Clinically Relevant Anti-Inflammatory Agents for Chemoprevention of Colorectal Cancer: New Perspectives
Abstract
:1. Introduction
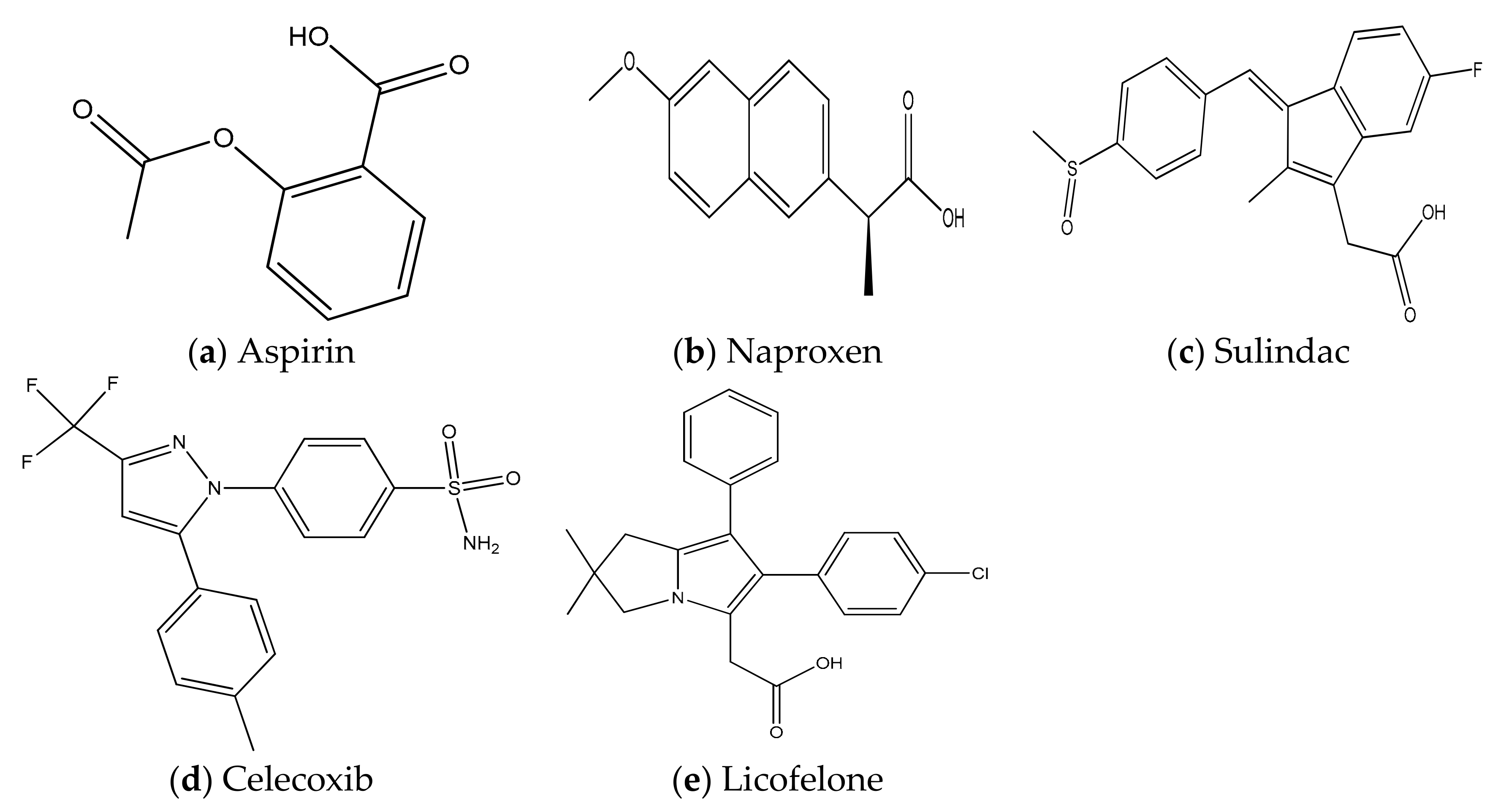
2. Selected Anti-Inflammatory Agents for Colon Cancer Prevention
2.1. NSAIDS for Colon Cancer Prevention
2.1.1. Aspirin for CRC Prevention
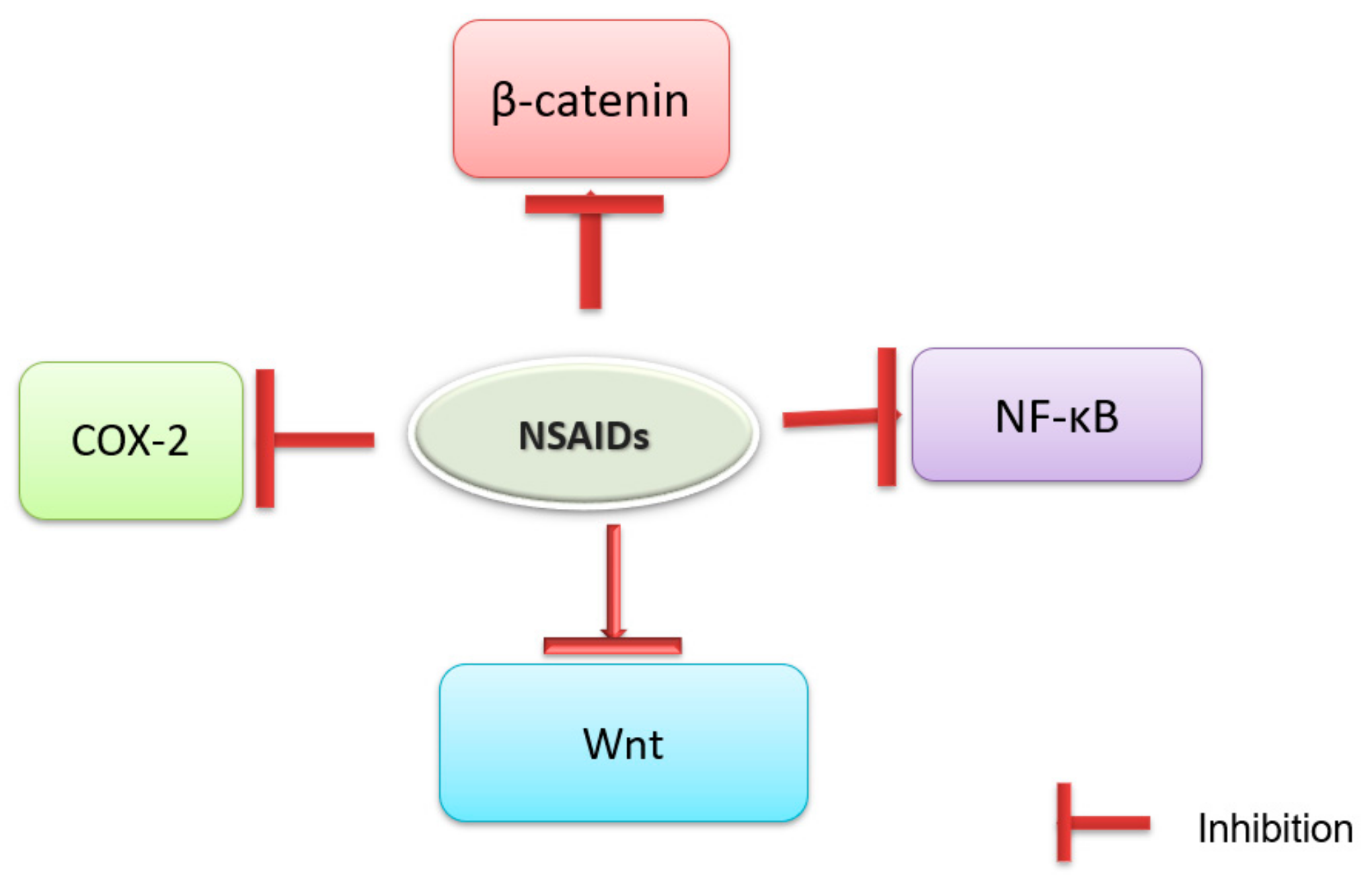
Molecular Targets
Pre-clinical Studies
Clinical Studies
Toxicity and Overcoming Strategies
2.1.2. Naproxen for CRC Prevention
Molecular Targets
Pre-clinical Studies
Clinical Studies
Toxicity and Overcoming Strategies
2.1.3. Sulindac for CRC Prevention
Molecular Targets
Pre-clinical Studies
Clinical Studies
Toxicity and Overcoming Strategies
2.1.4. Celecoxib for CRC Prevention
Molecular Targets
Pre-Clinical Studies
Clinical Studies
Toxicity and Overcoming Strategies
2.1.5. Licofelone for CRC Prevention
Molecular Targets
Preclinical Trials
Toxicities and Limitations
2.2. Combinational Intervention
3. Conclusions and Perspectives
Acknowledgments
Conflicts of Interest
Abbreviations
| ACF | Aberrant Crypt Foci |
| APC | Adenomatous Polyposis Coli |
| AMPK | Adenosine Monophosphate-activated Protein Kinase |
| AOM | Azoxymethane |
| CRC | Colorectal Cancers |
| COX | Cyclooxygenases |
| DFMO | Difluoromethylornithine |
| DMH | Dimethylhydrazine |
| FAP | Familial Adenomatous Polyposis |
| GI | Gastrointestinal |
| H2S | Hydrogen Sulfide |
| NOS | Nitric Oxide Synthase |
| NSAIDs | Non-Steroidal Anti-inflammatory Drugs |
| MPGES | Microsomal Prostaglandin E Synthase |
| PCNA | Proliferating Cell Nuclear Antigen |
| PGs | Prostaglandins |
References
- Arnold, M.; Sierra, M.S.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017, 66, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Cronin, K.A.; Lake, A.J.; Scott, S.; Sherman, R.L.; Noone, A.M.; Howlader, N.; Henley, S.J.; Anderson, R.N.; Firth, A.U.; Ma, J.; et al. Annual Report to the Nation on the Status of Cancer, part I: National cancer statistics. Cancer 2018, 124, 2785–2800. [Google Scholar] [CrossRef] [PubMed]
- Cancer Stat Facts: Colorectal Cancer. Available online: https://seer.cancer.gov/statfacts/html/colorect.html (accessed on 5 July 2018).
- American Cancer Society 2018: Cancer Facts & Figures 2018; American Cancer Society: Atlanta, GA, USA, 2018; p. 13.
- Jemal, A.; Thomas, M.T.; Thun, M. Cancer statistics, 2002. CA Cancer J. Clin. 2002, 52, 23–47. [Google Scholar] [CrossRef] [PubMed]
- Hardy, R.G.; Meltzer, S.J.; Jankowski, J.A. ABC of colorectal cancer. Molecular basis for risk factors. BMJ 2000, 321, 886–889. [Google Scholar] [CrossRef] [PubMed]
- Long, A.G.; Lundsmith, E.T.; Hamilton, K.E. Inflammation and Colorectal Cancer. Curr. Colorectal Cancer Rep. 2017, 13, 341–351. [Google Scholar] [CrossRef] [PubMed]
- Rasool, S.; Kadla, S.A.; Rasool, V.; Ganai, B.A. A comparative overview of general risk factors associated with the incidence of colorectal cancer. Tumor Biol. 2013, 34, 2469–2476. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.H.; Jung, Y.S.; Park, J.H.; Park, D.I.; Sohn, C.I. Abdominal Obesity is More Predictive of Advanced Colorectal Neoplasia Risk Than Overall Obesity in Men: A Cross-sectional Study. J. Clin. Gastroenterol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Chan, A.T.; Slattery, M.L.; Chang-Claude, J.; Potter, J.D.; Gallinger, S.; Caan, B.; Lampe, J.W.; Newcomb, P.A.; Zubair, N.; et al. Influence of smoking, body mass index and other factors on the preventive effect of nonsteroidal anti-inflammatory drugs on colorectal cancer risk. Cancer Res. 2018. [Google Scholar] [CrossRef] [PubMed]
- Hirai, H.W.; Ching, J.Y.L.; Wu, J.C.Y.; Sung, J.J.Y.; Chan, F.K.L.; Ng, S.C. Risk factors for advanced colorectal neoplasms in the proximal colon in 6218 subjects undergoing complete colonoscopy. J. Gastroenterol. Hepatol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Hamoya, T.; Fujii, G.; Miyamoto, S.; Takahashi, M.; Totsuka, Y.; Wakabayashi, K.; Toshima, J.; Mutoh, M. Effects of NSAIDs on the risk factors of colorectal cancer: A mini review. Genes Environ. 2016, 38, 6. [Google Scholar] [CrossRef] [PubMed]
