Abstract
Anti-apoptotic B cell lymphoma 2 (BCL2) family members (BCL2, MCL1, BCLxL, BCLW, and BFL1) are key players in the regulation of intrinsic apoptosis. Dysregulation of these proteins not only impairs normal development, but also contributes to tumor progression and resistance to various anti-cancer therapies. Therefore, cells maintain strict control over the expression of anti-apoptotic BCL2 family members using multiple mechanisms. Over the past two decades, the importance of post-transcriptional regulation of mRNA in controlling gene expression and its impact on normal homeostasis and disease have begun to be appreciated. In this review, we discuss the RNA binding proteins (RBPs) and microRNAs (miRNAs) that mediate post-transcriptional regulation of the anti-apoptotic BCL2 family members. We describe their roles and impact on alternative splicing, mRNA turnover, and mRNA subcellular localization. We also point out the importance of future studies in characterizing the crosstalk between RBPs and miRNAs in regulating anti-apoptotic BCL2 family member expression and ultimately apoptosis.
1. Introduction
Apoptosis is a physiological process of programmed cell death that maintains tissue function and homeostasis. It is generally characterized by several morphological features including cell shrinkage, chromatin condensation, membrane blebbing, and the formation of apoptotic bodies under light and electron microscopy [1]. Tightly regulated apoptosis plays important roles in multiple aspects of both normal physiology, such as development [2] and immune responses [3,4], and disease biology such as neurodegenerative diseases [5,6], cardiovascular diseases [7,8], carcinogenesis [9,10], and treatment responses to certain drugs [9,11].
Apoptosis is tightly regulated by two major pathways: the extrinsic/death receptor pathway and the intrinsic/mitochondrial pathway. The extrinsic apoptosis pathway is triggered by ligand–receptor interactions between tumor necrosis factor (TNF) family members and corresponding transmembrane death receptors. Once ligands bind, adaptor proteins are recruited and bind to death receptors, resulting in activation of downstream caspase cascades and ultimately cell death. For more details, see [12].
The intrinsic apoptosis pathway is mediated by the B cell lymphoma 2 (BCL2) family of proteins [13]. The BCL2 family, whose namesake was initially identified due to chromosomal translocations that activated BCL2 gene expression [14], has been identified through their composition of a series of shared BCL2 homology (BH) motifs (BH1, BH2, BH3, and BH4). Importantly, only the BH3 motif, which mediates protein–protein interactions between the family members, is strictly conserved across all family members. These proteins are divided into three major subfamilies based on their function and structure: the anti-apoptotic BCL2 proteins (BCL2, MCL1: myeloid cell leukemia 1; BCLxL: B-cell lymphoma extra large; BCLW: BCL2-like protein 2, and BFL1: BCL2-related protein A1), the pro-apoptotic effectors (BAK: BCL2 homologous antagonist/killer; BAX: BCL2-associated X; and BOK: BCL2-related ovarian killer), and the pro-apoptotic BH3 only proteins [15]. The BH3 only proteins can be subclassified into direct activators and sensitizers based on their binding ability to other BCL2 family members [13]. The direct activator BH3 only proteins (e.g., BID: BH3 interacting-domain death agonist and BIM: BCL2-like protein 11) can interact with both the anti-apoptotic BCL2 proteins and the effectors BAK/BAX while the sensitizer BH3 only proteins (e.g., BAD: BCL2-associated death promoter; NOXA: Phorbol-12-myristate-13-acetate-induced protein; and PUMA: p53 upregulated modulator of apoptosis) preferentially bind to the anti-apoptotic BCL2 proteins and thereby indirectly activate BAK/BAX [13]. Cell fate is determined by the balance between the activities of pro-apoptotic and anti-apoptotic BCL2 family members. Under normal cellular homeostasis, the anti-apoptotic members directly bind to the effectors BAK/BAX to counteract their ability to induce apoptosis. However, following cellular stress, such as that induced by radiation or treatment with cytotoxic agents, the BH3 only members are activated. These in turn directly activate BAK/BAX and/or neutralize the function of the anti-apoptotic BCL2 family members by competing for their binding with BAK/BAX. As a result, the effectors BAK/BAX oligomerize in the mitochondrial outer membrane and form pores. The resulting mitochondrial outer membrane permeabilization (MOMP) results in cytochrome c release, activation of downstream caspases, and finally cell death. In addition to their regulation of mitochondrial apoptosis, mediated by the crosstalk among BCL2 family members, BCL2 family proteins have also been shown to induce apoptosis via their regulation of Ca2+ signaling [16,17]. A simplified intrinsic apoptosis pathway is highlighted in Figure 1. For more details see [13,15].
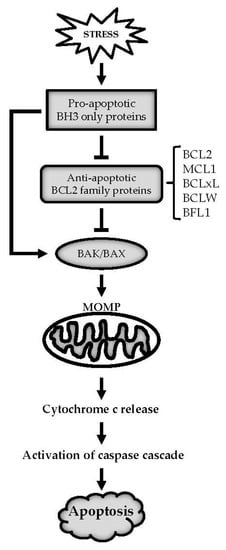
Figure 1.
B cell lymphoma 2 (BCL2) family mediated intrinsic apoptosis signaling. Under cellular stress, pro-apoptotic BCL2 homology 3 (BH3) only proteins are activated, which directly activates BAX/BAX and/or neutralizes the anti-apoptotic BCL2 family members such as BCL2, MCL1, BCLxL, BCLW, and BFL1. This in turn releases BAK/BAX to oligomerize on the mitochondria and results in mitochondrial outer membrane permeabilization (MOMP). The resulting MOMP causes cytochrome c release, which then activates downstream caspase cascade and ultimately triggers apoptosis.
The anti-apoptotic BCL2 family of proteins is commonly dysregulated in human cancers through multiple mechanisms including genomic amplification and genetic overexpression [18]. During tumorigenesis and cancer progression, cancer cells rely on upregulation of the anti-apoptotic BCL2 family of proteins and tend to be addicted to these survival mechanisms [19,20]. For example, a t(14;18) chromosomal translocation leads to the amplification of the BCL2 gene in follicular lymphoma [14]. Similarly, somatic copy number amplification of both the MCL1 and BCLxL genes have been detected across human cancers [21]. Transcriptional activation of the BCL2 family is controlled by multiple proteins. For instance, MCL1 transcription is activated by various transcription factors such as signal transducer and activator of transcription 3 (STAT3), STAT5, hypoxia-inducible factor 1 (HIF1), and E2F1 in a large variety of cancer types [19]. Further, recent studies have begun to identify feedback of the BCL2 family on transcriptional factors that induce their expression [22]. Due to their importance in normal physiology and disease biology especially cancers, regulatory mechanisms of the anti-apoptotic BCL2 family members are being widely studied with several reviews focused on their transcriptional controls [18,19] and post-translational modifications [23,24,25].
Improved genomic technologies and understanding of the importance of non-coding RNA on gene expression have highlighted the multiple mechanisms utilized by cells to regulate gene expression between transcription of the mRNA product and translational protein production. This post-transcriptional regulation of gene expression includes precursor mRNA (pre-mRNA) editing and maturation such as 5′ capping, 3′ polyadenylation, and alternative splicing; mRNA stability control; and mRNA transportation and localization control [26]. It is a dynamic and complicated system mediated by a number of RNA binding proteins (RBPs) and non-coding RNAs such as microRNAs (miRNAs). Understanding the post-transcriptional control of the BCL2 family can complete a comprehensive view of how BCL2 family members are regulated at different levels during gene expression. Further it will help us better understand how such dysregulated post-transcriptional control leads to disease biology, especially tumorigenesis, and make use of this knowledge to better target the anti-apoptotic BCL2 family members in cancer treatment. In this review, we will discuss the RBPs and miRNAs that mediate post-transcriptional regulation of the anti-apoptotic BCL2 family members and their corresponding identified roles in normal physiology and diseases.
2. RNA Binding Proteins (RBPs) and Anti-Apoptotic BCL2 Family Members
RBPs are a group of proteins containing multiple RNA binding modules that bind to single or double stranded RNAs [27]. By far the most common RNA binding module is the RNA recognition motif (RRM) [27]. The K-homology (KH) domain is also a conserved RNA binding module found in a number of RBPs [27]. The presence of multiple RNA binding modules together with the diversity of RNA binding sites on target RNA create an intricate system for controlling gene expression at the post-transcriptional level [27]. In this section, we will review the RBP-mediated post-transcriptional regulation of the anti-apoptotic BCL2 members with a focus on their identified roles in the control of mRNA splicing, stability, and subcellular localization controls.
2.1. Regulation of Pre-mRNA Alternative Splicing
Alternative splicing employs a highly ordered collection of RNA-RNA, protein-protein, and protein–RNA interactions to alter exon inclusion in mature mRNAs. This enables production of multiple protein variants from a single pre-mRNA and is an efficient way to increase the complexity of gene expression in cells. Pre-mRNA splicing is catalyzed by the spliceosomal small nuclear ribonuclear proteins (snRNPs) which bind to the 5′ splice site, 3′ splice site, and branch site in a pre-mRNA (reviewed in [28]). Pre-mRNA also contains cis-acting elements including exonic and intronic splicing enhancers or silencers associated with multiple regulatory RBP proteins that either enhance or repress spliceosomes assembled at the splice sites (reviewed in [29,30]). Thus far, several spliceosome components and regulatory RBPs have been identified to modulate variant splicing of two BCL2 family members, BCLx and MCL1. The splicing control of BCLx and MCL1 is central for regular apoptotic response in normal development with aberrant control of these proteins leading to tumorigenesis, cancer progression, and drug insensitivity. The splicing variants and the corresponding protein products of BCLx and MCL1 are summarized in Figure 2.

Figure 2.
Alternative splicing of BCLx and MCL1. Each panel represents an alternative splicing process from a pre-mRNA containing both introns and exons, to alternatively spliced mature mRNA isoforms, to different multi-motif protein products (L, long; S, short; ES, extra short). The 3′ end of each gene is truncated. The translational start and stop sites are specified on each alternatively spliced mature mRNA variant. Lastly, the impact of each protein product on apoptosis regulation is listed.
2.1.1. BCLx Splicing
BCLx can be alternatively spliced to produce either a long isoform, BCLxL, that contains three exons; or a short isoform, BCLxS, in which the 3′ portion of exon 2 is spliced out [31]. The mature BCLxL and BCLxS retain a shared 3′ untranslated region (UTR). The two protein products BCLxL and BCLxS have opposite functions wherein BCLxL is anti-apoptotic and BCLxS, losing the BH1 and BH2 motifs, is pro-apoptotic [31]. In vivo studies have demonstrated that neonatal hypoxia-ischemia induces BCLx splicing toward its short form, which increases the expression of the BCLxS variant in the rat hippocampus and cortex [32]. In colorectal cancers, BCLxL has been identified to be significantly upregulated in both adenoma and adenocarcinoma tissues compared with normal mucosa [33]. However, the expression profile of BCLxS has been poorly explored in vivo in cancer or other disease models.
Thus far, the regulatory mechanisms of BCLx splicing have been largely investigated using in vitro biochemistry methods or cell lines. Recently, a genome-wide small interfering RNA (siRNA) screen using a BCLx splice reporter construct in HELA cells identified several components of the spliceosome complex that are directly involved in BCLx splicing. The identified snRNP and splicing factors (SF) include: the U1 snRNP protein (SNRP70); U2AF1; U2 snRNP proteins (SF3B1, SF3B4, SF3B5, SF3A1, SF3A3, SNRNPA1); U5 snRNP proteins (U5-200K, PRPF6, UPS39); spliceosomal (Sm) and like Sm (LSM) core proteins (SmB/B′, SmD1, SmD2, SmD3); and survival motor neuron (SMN) complex proteins (SMN1, GEMIN4: Gem-associated protein 4) [34]. It was further determined, using western blot analysis and RT-qPCR, that knockdown of SF3B1 favors BCLx splicing to produce more BCLxS [34]. This alternative splicing network plays an important role in cell cycle control under mitotic stress [34]. In addition to the direct splicing factors, other regulatory RBPs have also been identified to enhance or inhibit BCLx splicing. We have grouped RBPs according to four families— heterogeneous nuclear ribonucleoprotein (hnRNP) proteins, serine/arginine-rich (SR) proteins, signal transduction and activation of RNA (STAR) proteins, and RNA binding motif (RBM) proteins. These RBPs and their impact on BCLx splicing are outlined in Table 1.

