Kinetics of Physiological and Behavioural Responses in Endotoxemic Pigs with or without Dexamethasone Treatment
Abstract
1. Introduction
2. Results
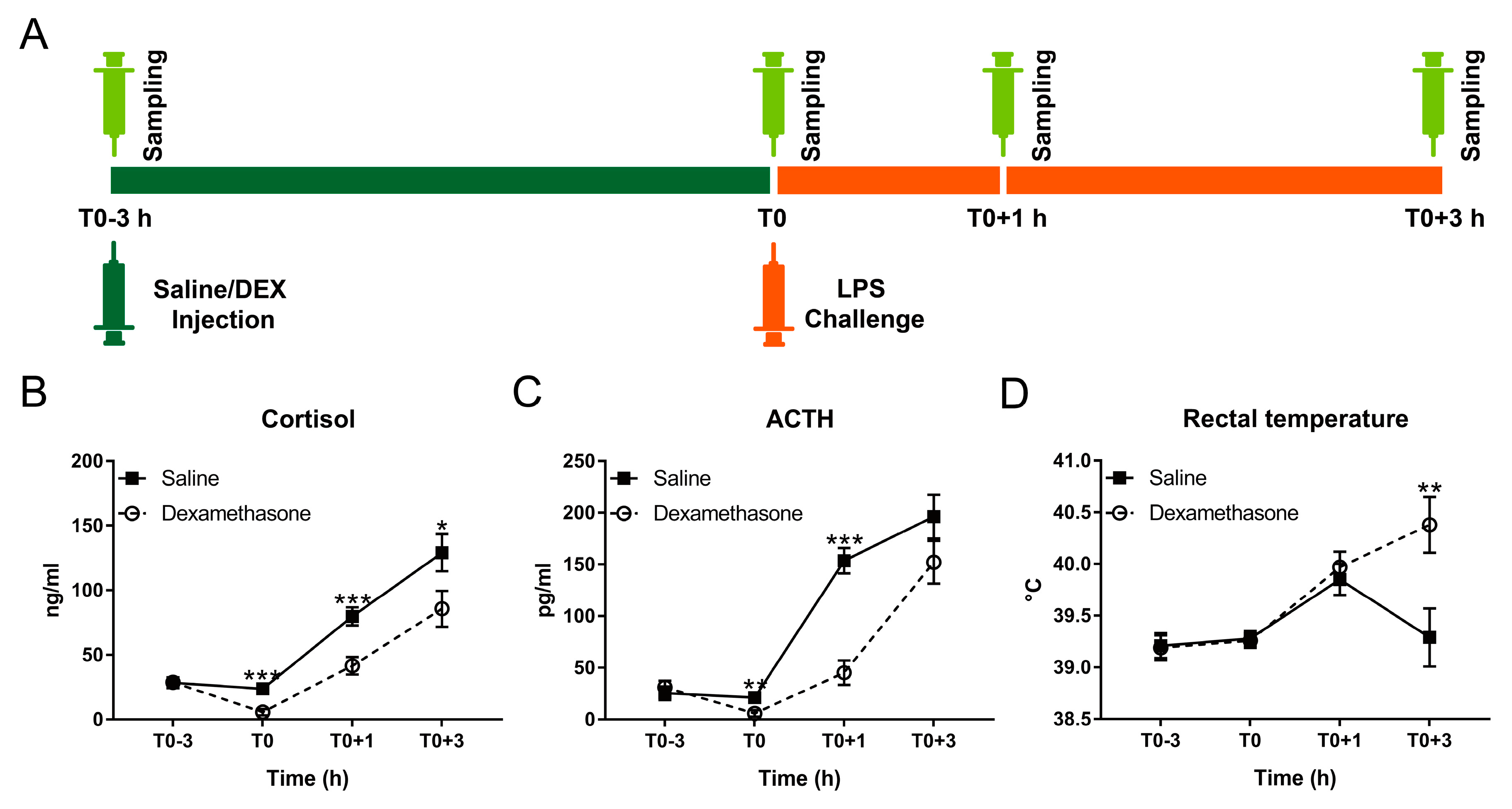
2.1. DEX Diminished LPS-Induced Neuroendocrine Response
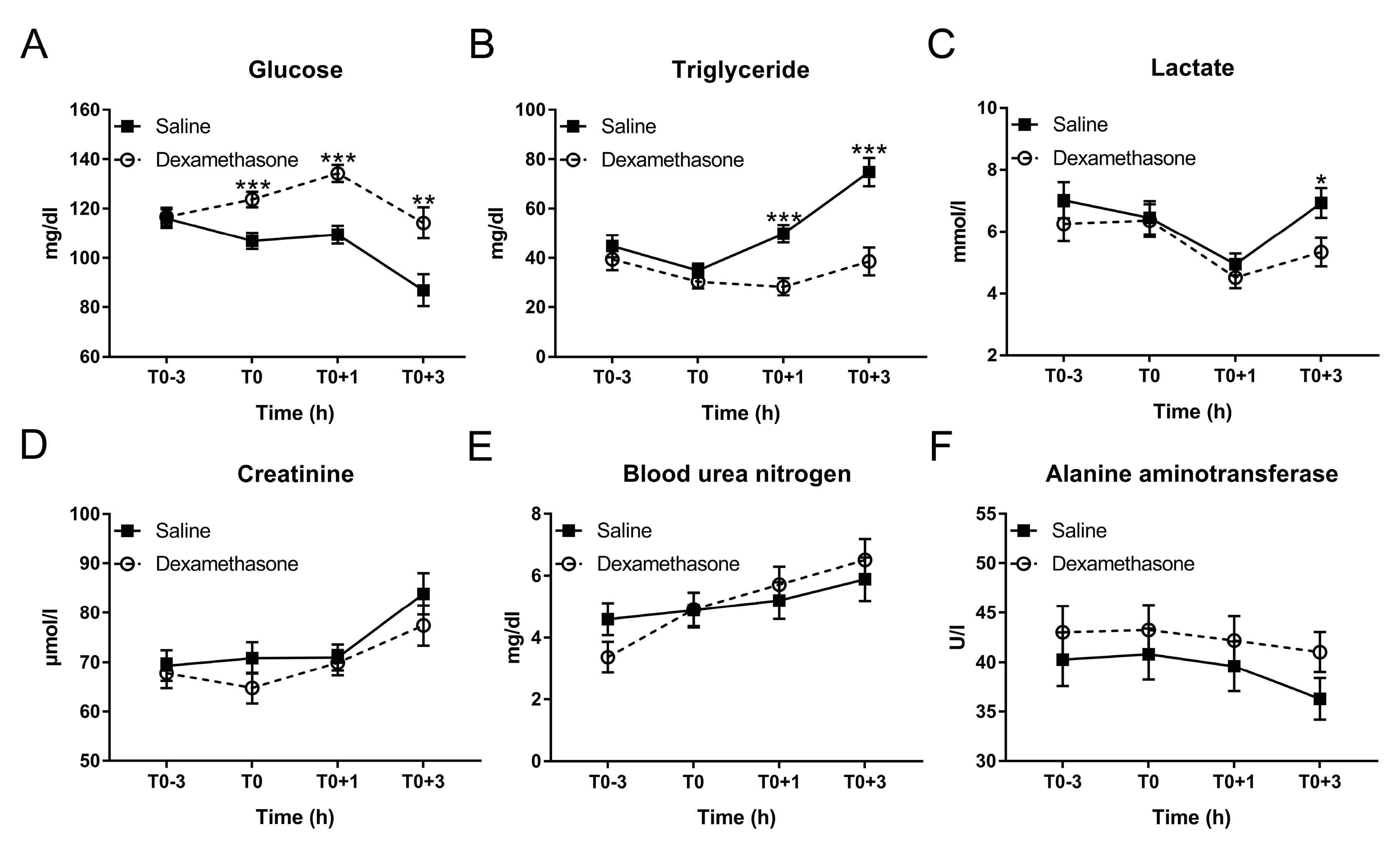
2.2. DEX Altered Glucose and Triglyceride Metabolism during Inflammation
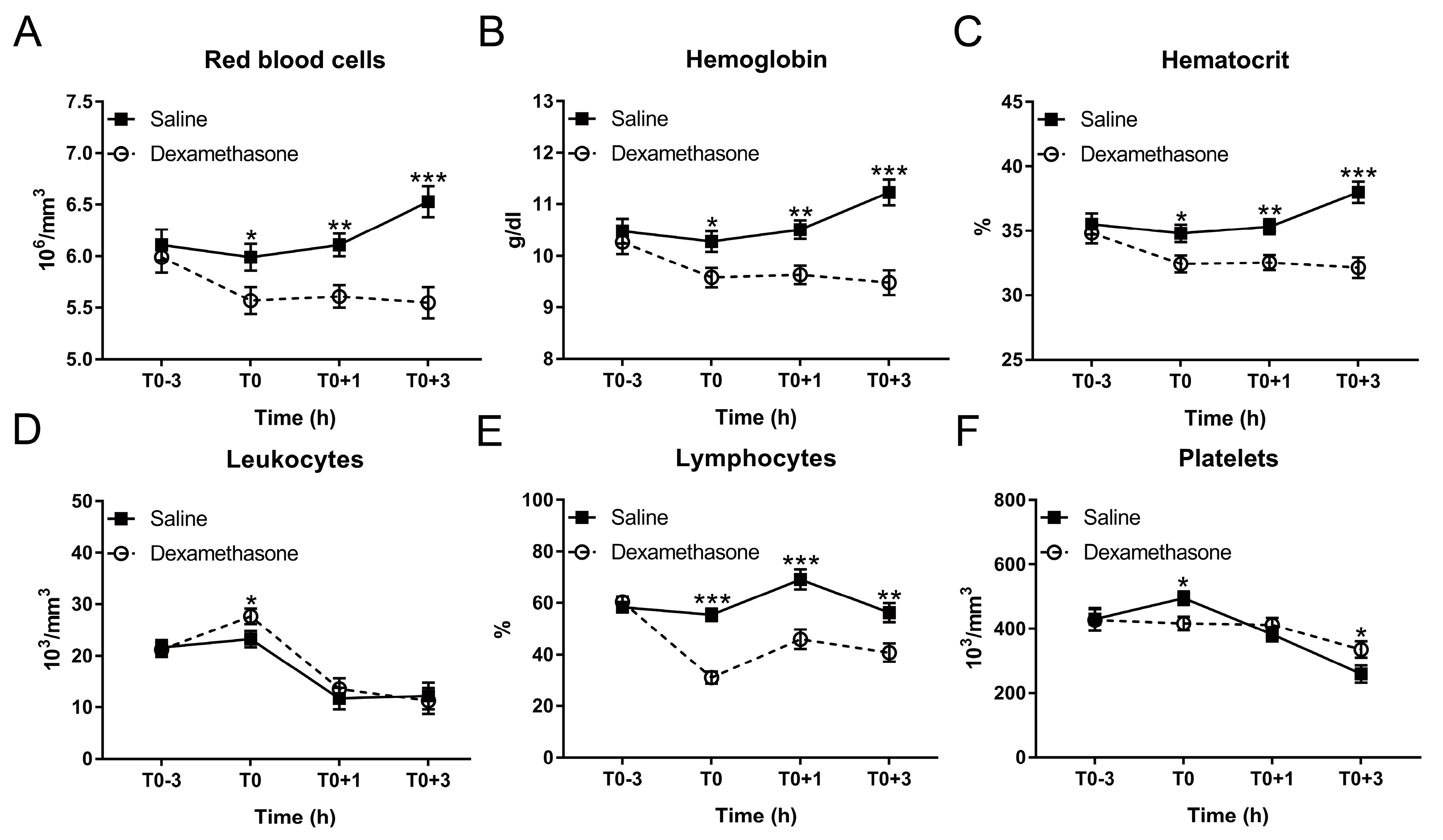
2.3. DEX Blocked LPS-Induced Hematological Response in Varying Degrees
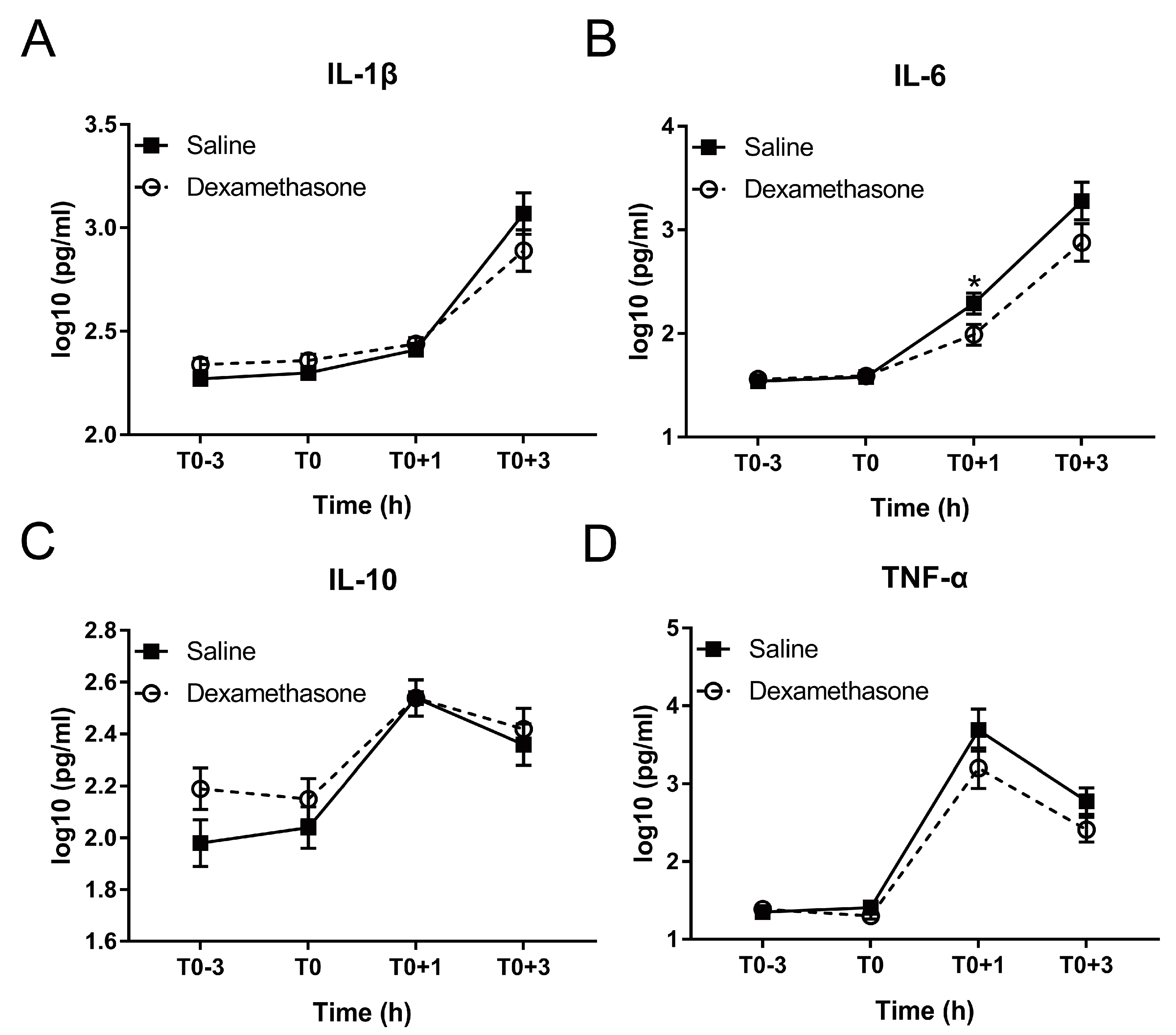
2.4. DEX Relieved LPS-Induced Systemic Inflammation
2.5. DEX Alleviated LPS-Induced Sickness Symptoms
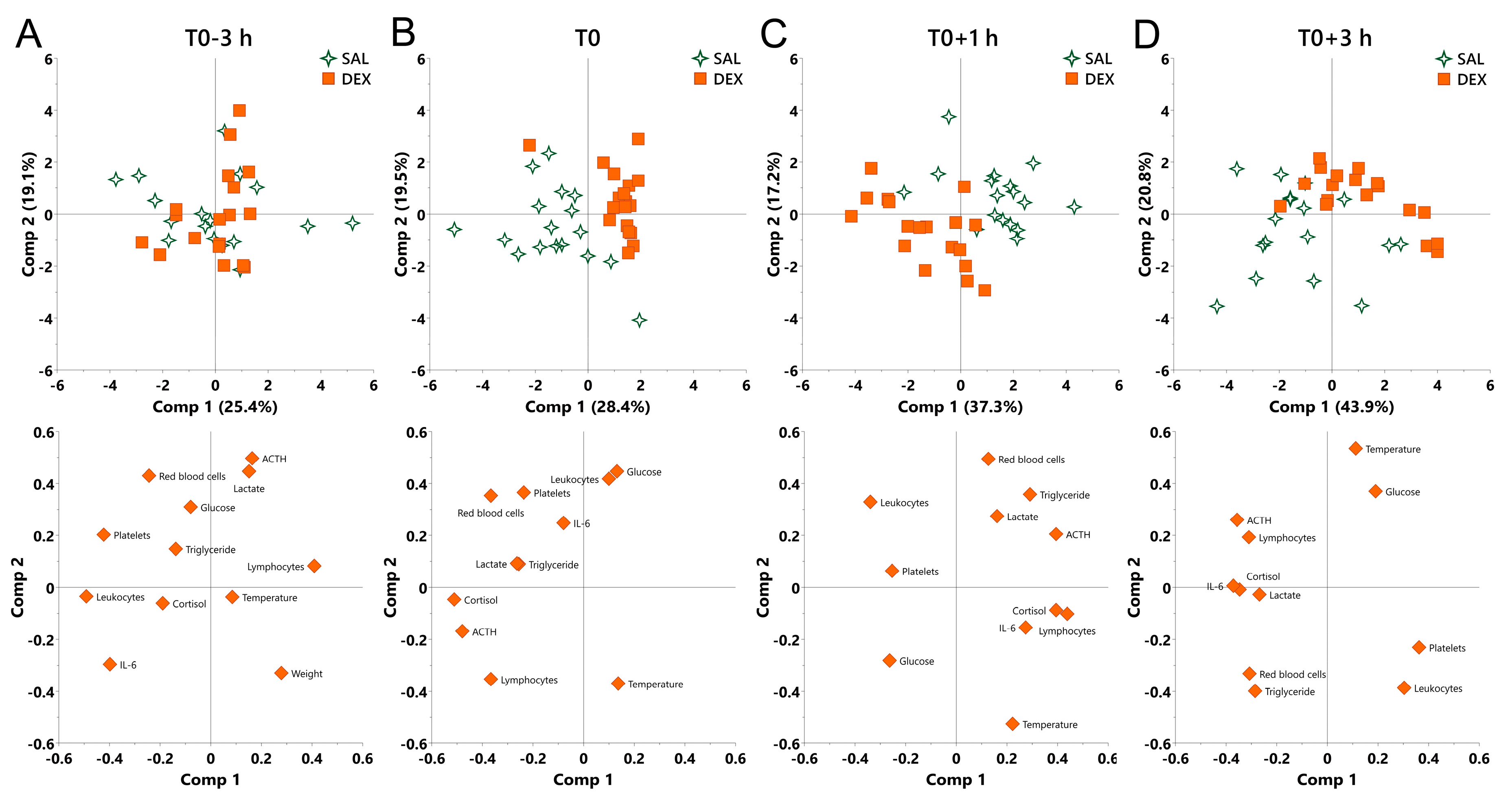
2.6. The Overall Effect of DEX on Physiological Responses in Normal and Endotoxemic Pigs
3. Discussion
4. Materials and Methods
4.1. Animals, Combined DEX/LPS Challenge, and Sampling
4.2. Measurement of Neuroendocrine Parameters
4.3. Measurement of Biochemical Parameters
4.4. Measurement of Hematological Parameters
4.5. Measurement of Inflammation-Associated Cytokines
4.6. Behavioural Observation
4.7. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| DEX | Dexamethasone |
| LPS | Lipopolysaccharide |
| PCA | Principal component analysis |
| GCs | Glucocorticoids |
| HPA | Hypothalamus-pituitary-adrenal |
| ACTH | Adrenocorticotropic hormone |
| BUN | Blood urea nitrogen |
| ALT | Alanine aminotransferase |
References
- Dendoncker, K.; Libert, C. Glucocorticoid resistance as a major drive in sepsis pathology. Cytokine Growth Factor Rev. 2017, 35, 85–96. [Google Scholar] [CrossRef]
- Zen, M.; Canova, M.; Campana, C.; Bettio, S.; Nalotto, L.; Rampudda, M.; Ramonda, R.; Iaccarino, L.; Doria, A. The kaleidoscope of glucorticoid effects on immune system. Autoimmun. Rev. 2011, 10, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Beishuizen, A.; Thijs, L.G. Endotoxin and the hypothalamo-pituitary-adrenal (HPA) axis. J. Endotoxin Res. 2003, 9, 3–24. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, D.; Dirikolu, L.; Hoenig, M. Glucocorticoids, mineralocorticoids and adrenolytic drugs. In Veterinary Pharmacology and Therapeutics; Wiley-Blackwell: Ames, IA, USA, 2009; pp. 771–802. [Google Scholar]
