An Ethanol Extract of Perilla frutescens Leaves Suppresses Adrenergic Agonist-Induced Metastatic Ability of Cancer Cells by Inhibiting Src-Mediated EMT
Abstract
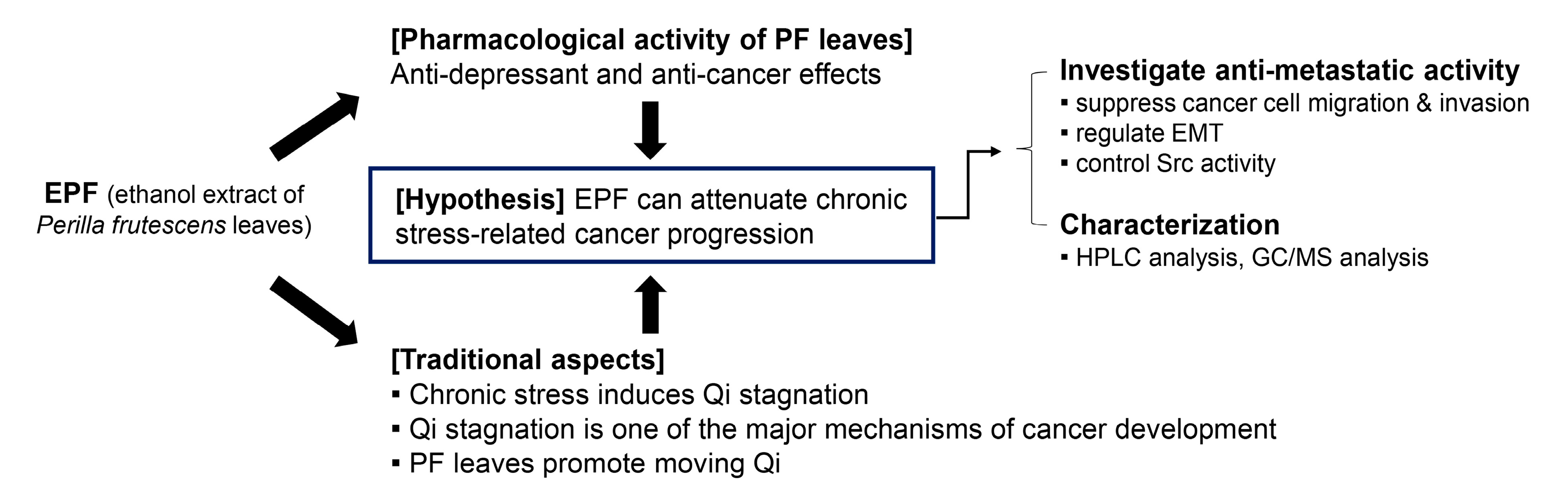
1. Introduction
2. Results
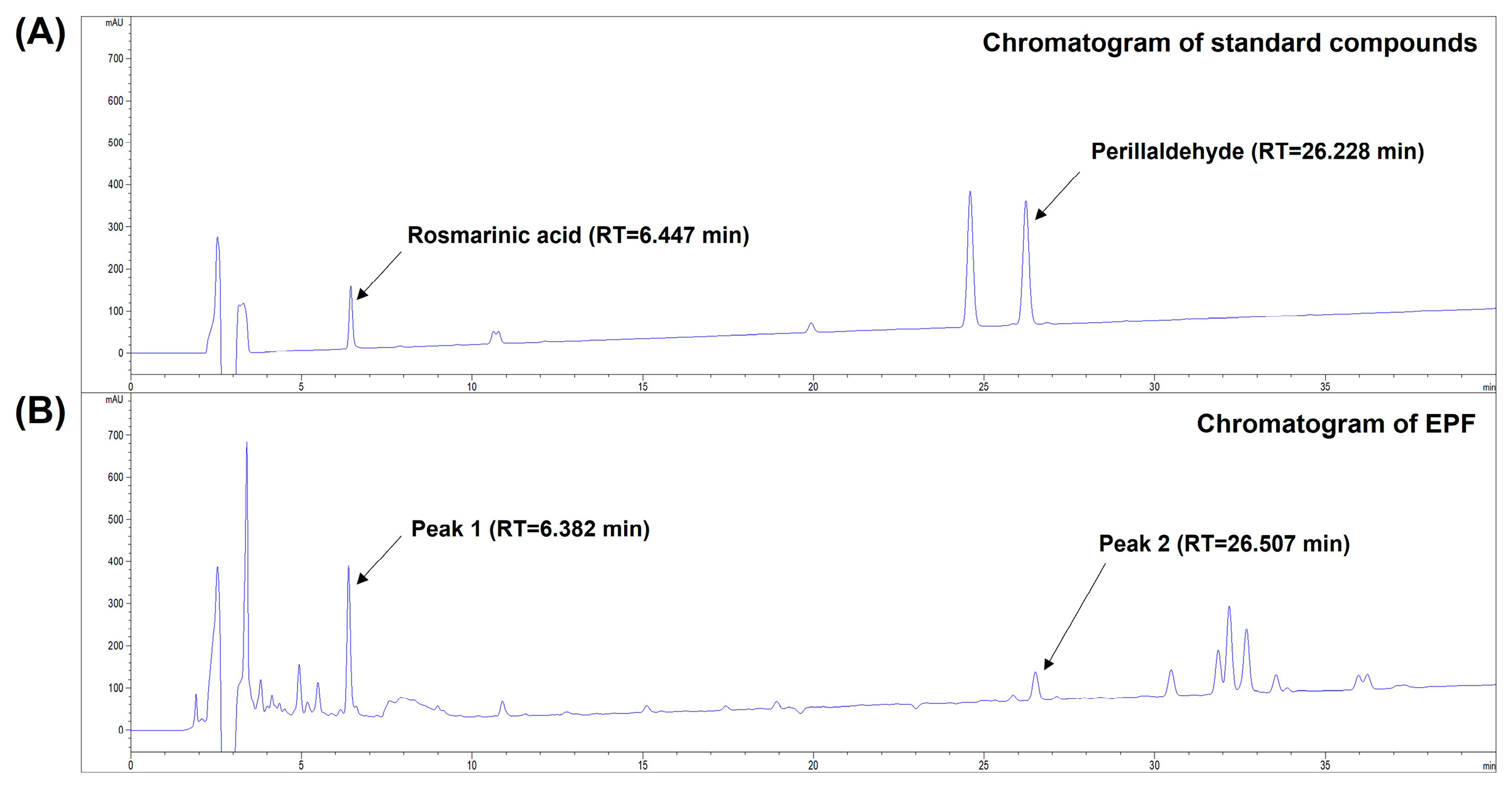
2.1. High-Performance Liquid Chromatography (HPLC) Analysis of Marker Constituents in EPF
2.2. Gas Chromatography–Mass Spectrometry (GC-MS) Analysis of EPF
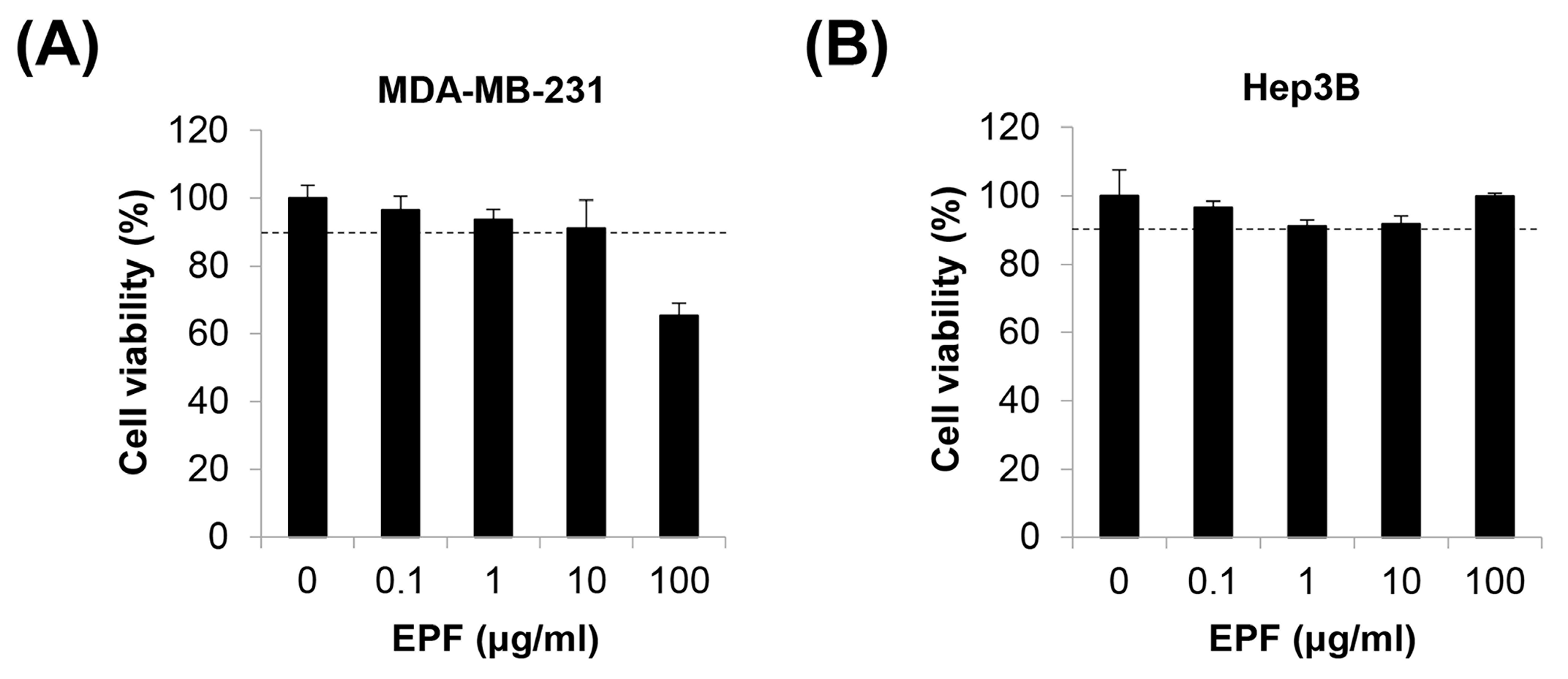
2.3. Determination of a Non-Toxic Concentration Range of EPF in Cancer Cells
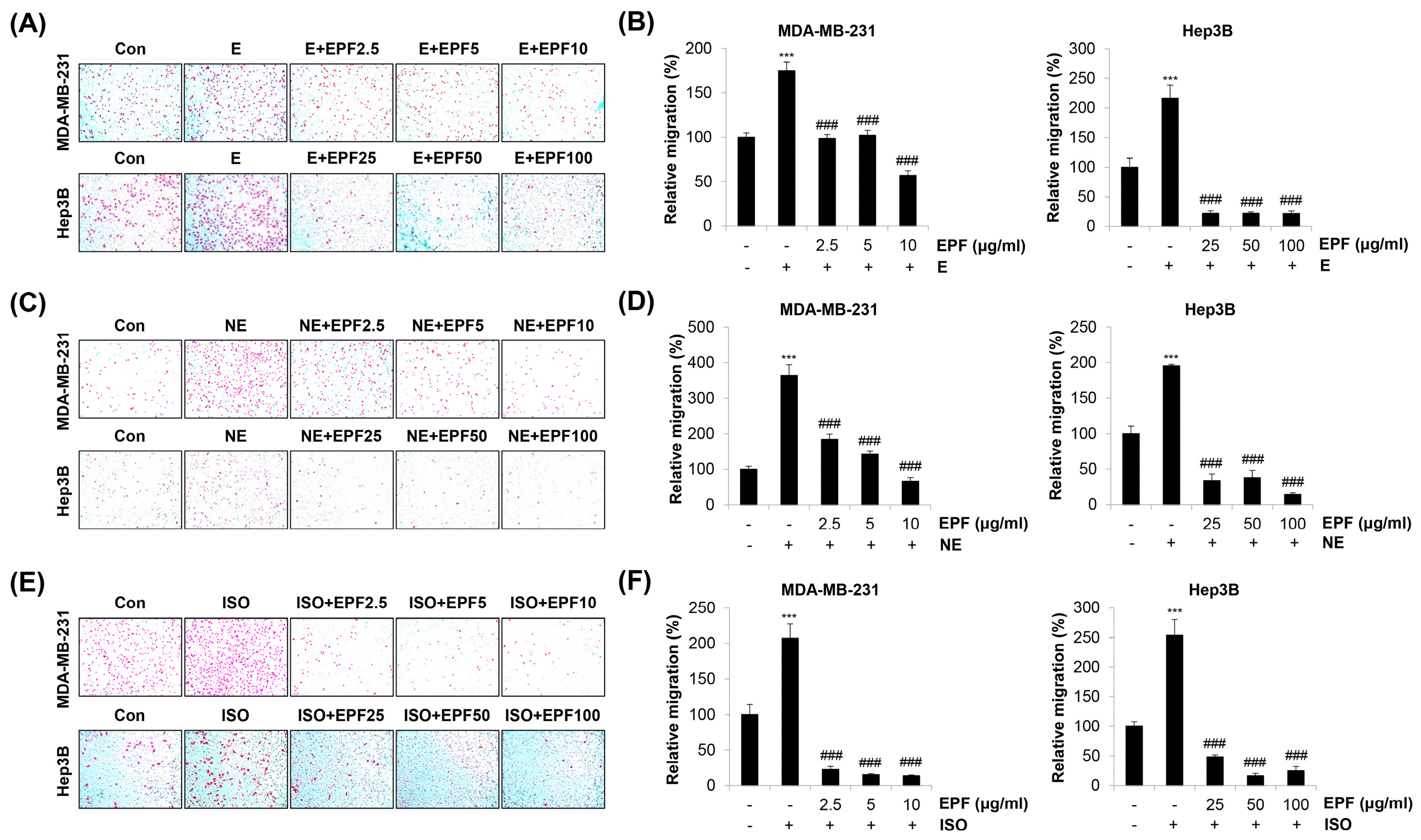
2.4. EPF Suppresses Adrenergic Agonist-Induced Cancer Cell Migration
2.5. EPF Inhibits Adrenergic Agonist-Induced Cancer Cell Invasion
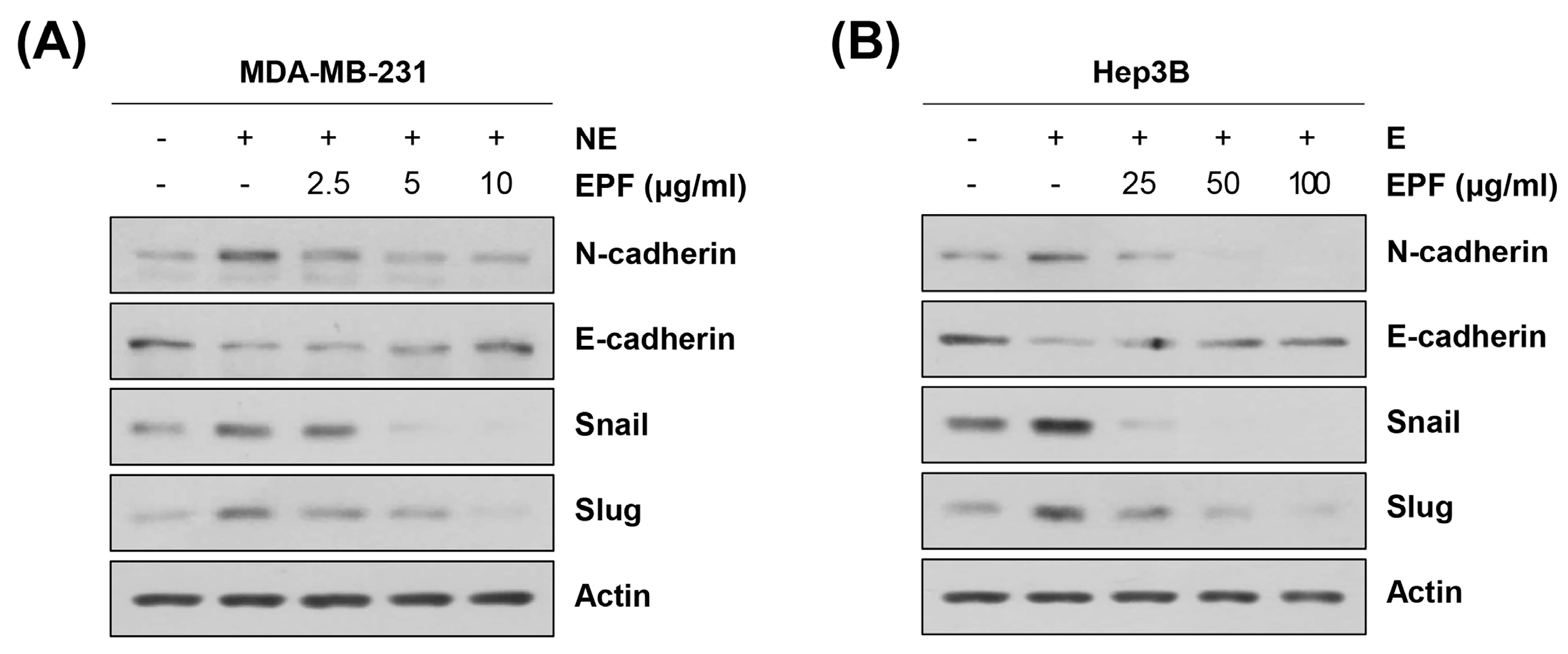
2.6. EPF Regulates EMT Marker Proteins
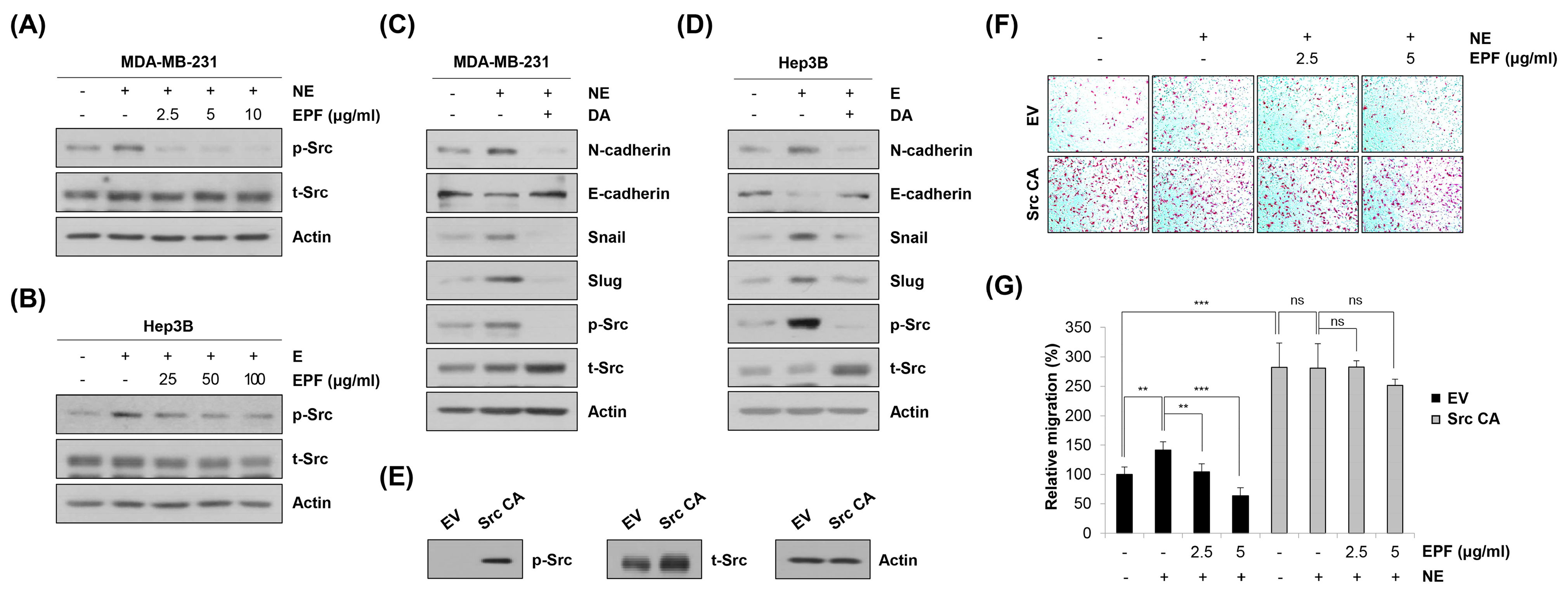
2.7. Involvement of Src in Regulating EMT and Migration in Cancer Cells
3. Discussion
4. Materials and Methods
4.1. Preparation of EPF
4.2. Cell Culture
4.3. HPLC Analysis
4.4. GC-MS Analysis
4.5. MTT Assay
4.6. Transwell Assay
4.7. Western Blot Analysis
4.8. Transfection
4.9. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oh, H.M.; Son, C.G. The Risk of Psychological Stress on Cancer Recurrence: A Systematic Review. Cancers 2021, 13, 5816. [Google Scholar] [CrossRef] [PubMed]
- Batty, G.D.; Russ, T.C.; Stamatakis, E.; Kivimäki, M. Psychological distress in relation to site specific cancer mortality: Pooling of unpublished data from 16 prospective cohort studies. BMJ 2017, 356, j108. [Google Scholar] [CrossRef] [PubMed]