- Soravia, C.; Berk, T.; Madlensky, L.; Mitri, A.; Cheng, H.; Gallinger, S.; Cohen, Z.; Bapat, B. Genotype-phenotype correlations in attenuated adenomatous polyposis coli. Am. J. Hum. Genet. 1998, 62, 1290–1301. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, N.K.; William, F.D. APC and its modifiers in colon cancer. Adv. Exp. Med. Biol. 2009, 656, 85–106. [Google Scholar]
- Vincent, W.Y.; Agnieszka, B.B. Intestinal Tumorigenesis: Mechanisms of Development & Progression; Springer: New York, NY, USA, 2015; pp. 1–445. [Google Scholar]
- Sancho, E.; Batlle, E.; Clevers, H. Signalling pathways in intestinal development and cancer. Annu. Rev. Cell Dev. Biol. 2004, 20, 695–723. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, B.; Sillars-Hardebol, A.H.; Postma, C.; Mongera, S.; Terhaar Sive Droste, J.; Obulkasim, A.; van de Wiel, M.; van Criekinge, W.; Ylstra, B.; Fijneman, R.J.; et al. Colorectal adenoma to carcinoma progression is accompanied by changes in gene expression associated with ageing, chromosomal instability, and fatty acid metabolism. Cell Oncol. 2012, 35, 53–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Septer, S.; Lawson, C.E.; Anant, S.; Attard, T. Familial adenomatous polyposis in pediatrics: Natural history, emerging surveillance and management protocols, chemopreventive strategies, and areas of ongoing debate. Fam. Cancer 2016, 15, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Boursi, B.; Arber, N. Current and future clinical strategies in colon cancer prevention and the emerging role of chemoprevention. Curr. Pharm Des. 2007, 13, 2274–2282. [Google Scholar] [CrossRef] [PubMed]
- Jun, Y. Tumor progression and metastasis. Carcinogenesis 2000, 21, 497–503. [Google Scholar] [Green Version]
- Grancher, A.; Michel, P.; Di Fiore, F.; Sefrioui, D. Aspirin and colorectal cancer. Bull Cancer 2018, 105, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Drew, D.A.; Cao, Y.; Chan, A.T. Aspirin and colorectal cancer: The promise of precision chemoprevention. Nat. Rev. Cancer 2016, 16, 173–186. [Google Scholar] [CrossRef] [PubMed]
- Alfonso, L.; Ai, G.; Spitale, R.C.; Bhat, G.J. Molecular targets of aspirin and cancer prevention. Br. J. Cancer 2014, 111, 61–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gala, M.K.; Chan, A.T. Molecular pathways: Aspirin and Wnt signaling-a molecularly targeted approach to cancer prevention and treatment. Clin. Cancer Res. 2015, 21, 1543–1548. [Google Scholar] [CrossRef] [PubMed]
- Reuter, B.K.; Zhang, X.J.; Miller, M.J. Therapeutic utility of aspirin in the ApcMin/+ murine model of colon carcinogenesis. BMC Cancer 2002, 2, 19. [Google Scholar] [CrossRef] [Green Version]
- Chen, J.; Stark, L.A. Aspirin Prevention of Colorectal Cancer: Focus on NF-κB Signalling and the Nucleolus. Biomedicines 2017, 5, 43. [Google Scholar] [CrossRef] [PubMed]
- Luciani, M.G.; Campregher, C.; Gasche, C. Aspirin blocks proliferation in colon cells by inducing a G1 arrest and apoptosis through activation of the checkpoint kinase ATM. Carcinogenesis 2007, 28, 2207–2217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stark, L.A.; Reid, K.; Sansom, O.J.; Din, F.V.; Guichard, S.; Mayer, I.; Jodrell, D.I.; Clarke, A.R.; Dunlop, M.G. Aspirin activates the NF-kappaB signalling pathway and induces apoptosis in intestinal neoplasia in two in vivo models of human colorectal cancer. Carcinogenesis 2007, 28, 968–976. [Google Scholar] [CrossRef] [PubMed]
- Rao, C.V.; Reddy, B.S.; Steele, V.E.; Wang, C.X.; Liu, X.; Ouyang, N.; Patlolla, J.M.; Simi, B.; Kopelovich, L.; Rigas, B. Nitric oxide–releasing aspirin and indomethacin are potent inhibitors against colon cancer in azoxymethane-treated rats: Effects on molecular targets. Mol. Cancer Ther. 2006, 5, 1530–1538. [Google Scholar] [CrossRef] [PubMed]
- Kagbo-Kue, S.; Ajose, T.; Bakinde, N. Aspirin inhibited the metastasis of colon cancer cells by inhibiting the expression of toll-like receptor 4. Cell Biosci. 2018, 8, 36. [Google Scholar] [CrossRef] [PubMed]