- Myers, M.J.; Farrell, D.E.; Palmer, D.C.; Post, L.O. Inflammatory mediator production in swine following endotoxin challenge with or without co-administration of dexamethasone. Int. Immunopharmacol. 2003, 3, 571–579. [Google Scholar] [CrossRef]
- Heming, N.; Sivanandamoorthy, S.; Meng, P.; Bounab, R.; Annane, D. Immune Effects of Corticosteroids in Sepsis. Front. Immunol. 2018, 9, 1736. [Google Scholar] [CrossRef] [PubMed]
- Wyns, H.; Meyer, E.; Watteyn, A.; Plessers, E.; De Baere, S.; De Backer, P.; Croubels, S. Pharmacokinetics of dexamethasone after intravenous and intramuscular administration in pigs. Vet. J. 2013, 198, 286–288. [Google Scholar] [CrossRef] [PubMed]
- Tenenbaum, T.; Matalon, D.; Adam, R.; Seibt, A.; Wewer, C.; Schwerk, C.; Galla, H.J.; Schroten, H. Dexamethasone prevents alteration of tight junction-associated proteins and barrier function in porcine choroid plexus epithelial cells after infection with Streptococcus suis in vitro. Brain Res. 2008, 1229, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Wooten, H.; McGlone, J.J.; Wachtel, M.; Thompson, G.; Rakhshandeh, A.R.; Rakhshandeh, A. A glucocorticoid receptor agonist improves post-weaning growth performance in segregated early-weaned pigs. Animal 2019. [Google Scholar] [CrossRef] [PubMed]
- Hicks, C.W.; Sweeney, D.A.; Danner, R.L.; Eichacker, P.Q.; Suffredini, A.F.; Feng, J.; Sun, J.; Behrend, E.N.; Solomon, S.B.; Natanson, C. Efficacy of selective mineralocorticoid and glucocorticoid agonists in canine septic shock. Crit. Care Med. 2012, 40, 199–207. [Google Scholar] [CrossRef]
- Jia, M.; Deng, C.; Luo, J.; Zhang, P.; Sun, X.; Zhang, Z.; Gong, T. A novel dexamethasone-loaded liposome alleviates rheumatoid arthritis in rats. Int. J. Pharm. 2018, 540, 57–64. [Google Scholar] [CrossRef]
- Flaming, K.; Goff, B.; Frank, D.; Roth, J. Pigs are relatively resistant to dexamethasone induced immunosuppression. Comp. Haematol. Int. 1994, 4, 218–225. [Google Scholar] [CrossRef]
- Pruett, J.; Fisher, W.; Deloach, J. Effects of dexamethasone on selected parameters of the bovine immune system. Vet. Res. Commun. 1987, 11, 305–323. [Google Scholar]
