Molecular Mechanisms and Determinants of Innovative Correction Approaches in Coagulation Factor Deficiencies
Abstract
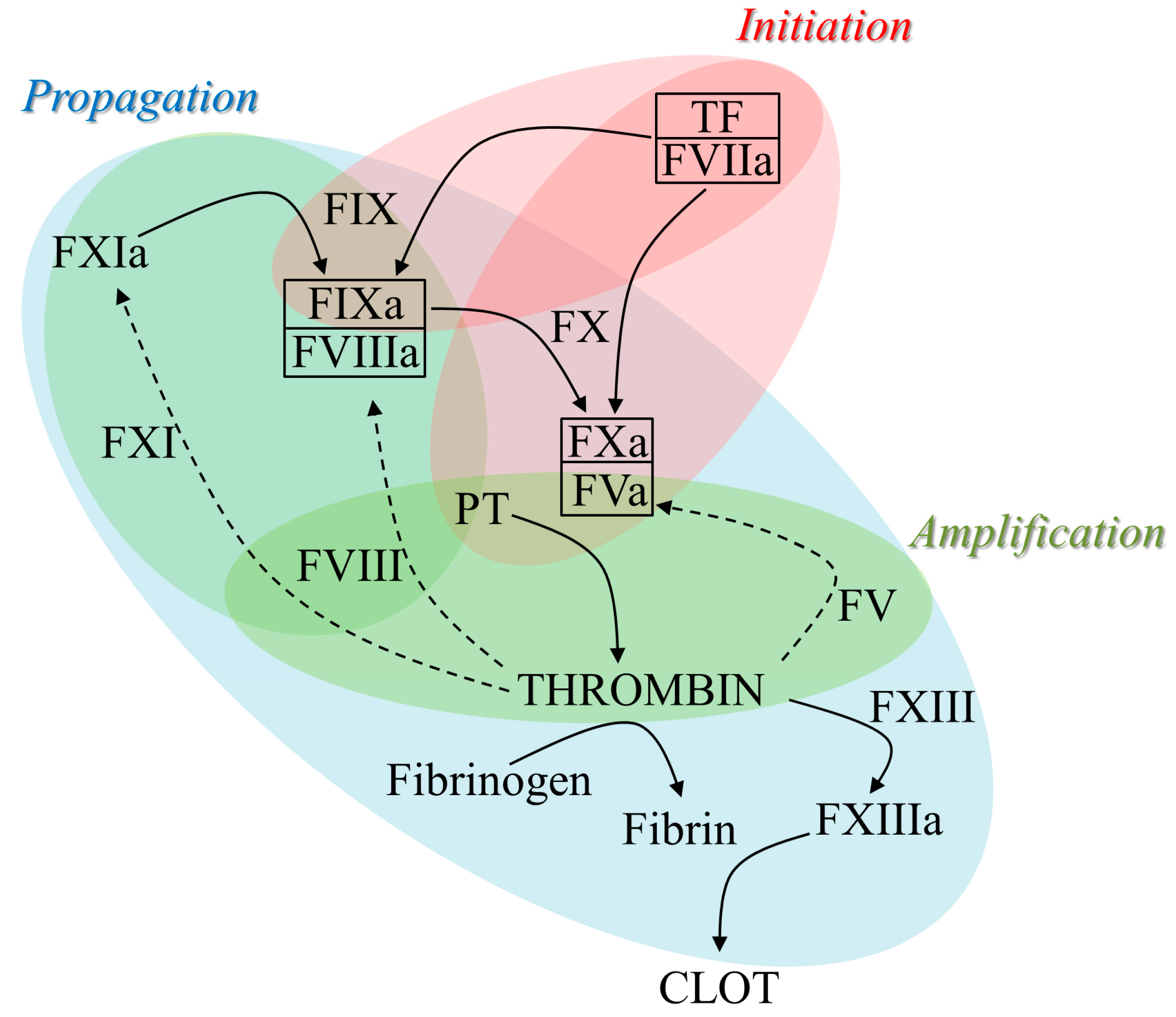
1. Blood Coagulation and Hemorrhagic Disorders
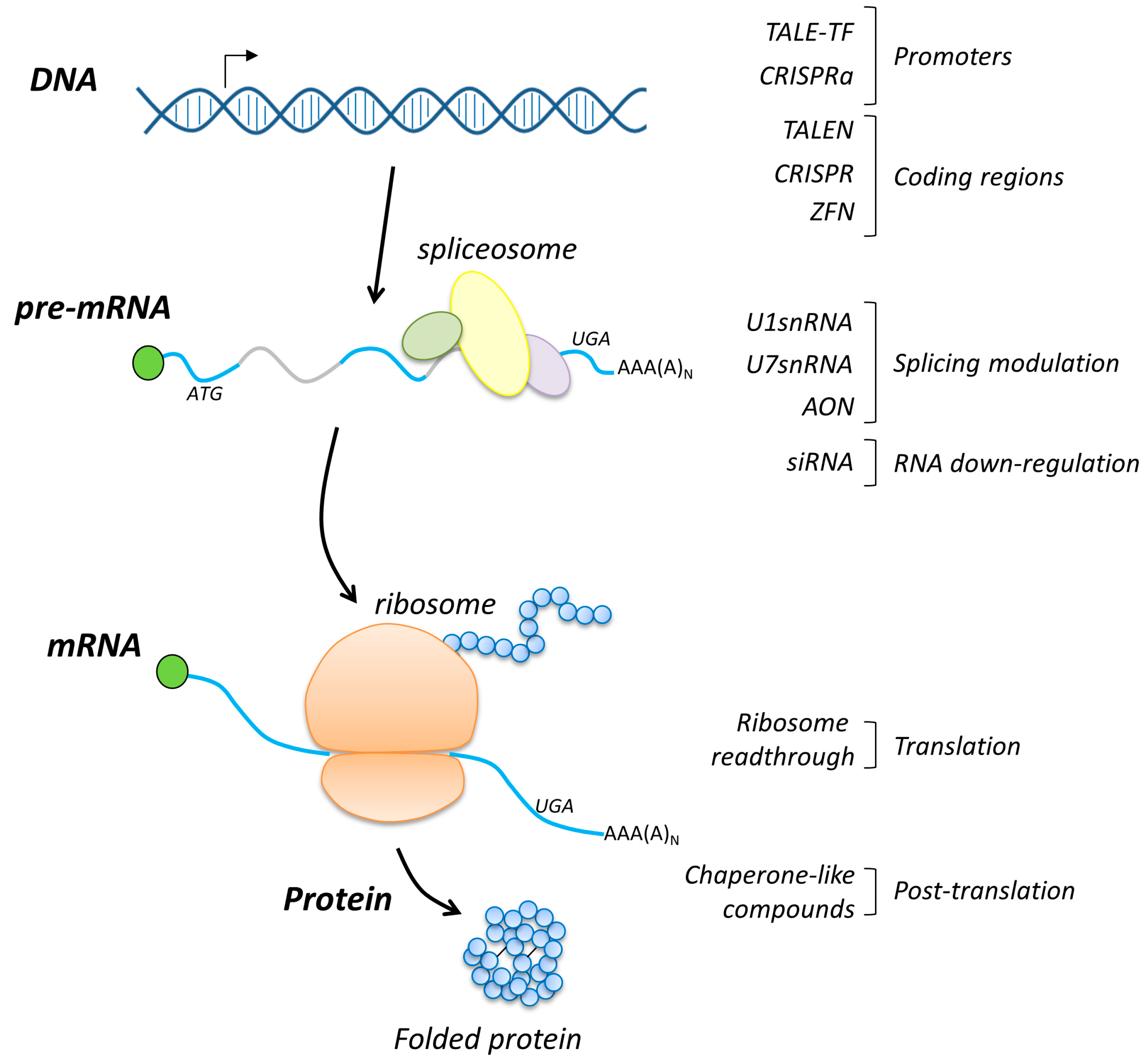
2. Overview of Correction Approaches at DNA, mRNA and Protein Levels
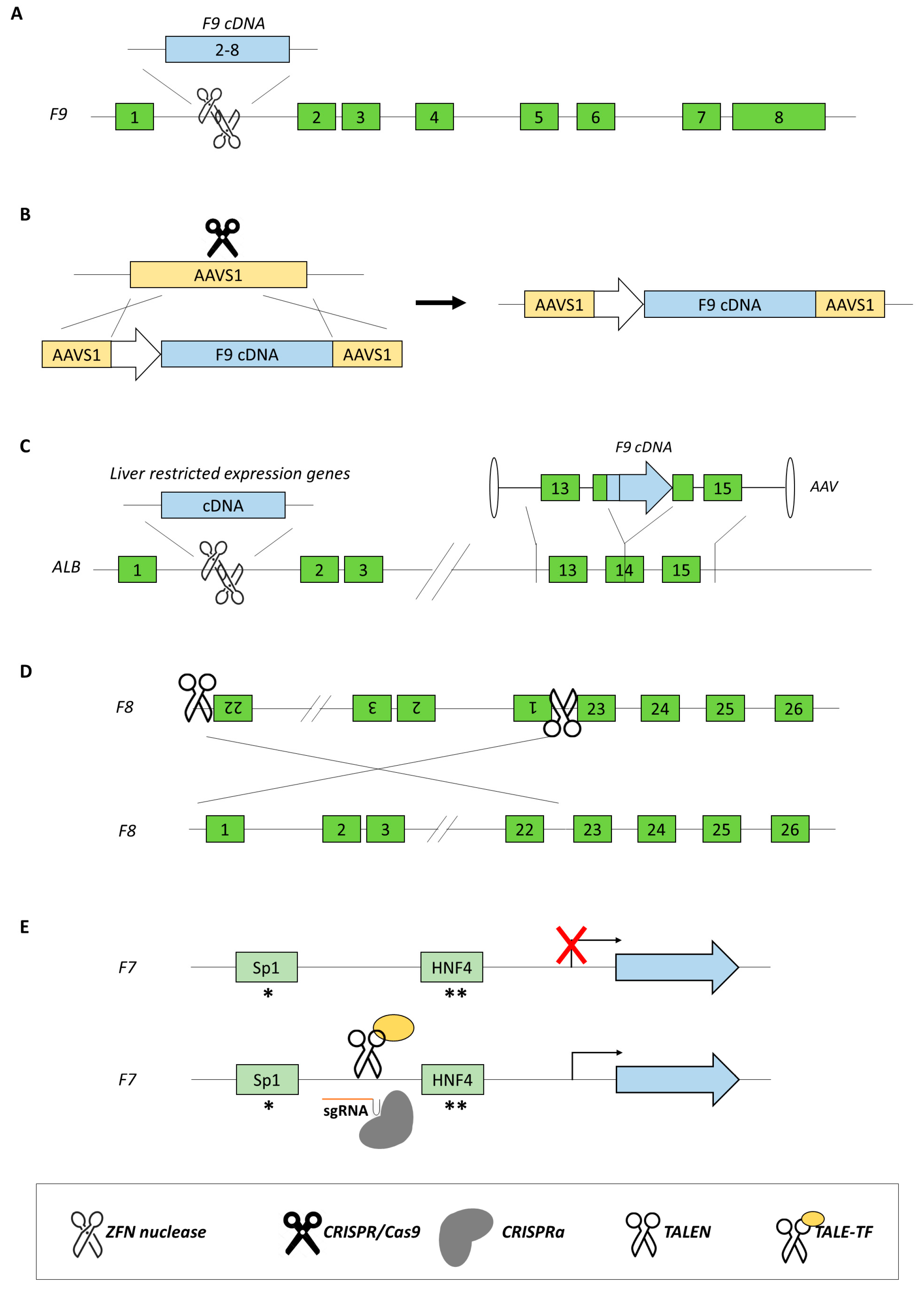
3. Rescue of Coagulation Factor Genes at the DNA Level
3.1. Gene Replacement
3.2. Gene Addition
3.3. New Approaches for Inversions
3.4. New Approaches for Point Mutations
3.5. Approaches for Promoter Transactivation
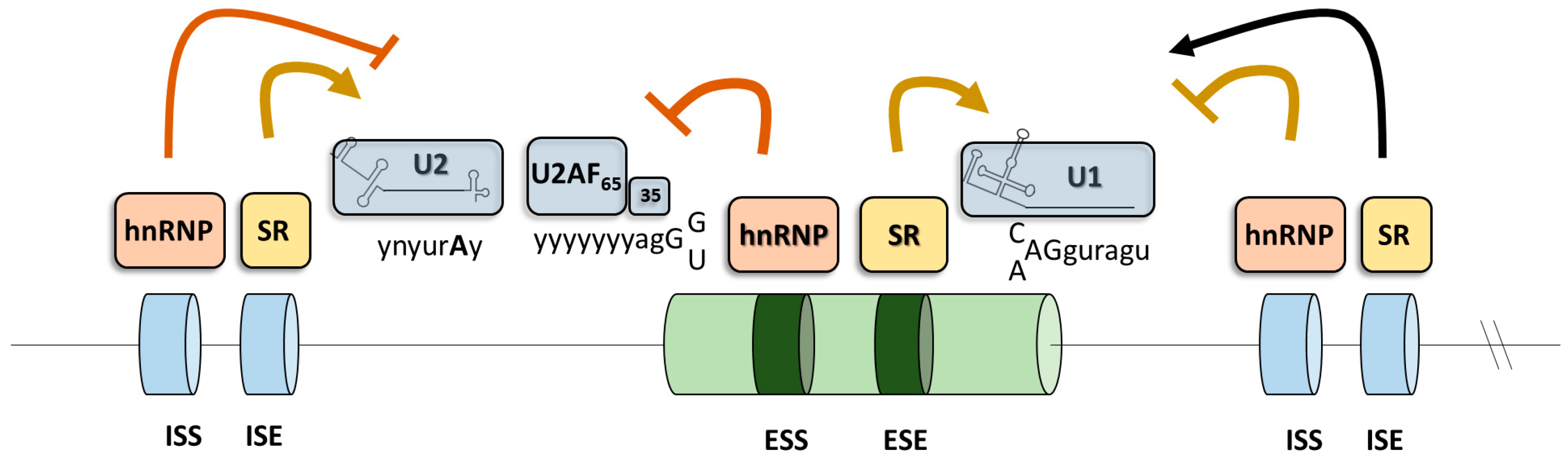
4. Modulation of Splicing for Therapeutic Purposes
4.1. The Splicing Process
4.2. Altered Splicing in Human Diseases
4.3. U1 snRNP
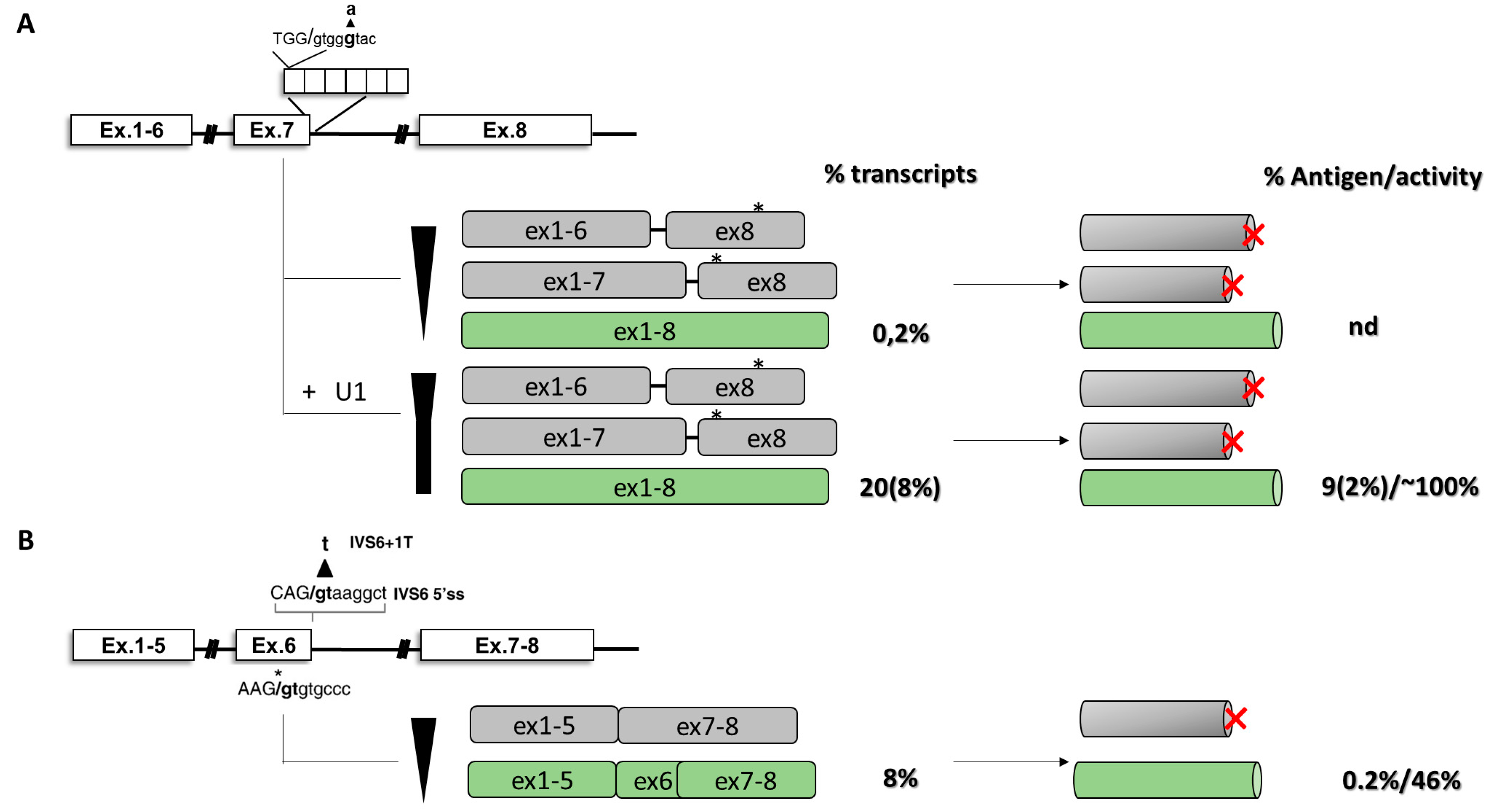
4.4. Compensatory U1 snRNA to Rescue Splicing
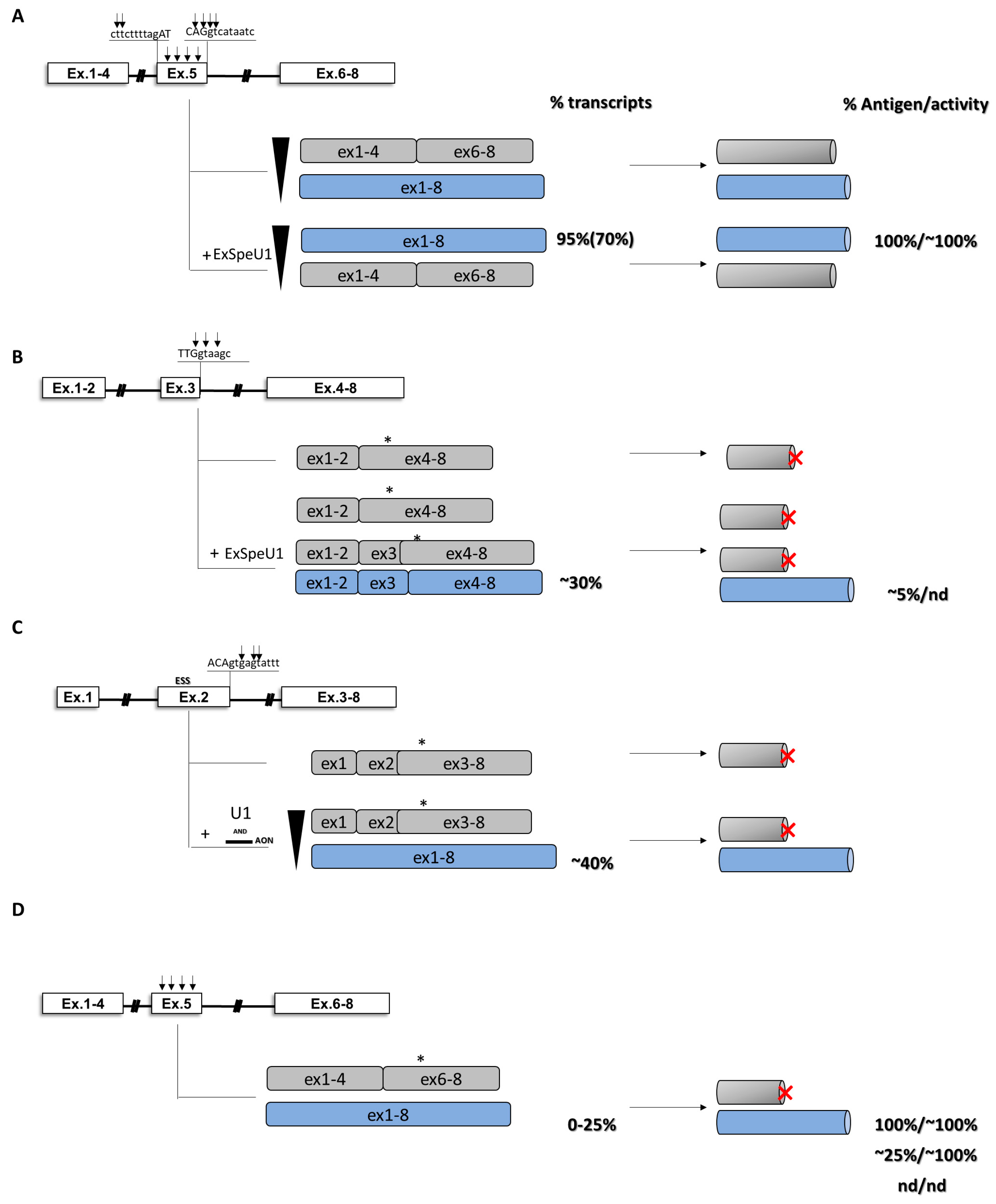
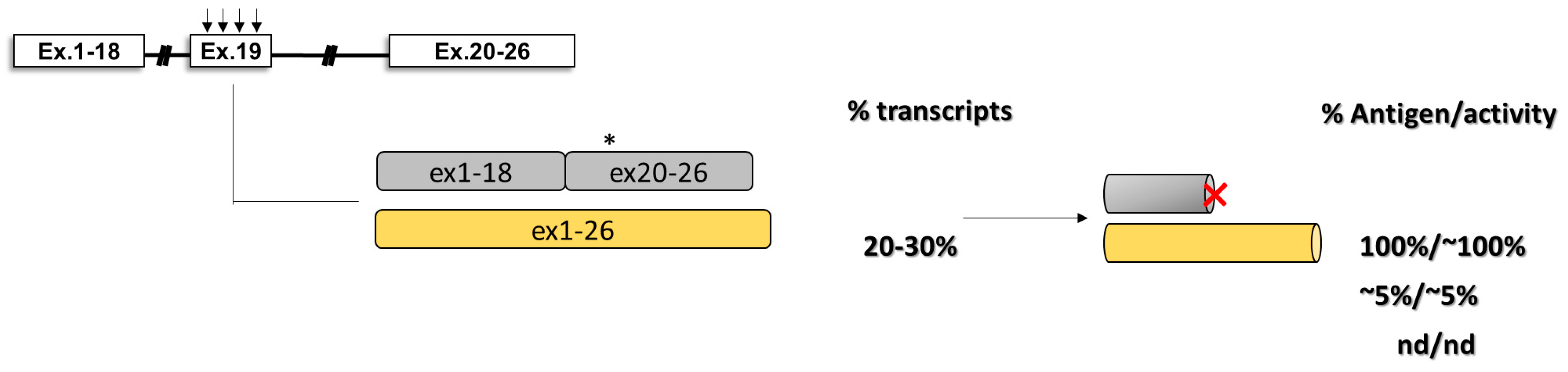
4.5. Exon-Specific U1 snRNAs (ExSpeU1)
4.6. Combination of Modified U1snRNAs and Antisense Oligonucleotides
4.7. Missense Mutations and Altered Splicing
4.8. Antisense Approaches for Splicing Modulation
4.9. Intervention at the RNA Level by siRNAs
5. Rescue of Coagulation Factor Expression by Translational and Post-Translational Modulation
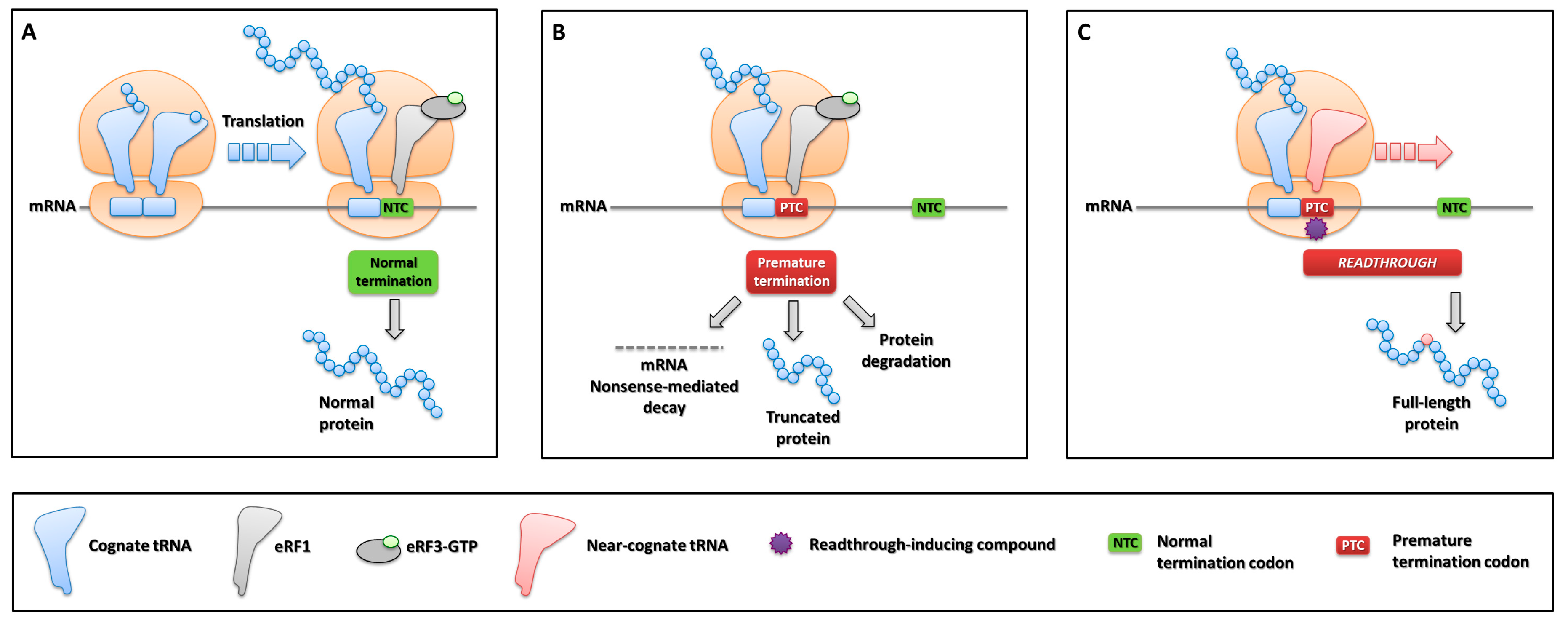
5.1. Translation Termination, Nonsense Mutations and Ribosome Readthrough
5.2. Nonsense Mutations in Coagulation Factor Genes
5.3. Pioneer Studies on Readthrough in Bleeding Disorders
5.4. Investigation of Readthrough Determinants in Bleeding Disorders
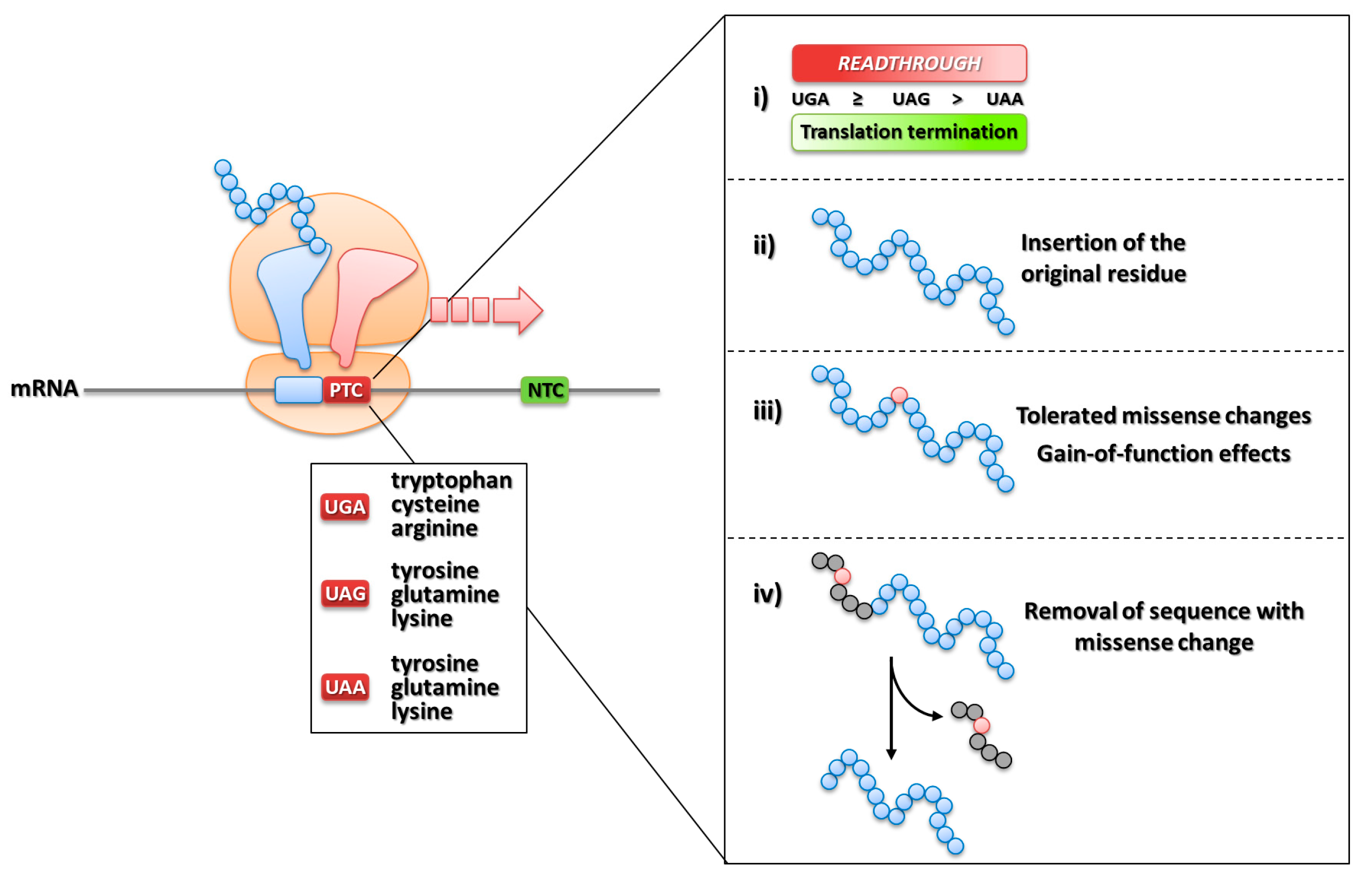
5.5. Molecular Determinants Underlying Productive Readthrough over PTCs
- (i)
- the degree of the susceptibility of sequence contexts to suppression, also promoted by the presence of readthrough-inducing compounds;
- (ii)
- the insertion of the original residue permitting the synthesis of a wild-type full-length protein;
- (iii)
- the insertion of amino acids tolerated for protein synthesis and function, or originating rare gain-of-function features providing advantageous protein outputs;
- (iv)
- the favorable localization of nonsense mutations in protein sequences (i.e., signal peptides) that are removed during processing.
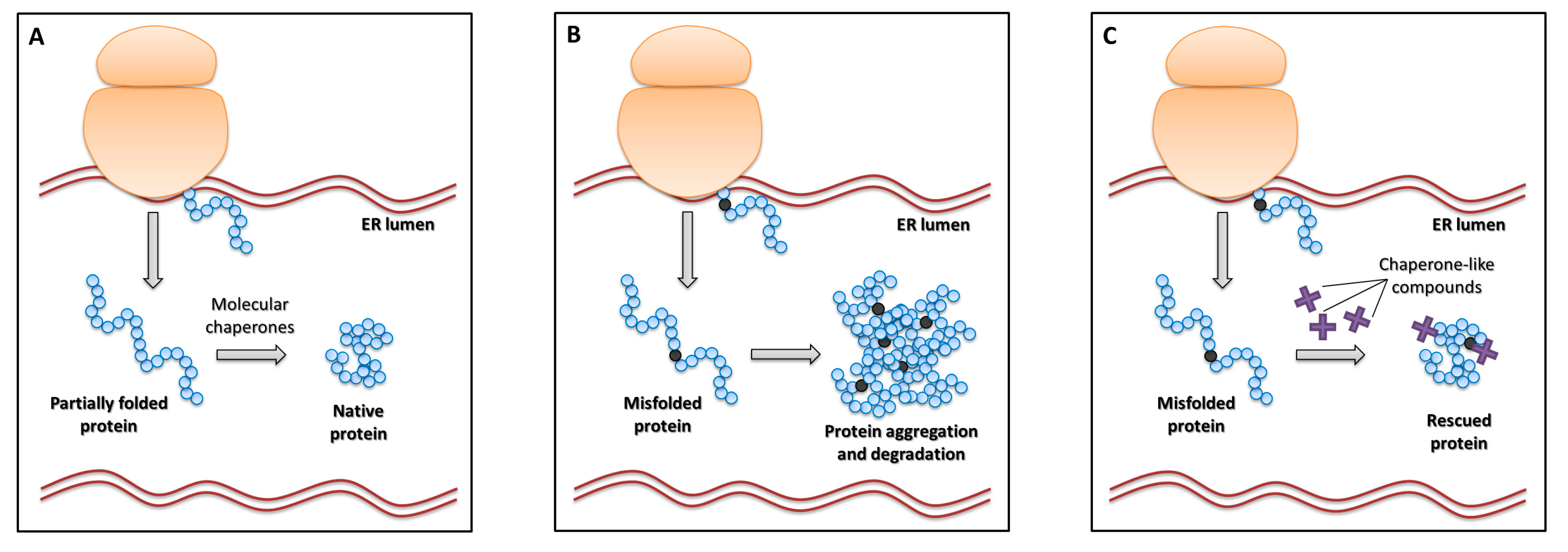
5.6. Protein Folding Defects and Chaperone-Like Compounds
5.7. Intervention on Defective Protein Folding in Bleeding Disorders through Chaperone-Like Compounds
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Monroe, D.M.; Hoffman, M. What Does It Take to Make the Perfect Clot? Arterioscler. Thromb. Vasc. Biol. 2006, 26, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Bolton-Maggs, P.H.B.; Pasi, K.J. Haemophilias A and B. Lancet 2003, 361, 1801–1809. [Google Scholar] [CrossRef]
- Giannelli, F.; Green, P.M.; Sommer, S.S.; Poon, M.-C.; Ludwig, M.; Schwaab, R.; Reitsma, P.H.; Goossens, M.; Yoshioka, A.; Figueiredo, M.S.; et al. Haemophilia B: Database of point mutations and short additions and deletions, 7th edition. Nucleic Acids Res. 1997, 25, 133–135. [Google Scholar] [CrossRef] [PubMed]
- Payne, A.B.; Miller, C.H.; Kelly, F.M.; Michael Soucie, J.; Craig Hooper, W. The CDC Hemophilia A Mutation Project (CHAMP) Mutation List: A New Online Resource. Hum. Mutat. 2012, 34, E2382–E2392. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Miller, C.H.; Payne, A.B.; Craig Hooper, W. The CDC Hemophilia B mutation project mutation list: A new online resource. Mol. Genet. Genomic Med. 2013, 1, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Antonarakis, S.E.; Kazazian, H.H.; Tuddenham, E.G.D. Molecular etiology of factor VIII deficiency in hemophilia A. Hum. Mutat. 1995, 5, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Mannucci, P.M. Recessively inherited coagulation disorders. Blood 2004, 104, 1243–1252. [Google Scholar] [CrossRef]
- Palla, R.; Peyvandi, F.; Shapiro, A.D. Rare bleeding disorders: Diagnosis and treatment. Blood 2015, 125, 2052–2061. [Google Scholar] [CrossRef]
- Rosen, E.D.; Chan, J.C.Y.Y.; Idusogie, E.; Clotman, F.; Vlasuk, G.; Luther, T.; Jalbert, L.R.; Albrecht, S.; Zhong, L.; Lissens, A.; et al. Mice lacking factor VII develop normally but suffer fatal perinatal bleeding. Nature 1997, 390, 290–294. [Google Scholar] [CrossRef]
- Dewerchin, M.; Liang, Z.; Moons, L.; Carmeliet, P.; Castellino, F.; Collen, D.; Rosen, E. Blood Coagulation Factor X Deficiency Causes Partial Embryonic Lethality and Fatal Neonatal Bleeding in Mice. Thromb. Haemost. 2000, 83, 185–190. [Google Scholar] [CrossRef]
- Xue, J.; Wu, Q.; Westfield, L.A.; Tuley, E.A.; Lu, D.; Zhang, Q.; Shim, K.; Zheng, X.; Sadler, J.E. Incomplete embryonic lethality and fatal neonatal hemorrhage caused by prothrombin deficiency in mice. Proc. Natl. Acad. Sci. USA 1998, 95, 7603–7607. [Google Scholar] [CrossRef] [PubMed]
- Mullins, E.S.; Kombrinck, K.W.; Talmage, K.E.; Shaw, M.A.; Witte, D.P.; Ullman, J.M.; Degen, S.J.; Sun, W.; Flick, M.J.; Degen, J.L. Genetic elimination of prothrombin in adult mice is not compatible with survival and results in spontaneous hemorrhagic events in both heart and brain. Blood 2008, 113, 696–704. [Google Scholar] [CrossRef] [PubMed]
- Salomon, O.; Steinberg, D.M.; Seligshon, U. Variable bleeding manifestations characterize different types of surgery in patients with severe factor XI deficiency enabling parsimonious use of replacement therapy. Haemophilia 2006, 12, 490–493. [Google Scholar] [CrossRef] [PubMed]
- Menegatti, M.; Peyvandi, F. Treatment of rare factor deficiencies other than hemophilia. Blood 2018, 133, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Magee, G.; Zbrozek, A. Fluid overload is associated with increases in length of stay and hospital costs: Pooled analysis of data from more than 600 US hospitals. Clin. Outcomes Res. 2013, 5, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, B.; Spahn, D.R.; Innerhofer, P.; Spannagl, M.; Rossaint, R. Clinical review: Prothrombin complex concentrates - evaluation of safety and thrombogenicity. Crit. Care 2011, 15, 201. [Google Scholar] [CrossRef]
- Shapiro, A. Plasma-derived human factor X concentrate for on-demand and perioperative treatment in factor X-deficient patients: Pharmacology, pharmacokinetics, efficacy, and safety. Expert Opin. Drug Metab. Toxicol. 2016, 13, 97–104. [Google Scholar] [CrossRef]
- Lovejoy, A.E. Safety and pharmacokinetics of recombinant factor XIII-A2 administration in patients with congenital factor XIII deficiency. Blood 2006, 108, 57–62. [Google Scholar] [CrossRef]
- Kerlin, B.; Brand, B.; Inbal, A.; Halimeh, S.; Nugent, D.; Lundblad, M.; Tehranchi, R. Pharmacokinetics of recombinant factor XIII at steady state in patients with congenital factor XIII A-subunit deficiency. J. Thromb. Haemost. 2014, 12, 2038–2043. [Google Scholar] [CrossRef]
- Bulato, C.; Novembrino, C.; Anzoletti, M.B.; Spiezia, L.; Gavasso, S.; Berbenni, C.; Tagariello, G.; Farina, C.; Nardini, I.; Campello, E.; et al. “In vitro” correction of the severe factor V deficiency-related coagulopathy by a novel plasma-derived factor V concentrate. Haemophilia 2018, 24, 648–656. [Google Scholar] [CrossRef]