- Wargovich, M.J.; Chen, C.D.; Harris, C.; Yang, E.; Velasco, M. Inhibition of aberrant crypt growth by non-steroidal anti-inflammatory agents and differentiation agents in the rat colon. Int. J. Cancer 1995, 60, 515–519. [Google Scholar] [CrossRef] [PubMed]
- Barnes, C.J.; Hardman, W.E.; Cameron, I.L.; Lee, M. Aspirin, but not sodium salicylate, indomethacin, or nabumetone, reversibly suppresses 1,2-dimethylhydrazine-induced colonic aberrant crypt foci in rats. Dig. Dis. Sci. 1997, 42, 920–926. [Google Scholar] [CrossRef] [PubMed]
- Bak, A.W.; McKnight, W.; Li, P.; Del, S.P.; Calignano, A.; Cirino, G.; Wallace, J.L. Cyclooxygenase-independent chemoprevention with an aspirin derivative in a rat model of colonic adenocarcinoma. Life Sci. 1998, 62, 367–373. [Google Scholar] [CrossRef]
- Verma, S.; Das, P.; Kumar, V.L. Chemoprevention by artesunate in a preclinical model of colorectal cancer involves down regulation of β-catenin, suppression of angiogenesis, cellular proliferation and induction of apoptosis. Chem. Biol. Interact. 2017, 278, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Shpitz, B.; Bomstein, Y.; Kariv, N.; Shalev, M.; Buklan, G.; Bernheim, J. Chemopreventive effect of aspirin on growth of aberrant crypt foci in rats. Int. J. Colorectal Dis. 1998, 13, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Kanwar, S.S.; Vaiphei, K.; Nehru, B.; Sanyal, S.N. Chemopreventive effects of nonsteroidal anti-inflammatory drugs on 1,2-dimethylhydrazine-induced colon carcinogenesis in rats. Toxicol. Mech. Methods 2007, 17, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Reddy, B.S.; Rao, C.V.; Rivenson, A.; Kelloff, G. Inhibitory effect of aspirin on azoxymethane-induced colon carcinogenesis in F344 rats. Carcinogenesis 1993, 14, 1493–1497. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, A.; Janakiram, N.B.; Madka, V.; Zhang, Y.; Singh, A.; Biddick, L.; Li, Q.; Lightfoot, S.; Steele, V.E.; Lubet, R.; et al. Intermittent dosing regimens of naproxen and aspirin inhibit azoxymethane-induced rat colon adenoma progression to adenocarcinoma and carcinoma invasion. In Proceedings of the AACR Annual Meeting of the American Association for Cancer Research, Chicago, IL, USA, 14–18 April 2018. Abstract Number, 4983. [Google Scholar]
- Bosetti, C.; Rosato, V.; Gallus, S.; Cuzick, J.; La Vecchia, C. Aspirin and cancer risk: A quantitative review to 2011. Ann. Oncol. 2012, 23, 1403–1415. [Google Scholar] [CrossRef] [PubMed]
- Ruder, E.H.; Laiyemo, A.O.; Graubard, B.I.; Hollenbeck, A.R.; Schatzkin, A.; Cross, A.J. Non-steroidal anti-inflammatory drugs and colorectal cancer risk in a large, prospective cohort. Am, J. Gastroenterol. 2011, 106, 1340–1350. [Google Scholar] [CrossRef] [PubMed]
- Friis, S.; Riis, A.H.; Erichsen, R.; Baron, J.A.; Sorensen, H.T. Low-Dose Aspirin or Nonsteroidal Anti-inflammatory Drug Use and Colorectal Cancer Risk: A. Population-Based, Case-Control Study. Ann. Intern. Med. 2015, 163, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Benamouzig, R.; Deyra, J.; Martin, A.; Girard, B.; Jullian, E.; Piednoir, B.; Couturier, D.; Coste, T.; Little, J.; Chaussade, S. Daily soluble aspirin and prevention of colorectal adenoma recurrence: One-year results of the APACC trial. Gastroenterology 2003, 125, 328–336. [Google Scholar] [CrossRef]
- Benamouzig, R.; Uzzan, B.; Deyra, J.; Martin, A.; Girard, B.; Little, J.; Chaussade, S.; Association pour la Prévention par l’Aspirine du Cancer Colorectal Study Group (APACC). Prevention by daily soluble aspirin of colorectal adenoma recurrence: 4-year results of the APACC randomised trial. Gut 2012, 61, 255–261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baron, J.A.; Cole, B.F.; Sandler, R.S.; Haile, R.W.; Ahnen, D.; Bresalier, R.; McKeown-Eyssen, G.; Summers, R.W.; Rothstein, R.; Burke, C.A.; et al. A randomized trial of aspirin to prevent colorectal adenomas. N. Engl. J. Med. 2003, 348, 891–899. [Google Scholar] [CrossRef] [PubMed]
