Design, Synthesis, and Pharmacology of New Triazole-Containing Quinolinones as CNS Active Agents
Abstract
1. Introduction
2. Results and Discussion
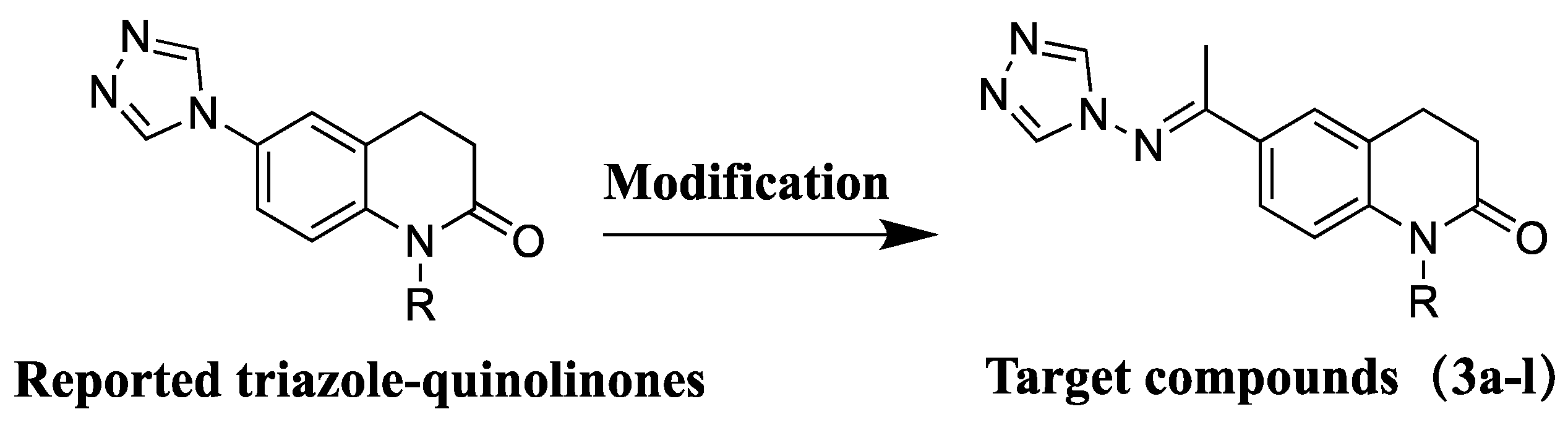
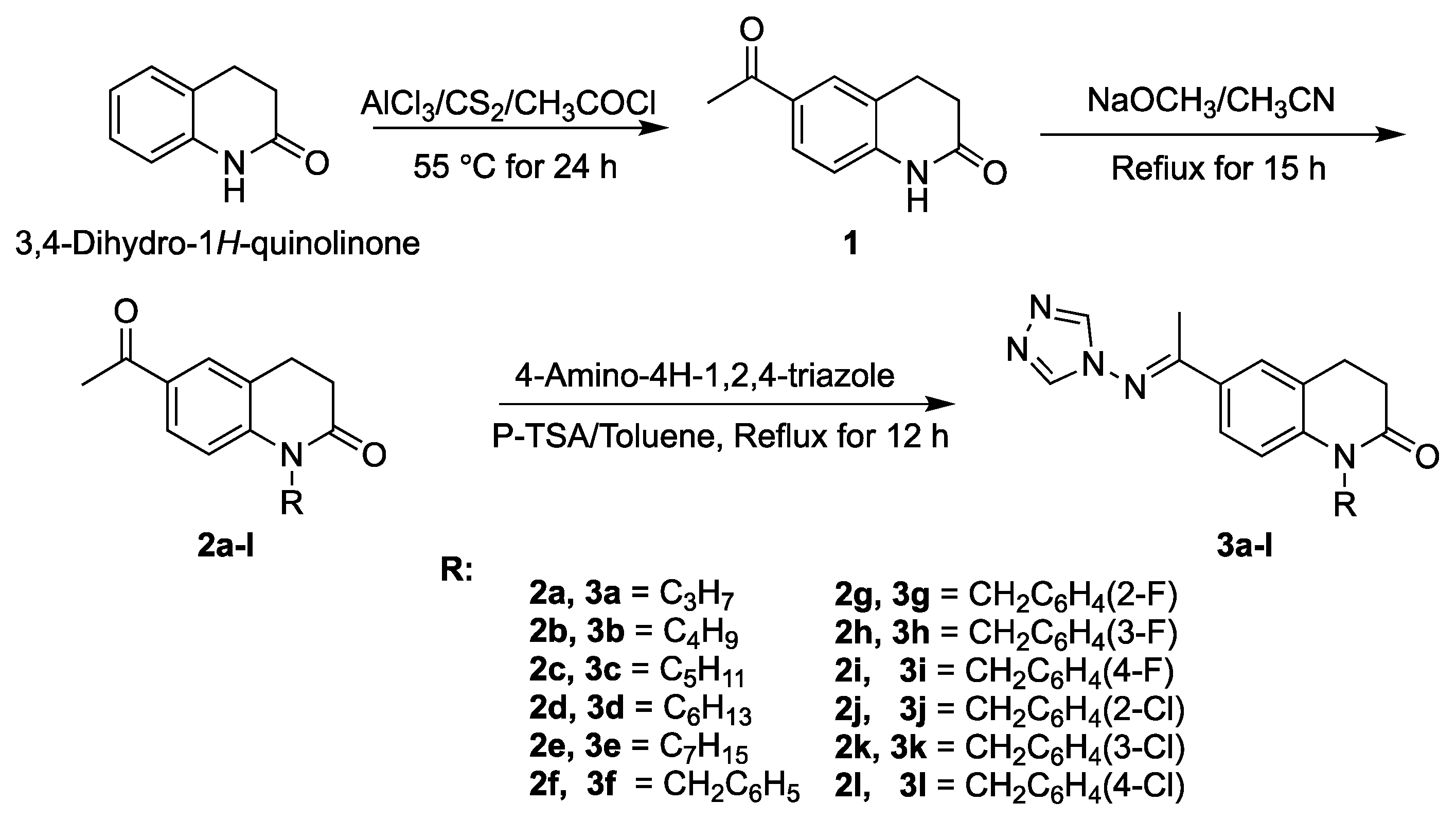
2.1. Chemistry
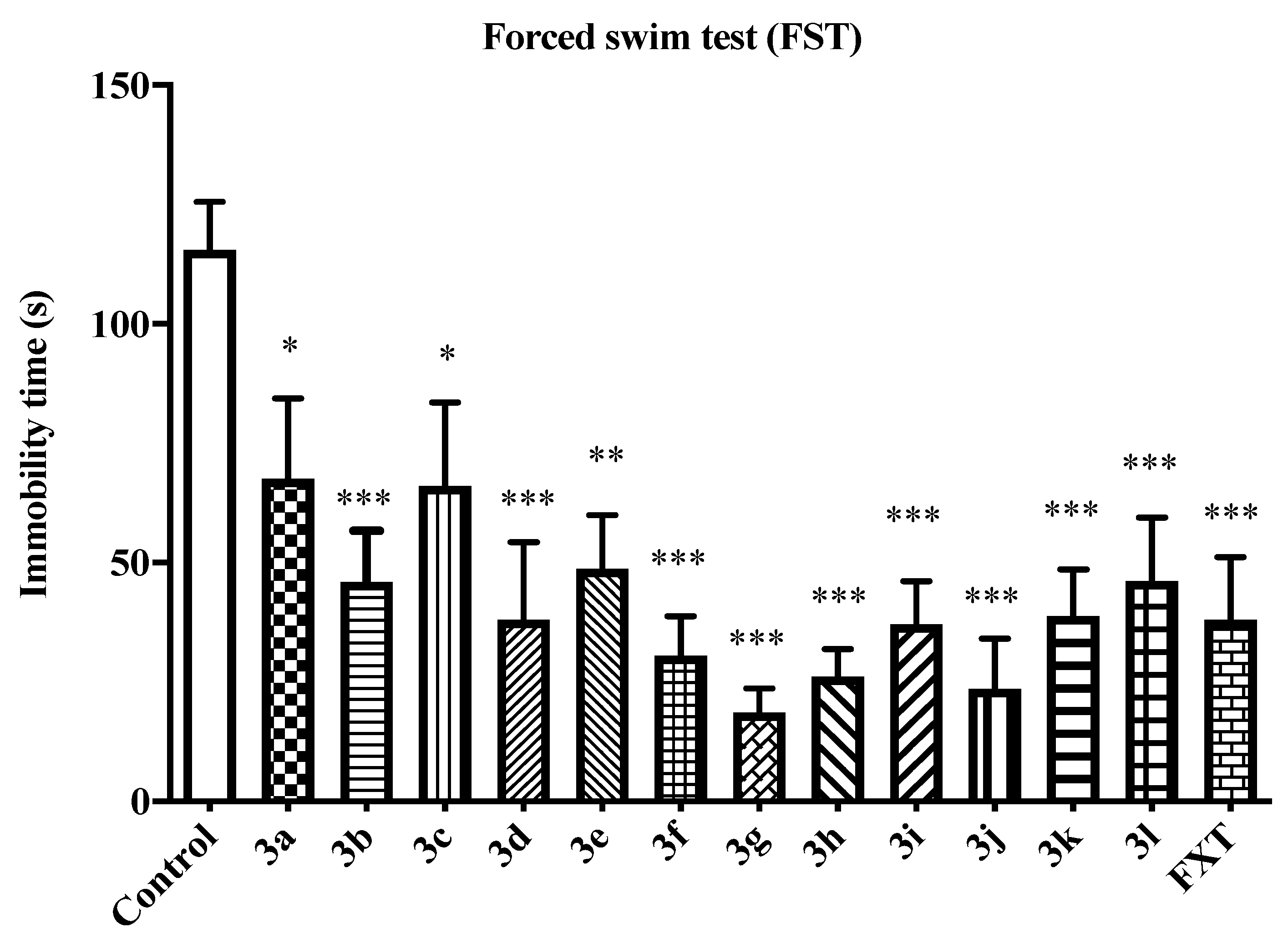
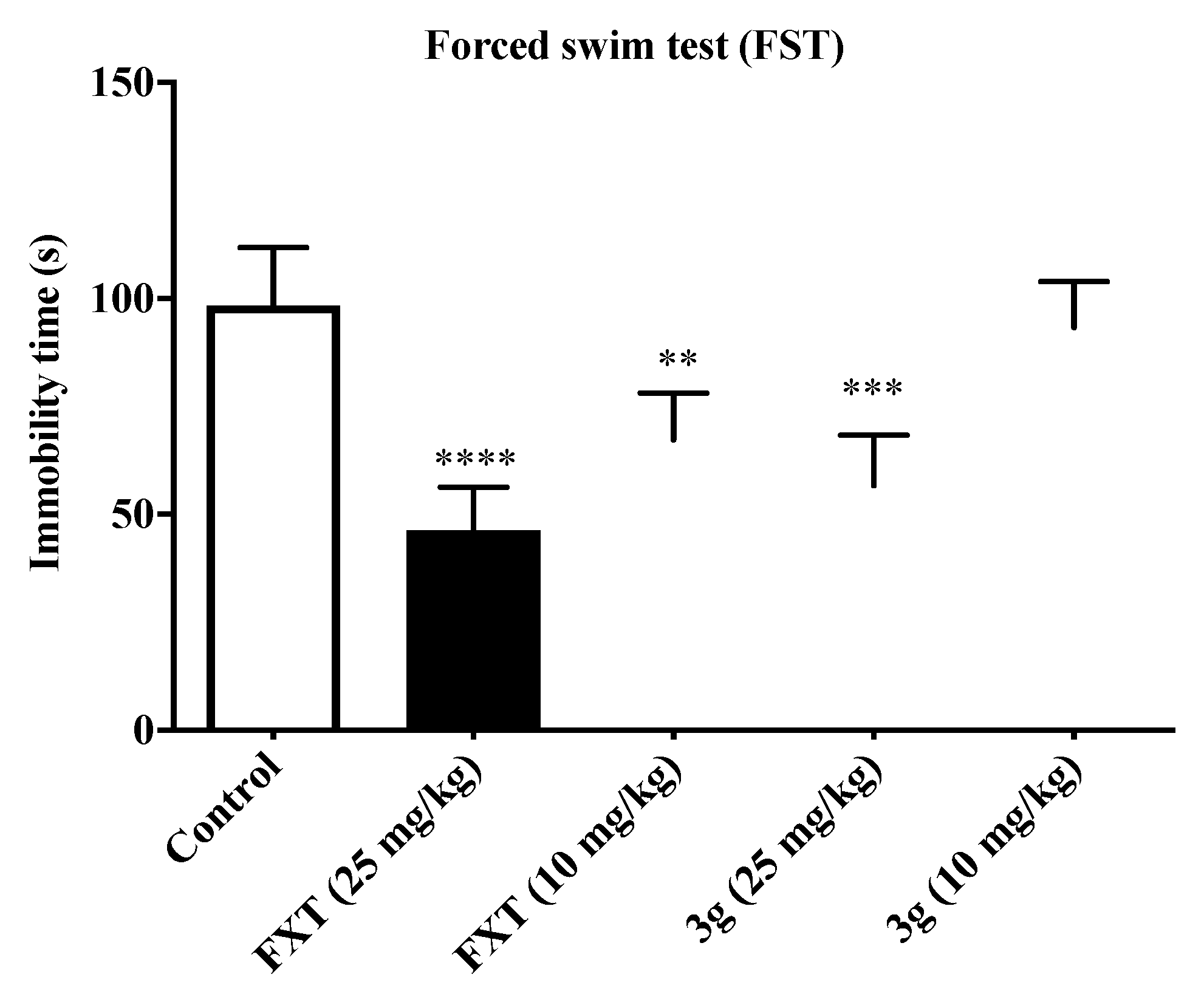
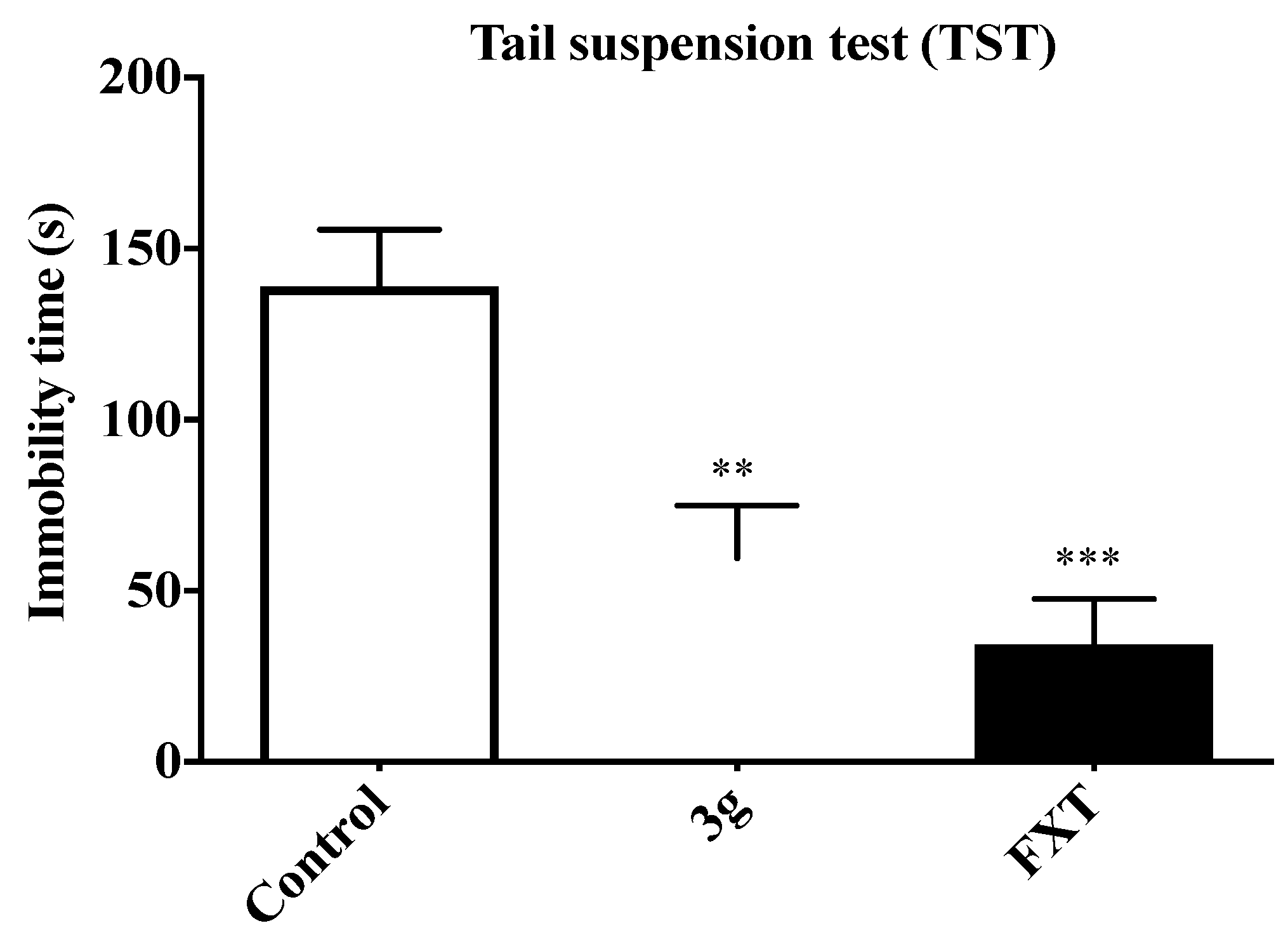
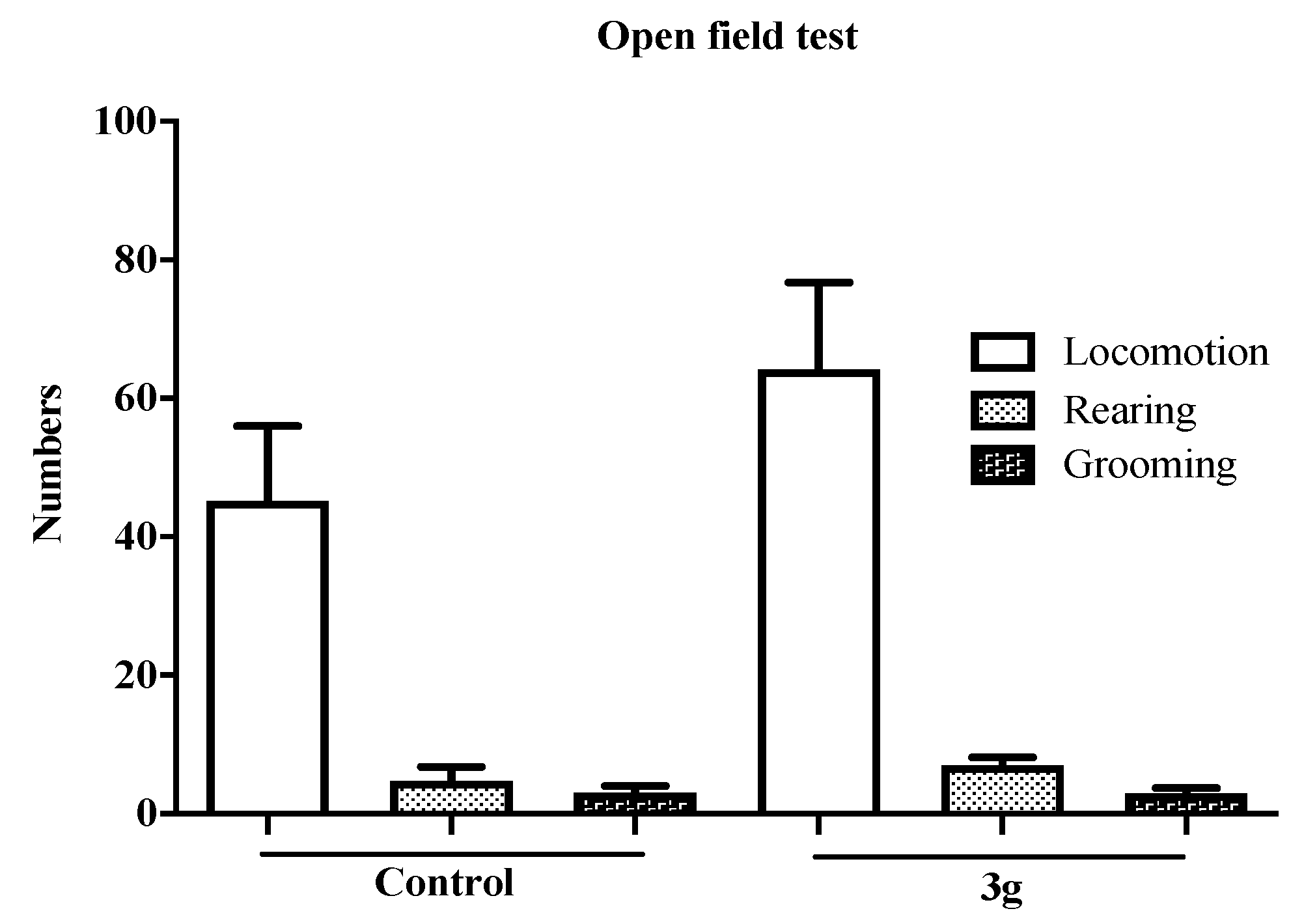
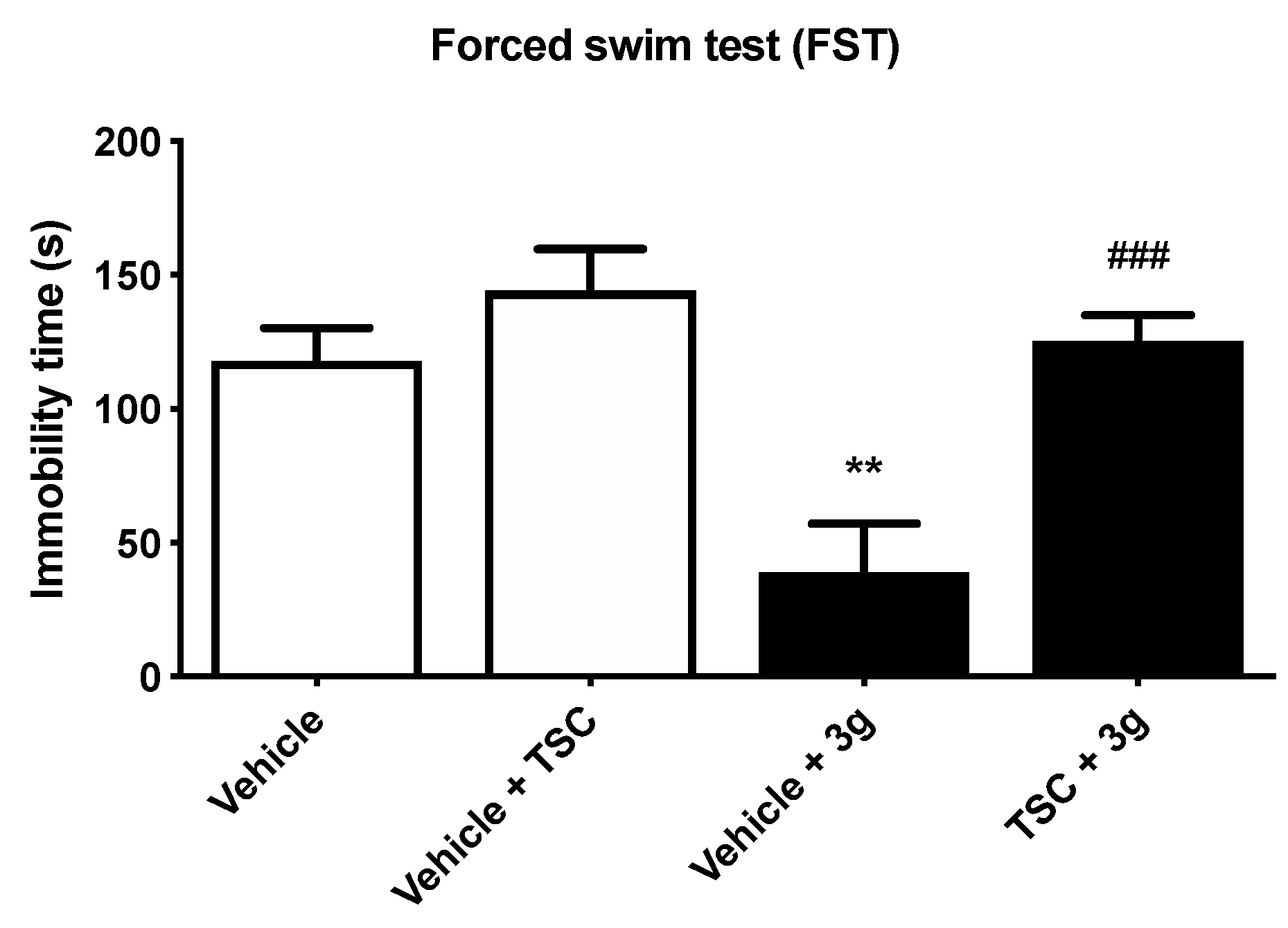
2.2. Antidepressant Activities
2.3. Antiseizure Activity and Neurotoxicity
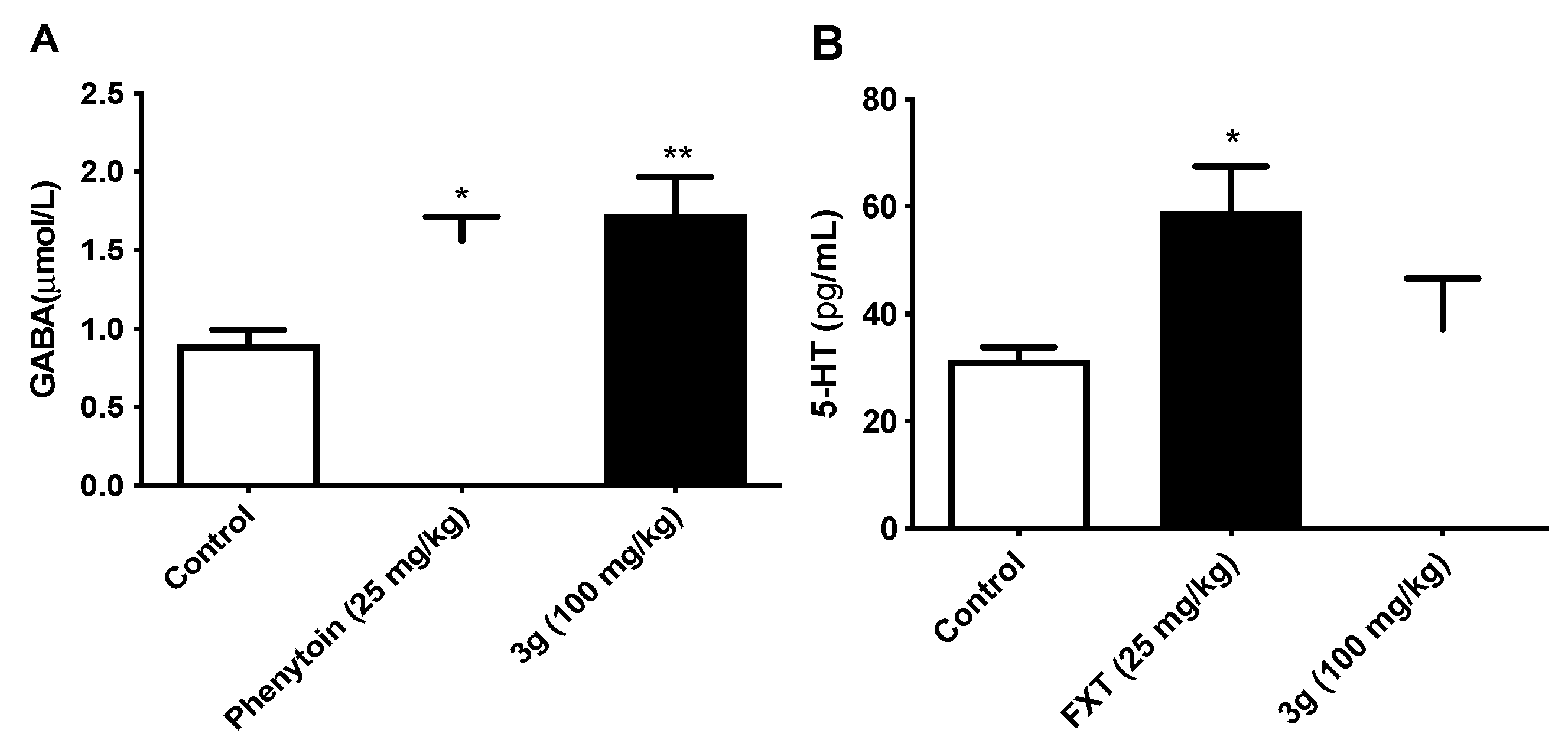
2.4. Effects of Compound 3g on the Level of Neurotransmitters GABA and 5-HT in Mouse Brain
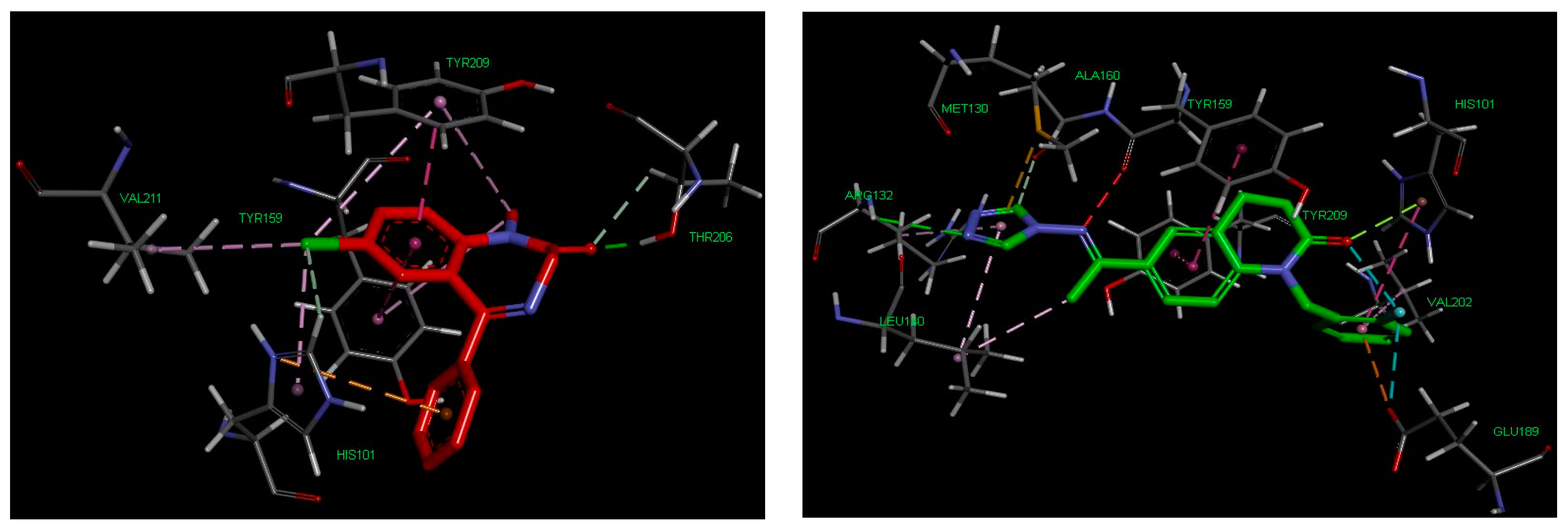
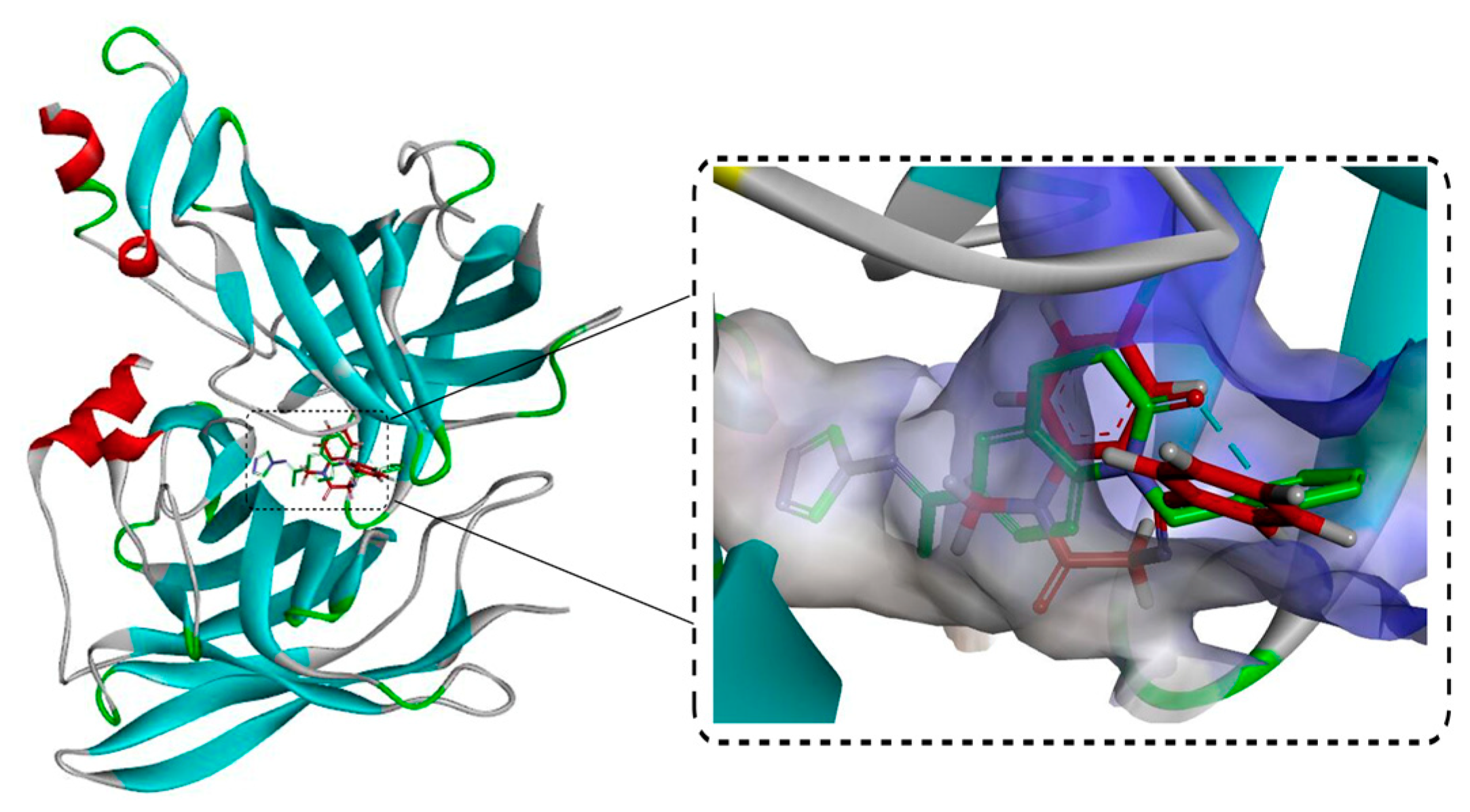
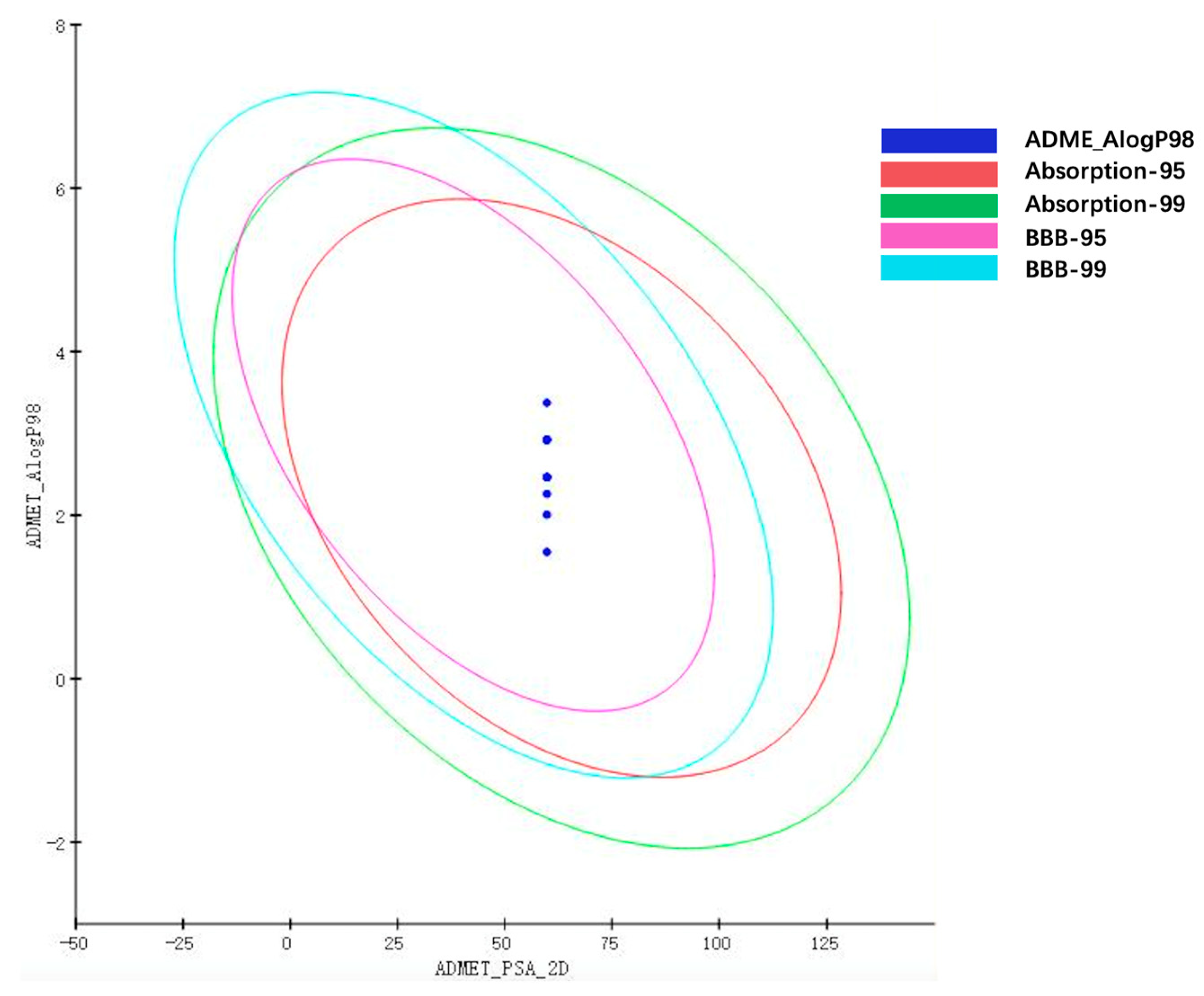
2.5. Molecular Docking, Drug-Like Properties, and Pharmacokinetic Properties Prediction
3. Materials and Methods
3.1. Chemiscal Part
3.1.1. Synthesis Procedure of 6-Acetyl-3,4-dihydroquinolin-2(1H)-one (1)
3.1.2. Synthesis Procedure of N-substituted-6-acetyl-3,4-dihydro-2(1H)-quinolinone (2a–l)
3.1.3. Synthesis Procedure of Target Compounds (3a–3l)
3.2. In Vivo Pharmacology
3.3. Molecular Docking, Drug-Like Properties, and Pharmacokinetic Properties Prediction
3.4. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- World Health Organisation (WHO). Depression and Other Common Mental Disorders Global Health Estimates; WHO: Geneva, Switzerland, 2017; Available online: https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf (accessed on 1 September 2020).
- Singh, G.; Sander, J.W. The global burden of epilepsy report: Implications for low- and middle-income countries. Epilepsy Behav. 2020, 5, 106949. [Google Scholar] [CrossRef] [PubMed]