- DiMichele, D. Inhibitor development in haemophilia B: An orphan disease in need of attention. Br. J. Haematol. 2007, 138, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Franchini, M.; Mannucci, P.M. Inhibitors of propagation of coagulation (factors VIII, IX and XI): A review of current therapeutic practice. Br. J. Clin. Pharmacol. 2011, 72, 553–562. [Google Scholar] [CrossRef] [PubMed]
- Persson, E.; Bolt, G.; Steenstrup, T.D.; Ezban, M. Recombinant coagulation factor VIIa – from molecular to clinical aspects of a versatile haemostatic agent. Thromb. Res. 2010, 125, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Kempton, C.L.; Meeks, S.L. Toward optimal therapy for inhibitors in hemophilia. Blood 2014, 124, 3365–3372. [Google Scholar] [CrossRef] [PubMed]
- Mannucci, P.M. Half-life extension technologies for haemostatic agents. Thromb. Haemost. 2015, 113, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Peyvandi, F.; Garagiola, I.; Biguzzi, E. Advances in the treatment of bleeding disorders. J. Thromb. Haemost. 2016, 14, 2095–2106. [Google Scholar] [CrossRef]
- Samelson-Jones, B.J.; Arruda, V.R. Protein-Engineered Coagulation Factors for Hemophilia Gene Therapy. Mol. Ther. Methods Clin. Dev. 2019, 12, 184–201. [Google Scholar] [CrossRef]
- Marcos-Contreras, O.A.; Smith, S.M.; Bellinger, D.A.; Raymer, R.A.; Merricks, E.; Faella, A.; Pavani, G.; Zhou, S.; Nichols, T.C.; High, K.A.; et al. Sustained correction of FVII deficiency in dogs using AAV-mediated expression of zymogen FVII. Blood 2015, 127, 565–571. [Google Scholar] [CrossRef]
- Binny, C.; McIntosh, J.; Della Peruta, M.; Kymalainen, H.; Tuddenham, E.G.D.; Buckley, S.M.K.; Waddington, S.N.; McVey, J.H.; Spence, Y.; Morton, C.L.; et al. AAV-mediated gene transfer in the perinatal period results in expression of FVII at levels that protect against fatal spontaneous hemorrhage. Blood 2012, 119, 957–966. [Google Scholar] [CrossRef]
- Carcao, M.D.; Aledort, L. Prophylactic factor replacement in hemophilia. Blood Rev. 2004, 18, 101–113. [Google Scholar] [CrossRef]
- Kontermann, R.E. Half-life extended biotherapeutics. Expert Opin. Biol. Ther. 2016, 16, 903–915. [Google Scholar] [CrossRef] [PubMed]
- Weimer, T.; Wormsbächer, W.; Kronthaler, U.; Lang, W.; Liebing, U.; Schulte, S. Prolonged in-vivo half-life of factor VIIa by fusion to albumin. Thromb. Haemost. 2008, 99, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Weimer, T.; Kronthaler, U.; Lang, W.; Schulte, S.; Metzner, H.J. Genetic fusion to albumin improves the pharmacokinetic properties of factor IX. Thromb. Haemost. 2009, 102, 634–644. [Google Scholar] [CrossRef] [PubMed]
- Ferrarese, M.; Pignani, S.; Lombardi, S.; Balestra, D.; Bernardi, F.; Pinotti, M.; Branchini, A. The carboxyl-terminal region of human coagulation factor X as a natural linker for fusion strategies. Thromb. Res. 2019, 173, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Millar, D.; Kemball-Cook, G.; McVey, J.; Tuddenham, E.; Mumford, A.; Attock, G.; Reverter, J.; Lanir, N.; Parapia, L.; Reynaud, J.; et al. Molecular analysis of the genotype-phenotype relationship in factor VII deficiency. Hum. Genet. 2000, 107, 327–342. [Google Scholar] [CrossRef] [PubMed]
- Millar, D.S.; Elliston, L.; Deex, P.; Krawczak, M.; Wacey, A.I.; Reynaud, J.; Nieuwenhuis, H.K.; Bolton-Maggs, P.; Mannucci, P.M.; Reverter, J.C.; et al. Molecular analysis of the genotype-phenotype relationship in factor X deficiency. Hum. Genet. 2000, 106, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Shee, C.D. Oxford Textbook of Medicine. J. R. Soc. Med. 2005, 98, 333–334. [Google Scholar] [CrossRef]
- Chuah, M.K.; Evens, H.; VandenDriessche, T. Gene therapy for hemophilia. J. Thromb. Haemost. 2013, 11, 99–110. [Google Scholar] [CrossRef] [PubMed]
- High, K.A. Gene Transfer as an Approach to Treating Hemophilia. Circ. Res. 2001, 88, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Pierce, G.F.; Lillicrap, D.; Pipe, S.W.; Vandendriessche, T. Gene therapy, bioengineered clotting factors and novel technologies for hemophilia treatment. J. Thromb. Haemost. 2007, 5, 901–906. [Google Scholar] [CrossRef]
- Nathwani, A.C.; Reiss, U.M.; Tuddenham, E.G.D.D.; Rosales, C.; Chowdary, P.; McIntosh, J.; Della Peruta, M.; Lheriteau, E.; Patel, N.; Raj, D.; et al. Long-Term Safety and Efficacy of Factor IX Gene Therapy in Hemophilia B. N. Engl. J. Med. 2014, 371, 1994–2004. [Google Scholar] [CrossRef] [PubMed]
- Mingozzi, F.; Büning, H. Adeno-Associated Viral Vectors at the Frontier between Tolerance and Immunity. Front. Immunol. 2015, 6. [Google Scholar] [CrossRef] [PubMed]
- Mariani, G.; Herrmann, F.H.; Schulman, S.; Batorova, A.; Wulff, K.; Etro, D.; Dolce, A.; Auerswald, G.; Astermark, J.; Schved, J.-F.; et al. Thrombosis in inherited factor VII deficiency. J. Thromb. Haemost. 2003, 1, 2153–2158. [Google Scholar] [CrossRef] [PubMed]
- Bonetta, L. RNA-Based Therapeutics: Ready for Delivery? Cell 2009, 136, 581–584. [Google Scholar] [CrossRef] [PubMed]
- Du, L.; Gatti, R.A. Progress toward therapy with antisense-mediated splicing modulation. Curr. Opin. Mol. Ther. 2009, 11, 116–123. [Google Scholar] [PubMed]
- Nlend Nlend, R.; Meyer, K.; Schümperli, D. Repair of pre-mRNA splicing: Prospects for a therapy for spinal muscular atrophy. RNA Biol. 2010, 7, 430–440. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ward, A.J.; Cooper, T.A. The pathobiology of splicing. J. Pathol. 2010, 220, 152–163. [Google Scholar] [CrossRef] [PubMed]
- Hammond, S.M.; Wood, M.J.A. Genetic therapies for RNA mis-splicing diseases. Trends Genet. 2011, 27, 196–205. [Google Scholar] [CrossRef]
- Casari, C.; Pinotti, M.; Lancellotti, S.; Adinolfi, E.; Casonato, A.; De Cristofaro, R.; Bernardi, F. The dominant-negative von Willebrand factor gene deletion p.P1127_C1948delinsR: Molecular mechanism and modulation. Blood 2010, 116, 5371–5376. [Google Scholar] [CrossRef]
- Gaj, T.; Gersbach, C.A.; Barbas, C.F. ZFN, TALEN, and CRISPR/Cas-based methods for genome engineering. Trends Biotechnol. 2013, 31, 397–405. [Google Scholar] [CrossRef]
- Sürün, D.; Kurrle, N.; Serve, H.; von Melchner, H.; Schnütgen, F. High efficiency gene correction in hematopoietic cells by donor-template-free CRISPR/Cas9 genome editing. Exp. Hematol. 2017, 53, S64. [Google Scholar] [CrossRef]
- Sadelain, M.; Papapetrou, E.P.; Bushman, F.D. Safe harbours for the integration of new DNA in the human genome. Nat. Rev. Cancer 2011, 12, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Haurigot, V.; Doyon, Y.; Li, T.; Wong, S.Y.; Bhagwat, A.S.; Malani, N.; Anguela, X.M.; Sharma, R.; Ivanciu, L.; et al. In vivo genome editing restores haemostasis in a mouse model of haemophilia. Nature 2011, 475, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Anguela, X.M.; Sharma, R.; Doyon, Y.; Miller, J.C.; Li, H.; Haurigot, V.; Rohde, M.E.; Wong, S.Y.; Davidson, R.J.; Zhou, S.; et al. Robust ZFN-mediated genome editing in adult hemophilic mice. Blood 2013, 122, 3283–3287. [Google Scholar] [CrossRef] [PubMed]
- Huai, C.; Jia, C.; Sun, R.; Xu, P.; Min, T.; Wang, Q.; Zheng, C.; Chen, H.; Lu, D. CRISPR/Cas9-mediated somatic and germline gene correction to restore hemostasis in hemophilia B mice. Hum. Genet. 2017, 136, 875–883. [Google Scholar] [CrossRef] [PubMed]