- Cole, B.F.; Logan, R.F.; Halabi, S.; Benamouzig, R.; Sandler, R.S.; Grainge, M.J.; Chaussade, S.; Baron, J.A. Aspirin for the chemoprevention of colorectal adenomas: Meta-analysis of the randomized trials. J. Natl. Cancer Inst. 2009, 101, 256–266. [Google Scholar] [CrossRef] [PubMed]
- Sandler, R.S.; Halabi, S.; Baron, J.A.; Budinger, S.; Paskett, E.; Keresztes, R.; Petrelli, N.; Pipas, J.M.; Karp, D.D.; Loprinzi, C.L.; et al. A randomized trial of aspirin to prevent colorectal adenomas in patients with previous colorectal cancer. N. Engl. J. Med. 2003, 348, 883–890. [Google Scholar] [CrossRef] [PubMed]
- Logan, R.F.A.; Grainge, M.J.; Shepherd, V.C.; Armitage, N.C.; Muir, K.R. Aspirin and folic acid for the prevention of recurrent colorectal adenomas. Gastroenterology 2008, 134, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Aspirin in Preventing Colorectal Cancer in Patients with Colorectal Adenoma. Clinical Trial Identification Number: NCT02965703. Available online: https://clinicaltrials.gov/ct2/show/NCT02965703 (accessed on 15 July 2018).
- Aspirin for Prevention of Postsurgical Recurrence and Metastasis in Asian Colorectal Cancer Patients: A Multi-center Randomized Trial (APREMEC). Clinical Trial Identification Number: NCT02607072. Available online: https://clinicaltrials.gov/ct2/show/NCT02607072 (accessed on 1 July 2018).
- Aspirin in Colorectal Cancer Liver Metastases (ASAC). Clinical Trial Identification Number: NCT03326791. Available online: https://clinicaltrials.gov/ct2/show/NCT03326791 (accessed on 1 July 2018).
- A Trial of Aspirin on Recurrence and Survival in Colon Cancer Patients (ASPIRIN). Clinical Trial Identification Number: NCT02301286. Available online: https://clinicaltrials.gov/ct2/show/NCT02301286 (accessed on 1 July 2018).
- Finding the Best Dose of Aspirin to Prevent Lynch Syndrome Cancers. Clinical Trial Identification Number: NCT02497820. Available online: https://clinicaltrials.gov/ct2/show/NCT02497820 (accessed on 1 July 2018).
- Hamada, T.; Cao, Y.; Qian, Z.R.; Masugi, Y.; Nowak, J.A.; Yang, J.; Song, M.; Mima, K.; Kosumi, K.; Liu, L.; et al. Aspirin Use and Colorectal Cancer Survival According to Tumor CD274 (Programmed Cell Death 1 Ligand 1) Expression Status. J. Clin. Oncol. 2017, 35, 1836–1844. [Google Scholar] [CrossRef] [PubMed]
- Patrignani, P.; Sacco, A.; Sostres, C.; Bruno, A.; Dovizio, M.; Piazuelo, E.; Di Francesco, L.; Contursi, A.; Zucchelli, M.; Schiavone, S.; et al. Low-Dose Aspirin Acetylates Cyclooxygenase-1 in Human Colorectal Mucosa: Implications for the Chemoprevention of Colorectal Cancer. Clin. Pharmacol. Ther. 2017, 102, 52–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frouws, M.A.; Bastiaannet, E.; Langley, R.E.; Chia, W.K.; van Herk-Sukel, M.P.; Lemmens, V.E.; Putter, H.; Hartgrink, H.H.; Bonsing, B.A.; Van de Velde, C.J.; et al. Effect of low-dose aspirin use on survival of patients with gastrointestinal malignancies; an observational study. Br. J. Cancer 2017, 116, 405–413. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gray, R.T.; Cantwell, M.M.; Coleman, H.G.; Loughrey, M.B.; Bankhead, P.; McQuaid, S.; O’Neill, R.F.; Arthur, K.; Bingham, V.; McGready, C.; et al. Evaluation of PTGS2 Expression, PIK3CA Mutation, Aspirin Use and Colon Cancer Survival in a Population-Based Cohort Study. Clin. Transl. Gastroenterol. 2017, 8, e91. [Google Scholar] [CrossRef] [PubMed]
- Gray, R.T.; Coleman, H.G.; Hughes, C.; Murray, L.J.; Cardwell, C.R. Low-dose aspirin use and survival in colorectal cancer: Results from a population-based cohort study. BMC Cancer 2018, 18, 228. [Google Scholar] [CrossRef] [PubMed]
- Veettil, S.K.; Lim, K.G.; Ching, S.M.; Saokaew, S.; Phisalprapa, P.; Chaiyakunapruk, N. Effects of aspirin and non-aspirin nonsteroidal anti-inflammatory drugs on the incidence of recurrent colorectal adenomas: A systematic review with meta-analysis and trial sequential analysis of randomized clinical trials. BMC Cancer 2017, 17, 763. [Google Scholar] [CrossRef] [PubMed]
- Adjuvant Aspirin Treatment for Colon Cancer Patients. Clinical Trial Identification Number: NCT02467582. Available online: https://clinicaltrials.gov/ct2/show/NCT02467582 (accessed on 1 June 2018).
