Abstract
The aim of this review is to critically analyze promises and limitations of pharmacological inducers of autophagy against protein misfolding-associated neurodegeneration. Effective therapies against neurodegenerative disorders can be developed by regulating the “self-defense” equipment of neurons, such as autophagy. Through the degradation and recycling of the intracellular content, autophagy promotes neuron survival in conditions of trophic factor deprivation, oxidative stress, mitochondrial and lysosomal damage, or accumulation of misfolded proteins. Autophagy involves the activation of self-digestive pathways, which is different for dynamics (macro, micro and chaperone-mediated autophagy), or degraded material (mitophagy, lysophagy, aggrephagy). All neurodegenerative disorders share common pathogenic mechanisms, including the impairment of autophagic flux, which causes the inability to remove the neurotoxic oligomers of misfolded proteins. Pharmacological activation of autophagy is typically achieved by blocking the kinase activity of mammalian target of rapamycin (mTOR) enzymatic complex 1 (mTORC1), removing its autophagy suppressor activity observed under physiological conditions; acting in this way, rapamycin provided the first proof of principle that pharmacological autophagy enhancement can induce neuroprotection through the facilitation of oligomers’ clearance. The demand for effective disease-modifying strategies against neurodegenerative disorders is currently stimulating the development of a wide number of novel molecules, as well as the re-evaluation of old drugs for their pro-autophagic potential.
1. Introduction
Neurons, as all long-lived cells, must face a ceaseless flow of damage, including reduction of trophic factor production and/or activity, oxidative damage of cytoplasmic structures, and accumulation of lipofuscins and misfolded proteins. Neuronal survival is hence made possible by the correct functioning of several homeostatic systems that allow the recycling of intracellular materials and degradation of malfunctioning structures.
Among these strategies, autophagy plays a crucial role in removing aggregated proteins and damaged organelles, thus promoting the clearance of cytoplasm from triggers of neuronal death. Autophagy is a process that has been highly conserved throughout eukaryote evolution, being present in yeast, plants, animals, and humans, but a full understanding of its exact biological role still represents a major challenge. In humans, autophagy is a main crossroad between health and disease, although the characterization of autophagy-related structures, as well as the genes and proteins that control its progression, derives from studies of adaptive strategies for environmental change in yeasts [1,2,3]. On the other hand, most of the proteins driving starvation-induced autophagy in yeasts have mammalian orthologues that hold similar roles throughout the process.
Three forms of autophagy—micro- and macro-autophagy, and chaperone-mediated autophagy (CMA)—have been described in mammals, according to the structures involved and the dynamics of sequestration of cytoplasm portions [4,5]. While CMA and, to a certain extent, microautophagy cooperate with ubiquitin-proteasome system (UPS) in targeting the degradation of specific proteins, macroautophagy is directed towards the removal of bulky protein aggregates and cytoplasmic bodies. Macroautophagy, often simply called autophagy, is initiated with the formation of the phagophore which is a cup-shaped double-membrane isolation structure whose edges expand, engulfing portions of cytoplasm along with the material committed to degradation. Phagophore closure produces a double-membrane vesicle called autophagosome or amphisome, in the case it receives material from extracellular space through the contribution of endosomes. Microtubules drive autophagosomes and amphisomes to fuse with lysosomes, thus generating single-membrane autolysosomes and autophagolysosomes, respectively [6]; thus, autophagy is completed when the cargo is degraded and its constituents recycled into cytosol. Further heterogeneity in autophagy is based on the targeted material, rather than on the nature of the structures involved; macroautophagy can be specifically targeted to large cytoplasmic protein complexes or entire organelles, such as peroxisomes, mitochondria, lysosomes, endoplasmic reticulum, and nuclei [7,8,9]. Although all these varieties of macroautophagy are conceptually and structurally similar, they involve different subsets of receptor and adaptor proteins. Particularly relevant in the pathogenesis of most neurodegenerative disorders of the central nervous system (CNS), aggrephagy and mitophagy are targeted to sequester aggregates of misfolded proteins and damaged mitochondria, respectively. It is widely accepted that they accomplish a major cytoprotective task in neurons, since defective autophagy is frequently observed in association with neuronal loss and cognitive decline, both in physiological conditions, such as in aging, and in neurodegenerative CNS [10,11].
This review aims to examine the most recent findings about neuroprotective potential of drugs that have been proposed to exert a pro-autophagy activity, focusing on their mechanism of action, efficacy and toxicity. In particular, between December 2018 and January 2019, we searched the PubMed database for “autophagy” and Alzheimer’s disease (AD, 735 entries), Parkinson’s disease (PD, 893), Huntington’s disease (HD, 262), prion diseases (191), or amyotrophic lateral sclerosis (ALS, 377); in particular, we focused our analysis on studies addressing the pharmacological modulation of autophagy as potential treatment for neurodegenerative diseases.
2. Protein Conformational Disorders (PCDs)
AD, PD, HD, ALS, and transmissible spongiform encephalopathies (TSE or prion diseases) are neurodegenerative disorders that differ greatly in terms of etiology, histopathology and clinical presentation. Nevertheless, a recent theory claims that all these neurodegenerative diseases recognize the conformational misfolding of specific proteins, whose function in the brain is often obscure, as a common mechanism of neurotoxicity [12]. Among these disorders, the differences in the mechanisms by which protein misfolding occurs may account for the heterogeneous etiology of the diseases; however, neuronal loss is likely caused by the generation of soluble protein oligomers along the process of aggregation and amyloidogenesis that follows the misfolding [13]. Another important pathogenic event that unifies PCDs and, to a certain extent, also occurs during aging, is represented by autophagy alterations and impaired proteostasis [14]. Efficient proteasome-mediated protein quality control cooperates with autophagy to induce neuroprotection: the former process prevents the generation of misfolded proteins, while the latter allows neurons to reduce their intracellular burden of aggregating oligomers, eliminating damaged intracellular structures [11,15]. A promising outcome of such unifying pathogenic hypothesis regards the possibility to set up a common neuroprotective strategy against several different forms of CNS amyloidosis through the pharmacological enhancement or restoration of the autophagic flow [16].
3. Protein Misfolding Generates Neurotoxic Oligomers
The deposition of amyloid protein as extracellular plaques and fibrils or intracellular bodies, and neurofibrillary tangles are associated with synaptic rarefaction, glial proliferation and neuronal death [17]. This evidence, mainly derived from AD research, underscores the amyloid theory, suggesting that misfolded β-amyloid (Aβ) aggregates represent the AD neurotoxic entity. This hypothesis led to several attempts to develop disease-modifying therapies aimed at removing amyloid aggregates from the brain or the prevention of their maturation. The overall failure of these approaches, together with the observation that increasing the burden of amyloid plaques in the brain can also be associated with healthy aging, led to the amplification and re-modulation of the amyloid theory, rather than a confutation [18]. The most striking hint arises from the observation that brains from AD patients differ from those of non-demented individuals with respect to the number of Aβ peptides in the form of soluble oligomers [19,20]; aggregates of Aβ oligomers have also been described as extracellular cluster at early stages of AD, and precede the detection of amyloid plaques in animal models of the disease [21]. Finally, the emergence of transmissible spongiform encephalopathies (TSEs), or prion diseases, introduced a definitive revolution in the scientific approaches to nearly all proteinopathy-associated neurodegenerative diseases [22]. Prion diseases are progressive neurodegenerative disorders that afflict humans and animals, with sporadic, inherited and acquired modalities; these pathological conditions are associated with an amyloidogenic misfolding of a normal glycoprotein, called cellular prion protein (PrPC), into a protease-insensitive isoform named prion protein Scrapie (PrPSc). Although the associated symptomatology may significantly differ on the basis of the specific brain areas that are primarily involved with PrPSc deposition, there is a spatial and temporal correlation between deposition of PrPSc and synaptic rarefaction, glial reaction and grey matter vacuolation. Different molecular events favor PrPC-PrPSc misfolding and account for the heterogeneity in prion diseases etiology: the conversion can be produced as a rare spontaneous stochastic event, as a consequence of mutations in PrPC-encoding gene, or induced by exogenous PrPSc that forces PrPC misfolding, acting as a template [23,24,25]. Although still not unanimously accepted, this modality of structural alteration is not unique to PrP, but could explain certain self-propagating property of other amyloidogenic proteins associated with different neurodegenerative PCDs of CNS [26,27]. Similarly to all the other proteinopathy-associated neurodegenerative diseases, the emerging theory about the molecular mechanisms of neurotoxicity during TSEs postulates that the process of protein misfolding initiates a path of aggregation that goes through the formation of toxic soluble oligomers responsible of the neuronal degeneration and neuroinflammation [28,29]. The newly acquired physico-chemical properties of the oligomers are the most accredited determinants of their gain-of-toxicity; in particular, the increased hydrophobicity and resistance to proteolysis of the oligomers favors their interaction with cell structures and their propensity to aggregate in the neurons, altering cytoplasmic homeostasis [30,31,32]. In support of this hypothesis, it was demonstrated that neuronal death in all neurodegenerative diseases is associated with the generation of soluble misfolded protein oligomers. Remarkably, the structural refolding of amyloidogenic proteins, even unrelated to disease development, can initiate a similar aggregation process that generates soluble oligomers endowed with neurotoxic properties [13,33]. However, there is relative uncertainty as to the neurotoxic signaling of misfolded oligomers and how they interact with neurons. Synaptic impairment is the most prominent initial alteration observed in proximity of Aβ oligomer deposits, and accounts for the first cognitive impairment in AD [34,35,36,37], although mitochondria and/or lysosome damage have also been described as early pathogens during AD [38,39] and are responsible for neuronal death in experimental models of TSEs [32,40,41,42]. The possibility of non-specific interactions of oligomers with cell structures is suggested by the observation that protein misfolding often produces the exposure of hydrophobic residues that are otherwise buried within the native protein spatial structure, and the degree of hydrophobicity correlates with cytotoxicity [30,31,43,44]. Finally, neuronal damage can also be amplified by the sustained neuroinflammatory response triggered by oligomers’ direct activation of astrocytes and microglia [45,46,47,48,49,50,51]. Therefore, the relative contribution between the intracellular formation and the extracellular deposition of misfolded oligomers in determining neuronal death is unclear. The prominent localization of the aggregates can also vary according to the different diseases and, perhaps, the level of aggregation. While in PD and HD mutant α-synuclein and huntingtin are mainly recovered as intracellular aggregates, in AD and TSEs Aβ peptides and PrPSc are localized in extracellular plaques, although intracellular clusters within the endosomal/lysosomal vesicles have also been described. It has therefore been hypothesized that mature amyloid fibrils and their organization in plaques represent a defensive attempt to remove otherwise neurotoxic soluble oligomers. However, plaques are not just deposits of irreversibly inactivated peptides, but can undergo a continuous dynamic balance of entrapment and release of neurotoxic entities. Thus, amyloidogenic peptides may form aggregates containing insoluble fractions that dynamically cycle with the soluble fraction, which is able to travel from the extracellular space to the cytoplasm. The balance between the accumulation of oligomers in extracellular and intracellular pools of amyloids is derived not only from the dynamic equilibrium between the production inside the cells and their subsequent release, but also from the ability of neuron and glia to take up misfolded peptides from the extracellular space [52,53].
Following the amyloid theory and its more recent developments, world-wide research has been oriented towards developing therapeutic strategies against AD, as well as other PCDs, having as a shared rationale the removal of pathogenic oligomers. To this end, passive, rather than active immunotherapy, is at present under active investigation, and various monoclonal antibodies raised against oligomeric forms of Aβ peptides are currently in phase I and III clinical trials [18], although the initial results are not really promising [54,55]. On the other hand, the pharmacological restoration of cytoplasmic proteostasis is attracting growing interest, as it may represent a “physiological” strategy for preventing the accumulation of and/or removal of toxic oligomers, regardless of the nature of the misfolded proteins or the causes/mechanisms of their misfolding [11,56].
The process of autophagy, the major subject of the present review, can be pharmacologically induced in cellular and animal models of PCDs to induce neuroprotection. In the context of drug repositioning [57,58], a growing number of old and novel drugs, so far placed in human therapy to treat a wide number of pathologies, often unrelated to neurodegeneration, are currently under re-evaluation as autophagy inducers to be introduced as disease-modifying strategies against PCDs of CNS.
4. Cytoplasmic Homeostasis and Neuronal Survival: Loss of Autophagy Efficiency is Associated with Protein Aggregation and Neuronal Loss
Protein quality control in the cells is accomplished by two major, highly interconnected, proteolytic systems: UPS and autophagy [16]. It is estimated that almost 30% of de novo synthesized proteins become substrates for the proteolytic machinery upon covalent binding with ubiquitin. While proteasome- and CMA-dependent degradation targets specific proteins in their monomeric state, the elimination of aggregated protein is mediated by aggrephagy, a specific form of macroautophagy. Given the fundamental role of proteostatic mechanisms in ensuring viability in long-living and post-mitotic cells, it is not surprising that impairment of UPS or autophagy is associated with cognitive decline and neuronal death. In particular, AD, PD, ALS, polyglutaminopathies, and other less common forms of CNS amyloidosis display aggregation of misfolded proteins that can be found as extracellular deposits or intracellular inclusion bodies and aggresomes [59,60]. It should be made clear, however, that the presence of increased autophagosomes in association with misfolded aggregates is not proof of the consequentiality of these conditions, since it does not distinguish whether autophagy imbalance (i.e., increased autophagosome content) is the cause or the effect of protein aggregation. The post-mitotic nature of neurons determines that, along with aging, these cells accumulate sequential damage derived from life-spanning insults [61]. Mitochondria and lysosomes are the organelles that most strikingly develop consequences of aging, with the former increasing in number but decreasing in efficiency with respect to electron chain transport, and the latter being filled with indigestible lipofuscin that impairs their functioning [62,63]. Generally speaking, during the aging process, a progressive reduction of the cellular systems that ensure the maintenance of proteostasis occurs. Specific protein degradation by UPS and CMA is most affected, but macroautophagy, which should function as a salvage bulk cytoplasmic recycler, also becomes less efficient; it has been proposed that intralysosomal lipofuscin burden inhibits their fusion with autophagosomes, reducing autophagy efficiency [64].
AD, the most frequent neurodegenerative disorder, is characterized by extracellular deposition of amyloid plaques and intracellular tangles, composed by aggregated Aβ peptides and hyperphosphorylated protein tau [65], paralleled by a robust activation of lysosomal-mediated proteolysis, albeit displaying defects in execution [38,66,67]. Importantly, studies using cell lines and transgenic mice overexpressing Aβ precursor protein, or mutant forms of presenilin 1 (PS1), show that defective autophagy is an early feature in AD, causing a gradual but persistent accumulation of Aβ and hyperphosphorylated tau [15,66,68,69,70]. Post-mortem electron-microscopy and immunoblotting analysis of AD patient brains show that dystrophic neurons containing neurofibrillary tangles also evidence a high number autophagosomes filled with electron-dense material [71,72]; the amount of insoluble ubiquitinated proteins in conjunction with sequestrosome 1/p62 (SQSTM1/p62) is also significantly increased in AD patient brains when compared with age-matched controls, and positively correlates with the density of extracellular amyloid plaques [15,73,74]. High rates of autophagosome formation are also evident in primary cultures of neurons bearing AD-associated mutations, but, in contrast to wild-type controls, the former show defective proteolysis, similar to what is observed when autophagosome-lysosome fusion is pharmacologically hampered [15].
On these bases, it has been hypothesized that the extent of the age-dependent neuronal loss is directly correlated with the sharp decline in neuronal proteostasis efficiency, causing misfolded protein accumulation and neuronal death, whereas at younger ages this event is prevented by an efficient autophagy flux [61]. Interestingly, the impairment of autophagy-mediated proteostasis, which favors amyloid brain deposition and tau hyperphosphorylation [75], is associated with excessive and steady activation of the mammalian target of rapamycin (mTOR), which is abnormally elevated in AD patients [76].
PD, the second most common neurodegenerative disease, is characterized by the presence of dopaminergic dystrophic neurites in the substantia nigra, in which aggregation of ubiquitinated α-synuclein forms intracellular inclusion named Lewy bodies [77,78]. The most relevant cytoplasmic alterations that may possibly be involved in neuronal death are the accumulation of damaged mitochondria and of α-synuclein aggregates, resulting from exposure to still-undefined environmental toxins, or inherited defects in the enzymatic control of α-synuclein metabolism. Defective mitophagy and CMA have been observed in neuronal cultures bearing PD-associated mutations, in animal models of the disease, and in human PD-affected brains [79,80,81]. Genetic and pharmacological enhancement of autophagy has been able to reduce the amount of α-synuclein aggregates, oxidative damage and increase neuronal viability [82,83]. Analogously to AD and PD, autophagy defects have also been found in other proteinopathies, such as polyglutamine disorders and ALS, in which intraneuronal inclusions are associated with neuronal death [84,85,86].
Significant accumulation of autophagic bodies has been described, along with brain spongiform alterations, in TSEs [87]; in murine models of TSEs, in PrPSc-infected cell lines, or in neuronal cultures treated with misfolded recombinant PrP fragments, an increased number of autophagosomes filled with electron-dense material containing PrPSc was reported. In these studies, the pharmacological activation of autophagy favored the clearance of the autophagosomes altogether, with reduced neurotoxicity. These data suggest that in the presence of intracellular PrPSc accumulation, neurons activate autophagy flux but are unable to complete the process [32,42,88,89]. Incomplete autophagy thus represents a prominent cause of neurotoxicity due to intracellular misfolded protein aggregation.
