Abstract
Fungal microbes are important in the creation of new drugs, given their unique genetic and metabolic diversity. As one of the most commonly found fungi in nature, Fusarium spp. has been well regarded as a prolific source of secondary metabolites (SMs) with diverse chemical structures and a broad spectrum of biological properties. However, little information is available concerning their derived SMs with antimicrobial effects. By extensive literature search and data analysis, as many as 185 antimicrobial natural products as SMs had been discovered from Fusarium strains by the end of 2022. This review first provides a comprehensive analysis of these substances in terms of various antimicrobial effects, including antibacterial, antifungal, antiviral, and antiparasitic. Future prospects for the efficient discovery of new bioactive SMs from Fusarium strains are also proposed.
1. Introduction
Antimicrobial agents play a significant role in the treatment of infectious diseases caused by pathogenic microorganisms with various modes of action. Since the fortuitous discovery of penicillin in 1928, hundreds of antibiotics have been approved for clinical use. However, some of these drugs have become less efficacy or unavailability simultaneously owing to the development of antimicrobial resistance (AMR), in which a pathogenic microbe evolves a survival mechanism that protects the drug target by modification or replacement, or degradation or modification of the antibiotic to render it harmless, such as MRSA (methicillin-resistant Staphylococcus aureus), multidrug-resistant S. aureus (MDRS), VREF (vancomycin-resistant Enterococcus faecium), CRKP (cephalosporin-resistant Klebsiella pneumoniae) [1]. Antimicrobial resistance has become an increasing threat to human health and is widely considered to be the next global pandemic [2]. Therefore, it is an urgent need for the discovery of new antimicrobial drugs with novel structural scaffolds and new modes of action.
Microorganisms are well recognized as a prolific source of biomolecules with diverse chemical structures and various biological properties. Microbial natural products have been, to date, our most successful defense against infectious disease. As one of the most commonly isolated filamentous fungi in terrestrial and marine environments, Fusarium spp. possess the potential capability to biosynthesize structurally diverse secondary metabolites (SMs), including alkaloids, peptides, amides, terpenoids, quinones, pyranones, and miscellaneous compounds [3]. Up to now, however, no document highlighting Fusarium-derived SMs with antimicrobial effects has been reported. With the aim to enrich our knowledge, this review comprehensively summarizes the occurrence of these antimicrobial substances, including antibacterials, antifungals, antivirals, and antiparasitics.
As of December 2022, the Dictionary of Natural Products (DNP) database listed 783 Fusarium-derived SMs, many of them also occurring in other microbial genera. By extensive literature search, as many as 185 antimicrobial SMs (1–185) had been discovered from Fusarium strains and are, respectively, introduced in terms of various antimicrobial activities, including antibacterial, antifungal, antiviral, and antiparasitic. Their detailed information is supplied in the Supplementary Materials.
2. Antibacterial Secondary Metabolites
Bacterial infection is a common clinical disease that can affect a variety of organs and tissues. Fusarium-derived antibacterial SMs have a wide array of structural motifs, most of which are polyketides, followed by alkaloids, terpenoids, and cyclopeptides. According to antibacterial properties, these chemicals are divided into three groups, including anti-Gram-positive bacterial SMs (1–50, Figure 1), anti-Gram-negative bacterial SMs (51–64, Figure 2) and both anti-Gram-positive and anti-Gram-negative bacterial SMs (65–81, Figure 3).
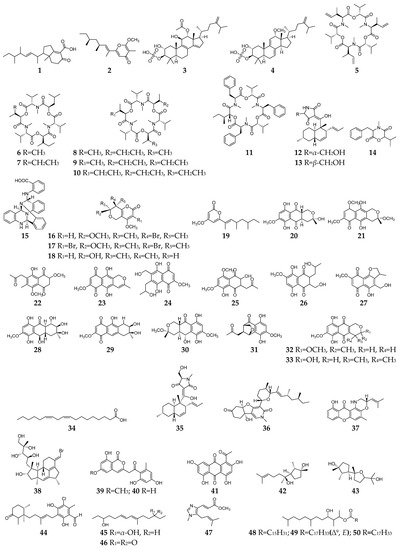
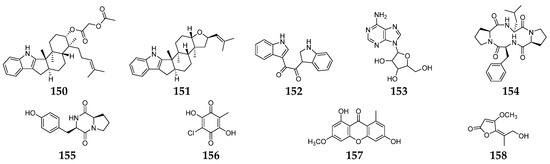
Figure 1.
Fusarium-derived anti-Gram-positive bacterial SMs (1–50).
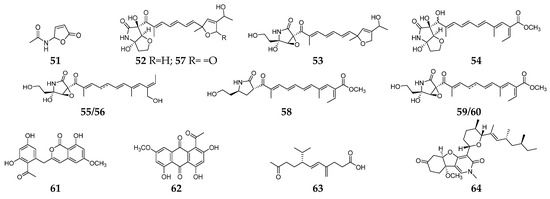
Figure 2.
Fusarium-derived anti-Gram-negative bacterial SMs (51–64).
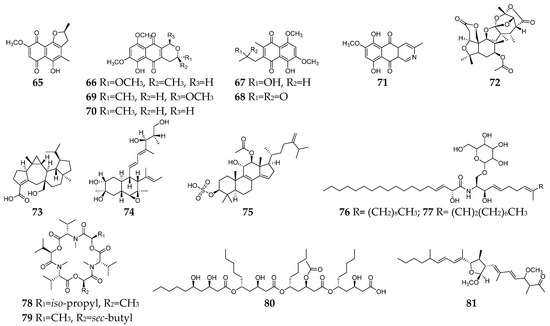
Figure 3.
Fusarium-derived anti-Gram-positive and anti-Gram-negative bacterial SMs (65–81).
2.1. Anti-Gram-Positive Bacterial SMs
Fifty Fusarium-derived SMs (1–50, Figure 1) had been characterized and displayed various bactericidal effects on Gram-positive strains, such as Staphylococcus aureus, methicillin-resistant Staphylococcus aureus, multidrug-resistant S. aureus, Mycobacterium tuberculosis, Bacillus subtilis, etc. Fusariumins C (1) and D (2) are two new polyketides produced by an endophytic strain F. oxysporum ZZP-R1 from coastal plant Rumex midair Makino displayed medium effect on S. aureus with MIC (minimum inhibitory concentration) values of 6.25 and 25.0 μM, respectively [4]. Two triterpene sulfates (3 and 4) isolated from F. compactum exhibited weak activity toward S. aureus and Streptococcus strains in the range of 6–50 µg/mL [5]. Enniatins (5–10), a group of antibiotics commonly synthesized by various Fusarium strains, are six-membered cyclic depsipeptides formed by the union of three molecules of D-α-hydroxyisovaleric acid and three N-methyl-L-amino acids [6]. Three enniatins (8–10), beauvericin A (11) and trichosetin (12) were obtained from an endophytic fungus, Fusarium sp. TP-G1 and showed moderate anti-S. aureus and anti-methicillin-resistant S. aureus effects with MIC values in the range of 2–16 µg/mL [7]. Two enantiomers (12 and 13) were separated from the culture broth of F. oxysporum FKI-4553 and found to have an inhibitory effect on the undecaprenyl pyrophosphate synthase activity of S. aureus with IC50 values of 83 and 30 µM, respectively [8].
Lateritin (14) derived from Fusarium sp. 2TnP1–2 showed anti-S. aureus activity at 2 µg per disc with 7 mm of inhibition zone [9]. A new polycyclic quinazoline alkaloid (15) displayed moderate antibacterial activity against methicillin-resistant S. aureus and multidrug-resistant S. aureus, with the same MIC value of 6.25 µg/mL [10]. Three pyranopyranones (16–18) showed weak inhibitory activities against S. aureus, methicillin-resistant S. aureus, and multidrug-resistant S. aureus [11]. Compound 19 was a new pyran-2-one with weak activity against methicillin-resistant S. aureus and was shown to be the inhibitor of the quorum-sensing mechanism of S. aureus and Pseudomonas aeruginosa [12]. Trans-dihydrofusarubin (20) and seven analogs (21–27) had significant antibiotic activity against S. aureus (MIC values < 4 µg/mL), and compounds 26 and 27 exhibited potent activity against S. pyogenes [13]. Five naphthoquinones 28–32 showed anti-Mycobacterium tuberculosis activity with MICs ranging from 25 to 50 µg/mL [14]. Compounds 32 and 33 displayed moderate antibacterial activity against S. aureus and potent activities against B. cereus and S. pyogenes with MIC values of <1 µg/mL as compared to ciprofloxacin, whose MIC value was 0.15 and 10 µg/mL, respectively [15].
