Safe and Effective Antioxidant: The Biological Mechanism and Potential Pathways of Ergothioneine in the Skin
Abstract
:1. Introduction
2. The Structural Foundation of Ergothioneine
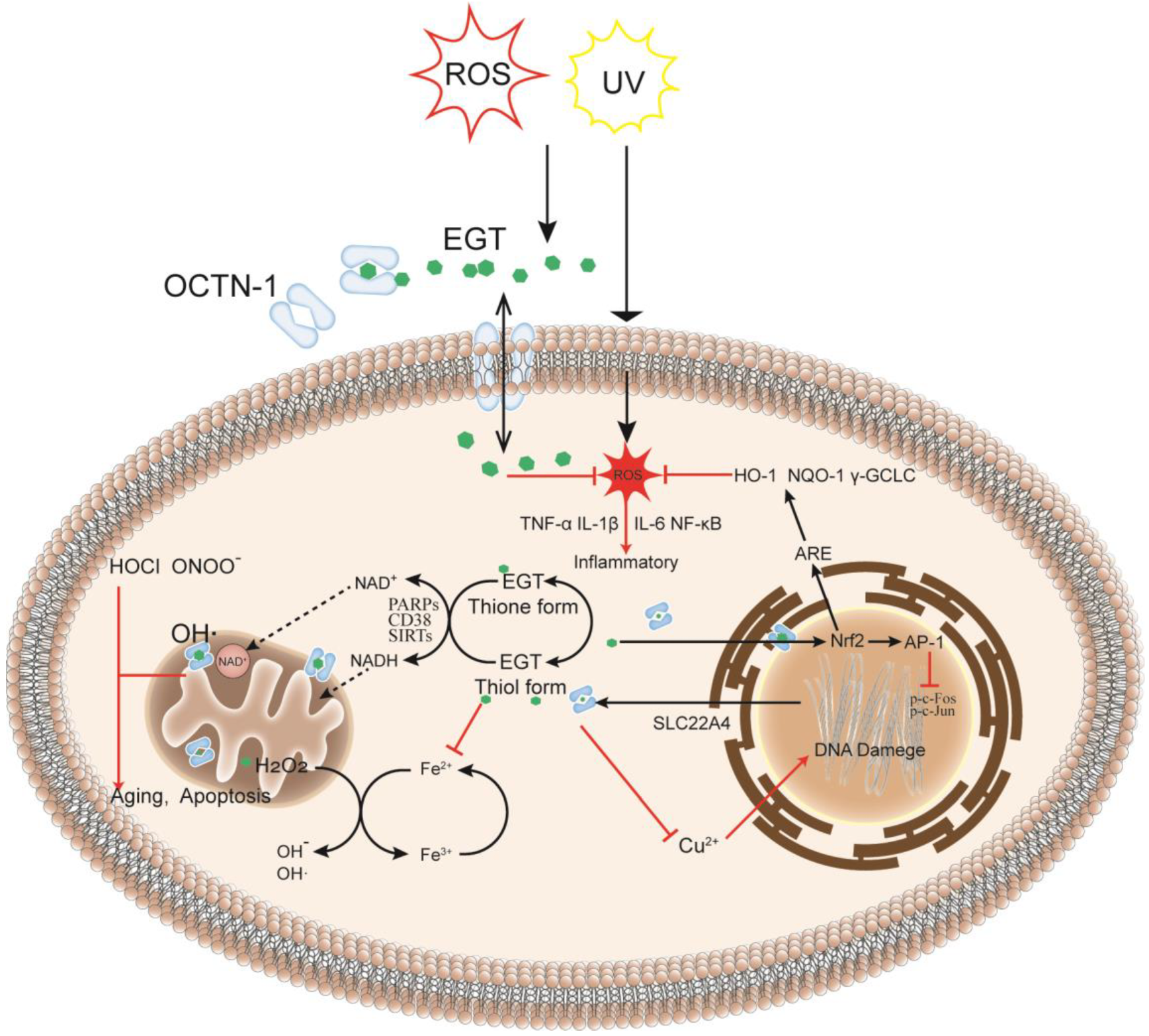
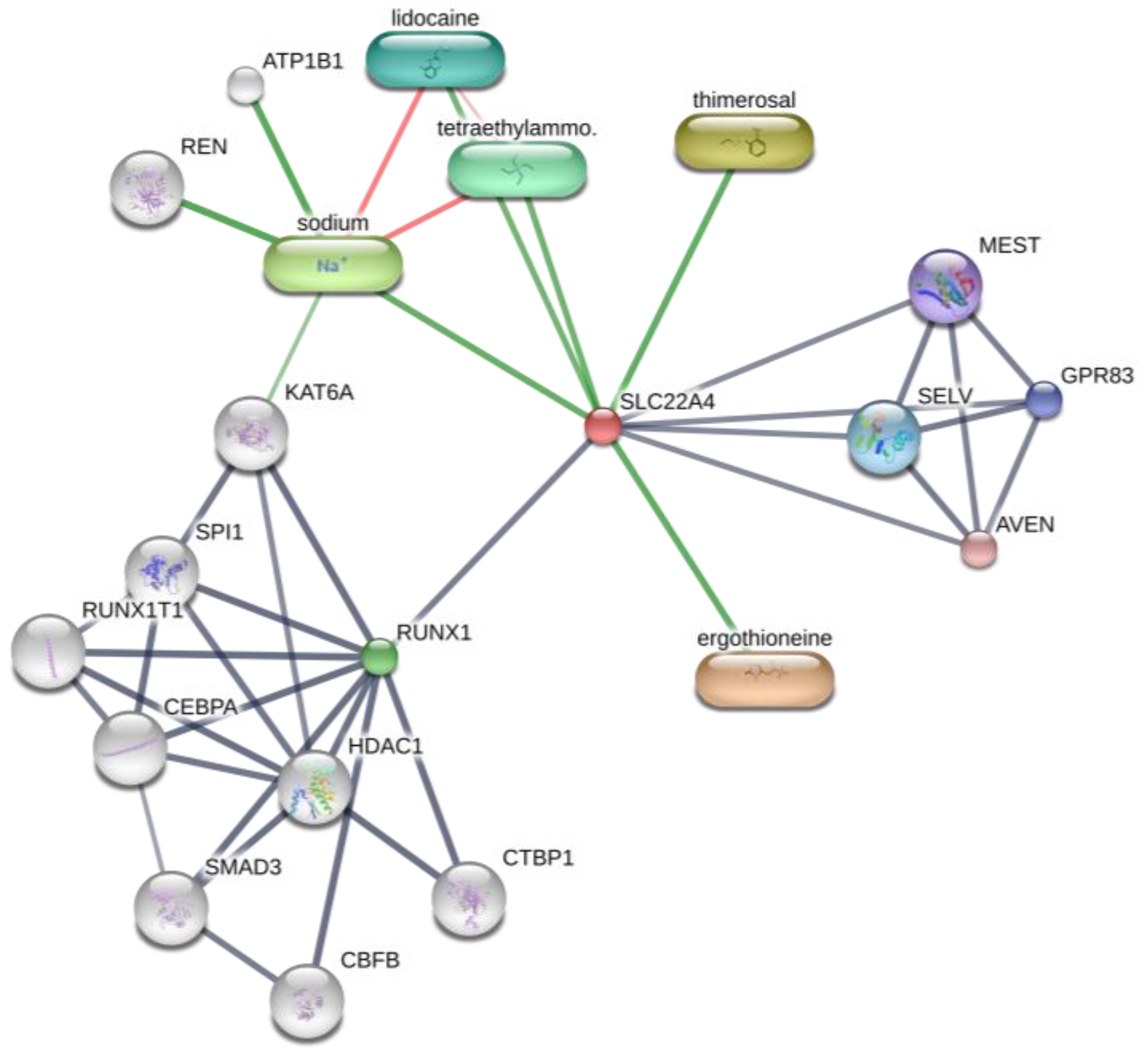
3. Transport and Metabolism Mechanism of Ergothioneine
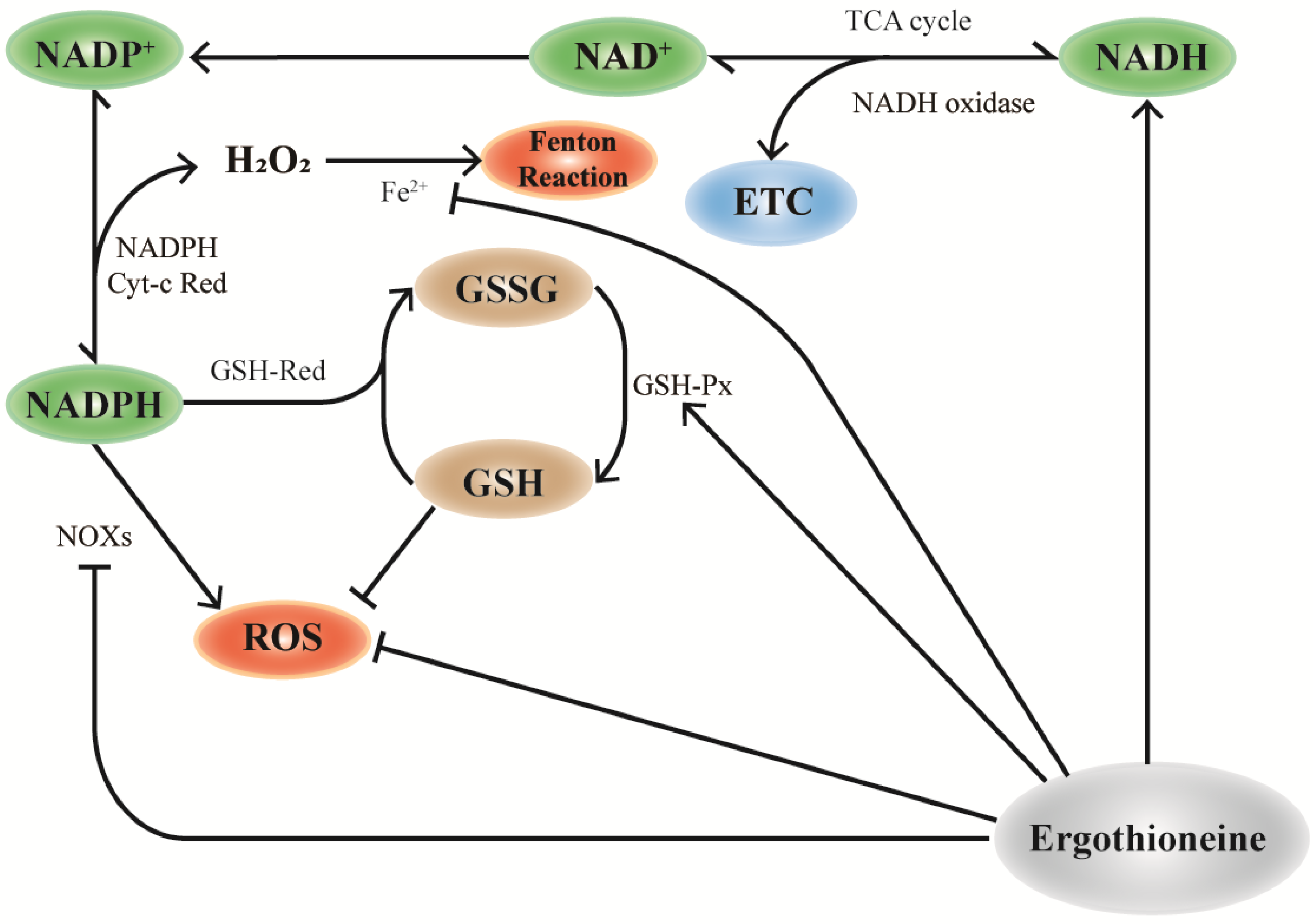
4. Participation in the Antioxidant Defense System
5. Targeted Intelligent Protection to Mitochondria
6. The Biological Effect of Ergothioneine
6.1. Antioxidant Effect