Table 1.
RNA binding protein (RBP)-mediated BCLx and MCL1 alternative splicing.
hnRNP Proteins
Heterogeneous nuclear ribonucleoproteins (hnRNPs) are a large family of RBPs that control multiple processes in RNA metabolism [52]. More than 20 hnRNPs have thus far been identified; each containing one or more RNA binding modules such as RRMs, KH domains, qRRMs (quasi-RNA recognition motifs), etc. [52]. The functions of hnRNPs are largely determined by their RNA binding ability and subcellular localization [52]. Thus far, six hnRNP family members have been characterized regarding their impact on BCLx splicing, with four promoting production of BCLxS and two BCLxL. In vitro studies have shown that hnRNP F and H interacted with a 30-nucleotide G-rich element in BCLx and improved the production of the BCLxS variant [39]. Consistent with the in vitro data, knockdown of hnRNP F and H using siRNAs in cells decreases the BCLxS/BCLxL ratio from either the plasmid-derived BCLx transcript or an endogenously expressed BCLx transcript [39]. Likewise, hnRNP K associates with BCLx RNA and enhances production of the BCLxS isoform in both PC3 and HELA cells [40]. hnRNP I/PTBP1 (polypyrimidine tract binding protein 1), another hnRNP family protein, directly binds to a polypyrimidine tract between two alternative 5′ splice sites on BCLx [41]. Overexpression of PTBP1 promotes distal 5′ splice site selection in BCLx exon 2 to generate the BCLxS splice variant while depletion of PTBP1 enhances the production of BCLxL [41]. Mechanistically, this 5′ splice site selection is due to the competition of PTBP1 with a SR protein SRSF1 binding for BCLx RNA [41]. Alternatively, interference with hnRNP A1 nuclear to cytoplasmic shuttling activity decreases the levels of BCLxL in normal and BCR/ABL-transformed myeloid progenitor cells [35]. In addition to interactions with other RBPs, hnRNP family member activity is also impacted by interactions with long non-coding RNA (lncRNA). It has been demonstrated that in breast cancers, the lncRNA, BC200, is oncogenic as its knockdown facilitates expression of the pro-apoptotic BCLxS isoform [36]. Mechanistically, BC200 binds to BCLx via a 17-nucleotide complementary sequence and recruits hnRNP A2B1, thereby impairing the association of BCLx with the BCLxS-promoting splicing factor SAM68 (Src-associated in mitosis of 68 kDa) (discussed in STAR Proteins section, below) and reducing the production of the BCLxS variant [36]. A number of additional hnRNP family members (hnRNP C, hnRNP D, and hnRNP H2) were recently identified to target BCLx [34], though more detailed analysis of these hnRNP family members is required to characterize their roles in regulating BCLx alternative splicing.
SR Proteins
The serine/arginine-rich protein family is a group of RBPs that contain a characteristic C-terminal arginine and serine rich domain (RS domain) and one or two N-terminal RRMs [53]. This protein family has been reported to play essential roles in splicing by promoting or suppressing the function of other splicing factors. Thus far a number of SR proteins have been identified as key regulators of BCLx splicing. SRSF10 has been shown to promote BCLxS production [42]. Following DNA damage, interactions of SRSF10 with other splicing factors, such as the hnRNP family proteins hnRNP K and hnRNP F/H, change; this alters the alternative splicing of a number of DNA damage response transcripts in apoptosis, cell cycle control, and DNA repair [42]. SC35, another member of the SR protein family, has been reported as a key direct target of the transcription factor E2F1. Following its expression, SC35 switches the cellular splicing profile, including that of BCLx towards the pro-apoptotic BCLxS splicing variant [43]. Alternatively, SRp30C has been characterized to bind to ML2 (HincII and XL+MscI treated downstream fragment) and AM2 (AccI and MscI treated downstream fragment) elements in BCLx exon 2 and shifts the splicing to the BCLxL variant by stabilizing U1 snRNP at the 5′ splice site [38]. Pinin (PNN), a serine/arginine related protein, has been shown to alter the expression and function of SR proteins wherein PNN depletion diminished expression of SR proteins [37]. Specifically, PNN loss alters SRSF1-mediated BCLx splicing to produce more of the BCLxS isoform and induces apoptosis in MCF7 cells [37]. Genome-wide siRNA screening has implicated the SR family proteins SRSF2B and SRSF3 in BCLx splicing during early spliceosome formation [34], but more detailed studies are required to characterize their roles in BCLx-splicing-mediated apoptosis.
STAR Proteins
The signal transduction and activation of RNA (STAR) family is a conserved group of KH-domain-containing RBPs [54]. In addition to the KH domain, STAR proteins contain a STAR domain, which is responsible for protein homodimerization and RNA recognition [55]. Like hnRNP and SR proteins, STAR proteins also regulate different aspects in RNA metabolism and processing including pre-mRNA alternative splicing. STAR proteins have been shown to be modified by multiple signaling pathways including phosphorylation [56], methylation [57], acetylation [58], and SUMOylation [59]. Thus, they are believed to play significant roles in linking cell signal transduction with RNA metabolism. Thus far among all the STAR family members, SAM68 is the only STAR protein with well characterized regulation of BCLx splicing. SAM68 was firstly identified to bind to BCLx RNA and regulate its alternative splicing and apoptosis function two decades ago [44]. Depletion of SAM68 induces accumulation of the anti-apoptotic BCLxL isoform whereas overexpression of SAM68 favors the pro-apoptotic BCLxS isoform [44]. Tyrosine phosphorylation (Y528) of SAM68 by FYN (tyrosine-protein kinase Fyn) suppresses SAM68 regulation of BCLx and favors BCLxL splice selection [44]. FYN control of BCLx splice factors has further been studied in the pancreatic cancer BxPc3 cell line, where it was shown that inhibition of FYN not only reduces SAM68 phosphorylation, it also decreases hnRNP A2B1 expression [60]. As downregulation of hnRNP A2B1 also favors BCLxS splicing, this study suggests that hnRNP A2B1 and SAM68 synergistically regulate BCLx splicing and apoptosis in pancreatic cancer [60]. Furthermore, SAM68 has been reported to interact with hnRNP A1 and disruption of the SAM68–hnRNP A1 interaction attenuates BCLxS splicing [44]. Other factors involved in SAM68-mediated BCLx splicing have also been reported. For example, protein arginine N-methyltransferase 2 (PRMT2) interacts with SAM68 and increases the BCLxL/BCLxS ratio in TNF-α or lipopolysaccharide (LPS) stimulated cells, suggesting a role during inflammatory response [61]. Also, the transcription factor FBI-1 (factor binding IST protein 1) interacts with SAM68 and reduces SAM68 binding to BCLx, thereby inhibiting SAM68-mediated BCLx alternative splicing to produce more anti-apoptotic variant BCLxL and suppressing Sam68-induced apoptosis [62]. Other STAR proteins such as T-STAR [63] and ASD-2 (alternative splicing defective protein 2) [64] have also been identified as splicing regulators, but more studies are necessary to pursue their roles in regulating BCLx alternative splicing.
RBM Proteins
RNA binding motif (RBM) containing proteins are not classified as a protein family but are designated RBM proteins due to the presence of one or more RRMs [47]. Multiple RBM proteins have been identified as novel apoptosis modulators [65]. RBM25 has been shown to specifically interact with a CGGGCA sequence in exon 2 of BCLx and promote the pro-apoptotic BCLxS 5′ splice site selection [48]. Likewise, RBM11 has been identified as a tissue-specific splicing regulator during neuron and germ cell differentiation [47]. In vitro and in vivo binding assays reveal that RBM11 binds to BCLx exon 2 at a sequence downstream of the 5′ distal splicing site through its RRM domain [47]. Splicing assays demonstrate that RBM11 facilitates BCLx splicing to produce more BCLxS variant and antagonizes the SR protein SRSF1 in modulating BCLx splicing [47]. Another RBP protein, RBM10 has been shown to promote a 5′ internal splicing site selection of BCLx and RBM10 knockdown reduces the levels of BCLxS variant [46]. Recently, RBM4 has been reported as a novel tumor suppressor by controlling cancer-related splicing [45]. Specifically, RBM4 induces cancer cell apoptosis by modulating BCLx splicing and shifting preference for the anti-apoptotic BCLxL to the pro-apoptotic BCLxS [45] isoform. Additionally, RBM4 can also antagonize the oncogenic SR protein SRSF1 to regulate BCLx splicing and inhibit cancer cell growth [45].
2.1.2. MCL1 Splicing
MCL1 has been reported to have three splicing variants: MCL1, MCL1S, and MCL1ES. MCL1 is the predominantly expressed isoform with three exons and its protein product, MCL1, is anti-apoptotic with one N-terminal PEST domain, four BH motifs, and one C-terminal transmembrane (TM) domain. MCL1S results from splice removal of exon 2 during mRNA processing to produce a pro-apoptotic protein, MCL1S, that lacks the C terminal BH2 motif and TM domain [66]. It has been shown that MCL1S, unlike MCL1, cannot interact with diverse pro-apoptotic BCL2 family proteins but rather dimerizes with MCL1, and works as a novel pro-apoptotic BH3 only protein in cells [66]. MCL1ES is another splicing variant that results from splicing removal of part of exon 1 and encodes a pro-apoptotic protein MCL1ES without the N-terminal PEST domain and BH4 motif [67]. MCL1ES has been shown to localize in cytoplasm with a significant concentration near mitochondria, interact with MCL1 but not BAK and BAX, and be able to induce mitochondrial cell death [67]. However, thus far no splicing factors have been identified that regulate MCL1ES production. Although an increase in MCL1 expression plays an important role during cell differentiation [68] and MCL1 is known to be overexpressed in multiple cancer types, the expression profile of the other two splicing variants (MCL1S and MCL1ES) in vivo has been largely ignored. The regulatory mechanisms of MCL1 splicing thus far have been investigated in vitro using multiple cell lines. A list of direct spliceosome components and regulatory splicing factors that regulate MCL1 splicing is summarized in Table 1.
MCL1 splicing to either the anti-apoptotic MCL1 or pro-apoptotic MCL1S isoforms are not as well studied as BCLx splicing, but still a number of spliceosome components and regulatory RBPs have been characterized to modulate MCL1 splicing. A genome-wide siRNA screen using MCL1 splice reporter constructs in HELA cells identified several spliceosome components (U2 snRNPs–SF3A1, SF3A3, SF3B1, SF3B4, SNRNPA1; Lsm/Sm core–SmB/B′, SmD1, SmD2, SmD3; U5 snRNPs–U5-299K, SRPF6) that are involved in MCL1 splicing with some of them working coordinately to regulate both BCLx and MCL1 splicing [34]. Recent identification that BCL2 targeted therapeutics, such as ABT-737 [69,70] or ABT-199 [71], could be resistant through upregulation of MCL1, has been exploited to further identify factors that control MCL1 expression. In neuroblastomas, a coupled siRNA screen identified that knockdown of splice factors UBL5 (ubiquitin-like protein 5), PRPF8 (pre-mRNA-processing-splicing factor 8), and SART (squamous cell carcinoma antigen recognized by T-cells) could restore sensitivity to ABT-737 in MCL1-dependent neuroblastomas and increased MCL1 splicing to produce more MCL1S variant [51]. Knockdown or biochemical inhibition of the spliceosome component U2 snRNP SF3B1 also favors MCL1 splicing toward the pro-apoptotic MCL1S variant and sensitizes MCL1-dependent neuroblastoma cells to ABT-737 [51].