- Lyu, C.; Shen, J.; Wang, R.; Gu, H.; Zhang, J.; Xue, F.; Liu, X.; Liu, W.; Fu, R.; Zhang, L.L.L.L.; et al. Targeted genome engineering in human induced pluripotent stem cells from patients with hemophilia B using the CRISPR-Cas9 system. Stem Cell Res. Ther. 2018, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wang, Y.; Hu, Z.; Wu, L.; Zhao, J.; Feng, M.; Li, Z.; Liang, D.; Zhang, Y.; Zhou, M.; et al. Paired CRISPR/Cas9 Nickases Mediate Efficient Site-Specific Integration of F9 into rDNA Locus of Mouse ESCs. Int. J. Mol. Sci. 2018, 19, 3035. [Google Scholar]
- Sharma, R.; Anguela, X.M.; Doyon, Y.; Wechsler, T.; DeKelver, R.C.; Sproul, S.; Paschon, D.E.; Miller, J.C.; Davidson, R.J.; Shivak, D.; et al. In vivo genome editing of the albumin locus as a platform for protein replacement therapy. Blood 2015, 126, 1777–1784. [Google Scholar] [CrossRef]
- Barzel, A.; Paulk, N.K.; Shi, Y.; Huang, Y.; Chu, K.; Zhang, F.; Valdmanis, P.N.; Spector, L.P.; Porteus, M.H.; Gaensler, K.M.; et al. Promoterless gene targeting without nucleases ameliorates haemophilia B in mice. Nature 2014, 517, 360–364. [Google Scholar] [CrossRef]
- Ohmori, T.; Nagao, Y.; Mizukami, H.; Sakata, A.; Muramatsu, S.I.; Ozawa, K.; Tominaga, S.I.; Hanazono, Y.; Nishimura, S.; Nureki, O.; et al. CRISPR/Cas9-mediated genome editing via postnatal administration of AAV vector cures haemophilia B mice. Sci. Rep. 2017, 7, 1–11. [Google Scholar] [CrossRef]
- Park, C.-Y.; Kim, J.; Kweon, J.; Son, J.S.; Lee, J.S.; Yoo, J.-E.; Cho, S.-R.; Kim, J.-H.; Kim, J.-S.; Kim, D.-W. Targeted inversion and reversion of the blood coagulation factor 8 gene in human iPS cells using TALENs. Proc. Natl. Acad. Sci. USA 2014, 111, 9253–9258. [Google Scholar] [CrossRef] [PubMed]
- Park, C.Y.; Kim, D.H.; Son, J.S.; Sung, J.J.; Lee, J.; Bae, S.; Kim, J.H.; Kim, D.W.; Kim, J.S. Functional Correction of Large Factor VIII Gene Chromosomal Inversions in Hemophilia A Patient-Derived iPSCs Using CRISPR-Cas9. Cell Stem Cell 2015, 17, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Guan, Y.; Ma, Y.; Li, Q.; Sun, Z.; Ma, L.; Wu, L.; Wang, L.; Zeng, L.; Shao, Y.; Chen, Y.; et al. CRISPR/Cas9-mediated somatic correction of a novel coagulator factor IX gene mutation ameliorates hemophilia in mouse. EMBO Mol. Med. 2016, 8, 477–488. [Google Scholar] [CrossRef] [PubMed]
- Barbon, E.; Pignani, S.; Branchini, A.; Bernardi, F.; Pinotti, M.; Bovolenta, M. An engineered tale-transcription factor rescues transcription of factor VII impaired by promoter mutations and enhances its endogenous expression in hepatocytes. Sci. Rep. 2016, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Arbini, A.A.; Pollak, E.S.; Bayleran, J.K.; High, K.A.; Bauer, K.A. Severe factor VII deficiency due to a mutation disrupting a hepatocyte nuclear factor 4 binding site in the factor VII promoter. Blood 1997, 89, 176–182. [Google Scholar] [PubMed]
- Carew, J.A.; Pollak, E.S.; High, K.A.; Bauer, K.A. Severe Factor VII Deficiency Due to a Mutation Disrupting an Sp1 Binding Site in the Factor VII Promoter. Blood 1998, 92, 1639–1645. [Google Scholar]
- Pignani, S.; Zappaterra, F.; Barbon, E.; Follenzi, A.; Bovolenta, M.; Bernardi, F.; Branchini, A.; Pinotti, M. Tailoring the CRISPR system to transactivate coagulation gene promoters in normal and mutated contexts. Biochim. Biophys. Acta Gene Regul. Mech. 2019, 1862, 619–624. [Google Scholar] [CrossRef]
- Lander, E.S.; Linton, L.M.; Birren, B.; Nusbaum, C.; Zody, M.C.; Baldwin, J.; Devon, K.; Dewar, K.; Doyle, M.; Fitzhugh, W.; et al. Initial sequencing and analysis of the human genome. Nature 2001, 409, 860–921. [Google Scholar]
- Ramanouskaya, T.V.; Grinev, V.V. The determinants of alternative RNA splicing in human cells. Mol. Genet. Genom. 2017, 292, 1175–1195. [Google Scholar] [CrossRef]
- Pan, Q.; Shai, O.; Lee, L.J.; Frey, B.J.; Blencowe, B.J. Deep surveying of alternative splicing complexity in the human transcriptome by high-throughput sequencing. Nat. Genet. 2008, 40, 1413–1415. [Google Scholar] [CrossRef]
- Barbosa-Morais, N.L.; Irimia, M.; Pan, Q.; Xiong, H.Y.; Gueroussov, S.; Lee, L.J.; Slobodeniuc, V.; Kutter, C.; Watt, S.; Colak, R.; et al. The Evolutionary Landscape of Alternative Splicing in Vertebrate Species. Science (80-) 2012, 338, 1587–1593. [Google Scholar] [CrossRef] [PubMed]
- Merkin, J.; Russell, C.; Chen, P.; Burge, C.B. Evolutionary Dynamics of Gene and Isoform Regulation in Mammalian Tissues. Science (80-) 2012, 338, 1593–1599. [Google Scholar] [CrossRef] [PubMed]
- Bentley, D.L. Coupling mRNA processing with transcription in time and space. Nat. Rev. Genet. 2014, 15, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Naftelberg, S.; Schor, I.E.; Ast, G.; Kornblihtt, A.R. Regulation of Alternative Splicing Through Coupling with Transcription and Chromatin Structure. Annu. Rev. Biochem. 2015, 84, 165–198. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Rio, D.C. Mechanisms and Regulation of Alternative Pre-mRNA Splicing. Annu. Rev. Biochem. 2015, 84, 291–323. [Google Scholar] [CrossRef] [PubMed]
- Sumanasekera, C.; Watt, D.S.; Stamm, S. Substances that can change alternative splice-site selection. Biochem. Soc. Trans. 2008, 36, 483–490. [Google Scholar] [CrossRef]
- Montes, M.; Becerra, S.; Sánchez-Álvarez, M.; Suñé, C. Functional coupling of transcription and splicing. Gene 2012, 501, 104–117. [Google Scholar] [CrossRef] [PubMed]
- Gómez Acuña, L.I.; Fiszbein, A.; Alló, M.; Schor, I.E.; Kornblihtt, A.R. Connections between chromatin signatures and splicing. Wiley Interdiscip. Rev. RNA 2013, 4, 77–91. [Google Scholar] [CrossRef]
- Kornblihtt, A.R.; De La Mata, M.; Fededa, J.P.; Muñoz, M.J.; Nogués, G. Multiple links between transcription and splicing. RNA 2004, 10, 1489–1498. [Google Scholar] [CrossRef]
- Shukla, S.; Oberdoerffer, S. Co-transcriptional regulation of alternative pre-mRNA splicing. Biochim. Biophys. Acta Gene Regul. Mech. 2012, 1819, 673–683. [Google Scholar] [CrossRef]
- Krawczak, M.; Thomas, N.S.T.; Hundrieser, B.; Mort, M.; Wittig, M.; Hampe, J.; Cooper, D.N. Single base-pair substitutions in exon-intron junctions of human genes: Nature, distribution, and consequences for mRNA splicing. Hum. Mutat. 2007, 28, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Baralle, D.; Buratti, E. RNA splicing in human disease and in the clinic. Clin. Sci. 2017, 131, 355–368. [Google Scholar] [CrossRef]
- Tazi, J.; Bakkour, N.; Stamm, S. Alternative splicing and disease. Biochim. Biophys. Acta Mol. Basis Dis. 2009, 1792, 14–26. [Google Scholar] [CrossRef] [PubMed]
- Faustino, N.A.; Cooper, T.A. Pre-mRNA splicing and human disease. Genes Dev. 2003, 17, 419–437. [Google Scholar] [CrossRef] [PubMed]
- Rogalska, M.E.; Tajnik, M.; Licastro, D.; Bussani, E.; Camparini, L.; Mattioli, C.; Pagani, F. Therapeutic activity of modified U1 core spliceosomal particles. Nat. Commun. 2016, 7, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Balestra, D.; Barbon, E.; Scalet, D.; Cavallari, N.; Perrone, D.; Zanibellato, S.; Bernardi, F.; Pinotti, M. Regulation of a strong F9 cryptic 5′ss by intrinsic elements and by combination of tailored U1snRNAs with antisense oligonucleotides. Hum. Mol. Genet. 2015, 24, 4809–4816. [Google Scholar] [CrossRef] [PubMed]
