Antimicrobial Activity of Some Steroidal Hydrazones
Abstract
1. Introduction
2. Results and Discussion
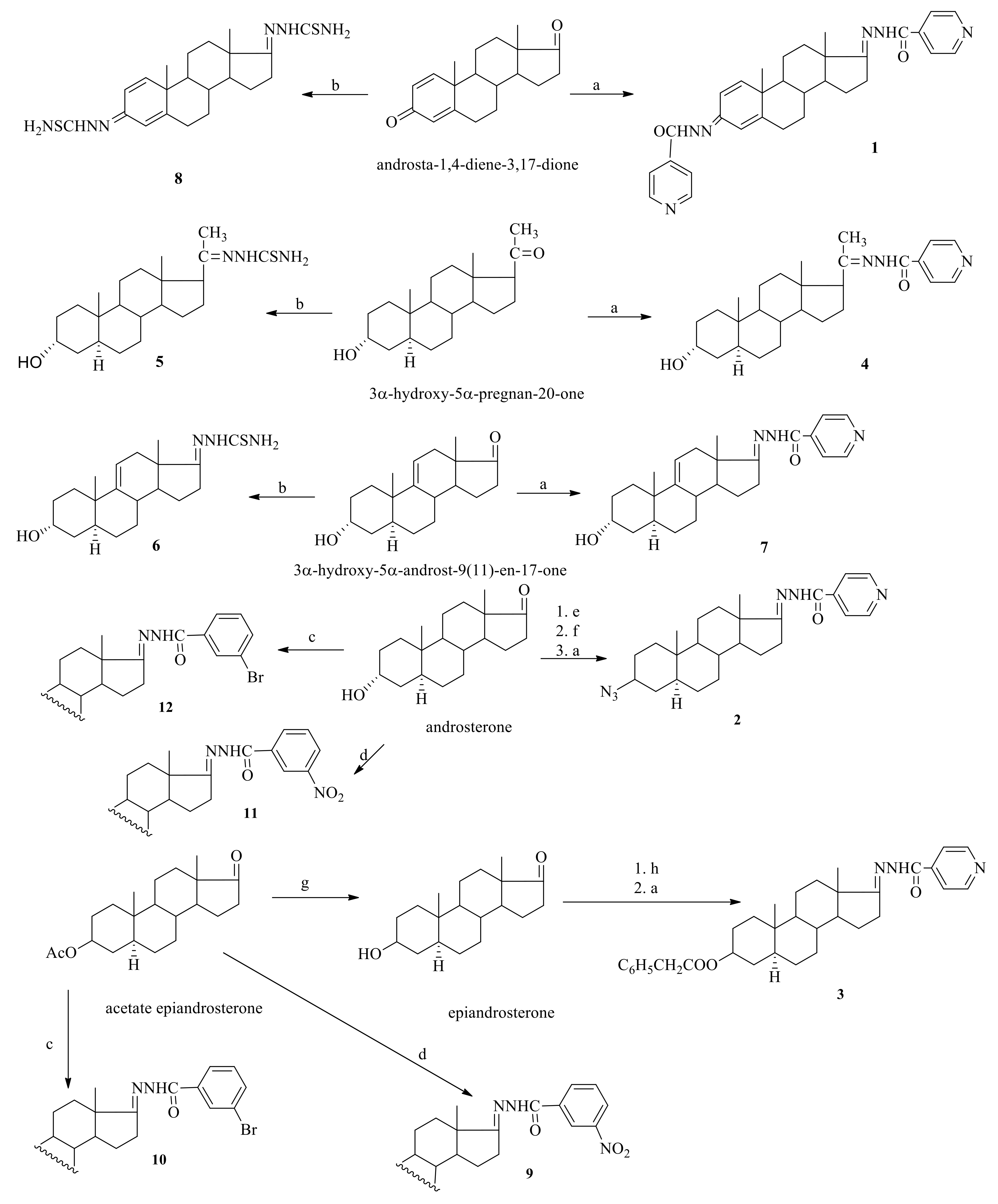
2.1. Chemistry
2.2. PASS Predictions
2.3. Biological Evaluation
2.3.1. Antibacterial Activity
2.3.2. Antifungal Activity
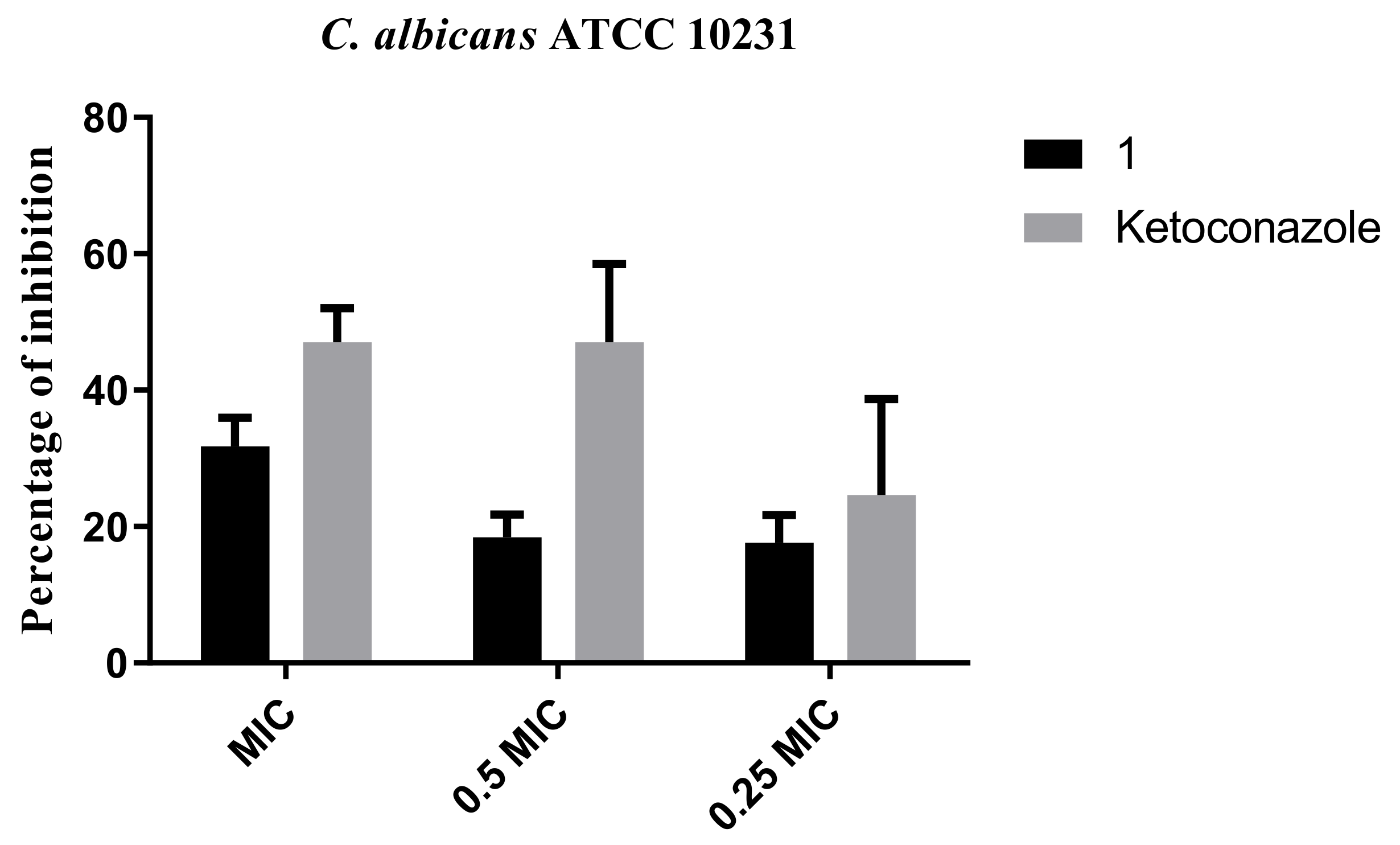
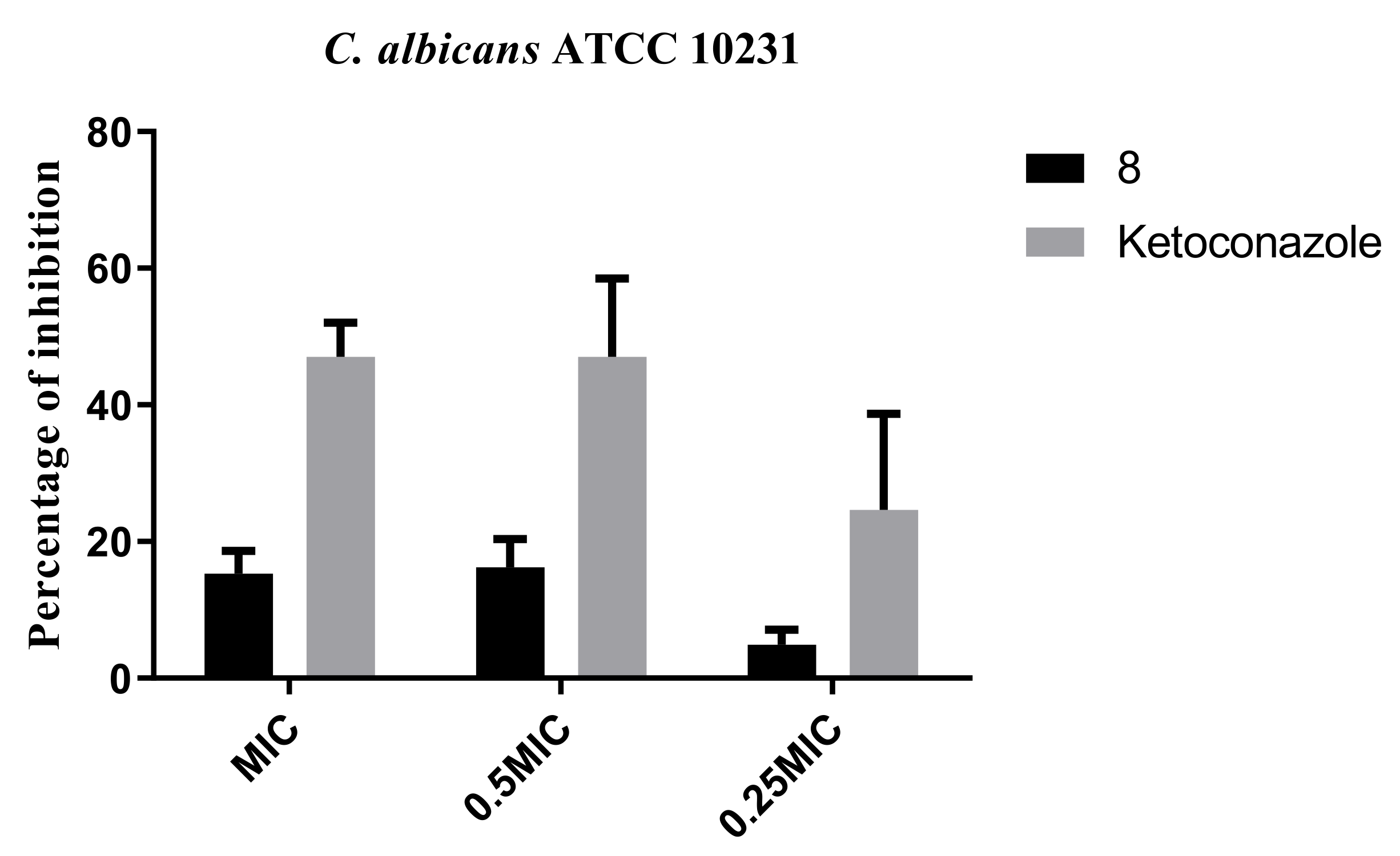
2.3.3. Inhibition of Biofilm Formation
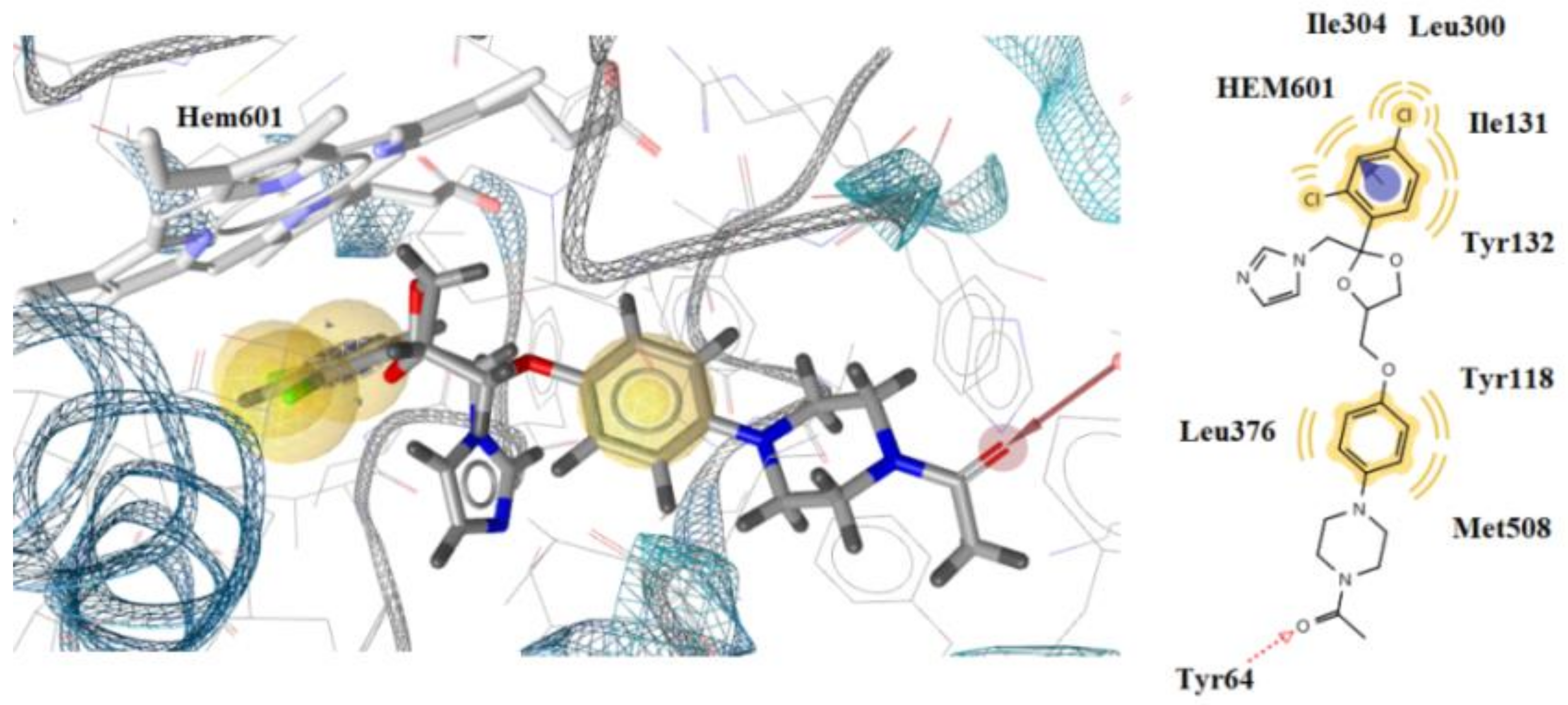
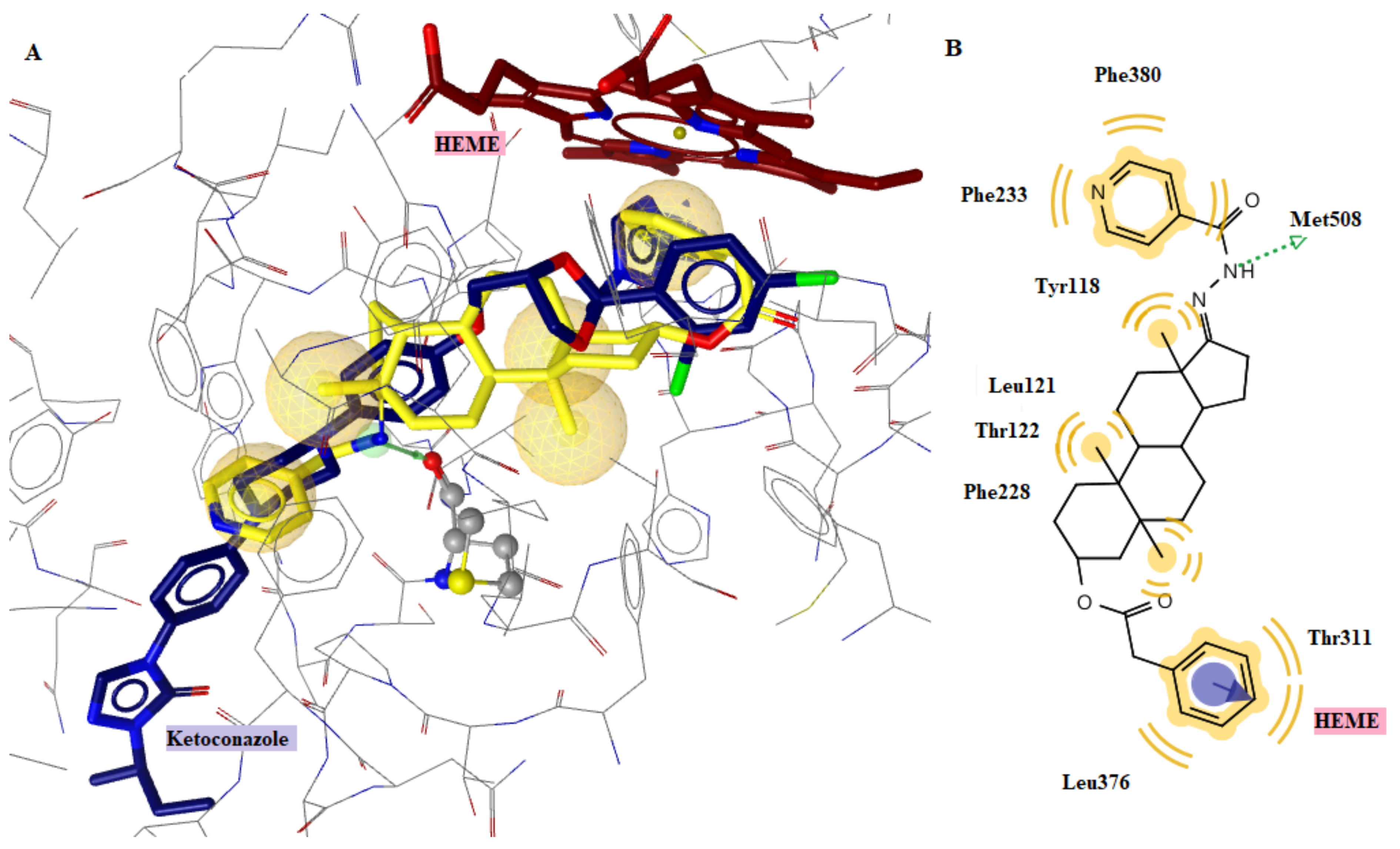
2.4. Docking to Antifungal Targets
2.5. Drug-Likeness
3. Materials and Methods
3.1. Chemistry—General Information
3.2. In Vitro Evaluation of Antimicrobial Activity
Inhibition of Biofilm Formation
3.3. Docking
3.4. Drug-Likeness
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Coates, A.R.M.; Hu, Y. Novel approaches to developing new antibiotics for bacterial infections. Br. J. Pharmacol. 2007, 152, 1147–1154. [Google Scholar] [CrossRef] [PubMed]
- Spellberg, B.; Bartlett, J.; Wunderink, R.; Gilbert, D.M. Novel approaches are needed to develop tomorrow’s antibacterial therapies. Am. J. Respir. Crit. Care Med. 2015, 191, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Cataldo, M.A.; Granata, G.; Petrosillo, N. Clostridium difficile infection: New approaches to prevention, non-antimicrobial treatment, and stewardship. Expert Rev. Anti Infect. Ther. 2017, 15, 1027–1040. [Google Scholar] [CrossRef] [PubMed]
- Hughes, G.; Webber, M.A. Novel approaches to the treatment of bacterial biofilm infections. Br. J. Pharmacol. 2017, 174, 2237–2246. [Google Scholar] [CrossRef]
- Parsek, M.R.; Singh, P.K. Bacterial biofilms: An emerging link to disease pathogenesis. Annu. Rev. Microbiol. 2003, 57, 677–701. [Google Scholar] [CrossRef]
- Verderosa, A.D.; Totsika, M.; Fairfull-Smith, K.E. Bacterial Biofilm Eradication Agents: A Current Review. Front. Chem. 2019, 28, 824–841. [Google Scholar] [CrossRef] [PubMed]
- Bjarnsholt, T. The role of bacterial biofilms in chronic infections. APMIS Suppl. 2013, 136, 1–51. [Google Scholar] [CrossRef] [PubMed]
- Tong, S.Y.; Davis, J.S.; Eichenberger, E.; Holland, T.L.; Fowler, V.G.J. Staphylococcus aureus infections: Epidemiology, pathophysiology, clinical manifestations, and management. Clin. Microbiol. Rev. 2015, 28, 603–661. [Google Scholar] [CrossRef] [PubMed]