6.2. Anti-Aging Effect
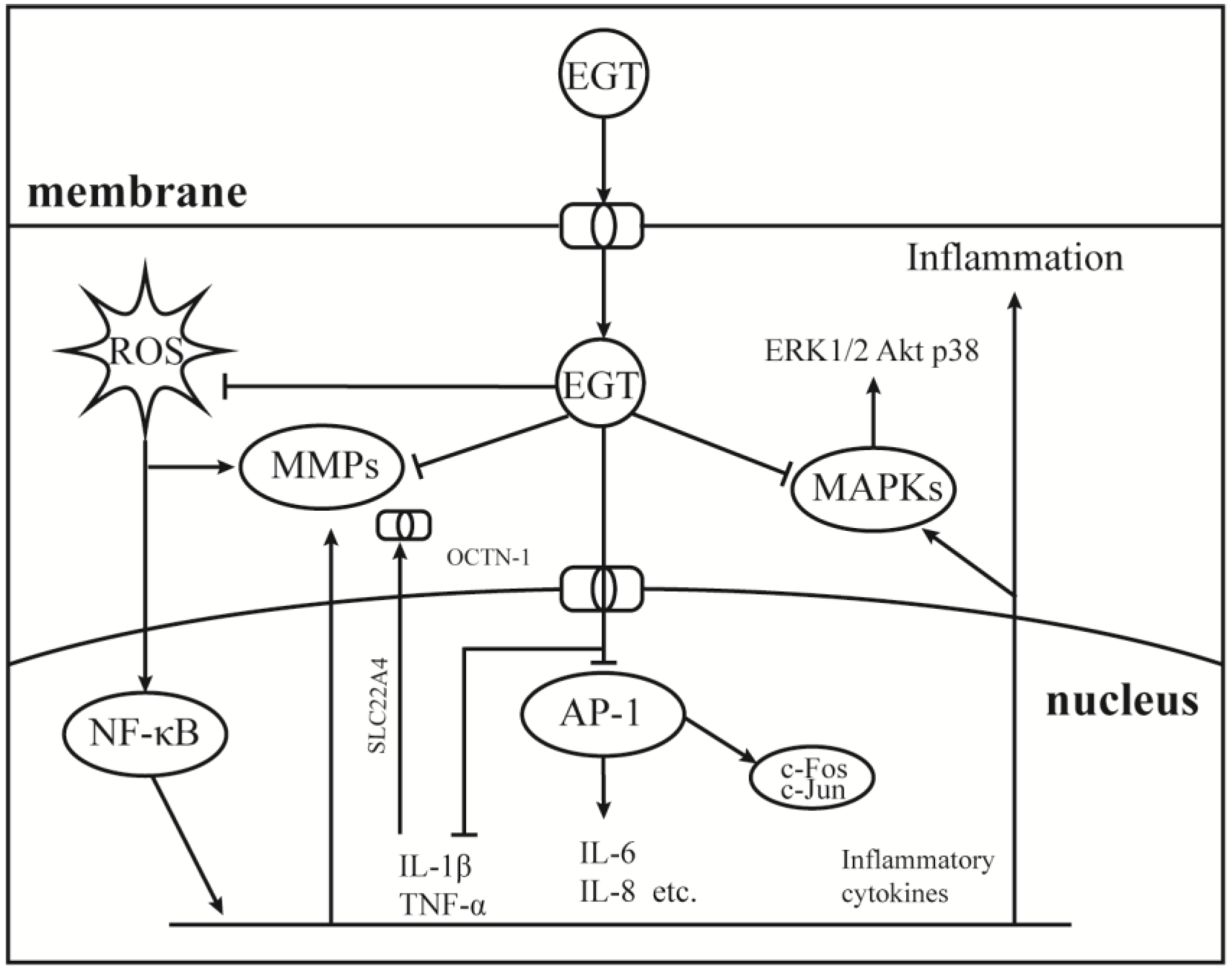
6.3. Anti-Inflammatory Action and Immunomodulation
6.4. Protective Effect on Skin Barrier
6.5. Protective Effect on UV Exposure
6.6. Inhibition Effect on Melanin
7. The Application of Ergothioneine in Cosmetics
8. Conclusions and Perspectives
- What negative effect can EGT deficiency or excess cause to the skin?
- What is the transdermal osmotic rate of EGT in each skin layer? Can OCTN-1 can promote the penetration and absorption of EGT?