5. Potentiation of Autophagy as Neurodegenerative Disease Therapy
In the last two decades, several studies have reported the neuroprotective activity of rapamycin, one of the most powerful pro-autophagy agents, in both cellular and animal models of neurodegenerative diseases and, with some limitations, in humans [90]. In neuronal cultures, the toxicity of different amyloidogenic peptides can be counteracted by treatment with rapamycin [15,91,92]. Positive results have also been obtained in animal models bearing age-related, inherited, or neurotoxicity-induced neurodegeneration associated with protein misfolding [91]. The translation of these results into human therapy is highly desirable, since, apart from symptomatic pharmacological treatments, which significantly improve quality of life in PD patients and produce extremely limited cognitive improvement in AD patients, disease-modifying therapies, aimed at slowing down the cognitive and neurological decline in neurodegenerative disorders, are still lacking. Some encouraging results from properly structured clinical trials have been produced treating ALS-affected patients with lithium [93,94] and, more recently, a randomized, placebo-controlled, phase II clinical trial was started to evaluate the efficacy of rapamycin in patients affected by ALS [94]. As a common trait, all these approaches are intended to favor neuronal ability to remove cytoplasmic harmful entities, such as misfolded aggregation-prone proteins, or damaged mitochondria and lysosomes. Particular efforts have been focused on the possibility of repurposing known drugs in the neurodegenerative disease field, on the basis of their ability to stimulate macroautophagy in neurons. This pharmacological approach, distinct from the so-far ineffective current disease-modifying therapies, targeting a common step of neurotoxicity of all CNS degenerative conditions, regardless of the nature of the proteins that are associated with the different diseases, may represent a general therapeutic approach for PCDs, independently from etiology or the specific misfolded protein.
6. Molecular Control of Autophagy
The modulation of autophagic flux involves a complex signaling pathway integration that couples the detection of environmental alterations with functional cell responses, including proliferation, differentiation and, more generally, the maintenance of cytoplasmic homeostasis.
Mammalian target of rapamycin (mTOR) is a Ser/Thr kinase belonging to the family of phosphatidylinositol 3-kinase (PI3K)-related kinase (PIKKs), whose activity restrains constitutive autophagy at a low level when there is a shortage of nutrients or cell stresses, including organelles senescence/damage, and an increase of misfolded aggregation-prone proteins perturbs cytoplasmic homeostasis [95]. mTOR is the central partner of two hetero-oligomeric complexes called mTOR complex 1 (mTORC1) and 2 (mTORC2), which can be distinguished with respect to their protein composition, mechanisms of regulation and biological role. mTORC2 is involved in the prevention of apoptosis, control of glucose metabolism, and cytoskeletal plasticity, while mTORC1 controls cell cycle progression and the extent of autophagic flux in response to environmental changes.
In addition to mTOR, mTORC1 includes the regulatory associated protein of mTOR (RAPTOR), the mammalian lethal with SEC13 protein 8 (mLST8), the inhibitory subunit 40-kDa proline rich AKT substrate (PRAS40), and the DEP domain-containing mTOR interacting protein (DEPTOR) [96]. The best characterized pathway by which mTORC1 regulates autophagy is dependent on the activation of tyrosine kinase growth factor receptors. Their activation elicits class I PI3K activity, with subsequent conversion of phosphatidylinositol 4′,5′-biphosphate (PIP2) into phosphatidylinositol 3,4,5-triphosphate (PIP3). PIP3 recruits the Ser/Thr kinase AKT to the plasmamembrane, where it is phosphorylated and activated by two other kinases (PDK 1 and 2). In turn, AKT phosphorylates and inactivates the tuberous sclerosis complex (TSC) and PRAS40, preventing their inhibitory activity on mTOR [97,98]. Non-phosphorylated TSC2 represses mTOR kinase via the enhancement of GTP hydrolysis to GDP, in the small GTP-binding protein RAS homolog enriched in brain (Rheb), which is expressed on lysosomal membranes; as another small GTPase, Rheb cycles from an inactive GDP-bound to active GTP-bound form that activates mTOR kinase. In addition, PRAS40 directly interacts with and inhibits mTOR. AKT thus induces mTOR activity, blocking the inhibitory pathways regulated by TSC2 and PRAS40 [99]. Thus, in conditions of sufficient availability of trophic factors and energetic supply, a sustained stimulation of the PI3K-AKT pathway will result in the activation of mTOR via the continuous blockade of its inhibitors TSC2 and PRAS40. mTOR kinase sustains the phosphorylation of its downstream effectors p70 ribosomal protein S6 kinase 1 (S6K1) and eukaryotic translation initiation factor 4E (eIF4E)-binding protein 1 (4E-BP1) to promote nucleotide synthesis, ribosome biogenesis, protein synthesis, and cell proliferation. Conversely, trophic factor shortage reduces AKT activity allowing the inhibitory functions of TSC2 and PRAS40, which respectively reduces the amount of GTP-bound Rheb and binds to mTORC1 complex, inhibiting the phosphorylation of mTOR substrates, resulting in the activation of autophagy flux. Another major environmental stress that downregulates energy consumption in cells and stimulates autophagy is the reduction of glucose availability and the consequent increase of ADP/ATP ratio. The increase of AMP and ADP stimulates the activation of AMP-activated protein kinase (AMPK), which blocks mTORC1 activity through direct activation of TSC2 and inhibition of RAPTOR. Moreover, AMPK promotes autophagy downstream of mTORC1 by direct activation of phagophore-forming enzymatic complex unc-51-like kinase (Ulk1)1/2 (UKC), which is considered the initiator of the autophagic cascade. These conditions are the metabolic basis for autophagy activation, and TSC2 is now regarded to be a central station in which environmental nutrient availability or stresses are integrated.
Within the mTORC1 complex, RAPTOR acts as a crucial scaffold unit, allowing mTOR to bind and activate S6K1 and 4EBP1, when PRAS40 is phosphorylated by AKT. Importantly, RAPTOR is also the target of the autophagy inducers sirolimus (rapamycin) and tacrolimus (FK506); these antibiotics interact with a regulatory protein that drives them to RAPTOR to destabilize RAPTOR-dependent downstream mTOR signaling. Rapamycin, in addition to suppressing mTORC1 kinase activity, also induces the dephosphorylation of AMBRA 1, which precedes the activation of ULK and phagophore-forming enzymatic complex UKC and the class III phosphatidylinositol 3-phosphate kinase, both representing the initial steps of autophagy [100,101].
7. Autophagic Structures and Associated Protein Markers
The first autophagic structure to be formed is a cup-shaped double-membrane vesicle, called an isolation membrane or phagophore. According to the analysis of the lipid and protein content, phagophores stem from endoplasmic reticulum, but, for their expansion, receive further contributions from multiple sources, including recycling endosomes, mitochondria, Golgi and lipid droplets [102,103,104,105,106,107]. The entire process of nucleation, expansion, closure and, eventually, fusion with lysosomes is made possible by the recruitment of a wide array of proteins from cytosol. Among these factors, a mammalian orthologue of yeast Atg8, the microtubule-associated protein 1 light chain 3 B (LC3), drives the elongation phase of phagophores [108]. As described in a seminal paper by Kabeya and Coll., the 30 kDa full-length precursor pro-LC3 is cleaved at the C-terminus, forming a mature 18 kDa cytosolic form (LC3-I) that is further trimmed to originate a 16 kDa fragment (LC3-II), bound to phosphoethanolamine and inserted into the membrane of the elongating phagophore [109]. LC3-II not only allows phagophore elongation, but is also involved in the caging of aggregated proteins into phagosomes; its amino acidic sequence contains a binding region for the autophagy receptors SQSTM1/p62 and NBR1 (neighbor of BRCA1 gene1) that, in turn, recognize committed-to-digestion ubiquitinated proteins. Thus, during the elongation phase, LC3-II binds to ubiquitinated cytoplasmic material, favoring the accumulation of aggregated proteins within the phagophore [108,110,111]. The edges of phagophores eventually seal to form double-membrane vesicles, the autophagosomes [112,113]. The fate of newly formed autophagosomes is not uniquely directed towards fusion with lysosomes, but other vesicular entities can converge within the autophagic pathway. Endosomes, in particular, and multivesicular bodies can fuse with autophagosomes, before the arrival of lysosomes, resulting in the formation of amphisomes [6].
In the late stages of autophagy, autophagosomes travel along microtubules in the direction of the microtubule organizing center, where they interact with lysosomes, allowing the degradation of the cargo; of note is that the complete fusion with lysosomes, although often described, is not an absolute requirement for the formation of autolysosomes, and the passage of hydrolytic enzymes may also occur through transient or partial fusion among autophagosomes and lysosomes [114,115]. The fusion produces a net reduction in LC3-II content, since the fraction bound with the internal membrane of the autophagosome is digested together with the internal cargo. Accordingly, the amount of LC3-II is the most reliable marker of the number of autophagosomes in the cytoplasm. The final stage of autophagy produces the degradation of cargo macromolecules up to their constitutive elements and their release to the cytosol for recycling. Although representing a major goal of the entire autophagic process in mammals, nutrient recycling has been far less investigated and characterized than the preceding steps. Most knowledge of this process is derived from studies in yeasts, in which autophagosomes eventually fuse their outer membrane with acidic vacuoles, where they are digested along with their cargo, mainly through the activity of vacuolar proteinases [116]. Yeast vacuole membranes contain several proteins that have been associated with catalysis of autophagic content [117,118] and amino acid efflux to the cytosol [119,120,121]. The best characterized among these mechanisms of extrusion from vacuole are represented by integral membrane proteins, called autophagic vacuole transporter (AVT), which produce cytosolic efflux of amino acids in a relative selective manner.
8. Autophagy of Damaged Mitochondria and Lysosomes
The major cause of oxidative damage in aging cells or caused by exposure to environmental stresses arises from malfunctioning mitochondria in which the respiratory chain produces excessive amounts of reactive oxygen species (ROS), or when the antioxidant ability declines. This is particularly troublesome in neurons in which the energy demand requires numerous and hyperactive mitochondria. Renewal of mitochondria and mitochondrial protein is thus a relevant neuroprotective activity and can be accomplished by either proteasome activity or autophagy, but it is reduced during aging or under neurodegenerative conditions [79]. Of note, removal of most mild dysfunctional and oxidized proteins that are exposed on the outer mitochondria membrane can be achieved through a proteasome-mediated process of fixation that does not require the digestion of the entire organelle [122]. However, when the production of ROS exceeds a threshold level, it can impair the activity of proteasome itself, making macroautophagy an absolute requirement for removing damaged mitochondria and preventing cell death. In the latter case, a mitochondrial-targeted form of macroautophagy, for this reason called mitophagy, takes place, in which mitochondria are labelled in order to be recognized by autophagic machinery. Impairment of mitochondrial electron transport chain by defective respiratory complex I and ROS-induced oxidative damage are the major contributors for dopaminergic neuron death in PD, not only in inherited forms, but also in those induced by chronic exposure to insecticides rotenone and paraquat [123,124,125]. The best characterization of mitophagic mechanisms arises from studies on proteostasis defects associated with inherited forms of PD [126], where point mutations in pathogenic genes cause the impairment of this pathway. A key protein in mitochondrial commitment to degradation is the PTEN-induced putative protein kinase 1 (PINK1). PINK1 undergoes a rapid turn-over on the mitochondrial surface in healthy conditions, but in PD it accumulates on the outer membrane of depolarized or damaged mitochondria [127]. PINK1 recruits a cytosolic E3-ubiquitin ligase, named Parkin, that attaches ubiquitin chains to mitochondrial outer membrane proteins. Ubiquitinated mitochondria are subjected to proteasome-mediated fixation or recognized as degradable cargo by the interaction with SQSTM1/p62, and included within the phagophore [128]. Reduction of mitophagy efficiency is also part of the physiological alterations during normal aging. In these conditions, the increase of defective mitochondria cause overproduction of ROS and oxidative damage of lysosomal enzymes, followed by the accumulation of lipofuscins within the lysosomes [63,80,129]. Defects in mitophagy machinery are the main pathogenetic alterations in early-onset inherited parkinsonisms, in which the most relevant mutations occur in PINK1 and Parkin genes [79,80,81,130]. Similarly, damage in mitophagy has also been hypothesized to represent a risk factor in sporadic forms of other neurodegenerative conditions such as AD, ALS, and HD [131]. Rapamycin reduces rotenone neurotoxicity, stimulating the autophagic clearance of swollen mitochondria [112,132]. This evidence suggests that the impairment of mitochondrial-targeted autophagy results in predisposition to dopaminergic loss in the substantia nigra in these forms of PD.
Another source of potentially deadly derangement from cytoplasmic integrity is represented by malfunctioning lysosomes. Lysosomes’ crucial role is to ensure continuous quality control in protein and organelle turnover, thus requiring the perfectly calibrated selective permeability of their membrane. Massive rupture of the lysosomal membrane typically occurs after strong physico-chemical insults and produces rapid cell necrosis and significant inflammatory response in the surrounding tissue. In contrast, a subtler lysosomal membrane permeabilization is associated with apoptosis and has been described to result from a great variety of physiologically frequent stresses, including phospholipid oxidation by free radicals, exposure to lysosomotropic agents, lysosomal rupture by proteolysis-resistant bacteria or viruses and, importantly, accumulation of aggregated indigestible proteins. The limited diffusion of hydrolytic enzymes is a well-characterized stimulus for mitochondrial depolarization, followed by release of Cytochrome C, the formation of apoptosome and the execution of extrinsic apoptotic pathway. Clinical and experimental evidence suggests that lysosomal loss of selective impermeability in neurons occurs in physiological aging, and, possibly, contributes to neuronal loss in neurodegenerative diseases [133,134].
A recently identified pattern of cell response to lysosomal alteration, named endo-lysosomal damage response, is a defensive system executed by cells to (i) achieve recovery of lysosomal proteins from light damage, (ii) modify lysosomal production to compensate for loss of proteolytic competence, or (iii) remove irreparably damaged lysosomes. The latter point is achieved through activating a specific form of macroautophagy, similar for many aspects to mitophagy, which has been named lysophagy [135]. Lysophagy plays also a relevant role in antibacterial cell defense [136]. Altered lysosomes are recognized by galectins (cytosolic glycan-binding proteins) that function as ELDR sensors through the binding to β-galactosides in the inner face of the damaged lysosomal membrane. Target-specific forms of lysophagy have been described on the basis of the damaging agent, in which lysosomes recruit different kinds of galectins (Gal1, 3, 8, 9) to activate different downstream signals [136,137,138]. Overall, ubiquitinated proteins on lysosomal surface are recognized by autophagy receptors, among which SQSTM1/p62 drives the nucleation of the phagophore.
Remarkably, for the purposes of this review, there is growing evidence that disturbances of lysophagy make a relevant contribution to neuronal death in genetic forms of tauopathies and ALS, although it is still unclear whether neuronal loss is dependent on specific impairment of lysophagy or it results from a general disturbance of autophagy [137].
9. Aggrephagy is a Form of Macroautophagy Directed Against Misfolded Proteins
The ability to form multimeric complexes is an inherent feature of all proteins and is required for their biological functions. Thus, its correct execution is tightly regulated. Altered amino acid sequences caused by gene mutations or ribosomal malfunctioning, oxidative stress, and other processes can produce failures in the proper protein assembly, commonly referred to as “misfolding”. The generation of these aberrant proteins is often harmful to cells, because they might lose activity or gain cytotoxic properties. Many neurodegenerative disorders of CNS are associated with the accumulation of highly expressed neuronal proteins, whose misfolding causes exposure of hydrophobic groups to the cytosol, initiating a process of aggregation that ultimately produces insoluble clumps as extracellular or intracellular deposits [33,139,140].
In contrast to microautophagy and CMA, macroautophagy has been classically described as a non-specific system for bulk degradation of cytosolic proteins. Although this concept may still be appropriated to identify forms of autophagy ensuring recycling of macromolecule for cell survival to trophic stresses, a significant heterogeneity in intracellular targets, mechanisms of regulation, and biological meaning has recently been identified. In 2007, Overbye and Coll. introduced the term “aggrephagy” to describe autophagosomes engulfed by high levels of aggregated proteins and marked by the chaperonine Hsc70 (heat shock complex 70) [141]. Aggrephagy is a particular form of macroautophagy that allows the removal of aggregated proteins and contributes to determining neuronal sensitivity to alterations of proteostasis [10,142]. When needed, monomeric forms of misfolded or overexpressed proteins are digested by heat shock-mediated proteolysis or by UPS, which represent the most active cellular proteolytic systems under physiological conditions. In the absence of a proper activity of proteosomal proteolytic digestion, aggregation-prone proteins undergo a process of multimerization that eventually produces cytosolic aggregates that move along microtubules and concentrate at the microtubule organizing center (MTOC) to form large clumps called aggresomes [143,144]. The relevance of aggresome formation for cell survival is still a matter of debate, and it is unclear whether they represent solely inert end-points of a self-defense strategy of the cells, or if their removal is needed to prevent cell death. Since Hsc70 recognizes ubiquitinated proteins, it is conceivable that autophagosomes may act as scavengers that recognize and engulf specific proteins that have undergone ubiquitin-mediated modifications. This aggrephagy process involves receptors for cargos and adaptor proteins, such as SQSTM1/p62 and NBRI, which contain both a domain that recognizes the autophagic core protein LC3, and a site of interaction with ubiquitin residues on cargo proteins; they specifically select and direct aggregated proteins into the elongating phagophore that grows around the aggregate [145]. SQSTM1/p62, beyond recognizing poly ubiquitins marking misfolded proteins, has the ability to favor the formation of larger aggregates that are more easily recognized by the phagophore core machinery [110]. Another protein crucial for aggrephagy is the scaffold protein PI3P-binding autophagy-linked FYVE domain protein (Alfy), which stabilizes the complex between SQSTM1/p62 and the ubiquitinated proteins, allowing the recognition by the autophagic core complex composed by Atg5, Atg12, Atg16, and LC3 [146,147]. Alfy belongs to the so-called “autophagy adaptor molecules” and, in non-stressful conditions, is detected in both the nuclear membrane and inside the nucleus. However, a nuclear-cytoplasmic shift of Alfy localization occurs when neurons necessitate the elimination of aggregated proteins. Importantly, the presence of Alfy excludes non-ubiquitinated protein from autophagosomes, increasing the specificity of aggrephagy toward aggregated proteins only. Alfy activity primarily occurs in the brain, where aggrephagy is far more important [147] and is necessary to prevent neurotoxicity in animal models [145]. Aggrephagy then proceeds, analogously to classical macroautophagy, with the fusion between autophagosome and lysosomes and the degradation of SQSTM1/p62/NBR1 complex along with the cargo proteins [110,111,148]. In contrast to starvation-induced autophagy, the mechanisms of regulation of aggrephagy are less characterized and do not depend on the blockade of mTORC1. Instead, cytosolic migration of SQSTM1/p62 and Alfy from the nuclear membrane and the binding with target proteins represents an initiating event and, perhaps, a rate-limiting step in aggrephagy.