- Błaszczyk, B.; Czuczwar, S.J. Epilepsy coexisting with depression. Pharmacol. Rep. 2016, 68, 1084–1092. [Google Scholar] [CrossRef] [PubMed]
- De Silva, S.; Isuru, A.; Rodrigo, A.; Kuruppuarachchi, L. Prevalence and correlates of depression in patients with epilepsy in Sri Lanka. Ceylon Med. J. 2021, 66, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Chen, Y.; Hu, Z.; Jiang, J.; Ye, J.; Zhou, Y.; Yu, Z.; Tang, H. Effectiveness of acupuncture for anxiety and depression in irritable bowel syndrome: A protocol for systematic review and meta-analysis. Medicine 2021, 100, e24958. [Google Scholar] [CrossRef] [PubMed]
- Valente, K.D.; Busatto, F.G. Depression and temporal lobe epilepsy represent an epiphenomenon sharing similar neural networks: Clinical and brain structural evidences. Arq. Neuropsiquiatr. 2013, 71, 183–190. [Google Scholar] [CrossRef]
- Butler, T.; Harvey, P.; Cardozo, L.; Zhu, Y.S.; Mosa, A.; Tanzi, E.; Pervez, F. Epilepsy, depression, and growth hormone. Epilepsy Behav. 2019, 94, 297–300. [Google Scholar] [CrossRef]
- Wei, Z.; Ren, L.; Wang, X.; Liu, C.; Cao, M.; Hu, M.; Jiang, Z.; Hui, B.; Xia, F.; Yang, Q.; et al. Network of depression and anxiety symptoms in patients with epilepsy. Epilepsy Res. 2021, 175, 106696. [Google Scholar] [CrossRef]
- Borgmann, M.; Holtkamp, M.; Adli, M.; Behr, J. Depression und Epilepsie: Zwei Krankheitsbilder mit gemeinsamen Ursachen? [Depression and epilepsy: Two clinical pictures with common causes?]. Nervenarzt 2016, 87, 724–730. [Google Scholar] [CrossRef]
- Kanner, A.M. The treatment of depressive disorders in epilepsy: What all neurologists should know. Epilepsia 2013, 54, 3–12. [Google Scholar] [CrossRef]
- Kanner, A.M. Depression in Epilepsy: A Neurobiologic Perspective. Epilepsy Curr. 2005, 5, 21–27. [Google Scholar] [CrossRef]
