Potential of Vitamin E Deficiency, Induced by Inhibition of α-Tocopherol Efflux, in Murine Malaria Infection
Abstract
1. Introduction
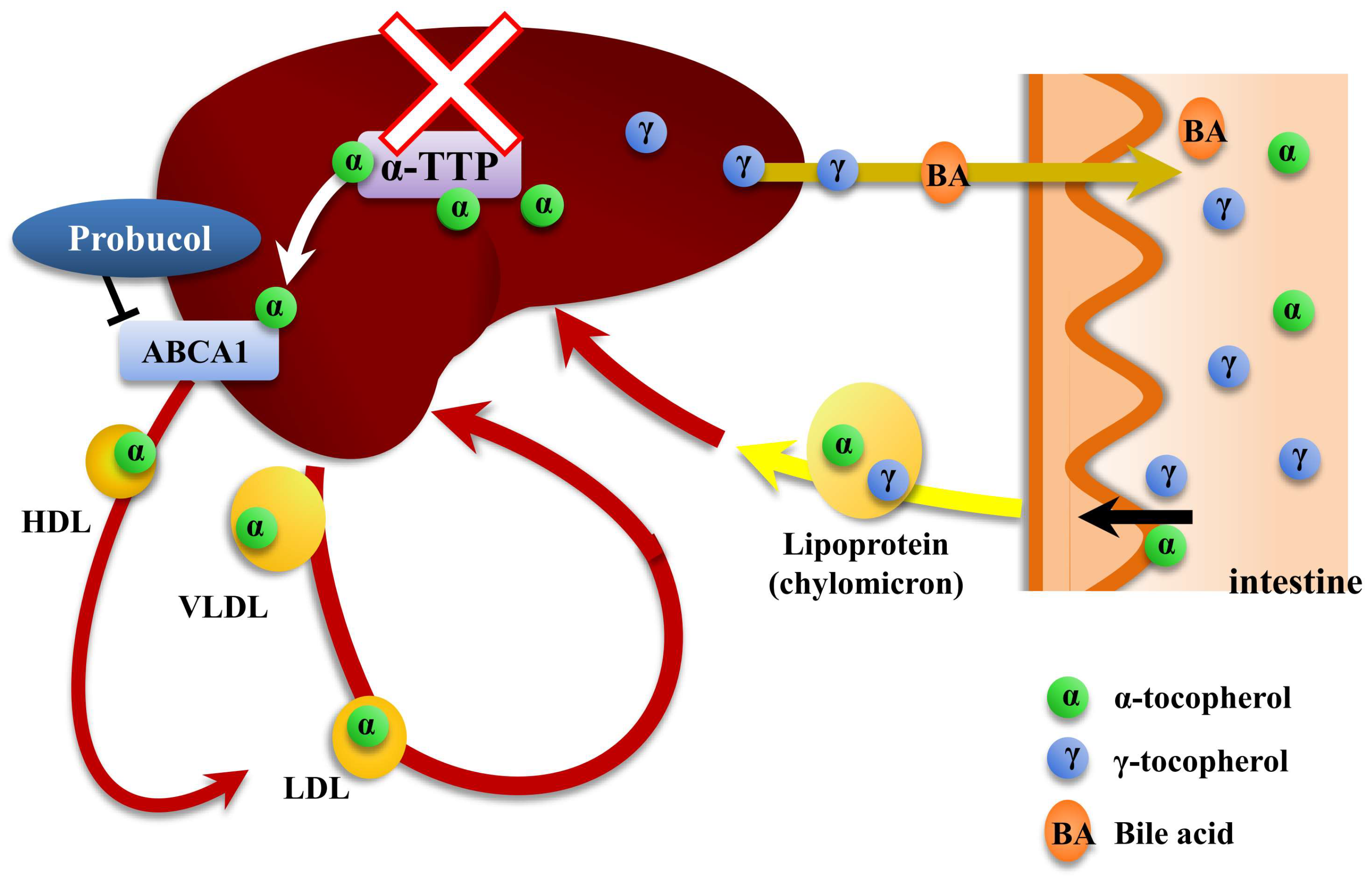
2. Effect of Vitamin E Deficiency, due to α-TTP Gene Disruption, on Murine Malaria Infection
2.1. Integrity of RBC Membrane in α-TTP Knockout Mice
2.2. Inhibition of α-TTP Confers Resistance to Malaria Infection
2.3. Expression Levels of Anti-Oxidative Stress Enzyme in the Infected Parasites
2.4. Cytokine Responses in α-TTP Knockout Mice
2.5. Enhancement of the Acquired Immune Response by α-TTP Inhibition
2.6. Expression of Erythropoietic Cytokines in α-TTP Knockout Mice with Malaria Infection
2.7. A Combination Therapy with Chloroquine Administration and α-TTP Inhibition
3. Effect of Probucol-Induced Vitamin E Deficiency on Murine Malaria Infection
3.1. Reduction in α-Tocopherol Concentration after Treatment with Probucol
3.2. Effect of Probucol on the Murine Malaria Infection
4. A Combination Therapy with Dihydroartemisinin and Probucol
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| α-TTP | α-Tocopherol transfer protein |
| ACT | Artemisinin-based Combination Therapy |
| VDL | Very Low Density Lipoprotein |
| LDL | Low Density Lipoprotein |
| ABCA1 | ATP-binding cassette transporter A1 |
| RBC | Red blood cell |
| EPO | Erythropoietin |
| 8-OHdG | 8-Hydroxy-2’-deoxyguanosine |
| VCAM | Vascular cellular adhesion molecule |
| ICAM | Intracellular adhesion molecule |
| LFA-1 | Lymphocyte function associated antigen |
| GFAP | Glial fibrillary acidic protein |
| LFA-1 | Lymphocyte function associated antigen |
| Grx | Glutaredoxin |
| γ-GCS | γ-glutamyl transferase |
| 2-Cys Prx | 2-Cys peroxiredoxin |
| TrxR | Thioredoxin reductase |
| EPOR | Erythropoietin receptor |
| MIF | Macrophage migration factor |
| DHA | Dihydroartemisinin |
References
- Bjørneboe, A.; Bjørneboe, G.E.; Drevon, C.A. Absorption, transport and distribution of vitamin E. J. Nutr. 1990, 120, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.J.; Murray, A.B.; Murray, N.J.; Murray, M.B. Diet and cerebral malaria: The effect of famine and refeeding. Am. J. Clin. Nutr. 1978, 31, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Greene, L.S. Genetic and dietary adaptation to malaria in human populations. Parassitologia 1999, 41, 185–192. [Google Scholar]
- Modiano, D.; Petrarca, V.; Sirima, B.S.; Nebié, I.; Diallo, D.; Esposito, F.; Coluzzi, M. Different response to Plasmodium falciparum malaria in west African sympatric ethnic groups. Proc. Natl. Acad. Sci. USA 1996, 93, 13206–13211. [Google Scholar] [CrossRef] [PubMed]
- Modiano, D.; Chiucchiuini, A.; Petrarca, V.; Sirima, B.S.; Luoni, G.; Perlmann, H.; Esposito, F.; Coluzzi, M. Humoral response to Plasmodium falciparum Pf155/ring-infected erythrocyte surface antigen and Pf332 in three sympatric ethnic groups of Burkina Faso. Am. J. Trop. Med. Hyg. 1998, 58, 220–224. [Google Scholar] [CrossRef]
