Gastroprotective and Antioxidant Activity of Kalanchoe brasiliensis and Kalanchoe pinnata Leaf Juices against Indomethacin and Ethanol-Induced Gastric Lesions in Rats
Abstract
:1. Introduction
2. Results
2.1. TLC Profile of Kalanchoe brasiliensis and Kalanchoe pinnata Leaf Juices
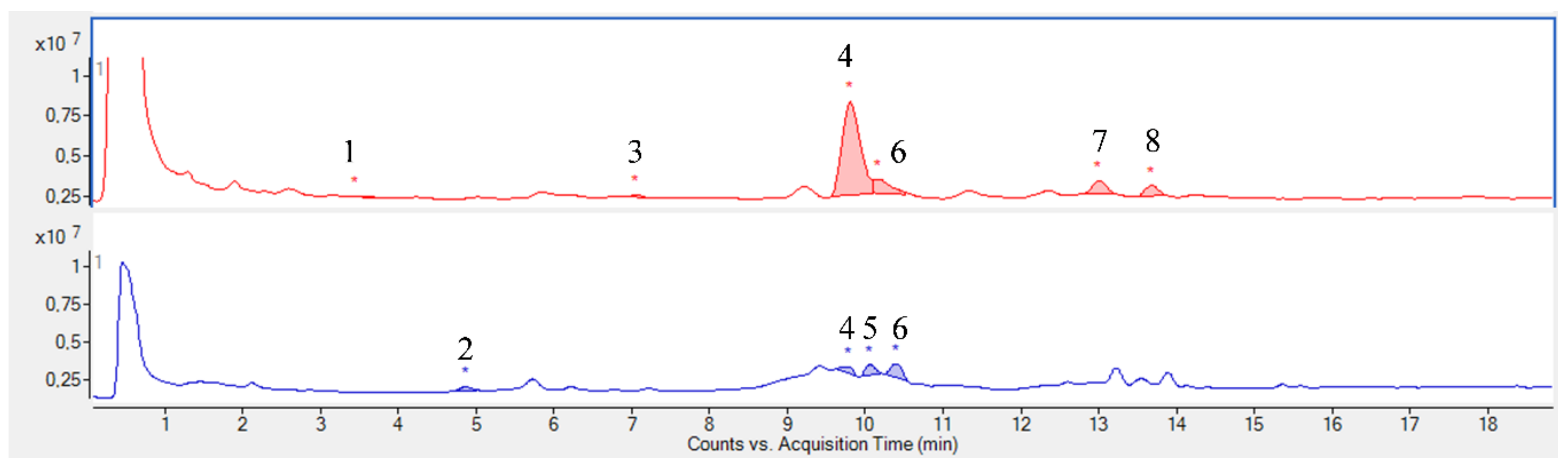
2.2. UHPLC-MS Profile of Kalanchoe brasiliensis and Kalanchoe pinnata Leaf Juices
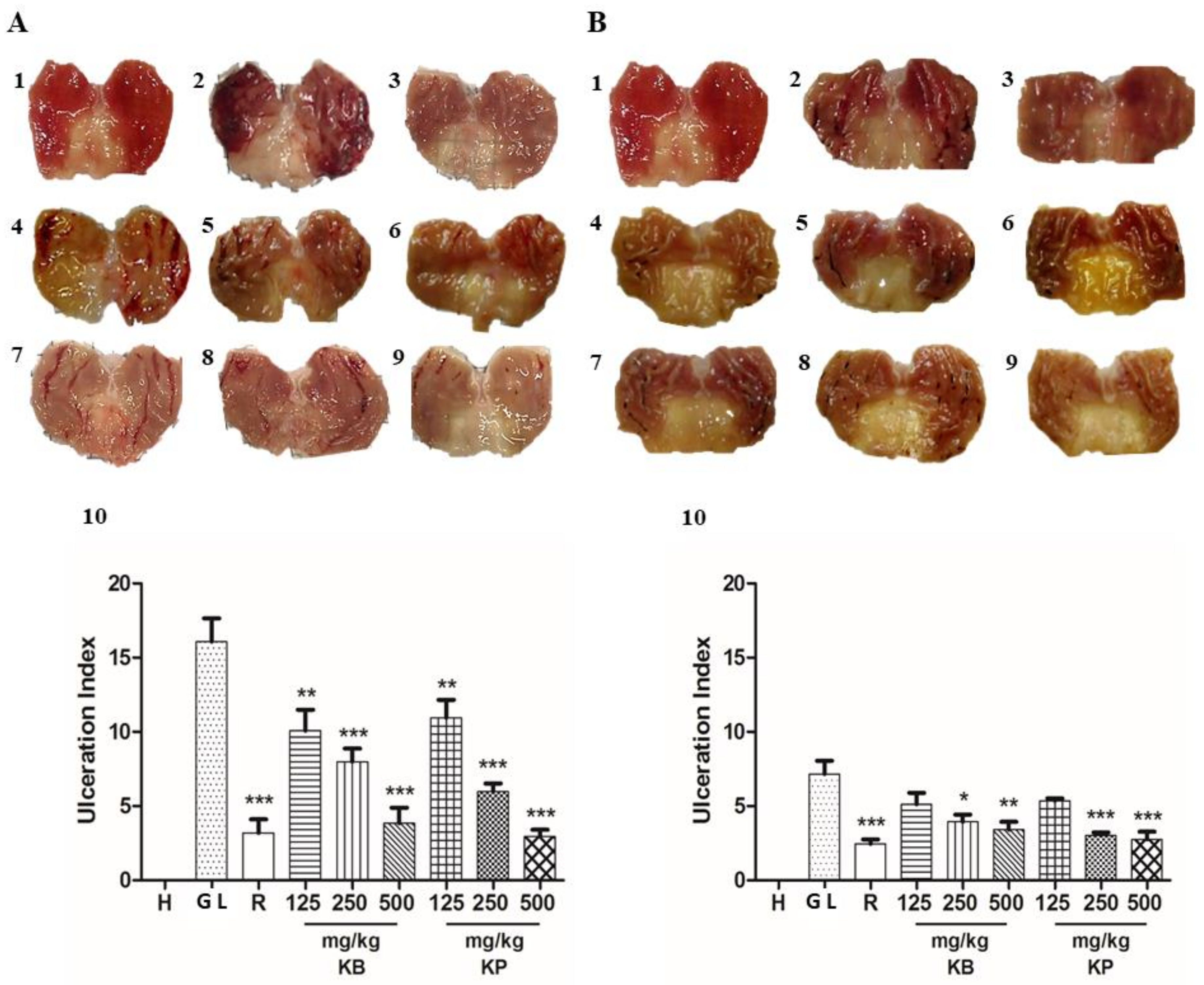
2.3. Macroscopic Evaluation of Gastric Lesions
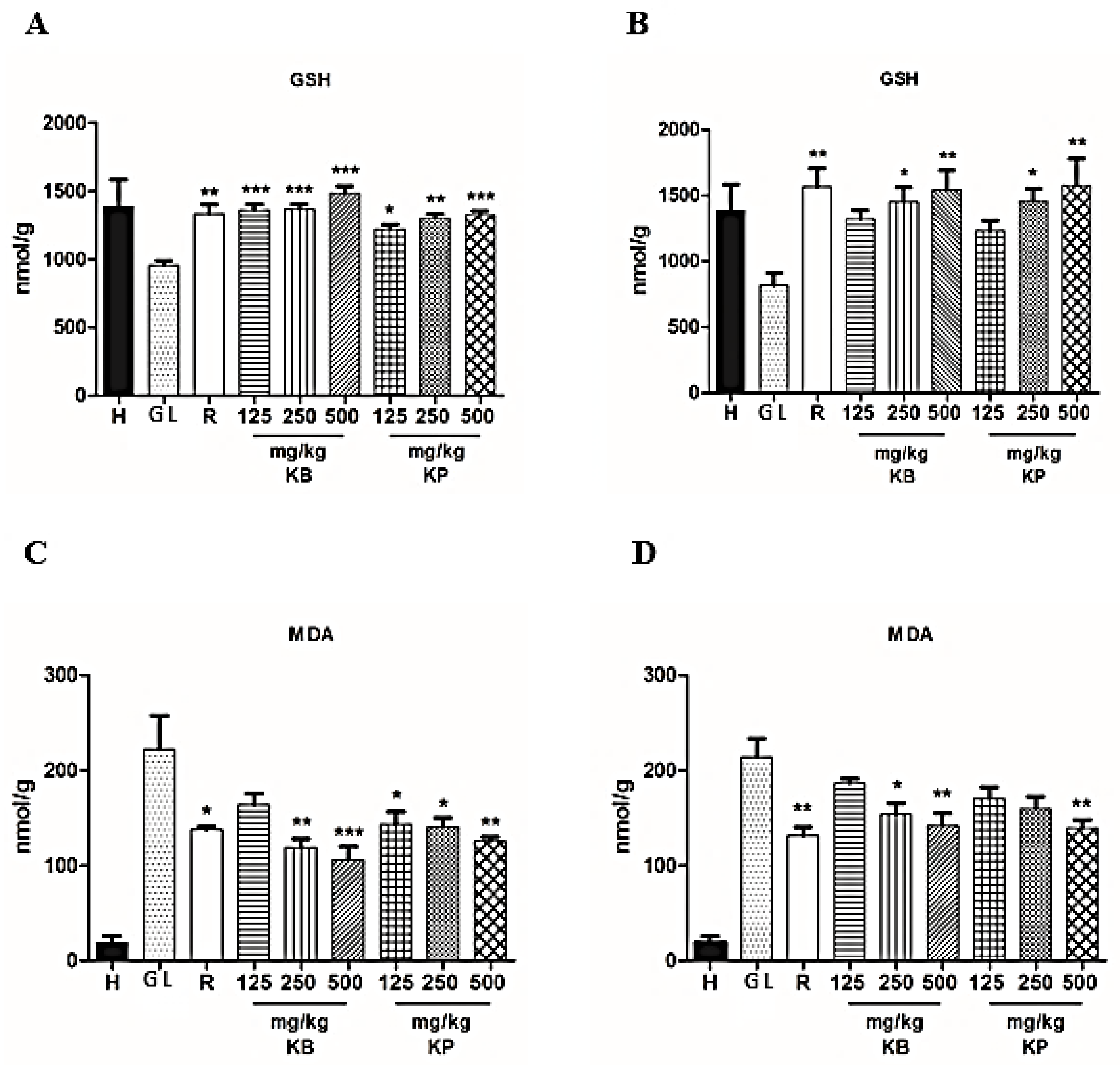
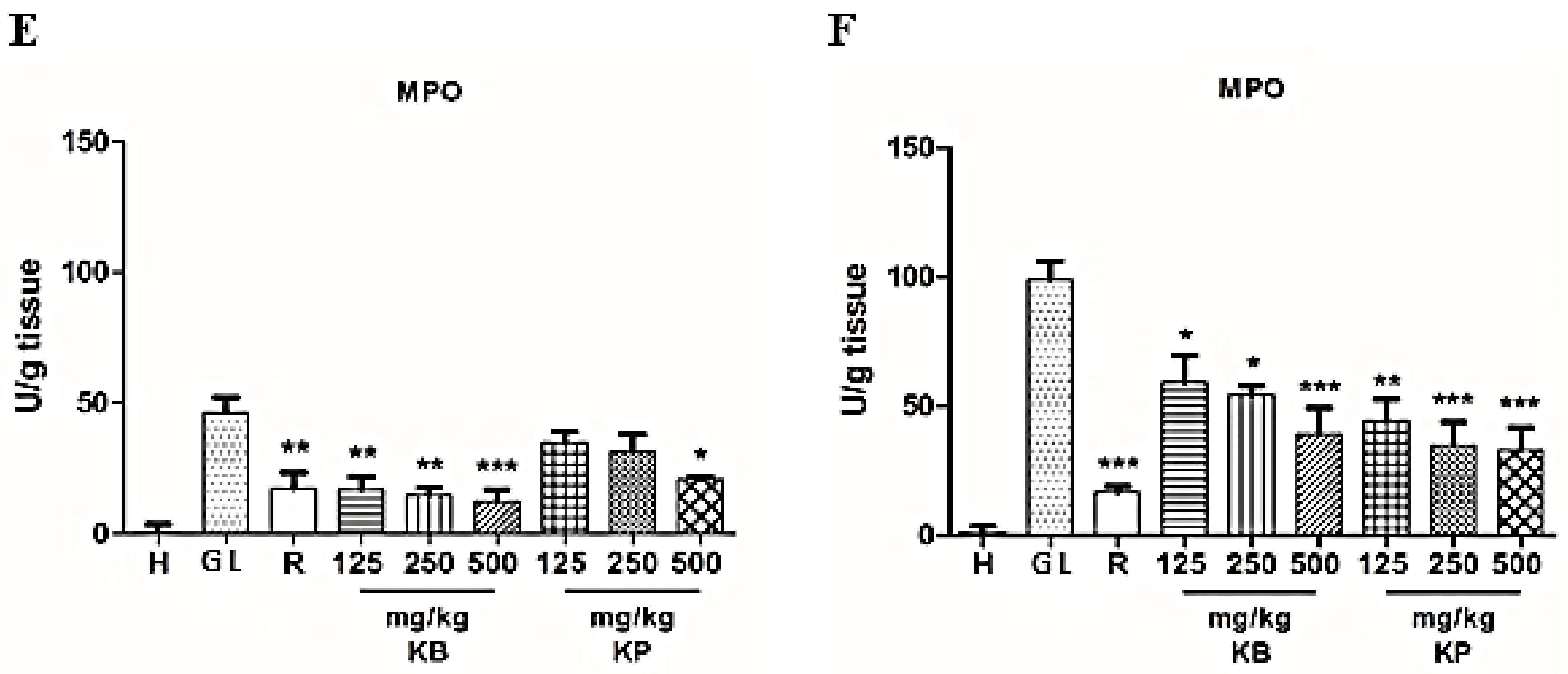
2.4. Effect of Kalanchoe brasiliensis and Kalanchoe pinnata Leaf Juices on Glutathione (GSH) and Malondialdehyde (MDA) Levels and Myeloperoxidase (MPO) Activity
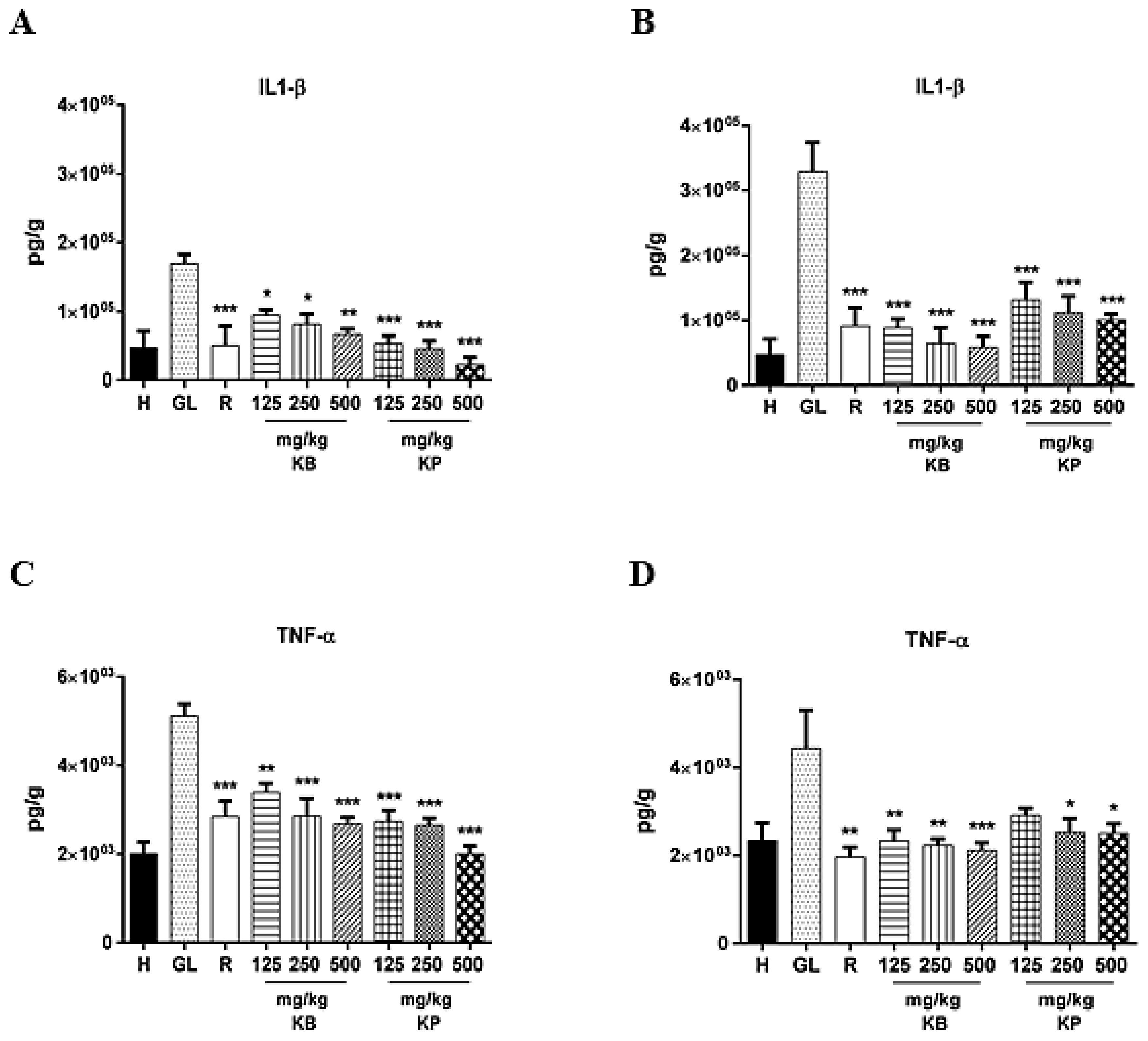
2.5. Effect of Kalanchoe brasiliensis and Kalanchoe pinnata Leaf Juice Pre-Treatment on Interleukin-1β (IL-1β) and Tumor Necrosis Factor-α (TNF-α) Levels
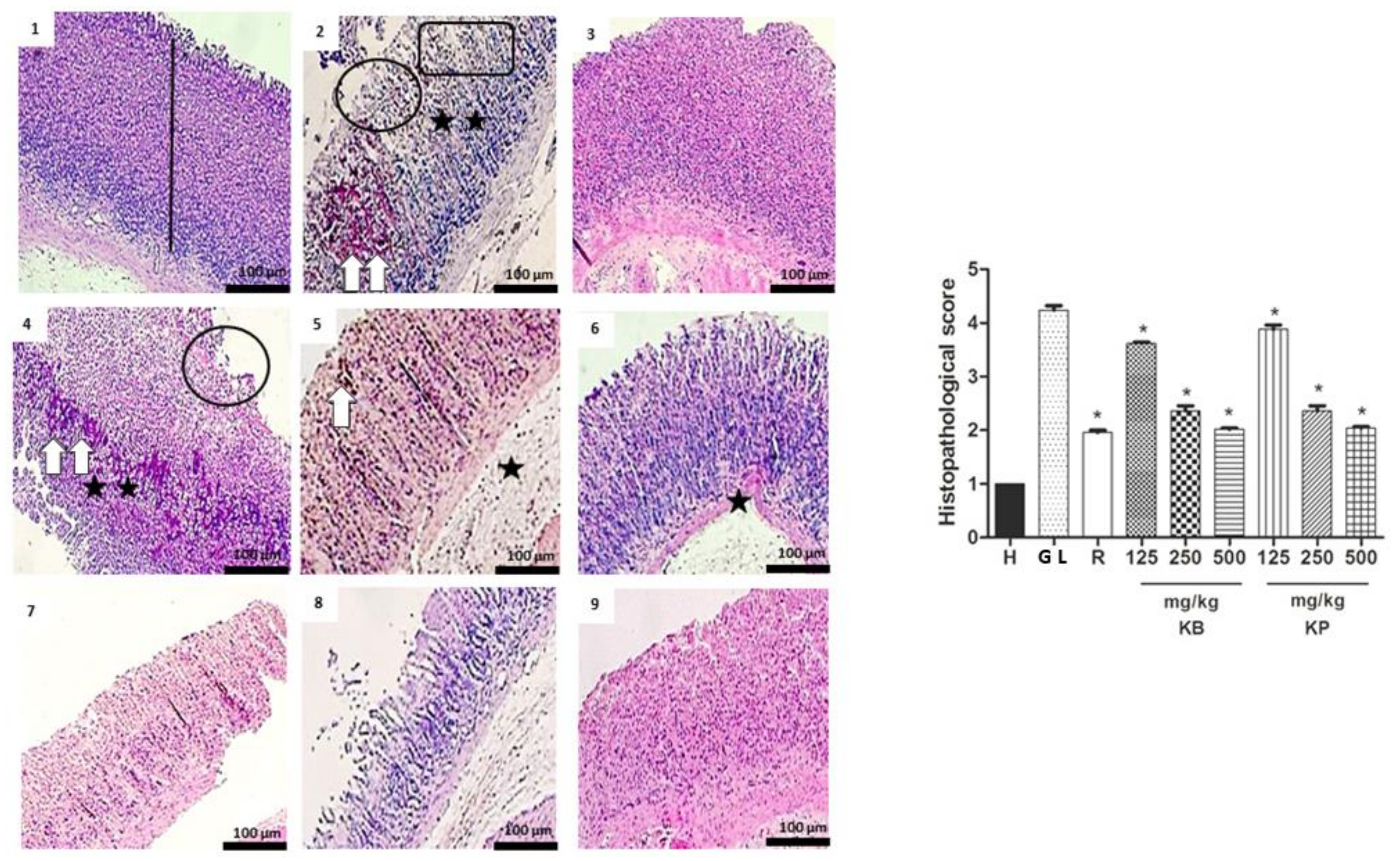
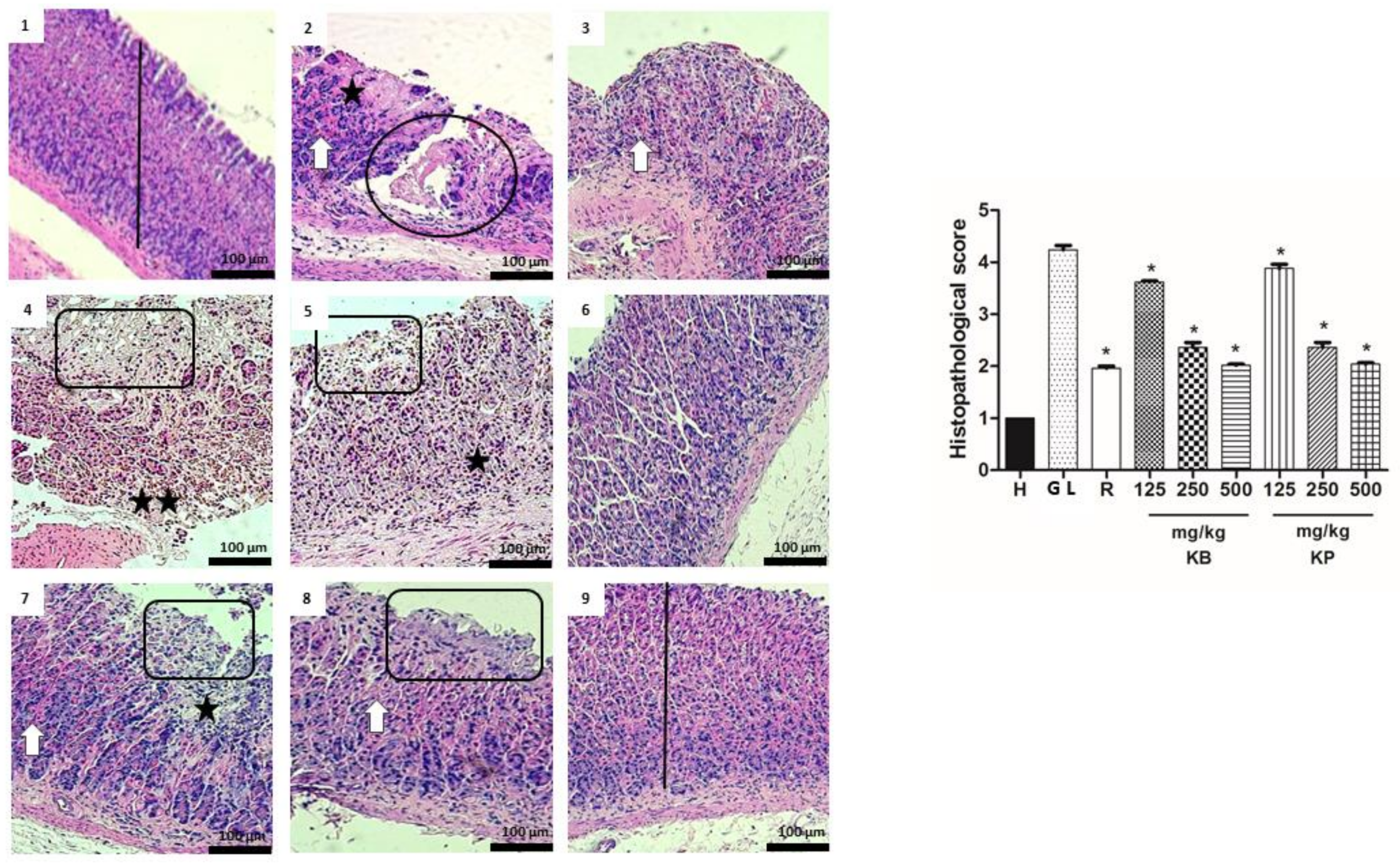
2.6. Histology
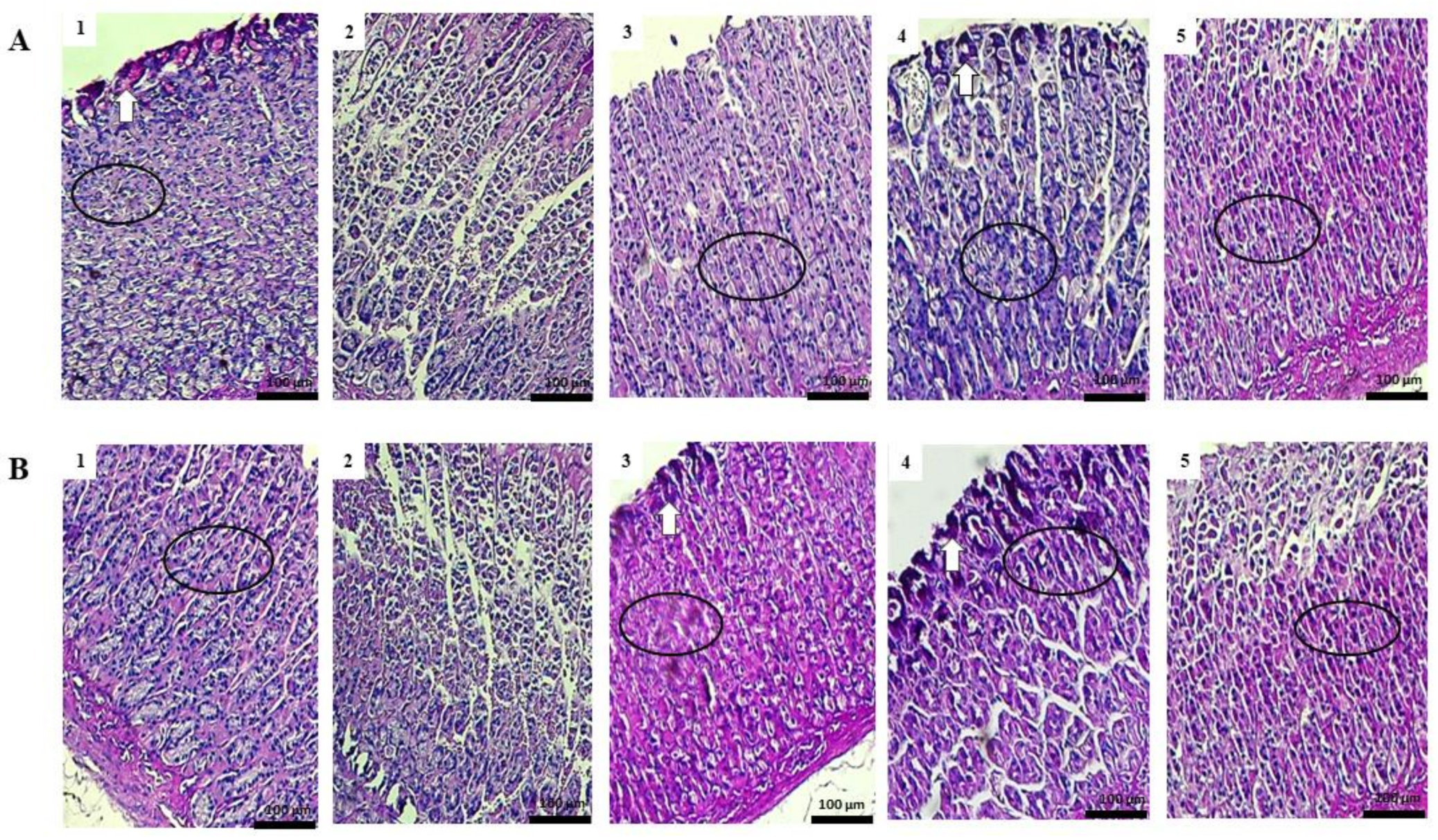
2.7. Study of Mucosal Glycoproteins