- Donadon, I.; McVey, J.H.; Garagiola, I.; Branchini, A.; Mortarino, M.; Peyvandi, F.; Bernardi, F.; Pinotti, M. Clustered F8 missense mutations cause hemophilia A by combined alteration of splicing and protein biosynthesis and activity. Haematologica 2017, 103, 344–350. [Google Scholar] [CrossRef]
- Cavallari, N.; Balestra, D.; Branchini, A.; Maestri, I.; Chuamsunrit, A.; Sasanakul, W.; Mariani, G.; Pagani, F.; Bernardi, F.; Pinotti, M. Activation of a cryptic splice site in a potentially lethal coagulation defect accounts for a functional protein variant. Biochim. Biophys. Acta Mol. Basis Dis. 2012, 1822, 1109–1113. [Google Scholar] [CrossRef]
- Grodecká, L.; Buratti, E.; Freiberger, T. Mutations of pre-mRNA splicing regulatory elements: Are predictions moving forward to clinical diagnostics? Int. J. Mol. Sci. 2017, 18, 1668. [Google Scholar] [CrossRef]
- Lenting, P.J.; van Mourik, J.A.; Mertens, K. Determinants of the inherent strength of human 5′ splice sites. Blood 1998, 92, 3983–3996. [Google Scholar]
- Tan, J.; Ho, J.X.J.X.J.; Zhong, Z.; Luo, S.; Chen, G.; Roca, X. Noncanonical registers and base pairs in human 5′ splice-site selection. Nucleic Acids Res. 2016, 44, 3908–3921. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Roca, X.; Akerman, M.; Gaus, H.; Berdeja, A.; Bennett, C.F.; Krainer, A.R. Widespread recognition of 5’ splice sites by noncanonical base-pairing to U1 snRNA involving bulged nucleotides. Genes Dev. 2012, 26, 1098–1109. [Google Scholar] [CrossRef] [PubMed]
- Krawczak, M.; Reiss, J.; Cooper, D.N. The mutational spectrum of single base-pair substitutions in mRNA splice junctions of human genes: Causes and consequences. Hum. Genet. 1992, 90, 41–54. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, Y.; Weiner, A.M. A compensatory base change in U1 snRNA suppresses a 5′ splice site mutation. Cell 1986, 46, 827–835. [Google Scholar] [CrossRef]
- Baralle, M. Identification of a mutation that perturbs NF1 agene splicing using genomic DNA samples and a minigene assay. J. Med. Genet. 2003, 40, 220–222. [Google Scholar] [CrossRef] [PubMed]
- Susani, L.; Pangrazio, A.; Sobacchi, C.; Taranta, A.; Mortier, G.; Savarirayan, R.; Villa, A.; Orchard, P.; Vezzoni, P.; Albertini, A.; et al. TCIRG1-dependent recessive osteopetrosis: Mutation analysis, functional identification of the splicing defects, andin vitro rescue by U1 snRNA. Hum. Mutat. 2004, 24, 225–235. [Google Scholar] [CrossRef]
- Pinotti, M.; Balestra, D.; Rizzotto, L.; Maestri, I.; Pagani, F.; Bernardi, F. Rescue of coagulation factor VII function by the U1+5A snRNA. Blood 2009, 113, 6461–6464. [Google Scholar] [CrossRef] [PubMed]
- Pinotti, M.; Rizzotto, L.; Balestra, D.; Lewandowska, M.A.; Cavallari, N.; Marchetti, G.; Bernardi, F.; Pagani, F. U1-snRNA-mediated rescue of mRNA processing in severe factor VII deficiency. Blood 2008, 111, 2681–2684. [Google Scholar] [CrossRef]
- Tanner, G.; Glaus, E.; Barthelmes, D.; Ader, M.; Fleischhauer, J.; Pagani, F.; Berger, W.; Neidhardt, J. Therapeutic strategy to rescue mutation-induced exon skipping in rhodopsin by adaptation of U1 snRNA. Hum. Mutat. 2009, 30, 255–263. [Google Scholar] [CrossRef]
- Hartmann, L.; Neveling, K.; Borkens, S.; Schneider, H.; Freund, M.; Grassman, E.; Theiss, S.; Wawer, A.; Burdach, S.; Auerbach, A.D.; et al. Correct mRNA Processing at a Mutant TT Splice Donor in FANCC Ameliorates the Clinical Phenotype in Patients and Is Enhanced by Delivery of Suppressor U1 snRNAs. Am. J. Hum. Genet. 2010, 87, 480–493. [Google Scholar] [CrossRef]
- Schmid, F.; Glaus, E.; Barthelmes, D.; Fliegauf, M.; Gaspar, H.; Nürnberg, G.; Nürnberg, P.; Omran, H.; Berger, W.; Neidhardt, J. U1 snRNA-mediated gene therapeutic correction of splice defects caused by an exceptionally mild BBS mutation. Hum. Mutat. 2011, 32, 815–824. [Google Scholar] [CrossRef] [PubMed]
- Glaus, E.; Schmid, F.; Da Costa, R.; Berger, W.; Neidhardt, J. Gene Therapeutic Approach Using Mutation-adapted U1 snRNA to Correct a RPGR Splice Defect in Patient-derived Cells. Mol. Ther. 2011, 19, 936–941. [Google Scholar] [CrossRef] [PubMed]
- Borensztajn, K.; Sobrier, M.-L.L.; Duquesnoy, P.; Fischer, A.-M.M.; Tapon-Bretaudière, J.; Amselem, S. Oriented Scanning Is the Leading Mechanism Underlying 5′ Splice Site Selection in Mammals. PLoS Genet. 2006, 2, e138. [Google Scholar] [CrossRef] [PubMed]
- Balestra, D.; Faella, A.; Margaritis, P.; Cavallari, N.; Pagani, F.; Bernardi, F.; Arruda, V.R.; Pinotti, M. An engineered U1 small nuclear RNA rescues splicing-defective coagulation F7 gene expression in mice. J. Thromb. Haemost. 2014, 12, 177–185. [Google Scholar] [CrossRef]
- Tajnik, M.; Rogalska, M.E.; Bussani, E.; Barbon, E.; Balestra, D.; Pinotti, M.; Pagani, F. Molecular Basis and Therapeutic Strategies to Rescue Factor IX Variants That Affect Splicing and Protein Function. PLoS Genet. 2016, 12, e1006082. [Google Scholar] [CrossRef] [PubMed]
- Dal Mas, A.; Fortugno, P.; Donadon, I.; Levati, L.; Castiglia, D.; Pagani, F. Exon-Specific U1s Correct SPINK5Exon 11 Skipping Caused by a Synonymous Substitution that Affects a Bifunctional Splicing Regulatory Element. Hum. Mutat. 2015, 36, 504–512. [Google Scholar] [CrossRef] [PubMed]
- Dal Mas, A.; Rogalska, M.E.E.; Bussani, E.; Pagani, F.; Dal Mas, A.; Rogalska, M.E.E.; Bussani, E.; Pagani, F. Improvement of SMN2 Pre-mRNA Processing Mediated by Exon-Specific U1 Small Nuclear RNA. Am. J. Hum. Genet. 2015, 96, 93–103. [Google Scholar] [CrossRef]
- Nizzardo, M.; Simone, C.; Dametti, S.; Salani, S.; Ulzi, G.; Pagliarani, S.; Rizzo, F.; Frattini, E.; Pagani, F.; Bresolin, N.; et al. Spinal muscular atrophy phenotype is ameliorated in human motor neurons by SMN increase via different novel RNA therapeutic approaches. Sci. Rep. 2015, 5, 1–13. [Google Scholar] [CrossRef]
- van der Woerd, W.L.; Mulder, J.; Pagani, F.; Beuers, U.; Houwen, R.H.J.; van de Graaf, S.F.J. Analysis of aberrant pre-messenger RNA splicing resulting from mutations in ATP8B1 and efficient in vitro rescue by adapted U1 small nuclear RNA. Hepatology 2015, 61, 1382–1391. [Google Scholar] [CrossRef]
- Donadon, I.; Pinotti, M.; Rajkowska, K.; Pianigiani, G.; Barbon, E.; Morini, E.; Motaln, H.; Rogelj, B.; Mingozzi, F.; Slaugenhaupt, S.A.; et al. Exon-specific U1 snRNAs improve ELP1 exon 20 definition and rescue ELP1 protein expression in a familial dysautonomia mouse model. Hum. Mol. Genet. 2018, 27, 2466–2476. [Google Scholar] [CrossRef]
- Scalet, D.; Balestra, D.; Rohban, S.; Bovolenta, M.; Perrone, D.; Bernardi, F.; Campaner, S.; Pinotti, M. Exploring Splicing-Switching Molecules For Seckel Syndrome Therapy. Biochim. Biophys. Acta - Mol. Basis Dis. 2017, 1863, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Fernandez Alanis, E.; Pinotti, M.; Dal Mas, A.; Balestra, D.; Cavallari, N.; Rogalska, M.E.; Bernardi, F.; Pagani, F.; Alanis, E.F.; Pinotti, M.; et al. An exon-specific U1 small nuclear RNA (snRNA) strategy to correct splicing defects. Hum. Mol. Genet. 2012, 21, 2389–2398. [Google Scholar] [CrossRef] [PubMed]
