Alpha-Synuclein RNA Expression is Increased in Major Depression
Abstract
1. Introduction
2. Results
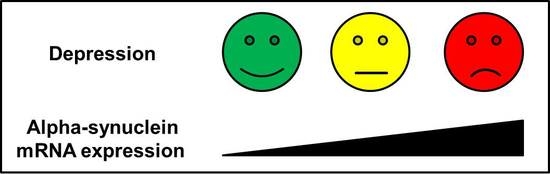
2.1. SNCA mRNA Expression Correlates Positively with the Severity of Depressive Symptoms
2.2. SNCA mRNA Expression is Increased in Patients with Severe Depression
3. Discussion
4. Materials and Methods
4.1. Ethics Statement
4.2. Study Sample
4.3. RNA Isolation and cDNA Synthesis
4.4. Quantitative PCR
4.5. Statistical Analysis
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Iwai, A.; Masliah, E.; Yoshimoto, M.; Ge, N.; Flanagan, L.; de Silva, H.A.; Kittel, A.; Saitoh, T. The precursor protein of non-Aβ component of Alzheimer’s disease amyloid is a presynaptic protein of the central nervous system. Neuron 1995, 14, 467–475. [Google Scholar] [CrossRef]
- Iwai, A.; Yoshimoto, M.; Masliah, E.; Saitoh, T. Non-Aβ component of Alzheimer’s disease amyloid (NAC) is amyloidogenic. Biochemistry 1995, 34, 10139–10145. [Google Scholar] [CrossRef] [PubMed]
- Bayer, T.A.; Jakala, P.; Hartmann, T.; Egensperger, R.; Buslei, R.; Falkai, P.; Beyreuther, K. Neural expression profile of alpha-synuclein in developing human cortex. Neuroreport 1999, 10, 2799–2803. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.; Wetherill, L.; Bucholz, K.K.; Kramer, J.; Kuperman, S.; Lynskey, M.T.; Nurnberger, J.I., Jr.; Schuckit, M.; Tischfield, J.A.; Edenberg, H.J.; et al. Genetic influences on craving for alcohol. Addict. Behav. 2013, 38, 1501–1508. [Google Scholar] [CrossRef]
- Pfefferkorn, C.M.; Lee, J.C. Tryptophan probes at the α-synuclein and membrane interface. J. Phys. Chem. B 2010, 114, 4615–4622. [Google Scholar] [CrossRef] [PubMed]
- Quilty, M.C.; Gai, W.-P.; Pountney, D.L.; West, A.K.; Vickers, J.C. Localization of α-, β-, and γ-synuclein during neuronal development and alterations associated with the neuronal response to axonal trauma. Exp. Neurol. 2003, 182, 195–207. [Google Scholar] [CrossRef]
- Madine, J.; Doig, A.J.; Middleton, D.A. A study of the regional effects of α-synuclein on the organization and stability of phospholipid bilayers. Biochemistry 2006, 45, 5783–5792. [Google Scholar] [CrossRef]
- Hsu, L.J.; Mallory, M.; Xia, Y.; Veinbergs, I.; Hashimoto, M.; Yoshimoto, M.; Thal, L.J.; Saitoh, T.; Masliah, E. Expression pattern of synucleins (non-β component of Alzheimer’s disease amyloid precursor protein/α-synuclein) during murine brain development. J. Neurochem. 1998, 71, 338–344. [Google Scholar] [CrossRef]
- George, J.M.; Jin, H.; Woods, W.S.; Clayton, D.F. Characterization of a novel protein regulated during the critical period for song learning in the zebra finch. Neuron 1995, 15, 361–372. [Google Scholar] [CrossRef]
- Gureviciene, I.; Gurevicius, K.; Tanila, H. Aging and α-synuclein affect synaptic plasticity in the dentate gyrus. J. Neural Transm. 2009, 116, 13–22. [Google Scholar] [PubMed]
- Stefanova, N.; Seppi, K.; Scherfler, C.; Puschban, Z.; Wenning, G.K. Depression in alpha-synucleinopathies: Prevalence, pathophysiology and treatment. J. Neural Transm. Suppl. 2000, 335–343. [Google Scholar]