Linoleic acid (34) and epi-equisetin (35) had certain inhibitory activity against S. aureus and multidrug-resistant S. aureus [16]. (−)-4,6′-anhydrooxysporidinone (36) was obtained from F. oxysporum and showed weak anti-multidrug-resistant S. aureus and moderate anti-B. subtilis effects [17]. Fusaroxazin (37), a novel antimicrobial xanthone derivative from F. oxysporum, possessed significant antibacterial activity towards S. aureus and B. cereus, with MIC values of 5.3 and 3.7 µg/mL, respectively [18]. Neomangicol B (38) isolated from the mycelial extract of a marine Fusarium strain was found to inhibit B. subtilis growth with a potency similar to that of the antibiotic gentamycin [19]. Three aromatic polyketides (39–41) were produced by strain F. proliferatum ZS07 and possessed potent antibacterial activity against B. subtilis with the same MIC values of 6.25 µg/mL [20]. Two sesterterpenes (42 and 43) produced by F. avenaceum SF-1502 displayed stronger antibacterial activity against B. megaterium than positive controls (ampicillin, erythromycin, and streptomycin) [21]. 4,5-Dihydroascochlorin (44) had strong antibacterial activity towards Bacillus megaterium [22]. Fusariumnols A (45) and B (46) were two novel anti-S. epidermidis aliphatic unsaturated alcohols isolated from F. proliferatum 13,294 [23]. Fungerin (47) displayed weak antibacterial activity against S. aureus and S. pneumoniae [24]. Compounds 48–50 were purified from F. oxysporum YP9B and showed a potent inhibitory effect on S. aureus, E.faecalis, S. mutans, B. cereus, and M. smegmatis with MICs of less than 4.5 µg/mL [25].
2.2. Anti-Gram-Negative Bacterial SMs
Butenolide (51) was a fusarium mycotoxin from unknown origin strain Fusaium sp. and showed selective inhibitory activity against E. coli [26]. Extensive chemical investigation of the endophytic fungus F. solani JK10 afforded nine 2-pyrrolidone derivatives (52–60), which displayed antibacterial activity against E. coli with MIC values of 5–10 µg/mL. Particularly, three lucilactaene analogs (52–54) had strong inhibitory effects on Acinetobacter sp., comparable to the positive control streptomycin [27]. One new aromatic polyketide, karimunones B (61), together with compounds 62 and 63, was obtained from sponge-associated Fusarium sp. KJMT.FP.4.3 and exhibited anti-multidrug resistant Salmonella enterica ser. Typhi activity with a MIC of 125 µg/mL [28]. Fusapyridon A (64) is produced by an endophytic strain, Fusarium sp. YG-45 demonstrated moderate antibacterial activity against Pseudomonas aeruginosa with a MIC value of 6.25 µg/mL [29].
2.3. Both Anti-Gram-Positive and Anti-Gram-Negative Bacterial SMs
Seventeen Fusarium-derived SMs (65–81, Figure 3) were shown to have both anti-Gram-positive and anti-Gram-negative activity. Seven naphthoquinones (65–71) demonstrated moderate activities against an array of Gram-positive and Gram-negative bacteria, such as B. megaterium, B. subtilis, C. perfringens, E. coli, methicillin-resistant S. aureus, P. aeruginosa, S. aureus, and S. pyogenes [13,21,30,31]. The mechanism of action (MoA) study indicated that compounds 66 and 71 could stimulate the oxygen consumption of bacterial cells and induce cyanide-insensitive oxygen consumption, which results in the generation of superoxide anion and hydrogen peroxide [32]. Compounds 72–75 were polycyclic terpenoids, respectively, produced by three Fusarium strains [33,34,35]. Compound 72 had significant activity against S. aureus and P. aeruginosa with a MIC value of 6.3 µg/mL, and 73 showed moderate activities against Salmonella enteritidis and Micrococcus luteus with MIC values of 6.3 and 25.2 µg/mL, respectively, while 74 showed a broad spectrum of antibacterial activity and 75 exhibited moderate antibacterial activities against S. aureus and E. coli with the same MIC value of 16 µg/mL. Two xanthine oxidase inhibitory cerebrosides (76 and 77) were identified and purified from the culture broth of Fusarium sp. IFB-121 and showed strong antibacterial activities against B. subtilis, E. coli, and P. fluorescens with MICs of less than 7.8 µg/mL [36]. Enniatins J1 (78) and J3 (79) were two hexadepsipeptides with an array of antibacterial activity toward C. perfringens, E. faecium, E. coli, S. dysenteriae, S. aureus, Y. enterocolitica, and lactic acid bacteria except for B. adolescentis [37]. Halymecin A (80) was produced by a marine-derived Fusarium sp. FE-71-1 and exhibited a moderate inhibitory effect on E. faecium, K. pneumoniae, and P. vulgaris with the MIC value of 10 µg/mL [38]. Fusaequisin A (81) was isolated from rice cultures of F. equiseti SF-3-17 and found to have moderate antimicrobial activity against S. aureus NBRC 13,276 and P. aeruginosa ATCC 15,442 [39].
3. Antifungal Secondary Metabolites
Invasive fungal infections are very common in immunocompromised patients (such as acquired immune deficiency syndrome and organ transplantation) and have become a global problem resulting in 1.7 million deaths every year [40,41,42]. Furthermore, the overuse of antifungal agents increases opportunistic pathogen resistance, which had been listed as one of the dominant threats by the World Health Organization in 2019. Therefore, the urgent need for new antimycotics with novel targets is undeniable. Till the end of 2022, twenty-seven antifungal SMs (82–108, Figure 4) had been discovered from Fusarium strains. Compounds 82–84 are three anti-C. albicans glycosides belong to the papulacandin class [43,44]. The MoA study suggested that compound 82 is an inhibitor of glutamine synthetase (GS) enzyme for (l,3)-β-glucan biosynthesis [43]. CR377 (85) was a new α-furanone derivative from an endophytic Fusarium sp. CR377 and showed a similar antifungal effect on C. albicans with nystatin [45]. Compounds 86 and 87 were two zearalenone analogs and exhibited weak activity against Cryptococcus neoformans [46]. Neofusapyrone (88) produced by a marine-derived Fusarium sp. FH-146 displayed moderate activity against A. clavatus F318a with a MIC value of 6.25 µg/mL [47]. Six cyclic depsipeptides 89–94 had been isolated from several Fusarium strains and found to have significant inhibitory activities against pathogenic fungi, such as C. albicans [48], C. glabrata, C. krusei, V. ceratosperma, and A. fumigates [49]. Cyclosporin A (91) has long been recognized as an immunosuppressant agent and could inhibit the growth of sensitive fungi after their germination [50,51]. Parnafungins A-D (95–98) were isoxazolidinone-containing natural products and demonstrated broad-spectrum antifungal activity with no observed activity against bacteria. The targeted pathway of these alkaloids was determined to be the mRNA 3`-cleavage and polyadenylation process [52,53]. One N-hydroxypyridine derivative (99) showed antifungal activity against C. albicans and Penicillium chrysogenum with MICs of 16 and 8 µg/mL, respectively [54]. Indole acetic acid (100) exhibited activity against the fluconazole-resistant C. albicans (MIC = 125 µg/mL) [55].
