Contribution of Inflammatory Cytokine Interleukin-18 Genotypes to Renal Cell Carcinoma
Abstract
1. Introduction
2. Results
2.1. Comparison of Characteristics Among Patients with Renal Cell Carcinoma (RCC) and Controls
2.2. Analysis of the Association of IL-18 Promoter Genotypes and RCC Risk in Taiwan
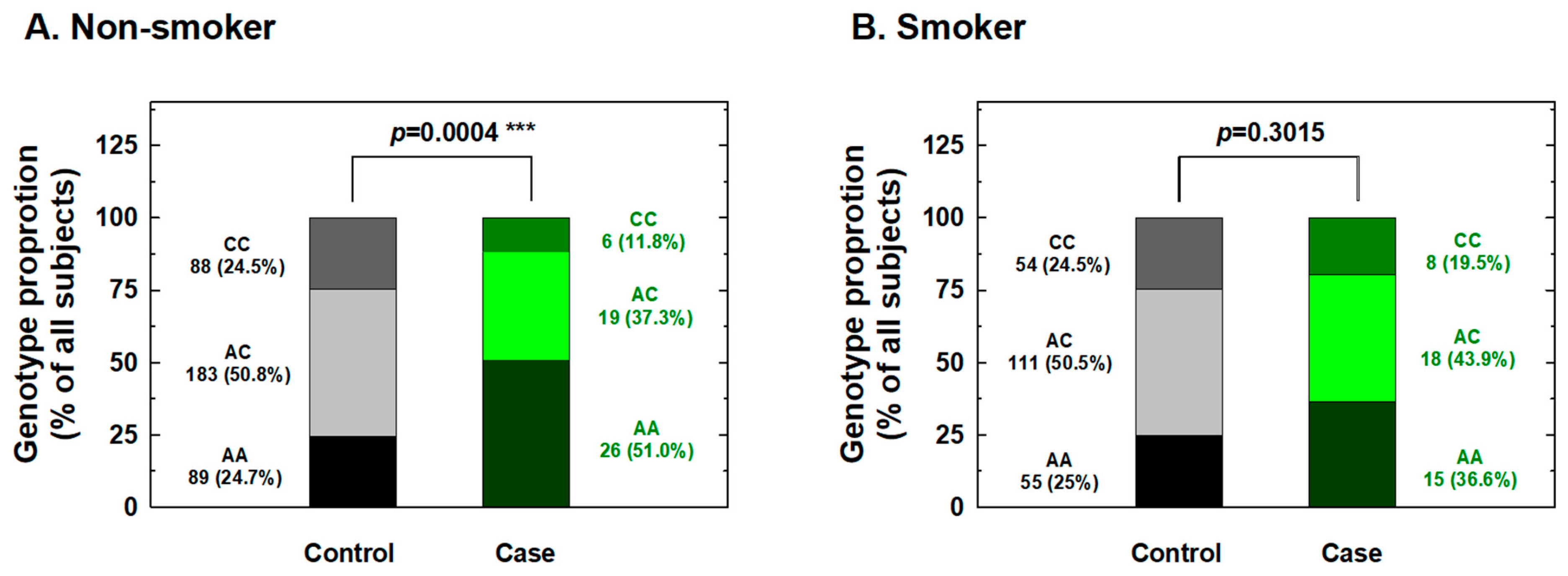
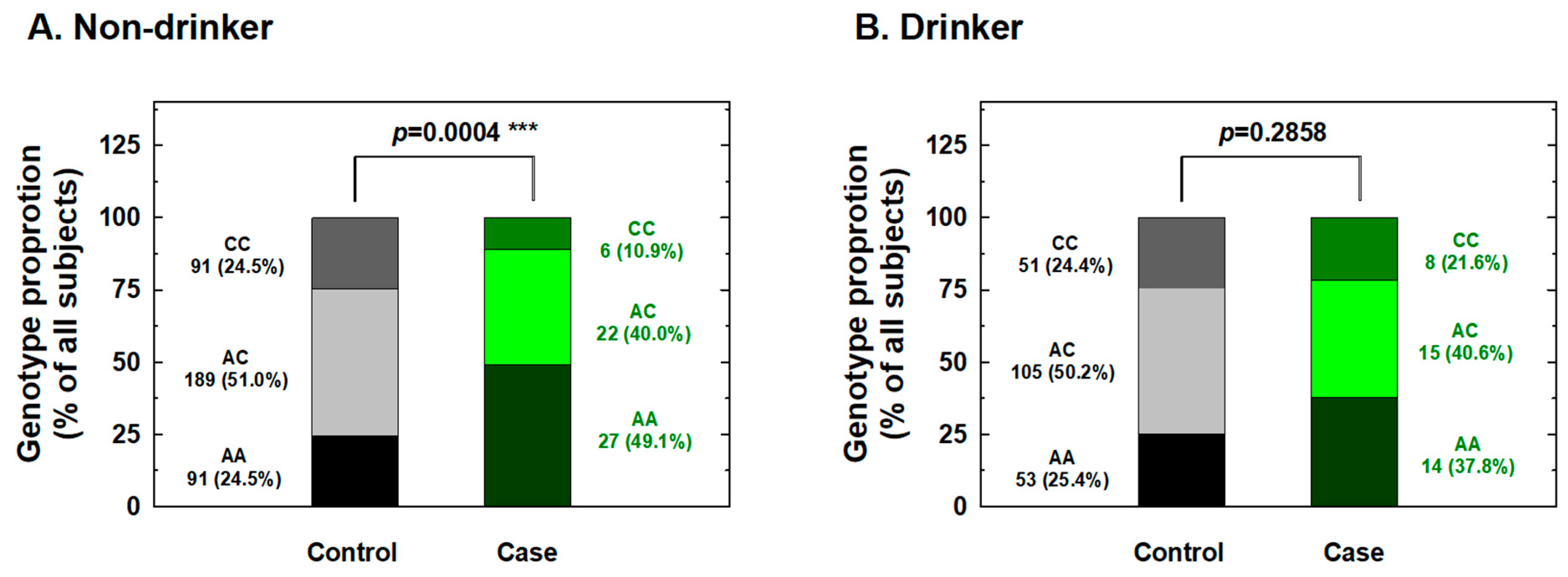
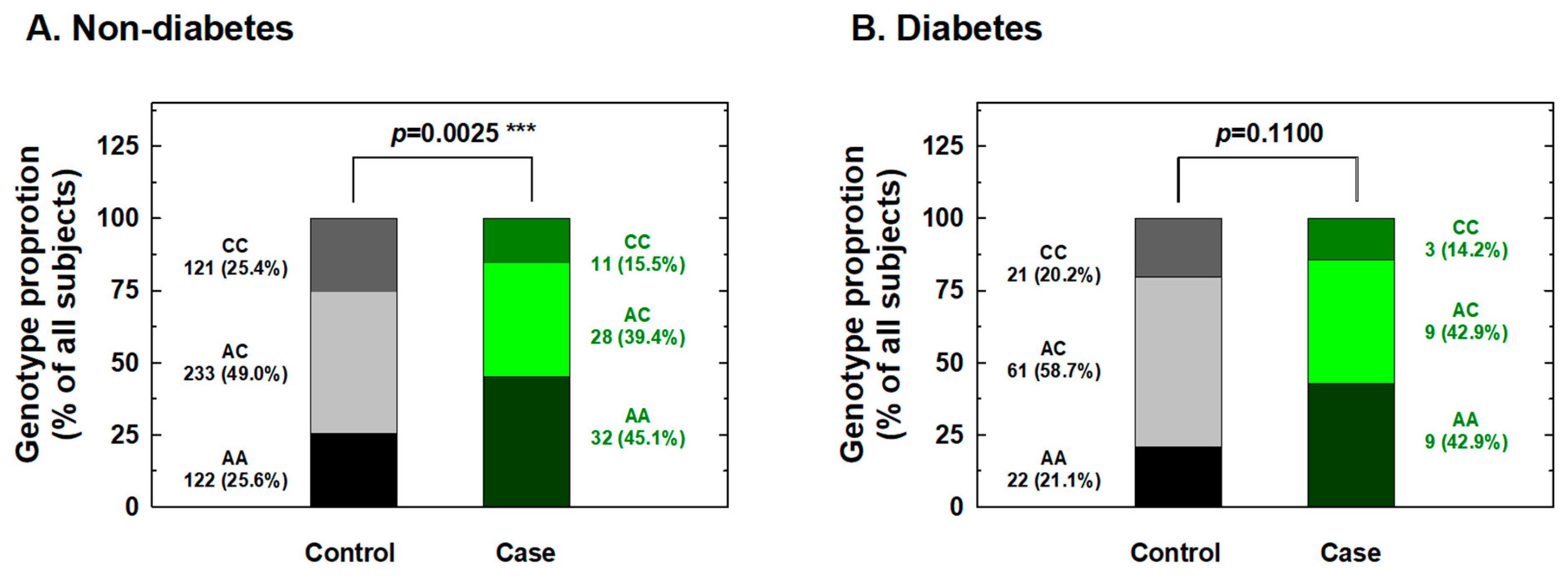
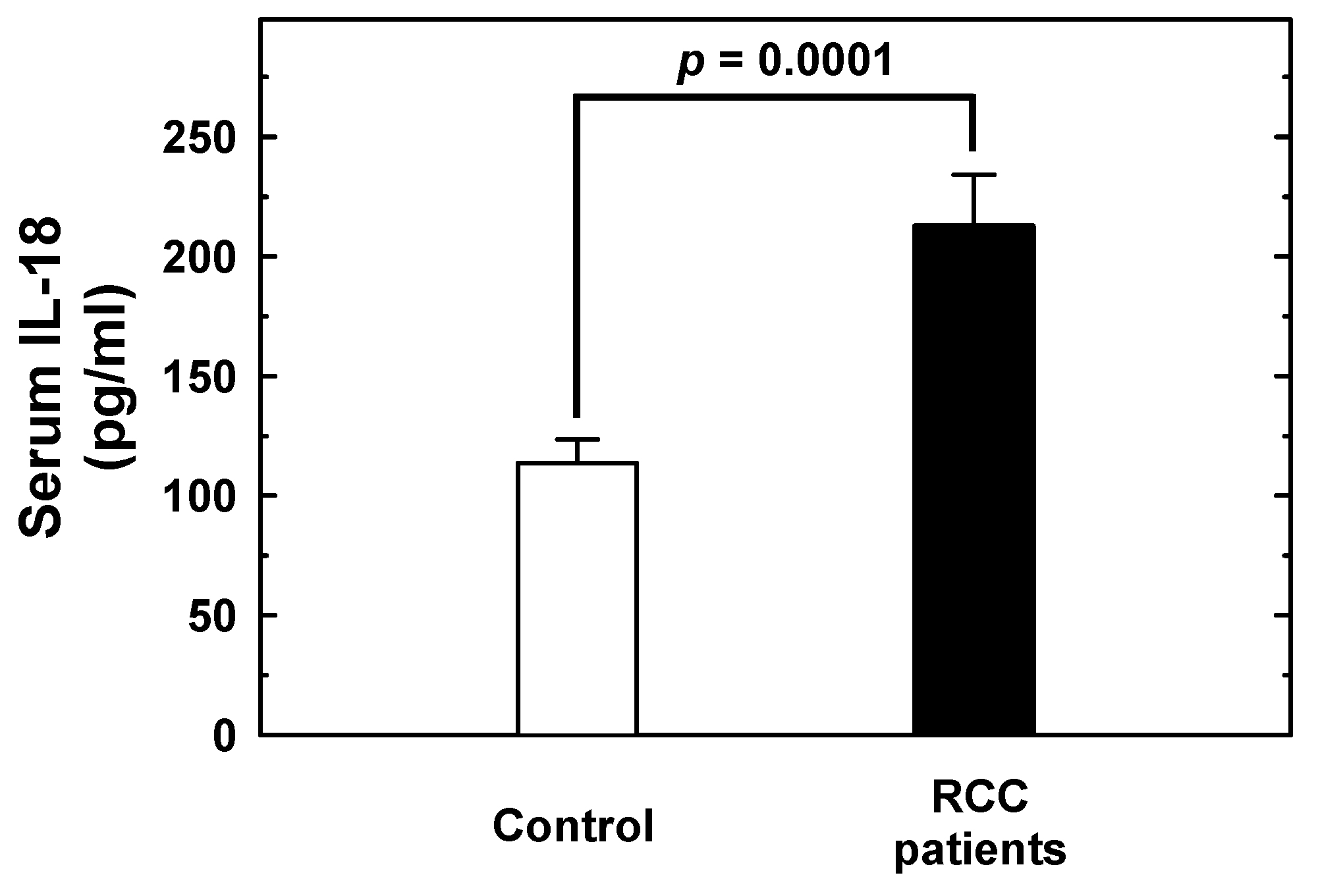
2.3. Stratified Analysis of IL-18 Genotypes According to Personal Behavioral and Clinical Factors
3. Discussion
4. Materials and Methods
4.1. Selected Subjects
4.2. DNA Preparation and Storage
4.3. IL-18 Genotype Discrimination Methodology
4.4. Enzyme-linked Immunosorbent Assay (ELISA) for Serum IL-18 Levels
4.5. Statistical Analysis Methodology
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2018. CA Cancer J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Shin, H.R.; Bray, F.; Forman, D.; Mathers, C.; Parkin, D.M. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer 2010, 127, 2893–2917. [Google Scholar] [CrossRef] [PubMed]
- Klaassen, Z.; Sayyid, R.K.; Wallis, C.J.D. Lessons learned from the global epidemiology of kidney cancer: A refresher in epidemiology 101. Eur. Urol. 2019, 75, 85–87. [Google Scholar] [CrossRef]
- Niedworok, C.; Dorrenhaus, B.; Vom Dorp, F.; Piotrowski, J.A.; Tschirdewahn, S.; Szarvas, T.; Rubben, H.; Schenck, M. Renal cell carcinoma and tumour thrombus in the inferior vena cava: Clinical outcome of 98 consecutive patients and the prognostic value of preoperative parameters. World J. Urol. 2015, 33, 1541–1552. [Google Scholar] [CrossRef]
- Cohen, H.T.; McGovern, F.J. Renal-cell carcinoma. N. Engl. J. Med. 2005, 353, 2477–2490. [Google Scholar] [CrossRef]