- Wyns, H.; Plessers, E.; De Backer, P.; Meyer, E.; Croubels, S. In vivo porcine lipopolysaccharide inflammation models to study immunomodulation of drugs. Vet. Immunol. Immunopathol. 2015, 166, 58–69. [Google Scholar] [CrossRef]
- Kanitz, E.; Tuchscherer, M.; Tuchscherer, A.; Stabenow, B.; Manteuffel, G. Neuroendocrine and immune responses to acute endotoxemia in suckling and weaned piglets. Neonatology 2002, 81, 203–209. [Google Scholar] [CrossRef]
- Direk, N.; Dekker, M.J.; Luik, A.I.; Kirschbaum, C.; de Rijke, Y.B.; Hofman, A.; Hoogendijk, W.J.; Tiemeier, H. The Very Low-Dose Dexamethasone Suppression Test in the General Population: A Cross-Sectional Study. PLoS ONE 2016, 11, e0164348. [Google Scholar] [CrossRef]
- Donn, R.; Berry, A.; Stevens, A.; Farrow, S.; Betts, J.; Stevens, R.; Clayton, C.; Wang, J.; Warnock, L.; Worthington, J.; et al. Use of gene expression profiling to identify a novel glucocorticoid sensitivity determining gene, BMPRII. FASEB J. 2007, 21, 402–414. [Google Scholar] [CrossRef]
- Murani, E.; Ponsuksili, S.; Jaeger, A.; Gorres, A.; Tuchscherer, A.; Wimmers, K. A naturally hypersensitive glucocorticoid receptor elicits a compensatory reduction of hypothalamus-pituitary-adrenal axis activity early in ontogeny. Open Biol. 2016, 6. [Google Scholar] [CrossRef]
- Silverman, M.N.; Mukhopadhyay, P.; Belyavskaya, E.; Tonelli, L.H.; Revenis, B.D.; Doran, J.H.; Ballard, B.E.; Tam, J.; Pacher, P.; Sternberg, E.M. Glucocorticoid receptor dimerization is required for proper recovery of LPS-induced inflammation, sickness behaviour and metabolism in mice. Mol. Psychiatry 2013, 18, 1006–1017. [Google Scholar] [CrossRef]
- Colditz, I.G.; Hine, B.C. Resilience in farm animals: Biology, management, breeding and implications for animal welfare. Anim. Prod. Sci. 2016, 56. [Google Scholar] [CrossRef]
- Taff, C.C.; Zimmer, C.; Vitousek, M.N. Efficacy of negative feedback in the HPA axis predicts recovery from acute challenges. Biol. Lett. 2018, 14. [Google Scholar] [CrossRef]
- Liu, Z.; Liu, W.; Huang, Y.; Guo, J.; Zhao, R.; Yang, X. Lipopolysaccharide significantly influences the hepatic triglyceride metabolism in growing pigs. Lipids Health Dis. 2015, 14, 64. [Google Scholar] [CrossRef]