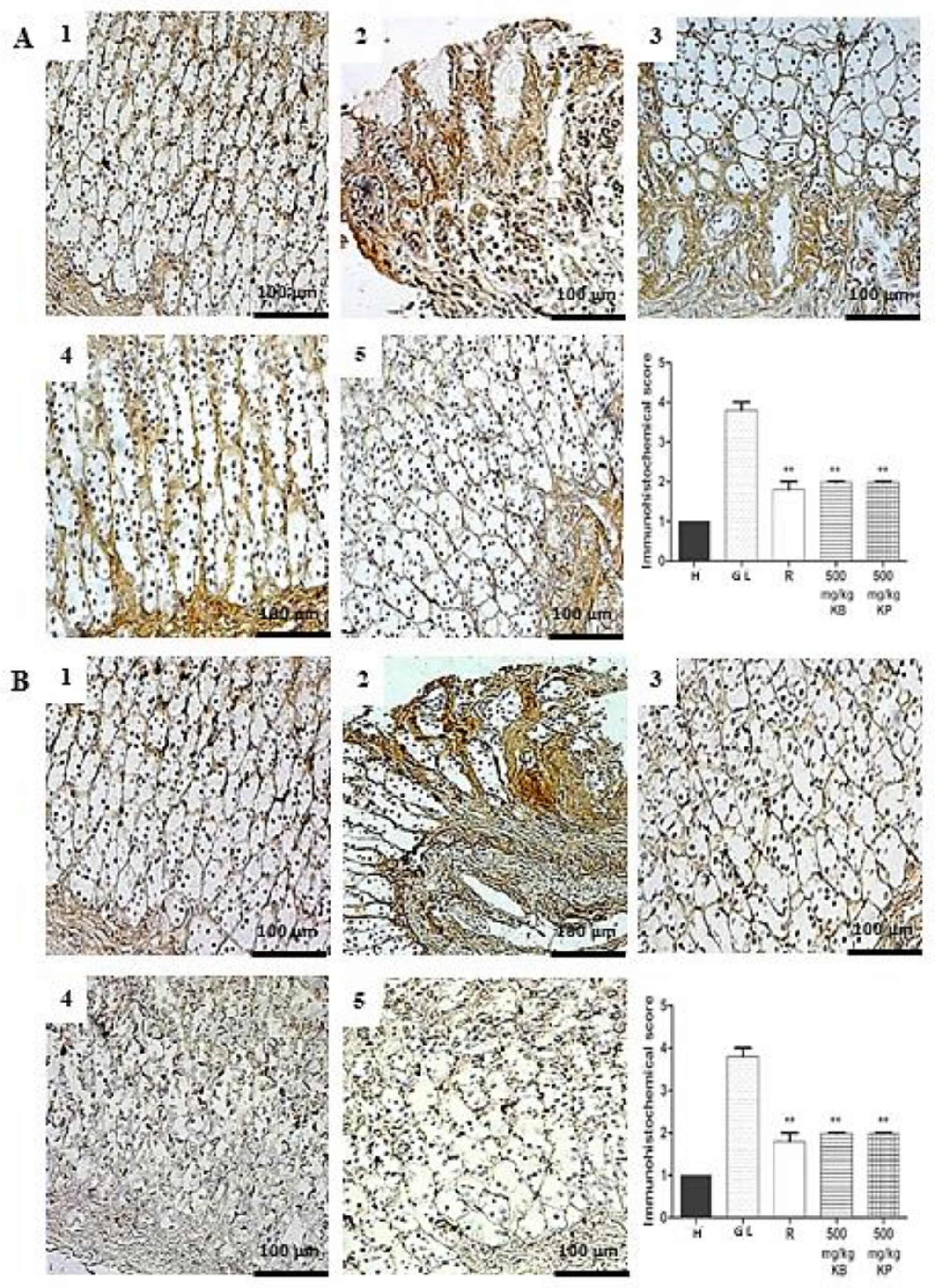
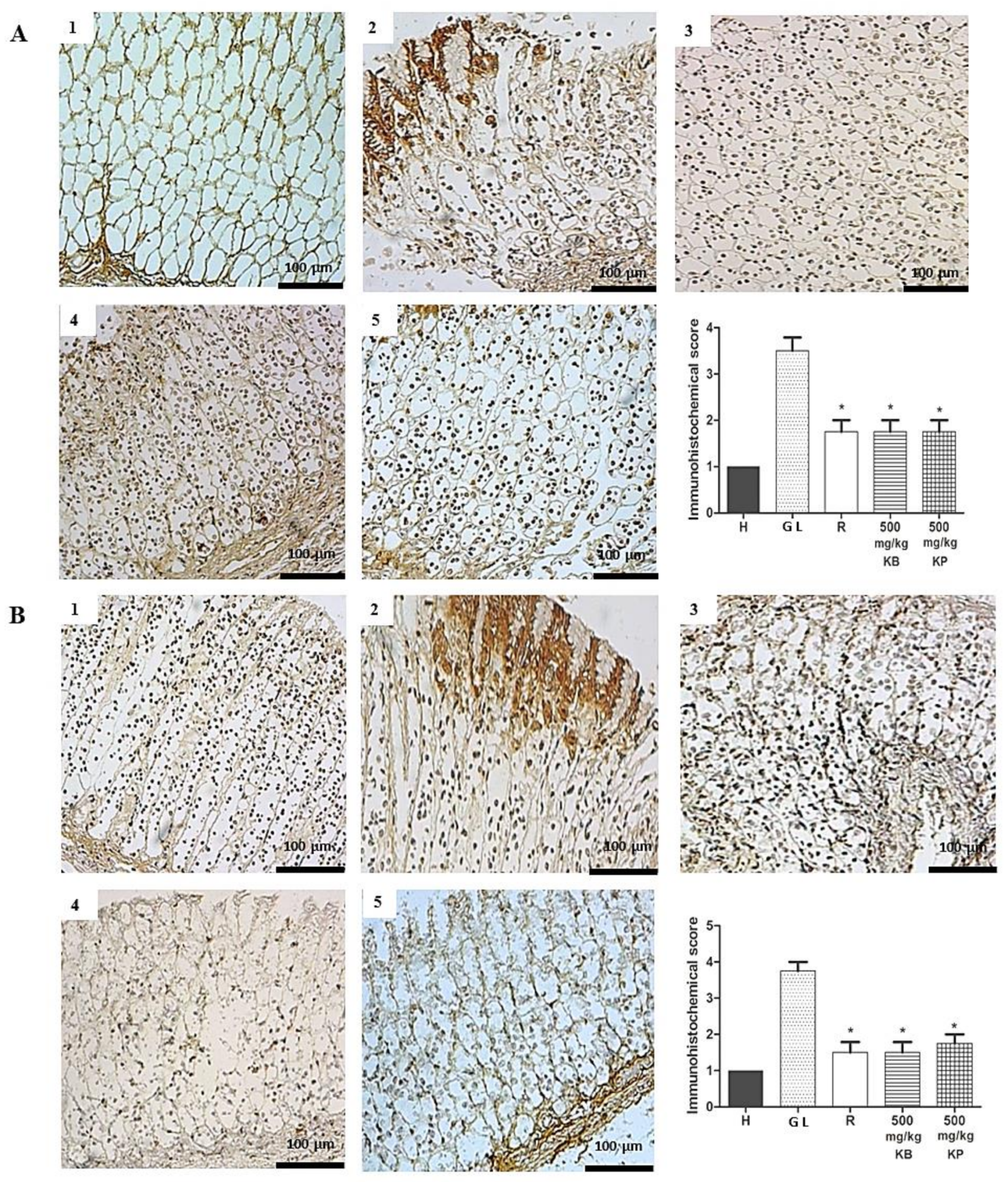
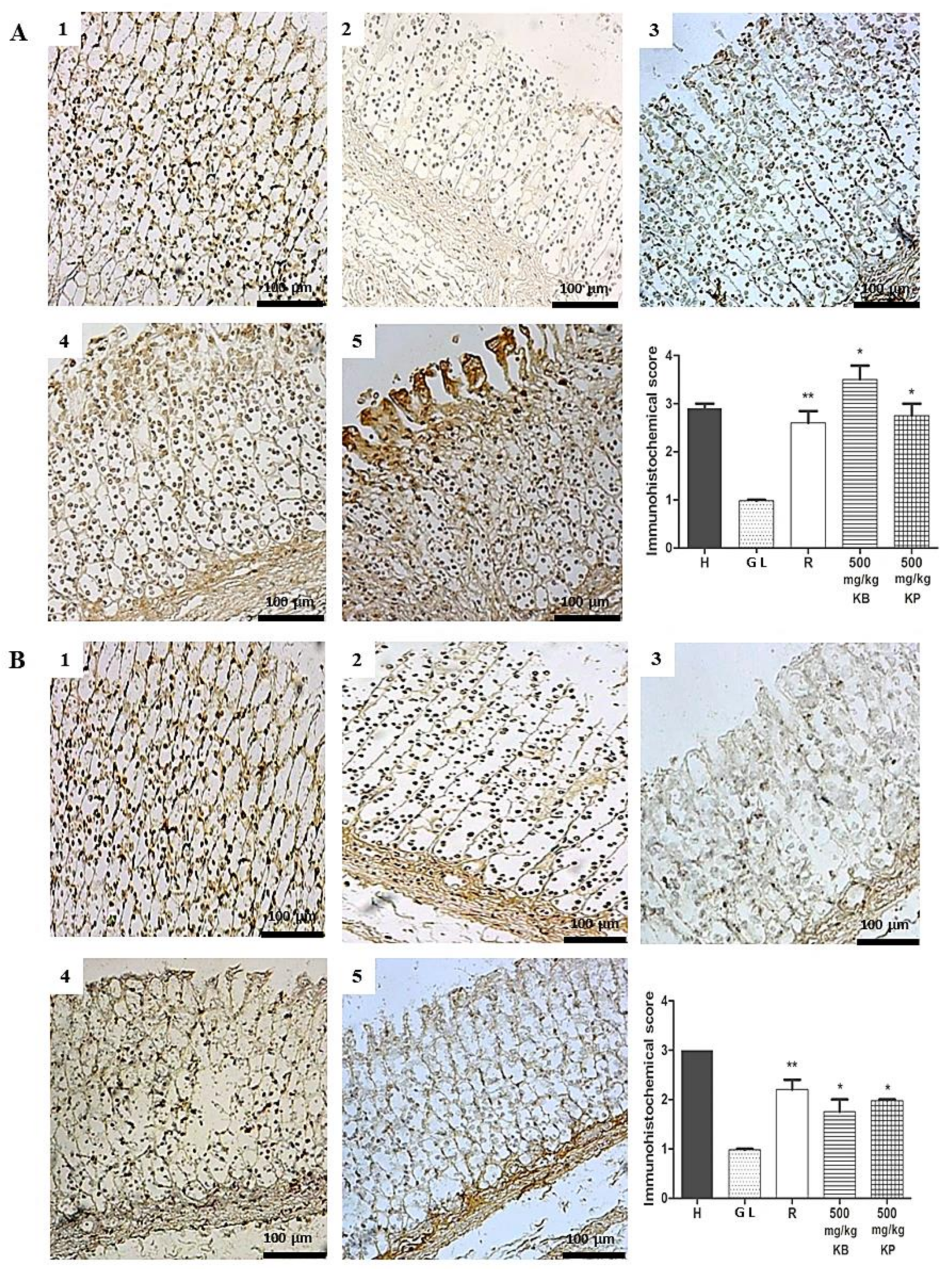
2.8. Immunohistochemistry
2.9. Evaluation of Gastric Secretion
3. Discussion
4. Materials and Methods
4.1. Plant Material
4.2. Preparation of the Kalanchoe brasiliensis and Kalanchoe pinnata Leaf Juices
4.3. Thin Layer Chromatography (TLC) Profile of the Kalanchoe brasiliensis and Kalanchoe pinnata Leaf Juices
4.4. Ultra High Performance Liquid Chromatography (UHPLC-MS) Profile of the Kalanchoe brasiliensis and Kalanchoe pinnata Leaf Juices
4.5. Animal Stock
4.6. Gastric Lesion Induction by Ethanol
4.7. Gastric Lesion Induction by Indomethacin
4.8. Macroscopic Stomach Lesion Assessment
4.9. Glutathione (GSH) Total
4.10. Malonyldialdehyde (MDA) Assay
4.11. Myeloperoxidase (MPO) Activity
4.12. Interleukin-1β (IL-1β) and Tumor Necrosis Factor-α (TNF-α) Assay
4.13. Histopathology Analysis
4.14. Study of Mucosal Glycoproteins
4.15. Immunohistochemical Staining of Inducible Nitric Oxide Synthase (iNOS), Factor Nuclear-κβ (NF-κB-p65) and Zone Occludes-1 (ZO-1)