- Ojemann, L.M.; Friel, P.N.; Trejo, W.J.; Dudley, D.L. Effect of doxepin on seizure frequency in depressed epileptic patients. Neurology 1982, 33, 646–648. [Google Scholar] [CrossRef]
- Rosenstein, D.; Nelson, J.; Jacobs, S. Seizures associated with antidepressants: A review. J. Clin. Psychol. 1993, 54, 289–299. [Google Scholar]
- Liu, B.; Anderson, G.; Mittmann, N.; To, T.; Axcell, T.; Shear, N. Use of selective serotonin-reuptake inhibitors or tricyclic antidepressants and risk of hip fractures in elderly people. Lancet 1998, 351, 1303–1307. [Google Scholar] [CrossRef]
- Warden, S.J.; Robling, A.G.; Sanders, M.S.; Bliziotes, M.M.; Turner, C.H. Inhibition of the serotonin (5-hydroxytryptamine) transporter reduces bone accrual during growth. Endocrinology 2005, 146, 685–693. [Google Scholar] [CrossRef] [PubMed]
- Diem, S.J.; Blackwell, T.L.; Stone, K.L.; Yaffe, K.; Haney, E.M.; Bliziotes, M.M.; Ensrud, K.E. Use of antidepressants and rates of hip bone loss in older women: The study of osteoporotic fractures. Arch. Intern. Med. 2007, 167, 1240–1245. [Google Scholar] [CrossRef] [PubMed]
- Hill, T.; Coupland, C.; Morriss, R.; Arthur, A.; Moore, M.; Hippisley-Cox, J. Antidepressant use and risk of epilepsy and seizures in people aged 20 to 64 years: Cohort study using a primary care database. BMC Psychiatry 2015, 15, 315. [Google Scholar] [CrossRef]
- Maguire, M.J.; Marson, A.G.; Nevitt, S.J. Antidepressants for people with epilepsy and depression. Cochrane Database Syst. Rev. 2021, 4, CD010682. [Google Scholar]
- Górska, N.; Słupski, J.; Cubała, W.J.; Wiglusz, M.S.; Gałuszko-Węgielnik, M. Antidepressants in epilepsy. Neurol. Neurochir. Pol. 2018, 52, 657–661. [Google Scholar] [CrossRef]