10. Pharmacological Control of Autophagy
The role of autophagy as a pivotal regulatory mechanism of cell fate in aging, neurodegeneration, and carcinogenicity, along with its therapeutic potentiality, has stimulated significant efforts in the identification of autophagy-enhancing activity in drugs already used in human therapy, or directly developed for this purpose. The structures of the main drugs tested as autophagy activators discussed in the next paragraphs are depicted in Figure 1, while their corresponding molecular targets are reported in Figure 2.
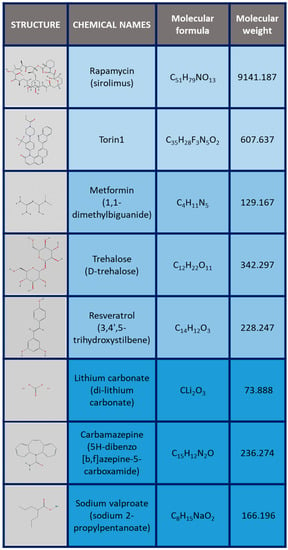
Figure 1.
Structures and molecular weights of the main drugs acting as autophagy inductors.
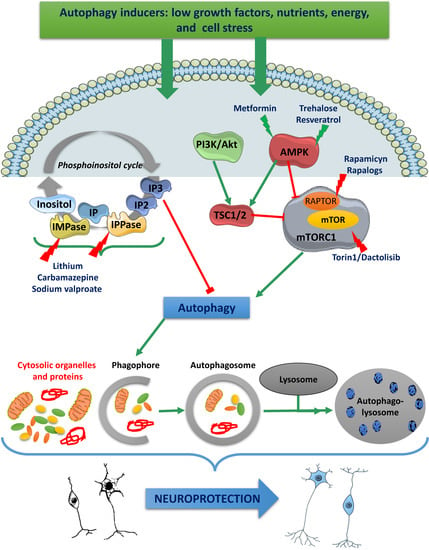
Figure 2.
Overview of the main pharmacological strategies for inducing autophagy through targeting of mTOR-dependent, mTOR-independent and phospho-inositol-signaling pathways.
Autophagy stimulation pathways converge to regulate mTOR. The growth factor pathway comprises PI3K/Akt/TSC/mTOR signaling and the ATP-energy depletion-activated AMPK/TSC/mTOR cascade, leading to TORC1 inhibition and autophagy induction.
Rapamycin and rapalogues enhance autophagy by stabilizing raptor-mTOR association and inhibiting mTOR activation; mTOR inhibition could also be achieved with torin1 and dactolisib.
Agents activating AMPK, such as metformin and trehalose or resveratrol, trigger AMPK-dependent mTOR inactivation.
One of the mTOR-independent autophagy activation pathways is a cascade of reactions triggered by low intracellular levels of inositol. This cascade is activated by the block of G-protein coupled receptors, leading to a reduction of IP3. Inositol arises as a result of hydrolysis of two phosphate moieties from IP3, forming IP2 and IP, IP is subsequently hydrolyzed IMPase.
Autophagy can be induced by drugs that decrease inositol or inositol IP3, such as lithium by IMPase, and carbamazepine and sodium valproate via impairment of inositol synthesis.
Abbreviations: mammalian target of (mTOR), mTOR complex 1 (mTORC1), regulatory-associated protein of mTOR (RAPTOR), tuberous sclerosis protein 1/2 (TSC1/2), phosphatidylinositol-4,5-bisphosphate 3-kinase (PI3K), protein kinase B (AKT), 5’AMP-activated protein kinase (AMPK), inositol triphosphate (IP3), inositol monophosphatase (IMPase), inositol polyphosphatase (IPP).
10.1. Rapamycin and Rapalogues
The blockade of mTORC1 activity, physiologically occurring during nutrient shortage [149], can be pharmacologically achieved by two structurally related macrolide antibiotics, sirolimus (rapamycin) and tacrolimus (FK506), and their derivatives (rapalogues) everolimus and temsirolimus; these drugs represent the most effective and powerful autophagy activators so far. Studies on brain tumors have demonstrated that rapamycin and its derivatives are able to cross the blood-brain barrier, with the newer compounds, such as temsirolimus, being more effective in this regard [150,151].
Rapamycin and tacrolimus reduce the kinase activity within mTORC1 upon binding with the intracellular receptor FK-506-binding protein 12 (FBP12), which, in turn, recognizes a binding site on mTOR. The complex FBP12-mTOR counteracts the scaffolding property of RAPTOR, preventing the mTOR dimerization and activation [152]. Rapamycin, tacrolimus and the rapalogue everolimus, have been introduced in therapy as immunosuppressant drugs to avoid transplant rejection; later on, everolimus became a first choice treatment for long-term control of tuberous sclerosis-associated angiomyolipomas [153,154] and for the therapy of neuroendocrine tumors of the gastro-entero-pancreatic tract [155].
The ability of rapamycin to reduce protein synthesis and block cell cycle progression produces immunosuppressive, antifungal, and anticancer activity; furthermore, rapamycin-dependent mTORC1 inhibition has recently been reported to function as a potent activator of autophagy. There is substantial evidence that the activation of autophagy flux induced by all rapamycin analogues provides neuroprotective effects in experimental models of neurodegenerative diseases, preventing the accumulation of aggregation-prone proteins and increasing neuronal viability [92,156]. The ability of rapamycin to restore autophagy flux has also been demonstrated in an in vitro TSE model of neurotoxicity in which neuronal death was induced by the recombinant misfolded PrP fragment 90–231. In this model, PrP90–231 rapidly accumulates in aggregates within neurons which try to remove them by activating the autophagy pathway. However, autophagic flux cannot be completed, and cells die by apoptosis, displaying a great number of unresolved autophagosomes [42]. In the presence of the autophagy-enhancing activity of rapamycin, the autophagic flux was completed and neurons survived. Similarly, tacrolimus also stimulates a sustained autophagic activity, leading to the degradation of newly misfolded PrPSc molecules [157]. The efficacy of rapamycin as an inducer of autophagy is unquestionable, but the benefits of its chronic administration in a clinical setting are significantly hampered by undeniable and common adverse reactions, including infections of the respiratory and urinary tracts, gastrointestinal pain, thrombocytopenia, and dyslipidemia [94]. Nevertheless, rapalogues, frequently prescribed as anti-cancer agents, are currently also under investigation for their ability to reduce the severity of neuronal loss due to proteinopathies, in view of their being a potential therapeutic extension to long-term treatment of neurodegenerative diseases [90].
Temsirolimus, an esterified rapamycin derivative, displays a remarkable antiproliferative activity in several forms of solid or hematological tumors, and it has recently been approved for treatment of advanced renal cancer [158]. Importantly, temsirolimus displays more tolerable side-effects than rapamycin and has no immunosuppressant activity. Temsirolimus demonstrated a remarkable capacity to stimulate autophagy and prevent neuronal death in vitro as well as in animal models of neurodegenerative proteinopathies induced by polyglutamine expansion of huntingtin [84] or ataxin-3 [159]. In transgenic mice bearing amyloid precursor protein (APP) overexpression, and point mutations of PS1 and tau genes, models of familiar AD, temsirolimus contrasted brain deposition of insoluble aggregates of Aβ and phosphorylated tau, lowering the amount of neurofibrillary tangle and apoptotic neurons. Importantly, temsirolimus-treated mice also exhibited better cognitive and motor performances in comparison with age-matched, untreated mutants [160,161,162]. Recently, significant beneficial activity of temsirolimus has also been observed in MPTP-induced animal models of PD: motor performance deficits, loss of dopaminergic neurons, and accumulation of α-synuclein were all prevented by simultaneous treatment with temsirolimus [163].
Finally, everolimus also showed a promising neuroprotective activity in AD animal models since, after acute intrathecal administration, reduced brain content of Aβ and hyperphosphorylated tau, via mTOR inhibition, and delayed animal cognitive decline were observed [164].
These encouraging results in support of mTOR inhibitors as pro-autophagic agents currently favors a great number of preclinical studies on innovative drugs that, although mainly focused on oncology, might expand the horizons of autophagy-based neuroprotective therapy [90].
10.2. ATP Analogues
ATP analogues can be sub-grouped, on the basis of their pharmacodynamics, as dual mTOR/PI3K inhibitors and pan-mTOR inhibitors [165].
Compared to rapamycin, dual mTOR/PI3K inhibitors have the advantage of producing the block of both TORC1 and TORC2 complexes. Among these, dactolisib (NVPBEZ235), developed as an antitumor drug, is able to reduce the in vitro toxicity of Aβ1-42 in mouse hippocampus, and to reverse the subsequent memory impairment [166]. Pan-mTOR inhibitors, showing better antitumor properties than rapamycin, have also been studied for neuroprotective activity. Among these, an interesting novel compound, although pharmacokinetically limited, is Torin1 which is able to inhibit the kinase domain of both TORC complexes in a highly specific manner, without appreciable effects on PI3K [167]. Recently, Torin1 demonstrated anti-aging capacity as a dietary supplement in a fly model without altering other parameters that may influence lifespan [168].
10.3. AMPK Activators
Metformin, the first line drug for type II diabetes, whose long-lasting practice in human therapy has evidenced excellent tolerability, is now attracting significant interest as an anti-aging, anti-ischemic and anti-cancer agent. Chronic administration of metformin for hypoglycemic purposes has been reported to reduce the incidence of cancer, stroke, AD, and PD in diabetic patients, in which the incidence of these pathologies is otherwise greater than in the non-diabetic population [169,170,171,172,173,174]. Metformin pro-autophagic activity is mediated by the activation of the AMP-activated protein kinase (AMPK), which has been proposed to contribute to its antiproliferative activity [174]. Metformin acts inducing AMPK activity through direct LKB1-mediated phosphorylation or, indirectly, through the reduction of mitochondrial production of ATP [175,176]. Active AMPK stimulates the formation of autophagosomes by inhibiting mTORC1 or eliciting the direct activation of its downstream effector ULK1. [177,178,179]. The growing interest in AMPK as a regulator of autophagy and the neuroprotective potential of this process is currently situating metformin and other AMPK activators as novel drugs endowed with anti-aging or anti-PCDs activity. Importantly, there is evidence that induction of macroautophagy, with the consequent prevention of protein aggregation or accumulation of damaged mitochondria and lysosomes, is not a unique neuroprotective effect of AMPK-dependent mTORC1 inhibition. Indeed, AMPK also improves mitochondrial function and exerts anti-inflammatory and antiapoptotic activities [180]. The most promising future application of AMPK activators, and in particular of metformin, is the therapy of PD in which multiple downstream effectors of AMPK activation directly contribute to the prevention of substantia nigra dopaminergic neuron death [181]. Dopaminergic neurons of substantia nigra are particularly sensitive to the age-dependent decline of the antioxidant system activity and reduced mitochondrial efficiency. Hence, AMPK activators, shifting the energy balance toward reduction of ATP consumption, along with the enhanced mitophagy and prevention of α-synuclein aggregation, can act as possible PD-modifying drugs. Although no results from clinical trials with metformin in PD patients have so far been reported, there is preclinical evidence that AMPK activation in neurons is protective, and the treatment with metformin can ameliorate symptoms and pathology in animal models of toxin-induced PD [182,183]. In 2017, a pilot study on patients diagnosed with mild cognitive impairment or early AD showed that treatment with metformin improved executive function, learning and memory [184]. Although it is difficult to ascertain the contribution of autophagy to the reported cognitive improvement, these results, associated with the capacity of metformin to cross the blood-brain barrier and its well-tolerated profile in elderly patients, represent significant incentives for further investigations on metformin’s neuroprotective activity.
An intriguing novelty in the research into neuroprotective compounds was introduced by the description of the cardioprotective, antiaging and antioxidant properties of the natural polyphenol resveratrol [185]. It was demonstrated that resveratrol effect is, in part, mediated by calorie-restriction, mimicking activity and induction of autophagy through AMPK activation [186,187]. Recently, the therapeutic promise of resveratrol was realized in the demonstration that it may provide neuroprotection in cellular and mouse models of PCDs, including AD, HD, ALS and PD [180]. Of note, it has been demonstrated that the neuroprotection exerted by resveratrol is partly due to the stimulation of AMPK- and PARKIN-mediated mitophagy, suggesting the value of further exploration of its therapeutic potential, particularly in neurodegenerative conditions associated with mitochondrial impairment [180,188,189]. Interestingly, other AMPK activators, and metformin in particular, can also restore mitophagy-modulating PARKIN activity [180].
10.4. Inhibitors of Phosphoinositol Turnover
Lithium, a mood-stabilizing drug used in psychiatry since 1950 for the treatment of bipolar disorder, has recently demonstrated the ability to provide neuronal protection against several stresses, including traumatic injuries, excitotoxicity, environmental toxins, neuroinflammation and proteinopathies [190,191,192,193]. In particular, neuronal death, occurring after cytoplasmic aggregation of disease-associated proteins such as Aβ peptides, as well as mutant huntingtin, α-synuclein, or superoxide dismutase, is significantly reduced by lithium through the induction of autophagy [194,195,196]. In these studies, autophagy activation by lithium favors the removal of misfolded proteins along their oligomerization path, preventing the neurotoxicity of soluble oligomeric forms, and the formation of large cytosolic insoluble aggregates. The neuroprotective and pro-autophagic activity of lithium has also been reported in vivo, using mouse models of ALS and tauopathies [93,197]. In these mice, oral or parenteral chronic lithium administration delayed sensory and motor decline in comparison with untreated animals; brain histochemical analysis often showed lower amounts of SQSTM1/p62 in lithium-treated mouse brains, whereas autophagosome-bound LC3-II was significantly increased, indicating that lithium can improve the efficacy of autophagosome-mediated proteolysis [93,197]. Given the complex biochemical signaling activated by lithium, the definition of the effectors of its neuroprotective activity is still not completely clear, but it is likely that lithium pro-survival efficacy does not rely entirely on the activation of autophagy. Lithium, in its cationic monovalent form, can compete with magnesium divalent cation (Mg2+) to inhibit many enzymes that require magnesium as a cofactor [198]. Lithium causes the direct inhibition of inositol monophosphatase (IMPase) and inositol polyphosphatase-1 (IPP), blocking the phosphoinositide cycle and causing a net reduction of intracellular 1,4,5 inositol triphosphate (IP3). Interestingly, IP3 acts as autophagy suppressor through its binding to intracellular receptors located in the endoplasmic reticulum and mitochondria [199]. Another enzyme whose inhibition is likely to mediate the lithium neuroprotective effect is the glycogen synthase kinase-3 β (GSK-3β); the activity of this enzyme facilitates tau hyperphosphorylation and augments Aβ accumulation, playing a role in AD-related neurite dystrophy and neuronal death [200]. Chronic treatment with lithium is also beneficial through other mechanisms, including the expression of antiapoptotic proteins, the reduction of oxidative damage in mitochondria, the production of neurotrophic factors and the proliferation of neuronal progenitor cells [198]. Given all these necessary premises, however, it must be remarked that the impairment of inositol turnover is the most relevant trigger for lithium induction of autophagy [196,197]. The neuroprotective activity of lithium in cell cultures and in mouse models of AD provided the rationale for clinical trials in patients in the mild and moderate phases of the disease [198,201,202,203]. These trials mainly addressed the progression of cognitive impairment, and did not report a significant improvement of life expectancy of the enrolled patients, although lithium was well tolerated. Only a limited slowing-down of cognitive deterioration was observed in lithium-treated patients, associated with a significant reduction of hyperphosphorylated tau in cerebrospinal fluid [198,203]. Similar possible disease-modifying capacity of lithium was also considered for ALS. Lithium stimulated post-injury neurite sprouting, synaptogenesis and reduced ALS-like pathology progression in transgenic mice [204,205,206]. Regrettably, the translation of lithium potential in human therapy for ALS has produced, thus far, conflicting results. Distinct clinical trials that have been conducted with daily treatment with lithium for at least 12 months in ALS-affected patients have reported efficacy or no effects with respect to reducing the progression of disease and symptomatology, and increasing survival [207,208]. The potential therapeutic use of lithium has also been tested in HD and PD. It was reported that neuron death and accumulation of cytoplasmic aggregates of mutant forms of huntingtin and α-synuclein is significantly counteracted by lithium administration [194,196,209].
Carbamazepine (CBZ) and valproic acid (VPA), two antiepileptic and mood-stabilizing drugs, share with lithium the ability to inhibit the phosphoinositide cycle and neuroprotective potential, as observed in neuronal cultures and animal models of neurodegenerative disease [210,211,212]. Of note, both VPA and CBZ counteracted the accumulation of protein aggregates through the increase of autophagy [211,213,214]. However, in light of the preclinical and clinical data available so far, a definite evaluation of the utility of lithium and other mood-stabilizing drugs in neuroprotective therapy is premature and requires further investigation. In contrast to rapamycin, lithium, CBZ and VPA do not directly affect the enzymatic activity of mTORC1, and do not prevent the phosphorylation of the mTORC1 downstream effectors S6K1 and 4EBP1, thus displaying no immunosuppressant activity. Synergistic neuroprotective activity between lithium, VPA, and rapamycin has been reported in different animal models of inherited neurodegenerative pathologies [206,215] and represents a promising rationale for a deeper characterization of their pharmacodynamics as anti-PCD agents.