Of the above identified RBP families, the SR proteins have thus far been most strongly characterized as having important roles in regulating MCL1 splicing. Maintaining a similar anti-apoptotic effect on MCL1 as it did to BCLx, knockdown of SRSF1 significantly increases the levels of MCL1S isoform in both MCF7 and MDA-MB-231 breast cancer cell lines, and the JAr choriocarcinoma cell line [49]. In clear cell renal cell carcinomas, SRSF2 is commonly decreased and knockdown of SRSF2 in renal cancer-derived cell lines results in decreased expression of MCL1S isoforms and inhibiting the apoptotic pathways [50]. Epigenetic modulators have also been characterized to modulate MCL1 alternative splicing [72]. Nonphosphorylated histone deacetylases 1/2 (HDAC1/2) have been shown to be recruited to pre-mRNA by binding to splicing factors, such as SRSF1, and act with lysine acetyltransferases (KATs), such as KAT2B, to catalyze histone acetylation of histone 3 (H3) and histone 4 (H4) of the histone 3 lysine 4 (H3K4) methylated MCL1 exon 2 [72]. As a result, HDAC1/2 activation regulates MCL1 alternative splicing to produce more anti-apoptotic MCL1 [72]. More research needs to be performed to characterize the roles of other RBPs and their upstream signaling regulators in modulating MCL1 splicing.
2.2. Regulation of mRNA Stability
In addition to splice regulation, mRNA turnover plays a critical role in regulating gene expression and quality control of RNA during biogenesis. Typically, mRNA decay is modulated by the RNA-stabilizing or RNA-destabilizing elements on a RNA and is influenced by RBPs bound to these elements [73]. These cis-acting elements are commonly located in the 3′ untranslated region (UTR) of a RNA [73]. The anti-apoptotic BCL2 family members contain 3′ UTRs of variable lengths (1506 to 5278 nt), and maintain significant variation in their mRNA half-lives (Table 2). Thus far, several cis-acting elements have been identified in the 3′ UTR of anti-apoptotic BCL2 family members including AU-rich elements, CU-rich elements, and GU-rich elements. All have been shown to regulate mRNA stability in a positive or negative fashion depending on the direct interactions they mediate with RBPs. RBPs that act as BCL2, MCL1, and BCLxL mRNA stabilizers or destabilizers are summarized in Table 2.
2.2.1. AU-Rich-Element (ARE) Mediated RNA Decay
AU-rich elements are the most studied mRNA stabilizing/destabilizing elements. The ARE-binding protein HuR (human antigen R) has been reported to bind to the 3′ UTRs of MCL1, BCL2, and BCLxL, stabilizing their RNA, and increasing their expression in glioma [74]. This post-transcriptional regulation promotes glioma growth and chemoresistance to standard treatments including etoposide, topotecan, and cisplatin [74]. In HELA cells, similar data have identified that HuR binds to MCL1 and BCL2 RNA with knockdown of HuR decreasing MCL1 and BCL2 expression, thereby inducing apoptosis [75]. Several in vitro and in vivo assays have identified that nucleolin binds to the ARE elements in both BCL2 and BCLxL 3′ UTRs, thereby stabilizing both BCL2 and BCLxL anti-apoptotic messages [76,77]. This stabilization of BCL2 and BCLxL has been identified to control apoptosis and cell survival in multiple normal and cancer cells [76,77,78,79,80]. Several other ARE-binding proteins have also been identified to stabilize BCL2. For example, ζ-crystallin, TRA2β (transformer 2β), and LARP1 (La-related protein 1) have been shown to stabilize BCL2 and enhance BCL2 expression in T cell acute lymphocytic leukemia, colon cancers, and ovarian cancers, respectively [81,82,83]. Alternatively, several ARE-binding proteins have been characterized to decrease mRNA stability. In pathogen-engaged neutrophils, the RNA-destabilizing protein tristetraprolin (TTP) regulates apoptosis during bacterial infection by binding to the ARE elements at the MCL1 3′ UTR, destabilizing MCL1, and decreasing MCL1 expression [84]. Additionally, AUF1 (AU-rich element RNA-binding protein 1) and ZFP36L1 (zinc finger protein 36, C3H1 type-like 1) have been shown to destabilize BCL2 and decrease BCL2 expression [85,86,87]. Further studies characterizing the interplay of these AU-rich binding proteins with one another and identification of the members responsible for regulation of BCLW and BFL1 are needed.

Table 2.
A summary of BCL2, MCL1, and BCLxL mRNA half-lives in different cell lines and their mRNA stabilizers and destabilizers.
Table 2.
A summary of BCL2, MCL1, and BCLxL mRNA half-lives in different cell lines and their mRNA stabilizers and destabilizers.
| mRNA | Half-Life | Cell Type | mRNA Stabilizer | mRNA Destabilizer |
|---|---|---|---|---|
| BCL2 | >6 h [74] | U251 | HuR [74], nucleolin [76], ζ-crystallin [81], TRA2β [82], LARP1 [83] | AUF1 [85], ZFP36L1 [87] |
| 5 h [81] | Jurkat | |||
| 7.5 h [81] | HEK 293 | |||
| 8 h [82] | HCT116 | |||
| 2.5 h [87] | Murine leukemia BCL1 cells | |||
| MCL1 | 1.4 h [88] | PC3 | HuR [74], CUGBP2 [89] | PTBP1 [88], TTP [84] |
| 2.0 h [88] | H1299 | |||
| 4 h [74] | U251 | |||
| 2.3 h [84] | Mice peritoneal neutrophil stimulated with LPS | |||
| 0.5 h [89] | HCT116 | |||
| BCLxL | 3.4 h [74] | U251 | HuR [74], nucleolin [77] | n.a |
| 4 h [77] | HELA | |||
| >6 h [78] | PAEC |
n.a: not available.
2.2.2. CU-Rich-Element Mediated RNA Decay
PTBP1 is a RBP that binds to CU-rich elements within RNA. PTBP1 has been reported to bind to MCL1 especially at its 3′ UTR and act to destabilize MCL1 mRNA [88]. Knockdown of PTBP1 has further been shown to increase MCL1 expression in multiple cancer cell lines due to its stabilization of MCL1 [88]. Further studies identified that the pro-apoptotic effect of PTBP1 under mitotic stress induced by antitubulin drugs vincristine and docetaxel results from its suppression of MCL1 expression in cancer cells [88]. Thus far no other RBPs binding to CU-rich elements have been reported to regulate the half-lives of either MCL1 or other anti-apoptotic BCL2 family members.
2.2.3. GU-Rich-Element (GRE) Mediated RNA Decay
CUGBP2 (CUG triplet repeat RNA-binding protein 2) is a GRE binding protein. Studies have shown that MCL1 is a novel target of CUGBP2 wherein CUGBP2 binds to the MCL1 3′ UTR and increases MCL1 mRNA stability in colon cancers [89]. However, overexpression of CUGBP2 in colon cancer cells reduces MCL1 protein levels possibly due to its inhibitory effect on translation [89].
2.3. Regulation of mRNA Subcellular Localization
mRNA localization is a conserved mechanism that employs proteins to localize mRNA transcripts and proteins to their site of function [90]. It is regulated by the dynamic remodeling of ribonucleoprotein (RNP) complexes via interactions between different trans-acting proteins and cis-acting mRNA sequences [90]. mRNA localization plays important roles in effective and precise protein translation and further regulates diverse cellular functions, including neuronal morphogenesis [91]. Characterization of the proteins that regulate BCL2 family mRNA has begun to identify some of the regulators of their subcellular localization. The first study to characterize RBP impact on BCL2 family mRNA localization demonstrated that HuR silencing in glioma cells results in a general shift of MCL1, BCL2, and BCLxL mRNA towards polyribosomes [74]. This indicates that HuR not only regulates the degradation of MCL1, BCL2, and BCLxL mRNA, but it also controls their translation [74]. Similarly, it has been shown that knockdown of PTBP1 increases MCL1 mRNA accumulation in the cytoplasm in prostate and lung cancer cells [88]. SFPQ (splicing factor, proline- and glutamine-rich) has been shown to bind to BCLW mRNA at its 3′ UTR and it is required for axonal trafficking of BCLW [92]. This SRPQ-mediated spatial gene expression is essential to promote axonal viability [92]. It is likely that a number of the RBPs identified in the previous two sections also impact subcellular localization of mRNA. However, thus far characterization of this portion of their effects has been largely ignored.
3. MicroRNAs (miRNAs) and Anti-Apoptotic BCL2 Family Members
In addition to RBPs, miRNAs are another group of molecules in cells that control gene expression post-transcriptionally. A number of studies have connected RBPs with miRNAs in regulating gene expression with RBPs either enhancing or counteracting miRNA targeting of a shared mRNA [93], though limited analysis of RBP impact on miRNA targeting of the BCL2 family has been conducted. miRNAs are small non-coding RNAs of around 22 nucleotides in length and are highly conserved in various organisms. miRNAs function via perfect or imperfect base-pairing with their target mRNAs typically in the 3′ UTR. Mechanistically, mature miRNAs are loaded onto the miRNA induced silencing complex (miRISC) where the core component argonaute (AGO) family proteins recruit other factors to induce target mRNA degradation or translational repression. For more details about the molecular mechanisms of miRNA-mediated gene silencing, see ref [94]. Over the past two decades, miRNAs have been identified as key regulators in cancer biology. Numerous studies have demonstrated that miRNA-mediated dysregulation of gene expression is involved in multiple aspects in cancer biology such as tumor cell growth, cell death resistance, dysregulated metabolism, invasion, metastasis, immune evasion, and so on (reviewed in [95]). Thus far, more than 35 miRNAs have been identified to target and decrease the expression of the anti-apoptotic BCL2 family members (Table 3 and Figure 3). All miRNAs referenced in this review were validated in the cited literature by assessing their impact on both the endogenous expression of their targets and the exogenous luciferase activity in constructs containing either wildtype or mutated miRNA binding sites after miRNA mimic/inhibitor transfections. A majority of miRNAs target only one anti-apoptotic family member while miR-125b, miR-133a/b, and miR-153 have been shown to target multiple members (Table 3). This implies that miR-125b, miR-133a/b, and miR-153 may have an additive effect on apoptosis compared with miRNAs that can only target one anti-apoptotic BCL2 family member. The positions of each of the discussed miRNAs are mapped on the 3′ UTR of each gene in Figure 3. In this section, we will review the miRNA-mediated post-transcriptional control of BCL2, MCL1, BCLxL, BCLW, and BFL1, and their identified roles in cancer biology and anti-cancer drug response.

Table 3.
Validated miRNAs targeting BCL2, MCL1, BCLxL, and BCLW.
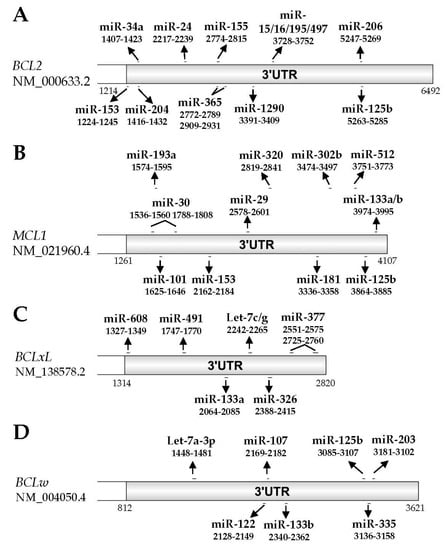
Figure 3.
Validated miRNA binding sites on the 3′ untranslated region (UTR) of anti-apoptotic family members. A schematic diagram of 3′ UTR of BCL2 (NM_000633.2, nucleotides 1214–6492), MCL1 (NM_021960.4, nucleotides 1261–4107), BCLxL (NM_138578.2, nucleotides 1314–2820), and BCLW (NM_004050.4, nucleotides 812–3621). Validated miRNAs and their binding positions to each mRNA transcript are shown in line.