- Balestra, D.; Scalet, D.; Pagani, F.; Rogalska, M.E.; Mari, R.; Bernardi, F.; Pinotti, M. An Exon-Specific U1snRNA Induces a Robust Factor IX Activity in Mice Expressing Multiple Human FIX Splicing Mutants. Mol. Ther. Nucleic Acids 2016, 5, e370. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Martínez-Pizarro, A.; Dembic, M.; Pérez, B.; Andresen, B.S.; Desviat, L.R. Intronic PAH gene mutations cause a splicing defect by a novel mechanism involving U1snRNP binding downstream of the 5’ splice site. PLoS Genet. 2018, 14, e1007360. [Google Scholar] [CrossRef] [PubMed]
- Scalet, D.; Sacchetto, C.; Bernardi, F.; Pinotti, M.; Van De Graaf, S.F.J.; Balestra, D. The somatic FAH C.1061C>A change counteracts the frequent FAH c.1062+5G>A mutation and permits U1snRNA-based splicing correction. J. Hum. Genet. 2018, 63, 683–686. [Google Scholar] [CrossRef] [PubMed]
- Scalet, D.; Maestri, I.; Branchini, A.; Bernardi, F.; Pinotti, M.; Balestra, D. Disease-causing variants of the conserved +2T of 5′ splice sites can be rescued by engineered U1snRNAs. Hum. Mutat. 2019, 40, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Sheth, N.; Roca, X.; Hastings, M.L.; Roeder, T.; Krainer, A.R.; Sachidanandam, R. Comprehensive splice-site analysis using comparative genomics. Nucleic Acids Res. 2006, 34, 3955–3967. [Google Scholar] [CrossRef]
- Thanaraj, T.A. Human GC-AG alternative intron isoforms with weak donor sites show enhanced consensus at acceptor exon positions. Nucleic Acids Res. 2001, 29, 2581–2593. [Google Scholar] [CrossRef]
- Nuzzo, F.; Bulato, C.; Nielsen, B.I.; Lee, K.; Wielders, S.J.; Simioni, P.; Key, N.S.; Castoldi, E. Characterization of an apparently synonymous F5 mutation causing aberrant splicing and factor V deficiency. Haemophilia 2014, 21, 241–248. [Google Scholar] [CrossRef]
- Nuzzo, F.; Radu, C.; Baralle, M.; Spiezia, L.; Hackeng, T.M.; Simioni, P.; Castoldi, E. Antisense-based RNA therapy of factor V deficiency: In vitro and ex vivo rescue of a F5 deep-intronic splicing mutation. Blood 2013, 122, 3825–3831. [Google Scholar] [CrossRef][Green Version]
- Davis, R.L.; Homer, V.M.; George, P.M.; Brennan, S.O. A deep intronic mutation in FGB creates a consensus exonic splicing enhancer motif that results in afibrinogenemia caused by aberrant mRNA splicing, which can be corrected in vitro with antisense oligonucleotide treatment. Hum. Mutat. 2009, 30, 221–227. [Google Scholar] [CrossRef] [PubMed]
- de Jong, A.; Dirven, R.J.; Oud, J.A.; Tio, D.; van Vlijmen, B.J.M.; Eikenboom, J. Correction of a dominant-negative von Willebrand factor multimerization defect by small interfering RNA-mediated allele-specific inhibition of mutant von Willebrand factor. J. Thromb. Haemost. 2018, 16, 1357–1368. [Google Scholar] [CrossRef] [PubMed]
- Sehgal, A.; Barros, S.; Ivanciu, L.; Cooley, B.; Qin, J.; Racie, T.; Hettinger, J.; Carioto, M.; Jiang, Y.; Brodsky, J.; et al. An RNAi therapeutic targeting antithrombin to rebalance the coagulation system and promote hemostasis in hemophilia. Nat. Med. 2015, 21, 492–497. [Google Scholar] [CrossRef] [PubMed]
- Pasi, K.J.; Rangarajan, S.; Georgiev, P.; Mant, T.; Creagh, M.D.; Lissitchkov, T.; Bevan, D.; Austin, S.; Hay, C.R.; Hegemann, I.; et al. Targeting of Antithrombin in Hemophilia A or B with RNAi Therapy. N. Engl. J. Med. 2017, 377, 819–828. [Google Scholar] [CrossRef]
- Rodnina, M.V.; Wintermeyer, W. Ribosome fidelity: tRNA discrimination, proofreading and induced fit. Trends Biochem. Sci. 2001, 26, 124–130. [Google Scholar] [CrossRef]
- Cochella, L.; Green, R. Fidelity in protein synthesis. Curr. Biol. 2005, 15, R536–R540. [Google Scholar] [CrossRef] [PubMed]
- Bereczky, Z.; Bardos, H.; Komaromi, I.; Kiss, C.; Haramura, G.; Ajzner, E.; Adany, R.; Muszbek, L. Factor XDebrecen: Gly204Arg mutation in factor X causes the synthesis of a non-secretable protein and severe factor X deficiency. Haematologica 2008, 93, 299–302. [Google Scholar] [CrossRef][Green Version]
- Branchini, A.; Campioni, M.; Mazzucconi, M.G.; Biondo, F.; Mari, R.; Bicocchi, M.P.; Bernardi, F.; Pinotti, M. Replacement of the Y450 (c234) phenyl ring in the carboxyl-terminal region of coagulation factor IX causes pleiotropic effects on secretion and enzyme activity. FEBS Lett. 2013, 587, 3249–3253. [Google Scholar] [CrossRef]
- Baroni, M.; Pavani, G.; Pinotti, M.; Branchini, A.; Bernardi, F.; Camire, R.M. Asymmetric processing of mutant factor X Arg386Cys reveals differences between intrinsic and extrinsic pathway activation. Biochim. Biophys. Acta Proteins Proteomics 2015, 1854, 1351–1356. [Google Scholar] [CrossRef]
- Pignani, S.; Todaro, A.; Ferrarese, M.; Marchi, S.; Lombardi, S.; Balestra, D.; Pinton, P.; Bernardi, F.; Pinotti, M.; Branchini, A. The chaperone-like sodium phenylbutyrate improves factor IX intracellular trafficking and activity impaired by the frequent p.R294Q mutation. J. Thromb. Haemost. 2018, 16, 2035–2043. [Google Scholar] [CrossRef]
- Kisselev, L.L.; Buckingham, R.H. Translational termination comes of age. Trends Biochem. Sci. 2000, 25, 561–566. [Google Scholar] [CrossRef]
- Mort, M.; Ivanov, D.; Cooper, D.N.; Chuzhanova, N.A. A meta-analysis of nonsense mutations causing human genetic disease. Hum. Mutat. 2008, 29, 1037–1047. [Google Scholar] [CrossRef] [PubMed]
- Nagy, E.; Maquat, L.E. A rule for termination-codon position within intron-containing genes: When nonsense affects RNA abundance. Trends Biochem. Sci. 1998, 23, 198–199. [Google Scholar] [CrossRef]
- Khajavi, M.; Inoue, K.; Lupski, J.R. Nonsense-mediated mRNA decay modulates clinical outcome of genetic disease. Eur. J. Hum. Genet. 2006, 14, 1074–1081. [Google Scholar] [CrossRef] [PubMed]
- Rospert, S.; Rakwalska, M.; Dubaquié, Y. Polypeptide chain termination and stop codon readthrough on eukaryotic ribosomes. Rev. Physiol. Biochem. Pharmacol. 2005, 155. [Google Scholar] [CrossRef]
- Roy, B.; Leszyk, J.D.; Mangus, D.A.; Jacobson, A. Nonsense suppression by near-cognate tRNAs employs alternative base pairing at codon positions 1 and 3. Proc. Natl. Acad. Sci. USA 2015, 112, 3038–3043. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.M.; Stockwell, P.A.; Trotman, C.N.A.; Tate, W.P. Sequence analysis suggests that tetra-nucleotides signal the termination of protein synthesis in eukaryotes. Nucleic Acids Res. 1990, 18, 6339–6345. [Google Scholar] [CrossRef]
- Manuvakhova, M.; Keeling, K.; Bedwell, D.M. Aminoglycoside antibiotics mediate context-dependent suppression of termination codons in a mammalian translation system. RNA 2000, 6, 1044–1055. [Google Scholar] [CrossRef]
- Cobucci-Ponzano, B.; Rossi, M.; Moracci, M. Recoding in Archaea. Mol. Microbiol. 2004, 55, 339–348. [Google Scholar] [CrossRef]
- Beier, H. Misreading of termination codons in eukaryotes by natural nonsense suppressor tRNAs. Nucleic Acids Res. 2001, 29, 4767–4782. [Google Scholar] [CrossRef]