- Kim-Fuchs, C.; Le, C.P.; Pimentel, M.A.; Shackleford, D.; Ferrari, D.; Angst, E.; Hollande, F.; Sloan, E.K. Chronic stress accelerates pancreatic cancer growth and invasion: A critical role for beta-adrenergic signaling in the pancreatic microenvironment. Brain Behav. Immun. 2014, 40, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Thaker, P.H.; Han, L.Y.; Kamat, A.A.; Arevalo, J.M.; Takahashi, R.; Lu, C.; Jennings, N.B.; Armaiz-Pena, G.; Bankson, J.A.; Ravoori, M.; et al. Chronic stress promotes tumor growth and angiogenesis in a mouse model of ovarian carcinoma. Nat. Med. 2006, 12, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.; Le, C.P.; Walker, A.K.; Creed, S.J.; Pon, C.K.; Albold, S.; Carroll, D.; Halls, M.L.; Lane, J.R.; Riedel, B.; et al. β2-Adrenoceptors on tumor cells play a critical role in stress-enhanced metastasis in a mouse model of breast cancer. Brain Behav. Immun. 2016, 57, 106–115. [Google Scholar] [CrossRef]
- Gudenkauf, L.M.; Ehlers, S.L. Psychosocial interventions in breast cancer survivorship care. Breast 2018, 38, 1–6. [Google Scholar] [CrossRef]
- Fawzy, F.I.; Fawzy, N.W.; Hyun, C.S.; Elashoff, R.; Guthrie, D.; Fahey, J.L.; Morton, D.L. Malignant melanoma. Effects of an early structured psychiatric intervention, coping, and affective state on recurrence and survival 6 years later. Arch. Gen. Psychiatry 1993, 50, 681–689. [Google Scholar] [CrossRef]
- Reiche, E.M.; Nunes, S.O.; Morimoto, H.K. Stress, depression, the immune system, and cancer. Lancet Oncol. 2004, 5, 617–625. [Google Scholar] [CrossRef]
- Cole, S.W.; Sood, A.K. Molecular pathways: Beta-adrenergic signaling in cancer. Clin. Cancer Res. 2012, 18, 1201–1206. [Google Scholar] [CrossRef]
- Abrass, C.K.; O’Connor, S.W.; Scarpace, P.J.; Abrass, I.B. Characterization of the beta-adrenergic receptor of the rat peritoneal macrophage. J. Immunol. 1985, 135, 1338–1341. [Google Scholar] [CrossRef]
- Graf, K.; Gräfe, M.; Dümmler, U.; O’Connor, A.; Regitz-Zagrosek, V.; Kunkel, G.; Auch-Schwelk, W.; Fleck, E. Regulation of beta-adrenergic receptors on endothelial cells in culture. Eur. Heart J. 1993, 14 (Suppl. SI), 173–176. [Google Scholar]
