Assist. Reprod. Genet. 2018, 35, 127–134. [Google Scholar] [CrossRef] [PubMed]
- McArthur, S.J.; Leigh, D.; Marshall, J.T.; de Boer, K.A.; Jansen, R.P. Pregnancies and live births after trophectoderm biopsy and preimplantation genetic testing of human blastocysts. Fertil. Steril. 2005, 84, 1628–1636. [Google Scholar] [CrossRef] [PubMed]
- Rubino, P.; Tapia, L.; Ruiz de Assin Alonso, R.; Mazmanian, K.; Guan, L.; Dearden, L.; Thiel, A.; Moon, C.; Kolb, B.; Norian, J.M.; et al. Trophectoderm biopsy protocols can affect clinical outcomes: Time to focus on the blastocyst biopsy technique. Fertil. Steril. 2020, 20, S0015–S0282. [Google Scholar] [CrossRef] [PubMed]
- Piccolomini, M.M.; Nicolielo, M.; Bonetti, T.C.; Motta, E.L.; Serafini, P.C.; Alegretti, J.R. Does slow embryo development predict a high aneuploidy rate on trophectoderm biopsy? Reprod. Biomed. Online 2016, 33, 398–403. [Google Scholar] [CrossRef]
- Taylor, T.H.; Patrick, J.L.; Gitlin, S.A.; Wilson, J.M.; Crain, J.L.; Griffin, D.K. Comparison of aneuploidy, pregnancy and live birth rates between day 5 and day 6 blastocysts. Reprod. Biomed. Online 2014, 29, 305–310. [Google Scholar] [CrossRef]
- Hernandez-Nieto, C.; Lee, J.A.; Slifkin, R.; Sandler, B.; Copperman, A.B.; Flisser, E. What is the reproductive potential of day 7 euploidembryos? Hum. Reprod. 2019, 34, 1697–1706. [Google Scholar] [CrossRef]
- Rienzi, L.; Capalbo, A.; Stoppa, M.; Romano, S.; Maggiulli, R.; Albricci, L.; Scarica, C.; Farcomeni, A.; Vajta, G.; Ubaldi, F.M. No evidence of association between blastocyst aneuploidy and morphokinetic assessment in a selected population of poor-prognosis patients: A longitudinal cohort study. Reprod. Biomed. Online 2015, 30, 57–66. [Google Scholar] [CrossRef]
- Hammond, E.R.; Cree, L.M.; Morbeck, D.E. Should extended blastocyst culture include Day 7? Hum. Reprod. 2018, 33, 991–997. [Google Scholar] [CrossRef] [PubMed]
- Poli, M.; Ori, A.; Child, T.; Jaroudi, S.; Spath, K.; Beck, M.; Wells, D. Characterization and quantification of proteins secreted by single human embryos prior to implantation. EMBO Mol. Med. 2015, 7, 1465–1479. [Google Scholar] [CrossRef] [PubMed]
- Magli, M.C.; Pomante, A.; Cafueri, G.; Valerio, M.; Crippa, A.; Ferraretti, A.P.; Gianaroli, L. Preimplantation genetic testing: Polar bodies, blastomeres, trophectoderm cells, or blastocoelic fluid? Fertil. Steril. 2016, 105, 676–683. [Google Scholar] [CrossRef]
- Marcos, J.; Pérez-Albalá, S.; Mifsud, A.; Molla, M.; Landeras, J.; Meseguer, M. Collapse of blastocysts is strongly related to lower implantation success: A time-lapse study. Hum. Reprod. 2015, 30, 2501–2508. [Google Scholar] [CrossRef]
- Bodri, D.; Sugimoto, T.; Yao Serna, J.; Kawachiya, S.; Kato, R.; Matsumoto, T. Blastocyst collapse is not an independent predictor of reduced live birth: A time-lapse study. Fertil. Steril. 2016, 105, 1476–1483. [Google Scholar] [CrossRef]
- Chen, S.U.; Lee, T.H.; Lien, Y.R.; Tsai, Y.Y.; Chang, L.J.; Yang, Y.S. Microsuction of blastocoelic fluid before vitrification increased survival and pregnancy of mouse expanded blastocysts, but pretreatment with the cytoskeletal stabilizer did not increase blastocyst survival. Fertil. Steril. 2005, 84 (Suppl. 2), 1156–1162. [Google Scholar] [CrossRef]
- Palini, S.; Galluzzi, L.; De Stefani, S.; Bianchi, M.; Wells, D.; Magnani, M.; Bulletti, C. Genomic DNA in human blastocoele fluid. Reprod. Biomed. Online 2013, 26, 603–610. [Google Scholar] [CrossRef]
- Tobler, K.J.; Zhao, Y.; Ross, R.; Benner, A.T.; Xu, X.; Du, L.; Broman, K.; Thrift, K.; Brezina, P.R.; Kearns, W.G. Blastocoel fluid from differentiated blastocysts harbors embryonic genomic material capable of a whole-genome deoxyribonucleic acid amplification and comprehensive chromosome microarray analysis. Fertil. Steril. 2015, 104, 418–425. [Google Scholar] [CrossRef]
- Handyside, A.H. Noninvasive preimplantation genetic testing: Dream or reality? Fertil. Steril. 2016, 106, 1324–1325. [Google Scholar] [CrossRef]
- Gianaroli, L.; Magli, M.C.; Pomante, A.; Crivello, A.M.; Cafueri, G.; Valerio, M.; Ferraretti, A.P. Blastocentesis: A source of DNA for preimplantation genetic testing. Results from a pilot study. Fertil. Steril. 2014, 102, 1692–1699. [Google Scholar] [CrossRef]
- Ho, J.R.; Arrach, N.; Rhodes-Long, K.; Ahmady, A.; Ingles, S.; Chung, K.; Bendikson, K.A.; Paulson, R.J.; McGinnis, L.K. Pushing the limits of detection: Investigation of cell-free DNA for aneuploidy screening in embryos. Fertil. Steril. 2018, 110, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Hammond, E.R.; McGillivray, B.C.; Wicker, S.M.; Peek, J.C.; Shelling, A.N.; Stone, P.; Chamley, L.W.; Cree, L.M. Characterizing nuclear and mitochondrial DNA in spent embryo culture media: Genetic contamination identified. Fertil. Steril. 2017, 107, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Capalbo, A.; Romanelli, V.; Patassini, C.; Poli, M.; Girardi, L.; Giancani, A.; Stoppa, M.; Cimadomo, D.; Ubaldi, F.M.; Rienzi, L. Diagnostic efficacy of blastocoel fluid and spent media as sources of DNA for preimplantation genetic testing in standard clinical conditions. Fertil. Steril. 2018, 110, 870–879. [Google Scholar] [CrossRef]