- Okamura, H.; Tsutsi, H.; Komatsu, T.; Yutsudo, M.; Hakura, A.; Tanimoto, T.; Torigoe, K.; Okura, T.; Nukada, Y.; Hattori, K.; et al. Cloning of a new cytokine that induces IFN-gamma production by T cells. Nature 1995, 378, 88–91. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, K.; Yoshimoto, T.; Tsutsui, H.; Okamura, H. Interleukin-18 is a unique cytokine that stimulates both Th1 and Th2 responses depending on its cytokine milieu. Cytokine Growth Factor Rev. 2001, 12, 53–72. [Google Scholar] [CrossRef]
- Golab, J. Interleukin 18--interferon gamma inducing factor--a novel player in tumour immunotherapy? Cytokine 2000, 12, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, T.; Akasaki, Y.; Joki, T.; Abe, T.; Kurimoto, M.; Ohno, T. Antitumor activity of interleukin-18 on mouse glioma cells. J. Immunother. 2000, 23, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Okano, F.; Yamada, K. Canine interleukin-18 induces apoptosis and enhances Fas ligand mRNA expression in a canine carcinoma cell line. Anticancer Res. 2000, 20, 3411–3415. [Google Scholar]
- Cao, R.; Farnebo, J.; Kurimoto, M.; Cao, Y. Interleukin-18 acts as an angiogenesis and tumor suppressor. FASEB J. 1999, 13, 2195–2202. [Google Scholar] [CrossRef] [PubMed]
- Park, C.C.; Morel, J.C.; Amin, M.A.; Connors, M.A.; Harlow, L.A.; Koch, A.E. Evidence of IL-18 as a novel angiogenic mediator. J. Immunol. 2001, 167, 1644–1653. [Google Scholar] [CrossRef] [PubMed]
- Vidal-Vanaclocha, F.; Mendoza, L.; Telleria, N.; Salado, C.; Valcarcel, M.; Gallot, N.; Carrascal, T.; Egilegor, E.; Beaskoetxea, J.; Dinarello, C.A. Clinical and experimental approaches to the pathophysiology of interleukin-18 in cancer progression. Cancer Metastasis Rev. 2006, 25, 417–434. [Google Scholar] [CrossRef] [PubMed]
- Jaiswal, P.K.; Singh, V.; Srivastava, P.; Mittal, R.D. Association of IL-12, IL-18 variants and serum IL-18 with bladder cancer susceptibility in North Indian population. Gene 2013, 519, 128–134. [Google Scholar] [CrossRef]
- Samsami Dehaghani, A.; Shahriary, K.; Kashef, M.A.; Naeimi, S.; Fattahi, M.J.; Mojtahedi, Z.; Ghaderi, A. Interleukin-18 gene promoter and serum level in women with ovarian cancer. Mol. Biol. Rep. 2009, 36, 2393–2397. [Google Scholar] [CrossRef]