- Melhem-Bertrandt, A.; Chavez-Macgregor, M.; Lei, X.; Brown, E.N.; Lee, R.T.; Meric-Bernstam, F.; Sood, A.K.; Conzen, S.D.; Hortobagyi, G.N.; Gonzalez-Angulo, A.M. Beta-blocker use is associated with improved relapse-free survival in patients with triple-negative breast cancer. J. Clin. Oncol. 2011, 29, 2645–2652. [Google Scholar] [CrossRef]
- Parada-Huerta, E.; Alvarez-Dominguez, T.; Uribe-Escamilla, R.; Rodriguez-Joya, J.; Ponce-Medrano, J.D.; Padron-Lucio, S.; Alfaro-Rodriguez, A.; Bandala, C. Metastasis Risk Reduction Related with Beta-Blocker Treatment in Mexican Women with Breast Cancer. Asian Pac. J. Cancer Prev. 2016, 17, 2953–2957. [Google Scholar]
- Udumyan, R.; Montgomery, S.; Fang, F.; Almroth, H.; Valdimarsdottir, U.; Ekbom, A.; Smedby, K.E.; Fall, K. Beta-Blocker Drug Use and Survival among Patients with Pancreatic Adenocarcinoma. Cancer Res. 2017, 77, 3700–3707. [Google Scholar] [CrossRef]
- Nkontchou, G.; Aout, M.; Mahmoudi, A.; Roulot, D.; Bourcier, V.; Grando-Lemaire, V.; Ganne-Carrie, N.; Trinchet, J.C.; Vicaut, E.; Beaugrand, M. Effect of long-term propranolol treatment on hepatocellular carcinoma incidence in patients with HCV-associated cirrhosis. Cancer Prev. Res. 2012, 5, 1007–1014. [Google Scholar] [CrossRef]
- Chang, H.; Lee, S.H. Beta-adrenergic receptor blockers and hepatocellular carcinoma survival: A systemic review and meta-analysis. Clin. Exp. Med. 2022. [Google Scholar] [CrossRef]
- Chambers, A.F.; Groom, A.C.; MacDonald, I.C. Dissemination and growth of cancer cells in metastatic sites. Nat. Rev. Cancer 2002, 2, 563–572. [Google Scholar] [CrossRef]
- Micalizzi, D.S.; Farabaugh, S.M.; Ford, H.L. Epithelial-mesenchymal transition in cancer: Parallels between normal development and tumor progression. J. Mammary Gland Biol. Neoplasia 2010, 15, 117–134. [Google Scholar] [CrossRef]