- Rodrigo, L.; Mateu, E.; Mercader, A.; Cobo, A.C.; Peinado, V.; Milán, M.; Al-Asmar, N.; Campos-Galindo, I.; García-Herrero, S.; Mir, P.; et al. New tools for embryo selection: Comprehensive chromosome screening by array comparative genomic hybridization. Biomed. Res. Int. 2014, 2014, 517125. [Google Scholar] [CrossRef]
- Northrop, L.E.; Treff, N.R.; Levy, B.; Scott, R.T., Jr. SNP microarray-based 24 chromosome aneuploidy screening demonstrates that cleavage-stage FISH poorly predicts aneuploidy in embryos that develop to morphologically normal blastocysts. Mol. Hum. Reprod. 2010, 16, 590–600. [Google Scholar] [CrossRef]
- Treff, N.R.; Tao, X.; Ferry, K.M.; Su, J.; Taylor, D.; Scott, R.T., Jr. Development and validation of an accurate quantitative real-time polymerase chain reaction-based assay for human blastocyst comprehensive chromosomal aneuploidy screening. Fertil. Steril. 2012, 97, 819–824. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Yan, L.; Lu, S.; Zhao, N.; Xie, X.S.; Qiao, J. Validation of a next-generation sequencing-based protocol for 24-chromosome aneuploidy screening of blastocysts. Fertil. Steril. 2016, 105, 1532–1536. [Google Scholar] [CrossRef]
- Vera-Rodríguez, M.; Michel, C.E.; Mercader, A.; Bladon, A.J.; Rodrigo, L.; Kokocinski, F.; Mateu, E.; Al-Asmar, N.; Blesa, D.; Simón, C.; et al. Distribution patterns of segmental aneuploidies in human blastocysts identified by next-generation sequencing. Fertil. Steril. 2016, 105, 1047–1055. [Google Scholar] [CrossRef]
- Fiorentino, F.; Biricik, A.; Bono, S.; Spizzichino, L.; Cotroneo, E.; Cottone, G.; Cottone, G.; Kokocinski, F.; Michel, C.M. Development and validation of a next-generation sequencing-based protocol for 24- chromosome aneuploidy screening of embryos. Fertil. Steril. 2014, 101, 1375–1382. [Google Scholar] [CrossRef]
- Friedenthal, J.; Maxwell, S.M.; Munné, S.; Kramer, Y.; McCulloh, D.H.; McCaffrey, C.; Grifo, J.A. Next generation sequencing for preimplantation genetic screening improves pregnancy outcomes compared with array comparative genomic hybridization in single thawed euploid embryo transfer cycles. Fertil. Steril. 2018, 109, 627–632. [Google Scholar] [CrossRef]
- Friedenthal, J.; Maxwell, S.M.; Tiegs, A.W.; Besser, A.G.; McCaffrey, C.; Munné, S.; Noyes, N.; Grifo, J.A. Clinical error rates of next generation sequencing and array comparative genomic hybridization with single thawed euploid embryo transfer. Eur. J. Med. Genet. 2020, 20, 103852. [Google Scholar] [CrossRef] [PubMed]
- Hassold, T.; Hunt, P. Maternal age and chromosomally abnormal pregnancies: What we know and what we wish we knew. Curr. Opin. Pediatr. 2009, 21, 703–708. [Google Scholar] [CrossRef]
- Rubio, C.; Rodrigo, L.; Mercader, A.; Mateu, E.; Buendia, P.; Pehlivan, T.; Viloria, T.; Santos, D.L.; Simon, C.; Remohi, J.; et al. Impact of chromosomal abnormalities on preimplantation embryo development. Prenat. Diagn. 2007, 27, 748–756. [Google Scholar] [CrossRef] [PubMed]
- Sandalinas, M.; Sadowy, S.; Alikani, M.; Calderon, G.; Cohen, J.; Munne, S. Developmental ability of chromosomally abnormal human embryos to develop to the blastocyst stage. Hum. Reprod. 2001, 16, 1954–1958. [Google Scholar] [CrossRef] [PubMed]
- Magli, M.C.; Jones, G.M.; Gras, L.; Gianaroli, L.; Korman, I.; Trounson, A.O. Chromosome mosaicism in day 3 aneuploid embryos that develop to morphologically normal blastocysts in vitro. Hum. Reprod. 2000, 15, 1781–1786. [Google Scholar] [CrossRef] [PubMed]
- Marquez, C.; Sandalinas, M.; Bahce, M.; Alikani, M.; Munne, S. Chromosome abnormalities in 1255 cleavage-stage human embryos. Reprod. Biomed. Online 2000, 1, 17–26. [Google Scholar] [CrossRef]
- Yang, Z.; Liu, J.; Collins, G.S.; Salem, S.A.; Liu, X.; Lyle, S.S.; Peck, A.C.; Scott, E.S.; Salem, R.D. Selection of single blastocysts for fresh transfer via standard morphology assessment alone and with array CGH for good prognosis IVF patients: Results from a randomized pilot study. Mol. Cytogenet. 2012, 5, 24. [Google Scholar] [CrossRef]
- Rabinowitz, M.; Ryan, A.; Gemelos, G.; Hill, M.; Baner, J.; Cinnioglu, C.; Banjevic, M.; Potter, D.; Petrov, D.A.; Demko, Z. Origins and rates of aneuploidy in human blastomeres. Fertil. Steril. 2012, 97, 395–400. [Google Scholar] [CrossRef]
- Jiang, X.; Yan, J.; Sheng, Y.; Sun, M.; Cui, L.; Chen, Z.J. Low anti-Müllerian hormone concentration is associated with increased risk of embryonic aneuploidy in women of advanced age. Reprod. Biomed. Online 2018, 37, 178–183. [Google Scholar] [CrossRef]
- Munne, S.; Chen, S.; Fischer, J.; Colls, P.; Zheng, X.; Stevens, J.; Escudero, T.; Oter, M.; Schoolcraft, B.; Simpson, J.L.; et al. Preimplantation genetic diagnosis reduces pregnancy loss in women aged 35 years and older with a history of recurrent miscarriages. Fertil. Steril. 2005, 4, 331–335. [Google Scholar] [CrossRef]
- Rubio, C.; Bellver, J.; Rodrigo, L.; Bosch, E.; Mercader, A.; Vidal, C.; De Los Santos, M.J.; Giles, J.; Labarta, E.; Domingo, J.; et al. Preimplantation genetic screening using fluorescence in situ hybridization in patients with repetitive implantation failure and advanced maternal age: Two randomized trials. Fertil. Steril. 2013, 99, 1400–1407. [Google Scholar] [CrossRef]
- Scott, R.T., Jr.; Ferry, K.; Su, J.; Tao, X.; Scott, K.; Treff, N.R. Comprehensive chromosome screening is highly predictive of the reproductive potential of human embryos: A prospective, blinded, nonselection study. Fertil. Steril. 2012, 97, 870–875. [Google Scholar] [CrossRef] [PubMed]