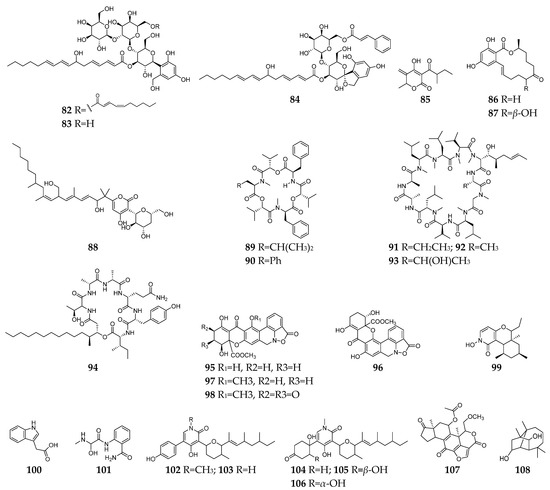
Figure 4.
Fusarium-derived antifungal SMs (82–108).
Fusaribenzamide A (101) possessed a significant anti-C. albicans activity with MIC of 11.9 µg/disc compared to nystatin (MIC = 4.9 µg/disc) [56]. Three pyridone derivatives (102–104) displayed significant activities against multidrug-sensitive S. cerevisiae 12geneΔ0HSR-iERG6, and the MoA study indicated that these substances have a potent inhibitory effect on NADH-cytochrome C oxidoreductase [57]. Compounds 105–107 were derived from strain F. oxysporum N17B, and the former (105 and 106) showed selective fungistatic activity against Aspergillus fumigatus, and the latter (107) had selective potent activity against C. albicans through inhibition of phosphatidylinositol 3-kinase [58]. Culmorin (108) displayed remarkable antifungal activity against both marine (S. marina, M. pelagica) and medically relevant fungi (A. fumigatus, A. niger, C. albicans, T. mentagrophytes) [59,60].
4. Both Antibacterial and Antifungal Secondary Metabolites
Till the end of 2022, forty-one SMs (109–149, Figure 5) with both antibacterial and antifungal effects had been discovered from Fusarium spp. Among these Fusarium-derived 1,4-naphthoquinone analogs (109–115), compound 109 showed potent anti-Gram-positive bacteria activity against B. cereus and S. pyogenes with MIC of <1 µg/mL and anti-C. albicans activity with IC50 (the half maximal inhibitory concentration) of 6.16 µg/mL [14], and 110–115 demonstrated moderate inhibitory effects on S. aureus, C. albicans, and B. subtilis [61]. Bikaverin (116) was found to have anti-E. coli and antifungal (P. notatum, Alternaria humicola, and A. flavus) activity [48,62,63]. Lateropyrone (117) was the same SM as F. acuminatum, F. lateritium, and F. tricinctum and displayed good antibacterial activity against B. subtilis, S. aureus, S. pneumoniae, methicillin-resistant S. aureus, Mycobacterium tuberculosis, and vancomycin-resistant of E. faecalis and significant inhibitory activity towards the growth of C. albicans [64,65,66,67]. BE-29,602 (118) was a novel antibiotic of the papulacandin family, showing good activity against C. albicans, S. cerevisiae, S. pombe with MIC values < 1 µg/mL and moderate activity against B. subtilis and P. chrysogenum with the MIC values < 8 µg/mL [44,68]. Fusarielin A (119) was a meroterpenoid with moderate antifungal activities against A. fumigatus and F. nivale and weak antibacterial effect on S. aureus, methicillin-resistant S. aureus, and multidrug-resistant S. aureus [11,69]. Three helvolic acid derivatives (120–122) displayed potent antifungal and antibacterial activities against B. subtilis, S. aureus, E. coli, B. cinerea, F. Graminearum, and P. capsica [70]. Fusartricin (123) had moderate antimicrobial activity against E. aerogenes, M. tetragenu, and C. albicans with the same MIC value of 19 µM [34].
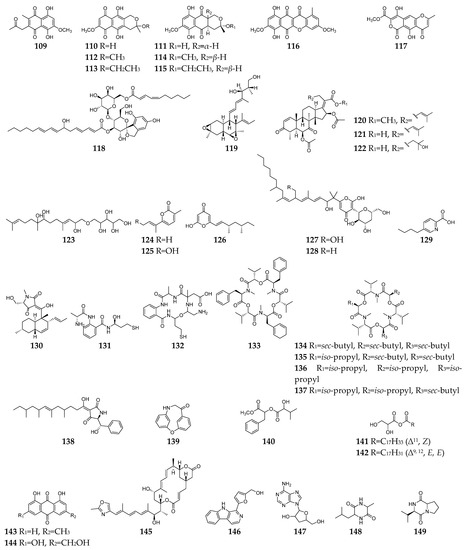
Figure 5.
Fusarium-derived antibacterial and antifungal SMs (109–149).
Compounds 124–128 are pyrone family members and showed antimicrobial activity against bacteria (such as B. subtilis, S. aureus, Vibrio parahaemolyticus, C. kefyr, and P. aeruginosa) and fungi (such as A. clavatus, Geotrichum candidum, C. albicans, M. albican, and S. cerevisiae) [47,71,72,73,74]. Fusaric acid (129), one of the most significant mycotoxins from Fusarium strains, displayed a broad spectrum of moderate antimicrobial activity against Bacillus species, Acinetobacter baumannii, Phytophthora infestans, etc. [75,76,77]. Equisetin (130) was shown to be active against several strains of Gram-positive bacteria (B. subtilis, Mycobacterium phlei, S. aureus, methicillin-resistant S. aureus, and S. erythraea) and the Gram-negative bacteria Neisseria perflava at concentrations of 0.5–4.0 µg/mL, as well as antifungal activity toward P. syringae and R. cerealis [78,79]. Fusarithioamides A (131) and B (132) demonstrated antibacterial potential towards B. cereus, S. aureus, and E. coli compared to ciprofloxacin and selective antifungal activity towards C. albicans compared to clotrimazole [80,81]. Beauvericin (133) and enniatins A, A1, B and B1 (134–137) are cyclic hexadepsipeptides with a wide array of highly antimicrobial activities against bacteria (such as B. subtilis, S. aureus, methicillin-resistant S. aureus, etc.) and fungi (such as C. albicans, B. bassiana, T. harzianum, etc.) [82,83,84,85,86]. Unlike most antibiotics, cell organelles or enzyme systems are the targets of the antibiotic 133 [87]. As a drug efflux pump modulator, furthermore, compound 133 had the capability to reverse the multi-drug resistant phenotype of C. albicans by blocking the ATP-binding cassette transporters and to repress the expression of many filament-specific genes, including the transcription factor BRG1, global regulator TORC1 kinase [88]. Fusaramin (138) displayed anti-Gram-positive and anti-Gram-negative bacterial activity and could inhibit the growth of S. cerevisiae 12geneΔ0HSR-iERG6 [57]. Compounds 139–142 were isolated from F. oxysporum YP9B and exhibited a significant antimicrobial effect against bacterial and fungi at concentrations of 0.8–6.3 µg/mL [25]. Seven SMs (143–149) were separated from an endophytic fungus F. equiseti, and showed antibacterial (such as B. subtilis, S. aureus, B. megaterium) and anti-C. albicans activities [89].
6. Antiparasitic Secondary Metabolites
Parasitic diseases caused by protozoa, helminths and ectoparasites affect millions of people each year and result in substantial morbidity and mortality, particularly in tropical regions [95]. Therefore, new antiparasitic agents are urgently needed to treat and control these diseases. A total of 39 antiparasitic SMs (23, 28, 29, 59, 108, 93, 116, 133–137, 159–185, Figure 7) had been isolated and characterized from Fusarium strains. Five naphthoquinones (23, 29, 30, 109, and 159) and one anthraquinone (160) showed weak inhibitory activity toward the most deadly malaria parasite Plasmodium falciparum K1 with IC50 values in the range 9.8–26.1 µM [96]. However, compound 93 displayed significant antiplasmodial activity toward P. falciparum (D6 clone) with an IC50 value of 0.34 µM [49]. Bikaverin (116) was specifically effective against Leishmania brasiliensis, which is one of the main causes of cutaneous leishmaniasis in the Americas [97]. Beauvericin (133) was reported to inhibit Trypanosoma cruzi with an IC50 value of 2.43 μM and L. braziliensis with an EC50 value of 1.86 μM [98,99]. In addition to antibacterial and antifungal effects, enniatins (134–137) exhibited mild anti-leishmanial activity by inhibition of the activity of thioredoxin reductase enzyme of P. falciparum [6]. Integracides F, G, H, and J (161–164) were also shown to have stronger anti-leishmanial activity towards L. donovani than the positive control pentamidine (IC50 = 6.35 µM) [100]. Among twelve lucilactaene derivatives (165–176), compounds 166–168 showed very potent antimalarial activity toward P. falciparum (IC50 = 0.0015, 0.15, and 0.68 μM, respectively) [101,102,103]. Structure−activity relationship study suggested that epoxide is extremely detrimental, and demethylation of the lucilactaene methyl ester and formation of the free carboxylic acid group resulted in a 300-fold decrease in activity. Nine cyclic tetrapeptides (177–185) are apicomplexan histone deacetylase (HDA) inhibitors [104,105,106]. Particularly, compound 177 was an excellent inhibitory agent (IC50 < 2 nM) and showed in vivo high efficacy against P. berghei malaria in mice at less than 10 mg/kg.