- Davis, T.M.; Binh, T.Q.; Danh, P.T.; Dyer, J.R.; St John, A.; Garcia-Webb, P.; Anh, T.K. Serum vitamin A and E concentrations in acute falciparum malaria: Modulators or markers of severity? Clin. Sci. 1994, 87, 505–511. [Google Scholar] [CrossRef]
- Eaton, J.W.; Eckman, J.R.; Berger, E.; Jacob, H.S. Suppression of malaria infection by oxidant-sensitive host erythrocytes. Nature 1976, 264, 758–760. [Google Scholar] [CrossRef]
- Friedman, M.J. Oxidant damage mediates variant red cell resistance to malaria. Nature 1979, 280, 245–247. [Google Scholar] [CrossRef]
- Levander, O.A. Selenium and sulfur in antioxidant protective systems: Relationships with vitamin E and malaria. Proc. Soc. Exp. Biol. Med. 1992, 200, 255–259. [Google Scholar] [CrossRef]
- Levander, O.A.; Ager, A.L., Jr.; Morris, V.C.; May, R.G. Qinghaosu, dietary vitamin E, selenium, and cod-liver oil: Effect on the susceptibility of mice to the malarial parasite Plasmodium yoelii. Am. J. Clin. Nutr. 1989, 50, 346–352. [Google Scholar] [CrossRef]
- Levander, O.A.; Ager, A.L., Jr. Malarial parasites and antioxidant nutrients. Parasitology 1993, 107, S95–S106. [Google Scholar] [CrossRef] [PubMed]
- Levander, O.A.; Fontela, R.; Morris, V.C.; Ager, A.L., Jr. Protection against murine cerebral malaria by dietary-induced oxidative stress. J. Parasitol. 1995, 81, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Shankar, A.H. Nutritional modulation of malaria morbidity and mortality. J. Infect. Dis. 2000, 182 (Suppl. 1), S37–S53. [Google Scholar] [CrossRef]
- Jishage, K.; Arita, M.; Igarashi, K.; Iwata, T.; Watanabe, M.; Ogawa, M.; Ueda, O.; Kamada, N.; Inoue, K.; Arai, H.; et al. Alpha-tocopherol transfer protein is important for the normal development of placental labyrinthine trophoblasts in mice. J. Biol. Chem. 2001, 276, 1669–1672. [Google Scholar] [CrossRef]
- Traber, M.G. Vitamin E regulatory mechanisms. Annu. Rev. Nutr. 2007, 27, 347–362. [Google Scholar] [CrossRef] [PubMed]
- Oram, J.F.; Vaughan, A.M.; Stocker, R. ATP-Binding cassette transporter A1 mediates cellular secretion of α-tocopherol. J. Biol. Chem. 2001, 276, 39898–39902. [Google Scholar] [CrossRef] [PubMed]
- Shichiri, M.; Takanezawa, Y.; Rotzoll, D.E.; Yoshida, Y.; Kokubu, T.; Ueda, K.; Tamai, H.; Arai, H. ATP-binding cassette transporter A1 is involved in hepatic alpha-tocopherol secretion. J. Nutr. Biochem. 2010, 21, 451–456. [Google Scholar] [CrossRef]
- Orso, E.; Bronccardo, C.; Kaminski, W.E.; Bottcher, A.; Liebish, G.; Drobnik, W.; Götz, A.; Chambenoit, O.; Diederich, W.; Langmann, T.; et al. Transport of lipids from Golgi to plasma membrane is defective in Tangier disease patients and Abc1-deficient mice. Nat. Genet. 2000, 24, 192–196. [Google Scholar] [CrossRef]
- Jacob, H.S.; Lux, S.E., IV. Degradation of membrane phospholipids and thiols in peroxide hemolysis: Studies in vitamin E deficiency. Blood 1968, 32, 549–568. [Google Scholar]