- Grifo, J.A.; Hodes-Wertz, B.; Lee, H.L.; Amperloquio, E.; Clarke-Williams, M.; Adler, A. Single thawed euploid embryo transfer improves IVF pregnancy, miscarriage, and multiple gestation outcomes and has similar implantation rates as egg donation. J. Assist. Reprod. Genet. 2013, 30, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Harton, G.L.; Munné, S.; Surrey, M.; Grifo, J.; Kaplan, B.; McCulloh, D.H.; Griffin, D.K.; Wells, D. Diminished effect of maternal age on implantation after preimplantation genetic diagnosis with array comparative genomic hybridization. Fertil. Steril. 2013, 100, 1695–1703. [Google Scholar] [CrossRef]
- Platteau, P.; Staessen, C.; Michiels, A.; Van Steirteghem, A.; Liebaers, I.; Devroey, P. Preimplantation genetic diagnosis for aneuploidy screening in women older than 37 years. Fertil. Steril. 2005, 84, 319–324. [Google Scholar] [CrossRef]
- Rubio, C.; Bellver, J.; Rodrigo, L.; Castillón, G.; Guillén, A.; Vidal, C.; Giles, J.; Ferrando, M.; Cabanillas, S.; Remohí, J.; et al. In vitro fertilization with preimplantation genetic diagnosis for aneuploidies in advanced maternal age: A randomized, controlled study. Fertil. Steril. 2017, 107, 1122–1129. [Google Scholar] [CrossRef]
- Sacchi, L.; Albani, E.; Cesana, A.; Smeraldi, A.; Parini, V.; Fabiani, M.; Poli, M.; Capalbo, A.; Levi-Setti, P.E. Preimplantation Genetic Testing for Aneuploidy Improves Clinical, Gestational, and Neonatal Outcomes in Advanced Maternal Age Patients Without Compromising Cumulative Live-Birth Rate. J. Assist. Reprod. Genet. 2019, 36, 2493–2504. [Google Scholar] [CrossRef]
- Ubaldi, F.M.; Cimadomo, D.; Capalbo, A.; Vaiarelli, A.; Buffo, L.; Trabucco, E.; Ferrero, S.; Albani, E.; Rienzi, L.; Levi-Setti, P.E. Preimplantation genetic diagnosis for aneuploidy testing in women older than 44 years: A multicenter experience. Fertil. Steril. 2017, 107, 1173–1180. [Google Scholar] [CrossRef]
- Lee, H.L.; McCulloh, D.H.; Hodes-Wertz, B.; Adler, A.; McCaffrey, C.; Grifo, J.A. In vitro fertilization with preimplantation genetic screening improves implantation and live birth in women age 40 through 43. J. Assist. Reprod. Genet. 2015, 32, 435–444. [Google Scholar] [CrossRef]
- Reig, A.; Franasiak, J.; Scott, R.T., Jr.; Seli, E. The impact of age beyond ploidy: Outcome data from 8175 euploid single embryo transfers. J. Assist. Reprod. Genet. 2020, 37, 595–602. [Google Scholar] [CrossRef]
- Jauniaux, E.; Farquharson, R.G.; Christiansen, O.B.; Exalto, N. Evidence-based guidelines for the investigation and medical treatment of recurrent miscarriage. Hum. Reprod. 2006, 21, 2216–2222. [Google Scholar] [CrossRef] [PubMed]
- Rai, R.; Regan, L. Recurrent miscarriage. Lancet 2006, 368, 601–611. [Google Scholar] [CrossRef]
- Stephenson, M.; Kutteh, W. Evaluation and management of recurrent early pregnancy loss. Clin. Obstet. Gynecol. 2007, 50, 132–145. [Google Scholar] [CrossRef]
- Stephenson, M.D.; Awartani, K.A.; Robinson, W.P. Cytogenetic analysis of miscarriages from couples with recurrent miscarriage: A case-control study. Hum. Reprod. 2002, 17, 446–451. [Google Scholar] [CrossRef]
- Bianco, K.; Caughey, A.B.; Shaffer, B.L.; Davis, R.; Norton, M.E. History of miscarriage and increased incidence of fetal aneuploidy in subsequent pregnancy. Obstet. Gynecol. 2006, 107, 1098–1102. [Google Scholar] [CrossRef]
- Fritz, B.; Hallermann, C.; Olert, J.; Fuchs, B.; Bruns, M.; Aslan, M.; Schmidt, S.; Coerdt, W.; Müntefering, H.; Rehder, H. Cytogenetic analyses of culture failures by comparative genomic hybridisation (CGH)-Re-evaluation of chromosome aberration rates in early spontaneous abortions. Eur. J. Hum. Genet. 2001, 9, 539–547. [Google Scholar] [CrossRef]
- Sullivan, A.E.; Silver, R.M.; LaCoursiere, D.Y.; Porter, T.F.; Branch, D.W. Recurrent fetal aneuploidy and recurrent miscarriage. Obstet. Gynecol. 2004, 104, 784–788. [Google Scholar] [CrossRef]
- Rubio, C.; Simon, C.; Vidal, F.; Rodrigo, L.; Pehlivan, T.; Remohi, J.; Pellicer, A. Chromosomal abnormalities and embryo development in recurrent miscarriage couples. Hum. Reprod. 2003, 18, 182–188. [Google Scholar] [CrossRef]
- Musters, A.M.; Repping, S.; Korevaar, J.C.; Mastenbroek, S.; Limpens, J.; van der Veen, F.; Goddijn, M. Pregnancy outcome after preimplantation genetic screening or natural conception in couples with unexplained recurrent miscarriage: A systematic review of the best available evidence. Fertil. Steril. 2011, 95, 2153–2157. [Google Scholar] [CrossRef]
- Platteau, P.; Staessen, C.; Michiels, A.; Van Steirteghem, A.; Liebaers, I.; Devroey, P. Preimplantation genetic diagnosis for aneuploidy screening in patients with unexplained recurrent miscarriages. Fertil. Steril. 2005, 83, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Wilding, M.; Forman, R.; Hogewind, G.; di Matteo, L.; Zullo, F.; Cappiello, F.; Dale, B. Preimplantation genetic diagnosis for the treatment of failed in vitro fertilization–embryo transfer and habitual abortion. Fertil. Steril. 2004, 81, 1302–1307. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.Y.; Fan, Q.; Wang, J.; Li, R.; Xu, Y.; Guo, J.; Wang, Y.Z.; Zeng, Y.H.; Ding, C.H.; Cai, B.; et al. Higher chromosomal abnormality rate in blastocysts from young patients with idiopathic recurrent pregnancy loss. Fertil. Steril. 2020, 113, 853–864. [Google Scholar] [CrossRef] [PubMed]