- Perri, A.M.; O’Sullivan, T.L.; Harding, J.C.; Wood, R.D.; Friendship, R.M. Hematology and biochemistry reference intervals for Ontario commercial nursing pigs close to the time of weaning. Can. Vet. J. 2017, 58, 371. [Google Scholar]
- Steven, S.; Jurk, K.; Kopp, M.; Kroller-Schon, S.; Mikhed, Y.; Schwierczek, K.; Roohani, S.; Kashani, F.; Oelze, M.; Klein, T.; et al. Glucagon-like peptide-1 receptor signalling reduces microvascular thrombosis, nitro-oxidative stress and platelet activation in endotoxaemic mice. Br. J. Pharmacol. 2017, 174, 1620–1632. [Google Scholar] [CrossRef]
- Steven, S.; Dib, M.; Roohani, S.; Kashani, F.; Munzel, T.; Daiber, A. Time Response of Oxidative/Nitrosative Stress and Inflammation in LPS-Induced Endotoxaemia-A Comparative Study of Mice and Rats. Int. J. Mol. Sci. 2017, 18, 2176. [Google Scholar] [CrossRef]
- Dantzer, R.; O’Connor, J.C.; Freund, G.G.; Johnson, R.W.; Kelley, K.W. From inflammation to sickness and depression: When the immune system subjugates the brain. Nat. Rev. Neurosci. 2008, 9, 46–56. [Google Scholar] [CrossRef]
- Remick, D.; Manohar, P.; Bolgos, G.; Rodriguez, J.; Moldawer, L.; Wollenberg, G. Blockade of tumor necrosis factor reduces lipopolysaccharide lethality, but not the lethality of cecal ligation and puncture. Shock 1995, 4, 89–95. [Google Scholar] [CrossRef]
- Paragliola, R.M.; Papi, G.; Pontecorvi, A.; Corsello, S.M. Treatment with Synthetic Glucocorticoids and the Hypothalamus-Pituitary-Adrenal Axis. Int. J. Mol. Sci. 2017, 18, 2201. [Google Scholar] [CrossRef]
- Silverman, M.N.; Pearce, B.D.; Biron, C.A.; Miller, A.H. Immune modulation of the hypothalamic-pituitary-adrenal (HPA) axis during viral infection. Viral Immunol. 2005, 18, 41–78. [Google Scholar] [CrossRef]
- Sun, H.; Huang, Y.; Yin, C.; Guo, J.; Zhao, R.; Yang, X. Lipopolysaccharide markedly changes glucose metabolism and mitochondrial function in the longissimus muscle of pigs. Animal 2016, 10, 1204–1212. [Google Scholar] [CrossRef]
- Xie, M.; Yu, Y.; Kang, R.; Zhu, S.; Yang, L.; Zeng, L.; Sun, X.; Yang, M.; Billiar, T.R.; Wang, H.; et al. PKM2-dependent glycolysis promotes NLRP3 and AIM2 inflammasome activation. Nat. Commun. 2016, 7, 13280. [Google Scholar] [CrossRef]