- Otto, M. Staphylococcal infections: Mechanisms of biofilm maturation and detachment as critical determinants of pathogenicity. Annu. Rev. Med. 2013, 64, 175–188. [Google Scholar] [CrossRef]
- Verma, G.; Marella, A.; Shaquiquzzaman, M.; Akhtar, M.; Ali, M.R.; Alam, M.M. A review exploring biological activities of hydrazones. J. Pharm. Bioallied Sci. 2014, 6, 69–80. [Google Scholar]
- Rollas, S.; Küçükgüzel, Ş.G. Biological Activities of Hydrazone Derivatives. Molecules 2007, 12, 1910–1939. [Google Scholar] [CrossRef] [PubMed]
- Belskaya, N.P.; Dehaen, W.; Bakulev, V.A. Synthesis and properties of hydrazones bearing amide, thioamide and amidine functions. Arch. Org. Chem. 2010, 1, 275–332. [Google Scholar] [CrossRef]
- Tantawy, M.A.; Nafie, M.S.; Elmegeed, G.A.; Ali, I.A. Auspicious role of the steroidal heterocyclic derivatives as a platform for anti-cancer drugs. Bioorg. Chem. 2017, 73, 128–146. [Google Scholar] [CrossRef] [PubMed]
- Ericson-Neilsen, W.; Kaye, A.D. Steroids: Pharmacology, complications, and practice delivery issues. Ochsner J. 2014, 14, 203–207. [Google Scholar]
- Krstić, N.M.; Bjelaković, M.S.; Pavlović, V.D.; Robeyns, K.; Juranić, Z.D.; Matić, I.; Novakovic, I.; Sladić, D.M. New androst-4-en-17-spiro-1, 3, 2-oxathiaphospholanes. Synthesis, assignment of absolute configuration and in vitro cytotoxic and antimicrobial activities. Steroids 2012, 77, 558–565. [Google Scholar] [CrossRef]
- Hryniewicka, A.; Malinowska, M.; Hauschild, T.; Pieczul, K.; Morzycki, J.W. Synthesis and antimicrobial properties of steroid-based imidazolium salts. J. Steroid. Biochem. Mol. Biol. 2019, 189, 65–72. [Google Scholar] [CrossRef]
- Farhan, A.M.; Alshamusi, Q.K.; Jebur, M.H. Synthesis of steroid bearing heterocyclic derivatives and biological activity. Review 2014–2020. J. Phys. Conf. Ser. 2021, 1853, 01205. [Google Scholar]
- Vollaro, A.; Esposito, A.; Esposito, E.P.; Zarrilli, R.; Guaragna, A.; De Gregorio, E. PYED-1 Inhibits Biofilm Formation and Disrupts the Preformed Biofilm of Staphylococcus aureus. Antibiotics 2020, 9, 240. [Google Scholar] [CrossRef]