- Ahmed, H.M. Ethnomedicinal, Phytochemical and Pharmacological Investigations of Perilla frutescens (L.) Britt. Molecules 2018, 24, 102. [Google Scholar] [CrossRef]
- Kim, C.L.; Shin, Y.S.; Choi, S.H.; Oh, S.; Kim, K.; Jeong, H.S.; Mo, J.S. Extracts of Perilla frutescens var. Acuta (Odash.) Kudo Leaves Have Antitumor Effects on Breast Cancer Cells by Suppressing YAP Activity. Evid. Based Complement. Alternat. Med. 2021, 2021, 5619761. [Google Scholar] [CrossRef]
- Maeda, A.; Fujimura, T.; Hirakawa, N.; Baba, K.; Kawamoto, S. A Methoxyflavanone from Perilla frutescens Induces Cellular Senescence in A549 Human Lung Adenocarcinoma Cells but Not in Normal Human Bronchial Epithelial Cells. Biol. Pharm. Bull. 2022, 45, 1581–1584. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Tian, D. A review on nasopharyngeal carcinoma in ancient Chinese literature. Zhonghua Yi Shi Za Zhi 2001, 31, 115–118. [Google Scholar]
- Zhang, Y.H.; Qin, X.; Xu, J. Analysis of Chinese medical syndrome features of patients with primary liver cancer before and after transcatheter arterial chemoembolization. Zhongguo Zhong Xi Yi Jie He Za Zhi 2012, 32, 1171–1174. [Google Scholar] [PubMed]
- Huang, H.; Song, Q.; Chen, J.; Zeng, Y.; Wang, W.; Jiao, B.; Lin, J.; Li, Y.; Zhang, R.; Ma, L.; et al. The Role of Qi-Stagnation Constitution and Emotion Regulation in the Association Between Childhood Maltreatment and Depression in Chinese College Students. Front. Psychiatry 2022, 13, 825198. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Wan, Y.; Zhao, Z.; Chen, H. Determination of the content of rosmarinic acid by HPLC and analytical comparison of volatile constituents by GC-MS in different parts of Perilla frutescens (L.) Britt. Chem. Cent. J. 2013, 7, 61. [Google Scholar] [CrossRef]