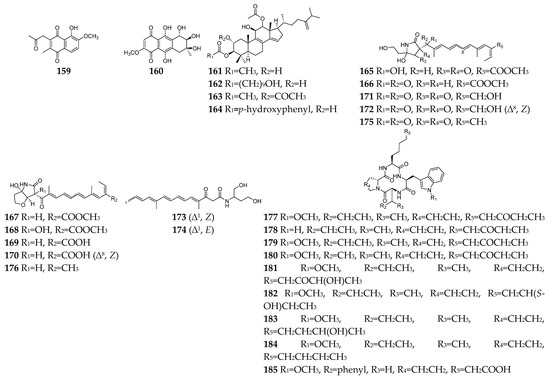
Figure 7.
Fusarium-derived antiparasitic SMs (159–185).
7. Conclusions
In summary, the genus Fusarium is one of the excellent producers of antimicrobial SMs, some of which have great potential in new drug development, such as anti-Gram-positive bacterial terpenes 38, 42 and 43, anti-Gram-negative lucilactaenes 52–54, antifungal papulacandin 82 and pyridones 102–104, antiviral enniatins 135–137, and antiparasitic integracides 161–164, etc. In the past two decades, however, the rate of discovery of novel SMs from Fusarium has constantly been decreasing [3]. Fortunately, a growing number of evidence suggest that the potential of Fusarium spp. to make novel SMs is still immense since most of their SM biosynthetic gene clusters (BGCs) are inactive or un-awakened under traditional fermentation and culture conditions [107]. More and more cryptic BGCs responsible for the biosynthesis of novel SMs have been disclosed by various bio-informative tools and approaches and efficiently activated using genome mining strategies, such as BGC heterogeneous expression [108], promoter engineering [109] and gene transcriptional regulation [110]. In addition, more efforts should be made to analyze and interpret the action mechanisms of Fusarium-derived leading compounds, which have similar or more potent antimicrobial effects compared to positive controls.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/molecules28083424/s1, Table S1: Detail information for Fusarium-derived anti-Gram-positive bacterial SMs; Table S2: Detail information for Fusarium-derived anti-Gram-negative bacterial SMs; Table S3: Detail information for Fusarium-derived both anti-Gram-positive and anti-Gram-negative bacterial SMs; Table S4: Detail information for Fusarium-derived antifungal SMs; Table S5: Detail information for Fusarium-derived both antibacterial and antifungal SMs; Table S6: Detail information for Fusarium-derived antiviral SMs; Table S7: Detail information for Fusarium-derived antiparasitic SMs.
Author Contributions
Conceptualization, Funding acquisition and Project administration, H.Z.; Writing—original draft, M.X., Z.H., W.Z. and Y.L.; Writing—review & editing, X.B. and H.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This work was co-financially supported by the National Key Research and Development Program of China (2022YFC2804203 and 2018YFC0311004) and the National Natural Science Foundation of China (41776139).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available in the Supplementary Material.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Denissen, J.; Reyneke, B.; Waso-Reyneke, M.; Havenga, B.; Barnard, T.; Khan, S.; Khan, W. Prevalence of ESKAPE pathogens in the environment: Antibiotic resistance status, community-acquired infection and risk to human health. Int. J. Hyg. Environ. Health 2022, 244, 114006. [Google Scholar] [CrossRef] [PubMed]
- Nadimpalli, M.L.; Chan, C.W.; Doron, S. Antibiotic resistance: A call to action to prevent the next epidemic of inequality. Nat. Med. 2021, 27, 187–188. [Google Scholar] [CrossRef]
- Li, M.; Yu, R.; Bai, X.; Wang, H.; Zhang, H. Fusarium: A treasure trove of bioactive secondary metabolites. Nat. Prod. Rep. 2020, 37, 1568–1588. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Bai, X.; Hua, Y.; Zhang, H.; Wang, H. Fusariumins C and D, two novel antimicrobial agents from Fusarium oxysporum ZZP-R1 symbiotic on Rumex madaio Makino. Fitoterapia 2019, 134, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Brill, G.M.; Kati, W.M.; Montgomery, D.; Karwowski, J.P.; Humphrey, P.E.; Jackson, M.; Clement, J.J.; Kadam, S.; Chen, R.H.; McAlpine, J.B. Novel triterpene sulfates from Fusarium compactum using a rhinovirus 3C protease inhibitor screen. J. Antibiot. 1996, 49, 541–546. [Google Scholar] [CrossRef]
- Zaher, A.M.; Makboul, M.A.; Moharram, A.M.; Tekwani, B.L.; Calderon, A.I. A new enniatin antibiotic from the endophyte Fusarium tricinctum Corda. J. Antibiot. 2015, 68, 197–200. [Google Scholar] [CrossRef]
- Shi, S.; Li, Y.; Ming, Y.; Li, C.; Li, Z.; Chen, J.; Luo, M. Biological activity and chemical composition of the endophytic fungus Fusarium sp. TP-G1 obtained from the root of Dendrobium officinale Kimura et Migo. Rec. Nat. Prod. 2018, 12, 549–556. [Google Scholar] [CrossRef]
- Inokoshi, J.; Shigeta, N.; Fukuda, T.; Uchida, R.; Nonaka, K.; Masuma, R.; Tomoda, H. Epi-trichosetin, a new undecaprenyl pyrophosphate synthase inhibitor, produced by Fusarium oxysporum FKI-4553. J. Antibiot. 2013, 66, 549–554. [Google Scholar] [CrossRef]
- Du, Z.; Song, C.; Yu, B.; Luo, X. Secondary metabolites produced by Fusarium sp. 2TnP1-2, an endophytic fungus from Trewia nudiflora. Chin. J. Med. Chem. 2008, 18, 452–456. [Google Scholar]
- Nenkep, V.; Yun, K.; Son, B.W. Oxysporizoline, an antibacterial polycyclic quinazoline alkaloid from the marine-mudflat-derived fungus Fusarium oxysporum. J. Antibiot. 2016, 69, 709–711. [Google Scholar] [CrossRef]
- Nenkep, V.; Yun, K.; Zhang, D.; Choi, H.D.; Kang, J.S.; Son, B.W. Induced production of bromomethylchlamydosporols A and B from the marine-derived fungus Fusarium tricinctum. J. Nat. Prod. 2010, 73, 2061–2063. [Google Scholar] [CrossRef]
- Alfattani, A.; Marcourt, L.; Hofstetter, V.; Queiroz, E.F.; Leoni, S.; Allard, P.M.; Gindro, K.; Stien, D.; Perron, K.; Wolfender, J.L. Combination of pseudo-LC-NMR and HRMS/MS-based molecular networking for the rapid identification of antimicrobial metabolites from Fusarium petroliphilum. Front. Mol. Biosci. 2021, 8, 725691. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.A.; Tatum, J.H.; Nemec, S., Jr. Antimicrobial activity of naphthoquinones from Fusaria. Mycopathologia 1990, 111, 9–15. [Google Scholar] [CrossRef]
- Kornsakulkarn, J.; Dolsophon, K.; Boonyuen, N.; Boonruangprapa, T.; Rachtawee, P.; Prabpai, S.; Kongsaeree, P.; Thongpanchang, C. Dihydronaphthalenones from endophytic fungus Fusarium sp. BCC14842. Tetrahedron 2011, 67, 7540–7547. [Google Scholar] [CrossRef]