3.1. BCL2
Thus far 12 miRNAs have been validated to target BCL2. In 2002, the miR-15/16 cluster was identified as one of the first examples of tumor suppressor miRNAs [134]. It was deleted by 13q14 deletions or downregulated by other mechanisms in approximately 70% of chronic lymphoid leukemia (CLL) patients [134]. In 2005, further studies identified that the miR-15/16 cluster directly targets BCL2 and is now recognized as one of the major negative regulators of BCL2 expression [96]. Subsequent studies have identified that miR-155 and miR-125b also repress BCL2 through the interactions with its 3′ UTR and partially mediate proliferation and cell cycle arrest response to CD40 ligand (CD154) in human leukemia B-cells [100]. The direct repression of BCL2 by miR-125b has also been demonstrated in hepatocellular carcinoma (HCC), in which it suppresses HCC cells proliferation and induces apoptosis [99]. Recently, miR-34a has been shown to directly target the BCL2 3′ UTR with an inverse correlation between miR-34a and BCL2 expression levels identified in HCC tissues [98]. Functional assays have demonstrated that miR-34a inhibits cell viability, induces apoptosis, and sensitizes HCC cells to sorafenib treatment by suppressing BCL2 expression [98]. In neuroblastoma cells, miR-204 has been reported to significantly increase sensitivity to cisplatin and its expression is predictive with better clinical outcome for primary neuroblastoma tumors [102]. This effect is in part due to miR-204’s direct targeting to the 3′ UTR of BCL2 [102]. Additionally, miR-206 has been shown to directly target BCL2 in glioblastoma cell lines and the decreased miR-206 expression is inversely correlated with the increased BCL2 expression levels in glioblastoma tissues [104]. miR-153, a brain-specific miRNA, has been reported to directly down-regulate both BCL2 and MCL1 to induce apoptosis in glioblastoma [101]. BCL2 is also a direct target of miR-1290 and miR-206 in non-small cell lung cancer (NSCLC) [103,106], with miR-1290 mediated silencing of BCL2 has been reported to regulate the apoptotic effect to asiatic acid—a putative anti-cancer agent—in A549 cells [106]. miR-206 expression is very low in NSCLC and functions as a tumor suppressor through its downregulation of BCL2 and MET (hepatocyte growth factor receptor) [103]. In breast cancers, miR-195, miR-24-2, and miR-365-2 have been validated as negative regulators of BCL2 via their direct binding at its 3′ UTR [97]. It has been demonstrated that these miRNAs not only promote apoptosis but also enhance the apoptotic response to the anti-tumor drug etoposide in MCF7 cells [97]. Lastly, in breast cancer specimens, miR-497 levels have been shown to be inversely correlated with BCL2 expression [105]. Molecular studies have confirmed that miR-497 directly targets BCL2 and regulates apoptosis in breast cancer [105].
3.2. MCL1
In addition to miR-153 discussed above [101], twelve additional miRNAs have been validated to target MCL1. The first miRNA targeting MCL1, miR-29, was identified in 2007 and shown to directly and negatively regulate MCL1 expression through its 3′ UTR and control apoptosis in non-malignant H69 cholangiocytes and malignant KMCH cholangiocarcinoma cell lines [108]. Later studies have shown that miR-29 suppresses MCL1 expression and induces apoptosis in HCC [107] and ALK (anaplastic lymphoma kinase)-positive anaplastic large cell lymphoma [109]. miR-101 is another well-studied miRNA targeting MCL1. It was firstly identified that HCC commonly express low levels of miR-101 with reintroduction of miR-101 reducing MCL1 expression, thereby inducing apoptosis and suppressing tumorigenesis [114]. Further studies have reported the miR-101 induces MCL1 silencing in gastric cancer [112], NSCLC [135], endometrial cancer [113], and triple negative breast cancer (TNBC) [111]. In these studies, miR-101 not only induces apoptosis, but it is also implicated in clinical outcomes in NSCLC [135] and regulates sensitivity to paclitaxel in TNBC [111]. In addition to miR-29 and miR-101, several other miRNAs have been validated to target MCL1 in multiple cancer types in the past decade. In mouse and human hematopoietic cells, radiation induces miR-30 expression, which inhibits MCL1, but not BCL2 expression, and promotes radiation-induced apoptosis [110]. In chronic myelogenous leukemia (CML), overexpression of tyrosine-protein kinase, Lyn, has been shown to reduce miR-181 expression, which directly targets MCL1 [118]. This mechanism plays a key role for MCL1-mediated imatinib resistance in CML [118]. Likewise, ionizing radiation has been shown to induce miR-193a-3p expression and promote apoptosis by directly targeting MCL1 in U251 glioma cells [119]. In HCC, miR-125b has been shown to induce apoptosis by downregulating MCL1, BCLW, and IL6R [115]. However a microRNA screen in HCT116 colon cancer cells shows that miR-125b has no effects on MCL1 expression or on cell viability and apoptosis when treated with the BCL2 inhibitor ABT-263 [136]. These conflicting studies suggest that miR-125b-mediated MCL1 repression is cell-type-dependent and highlight the importance that specific cell-type miRNA profiles have in regulating apoptosis. In lung cancer, miR-133b expression is largely reduced compared to adjacent normal tissues and studies have shown that miR-133b targets the 3′ UTR of both MCL1 and BCLW and promotes gemcitabine-induced apoptosis [117]. Also, miR-133a has been shown to target and downregulate MCL1 in osteosarcoma [116]. Additionally, miR-302b, miR-320, and miR-512-5p have been validated to target MCL1 and regulate cancer progression and apoptosis in malignant pleural mesothelioma [120], cervical cancer [121], and gastric cancer [122], respectively.
3.3. BCLxL
There are six miRNAs validated to target BCLxL. Let-7c/g, members of the first known human miRNA family [137,138], have been shown to negatively regulate BCLxL expression via its 3′ UTR and promote sorafenib-induced apoptosis in HCC [123]. Later reports have shown that miR-491 induces apoptosis by targeting BCLxL in colorectal cancer [139], glioblastoma [140], and ovarian cancer [126]. Further studies have reported that miR-34a and miR-608 modulate chordoma malignancy, a rare malignant tumor originating from notochord, by directly targeting BCLxL, EGFR (epidermal growth factor receptor), and MET [127]. In osteosarcoma, miR-133a not only targets MCL1 but also BCLxL where its expression level is commonly down-regulated [116]. This significantly correlates with tumor progression and patient prognosis [116]. Development of BCL2 inhibitors has revealed multiple miRNAs that regulate BCLxL expression. CLL cells resistant to ABT-199 were found to express low level of miR-377 and high level of BCLxL [125]. Further they show that miR-377 represses BCLxL expression via direct association at two binding sites in the BCLxL 3′UTR [125]. These findings suggest that the miR-377-mediated BCLxL repression inversely drives resistance to ABT-199 in CLL [125]. miRNA-dependent BCLxL regulation is not exclusively employed by cancers, but is also involved in normal cell homeostasis. For example, the miR-302/miR-367 cluster controls human embryonic stem cell (hESC) apoptosis by upregulating pro-apoptotic BNIP3L/Nix (BCL2/adenovirus E1B 19kDa protein-interacting protein 3-like) and downregulating BCLxL [141]. Moreover, miR-326 has been shown to target the BCLxL 3′ UTR and regulate apoptosis in human platelets [124].
3.4. BCLW
Seven miRNAs have been validated to target BCLW. miR-133b was the first validated miRNA to target BCLW in lung cancer [117]. Subsequent studies have identified that miR-203 also downregulates BCLW by directly targeting its 3′ UTR, which regulates the apoptosis response following treatment with the DNA damage agent camptothecin (CPT) in HCT116 colon cancer cells and chemosensitivity to cisplatin in bladder cancer [131,132,142]. Recently, let-7a-3p, miR-107, miR-122, miR-125b, and miR-335 have been shown to target BCLW in glioblastoma [128], NSCLC [129], pterygium [130], HCC [115], and clear cell renal cell carcinoma [133], respectively. Interestingly, although miR-184 cannot target BCLW and BCLxL in its native state, oxidation of miR-184 by reactive oxygen species (ROS) induces its association with the 3′ UTR of both BCLW and BCLxL and promotes apoptosis in heart tissue following ischemia/reperfusion injury [143]. However this study was performed in mouse models [143]. Since the 3′ UTR sequences of BCLW and BCLxL in mouse are different from those in humans, we do not know if this mechanism is maintained in a human genetic background.
3.5. BFL1
BFL1 has been much less well studied among the anti-apoptotic BCL2 subfamily, especially for its post-transcriptional regulation. The detailed regulation of BFL1 is reviewed in [144], but thus far no validated miRNA targeting BFL1 have been reported. A single human apoptosis array study in medullablastoma included BFL1 and identified that miR-10b downregulates BFL1 expression by approximately 31-fold [145]. BFL1 is also a predicted target of miR-181a using different bioinformatics platforms [146]. However, there have been no further studies confirming that these two miRNAs directly target BFL1. Given the importance that BFL1 may have in regulation of human BCL2 family signaling, more studies need to be carried out to build up the post-transcriptional regulation of BFL1.
4. Conclusions and Future Perspectives
Because of the essential roles of the BCL2 family in apoptosis regulation and cancer cell survival [19], in the past decade BH3 mimics targeting the anti-apoptotic BCL2 members have been developed from bench to bedside and back again. In 2016, ABT-199 (Venclexta), a selective BCL2 inhibitor, was approved by the U.S. Food and Drug Administration (FDA) to treat CLL in patients carrying a 17p deletion demonstrating an overall response rate of 80 percent [147]. In the meantime, several other drugs targeting single or multiple anti-apoptotic BCL2 family members have shown promising responses in single-agent or combination therapies for solid and hematopoietic tumors in pre-clinical studies and phase I/II/III clinical trials [18,148]. However, the regulatory network of the anti-apoptotic BCL2 members is still complex and unclear. In this review, we have summarized the current literature about the RBP and miRNA mediated post-transcriptional regulation of the anti-apoptotic BCL2 family. While numerous regulatory RBPs and miRNAs have been identified, the crosstalk among them has been largely ignored. A lone example is the finding that the RBP, TRA2β, competes with miR-204 binding to BCL2 3′ UTR to modulate BCL2 mRNA stability [82]. Further research needs to be done to investigate the potential competitive or cooperative roles between different RBPs, and between different RBPs and miRNAs.
While the initial identification of the anti-apoptotic nature of BCL2 arose due to a chromosomal translocation resulting in its upregulation, similar genetic events have not been identified to regulate other BCL2 family members. Yet, upregulation of MCL1, BCL2, BCLxL, BCLW, and BFL1 have all been identified as drivers of tumorigenesis and chemoresistance. By understanding the post-transcriptional regulation of the anti-apoptotic family, the field will gain critical insight into the complex mechanisms that govern cellular control of apoptosis.