- Jeong, J.H.; Park, H.J.; Park, S.H.; Choi, Y.H.; Chi, G.Y. β2-Adrenergic Receptor Signaling Pathway Stimulates the Migration and Invasion of Cancer Cells via Src Activation. Molecules 2022, 27, 5940. [Google Scholar] [CrossRef]
- Zhang, J.; Liu, Y.; Xu, Y. Soothing liver-qi stagnation method for cancer-related depression: A protocol for systematic review and meta-analysis. Medicine 2020, 99, e22797. [Google Scholar] [CrossRef]
- Zhang, S.; Yu, D. Targeting Src family kinases in anti-cancer therapies: Turning promise into triumph. Trends Pharmacol. Sci. 2012, 33, 122–128. [Google Scholar] [CrossRef]
- Liu, X.; Feng, R. Inhibition of epithelial to mesenchymal transition in metastatic breast carcinoma cells by c-Src suppression. Acta Biochim. Biophys. Sin. 2010, 42, 496–501. [Google Scholar] [CrossRef]
- Srivastava, K.; Pickard, A.; Craig, S.G.; Quinn, G.P.; Lambe, S.M.; James, J.A.; McDade, S.S.; McCance, D.J. ΔNp63γ/SRC/Slug Signaling Axis Promotes Epithelial-to-Mesenchymal Transition in Squamous Cancers. Clin. Cancer Res. 2018, 24, 3917–3927. [Google Scholar] [CrossRef]
- Lang, L.; Shay, C.; Xiong, Y.; Thakkar, P.; Chemmalakuzhy, R.; Wang, X.; Teng, Y. Combating head and neck cancer metastases by targeting Src using multifunctional nanoparticle-based saracatinib. J. Hematol. Oncol. 2018, 11, 85. [Google Scholar] [CrossRef]
- Takeda, H.; Tsuji, M.; Inazu, M.; Egashira, T.; Matsumiya, T. Rosmarinic acid and caffeic acid produce antidepressive-like effect in the forced swimming test in mice. Eur. J. Pharmacol. 2002, 449, 261–267. [Google Scholar] [CrossRef]
- Takeda, H.; Tsuji, M.; Miyamoto, J.; Matsumiya, T. Rosmarinic acid and caffeic acid reduce the defensive freezing behavior of mice exposed to conditioned fear stress. Psychopharmacology 2002, 164, 233–235. [Google Scholar] [CrossRef]