- Mistry, S.; Singh, A.K. Synthesis and in vitro antimicrobial activity of new steroidal hydrazone derivatives. FJPS 2022, 8, 7. [Google Scholar] [CrossRef]
- Popiołek, Ł. Hydrazide–hydrazones as potential antimicrobial agents: Overview of the literature since 2010. Med. Chem. Res. 2016, 26, 287–301. [Google Scholar] [CrossRef]
- Visbal, G.; San-Blas, G.; Maldonado, A.; Alvarez-Aular, A.; Capparelli, M.V.; Murgich, J. Synthesis, in vitro antifungal activity and mechanism of action of four sterol hydrazone analogues against the dimorphic fungus Paracoccidioides brasiliensis. Steroids 2011, 76, 1069–1081. [Google Scholar] [CrossRef] [PubMed]
- Gan, C.; Cui, J.; Su, S.; Lin, Q.; Jia, L.; Fan, L.; Huang, Y. Synthesis and antiproliferative activity of some steroidal thiosemicarbazones, semicarbazones and hydrozones. Steroids 2014, 87, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.A.; Asiri, A.M. Synthesis and spectroscopic studies of Ru(II) complexes of steroidal thiosemicarbazones by multi step reaction: As anti-bacterial agents. Steroids 2017, 124, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Loncle, C.; Brunel, J.M.; Vidal, N.; Dherbomez, M.; Letourneux, Y. Synthesis and antifungal activity of cholesterol-hydrazone derivatives. Eur. J. Med. Chem. 2004, 39, 1067–1071. [Google Scholar] [CrossRef] [PubMed]
- Merlani, M.I.; Amiranashvili, L.S.; Mulkidzhanyan, K.G.; Shelar, A.R.; Manvi, F.V. Synthesis and antituberculosis activity of certain steroidal derivatives of the 5α –series. Chem. Nat. Compd. 2008, 44, 618–620. [Google Scholar] [CrossRef]
- Merlani, M.I.; Amiranashvili, L.S.; Kemertelidze, E.O.; Mulkidzhanyan, K.G. Synthesis and antimicobacterial activity of some steroidal derivatives of tigogenin. Chem. Nat. Compd. 2009, 45, 389–392. [Google Scholar] [CrossRef]
- Shelar, A.R.; Merlani, M.; Shelar, M.; Amiranashvili, L.; Shelar, B. Medicinal Applications of Benzoic Acid Hydrazones Synthesized on the Basis of Steroidal Tigogenin. U.S. PATENT 8623849B2, 7 January 2014. [Google Scholar]