Acknowledgments
We thank Rui Zhao, University of Alabama at Birmingham (UAB), for critical reading of the manuscript prior to submission. This work was supported by a grant from the National Institutes of Health [RO1 GM117391], the UAB New Faculty Development Grant, and the UAB Comprehensive Cancer Center New Faculty Development Award in Cancer Research (to William J. Placzek); the UAB Howard Hughes Medical Institute Med into Grad Fellowship and the UAB Carmichael Scholarship (to Jia Cui). This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Contributions
Jia Cui analyzed the data; Jia Cui and William J. Placzek wrote the paper.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| AGO | Argonaute |
| ALK | Anaplastic lymphoma kinase |
| ARE | AU rich element |
| ASD-2 | Alternative splicing defective protein 2 |
| AUF1 | AU-rich element RNA-binding protein 1 |
| BAD | BCL2-associated death promoter |
| BAK | BCL2 homologous antagonist/killer |
| BAX | BCL2-associated X |
| BCLW | BCL2-like protein 2 |
| BCLxL | B-cell lymphoma extra large |
| BCL2 | B cell lymphoma 2 |
| BFL1 | BCL2-related protein A1 |
| BH | BCL2 homology |
| BID | BH3 interacting-domain death agonist |
| BIM | BCL2-like protein 11 |
| BNIP3L | BCL2/adenovirus E1B 19kDa protein-interacting protein 3-like |
| BOK | BCL2-related ovarian killer |
| CLL | Chronic lymphoid leukemia |
| CPT | Camptothecin |
| CUGBP2 | CUG triplet repeat RNA-binding protein 2 |
| EGFR | Epidermal growth factor receptor |
| FBI-1 | Factor binding IST protein 1 |
| GEMIN4 | Gem-associated protein 4 |
| GRE | GU rich element |
| H3 | Histone 3 |
| H3K4 | Histone 3 lysine 4 |
| H4 | Histone 4 |
| HCC | Hepatocellular carcinoma |
| HDAC | Histone deacetylase |
| HIF | Hypoxia inducible factor |
| hnRNP | Heterogeneous nuclear ribonucleoprotein |
| HuR | Human antigen R |
| KAT | Lysine acetyltransferase |
| LARP1 | La-related protein 1 |
| lncRNA | Long non-coding RNA |
| LPS | Lipopolysaccharide |
| LSM | Like-spliceosomal |
| MCL1 | Myeloid cell leukemia 1 |
| MET | Hepatocyte growth factor receptor |
| miRISC | microRNA induced silencing complex |
| miRNA | microRNA |
| MOMP | Mitochondrial outer membrane permeabilization |
| NOXA | Phorbol-12-myristate-13-acetate-induced protein |
| NSCLC | Non-small cell lung cancer |
| PEST domain | Proline, glutamic acid, serine, threonine rich domain |
| PNN | Pinin |
| Pre-mRNA | Precursor messenger RNA |
| PRMT2 | Protein-arginine methyltransferase 2 |
| PRPF8 | Pre-mRNA-processing-splicing factor 8 |
| PTBP1 | Polypyrimidine tract binding protein 1 |
| PUMA | p53 upregulated modulator of apoptosis |
| qRRM | Quasi-RNA recognition motif |
| RBM | RNA binding motif |
| RBP | RNA binding protein |
| RNP | Ribonucleoprotein |
| ROS | Reactive oxygen species |
| RRM | RNA recognition motif |
| SAM68 | SRC associated in mitosis of 68 kDa |
| SART | Squamous cell carcinoma antigen recognized by T-cells |
| SF | Splicing factor |
| SFPQ | Splicing factor, proline and glutamine rich |
| siRNA | Small interfering RNA |
| Sm | Spliceosomal |
| SMN | Survival motor neuron |
| snRNP | Spliceosomal small nuclear ribonuclear protein |
| SR protein | Serine/arginine-rich protein |
| STAR | Signal transduction and activation of RNA |
| STAT | Signal transducer and activator of transcription |
| TNBC | Triple-negative breast cancer |
| TNF | Tumor necrosis factor |
| TRA2β | Transformer 2β |
| TTP | Tristetraprolin |
| TM domain | Transmembrane domain |
| UBL5 | Ubiquitin-like protein 5 |
| UTR | Untranslated region |
| ZFP36L1 | Zinc finger protein 36, C3H1 type-like 1 |
References
- Elmore, S. Apoptosis: A Review of Programmed Cell Death. Toxicol. Pathol. 2016, 35, 495–516. [Google Scholar] [CrossRef] [PubMed]
- Opferman, J.T.; Kothari, A. Anti-apoptotic BCL2 family members in development. Cell Death Differ. 2017, 25, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Opferman, J.T. Apoptosis in the development of the immune system. Cell Death Differ. 2008, 15, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Creagh, E.M. Caspase crosstalk: Integration of apoptotic and innate immune signalling pathways. Trends Immunol. 2014, 35, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Friedlander, R.M. Apoptosis and caspases in neurodegenerative diseases. N. Engl. J. Med. 2003, 348, 1365–1375. [Google Scholar] [CrossRef] [PubMed]
- Ghavami, S.; Shojaei, S.; Yeganeh, B.; Ande, S.R.; Jangamreddy, J.R.; Mehrpour, M.; Mehrpour, M.; Christoffersson, J.; Chaabane, W.; Moghadam, A.R.; et al. Autophagy and apoptosis dysfunction in neurodegenerative disorders. Prog. Neurobiol. 2014, 112, 24–49. [Google Scholar] [CrossRef] [PubMed]
- Kang, P.M.; Izumo, S. Apoptosis in heart: Basic mechanisms and implications in cardiovascular diseases. Trends Mol. Med. 2003, 9, 177–182. [Google Scholar] [CrossRef]
- Teringova, E.; Tousek, P. Apoptosis in ischemic heart disease. J. Transl. Med. 2017, 15, 87. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.M.; Attardi, L.D. The role of apoptosis in cancer development and treatment response. Nat. Rev. Cancer 2005, 5, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Lopez, J.; Tait, S.W. Mitochondrial apoptosis: Killing cancer using the enemy within. Br. J. Cancer 2015, 112, 957–962. [Google Scholar] [CrossRef] [PubMed]
- Delbridge, A.R.; Strasser, A. The BCL2 protein family, BH3-mimetics and cancer therapy. Cell Death Differ. 2015, 22, 1071–1080. [Google Scholar] [CrossRef] [PubMed]
- Verbrugge, I.; Johnstone, R.W.; Smyth, M.J. SnapShot: Extrinsic apoptosis pathways. Cell 2010, 143, 1192–1192.e2. [Google Scholar] [CrossRef] [PubMed]
- Chipuk, J.E.; Moldoveanu, T.; Llambi, F.; Parsons, M.J.; Green, D.R. The BCL2 family reunion. Mol. Cell 2010, 37, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Tsujimoto, Y.; Finger, L.; Yunis, J.; Nowell, P.; Croce, C. Cloning of the chromosome breakpoint of neoplastic B cells with the t(14;18) chromosome translocation. Science 1984, 226, 1097–1099. [Google Scholar] [CrossRef] [PubMed]
- Hardwick, J.M.; Soane, L. Multiple functions of BCL2 family proteins. Cold Spring Harb. Perspect. Biol. 2013, 5. [Google Scholar] [CrossRef] [PubMed]
- Vervliet, T.; Parys, J.B.; Bultynck, G. BCL2 proteins and calcium signaling: Complexity beneath the surface. Oncogene 2016, 35, 5079–5092. [Google Scholar] [CrossRef] [PubMed]
- Rong, Y.P.; Bultynck, G.; Aromolaran, A.S.; Zhong, F.; Parys, J.B.; De Smedt, H.; Mignery, G.A.; Roderick, H.L.; Bootman, M.D.; Distelhorst, C.W. The BH4 domain of BCL2 inhibits ER calcium release and apoptosis by binding the regulatory and coupling domain of the IP3 receptor. Proc. Natl. Acad. Sci. USA 2009, 106, 14397–14402. [Google Scholar] [CrossRef] [PubMed]
- Delbridge, A.R.; Grabow, S.; Strasser, A.; Vaux, D.L. Thirty years of BCL2: Translating cell death discoveries into novel cancer therapies. Nat. Rev. Cancer 2016, 16, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Juin, P.; Geneste, O.; Gautier, F.; Depil, S.; Campone, M. Decoding and unlocking the BCL2 dependency of cancer cells. Nat. Rev. Cancer 2013, 13, 455–465. [Google Scholar] [CrossRef] [PubMed]
- Certo, M.; Del Gaizo Moore, V.; Nishino, M.; Wei, G.; Korsmeyer, S.; Armstrong, S.A.; Letai, A. Mitochondria primed by death signals determine cellular addiction to antiapoptotic BCL2 family members. Cancer Cell 2006, 9, 351–365. [Google Scholar] [CrossRef] [PubMed]
- Beroukhim, R.; Mermel, C.H.; Porter, D.; Wei, G.; Raychaudhuri, S.; Donovan, J.; Barretina, J.; Boehm, J.S.; Dobson, J.; Urashima, M.; et al. The landscape of somatic copy-number alteration across human cancers. Nature 2010, 463, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Zhang, L.S.; Toombs, J.; Kuo, Y.C.; Piazza, J.T.; Tuladhar, R.; Barrett, Q.; Fan, C.W.; Zhang, X.; Walensky, L.D.; et al. Extra-mitochondrial prosurvival BCL2 proteins regulate gene transcription by inhibiting the SUFU tumour suppressor. Nat. Cell Biol. 2017, 19, 1226–1236. [Google Scholar] [CrossRef] [PubMed]
- Thomas, L.W.; Lam, C.; Edwards, S.W. Mcl-1; the molecular regulation of protein function. FEBS Lett. 2010, 584, 2981–2989. [Google Scholar] [CrossRef] [PubMed]
- Vucic, D.; Dixit, V.M.; Wertz, I.E. Ubiquitylation in apoptosis: A post-translational modification at the edge of life and death. Nat. Rev. Mol. Cell Biol. 2011, 12, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Letai, A.; Kutuk, O. Regulation of BCL2 Family Proteins by Posttranslational Modifications. Curr. Mol. Med. 2008, 8, 102–118. [Google Scholar] [CrossRef]
- Ascano, M.; Gerstberger, S.; Tuschl, T. Multi-disciplinary methods to define RNA-protein interactions and regulatory networks. Curr. Opin. Genet. Dev. 2013, 23, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Lunde, B.M.; Moore, C.; Varani, G. RNA-binding proteins: Modular design for efficient function. Nat. Rev. Mol. Cell Biol. 2007, 8, 479–490. [Google Scholar] [CrossRef] [PubMed]
- Will, C.L.; Luhrmann, R. Spliceosome structure and function. Cold Spring Harb. Perspect. Biol. 2011, 3. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Burge, C.B. Splicing regulation: From a parts list of regulatory elements to an integrated splicing code. RNA 2008, 14, 802–813. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.D.; Ares, M., Jr. Context-dependent control of alternative splicing by RNA-binding proteins. Nat. Rev. Genet. 2014, 15, 689–701. [Google Scholar] [CrossRef] [PubMed]
- Boise, L.H.; González-García, M.; Postema, C.E.; Ding, L.; Lindsten, T.; Turka, L.A.; Mao, X.; Nuñez, G.; Thompson, C.B. BCLx, a BCL2-related gene that functions as a dominant regulator of apoptotic cell death. Cell 1993, 74, 597–608. [Google Scholar] [CrossRef]