4.16. Evaluation of Gastric Secretion
4.17. Statistical Analysis
Author Contributions
Acknowledgments
Conflicts of Interest
Abbreviations
| CIOMS | International Organizations of Medical Sciences |
| CONSEA | National Council for the Control of Animal Experimentation of Brazil |
| COX-1 | Cyclooxygenase-1 |
| COX-2 | Cyclooxygenase-2 |
| DTNB | 5,5′-Dithiobis(2-nitrobenzoic acid) |
| GL | Gastric Lesion Control |
| GLI | Gastric Lesion Index |
| GSH | Glutatione |
| H | Healthy |
| H&E | Hematoxylin and Eosin |
| I% | Percentage inhibition |
| IL-1β | Interleukin 1 beta |
| iNOS | Inducible nitric oxide synthase |
| KB | Kalanchoe brasiliensis |
| KP | Kalanchoe pinnata |
| MDA | Malondialdehyde |
| MPO | Myeloperoxidase |
| NF-κB | Factor nuclear-κβ transcription |
| NO | Nitric oxide |
| NSAIDs | Nonsteroidal anti-inflammatory drugs |
| PAS | Periodic acid-Schiff |
| PB | Phosphate buffer |
| PGE2 | Prostaglandin E2 |
| R | Ranitidine |
| RENISUS | Relation of Species of Interest of Health Unic System |
| Rf | Retention factors |
| ROS | Reactive oxygen species |