- Herbas, M.S.; Thekisoe, O.M.; Inoue, N.; Xuan, X.; Arai, H.; Suzuki, H. The effect of alpha-tocopherol transfer protein gene disruption on Trypanosoma congolense infection in mice. Free Radic. Biol. Med. 2009, 47, 1408–1413. [Google Scholar] [CrossRef]
- Traber, M.G.; Sokol, R.J.; Burton, G.W.; Ingold, K.U.; Papas, A.M.; Huffaker, J.E.; Kayden, H.J. Impaired ability of patients with familial isolated vitamin E deficiency to incorporate alpha-tocopherol into lipoproteins secreted by the liver. J. Clin. Investig. 1990, 85, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Herbas, M.S.; Ueta, Y.Y.; Ichikawa, C.; Chiba, M.; Ishibashi, K.; Shichiri, M.; Fukumoto, S.; Yokoyama, N.; Takeya, M.; Xuan, X.; et al. Alpha-tocopherol transfer protein disruption confers resistance to malarial infection in mice. Malar. J. 2010, 9, 101. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.W.; Levander, O.A.; Krishna, V.R.; Evans, C.B.; Morris, V.C.; Barta, J.R. Vitamin E-deficient diets enriched with fish oil suppress lethal Plasmodium yoelii infections in athymic and scid/bg mice. Infect. Immun. 1997, 65, 197–202. [Google Scholar] [PubMed]
- Herbas, M.S.; Ueta, Y.Y.; Ishibashi, K.; Suzuki, H. Expression of erythropoietic cytokines in α-tocopherol transfer protein knockout mice with murine malaria infection. Parasitol. Res. 2011, 109, 1243–1250. [Google Scholar] [CrossRef] [PubMed]
- van der Heyde, H.C.; Nolan, J.; Combes, V.; Gramaglia, I.; Grau, G.E. A unified hypothesis for the genesis of cerebral malaria: Sequestration, inflammation and hemostasis leading to microcirculatory dysfunction. Trends Parasitol. 2006, 22, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Herbas, M.S.; Okazaki, M.; Terao, E.; Xuan, X.; Arai, H.; Suzuki, H. Alpha-Tocopherol transfer protein inhibition is effective in the prevention of cerebral malaria in mice. Am. J. Clin. Nutr. 2010, 91, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Favre, N.; Da Laperousaz, C.; Ryffel, B.; Weiss, N.A.; Imhof, B.A.; Rudin, W.; Lucas, R.; Piguet, P.F. Role of ICAM-1 (CD54) in the development of murine cerebral malaria. Microbes Infect. 1999, 1, 961–968. [Google Scholar] [CrossRef]
- Kawazu, S.; Nozaki, T.; Tsuboi, T.; Nakano, Y.; Komaki-Yasuda, K.; Ikenoue, N.; Torii, M.; Kano, S. Expression profiles of peroxiredoxin proteins of the rodent malaria parasite Plasmodium yoelii. Int. J. Parasitol. 2003, 33, 1455–1461. [Google Scholar] [CrossRef]
- Komaki-Yasuda, K.; Kawazu, S.; Kano, S. Disruption of the Plasmodium falciparum 2-Cys peroxiredoxin gene renders parasites hypersensitive to reactive oxygen and nitrogen species. FEBS Lett. 2003, 547, 140–144. [Google Scholar] [CrossRef]
- Yano, K.; Komaki-Yasuda, K.; Kobayashi, T.; Takemae, H.; Kita, K.; Kano, S.; Kawazu, S. Expression of mRNAs and proteins for peroxiredoxins in Plasmodium falciparum erythrocytic stage. Parasitol. Int. 2005, 54, 35–41. [Google Scholar] [CrossRef]