- Bekpinar, S.; Develi-Is, S.; Unlucerci, Y.; Kusku-Kiraz, Z.; Uysal, M.; Gurdol, F. Modulation of arginine and asymmetric dimethylarginine concentrations in liver and plasma by exogenous hydrogen sulfide in LPS-induced endotoxemia. Can. J. Physiol. Pharmacol. 2013, 91, 1071–1075. [Google Scholar] [CrossRef]
- Hui, S.; Ghergurovich, J.M.; Morscher, R.J.; Jang, C.; Teng, X.; Lu, W.; Esparza, L.A.; Reya, T.; Le, Z.; Yanxiang Guo, J.; et al. Glucose feeds the TCA cycle via circulating lactate. Nature 2017, 551, 115–118. [Google Scholar] [CrossRef]
- Feingold, K.R.; Staprans, I.; Memon, R.; Moser, A.; Shigenaga, J.; Doerrler, W.; Dinarello, C.; Grunfeld, C. Endotoxin rapidly induces changes in lipid metabolism that produce hypertriglyceridemia: Low doses stimulate hepatic triglyceride production while high doses inhibit clearance. J. Lipid Res. 1992, 33, 1765–1776. [Google Scholar]
- Macfarlane, D.P.; Forbes, S.; Walker, B.R. Glucocorticoids and fatty acid metabolism in humans: Fuelling fat redistribution in the metabolic syndrome. J. Endocrinol. 2008, 197, 189–204. [Google Scholar] [CrossRef]
- Peckett, A.J.; Wright, D.C.; Riddell, M.C. The effects of glucocorticoids on adipose tissue lipid metabolism. Metabolism 2011, 60, 1500–1510. [Google Scholar] [CrossRef]
- Chen, Y.; Du, Y.; Li, Y.; Wang, X.; Gao, P.; Yang, G.; Fang, Y.; Meng, Y.; Zhao, X. Panaxadiol Saponin and Dexamethasone Improve Renal Function in Lipopolysaccharide-Induced Mouse Model of Acute Kidney Injury. PLoS ONE 2015, 10, e0134653. [Google Scholar] [CrossRef]
- Webel, D.; Finck, B.; Baker, D.; Johnson, R. Time course of increased plasma cytokines, cortisol, and urea nitrogen in pigs following intraperitoneal injection of lipopolysaccharide. J. Anim. Sci. 1997, 75, 1514–1520. [Google Scholar] [CrossRef]
- Wang, L.; Hou, Y.; Yi, D.; Li, Y.; Ding, B.; Zhu, H.; Liu, J.; Xiao, H.; Wu, G. Dietary supplementation with glutamate precursor alpha-ketoglutarate attenuates lipopolysaccharide-induced liver injury in young pigs. Amino Acids 2015, 47, 1309–1318. [Google Scholar] [CrossRef]