10.5. Trehalose
Trehalose is a natural disaccharide derived by the condensation of two molecules of glucose. It is particularly abundant in bacteria, yeast, insects, and other invertebrates, where it acts to protect cells against environmental stresses, particularly preventing protein denaturation [216,217,218]. The protein-stabilizing activity of trehalose is not limited to the organism in which it is produced, but can be observed when exogenously administered to mammalian cells, in which it protects protein integrity in freeze-drying procedures [219]. Trehalose also shows neuroprotective potential against aggregation-prone proteins, as demonstrated in cell-free systems, where it inhibits amyloid fibril formation from Aβ peptides, polyglutamine-containing myoglobin and insulin. Moreover, trehalose prevents neuron death induced by Aβ1-40 and mutant huntingtin, and reduces amyloid deposition and striatal atrophy in a mouse model of HD [220,221,222]. Given this neuroprotective potential of trehalose against PCDs, the characterization of its protein-stabilizing activity has attracted significant interest. Different mechanisms have been proposed to explain the anti-aggregating and neuroprotective effects of trehalose, including the direct binding to proteins, favoring the maintenance of a soluble state, and the inhibition of aggregation [222]. Trehalose exerts neuroprotection in cellular and animal models of PCDs caused by mutant forms of huntingtin, α-synuclein, tau, or SOD1, or by the inhibition proteosomal activity. In all these models, the reduction of neurodegeneration was associated with an increased number of autophagosomes, degradation of mutant proteins, and improved mitochondrial function [85,222,223,224,225]. Importantly, trehalose neuroprotection was reverted by the autophagy blocker 3-methyladenine, suggesting that macroautophagy plays a major role in trehalose activity [85]. However, since trehalose does not reduce the phosphorylation of the two main mTOR effectors, S6K1 and 4E-BP1, its activity is likely not dependent on the canonic rapamycin-mediated blockade of mTOR. Conversely, trehalose activity was proposed to be mediated by the activation of gene transcription for many autophagy-related and antioxidant proteins [226,227,228]. Moreover, studies on liver non-alcoholic fatty lipid disease demonstrate that trehalose causes AMPK-dependent activation of autophagy to determine the inhibition of glucose transporter at hepatocytes plasmamembrane [229,230]. Two important hints outline the potential of trehalose as neuroprotective agent in PCDs: (i) substantial evidence supports that trehalose stimulates the clearance of oligomers, the main neurotoxic entities, rather than the removal of large aggregates [231], (ii) trehalose stimulates autophagy independently of mTOR inhibition and its neuroprotective activity was additive with that of rapamycin [232]. In this regard, considering the potential toxicity of rapamycin and rapalogues, particularly in conditions of chronic treatment, the possibility of reducing the rapamycin dose through co-administration of a clearly tolerable molecule such as trehalose should definitely be pursued in the future.
10.6. Screenings for Novel Autophagy Enhancer Drugs
Potential novel pro-autophagic drugs were screened on the basis of their effect on cell proliferation, clearance of long-lived proteins, or on the expression of autophagy-related proteins. [233,234]. Sarkar and Coll. developed a yeast-based screening of substances able to strengthen the cytostatic activity of rapamycin, with the aim of identifying pro-autophagy effects on mammalian cells. In total, 21 molecules were detected and collectively grouped under the acronym “SMERs” (small-molecule enhancers of rapamycin) for their additive effect on antiproliferative activity of rapamycin. Three of these compounds were characterized in detail for their ability to accelerate mTOR-independent clearance of mutant α-synuclein and huntingtin in stably transfected cells. Notably, the neuroprotective activity of SMERs was successfully tested in vivo in a fly model of neurodegeneration induced by the expression of mutant huntingtin [85,233]. The same purpose was adopted to screen pro-autophagic activity of drugs already approved for human therapy, although with different indications from neuroprotection. Zhang and Coll. analyzed more than 30 known drugs for their capacity to elicit autophagy, and found that eight structurally unrelated compounds, mostly belonging to antipsychotic and calcium antagonist families, stimulated autophagosome formation and the degradation of aggregation-prone long-lived peptides [234]. In a contemporary, albeit independent, screening, other mTOR-independent activators of autophagy were identified, including, but not limited to, calcium antagonists, which could be effective in the intracellular clearance of aggregation-prone huntingtin and α-synuclein mutants [235]. Importantly, both studies provided proofs of principles of the neuroprotective repurposing of drugs already validated for prolonged therapy in humans. The most promising drugs, whose repositioning as pro-autophagic compounds is currently under investigation as neuroprotective agents, are listed in Table 1.

Table 1.
Neuroprotective drugs with pro-autophagic properties.
11. Future Development of Autophagy Enhancers in Neurodegeneration Therapy
The aging process produces an inevitable reduction of the efficiency of most physiological functions, representing a risk factor for the development of several neurodegenerative disorders, including AD and PD [168]. A key topic of research on aging has been, for a long time, the characterization of the cellular mechanisms that affect neuronal sensitivity to neurotoxic stresses, focusing on those whose decline in efficiency with aging allows intracellular accumulation of neurotoxic misfolded proteins. Of note, there is growing evidence that neuronal resistance to aging-related processes can be ameliorated by either nutritional or pharmacological strategies. The same treatments can also be successful in delaying the onset of sporadic and genetic neurodegenerative diseases [236,237]. Autophagy, through its renewing function of cytoplasmic content, which in neurons assumes crucial life-saving effects, is the main target of these novel approaches. Remarkably, autophagy works as a constitutive process that degrades bulk cytoplasm cargo under normal circumstances, or can be up-regulated under nutrient shortage when a rapid supply of nutrients is needed [149]. In addition to this non-specific recruitment of nutrients, autophagy can be specifically targeted to remove misfolded proteins during their path to aggregation or damaged organelles, thus acting as an inhibitor of cell death. This is particularly evident in neurons in which autophagy inhibition causes neuronal loss and intracellular accumulation of structurally altered proteins [238]. Moreover, the execution of apoptosis following neurotoxic insults can be prevented by contemporary activation of autophagy.
Protein quality controls, including proteasome-mediated degradation of short-lived proteins and all forms of autophagy, decline with aging, and this dysfunction favors the accumulation of damaged proteins and organelles in the cytoplasm [239,240]. To preface the possible placement of autophagy-enhancers as disease-modifying therapies against PCDs, it is necessary to note that, to date, all the clinical trials that have been performed with these compounds have produced, at most, limited improvement of cognitive scores, with no beneficial effects on survival [93,207].
The evidence that long-term non-pharmacological interventions, in particular caloric restriction or intermittent fasting, can significantly delay brain atrophy and cognitive decline [237], sharply contrasts with the failure of even the most promising pro-autophagic drugs in anti-PCD clinical trials.
It is unquestionable that the delay existing between therapy onset and actual neuronal damage in human neurodegenerative diseases can barely be modeled in animals. This discrepancy represents a major hindrance for the efficacy of disease-modifying therapies when translated from preclinical to clinical settings. For this reason, to optimize anti-aging therapies, it is recommended that the treatment begin well before the age “symptomatology” onset [241]. Of note, an important clinical trial was recently started for preventive purposes [242], enrolling still asymptomatic subjects that are at risk of developing a rare form of prion disease, fatal familial insomnia, since they bear a high-penetrance mutation of the PRNP gene [243]. Although this trial is still currently in progress, and it is not being performed using autophagy-enhancing molecules, its results could represent a future proof of concept regarding the opportunity to begin neuroprotective treatments in individuals at risk for neurodegenerative diseases at the very beginning of neurological onset, or even in the asymptomatic phase. Therefore, the decision to determine an early start of neuroprotective strategies should be based on: (i) an accurate diagnosis that could evaluate risk factors and evidence light symptoms as early as possible; and (ii) the availability of relatively side-effect-free drugs that patients, in early or still asymptomatic phases of disease, could tolerate for years if not for decades.
Rapamycin and rapalogues are, to date, the most powerful autophagy enhancer agents, although they are loaded with frequent and unwanted effects that currently limit their use to few selected conditions, such as anti-cancer and anti-transplant rejection therapies [244,245]. The recent great surge of scientific interest in autophagy as an anti-aging strategy stimulated the identification of molecular pathways that control the process and led to the definition of new targets for less toxic molecules to be used for long periods under non-life-threatening conditions. In this regard, the antipsychotic and antiepileptic drugs lithium, VPA and CBZ, which antagonize IP3 autophagy-repressing activity, represent proof-of-principle regarding the possibility of activating phagophore nucleation without blocking the kinase activity of mTOR [195]. Other molecules that have a well-established positioning in human therapy against a wide number of pathologies are currently under reevaluation by virtue of their promising, although still not-well-defined, pro-autophagic activity [85,233,235]. In addition, molecules so far devoid of clinical indications are able to activate mTOR-independent autophagy; among these, the disaccharide trehalose and grape polyphenol resveratrol convincingly show neuroprotective and pro-autophagic effects through multiple mechanisms, including the activation of transcription factors for autophagy-related proteins and antioxidants [226,227,228] or mimicking starvation-dependent reduction of glucose uptake and AMPK activation [229,230,246]. As already mentioned, all these substances have demonstrated anti-aggregating and neuroprotective properties, but have so far attracted limited interest towards translation into clinical research, as PCD disease-modifying drugs. In this regard, several clinical trials, reported in Table 2, are ongoing to test potential neuroprotective activity of autophagy enhancers, in the early phases of AD, HD and ALS, and these are expected to be concluded in the near future.

Table 2.
Ongoing clinical trials for PCDs using autophagy-enhancing drugs. Data were collected from NIH, US national Library of medicine (www.ClinicalTrials.gov) using “autophagy” and the drug names as key-words; only active trials are reported.
Evidence of successful additive autophagy activation by co-treatment with the mTOR-dependent rapamycin and mTOR-independent trehalose in a PD mouse model was recently reported [232], suggesting the efficacy of non-toxic low-dose, long-term combination treatments. It is also important to remark that the classic division of autophagy into micro, macro and chaperone-mediated has recently been challenged by clear evidence that macroautophagy does not just remove bulk cytoplasmic content; rather, neuroprotective macroautophagy is often specifically targeted to damaged organelles or proteinaceous aggregates. Hence, improved knowledge of such heterogeneity prefigures a futurible combined pharmacological approach in which the additive effects of two or more drugs might provide neuroprotection through specific action on multiple cell stresses that may be differently relevant in each PCDs.
12. Conclusions
The role of autophagy is becoming more and more relevant in different physiological and pathological conditions. In particular, several drugs acting through the modulation of the autophagic flux are now currently being used or are in clinical trials in oncology. However, the unifying theory regarding the molecular mechanisms of neuronal death in different neurodegenerative conditions in which defective autophagy leads to oligomers accumulation has prompted the analysis of the potential use of several pro-autophagic drugs also in these conditions. In particular, both novel and repositioned molecules are currently in preclinical and clinical trials to induce clearance of misfolded oligomers via the potentiation of the autophagic pathway.
Author Contributions
All the authors equally contributed to literature search, analysis and discussion; S.T. and T.F. wrote the article, and all the authors revised it; F.B. drown the figures.
Funding
This research was funded by Italian Ministry for University and Research (FFABR) to F.B.
Conflicts of Interest
The authors have no conflict of interest to declare.
Abbreviations
| Alfy | Autophagy-linked FYVE-domain protein |
| AD | Alzheimer’s disease |
| AMPK | AMP-activated protein kinase |
| ALS | Amyotrophic lateral sclerosis |
| Aβ | β-amyloid |
| CBZ | Carbamazepine |
| PrPC | Cellular prion protein |
| CNS | Central nervous system |
| CMA | Chaperone-mediated autophagy |
| DEPTOR | DEP domain-containing mTOR interacting protein |
| 4E-BP1 | EIF4E-binding protein 1 |
| eIF4E | Eukaryotic translation initiation factor 4E |
| GSK-3β | Glycogen synthase kinase-3 β |
| Hsc70 | Heat shock complex 70 |
| HD | Huntington’s disease |
| IMPase | Inositol monophosphatase |
| IPP | Inositol polyphosphatase-1 |
| IP3 | 1,4,5 inositol triphosphate |
| mLST8 | Mammalian lethal with SEC13 protein 8 |
| mTOR | Mammalian target of rapamycin |
| LC3B | Microtubule-associated protein 1 light chain 3 B |
| MTOC | Microtubule organizing center |
| mTORC1 | MTOR enzymatic complex 1 |
| mTORC2 | MTOR enzymatic complex 2 |
| NBR1 | Neighbor of BRCA1 gene1 |
| PD | Parkinson’s disease |
| PIP2 | Phosphatidylinositol 4′,5′-biphosphate |
| PIP3 | Phosphatidylinositol 3,4,5-triphosphate |
| PI3K | Phosphoinositide 3-kinase |
| PIKKs | PI3K-related kinase |
| PrPSc | Prion protein Scrapie |
