Molecular Signature of Prospero Homeobox 1 (PROX1) in Follicular Thyroid Carcinoma Cells
Abstract
1. Introduction
2. Results
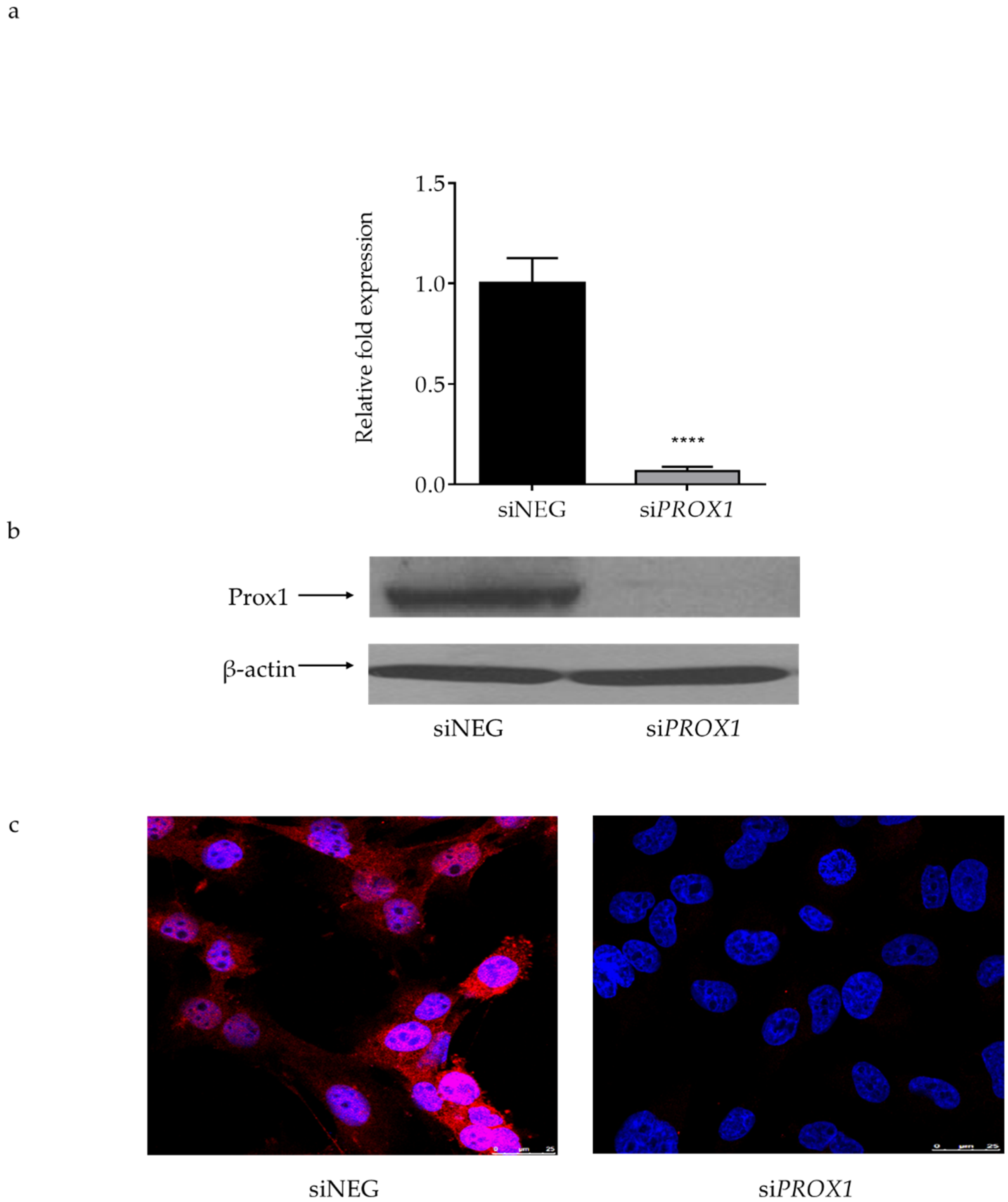
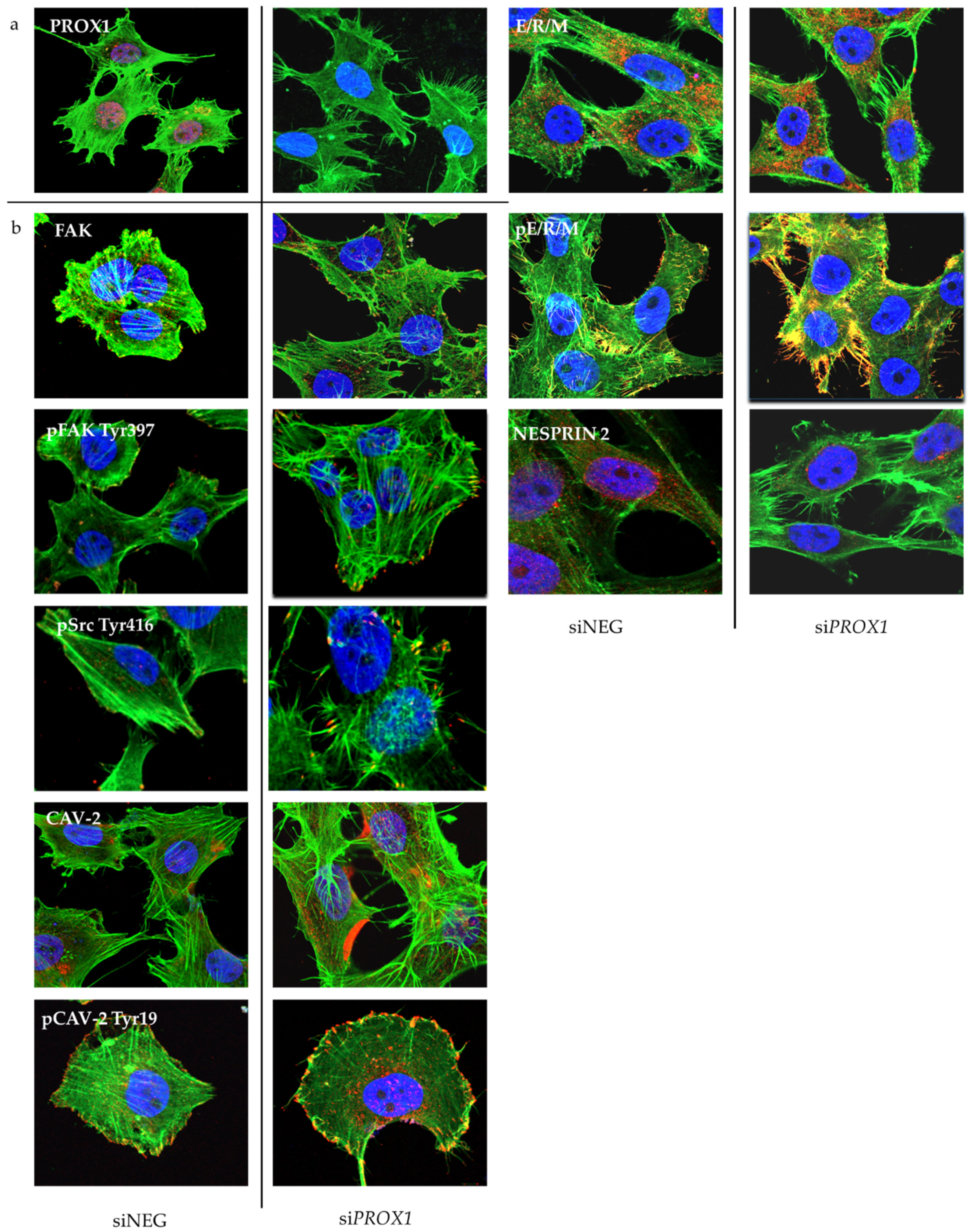
2.1. PROX1 Knock-Down CGTH-W-1 Cells and Its Effect on Cell Motility and Invasive Potential
2.2. Effect of PROX1 on Cell Viability, Cell Cycle and Apoptosis
2.3. PROX1 Expression Deficiency and Changes in Gene Expression Profiles
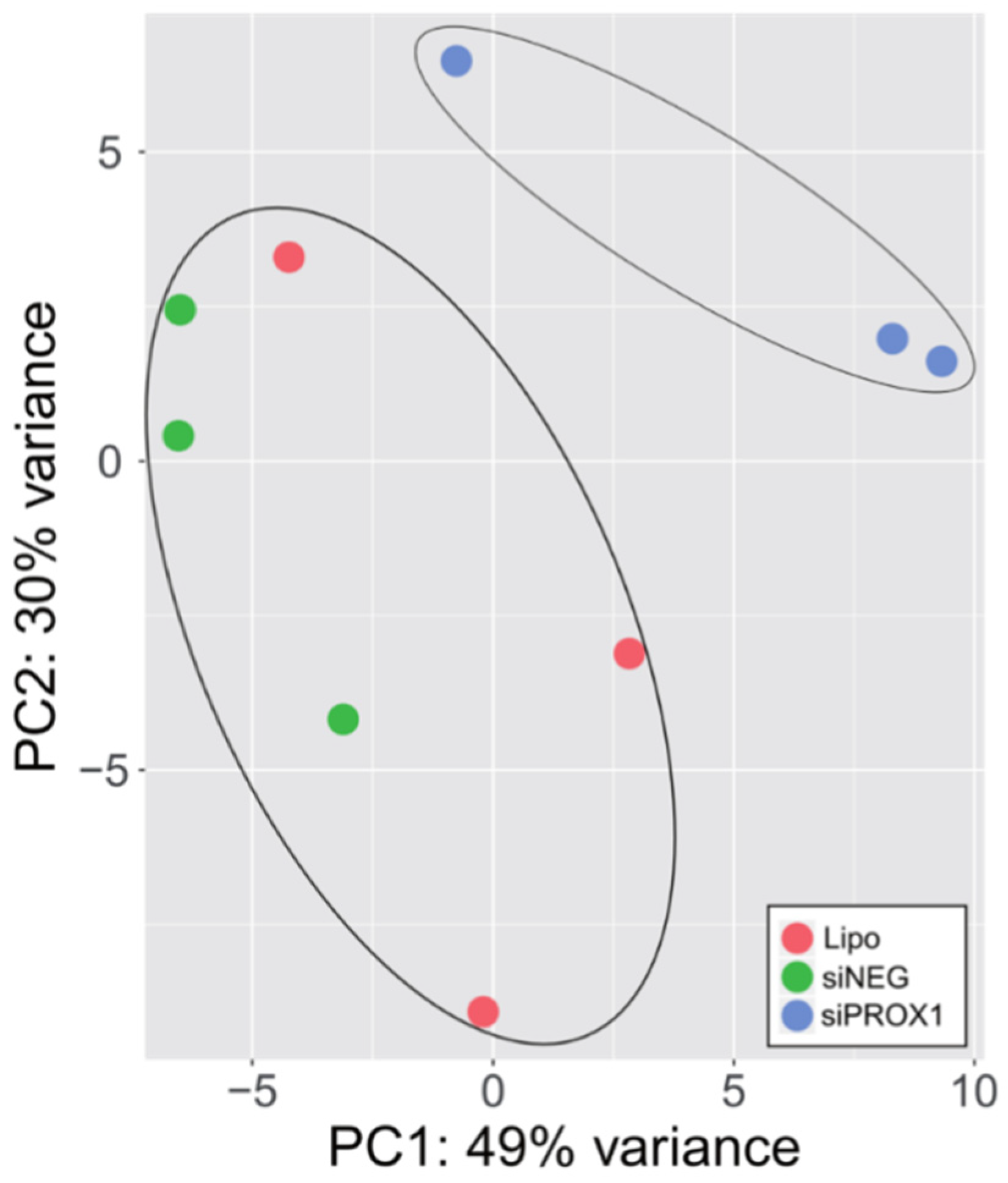
2.3.1. RNA-seq Analysis
2.3.2. Gene Ontology Analysis
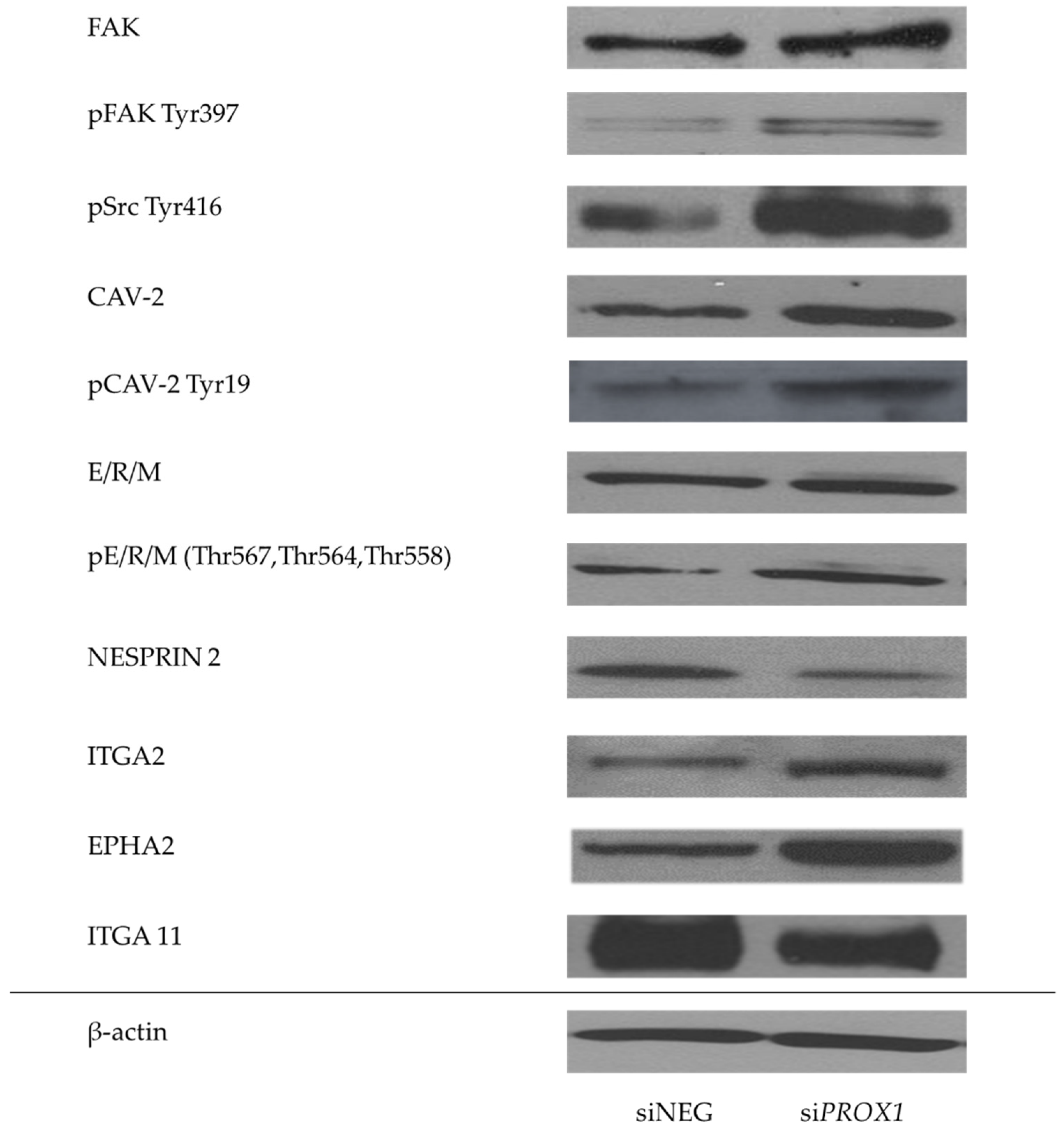
2.3.3. Validation of RNA-seq Data
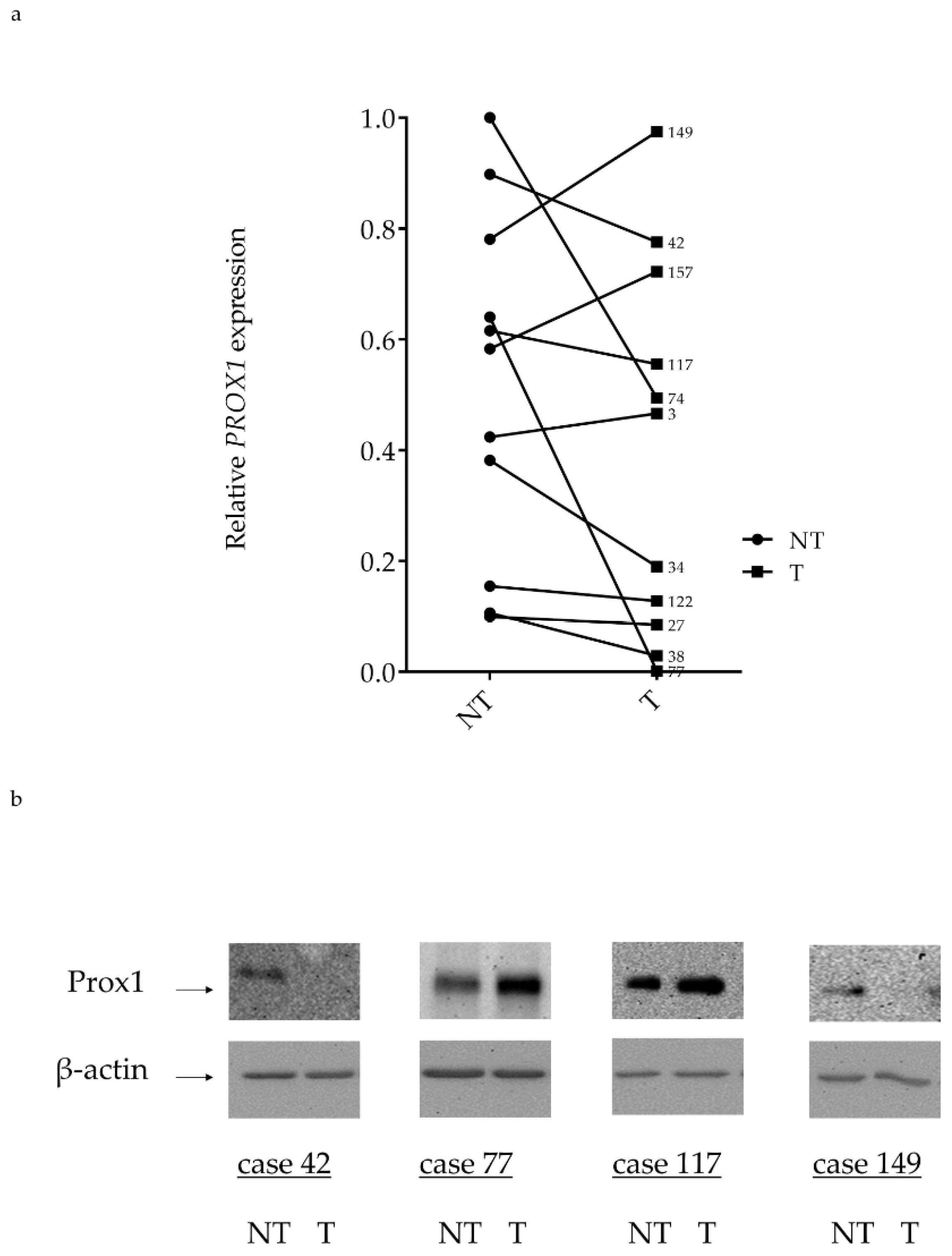
2.4. PROX1 Expression in Human FTC Tissues
3. Discussion
4. Materials and Methods
4.1. Thyroid Cell Line
4.2. Silencing PROX1 by Small Interfering RNA
4.3. RNA Extraction and cDNA Synthesis
4.4. Real-Time Quantitative PCR (RT-qPCR)
4.5. RNA-Seq Library Preparation and Sequencing
4.6. Western Blotting
4.7. Immunocytochemistry
4.8. Cell Migration and Matrigel Invasion Assays
4.9. In Vitro Wound Healing Motility Assay
4.10. Cell Viability Assay
4.11. Apoptosis and Cell Cycle Analysis
4.12. Tissue samples and Immunohistochemistry
4.13. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ACTB | beta-actin gene |
| AKT | protein kinase B |
| BSA | bovine serum albumin |
| CAV | caveolin |
| ChIP-seq | chromatin immunoprecipitation genome wide |
| DAPI | 4′,6-Diamidino-2-Phenylindole |
| DCLK1 | doublecortin like kinase 1 |
| DMEM | Dulbecco’s modified Eagle’s medium |
| EPHA2 | ephrin type-A receptor 2 |
| ERM | ezrin, radixin and moesin |
| FAK | focal adhesion kinase |
| FBS | foetal bovine serum |
| FITC | fluorescein isothiocyanate |
| FTC | follicular thyroid carcinoma |
| GO | gene ontology |
| H&E | haematoxylin and eosin |
| HRP | horseradish peroxidase |
| LEC | lymphatic endothelial cells |
| LYVE- | lymphatic vessel endothelial hyaluronan receptor 1 |
| PBS | phosphate buffered saline |
| PCA | principal component analysis |
| PEAK | pseudopodium enriched atypical kinase 1 |
| PIP5KIC | phosphatidylinositol-4-phosphate 5-kinase type 1 gamma |
| PROX1 | Prospero homeobox protein 1 |
| PTC | papillary thyroid carcinoma |
| qPCR | quantitative polymerase chain reaction |
| ROCK | the Rho associated coiled-coil containing protein kinase 1 |
| RT-PCR | real-time polymerase chain reaction |
| SD | standard deviation |
| SRC | Proto-oncogene tyrosine-protein kinase |
| SYNE | nesprin |
| VEGFR | vascular endothelial growth factor receptor |
References
- Bruyere, F.; Noel, A. Lymphangiogenesis: In vitro and in vivo models. FASEB J. 2010, 24, 8–21. [Google Scholar] [CrossRef]