- Rodrigues, J.R.; Gamboa, N.D. Effect of dequalinium on the oxidative stress in Plasmodium berghei-infected erythrocytes. Parasitol. Res. 2009, 104, 1491–1496. [Google Scholar] [CrossRef] [PubMed]
- Herbas, M.S.; Natama, M.H.; Suzuki, H. Alpha-tocopherol transfer protein gene inhibition enhances the acquired immune response during malaria infection in mice. Parasitol. Res. 2014, 113, 1019–1027. [Google Scholar] [CrossRef] [PubMed]
- Mueller, A.K.; Labaied, M.; Kappe, S.H.; Matuschewski, K. Genetically modified Plasmodium parasites as a protective experimental malaria vaccine. Nature 2005, 433, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Voza, T.; Vigário, A.M.; Belnoue, E.; Grüner, A.C.; Deschemin, J.C.; Kayibanda, M.; Delmas, F.; Janse, C.J.; Franke-Fayard, B.; Waters, A.P.; et al. Species-specific inhibition of cerebral malaria in mice coinfected with Plasmodium spp. Infect. Immun. 2005, 73, 4777–4786. [Google Scholar] [CrossRef] [PubMed]
- Niikura, M.; Kamiya, S.; Kita, K.; Kobayashi, F. Coinfection with nonlethal murine malaria parasites suppresses pathogenesis caused by Plasmodium berghei NK65. J. Immunol. 2008, 180, 6877–6884. [Google Scholar] [CrossRef] [PubMed]
- Ting, L.M.; Gissot, M.; Coppi, A.; Sinnis, P.; Kim, K. Attenuated Plasmodium yoelii lacking purine nucleoside phosphorylase confer protective immunity. Nat. Med. 2008, 14, 954–958. [Google Scholar] [CrossRef] [PubMed]
- Lamikanra, A.A.; Brown, D.; Potocnik, A.; Casals-Pascual, C.; Langhorne, J.; Roberts, D.J. Malarial anemia: Of mice and men. Blood 2007, 110, 18–28. [Google Scholar] [CrossRef]
- Ghosh, K.; Ghosh, K. Pathogenesis of anemia in malaria: A concise review. Parasitol. Res. 2007, 101, 1463–1469. [Google Scholar] [CrossRef]
- Maiese, K.; Chong, Z.Z.; Hou, J.; Shang, Y.C. Erythropoietin and oxidative stress. Curr. Neurovasc. Res. 2008, 5, 125–142. [Google Scholar] [CrossRef]
- Chang, K.H.; Stevenson, M.M. Malarial anaemia: Mechanisms and implications of insufficient erythropoiesis during blood-stage malaria. Int. J. Parasitol. 2004, 34, 1501–1516. [Google Scholar] [CrossRef]
- Chang, K.H.; Tam, M.; Stevenson, M.M. Inappropriately low reticulocytosis in severe malarial anemia correlates with suppression in the development of late erythroid precursors. Blood 2004, 103, 3727–3735. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.H.; Stevenson, M.M. Effect of anemia and renal cytokine production on erythropoietin production during blood-stage malaria. Kidney Int. 2004, 65, 1640–1646. [Google Scholar] [CrossRef] [PubMed]
- McDevitt, M.A.; Xie, J.; Ganapathy-Kanniappan, S.; Griffith, J.; Liu, A.; McDonald, C.; Thuma, P.; Gordeuk, V.R.; Metz, C.N.; Mitchell, R.; et al. A critical role for the host mediator macrophage migration inhibitory factor in the pathogenesis of malarial anemia. J. Exp. Med. 2006, 203, 1185–1196. [Google Scholar] [CrossRef] [PubMed]