- Sautron, V.; Terenina, E.; Gress, L.; Lippi, Y.; Billon, Y.; Larzul, C.; Liaubet, L.; Villa-Vialaneix, N.; Mormede, P. Time course of the response to ACTH in pig: Biological and transcriptomic study. BMC Genom. 2015, 16, 961. [Google Scholar] [CrossRef]
- Lv, Y.; Kim, K.; Sheng, Y.; Cho, J.; Qian, Z.; Zhao, Y.Y.; Hu, G.; Pan, D.; Malik, A.B.; Hu, G. YAP Controls Endothelial Activation and Vascular Inflammation Through TRAF6. Circ. Res. 2018, 123, 43–56. [Google Scholar] [CrossRef]
- Ventrella, D.; Dondi, F.; Barone, F.; Serafini, F.; Elmi, A.; Giunti, M.; Romagnoli, N.; Forni, M.; Bacci, M.L. The biomedical piglet: Establishing reference intervals for haematology and clinical chemistry parameters of two age groups with and without iron supplementation. BMC Vet. Res. 2017, 13, 23. [Google Scholar] [CrossRef]
- Ricci, E.; Ronchetti, S.; Pericolini, E.; Gabrielli, E.; Cari, L.; Gentili, M.; Roselletti, E.; Migliorati, G.; Vecchiarelli, A.; Riccardi, C. Role of the glucocorticoid-induced leucine zipper gene in dexamethasone-induced inhibition of mouse neutrophil migration via control of annexin A1 expression. FASEB J. 2017, 31, 3054–3065. [Google Scholar] [CrossRef]
- Nakagawa, M.; Terashima, T.; D’yachkova, Y.; Bondy, G.P.; Hogg, J.C.; van Eeden, S.F. Glucocorticoid-induced granulocytosis: Contribution of marrow release and demargination of intravascular granulocytes. Circulation 1998, 98, 2307–2313. [Google Scholar] [CrossRef]
- Xiang, B.; Zhang, G.; Guo, L.; Li, X.-A.; Morris, A.J.; Daugherty, A.; Whiteheart, S.W.; Smyth, S.S.; Li, Z. Platelets protect from septic shock by inhibiting macrophage-dependent inflammation via the cyclooxygenase 1 signalling pathway. Nat. Commun. 2013, 4. [Google Scholar] [CrossRef]
- Bedet, A.; Razazi, K.; Boissier, F.; Surenaud, M.; Hue, S.; Giraudier, S.; Brun-Buisson, C.; Mekontso Dessap, A. Mechanisms of Thrombocytopenia During Septic Shock: A Multiplex Cluster Analysis of Endogenous Sepsis Mediators. Shock 2018, 49, 641–648. [Google Scholar] [CrossRef]
- de Stoppelaar, S.F.; van’t Veer, C.; van der Poll, T. The role of platelets in sepsis. Thromb. Haemost. 2014, 112, 666–677. [Google Scholar] [CrossRef]