- DeRubeis, R.J.; Siegle, G.J.; Hollon, S.D. Cognitive therapy versus medication for depression: Treatment outcomes and neural mechanisms. Nat. Rev. Neurosci. 2008, 9, 788–796. [Google Scholar] [CrossRef] [PubMed]
- Howren, M.B.; Lamkin, D.M.; Suls, J. Associations of depression with C-reactive protein, IL-1, and IL-6: A meta-analysis. Psychosom. Med. 2009, 71, 171–186. [Google Scholar] [CrossRef]
- Dowlati, Y.; Herrmann, N.; Swardfager, W.; Liu, H.; Sham, L.; Reim, E.K.; Lanctôt, K.L. A meta-analysis of cytokines in major depression. Biol. Psychiatry 2010, 67, 446–457. [Google Scholar] [CrossRef] [PubMed]
- Lenz, B.; Sysk, C.; Thuerauf, N.; Clepce, M.; Reich, K.; Frieling, H.; Winterer, G.; Bleich, S.; Kornhuber, J. Erratum to: NACP-Rep1 relates to Beck Depression Inventory scores in healthy humans. J. Mol. Neurosci. 2013, 50, 376–377. [Google Scholar] [CrossRef][Green Version]
- Zhang, X.; Beaulieu, J.-M.; Sotnikova, T.D.; Gainetdinov, R.R.; Caron, M.G. Tryptophan hydroxylase-2 controls brain serotonin synthesis. Science 2004, 305, 217. [Google Scholar] [CrossRef]
- Frieling, H.; Gozner, A.; Römer, K.D.; Wilhelm, J.; Hillemacher, T.; Kornhuber, J.; de Zwaan, M.; Jacoby, G.E.; Bleich, S. Alpha-synuclein mRNA levels correspond to beck depression inventory scores in females with eating disorders. Neuropsychobiology 2008, 58, 48–52. [Google Scholar] [CrossRef]
- Oaks, A.W.; Sidhu, A. Synuclein modulation of monoamine transporters. FEBS Lett. 2011, 585, 1001–1006. [Google Scholar] [CrossRef]
- Jeannotte, A.M.; Sidhu, A. Regulation of the norepinephrine transporter by α-synuclein-mediated interactions with microtubules. Eur. J. Neurosci. 2007, 26, 1509–1520. [Google Scholar] [CrossRef]
- Wersinger, C.; Jeannotte, A.; Sidhu, A. Attenuation of the norepinephrine transporter activity and trafficking via interactions with α-synuclein. Eur. J. Neurosci. 2006, 24, 3141–3152. [Google Scholar] [CrossRef]
- Wersinger, C.; Rusnak, M.; Sidhu, A. Modulation of the trafficking of the human serotonin transporter by human alpha-synuclein. Eur. J. Neurosci. 2006, 24, 55–64. [Google Scholar] [CrossRef]
- Henningsen, K.; Palmfeldt, J.; Christiansen, S.; Baiges, I.; Bak, S.; Jensen, O.N.; Gregersen, N.; Wiborg, O. Candidate hippocampal biomarkers of susceptibility and resilience to stress in a rat model of depression. Mol. Cell Proteom. 2012, 11, M111 016428. [Google Scholar] [CrossRef]
- Jeannotte, A.M.; McCarthy, J.G.; Redei, E.E.; Sidhu, A. Desipramine modulation of α-, γ-synuclein, and the norepinephrine transporter in an animal model of depression. Neuropsychopharmacology 2009, 34, 987–998. [Google Scholar] [CrossRef]
- Lee, J.H.; Ko, E.; Kim, Y.E.; Min, J.Y.; Liu, J.; Kim, Y.; Shin, M.; Hong, M.; Bae, H. Gene expression profile analysis of genes in rat hippocampus from antidepressant treated rats using DNA microarray. BMC Neurosci. 2010, 11, 152. [Google Scholar] [CrossRef]