- Halder, R.C.; Abe, T.; Mannoor, M.K.; Morshed, S.R.; Ariyasinghe, A.; Watanabe, H.; Kawamura, H.; Sekikawa, H.; Hamada, H.; Nishiyama, Y.; et al. Onset of hepatic erythropoiesis after malarial infection in mice. Parasitol. Int. 2003, 52, 259–268. [Google Scholar] [CrossRef]
- Giribaldi, G.; Ulliers, D.; Schwarzer, E.; Roberts, I.; Piacibello, W.; Arese, P. Hemozoin- and 4-hydroxynonenal-mediated inhibition of erythropoiesis. Possible role in malarial dyserythropoiesis and anemia. Haematologica 2004, 89, 492–493. [Google Scholar]
- Helleberg, M.; Goka, B.Q.; Akanmori, B.D.; Obeng-Adjei, G.; Rodriques, O.; Kurtzhals, J.A. Bone marrow suppression and severe anaemia associated with persistent Plasmodium falciparum infection in African children with microscopically undetectable parasitaemia. Malar. J. 2005, 4, 56. [Google Scholar] [CrossRef]
- Keller, C.C.; Yamo, O.; Ouma, C.; Ong’echa, J.M.; Ounah, D.; Hittner, J.B.; Vulule, J.M.; Perkins, D.J. Acquisition of hemozoin by monocytes down-regulates interleukin-12 p40 (IL-12p40) transcripts and circulating IL-12p70 through an IL-10-dependent mechanism: In vivo and in vitro findings in severe malarial anemia. Infect. Immun. 2006, 74, 5249–5260. [Google Scholar] [CrossRef]
- Engwerda, C.R.; Beattie, L.; Amante, F.H. The importance of the spleen in malaria. Trends Parasitol. 2005, 21, 75–80. [Google Scholar] [CrossRef]
- Min, K.C.; Kovall, R.A.; Hendrickson, W.A. Crystal structure of human alpha-tocopherol transfer protein bound to its ligand: Implications for ataxia with vitamin E deficiency. Proc. Natl. Acad. Sci. USA 2003, 100, 14713–14718. [Google Scholar] [CrossRef]
- Elinder, L.S.; Hådell, K.; Johansson, J.; Mølgaard, J.; Holme, I.; Olsson, A.G.; Walldius, G. Probucol treatment decreases serum concentrations of diet-derived antioxidants. Arterioscler. Thromb. Vasc. Biol. 1995, 15, 1057–1063. [Google Scholar] [CrossRef]
- Bird, D.A.; Tangirala, R.K.; Fruebis, J.; Steinberg, D.; Witztum, J.L.; Palinski, W. Effect of probucol on LDL oxidation and atherosclerosis in LDL receptor-deficient mice. J. Lipid Res. 1998, 39, 1079–1090. [Google Scholar] [PubMed]
- Choy, K.; Beck, K.; Png, F.Y.; Wu, B.J.; Leichtweis, S.B.; Thomas, S.R.; Hou, J.Y.; Croft, K.D.; Mori, T.A.; Stocker, R. Processes involved in the site-specific effect of probucol on atherosclerosis in apolipoprotein E gene knockout mice. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 1684–1690. [Google Scholar] [CrossRef] [PubMed]
- Herbas, M.S.; Shichiri, M.; Ishida, N.; Kume, A.; Hagihara, Y.; Yoshida, Y.; Suzuki, H. Probucol-induced α-tocopherol deficiency protects mice against malaria infection. PLoS ONE 2015, 10, e0136014. [Google Scholar] [CrossRef] [PubMed]