- Haghshenas, M.R.; Hosseini, S.V.; Mahmoudi, M.; Saberi-Firozi, M.; Farjadian, S.; Ghaderi, A. IL-18 serum level and IL-18 promoter gene polymorphism in Iranian patients with gastrointestinal cancers. J. Gastroenterol. Hepatol. 2009, 24, 1119–1122. [Google Scholar] [CrossRef]
- Okamoto, M.; Azuma, K.; Hoshino, T.; Imaoka, H.; Ikeda, J.; Kinoshita, T.; Takamori, S.; Ohshima, K.; Edakuni, N.; Kato, S.; et al. Correlation of decreased survival and IL-18 in bone metastasis. Intern. Med. 2009, 48, 763–773. [Google Scholar] [CrossRef]
- Gunel, N.; Coskun, U.; Sancak, B.; Gunel, U.; Hasdemir, O.; Bozkurt, S. Clinical importance of serum interleukin-18 and nitric oxide activities in breast carcinoma patients. Cancer 2002, 95, 663–667. [Google Scholar] [CrossRef]
- Giedraitis, V.; He, B.; Huang, W.X.; Hillert, J. Cloning and mutation analysis of the human IL-18 promoter: A possible role of polymorphisms in expression regulation. J. Neuroimmunol. 2001, 112, 146–152. [Google Scholar] [CrossRef]
- Wei, Y.S.; Lan, Y.; Liu, Y.G.; Tang, H.; Tang, R.G.; Wang, J.C. Interleukin-18 gene promoter polymorphisms and the risk of esophageal squamous cell carcinoma. Acta. Oncol. 2007, 46, 1090–1096. [Google Scholar] [CrossRef]
- Liu, Y.; Lin, N.; Huang, L.; Xu, Q.; Pang, G. Genetic polymorphisms of the interleukin-18 gene and risk of prostate cancer. DNA Cell. Biol. 2007, 26, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Nikiteas, N.; Yannopoulos, A.; Chatzitheofylaktou, A.; Tsigris, C. Heterozygosity for interleukin-18 -607 A/C polymorphism is associated with risk for colorectal cancer. Anticancer Res. 2007, 27, 3849–3853. [Google Scholar] [PubMed]