| PRAS40 | Proline rich AKT substrate 40-kDa |
| PCDs | Protein conformational disorders |
| PINK1 | PTEN-induced putative protein kinase 1 |
| Rheb | RAS homolog enriched in brain |
| RAPTOR | Regulatory associated protein of mTOR |
| ROS | Reactive oxygen species |
| S6K1 | S6 kinase 1 |
| SQSTM1/p62 | Sequestrosome 1/p62 |
| SMERs | Small-molecule enhancers of rapamycin |
| TSE | Transmissible spongiform encephalopathies |
| TSC | Tuberous sclerosis complex |
| UPS | Ubiquitin-proteasome system |
| Ulk1 | Unc-51-like kinase 1 |
| VPA | Valproic acid |
References
- Scott, S.V.; Klionsky, D.J. Delivery of proteins and organelles to the vacuole from the cytoplasm. Curr. Opin. Cell Biol. 1998, 10, 523–529. [Google Scholar] [CrossRef]
- Noda, T.; Suzuki, K.; Ohsumi, Y. Yeast autophagosomes: De novo formation of a membrane structure. Trends Cell Biol. 2002, 12, 231–235. [Google Scholar] [CrossRef]
- Abeliovich, H. Regulation of autophagy by amino acid availability in S. cerevisiae and mammalian cells. Amino Acids 2015, 47, 2165–2175. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, S.; Cuervo, A.M. Chaperone-mediated autophagy: A unique way to enter the lysosome world. Trends Cell Biol. 2012, 22, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Li, W.W.; Li, J.; Bao, J.K. Microautophagy: Lesser-known self-eating. Cell. Mol. Life Sci. 2012, 69, 1125–1136. [Google Scholar] [CrossRef] [PubMed]
- Klionsky, D.J.; Eskelinen, E.L.; Deretic, V. Autophagosomes, phagosomes, autolysosomes, phagolysosomes, autophagolysosomes... wait, I’m confused. Autophagy 2014, 10, 549–551. [Google Scholar] [CrossRef] [PubMed]
- Lamark, T.; Johansen, T. Aggrephagy: Selective disposal of protein aggregates by macroautophagy. Int. J. Cell Biol. 2012, 2012, 736905. [Google Scholar] [CrossRef]
- Hyttinen, J.M.; Amadio, M.; Viiri, J.; Pascale, A.; Salminen, A.; Kaarniranta, K. Clearance of misfolded and aggregated proteins by aggrephagy and implications for aggregation diseases. Ageing Res. Rev. 2014, 18, 16–28. [Google Scholar] [CrossRef]
- Anding, A.L.; Baehrecke, E.H. Cleaning House: Selective Autophagy of Organelles. Dev. Cell 2017, 41, 10–22. [Google Scholar] [CrossRef]
- Yamamoto, A.; Simonsen, A. The elimination of accumulated and aggregated proteins: A role for aggrephagy in neurodegeneration. Neurobiol. Dis. 2011, 43, 17–28. [Google Scholar] [CrossRef]
- Boland, B.; Yu, W.H.; Corti, O.; Mollereau, B.; Henriques, A.; Bezard, E.; Pastores, G.M.; Rubinsztein, D.C.; Nixon, R.A.; Duchen, M.R.; et al. Promoting the clearance of neurotoxic proteins in neurodegenerative disorders of ageing. Nat. Rev. Drug Discov. 2018, 17, 660–688. [Google Scholar] [CrossRef] [PubMed]
- Soto, C. Protein misfolding and disease; protein refolding and therapy. FEBS Lett. 2001, 498, 204–207. [Google Scholar] [CrossRef]
- Bucciantini, M.; Giannoni, E.; Chiti, F.; Baroni, F.; Formigli, L.; Zurdo, J.; Taddei, N.; Ramponi, G.; Dobson, C.M.; Stefani, M. Inherent toxicity of aggregates implies a common mechanism for protein misfolding diseases. Nature 2002, 416, 507–511. [Google Scholar] [CrossRef] [PubMed]
- Klaips, C.L.; Jayaraj, G.G.; Hartl, F.U. Pathways of cellular proteostasis in aging and disease. J. Cell Biol. 2018, 217, 51–63. [Google Scholar] [CrossRef] [PubMed]
- Boland, B.; Kumar, A.; Lee, S.; Platt, F.M.; Wegiel, J.; Yu, W.H.; Nixon, R.A. Autophagy induction and autophagosome clearance in neurons: Relationship to autophagic pathology in Alzheimer’s disease. J. Neurosci. 2008, 28, 6926–6937. [Google Scholar] [CrossRef] [PubMed]
- Dikic, I. Proteasomal and Autophagic Degradation Systems. Annu. Rev. Biochem. 2017, 86, 193–224. [Google Scholar] [CrossRef] [PubMed]
- Selkoe, D.J.; Hardy, J. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol. Med. 2016, 8, 595–608. [Google Scholar] [CrossRef] [PubMed]
- Mroczko, B.; Groblewska, M.; Litman-Zawadzka, A.; Kornhuber, J.; Lewczuk, P. Amyloid beta oligomers (AbetaOs) in Alzheimer’s disease. J. Neural Transm. (Vienna) 2018, 125, 177–191. [Google Scholar] [CrossRef]
- McLean, C.A.; Cherny, R.A.; Fraser, F.W.; Fuller, S.J.; Smith, M.J.; Beyreuther, K.; Bush, A.I.; Masters, C.L. Soluble pool of Abeta amyloid as a determinant of severity of neurodegeneration in Alzheimer’s disease. Ann. Neurol. 1999, 46, 860–866. [Google Scholar] [CrossRef]
- Esparza, T.J.; Zhao, H.; Cirrito, J.R.; Cairns, N.J.; Bateman, R.J.; Holtzman, D.M.; Brody, D.L. Amyloid-beta oligomerization in Alzheimer dementia versus high-pathology controls. Ann. Neurol. 2013, 73, 104–119. [Google Scholar] [CrossRef]
- Wirths, O.; Multhaup, G.; Czech, C.; Blanchard, V.; Moussaoui, S.; Tremp, G.; Pradier, L.; Beyreuther, K.; Bayer, T.A. Intraneuronal Abeta accumulation precedes plaque formation in beta-amyloid precursor protein and presenilin-1 double-transgenic mice. Neurosci. Lett. 2001, 306, 116–120. [Google Scholar] [CrossRef]
- Prusiner, S.B. Biology and genetics of prions causing neurodegeneration. Annu. Rev. Genet. 2013, 47, 601–623. [Google Scholar] [CrossRef] [PubMed]
- Prusiner, S.B. Prions. Proc. Natl. Acad. Sci. USA 1998, 95, 13363–13383. [Google Scholar] [CrossRef] [PubMed]
- Mays, C.E.; Soto, C. The stress of prion disease. Brain Res. 2016, 1648 Pt B, 553–560. [Google Scholar] [CrossRef]
- Scheckel, C.; Aguzzi, A. Prions, prionoids and protein misfolding disorders. Nat. Rev. Genet. 2018, 19, 405–418. [Google Scholar] [CrossRef] [PubMed]
- Watts, J.C.; Prusiner, S.B. beta-Amyloid Prions and the Pathobiology of Alzheimer’s Disease. Cold Spring Harb. Perspect. Med. 2018, 8, a023507. [Google Scholar] [CrossRef] [PubMed]
- Woerman, A.L.; Watts, J.C.; Aoyagi, A.; Giles, K.; Middleton, L.T.; Prusiner, S.B. alpha-Synuclein: Multiple System Atrophy Prions. Cold Spring Harb. Perspect. Med. 2018, 8, a024588. [Google Scholar] [CrossRef]
- Mallucci, G.; Dickinson, A.; Linehan, J.; Klohn, P.C.; Brandner, S.; Collinge, J. Depleting neuronal PrP in prion infection prevents disease and reverses spongiosis. Science 2003, 302, 871–874. [Google Scholar] [CrossRef] [PubMed]
- Corsaro, A.; Thellung, S.; Villa, V.; Nizzari, M.; Florio, T. Role of prion protein aggregation in neurotoxicity. Int. J. Mol. Sci. 2012, 13, 8648–8669. [Google Scholar] [CrossRef]
- Corsaro, A.; Thellung, S.; Bucciarelli, T.; Scotti, L.; Chiovitti, K.; Villa, V.; D’Arrigo, C.; Aceto, A.; Florio, T. High hydrophobic amino acid exposure is responsible of the neurotoxic effects induced by E200K or D202N disease-related mutations of the human prion protein. Int. J. Biochem. Cell Biol. 2011, 43, 372–382. [Google Scholar] [CrossRef]
- Chiovitti, K.; Corsaro, A.; Thellung, S.; Villa, V.; Paludi, D.; D’Arrigo, C.; Russo, C.; Perico, A.; Ianieri, A.; Di Cola, D.; et al. Intracellular accumulation of a mild-denatured monomer of the human PrP fragment 90-231, as possible mechanism of its neurotoxic effects. J. Neurochem. 2007, 103, 2597–2609. [Google Scholar] [CrossRef] [PubMed]
- Thellung, S.; Corsaro, A.; Villa, V.; Simi, A.; Vella, S.; Pagano, A.; Florio, T. Human PrP90-231-induced cell death is associated with intracellular accumulation of insoluble and protease-resistant macroaggregates and lysosomal dysfunction. Cell Death Dis. 2011, 2, e138. [Google Scholar] [CrossRef] [PubMed]
- Chiti, F.; Dobson, C.M. Protein Misfolding, Amyloid Formation, and Human Disease: A Summary of Progress Over the Last Decade. Annu. Rev. Biochem. 2017, 86, 27–68. [Google Scholar] [CrossRef] [PubMed]
- Lacor, P.N.; Buniel, M.C.; Chang, L.; Fernandez, S.J.; Gong, Y.; Viola, K.L.; Lambert, M.P.; Velasco, P.T.; Bigio, E.H.; Finch, C.E.; et al. Synaptic targeting by Alzheimer’s-related amyloid beta oligomers. J. Neurosci. 2004, 24, 10191–10200. [Google Scholar] [CrossRef] [PubMed]
- Lacor, P.N.; Buniel, M.C.; Furlow, P.W.; Clemente, A.S.; Velasco, P.T.; Wood, M.; Viola, K.L.; Klein, W.L. Abeta oligomer-induced aberrations in synapse composition, shape, and density provide a molecular basis for loss of connectivity in Alzheimer’s disease. J. Neurosci. 2007, 27, 796–807. [Google Scholar] [CrossRef] [PubMed]
- Koffie, R.M.; Meyer-Luehmann, M.; Hashimoto, T.; Adams, K.W.; Mielke, M.L.; Garcia-Alloza, M.; Micheva, K.D.; Smith, S.J.; Kim, M.L.; Lee, V.M.; et al. Oligomeric amyloid beta associates with postsynaptic densities and correlates with excitatory synapse loss near senile plaques. Proc. Natl. Acad. Sci. USA 2009, 106, 4012–4017. [Google Scholar] [CrossRef] [PubMed]
- Wilcox, K.C.; Lacor, P.N.; Pitt, J.; Klein, W.L. Abeta oligomer-induced synapse degeneration in Alzheimer’s disease. Cell. Mol. Neurobiol. 2011, 31, 939–948. [Google Scholar] [CrossRef] [PubMed]
- Nixon, R.A.; Cataldo, A.M.; Mathews, P.M. The endosomal-lysosomal system of neurons in Alzheimer’s disease pathogenesis: A review. Neurochem. Res. 2000, 25, 1161–1172. [Google Scholar] [CrossRef]
- Cadonic, C.; Sabbir, M.G.; Albensi, B.C. Mechanisms of Mitochondrial Dysfunction in Alzheimer’s Disease. Mol. Neurobiol. 2016, 53, 6078–6090. [Google Scholar] [CrossRef]
- Mayer, R.J.; Landon, M.; Laszlo, L.; Lennox, G.; Lowe, J. Protein processing in lysosomes: The new therapeutic target in neurodegenerative disease. Lancet 1992, 340, 156–159. [Google Scholar] [CrossRef]
- Choi, H.S.; Choi, Y.G.; Shin, H.Y.; Oh, J.M.; Park, J.H.; Kim, J.I.; Carp, R.I.; Choi, E.K.; Kim, Y.S. Dysfunction of mitochondrial dynamics in the brains of scrapie-infected mice. Biochem. Biophys. Res. Commun. 2014, 448, 157–162. [Google Scholar] [CrossRef]
- Thellung, S.; Scoti, B.; Corsaro, A.; Villa, V.; Nizzari, M.; Gagliani, M.C.; Porcile, C.; Russo, C.; Pagano, A.; Tacchetti, C.; et al. Pharmacological activation of autophagy favors the clearing of intracellular aggregates of misfolded prion protein peptide to prevent neuronal death. Cell Death Dis. 2018, 9, 166. [Google Scholar] [CrossRef] [PubMed]
- Mannini, B.; Mulvihill, E.; Sgromo, C.; Cascella, R.; Khodarahmi, R.; Ramazzotti, M.; Dobson, C.M.; Cecchi, C.; Chiti, F. Toxicity of protein oligomers is rationalized by a function combining size and surface hydrophobicity. ACS Chem. Biol. 2014, 9, 2309–2317. [Google Scholar] [CrossRef]
- Corsaro, A.; Thellung, S.; Villa, V.; Principe, D.R.; Paludi, D.; Arena, S.; Millo, E.; Schettini, D.; Damonte, G.; Aceto, A.; et al. Prion protein fragment 106-126 induces a p38 MAP kinase-dependent apoptosis in SH-SY5Y neuroblastoma cells independently from the amyloid fibril formation. Ann. N. Y. Acad. Sci. 2003, 1010, 610–622. [Google Scholar] [CrossRef] [PubMed]
- Thellung, S.; Villa, V.; Corsaro, A.; Pellistri, F.; Venezia, V.; Russo, C.; Aceto, A.; Robello, M.; Florio, T. ERK1/2 and p38 MAP kinases control prion protein fragment 90-231-induced astrocyte proliferation and microglia activation. Glia 2007, 55, 1469–1485. [Google Scholar] [CrossRef] [PubMed]
- Thellung, S.; Florio, T.; Corsaro, A.; Arena, S.; Merlino, M.; Salmona, M.; Tagliavini, F.; Bugiani, O.; Forloni, G.; Schettini, G. Intracellular mechanisms mediating the neuronal death and astrogliosis induced by the prion protein fragment 106–126. Int. J. Dev. Neurosci 2000, 18, 481–492. [Google Scholar] [CrossRef]
- Villa, V.; Thellung, S.; Bajetto, A.; Gatta, E.; Robello, M.; Novelli, F.; Tasso, B.; Tonelli, M.; Florio, T. Novel celecoxib analogues inhibit glial production of prostaglandin E2, nitric oxide, and oxygen radicals reverting the neuroinflammatory responses induced by misfolded prion protein fragment 90–231 or lipopolysaccharide. Pharmacol. Res. 2016, 113 Pt A, 500–514. [Google Scholar] [CrossRef]
- Villa, V.; Thellung, S.; Corsaro, A.; Novelli, F.; Tasso, B.; Colucci-D’Amato, L.; Gatta, E.; Tonelli, M.; Florio, T. Celecoxib Inhibits Prion Protein 90-231-Mediated Pro-inflammatory Responses in Microglial Cells. Mol. Neurobiol. 2016, 53, 57–72. [Google Scholar] [CrossRef]
- Rajendran, L.; Paolicelli, R.C. Microglia-Mediated Synapse Loss in Alzheimer’s Disease. J. Neurosci. 2018, 38, 2911–2919. [Google Scholar] [CrossRef]
- Tu, J.; Chen, B.; Yang, L.; Qi, K.; Lu, J.; Zhao, D. Amyloid-beta Activates Microglia and Regulates Protein Expression in a Manner Similar to Prions. J. Mol. Neurosci. 2015, 56, 509–518. [Google Scholar] [CrossRef]
- Thellung, S.; Gatta, E.; Pellistri, F.; Villa, V.; Corsaro, A.; Nizzari, M.; Robello, M.; Florio, T. Different Molecular Mechanisms Mediate Direct or Glia-Dependent Prion Protein Fragment 90–231 Neurotoxic Effects in Cerebellar Granule Neurons. Neurotox. Res. 2017, 32, 381–397. [Google Scholar] [CrossRef] [PubMed]
- Oddo, S.; Caccamo, A.; Smith, I.F.; Green, K.N.; LaFerla, F.M. A dynamic relationship between intracellular and extracellular pools of Abeta. Am. J. Pathol. 2006, 168, 184–194. [Google Scholar] [CrossRef] [PubMed]
- Gaspar, R.C.; Villarreal, S.A.; Bowles, N.; Hepler, R.W.; Joyce, J.G.; Shughrue, P.J. Oligomers of beta-amyloid are sequestered into and seed new plaques in the brains of an AD mouse model. Exp. Neurol. 2010, 223, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Egan, M.F.; Kost, J.; Tariot, P.N.; Aisen, P.S.; Cummings, J.L.; Vellas, B.; Sur, C.; Mukai, Y.; Voss, T.; Furtek, C.; et al. Randomized Trial of Verubecestat for Mild-to-Moderate Alzheimer’s Disease. N. Engl. J. Med. 2018, 378, 1691–1703. [Google Scholar] [CrossRef] [PubMed]
- Golde, T.E.; DeKosky, S.T.; Galasko, D. Alzheimer’s disease: The right drug, the right time. Science 2018, 362, 1250–1251. [Google Scholar] [CrossRef] [PubMed]
- Marino, G.; Madeo, F.; Kroemer, G. Autophagy for tissue homeostasis and neuroprotection. Curr. Opin. Cell Biol. 2011, 23, 198–206. [Google Scholar] [CrossRef]
- Wurth, R.; Thellung, S.; Bajetto, A.; Mazzanti, M.; Florio, T.; Barbieri, F. Drug-repositioning opportunities for cancer therapy: Novel molecular targets for known compounds. Drug Discov. Today 2016, 21, 190–199. [Google Scholar] [CrossRef]
- Pushpakom, S.; Iorio, F.; Eyers, P.A.; Escott, K.J.; Hopper, S.; Wells, A.; Doig, A.; Guilliams, T.; Latimer, J.; McNamee, C.; et al. Drug repurposing: Progress, challenges and recommendations. Nat. Rev. Drug Discov. 2018. [Google Scholar] [CrossRef]
- Suresh, S.N.; Verma, V.; Sateesh, S.; Clement, J.P.; Manjithaya, R. Neurodegenerative diseases: Model organisms, pathology and autophagy. J. Genet. 2018, 97, 679–701. [Google Scholar] [CrossRef]
- Liberski, P.P.; Brown, D.R.; Sikorska, B.; Caughey, B.; Brown, P. Cell death and autophagy in prion diseases (transmissible spongiform encephalopathies). Folia Neuropathol. 2008, 46, 1–25. [Google Scholar]
- Hubbard, V.M.; Valdor, R.; Macian, F.; Cuervo, A.M. Selective autophagy in the maintenance of cellular homeostasis in aging organisms. Biogerontology 2012, 13, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Shigenaga, M.K.; Hagen, T.M.; Ames, B.N. Oxidative damage and mitochondrial decay in aging. Proc. Natl. Acad. Sci. USA 1994, 91, 10771–10778. [Google Scholar] [CrossRef] [PubMed]
- Brunk, U.T.; Terman, A. The mitochondrial-lysosomal axis theory of aging: Accumulation of damaged mitochondria as a result of imperfect autophagocytosis. Eur. J. Biochem. 2002, 269, 1996–2002. [Google Scholar] [CrossRef] [PubMed]