- Shaik, N.; Lupescu, A.; Lang, F. Inhibition of suicidal erythrocyte death by probucol. J. Cardiovasc. Pharmacol. 2013, 61, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Favari, E.; Zanotti, I.; Zimetti, F.; Ronda, N.; Bernini, F.; Rothblat, G.H. Probucol inhibits ABCA1-mediated cellular lipid efflux. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 2345–2350. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.A.; Tsujita, M.; Hayashi, M.; Yokoyama, S. Probucol inactivates ABCA1 in the plasma membrane with respect to its mediation of apolipoprotein binding and high density lipoprotein assembly and to its proteolytic degradation. J. Biol. Chem. 2004, 279, 30168–30174. [Google Scholar] [CrossRef] [PubMed]
- Seedorf, U.; Engel, T.; Lueken, A.; Bode, G.; Lorkowski, S.; Assmann, G. Cholesterol absorption inhibitor Ezetimibe blocks uptake of oxidized LDL in human macrophages. Biochem. Biophys. Res. Commun. 2004, 320, 1337–1341. [Google Scholar] [CrossRef] [PubMed]
- Kong, W.; Wei, J.; Abidi, P.; Lin, M.; Inaba, S.; Li, C.; Wang, Y.; Wang, Z.; Si, S.; Pan, H.; et al. Berberine is a novel cholesterol-lowering drug working through a unique mechanism distinct from statins. Nat. Med. 2004, 10, 1344–1351. [Google Scholar] [CrossRef]
- West, R.J.; Lloyd, J.K. The effect of cholestyramine on intestinal absorption. Gut 1975, 16, 93–98. [Google Scholar] [CrossRef]
- Kume, A.; Herbas, M.S.; Shichiri, M.; Ishida, N.; Suzuki, H. Effect of anti-hyperlipidemia drugs on the alpha-tocopherol concentration and their potential for murine malaria infection. Parasitol. Res. 2016, 115, 69–75. [Google Scholar] [CrossRef]
- Kume, A.; Anh, D.T.; Shichiri, M.; Ishida, N.; Suzuki, H. Probucol dramatically enhances dihydroartemisinin effect in murine malaria. Malar. J. 2016, 15, 472. [Google Scholar] [CrossRef]
- Wootton, J.C.; Feng, X.; Ferdig, M.T.; Cooper, R.A.; Mu, J.; Baruch, D.I. Genetic diversity and chloroquine selective sweeps in Plasmodium falciparum. Nature 2002, 418, 320–323. [Google Scholar] [CrossRef]
- Attaran, A.; Barnes, K.I.; Curtis, C.; d’Alessandro, U.; Fanello, C.I.; Galinski, M.R. WHO, the Global Fund, and medical malpractice in malaria treatment. Lancet 2004, 363, 237–240. [Google Scholar] [CrossRef]
- Sutherland, C.J.; Haustein, T.; Gadalla, N.; Armstrong, M.; Doherty, J.F.; Chiodini, P.L. Chloroquine-resistant Plasmodium falciparum infections among UK travellers returning with malaria after chloroquine prophylaxis. J. Antimicrob. Chemother. 2007, 59, 1197–1199. [Google Scholar] [CrossRef]
- White, N.J. Qinghaosu (artemisinin): The price of success. Science 2008, 320, 330–334. [Google Scholar] [CrossRef]
- “Noedl, H.; Se, Y.; Smith, B.L.; Socheat, D.; Fukuda, M.M. Evidence of artemisinin-resistant malaria in western Cambodia. N. Engl. J. Med. 2008, 359, 2619–2620. [Google Scholar]
- World Health Organization. World Malaria Report 2014; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- White, N.J. Preventing antimalarial drug resistance through combinations. Drug Resist. Updat. 1998, 1, 3–9. [Google Scholar] [CrossRef]
- Hodel, E.M.; Kay, K.; Hayes, D.J.; Terlouw, D.J.; Hastings, I.M. Optimizing the programmatic deployment of the anti-malarials artemether-lumefantrine and dihydroartemisinin-piperaquine using pharmacological modelling. Malar. J. 2014, 13, 138. [Google Scholar] [CrossRef]