- What is the central role of EGT in the body’s antioxidant network? What is a possible mechanism of action?
- Can EGT transport and penetration be enhanced by adding artificially extracted or synthetic OCTN-1?
- There are few studies on the effect of EGT in inhibiting melanogenesis, and blocking the melanogenesis pathway is not yet clear.
- Most of the evidence is based on animal experiments or cell experiments in vitro, and human and clinical evidence is lacking, especially evidence for external application on the skin.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Oxidant | Test System | Effective Concentration (IC50) | Reference |
|---|---|---|---|
| DPPH radicals | 0.5 mL of a 0.4 mM DPPH ethanol solution was increased to a final volume of 2 mL by distilled water as a control mixture. | 0.07 mg/mL | [125] |
| Different volumes (1.5 to 7.5 μL) of the mushroom extract were mixed with 0.5 mL of a 0.4 mM DPPH ethanol solution and increased to a final volume of 2 mL with distilled water as a control mixture. | 2.9 μL mushroom extract (17.6 mg EGT). | [126] | |
| 150 μL of DPPH was added to 50 μL of PBS mixed with 50 μL EGT. | 6.110 ± 0.305 mg/mL | [120] | |
| Different volumes (2 to 80 μL) of the solution were mixed with 0.5 mL of a 0.4 mM DPPH ethanol solution and increased to a final volume of 2 mL by distilled water as a control mixture. | 0.008 mg/mL. | [127] | |
| 0.9 mL of a 60 μM DPPH ethanol solution was increased to a final volume of 1 mL by distilled water as a control mixture. | 0.6531 mg/mL EGT in the rhizome extracts | [128] | |
| ABTS radicals | Different concentrations (10 μL) of the antioxidant were mixed with 1.0 mL of diluted ABTS solution (A734nm = 0.700 ± 0.020) | 0.7411 mg/mL EGT in the rhizome extracts | [128] |
| 2.80 mL of 7 mM ABTS working solution was diluted to 65 mL with acetic acid buffer (pH 4). | 50 μg/mL (58.58%) | [129] | |
| 0.1 mL mushroom extract were mixed with 3.9 mL of diluted ABTS solution (A734nm = 0.700 ± 0.020). | 15.29 μg/mg mushroom extract (96%) | [68] | |
| Peroxyl radicals | Peroxyl radicals were generated by thermal homolysis of 20 mM ABAP at 35 °C in 100 mM potassium phosphate buffer, pH 7.4. | 11.74 μM | [51] |
| Hydroxyl radicals | 10 μL of EGT and ascorbic acid at different concentrations, 10 μL of H2O2, 10 μL of CuCl, 10 μL of phenanthroline, and 150 μL of a mixture containing 1 mM luminol (1 mL) and carbonate buffer (pH 8.5, 17 mL) were dissolved and mixed. | 70.31 ± 1.59 μg/mL | [130] |
| Peroxynitrite radicals | Peroxynitrite was generated from the decomposition of SIN−1 in the presence of 0.2 mM KMBA, 100 mM potassium phosphate buffer, pH 7.4, and 0.1 mM DTPA, at 35 °C. | 15.8 μM | [51] |
| Superoxide anions | 10 μL of EGT and ascorbic acid at different concentrations, 10 μL of H2O2, 10 μL of CuCl, 10 μL of phenanthroline, and 150 μL of a mixture containing 1 mM luminol (10 mL) and carbonate buffer (pH 10.0, 20 mL) were dissolved and mixed. | 160.44 ± 0.32 μg/mL | [130] |
| Hydrogen peroxides | 10 μL of EGT and ascorbic acid at different concentrations, 10 μL of 6% H2O2, and 150 μL of a mixture containing 1 mM luminol (1 mL) and carbonate buffer (pH 9.5, 17 mL) were dissolved and mixed. | 11.65 ± 0.31 μg/mL | [130] |
| 500 mg/mL phosphatidylcholine liposomes were pretreated with 4.6, 22.9, and 57.3 μg/mL EGT and then treated with 10 mM alloxan. | 4.6 μg/mL (67%) | [112] | |
| Lipid peroxidation | 0.1 mL of 500 mM catechol as a substrate, 0.1 mL of 500 mM L-(-)-proline, 0.2 mL hemolymph, 2.7 mL of a 50 mM phosphate buffer (pH 6.8), and 0.1 mL of 100 units/mL mushroom PPO in a total volume of 3.2 mL. | 122.5 μM | [125] |
| Product Name | Brand | Main Function | Sources (Accessed on 25 January 2023) |
|---|---|---|---|
| Nutritious Super-Pomegranate Moisturizer Radiant Energy Night Creme/Mask | Estée Lauder | Antioxidant, recharges skin’s radiance | https://www.esteelauder.com/ |
| DayWear Moisturizer Multi-Protection Anti-Oxidant 24h-Moisture Creme SPF 15 | Estée Lauder | Antioxidant, diminish first signs of aging | https://www.esteelauder.com/ |
| NightWear Plus MoisturizerAnti-Oxidant Night Detox Crème | Estée Lauder | Antioxidant, detoxify, soothe, hydrate | https://www.esteelauder.com/ |
| Perfectionist Pro Serum | Estée Lauder | Anti-aging, skin looking smoother | https://www.esteelauder.com/ |
| Re-Nutriv Ultra Radiance Liquid Makeup SPF 20 | Estée Lauder | Anti-ultraviolet, look radiant | https://www.esteelauder.com/ |
| Rapid Firm + Lift Treatment with Acetyl Hexapeptide−8 NightWear Plus Moisturizer | Estée Lauder | Antioxidant, anti-aging, repair | https://www.esteelauder.com/ |
| Skin Caviar Essence-In-Lotion | La Prairie | Hydrate skin, make skin vitalized | https://www.laprairie.com/ |
| The Perfecting Primer | La MER | Improve skin’s texture and tone | https://www.cremedelamer.com/ |
| Prevage Anti-aging Hydrating Fluid | Elizabeth Arden | Antioxidant, restore skin’s natural defenses | https://www.cremedelamer.com/ |
| Prevage Anti-Aging + Intensive Repair Daily Serum | Elizabeth Arden | Anti-aging, brightened the look of skin | https://www.cremedelamer.com/ |
| DIORSNOW Essence of light micro-infused lotion | Dior | Moisturizing, maintain skin balance | https://www.dior.com/ |
| DIORSNOW Essence of light purifying brightening foam | Dior | Cleanse the skin, brightening | https://www.dior.com/ |
| DIORSNOW Ultimate UV Shield tone up—SPF 50+ PA+++ | Dior | Anti-ultraviolet, improve skin’s tone | https://www.dior.com/ |
| A PERFECT WORLD™ SPF 40 Age-Defense Moisturizer with White Tea | Origins | Anti-ultraviolet, age prevention | https://www.origins.com/ |
| Dr. Andrew Weil for Origins™ Mega-Mushroom Weightless Hydrating Moisturizer | Origins | Barrier Boosting, hydration boost | https://www.origins.com/ |
| Energizing Gel Cream | Lab Series | Anti-aging, hydration, revive tired skin | https://www.labseries.com/ |
| Universal Defense Broad Spectrum SPF 50+ Sunscreen | Shiseido | Anti-ultraviolet, against stressors | https://www.shiseido.com/ |
| UV Glow Broad-Spectrum SPF 36 | EltaMD | Anti-ultraviolet, anti-aging | https://www.meyerspa.com/ |
| Prep + Prime Face Protect Lotion SPF 50 | MAC | Anti-ultraviolet, antioxidant | https://www.maccosmetics.com/ |
| Stimulskin Plus Multi-Corrective Divine Splash Mask Lotion | Darphin | Minimizes major signs of aging | https://www.darphin.com/ |