- Terman, A.; Gustafsson, B.; Brunk, U.T. Autophagy, organelles and ageing. J. Pathol. 2007, 211, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Hardy, J.; Selkoe, D.J. The amyloid hypothesis of Alzheimer’s disease: Progress and problems on the road to therapeutics. Science 2002, 297, 353–356. [Google Scholar] [CrossRef] [PubMed]
- Caccamo, A.; Magri, A.; Medina, D.X.; Wisely, E.V.; Lopez-Aranda, M.F.; Silva, A.J.; Oddo, S. mTOR regulates tau phosphorylation and degradation: Implications for Alzheimer’s disease and other tauopathies. Aging Cell 2013, 12, 370–380. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, D.M.; Lee, J.H.; Kumar, A.; Lee, S.; Orenstein, S.J.; Nixon, R.A. Autophagy failure in Alzheimer’s disease and the role of defective lysosomal acidification. Eur. J. Neurosci. 2013, 37, 1949–1961. [Google Scholar] [CrossRef]
- Cataldo, A.M.; Hamilton, D.J.; Barnett, J.L.; Paskevich, P.A.; Nixon, R.A. Abnormalities of the endosomal-lysosomal system in Alzheimer’s disease: Relationship to disease pathogenesis. Adv. Exp. Med. Biol. 1996, 389, 271–280. [Google Scholar]
- Cataldo, A.M.; Petanceska, S.; Terio, N.B.; Peterhoff, C.M.; Durham, R.; Mercken, M.; Mehta, P.D.; Buxbaum, J.; Haroutunian, V.; Nixon, R.A. Abeta localization in abnormal endosomes: Association with earliest Abeta elevations in AD and Down syndrome. Neurobiol. Aging 2004, 25, 1263–1272. [Google Scholar] [CrossRef]
- Tramutola, A.; Triplett, J.C.; Di Domenico, F.; Niedowicz, D.M.; Murphy, M.P.; Coccia, R.; Perluigi, M.; Butterfield, D.A. Alteration of mTOR signaling occurs early in the progression of Alzheimer disease (AD): analysis of brain from subjects with pre-clinical AD, amnestic mild cognitive impairment and late-stage AD. J. Neurochem. 2015, 133, 739–749. [Google Scholar] [CrossRef]
- An, W.L.; Cowburn, R.F.; Li, L.; Braak, H.; Alafuzoff, I.; Iqbal, K.; Iqbal, I.G.; Winblad, B.; Pei, J.J. Up-regulation of phosphorylated/activated p70 S6 kinase and its relationship to neurofibrillary pathology in Alzheimer’s disease. Am. J. Pathol. 2003, 163, 591–607. [Google Scholar] [CrossRef]
- Li, X.; Alafuzoff, I.; Soininen, H.; Winblad, B.; Pei, J.J. Levels of mTOR and its downstream targets 4E-BP1, eEF2, and eEF2 kinase in relationships with tau in Alzheimer’s disease brain. FEBS J. 2005, 272, 4211–4220. [Google Scholar] [CrossRef] [PubMed]
- Nixon, R.A.; Wegiel, J.; Kumar, A.; Yu, W.H.; Peterhoff, C.; Cataldo, A.; Cuervo, A.M. Extensive involvement of autophagy in Alzheimer disease: An immuno-electron microscopy study. J. Neuropathol. Exp. Neurol. 2005, 64, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, B.J.; Isakson, P.; Lewerenz, J.; Sanchez, H.; Kotzebue, R.W.; Cumming, R.C.; Harris, G.L.; Nezis, I.P.; Schubert, D.R.; Simonsen, A.; et al. p62, Ref(2)P and ubiquitinated proteins are conserved markers of neuronal aging, aggregate formation and progressive autophagic defects. Autophagy 2011, 7, 572–583. [Google Scholar] [CrossRef] [PubMed]
- Ntsapi, C.; Lumkwana, D.; Swart, C.; du Toit, A.; Loos, B. New Insights Into Autophagy Dysfunction Related to Amyloid Beta Toxicity and Neuropathology in Alzheimer’s Disease. Int. Rev. Cell Mol. Biol. 2018, 336, 321–361. [Google Scholar]
- Orr, M.E.; Salinas, A.; Buffenstein, R.; Oddo, S. Mammalian target of rapamycin hyperactivity mediates the detrimental effects of a high sucrose diet on Alzheimer’s disease pathology. Neurobiol. Aging 2014, 35, 1233–1242. [Google Scholar] [CrossRef]
- Dawson, T.M.; Dawson, V.L. Molecular pathways of neurodegeneration in Parkinson’s disease. Science 2003, 302, 819–822. [Google Scholar] [CrossRef]
- Engelender, S. Ubiquitination of alpha-synuclein and autophagy in Parkinson’s disease. Autophagy 2008, 4, 372–374. [Google Scholar] [CrossRef]
- Chu, C.T. A pivotal role for PINK1 and autophagy in mitochondrial quality control: Implications for Parkinson disease. Hum. Mol. Genet. 2010, 19, R28–R37. [Google Scholar] [CrossRef]
- Geisler, S.; Holmstrom, K.M.; Treis, A.; Skujat, D.; Weber, S.S.; Fiesel, F.C.; Kahle, P.J.; Springer, W. The PINK1/Parkin-mediated mitophagy is compromised by PD-associated mutations. Autophagy 2010, 6, 871–878. [Google Scholar] [CrossRef]
- Winslow, A.R.; Chen, C.W.; Corrochano, S.; Acevedo-Arozena, A.; Gordon, D.E.; Peden, A.A.; Lichtenberg, M.; Menzies, F.M.; Ravikumar, B.; Imarisio, S.; et al. alpha-Synuclein impairs macroautophagy: Implications for Parkinson’s disease. J. Cell Biol. 2010, 190, 1023–1037. [Google Scholar] [CrossRef] [PubMed]
- Spencer, B.; Potkar, R.; Trejo, M.; Rockenstein, E.; Patrick, C.; Gindi, R.; Adame, A.; Wyss-Coray, T.; Masliah, E. Beclin 1 gene transfer activates autophagy and ameliorates the neurodegenerative pathology in alpha-synuclein models of Parkinson’s and Lewy body diseases. J. Neurosci. 2009, 29, 13578–13588. [Google Scholar] [CrossRef] [PubMed]
- Xilouri, M.; Vogiatzi, T.; Vekrellis, K.; Park, D.; Stefanis, L. Abberant alpha-synuclein confers toxicity to neurons in part through inhibition of chaperone-mediated autophagy. PLoS ONE 2009, 4, e5515. [Google Scholar] [CrossRef] [PubMed]
- Ravikumar, B.; Vacher, C.; Berger, Z.; Davies, J.E.; Luo, S.; Oroz, L.G.; Scaravilli, F.; Easton, D.F.; Duden, R.; O’Kane, C.J.; et al. Inhibition of mTOR induces autophagy and reduces toxicity of polyglutamine expansions in fly and mouse models of Huntington disease. Nat. Genet. 2004, 36, 585–595. [Google Scholar] [CrossRef]
- Sarkar, S.; Perlstein, E.O.; Imarisio, S.; Pineau, S.; Cordenier, A.; Maglathlin, R.L.; Webster, J.A.; Lewis, T.A.; O’Kane, C.J.; Schreiber, S.L.; et al. Small molecules enhance autophagy and reduce toxicity in Huntington’s disease models. Nat. Chem. Biol. 2007, 3, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.S.; Holzbaur, E.L.F. Autophagy and mitophagy in ALS. Neurobiol. Dis. 2018, 122, 35–40. [Google Scholar] [CrossRef]
- Sikorska, B.; Liberski, P.P.; Giraud, P.; Kopp, N.; Brown, P. Autophagy is a part of ultrastructural synaptic pathology in Creutzfeldt-Jakob disease: A brain biopsy study. Int. J. Biochem. Cell Biol. 2004, 36, 2563–2573. [Google Scholar] [CrossRef]
- Heiseke, A.; Aguib, Y.; Riemer, C.; Baier, M.; Schatzl, H.M. Lithium induces clearance of protease resistant prion protein in prion-infected cells by induction of autophagy. J. Neurochem. 2009, 109, 25–34. [Google Scholar] [CrossRef]
- Cortes, C.J.; Qin, K.; Norstrom, E.M.; Green, W.N.; Bindokas, V.P.; Mastrianni, J.A. Early Delivery of Misfolded PrP from ER to Lysosomes by Autophagy. Int. J. Cell Biol. 2013, 2013, 560421. [Google Scholar] [CrossRef]
- Kaeberlein, M.; Galvan, V. Rapamycin and Alzheimer’s disease: Time for a clinical trial? Sci. Transl. Med. 2019, 11, eaar4289. [Google Scholar] [CrossRef]
- Malagelada, C.; Jin, Z.H.; Jackson-Lewis, V.; Przedborski, S.; Greene, L.A. Rapamycin protects against neuron death in in vitro and in vivo models of Parkinson’s disease. J. Neurosci. 2010, 30, 1166–1175. [Google Scholar] [CrossRef] [PubMed]
- Spilman, P.; Podlutskaya, N.; Hart, M.J.; Debnath, J.; Gorostiza, O.; Bredesen, D.; Richardson, A.; Strong, R.; Galvan, V. Inhibition of mTOR by rapamycin abolishes cognitive deficits and reduces amyloid-beta levels in a mouse model of Alzheimer’s disease. PLoS ONE 2010, 5, e9979. [Google Scholar] [CrossRef]
- Fornai, F.; Longone, P.; Cafaro, L.; Kastsiuchenka, O.; Ferrucci, M.; Manca, M.L.; Lazzeri, G.; Spalloni, A.; Bellio, N.; Lenzi, P.; et al. Lithium delays progression of amyotrophic lateral sclerosis. Proc. Natl. Acad. Sci. USA 2008, 105, 2052–2057. [Google Scholar] [CrossRef]
- Mandrioli, J.; D’Amico, R.; Zucchi, E.; Gessani, A.; Fini, N.; Fasano, A.; Caponnetto, C.; Chio, A.; Dalla Bella, E.; Lunetta, C.; et al. Rapamycin treatment for amyotrophic lateral sclerosis: Protocol for a phase II randomized, double-blind, placebo-controlled, multicenter, clinical trial (RAP-ALS trial). Medicine (Baltim.) 2018, 97, e11119. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Guan, K.L. mTOR as a central hub of nutrient signalling and cell growth. Nat. Cell Biol. 2019, 21, 63–71. [Google Scholar] [CrossRef]
- Dibble, C.C.; Cantley, L.C. Regulation of mTORC1 by PI3K signaling. Trends Cell Biol. 2015, 25, 545–555. [Google Scholar] [CrossRef]
- Hahn-Windgassen, A.; Nogueira, V.; Chen, C.C.; Skeen, J.E.; Sonenberg, N.; Hay, N. Akt activates the mammalian target of rapamycin by regulating cellular ATP level and AMPK activity. J. Biol. Chem. 2005, 280, 32081–32089. [Google Scholar] [CrossRef]
- Heras-Sandoval, D.; Perez-Rojas, J.M.; Hernandez-Damian, J.; Pedraza-Chaverri, J. The role of PI3K/AKT/mTOR pathway in the modulation of autophagy and the clearance of protein aggregates in neurodegeneration. Cell. Signal. 2014, 26, 2694–2701. [Google Scholar] [CrossRef] [PubMed]
- Manning, B.D.; Cantley, L.C. AKT/PKB signaling: Navigating downstream. Cell 2007, 129, 1261–1274. [Google Scholar] [CrossRef]
- Mizushima, N. The role of the Atg1/ULK1 complex in autophagy regulation. Curr. Opin. Cell Biol. 2010, 22, 132–139. [Google Scholar] [CrossRef]
- Zachari, M.; Ganley, I.G. The mammalian ULK1 complex and autophagy initiation. Essays Biochem. 2017, 61, 585–596. [Google Scholar] [CrossRef]
- Dupont, N.; Chauhan, S.; Arko-Mensah, J.; Castillo, E.F.; Masedunskas, A.; Weigert, R.; Robenek, H.; Proikas-Cezanne, T.; Deretic, V. Neutral lipid stores and lipase PNPLA5 contribute to autophagosome biogenesis. Curr. Biol. 2014, 24, 609–620. [Google Scholar] [CrossRef] [PubMed]
- Hamasaki, M.; Furuta, N.; Matsuda, A.; Nezu, A.; Yamamoto, A.; Fujita, N.; Oomori, H.; Noda, T.; Haraguchi, T.; Hiraoka, Y.; et al. Autophagosomes form at ER-mitochondria contact sites. Nature 2013, 495, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Haobam, B.; Nozawa, T.; Minowa-Nozawa, A.; Tanaka, M.; Oda, S.; Watanabe, T.; Aikawa, C.; Maruyama, F.; Nakagawa, I. Rab17-mediated recycling endosomes contribute to autophagosome formation in response to Group A Streptococcus invasion. Cell Microbiol. 2014, 16, 1806–1821. [Google Scholar] [CrossRef] [PubMed]
- Longatti, A.; Tooze, S.A. Recycling endosomes contribute to autophagosome formation. Autophagy 2012, 8, 1682–1683. [Google Scholar] [CrossRef]
- Orsi, A.; Polson, H.E.; Tooze, S.A. Membrane trafficking events that partake in autophagy. Curr. Opin. Cell Biol. 2010, 22, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Puri, C.; Vicinanza, M.; Rubinsztein, D.C. Phagophores evolve from recycling endosomes. Autophagy 2018, 14, 1475–1477. [Google Scholar] [CrossRef] [PubMed]
- Kirkin, V.; Lamark, T.; Sou, Y.S.; Bjorkoy, G.; Nunn, J.L.; Bruun, J.A.; Shvets, E.; McEwan, D.G.; Clausen, T.H.; Wild, P.; et al. A role for NBR1 in autophagosomal degradation of ubiquitinated substrates. Mol. Cell 2009, 33, 505–516. [Google Scholar] [CrossRef]
- Kabeya, Y.; Mizushima, N.; Ueno, T.; Yamamoto, A.; Kirisako, T.; Noda, T.; Kominami, E.; Ohsumi, Y.; Yoshimori, T. LC3, a mammalian homologue of yeast Apg8p, is localized in autophagosome membranes after processing. EMBO J. 2000, 19, 5720–5728. [Google Scholar] [CrossRef]
- Bjorkoy, G.; Lamark, T.; Brech, A.; Outzen, H.; Perander, M.; Overvatn, A.; Stenmark, H.; Johansen, T. p62/SQSTM1 forms protein aggregates degraded by autophagy and has a protective effect on huntingtin-induced cell death. J. Cell Biol. 2005, 171, 603–614. [Google Scholar] [CrossRef]
- Pankiv, S.; Clausen, T.H.; Lamark, T.; Brech, A.; Bruun, J.A.; Outzen, H.; Overvatn, A.; Bjorkoy, G.; Johansen, T. p62/SQSTM1 binds directly to Atg8/LC3 to facilitate degradation of ubiquitinated protein aggregates by autophagy. J. Biol. Chem. 2007, 282, 24131–24145. [Google Scholar] [CrossRef] [PubMed]
- Kabeya, Y.; Mizushima, N.; Yamamoto, A.; Oshitani-Okamoto, S.; Ohsumi, Y.; Yoshimori, T. LC3, GABARAP and GATE16 localize to autophagosomal membrane depending on form-II formation. J. Cell Sci. 2004, 117, 2805–2812. [Google Scholar] [CrossRef] [PubMed]
- Weidberg, H.; Shvets, E.; Shpilka, T.; Shimron, F.; Shinder, V.; Elazar, Z. LC3 and GATE-16/GABARAP subfamilies are both essential yet act differently in autophagosome biogenesis. EMBO J. 2010, 29, 1792–1802. [Google Scholar] [CrossRef] [PubMed]
- Jahreiss, L.; Menzies, F.M.; Rubinsztein, D.C. The itinerary of autophagosomes: From peripheral formation to kiss-and-run fusion with lysosomes. Traffic 2008, 9, 574–587. [Google Scholar] [CrossRef]
- Kochl, R.; Hu, X.W.; Chan, E.Y.; Tooze, S.A. Microtubules facilitate autophagosome formation and fusion of autophagosomes with endosomes. Traffic 2006, 7, 129–145. [Google Scholar] [CrossRef] [PubMed]
- Parzych, K.R.; Ariosa, A.; Mari, M.; Klionsky, D.J. A newly characterized vacuolar serine carboxypeptidase, Atg42/Ybr139w, is required for normal vacuole function and the terminal steps of autophagy in the yeast Saccharomyces cerevisiae. Mol. Biol. Cell 2018, 29, 1089–1099. [Google Scholar] [CrossRef] [PubMed]
- Epple, U.D.; Eskelinen, E.L.; Thumm, M. Lysis of autophagic vesicles depends on the putative lipase Aut5p. Yeast 2001, 18, S249. [Google Scholar]
- Teter, S.A.; Eggerton, K.P.; Scott, S.V.; Kim, J.; Fischer, A.M.; Klionsky, D.J. Degradation of lipid vesicles in the yeast vacuole requires function of Cvt17, a putative lipase. J. Biol. Chem. 2001, 276, 2083–2087. [Google Scholar] [CrossRef]
- Parzych, K.R.; Klionsky, D.J. Vacuolar hydrolysis and efflux: Current knowledge and unanswered questions. Autophagy 2018, 1–16. [Google Scholar] [CrossRef]
- Sekito, T.; Chardwiriyapreecha, S.; Sugimoto, N.; Ishimoto, M.; Kawano-Kawada, M.; Kakinuma, Y. Vacuolar transporter Avt4 is involved in excretion of basic amino acids from the vacuoles of Saccharomyces cerevisiae. Biosci. Biotechnol. Biochem. 2014, 78, 969–975. [Google Scholar] [CrossRef]
- Yang, Z.F.; Huang, J.; Geng, J.F.; Nair, U.; Klionsky, D.J. Atg22 recycles amino acids to link the degradative and recycling functions of autophagy. Mol. Biol. Cell 2006, 17, 5094–5104. [Google Scholar] [CrossRef] [PubMed]
- Franco-Iborra, S.; Vila, M.; Perier, C. Mitochondrial Quality Control in Neurodegenerative Diseases: Focus on Parkinson’s Disease and Huntington’s Disease. Front. Neurosci. 2018, 12, 342. [Google Scholar] [CrossRef] [PubMed]
- Sherer, T.B.; Betarbet, R.; Stout, A.K.; Lund, S.; Baptista, M.; Panov, A.V.; Cookson, M.R.; Greenamyre, J.T. An in vitro model of Parkinson’s disease: Linking mitochondrial impairment to altered alpha-synuclein metabolism and oxidative damage. J. Neurosci. 2002, 22, 7006–7015. [Google Scholar] [CrossRef] [PubMed]
- Sherer, T.B.; Richardson, J.R.; Testa, C.M.; Seo, B.B.; Panov, A.V.; Yagi, T.; Matsuno-Yagi, A.; Miller, G.W.; Greenamyre, J.T. Mechanism of toxicity of pesticides acting at complex I: Relevance to environmental etiologies of Parkinson’s disease. J. Neurochem. 2007, 100, 1469–1479. [Google Scholar] [CrossRef] [PubMed]