- Han, Y.H.; Kee, J.Y.; Hong, S.H. Rosm arinic Acid Activates AMPK to Inhibit Metastasis of Colorectal Cancer. Front. Pharmacol. 2018, 9, 68. [Google Scholar] [CrossRef]
- Han, Y.; Ma, L.; Zhao, L.; Feng, W.; Zheng, X. Rosmarinic inhibits cell proliferation, invasion and migration via up-regulating miR-506 and suppressing MMP2/16 expression in pancreatic cancer. Biomed. Pharmacother. 2019, 115, 108878. [Google Scholar] [CrossRef]
- Highland, H.N.; Thakur, M.B.; George, L.B. Controlling non-small cell lung cancer progression by blocking focal adhesion kinase-c-Src active site with Rosmarinus officinalis L. phytocomponents: An in silico and in vitro study. J. Cancer Res. Ther. 2022, 18, 1674–1682. [Google Scholar] [CrossRef]
- Byun, S.; Park, J.; Lee, E.; Lim, S.; Yu, J.G.; Lee, S.J.; Chen, H.; Dong, Z.; Lee, K.W.; Lee, H.J. Src kinase is a direct target of apigenin against UVB-induced skin inflammation. Carcinogenesis 2013, 34, 397–405. [Google Scholar] [CrossRef]
- Rahmani, A.H.; Alsahli, M.A.; Almatroudi, A.; Almogbel, M.A.; Khan, A.A.; Anwar, S.; Almatroodi, S.A. The Potential Role of Apigenin in Cancer Prevention and Treatment. Molecules 2022, 27, 6051. [Google Scholar] [CrossRef]
- Nakazawa, T.; Yasuda, T.; Ueda, J.; Ohsawa, K. Antidepressant-like effects of apigenin and 2,4,5-trimethoxycinnamic acid from Perilla frutescens in the forced swimming test. Biol. Pharm. Bull. 2003, 26, 474–480. [Google Scholar] [CrossRef]
- Ji, W.W.; Li, R.P.; Li, M.; Wang, S.Y.; Zhang, X.; Niu, X.X.; Li, W.; Yan, L.; Wang, Y.; Fu, Q.; et al. Antidepressant-like effect of essential oil of Perilla frutescens in a chronic, unpredictable, mild stress-induced depression model mice. Chin. J. Nat. Med. 2014, 12, 753–759. [Google Scholar] [CrossRef]