- World Health Organization. Artemisinin Resistance and Artemisinin-Based Combination Therapy Efficacy; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Ashley, E.A.; Dhorda, M.; Fairhurst, R.M.; Amaratunga, C.; Lim, P.; Suon, S.; Sreng, S.; Anderson, J.M.; Mao, S.; Sam, B.; et al. Tracking Resistance to Artemisinin Collaboration (TRAC). Spread of artemisinin resistance in Plasmodium falciparum malaria. N. Engl. J. Med. 2014, 371, 411–423. [Google Scholar] [CrossRef]
- World Health Organization. Status Report on Artemisinin Resistance; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Krungkrai, S.R.; Yuthavong, Y. The antimalarial action on Plasmodium falciparum of qinghaosu and artesunate in combination with agents which modulate oxidant stress. Trans. R. Soc. Trop. Med. Hyg. 1987, 81, 710–714. [Google Scholar] [CrossRef]
- Meshnick, S.R.; Yang, Y.Z.; Lima, V.; Kuypers, F.; Kamchonwongpaisan, S.; Yuthavong, Y. Iron-dependent free radical generation from the antimalarial agent artemisinin (qinghaosu). Antimicrob. Agents Chemother. 1993, 37, 1108–1114. [Google Scholar] [CrossRef]
- Zhang, F.; Gosser, D.K., Jr.; Meshnick, S.R. Hemin-catalyzed decomposition of artemisinin (qinghaosu). Biochem. Pharmacol. 1992, 43, 1805–1809. [Google Scholar] [CrossRef]
- Woodrow, C.J.; Haynes, R.K.; Krishna, S. Artemisinins. Postgrad. Med. J. 2005, 81, 71–78. [Google Scholar] [CrossRef]
- Meshnick, S.R. Artemisinin: Mechanisms of action, resistance and toxicity. Int. J. Parasitol. 2002, 32, 1655–1660. [Google Scholar] [CrossRef]
- Awodele, O.; Emeka, P.M.; Akintonwa, A.; Aina, O.O. Antagonistic effect of vitamin E on the efficacy of artesunate against Plasmodium berghei infection in mice. Afr. J. Biomed. Res. 2007, 10, 51–57. [Google Scholar] [CrossRef]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suzuki, H.; Kume, A.; Herbas, M.S. Potential of Vitamin E Deficiency, Induced by Inhibition of α-Tocopherol Efflux, in Murine Malaria Infection. Int. J. Mol. Sci. 2019, 20, 64. https://doi.org/10.3390/ijms20010064
Suzuki H, Kume A, Herbas MS. Potential of Vitamin E Deficiency, Induced by Inhibition of α-Tocopherol Efflux, in Murine Malaria Infection. International Journal of Molecular Sciences. 2019; 20(1):64. https://doi.org/10.3390/ijms20010064
Chicago/Turabian StyleSuzuki, Hiroshi, Aiko Kume, and Maria Shirely Herbas. 2019. "Potential of Vitamin E Deficiency, Induced by Inhibition of α-Tocopherol Efflux, in Murine Malaria Infection" International Journal of Molecular Sciences 20, no. 1: 64. https://doi.org/10.3390/ijms20010064
APA StyleSuzuki, H., Kume, A., & Herbas, M. S. (2019). Potential of Vitamin E Deficiency, Induced by Inhibition of α-Tocopherol Efflux, in Murine Malaria Infection. International Journal of Molecular Sciences, 20(1), 64. https://doi.org/10.3390/ijms20010064