- Hodes-Wertz, B.; Grifo, J.; Ghadir, S.; Kaplan, B.; Laskin, C.A.; Glassner, M.; Munné, S. Idiopathic recurrent miscarriage is caused mostly by aneuploid embryos. Fertil. Steril. 2012, 98, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Sugiura-Ogasawara, M.; Ozawa, F.; Yamamoto, T.; Kato, T.; Kurahashi, H.; Kuroda, T.; Aoyama, N.; Kato, K.; Kobayashi, R.; et al. Preimplantation genetic testing for aneuploidy: A comparison of live birth rates in patients with recurrent pregnancy loss due to embryonic aneuploidy or recurrent implantation failure. Hum. Reprod. 2019, 34, 2340–2348. [Google Scholar] [CrossRef] [PubMed]
- Murugappan, G.; Ohno, M.S.; Lathi, R.B. Cost-effectiveness analysis of preimplantation genetic screening and in vitro fertilization versus expectant management in patients with unexplained recurrent pregnancy loss. Fertil. Steril. 2015, 103, 1215–1220. [Google Scholar] [CrossRef] [PubMed]
- Katz-Jaffe, M.G.; Surrey, E.S.; Minjarez, D.A.; Gustofson, R.L.; Stevens, J.M.; Schoolcraft, W.B. Association of abnormal ovarian reserve parameters with a higher incidence of aneuploidy blastocysts. Obstet. Gynecol. 2013, 121, 71–77. [Google Scholar] [CrossRef]
- Trout, S.W.; Seifer, D.B. Do women with unexplained recurrent pregnancy loss have higher day 3 serum FSH and estradiol values? Fertil. Steril. 2000, 74, 335–337. [Google Scholar] [CrossRef]
- Shahine, L.K.; Marshall, L.; Lamb, J.D.; Hickok, L.R. Higher rates of aneuploidy in blastocysts and higher risk of no embryo transfer in recurrent pregnancy loss patients with diminished ovarian reserve undergoing in vitro fertilization. Fertil. Steril. 2016, 106, 1124–1128. [Google Scholar] [CrossRef]
- Harton, G.; Braude, P.; Lashwood, A.; Schmutzler, A.; Traeger-Synodinos, J.; Wilton, L.; Harper, J.C. ESHRE PGD consortium best practice guidelines for organization of a PGD centre for PGD/preimplantation genetic screening. European Society for Human Reproduction and Embryology (ESHRE) PGD Consortium. Hum. Reprod. 2011, 26, 14–24. [Google Scholar] [CrossRef]
- Somigliana, E.; Vigano, P.; Busnelli, A.; Paffoni, A.; Vegetti, W.; Vercellini, P. Repeated implantation failure at the crossroad between statistics, clinics and over-diagnosis. Reprod. Biomed. Online 2018, 36, 32–38. [Google Scholar] [CrossRef]
- Coughlan, C.; Ledger, W.; Wang, Q.; Liu, F.; Demirol, A.; Gurgan, T.; Cutting, R.; Ong, K.; Sallam, H.; Li, T.C. Recurrent implantation failure: Definition and management. Reprod. BioMed. Online 2014, 28, 14–38. [Google Scholar] [CrossRef]
- Rubio, C.; Pehlivan, T.; Rodrigo, L.; Simón, C.; Remohí, J.; Pellicer, A. Embryo aneuploidy screening for unexplained recurrent miscarriage: A minireview. Am. J. Reprod. Immunol. 2005, 53, 159–165. [Google Scholar] [CrossRef]
- Pehlivan, T.; Rubio, C.; Rodrigo, L.; Romero, J.; Remohi, J.; Simón, C.; Pellicer, A. Impact of preimplantation genetic diagnosis on IVF outcome in implantation failure patients. Reprod. Biomed. Online 2003, 6, 232–237. [Google Scholar] [CrossRef]
- Simón, C.; Mercader, A.; Garcia-Velasco, J.; Nikas, G.; Moreno, C.; Remohí, J.; Pellicer, A. Coculture of human embryos with autologous human endometrial epithelial cells in patients with implantation failure. J. Clin. Endocrinol. Metab. 1999, 84, 2638–2646. [Google Scholar] [CrossRef]
- Gianaroli, L.; Magli, M.C.; Ferraretti, A.P.; Tabanelli, C.; Trombetta, C.; Boudjema, E. The role of preimplantation diagnosis for aneuploidies. Reprod. Biomed. Online 2002, 4, 31–33. [Google Scholar] [CrossRef]
- Gianaroli, L.; Magli, M.C.; Ferraretti, A.P.; Munne, S. Preimplantation diagnosis for aneuploidies in patients undergoing in vitro fertilization with a poor prognosis: Identification of the categories for which it should be proposed. Fertil. Steril. 1999, 72, 837–844. [Google Scholar] [CrossRef]
- Kahraman, S.; Sahin, Y.; Yelke, H.; Kumtepe, Y.; Tufekci, M.A.; Yapan, C.C.; Yesil, M.; Cetinkaya, M. High rates ofaneuploidy, mosaicism and abnormal morphokinetic development in cases with low sperm concentration. J. Assist. Reprod. Genet. 2020, 37, 629–664. [Google Scholar] [CrossRef]
- Voullaire, L.; Wilton, L.; McBain, J.; Callaghan, T.; Williamson, R. Chromosome abnormalities identified by comparative genomic hybridization in embryos from women with repeated implantation failure. Mol. Hum. Reprod. 2002, 8, 1035–1041. [Google Scholar] [CrossRef]
- ESHRE PGD Consortium Steering Committee. ESHRE Preimplantation Genetic Diagnosis Consortium: Data collection III (May 2001). Hum. Reprod. 2002, 17, 233–246. [Google Scholar] [CrossRef]
- Greco, E.; Bono, S.; Ruberti, A.; Lobascio, A.M.; Greco, P.; Biricik, A.; Spizzichino, L.; Greco, A.; Tesarik, J.; Minasi, M.G.; et al. Comparative Genomic Hybridization Selection of Blastocysts for Repeated Implantation Failure Treatment: A Pilot Study. Biomed. Res. Int. 2014, 457913. [Google Scholar] [CrossRef]
- Petousis, S.; Prapas, Y.; Papatheodorou, A.; Margioula-Siarkou, C.; Papatzikas, G.; Panagiotidis, Y.; Karkanaki, A.; Ravanos, K.; Prapas, N. Fluorescence in situ hybridization sperm examination is significantly impaired in all categories of male infertility. Andrologia 2018, 50, 12847. [Google Scholar] [CrossRef]