- Bushley, A.W.; Ferrell, R.; McDuffie, K.; Terada, K.Y.; Carney, M.E.; Thompson, P.J.; Wilkens, L.R.; Tung, K.H.; Ness, R.B.; Goodman, M.T. Polymorphisms of interleukin (IL)-1alpha, IL-1beta, IL-6, IL-10, and IL-18 and the risk of ovarian cancer. Gynecol. Oncol. 2004, 95, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Khalili-Azad, T.; Razmkhah, M.; Ghiam, A.F.; Doroudchi, M.; Talei, A.R.; Mojtahedi, Z.; Ghaderi, A. Association of interleukin-18 gene promoter polymorphisms with breast cancer. Neoplasma 2009, 56, 22–25. [Google Scholar] [CrossRef]
- Vairaktaris, E.; Serefoglou, Z.C.; Yapijakis, C.; Agapi, C.; Vassiliou, S.; Nkenke, E.; Antonis, V.; Sofia, S.; Neukam, F.W.; Patsouris, E. The interleukin-18 -607A/C polymorphism is not associated with risk for oral cancer. Anticancer Res. 2007, 27, 4011–4014. [Google Scholar] [PubMed]
- Asefi, V.; Mojtahedi, Z.; Khademi, B.; Naeimi, S.; Ghaderi, A. Head and neck squamous cell carcinoma is not associated with interleukin-18 promoter gene polymorphisms: A case-control study. J. Laryngol. Otol. 2009, 123, 444–448. [Google Scholar] [CrossRef]
- Saenz-Lopez, P.; Carretero, R.; Vazquez, F.; Martin, J.; Sanchez, E.; Tallada, M.; Garrido, F.; Cozar, J.M.; Ruiz-Cabello, F. Impact of interleukin-18 polymorphisms-607 and -137 on clinical characteristics of renal cell carcinoma patients. Hum. Immunol. 2010, 71, 309–313. [Google Scholar] [CrossRef]
- Chang, W.S.; Ke, H.L.; Tsai, C.W.; Lien, C.S.; Liao, W.L.; Lin, H.H.; Lee, M.H.; Wu, H.C.; Chang, C.H.; Chen, C.C.; et al. The role of XRCC6 T-991C functional polymorphism in renal cell carcinoma. Anticancer Res. 2012, 32, 3855–3860. [Google Scholar]
- Chang, W.S.; Tsai, C.W.; Wang, S.M.; Wang, S.W.; Wu, H.C.; Ji, H.X.; Lin, C.H.; Wang, Z.H.; Chou, J.C.; Bau, D.T.; et al. Association of caveolin-1 genotypes with renal cell carcinoma risk in Taiwan. Chin. J. Physiol. 2014, 57, 220–226. [Google Scholar] [CrossRef]
- Chang, W.S.; Liao, C.H.; Miao, C.E.; Wu, H.C.; Hou, L.L.; Hsiao, C.L.; Ji, H.X.; Tsai, C.W.; Bau, D.T. The role of functional polymorphisms of cyclooxygenase 2 in renal cell carcinoma. Anticancer Res. 2014, 34, 5481–5486. [Google Scholar]