| SISBIO | Biodiversity Information System |
| TLC | Thin Layer Chromatography |
| TNF-α | Tumor necrosis factor alpha |
| UFC | Federal University of Ceará |
| UFRN | Federal University of Rio Grande do Norte |
| UHPLC-MS | Ultra High Performance Liquid Chromatography coupled to Mass Spectrometer |
| UV | Ultra violet |
| WHO | World Health Organization |
| ZO-1 | Zone Occludes-1 |
References
- Saxena, B.S.; Singh, S. Investigations on gastroprotective effect of citalopram, an antidepressant drug against stress and pyloric ligation induced ulcers. Pharmacology 2011, 63, 1413–1426. [Google Scholar] [CrossRef]
- Kangwan, N.; Park, J.M.; Kim, E.H.; Hahm, K.B. Quality of healing of gastric ulcers: Natural products beyond acid suppression. World J. Gastrointest. Pathophysiol. 2014, 5, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Harbison, S.P.E.; Dempsey, D.T. Peptic ulcer disease. Curr. Prob. Surg. 2005, 42, 346–454. [Google Scholar] [CrossRef] [PubMed]
- Rocha, N.F.M.; Oliveira, G.V.; Araújo, F.Y.; Rios, E.R.; Carvalho, A.M.; Vasconcelos, L.F.; Macêdo, D.S.; Soares, P.M.; Sousa, D.P.; Sousa, F.C. (−)-α-Bisabolol-induced gastroprotection is associated with reduction in lipid peroxidation, superoxide dismutase activity and neutrophil migration. Eur. J. Pharm. Sci. 2011, 44, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Sid, B.; Verrax, J.; Calderon, B.P. Role of oxidative stress in the pathogenesis of 426 alcohol-induced liver disease. Free Radic. Res. 2013, 47, 894–904. [Google Scholar] [CrossRef] [PubMed]
- Suleyman, H.; Albayrak, A.; Bilici, M.; Cardici, E.; Halici, Z. Different mechanisms in formation and prevention of indomethacin-inducd gastric ulcers. Inflammation 2010, 3, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Tarnawski, A.; Ahluwalia, A.K.; Jones, M. Gastric cytoprotection beyond ulcer healing actions of antacids. Curr. Pharm. Des. 2013, 19, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Brazil. 2006; Fitoterapia no SUS e o Programa de Pesquisas de Plantas Medicinais da Central de Medicamentos. Ministério da Saúde. Available online: http://bvsms.saude.gov.br/bvs/publicacoes/fitoterapia_no_sus.pdf (accessed on 20 March 2016).