- Böck, A.; Forchhammer, K.; Heider, J.; Leinfelder, W.; Sawers, G.; Veprek, B.; Zinoni, F. Selenocysteine: The 21st amino acid. Mol. Microbiol. 1991, 5, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Berry, M.J.; Small-Howard, A.L. Unique features of selenocysteine incorporation function within the context of general eukaryotic translational processes. Biochem. Soc. Trans. 2005, 33, 1493–1497. [Google Scholar] [CrossRef] [PubMed]
- James, C.M.; Ferguson, T.K.; Leykam, J.F.; Krzycki, J.A. The Amber Codon in the Gene Encoding the Monomethylamine Methyltransferase Isolated fromMethanosarcina barkeriIs Translated as a Sense Codon. J. Biol. Chem. 2001, 276, 34252–34258. [Google Scholar] [CrossRef] [PubMed]
- Atkins, J.F.; Gesteland, R. Biochemistry: The 22nd amino acid. Science (80-) 2002, 296, 1409–1410. [Google Scholar] [CrossRef] [PubMed]
- Burke, J.F.; Mogg, A.E. Suppression of a nonsense mutation in mammalian cellsin vivoby the aminoglycoside anthiotics G–418 and paromomycin. Nucleic Acids Res. 1985, 13, 6265–6272. [Google Scholar] [CrossRef] [PubMed]
- Ogle, J.M.; Brodersen, D.E.; Clemons W.M., J.; Tarry, M.J.; Carter, A.P.; Ramakrishnan, V. Recognition of cognate transfer RNA by the 30S ribosomal subunit. Science (80-) 2001, 292, 897–902. [Google Scholar] [CrossRef] [PubMed]
- Howard, M.; Frizzell, R.A.; Bedwell, D.M. Aminoglycoside antibiotics restore CFTR function by overcoming premature stop mutations. Nat. Med. 1996, 2, 467–469. [Google Scholar] [CrossRef]
- Keeling, K.M.; Xue, X.; Gunn, G.; Bedwell, D.M. Therapeutics Based on Stop Codon Readthrough. Annu. Rev. Genomics Hum. Genet. 2014, 15, 371–394. [Google Scholar] [CrossRef]
- Keeling, K. Nonsense Suppression as an Approach to Treat Lysosomal Storage Diseases. Diseases 2016, 4, 32. [Google Scholar] [CrossRef]
- Blanchet, S.; Cornu, D.; Argentini, M.; Namy, O. New insights into the incorporation of natural suppressor tRNAs at stop codons in Saccharomyces cerevisiae. Nucleic Acids Res. 2014, 42, 10061–10072. [Google Scholar] [CrossRef]
- Roy, B.; Friesen, W.J.; Tomizawa, Y.; Leszyk, J.D.; Zhuo, J.; Johnson, B.; Dakka, J.; Trotta, C.R.; Xue, X.; Mutyam, V.; et al. Ataluren stimulates ribosomal selection of near-cognate tRNAs to promote nonsense suppression. Proc. Natl. Acad. Sci. USA 2016, 113, 12508–12513. [Google Scholar] [CrossRef] [PubMed]
- Branchini, A.; Rizzotto, L.; Mariani, G.; Napolitano, M.; Lapecorella, M.; Giansily-Blaizot, M.; Mari, R.; Canella, A.; Pinotti, M.; Bernardi, F. Natural and engineered carboxy-terminal variants: Decreased secretion and gain-of-function result in asymptomatic coagulation factor VII deficiency. Haematologica 2012, 97, 705–709. [Google Scholar] [CrossRef] [PubMed]
- Branchini, A.; Baroni, M.; Pfeiffer, C.; Batorova, A.; Giansily-Blaizot, M.; Schved, J.F.; Mariani, G.; Bernardi, F.; Pinotti, M. Coagulation factor VII variants resistant to inhibitory antibodies. Thromb. Haemost. 2014, 112, 972–980. [Google Scholar] [PubMed]
- Borhany, M.; Buthiau, D.; Rousseau, F.; Guillot, O.; Naveena, F.; Abid, M.; Shamsi, T.; Giansily-Blaizot, M. Genotyping of five Pakistani patients with severe inherited factor X deficiency. Blood Coagul. Fibrinolysis 2018, 29, 622–625. [Google Scholar] [CrossRef] [PubMed]
- Ferrarese, M.; Baroni, M.; Della Valle, P.; Spiga, I.; Poloniato, A.; D’Angelo, A.; Pinotti, M.; Bernardi, F.; Branchini, A. Missense changes in the catalytic domain of coagulation factor X account for minimal function preventing a perinatal lethal condition. Haemophilia 2019. [Google Scholar] [CrossRef] [PubMed]
- Branchini, A.; Baroni, M.; Burini, F.; Puzzo, F.; Nicolosi, F.; Mari, R.; Gemmati, D.; Bernardi, F.; Pinotti, M. The carboxyl-terminal region is NOT essential for secreted and functional levels of coagulation factor X. J. Thromb. Haemost. 2015, 13, 1468–1474. [Google Scholar] [CrossRef]
- Pinotti, M.; Caruso, P.; Canella, A.; Campioni, M.; Tagariello, G.; Castaman, G.; Giacomelli, S.; Belvini, D.; Bernardi, F. Ribosome readthrough accounts for secreted full-length factor IX in hemophilia B patients with nonsense mutations. Hum. Mutat. 2012, 33, 1373–1376. [Google Scholar] [CrossRef]
- James, P.D. Aminoglycoside suppression of nonsense mutations in severe hemophilia. Blood 2005, 106, 3043–3048. [Google Scholar] [CrossRef]
- Yang, C.; Feng, J.; Song, W.; Wang, J.; Tsai, B.; Zhang, Y.; Scaringe, W.A.; Hill, K.A.; Margaritis, P.; High, K.A.; et al. A mouse model for nonsense mutation bypass therapy shows a dramatic multiday response to geneticin. Proc. Natl. Acad. Sci. USA 2007, 104, 15394–15399. [Google Scholar] [CrossRef]
- Ferrarese, M.; Testa, M.F.; Balestra, D.; Bernardi, F.; Pinotti, M.; Branchini, A. Secretion of wild-type factor IX upon readthrough over F9 pre-peptide nonsense mutations causing hemophilia B. Hum. Mutat. 2018, 39, 702–708. [Google Scholar] [CrossRef]
- Branchini, A.; Ferrarese, M.; Campioni, M.; Castaman, G.; Mari, R.; Bernardi, F.; Pinotti, M. Specific factor IX mRNA and protein features favor drug-induced readthrough over recurrent nonsense mutations. Blood 2017, 129, 2303–2307. [Google Scholar] [CrossRef] [PubMed]
- Simioni, P.; Tormene, D.; Tognin, G.; Gavasso, S.; Bulato, C.; Iacobelli, N.P.; Finn, J.D.; Spiezia, L.; Radu, C.; Arruda, V.R. X-Linked Thrombophilia with a Mutant Factor IX (Factor IX Padua). N. Engl. J. Med. 2009, 361, 1671–1675. [Google Scholar] [CrossRef] [PubMed]
- Branchini, A.; Ferrarese, M.; Lombardi, S.; Mari, R.; Bernardi, F.; Pinotti, M. Differential functional readthrough over homozygous nonsense mutations contributes to the bleeding phenotype in coagulation factor VII deficiency. J. Thromb. Haemost. 2016, 14, 1994–2000. [Google Scholar] [CrossRef] [PubMed]
- Pinotti, M.; Rizzotto, L.; Pinton, P.; Ferraresi, P.; Chuansumrit, A.; Charoenkwan, P.; Marchetti, G.; Rizzuto, R.; Mariani, G.; Bernardi, F. Intracellular readthrough of nonsense mutations by aminoglycosides in coagulation factor VII. J. Thromb. Haemost. 2006, 4, 1308–1314. [Google Scholar] [CrossRef] [PubMed]
- Pinotti, M.; Rizzotto, L.; Chuansumrit, A.; Mariani, G.; Bernardi, F. Gentamicin induces sub-therapeutic levels of coagulation factor VII in patients with nonsense mutations. J. Thromb. Haemost. 2006, 4, 1828–1830. [Google Scholar] [CrossRef] [PubMed]
- Giansily-Blaizot, M.; Aguilar-Martinez, P.; Briquel, M.-E.; d’Oiron, R.; De Maistre, E.; Epelbaum, S.; Schved, J.-F. Two novel cases of cerebral haemorrhages at the neonatal period associated with inherited factor VII deficiency, one of them revealing a new nonsense mutation (Ser52Stop). Blood Coagul. Fibrinolysis 2003, 14, 217–220. [Google Scholar] [CrossRef]
- Chafa, O.; Fischer, A.M.; Reghis, A.; Tapon-Bretaudiere, J. Homozygous nonsense mutation (Cys72→stop) in the human F7 gene: A not life-threatening mutation despite the absence of circulating factor VII. J. Thromb. Haemost. 2005, 3, 175–177. [Google Scholar] [CrossRef]
- Jayandharan, G.R.; Shaji, R.V.; Baidya, S.; Nair, S.C.; Chandy, M.; Srivastava, A. Molecular characterization of factor IX gene mutations in 53 patients with haemophilia B in India. Thromb. Haemost. 2005, 94, 883–886. [Google Scholar]
- Thompson, A.R.; Schoof, J.M.; Weinmann, A.F.; Chen, S.H. Factor IX mutations: Rapid, direct screening methods for 20 new families with hemophilia B. Thromb. Res. 1992, 65, 289–295. [Google Scholar] [CrossRef]