| Lumière Essentielle Instant Purifying & Illuminating Mask | Darphin | Anti-aging, refine skin texture | https://www.darphin.com/ |
| Repairwear Laser Focus™ Wrinkle Correcting Eye Cream | Clinique | Diminish fine lines and wrinkles, hydrates | https://www.clinique.com/ |
| Superdefense Broad Spectrum SPF 25 Fatigue + 1st Signs of Age Multi-Correcting Cream | Clinique | Anti-ultraviolet, fights fatigue and first signs of aging | https://www.clinique.com/ |
References
- Tanret, C. Sur une base nouvelle retiree du seigle ergote, l’ergothioneine. Rend. Acad. Sci. 1909, 149, 222–224. [Google Scholar]
- Forster, R.; Spezia, F.; Papineau, D.; Sabadie, C.; Erdelmeier, I.; Moutet, M.; Yadan, J.C. Reproductive safety evaluation of L-Ergothioneine. Food Chem Toxicol. 2015, 80, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Fujitani, Y.; Alamgir, K.M.; Tani, A. Ergothioneine production using Methylobacterium species, yeast, and fungi. J. Biosci. Bioeng. 2018, 126, 715–722. [Google Scholar] [CrossRef] [PubMed]
- Stampfli, A.R.; Blankenfeldt, W.; Seebeck, F.P. Structural basis of ergothioneine biosynthesis. Curr. Opin. Struct. Biol. 2020, 65, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Yan, Q.; Huang, H.; Zhang, X. In Vitro Reconstitution of a Bacterial Ergothioneine Sulfonate Catabolic Pathway. ACS Catal. 2022, 12, 4825–4832. [Google Scholar] [CrossRef]
- Melville, D.B. Ergothioneine, Vitamins & Hormones; Elsevier: Amsterdam, The Netherlands, 1959; pp. 155–204. [Google Scholar]
- Halliwell, B. Reflections of an aging free radical. Free Radic. Biol. Med. 2020, 161, 234–245. [Google Scholar] [CrossRef] [PubMed]
- Cheah, I.K.; Tang, R.M.; Yew, T.S.; Lim, K.H.; Halliwell, B. Administration of Pure Ergothioneine to Healthy Human Subjects: Uptake, Metabolism, and Effects on Biomarkers of Oxidative Damage and Inflammation. Antioxid. Redox Signal. 2017, 26, 193–206. [Google Scholar] [CrossRef]
- Kondoh, H.; Teruya, T.; Yanagida, M. Metabolomics of human fasting: New insights about old questions. Open Biol. 2020, 10, 200176. [Google Scholar] [CrossRef]
- Paul, B.D.; Snyder, S.H. The unusual amino acid L-ergothioneine is a physiologic cytoprotectant. Cell Death Differ. 2010, 17, 1134–1140. [Google Scholar] [CrossRef]
- Repine, J.E.; Elkins, N.D. Effect of ergothioneine on acute lung injury and inflammation in cytokine insufflated rats. Prev. Med. 2012, 54, S79–S82. [Google Scholar] [CrossRef]
- Cheah, I.K.; Tang, R.; Ye, P.; Yew, T.S.; Lim, K.H.; Halliwell, B. Liver ergothioneine accumulation in a guinea pig model of non-alcoholic fatty liver disease. A possible mechanism of defence? Free Radic. Res. 2016, 50, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Cheah, I.K.; Halliwell, B. Could ergothioneine aid in the treatment of coronavirus patients? Antioxidants 2020, 9, 595. [Google Scholar] [CrossRef] [PubMed]
- Kawano, H.; Otani, M.; Takeyama, K.; Kawai, Y.; Mayumi, T.; Hama, T. Studies on ergothioneine. VI. Distribution and fluctuations of ergothioneine in rats. Chem. Pharm. Bull. 1982, 30, 1760–1765. [Google Scholar] [CrossRef] [PubMed]
- Tang, R.M.Y.; Cheah, I.K.; Yew, T.S.K.; Halliwell, B. Distribution and accumulation of dietary ergothioneine and its metabolites in mouse tissues. Sci. Rep. 2018, 8, 1601. [Google Scholar] [CrossRef] [PubMed]
- Halliwell, B.; Cheah, I.K.; Drum, C.L. Ergothioneine, an adaptive antioxidant for the protection of injured tissues? A hypothesis. Biochem. Biophys. Res. Commun. 2016, 470, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Kroepfl, N.; Francesconi, K.A.; Schwerdtle, T.; Kuehnelt, D. Selenoneine and ergothioneine in human blood cells determined simultaneously by HPLC/ICP-QQQ-MS. J. Anal. At. Spectrometry 2019, 34, 127–134. [Google Scholar] [CrossRef]
- Kato, Y.; Kubo, Y.; Iwata, D.; Kato, S.; Sudo, T.; Sugiura, T.; Kagaya, T.; Wakayama, T.; Hirayama, A.; Sugimoto, M.; et al. Gene knockout and metabolome analysis of carnitine/organic cation transporter OCTN1. Pharm. Res. 2010, 27, 832–840. [Google Scholar] [CrossRef]
- Peckelsen, K.; Martens, J.; Czympiel, L.; Oomens, J.; Berden, G.; Grundemann, D.; Meijer, A.; Schafer, M. Ergothioneine and related histidine derivatives in the gas phase: Tautomer structures determined by IRMPD spectroscopy and theory. Phys. Chem. Chem. Phys. 2017, 19, 23362–23372. [Google Scholar] [CrossRef]
- Oumari, M.; Goldfuss, B.; Stoffels, C.; Schmalz, H.G.; Grundemann, D. Regeneration of ergothioneine after reaction with singlet oxygen. Free Radic. Biol. Med. 2019, 134, 498–504. [Google Scholar] [CrossRef]
- Leisinger, F.; Burn, R.; Meury, M.; Lukat, P.; Seebeck, F.P. Structural and Mechanistic Basis for Anaerobic Ergothioneine Biosynthesis. J. Am. Chem. Soc. 2019, 141, 6906–6914. [Google Scholar] [CrossRef]
- Thiele, J.J.; Dreher, F.; Packer, L. Antioxidant defense systems in skin. J. Toxicol. Cutan. Ocul. Toxicol. 2002, 21, 119–160. [Google Scholar] [CrossRef]
- Packer, L.; Hiramatsu, M.; Yoshikawa, T. Antioxidant Food Supplements in Human Health; Elsevier: Amsterdam, The Netherlands, 1999. [Google Scholar] [CrossRef]
- Bae, J.-T.; Lee, C.-H.; Lee, G.-S.; Kim, J.-H.; Hong, J.-T. Glycation Inhibitory and Antioxidative Activities of Ergothioneine. J. Soc. Cosmet. Sci. Korea 2019, 45, 151–159. [Google Scholar] [CrossRef]
- Hseu, Y.C.; Vudhya Gowrisankar, Y.; Chen, X.Z.; Yang, Y.C.; Yang, H.L. The Antiaging Activity of Ergothioneine in UVA-Irradiated Human Dermal Fibroblasts via the Inhibition of the AP-1 Pathway and the Activation of Nrf2-Mediated Antioxidant Genes. Oxid. Med. Cell Longev. 2020, 2020, 2576823. [Google Scholar] [CrossRef] [PubMed]
- Aruoma, O.I.; Spencer, J.P.; Mahmood, N. Protection against oxidative damage and cell death by the natural antioxidant ergothioneine. Food Chem. Toxicol. 1999, 37, 1043–1053. [Google Scholar] [CrossRef]
- Colognato, R.; Laurenza, I.; Fontana, I.; Coppede, F.; Siciliano, G.; Coecke, S.; Aruoma, O.I.; Benzi, L.; Migliore, L. Modulation of hydrogen peroxide-induced DNA damage, MAPKs activation and cell death in PC12 by ergothioneine. Clin. Nutr. 2006, 25, 135–145. [Google Scholar] [CrossRef]
- Ames, B.N. Prolonging healthy aging: Longevity vitamins and proteins. Proc. Natl. Acad. Sci. USA 2018, 115, 10836–10844. [Google Scholar] [CrossRef]
- Gründemann, D.; Harlfinger, S.; Golz, S.; Geerts, A.; Lazar, A.; Berkels, R.; Jung, N.; Rubbert, A.; Schömig, E. Discovery of the ergothioneine transporter. Proc. Natl. Acad. Sci. USA 2005, 102, 5256–5261. [Google Scholar] [CrossRef]