- Shah, A.; Rather, M.A.; Hassan, Q.P.; Aga, M.A.; Mushtaq, S.; Shah, A.M.; Hussain, A.; Baba, S.A.; Ahmad, Z. Discovery of anti-microbial and anti-tubercular molecules from Fusarium solani: An endophyte of Glycyrrhiza glabra. J. Appl. Microbiol. 2017, 122, 1168–1176. [Google Scholar] [CrossRef]
- Chen, C.; Luo, X.; Li, K.; Guo, C.; Li, J.; Lin, X. Antibacterial secondary metabolites from a marine sponge-derived fungus Fusarium equiseti SCSIO 41019. Chin. J. Antibiot. 2019, 44, 1035–1040. [Google Scholar] [CrossRef]
- Wang, Q.X.; Li, S.F.; Zhao, F.; Dai, H.Q.; Bao, L.; Ding, R.; Gao, H.; Zhang, L.X.; Wen, H.A.; Liu, H.W. Chemical constituents from endophytic fungus Fusarium oxysporum. Fitoterapia 2011, 82, 777–781. [Google Scholar] [CrossRef]
- Mohamed, G.A.; Ibrahim, S.R.M.; Alhakamy, N.A.; Aljohani, O.S. Fusaroxazin, a novel cytotoxic and antimicrobial xanthone derivative from Fusarium oxysporum. Nat. Prod. Res. 2022, 36, 952–960. [Google Scholar] [CrossRef] [PubMed]
- Renner, M.K.; Jensen, P.R.; Fenical, W. Neomangicols: Structures and absolute stereochemistries of unprecedented halogenated sesterterpenes from a marine fungus of the genus Fusarium. J. Org. Chem. 1998, 63, 8346–8354. [Google Scholar] [CrossRef]
- Li, S.; Shao, M.-W.; Lu, Y.-H.; Kong, L.-C.; Jiang, D.-H.; Zhang, Y.-L. Phytotoxic and antibacterial metabolites from Fusarium proliferatum ZS07 Isolated from the gut of long-horned grasshoppers. J. Agric. Food Chem. 2014, 62, 8997–9001. [Google Scholar] [CrossRef]
- Jiang, C.X.; Li, J.; Zhang, J.M.; Jin, X.J.; Yu, B.; Fang, J.G.; Wu, Q.X. Isolation, identification, and activity evaluation of chemical constituents from soil fungus Fusarium avenaceum SF-1502 and endophytic fungus Fusarium proliferatum AF-04. J. Agric. Food Chem. 2019, 67, 1839–1846. [Google Scholar] [CrossRef] [PubMed]
- Hussain, H.; Drogies, K.-H.; Al-Harrasi, A.; Hassan, Z.; Shah, A.; Rana, U.A.; Green, I.R.; Draeger, S.; Schulz, B.; Krohn, K. Antimicrobial constituents from endophytic fungus Fusarium sp. Asian Pac. J. Trop. Dis. 2015, 5, 186–189. [Google Scholar] [CrossRef]
- Lu, W.; Zhu, G.; Yuan, W.; Han, Z.; Dai, H.; Basiony, M.; Zhang, L.; Liu, X.; Hsiang, T.; Zhang, J. Two novel aliphatic unsaturated alcohols isolated from a pathogenic fungus Fusarium proliferatum. Synth. Syst. Biotechnol. 2021, 6, 446–451. [Google Scholar] [CrossRef] [PubMed]
- Wen, H.; Li, Y.; Liu, X.; Ye, W.; Yao, X.; Che, Y. Fusagerins A-F, new alkaloids from the fungus Fusarium sp. Nat. Prod. Bioprospect. 2015, 5, 195–203. [Google Scholar] [CrossRef]
- Kılıç, G.; Tosun, G.; Bozdeveci, A.; Erik, İ.; Öztürk, E.; Reis, R.; Sipahi, H.; Cora, M.; Karaoğlu, Ş.A.; Yaylı, N. Antimicrobial, cytotoxic, antiviral wffects, and apectroscopic characterization of metabolites produced by fusarium oxysporum YP9B. Rec. Nat. Prod. 2021, 15, 547–567. [Google Scholar] [CrossRef]
- Valla, A.; Giraud, M.; Labia, R.; Morand, A. In vitro inhibitory activity against bacteria of a fusarium mycotoxin and new synthetic derivatives. Bull. Soc. Chim. Fr. 1997, 6, 601–603. [Google Scholar] [CrossRef]
- Kyekyeku, J.O.; Kusari, S.; Adosraku, R.K.; Bullach, A.; Golz, C.; Strohmann, C.; Spiteller, M. Antibacterial secondary metabolites from an endophytic fungus, Fusarium solani JK10. Fitoterapia 2017, 119, 108–114. [Google Scholar] [CrossRef]
- Sibero, M.T.; Zhou, T.; Fukaya, K.; Urabe, D.; Radjasa, O.K.K.; Sabdono, A.; Trianto, A.; Igarashi, Y. Two new aromatic polyketides from a sponge-derived Fusarium. Beilstein. J. Org. Chem. 2019, 15, 2941–2947. [Google Scholar] [CrossRef]
- Tsuchinari, M.; Shimanuki, K.; Hiramatsu, F.; Murayama, T.; Koseki, T.; Shiono, Y. Fusapyridons A and B, novel pyridone alkaloids from an endophytic fungus, Fusarium sp. YG-45. Z. Naturforsch. B. 2007, 62, 1203–1207. [Google Scholar] [CrossRef]
- Supratman, U.; Hirai, N.; Sato, S.; Watanabe, K.; Malik, A.; Annas, S.; Harneti, D.; Maharani, R.; Koseki, T.; Shiono, Y. New naphthoquinone derivatives from Fusarium napiforme of a mangrove plant. Nat. Prod. Res. 2021, 35, 1406–1412. [Google Scholar] [CrossRef]
- Khan, N.; Afroz, F.; Begum, M.N.; Roy Rony, S.; Sharmin, S.; Moni, F.; Mahmood Hasan, C.; Shaha, K.; Sohrab, M.H. Endophytic Fusarium solani: A rich source of cytotoxic and antimicrobial napthaquinone and aza-anthraquinone derivatives. Toxicol. Rep. 2018, 5, 970–976. [Google Scholar] [CrossRef]
- Haraguchi, H.; Yokoyama, K.; Oike, S.; Ito, M.; Nozaki, H. Respiratory stimulation and generation of superoxide radicals in Pseudomonas aeruginosa by fungal naphthoquinones. Arch. Microbiol. 1997, 167, 6–10. [Google Scholar] [CrossRef]
- Yan, C.; Liu, W.; Li, J.; Deng, Y.; Chen, S.; Liu, H. Bioactive terpenoids from Santalum album derived endophytic fungus Fusarium sp. YD-2. RSC Adv. 2018, 8, 14823–14828. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Liu, D.; Wang, H.; Liu, T.; Xin, Z. Fusartricin, a sesquiterpenoid ether produced by an endophytic fungus Fusarium tricinctum Salicorn 19. Eur. Food Res. Technol. 2014, 240, 805–814. [Google Scholar] [CrossRef]
- Dong, J.W.; Cai, L.; Li, X.J.; Duan, R.T.; Shu, Y.; Chen, F.Y.; Wang, J.P.; Zhou, H.; Ding, Z.T. Production of a new tetracyclic triterpene sulfate metabolite sambacide by solid-state cultivated Fusarium sambucinum B10.2 using potato as substrate. Bioresour. Technol. 2016, 218, 1266–1270. [Google Scholar] [CrossRef] [PubMed]
- Shu, R.; Wang, F.; Yang, Y.; Liu, Y.; Tan, R. Antibacterial and xanthine oxidase inhibitory cerebrosides from Fusarium sp. IFB-121, and endophytic fungus in Quercus variabilis. Lipids 2004, 39, 667–673. [Google Scholar] [CrossRef]
- Sebastià, N.; Meca, G.; Soriano, J.M.; Mañes, J. Antibacterial effects of enniatins J(1) and J(3) on pathogenic and lactic acid bacteria. Food Chem. Toxicol. 2011, 49, 2710–2717. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Imamura, N.; Nishijima, M.; Adachi, K.; Sakai, M.; Sano, H. Halymecins, new antimicroalgal substances produced by fungi isolated from marine algae. J. Antibiot. 1996, 49, 998–1005. [Google Scholar] [CrossRef]