- Tammela, T.; Petrova, T.V.; Alitalo, K. Molecular lymphangiogenesis: New players. Trends Cell Biol. 2005, 15, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Bolenz, C.; Fernandez, M.I.; Tilki, D.; Herrmann, E.; Heinzelbecker, J.; Ergun, S.; Strobel, P.; Reich, O.; Michel, M.S.; Trojan, L. The role of lymphangiogenesis in lymphatic tumour spread of urological cancers. BJU Int. 2009, 104, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Sundar, S.S.; Ganesan, T.S. Role of lymphangiogenesis in cancer. J. Clin. Oncol. 2007, 25, 4298–4307. [Google Scholar] [CrossRef] [PubMed]
- Banerji, S.; Ni, J.; Wang, S.X.; Clasper, S.; Su, J.; Tammi, R.; Jones, M.; Jackson, D.G. LYVE-1, a new homologue of the CD44 glycoprotein, is a lymph-specific receptor for hyaluronan. J. Cell Biol. 1999, 144, 789–801. [Google Scholar] [CrossRef] [PubMed]
- Breiteneder-Geleff, S.; Soleiman, A.; Horvat, R.; Amann, G.; Kowalski, H.; Kerjaschki, D. Podoplanin—A specific marker for lymphatic endothelium expressed in angiosarcoma. Verh. Dtsch. Ges. Pathol. 1999, 83, 270–275. [Google Scholar]
- Dudas, J.; Mansuroglu, T.; Moriconi, F.; Haller, F.; Wilting, J.; Lorf, T.; Fuzesi, L.; Ramadori, G. Altered regulation of Prox1-gene-expression in liver tumors. BMC Cancer 2008, 8. [Google Scholar] [CrossRef]
- Hong, Y.K.; Harvey, N.; Noh, Y.H.; Schacht, V.; Hirakawa, S.; Detmar, M.; Oliver, G. Prox1 is a master control gene in the program specifying lymphatic endothelial cell fate. Dev. Dyn. 2002, 225, 351–357. [Google Scholar] [CrossRef]
- Joukov, V.; Pajusola, K.; Kaipainen, A.; Chilov, D.; Lahtinen, I.; Kukk, E.; Saksela, O.; Kalkkinen, N.; Alitalo, K. A novel vascular endothelial growth factor, VEGF-C, is a ligand for the Flt4 (VEGFR-3) and KDR (VEGFR-2) receptor tyrosine kinases. EMBO J. 1996, 15, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Burglin, T.R. A Caenorhabditis elegans prospero homologue defines a novel domain. Trends Biochem. Sci. 1994, 19, 70–71. [Google Scholar] [CrossRef]
- Laerm, A.; Helmbold, P.; Goldberg, M.; Dammann, R.; Holzhausen, H.J.; Ballhausen, W.G. Prospero-related homeobox 1 (PROX1) is frequently inactivated by genomic deletions and epigenetic silencing in carcinomas of the bilary system. J. Hepatol. 2007, 46, 89–97. [Google Scholar] [CrossRef]
- Lu, M.H.; Huang, C.C.; Pan, M.R.; Chen, H.H.; Hung, W.C. Prospero Homeobox 1 Promotes Epithelial-Mesenchymal Transition in Colon Cancer Cells by Inhibiting E-cadherin via miR-9. Clin. Cancer Res. 2012, 18, 6416–6425. [Google Scholar] [CrossRef] [PubMed]
- Makinena, T.; Norrmen, C.; Petrova, T.V. Molecular mechanisms of lymphatic vascular development. Cell. Mol. Life Sci. 2007, 64, 1915–1929. [Google Scholar] [CrossRef]
- Schwertfeger, K.L.; Cowman, M.K.; Telmer, P.G.; Turley, E.A.; McCarthy, J.B. Hyaluronan, Inflammation, and Breast Cancer Progression. Front. Immunol. 2015, 6, 236. [Google Scholar] [CrossRef] [PubMed]
- Su, J.L.; Yen, C.J.; Chen, P.S.; Chuang, S.E.; Hong, C.C.; Kuo, I.H.; Chen, H.Y.; Hung, M.C.; Kuo, M.L. The role of the VEGF-C/VEGFR-3 axis in cancer progression. Br. J. Cancer 2007, 96, 541–545. [Google Scholar] [CrossRef]