- Kitsanayanyong, L.; Pahila, J.; Ishikawa, Y.; Koyama, T.; Kiron, V.; Ohshima, T. Functional identification of ergothioneine transporter in rainbow trout (Oncorhynchus mykiss). Comp. Biochem. Physiol. B Biochem. Mol. Biol. 2021, 256, 110631. [Google Scholar] [CrossRef]
- Li, R.W.; Yang, C.; Sit, A.S.; Kwan, Y.W.; Lee, S.M.; Hoi, M.P.; Chan, S.W.; Hausman, M.; Vanhoutte, P.M.; Leung, G.P. Uptake and protective effects of ergothioneine in human endothelial cells. J. Pharmacol. Exp. Ther. 2014, 350, 691–700. [Google Scholar] [CrossRef]
- Finch, M. Assessment of skin in older people: As the largest organ in the body, the skin can offer valuable information about the general health of an older person. Nurs. Older People 2003, 15, 29–31. [Google Scholar] [CrossRef]
- Markova, N.G.; Karaman-Jurukovska, N.; Dong, K.K.; Damaghi, N.; Smiles, K.A.; Yarosh, D.B. Skin cells and tissue are capable of using L-ergothioneine as an integral component of their antioxidant defense system. Free Radic. Biol. Med. 2009, 46, 1168–1176. [Google Scholar] [CrossRef] [PubMed]
- Lamhonwah, A.M.; Tein, I. Novel localization of OCTN1, an organic cation/carnitine transporter, to mammalian mitochondria. Biochem. Biophys. Res. Commun. 2006, 345, 1315–1325. [Google Scholar] [CrossRef] [PubMed]
- Blander, G.; Bhimavarapu, A.; Mammone, T.; Maes, D.; Elliston, K.; Reich, C.; Matsui, M.S.; Guarente, L.; Loureiro, J.J. SIRT1 promotes differentiation of normal human keratinocytes. J. Investig. Dermatol. 2009, 129, 41–49. [Google Scholar] [CrossRef] [PubMed]
- D’Onofrio, N.; Martino, E.; Balestrieri, A.; Mele, L.; Cautela, D.; Castaldo, D.; Balestrieri, M.L. Diet-derived ergothioneine induces necroptosis in colorectal cancer cells by activating the SIRT3/MLKL pathway. FEBS Lett. 2022, 596, 1313–1329. [Google Scholar] [CrossRef] [PubMed]
- Makiishi, S.; Furuichi, K.; Yamamura, Y.; Sako, K.; Shinozaki, Y.; Toyama, T.; Kitajima, S.; Iwata, Y.; Sakai, N.; Shimizu, M. Carnitine/organic cation transporter 1 precipitates the progression of interstitial fibrosis through oxidative stress in diabetic nephropathy in mice. Sci. Rep. 2021, 11, 9093. [Google Scholar] [CrossRef] [PubMed]
- Martin-Oliva, D.; Aguilar-Quesada, R.; O’Valle, F.; Munoz-Gamez, J.A.; Martinez-Romero, R.; Garcia Del Moral, R.; de Almodovar, J.M.R.; Villuendas, R.; Piris, M.A.; Oliver, F.J. Inhibition of poly(ADP-ribose) polymerase modulates tumor-related gene expression, including hypoxia-inducible factor-1 activation, during skin carcinogenesis. Cancer Res. 2006, 66, 5744–5756. [Google Scholar] [CrossRef] [PubMed]
- Kehe, K.; Raithel, K.; Kreppel, H.; Jochum, M.; Worek, F.; Thiermann, H. Inhibition of poly(ADP-ribose) polymerase (PARP) influences the mode of sulfur mustard (SM)-induced cell death in HaCaT cells. Arch. Toxicol. 2008, 82, 461–470. [Google Scholar] [CrossRef]
- Geierstanger, B.H.; Kagawa, T.F.; Chen, S.L.; Quigley, G.J.; Ho, P.S. Base-specific binding of copper(II) to Z-DNA. The 1.3-A single crystal structure of d(m5CGUAm5CG) in the presence of CuCl2. J. Biol. Chem. 1991, 266, 20185–20191. [Google Scholar] [CrossRef]
- Aversa, R.; Petrescu, R.V.; Apicella, A.; Petrescu, F.I. One can slow down the aging through antioxidants. Am. J. Eng. Appl. Sci. 2016, 9, 1112–1126. [Google Scholar] [CrossRef]
- Asmus, K.D.; Bensasson, R.V.; Bernier, J.L.; Houssin, R.; Land, E.J. One-electron oxidation of ergothioneine and analogues investigated by pulse radiolysis: Redox reaction involving ergothioneine and vitamin C. Biochem. J. 1996, 315 Pt 2, 625–629. [Google Scholar] [CrossRef]
- Davies, M.J.; Forni, L.G.; Willson, R.L. Vitamin E analogue Trolox CEsr and pulse-radiolysis studies of free-radical reactions. Biochem. J. 1988, 255, 513. [Google Scholar]
- Guijarro, M.V.; Indart, A.; Aruoma, O.I.; Viana, M.; Bonet, B. Effects of ergothioneine on diabetic embryopathy in pregnant rats. Food Chem. Toxicol. 2002, 40, 1751–1755. [Google Scholar] [CrossRef] [PubMed]
- Shen, G.; Jeong, W.-S.; Hu, R.; Kong, A.-N.T. Regulation of Nrf2, NF-κB, and AP-1 signaling pathways by chemopreventive agents. Antioxid. Redox Signal. 2005, 7, 1648–1663. [Google Scholar] [CrossRef] [PubMed]
- Valachová, K.; Šoltés, L. Self-associating polymers chitosan and hyaluronan for Constructing composite membranes as skin-wound dressings carrying therapeutics. Molecules 2021, 26, 2535. [Google Scholar] [CrossRef] [PubMed]
- Arduini, A.; Eddy, L.; Hochstein, P. The reduction of ferryl myoglobin by ergothioneine: A novel function for ergothioneine. Arch. Biochem. Biophys. 1990, 281, 41–43. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.-H.; Aruoma, O.I.; Jen, L.-S.; Chung, H.Y.; Surh, Y.-J. Ergothioneine rescues PC12 cells from β-amyloid-induced apoptotic death. Free Radic. Biol. Med. 2004, 36, 288–299. [Google Scholar] [CrossRef] [PubMed]
- Williamson, R.D.; McCarthy, F.P.; Manna, S.; Groarke, E.; Kell, D.B.; Kenny, L.C.; McCarthy, C.M. L-(+)-ergothioneine significantly improves the clinical characteristics of preeclampsia in the reduced uterine perfusion pressure rat model. Hypertension 2020, 75, 561–568. [Google Scholar] [CrossRef]
- Hseu, Y.-C.; Lo, H.-W.; Korivi, M.; Tsai, Y.-C.; Tang, M.-J.; Yang, H.-L. Dermato-protective properties of ergothioneine through induction of Nrf2/ARE-mediated antioxidant genes in UVA-irradiated Human keratinocytes. Free Radic. Biol. Med. 2015, 86, 102–117. [Google Scholar] [CrossRef]
- Franzoni, F.; Colognato, R.; Galetta, F.; Laurenza, I.; Barsotti, M.; Di Stefano, R.; Bocchetti, R.; Regoli, F.; Carpi, A.; Balbarini, A.; et al. An in vitro study on the free radical scavenging capacity of ergothioneine: Comparison with reduced glutathione, uric acid and trolox. Biomed. Pharm. 2006, 60, 453–457. [Google Scholar] [CrossRef]
- Obayashi, K.; Kurihara, K.; Okano, Y.; Masaki, H.; Yarosh, D.B. L-Ergothioneine scavenges superoxide and singlet oxygen and suppresses TNF-α and MMP-1 expression in UV-irradiated human dermal fibroblasts. Int. J. Cosmet. Sci. 2005, 56, 17–27. [Google Scholar] [CrossRef]
- Nguyen, T.H.; Nagasaka, R.; Ohshima, T. The natural antioxidant ergothioneine: Resources, chemical characterization, and applications. Lipid Oxid. 2013, 12, 381–415. [Google Scholar] [CrossRef]