- Steinert, T.; Fröscher, W. Epileptic Seizures Under Antidepressive Drug Treatment: Systematic Review. Pharmacopsychiatry 2018, 51, 121–135. [Google Scholar] [CrossRef]
- Guan, L.P.; Quan, Z.S. 3,4-DHQLO and Triazole and Its Related Analogues with Anticonvulsant Effects. Mini Rev. Med. Chem. 2016, 16, 323–342. [Google Scholar] [CrossRef]
- Gao, F.; Zhang, X.; Wang, T.; Xiao, J. Quinolone hybrids and their anti-cancer activities: An overview. Eur. J. Med. Chem. 2019, 165, 59–79. [Google Scholar] [CrossRef]
- Kalkhambkar, R.G.; Aridoss, G.; Kulkarni, G.M. Synthesis and biological studies of some new acrylic acid ethyl esters of quinolinone. Monatsh. Chem. 2012, 143, 1075–1086. [Google Scholar] [CrossRef]
- Kumar, S.; Bawa, S.; Drabu, S.; Gupta, H.; Machwal, L.; Kumar, R. Synthesis, antidepressant and antifungal evaluation of novel 2-chloro-8-methylquinoline amine derivatives. Eur. J. Med. Chem. 2011, 46, 670–675. [Google Scholar] [CrossRef] [PubMed]
- Oshiro, Y.; Sakurai, Y.; Sato, S. 3,4-dihydro-2(1H)-quinolinone as a novel anti- depressant drug: Synthesis and pharmacology of 1-[3-[4-(3-chlorophenyl)-1-piperazinyl]propyl]-3,4-dihydro-5-methoxy-2(1H)-quinolinone and its derivatives. J. Med. Chem. 2000, 43, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Bauman, J.N.; Frederick, K.S.; Sawant, A.; Walsky, R.L.; Cox, L.M.; Obach, R.S.; Kalgutkar, A.S. Comparison of the bioactivation potential of the antidepressant and hepatotoxin nefazodone with aripiprazole, a structural analog and marketed drug. Drug Metab. Dispos. 2008, 36, 1016–1029. [Google Scholar] [CrossRef]
- Weber, J.; Lyseng-Williamson, K.A.; Scott, L.J. Aripiprazole: In major depressive disorder. CNS Drugs 2008, 22, 807–813. [Google Scholar] [CrossRef]