- Nadaraia, N.S.; Amiranashvili, L.S.; Merlani, M.; Kakhabrishvili, M.I.; Barbakadze, N.N.; Geronikaki, A.; Petrou, A.; Poroikov, V.; Ciric, A.; Glamoclija, J.; et al. Novel antimicrobial agents’ discovery among the steroid derivatives. Steroids 2019, 144, 52–65. [Google Scholar] [CrossRef]
- Amiranashvili, L.; Nadaraia, N.; Merlani, M.; Kamoutsis, C.; Petrou, A.; Geronikaki, A.; Pogodin, P.; Druzhilovskiy, D.; Poroikov, V.; Ciric, A.; et al. Antimicrobial Activity of Nitrogen-Containing 5-α-Androstane Derivatives: In Silico and Experimental Studies. Antibiotics 2020, 9, 224. [Google Scholar] [CrossRef]
- Lagunin, A.; Stepanchikova, A.; Filimonov, D.; Poroikov, V. PASS: Prediction of activity spectra for biologically active substances. Bioinformatics 2000, 16, 747–748. [Google Scholar] [CrossRef]
- Kartsev, V.; Lichitsky, B.; Geronikaki, A.; Petrou, A.; Smiljkovic, M.; Kostic, M.; Radanovic, O.; Soković, M. Design, synthesis and antimicrobial activity of usnic acid derivatives. MedChemComm 2018, 9, 870–882. [Google Scholar] [CrossRef]
- Haroun, M.; Tratrat, C.; Kositsi, K.; Tsolaki, E.; Petrou, A.; Aldhubiab, B.; Attimarad, M.; Harsha, S.; Geronikaki, A.; Venugopala, K.N.; et al. New Benzothiazole-based Thiazolidinones as Potent Antimicrobial Agents. Design, synthesis and Biological Evaluation. Curr. Top. Med. Chem. 2018, 18, 75–87. [Google Scholar] [CrossRef] [PubMed]
- Kritsi, E.; Matsoukas, M.T.; Potamitis, C.; Detsi, A.; Ivanov, M.; Sokovic, M.; Zoumpoulakis, P. Novel Hit Compounds as Putative Antifungals: The Case of Aspergillus fumigatus. Molecules 2019, 24, 3853. [Google Scholar] [CrossRef] [PubMed]
- Clinical and Laboratory Standards Institute—CLSI. Methods for Dilution Antimicrobial Susceptibility Test for Bacteria That Grow Aerobically. Approv. Stand. 2009, 29, 1–65. [Google Scholar]
- Horishny, V.; Kartsev, V.; Matiychuk, V.; Geronikaki, A.; Anthi, P.; Pogodin, P.; Poroikov, V.; Ivanov, M.; Kostic, M.; Soković, M.D.; et al. 3-Amino-5-(indol-3-yl)methylene-4-oxo-2-thioxothiazolidine Derivatives as Antimicrobial Agents: Synthesis, Computational and Biological Evaluation. Pharmaceuticals 2020, 13, 229. [Google Scholar] [CrossRef] [PubMed]