- Shiono, Y.; Shibuya, F.; Murayama, T.; Koseki, T.; Poumale, H.M.P.; Ngadjui, B.T. A polyketide metabolite from an endophytic Fusarium equiseti in a medicinal plant. Z. Naturforsch. B. 2013, 68, 289–292. [Google Scholar] [CrossRef]
- Ivanov, M.; Ćirić, A.; Stojković, D. Emerging antifungal targets and strategies. Int. J. Mol. Sci. 2022, 23, 2756. [Google Scholar] [CrossRef]
- Van Daele, R.; Spriet, I.; Wauters, J.; Maertens, J.; Mercier, T.; Van Hecke, S.; Brüggemann, R. Antifungal drugs: What brings the future? Med. Mycol. 2019, 57, S328–S343. [Google Scholar] [CrossRef]
- Campoy, S.; Adrio, J.L. Antifungals. Biochem. Pharmacol. 2017, 133, 86–96. [Google Scholar] [CrossRef] [PubMed]
- Jackson, M.; Frost, D.J.; Karwowski, J.P.; Humphrey, P.E.; Dahod, S.K.; Choi, W.S.; Brandt, K.; Malmberg, L.-H.; Rasmussen, R.R.; Scherr, M.H. Fusacandins A and B; Novel Antifungal Antibiotics of the Papulacandin Class from Fusarium sambucinum I. Identity of the Producing Organism, Fermentation and Biological Activity. J. Antibiot. 1995, 48, 608–613. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.H.; Tennant, S.; Frost, D.; O’Beirne, M.J.; Karwowski, J.P.; Humphrey, P.E.; Malmberg, L.-H.; Choi, W.; Brandt, K.D.; West, P. Discovery of saricandin, a novel papulacandin, from a Fusarium species. J. Antibiot. 1996, 49, 596–598. [Google Scholar] [CrossRef]
- Brady, S.F.; Clardy, J. CR377, a new pentaketide antifungal agent isolated from an endophytic fungus. J. Nat. Prod. 2000, 63, 1447–1448. [Google Scholar] [CrossRef]
- Saetang, P.; Rukachaisirikul, V.; Phongpaichit, S.; Sakayaroj, J.; Shi, X.; Chen, J.; Shen, X. β-Resorcylic macrolide and octahydronaphthalene derivatives from a seagrass-derived fungus Fusarium sp. PSU-ES123. Tetrahedron 2016, 72, 6421–6427. [Google Scholar] [CrossRef]
- Hiramatsu, F.; Miyajima, T.; Murayama, T.; Takahashi, K.; Koseki, T.; Shiono, Y. Isolation and structure elucidation of neofusapyrone from a marine-derived Fusarium species, and structural revision of fusapyrone and deoxyfusapyrone. J. Antibiot. 2006, 59, 704–709. [Google Scholar] [CrossRef]
- Xu, X.; Zhao, S.; Yu, Y.; Chen, Z.; Shen, H.; Zhou, L. Beauvericin K, a new antifungal beauvericin analogue from a marine-derived Fusarium sp. Nat. Prod. Commun. 2016, 11, 1825–1826. [Google Scholar] [CrossRef]
- Ibrahim, S.R.M.; Abdallah, H.M.; Elkhayat, E.S.; Al Musayeib, N.M.; Asfour, H.Z.; Zayed, M.F.; Mohamed, G.A. Fusaripeptide A: New antifungal and anti-malarial cyclodepsipeptide from the endophytic fungus Fusarium sp. J. Asian Nat. Prod. Res. 2018, 20, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Dreyfuss, M.; Härri, E.; Hofmann, H.e.a.; Kobel, H.; Pache, W.; Tscherter, H. Cyclosporin A and C: New metabolites from Trichoderma polysporum (Link ex Pers.) Rifai. Appl. Microbiol. Biot. 1976, 3, 125–133. [Google Scholar] [CrossRef]
- Baráth, Z.; Baráthová, H.; Betina, V.; Nemec, P. Ramihyphins—Antifungal and morphogenic antibiotics from Fusarium sp. S-435. Folia. Microbiol. 1974, 19, 507–511. [Google Scholar] [CrossRef] [PubMed]
- Parish, C.A.; Smith, S.K.; Calati, K.; Zink, D.; Wilson, K.; Roemer, T.; Jiang, B.; Xu, D.; Bills, G.; Platas, G. Isolation and structure elucidation of parnafungins, antifungal natural products that inhibit mRNA polyadenylation. J. Am. Chem. Soc. 2008, 130, 7060–7066. [Google Scholar] [CrossRef] [PubMed]
- Overy, D.; Calati, K.; Kahn, J.N.; Hsu, M.J.; Martin, J.; Collado, J.; Roemer, T.; Harris, G.; Parish, C.A. Isolation and structure elucidation of parnafungins C and D, isoxazolidinone-containing antifungal natural products. Bioorg. Med. Chem. Lett. 2009, 19, 1224–1227. [Google Scholar] [CrossRef] [PubMed]
- McBrien, K.D.; Gao, Q.; Huang, S.; Klohr, S.E.; Wang, R.R.; Pirnik, D.M.; Neddermann, K.M.; Bursuker, I.; Kadow, K.F.; Leet, J.E. Fusaricide, a new cytotoxic N-hydroxypyridone from Fusarium sp. J. Nat. Prod. 1996, 59, 1151–1153. [Google Scholar] [CrossRef]
- Hilário, F.; Chapla, V.; Araujo, A.; Sano, P.; Bauab, T.; dos Santos, L. Antimicrobial Screening of Endophytic Fungi Isolated from the Aerial Parts of Paepalanthus chiquitensis (Eriocaulaceae) Led to the Isolation of Secondary Metabolites Produced by Fusarium fujikuroi. J. Braz. Chem. Soc. 2016, 28, 1389–1395. [Google Scholar] [CrossRef]
- Ibrahim, S.M.; Mohamed, G.; Khayat, M.; Al Haidari, R.; El-Kholy, A.; Zayed, M. A new antifungal aminobenzamide derivative from the endophytic fungus Fusarium sp. Pharmacogn. Mag. 2019, 15, 204–207. [Google Scholar] [CrossRef]
- Sakai, K.; Unten, Y.; Iwatsuki, M.; Matsuo, H.; Fukasawa, W.; Hirose, T.; Chinen, T.; Nonaka, K.; Nakashima, T.; Sunazuka, T.; et al. Fusaramin, an antimitochondrial compound produced by Fusarium sp., discovered using multidrug-sensitive Saccharomyces cerevisiae. J. Antibiot. 2019, 72, 645–652. [Google Scholar] [CrossRef]
- Woscholski, R.; Kodaki, T.; McKinnon, M.; Waterfield, M.D.; Parker, P.J. A comparison of demethoxyviridin and wortmannin as inhibitors of phosphatidylinositol 3-kinase. FEBS Lett. 1994, 342, 109–114. [Google Scholar] [CrossRef]
- Pedersen, P.B.; Miller, J.D. The fungal metabolite culmorin and related compounds. Nat. Toxins 1999, 7, 305–309. [Google Scholar] [CrossRef]
- Strongman, D.; Miller, J.; Calhoun, L.; Findlay, J.; Whitney, N. The biochemical basis for interference competition among some lignicolous marine fungi. Bot. Mar. 1987, 30, 21–26. [Google Scholar] [CrossRef]
- Kurobane, I.; Zaita, N.; Fukuda, A. New metabolites of Fusarium martii related to dihydrofusarubin. J. Antibiot. 1986, 39, 205–214. [Google Scholar] [CrossRef]
- Limón, M.C.; Rodríguez-Ortiz, R.; Avalos, J. Bikaverin production and applications. Appl. Microbiol. Biotechnol. 2010, 87, 21–29. [Google Scholar] [CrossRef]
- Deshmukh, R.; Mathew, A.; Purohit, H.J. Characterization of antibacterial activity of bikaverin from Fusarium sp. HKF15. J. Biosci. Bioeng. 2014, 117, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Bushnell, G.W.; Li, Y.-L.; Poulton, G.A. Pyrones. X. Lateropyrone, a new antibiotic from the fungus Fusarium lateritium Nees. Can. J. Chem. 1984, 62, 2101–2106. [Google Scholar] [CrossRef]