- Furukawa, Y.; Hamza, T.; Cipriani, A.; Furukawa, T.A.; Salanti, G.; Ostinelli, E.G. Optimal dose of aripiprazole for augmentation therapy of antidepressant-refractory depression: Preliminary findings based on a systematic review and dose-effect meta-analysis. Br. J. Psychiatry 2022, 221, 440–447. [Google Scholar] [CrossRef]
- Deng, X.Q.; Song, M.X.; Zheng, Y.; Quan, Z.S. Design, synthesis and evaluation of the antidepressant and anticonvulsant activities of triazole-containing quinolinones. Eur. J. Med. Chem. 2014, 73, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Martinez, G.R.; Walker, K.A.; Hirschfeld, D.R.; Bruno, J.J.; Yang, D.S.; Maloney, P.J. 3,4-Dihydroquinolin-2(1H)-ones as combined inhibitors of thromboxane A2 synthase and cAMP phosphodiesterase. J. Med. Chem. 1992, 35, 620–628. [Google Scholar] [CrossRef]
- Porsolt, R.D.; Bertin, A.; Jalfre, M. Behavioral despair in mice: A primary screening test for antidepressants. Arch. Int. Pharmacodyn. Ther. 1977, 229, 327–336. [Google Scholar]
- Cryan, J.F.; Valentino, R.J.; Lucki, I. Assessing substrates underlying the. behavioral effects of antidepressants using the modified rat forced swimming test. Neurosci. Biobehav. Rev. 2005, 29, 547–569. [Google Scholar] [CrossRef]
- Bourin, M.; Chenu, F.; Ripoll, N.; David, D.J. A proposal of decision tree to screen putative antidepressants using forced swim and tail suspension tests. Behav. Brain. Res. 2005, 164, 266–269. [Google Scholar] [CrossRef]
- Yankelevitch-Yahav, R.; Franko, M.; Huly, A.; Doron, R. The forced swim test as a model of depressive-like behavior. J. Vis. Exp. 2015, 97, 52587. [Google Scholar]
- Can, A.; Dao, D.T.; Terrillion, C.E.; Piantadosi, S.C.; Bhat, S.; Gould, T.D. The tail suspension test. J. Vis. Exp. 2012, 59, e3769. [Google Scholar] [CrossRef]
- Kraeuter, A.K.; Guest, P.C.; Sarnyai, Z. The Open Field Test for Measuring Locomotor Activity and Anxiety-Like Behavior. Methods Mol. Biol. 2019, 1916, 99–103. [Google Scholar] [PubMed]