- Becker, J.; Wang, B.G.; Pavlakovic, H.; Buttler, K.; Wilting, J. Homeobox Transcription Factor Prox1 in Sympathetic Ganglia of Vertebrate Embryos: Correlation With Human Stage 4s Neuroblastoma. Pediatr. Res. 2010, 68, 112–117. [Google Scholar] [CrossRef]
- Oliver, G.; Sosa-Pineda, B.; Geisendorf, S.; Spana, E.P.; Doe, C.Q.; Gruss, P. Prox 1, a prospero-related homeobox gene expressed during mouse development. Mech. Dev. 1993, 44, 3–16. [Google Scholar] [CrossRef]
- Pistocchi, A.; Feijoo, C.G.; Cabrera, P.; Villablanca, E.J.; Allende, M.L.; Cotelli, F. The zebrafish prospero homolog prox1 is required for mechanosensory hair cell differentiation and functionality in the lateral line. BMC Dev. Biol. 2009, 9. [Google Scholar] [CrossRef] [PubMed]
- Tomarev, S.I.; Sundin, O.; Banerjee-Basu, S.; Duncan, M.K.; Yang, J.M.; Piatigorsky, J. Chicken homeobox gene Prox 1 related to Drosophila prospero is expressed in the developing lens and retina. Dev. Dyn. 1996, 206, 354–367. [Google Scholar] [CrossRef]
- Torii, M.A.; Matsuzaki, F.; Osumi, N.; Kaibuchi, K.; Nakamura, S.; Casarosa, S.; Guillemot, F.; Nakafuku, M. Transcription factors Mash-1 and Prox-1 delineate early steps in differentiation of neural stem cells in the developing central nervous system. Development 1999, 126, 443–456. [Google Scholar]
- Duncan, M.K.; Cui, W.W.; Oh, D.J.; Tomarev, S.I. Prox1 is differentially localized during lens development. Mech. Dev. 2002, 112, 195–198. [Google Scholar] [CrossRef]
- Elsir, T.; Smits, A.; Lindstrom, M.S.; Nister, M. Transcription factor PROX1: Its role in development and cancer. Cancer Metastasis Rev. 2012, 31, 793–805. [Google Scholar] [CrossRef]
- Burke, Z.; Oliver, G. Prox1 is an early specific marker for the developing liver and pancreas in the mammalian foregut endoderm. Mech. Dev. 2002, 118, 147–155. [Google Scholar] [CrossRef]
- Song, K.H.; Li, T.G.; Chiang, J.Y.L. A prospero-related homeodomain protein is a novel co-regulator of hepatocyte nuclear factor 4 alpha that regulates the cholesterol 7 alpha-hydroxylase gene. J. Biol. Chem. 2006, 281, 10081–10088. [Google Scholar] [CrossRef]
- Akagami, M.; Kawada, K.; Kubo, H.; Kawada, M.; Takahashi, M.; Kaganoi, J.; Kato, S.; Itami, A.; Shimada, Y.; Watanabe, G.; et al. Transcriptional Factor Prox1 Plays an Essential Role in the Antiproliferative Action of Interferon-gamma in Esophageal Cancer Cells. Ann. Surg. Oncol. 2011, 18, 3868–3877. [Google Scholar] [CrossRef]
- Choi, D.; Ramu, S.; Park, E.; Jung, E.; Yang, S.; Jung, W.; Choi, I.; Lee, S.; Kim, K.E.; Seong, Y.J.; et al. Aberrant Activation of Notch Signaling Inhibits PROX1 Activity to Enhance the Malignant Behavior of Thyroid Cancer Cells. Cancer Res. 2016, 76, 582–593. [Google Scholar] [CrossRef]