- Adjuvant Low Dose Aspirin in Colorectal Cancer (ALASCCA). Clinical Trial Identification Number: NCT02647099. Available online: https://clinicaltrials.gov/ct2/show/NCT02647099 (accessed on 1 June 2018).
- Aspirin for Dukes C and High Risk Dukes B Colorectal Cancers (ASCOLT). Clinical Trial Identification Number: NCT00565708. Available online: https://clinicaltrials.gov/ct2/show/NCT00565708 (accessed on 5 June 2018).
- Varga, Z.; Sabzwari, S.R.A.; Vargova, V. Cardiovascular Risk of Nonsteroidal Anti-Inflammatory Drugs: An Under-Recognized Public Health Issue. Cureus 2017, 9, e1144. [Google Scholar] [CrossRef] [PubMed]
- Sostres, C.; Gargallo, C.J.; Lanas, A. Nonsteroidal anti-inflammatory drugs and upper and lower gastrointestinalmucosal damage. Arthritis Res. Ther. 2013, 15, S3. [Google Scholar] [CrossRef] [PubMed]
- Endo, H.; Sakai, E.; Kato, T.; Umezawa, S.; Higurashi, T.; Ohkubo, H.; Nakajima, A. Small bowel injury in low-dose aspirin users. J. Gastroenterol. 2015, 50, 378–386. [Google Scholar] [CrossRef] [PubMed]
- Kodela, R.; Chattopadhyay, M.; Velázquez-Martínez, C.A.; Kashfi, K. NOSH-aspirin (NBS-1120), a novel nitric oxide-and hydrogen sulfide releasing hybrid has enhanced chemopreventive properties compared to aspirin, is gastrointestinal safe with all the classic therapeutic indications. Biochem. Pharmacol. 2015, 98, 564–572. [Google Scholar] [CrossRef] [PubMed]
- Paul-Clark, M.; Elsheikh, W.; Kirkby, N.; Chan, M.; Devchand, P.; Agbor, T.A.; Flannigan, K.L.; Cheadle, C.; Freydin, M.; Ianaro, A.; et al. Profound Chemopreventative Effects of a Hydrogen Sulfide-Releasing NSAID in the APCMin/+ Mouse Model of Intestinal Tumorigenesis. PLoS ONE 2016, 11, e0147289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elsheikh, W.; Blackler, R.W.; Flannigan, K.L.; Wallace, J.L. Enhanced chemopreventive effects of a hydrogen sulfide-releasing anti-inflammatory drug (ATB-346) in experimental colorectal cancer. Nitric Oxide. 2014, 41, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Suh, N.; Reddy, B.S.; DeCastro, A.; Paul, S.; Lee, H.J.; Smolarek, A.K.; So, J.Y.; Simi, B.; Wang, C.X.; Janakiram, N.B.; et al. Combination of atorvastatin with sulindac or naproxen profoundly inhibits colonic adenocarcinomas by suppressing the p65/β-catenin/cyclin D1 signaling pathway in rats. Cancer Prev. Res. 2011, 4, 1895–1902. [Google Scholar] [CrossRef] [PubMed]
- Naproxen in Preventing DNA Mismatch Repair Deficient Colorectal Cancer in Patients with Lynch Syndrome. Clinical Trial Identification Number: NCT02052908. Available online: https://clinicaltrials.gov/ct2/show/NCT02052908 (accessed on 2 June 2018).
- Lisse, J.R.; Perlman, M.; Johansson, G.; Shoemaker, J.R.; Schechtman, J.; Skalky, C.S.; Dixon, M.E.; Polis, A.B.; Mollen, A.J.; Geba, G.P.; et al. Gastrointestinal tolerability and effectiveness of rofecoxib versus naproxen in the treatment of osteoarthritis: A randomized, controlled trial. Ann. Intern. Med. 2003, 139, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Chattopadhyay, M.; Kodela, R.; Duvalsaint, P.L.; Kashfi, K. Gastrointestinal safety, chemotherapeutic potential, and classic pharmacological profile of NOSH-naproxen (AVT-219) a dual NO- and H2S-releasing hybrid. Pharmacol. Res. Perspect. 2016, 4, e00224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rao, C.V.; Rivenson, A.; Simi, B.; Zang, E.; Kelloff, G.; Steele, V.; Reddy, B.S. Chemoprevention of colon carcinogenesis by sulindac, a nonsteroidal anti-inflammatory agent. Cancer Res. 1995, 55, 1464–1472. [Google Scholar] [PubMed]
- Takayama, T.; Nagashima, H.; Maeda, M.; Nojiri, S.; Hirayama, M.; Nakano, Y.; Takahashi, Y.; Sato, Y.; Sekikawa, H.; Mori, M.; et al. Randomized double-blind trial of sulindac and etodolac to eradicate aberrant crypt foci and to prevent sporadic colorectal polyps. Clin. Cancer Res. 2011, 17, 3803–3811. [Google Scholar] [CrossRef] [PubMed]
- Reddy, B.S.; Hirose, Y.; Lubet, R.; Steele, V.; Kelloff, G.; Paulson, S.; Seibert, K.; Rao, C.V. Chemoprevention of colon cancer by specific cyclooxygenase-2 inhibitor, celecoxib, administered during different stages of carcinogenesis. Cancer Res. 2000, 60, 293–297. [Google Scholar] [PubMed]
- Wang, J.; Cho, N.L.; Zauber, A.G.; Hsu, M.; Dawson, D.; Srivastava, A.; Mitchell-Richards, K.A.; Markowitz, S.D.; Bertagnolli, M.M. Chemopreventive Efficacy of the Cyclooxygenase-2 (COX-2) Inhibitor, Celecoxib, Is Predicted by Adenoma Expression of COX-2 and 15-PGDH. Cancer Epidemiol. Biomarkers Prev. 2018. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.D.; McMurray, J.J.; Pfeffer, M.A.; Wittes, J.; Fowler, R.; Finn, P.; Anderson, W.F.; Zauber, A.; Hawk, E.; Bertagnolli, M. Adenoma Prevention with Celecoxib (APC) Study Investigators. Cardiovascular risk associated with celecoxib in a clinical trial for colorectal adenoma prevention. N. Engl. J. Med. 2005, 352, 1071–1080. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, A.; Janakiram, N.B.; Li, Q.; Choi, CI.; Zhang, Y.; Steele, V.E.; Rao, C.V. Chemoprevention of colon and small intestinal tumorigenesis in APC(Min/+) mice by licofelone, a novel dual 5-LOX/COX inhibitor: Potential implications for human colon cancer prevention. Cancer Prev. Res. 2011, 4, 2015–2026. [Google Scholar] [CrossRef] [PubMed]