- Smiljkovic, M.; Matsoukas, M.T.; Kritsi, E.; Zelenko, U.; Grdadolnik, S.G.; Calhelha, R.C.; Ferreira, I.C.F.R.; Sankovic-Babic, S.; Glamoclija, J.; Fotopoulou, T.; et al. Nitrate Esters of Heteroaromatic Compounds as Candida albicans CYP51 Enzyme Inhibitors. ChemMedChem 2018, 13, 251–258. [Google Scholar] [CrossRef]
- Fesatidou, M.; Zagaliotis, P.; Camoutsis, C.; Petrou, A.; Eleftheriou, P.; Tratrtat, C.; Haroun, M.; Geronikaki, A.; Ciric, A.; Sokovic, M. 5-Adamantan thiadiazole-based thiazolidinones as antimicrobial agents. Design, synthesis, molecular docking and evaluation. Bioorg. Med. Chem. 2018, 26, 4664–4676. [Google Scholar] [CrossRef]
- Lipinski, C.A. Lead- and drug-like compounds: The rule-of-five revolution. Drug Discov. Today Technol. 2004, 1, 337–341. [Google Scholar] [CrossRef]
- SwissADME Program. Available online: https://swissadme.ch (accessed on 19 October 2022).



| Compounds | S.a. | MRSA | B.c | L.m. | E. coli | Rez E. coli | P.a. | Rez P.a. | S.Thy | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | MIC | 1.50 | 1.50 | 0.37 | 0.75 | 1.00 | 4.50 | 1.50 | 1.00 | 0.75 |
| MBC | 3.00 | 3.00 | 0.75 | 1.50 | 3.00 | 6.00 | 3.00 | 1.50 | 1.50 | |
| 2 | MIC | 3.00 | 4.50 | 0.75 | 3.00 | 3.00 | 6.00 | 6.00 | 6.00 | 6.00 |
| MBC | 6.00 | 6.00 | 1.50 | 6.00 | 6.00 | 9.00 | 9.00 | 9.00 | 9.00 | |
| 3 | MIC | 1.00 | 0.75 | 0.37 | 1.00 | 1.00 | 1.50 | 1.50 | 0.75 | 1.00 |
| MBC | 1.50 | 1.50 | 0.75 | 1.50 | 1.50 | 3.00 | 3.00 | 1.50 | 1.50 | |
| 4 | MIC | 0.75 | 3.00 | 0.37 | 0.75 | 1.50 | 1.50 | 0.75 | 0.75 | 0.75 |
| MBC | 1.50 | 6.00 | 0.75 | 1.50 | 3.00 | 3.00 | 1.50 | 1.50 | 1.50 | |
| 5 | MIC | 0.75 | 1.50 | 0.37 | 0.75 | 1.50 | 1.50 | 0.75 | 1.00 | 0.75 |
| MBC | 1.50 | 3.00 | 0.75 | 1.50 | 3.00 | 3.00 | 1.50 | 1.50 | 1.50 | |
| 6 | MIC | 0.75 | 1.50 | 0.37 | 1.50 | 1.50 | 0.75 | 3.00 | 1.50 | 1.50 |
| MBC | 1.50 | 3.00 | 0.75 | 3.00 | 3.00 | 1.50 | 6.00 | 3.00 | 3.00 | |
| 7 | MIC | 0.75 | 1.50 | 0.50 | 1.50 | 1.50 | 0.75 | 3.00 | 1.50 | 1.50 |
| MBC | 1.50 | 3.00 | 0.75 | 3.00 | 3.00 | 1.50 | 6.00 | 3.00 | 3.00 | |
| 8 | MIC | 1.50 | 1.50 | 0.37 | 1.50 | 1.50 | 1.50 | 3.00 | 1.50 | 1.50 |
| MBC | 3.00 | 3.00 | 0.75 | 3.00 | 3.00 | 3.00 | 6.00 | 3.00 | 3.00 | |