- Wang, J.F.; Kilic, G.; Aydin, M.; Burke, Z.; Oliver, G.; Sosa-Pineda, B. Prox1 activity controls pancreas morphogenesis and participates in the production of “secondary transition” pancreatic endocrine cells. Dev. Biol. 2005, 286, 182–194. [Google Scholar] [CrossRef]
- Elsir, T.; Eriksson, A.; Orrego, A.; Lindstrom, M.S.; Nister, M. Expression of PROX1 Is a Common Feature of High-Grade Malignant Astrocytic Gliomas. J. Neuropathol. Exp. Neurol. 2010, 69, 129–138. [Google Scholar] [CrossRef]
- Elsir, T.; Qu, M.; Berntsson, S.G.; Orrego, A.; Olofsson, T.; Lindstrom, M.S.; Nister, M.; von Deimling, A.; Hartmann, C.; Ribom, D.; et al. PROX1 is a predictor of survival for gliomas WHO grade II. Br. J. Cancer 2011, 104, 1747–1754. [Google Scholar] [CrossRef]
- Liu, Y.; Ye, X.; Zhang, J.B.; Ouyang, H.; Shen, Z.; Wu, Y.; Wang, W.; Wu, J.; Tao, S.; Yang, X.; et al. PROX1 promotes hepatocellular carcinoma proliferation and sorafenib resistance by enhancing beta-catenin expression and nuclear translocation. Oncogene 2015, 34, 5524–5535. [Google Scholar] [CrossRef]
- Nagai, H.; Li, Y.H.; Hatano, S.; Toshihito, O.; Yuge, M.; Ito, E.; Utsumi, M.; Saito, H.; Kinoshita, T. Mutations and aberrant DNA methylation of the PROX1 gene in hematologic malignancies. Genes Chromosom. Cancer 2003, 38, 13–21. [Google Scholar] [CrossRef]
- Petrova, T.V.; Nykanen, A.; Norrmen, C.; Ivanov, K.I.; Andersson, L.C.; Haglund, C.; Puolakkainen, P.; Wempe, F.; von Melchner, H.; Gradwohl, G.; et al. Transcription factor PROM induces colon cancer progression by promoting the transition from benign to highly dysplastic phenotype. Cancer Cell 2008, 13, 407–419. [Google Scholar] [CrossRef]
- Rodrigues, M.; Rodini, C.D.O.; Xavier, F.; Paiva, K.B.; Severino, P.; Moyses, R.A.; Lopez, R.M.; DeCicco, R.; Rocha, L.A.; Carvalho, M.B.; et al. PROX1 Gene is Differentially Expressed in Oral Cancer and Reduces Cellular Proliferation. Medicine 2014, 93. [Google Scholar] [CrossRef]
- Saukkonen, K.; Hagstrom, J.; Mustonen, H.; Juuti, A.; Nordling, S.; Kallio, P.; Alitalo, K.; Seppanen, H.; Haglund, C. PROX1 and beta-catenin are prognostic markers in pancreatic ductal adenocarcinoma. BMC Cancer 2016, 16. [Google Scholar] [CrossRef]
- Versmold, B.; Felsberg, J.; Mikeska, T.; Ehrentraut, D.; Kohler, J.; Hampl, J.A.; Rohn, G.; Niederacher, D.; Betz, B.; Hellmich, M.; et al. Epigenetic silencing of the candidate tumor suppressor gene PROX1 in sporadic breast cancer. Int. J. Cancer 2007, 121, 547–554. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, J.B.; Qin, Y.; Wang, W.; Wei, L.; Teng, Y.; Guo, L.; Zhang, B.; Lin, Z.; Liu, J.; Ren, Z.G.; Ye, Q.H.; Xie, Y. PROX1 promotes hepatocellular carcinoma metastasis by way of up-regulating hypoxia-inducible factor 1 alpha expression and protein stability. Hepatology 2013, 58, 692–705. [Google Scholar] [CrossRef]
- Rudzinska, M.; Ledwon, J.K.; Gawel, D.; Sikorska, J.; Czarnocka, B. The role of prospero homeobox 1 (PROX1) expression in follicular thyroid carcinoma cells. Oncotarget 2017, 8, 114136–114155. [Google Scholar] [CrossRef][Green Version]