- Zhao, H.; Zhang, M.; Liu, Q.; Wang, X.; Zhao, R.; Geng, Y.; Wong, T.; Li, S.; Wang, X. A comprehensive screening shows that ergothioneine is the most abundant antioxidant in the wild macrofungus Phylloporia ribis Ryvarden. J. Environ. Sci. Health Part C 2018, 36, 98–111. [Google Scholar] [CrossRef] [PubMed]
- Luisi, G.; Stefanucci, A.; Zengin, G.; Dimmito, M.P.; Mollica, A. Anti-Oxidant and Tyrosinase Inhibitory In Vitro Activity of Amino Acids and Small Peptides: New Hints for the Multifaceted Treatment of Neurologic and Metabolic Disfunctions. Antioxidants 2018, 8, 7. [Google Scholar] [CrossRef] [PubMed]
- Valko, M.; Jomova, K.; Rhodes, C.J.; Kuča, K.; Musílek, K. Redox-and non-redox-metal-induced formation of free radicals and their role in human disease. Arch. Toxicol. 2016, 90, 1–37. [Google Scholar] [CrossRef]
- Liu, J.; Chakraborty, S.; Hosseinzadeh, P.; Yu, Y.; Tian, S.; Petrik, I.; Bhagi, A.; Lu, Y. Metalloproteins containing cytochrome, iron–sulfur, or copper redox centers. Chem. Rev. 2014, 114, 4366–4469. [Google Scholar] [CrossRef]
- Kagawa, T.F.; Geierstanger, B.H.; Wang, A.H.; Ho, P.S. Covalent modification of guanine bases in double-stranded DNA. The 1.2-A Z-DNA structure of d(CGCGCG) in the presence of CuCl2. J. Biol. Chem. 1991, 266, 20175–20184. [Google Scholar] [CrossRef]
- Simonian, N.A.; Coyle, J.T. Oxidative stress in neurodegenerative diseases. Annu. Rev. Pharmacol. Toxicol. 1996, 36, 83–106. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, H.; Shao, Y.; Liu, J.; Li, J.; Luo, L.; Xing, M. Copper (II) and/or arsenite-induced oxidative stress cascades apoptosis and autophagy in the skeletal muscles of chicken. Chemosphere 2018, 206, 597–605. [Google Scholar] [CrossRef]
- Zhao, H.; Wang, Y.; Shao, Y.; Liu, J.; Wang, S.; Xing, M. Oxidative stress-induced skeletal muscle injury involves in NF-κB/p53-activated immunosuppression and apoptosis response in copper (II) or/and arsenite-exposed chicken. Chemosphere 2018, 210, 76–84. [Google Scholar] [CrossRef]
- Gaetke, L.M.; Chow, C.K. Copper toxicity, oxidative stress, and antioxidant nutrients. Toxicology 2003, 189, 147–163. [Google Scholar] [CrossRef]
- Hanlon, D.P. Interaction of ergothioneine with metal ions and metalloenzymes. J. Med. Chem. 1971, 14, 1084–1087. [Google Scholar] [CrossRef] [PubMed]
- Motohashi, N.; Mori, I.; Sugiura, Y. Complexing of copper ion by ergothioneine. Chem. Pharm. Bull. 1976, 24, 2364–2368. [Google Scholar] [CrossRef] [PubMed]
- Zhu, B.Z.; Mao, L.; Fan, R.M.; Zhu, J.G.; Zhang, Y.N.; Wang, J.; Kalyanaraman, B.; Frei, B. Ergothioneine prevents copper-induced oxidative damage to DNA and protein by forming a redox-inactive ergothioneine-copper complex. Chem. Res. Toxicol. 2011, 24, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Tsay, G.J.; Lin, S.-Y.; Li, C.-Y.; Mau, J.-L.; Tsai, S.-Y. Comparison of Single and Combined Use of Ergothioneine, Ferulic Acid, and Glutathione as Antioxidants for the Prevention of Ultraviolet B Radiation-Induced Photoaging Damage in Human Skin Fibroblasts. Processes 2021, 9, 1204. [Google Scholar] [CrossRef]
- Narainsamy, K.; Farci, S.; Braun, E.; Junot, C.; Cassier-Chauvat, C.; Chauvat, F. Oxidative-stress detoxification and signalling in cyanobacteria: The crucial glutathione synthesis pathway supports the production of ergothioneine and ophthalmate. Mol. Microbiol. 2016, 100, 15–24. [Google Scholar] [CrossRef]
- Pahila, J.; Kaneda, H.; Nagasaka, R.; Koyama, T.; Ohshima, T. Effects of ergothioneine-rich mushroom extracts on lipid oxidation and discoloration in salmon muscle stored at low temperatures. Food Chem. 2017, 233, 273–281. [Google Scholar] [CrossRef]
- Bao, H.N.D.; Osako, K.; Ohshima, T. Value-added use of mushroom ergothioneine as a colour stabilizer in processed fish meats. J. Sci. Food Agric. 2010, 90, 1634–1641. [Google Scholar] [CrossRef]
- Ju, H.Q.; Lin, J.F.; Tian, T.; Xie, D.; Xu, R.H. NADPH homeostasis in cancer: Functions, mechanisms and therapeutic implications. Signal Transduct. Target. Ther. 2020, 5, 231. [Google Scholar] [CrossRef]
- Covarrubias, A.J.; Perrone, R.; Grozio, A.; Verdin, E. NAD+ metabolism and its roles in cellular processes during ageing. Nat. Rev. Mol. Cell Biol. 2021, 22, 119–141. [Google Scholar] [CrossRef]
- Perez, S.; Talens-Visconti, R.; Rius-Perez, S.; Finamor, I.; Sastre, J. Redox signaling in the gastrointestinal tract. Free Radic. Biol. Med. 2017, 104, 75–103. [Google Scholar] [CrossRef]
- Gu, Y.; Han, J.; Jiang, C.; Zhang, Y. Biomarkers, oxidative stress and autophagy in skin aging. Ageing Res. Rev. 2020, 59, 101036. [Google Scholar] [CrossRef] [PubMed]
- Makrantonaki, E.; Zouboulis, C.C.; William, J. Cunliffe Scientific Awards. Characteristics and pathomechanisms of endogenously aged skin. Dermatology 2007, 214, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Schikowski, T.; Huls, A. Air Pollution and Skin Aging. Curr. Environ. Health Rep. 2020, 7, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Fulop, T.; Le Page, A.; Fortin, C.; Witkowski, J.M.; Dupuis, G.; Larbi, A. Cellular signaling in the aging immune system. Curr. Opin. Immunol. 2014, 29, 105–111. [Google Scholar] [CrossRef]
- Lui, P.P.Y.; Wong, C.M. Biology of Tendon Stem Cells and Tendon in Aging. Front. Genet. 2019, 10, 1338. [Google Scholar] [CrossRef]
- Ren, R.; Ocampo, A.; Liu, G.H.; Izpisua Belmonte, J.C. Regulation of Stem Cell Aging by Metabolism and Epigenetics. Cell Metab. 2017, 26, 460–474. [Google Scholar] [CrossRef]
- Bazela, K.; Solyga-Zurek, A.; Debowska, R.; Rogiewicz, K.; Bartnik, E.; Eris, I. l-Ergothioneine Protects Skin Cells against UV-Induced Damage—A Preliminary Study. Cosmetics 2014, 1, 51–60. [Google Scholar] [CrossRef]
- Aviello, G.; Knaus, U.G. NADPH oxidases and ROS signaling in the gastrointestinal tract. Mucosal. Immunol. 2018, 11, 1011–1023. [Google Scholar] [CrossRef]
- Blinova, K.; Carroll, S.; Bose, S.; Smirnov, A.V.; Harvey, J.J.; Knutson, J.R.; Balaban, R.S. Distribution of mitochondrial NADH fluorescence lifetimes: Steady-state kinetics of matrix NADH interactions. Biochemistry 2005, 44, 2585–2594. [Google Scholar] [CrossRef]
- Tang, Y.; Masuo, Y.; Sakai, Y.; Wakayama, T.; Sugiura, T.; Harada, R.; Futatsugi, A.; Komura, T.; Nakamichi, N.; Sekiguchi, H. Localization of xenobiotic transporter OCTN1/SLC22A4 in hepatic stellate cells and its protective role in liver fibrosis. J. Pharm. Sci. 2016, 105, 1779–1789. [Google Scholar] [CrossRef]