- McHugh, P.C.; Rogers, G.R.; Glubb, D.M.; Joyce, P.R.; Kennedy, M.A. Proteomic analysis of rat hippocampus exposed to the antidepressant paroxetine. J. Psychopharmacol 2010, 24, 1243–1251. [Google Scholar] [CrossRef]
- Bönsch, D.; Greifenberg, V.; Bayerlein, K.; Biermann, T.; Reulbach, U.; Hillemacher, T.; Kornhuber, J.; Bleich, S. α-Synuclein protein levels are increased in alcoholic patients and are linked to craving. Alcohol Clin. Exp. Res. 2005, 29, 763–765. [Google Scholar] [CrossRef]
- Bönsch, D.; Lederer, T.; Reulbach, U.; Hothorn, T.; Kornhuber, J.; Bleich, S. Joint analysis of the NACP-REP1 marker within the alpha synuclein gene concludes association with alcohol dependence. Hum. Mol. Genet. 2005, 14, 967–971. [Google Scholar] [CrossRef]
- Levey, D.F.; Le-Niculescu, H.; Frank, J.; Ayalew, M.; Jain, N.; Kirlin, B.; Learman, R.; Winiger, E.; Rodd, Z.; Shekhar, A.; et al. Genetic risk prediction and neurobiological understanding of alcoholism. Transl. Psychiatry 2014, 4, e391. [Google Scholar] [CrossRef]
- Ishiguro, M.; Baba, H.; Maeshima, H.; Shimano, T.; Inoue, M.; Ichikawa, T.; Yasuda, S.; Shukuzawa, H.; Suzuki, T.; Arai, H. Increased serum levels of α-synuclein in patients with major depressive disorder. Am. J. Geriatr. Psychiatry 2019, 27, 280–286. [Google Scholar] [CrossRef]
- Eyre, H.A.; Eskin, A.; Nelson, S.F.; Cyr, N.M. St.; Siddarth, P.; Baune, B.T.; Lavretsky, H. Genomic predictors of remission to antidepressant treatment in geriatric depression using genome-wide expression analyses: A pilot study. Int. J. Geriatr. Psychiatry 2016, 31, 510–517. [Google Scholar] [CrossRef]
- Caudal, D.; Alvarsson, A.; Bjorklund, A.; Svenningsson, P. Depressive-like phenotype induced by AAV-mediated overexpression of human α-synuclein in midbrain dopaminergic neurons. Exp. Neurol. 2015, 273, 243–252. [Google Scholar] [CrossRef]
- Kohl, Z.; Winner, B.; Ubhi, K.; Rockenstein, E.; Mante, M.; Münch, M.; Barlow, C.; Carter, T.; Masliah, E.; Winkler, J. Fluoxetine rescues impaired hippocampal neurogenesis in a transgenic A53T synuclein mouse model. Eur. J. Neurosci. 2012, 35, 10–19. [Google Scholar] [CrossRef]
- Brenz Verca, M.S.; Bahi, A.; Boyer, F.; Wagner, G.C.; Dreyer, J.L. Distribution of α- and γ-synucleins in the adult rat brain and their modification by high-dose cocaine treatment. Eur. J. Neurosci. 2003, 18, 1923–1938. [Google Scholar] [CrossRef]
- Gallagher, D.A.; Lees, A.J.; Schrag, A. What are the most important nonmotor symptoms in patients with Parkinson’s disease and are we missing them? Mov. Disord. 2010, 25, 2493–2500. [Google Scholar] [CrossRef]
- Devos, D.; Dujardin, K.; Poirot, I.; Moreau, C.; Cottencin, O.; Thomas, P.; Destée, A.; Bordet, R.; Defebvre, L. Comparison of desipramine and citalopram treatments for depression in Parkinson’s disease: A double-blind, randomized, placebo-controlled study. Mov. Disord. 2008, 23, 850–857. [Google Scholar] [CrossRef]