- Shimoda, M.; Takahashi, M.; Yoshimoto, T.; Kono, T.; Ikai, I.; Kubo, H. A homeobox protein, Prox1, is involved in the differentiation, proliferation, and prognosis in hepatocellular carcinoma. Clin. Cancer Res. 2006, 12, 6005–6011. [Google Scholar] [CrossRef]
- Lin, J.D.; Chao, T.C.; Weng, H.F.; Huang, H.S.; Ho, Y.S. Establishment of xenografts and cell lines from well-differentiated human thyroid carcinoma. J. Surg. Oncol. 1996, 63, 112–118. [Google Scholar] [CrossRef]
- Young, L.; Sung, J.; Stacey, G.; Masters, J.R. Detection of Mycoplasma in cell cultures. Nat. Protoc. 2010, 5, 929–934. [Google Scholar] [CrossRef]
- Xu, X.; Wan, X.; Wei, X. PROX1 promotes human glioblastoma cell proliferation and invasion via activation of the nuclear factor-kappaB signaling pathway. Mol. Med. Rep. 2017, 15, 963–968. [Google Scholar] [CrossRef] [PubMed]
- Park, K.J.; Cho, S.B.; Park, Y.L.; Kim, N.; Park, S.Y.; Myung, D.S.; Lee, W.S.; Kweon, S.S.; Joo, Y.E. Prospero homeobox 1 mediates the progression of gastric cancer by inducing tumor cell proliferation and lymphangiogenesis. Gastric Cancer 2017, 20, 104–115. [Google Scholar] [CrossRef]
- Fincham, V.J.; Frame, M.C. The catalytic activity of Src is dispensable for translocation to focal adhesions but controls the turnover of these structures during cell motility. EMBO J. 1998, 17, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Fehon, R.G.; McClatchey, A.I.; Bretscher, A. Organizing the cell cortex: The role of ERM proteins. Nat. Rev. Mol. Cell Biol. 2010, 11, 276–287. [Google Scholar] [CrossRef]
- Liu, Y.J.; Jang, S.C.; Xie, L.K.; Sowa, G. Host Deficiency in Caveolin-2 Inhibits Lung Carcinoma Tumor Growth by Impairing Tumor Angiogenesis. Cancer Res. 2014, 74, 6452–6462. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Park, D.S.; Wang, X.B.; Scherer, P.E.; Schwartz, P.E.; Lisanti, M.P. Src-induced phosphorylation of caveolin-2 on tyrosine 19. Phospho-caveolin-2 (Tyr(P)19) is localized near focal adhesions, remains associated with lipid rafts/caveolae, but no longer forms a high molecular mass hetero-oligomer with caveolin-1. J. Biol. Chem. 2002, 277, 34556–34567. [Google Scholar] [CrossRef]
- Echarri, A.; Del Pozo, M.A. Caveolae—Mechanosensitive membrane invaginations linked to actin filaments. J. Cell Sci. 2015, 128, 2747–2758. [Google Scholar] [CrossRef]
- King, S.J.; Nowak, K.; Suryavanshi, N.; Holt, I.; Shanahan, C.M.; Ridley, A.J. Nesprin-1 and nesprin-2 regulate endothelial cell shape and migration. Cytoskeleton 2014, 71, 423–434. [Google Scholar] [CrossRef]
- Rajgor, D.; Shanahan, C.M. Nesprins: From the nuclear envelope and beyond. Expert Rev. Mol. Med. 2013, 15, e5. [Google Scholar] [CrossRef]