- Brazil. 2014; Resolução de Diretoria Colegiada n° 26 de 13 de Maio de 2014. Registro de Medicamentos Fitoterápicos no Brasil. Agência Nacional de Vigilância Sanitária. Ministério da Saúde. Available online: http://bvsms.saude.gov.br/bvs/saudelegis/anvisa/2014/rdc0026_13_05_2014.pdf (accessed on 20 March 2016).
- Lorenzi, H.; Mtos, F.J.A. Plantas Medicinais no Brasil: Nativas e Exóticas, 2nd ed.; Instituto Plantarum: Nova Odessa, Brazil, 2008; pp. 223–224. [Google Scholar]
- Wagner, H.; Bladt, S. Plant Drug Analysis: A Thin Layer Chromatography Atlas, 2nd ed.; Springer: Berlin, Germany, 2001. [Google Scholar]
- Fernandes, J.M.; Félix-Silva, J.; Cunha, L.M.; Gomes, J.A.S.; Siqueira, E.M.S.; Gimenes, L.P.; Lopes, N.P.; Soares, L.A.L.; Fernandes-Pedrosa, M.F.; Zucolotto, S.M. Inhibitory Effects of Hydroethanolic Leaf Extracts of Kalanchoe brasiliensis and Kalanchoe pinnata (Crassulaceae) against Local Effects Induced by Bothrops jararaca Snake Venom. PLoS ONE 2016, 12. [Google Scholar] [CrossRef] [PubMed]
- Costa, S.S.; Jossang, A.; Bodo, B. Patuletinacetylr hamnosides from Kalanchoe brasiliensis as inhibitors of human lymphocyte proliferative activity. J. Nat. Prod. 1994, 57, 1503–1510. [Google Scholar] [CrossRef] [PubMed]
- Muzitano, M.F.; Cruz, A.P.; Almeida, S.A.G.; Da-Silva, C.R.; Kaiser, C.; Guette, B.; Rossi-Bergmann; Costa, S.S. Quercitrin: Anantileishmanial flavonoid glycoside from Kalanchoe pinnata. Planta Med. 2006, 81–83. [Google Scholar] [CrossRef]
- Kwiecień, S.; Brzozowski, T.; Konturek, S.J. Effects of reactive oxygen species action on gastric mucosa in various models of mucosal injury. J. Physiol. Pharmacol. 2002, 53, 39–50. [Google Scholar] [PubMed]
- Repetto, M.G.; Llesuy, S.F. Antioxidant properties of natural compounds used in popular medicine for gastric ulcers. Braz. J. Med. Biol. Res. 2002, 35, 523–534. [Google Scholar] [CrossRef] [PubMed]
- Othman, A.I.; El-Missiry, M.A.; Amer, M.A. The protective action of melatonin on indomethacin-induced gastric and testicular oxidative stress in rats. Redox Rep. 2001, 6, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Rozza, A.; Moraes, T.M.; Kushima, H.; Tanimoto, A.; Marques, M.O.; Baub, T.M.; Hiruma-Lima, C.A.; Pellizzon, C.H. Gastroprotective mechanisms of Citrus lemon (Rutaceae) essential oil and its majority compounds limonene and β-pinene: Involvement of heat-shock protein-70, vasoactive intestinal peptide, glutathione, sulfhydryl compounds, nitric oxide and prostaglandin E2. Chem. Biol. Interact. 2011, 189, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Koo, M. Effect of Centella asiatica on ethanol induced gastric mucosal lesions in rats. Life Sci. 2000, 67, 2647–2653. [Google Scholar] [CrossRef]
- Hansson, M.; Olsson, I.; Nauseef, W.M. Biosynthesis, processing, and sorting of human myeloperoxidase. Arch. Biochem. Biophys. 2006, 445, 214–224. [Google Scholar] [CrossRef] [PubMed]
- Salga, M.; Ali, H.; Abdulla, M.; Abdelwahab, S. Gastroprotective activity and mechanism of novel dichloride-zinc (II)-4–2(2-(5-methoxybenzylidenamino)ethyl) piperazin-1-iumphenolate complex on ethanol-induced gastric ulceration. Chem.-Biol. Interact. 2012, 195, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.C.; Chen, Y.M.; Wang, D.C.; Chiu, C.C.; Lin, W.T.; Wang, C.Y.; Hsu, M.C. Cytoprotective effect of American ginseng in a rat ethanol gastric ulcer model. Molecules 2014, 19, 316–326. [Google Scholar] [CrossRef] [PubMed]
- El-Maraghy, S.A.; Rizk, S.M.; Shahin, N.N. Gastroprotective effect of crocin in ethanolinduced gastric injury in rats. Chem. Biol. Interact. 2015, 229, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Mei, X.; Xu, D.; Xu, S.; Zheng, Y.; Xu, S. Novel role of Zn(II)–curcumin in enhancing cell proliferation and adjusting proinflammatory cytokine-mediated oxidative damage of ethanol-induced acute gastric ulcers. Chem. Biol. Interact. 2012, 197, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Piotrowski, J.; Piotrowski, E.; Skrodzka, D.; Slomiany, A.; Slomiany, B.L. Gastric mucosal apoptosis induced by ethanol: Effect of antiulcer agents. Biochem. Mol. Biol. Int. 1997, 42, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Handa, O.; Naito, Y.; Takagi, T.; Shimozawa, M.; Kokura, S.; Yoshida, N.; Matsui, H.; Cepinskas, G.; Kvietys, P.R.; Yoshikawa, T. Tumor necrosis factor-alpha-induced cytokine-induced neutrophil chemoattractant-1 (CINC-1) production by rat gastric epithelial cells: Role of reactive oxygen species and nuclear factor-kappaB. J. Pharmacol. Exp. Ther. 2004, 309, 670–676. [Google Scholar] [CrossRef] [PubMed]
- Taha, M.M.; Salga, M.S.; Ali, H.M.; Abdulla, M.A.; Abdelwahab, S.I.; Hadi, A.H.A. Gastroprotective activities of Tunera diffusa wild. ex Schult. Reviited: Role of arbutin. J. Ethnopharmacol. 2012, 141, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Sangiovanni, E.; Vrhovsek, U.; Rossoni, G.; Colombo, E.; Brunelli, C.; Brembati, L.; Trivulsio, S.; Gasperotti, M.; Mattivi, F.; Bosisio, E.; et al. Ellagitannins from Rubus berries for the control of gastric inflammation: In vitro and in vivo studies. PLoS ONE 2013, 8. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Huang, H.; Niu, X.; Fan, T.; Mu, Q.; Li, H. Protective effect of tetrahydrocoptisine against ethanol-induced gastric ulcer in mice. Toxicol. Appl. Pharmacol. 2013, 272, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Alqasoumi, S.; Al-Howiriny, T.A.; Al-Yahya, M.; Rafatulla, S. Gastroprotective effects of radish “raphanus sativus” L. on experimental gastric ulcer models in rats. Farmacia 2008, 46, 204–214. [Google Scholar] [CrossRef]
- Hajrezaie, M.; Golbabapour, S.; Hassandarvish, P.; Nura Suleiman Gwaram, N.S.; Hadi, A.H.; Ali, H.M.; Majid, N.; Abdulla, M.A. Acute toxicity and gastroprotection studies of a new Schiff base derived copper (II) complex against ethanol-induced acute gastric lesions in rats. PLoS ONE 2012, 7, e51537. [Google Scholar] [CrossRef] [PubMed]
- Golbabapour, S.; Hajrezaie, M.; Hassandarvish, P.; Abdul Majid, N.; Hadi, A.; Nordin, N.; Abdula, M.A. Acute toxicity and gastroprotective role of M. pruriens in ethanol-induced gastric mucosal injuries in rats. Int. J. Biomed. Res. 2013, 2013. [Google Scholar] [CrossRef]
- Huang, S.; Chang, S.; Mu, S.; Jiang, H.; Wang, T.; Kao, J.; Huang, J.L.; Wu, C.Y.; Chen, Y.J.; Shie, J.J. Imiquimod activates p53-dependent apoptosis in a human basal cell carcinoma cell line. J. Dermatol. Sci. 2016, 81, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, J.; Yuda, Y.; Ynouye, S.; Yamakawa, T. The role of nitric oxide in the gastric acid secretion induced by ischemia-reperfusion in the pylorus-ligated rat. Eur. J. Pharmacol. 2001, 13, 69–74. [Google Scholar] [CrossRef]