- Magli, M.C.; Gianaroli, L.; Ferraretti, A.P.; Gordts, S.; Fredericks, V.; Crippa, A. Paternal contribution to aneuploidy in preimplantation embryos. Reprod. Biomed. Online 2009, 18, 536–542. [Google Scholar] [CrossRef]
- Silber, S.; Escudero, T.; Lenahan, K.; Abdelhadi, I.; Kilani, Z.; Munne, S. Chromosomal abnormalities in embryos derived from testicular sperm extraction. Fertil. Steril. 2003, 79, 30–38. [Google Scholar] [CrossRef]
- Coates, A.; Hesla, J.S.; Hurliman, A.; Coate, B.; Holmes, E.; Matthews, R.; Mounts, E.L.; Turner, K.J.; Thornhill, A.R.; Griffin, D.K. Use of suboptimal sperm increases the risk of aneuploidy of the sex chromosomes in preimplantation blastocyst embryos. Fertil. Steril. 2015, 104, 866–872. [Google Scholar] [CrossRef]
- Mazzilli, R.; Cimadomo, D.; Vaiarelli, A.; Capalbo, A.; Dovere, L.; Alviggi, E.; Dusi, L.; Foresta, C.; Lombardo, F.; Lenzi, A.; et al. Effect of themalefactor on the clinical outcome of intracytoplasmic sperm injection combined with preimplantation aneuploidy testing: Observational longitudinal cohort study of 1,219 consecutive cycles. Fertil. Steril. 2017, 108, 961–972. [Google Scholar] [CrossRef]
- Liebaers, I.; Desmyttere, S.; Verpoest, W.; de Rycke, M.; Staessen, C.; Sermon, K.; Devroey, P.; Haentjens, P.; Bonduelle, M. Report on a consecutive series of 581 children born after blastomere biopsy for preimplantation genetic diagnosis. Hum. Reprod. 2010, 25, 275–282. [Google Scholar] [CrossRef]
- Levi-Setti, P.E.; Moioli, M.; Smeraldi, A.; Cesaratto, E.; Menduni, F.; Livio, S.; Morenghi, M.; Patrizio, P. Obstetric outcome and incidence of congenital anomalies in 2351 IVF/ICSI babies. J. Assist. Reprod. Genet. 2016, 33, 711–717. [Google Scholar] [CrossRef]
- Hobbs, C.A.; Cleves, M.A.; Simmons, C.J. Genetic epidemiology and congenital malformations: From the chromosome to the crib. Arch. Pediatr. Adolesc. Med. 2002, 156, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Matthews, T.J.; MacDorman, M.F.; Thoma, M.E. Infant mortality statistics from the 2013 period linked birth/infant death data set. Natl. Vital. Stat. Rep. 2015, 64, 1–30. [Google Scholar]
- Ahmadi, A.; Ng, S.C. Fertilizing ability of DNA-damaged spermatozoa. J. Exp. Zool. 1999, 284, 696–704. [Google Scholar] [CrossRef]
- Loutradi, K.E.; Tarlatzis, B.C.; Goulis, D.G.; Zepiridis, L.; Pagou, T.; Chatziioannou, E.; Grimbizis, G.F.; Papadimas, I.; Bontis, I. The effects of sperm quality on embryo development after intracytoplasmic sperm injection. J. Assist. Reprod. Genet. 2006, 23, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Tarozzi, N.; Nadalini, M.; Lagalla, C.; Coticchio, G.; Zacà, C.; Borini, A. Male factor in fertility impacts the rate of mosaic blastocysts in cycles of preimplantation genetic testing for aneuploidy. J. Assist. Reprod. Genet. 2019, 36, 2047–2055. [Google Scholar] [CrossRef]
- Scarselli, F.; Cursio, E.; Muzzì, S.; Casciani, V.; Ruberti, A.; Gatti, S.; Greco, P.; Varricchio, M.T.; Minasi, M.G.; Greco, E. How 1h of abstinence improves sperm quality and increases embryo euploidy rate after PGT-A: A study on 106 sibling biopsied blastocysts. J. Assist. Reprod. Genet. 2019, 36, 1591–1597. [Google Scholar] [CrossRef]
- Fullerton, G.; Hamilton, M.; Maheshwari, A. Should non-mosaic Klinefelter syndrome men be labelled as infertile in 2009? Hum. Reprod. 2010, 25, 588–597. [Google Scholar] [CrossRef]
- Ron-El, R.; Strassburger, D.; Gelman-Kohan, S.; Friedler, S.; Raziel, A.; Appelman, Z. A 47,XXY fetus conceived after ICSI of spermatozoa from a patient with non-mosaic Klinefelter’s syndrome: Case report. Hum. Reprod. 2000, 15, 1804–1806. [Google Scholar] [CrossRef]
- Friedler, S.; Raziel, A.; Strassburger, D.; Schachter, M.; Bern, O.; Ron-El, R. Outcome of ICSI using fresh and cryopreserved-thawed testicular spermatozoa in patients with non-mosaic Klinefelter’s syndrome. Hum. Reprod. 2001, 16, 2616–2620. [Google Scholar] [CrossRef]
- Greco, E.; Scarselli, F.; Minasi, M.G.; Casciani, V.; Zavaglia, D.; Dente, D.; Tesarik, J.; Franco, G. Birth of 16 healthy children after ICSI in cases of non-mosaic Klinefelter syndrome. Hum. Reprod. 2013, 28, 1155–1160. [Google Scholar] [CrossRef]
- Staessen, C.; Tournaye, H.; Van Assche, E.; Michiels, A.; Van Landuyt, L.; Devroey, P.; Liebaers, I.; Van Steirteghem, A. PGD in 47,XXY Klinefelter’syndrome patients. Hum. Reprod. Update 2003, 9, 319–330. [Google Scholar] [CrossRef]
- García-Ferreyra, J.; Luna, D.; Villegas, L.; Romero, R.; Zavala, P.; Hilario, R.; Dueñas-Chacón, J. High aneuploidy rates observed in embryos derived from donated oocytes are related to male aging and high percentages of sperm DNA fragmentation. Clin. Med. Insights Reprod. Health 2015, 9, 21–27. [Google Scholar] [CrossRef]
- García-Ferreyra, J.; Hilario, R.; Dueñas, J. High percentages of embryos with 21, 18 or 13 trisomy are related to advanced paternal age in donor egg cycles. JBRA Assist. Reprod. 2018, 22, 26–34. [Google Scholar] [CrossRef]
- El-Domyati, M.M.; Al-Din, A.B.; Barakat, M.T.; El-Fakahany, H.M.; Xu, J.; Sakkas, D. Deoxyribonucleic acid repair and apoptosis in testicular germ cells of aging fertile men: The role of the poly [adenosine diphosphate-ribosyl] ation pathway. Fertil. Steril. 2009, 1, 2221–2229. [Google Scholar] [CrossRef]