- Samaha, H.S.; Kelloff, G.J.; Steele, V.; Rao, C.V.; Reddy, B.S. Modulation of apoptosis by sulindac, curcumin, phenylethyl-3-methylcaffeate, and 6-phenylhexyl isothiocyanate: Apoptotic index as a biomarker in colon cancer chemoprevention and promotion. Cancer Res. 1997, 57, 1301–1305. [Google Scholar] [PubMed]
- Singh, J.; Reddy, B.S. Molecular markers in chemoprevention of colon cancer. Inhibition of expression of ras-p21 and p53 by sulindac during azoxymethane-induced colon carcinogenesis. Ann. N. Y. Acad. Sci. 1995, 768, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Moorghen, M.; Ince, P.; Finney, K.J.; Sunter, J.P.; Appleton, D.R.; Watson, A.J. A protective effect of sulindac against chemically-induced primary colonic tumours in mice. 1. J. Pathol. Clin. Res. 1988, 156, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Skinner, S.A.; Penney, A.G.; OBrien, P.E. Sulindac inhibits the rate of growth and appearance of colon tumors in the rat. Arch. Surg. 1991, 126, 1094–1096. [Google Scholar] [CrossRef] [PubMed]
- Kelloff, G.J.; Crowell, J.A.; Boone, C.W.; Steele, V.E.; Lubet, R.A.; Greenwald, P.; Alberts, D.S.; Covey, J.M.; Doody, L.A.; Knapp, G.G.; et al. Clinical development plan: Sulindac. J. Cell Biochem. Suppl. 1994, 20, 240–251. [Google Scholar] [PubMed]
- Alberts, D.; Hixson, L.; Ahnen, D.; Bogert, C.; Einspahr, J.; Brendel, K.; Gross, P.; Paranka, N.; Burt, R.; Pamukcu, R. Do non-steroidal anti-inflammatory drugs (NSAIDs) inhibit rat azoxymethane (AOM) colon carcinogenesis through inhibition of colonic mucosal prostaglandin synthesis? Proc. Am. Assoc. Cancer Res. 1994, 35, 632. [Google Scholar]
- Femia, A.P.; Soares, P.V.; Luceri, C.; Lodovici, M.; Giannini, A.; Caderni, G. Sulindac, 3,3′-diindolylmethane and curcumin reduce carcinogenesis in the Pirc rat, an Apc-driven model of colon carcinogenesis. BMC Cancer 2015, 15, 611. [Google Scholar] [CrossRef] [PubMed]
- Giardiello, F.M.; Hamilton, S.R.; Krush, A.J.; Piantadosi, S.; Hylind, L.M.; Celano, P.; Booker, S.V.; Robinson, C.R.; Offerhaus, G.J. Treatment of colonic and rectal adenomas with sulindac in familial adenomatous polyposis. N. Engl. J. Med. 1993, 328, 1313–1316. [Google Scholar] [CrossRef] [PubMed]
- Giardiello, F.M.; Yang, V.W.; Hylind, L.M.; Krush, A.J.; Petersen, G.M.; Trimbath, J.D.; Piantadosi, S.; Garrett, E.; Geiman, D.E.; Hubbard, W.; et al. Primary chemoprevention of familial adenomatous polyposis with sulindac. N. Engl. J. Med. 2002, 346, 1054–1059. [Google Scholar] [CrossRef] [PubMed]
- Kashfi, K.; Chattopadhyay, M.; Kodela, R. NOSH-sulindac (AVT-18A) is a novel nitric oxide- and hydrogen sulfide-releasing hybrid that is gastrointestinal safe and has potent anti-inflammatory, analgesic, antipyretic, anti-platelet, and anti-cancer properties. Redox Biol. 2015, 6, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Fidahic, M.; Jelicic Kadic, A.; Radic, M.; Puljak, L. Celecoxib for rheumatoid arthritis. Cochrane Database Syst. Rev. 2017, 9, 6:CD012095. [Google Scholar] [CrossRef] [PubMed]
- Reddy, B.S.; Rao, C.V. Novel approaches for colon cancer prevention by cyclooxygenase-2 inhibitors. J. Environ. Pathol. Toxicol. Oncol. 2002, 21, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Atari-Hajipirloo, S.; Nikanfar, S.; Heydari, A.; Noori, F.; Kheradmand, F. The effect of celecoxib and its combination with imatinib on human HT-29 colorectal cancer cells: Involvement of COX-2, Caspase-3, VEGF and NF-κB genes expression. Cell Mol. Biol. 2016, 62, 68–74. [Google Scholar] [PubMed]
- Sakoguchi-Okada, N.; Takahashi-Yanaga, F.; Fukada, K.; Shiraishi, F.; Taba, Y.; Miwa, Y.; Morimoto, S.; Iida, M.; Sasaguri, T. Celecoxib inhibits the expression of survivin via the suppression of promoter activity in human colon cancer cells. Biochem. Pharmacol. 2007, 73, 1318–1329. [Google Scholar] [CrossRef] [PubMed]
- Egashira, I.; Takahashi-Yanaga, F.; Nishida, R.; Arioka, M.; Igawa, K.; Tomooka, K.; Nakatsu, Y.; Tsuzuki, T.; Nakabeppu, Y.; Kitazono, T.; et al. Celecoxib and 2,5-dimethylcelecoxib inhibit intestinal cancer growth by suppressing the Wnt/β-catenin signaling pathway. Cancer Sci. 2017, 108, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Reddy, B.S.; Rao, C.V.; Seibert, K. Evaluation of cyclooxygenase-2 inhibitor for potential chemopreventive properties in colon carcinogenesis. Cancer Res. 1996, 56, 4566–4569. [Google Scholar] [PubMed]
- Kawamori, T.; Rao, C.V.; Seibert, K.; Reddy, B.S. Chemopreventive activity of celecoxib, a specific cyclooxygenase-2 inhibitor, against colon carcinogenesis. Cancer Res. 1998, 58, 409–412. [Google Scholar] [PubMed]
- Swamy, M.V.; Patlolla, J.M.; Steele, V.E.; Kopelovich, L.; Reddy, B.S.; Rao, C.V. Chemoprevention of familial adenomatous polyposis by low doses of atorvastatin and celecoxib given individually and in combination to APCM in mice. Cancer Res. 2006, 66, 7370–7377. [Google Scholar] [CrossRef] [PubMed]
- Jacoby, R.F.; Seibert, K.; Cole, C.E.; Kelloff, G.; Lubet, R.A. The cyclooxygenase-2 inhibitor celecoxib is a potent preventive and therapeutic agent in the Min mouse model of adenomatous polyposis. Cancer Res. 2000, 60, 5040–5044. [Google Scholar] [PubMed]