| 9 | MIC | 1.50 | 3.00 | 1.50 | 0.75 | 3.00 | 6.00 | 1.50 | 3.00 | 3.00 |
| MBC | 3.00 | 6.00 | 3.00 | 1.50 | 6.00 | 9.00 | 3.00 | 6.00 | 6.00 | |
| 10 | MIC | 1.50 | 3.00 | 1.50 | 0.75 | 3.00 | 6.00 | 1.50 | 1.50 | 0.75 |
| MBC | 3.00 | 6.00 | 3.00 | 1.50 | 6.00 | 9.00 | 3.00 | 3.00 | 1.50 | |
| 11 | MIC | 0.75 | 1.50 | 0.75 | 0.75 | 0.75 | 1.50 | 0.75 | 0.75 | 0.75 |
| MBC | 1.50 | 3.00 | 1.50 | 1.50 | 1.50 | 3.00 | 1.50 | 1.50 | 1.50 | |
| 12 | MIC | 0.75 | 1.50 | 0.75 | 0.75 | 0.75 | 1.50 | 0.75 | 0.75 | 0.75 |
| MBC | 1.50 | 3.00 | 1.50 | 1.50 | 1.50 | 3.00 | 1.50 | 1.50 | 1.50 | |
| Ampicillin | MIC | 0.10 | - | 0.10 | 0.15 | 0.15 | 0.20 | 0.30 | 0.20 | 0.10 |
| MBC | 0.15 | - | 0.15 | 0.30 | 0.20 | - | 0.50 | - | 0.20 | |
| Streptomycin | MIC | 0.10 | 0.10 | 0.025 | 0.15 | 0.10 | 0.05 | 0.10 | 0.10 | 0.10 |
| MBC | 0.20 | - | 0.050 | 0.30 | 0.20 | 0.10 | 0.20 | 0.20 | 0.20 | |
| Compounds | A.fu | A.n. | T.v. | P.f. | P.v.c. | C.a. | |
|---|---|---|---|---|---|---|---|
| 1 | MIC | 0.75 | 0.75 | 0.37 | 0.75 | 0.37 | 0.37 |
| MFC | 1.50 | 1.50 | 0.75 | 1.50 | 0.75 | 0.75 | |
| 2 | MIC | 1.50 | 1.50 | 1.50 | 1.50 | 3.00 | 0.37 |
| MFC | 3.00 | 3.00 | 3.00 | 3.00 | 6.00 | 0.75 | |
| 3 | MIC | 0.37 | 0.37 | 0.37 | 0.37 | 0.37 | 0.75 |
| MFC | 0.75 | 0.75 | 0.75 | 0.75 | 0.75 | 1.50 | |
| 4 | MIC | 1.50 | 3.00 | 3.00 | 3.00 | 3.00 | 0.75 |
| MFC | 3.00 | 6.00 | 6.00 | 6.00 | 6.00 | 1.50 | |
| 5 | MIC | 1.50 | 1.50 | 1.50 | 1.50 | 0.75 | 0.75 |
| MFC | 3.00 | 3.00 | 3.00 | 3.00 | 1.50 | 1.50 | |
| 6 | MIC | 1.50 | 1.50 | 1.50 | 0.75 | 0.75 | 0.75 |
| MFC | 3.00 | 3.00 | 3.00 | 1.50 | 1.50 | 1.50 | |
| 7 | MIC | 0.37 | 0.37 | 0.37 | 0.37 | 0.37 | 0.37 |
| MFC | 0.75 | 0.75 | 0.75 | 0.75 | 0.75 | 0.75 | |
| 8 | MIC | 0.37 | 0.37 | 0.37 | 0.37 | 0.37 | 0.37 |
| MFC | 0.75 | 0.75 | 0.75 | 0.75 | 0.75 | 0.75 | |
| 9 | MIC | 0.37 | 0.75 | 0.37 | 0.75 | 0.75 | 0.37 |
| MFC | 0.75 | 1.50 | 0.75 | 1.50 | 1.50 | 0.75 | |
| 10 | MIC | 0.37 | 1.50 | 0.75 | 1.50 | 3.00 | 0.37 |
| MFC | 0.50 | 3.00 | 1.50 | 3.00 | 6.00 | 0.75 | |
| 11 | MIC | 0.75 | 1.50 | 0.75 | 0.75 | 1.50 | 1.50 |
| MFC | 1.50 | 3.00 | 1.50 | 1.50 | 3.00 | 3.00 | |