- Yuen, E.S.; Trocóniz, I.F. Can pentylenetetrazole and maximal electroshock rodent seizure models quantitatively predict antiepileptic efficacy in humans? Seizure 2015, 24, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Sills, G.J.; Rogawski, M.A. Mechanisms of action of currently used antiseizure drugs. Neuropharmacology 2020, 168, 107966. [Google Scholar] [CrossRef] [PubMed]
- Song, M.X.; Rao, B.-Q.; Cheng, B.B.; Wu, Y.; Zeng, H.; Luo, Y.; Deng, X.Q. Design, Synthesis and Evaluation of the Antidepressant and Anticonvulsant Activities of Triazole-Containing Benzo[d]oxazoles. CNS Neurol. Disord. Drug Targets 2017, 16, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Song, M.X.; Huang, Y.S.; Zhou, Q.G.; Deng, X.Q.; Yao, X.D. Synthesis of ring-opened derivatives of triazole-containing quinolinones and their antidepressant and anticonvulsant activities. Bioorg. Chem. 2021, 106, 104505. [Google Scholar] [CrossRef]
- Kendell, S.F.; Krystal, J.H.; Sanacora, G. GABA and glutamate systems as therapeutic targets in depression and mood disorders. Expert Opin. Ther. Targets. 2005, 9, 153–168. [Google Scholar] [CrossRef]
- Croarkin, P.E.; Levinson, A.J.; Daskalakis, Z.J. Evidence for GABAergic inhibitory deficits in major depressive disorder. Neurosci. Biobehav. Rev. 2011, 35, 818–825. [Google Scholar] [CrossRef] [PubMed]
- Walter, M.; Henning, A.; Grimm, S.; Schulte, R.F.; Beck, J.; Dydak, U.; Schnepf, B.; Boeker, H.; Boesiger, P.; Northoff, G. The relationship between aberrant neuronal activation in the pregenual anterior cingulate, altered glutamatergic metabolism, and anhedonia in major depression. Arch. Gen. Psychiatry 2009, 66, 478–486. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.J.; Wang, S.B.; Quan, Z.S. Synthesis and antidepressant activities of 4-(substituted-phenyl)tetrazolo[1,5-a]quinazolin-5(4H)-ones and their derivatives. Mol. Divers. 2015, 19, 817–828. [Google Scholar] [CrossRef] [PubMed]