- Brakkee, J.; Dreteler, G.; Bouma, B.; Jansen, J. Dexamethasone affects platelet aggregation and fibrinolytic activity in rats at different doses which is reflected by their effect on arterial thrombosis. Blood Coagul. Fibrinolysis Int. J. Haemost. Thromb. 1994, 5, 249–255. [Google Scholar]
- Andonegui, G.; Kerfoot, S.M.; McNagny, K.; Ebbert, K.V.; Patel, K.D.; Kubes, P. Platelets express functional Toll-like receptor-4. Blood 2005, 106, 2417–2423. [Google Scholar] [CrossRef]
- Bosmann, M.; Sarma, J.V.; Atefi, G.; Zetoune, F.S.; Ward, P.A. Evidence for anti-inflammatory effects of C5a on the innate IL-17A/IL-23 axis. FASEB J. 2012, 26, 1640–1651. [Google Scholar] [CrossRef]
- Nordgreen, J.; Munsterhjelm, C.; Aae, F.; Popova, A.; Boysen, P.; Ranheim, B.; Heinonen, M.; Raszplewicz, J.; Piepponen, P.; Lervik, A.; et al. The effect of lipopolysaccharide (LPS) on inflammatory markers in blood and brain and on behaviour in individually-housed pigs. Physiol. Behav. 2018, 195, 98–111. [Google Scholar] [CrossRef]
- Alvarez, S.; Vico, T.; Vanasco, V. Cardiac dysfunction, mitochondrial architecture, energy production, and inflammatory pathways: Interrelated aspects in endotoxemia and sepsis. Int. J. Biochem. Cell Biol. 2016, 81, 307–314. [Google Scholar] [CrossRef]
- Wirthgen, E.; Tuchscherer, M.; Otten, W.; Domanska, G.; Wollenhaupt, K.; Tuchscherer, A.; Kanitz, E. Activation of indoleamine 2,3-dioxygenase by LPS in a porcine model. Innate Immun. 2014, 20, 30–39. [Google Scholar] [CrossRef]
- Lehner, P.N. Sampling Methods in Behaviour Research. Poult. Sci. 1992, 71, 643–649. [Google Scholar] [CrossRef]
| Symptoms | Hour after LPS | Saline 1 | Dexamethasone 1 | p-Value |
|---|---|---|---|---|
| Panting | 1st hour | 2.67 ± 0.79 | 1.08 ± 0.80 | 0.849 |
| 2nd hour | 6.29 ± 0.79 | 0.99 ± 0.80 | < 0.001 | |
| 3rd hour | 4.67 ± 0.79 | 0.96 ± 0.80 | 0.030 | |
| 4th hour | 4.22 ± 0.79 | 0.68 ± 0.80 | 0.045 | |
| Overall | 4.46 ± 0.54 | 0.93 ± 0.61 | < 0.001 | |
| Shivering | 1st hour | 2.22 ± 0.92 | 2.14 ± 0.94 | 1.000 |
| 2nd hour | 3.44 ± 0.92 | 6.47 ± 0.94 | 0.307 | |
| 3rd hour | 4.33 ± 0.92 | 6.04 ± 0.94 | 0.896 | |
| 4th hour | 3.44 ± 0.92 | 5.21 ± 0.94 | 0.879 | |
| Overall | 3.36 ± 0.63 | 4.97 ± 0.64 | 0.088 | |