- Gat, I.; Tang, K.; Quach, K.; Kuznyetsov, V.; Antes, R.; Filice, M.; Zohni, K.; Librach, C. Sperm DNA fragmentation index does not correlate with blastocyst aneuploidy or morphological grading. PLoS ONE 2017, 12, e0179002. [Google Scholar] [CrossRef] [PubMed]
- Bronet, F.; Martinez, E.; Gaytan, M.; Linan, A.; Cernuda, D.; Ariza, M.; Nogales, M.; Pacheco, A.; San Celestino, M.; Garcia-Velasco, J.A. Sperm DNA fragmentation index does not correlate with the sperm or embryo aneuploidy rate in recurrent miscarriage or implantation failure patients. Hum. Reprod. 2012, 27, 1922–1929. [Google Scholar] [CrossRef] [PubMed]
- Stacy, C.; Deepak, M. Y Genetics of the human Y chromosomeand its association with male infertility. Reprod. Biol. Endocrinol. 2018, 16, 14. [Google Scholar]
- Capalbo, A.; Rienzi, L.; Cimadomo, D.; Maggiulli, R.; Elliott, T.; Wright, G.; Nagy, Z.P.; Ubaldi, F.M. Correlation between standard blastocyst morphology, euploidy and implantation: An observational study in two centers involving 956 screened blastocysts. Hum. Reprod. 2014, 29, 1173–1181. [Google Scholar] [CrossRef]
- Ozgur, K.; Berkkanoglu, M.; Bulut, H.; Yoruk, G.D.A.; Candurmaz, N.N.; Coetzee, K. Single best euploid versus single best unknown-ploidy blastocyst frozen embryo transfers: A randomized controlled trial. J. Assist. Reprod. Genet. 2019, 36, 629–636. [Google Scholar] [CrossRef]
- Munné, S.; Kaplan, B.; Frattarelli, J.L.; Child, T.; Nakhuda, G.; Shamma, F.N.; Silverberg, K.; Kalista, T.; Handyside, A.H.; Katz-Jaffe, M.; et al. Preimplantation genetic testing for aneuploidy versus morphology as selection criteria for single frozen-thawed embryo transfer in good-prognosis patients: A multicenter randomized clinical trial. Fertil. Steril. 2019, 112, 1071–1079. [Google Scholar] [CrossRef] [PubMed]
- Forman, E.J.; Hong, K.H.; Ferry, K.M.; Tao, X.; Taylor, D.; Levy, B.; Treff, N.R.; Scott, R.T., Jr. In vitro fertilization with single euploid blastocyst transfer: A randomized controlled trial. Fertil. Steril. 2013, 100, 100–107. [Google Scholar] [CrossRef]
- Nakasuji, T.; Saito, H.; Araki, R.; Nakaza, A.; Nakashima, A.; Kuwahara, A.; Ishihara, O.; Irahara, M.; Kubota, T.; Yoshimura, Y.; et al. The incidence of monozygotic twinning in assisted reproductive technology: Analysis based on results from the 2010 Japanese ART national registry. J. Assist. Reprod. Genet. 2014, 31, 803–807. [Google Scholar] [CrossRef][Green Version]
- Da Costa, A.L.A.L.; Abdelmassih, S.; de Oliveira, F.G.; Abdelmassih, V.; Abdelmassih, R.; Nagy, Z.P.; Balmaceda, J.P. Monozygotic twins and transfer at the blastocyst stage after ICSI. Hum. Reprod. 2001, 16, 333–336. [Google Scholar] [CrossRef]
- Vaughan, D.A.; Ruthazer, R.; Penzias, A.S.; Norwitz, E.R.; Sakkas, D. Clustering of monozygotic twinning in IVF. J. Assist. Reprod. Genet. 2016, 33, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Ikemoto, Y.; Kuroda, K.; Ochiai, A.; Yamashita, S.; Ikuma, S.; Nojiri, S.; Itakura, A.; Takeda, S. Prevalence and risk factors of zygotic splitting after 937,848 single embryo transfer cycles. Hum. Reprod. 2018, 33, 1984–1991. [Google Scholar] [CrossRef] [PubMed]
- Verpoest, W.; Van Landuyt, L.; Desmyttere, S.; Cremers, A.; Devroey, P.; Liebaers, I. The incidence of monozygotic twinning following PGD is not increased. Hum. Reprod. 2009, 24, 2945–2950. [Google Scholar] [CrossRef]
- Busnelli, A.; Dallagiovanna, C.; Reschini, M.; Paffoni, A.; Fedele, L.; Somigliana, E. Risk factors for monozygotic twinning after in vitro fertilization: A systematic review and meta-analysis. Fertil. Steril. 2019, 111, 302–317. [Google Scholar] [CrossRef] [PubMed]
- Kamath, M.S.; Antonisamy, B.; Sunkara, S.K. Zygotic splitting following embryo biopsy: A cohort study of 207697 single-embryo transfers following IVF treatment. BJOG 2020, 127, 562–569. [Google Scholar] [CrossRef]
- Masbou, A.K.; Friedenthal, J.B.; McCulloh, D.H.; McCaffrey, C.; Fino, M.E.; Grifo, J.A.; Licciardi, F. A Comparison of Pregnancy Outcomes in Patients Undergoing Donor Egg Single Embryo Transfers with and Without Preimplantation Genetic Testing. Reprod. Sci. 2019, 26, 1661–1665. [Google Scholar] [CrossRef]
- Sills, E.; Li, X.; Frederick, J.L.; Khoury, C.D.; Potter, D.A. Determining parental origin of embryo aneuploidy: Analysis of genetic error observed in 305 embryos derived from anonymous donor oocyte IVF cycles. Mol. Cytogenet. 2014, 7, 68. [Google Scholar] [CrossRef]
- Hoyos, L.R.; Cheng, C.Y.; Brennan, K.; Hubert, G.; Wang, B.; Buyalos, R.P.; Quinn, M.; Shamonki, M.J. Euploid rates amongoocytedonors: Is there an optimal age fordonation? Assist. Reprod. Genet. 2020, 37, 589–594. [Google Scholar] [CrossRef]
- Haddad, G.; Deng, M.; Wang, C.T.; Witz, C.; Williams, D.; Griffith, J.; Skorupski, J.; Gill, J.; Wang, W.H. Assessment of aneuploidy formation in human blastocysts resulting from donated eggs and the necessity of the embryos for aneuploidy screening. J. Assist. Reprod. Genet. 2015, 32, 999–1006. [Google Scholar] [CrossRef]
- Forman, E.J.; Li, X.; Ferry, K.M.; Scott, K.; Treff, N.R.; Scott, R.T., Jr. Oocyte vitrification does not increase the risk of embryonic aneuploidyor diminish the implantation potential of blastocysts created after intracytoplasmic sperm injection: A novel, paired randomized controlled trial using DNA fingerprinting. Fertil. Steril. 2012, 98, 644–649. [Google Scholar] [CrossRef]