- Chang, W.S.; Liao, C.H.; Tsai, C.W.; Hu, P.S.; Wu, H.C.; Hsu, S.W.; Ji, H.X.; Hsiao, C.L.; Bau, D.T. The Role of IL-10 Promoter Polymorphisms in Renal Cell Carcinoma. Anticancer Res. 2016, 36, 2205–2209. [Google Scholar]
- Liao, C.H.; Chang, W.S.; Hu, P.S.; Wu, H.C.; Hsu, S.W.; Liu, Y.F.; Liu, S.P.; Hung, H.S.; Bau, D.T.; Tsai, C.W. The Contribution of MMP-7 Promoter Polymorphisms in Renal Cell Carcinoma. In Vivo 2017, 31, 631–635. [Google Scholar] [PubMed]
- Aggarwal, B.B.; Shishodia, S.; Sandur, S.K.; Pandey, M.K.; Sethi, G. Inflammation and cancer: How hot is the link? Biochem. Pharmacol. 2006, 72, 1605–1621. [Google Scholar] [CrossRef] [PubMed]
- Lian, H.; Jin, N.; Li, X.; Mi, Z.; Zhang, J.; Sun, L.; Li, X.; Zheng, H.; Li, P. Induction of an effective anti-tumor immune response and tumor regression by combined administration of IL-18 and Apoptin. Cancer Immunol. Immunother. 2007, 56, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Herzyk, D.J.; Bugelski, P.J.; Hart, T.K.; Wier, P.J. Preclinical safety of recombinant human interleukin-18. Toxicol. Pathol. 2003, 31, 554–561. [Google Scholar] [CrossRef] [PubMed]
- Sozen, S.; Coskun, U.; Sancak, B.; Bukan, N.; Gunel, N.; Tunc, L.; Bozkirli, I. Serum levels of interleukin-18 and nitrite+nitrate in renal cell carcinoma patients with different tumor stage and grade. Neoplasma 2004, 51, 25–29. [Google Scholar] [PubMed]
- Jia, Y.; Zang, A.; Jiao, S.; Chen, S.; Yan, F. The interleukin-18 gene promoter -607 A/C polymorphism contributes to non-small-cell lung cancer risk in a Chinese population. Onco. Targets. Ther. 2016, 9, 1715–1719. [Google Scholar] [CrossRef]
- Xu, L.; Zhu, Y.; An, H.; Liu, Y.; Lin, Z.; Wang, G.; Xu, J. Clinical significance of tumor-derived IL-1β and IL-18 in localized renal cell carcinoma: Associations with recurrence and survival. Urol. Oncol. 2015, 33, 68.e9–68.e16. [Google Scholar] [CrossRef]
- Yueh, T.C.; Wu, C.N.; Hung, Y.W.; Chang, W.S.; Fu, C.K.; Pei, J.S.; Wu, M.H.; Lai, Y.L.; Lee, Y.M.; Yen, S.T.; et al. The Contribution of MMP-7 Genotypes to Colorectal Cancer Susceptibility in Taiwan. Cancer Genomics Proteomics 2018, 15, 207–212. [Google Scholar] [CrossRef]