| 12 | MIC | 0.37 | 0.37 | 0.37 | 0.75 | 1.50 | 1.50 |
| MFC | 0.50 | 0.50 | 0.75 | 1.50 | 3.00 | 3.00 | |
| Ketoconazole | MIC | 0.20 | 0.20 | 1.00 | 0.20 | 0.20 | 1.00 |
| MFC | 0.50 | 0.50 | 1.50 | 0.50 | 0.30 | 2.00 | |
| Bifonazole | MIC | 0.15 | 0.15 | 0.15 | 0.20 | 0.10 | 0.20 |
| MFC | 0.20 | 0.20 | 0.20 | 0.25 | 0.20 | 0.30 | |
| Est. Binding Energy (kcal/mol) | Residues Involved in H-bond Formation | Residues Involved in Hydrophobic Interactions | Residues Involved in Aromatic Interactions | Interactions with HEM601 | ||
|---|---|---|---|---|---|---|
| Comp. | CYP51 of C. albicans 5V5Z | DNA TopoIV 1S16 | ||||
| 1 | −4.11 | −8.52 | Tyr132 | Tyr118, Thr122, Thr311, Phe380, Met508, Hem601 | Hem601 | Hydrophobic, aromatic |
| 2 | −3.31 | −6.38 | - | Tyr118, Thr311, Leu376, Hem601 | - | Hydrophobic |
| 3 | −3.58 | −9.04 | Met508 | Tyr118, Thr122, Phe228, Phe233, Thr311, Leu376, Phe380, Met508, Hem601 | Hem601 | Hydrophobic, aromatic |
| 4 | −1.77 | −6.01 | - | Tyr118, Leu376, Met508, Hem601 | - | Hydrophobic |
| 5 | −2.47 | −6.80 | - | Tyr118, Tyr122, Leu376, Met508, Hem601 | Tyr118 | Hydrophobic |
| 6 | −4.20 | −7.32 | - | Tyr118, Tyr122, Thr311, Leu37, Hem601 | Tyr118 | Hydrophobic |
| 7 | −3.18 | −9.86 | Tyr132 | Tyr118, Leu121, Thr311, Met508, Hem601 | Hem601 | Hydrophobic, aromatic |
| 8 | −2.54 | −10.23 | Tyr64 | Tyr118, Thr122, Ile131, Tyr132, Leu376, Met508, Hem601 | - | Hydrophobic, Fe binding |
| 9 | −3.61 | −8.48 | Tyr132 | Tyr118, Leu121, Thr122, Thr311, Met508, Hem601 | Hem601 | Hydrophobic, aromatic |
| 10 | −1.38 | −7.11 | - | Tyr118, Thr311, Met508, Hem601 | Tyr118 | Hydrophobic |
| 11 | −2.47 | −7.55 | Tyr118 | Tyr118, Leu121, Met508, Hem601 | - | Hydrophobic |
| 12 | −1.28 | −8.02 | Tyr118 | Tyr118, Tyr122, Thr311, Met508, Hem601 | Hem601 | Hydrophobic, aromatic |
| ketoconazole | - | −8.93 | Tyr64 | Tyr118, Ile131, Tyr132, Leu300, Ile304, Leu376, Met508, Hem601 | Hem601 | Hydrophobic, aromatic |
| No | MW | Number of HBA a | Number of HBD b | Log Po/w (WLOGP) c | Log S d | TPSA e | Lipinski | Bioavailability Score | Drug-Likeness Model Score |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 522.64 | 6 | 2 | 5.09 | Moderately soluble | 108.70 | 0 | 0.55 | 1.09 |