- Lin, Z.; Huang, S.; LingHu, X.; Wang, Y.; Wang, B.; Zhong, S.; Xie, S.; Xu, X.; Yu, A.; Nagai, A.; et al. Perillaldehyde inhibits bone metastasis and receptor activator of nuclear factor-κB ligand (RANKL) signaling-induced osteoclastogenesis in prostate cancer cell lines. Bioengineered 2022, 13, 2710–2719. [Google Scholar] [CrossRef]
- Erhunmwunsee, F.; Pan, C.; Yang, K.; Li, Y.; Liu, M.; Tian, J. Recent development in biological activities and safety concerns of perillaldehyde from perilla plants: A review. Crit. Rev. Food Sci. Nutr. 2022, 62, 6328–6340. [Google Scholar] [CrossRef] [PubMed]
- Singla, R.K.; De, R.; Efferth, T.; Mezzetti, B.; Sahab Uddin, M.; Sanusi; Ntie-Kang, F.; Wang, D.; Schultz, F.; Kharat, K.R.; et al. The International Natural Product Sciences Taskforce (INPST) and the power of Twitter networking exemplified through #INPST hashtag analysis. Phytomedicine 2023, 108, 154520. [Google Scholar] [CrossRef] [PubMed]
- Min, T.R.; Park, H.J.; Ha, K.T.; Chi, G.Y.; Choi, Y.H.; Park, S.H. Suppression of EGFR/STAT3 activity by lupeol contributes to the induction of the apoptosis of human non-small cell lung cancer cells. Int. J. Oncol. 2019, 55, 320–330. [Google Scholar] [CrossRef] [PubMed]
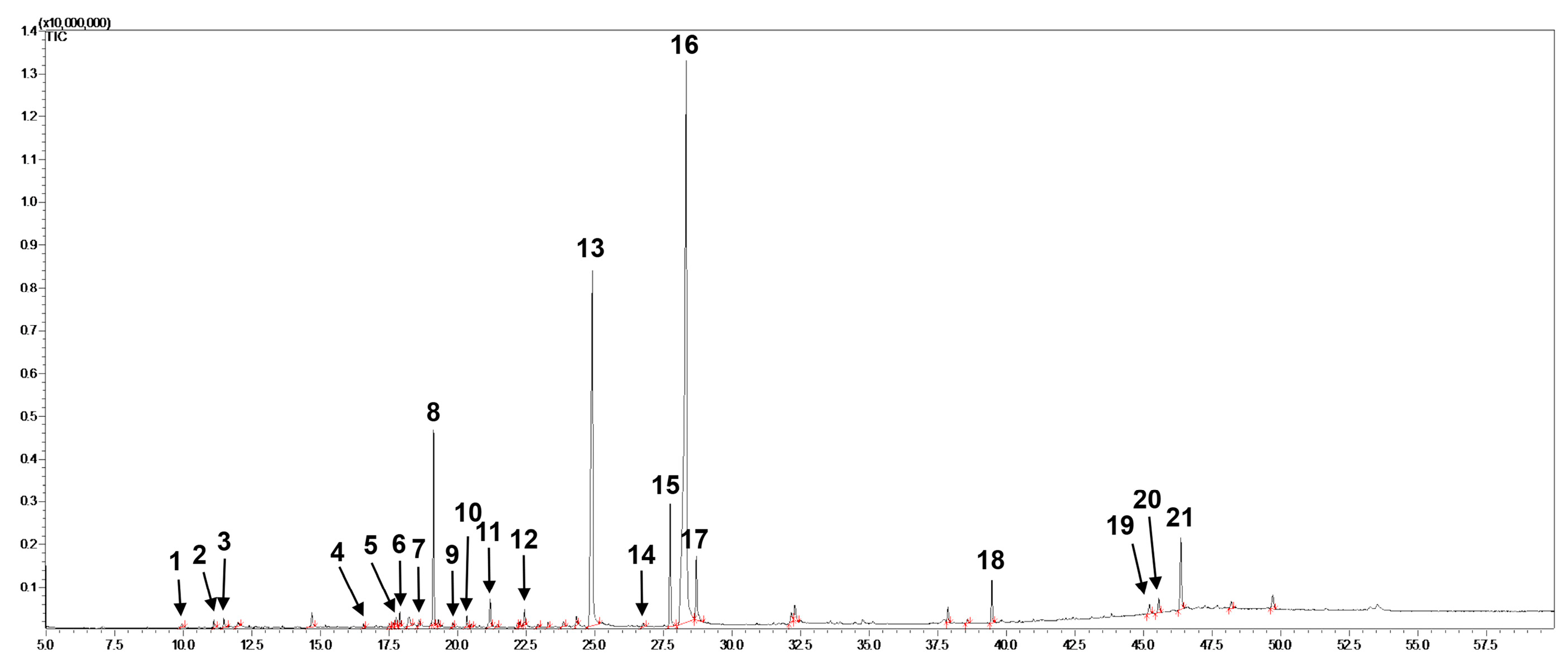

| Peak # 1 | RT 2 (min) | Formula | MW 3 (m/z) | Identification |
|---|---|---|---|---|
| 1 | 9.937 | C6H8O4 | 144 | 2,3-Dihydro-3,5-dihydroxy-6-methyl-4H-pyran-4-one |
| 2 | 11.118 | C8H8O | 120 | 2,3-Dihydro-benzofuran |
| 3 | 11.473 | C5H10O4 | 134 | 2,3-Dihydroxypropyl acetate |
| 4 | 16.569 | C11H16O2 | 180 | Dihydroactinidiolide |
| 5 | 17.508 | C15H24O | 220 | (-)-Spathulenol |
| 6 | 17.647 | C15H24O | 220 | (-)-Caryophyllene oxide |
| 7 | 18.595 | C12H16O3 | 208 | Isoelemicin |
| 8 | 19.125 | C12H16O3 | 208 | cis-Asarone |
| 9 | 19.833 | C10H12O4 | 196 | Benzaldehyde, 2,4,5-trimethoxy- |