- Warren, D.T.; Zhang, Q.; Weissberg, P.L.; Shanahan, C.M. Nesprins: Intracellular scaffolds that maintain cell architecture and coordinate cell function? Expert Rev. Mol. Med. 2005, 7, 1–15. [Google Scholar] [CrossRef]
- Cong, D.; He, M.; Chen, S.; Liu, X.; Sun, H. Expression profiles of pivotal microRNAs and targets in thyroid papillary carcinoma: An analysis of The Cancer Genome Atlas. Onco Targets Ther. 2015, 8, 2271–2277. [Google Scholar] [CrossRef] [PubMed]
- Park, J.E.; Son, A.I.; Zhou, R. Roles of EphA2 in Development and Disease. Genes 2013, 4, 334–357. [Google Scholar] [CrossRef]
- Tandon, M.; Vemula, S.V.; Mittal, S.K. Emerging strategies for EphA2 receptor targeting for cancer therapeutics. Expert Opin. Ther. Targets 2011, 15, 31–51. [Google Scholar] [CrossRef] [PubMed]
- Laitinen, A.; Bockelman, C.; Hagstrom, J.; Kokkola, A.; Kallio, P.; Haglund, C. High PROX1 expression in gastric cancer predicts better survival. PLoS ONE 2017, 12, e0183868. [Google Scholar] [CrossRef] [PubMed]
- Skog, M.; Bono, P.; Lundin, M.; Lundin, J.; Louhimo, J.; Linder, N.; Petrova, T.V.; Andersson, L.C.; Joensuu, H.; Alitalo, K.; et al. Expression and prognostic value of transcription factor PROX1 in colorectal cancer. Br. J. Cancer 2011, 105, 1346–1351. [Google Scholar] [CrossRef] [PubMed]
- Taban, O.; Cimpean, A.M.; Raica, M.; Olariu, S. PROX1 Expression in Gastric Cancer: From Hypothesis to Evidence. Anticancer Res. 2014, 34, 3439–3446. [Google Scholar] [CrossRef] [PubMed]
- Giordano, T.J.; Kuick, R.; Thomas, D.G.; Misek, D.E.; Vinco, M.; Sanders, D.; Zhu, Z.W.; Ciampi, R.; Roh, M.; Shedden, K.; et al. Molecular classification of papillary thyroid carcinoma: Distinct BRAF, RAS, and RET/PTC mutation-specific gene expression profiles discovered by DNA microarray analysis. Oncogene 2005, 24, 6646–6656. [Google Scholar] [CrossRef]
- Giordano, T.J.; Au, A.Y.; Kuick, R.; Thomas, D.G.; Rhodes, D.R.; Wilhelm, K.G., Jr.; Vinco, M.; Misek, D.E.; Sanders, D.; Zhu, Z.; et al. Delineation, functional validation, and bioinformatic evaluation of gene expression in thyroid follicular carcinomas with the PAX8-PPARG translocation. Clin. Cancer Res. 2006, 12, 1983–1993. [Google Scholar] [CrossRef]
- Wojtas, B.; Pfeifer, A.; Oczko-Wojciechowska, M.; Krajewska, J.; Czarniecka, A.; Kukulska, A.; Eszlinger, M.; Musholt, T.; Stokowy, T.; Swierniak, M.; et al. Gene Expression (mRNA) Markers for Differentiating between Malignant and Benign Follicular Thyroid Tumours. Int. J. Mol. Sci. 2017, 18, 1184. [Google Scholar] [CrossRef]
- Li, W.; Turner, A.; Aggarwal, P.; Matter, A.; Storvick, E.; Arnett, D.K.; Broeckel, U. Comprehensive evaluation of AmpliSeq transcriptome, a novel targeted whole transcriptome RNA sequencing methodology for global gene expression analysis. BMC Genomics 2015, 16, 1069. [Google Scholar] [CrossRef]
- Love, M.I.; Huber, W.; Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014, 15, 550. [Google Scholar] [CrossRef]