- Keppel Hesselink, J.M. Phenytoin: A step by step insight into its multiple mechanisms of action—80 years of mechanistic studies in neuropharmacology. J. Neurol. 2017, 264, 2043–2047. [Google Scholar] [CrossRef]
- Collins, G.S. Effect of aminooxyacetic acid, thiosemicarbazide and haloperidol on the metabolism and half-lives of glutamate and GABA in rat brain. Biochem. Pharmacol. 1973, 22, 101–111. [Google Scholar] [CrossRef]
| Compd. | -R | Maximal Electroshock Test | Pentylenetetrazole Test | Rotarod Test | |||
|---|---|---|---|---|---|---|---|
| 0.5 h | 4 h | 0.5 h | 4 h | 0.5 h | 4 h | ||
| 3a | -C3H7 | 300 | - | - | - | - | - |
| 3b | -C4H9 | 300 | - | - | - | - | - |
| 3c | -C5H11 | 100 | 300 | - | - | 300 | - |
| 3d | -C6H13 | 300 | 300 | - | - | 300 | - |
| 3e | -C7H15 | 300 | - | - | - | - | - |
| 3f | -CH2C6H5 | 100 | 300 | - | - | 300 | - |
| 3g | -CH2C6H4(2-F) | 100 | - | - | - | - | - |
| 3h | -CH2C6H4(3-F) | 300 | - | - | - | - | - |
| 3i | -CH2C6H4(4-F) | 300 | - | - | - | - | - |
| 3j | -CH2C6H4(2-Cl) | 300 | - | - | - | - | - |
| 3k | -CH2C6H4(3-CI) | - | - | - | - | - | - |
| 3l | -CH2C6H4(4-CI) | 300 | 300 | - | - | 300 | - |
| Carbamazepine | - | 30 | 100 | - | - | 100 | 100 |
| Valproate | - | 300 | - | 300 | - | - | - |
| Compounds | ED50 a | TD50 b | PI c |
|---|---|---|---|
| 3c | 63.4 (58.0–69.3) | 264.1 (240.1–290.5) | 4.2 |
| 3f | 78.9 (71.7–86.8) | 253.5 (230.5–278.8) | 3.2 |
| 3g | 84.9 (75.16–95.83) | 439.9 (394.45–490.70) | 5.2 |
| Carbamazepine | 8.7 (8.3–10.2) | 41.5 (38.1–46.3) | 4.8 |