- Obradors, A.; Fernández, E.; Oliver-Bonet, M.; Rius, M.; de la Fuente, A.; Wells, D.; Benet, J.; Navarro, J. Birth of a healthy boy after a double factor PGD in a couple carrying a genetic disease and at risk for aneuploidy: Case report. Hum. Reprod. 2008, 23, 1949–1956. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Obradors, A.; Fernández, E.; Rius, M.; Oliver-Bonet, M.; Martínez-Fresno, M.; Benet, J.; Navarro, J. Outcome of twin babies free of Von Hippel-Lindau disease after a double-factor preimplantation genetic diagnosis: Monogenetic mutation analysis and comprehensive aneuploidy screening. Fertil. Steril. 2009, 91, 933.e1–933.e7. [Google Scholar] [CrossRef]
- Rechitsky, S.; Verlinsky, O.; Kuliev, A. PGD for cystic fibrosis patients and couples at risk of an additional genetic disorder combined with 24-chromosome aneuploidy testing. Reprod. Biomed. Online 2013, 26, 420–430. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Goldman, K.N.; Nazem, T.; Berkeley, A.; Palter, S.; Grifo, J.A. Preimplantation Genetic Diagnosis (PGD) for Monogenic Disorders: The Value of Concurrent Aneuploidy Screening. J. Genet. Couns. 2016, 25, 1327–1337. [Google Scholar] [CrossRef] [PubMed]
- Spinella, F.; Fiorentino, F.; Biricik, A.; Bono, S.; Ruberti, A.; Cotroneo, E.; Baldi, M.; Cursio, E.; Minasi, M.G.; Greco, E. Extent of chromosomal mosaicism influences the clinical outcome of in vitro fertilization treatments. Fertil. Steril. 2018, 109, 77–83. [Google Scholar] [CrossRef]
- Delhanty, J.D.; Griffin, D.K.; Handyside, A.H.; Harper, J.; Atkinson, G.H.; Pieters, M.H.; Winston, R.M. Detection of aneuploidy and chromosomal mosaicism in human embryos during preimplantation sex determination by fluorescent in situ hybridisation, (FISH). Hum. Mol. Genet. 1993, 2, 1183–1185. [Google Scholar] [CrossRef] [PubMed]
- Fragouli, E.; Alfarawati, S.; Spath, K.; Babariya, D.; Tarozzi, N.; Borini, A.; Wells, D. Analysis of implantation and ongoing pregnancy rates following the transfer of mosaic diploid-aneuploid blastocysts. Hum. Genet. 2017, 136, 805–819. [Google Scholar] [CrossRef]
- Daphnis, D.D.; Delhanty, J.D.; Jerkovic, S.; Geyer, J.; Craft, I.; Harper, J.C. Detailed FISH analysis of day 5 human embryos reveals the mechanisms leading to mosaic aneuploidy. Hum. Reprod. 2005, 20, 129–137. [Google Scholar] [CrossRef]
- Mantikou, E.; Wong, K.M.; Repping, S.; Mastenbroek, S. Molecular origin of mitotic aneuploidies in preimplantation embryos. Biochim. Biophys. Acta 2012, 1822, 1921–1930. [Google Scholar] [CrossRef]
- Fragouli, E.; Alfarawati, S.; Daphnis, D.D.; Goodall, N.N.; Mania, A.; Griffiths, T.; Gordon, A.; Wells, D. Cytogenetic analysis of human blastocysts with the use of FISH, CGH and aCGH: Scientific data and technical evaluation. Hum. Reprod. 2011, 26, 480–490. [Google Scholar] [CrossRef]
- Bielanska, M.; Tan, S.L.; Ao, A. Chromosomal mosaicism throughout human preimplantation development in vitro: Incidence, type, and relevance to embryo outcome. Hum. Reprod. 2002, 17, 413–419. [Google Scholar] [CrossRef]
- Munné, S.; Grifo, J.; Wells, D. Mosaicism: “survival of the fittest” versus “no embryo left behind”. Fertil. Steril. 2016, 105, 1146–1149. [Google Scholar] [CrossRef]
- Capalbo, A.; Rienzi, L. Mosaicism between trophectoderm and inner cell mass. Fertil. Steril. 2017, 107, 1098–1106. [Google Scholar] [CrossRef]
- Munné, S.; Spinella, F.; Grifo, J.; Zhang, J.; Beltran, M.P.; Fragouli, E.; Fiorentino, F. Clinical outcomes after the transfer of blastocysts characterized as mosaic by high resolution Next Generation Sequencing- further insights. Eur. J. Med. Genet. 2020, 63, 103741. [Google Scholar] [CrossRef]
- Greco, E.; Minasi, M.G.; Fiorentino, F. Healthy babies born after intrauterine transfer of mosaic aneuploid blastocyst. N. Engl. J. Med. 2015, 373, 2089–2090. [Google Scholar] [CrossRef]
- Munné, S.; Blazek, J.; Large, M.; Martinez-Ortiz, P.A.; Nisson, H.; Liu, E.; Tarozzi, N.; Borini, A.; Becker, A.; Zhang, J.; et al. Detailed investigation into the cytogenetic constitution and pregnancy outcome of replacing mosaic blastocysts detected with the use of high-resolution next-generation sequencing. Fertil. Steril. 2017, 108, 62–71. [Google Scholar] [CrossRef]
- Victor, A.R.; Tyndall, J.C.; Brake, A.J.; Lepkowsky, L.T.; Murphy, A.E.; Griffin, D.K.; McCoy, R.C.; Barnes, F.L.; Zouves, C.G.; Viotti, M. One hundred mosaic embryos transferred prospectively in a single clinic: Exploring when and why they result in healthy pregnancies. Fertil. Steril. 2019, 111, 280–293. [Google Scholar] [CrossRef]
- Viotti, M. Mosaic embryos. A comprehensive and powered analysis of clinical outcomes. Fertil. Steril. 2019, 112, e33. [Google Scholar] [CrossRef]
- Kahraman, S.; Cetinkaya, M.; Yuksel, B.; Yesil, M.; Cetinkaya, C.P. The birth of a baby with mosaicism resulting from a known mosaic embryo transfer: A case report. Hum. Reprod. 2020, 35, 727–733. [Google Scholar] [CrossRef]
- Cram, D.S.; Leigh, D.; Handyside, A.; Rechitsky, L.; Xu, K.; Harton, G.; Grifo, J.; Rubio, C.; Fragouli, E.; Kahraman, S.; et al. PGDIS Position Statement on the Transfer of Mosaic Embryos 2019. Reprod. Biomed. Online 2019, 39 (Suppl. 1), e1. [Google Scholar] [CrossRef]
- CoGEN 2017. COGEN Position Statement on Chromosomal Mosaicism Detected in Preimplantation Blastocyst Biopsies. Available online: https://www.ivfworldwide.com (accessed on 20 April 2018).