- Bertagnolli, M.M.; Eagle, C.J.; Zauber, A.G.; Redston, M.; Breazna, A.; Kim, K.; Tang, J.; Rosenstein, R.B.; Umar, A.; Bagheri, D.; et al. Adenoma Prevention with Celecoxib Study Investigators. Five-year efficacy and safety analysis of the Adenoma Prevention with Celecoxib Trial. Cancer Prev. Res. 2009, 2, 310–321. [Google Scholar] [CrossRef] [PubMed]
- Bertagnolli, M.M.; Eagle, C.J.; Zauber, A.G.; Redston, M.; Solomon, S.D.; Kim, K.; Tang, J.; Rosenstein, R.B.; Wittes, J.; Corle, D.; et al. APC Study Investigators. Celecoxib for the prevention of sporadic colorectal adenomas. N. Engl. J. Med. 2006, 355, 873–884. [Google Scholar] [CrossRef] [PubMed]
- Arber, N.; Eagle, C.J.; Spicak, J.; Rácz, I.; Dite, P.; Hajer, J.; Zavoral, M.; Lechuga, M.J.; Gerletti, P.; Tang, J.; et al. PreSAP Trial Investigators. Celecoxib for the prevention of colorectal adenomatous polyps. N. Engl. J. Med. 2006, 355, 885–895. [Google Scholar] [CrossRef] [PubMed]
- De Vecchis, R.; Baldi, C.; Di Biase, G.; Ariano, C.; Cioppa, C.; Giasi, A.; Valente, L.; Cantatrione, S. Cardiovascular risk associated with celecoxib or etoricoxib: A meta-analysis of randomized controlled trials which adopted comparison with placebo or naproxen. Minerva Cardioangiol. 2014, 62, 437–448. [Google Scholar] [PubMed]
- Alvaro-Gracia, J.M. Licofelone—Clinical update on a novel LOX/COX inhibitor for the treatment of osteoarthritis. Rheumatology 2004, 43, i21–i25. [Google Scholar] [CrossRef] [PubMed]
- Tavolari, S.; Bonafè, M.; Marini, M.; Ferreri, C.; Bartolini, G.; Brighenti, E.; Manara, S.; Tomasi, V.; Laufer, S.; Guarnieri, T. Licofelone, a dual COX/5-LOX inhibitor, induces apoptosis in HCA-7 colon cancer cells through the mitochondrial pathway independently from its ability to affect the arachidonic acid cascade. Carcinogenesis 2008, 29, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Petrera, M.; Laura, P.; Matteo, P.; Silvia, C.; Matteo, C.; Paola, R.; Michael, G.; Walter, E.H.; Wilfried, R.; Dominique, S.; et al. ASAMET: A. randomized, 2 × 2 biomarker prevention trial of low-dose aspirin and metformin in colorectal cancer. J. Clin. Oncol. 2017, 35, TPS1591. [Google Scholar]
- De Monte, A.; Brunetti, D.; Cattin, L.; Lavanda, F.; Naibo, E.; Malagoli, M.; Stanta, G.; Bonin, S. Metformin and aspirin treatment could lead to an improved survival rate for Type 2 diabetic patients with stage II and III colorectal adenocarcinoma relative to non-diabetic patients. Mol. Clin. Oncol. 2018, 8, 504–512. [Google Scholar] [CrossRef] [PubMed]
- Pence, B.C.; Belasco, E.J.; Lyford, C.P. Combination aspirin and/or calcium chemoprevention with colonoscopy in colorectal cancer prevention: Cost-effectiveness analyses. Cancer Epidemiol. Biomarkers Prev. 2013, 22, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Samadder, N.J.; Kuwada, S.K.; Boucher, K.M.; Byrne, K.; Kanth, P.; Samowitz, W.; Jones, D.; Tavtigian, S.V.; Westover, M.; Berry, T.; et al. Association of Sulindac and Erlotinib vs Placebo With Colorectal Neoplasia in Familial Adenomatous Polyposis: Secondary Analysis of a Randomized Clinical Trial. JAMA Oncol. 2018, 4, 671–677. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.L.; Jackson, C.; Riel, S.; Cooper, H.S.; Devarajan, K.; Hensley, H.H.; Zhou, Y.; Vanderveer, LA.; Nguyen, M.T.; Clapper, M.L. Differential preventive activity of sulindac and atorvastatin in Apc+/Min-FCCCmice with or without colorectal adenomas. Gut 2018, 67, 1290–1298. [Google Scholar] [CrossRef] [PubMed]
- Jagan, M.R.P.; Ronald, L.; Misty, E.; Zhang, Y.; Naveena, B.J.; Venkateshwar, M.; Altaf, M.; Vernon, E.S.; Rao, C.V. Chemoprevention of colon cancer by DFMO, sulindac and NO-sulindac administered individually or in combinations in male F344 rats. In Proceedings of the AACR 102nd Annual Meeting of the American Association for Cancer Research, Orlando, FL, USA, 2–4 April 2011. Abstract Number 808. [Google Scholar]
- Meyskens, F.L.; McLaren, C.E.; Pelot, D.; Fujikawa-Brooks, S.; Carpenter, P.M.; Hawk, E.; Kelloff, G.; Lawson, M.J.; Kidao, J.; McCracken, J.; et al. Difluoromethylornithine plus sulindac for the prevention of sporadic colorectal adenomas: A randomized placebo-controlled, double-blind trial. Cancer Prev. Res. 2008, 1, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Sporn, M.B.; Hong, W.K. Concomitant DFMO and sulindac chemoprevention of colorectal adenomas: A major clinical advance. Nat. Clin. Pract. Oncol. 2008, 5, 628–629. [Google Scholar] [CrossRef] [PubMed]
- Carol, A.B.; Evelien, D.; Jewel, S.; Elena, S.; Alfred, C. Efficacy and safety of eflornithine (CPP-1X)/sulindac combination therapy versus each as monotherapy in patients with familial adenomatous polyposis (FAP): Design and rationale of a randomized, double-blind, Phase III trial. BMC Gastroenterol. 2016, 16, 87. [Google Scholar]
- Trial of Eflornithine Plus Sulindac in Patients With Familial Adenomatous Polyposis (FAP). Clinical Trial Identification Number: NCT01483144. Available online: https://clinicaltrials.gov/ct2/show/NCT01483144 (accessed on 4 June 2018).