- Abdulwahid Arif, I.; Ahmad Khan, H. Environmental toxins and Parkinson’s disease: Putative roles of impaired electron transport chain and oxidative stress. Toxicol. Ind. Health 2010, 26, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Eiyama, A.; Okamoto, K. PINK1/Parkin-mediated mitophagy in mammalian cells. Curr. Opin. Cell Biol. 2015, 33, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Narendra, D.P.; Jin, S.M.; Tanaka, A.; Suen, D.F.; Gautier, C.A.; Shen, J.; Cookson, M.R.; Youle, R.J. PINK1 is selectively stabilized on impaired mitochondria to activate Parkin. PLoS Biol. 2010, 8, e1000298. [Google Scholar] [CrossRef] [PubMed]
- Itakura, E.; Kishi-Itakura, C.; Koyama-Honda, I.; Mizushima, N. Structures containing Atg9A and the ULK1 complex independently target depolarized mitochondria at initial stages of Parkin-mediated mitophagy. J. Cell Sci. 2012, 125 Pt 6, 1488–1499. [Google Scholar] [CrossRef]
- Ashrafi, G.; Schlehe, J.S.; LaVoie, M.J.; Schwarz, T.L. Mitophagy of damaged mitochondria occurs locally in distal neuronal axons and requires PINK1 and Parkin. J. Cell Biol. 2014, 206, 655–670. [Google Scholar] [CrossRef]
- Youle, R.J.; Narendra, D.P. Mechanisms of mitophagy. Nat. Rev. Mol. Cell Biol. 2011, 12, 9–14. [Google Scholar] [CrossRef]
- Rodolfo, C.; Campello, S.; Cecconi, F. Mitophagy in neurodegenerative diseases. Neurochem. Int. 2018, 117, 156–166. [Google Scholar] [CrossRef]
- Pan, T.; Rawal, P.; Wu, Y.; Xie, W.; Jankovic, J.; Le, W. Rapamycin protects against rotenone-induced apoptosis through autophagy induction. Neuroscience 2009, 164, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Bove, J.; Martinez-Vicente, M.; Dehay, B.; Perier, C.; Recasens, A.; Bombrun, A.; Antonsson, B.; Vila, M. BAX channel activity mediates lysosomal disruption linked to Parkinson disease. Autophagy 2014, 10, 889–900. [Google Scholar] [CrossRef] [PubMed]
- Dehay, B.; Bove, J.; Rodriguez-Muela, N.; Perier, C.; Recasens, A.; Boya, P.; Vila, M. Pathogenic lysosomal depletion in Parkinson’s disease. J. Neurosci. 2010, 30, 12535–12544. [Google Scholar] [CrossRef]
- Hung, Y.H.; Chen, L.M.; Yang, J.Y.; Yang, W.Y. Spatiotemporally controlled induction of autophagy-mediated lysosome turnover. Nat. Commun. 2013, 4, 2111. [Google Scholar] [CrossRef] [PubMed]
- Thurston, T.L.M.; Wandel, M.P.; von Muhlinen, N.; Foeglein, A.; Randow, F. Galectin 8 targets damaged vesicles for autophagy to defend cells against bacterial invasion. Nature 2012, 482, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, C.; Meyer, H. Detection and Clearance of Damaged Lysosomes by the Endo-Lysosomal Damage Response and Lysophagy. Curr. Biol. 2017, 27, R1330–R1341. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, S.; Kumar, S.; Jain, A.; Ponpuak, M.; Mudd, M.H.; Kimura, T.; Choi, S.W.; Peters, R.; Mandell, M.; Bruun, J.A.; et al. TRIMs and Galectins Globally Cooperate and TRIM16 and Galectin-3 Co-direct Autophagy in Endomembrane Damage Homeostasis. Dev. Cell 2016, 39, 13–27. [Google Scholar] [CrossRef]
- Jagust, W. Imaging the evolution and pathophysiology of Alzheimer disease. Nat. Rev. Neurosci. 2018, 19, 687–700. [Google Scholar] [CrossRef]
- Sengupta, I.; Udgaonkar, J.B. Structural mechanisms of oligomer and amyloid fibril formation by the prion protein. Chem. Commun. 2018, 54, 6230–6242. [Google Scholar] [CrossRef]
- Overbye, A.; Fengsrud, M.; Seglen, P.O. Proteomic analysis of membrane-associated proteins from rat liver autophagosomes. Autophagy 2007, 3, 300–322. [Google Scholar] [CrossRef] [PubMed]
- Fortun, J.; Dunn, W.A. Jr.; Joy, S.; Li, J.; Notterpek, L. Emerging role for autophagy in the removal of aggresomes in Schwann cells. J. Neurosci. 2003, 23, 10672–10680. [Google Scholar] [CrossRef] [PubMed]
- Corboy, M.J.; Thomas, P.J.; Wigley, W.C. Aggresome formation. Methods Mol. Biol. 2005, 301, 305–327. [Google Scholar] [PubMed]
- Dehvari, N.; Mahmud, T.; Persson, J.; Bengtsson, T.; Graff, C.; Winblad, B.; Ronnback, A.; Behbahani, H. Amyloid precursor protein accumulates in aggresomes in response to proteasome inhibitor. Neurochem. Int. 2012, 60, 533–542. [Google Scholar] [CrossRef] [PubMed]
- Napoli, E.; Song, G.; Panoutsopoulos, A.; Riyadh, M.A.; Kaushik, G.; Halmai, J.; Levenson, R.; Zarbalis, K.S.; Giulivi, C. Beyond autophagy: A novel role for autism-linked Wdfy3 in brain mitophagy. Sci. Rep. 2018, 8, 11348. [Google Scholar] [CrossRef] [PubMed]
- Clausen, T.H.; Lamark, T.; Isakson, P.; Finley, K.; Larsen, K.B.; Brech, A.; Overvatn, A.; Stenmark, H.; Bjorkoy, G.; Simonsen, A.; et al. p62/SQSTM1 and ALFY interact to facilitate the formation of p62 bodies/ALIS and their degradation by autophagy. Autophagy 2010, 6, 330–344. [Google Scholar] [CrossRef] [PubMed]
- Filimonenko, M.; Isakson, P.; Finley, K.D.; Anderson, M.; Jeong, H.; Melia, T.J.; Bartlett, B.J.; Myers, K.M.; Birkeland, H.C.; Lamark, T.; et al. The selective macroautophagic degradation of aggregated proteins requires the PI3P-binding protein Alfy. Mol. Cell 2010, 38, 265–279. [Google Scholar] [CrossRef]
- Yamamoto, A.; Simonsen, A. Alfy-dependent elimination of aggregated proteins by macroautophagy: Can there be too much of a good thing? Autophagy 2011, 7, 346–350. [Google Scholar] [CrossRef]
- Young, J.E.; Martinez, R.A.; La Spada, A.R. Nutrient deprivation induces neuronal autophagy and implicates reduced insulin signaling in neuroprotective autophagy activation. J. Biol. Chem. 2009, 284, 2363–2373. [Google Scholar] [CrossRef]
- Cloughesy, T.F.; Yoshimoto, K.; Nghiemphu, P.; Brown, K.; Dang, J.; Zhu, S.; Hsueh, T.; Chen, Y.; Wang, W.; Youngkin, D.; et al. Antitumor activity of rapamycin in a Phase I trial for patients with recurrent PTEN-deficient glioblastoma. PLoS Med. 2008, 5, e8. [Google Scholar] [CrossRef]
- Kuhn, J.G.; Chang, S.M.; Wen, P.Y.; Cloughesy, T.F.; Greenberg, H.; Schiff, D.; Conrad, C.; Fink, K.L.; Robins, H.I.; Mehta, M.; et al. Pharmacokinetic and tumor distribution characteristics of temsirolimus in patients with recurrent malignant glioma. Clin. Cancer Res. 2007, 13, 7401–7406. [Google Scholar] [CrossRef] [PubMed]
- Yip, C.K.; Murata, K.; Walz, T.; Sabatini, D.M.; Kang, S.A. Structure of the human mTOR complex I and its implications for rapamycin inhibition. Mol. Cell 2010, 38, 768–774. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, C.; Oberbauer, R. The future role of target of rapamycin inhibitors in renal transplantation. Curr. Opin. Urol. 2002, 12, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Bissler, J.J.; Kingswood, J.C.; Radzikowska, E.; Zonnenberg, B.A.; Belousova, E.; Frost, M.D.; Sauter, M.; Brakemeier, S.; de Vries, P.J.; Berkowitz, N.; et al. Everolimus long-term use in patients with tuberous sclerosis complex: Four-year update of the EXIST-2 study. PLoS ONE 2017, 12, e0180939. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, F.; Albertelli, M.; Grillo, F.; Mohamed, A.; Saveanu, A.; Barlier, A.; Ferone, D.; Florio, T. Neuroendocrine tumors: Insights into innovative therapeutic options and rational development of targeted therapies. Drug Discov. Today 2014, 19, 458–468. [Google Scholar] [CrossRef] [PubMed]
- Berger, Z.; Ravikumar, B.; Menzies, F.M.; Oroz, L.G.; Underwood, B.R.; Pangalos, M.N.; Schmitt, I.; Wullner, U.; Evert, B.O.; O’Kane, C.J.; et al. Rapamycin alleviates toxicity of different aggregate-prone proteins. Hum. Mol. Genet. 2006, 15, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Nakagaki, T.; Satoh, K.; Ishibashi, D.; Fuse, T.; Sano, K.; Kamatari, Y.O.; Kuwata, K.; Shigematsu, K.; Iwamaru, Y.; Takenouchi, T.; et al. FK506 reduces abnormal prion protein through the activation of autolysosomal degradation and prolongs survival in prion-infected mice. Autophagy 2013, 9, 1386–1394. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.H.; Zheng, X.F. Toward rapamycin analog (rapalog)-based precision cancer therapy. Acta Pharmacol. Sin. 2015, 36, 1163–1169. [Google Scholar] [CrossRef]
- Menzies, F.M.; Huebener, J.; Renna, M.; Bonin, M.; Riess, O.; Rubinsztein, D.C. Autophagy induction reduces mutant ataxin-3 levels and toxicity in a mouse model of spinocerebellar ataxia type 3. Brain 2010, 133 Pt 1, 93–104. [Google Scholar] [CrossRef]
- Jiang, T.; Yu, J.T.; Zhu, X.C.; Tan, M.S.; Wang, H.F.; Cao, L.; Zhang, Q.Q.; Shi, J.Q.; Gao, L.; Qin, H.; et al. Temsirolimus promotes autophagic clearance of amyloid-beta and provides protective effects in cellular and animal models of Alzheimer’s disease. Pharmacol. Res. 2014, 81, 54–63. [Google Scholar] [CrossRef]
- Jiang, T.; Yu, J.T.; Zhu, X.C.; Zhang, Q.Q.; Cao, L.; Wang, H.F.; Tan, M.S.; Gao, Q.; Qin, H.; Zhang, Y.D.; et al. Temsirolimus attenuates tauopathy in vitro and in vivo by targeting tau hyperphosphorylation and autophagic clearance. Neuropharmacology 2014, 85, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Frederick, C.; Ando, K.; Leroy, K.; Heraud, C.; Suain, V.; Buee, L.; Brion, J.P. Rapamycin ester analog CCI-779/Temsirolimus alleviates tau pathology and improves motor deficit in mutant tau transgenic mice. J. Alzheimer’s Dis. JAD 2015, 44, 1145–1156. [Google Scholar] [CrossRef] [PubMed]
- Siracusa, R.; Paterniti, I.; Cordaro, M.; Crupi, R.; Bruschetta, G.; Campolo, M.; Cuzzocrea, S.; Esposito, E. Neuroprotective Effects of Temsirolimus in Animal Models of Parkinson’s Disease. Mol. Neurobiol. 2018, 55, 2403–2419. [Google Scholar] [CrossRef] [PubMed]
- Cassano, T.; Magini, A.; Giovagnoli, S.; Polchi, A.; Calcagnini, S.; Pace, L.; Lavecchia, M.A.; Scuderi, C.; Bronzuoli, M.R.; Ruggeri, L.; et al. Early intrathecal infusion of everolimus restores cognitive function and mood in a murine model of Alzheimer’s disease. Exp. Neurol. 2019, 311, 88–105. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, D.; Colombi, M.; Moroni, C.; Hall, M.N. Rapamycin passes the torch: A new generation of mTOR inhibitors. Nat. Rev. Drug Discov. 2011, 10, 868–880. [Google Scholar] [CrossRef] [PubMed]
- Bellozi, P.M.; Lima, I.V.; Doria, J.G.; Vieira, E.L.; Campos, A.C.; Candelario-Jalil, E.; Reis, H.J.; Teixeira, A.L.; Ribeiro, F.M.; de Oliveira, A.C. Neuroprotective effects of the anticancer drug NVP-BEZ235 (dactolisib) on amyloid-beta 1-42 induced neurotoxicity and memory impairment. Sci. Rep. 2016, 6, 25226. [Google Scholar] [CrossRef] [PubMed]
- Thoreen, C.C.; Kang, S.A.; Chang, J.W.; Liu, Q.S.; Zhang, J.M.; Gao, Y.; Reichling, L.J.; Sim, T.B.; Sabatini, D.M.; Gray, N.S. An ATP-competitive Mammalian Target of Rapamycin Inhibitor Reveals Rapamycin-resistant Functions of mTORC1. J. Biol. Chem. 2009, 284, 8023–8032. [Google Scholar] [CrossRef]
- Mason, J.S.; Wileman, T.; Chapman, T. Lifespan extension without fertility reduction following dietary addition of the autophagy activator Torin1 in Drosophila melanogaster. PLoS ONE 2018, 13, e0190105. [Google Scholar] [CrossRef]
- Arbelaez-Quintero, I.; Palacios, M. To Use or Not to Use Metformin in Cerebral Ischemia: A Review of the Application of Metformin in Stroke Rodents. Stroke Res. Treat. 2017, 2017, 9756429. [Google Scholar] [CrossRef]
- Hsu, C.C.; Wahlqvist, M.L.; Lee, M.S.; Tsai, H.N. Incidence of dementia is increased in type 2 diabetes and reduced by the use of sulfonylureas and metformin. J. Alzheimer’s Dis. JAD 2011, 24, 485–493. [Google Scholar] [CrossRef]
- Martin-Montalvo, A.; Mercken, E.M.; Mitchell, S.J.; Palacios, H.H.; Mote, P.L.; Scheibye-Knudsen, M.; Gomes, A.P.; Ward, T.M.; Minor, R.K.; Blouin, M.J.; et al. Metformin improves healthspan and lifespan in mice. Nat. Commun. 2013, 4, 2192. [Google Scholar] [CrossRef] [PubMed]
- Rizos, C.V.; Elisaf, M.S. Metformin and cancer. Eur. J. Pharmacol. 2013, 705, 96–108. [Google Scholar] [CrossRef] [PubMed]
- Wahlqvist, M.L.; Lee, M.S.; Hsu, C.C.; Chuang, S.Y.; Lee, J.T.; Tsai, H.N. Metformin-inclusive sulfonylurea therapy reduces the risk of Parkinson’s disease occurring with Type 2 diabetes in a Taiwanese population cohort. Parkinsonism Relat. Disord. 2012, 18, 753–758. [Google Scholar] [CrossRef] [PubMed]
- Wurth, R.; Barbieri, F.; Florio, T. New molecules and old drugs as emerging approaches to selectively target human glioblastoma cancer stem cells. BioMed Res. Int. 2014, 2014, 126586. [Google Scholar] [CrossRef] [PubMed]
- Cameron, A.R.; Logie, L.; Patel, K.; Erhardt, S.; Bacon, S.; Middleton, P.; Harthill, J.; Forteath, C.; Coats, J.T.; Kerr, C.; et al. Metformin selectively targets redox control of complex I energy transduction. Redox Biol. 2018, 14, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.S.; Li, M.; Ma, T.; Zong, Y.; Cui, J.; Feng, J.W.; Wu, Y.Q.; Lin, S.Y.; Lin, S.C. Metformin Activates AMPK through the Lysosomal Pathway. Cell Metab. 2016, 24, 521–522. [Google Scholar] [CrossRef]
- Tamargo-Gomez, I.; Marino, G. AMPK: Regulation of Metabolic Dynamics in the Context of Autophagy. Int. J. Mol. Sci. 2018, 19, 3812. [Google Scholar] [CrossRef]
- Zhang, C.S.; Lin, S.C. AMPK Promotes Autophagy by Facilitating Mitochondrial Fission. Cell Metab. 2016, 23, 399–401. [Google Scholar] [CrossRef]
- Garcia, D.; Shaw, R.J. AMPK: Mechanisms of Cellular Energy Sensing and Restoration of Metabolic Balance. Mol. Cell 2017, 66, 789–800. [Google Scholar] [CrossRef]
- Curry, D.W.; Stutz, B.; Andrews, Z.B.; Elsworth, J.D. Targeting AMPK Signaling as a Neuroprotective Strategy in Parkinson’s Disease. J. Parkinson’s Dis. 2018, 8, 161–181. [Google Scholar] [CrossRef]
- Lu, M.; Su, C.J.; Qiao, C.; Bian, Y.Q.; Ding, J.H.; Hu, G. Metformin Prevents Dopaminergic Neuron Death in MPTP/P-Induced Mouse Model of Parkinson’s Disease via Autophagy and Mitochondrial ROS Clearance. Int. J. Neuropsychopharmacol. 2016, 19, pyw047. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.S.; Park, C.; Jeong, J.W. AMP-activated protein kinase is activated in Parkinson’s disease models mediated by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine. Biochem. Biophys. Res. Commun. 2010, 391, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Tayara, K.; Espinosa-Oliva, A.M.; Garcia-Dominguez, I.; Ismaiel, A.A.; Boza-Serrano, A.; Deierborg, T.; Machado, A.; Herrera, A.J.; Venero, J.L.; de Pablos, R.M. Divergent Effects of Metformin on an Inflammatory Model of Parkinson’s Disease. Front. Cell. Neurosci. 2018, 12, 440. [Google Scholar] [CrossRef] [PubMed]
- Koenig, A.M.; Mechanic-Hamilton, D.; Xie, S.X.; Combs, M.F.; Cappola, A.R.; Xie, L.; Detre, J.A.; Wolk, D.A.; Arnold, S.E. Effects of the Insulin Sensitizer Metformin in Alzheimer Disease: Pilot Data From a Randomized Placebo-controlled Crossover Study. Alzheimer Dis. Assoc. Disord. 2017, 31, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Bertelli, A.A.; Das, D.K. Grapes, wines, resveratrol, and heart health. J. Cardiovasc. Pharmacol. 2009, 54, 468–476. [Google Scholar] [CrossRef] [PubMed]
- Timmers, S.; Konings, E.; Bilet, L.; Houtkooper, R.H.; van de Weijer, T.; Goossens, G.H.; Hoeks, J.; van der Krieken, S.; Ryu, D.; Kersten, S.; et al. Calorie restriction-like effects of 30 days of resveratrol supplementation on energy metabolism and metabolic profile in obese humans. Cell Metab. 2011, 14, 612–622. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, M.L.; Zhou, Y.; Yi, L.; Gao, Y.X.; Ran, L.; Chen, S.H.; Zhang, T.; Zhou, X.; Zou, D.; et al. Resveratrol improves hepatic steatosis by inducing autophagy through the cAMP signaling pathway. Mol. Nutr. Food Res. 2015, 59, 1443–1457. [Google Scholar] [CrossRef]