- Xiao, Q.; Ford, A.L.; Xu, J.; Yan, P.; Lee, K.Y.; Gonzales, E.; West, T.; Holtzman, D.M.; Lee, J.M. BCLx pre-mRNA splicing regulates brain injury after neonatal hypoxia-ischemia. J. Neurosci. 2012, 32, 13587–13596. [Google Scholar] [CrossRef] [PubMed]
- Scherr, A.L.; Gdynia, G.; Salou, M.; Radhakrishnan, P.; Duglova, K.; Heller, A.; Keim, S.; Kautz, N.; Jassowicz, A.; Elssner, C.; et al. BCLxL is an oncogenic driver in colorectal cancer. Cell Death Dis. 2016, 7, e2342. [Google Scholar] [CrossRef] [PubMed]
- Moore, M.J.; Wang, Q.; Kennedy, C.J.; Silver, P.A. An alternative splicing network links cell-cycle control to apoptosis. Cell 2010, 142, 625–636. [Google Scholar] [CrossRef] [PubMed]
- Iervolino, A.; Santilli, G.; Trotta, R.; Guerzoni, C.; Cesi, V.; Bergamaschi, A.; Gambacorti-Passerini, C.; Calabretta, B.; Perrotti, D. hnRNP A1 Nucleocytoplasmic Shuttling Activity Is Required for Normal Myelopoiesis and BCR/ABL Leukemogenesis. Mol. Cell. Biol. 2002, 22, 2255–2266. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Gupta, S.C.; Peng, W.X.; Zhou, N.; Pochampally, R.; Atfi, A.; Watabe, K.; Lu, Z.; Mo, Y.Y. Regulation of alternative splicing of BCLx by BC200 contributes to breast cancer pathogenesis. Cell Death Dis. 2016, 7, e2262. [Google Scholar] [CrossRef] [PubMed]
- Leu, S.; Lin, Y.M.; Wu, C.H.; Ouyang, P. Loss of Pnn expression results in mouse early embryonic lethality and cellular apoptosis through SRSF1-mediated alternative expression of BCLxS and ICAD. J. Cell Sci. 2012, 125, 3164–3172. [Google Scholar] [CrossRef] [PubMed]
- Cloutier, P.; Toutant, J.; Shkreta, L.; Goekjian, S.; Revil, T.; Chabot, B. Antagonistic effects of the SRp30c protein and cryptic 5′ splice sites on the alternative splicing of the apoptotic regulator BCLx. J. Biol. Chem. 2008, 283, 21315–21324. [Google Scholar] [CrossRef] [PubMed]
- Garneau, D.; Revil, T.; Fisette, J.F.; Chabot, B. Heterogeneous nuclear ribonucleoprotein F/H proteins modulate the alternative splicing of the apoptotic mediator BCLx. J. Biol. Chem. 2005, 280, 22641–22650. [Google Scholar] [CrossRef] [PubMed]
- Revil, T.; Pelletier, J.; Toutant, J.; Cloutier, A.; Chabot, B. Heterogeneous nuclear ribonucleoprotein K represses the production of pro-apoptotic BCLxS splice isoform. J. Biol. Chem. 2009, 284, 21458–21467. [Google Scholar] [CrossRef] [PubMed]
- Bielli, P.; Bordi, M.; Di Biasio, V.; Sette, C. Regulation of BCLX splicing reveals a role for the polypyrimidine tract binding protein (PTBP1/hnRNP I) in alternative 5′ splice site selection. Nucleic Acids Res. 2014, 42, 12070–12081. [Google Scholar] [CrossRef] [PubMed]
- Shkreta, L.; Toutant, J.; Durand, M.; Manley, J.L.; Chabot, B. SRSF10 Connects DNA Damage to the Alternative Splicing of Transcripts Encoding Apoptosis, Cell-Cycle Control, and DNA Repair Factors. Cell Rep. 2016, 17, 1990–2003. [Google Scholar] [CrossRef] [PubMed]
- Merdzhanova, G.; Edmond, V.; De Seranno, S.; Van den Broeck, A.; Corcos, L.; Brambilla, C.; Brambilla, E.; Gazzeri, S.; Eymin, B. E2F1 controls alternative splicing pattern of genes involved in apoptosis through upregulation of the splicing factor SC35. Cell Death Differ. 2008, 15, 1815–1823. [Google Scholar] [CrossRef] [PubMed]
- Paronetto, M.P.; Achsel, T.; Massiello, A.; Chalfant, C.E.; Sette, C. The RNA-binding protein Sam68 modulates the alternative splicing of BCLx. J. Cell Biol. 2007, 176, 929–939. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Chen, D.; Qian, H.; Tsai, Y.S.; Shao, S.; Liu, Q.; Dominguez, D.; Wang, Z. The splicing factor RBM4 controls apoptosis, proliferation, and migration to suppress tumor progression. Cancer Cell 2014, 26, 374–389. [Google Scholar] [CrossRef] [PubMed]
- Inoue, A.; Yamamoto, N.; Kimura, M.; Nishio, K.; Yamane, H.; Nakajima, K. RBM10 regulates alternative splicing. FEBS Lett. 2014, 588, 942–947. [Google Scholar] [CrossRef] [PubMed]
- Pedrotti, S.; Busa, R.; Compagnucci, C.; Sette, C. The RNA recognition motif protein RBM11 is a novel tissue-specific splicing regulator. Nucleic Acids Res. 2012, 40, 1021–1032. [Google Scholar] [CrossRef] [PubMed]
- Zhou, A.; Ou, A.C.; Cho, A.; Benz, E.J., Jr.; Huang, S.C. Novel splicing factor RBM25 modulates BCLx pre-mRNA 5′ splice site selection. Mol. Cell. Biol. 2008, 28, 5924–5936. [Google Scholar] [CrossRef] [PubMed]
- Gautrey, H.L.; Tyson-Capper, A.J. Regulation of Mcl-1 by SRSF1 and SRSF5 in cancer cells. PLoS ONE 2012, 7, e51497. [Google Scholar] [CrossRef] [PubMed]
- Kedzierska, H.; Poplawski, P.; Hoser, G.; Rybicka, B.; Rodzik, K.; Sokol, E.; Boguslawska, J.; Tanski, Z.; Fogtman, A.; Koblowska, M.; et al. Decreased Expression of SRSF2 Splicing Factor Inhibits Apoptotic Pathways in Renal Cancer. Int. J. Mol. Sci. 2016, 17, 1598. [Google Scholar] [CrossRef] [PubMed]
- Laetsch, T.W.; Liu, X.; Vu, A.; Sliozberg, M.; Vido, M.; Elci, O.U.; Goldsmith, K.C.; Hogarty, M.D. Multiple components of the spliceosome regulate Mcl1 activity in neuroblastoma. Cell Death Dis. 2014, 5, e1072. [Google Scholar] [CrossRef] [PubMed]
- Geuens, T.; Bouhy, D.; Timmerman, V. The hnRNP family: Insights into their role in health and disease. Hum. Genet. 2016, 135, 851–867. [Google Scholar] [CrossRef] [PubMed]
- Bradley, T.; Cook, M.E.; Blanchette, M. SR proteins control a complex network of RNA-processing events. RNA 2015, 21, 75–92. [Google Scholar] [CrossRef] [PubMed]
- Vernet, C.; Artzt, K. STAR, a gene family involved in signal transduction and activation of RNA. Trends Genet. 1997, 13, 479–484. [Google Scholar] [CrossRef]
- Feracci, M.; Foot, J.N.; Grellscheid, S.N.; Danilenko, M.; Stehle, R.; Gonchar, O.; Kang, H.S.; Dalgliesh, C.; Meyer, N.H.; Liu, Y.; et al. Structural basis of RNA recognition and dimerization by the STAR proteins T-STAR and Sam68. Nat. Commun. 2016, 7, 10355. [Google Scholar] [CrossRef] [PubMed]
- Matter, N.; Herrlich, P.; Konig, H. Signal-dependent regulation of splicing via phosphorylation of Sam68. Nature 2002, 420, 691–695. [Google Scholar] [CrossRef] [PubMed]
- Cote, J.; Boisvert, F.M.; Boulanger, M.C.; Bedford, M.T.; Richard, S. Sam68 RNA binding protein is an in vivo substrate for protein arginine N-methyltransferase 1. Mol. Biol. Cell 2003, 14, 274–287. [Google Scholar] [CrossRef] [PubMed]
- Babic, I.; Jakymiw, A.; Fujita, D.J. The RNA binding protein Sam68 is acetylated in tumor cell lines, and its acetylation correlates with enhanced RNA binding activity. Oncogene 2004, 23, 3781–3789. [Google Scholar] [CrossRef] [PubMed]
- Babic, I.; Cherry, E.; Fujita, D.J. SUMO modification of Sam68 enhances its ability to repress cyclin D1 expression and inhibits its ability to induce apoptosis. Oncogene 2006, 25, 4955–4964. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.Y.; Cai, L.; Zhu, J.; Chen, M.; Chen, J.; Li, Z.H.; Liu, X.D.; Wang, S.G.; Bie, P.; Jiang, P.; et al. Fyn requires HnRNPA2B1 and Sam68 to synergistically regulate apoptosis in pancreatic cancer. Carcinogenesis 2011, 32, 1419–1426. [Google Scholar] [CrossRef] [PubMed]
- Vhuiyan, M.I.; Pak, M.L.; Park, M.A.; Thomas, D.; Lakowski, T.M.; Chalfant, C.E.; Frankel, A. PRMT2 interacts with splicing factors and regulates the alternative splicing of BCLX. J. Biochem. 2017, 162, 17–25. [Google Scholar] [PubMed]
- Bielli, P.; Busa, R.; Di Stasi, S.M.; Munoz, M.J.; Botti, F.; Kornblihtt, A.R.; Sette, C. The transcription factor FBI-1 inhibits SAM68-mediated BCLX alternative splicing and apoptosis. EMBO Rep. 2014, 15, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Ehrmann, I.; Dalgliesh, C.; Liu, Y.; Danilenko, M.; Crosier, M.; Overman, L.; Arthur, H.M.; Lindsay, S.; Clowry, G.J.; Venables, J.P.; et al. The tissue-specific RNA binding protein T-STAR controls regional splicing patterns of neurexin pre-mRNAs in the brain. PLoS Genet. 2013, 9, e1003474. [Google Scholar] [CrossRef] [PubMed]
- Ohno, G.; Hagiwara, M.; Kuroyanagi, H. STAR family RNA-binding protein ASD-2 regulates developmental switching of mutually exclusive alternative splicing in vivo. Genes Dev. 2008, 22, 360–374. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, L.C.; Rintala-Maki, N.D.; White, R.D.; Morin, C.D. RNA binding motif (RBM) proteins: A novel family of apoptosis modulators? J. Cell. Biochem. 2005, 94, 5–24. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.; Leo, C.P.; Hsu, S.Y.; Hsueh, A.J. MCL-1S, a splicing variant of the antiapoptotic BCL2 family member MCL-1, encodes a proapoptotic protein possessing only the BH3 domain. J. Biol. Chem. 2000, 275, 25255–25261. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Sim, S.H.; Ha, H.J.; Ko, J.J.; Lee, K.; Bae, J. MCL-1ES, a novel variant of MCL-1, associates with MCL-1L and induces mitochondrial cell death. FEBS Lett. 2009, 583, 2758–2764. [Google Scholar] [CrossRef] [PubMed]
- Craig, R.W. MCL1 provides a window on the role of the BCL2 family in cell proliferation, differentiation and tumorigenesis. Leukemia 2002, 16, 444–454. [Google Scholar] [CrossRef] [PubMed]
- Yecies, D.; Carlson, N.E.; Deng, J.; Letai, A. Acquired resistance to ABT-737 in lymphoma cells that up-regulate MCL-1 and BFL-1. Blood 2010, 115, 3304–3313. [Google Scholar] [CrossRef] [PubMed]
- Pan, R.; Ruvolo, V.R.; Wei, J.; Konopleva, M.; Reed, J.C.; Pellecchia, M.; Andreeff, M.; Ruvolo, P.P. Inhibition of Mcl-1 with the pan-BCL2 family inhibitor (-)BI97D6 overcomes ABT-737 resistance in acute myeloid leukemia. Blood 2015, 126, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.H.; Winter, P.S.; Xie, A.; Roth, C.; Martz, C.A.; Stein, E.M.; Anderson, G.R.; Tingley, J.P.; Wood, K.C. Targeting MCL-1/BCLXL Forestalls the Acquisition of Resistance to ABT-199 in Acute Myeloid Leukemia. Sci. Rep. 2016, 6. [Google Scholar] [CrossRef]
- Khan, D.H.; Gonzalez, C.; Cooper, C.; Sun, J.M.; Chen, H.Y.; Healy, S.; Xu, W.; Smith, K.T.; Workman, J.L.; Leygue, E.; et al. RNA-dependent dynamic histone acetylation regulates MCL1 alternative splicing. Nucleic Acids Res. 2014, 42, 1656–1670. [Google Scholar] [CrossRef] [PubMed]