- Pan, H.Y.; Ye, Z.W.; Zheng, Q.W.; Yun, F.; Tu, M.Z.; Hong, W.G.; Chen, B.X.; Guo, L.Q.; Lin, J.F. Ergothioneine exhibits longevity-extension effect in Drosophila melanogaster via regulation of cholinergic neurotransmission, tyrosine metabolism, and fatty acid oxidation. Food Funct. 2022, 13, 227–241. [Google Scholar] [CrossRef] [PubMed]
- Kawano, H.; Murata, H.; Iriguchi, S.; Mayumi, T.; Hama, T. Studies on ergothioneine. XI. Inhibitory effect on lipid peroxide formation in mouse liver. Chem. Pharm. Bull. 1983, 31, 1682–1687. [Google Scholar] [CrossRef] [PubMed]
- Stein, L.R.; Imai, S. The dynamic regulation of NAD metabolism in mitochondria. Trends Endocrinol. Metab. 2012, 23, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S. Oxidative stress, inflammation, and disease. In Oxidative Stress Biomater; Academic Press: Cambridge, MA, USA, 2016; pp. 35–58. [Google Scholar] [CrossRef]
- Köck, A.; Schwarz, T.; Kirnbauer, R.; Urbanski, A.; Perry, P.; Ansel, J.C.; Luger, T.A. Human keratinocytes are a source for tumor necrosis factor alpha: Evidence for synthesis and release upon stimulation with endotoxin or ultraviolet light. J. Exp. Med. 1990, 172, 1609–1614. [Google Scholar] [CrossRef] [PubMed]
- Facchinetti, F.; Amadei, F.; Geppetti, P.; Tarantini, F.; Di Serio, C.; Dragotto, A.; Gigli, P.M.; Catinella, S.; Civelli, M.; Patacchini, R. α, β-unsaturated aldehydes in cigarette smoke release inflammatory mediators from human macrophages. Am. J. Respir. Cell Mol. Biol. 2007, 37, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Robert, C.; Kupper, T.S. Inflammatory skin diseases, T cells, and immune surveillance. N. Engl. J. Med. 1999, 341, 1817–1828. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, H.; Shanmugam, V.K. Mechanism-based approach of medicinal plants mediated treatment of inflammatory disorders: A review. S. Afr. J. Bot. 2022, 147, 380–390. [Google Scholar] [CrossRef]
- Kannourakis, G.; Abbas, A. The Role of Cytokines in the Pathogenesis of Pulmonary Langerhans’ Cell Histiocytosis. Br. J. Cancer Suppl. 1994, 23, S37–S40. [Google Scholar] [CrossRef]
- Bhatia, M.; Brady, M.; Shokuhi, S.; Christmas, S.; Neoptolemos, J.P.; Slavin, J. Inflammatory mediators in acute pancreatitis. J. Pathol. 2000, 190, 117–125. [Google Scholar] [CrossRef]
- Patra, V.; Gallais Serezal, I.; Wolf, P. Potential of Skin Microbiome, Pro- and/or Pre-Biotics to Affect Local Cutaneous Responses to UV Exposure. Nutrients 2020, 12, 1795. [Google Scholar] [CrossRef]
- Asahi, T.; Wu, X.; Shimoda, H.; Hisaka, S.; Harada, E.; Kanno, T.; Nakamura, Y.; Kato, Y.; Osawa, T. A mushroom-derived amino acid, ergothioneine, is a potential inhibitor of inflammation-related DNA halogenation. Biosci. Biotechnol. Biochem. 2016, 80, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Maeda, T.; Hirayama, M.; Kobayashi, D.; Miyazawa, K.; Tamai, I. Mechanism of the regulation of organic cation/carnitine transporter 1 (SLC22A4) by rheumatoid arthritis-associated transcriptional factor RUNX1 and inflammatory cytokines. Drug Metab. Dispos. 2007, 35, 394–401. [Google Scholar] [CrossRef]
- Laurenza, I.; Colognato, R.; Migliore, L.; Del Prato, S.; Benzi, L. Modulation of palmitic acid-induced cell death by ergothioneine: Evidence of an anti-inflammatory action. Biofactors 2008, 33, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, S.; Shime, H.; Funami, K.; Takaki, H.; Matsumoto, M.; Kasahara, M.; Seya, T. The anti-oxidant ergothioneine augments the immunomodulatory function of TLR agonists by direct action on macrophages. PLoS ONE 2017, 12, e0169360. [Google Scholar] [CrossRef]
- Tenaud, I.; Khammari, A. Dreno, B. In vitro modulation of TLR-2, CD1d and IL-10 by adapalene on normal human skin and acne inflammatory lesions. Exp. Dermatol. 2007, 16, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Rahman, I.; Gilmour, P.S.; Jimenez, L.A.; Biswas, S.K.; Antonicelli, F.; Aruoma, O.I. Ergothioneine inhibits oxidative stress-and TNF-α-induced NF-κB activation and interleukin-8 release in alveolar epithelial cells. Biochem. Biophys. Res. Commun. 2003, 302, 860–864. [Google Scholar] [CrossRef]
- Rizzo, J.M.; Oyelakin, A.; Min, S.; Smalley, K.; Bard, J.; Luo, W.; Nyquist, J.; Guttman-Yassky, E.; Yoshida, T.; De Benedetto, A. ΔNp63 regulates IL-33 and IL-31 signaling in atopic dermatitis. Cell Death Differ. 2016, 23, 1073–1085. [Google Scholar] [CrossRef]
- Masse, I.; Barbollat-Boutrand, L.; Molina, M.; Berthier-Vergnes, O.; Joly-Tonetti, N.; Martin, M.T.; De Fromentel, C.C.; Kanitakis, J.; Lamartine, J. Functional interplay between p63 and p53 controls RUNX1 function in the transition from proliferation to differentiation in human keratinocytes. Cell Death Dis. 2012, 3, e318. [Google Scholar] [CrossRef]
- Martínez, A.; Valdivia, A.; Pascual-Salcedo, D.; Balsa, A.; Fernández-Gutiérrez, B.; De la Concha, E.; Urcelay, E. Role of SLC22A4, SLC22A5, and RUNX1 genes in rheumatoid arthritis. J. Rheumatol. 2006, 33, 842–846. [Google Scholar] [CrossRef]
- Taubert, D.; Lazar, A.; Grimberg, G.; Jung, N.; Rubbert, A.; Delank, K.S.; Perniok, A.; Erdmann, E.; Schomig, E. Association of rheumatoid arthritis with ergothioneine levels in red blood cells: A case control study. J. Rheumatol. 2006, 33, 2139–2145. [Google Scholar]
- Harrach, S.; Edemir, B.; Schmidt-Lauber, C.; Pap, T.; Bertrand, J.; Ciarimboli, G. Importance of the novel organic cation transporter 1 for tyrosine kinase inhibition by saracatinib in rheumatoid arthritis synovial fibroblasts. Sci. Rep. 2017, 7, 1258. [Google Scholar] [CrossRef] [PubMed]
- Deltcheva, E.; Nimmo, R. RUNX transcription factors at the interface of stem cells and cancer. Biochem. J. 2017, 474, 1755–1768. [Google Scholar] [CrossRef] [PubMed]
- Dai, X.; Utsunomiya, R.; Shiraishi, K.; Mori, H.; Muto, J.; Murakami, M.; Sayama, K. Nuclear IL-33 Plays an Important Role in the Suppression of FLG, LOR, Keratin 1, and Keratin 10 by IL-4 and IL-13 in Human Keratinocytes. J. Investig. Dermatol. 2021, 141, 2646–2655. [Google Scholar] [CrossRef] [PubMed]
- Kohl, E.; Steinbauer, J.; Landthaler, M.; Szeimies, R.M. Skin ageing. J. Eur. Acad. Dermatol. Venereol. 2011, 25, 873–884. [Google Scholar] [CrossRef]
- Black, H.S. Potential involvement of free radical reactions in ultraviolet light-mediated cutaneous damage. Photochem. Photobiol. 1987, 46, 213–221. [Google Scholar] [CrossRef]