- Clark, T.N.; Carroll, M.; Ellsworth, K.; Guerrette, R.; Robichaud, G.A.; Johnson, J.A.; Gray, C.A. Antibiotic mycotoxins from an endophytic Fusarium acuminatum isolated from the medicinal plant Geum macrophyllum. Nat. Prod. Commun. 2018, 13, 1934578X1801301017. [Google Scholar] [CrossRef]
- Ariantari, N.P.; Frank, M.; Gao, Y.; Stuhldreier, F.; Kiffe-Delf, A.-L.; Hartmann, R.; Höfert, S.-P.; Janiak, C.; Wesselborg, S.; Müller, W.E.G.; et al. Fusaristatins D–F and (7S,8R)-(−)-chlamydospordiol from Fusarium sp. BZCB-CA, an endophyte of Bothriospermum chinense. Tetrahedron 2021, 85, 132065–132071. [Google Scholar] [CrossRef]
- Ola, A.R.B.; Thomy, D.; Lai, D.; Brötz-Oesterhelt, H.; Proksch, P. Inducing secondary metabolite production by the endophytic fungus Fusarium tricinctum through coculture with Bacillus subtilis. J. Nat. Prod. 2013, 76, 2094–2099. [Google Scholar] [CrossRef]
- Okada, H.; Nagashima, M.; Suzuki, H.; Nakajima, S.; Kojiri, K.; Suda, H. BE-29602, a new member of the papulacandin family. J. Antibiot. 1996, 49, 103–106. [Google Scholar] [CrossRef]
- Kobayashi, H.; Sunaga, R.; Furihata, K.; Morisaki, N.; IWasaki, S. Isolation and structures of an antifungal antibiotic, fusarielin A, and related compounds produced by a Fusarium sp. J. Antibiot. 1995, 48, 42–52. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.A.; Ma, Y.M.; Zhang, H.C.; Liu, R. A new helvolic acid derivative from an endophytic Fusarium sp. of Ficus carica. Nat. Prod. Res. 2016, 30, 2407–2412. [Google Scholar] [CrossRef] [PubMed]
- Janevska, S.; Arndt, B.; Niehaus, E.-M.; Burkhardt, I.; Rösler, S.M.; Brock, N.L.; Humpf, H.-U.; Dickschat, J.S.; Tudzynski, B. Gibepyrone biosynthesis in the rice pathogen Fusarium fujikuroi is facilitated by a small polyketide synthase gene cluster. J. Biol. Chem. 2016, 291, 27403–27420. [Google Scholar] [CrossRef]
- Zhou, G.; Qiao, L.; Zhang, X.; Sun, C.; Che, Q.; Zhang, G.; Zhu, T.; Gu, Q.; Li, D. Fusaricates H-K and fusolanones A-B from a mangrove endophytic fungus Fusarium solani HDN15-410. Phytochemistry 2019, 158, 13–19. [Google Scholar] [CrossRef]
- Evidente, A.; Conti, L.; Altomare, C.; Bottalico, A.; Sindona, G.; Segre, A.L.; Logrieco, A. Fusapyrone and deoxyfusapyrone, two antifungal α-pyrones from Fusarium semitectum. Nat. Toxins 1994, 2, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Altomare, C.; Perrone, G.; Zonno, M.C.; Evidente, A.; Pengue, R.; Fanti, F.; Polonelli, L. Biological characterization of fusapyrone and deoxyfusapyrone, two bioactive secondary metabolites of Fusarium semitectum. J. Nat. Prod. 2000, 63, 1131–1135. [Google Scholar] [CrossRef] [PubMed]
- Son, S.; Kim, H.; Choi, G.; Lim, H.; Jang, K.; Lee, S.; Lee, S.; Sung, N.; Kim, J.C. Bikaverin and fusaric acid from Fusarium oxysporum show antioomycete activity against Phytophthora infestans. J. Appl. Microbiol. 2008, 104, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Bacon, C.W.; Hinton, D.M.; Hinton, A., Jr. Growth-inhibiting effects of concentrations of fusaric acid on the growth of Bacillus mojavensis and other biocontrol Bacillus species. J. Appl. Microbiol. 2006, 100, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Poleto, L.; da Rosa, L.O.; Fontana, R.C.; Rodrigues, E.; Poletto, E.; Baldo, G.; Paesi, S.; Sales-Campos, C.; Camassola, M. Production of antimicrobial metabolites against pathogenic bacteria and yeasts by Fusarium oxysporum in submerged culture processes. Bioproc. Biosyst. Eng. 2021, 44, 1321–1332. [Google Scholar] [CrossRef] [PubMed]
- Vesonder, R.F.; Tjarks, L.W.; Rohwedder, W.K.; Burmeister, H.R.; Laugal, J.A. Equisetin, an antibiotic from Fusarium equisetin NRRL 5537, identified as a derivative of N-methyl-2, 4-pyrollidone. J. Antibiot. 1979, 32, 759–761. [Google Scholar] [CrossRef]
- Ratnaweera, P.B.; de Silva, E.D.; Williams, D.E.; Andersen, R.J. Antimicrobial activities of endophytic fungi obtained from the arid zone invasive plant Opuntia dillenii and the isolation of equisetin, from endophytic Fusarium sp. BMC Complement. Altern. Med. 2015, 15, 220. [Google Scholar] [CrossRef]
- Ibrahim, S.R.M.; Elkhayat, E.S.; Mohamed, G.A.A.; Fat’hi, S.M.; Ross, S.A. Fusarithioamide A, a new antimicrobial and cytotoxic benzamide derivative from the endophytic fungus Fusarium chlamydosporium. Biochem. Biophys. Res. Commun. 2016, 479, 211–216. [Google Scholar] [CrossRef]
- Ibrahim, S.R.M.; Mohamed, G.A.; Al Haidari, R.A.; Zayed, M.F.; El-Kholy, A.A.; Elkhayat, E.S.; Ross, S.A. Fusarithioamide B, a new benzamide derivative from the endophytic fungus Fusarium chlamydosporium with potent cytotoxic and antimicrobial activities. Bioorg. Med. Chem. 2018, 26, 786–790. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Barret, M.-O.; Boyd, K.G.; Adams, D.R.; Boyd, A.S.; Burgess, J.G. JM47, a cyclic tetrapeptide HC-toxin analogue from a marine Fusarium species. Phytochemistry 2002, 60, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Roig, M.; Meca, G.; Marin, R.; Ferrer, E.; Manes, J. Antibacterial activity of the emerging Fusarium mycotoxins enniatins A, A(1), A(2), B, B(1), and B(4) on probiotic microorganisms. Toxicon 2014, 85, 1–4. [Google Scholar] [CrossRef]
- Meca, G.; Sospedra, I.; Valero, M.A.; Manes, J.; Font, G.; Ruiz, M.J. Antibacterial activity of the enniatin B, produced by Fusarium tricinctum in liquid culture, and cytotoxic effects on Caco-2 cells. Toxicol. Mech. Method. 2011, 21, 503–512. [Google Scholar] [CrossRef]
- Meca, G.; Soriano, J.M.; Gaspari, A.; Ritieni, A.; Moretti, A.; Manes, J. Antifungal effects of the bioactive compounds enniatins A, A(1), B, B(1). Toxicon 2010, 56, 480–485. [Google Scholar] [CrossRef]
- Tsantrizos, Y.S.; Xu, X.-J.; Sauriol, F.; Hynes, R.C. Novel quinazolinones and enniatins from Fusarium lateritium Nees. Can. J. Chem. 1993, 71, 1362–1367. [Google Scholar] [CrossRef]
- Meca, G.; Sospedra, I.; Soriano, J.M.; Ritieni, A.; Moretti, A.; Manes, J. Antibacterial effect of the bioactive compound beauvericin produced by Fusarium proliferatum on solid medium of wheat. Toxicon 2010, 56, 349–354. [Google Scholar] [CrossRef]