- Ledbetter, D.H.; Zachary, J.M.; Simpson, J.L.; Golbus, M.S.; Pergament, E.; Jackson, L.; Mahoney, M.J.; Desnick, R.J.; Schulman, J.; Copeland, K.L. Cytogenetic results from the U.S. Collaborative Study on CVS. Prenat. Diagn. 1992, 12, 317–345. [Google Scholar] [CrossRef]
- Santos, M.A.; Teklenburg, G.; Macklon, N.S.; Van Opstal, D.; Schuring-Blom, G.H.; Krijtenburg, P.J.; de Vreeden-Elbertse, J.; Fauser, B.C.; Baart, E.B. The fate of the mosaic embryo: Chromosomal constitution and development of Day 4, 5 and 8 human embryos. Hum. Reprod. 2010, 25, 1916–1926. [Google Scholar] [CrossRef]
- Popovic, M.; Dhaenens, L.; Taelman, J.; Dheedene, A.; Bialecka, M.; De Sutter, P.; Chuva de Sousa Lopes, S.M.; Menten, B.; Heindryckx, B. Extended in vitro culture of human embryos demonstrates the complex nature of diagnosing chromosomal mosaicism from a single trophectoderm biopsy. Hum. Reprod. 2019, 34, 758–769. [Google Scholar] [CrossRef]
- Shapiro, B.S.; Daneshmand, S.T.; Garner, F.C.; Aguirre, M.; Hudson, C. Clinical rationale for cryopreservation of entire embryo cohorts in lieu of fresh transfer. Fertil. Steril. 2014, 102, 3–9. [Google Scholar] [CrossRef]
- Zhang, S.; Luo, K.; Cheng, D.; Tan, Y.; Lu, C.; He, H.; Gu, Y.; Lu, G.; Gong, F.; Lin, G. Number of biopsied trophectoderm cells is likely to affect the implantation potential of blasto- cysts with poor trophectoderm quality. Fertil. Steril. 2016, 105, 1222–1227. [Google Scholar] [CrossRef]
- Farhi, J.; Ben-Haroush, A.; Andrawus, N.; Pinkas, H.; Sapir, O.; Fisch, B.; Ashkenazi, J. High serum oestradiol concentrations in IVF cycles increase the risk of pregnancy complications related to abnormal placentation. Reprod. Biomed. Online 2010, 21, 331–337. [Google Scholar] [CrossRef]
- Healy, D.L.; Breheny, S.; Halliday, J.; Jaques, A.; Rushford, D.; Garrett, C.; Talbot, J.M.; Baker, H.W.B. Prevalence and risk factors for obstetric haemorrhage in 6730 singleton births after assisted reproductive technology in Victoria Australia. Hum. Reprod. 2010, 25, 265–274. [Google Scholar] [CrossRef]
- Coates, A.; Kung, A.; Mounts, E.; Hesla, J.; Bankowski, B.; Barbieri, E.; Ata, B.; Cohen, J.; Munné, S. Optimal euploidembryo transfer strategy, fresh versus frozen, after preimplantation genetic screening with next generation sequencing: A randomized controlled trial. Fertil. Steril. 2017, 107, 723–730. [Google Scholar] [CrossRef]
- Greco, E.; Litwicka, K.; Arrivi, C.; Varricchio, M.T.; Caragia, A.; Greco, A.; Minasi, M.G.; Fiorentino, F. The endometrial preparation for frozen-thawed euploid blastocyst transfer: A prospective randomized trial comparing clinical results from natural modified cycle and exogenous hormone stimulation with GnRH agonist. J. Assist. Reprod. Genet. 2016, 33, 873–884. [Google Scholar] [CrossRef]
- Wang, A.; Murugappan, G.; Kort, J.; Westphal, L. Hormone replacement versus natural frozen embryo transfer for euploid embryos. Arch. Gynecol. Obstet. 2019, 300, 1053–1060. [Google Scholar] [CrossRef]
- Sekhon, L.; Feuerstein, J.; Pan, S.; Overbey, J.; Lee, J.A.; Briton-Jones, C.; Flisser, E.; Stein, D.E.; Mukherjee, T.; Grunfeld, L.; et al. Endometrial Preparation Before the Transfer of Single, Vitrified-Warmed, Euploid Blastocysts: Does the Duration of Estradiol Treatment Influence Clinical Outcome? Fertil. Steril. 2019, 111, 1177–1185. [Google Scholar] [CrossRef] [PubMed]
- Gaggiotti-Marre, S.; Martinez, F.; Coll, L.; Garcia, S.; Álvarez, M.; Parriego, M.; Barri, P.N.; Polyzos, N.; Coroleu, B. Low serum progesterone the day prior to frozen embryo transfer of euploid embryos is associated with significant reduction in live birth rates. Gynecol. Endocrinol. 2019, 35, 439–442. [Google Scholar] [CrossRef] [PubMed]
- Boynukalin, F.K.; Gultomruk, M.; Turgut, E.; Demir, B.; Findikli, N.; Serdarogullari, M.; Coban, O.; Yarkiner, Z.; Bahceci, M. Measuring the serum progesterone level on the day of transfercan be an additional tool to maximize ongoing pregnancies in single euploid frozen blastocyst transfers. Reprod. Biol. Endocrinol. 2019, 17, 102. [Google Scholar] [CrossRef]
- Scott, R.J.; Upham, K.M.; Forman, E.J.; Zhao, T.; Treff, N.R. Cleavage-stage biopsy significantly impairs human embryonic implantation potential while blasto cyst biopsy does not: A randomized and paired clinical trial. Fertil. Steril. 2013, 100, 624–630. [Google Scholar] [CrossRef]
- Dokras, A.; Sargent, I.L.; Gardner, R.L.; Barlow, D.H. Human trophectoderm biopsy and secretion of chorionic gonadotrophin. Hum. Reprod. 1991, 6, 1453–1459. [Google Scholar] [CrossRef]
- Zhang, W.Y.; von Versen-Höynck, F.; Kapphahn, K.I.; Fleischmann, R.R.; Zhao, Q.; Baker, V.L. Maternal and neonatal outcomes associated with trophectoderm biopsy. Fertil. Steril. 2019, 112, 283–290. [Google Scholar] [CrossRef]
- He, H.; Jing, S.; Lu, C.F.; Tan, Y.Q.; Luo, K.L.; Zhang, S.P.; Gong, F.; Lu, G.X.; Lin, G. Neonatal outcomes of live births after blastocyst biopsy in preimplantation genetic testing cycles: A follow-up of 1721 children. Fertil. Steril. 2019, 112, 82–88. [Google Scholar] [CrossRef]
- Jing, S.; Luo, K.; He, H.; Lu, C.; Zhang, S.; Tan, Y.; Gong, F.; Lu, G.; Lin, G. Obstetric and neonatal outcomes in blastocyst-stage biopsy with frozen embryo transfer and cleavage-stage biopsy with fresh embryo transfer after preimplantation genetic diagnosis/screening. Fertil. Steril. 2016, 106, 105–112. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Greco, E.; Litwicka, K.; Minasi, M.G.; Cursio, E.; Greco, P.F.; Barillari, P. Preimplantation Genetic Testing: Where We Are Today. Int. J. Mol. Sci. 2020, 21, 4381. https://doi.org/10.3390/ijms21124381
Greco E, Litwicka K, Minasi MG, Cursio E, Greco PF, Barillari P. Preimplantation Genetic Testing: Where We Are Today. International Journal of Molecular Sciences. 2020; 21(12):4381. https://doi.org/10.3390/ijms21124381
Chicago/Turabian StyleGreco, Ermanno, Katarzyna Litwicka, Maria Giulia Minasi, Elisabetta Cursio, Pier Francesco Greco, and Paolo Barillari. 2020. "Preimplantation Genetic Testing: Where We Are Today" International Journal of Molecular Sciences 21, no. 12: 4381. https://doi.org/10.3390/ijms21124381
APA StyleGreco, E., Litwicka, K., Minasi, M. G., Cursio, E., Greco, P. F., & Barillari, P. (2020). Preimplantation Genetic Testing: Where We Are Today. International Journal of Molecular Sciences, 21(12), 4381. https://doi.org/10.3390/ijms21124381