- Takeuchi, K.; Araki, H.; Kawachi, S.; Kunikata, T.; Mizoguchi, H.; Tashima, K. Regulatory mechanism of acid secretion in the damaged stomach: Role of endogenous nitric oxide. J. Gastroenterol. Hepatol. 2000, 15, 37–45. [Google Scholar] [CrossRef]
- Cho, C.H. Current roles of nitric oxide in gastrointestinal disorders. J. Physiol. Paris 2001, 95, 253–256. [Google Scholar] [CrossRef]
- Laine, L.; Weinstein, W.M. Histology of alcoholic haemorrhagic gastritis; A prospective evaluation. Gastroenterology 1988, 94, 1254–1264. [Google Scholar] [CrossRef]
- Davis, M.M. A new trigger for T cells. Cell 2002, 110, 285–287. [Google Scholar] [CrossRef]
- Jabeen, A.; Mesaik, M.A.; Simjee, S.U.; Lubna; Bano, S.; Faizi, S. Anti-TNF-α and anti-arthritic effect of patuletin: A rare flavonoid from Tagetes patula. Int. Immunopharmacol. 2016, 36, 232–240. [Google Scholar] [CrossRef]
- Pal, S.; Chaudhuri, A.K.N. Studies on the anti-ulcer activity of a Bryophyllum pinnatum leaf extract in experimental animals. J. Ethnopharmacol. 1991, 33, 97–102. [Google Scholar] [CrossRef]
- Adesanwo, J.K.; Raji, Y.; Olaleye, S.B.; Onasanwo, S.A.; Fadare, O.O.; Ige, O.O.; Odusanya, O.O. Antiulcer Activity of Methanolic Extract of Bryophyllum pinnatum in Rats. J. Biol. Sci. 2007, 7, 409–412. [Google Scholar] [CrossRef]
- Braz, D.C.; Oliveira, L.R.S.; Viana, A.F.S.C. Atividade antiulcerogênica do extrato aquoso da Bryophyllum pinnatum (Lam.) Kurz. Revista Brasileira de Plantas Medicinais 2013, 15, 86–90. [Google Scholar] [CrossRef]
- Sobreira, F.; Hernandes, L.S.; Vetore-Neto, A.; Díaz, I.E.C.; Santana, F.C.; Mancini-Filho, J.; Bacchi, E.M. Gastroprotective activity of the hydroethanolic extract and ethyl acetate fraction from Kalanchoe pinnata (Lam.) Pers. Braz. J. Pharm. Sci. 2017, 53, e16027. [Google Scholar] [CrossRef]
- Sharma, A.L.; Bhot, M.A.; Chandra, N. Gastroprotective effect of aqueous extract and mucilage from Bryophyllum pinnatum (Lam.) Kurz. Ancient Sci. Life 2014, 33, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Costa, J.L.C. Avaliação Farmacológicadas Atividades Anti-Inflamatória e Antiulcerogênica do Extrato Seco Obtido por Aspersão de Kalanchoe brasiliensis Cambess e sua Toxicidade Reprodutiva em Ratas Wistar. Master’s Thesis, Universidade Federal de Pernambuco, Pernambuco, Brasil, 2010. [Google Scholar]
- Souza, R.F.; Giovani, W.F. Antioxidant properties of complexes of flavonoids with metal ions. Redox Rep. 2004, 9, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.T.; Ding, C.; Zhou, N.; Xu, C. Quercetin protects gastric epithelial cell from oxidative damage in vitro and in vivo. Eur. J. Pharmacol. 2015, 754, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Tsai, M.H.; Lin, Z.C.; Liang, C.J.; Yen, F.L.; Chiang, Y.C.; Lee, C.W. Eupafolin inhibits PGE2 production and COX2 expression in LPS-stimulated human dermal fibroblasts by blocking JNK/AP-1 and Nox2/p47(phox) pathway. Toxicol. Appl. Pharmacol. 2014, 279, 240–251. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.C.; Liang, C.J.; Lee, C.W.; Yen, F.L.; Hsiao, C.Y.; Wang, S.H.; Jiang-Shieh, Y.F.; Tsai, J.S.; Chen, Y.L. The protective effect of eupafolin against TNF-α-induced lung inflammation via the reduction of intercellular cell adhesion molecule-1 expression. J. Ethnopharmacol. 2015, 170, 136–147. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.J.; Yen, F.L.; Chen, P.C.; Wang, M.C.; Lin, C.N.; Lee, C.W.; Ko, H.H. HPLC-fingerprints and antioxidant constituents of Phyla nodiflora. Sci. World J. 2014, 1–8. [Google Scholar] [CrossRef]
- Maas, M.; Deters, A.M.; Hensel, A. Anti-inflammatory activity of Eupatorium perfoliatum L. extracts, eupafolin, and dimeric guaianolide via iNOS inhibitory activity and modulation of inflammation-related cytokines and chemokines. J. Ethnopharmacol. 2011, 137, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Lai, Z.R.; Ho, Y.L.; Huang, S.C.; Huang, T.H.; Lai, S.C.; Tsai, J.C.; Wang, C.Y.; Huang, G.J.; Chang, Y.S. Antioxidant, anti-inflammatory and antiproliferative activities of Kalanchoe gracilis (L.) DC stem. Am. J. Chin. Med. 2011, 39, 1275–1290. [Google Scholar] [CrossRef] [PubMed]
- Abo-Salem, O.M. Kaempferol attenuates the development of diabetic neuropathic pain in mice: Possible anti-inflammatory and anti-oxidant mechanisms. Maced. J. Med. Sci. 2014, 7, 424–430. [Google Scholar] [CrossRef]
- Kim, S.K.; Kim, H.J.; Choi, S.E.; Park, K.H.; Choi, H.K.; Lee, M.W. Anti-oxidative and inhibitory activities on nitric oxide (NO) and prostaglandin E2 (COX-2) production of flavonoids from seeds of Prunus tomentosa Thunberg. Arch. Pharm. Res. 2008, 31, 424–428. [Google Scholar] [CrossRef] [PubMed]
- Coelho, R.G.; Batista, L.M.; Santos, C.S.; Brito, A.R.M.S.; Vilegas, W. Phytochemical study and antiulcerogenic activity of Syngonanthus bisulcatus (Eriocaulaceae). J. Pharmacol. Sci. 2006, 42, 413–417. [Google Scholar] [CrossRef]
- Olaleye, S.B.; Farombi, E.O. Attenuation of indomethacin- and HCl/ethanol-induced oxidative gastric mucosa damage in rats by kolaviron, a natural biflavonoid of Garcinia kola seed. Phytother. Res. 2006, 20, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, F.; Izzo, A.A. The Plant kingdom as a source of anti-ulcer remedies. Phytother. Res. 2000, 14, 581–591. [Google Scholar] [CrossRef]
- Hollander, D.; Tarnawski, A. Dietary essential fatty acids and the decline in peptic ulcer diseasea hypothesis. Gut 1986, 27, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Kakub, G.; Gulfraz, M. Cytoprotective effects of Bergenia ciliate sternb, extract on gastric ulcer in rats. Phytother. Res. 2007, 21, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Magistretti, J.; Brevi, S.; de Curtis, M. The antiulcer activity of Treculia acuminate extract against ethanol induced gastric ulcer in rats. J. Clin. Exp. Pharmacol. 1988, 41, 34–41. [Google Scholar] [CrossRef]
- Anderson, M.E. Determination of glutathione and glutathione disulfide in biological samples. Methods Enzymol. 1985, 113, 548–555. [Google Scholar] [CrossRef] [PubMed]
- Esterbauer, H.; Cheeseman, K.H. Determination of aldehydic lipid peroxidation products: Malonaldehyde and 4-hydroxynonenal. Methods Enzymol. 1990, 186, 407–421. [Google Scholar] [CrossRef] [PubMed]
- Krawisz, J.E.; Sharon, P.S.W.; Stenson, W.F. Quantitative assay for acute intestinal inflammation based on myeloperoxidase activity. Assessment of inflammation in rat and hamster models. Gastroenterology 1984, 87, 1344–1350. [Google Scholar] [PubMed]
- Safieh-Garabedian, B.; Poole, S.; Allchorne, A.; Winter, J.; Woolf, C.J. Contribution of interleukin-1 beta to the inflammation-induced increase in nerve growth factor levels and inflammatory hyperalgesia. Br. J. Pharmacol. 1995, 115, 1265–1275. [Google Scholar] [CrossRef] [PubMed]