| Vomiting | 1st hour | 0.78 ± 0.14 | 0.20 ± 0.15 | 0.099 |
| 2nd hour | 0.67 ± 0.14 | 0.43 ± 0.15 | 0.940 | |
| 3rd hour | 0.11 ± 0.14 | 0.01 ± 0.15 | 0.990 | |
| 4th hour | 0.01 ± 0.14 | 0.01 ± 0.15 | 1.000 | |
| Overall | 0.39 ± 0.08 | 0.16 ± 0.09 | 0.062 | |
| Cyanosis | 1st hour | 0.01 ± 0.64 | 0.01 ± 0.65 | 1.000 |
| 2nd hour | 1.39 ± 0.64 | 0.01 ± 0.65 | 0.789 | |
| 3rd hour | 2.11 ± 0.64 | 0.01 ± 0.65 | 0.298 | |
| 4th hour | 3.11 ± 0.64 | 0.38 ± 0.65 | 0.071 | |
| Overall | 1.65 ± 0.45 | 0.08 ± 0.46 | 0.024 | |
| Inactivity | 1st hour | 11.11 ± 0.29 | 10.42 ± 0.30 | 0.709 |
| 2nd hour | 11.72 ± 0.29 | 11.35 ± 0.30 | 0.985 | |
| 3rd hour | 11.11 ± 0.29 | 11.39 ± 0.30 | 0.990 | |
| 4th hour | 11.22 ± 0.29 | 11.29 ± 0.30 | 1.000 | |
| Overall | 11.29 ± 0.21 | 11.11 ± 0.21 | 0.548 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Z.; Kanitz, E.; Tuchscherer, M.; Tuchscherer, A.; Metges, C.C.; Trakooljul, N.; Wimmers, K.; Murani, E. Kinetics of Physiological and Behavioural Responses in Endotoxemic Pigs with or without Dexamethasone Treatment. Int. J. Mol. Sci. 2019, 20, 1393. https://doi.org/10.3390/ijms20061393
Li Z, Kanitz E, Tuchscherer M, Tuchscherer A, Metges CC, Trakooljul N, Wimmers K, Murani E. Kinetics of Physiological and Behavioural Responses in Endotoxemic Pigs with or without Dexamethasone Treatment. International Journal of Molecular Sciences. 2019; 20(6):1393. https://doi.org/10.3390/ijms20061393
Chicago/Turabian StyleLi, Zhiwei, Ellen Kanitz, Margret Tuchscherer, Armin Tuchscherer, Cornelia C. Metges, Nares Trakooljul, Klaus Wimmers, and Eduard Murani. 2019. "Kinetics of Physiological and Behavioural Responses in Endotoxemic Pigs with or without Dexamethasone Treatment" International Journal of Molecular Sciences 20, no. 6: 1393. https://doi.org/10.3390/ijms20061393
APA StyleLi, Z., Kanitz, E., Tuchscherer, M., Tuchscherer, A., Metges, C. C., Trakooljul, N., Wimmers, K., & Murani, E. (2019). Kinetics of Physiological and Behavioural Responses in Endotoxemic Pigs with or without Dexamethasone Treatment. International Journal of Molecular Sciences, 20(6), 1393. https://doi.org/10.3390/ijms20061393