- Lynch, P.M.; Burke, C.A.; Phillips, R.; Morris, J.S.; Slack, R.; Wang, X.; Liu, J.; Patterson, S.; Sinicrope, F.A.; Rodriguez-Bigas, M.A.; et al. An international randomised trial of celecoxib versus celecoxib plus difluoromethylornithine in patients with familial adenomatous polyposis. Gut 2016, 65, 286–295. [Google Scholar] [CrossRef] [PubMed]
- Naveena, B.J.; Altaf, M.; Gopal, P.; Venkateshwar, M.; Rebekah, R.; Taylor, B.; Zhang, Y.; Qian, L.; Stan, L.; Hariprasad, G.; et al. Chemoprevention of colorectal cancer by LFA-9, a novel dual mPGES-1/5-LOX inhibitor: Safer approaches to chemoprevention. In Proceedings of the 107th Annual Meeting of the American Association for Cancer Research, New Orleans, LA, USA, 16–20 April 2016. Abstract Number 2604. [Google Scholar]
- Rao, C.V.; Altaf, M.; Naveena, B.J. Safer approaches to colorectal cancer chemoprevention. In Proceedings of the AACR International Conference held in Cooperation with the Latin American Cooperative Oncology Group (LACOG) on Translational Cancer Medicine, São Paulo, Brazil, 4–6 May 2017. Abstract Number B42. [Google Scholar]
- Nieuwenhuis, M.H.; Mathus-Vliegen, E.M.; Baeten, C.G.; Nagengast, F.M.; Van der Bijl, J.; Van Dalsen, A.D.; Kleibeuker, J.H.; Dekker, E.; Langers, A.M.; Vecht, J.; et al. Evaluation of management of desmoid tumours associated with familial adenomatous polyposis in Dutch patients. Br. J. Cancer 2011, 104, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Inoue, Y.; Ishida, H.; Ueno, H.; Kobayashi, H.; Yamaguchi, T.; Konishi, T.; Tomita, N.; Matsubara, N.; Ishida, F.; Hinoi, T.; et al. The treatment of desmoid tumors associated with familial adenomatous polyposis: The results of a Japanese multicenter observational study. Surg. Today 2017, 47, 1259–1267. [Google Scholar] [CrossRef] [PubMed]
- Quast, D.R.; Schneider, R.; Burdzik, E.; Hoppe, S.; Möslein, G. Long-term outcome of sporadic and FAP-associated desmoid tumors treated with high-dose selective estrogen receptor modulators and sulindac: A single-center long-term observational study in 134 patients. Fam. Cancer 2016, 15, 31–40. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Aspirin | Naproxen | Sulindac | Celecoxib |
|---|---|---|---|---|
| Current stage of drug development for CRC | Pre-clinical and clinical | Pre-clinical and clinical | Pre-clinical and clinical | Pre-clinical and clinical |
| Clinically relevant and effective doses | 81 mg to 325 mg/day | 220 to 440 mg/day | 300 mg/day | <800 mg/day |
| Molecular Targets | COX-1&2, wnt, β-catenin, NF-κB, p53, toll-like receptor 4, NOS-2 and caspases | COX, c-Myc, NF-κB and β-catenin | p21, p53, Wnt, NF-κB, STAT3, TNF-α, IL-1β, IL-4, AMPK, PCNA, cyclin D1, β-catenin, inducible NOS, COX-2 and p65 | COX-2, VEGF, NF-κB, caspases-3, Wnt, β-catenin, survivin and cyclin D1 |
| Toxicity | Gastro-duodenal damage, hemorrhage, enteropathy and ulceration as well as cardiovascular side effects | Gastro-duodenal damage, hemorrhage, enteropathy and ulceration. | Gastro-duodenal damage, hemorrhage, enteropathy and ulceration | Cardiovascular side effects |
| Type of Agent | Experimental Type | Observation | References |
|---|---|---|---|
| Aspirin | Pre-clinical | Colon cancer precursor lesions aberrant crypt foci (ACF) formation and progression were significantly lowered in chemical carcinogens (DMH/AOM)-induced CRC in rats. | [31,32,33,34] |
| Clinical trail | Aspirin at 160 and 300 mg/day doses showed that daily low-dose aspirin decreased adenoma recurrence significantly at 1 year but not at year 4. | [42,43] | |
| Clinical data analysis | Aspirin at the doses ranging from 81 mg to 325 mg/day to analyze the adenoma occurrence and advanced lesion occurrence after median follow up of 33 months and observed that aspirin is effective chemopreventive agent in the individuals with these lesions. | [54] | |
| Clinical trials | Low-dose of aspirin use improves overall survival of patients with CRC by modulating various biomarkers. | [53,54,55,56] | |
| Naproxen | Pre-clinical | Administration of 200 and 400 ppm of Naproxen inhibited colon adenocarcinoma multiplicity | [38] |
| Pre-clinical | Dose-dependent prevention of AOM-induced ACF in the colon of mice by naproxen treated twice-daily for 4 weeks. | [67] | |
| Pre-clinical | H2S-releasing naproxen derivative ATB-346 exhibits better intestinal polyp formation as well as GI-sparing effects in ApcMin/+ mice than naproxen. | [66] | |
| A phase Ib clinical trial | In progress to determine the adverse effects and optimal dose of naproxen in preventing DNA mismatch-repair deficient colorectal cancer in patients with Lynch syndrome. | [69] | |
| Sulindac | Pre-clinical | Sulindac (160 and 320 ppm) reduced tumor volume of the colon by > 52–62% as compared to the control. | [72] |
| Clinical trail | ACF numbers were significantly suppressed by sulindac at 300 mg daily in a randomized trial. | [73] | |
| Celecoxib | Pre-clinical | Initiation and post-initiation stages significantly inhibited the incidence as well as the multiplicity of colon adenocarcinomas in rats. | [74] |
| Clinical trail | Celecoxib-treatment caused substantial reduction in adenomas in which COX-2 expression is more. | [75] | |
| Clinical study | 800 mg daily dose showed substantial adenoma prevention, but this dose caused cardiovascular toxicity. | [76] | |
| Licofelone | Pre-clinical | Licofelone significantly dose-dependently inhibited size as wells as multiplicity of the intestinal tumors in both male and female ApcMin/+ mice. | [77] |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohammed, A.; Yarla, N.S.; Madka, V.; Rao, C.V. Clinically Relevant Anti-Inflammatory Agents for Chemoprevention of Colorectal Cancer: New Perspectives. Int. J. Mol. Sci. 2018, 19, 2332. https://doi.org/10.3390/ijms19082332
Mohammed A, Yarla NS, Madka V, Rao CV. Clinically Relevant Anti-Inflammatory Agents for Chemoprevention of Colorectal Cancer: New Perspectives. International Journal of Molecular Sciences. 2018; 19(8):2332. https://doi.org/10.3390/ijms19082332
Chicago/Turabian StyleMohammed, Altaf, Nagendra Sastry Yarla, Venkateshwar Madka, and Chinthalapally V. Rao. 2018. "Clinically Relevant Anti-Inflammatory Agents for Chemoprevention of Colorectal Cancer: New Perspectives" International Journal of Molecular Sciences 19, no. 8: 2332. https://doi.org/10.3390/ijms19082332
APA StyleMohammed, A., Yarla, N. S., Madka, V., & Rao, C. V. (2018). Clinically Relevant Anti-Inflammatory Agents for Chemoprevention of Colorectal Cancer: New Perspectives. International Journal of Molecular Sciences, 19(8), 2332. https://doi.org/10.3390/ijms19082332