- Shen, T.C.; Chang, W.S.; Tsai, C.W.; Chao, C.Y.; Lin, Y.T.; Hsiao, C.L.; Hsu, C.L.; Chen, W.C.; Hsia, T.C.; Bau, D.T. The Contribution of Matrix Metalloproteinase-1 Promoter Genotypes in Taiwan Lung Cancer Risk. Anticancer Res. 2018, 38, 253–257. [Google Scholar]
- Huang, C.Y.; Chang, W.S.; Tsai, C.W.; Hsia, T.C.; Shen, T.C.; Bau, D.T.; Shui, H.A. Interleukin-18 promoter genotype is associated with the risk of nasopharyngeal carcinoma in Taiwan. Cancer Manag. Res. 2018, 10, 5199–5207. [Google Scholar] [CrossRef] [PubMed]
- Folwaczny, M.; Glas, J.; Torok, H.P.; Tonenchi, L.; Paschos, E.; Bauer, B.; Limbersky, O.; Folwaczny, C. Polymorphisms of the interleukin-18 gene in periodontitis patients. J. Clin. Periodontol. 2005, 32, 530–534. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Cases (n = 92) | Controls (n = 580) | p-Value | |||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Age (year) (mean ± SD) | 58.8 ± 11.7 | 58.3 ± 11.5 | 0.8971 | |||
| ≤60 | 47 | 51.1% | 307 | 52.9% | 0.8223 | |
| >60 | 45 | 48.9% | 273 | 47.1% | ||
| Gender | ||||||
| Male | 59 | 64.1% | 371 | 64.0% | 1.0000 | |
| Female | 33 | 35.9% | 209 | 36.0% | ||
| Smoking status | ||||||
| Smokers | 41 | 44.6% | 220 | 37.9% | 0.2499 | |
| Non-smokers | 51 | 55.4% | 360 | 62.1% | ||
| Alcohol drinking status | ||||||
| Drinkers | 37 | 40.2% | 209 | 36.0% | 0.4848 | |
| Non-drinkers | 55 | 59.8% | 371 | 64.0% | ||
| Hypertension | ||||||
| Yes | 61 | 66.3% | 302 | 52.1% | 0.0130 * | |
| No | 31 | 33.7% | 278 | 47.9% | ||
| Diabetes | ||||||
| Yes | 21 | 22.8% | 104 | 17.9% | 0.2523 | |
| No | 71 | 77.2% | 476 | 82.1% | ||
| Family cancer history | ||||||
| Yes | 6 | 6.5% | 17 | 2.9% | 0.1125 | |
| No | 86 | 93.5% | 563 | 97.1% | ||
| Histological types | ||||||
| Clear cell | 71 | 77.2% | ||||
| Non-clear cell | 21 | 22.8% | ||||