- Schoenberg, D.R.; Maquat, L.E. Regulation of cytoplasmic mRNA decay. Nat. Rev. Genet. 2012, 13, 246–259. [Google Scholar] [CrossRef] [PubMed]
- Filippova, N.; Yang, X.; Wang, Y.; Gillespie, G.Y.; Langford, C.; King, P.H.; Wheeler, C.; Nabors, L.B. The RNA-binding protein HuR promotes glioma growth and treatment resistance. Mol. Cancer Res. 2011, 9, 648–659. [Google Scholar] [CrossRef] [PubMed]
- Abdelmohsen, K.; Lal, A.; Kim, H.H.; Gorospe, M. Posttranscriptional orchestration of an anti-apoptotic program by HuR. Cell Cycle 2007, 6, 1288–1292. [Google Scholar] [CrossRef] [PubMed]
- Sengupta, T.K.; Bandyopadhyay, S.; Fernandes, D.J.; Spicer, E.K. Identification of nucleolin as an AU-rich element binding protein involved in BCL2 mRNA stabilization. J. Biol. Chem. 2004, 279, 10855–10863. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Tsaprailis, G.; Bowden, G.T. Nucleolin stabilizes BCLx L messenger RNA in response to UVA irradiation. Cancer Res. 2008, 68, 1046–1054. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Mungunsukh, O.; Tutino, R.L.; Marquez, A.P.; Day, R.M. Angiotensin-II-induced apoptosis requires regulation of nucleolin and BCLxL by SHP-2 in primary lung endothelial cells. J. Cell Sci. 2010, 123, 1634–1643. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.A.; Li, H.Y.; Hsu, T.I.; Chen, S.H.; Wu, C.J.; Chang, W.C.; Hung, J.J. Heat shock protein 90 stabilizes nucleolin to increase mRNA stability in mitosis. J. Biol. Chem. 2011, 286, 43816–43829. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.H.; Childress, M.O.; Geahlen, R.L. Syk interacts with and phosphorylates nucleolin to stabilize BCLx(L) mRNA and promote cell survival. Mol. Cell. Biol. 2014, 34, 3788–3799. [Google Scholar] [CrossRef] [PubMed]
- Lapucci, A.; Lulli, M.; Amedei, A.; Papucci, L.; Witort, E.; Di Gesualdo, F.; Bertolini, F.; Brewer, G.; Nicolin, A.; Bevilacqua, A.; et al. zeta-Crystallin is a BCL2 mRNA binding protein involved in BCL2 overexpression in T-cell acute lymphocytic leukemia. FASEB J. 2010, 24, 1852–1865. [Google Scholar] [CrossRef] [PubMed]
- Kuwano, Y.; Nishida, K.; Kajita, K.; Satake, Y.; Akaike, Y.; Fujita, K.; Kano, S.; Masuda, K.; Rokutan, K. Transformer 2beta and miR-204 regulate apoptosis through competitive binding to 3′ UTR of BCL2 mRNA. Cell Death Differ. 2015, 22, 815–825. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, T.G.; Mura, M.; Al-Ashtal, H.A.; Lahr, R.M.; Abd-Latip, N.; Sweeney, K.; Lu, H.; Weir, J.; El-Bahrawy, M.; Steel, J.H.; et al. The RNA-binding protein LARP1 is a post-transcriptional regulator of survival and tumorigenesis in ovarian cancer. Nucleic Acids Res. 2016, 44, 1227–1246. [Google Scholar] [CrossRef] [PubMed]
- Ebner, F.; Sedlyarov, V.; Tasciyan, S.; Ivin, M.; Kratochvill, F.; Gratz, N.; Kenner, L.; Villunger, A.; Sixt, M.; Kovarik, P. The RNA-binding protein tristetraprolin schedules apoptosis of pathogen-engaged neutrophils during bacterial infection. J. Clin. Investig. 2017, 127, 2051–2065. [Google Scholar] [CrossRef] [PubMed]
- Lapucci, A.; Donnini, M.; Papucci, L.; Witort, E.; Tempestini, A.; Bevilacqua, A.; Nicolin, A.; Brewer, G.; Schiavone, N.; Capaccioli, S. AUF1 Is a BCL2 A + U-rich element-binding protein involved in BCL2 mRNA destabilization during apoptosis. J. Biol. Chem. 2002, 277, 16139–16146. [Google Scholar] [CrossRef] [PubMed]
- Ishimaru, D.; Zuraw, L.; Ramalingam, S.; Sengupta, T.K.; Bandyopadhyay, S.; Reuben, A.; Fernandes, D.J.; Spicer, E.K. Mechanism of regulation of BCL2 mRNA by nucleolin and A+U-rich element-binding factor 1 (AUF1). J. Biol. Chem. 2010, 285, 27182–27191. [Google Scholar] [CrossRef] [PubMed]
- Zekavati, A.; Nasir, A.; Alcaraz, A.; Aldrovandi, M.; Marsh, P.; Norton, J.D.; Murphy, J.J. Post-transcriptional regulation of BCL2 mRNA by the RNA-binding protein ZFP36L1 in malignant B cells. PLoS ONE 2014, 9, e102625. [Google Scholar] [CrossRef] [PubMed]
- Cui, J.; Placzek, W.J. PTBP1 modulation of MCL1 expression regulates cellular apoptosis induced by antitubulin chemotherapeutics. Cell Death Differ. 2016, 23, 1681–1690. [Google Scholar] [CrossRef] [PubMed]
- Subramaniam, D.; Natarajan, G.; Ramalingam, S.; Ramachandran, I.; May, R.; Queimado, L.; Houchen, C.W.; Anant, S. Translation inhibition during cell cycle arrest and apoptosis: Mcl-1 is a novel target for RNA binding protein CUGBP2. Am. J. Physiol. Gastrointest. Liver Physiol. 2008, 294, G1025–G1032. [Google Scholar] [CrossRef] [PubMed]
- Parton, R.M.; Davidson, A.; Davis, I.; Weil, T.T. Subcellular mRNA localisation at a glance. J. Cell Sci. 2014, 127, 2127–2133. [Google Scholar] [CrossRef] [PubMed]
- Mofatteh, M.; Bullock, S.L. SnapShot: Subcellular mRNA Localization. Cell 2017, 169, 178–178.e1. [Google Scholar] [CrossRef] [PubMed]
- Cosker, K.E.; Fenstermacher, S.J.; Pazyra-Murphy, M.F.; Elliott, H.L.; Segal, R.A. The RNA-binding protein SFPQ orchestrates an RNA regulon to promote axon viability. Nat. Neurosci. 2016, 19, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Ciafre, S.A.; Galardi, S. microRNAs and RNA-binding proteins: A complex network of interactions and reciprocal regulations in cancer. RNA Biol. 2013, 10, 935–942. [Google Scholar] [CrossRef] [PubMed]
- Jonas, S.; Izaurralde, E. Towards a molecular understanding of microRNA-mediated gene silencing. Nat. Rev. Genet. 2015, 16, 421–433. [Google Scholar] [CrossRef] [PubMed]
- Hayes, J.; Peruzzi, P.P.; Lawler, S. MicroRNAs in cancer: Biomarkers, functions and therapy. Trends Mol. Med. 2014, 20, 460–469. [Google Scholar] [CrossRef] [PubMed]
- Cimmino, A.; Calin, G.A.; Fabbri, M.; Iorio, M.V.; Ferracin, M.; Shimizu, M.; Wojcik, S.E.; Aqeilan, R.I.; Zupo, S.; Dono, M.; et al. miR-15 and miR-16 induce apoptosis by targeting BCL2. Proc. Natl. Acad. Sci. USA 2005, 102, 13944–13949. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Saini, N. Downregulation of BCL2 by miRNAs augments drug-induced apoptosis—A combined computational and experimental approach. J. Cell Sci. 2012, 125 Pt 6, 1568–1578. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Li, Q.J.; Gong, Z.B.; Zhou, L.; You, N.; Wang, S.; Li, X.L.; Li, J.J.; An, J.Z.; Wang, D.S.; et al. MicroRNA-34a targets BCL2 and sensitizes human hepatocellular carcinoma cells to sorafenib treatment. Technol. Cancer Res. Treat. 2014, 13, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Zhao, A.; Zeng, Q.; Xie, X.; Zhou, J.; Yue, W.; Li, Y.; Pei, X. MicroRNA-125b induces cancer cell apoptosis through suppression of BCL2 expression. J. Genet. Genom. 2012, 39, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Willimott, S.; Wagner, S.D. miR-125b and miR-155 contribute to BCL2 repression and proliferation in response to CD40 ligand (CD154) in human leukemic B-cells. J. Biol. Chem. 2012, 287, 2608–2617. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Liao, X.; Wong, C. Downregulations of B-cell lymphoma 2 and myeloid cell leukemia sequence 1 by microRNA 153 induce apoptosis in a glioblastoma cell line DBTRG-05MG. Int. J. Cancer 2010, 126, 1029–1035. [Google Scholar] [CrossRef] [PubMed]
- Ryan, J.; Tivnan, A.; Fay, J.; Bryan, K.; Meehan, M.; Creevey, L.; Lynch, J.; Bray, I.M.; O’Meara, A.; Tracey, L.; et al. MicroRNA-204 increases sensitivity of neuroblastoma cells to cisplatin and is associated with a favourable clinical outcome. Br. J. Cancer 2012, 107, 967–976. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Liu, Z.; Li, S.; Yang, C.; Xue, R.; Xi, Y.; Wang, L.; Wang, S.; He, Q.; Huang, J.; et al. Down-regulation of c-Met and BCL2 by microRNA-206, activates apoptosis, and inhibits tumor cell proliferation, migration and colony formation. Oncotarget 2015, 6, 25533–25574. [Google Scholar] [CrossRef] [PubMed]
- Hao, W.; Luo, W.; Bai, M.; Li, J.; Bai, X.; Guo, J.; Wu, J.; Wang, M. MicroRNA-206 Inhibited the Progression of Glioblastoma Through BCL2. J. Mol. Neurosci. 2016, 60, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Wei C, L.Q.; Sun, X.; Li, D.; Song, H.; Li, X.; Song, J.; Hua, K.; Fang, L. microRNA-497 induces cell apoptosis by negatively regulating BCL2 protein expression at the posttranscriptional level in human breast cancer. Int. J. Clin. Exp. Pathol. 2015, 8, 7729–7739. [Google Scholar] [PubMed]
- Kim, K.B.; Kim, K.; Bae, S.; Choi, Y.; Cha, H.J.; Kim, S.Y.; Lee, J.H.; Jeon, S.H.; Jung, H.J.; Ahn, K.J.; et al. MicroRNA-1290 promotes asiatic acidinduced apoptosis by decreasing BCL2 protein level in A549 nonsmall cell lung carcinoma cells. Oncol. Rep. 2014, 32, 1029–1036. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Y.; Fang, J.H.; Yun, J.P.; Yang, J.; Zhang, Y.; Jia, W.H.; Zhuang, S.M. Effects of microRNA-29 on apoptosis, tumorigenicity, and prognosis of hepatocellular carcinoma. Hepatology 2010, 51, 836–845. [Google Scholar] [CrossRef] [PubMed]
- Mott, J.L.; Kobayashi, S.; Bronk, S.F.; Gores, G.J. mir-29 regulates Mcl-1 protein expression and apoptosis. Oncogene 2007, 26, 6133–6140. [Google Scholar] [CrossRef] [PubMed]
- Desjobert, C.; Renalier, M.H.; Bergalet, J.; Dejean, E.; Joseph, N.; Kruczynski, A.; Soulier, J.; Espinos, E.; Meggetto, F.; Cavaille, J.; et al. MiR-29a down-regulation in ALK-positive anaplastic large cell lymphomas contributes to apoptosis blockade through MCL-1 overexpression. Blood 2011, 117, 6627–6637. [Google Scholar] [CrossRef] [PubMed]
- Li, X.H.; Ha, C.T.; Xiao, M. MicroRNA-30 inhibits antiapoptotic factor Mcl-1 in mouse and human hematopoietic cells after radiation exposure. Apoptosis 2016, 21, 708–720. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Tang, H.; Chen, J.; Song, C.; Yang, L.; Liu, P.; Wang, N.; Xie, X.; Lin, X.; Xie, X. MicroRNA-101 inhibits cell progression and increases paclitaxel sensitivity by suppressing MCL-1 expression in human triple-negative breast cancer. Oncotarget 2015, 6, 20070–20083. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.J.; Ruan, H.J.; He, X.J.; Ma, Y.Y.; Jiang, X.T.; Xia, Y.J.; Ye, Z.Y.; Tao, H.Q. MicroRNA-101 is down-regulated in gastric cancer and involved in cell migration and invasion. Eur. J. Cancer 2010, 46, 2295–2303. [Google Scholar] [CrossRef] [PubMed]