- Álvarez-Maqueda, M.; El Bekay, R.; Monteseirın, J.; Alba, G.; Chacón, P.; Vega, A.; Santa Marıa, C.; Tejedo, J.R.; Martın-Nieto, J.; Bedoya, F.J. Homocysteine enhances superoxide anion release and NADPH oxidase assembly by human neutrophils. Effects on MAPK activation and neutrophil migration. Atherosclerosis 2004, 172, 229–238. [Google Scholar] [CrossRef]
- Serpone, N.; Salinaro, A.; Emeline, A.V.; Horikoshi, S.; Hidaka, H.; Zhao, J. An in vitro systematic spectroscopic examination of the photostabilities of a random set of commercial sunscreen lotions and their chemical UVB/UVA active agents. Photochem. Photobiol. Sci. 2002, 1, 970–981. [Google Scholar] [CrossRef]
- Carlsson, J.; Kierstan, M.P.J.; Brocklehurst, K. Reactions of L-ergothioneine and some other aminothiones with 2, 2′-and 4, 4′-dipyridyl disulphides and of L-ergothioneine with iodoacetamide. 2-Mercaptoimidazoles, 2-and 4-thiopyridones, thiourea and thioacetamide as highly reactive neutral sulphur nucleophiles. Biochem. J. 1974, 139, 221–235. [Google Scholar] [CrossRef]
- Dong, K.K.; Damaghi, N.; Kibitel, J.; Canning, M.T.; Smiles, K.A.; Yarosh, D.B. A comparison of the relative antioxidant potency of L-ergothioneine and idebenone. J. Cosmet. Dermatol. 2007, 6, 183–188. [Google Scholar] [CrossRef]
- Krutmann, J.; Schroeder, P. Role of mitochondria in photoaging of human skin: The defective powerhouse model. J. Investig. Dermatol. Symp. Proc. 2009, 14, 44–49. [Google Scholar] [CrossRef]
- Birch-Machin, M.A.; Tindall, M.; Turner, R.; Haldane, F.; Rees, J.L. Mitochondrial DNA deletions in human skin reflect photo-rather than chronologic aging. J. Investig. Dermatol. 1998, 110, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.H.; Lee, H.C.; Lin, K.J.; Wei, Y.H. A specific 4977-bp deletion of mitochondrial DNA in human ageing skin. Arch. Dermatol. Res. 1994, 286, 386–390. [Google Scholar] [CrossRef] [PubMed]
- Solano, F. Photoprotection and skin pigmentation: Melanin-related molecules and some other new agents obtained from natural sources. Molecules 2020, 25, 1537. [Google Scholar] [CrossRef] [PubMed]
- Spritz, R.A.; Hearing, V.J., Jr. Genetic disorders of pigmentation. Adv. Hum. Genet. 1994, 22, 1–45. [Google Scholar] [CrossRef] [PubMed]
- Baek, S.H.; Kang, M.G.; Park, D. Inhibitory Effect of Sesamolin on Melanogenesis in B16F10 Cells Determined by In Vitro and Molecular Docking Analyses. Curr. Pharm. Biotechnol. 2020, 21, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Ünver, N.; Freyschmidt-Paul, P.; Hörster, S.; Wenck, H.; Stäb, F.; Blatt, T.; Elsässer, H.P. Alterations in the epidermal–dermal melanin axis and factor XIIIa melanophages in senile lentigo and ageing skin. Br. J. Dermatol. 2006, 155, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Liao, W.C.; Wu, W.H.; Tsai, P.C.; Wang, H.F.; Liu, Y.H.; Chan, C.F. Kinetics of ergothioneine inhibition of mushroom tyrosinase. Appl. Biochem. Biotechnol. 2012, 166, 259–267. [Google Scholar] [CrossRef]
- Shim, E.; Song, E.; Choi, K.S.; Choi, H.J.; Hwang, J. Inhibitory effect of Gastrodia elata Blume extract on alpha-melanocyte stimulating hormone-induced melanogenesis in murine B16F10 melanoma. Nutr. Res. Pract. 2017, 11, 173–179. [Google Scholar] [CrossRef]
- Tsuji-Naito, K.; Hatani, T.; Okada, T.; Tehara, T. Modulating effects of a novel skin-lightening agent, alpha-lipoic acid derivative, on melanin production by the formation of DOPA conjugate products. Bioorg. Med. Chem. 2007, 15, 1967–1975. [Google Scholar] [CrossRef]
- Akanmu, D.; Cecchini, R.; Aruoma, O.I.; Halliwell, B. The antioxidant action of ergothioneine. Arch Biochem. Biophys. 1991, 288, 10–16. [Google Scholar] [CrossRef]
- Chan, C.F.; Lai, S.T.; Guo, Y.C.; Chen, M.J. Inhibitory effects of novel synthetic methimazole derivatives on mushroom tyrosinase and melanogenesis. Bioorg. Med. Chem. 2014, 22, 2809–2815. [Google Scholar] [CrossRef] [PubMed]
- Encarnacion, A.B.; Fagutao, F.; Hirono, I.; Ushio, H.; Ohshima, T. Effects of ergothioneine from mushrooms (Flammulina velutipes) on melanosis and lipid oxidation of kuruma shrimp (Marsupenaeus japonicus). J. Agric. Food Chem. 2010, 58, 2577–2585. [Google Scholar] [CrossRef] [PubMed]
- Bao, H.N.; Ushio, H.; Ohshima, T. Antioxidative activity and antidiscoloration efficacy of ergothioneine in mushroom (Flammulina velutipes) extract added to beef and fish meats. J. Agric. Food Chem. 2008, 56, 10032–10040. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, M.; Srivastav, P.P.; Mishra, H.N. Optimization of process variables for supercritical fluid extraction of ergothioneine and polyphenols from Pleurotus ostreatus and correlation to free-radical scavenging activity. J. Supercrit. Fluids 2014, 95, 51–59. [Google Scholar] [CrossRef]
- Eung-Jun, P.; Wi, Y.L.; Seung, T.K.; Jin, K.A.; Eun, K.B. Ergothioneine accumulation in a medicinal plant Gastrodia elata. J. Med. Plants Res. 2010, 4, 1141–1147. [Google Scholar] [CrossRef]
- Kim, M.; Jeong, D.W.; Oh, J.W.; Jeong, H.J.; Ko, Y.J.; Park, S.E.; Han, S.O. Efficient Synthesis of Food-Derived Antioxidant l-Ergothioneine by Engineered Corynebacterium glutamicum. J. Agric. Food Chem. 2022, 70, 1516–1524. [Google Scholar] [CrossRef]
- Liu, X.; Huang, Y.; Wang, J.; Zhou, S.; Wang, Y.; Cai, M.; Yu, L.; Tang, Q. A Study on the Antioxidant Properties and Stability of Ergothioneine from Culinary-Medicinal Mushrooms. Int. J. Med. Mushrooms 2020, 22, 211–220. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, H.-M.; Tang, W.; Wang, X.-Y.; Jiang, J.-J.; Zhang, W.; Wang, W. Safe and Effective Antioxidant: The Biological Mechanism and Potential Pathways of Ergothioneine in the Skin. Molecules 2023, 28, 1648. https://doi.org/10.3390/molecules28041648
Liu H-M, Tang W, Wang X-Y, Jiang J-J, Zhang W, Wang W. Safe and Effective Antioxidant: The Biological Mechanism and Potential Pathways of Ergothioneine in the Skin. Molecules. 2023; 28(4):1648. https://doi.org/10.3390/molecules28041648
Chicago/Turabian StyleLiu, Hui-Min, Wei Tang, Xiao-Yi Wang, Jing-Jing Jiang, Wei Zhang, and Wei Wang. 2023. "Safe and Effective Antioxidant: The Biological Mechanism and Potential Pathways of Ergothioneine in the Skin" Molecules 28, no. 4: 1648. https://doi.org/10.3390/molecules28041648
APA StyleLiu, H.-M., Tang, W., Wang, X.-Y., Jiang, J.-J., Zhang, W., & Wang, W. (2023). Safe and Effective Antioxidant: The Biological Mechanism and Potential Pathways of Ergothioneine in the Skin. Molecules, 28(4), 1648. https://doi.org/10.3390/molecules28041648