| Histological grades | ||||||
| Low | 48 | 52.2% | ||||
| Middle and high | 44 | 47.8% | ||||
| Genotypes | Controls | Patients | OR (95% CI) a | aOR (95% CI) a | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||||||
| IL-18 -656 | |||||||||||
| AA | 221 | 38.1% | 32 | 34.8% | 1.00 (Reference) | 1.00 (Reference) | |||||
| AC | 252 | 43.5% | 44 | 47.8% | 1.21 (0.74–1.97) | 1.20 (0.69–1.84) | 0.4535 | ||||
| CC | 107 | 18.4% | 16 | 17.4% | 1.03 (0.54–1.96) | 1.04 (0.52–1.93) | 0.9218 | ||||
| Ptrend | 0.7311 | ||||||||||
| Carrier comparison | |||||||||||
| AA + AC | 473 | 81.6% | 76 | 82.6% | 1.00 (Reference) | 1.00 (Reference) | |||||
| CC | 107 | 18.4% | 16 | 17.4% | 0.93 (0.52–1.66) | 0.96 (0.56–1.46) | 0.8076 | ||||
| AA | 221 | 38.1% | 32 | 34.8% | 1.00 (Reference) | 1.00 (Reference) | |||||
| AC + CC | 359 | 61.9% | 60 | 65.2% | 1.15 (0.73–1.83) | 1.12 (0.70–1.79) | 0.5414 | ||||
| IL-18 -607 | |||||||||||
| AA | 144 | 24.8% | 41 | 44.6% | 1.00 (Reference) | 1.00 (Reference) | |||||
| AC | 294 | 50.7% | 37 | 40.2% | 0.44 (0.27–0.72) | 0.41 (0.22–0.64) | 0.0008 * | ||||
| CC | 142 | 24.5% | 14 | 15.2% | 0.35 (0.18–0.66) | 0.33 (0.15–0.58) | 0.0010 * | ||||
| Ptrend | 0.0004 * | ||||||||||
| Carrier comparison | |||||||||||
| AA + AC | 438 | 75.5% | 78 | 84.8% | 1.00 (Reference) | 1.00 (Reference) | |||||
| CC | 142 | 24.5% | 14 | 15.2% | 0.55 (0.30-1.00) | 0.51 (0.32–0.96) | 0.0505 | ||||
| AA | 144 | 24.8% | 41 | 44.6% | 1.00 (Reference) | 1.00 (Reference) | |||||
| AC + CC | 436 | 75.2% | 51 | 55.4% | 0.41 (0.26–0.65) | 0.39 (0.25–0.66) | 0.0001 * | ||||
| IL-18 -137 | |||||||||||
| GG | 463 | 79.8% | 72 | 78.3% | 1.00 (Reference) | 1.00 (Reference) | |||||
| GC | 108 | 18.6% | 18 | 19.5% | 1.07 (0.61-1.87) | 1.06 (0.60-1.66) | 0.8074 | ||||
| CC | 9 | 1.6% | 2 | 2.2% | 1.42 (0.30-6.75) | 1.37 (0.35-6.23) | 0.6505 | ||||
| Ptrend | 0.8825 | ||||||||||
| Carrier comparison | |||||||||||
| GG + GC | 571 | 98.4% | 90 | 97.8% | 1.00 (Reference) | 1.00 (Reference) | |||||