- Dokmeci, D.; Akpolat, M.; Aydogdu, N.; Doganay, L.; Turan, F.N. L-carnitine inhibits ethanol-induced gastric mucosal injury in rats. Pharmacol. Rep. 2005, 57, 481–488. [Google Scholar] [PubMed]
- McManus, J. Histological and histochemical uses of periodic acid. Biotech. Histochem. 1948, 23, 99–108. [Google Scholar] [CrossRef]
- Araújo Júnior, R.F.; Reinaldo, M.P.O.S.; Brito, G.A.C.; Cavalcanti, P.F.; Freire, M.A.M.; De Medeiros, C.A.X.; Araújo, A.A. Olmesartan decreased levels of IL-1 b and COX-2, RANK/RANKL and up-regulated SOCs-1 in an intestinal mucositis model. PLoS ONE 2014, 12, e114923. [Google Scholar] [CrossRef]
- Takayama, C.; de-Faria, F.M.; de Almeida, A.C.; Valim-Araújo, D.A.; Rehen, C.S.; Dunder, R.J.; Socca, E.A.; Manzo, L.P.; Rozza, A.L.; Salvador, M.J.; et al. Gastroprotective and ulcer healing effects of essential oil from Hyptis spicigera Lam. (Lamiaceae). J. Ethnopharmacol. 2011, 135, 147–155. [Google Scholar] [CrossRef] [PubMed]

| Peak | [M + H]+ | [M − H]− | Compounds | Peak | [M + H]+ | [M − H]− | Compounds | Peak | [M + H]+ | [M − H]− | Compounds |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 787.2277 | Patuletin-O-hexoside-di-O-deoxy-hexoside | 10 | 667.1871 | 665.1798 | Patuletin-O-deoxy-hexoside-O-acetyl-deoxy-hexoside | 19 | 707.1892 | Patuletin-di-O-acetyl-deoxy-hexoside | ||
| 2 | 641.1698 | Patuletin-O-hexoside-O-deoxy-hexoside | 11 | 667.1874 | 665.179 | Patuletin-O-deoxy-hexoside-O-acetyl-deoxy-hexoside | 20 | 707.1886 | Patuletin-di-O-acetyl-deoxy-hexoside | ||
| 3 | 771.2316 | Eupafolin-O-hexoside-di-O-deoxy-hexoside | 12 | 651.1913 | 649.1833 | Eupafolin-O-deoxy-hexoside-O-acetyl-deoxy-hexoside | 21 | 709.1962 | 707.1898 | Patuletin-di-O-acetyl-deoxy-hexoside | |
| 4 | 479.1179 | 477.1102 | Patuletin-O-deoxy-hexoside | 13 | 651.1916 | 649.1833 | Eupafolin-O-deoxy-hexoside-O-acetyl-deoxy-hexoside | 22 | 693.2003 | Eupafolin-di-O-acetyl-deoxy-hexoside | |
| 5 | 609.1811 | Eupafolin-di-O-deoxy-hexoside | 14 | 649.1832 | Eupafolin-O-deoxy-hexoside-O-acetyl-deoxy-hexoside | 23 | 709.195 | 707.1891 | Patuletin-di-O-acetyl-deoxy-hexoside | ||
| 6 | 667.1874 | 665.1802 | Patuletin-O-deoxy-hexoside-O-acetyl-deoxy-hexoside | 15 | 667.1856 | 665.1782 | Patuletin-O-deoxy-hexoside-O-acetyl-deoxy-hexoside | 24 | 707.1896 | Patuletin-di-O-acetyl-deoxy-hexoside | |
| 7 | 665.1805 | Patuletin-O-deoxy-hexoside-O-acetyl-deoxy-hexoside | 16 | 707.1891 | Patuletin-di-O-acetyl-deoxy-hexoside | 25 | 707.1904 | Patuletin-di-O-acetyl-deoxy-hexoside | |||
| 8 | 665.1806 | Patuletin-O-deoxy-hexoside-O-acetyl-deoxy-hexoside | 17 | 709.1967 | 707.1883 | Patuletin-di-O-acetyl-deoxy-hexoside | 26 | 691.1957 | Eupafolin-di-O-acetyl-deoxy-hexoside | ||
| 9 | 665.1798 | Patuletin-O-deoxy-hexoside-O-acetyl-deoxy-hexoside | 18 | 707.1893 | Patuletin-di-O-acetyl-deoxy-hexoside | 27 | 707.1905 | Patuletin-di-O-acetyl-deoxy-hexoside |
| Peak | [M + H]+ | [M − H]− | Compounds |
|---|---|---|---|
| 1 | 641.1353 | Patuletin-O-deoxy-hexoside-O-hexoside. | |
| 2 | 463.0937 | Quercetin-O-hexoside | |
| 3 | 463.0869 | Kaempferol | |
| 4 | 581.1527 | 579.1425 | Quercetin-O-deoxy-hexoside-O-pentoside |
| 5 | 579.1426 | Quercetin-O-deoxy-hexoside-O-pentoside | |
| 6 | 581.1513 | 579.1421 | Quercetin-O-deoxy-hexoside-O-pentoside |
| 7 | 565.1558 | Kaempferol-O-deoxy-hexoside-O-pentoside | |
| 8 | 595.1667 | Eupafolin-O-deoxy-hexoside-O-pentoside |
| Experimental Group | Lesion Area (mm) | Percent of Inhibition (%) |
|---|---|---|
| Gastric lesion | 93.83 ± 14.00 | - |
| Ranitidine (50 mg/kg) | 31.86 ± 9.17 *** | 80.02 |
| K. brasiliensis 125 mg/kg | 65.42 ± 15.67 ** | 37.31 |
| K. brasiliensis 250 mg/kg | 50.33 ± 4.08 *** | 50.37 |
| K. brasiliensis 500 mg/kg | 18.80 ± 5.71 *** | 76.18 |
| K. pinnata 125 mg/kg | 77.71 ± 15.68 ** | 31.96 |
| K. pinnata 250 mg/kg | 43.28 ± 10.04 *** | 62.87 |
| K. pinnata 500 mg/kg | 21.33 ± 6.37 *** | 81.71 |
| Experimental Group | Lesion Area (mm) | Inhibition Percentage (%) |
|---|---|---|
| Gastric lesion | 48.20 ± 4.55 | - |
| Ranitidine (50 mg/kg) | 14.75 ± 3.59 *** | 67.02 |
| K. brasiliensis 125 mg/kg | 31.83 ± 1.47 | 31.50 |
| K. brasiliensis 250 mg/kg | 26.00 ± 5.29 * | 47.18 |
| K. brasiliensis 500 mg/kg | 18.75 ± 5.73 * | 63.53 |
| K. pinnata 125 mg/kg | 30.25 ± 0.95 | 28.15 |
| K. pinnata 250 mg/kg | 21.00 ± 4.83 | 59.51 |
| K. pinnata 500 mg/kg | 20.57 ± 5.85 * | 63.13 |
| Experimental Groups | pH | Intragastric Volume (mL) | Acidity (mEq [H+]) |
|---|---|---|---|
| Positive Control | 1.82 ± 0.03 | 2.23 ± 0.25 | 60.83 ± 17.09 |
| Ranitidine (50 mg/kg) | 3.38 ± 1.60 *** | 2.10 ± 0.95 | 10.35 ± 24.33 *** |
| K. brasiliensis 250 mg/kg | 1.80 ± 0.07 | 2.00 ± 0.45 | 39.61 ± 4.87 |
| K. brasiliensis 500 mg/kg | 1.83 ± 0.06 | 2.28 ± 0.44 | 42.92 ± 12.11 |
| K. pinnata 250 mg/kg | 1.72 ± 0.05 | 2.20 ± 0.20 | 41.21 ± 3.06 |
| K. pinnata 500 mg/kg | 1.74 ± 0.05 | 2.13 ± 0.32 | 45.39 ± 2.41 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Araújo, E.R.D.; Guerra, G.C.B.; Araújo, D.F.d.S.; De Araújo, A.A.; Fernandes, J.M.; De Araújo Júnior, R.F.; Da Silva, V.C.; De Carvalho, T.G.; Ferreira, L.D.S.; Zucolotto, S.M. Gastroprotective and Antioxidant Activity of Kalanchoe brasiliensis and Kalanchoe pinnata Leaf Juices against Indomethacin and Ethanol-Induced Gastric Lesions in Rats. Int. J. Mol. Sci. 2018, 19, 1265. https://doi.org/10.3390/ijms19051265
De Araújo ERD, Guerra GCB, Araújo DFdS, De Araújo AA, Fernandes JM, De Araújo Júnior RF, Da Silva VC, De Carvalho TG, Ferreira LDS, Zucolotto SM. Gastroprotective and Antioxidant Activity of Kalanchoe brasiliensis and Kalanchoe pinnata Leaf Juices against Indomethacin and Ethanol-Induced Gastric Lesions in Rats. International Journal of Molecular Sciences. 2018; 19(5):1265. https://doi.org/10.3390/ijms19051265
Chicago/Turabian StyleDe Araújo, Edilane Rodrigues Dantas, Gerlane Coelho Bernardo Guerra, Daline Fernandes de Souza Araújo, Aurigena Antunes De Araújo, Júlia Morais Fernandes, Raimundo Fernandes De Araújo Júnior, Valéria Costa Da Silva, Thaís Gomes De Carvalho, Leandro De Santis Ferreira, and Silvana Maria Zucolotto. 2018. "Gastroprotective and Antioxidant Activity of Kalanchoe brasiliensis and Kalanchoe pinnata Leaf Juices against Indomethacin and Ethanol-Induced Gastric Lesions in Rats" International Journal of Molecular Sciences 19, no. 5: 1265. https://doi.org/10.3390/ijms19051265
APA StyleDe Araújo, E. R. D., Guerra, G. C. B., Araújo, D. F. d. S., De Araújo, A. A., Fernandes, J. M., De Araújo Júnior, R. F., Da Silva, V. C., De Carvalho, T. G., Ferreira, L. D. S., & Zucolotto, S. M. (2018). Gastroprotective and Antioxidant Activity of Kalanchoe brasiliensis and Kalanchoe pinnata Leaf Juices against Indomethacin and Ethanol-Induced Gastric Lesions in Rats. International Journal of Molecular Sciences, 19(5), 1265. https://doi.org/10.3390/ijms19051265