- Anders, S.; Pyl, P.T.; Huber, W. HTSeq—A Python framework to work with high-throughput sequencing data. Bioinformatics 2015, 31, 166–169. [Google Scholar] [CrossRef] [PubMed]
- Yu, G.; Wang, L.G.; Han, Y.; He, Q.Y. clusterProfiler: An R package for comparing biological themes among gene clusters. Omics 2012, 16, 284–287. [Google Scholar] [CrossRef]
- Walter, W.; Sanchez-Cabo, F.; Ricote, M. GOplot: An R package for visually combining expression data with functional analysis. Bioinformatics 2015, 31, 2912–2914. [Google Scholar] [CrossRef] [PubMed]



| Gene | Refseq ID | RNA-Seq | RT-qPCR | |||
|---|---|---|---|---|---|---|
| p-Value | Fold Change | p-Value | Fold Change | SD | ||
| TUBB2A | NM_001069 | 0.063 | 0.775 | 0.001 | 0.41 | 0.03 |
| CALD1 | NM_033138 | <0.0001 | 0.558 | <0.0001 | 0.54 | 0.08 |
| ADAM12 | NM_003474 | 0.001 | 0.518 | 0.001 | 0.57 | 0.11 |
| EPS8 | NM_004447 | 0.022 | 0.653 | 0.001 | 0.62 | 0.09 |
| SDC3 | NM_014654 | 0.012 | 0.694 | 0.016 | 0.63 | 0.12 |
| MYO6 | NM_004999 | 0.012 | 0.555 | 0.039 | 0.65 | 0.10 |
| MVP | NM_005115 | 0.005 | 0.666 | 0.029 | 0.66 | 0.09 |
| PIP5K1C | NM_012398 | 0.011 | 0.696 | 0.015 | 0.67 | 0.08 |
| MAP4 | NM_002375 | 0.003 | 0.650 | 0.049 | 0.68 | 0.19 |
| SEPT6 | NM_015129 | 0.053 | 0.744 | 0.006 | 0.68 | 0.13 |
| COL6A1 | NM_001848 | 0.002 | 0.651 | 0.000 | 0.68 | 0.13 |
| WASL | NM_003941 | 0.010 | 0.714 | 0.015 | 0.74 | 0.09 |
| DYNC1H1 | NM_001376 | 0.001 | 0.633 | 0.002 | 0.76 | 0.21 |
| ADAMTS3 | NM_014243 | 0.011 | 0.503 | 0.033 | 0.77 | 0.13 |
| DAG1 | NM_001177639 | 0.000 | 0.631 | 0.005 | 0.79 | 0.16 |
| COL15A1 | NM_001855 | 0.000 | 0.274 | 0.041 | 0.79 | 0.15 |
| DOCK1 | NM_001380 | 0.017 | 0.680 | 0.001 | 0.79 | 0.09 |
| CDC42EP3 | NM_006449 | 0.048 | 0.761 | 0.049 | 0.81 | 0.18 |
| RAPH1 | NM_213589 | 0.002 | 0.544 | 0.002 | 0.81 | 0.15 |
| PFN2 | NM_053024 | 0.030 | 0.773 | 0.017 | 0.83 | 0.05 |
| BRWD3 | NM_153252 | 0.016 | 0.588 | 0.034 | 0.86 | 0.04 |
| FARP1 | NM_005766 | 0.041 | 0.726 | 0.009 | 0.86 | 0.08 |
| ALCAM | NM_001627 | 0.001 | 1.511 | 0.000 | 1.24 | 0.11 |
| ILK | NM_004517 | 0.004 | 1.515 | 0.044 | 1.24 | 0.17 |
| CD63 | NM_001780 | 0.007 | 1.369 | 0.040 | 1.25 | 0.16 |
| NPM1 | NM_002520 | 0.001 | 1.520 | 0.001 | 1.54 | 0.12 |
| NUP50 | NM_007172 | 0.004 | 1.420 | 0.017 | 1.55 | 0.20 |
| CLDN12 | NM_012129 | 0.038 | 1.589 | 0.005 | 1.65 | 0.26 |
| EIF6 | NM_181468 | 0.000 | 1.749 | 0.024 | 1.65 | 0.20 |
| FRMD5 | NM_032892 | 0.008 | 1.538 | 0.000 | 1.81 | 0.20 |
| Gene | Refseq ID | RNA-Seq | RT-qPCR | |||
|---|---|---|---|---|---|---|
| p-Value | Fold Change | p-Value | Fold Change | SD | ||
| MIGRATION | ||||||
| CEMIP | NM_018689 | 0.001 | 0.459 | <0.0001 | 0.37 | 0.04 |
| SOX2 | NM_003106 | 0.000 | 0.412 | 0.001 | 0.45 | 0.04 |
| DCLK1 | NM_004734 | 0.010 | 0.504 | 0.020 | 0.52 | 0.11 |
| EPHA2 | NM_004431 | 0.001 | 1.696 | 0.001 | 0.66 | 0.09 |