| Valproate | 288 (257–329) | 432 (370–492) | 1.5 |
| Compound | MW | CLogP | HBD | HBA | n-ROTB | Lipinski’s Violation |
|---|---|---|---|---|---|---|
| Rule | 500 | ≤5 | ≤5 | <10 | ≤10 | ≤1 |
| 3a | 297.355 | 1.549 | 0 | 4 | 4 | 0 |
| 3b | 311.382 | 2.005 | 0 | 4 | 5 | 0 |
| 3c | 325.408 | 2.462 | 0 | 4 | 6 | 0 |
| 3d | 339.435 | 2.918 | 0 | 4 | 7 | 0 |
| 3e | 353.461 | 3.374 | 0 | 4 | 8 | 0 |
| 3f | 345.398 | 2.26 | 0 | 4 | 4 | 0 |
| 3g | 363.388 | 2.466 | 0 | 4 | 4 | 0 |
| 3h | 363.388 | 2.466 | 0 | 4 | 4 | 0 |
| 3i | 363.388 | 2.466 | 0 | 4 | 4 | 0 |
| 3j | 379.843 | 2.925 | 0 | 4 | 4 | 0 |
| 3k | 379.843 | 2.925 | 0 | 4 | 4 | 0 |
| 3l | 379.843 | 2.925 | 0 | 4 | 4 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, W.; Song, M.; Hua, Y.; Zhu, Y.; Liu, W.; Xia, Q.; Deng, X.; Huang, Y. Design, Synthesis, and Pharmacology of New Triazole-Containing Quinolinones as CNS Active Agents. Molecules 2023, 28, 1987. https://doi.org/10.3390/molecules28041987
Zhao W, Song M, Hua Y, Zhu Y, Liu W, Xia Q, Deng X, Huang Y. Design, Synthesis, and Pharmacology of New Triazole-Containing Quinolinones as CNS Active Agents. Molecules. 2023; 28(4):1987. https://doi.org/10.3390/molecules28041987
Chicago/Turabian StyleZhao, Wennan, Mingxia Song, Yi Hua, Yangnv Zhu, Wenli Liu, Qishan Xia, Xianqing Deng, and Yushan Huang. 2023. "Design, Synthesis, and Pharmacology of New Triazole-Containing Quinolinones as CNS Active Agents" Molecules 28, no. 4: 1987. https://doi.org/10.3390/molecules28041987
APA StyleZhao, W., Song, M., Hua, Y., Zhu, Y., Liu, W., Xia, Q., Deng, X., & Huang, Y. (2023). Design, Synthesis, and Pharmacology of New Triazole-Containing Quinolinones as CNS Active Agents. Molecules, 28(4), 1987. https://doi.org/10.3390/molecules28041987