| 2 | 448.60 | 6 | 1 | 6.28 | Moderately soluble | 104.10 | 0 | 0.55 | 1.30 |
| 3 | 541.72 | 5 | 1 | 6.75 | Moderately soluble | 80.65 | 2 violations: MW > 500, MLOGP > 4.15 | 0.17 | 1.54 |
| 4 | 423.59 | 4 | 2 | 3.75 | Moderately soluble | 74.58 | 0 | 0.55 | 1.48 |
| 5 | 405.64 | 2 | 3 | 4.61 | Moderately soluble | 102.73 | 0 | 0.55 | 0.71 |
| 6 | 375.57 | 3 | 2 | 3.44 | Moderately soluble | 102.73 | 0 | 0.55 | 0.74 |
| 7 | 407.55 | 4 | 2 | 4.49 | Moderately soluble | 74.78 | 0 | 0.55 | 1.29 |
| 8 | 430.66 | 2 | 4 | 3.10 | Soluble | 165.00 | 0 | 0.55 | 0.78 |
| 9 | 509.64 | 6 | 1 | 6.05 | Poorly soluble | 113.58 | 2 violations: MW > 500, MLOGP > 4.15 | 0.17 | 0.98 |
| 10 | 543.54 | 4 | 1 | 6.90 | Poorly soluble | 67.76 | 2 violations: MW > 500, MLOGP > 4.15 | 0.17 | 1.18 |
| 11 | 467.60 | 5 | 2 | 5.47 | Moderately soluble | 107.51 | 0 | 0.55 | 0.85 |
| 12 | 501.50 | 3 | 2 | 6.33 | Moderately soluble | 61.69 | 2 violations: MW > 500, MLOGP > 4.15 | 0.17 | 1.07 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Merlani, M.; Nadaraia, N.; Amiranashvili, L.; Petrou, A.; Geronikaki, A.; Ciric, A.; Glamoclija, J.; Carevic, T.; Sokovic, M. Antimicrobial Activity of Some Steroidal Hydrazones. Molecules 2023, 28, 1167. https://doi.org/10.3390/molecules28031167
Merlani M, Nadaraia N, Amiranashvili L, Petrou A, Geronikaki A, Ciric A, Glamoclija J, Carevic T, Sokovic M. Antimicrobial Activity of Some Steroidal Hydrazones. Molecules. 2023; 28(3):1167. https://doi.org/10.3390/molecules28031167
Chicago/Turabian StyleMerlani, Maia, Nanuli Nadaraia, Lela Amiranashvili, Anthi Petrou, Athina Geronikaki, Ana Ciric, Jasmina Glamoclija, Tamara Carevic, and Marina Sokovic. 2023. "Antimicrobial Activity of Some Steroidal Hydrazones" Molecules 28, no. 3: 1167. https://doi.org/10.3390/molecules28031167
APA StyleMerlani, M., Nadaraia, N., Amiranashvili, L., Petrou, A., Geronikaki, A., Ciric, A., Glamoclija, J., Carevic, T., & Sokovic, M. (2023). Antimicrobial Activity of Some Steroidal Hydrazones. Molecules, 28(3), 1167. https://doi.org/10.3390/molecules28031167