| PTPN13 | NM_080685 | 0.008 | 0.660 | 0.077 | 0.66 | 0.09 |
| COL18A1 | NM_030582 | 0.013 | 0.614 | 0.001 | 0.68 | 0.13 |
| GATA3 | NM_001002295 | 0.001 | 0.555 | 0.001 | 0.70 | 0.07 |
| PLXNB2 | NM_012401 | 0.041 | 0.731 | 0.001 | 0.73 | 0.17 |
| PLXNA1 | NM_032242 | 0.022 | 0.712 | 0.006 | 0.73 | 0.09 |
| PTPN14 | NM_005401 | 0.003 | 0.667 | <0.0001 | 0.74 | 0.16 |
| SOX9 | NM_000346 | 0.002 | 0.623 | 0.002 | 0.77 | 0.12 |
| NRP2 | NM_201266 | 0.046 | 0.752 | 0.002 | 0.81 | 0.12 |
| PIK3CA | NM_006218 | 0.015 | 0.678 | 0.022 | 0.81 | 0.10 |
| ARHGAP18 | NM_033515 | 0.012 | 1.463 | 0.002 | 1.30 | 0.11 |
| HAS2 | NM_005328 | 0.000 | 2.097 | <0.0001 | 2.13 | 0.13 |
| FOCAL ADHESION | ||||||
| TRIOBP | NM_001039141 | 0.002 | 0.623 | <0.0001 | 0.40 | 0.10 |
| POSTN | NM_006475 | 0.030 | 0.566 | <0.0001 | 0.44 | 0.09 |
| ITGA11 | NM_001004439 | 0.000 | 0.456 | <0.0001 | 0.49 | 0.10 |
| SVIL | NM_021738 | 0.001 | 0.513 | 0.008 | 0.55 | 0.11 |
| SYNE2 | NM_182914 | 0.046 | 0.672 | 0.006 | 0.58 | 0.10 |
| PEAK1 | NM_024776 | 0.000 | 0.492 | 0.006 | 0.68 | 0.10 |
| ITGA6 | NM_001079818 | 0.021 | 0.723 | 0.030 | 0.73 | 0.07 |
| ROCK1 | NM_005406 | 0.001 | 0.585 | 0.002 | 0.80 | 0.23 |
| PTK2 | NM_005607 | 0.013 | 1.350 | 0.004 | 1.24 | 0.18 |
| DAPK3 | NM_001348 | 0.002 | 1.731 | 0.024 | 1.34 | 0.20 |
| MCAM | NM_006500 | 0.003 | 1.517 | 0.023 | 1.44 | 0.19 |
| ITGA2 | NM_002203 | 0.003 | 1.403 | <0.0001 | 1.85 | 0.25 |
| CAV2 | NM_001233 | 0.000 | 1.706 | <0.0001 | 1.88 | 0.41 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rudzińska, M.; Grzanka, M.; Stachurska, A.; Mikula, M.; Paczkowska, K.; Stępień, T.; Paziewska, A.; Ostrowski, J.; Czarnocka, B. Molecular Signature of Prospero Homeobox 1 (PROX1) in Follicular Thyroid Carcinoma Cells. Int. J. Mol. Sci. 2019, 20, 2212. https://doi.org/10.3390/ijms20092212
Rudzińska M, Grzanka M, Stachurska A, Mikula M, Paczkowska K, Stępień T, Paziewska A, Ostrowski J, Czarnocka B. Molecular Signature of Prospero Homeobox 1 (PROX1) in Follicular Thyroid Carcinoma Cells. International Journal of Molecular Sciences. 2019; 20(9):2212. https://doi.org/10.3390/ijms20092212
Chicago/Turabian StyleRudzińska, Magdalena, Małgorzata Grzanka, Anna Stachurska, Michał Mikula, Katarzyna Paczkowska, Tomasz Stępień, Agnieszka Paziewska, Jerzy Ostrowski, and Barbara Czarnocka. 2019. "Molecular Signature of Prospero Homeobox 1 (PROX1) in Follicular Thyroid Carcinoma Cells" International Journal of Molecular Sciences 20, no. 9: 2212. https://doi.org/10.3390/ijms20092212
APA StyleRudzińska, M., Grzanka, M., Stachurska, A., Mikula, M., Paczkowska, K., Stępień, T., Paziewska, A., Ostrowski, J., & Czarnocka, B. (2019). Molecular Signature of Prospero Homeobox 1 (PROX1) in Follicular Thyroid Carcinoma Cells. International Journal of Molecular Sciences, 20(9), 2212. https://doi.org/10.3390/ijms20092212