| CC | 9 | 1.6% | 2 | 2.2% | 1.41 (0.30-6.63) | 1.38 (0.32-5.98) | 0.6622 | ||||
| GG | 463 | 79.8% | 72 | 78.3% | 1.00 (Reference) | 1.00 (Reference) | |||||
| GC + CC | 117 | 20.2% | 20 | 21.7% | 1.10 (0.64-1.88) | 1.10 (0.65-1.85) | 0.7289 | ||||
| Allele | Controls n (%) | Patients n (%) | aOR (95% CI) a | p-Value |
|---|---|---|---|---|
| IL-18 -656 | ||||
| G | 694 (59.8%) | 108 (58.7%) | 1.00 (Reference) | |
| T | 466 (40.2%) | 76 (41.3%) | 1.06 (0.73-1.31) | 0.7712 |
| IL-18 -607 | ||||
| A | 582 (50.2%) | 119 (64.7%) | 1.00 (Reference) | |
| C | 578 (49.8%) | 65 (35.3%) | 0.53 (0.35-0.71) | 0.0003 * |
| IL-18 -137 | ||||
| G | 1034 (89.1%) | 162 (88.0%) | 1.00 (Reference) | |
| C | 126 (10.9%) | 22 (12.0%) | 1.11 (0.69-1.83) | 0.6595 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, W.-S.; Shen, T.-C.; Yeh, W.-L.; Yu, C.-C.; Lin, H.-Y.; Wu, H.-C.; Tsai, C.-W.; Bau, D.-T. Contribution of Inflammatory Cytokine Interleukin-18 Genotypes to Renal Cell Carcinoma. Int. J. Mol. Sci. 2019, 20, 1563. https://doi.org/10.3390/ijms20071563
Chang W-S, Shen T-C, Yeh W-L, Yu C-C, Lin H-Y, Wu H-C, Tsai C-W, Bau D-T. Contribution of Inflammatory Cytokine Interleukin-18 Genotypes to Renal Cell Carcinoma. International Journal of Molecular Sciences. 2019; 20(7):1563. https://doi.org/10.3390/ijms20071563
Chicago/Turabian StyleChang, Wen-Shin, Te-Chun Shen, Wei-Lan Yeh, Chien-Chih Yu, Hui-Yi Lin, Hsi-Chin Wu, Chia-Wen Tsai, and Da-Tian Bau. 2019. "Contribution of Inflammatory Cytokine Interleukin-18 Genotypes to Renal Cell Carcinoma" International Journal of Molecular Sciences 20, no. 7: 1563. https://doi.org/10.3390/ijms20071563
APA StyleChang, W.-S., Shen, T.-C., Yeh, W.-L., Yu, C.-C., Lin, H.-Y., Wu, H.-C., Tsai, C.-W., & Bau, D.-T. (2019). Contribution of Inflammatory Cytokine Interleukin-18 Genotypes to Renal Cell Carcinoma. International Journal of Molecular Sciences, 20(7), 1563. https://doi.org/10.3390/ijms20071563