| 10 | 20.335 | C12H16O4 | 224 | 1-(2,4,5-Trimethoxyphenyl)propan-2-one |
| 11 | 21.183 | C12H14O4 | 222 | Isodillapiole |
| 12 | 22.441 | C20H38 | 278 | Neophytadiene |
| 13 | 24.919 | C16H32O2 | 256 | Palmitic acid |
| 14 | 26.764 | C17H34O2 | 270 | Heptadecanoic acid |
| 15 | 27.748 | C20H40O | 296 | Phytol |
| 16 | 28.338 | C18H30O2 | 278 | Linolenic acid |
| 17 | 28.703 | C18H36O2 | 284 | stearic acid |
| 18 | 39.469 | C30H50 | 410 | Squalene |
| 19 | 45.213 | C28H48O | 400 | Campesterol |
| 20 | 45.551 | C29H48O | 412 | stigmasterol |
| 21 | 46.355 | C29H50O | 414 | Clionasterol |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, J.-H.; Park, H.-J.; Chi, G.-Y.; Choi, Y.-H.; Park, S.-H. An Ethanol Extract of Perilla frutescens Leaves Suppresses Adrenergic Agonist-Induced Metastatic Ability of Cancer Cells by Inhibiting Src-Mediated EMT. Molecules 2023, 28, 3414. https://doi.org/10.3390/molecules28083414
Jeong J-H, Park H-J, Chi G-Y, Choi Y-H, Park S-H. An Ethanol Extract of Perilla frutescens Leaves Suppresses Adrenergic Agonist-Induced Metastatic Ability of Cancer Cells by Inhibiting Src-Mediated EMT. Molecules. 2023; 28(8):3414. https://doi.org/10.3390/molecules28083414
Chicago/Turabian StyleJeong, Jae-Hoon, Hyun-Ji Park, Gyoo-Yong Chi, Yung-Hyun Choi, and Shin-Hyung Park. 2023. "An Ethanol Extract of Perilla frutescens Leaves Suppresses Adrenergic Agonist-Induced Metastatic Ability of Cancer Cells by Inhibiting Src-Mediated EMT" Molecules 28, no. 8: 3414. https://doi.org/10.3390/molecules28083414
APA StyleJeong, J.-H., Park, H.-J., Chi, G.-Y., Choi, Y.-H., & Park, S.-H. (2023). An Ethanol Extract of Perilla frutescens Leaves Suppresses Adrenergic Agonist-Induced Metastatic Ability of Cancer Cells by Inhibiting Src-Mediated EMT. Molecules, 28(8), 3414. https://doi.org/10.3390/molecules28083414