- Wu, Q.; Patocka, J.; Nepovimova, E.; Kuca, K. A Review on the Synthesis and Bioactivity Aspects of Beauvericin, a Fusarium Mycotoxin. Front. Pharmacol. 2018, 9, 1338. [Google Scholar] [CrossRef]
- Hawas, U.W.; Al-Farawati, R.; Abou El-Kassem, L.T.; Turki, A.J. Different Culture Metabolites of the Red Sea Fungus Fusarium equiseti Optimize the Inhibition of Hepatitis C Virus NS3/4A Protease (HCV PR). Mar. Drugs 2016, 14, 190. [Google Scholar] [CrossRef]
- Tompa, D.R.; Immanuel, A.; Srikanth, S.; Kadhirvel, S. Trends and strategies to combat viral infections: A review on FDA approved antiviral drugs. Int. J. Biol. Macromol. 2021, 172, 524–541. [Google Scholar] [CrossRef]
- Chang, S.; Yan, B.; Chen, Y.; Zhao, W.; Gao, R.; Li, Y.; Yu, L.; Xie, Y.; Si, S.; Chen, M. Cytotoxic hexadepsipeptides and anti-coronaviral 4-hydroxy-2-pyridones from an endophytic Fusarium sp. Front. Chem. 2022, 10, 1106869. [Google Scholar] [CrossRef] [PubMed]
- McKee, T.C.; Bokesch, H.R.; McCormick, J.L.; Rashid, M.A.; Spielvogel, D.; Gustafson, K.R.; Alavanja, M.M.; Cardelline, J.H., 2nd; Boyd, M.R. Isolation and characterization of new anti-HIV and cytotoxic leads from plants, marine, and microbial organisms. J. Nat. Prod. 1997, 60, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.W.; Liu, X.J.; Yuan, J.; Li, H.J.; Mahmud, T.; Hong, M.J.; Yu, J.C.; Lan, W.J. l-Tryptophan induces a marine-derived Fusarium sp. to produce indole alkaloids with activity against the Zika virus. J. Nat. Prod. 2020, 83, 3372–3380. [Google Scholar] [CrossRef] [PubMed]
- Nonaka, K.; Chiba, T.; Suga, T.; Asami, Y.; Iwatsuki, M.; Masuma, R.; Ōmura, S.; Shiomi, K. Coculnol, a new penicillic acid produced by a coculture of Fusarium solani FKI-6853 and Talaromyces sp. FKA-65. J. Antibiot. 2015, 68, 530–532. [Google Scholar] [CrossRef]
- Lee, S.M.; Kim, M.S.; Hayat, F.; Shin, D. Recent Advances in the Discovery of Novel Antiprotozoal Agents. Molecules 2019, 24, 3386. [Google Scholar] [CrossRef]
- Trisuwan, K.; Khamthong, N.; Rukachaisirikul, V.; Phongpaichit, S.; Preedanon, S.; Sakayaroj, J. Anthraquinone, cyclopentanone, and naphthoquinone derivatives from the sea fan-derived fungi Fusarium spp. PSU-F14 and PSU-F135. J. Nat. Prod. 2010, 73, 1507–1511. [Google Scholar] [CrossRef]
- Balan, J.; Fuska, J.; Kuhr, I.; Kuhrová, V. Bikaverin, an antibiotic from Gibberella fujikuroi, effective against Leishmania brasiliensis. Folia Microbiol. 1970, 15, 479–484. [Google Scholar] [CrossRef]
- Nascimento, A.M.d.; Conti, R.; Turatti, I.C.; Cavalcanti, B.C.; Costa-Lotufo, L.V.; Pessoa, C.; Moraes, M.O.d.; Manfrim, V.; Toledo, J.S.; Cruz, A.K. Bioactive extracts and chemical constituents of two endophytic strains of Fusarium oxysporum. Rev. Bras. Farmacogn. 2012, 22, 1276–1281. [Google Scholar] [CrossRef]
- Campos, F.F.; Sales Junior, P.A.; Romanha, A.J.; Araújo, M.S.; Siqueira, E.P.; Resende, J.M.; Alves, T.; Martins-Filho, O.A.; Santos, V.L.d.; Rosa, C.A. Bioactive endophytic fungi isolated from Caesalpinia echinata Lam. (Brazilwood) and identification of beauvericin as a trypanocidal metabolite from Fusarium sp. Mem. Inst. Oswaldo Cruz 2015, 110, 65–74. [Google Scholar] [CrossRef]
- Ibrahim, S.R.; Abdallah, H.M.; Mohamed, G.A.; Ross, S.A. Integracides H-J: New tetracyclic triterpenoids from the endophytic fungus Fusarium sp. Fitoterapia 2016, 112, 161–167. [Google Scholar] [CrossRef]
- Abdelhakim, I.; Bin Mahmud, F.; Motoyama, T.; Futamura, Y.; Takahashi, S.; Osada, H. Dihydrolucilactaene, a potent antimalarial compound from Fusarium sp. RK97-94. J. Nat. Prod. 2021, 85, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Motoyama, T.; Futamura, Y.; Uramoto, M.; Nogawa, T.; Hayashi, T.; Hirota, H.; Tanaka, A.; Takahashi-Ando, N.; Kamakura, T. Biosynthetic gene cluster identification and biological activity of lucilactaene from Fusarium sp. RK97-94. Biosci. Biotechnol. Biochem. 2020, 84, 1303–1307. [Google Scholar] [CrossRef] [PubMed]
- Abdelhakim, I.A.; Motoyama, T.; Nogawa, T.; Mahmud, F.B.; Futamura, Y.; Takahashi, S.; Osada, H. Isolation of new lucilactaene derivatives from P450 monooxygenase and aldehyde dehydrogenase knockout Fusarium sp. RK97-94 strains and their biological activities. J. Antibiot. 2022, 75, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.B.; Zink, D.L.; Polishook, J.D.; Dombrowski, A.W.; Darkin-Rattray, S.J.; Schmatz, D.M.; Goetz, M.A. Apicidins: Novel cyclic tetrapeptides as coccidiostats and antimalarial agents from Fusarium pallidoroseum. Tetrahedron Lett. 1996, 37, 8077–8080. [Google Scholar] [CrossRef]
- Singh, S.B.; Zink, D.L.; Liesch, J.M.; Dombrowski, A.W.; Darkin-Rattray, S.J.; Schmatz, D.M.; Goetz, M.A. Structure, histone deacetylase, and antiprotozoal activities of apicidins B and C, congeners of apicidin with proline and valine substitutions. Org. Lett. 2001, 3, 2815–2818. [Google Scholar] [CrossRef]
- Von Bargen, K.W.; Niehaus, E.-M.; Bergander, K.; Brun, R.; Tudzynski, B.; Humpf, H.-U. Structure elucidation and antimalarial activity of apicidin F: An apicidin-like compound produced by Fusarium fujikuroi. J. Nat. Prod. 2013, 76, 2136–2140. [Google Scholar] [CrossRef]
- Liu, Y.; Xu, M.; Tang, Y.; Shao, Y.; Wang, H.; Zhang, H. Genome features and antiSMASH analysis of an endophytic strain Fusarium sp. R1. Metabolites 2022, 12, 521. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhang, C.; Li, Q.; Ma, J.; Ju, J. Metabolic blockade-based genome mining reveals lipochain-linked dihydro-β-alanine synthetases involved in autucedine biosynthesis. Org. Lett. 2022, 24, 5535–5540. [Google Scholar] [CrossRef]
- Kang, H.S.; Charlop-Powers, Z.; Brady, S.F. Multiplexed CRISPR/Cas9- and TAR-mediated promoter engineering of natural product biosynthetic gene clusters in yeast. ACS Synth. Biol. 2016, 5, 1002–1010. [Google Scholar] [CrossRef]
- Keller, N.P. Fungal secondary metabolism: Regulation, function and drug discovery. Nat. Rev. Microbiol. 2019, 17, 167–180. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).