- Menza, M.; Dobkin, R.D.; Marin, H.; Mark, M.H.; Gara, M.; Buyske, S.; Bienfait, K.; Dicke, A. A controlled trial of antidepressants in patients with Parkinson disease and depression. Neurology 2009, 72, 886–892. [Google Scholar] [CrossRef]
- Deusser, J.; Schmidt, S.; Ettle, B.; Plötz, S.; Huber, S.; Müller, C.P.; Masliah, E.; Winkler, J.; Kohl, Z. Serotonergic dysfunction in the A53T alpha-synuclein mouse model of Parkinson’s disease. J. Neurochem. 2015, 135, 589–597. [Google Scholar] [CrossRef]
- Rotter, A.; Asemann, R.; Decker, A.; Kornhuber, J.; Biermann, T. Orexin expression and promoter-methylation in peripheral blood of patients suffering from major depressive disorder. J. Affect. Disord. 2011, 131, 186–192. [Google Scholar] [CrossRef]
- Lenz, B.; Klafki, H.W.; Hillemacher, T.; Frieling, H.; Clepce, M.; Gossler, A.; Thuerauf, N.; Winterer, G.; Kornhuber, J.; Bleich, S. ERK1/2 protein and mRNA levels in human blood are linked to smoking behavior. Addict. Biol. 2012, 17, 1026–1035. [Google Scholar] [CrossRef]
| BLADe | ADT | Healthy Controls | p-Value | |
|---|---|---|---|---|
| N (male/female) | 39 (15/24) | 31 (15/16) | 18 (13/5) | 0.060 |
| Age (years ± SD) | 46.3 ± 14.2 | 39.7 ± 16.5 | 30.4 ± 8.8 | 0.001 |
| BLADe | ADT | Healthy Controls | p-Value | |
|---|---|---|---|---|
| SNCA expression ± SD | 31.9 ± 15.3 | 24.3 ± 13.8 | 17.4 ± 5.4 | 0.004 |
| HAM-D scores ± SD | 21.4 ± 5.2 | 17.9 ± 8.2 | - | 0.034 |
| SNCA-F | 5′-CTC CTT TTC CTT CTT CTT TCC T-3′ |
| SNCA-R | 5′-TGT TTG GTT TTC TCA GCA GC-3′ |
| B-Actin-F | 5′-GTC TTC CCC TCC ATC GTG-3′ |
| B-Actin-R | 5′-AGG TGT GGT GCC AGA TTT TC-3′ |
| B-Actin-probe | 5′ Cy5-GAG CAA GAG AGG CAT CCT CAC CCT GAA GTA-Eclipse 3′ |
| ODC1-F | 5′-CGC TTA CAC TGT TGC TGC TG-3′ |
| ODC1-R | 5′-CAT CCT GTT CCT CTA CTT CGG G-3′ |
| ODC1-probe | 5′ HEX-TCC AGA GGC CGA CGA TCT ACT ATG TGA TGT-BHQ1 3′ |
| B2M-F | 5′-CGC TAC TCTC TCT TTC TGG C-3′ |
| B2M-R | 5′-GTC AAC TTC AAT GTC GGA TGG AT-3′ |
| B2M-probe | #42 of Roche Universal Probe Library |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rotter, A.; Lenz, B.; Pitsch, R.; Richter-Schmidinger, T.; Kornhuber, J.; Rhein, C. Alpha-Synuclein RNA Expression is Increased in Major Depression. Int. J. Mol. Sci. 2019, 20, 2029. https://doi.org/10.3390/ijms20082029
Rotter A, Lenz B, Pitsch R, Richter-Schmidinger T, Kornhuber J, Rhein C. Alpha-Synuclein RNA Expression is Increased in Major Depression. International Journal of Molecular Sciences. 2019; 20(8):2029. https://doi.org/10.3390/ijms20082029
Chicago/Turabian StyleRotter, Andrea, Bernd Lenz, Ruben Pitsch, Tanja Richter-Schmidinger, Johannes Kornhuber, and Cosima Rhein. 2019. "Alpha-Synuclein RNA Expression is Increased in Major Depression" International Journal of Molecular Sciences 20, no. 8: 2029. https://doi.org/10.3390/ijms20082029
APA StyleRotter, A., Lenz, B., Pitsch, R., Richter-Schmidinger, T., Kornhuber, J., & Rhein, C. (2019). Alpha-Synuclein RNA Expression is Increased in Major Depression. International Journal of Molecular Sciences, 20(8), 2029. https://doi.org/10.3390/ijms20082029