- Konno, Y.; Dong, P.; Xiong, Y.; Suzuki, F.; Lu, J.; Cai, M.; Watari, H.; Mitamura, T.; Hosaka, M.; Hanley, S.J.; et al. MicroRNA-101 targets EZH2, MCL-1 and FOS to suppress proliferation, invasion and stem cell-like phenotype of aggressive endometrial cancer cells. Oncotarget 2014, 5, 6049–6062. [Google Scholar] [CrossRef] [PubMed]
- Su, H.; Yang, J.R.; Xu, T.; Huang, J.; Xu, L.; Yuan, Y.; Zhuang, S.M. MicroRNA-101, down-regulated in hepatocellular carcinoma, promotes apoptosis and suppresses tumorigenicity. Cancer Res. 2009, 69, 1135–1142. [Google Scholar] [CrossRef] [PubMed]
- Gong, J.; Zhang, J.P.; Li, B.; Zeng, C.; You, K.; Chen, M.X.; Yuan, Y.; Zhuang, S.M. MicroRNA-125b promotes apoptosis by regulating the expression of Mcl-1, BCLW and IL-6R. Oncogene 2013, 32, 3071–3079. [Google Scholar] [CrossRef] [PubMed]
- Ji, F.; Zhang, H.; Wang, Y.; Li, M.; Xu, W.; Kang, Y.; Wang, Z.; Wang, Z.; Cheng, P.; Tong, D.; et al. MicroRNA-133a, downregulated in osteosarcoma, suppresses proliferation and promotes apoptosis by targeting BCLxL and Mcl-1. Bone 2013, 56, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Crawford, M.; Batte, K.; Yu, L.; Wu, X.; Nuovo, G.J.; Marsh, C.B.; Otterson, G.A.; Nana-Sinkam, S.P. MicroRNA 133B targets pro-survival molecules MCL-1 and BCL2L2 in lung cancer. Biochem. Biophys. Res. Commun. 2009, 388, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, E.I.; Dollins, C.M.; Crawford, M.; Grant, S.; Nana-Sinkam, S.P.; Richards, K.L.; Hammond, S.M.; Graves, L.M. Lyn kinase-dependent regulation of miR181 and myeloid cell leukemia-1 expression: Implications for drug resistance in myelogenous leukemia. Mol. Pharmacol. 2010, 78, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.E.; Kim, B.Y.; Kwak, S.Y.; Bae, I.H.; Han, Y.H. Ionizing radiation-inducible microRNA miR-193a-3p induces apoptosis by directly targeting Mcl-1. Apoptosis 2013, 18, 896–909. [Google Scholar] [CrossRef] [PubMed]
- Khodayari, N.; Mohammed, K.A.; Lee, H.; Kaye, F.; Nasreen, N. MicroRNA-302b targets Mcl-1 and inhibits cell proliferation and induces apoptosis in malignant pleural mesothelioma cells. Am. J. Cancer Res. 2016, 6, 1996–2009. [Google Scholar] [PubMed]
- Zhang, T.; Zou, P.; Wang, T.; Xiang, J.; Cheng, J.; Chen, D.; Zhou, J. Down-regulation of miR-320 associated with cancer progression and cell apoptosis via targeting Mcl-1 in cervical cancer. Tumour Biol. 2016, 37, 8931–8940. [Google Scholar] [CrossRef] [PubMed]
- Saito, Y.; Suzuki, H.; Tsugawa, H.; Nakagawa, I.; Matsuzaki, J.; Kanai, Y.; Hibi, T. Chromatin remodeling at Alu repeats by epigenetic treatment activates silenced microRNA-512-5p with downregulation of Mcl-1 in human gastric cancer cells. Oncogene 2009, 28, 2738–2744. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, S.; Takehara, T.; Hikita, H.; Kodama, T.; Miyagi, T.; Hosui, A.; Tatsumi, T.; Ishida, H.; Noda, T.; Nagano, H.; et al. The let-7 family of microRNAs inhibits BCLxL expression and potentiates sorafenib-induced apoptosis in human hepatocellular carcinoma. J. Hepatol. 2010, 52, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.; Huang, H.; Deng, G.; Xie, Z.; Ye, Y.; Guo, R.; Cai, X.; Hong, J.; Qian, D.; Zhou, X.; et al. miR-326 targets antiapoptotic BCLxL and mediates apoptosis in human platelets. PLoS ONE 2015, 10, e0122784. [Google Scholar]
- Al-Harbi, S.; Choudhary, G.S.; Ebron, J.S.; Hill, B.T.; Vivekanathan, N.; Ting, A.H.; Radivoyevitch, T.; Smith, M.R.; Shukla, G.C.; Almasan, A. miR-377-dependent BCLxL regulation drives chemotherapeutic resistance in B-cell lymphoid malignancies. Mol. Cancer 2015, 14. [Google Scholar] [CrossRef] [PubMed]
- Denoyelle, C.; Lambert, B.; Meryet-Figuiere, M.; Vigneron, N.; Brotin, E.; Lecerf, C.; Abeilard, E.; Giffard, F.; Louis, M.H.; Gauduchon, P.; et al. miR-491-5p-induced apoptosis in ovarian carcinoma depends on the direct inhibition of both BCLXL and EGFR leading to BIM activation. Cell Death Dis. 2014, 5, e1445. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Schiff, D.; Park, D.; Abounader, R. MicroRNA-608 and microRNA-34a regulate chordoma malignancy by targeting EGFR, BCLxL and MET. PLoS ONE 2014, 9, e91546. [Google Scholar]
- Dong, Z.; Lei, Q.; Yang, R.; Zhu, S.; Ke, X.X.; Yang, L.; Cui, H.; Yi, L. Inhibition of neurotensin receptor 1 induces intrinsic apoptosis via let-7a-3p/BCLW axis in glioblastoma. Br. J. Cancer 2017, 116, 1572–1584. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Xie, Z.; Peng, Q. MiRNA-107 enhances chemosensitivity to paclitaxel by targeting antiapoptotic factor BCLW in non small cell lung cancer. Am. J. Cancer Res. 2017, 7, 1863–1873. [Google Scholar] [PubMed]
- Cui, Y.H.; Li, H.Y.; Gao, Z.X.; Liang, N.; Ma, S.S.; Meng, F.J.; Li, Z.J.; Pan, H.W. Regulation of Apoptosis by miR-122 in Pterygium via Targeting BCLW. Investig. Ophthalmol. Vis. Sci. 2016, 57, 3723–3730. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhang, Y.; Liu, X.; Fang, A.; Li, P.; Li, Z.; Liu, T.; Yang, Y.; Du, L.; Wang, C. MicroRNA-203 Is a Prognostic Indicator in Bladder Cancer and Enhances Chemosensitivity to Cisplatin via Apoptosis by Targeting BCLW and Survivin. PLoS ONE 2015, 10, e0143441. [Google Scholar]
- Bo, J.; Yang, G.; Huo, K.; Jiang, H.; Zhang, L.; Liu, D.; Huang, Y. MicroRNA-203 suppresses bladder cancer development by repressing BCLw expression. FEBS J. 2011, 278, 786–792. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Chen, X.; Zhan, Y.; Jiang, W.; Liu, X.; Wang, X.; Wu, B. miR-335 inhibits the proliferation and invasion of clear cell renal cell carcinoma cells through direct suppression of BCLW. Tumour Biol. 2015, 36, 6875–6882. [Google Scholar] [CrossRef] [PubMed]
- Calin, G.A.; Dumitru, C.D.; Shimizu, M.; Bichi, R.; Zupo, S.; Noch, E.; Aldler, H.; Rattan, S.; Keating, M.; Rai, K.; et al. Frequent deletions and down-regulation of micro-RNA genes miR15 and miR16 at 13q14 in chronic lymphocytic leukemia. Proc. Natl. Acad. Sci. USA 2002, 99, 15524–15529. [Google Scholar] [CrossRef] [PubMed]
- Luo, L.; Zhang, T.; Liu, H.; Lv, T.; Yuan, D.; Yao, Y.; Lv, Y.; Song, Y. miR-101 and Mcl-1 in non-small-cell lung cancer: Expression profile and clinical significance. Med. Oncol. 2012, 29, 1681–1686. [Google Scholar] [CrossRef] [PubMed]
- Lam, L.T.; Lu, X.; Zhang, H.; Lesniewski, R.; Rosenberg, S.; Semizarov, D. A microRNA screen to identify modulators of sensitivity to BCL2 inhibitor ABT-263 (navitoclax). Mol. Cancer Ther. 2010, 9, 2943–2950. [Google Scholar] [CrossRef] [PubMed]
- Reinhart, B.J.; Slack, F.J.; Basson, M.; Pasquinelli, A.E.; Bettinger, J.C.; Rougvie, A.E.; Horvitz, H.R.; Ruvkun, G. The 21-nucleotide let-7 RNA regulates developmental timing in Caenorhabditis elegans. Nature 2000, 403, 901–906. [Google Scholar] [CrossRef] [PubMed]
- Pasquinelli, A.E.; Reinhart, B.J.; Slack, F.; Martindale, M.Q.; Kuroda, M.I.; Maller, B.; Hayward, D.C.; Ball, E.E.; Degnan, B.; Muller, P.; et al. Conservation of the sequence and temporal expression of let-7 heterochronic regulatory RNA. Nature 2000, 408, 86–89. [Google Scholar] [PubMed]
- Nakano, H.; Miyazawa, T.; Kinoshita, K.; Yamada, Y.; Yoshida, T. Functional screening identifies a microRNA, miR-491 that induces apoptosis by targeting BCLx(L) in colorectal cancer cells. Int. J. Cancer 2010, 127, 1072–1080. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Liu, Y.; Granberg, K.J.; Wang, Q.; Moore, L.M.; Ji, P.; Gumin, J.; Sulman, E.P.; Calin, G.A.; Haapasalo, H.; et al. Two mature products of MIR-491 coordinate to suppress key cancer hallmarks in glioblastoma. Oncogene 2015, 34, 1619–1628. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Hong, Y.; Xiang, D.; Zhu, P.; Wu, E.; Li, W.; Mosenson, J.; Wu, W.S. MicroRNA-302/367 cluster governs hESC self-renewal by dually regulating cell cycle and apoptosis pathways. Stem Cell Rep. 2015, 4, 645–657. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.; Davis-Dusenbery, B.N.; Kashima, R.; Jiang, X.; Marathe, N.; Sessa, R.; Louie, J.; Gu, W.; Lagna, G.; Hata, A. Acetylation of p53 stimulates miRNA processing and determines cell survival following genotoxic stress. EMBO J. 2013, 32, 3192–3205. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.X.; Gao, J.; Ding, S.L.; Wang, K.; Jiao, J.Q.; Wang, Y.; Sun, T.; Zhou, L.Y.; Long, B.; Zhang, X.J.; et al. Oxidative Modification of miR-184 Enables It to Target BCLxL and BCLW. Mol. Cell 2015, 59, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Vogler, M. BCL2A1: The underdog in the BCL2 family. Cell Death Differ. 2012, 19, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Pal, R.; Greene, S. microRNA-10b Is Overexpressed and Critical for Cell Survival and Proliferation in Medulloblastoma. PLoS ONE 2015, 10, e0137845. [Google Scholar] [CrossRef] [PubMed]
- He, S.; Zeng, S.; Zhou, Z.W.; He, Z.X.; Zhou, S.F. Hsa-microRNA-181a is a regulator of a number of cancer genes and a biomarker for endometrial carcinoma in patients: A bioinformatic and clinical study and the therapeutic implication. Drug Des. Dev. Ther. 2015, 9, 1103–1175. [Google Scholar]
- Cang, S.; Iragavarapu, C.; Savooji, J.; Song, Y.; Liu, D. ABT-199 (venetoclax) and BCL2 inhibitors in clinical development. J. Hematol. Oncol. 2015, 8. [Google Scholar] [CrossRef] [PubMed]
- Ashkenazi, A.; Fairbrother, W.J.; Leverson, J.D.; Souers, A.J. From basic apoptosis discoveries to advanced selective BCL2 family inhibitors. Nat. Rev. Drug Discov. 2017, 16, 273–284. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).