- von Heijne, G. Signal sequences. J. Mol. Biol. 1985, 184, 99–105. [Google Scholar] [CrossRef]
- Bristol, J.A.; Freedman, S.J.; Furie, B.C.; Furie, B. Profactor IX: The propeptide inhibits binding to membrane surfaces and activation by factor XIA. Biochemistry 1994, 33, 14136–14143. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, R. Post-translational Modifications Required for Coagulation Factor Secretion and Function. Thromb. Haemost. 1998, 79, 1068–1079. [Google Scholar] [CrossRef] [PubMed]
- Liddell, M.B.; Lillicrap, D.P.; Peake, I.R.; Bloom, A.L. Defective propeptide processing and abnormal activation underlie the molecular pathology of factor IX Troed-y-Rhiw. Br. J. Haematol. 1989, 72, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Montejo, J.M.; Magallón, M.; Tizzano, E.; Solera, J. Identification of twenty-one new mutations in the factor IX gene by SSCP analysis. Hum. Mutat. 1999, 13, 160–165. [Google Scholar] [CrossRef]
- Wulff, K.; Schröder, W.; Wehnert, M.; Herrmann, F.H. Twenty-five novel mutations of the factor IX gene in haemophilia B. Hum. Mutat. 1995, 6, 346–348. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, Y.; Zhu, M.; Zhang, B. Identification of candidate nonsense mutations of FVIII for ribosomal readthrough therapy. Haematologica 2019. [Google Scholar] [CrossRef]
- Hartl, F.U. Molecular Chaperones in the Cytosol: From Nascent Chain to Folded Protein. Science (80-) 2002, 295, 1852–1858. [Google Scholar] [CrossRef]
- Sitia, R.; Braakman, I. Quality control in the endoplasmic reticulum protein factory. Nature 2003, 426, 891–894. [Google Scholar] [CrossRef]
- Ciechanover, A.; Orian, A.; Schwartz, A.L. Ubiquitin-mediated proteolysis: Biological regulation via destruction. BioEssays 2000, 22, 442–451. [Google Scholar] [CrossRef]
- Schröder, M.; Kaufman, R.J. ER stress and the unfolded protein response. Mutat. Res. Mol. Mech. Mutagen. 2005, 569, 29–63. [Google Scholar] [CrossRef]
- Muntau, A.C.; Leandro, J.; Staudigl, M.; Mayer, F.; Gersting, S.W. Innovative strategies to treat protein misfolding in inborn errors of metabolism: Pharmacological chaperones and proteostasis regulators. J. Inherit. Metab. Dis. 2014, 37, 505–523. [Google Scholar] [CrossRef] [PubMed]
- Engin, F.; Hotamisligil, G.S. Restoring endoplasmic reticulum function by chemical chaperones: An emerging therapeutic approach for metabolic diseases. Diabetes Obes. Metab. 2010, 12, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Rajan, R.S.; Tsumoto, K.; Tokunaga, M.; Tokunaga, H.; Kita, Y.; Arakawa, T. Chemical and Pharmacological Chaperones: Application for Recombinant Protein Production and Protein Folding Diseases. Curr. Med. Chem. 2011, 18, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Cortez, L.; Sim, V. The therapeutic potential of chemical chaperones in protein folding diseases. Prion 2014, 8, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Arakawa, T.; Timasheff, S.N. The stabilization of proteins by osmolytes. Biophys. J. 1985, 47, 411–414. [Google Scholar] [CrossRef]
- Brown, C.R.; Hong-Brown, L.Q.; Biwersi, J.; Verkman, A.S.; Welch, W.J. Chemical chaperones correct the mutant phenotype of the ΔF508 cystic fibrosis transmembrane conductance regulator protein. Cell Stress Chaperones 1996, 1, 117–125. [Google Scholar] [CrossRef]
- Sato, S.; Ward, C.L.; Krouse, M.E.; Wine, J.J.; Kopito, R.R. Glycerol Reverses the Misfolding Phenotype of the Most Common Cystic Fibrosis Mutation. J. Biol. Chem. 1996, 271, 635–638. [Google Scholar] [CrossRef] [PubMed]
- Howard, M.; Welch, W.J. Manipulating the Folding Pathway of ΔF508 CFTR Using Chemical Chaperones. Cyst. Fibros. Methods Protoc. 2002, 70, 267–276. [Google Scholar]
- Howard, M.; Fischer, H.; Roux, J.; Santos, B.C.; Gullans, S.R.; Yancey, P.H.; Welch, W.J. Mammalian Osmolytes andS-Nitrosoglutathione Promote ΔF508 Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) Protein Maturation and Function. J. Biol. Chem. 2003, 278, 35159–35167. [Google Scholar] [CrossRef]
- Lim, M.; McKenzie, K.; Floyd, A.D.; Kwon, E.; Zeitlin, P.L. Modulation of ΔF508 Cystic Fibrosis Transmembrane Regulator Trafficking and Function with 4-Phenylbutyrate and Flavonoids. Am. J. Respir. Cell Mol. Biol. 2004, 31, 351–357. [Google Scholar] [CrossRef]
- Burrows, J.A.J.; Willis, L.K.; Perlmutter, D.H. Chemical chaperones mediate increased secretion of mutant alpha 1-antitrypsin (alpha 1-AT) Z: A potential pharmacological strategy for prevention of liver injury and emphysema in alpha 1-AT deficiency. Proc. Natl. Acad. Sci. USA 2000, 97, 1796–1801. [Google Scholar] [CrossRef] [PubMed]
- Maegawa, G.H.B.; Tropak, M.B.; Buttner, J.D.; Rigat, B.A.; Fuller, M.; Pandit, D.; Tang, L.; Kornhaber, G.J.; Hamuro, Y.; Clarke, J.T.R.; et al. Identification and Characterization of Ambroxol as an Enzyme Enhancement Agent for Gaucher Disease. J. Biol. Chem. 2009, 284, 23502–23516. [Google Scholar] [CrossRef] [PubMed]
- Zimran, A.; Altarescu, G.; Elstein, D. Pilot study using ambroxol as a pharmacological chaperone in type 1 Gaucher disease. Blood Cells, Mol. Dis. 2013, 50, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Porto, C.; Ferrara, M.C.; Meli, M.; Acampora, E.; Avolio, V.; Rosa, M.; Cobucci-Ponzano, B.; Colombo, G.; Moracci, M.; Andria, G.; et al. Pharmacological Enhancement of α-Glucosidase by the Allosteric Chaperone N-acetylcysteine. Mol. Ther. 2012, 20, 2201–2211. [Google Scholar] [CrossRef] [PubMed]
- Claudio, M.G. Protein Misfolding in Disease and Small Molecule Therapies. Curr. Top. Med. Chem. 2013, 12, 2460–2469. [Google Scholar]
- Bernier, V.; Lagacé, M.; Bichet, D.G.; Bouvier, M. Pharmacological chaperones: Potential treatment for conformational diseases. Trends Endocrinol. Metab. 2004, 15, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Loo, T.W.; Bartlett, M.C.; Clarke, D.M. Rescue of Folding Defects in ABC Transporters Using Pharmacological Chaperones. J. Bioenerg. Biomembr. 2005, 37, 501–507. [Google Scholar] [CrossRef]
- Johnson, S.M.; Connelly, S.; Fearns, C.; Powers, E.T.; Kelly, J.W. The Transthyretin Amyloidoses: From Delineating the Molecular Mechanism of Aggregation Linked to Pathology to a Regulatory-Agency-Approved Drug. J. Mol. Biol. 2012, 421, 185–203. [Google Scholar] [CrossRef]
- Pereira, D.M.; Valentão, P.; Andrade, P.B. Tuning protein folding in lysosomal storage diseases: The chemistry behind pharmacological chaperones. Chem. Sci. 2018, 9, 1740–1752. [Google Scholar] [CrossRef]
- Tao, Y.-X.; Conn, P.M. Pharmacoperones as Novel Therapeutics for Diverse Protein Conformational Diseases. Physiol. Rev. 2018, 98, 697–725. [Google Scholar] [CrossRef]
- Hou, Z.-S.; Ulloa-Aguirre, A.; Tao, Y.-X. Pharmacoperone drugs: Targeting misfolded proteins causing lysosomal storage-, ion channels-, and G protein-coupled receptors-associated conformational disorders. Expert Rev. Clin. Pharmacol. 2018, 11, 611–624. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, J.D.; Miao, H.; Zhang, K.; Wolfson, A.; Pennathur, S.; Pipe, S.W.; Kaufman, R.J. Antioxidants reduce endoplasmic reticulum stress and improve protein secretion. Proc. Natl. Acad. Sci. USA 2008, 105, 18525–18530. [Google Scholar] [CrossRef]