- Ferretta, A.; Gaballo, A.; Tanzarella, P.; Piccoli, C.; Capitanio, N.; Nico, B.; Annese, T.; Di Paola, M.; Dell’aquila, C.; De Mari, M.; et al. Effect of resveratrol on mitochondrial function: Implications in parkin-associated familiar Parkinson’s disease. Biochim. Biophys. Acta 2014, 1842, 902–915. [Google Scholar] [CrossRef]
- Wang, H.; Jiang, T.; Li, W.; Gao, N.; Zhang, T. Resveratrol attenuates oxidative damage through activating mitophagy in an in vitro model of Alzheimer’s disease. Toxicol. Lett. 2018, 282, 100–108. [Google Scholar] [CrossRef]
- Hashimoto, R.; Hough, C.; Nakazawa, T.; Yamamoto, T.; Chuang, D.M. Lithium protection against glutamate excitotoxicity in rat cerebral cortical neurons: Involvement of NMDA receptor inhibition possibly by decreasing NR2B tyrosine phosphorylation. J. Neurochem. 2002, 80, 589–597. [Google Scholar] [CrossRef]
- Hou, L.; Xiong, N.; Liu, L.; Huang, J.; Han, C.; Zhang, G.; Li, J.; Xu, X.; Lin, Z.; Wang, T. Lithium protects dopaminergic cells from rotenone toxicity via autophagy enhancement. BMC Neurosci. 2015, 16, 82. [Google Scholar] [CrossRef] [PubMed]
- Nonaka, S.; Hough, C.J.; Chuang, D.M. Chronic lithium treatment robustly protects neurons in the central nervous system against excitotoxicity by inhibiting N-methyl-D-aspartate receptor-mediated calcium influx. Proc. Natl. Acad. Sci. USA 1998, 95, 2642–2647. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Wang, F.; Zhai, X.; Li, X.H.; He, X.J. Lithium promotes recovery of neurological function after spinal cord injury by inducing autophagy. Neural Regen. Res. 2018, 13, 2191–2199. [Google Scholar] [CrossRef] [PubMed]
- Carmichael, J.; Sugars, K.L.; Bao, Y.P.; Rubinsztein, D.C. Glycogen synthase kinase-3beta inhibitors prevent cellular polyglutamine toxicity caused by the Huntington’s disease mutation. J. Biol. Chem. 2002, 277, 33791–33798. [Google Scholar] [CrossRef] [PubMed]
- Motoi, Y.; Shimada, K.; Ishiguro, K.; Hattori, N. Lithium and autophagy. ACS Chem. Neurosci. 2014, 5, 434–442. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, S.; Floto, R.A.; Berger, Z.; Imarisio, S.; Cordenier, A.; Pasco, M.; Cook, L.J.; Rubinsztein, D.C. Lithium induces autophagy by inhibiting inositol monophosphatase. J. Cell Biol. 2005, 170, 1101–1111. [Google Scholar] [CrossRef] [PubMed]
- Shimada, K.; Motoi, Y.; Ishiguro, K.; Kambe, T.; Matsumoto, S.E.; Itaya, M.; Kunichika, M.; Mori, H.; Shinohara, A.; Chiba, M.; et al. Long-term oral lithium treatment attenuates motor disturbance in tauopathy model mice: Implications of autophagy promotion. Neurobiol. Dis. 2012, 46, 101–108. [Google Scholar] [CrossRef]
- Forlenza, O.V.; Diniz, B.S.; Radanovic, M.; Santos, F.S.; Talib, L.L.; Gattaz, W.F. Disease-modifying properties of long-term lithium treatment for amnestic mild cognitive impairment: Randomised controlled trial. Br. J. Psychiatry 2011, 198, 351–356. [Google Scholar] [CrossRef]
- Maiuri, M.C.; Criollo, A.; Kroemer, G. Crosstalk between apoptosis and autophagy within the Beclin 1 interactome. EMBO J. 2010, 29, 515–516. [Google Scholar] [CrossRef]
- Hooper, C.; Killick, R.; Lovestone, S. The GSK3 hypothesis of Alzheimer’s disease. J. Neurochem. 2008, 104, 1433–1439. [Google Scholar] [CrossRef]
- Hampel, H.; Ewers, M.; Burger, K.; Annas, P.; Mortberg, A.; Bogstedt, A.; Frolich, L.; Schroder, J.; Schonknecht, P.; Riepe, M.W.; et al. Lithium trial in Alzheimer’s disease: A randomized, single-blind, placebo-controlled, multicenter 10-week study. J. Clin. Psychiatry 2009, 70, 922–931. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, A.; Briggs, K.; Poppe, M.; Higgins, A.; Velayudhan, L.; Lovestone, S. A feasibility and tolerability study of lithium in Alzheimer’s disease. Int. J. Geriatr. Psychiatry 2008, 23, 704–711. [Google Scholar] [CrossRef] [PubMed]
- Nunes, P.V.; Forlenza, O.V.; Gattaz, W.F. Lithium and risk for Alzheimer’s disease in elderly patients with bipolar disorder. Br. J. Psychiatry 2007, 190, 359–360. [Google Scholar] [CrossRef] [PubMed]
- Busceti, C.L.; Biagioni, F.; Riozzi, B.; Battaglia, G.; Storto, M.; Cinque, C.; Molinaro, G.; Gradini, R.; Caricasole, A.; Canudas, A.M.; et al. Enhanced tau phosphorylation in the hippocampus of mice treated with 3,4-methylenedioxymethamphetamine (“Ecstasy”). J. Neurosci. 2008, 28, 3234–3245. [Google Scholar] [CrossRef] [PubMed]
- Dill, J.; Wang, H.; Zhou, F.; Li, S. Inactivation of glycogen synthase kinase 3 promotes axonal growth and recovery in the CNS. J. Neurosci. 2008, 28, 8914–8928. [Google Scholar] [CrossRef] [PubMed]
- Feng, H.L.; Leng, Y.; Ma, C.H.; Zhang, J.; Ren, M.; Chuang, D.M. Combined lithium and valproate treatment delays disease onset, reduces neurological deficits and prolongs survival in an amyotrophic lateral sclerosis mouse model. Neuroscience 2008, 155, 567–572. [Google Scholar] [CrossRef] [PubMed]
- Chio, A.; Mora, G. The final chapter of the ALS lithium saga. Lancet Neurol. 2013, 12, 324–325. [Google Scholar] [CrossRef]
- Fornai, F.; Longone, P.; Ferrucci, M.; Lenzi, P.; Isidoro, C.; Ruggieri, S.; Paparelli, A. Autophagy and amyotrophic lateral sclerosis: The multiple roles of lithium. Autophagy 2008, 4, 527–530. [Google Scholar] [CrossRef]
- Kim, Y.H.; Rane, A.; Lussier, S.; Andersen, J.K. Lithium protects against oxidative stress-mediated cell death in alpha-synuclein-overexpressing in vitro and in vivo models of Parkinson’s disease. J. Neurosci. Res. 2011, 89, 1666–1675. [Google Scholar] [CrossRef]
- Williams, R.S.; Cheng, L.; Mudge, A.W.; Harwood, A.J. A common mechanism of action for three mood-stabilizing drugs. Nature 2002, 417, 292–295. [Google Scholar] [CrossRef]
- Xiong, N.; Jia, M.; Chen, C.; Xiong, J.; Zhang, Z.; Huang, J.; Hou, L.; Yang, H.; Cao, X.; Liang, Z.; et al. Potential autophagy enhancers attenuate rotenone-induced toxicity in SH-SY5Y. Neuroscience 2011, 199, 292–302. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wu, J.Y.; Weng, L.H.; Li, X.X.; Yu, L.J.; Xu, Y. Valproic acid protects against MPP(+)-mediated neurotoxicity in SH-SY5Y Cells through autophagy. Neurosci. Lett. 2017, 638, 60–68. [Google Scholar] [CrossRef]
- Li, L.; Zhang, S.; Zhang, X.; Li, T.; Tang, Y.; Liu, H.; Yang, W.; Le, W. Autophagy enhancer carbamazepine alleviates memory deficits and cerebral amyloid-beta pathology in a mouse model of Alzheimer’s disease. Curr. Alzheimer Res. 2013, 10, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.J.; Zhou, Q.M.; Chen, S.; Le, W.D. Repurposing carbamazepine for the treatment of amyotrophic lateral sclerosis in SOD1-G93A mouse model. CNS Neurosci. Ther. 2018, 24, 1163–1174. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, S.; Krishna, G.; Imarisio, S.; Saiki, S.; O’Kane, C.J.; Rubinsztein, D.C. A rational mechanism for combination treatment of Huntington’s disease using lithium and rapamycin. Hum. Mol. Genet. 2008, 17, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Arguelles, J.C. Physiological roles of trehalose in bacteria and yeasts: A comparative analysis. Arch. Microbiol. 2000, 174, 217–224. [Google Scholar]
- Kaushik, J.K.; Bhat, R. Why is trehalose an exceptional protein stabilizer? An analysis of the thermal stability of proteins in the presence of the compatible osmolyte trehalose. J. Biol. Chem. 2003, 278, 26458–26465. [Google Scholar] [CrossRef]
- Lee, H.J.; Yoon, Y.S.; Lee, S.J. Mechanism of neuroprotection by trehalose: Controversy surrounding autophagy induction. Cell Death Dis. 2018, 9, 712. [Google Scholar] [CrossRef]
- Wolkers, W.F.; Walker, N.J.; Tablin, F.; Crowe, J.H. Human platelets loaded with trehalose survive freeze-drying. Cryobiology 2001, 42, 79–87. [Google Scholar] [CrossRef]
- Arora, A.; Ha, C.; Park, C.B. Inhibition of insulin amyloid formation by small stress molecules. FEBS Lett. 2004, 564, 121–125. [Google Scholar] [CrossRef]
- Liu, R.; Barkhordarian, H.; Emadi, S.; Park, C.B.; Sierks, M.R. Trehalose differentially inhibits aggregation and neurotoxicity of beta-amyloid 40 and 42. Neurobiol. Dis. 2005, 20, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Machida, Y.; Niu, S.; Ikeda, T.; Jana, N.R.; Doi, H.; Kurosawa, M.; Nekooki, M.; Nukina, N. Trehalose alleviates polyglutamine-mediated pathology in a mouse model of Huntington disease. Nat. Med. 2004, 10, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Casarejos, M.J.; Solano, R.M.; Gomez, A.; Perucho, J.; de Yebenes, J.G.; Mena, M.A. The accumulation of neurotoxic proteins, induced by proteasome inhibition, is reverted by trehalose, an enhancer of autophagy, in human neuroblastoma cells. Neurochem. Int. 2011, 58, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Castillo, K.; Nassif, M.; Valenzuela, V.; Rojas, F.; Matus, S.; Mercado, G.; Court, F.A.; van Zundert, B.; Hetz, C. Trehalose delays the progression of amyotrophic lateral sclerosis by enhancing autophagy in motoneurons. Autophagy 2013, 9, 1308–1320. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Navarro, J.A.; Rodriguez, L.; Casarejos, M.J.; Solano, R.M.; Gomez, A.; Perucho, J.; Cuervo, A.M.; Garcia de Yebenes, J.; Mena, M.A. Trehalose ameliorates dopaminergic and tau pathology in parkin deleted/tau overexpressing mice through autophagy activation. Neurobiol. Dis. 2010, 39, 423–438. [Google Scholar] [CrossRef] [PubMed]
- Rusmini, P.; Cortese, K.; Crippa, V.; Cristofani, R.; Cicardi, M.E.; Ferrari, V.; Vezzoli, G.; Tedesco, B.; Meroni, M.; Messi, E.; et al. Trehalose induces autophagy via lysosomal-mediated TFEB activation in models of motoneuron degeneration. Autophagy 2018, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Tang, Q.; Zheng, G.; Feng, Z.; Chen, Y.; Lou, Y.; Wang, C.; Zhang, X.; Zhang, Y.; Xu, H.; Shang, P.; et al. Trehalose ameliorates oxidative stress-mediated mitochondrial dysfunction and ER stress via selective autophagy stimulation and autophagic flux restoration in osteoarthritis development. Cell Death Dis. 2017, 8, e3081. [Google Scholar] [CrossRef] [PubMed]
- Mizunoe, Y.; Kobayashi, M.; Sudo, Y.; Watanabe, S.; Yasukawa, H.; Natori, D.; Hoshino, A.; Negishi, A.; Okita, N.; Komatsu, M.; et al. Trehalose protects against oxidative stress by regulating the Keap1-Nrf2 and autophagy pathways. Redox Biol. 2018, 15, 115–124. [Google Scholar] [CrossRef]
- DeBosch, B.J.; Heitmeier, M.R.; Mayer, A.L.; Higgins, C.B.; Crowley, J.R.; Kraft, T.E.; Chi, M.; Newberry, E.P.; Chen, Z.; Finck, B.N.; et al. Trehalose inhibits solute carrier 2A (SLC2A) proteins to induce autophagy and prevent hepatic steatosis. Sci. Signal. 2016, 9, ra21. [Google Scholar] [CrossRef]
- Mardones, P.; Rubinsztein, D.C.; Hetz, C. Mystery solved: Trehalose kickstarts autophagy by blocking glucose transport. Sci. Signal. 2016, 9, fs2. [Google Scholar] [CrossRef]
- Aguib, Y.; Heiseke, A.; Gilch, S.; Riemer, C.; Baier, M.; Schatzl, H.M.; Ertmer, A. Autophagy induction by trehalose counteracts cellular prion infection. Autophagy 2009, 5, 361–369. [Google Scholar] [CrossRef]
- Pupyshev, A.B.; Tikhonova, M.A.; Akopyan, A.A.; Tenditnik, M.V.; Dubrovina, N.I.; Korolenko, T.A. Therapeutic activation of autophagy by combined treatment with rapamycin and trehalose in a mouse MPTP-induced model of Parkinson’s disease. Pharmacol. Biochem. Behav. 2018, 177, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, S.; Rubinsztein, D.C. Small molecule enhancers of autophagy for neurodegenerative diseases. Mol. Biosyst. 2008, 4, 895–901. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Yu, J.; Pan, H.; Hu, P.; Hao, Y.; Cai, W.; Zhu, H.; Yu, A.D.; Xie, X.; Ma, D.; et al. Small molecule regulators of autophagy identified by an image-based high-throughput screen. Proc. Natl. Acad. Sci. USA 2007, 104, 19023–19028. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.; Sarkar, S.; Cuddon, P.; Ttofi, E.K.; Saiki, S.; Siddiqi, F.H.; Jahreiss, L.; Fleming, A.; Pask, D.; Goldsmith, P.; et al. Novel targets for Huntington’s disease in an mTOR-independent autophagy pathway. Nat. Chem. Biol. 2008, 4, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Escobar, K.A.; Cole, N.H.; Mermier, C.M.; VanDusseldorp, T.A. Autophagy and aging: Maintaining the proteome through exercise and caloric restriction. Aging Cell 2019, 18, e12876. [Google Scholar] [CrossRef] [PubMed]
- Mattson, M.P.; Arumugam, T.V. Hallmarks of Brain Aging: Adaptive and Pathological Modification by Metabolic States. Cell Metab. 2018, 27, 1176–1199. [Google Scholar] [CrossRef]
- Hara, T.; Nakamura, K.; Matsui, M.; Yamamoto, A.; Nakahara, Y.; Suzuki-Migishima, R.; Yokoyama, M.; Mishima, K.; Saito, I.; Okano, H.; et al. Suppression of basal autophagy in neural cells causes neurodegenerative disease in mice. Nature 2006, 441, 885–889. [Google Scholar] [CrossRef]
- Grune, T. Oxidative stress, aging and the proteasomal system. Biogerontology 2000, 1, 31–40. [Google Scholar] [CrossRef]
- Kastle, M.; Grune, T. Protein oxidative modification in the aging organism and the role of the ubiquitin proteasomal system. Curr. Pharm. Des. 2011, 17, 4007–4022. [Google Scholar] [CrossRef]
- Shetty, A.K.; Kodali, M.; Upadhya, R.; Madhu, L.N. Emerging Anti-Aging Strategies—Scientific Basis and Efficacy. Aging Dis. 2018, 9, 1165–1184. [Google Scholar] [CrossRef] [PubMed]
- Forloni, G.; Tettamanti, M.; Lucca, U.; Albanese, Y.; Quaglio, E.; Chiesa, R.; Erbetta, A.; Villani, F.; Redaelli, V.; Tagliavini, F.; et al. Preventive study in subjects at risk of fatal familial insomnia: Innovative approach to rare diseases. Prion 2015, 9, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.; Macchi, G.; Porro, M.; Giaccone, G.; Bugiani, M.; Scarpini, E.; Scarlato, G.; Molini, G.E.; Sasanelli, F.; Bugiani, O.; et al. Fatal familial insomnia: Genetic, neuropathologic, and biochemical study of a patient from a new Italian kindred. Neurology 1998, 50, 688–692. [Google Scholar] [CrossRef] [PubMed]
- Kahan, B. Toxicity spectrum of inhibitors of mammalian target of rapamycin in organ transplantation: Etiology, pathogenesis and treatment. Expert Opin. Drug Saf. 2011, 10, 727–749. [Google Scholar] [CrossRef] [PubMed]
- Wermke, M.; Schuster, C.; Nolte, F.; Al-Ali, H.K.; Kiewe, P.; Schonefeldt, C.; Jakob, C.; von Bonin, M.; Hentschel, L.; Klut, I.M.; et al. Mammalian-target of rapamycin inhibition with temsirolimus in myelodysplastic syndromes (MDS) patients is associated with considerable toxicity: Results of the temsirolimus pilot trial by the German MDS Study Group (D-MDS). Br. J. Haematol. 2016, 175, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Huang, Y.; Zheng, W.; Yan, J.; Cheng, M.; Zhao, R.; Chen, L.; Hu, C.; Jia, W. Resveratrol reduces intracellular reactive oxygen species levels by inducing autophagy through the AMPK-mTOR pathway. Front. Med. 2018, 12, 697–706. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).