- Roelse, J.C.; De Laaf, R.T.M.; Timmermans, S.M.H.; Peters, M.; van Mourik, J.A.; Voorberg, J. Intracellular accumulation of factor VIII induced by missense mutations Arg593Cys and Asn618Ser explains cross-reacting material-reduced haemophilia A. Br. J. Haematol. 2000, 108, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Roth, S.D.; Schüttrumpf, J.; Milanov, P.; Abriss, D.; Ungerer, C.; Quade-Lyssy, P.; Simpson, J.C.; Pepperkok, R.; Seifried, E.; Tonn, T. Chemical Chaperones Improve Protein Secretion and Rescue Mutant Factor VIII in Mice with Hemophilia A. PLoS ONE 2012, 7, e44505. [Google Scholar] [CrossRef] [PubMed]
- Guillet, B.; Lambert, T.; d’Oiron, R.; Proulle, V.; Plantier, J.-L.; Rafowicz, A.; Peynet, J.; Costa, J.-M.; Bendelac, L.; Laurian, Y.; et al. Detection of 95 novel mutations in coagulation factor VIII geneF8responsible for hemophilia A: Results from a single institution. Hum. Mutat. 2006, 27, 676–685. [Google Scholar] [CrossRef] [PubMed]
- Tjeldhorn, L.; Iversen, N.; Sandvig, K.; Bergan, J.; Sandset, P.; Skretting, G. Functional characterization of the protein C A267T mutation: Evidence for impaired secretion due to defective intracellular transport. BMC Cell Biol. 2010, 11, 67. [Google Scholar] [CrossRef]
- Chollet, M.E.; Skarpen, E.; Iversen, N.; Sandset, P.M.; Skretting, G. The chemical chaperone sodium 4-phenylbutyrate improves the secretion of the protein CA267T mutant in CHO-K1 cells trough the GRASP55 pathway. Cell Biosci. 2015, 5. [Google Scholar] [CrossRef]
- Nagel-Wolfrum, K.; Möller, F.; Penner, I.; Baasov, T.; Wolfrum, U. Targeting Nonsense Mutations in Diseases with Translational Read-Through-Inducing Drugs (TRIDs). BioDrugs 2016, 30, 49–74. [Google Scholar] [CrossRef]
- Yukihara, M.; Ito, K.; Tanoue, O.; Goto, K.; Matsushita, T.; Matsumoto, Y.; Masuda, M.; Kimura, S.; Ueoka, R. Effective Drug Delivery System for Duchenne Muscular Dystrophy Using Hybrid Liposomes Including Gentamicin along with Reduced Toxicity. Biol. Pharm. Bull. 2011, 34, 712–716. [Google Scholar] [CrossRef]
- Bidou, L.; Allamand, V.; Rousset, J.-P.; Namy, O. Sense from nonsense: Therapies for premature stop codon diseases. Trends Mol. Med. 2012, 18, 679–688. [Google Scholar] [CrossRef]
- Dabrowski, M.; Bukowy-Bieryllo, Z.; Zietkiewicz, E. Advances in therapeutic use of a drug-stimulated translational readthrough of premature termination codons. Mol. Med. 2018, 24. [Google Scholar] [CrossRef] [PubMed]
- Batshaw, M.L.; Tuchman, M.; Summar, M.; Seminara, J. A longitudinal study of urea cycle disorders. Mol. Genet. Metab. 2014, 113, 127–130. [Google Scholar] [CrossRef] [PubMed]
| Pattern of Inheritance | Deficientfactor | OMIM* Number | Prevalence in the Population | Gene (Chromosome) | Severe Clinical Symptoms | Treatment Options** |
|---|---|---|---|---|---|---|
| X-linked | factor VIII§ | 306700 | 1:5,000 | F8 (Xq28) | Hemarthrosis, Intracranical hemorrhage | pdFVIII, rFVIII, EHL-FVIII |
| factor IX§ | 306900 | 1:30,000 | F9 (Xq27.1) | Hemarthrosis, Intracranical hemorrhage | pdFIX, rFIX, EHL-FIX | |
| Autosomal | Fibrinogen | 202400 | 1:1,000,000 | FGA (4q31.3) | Thrombosis, Umbilical stump bleeding, Mucocutaneous bleeding | FFP, pd Fibrinogen |
| FGB (4q31.3) | ||||||
| FGG (4q32.1) | ||||||
| Prothrombin† | 613679 | 1:2,000,000 | F2 (11p11.2) | Mucosal bleeding, Hemarthrosis, Intracranical hemorrhage | FFP, PCC | |
| factor V | 227400 | 1:1,000,000 | F5 (1q24.2) | Epistaxis, Muscle hematoma | FFP | |
| factor VII†§ | 227500 | 1:500,000 | F7 (13q24) | Intracranical hemorrhage, Hemarthrosis | FFP, pdFVII, rFVIIa | |
| factor X† | 227600 | 1:1,000,000 | F10 (13q34) | Gastrointesinal bleeding, Intracranical hemorrhage | FFP, PCC, pdFX/FIX, pdFX | |
| factor XI | 612416 | 1:1,000,000 | F11 (4q35.2) | Post-trauma bleed | FFP, pdFXI | |
| factor XIII | 613225 | 1:2,000,000 | F13A (6q25.1) | Delayed wound healing, Intracranical hemorrhage, Miscarriages | FFP, pdFXIII, rFXIII-A | |
| 613235 | F13B (1q31.3) |
| Mutation (HGVS)* | Mutation (Legacy)** | Sense Codon | PTC Sequence Context | Predicted Amino Acid Insertion† | Cellular Model | Mouse Model | Patients | Ref | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Drug | Response | Drug | Response | Drug | Response | |||||||
| F8 | p.R446X | R427X | CGA | UGA-U | W / C / R | - | - | - | - | Gentamycin | No | [158] |
| p.S1414X | S1395X | TCA | UAA-U | Y / Q / K | - | - | - | - | Gentamycin | 1.6% | [158] | |
| p.R2135X | R2116X | CGA | UGA-G | W / C / R | - | - | - | - | Gentamycin | No | [158] | |
| F9 | p.G21X | G(-26)X | GGA | UGA-U | W / C / R | Geneticin | 4% | - | - | - | - | [160] |
| p.R75X | R29X | CGA | UGA-G | W / C / R | Geneticin | No | Geneticin / Gentamycin | No | - | - | [159,161] | |
| p.L103X | L57X | UUA | UAA-A | Y / Q / K | Geneticin | No | - | - | - | - | [161] | |
| p.R162X | R116X | CGA | UGA-C | W / C / R | Geneticin | ~1% | - | - | - | - | [161] | |
| p.W240X | R194X | UGG | UGA-C | W / C / R | Geneticin | 5–6% | - | - | - | - | [161] | |
| p.R294X | R248X | CGA | UGA-A | W / C / R | Geneticin | 0.5–1% | - | - | - | - | [161] | |
| p.R298X | R252X | CGA | UGA-A | W / C / R | Geneticin | No | - | - | Gentamycin | No | [158,161] | |
| p.R379X | R333X | CGA | UGA-G | W / C / R | Geneticin | 1% | - | - | Gentamycin | 2% / No | [158,162] | |
| p.Q370X | R324X | CAG | UAG-U | Y / Q / K | Geneticin | ~1% | - | - | - | - | [161] | |
| p.R384X | R338X | CGA | UGA-U | W / C / R | Geneticin | 7-8% | Geneticin / Gentamycin | - | - | - | [159,161] | |
| F7 | p.S112X | S52X | UCA | UGA-A | W / C / R | Geneticin | 2–3% | - | - | - | - | [163] |
| p.C132X | C72X | UGC | UGA-C | W / C / R | Geneticin | 12–13% | - | - | - | - | [163] | |
| p.K376X | K316X | AAG | UAG-G | Y / Q / K | Geneticin / Gentamycin | >3% / >2% | - | - | Gentamycin | sub-therapeutic | [164,165] | |
| p.W424X | W364X | UGG | UGA-G | W / C / R | Geneticin / Gentamycin | >3% / >2% | - | - | Gentamycin | sub-therapeutic | [164,165] | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balestra, D.; Branchini, A. Molecular Mechanisms and Determinants of Innovative Correction Approaches in Coagulation Factor Deficiencies. Int. J. Mol. Sci. 2019, 20, 3036. https://doi.org/10.3390/ijms20123036
Balestra D, Branchini A. Molecular Mechanisms and Determinants of Innovative Correction Approaches in Coagulation Factor Deficiencies. International Journal of Molecular Sciences. 2019; 20(12):3036. https://doi.org/10.3390/ijms20123036
Chicago/Turabian StyleBalestra, Dario, and Alessio Branchini. 2019. "Molecular Mechanisms and Determinants of Innovative Correction Approaches in Coagulation Factor Deficiencies" International Journal of Molecular Sciences 20, no. 12: 3036. https://doi.org/10.3390/ijms20123036
APA StyleBalestra, D., & Branchini, A. (2019). Molecular Mechanisms and Determinants of Innovative Correction Approaches in Coagulation Factor Deficiencies. International Journal of Molecular Sciences, 20(12), 3036. https://doi.org/10.3390/ijms20123036






